Living with bipolar ii
Living With Bipolar Disorder - What is Bipolar Disorder?
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
With proper treatment, along with support and self-care, people with bipolar disorder can live healthy, fulfilling lives.On this page:
-
A person who has bipolar disorder also experiences changes in their energy, thinking, behavior, and sleep. During bipolar mood swings, it is difficult to carry out day-to-day tasks, work, go to school, and maintain relationships.
When a person has a manic episode, they feel overly excited, productive, and even invincible. These drastic behavior changes usually cause concern among friends and family. On the other hand, when a person has a depressive episode, they feel extremely sad, hopeless, and tired. They may avoid friends, family, and participating in their usual activities.
-
Video: Living With Bipolar Disorder
Learn about Phil's experience with bipolar disorder.
-
A severe manic or depressive episode may trigger psychotic symptoms such as delusions (false beliefs) or hallucinations (seeing or hearing things that others do not see or hear).
Tips for Living with Bipolar Disorder
Bipolar disorder is a lifelong condition that doesn’t go away on its own. While it can feel overwhelming and isolating at first, an early, accurate diagnosis is the first step toward getting better. Proper treatment, along with support and self-care, helps people with bipolar disorder live healthy, fulfilling lives.
Treatment Options
Bipolar disorder is treatable with a combination of medication and therapy.

- Medications. Mood stabilizers, antipsychotics, and antidepressants can help manage mood swings and other symptoms. It is important to understand the benefits and risks of medications. People may need to try different medications before determining which works best for them. They should never stop taking a medication without their doctor’s guidance.
- “Talk therapy” (psychotherapy). Therapy helps people accept their disorder, recognize the warning signs of a manic or depressive episode, develop coping skills for handling stress, and stick with a medication schedule. Therapy also improves communication and relationships among families.
- Long-term, continuous treatment. While there may be times between episodes where a person feels fine, a long-term, continuous treatment plan can reduce the severity and frequency of mood swings.
What You Can Do: Daily Habits Make a Difference
These healthy lifestyle habits, along with professional treatment, can help manage the symptoms of bipolar disorder:
- Stick to a consistent routine.
 Go to sleep and wake up at the same time each day. Being sleep deprived can put people at risk for manic or depressive episodes. Sleeping more than usual may be a sign of a depressive episode. Limit caffeine, which can disrupt sleep.
Go to sleep and wake up at the same time each day. Being sleep deprived can put people at risk for manic or depressive episodes. Sleeping more than usual may be a sign of a depressive episode. Limit caffeine, which can disrupt sleep. - Eat well and get regular exercise. A healthy diet will give your body proper nutrition, and exercise may help improve your mood.
- Always take your medicine as prescribed. You should do this even when your mood is stable.
- Check with your treating doctor. Always check before taking over-the-counter supplements or any medications prescribed by another doctor.
- Keep a mood journal. By tracking how you feel day-to-day, you can notice triggers, monitor how your treatment is working, and spot changes in your eating or sleeping patterns. Writing down this information can be especially helpful to your doctor if your medication needs to be adjusted.

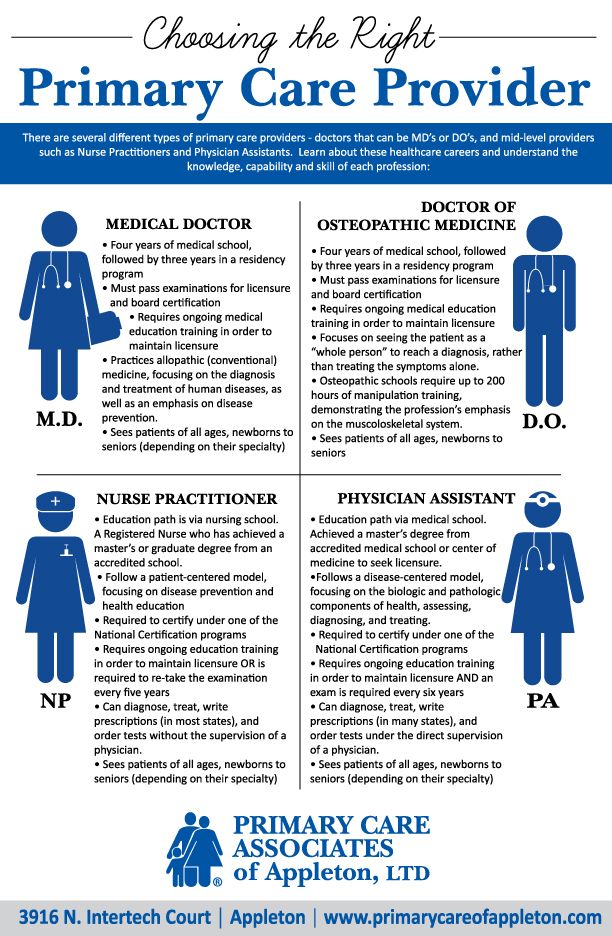
- Keep your primary care physician updated. They are an important part of the long-term management of bipolar disorder, even if you also see a psychiatrist.
- Avoid using alcohol and illegal drugs.
- Minimize stress. Try activities like meditation or tai chi. Make changes to simplify your life when possible.
- Turn to a support network. Know which family and friends are there to help during a crisis or a tough time. Educate your loved ones about bipolar disorder so they can best support you. Ask them to help you recognize the warning signs of manic or depressive episodes.
-
References and Relevant Resources
- 2019 National Survey on Drug Use and Health | Substance Abuse and Mental Health Services Administration (SAMHSA)
- Addressing Mental Illness and Substance Use as a Young Adults | SAMHSA
- Co-Occurring Disorders: Diagnoses and Integrated Treatments | SAMHSA
- Helping Families: Resources for Mental and Substance Use Disorders | SAMHSA
- Preventing Suicide | SAMHSA
- Bipolar Disorder | National Institute of Mental Health (NIMH)
- The Diagnosis and Treatment of Bipolar Disorder: Decision-Making in Primary Care | The Primary Care Companion for CNS Disorders
- Bipolar Disorder | Mayo Clinic
- Interdepartmental Serious Mental Illness Coordinating Committee (ISMICC) | SAMHSA
- SMI Adviser | American Psychological Association (APA) and SAMHSA
- Technology Transfer Centers (TTC) Program | SAMHSA
Last Updated: 09/27/2022
Symptoms, Causes, Diagnosis, and Treatment
Bipolar 2 disorder means you experience periods of hypomania. Hypomania is a temporary surge in emotions, energy levels, self-esteem, and drive. This is followed by periods of deep depression.
Hypomania is a temporary surge in emotions, energy levels, self-esteem, and drive. This is followed by periods of deep depression.
Learning how to live with a mental health diagnosis can be like beginning an entirely new life. Now that you know you have bipolar disorder 2, you can:
- learn what to expect from this condition
- plan how you’ll respond to changes in your health
- discover systems of support
- practice habits to help you create a greater sense of balance
- fine-tune your treatment plan so it works for you
Here’s a good starting place: a quick primer on this condition and science-backed strategies for a healthier life.
Having bipolar 2 disorder means you experience periods of hypomania, during which you have a temporary surge in emotions, energy levels, self-esteem, and drive. These bursts of feeling, motivation, and activity are followed by periods of deep depression, when your feelings may be overwhelmingly dark — if you have any feelings at all. During an episode of depression, it can be tough just to get on your feet in the morning.
During an episode of depression, it can be tough just to get on your feet in the morning.
Though your highs may not be as extreme as those with bipolar disorder 1, these cycles can nevertheless be damaging to your self-concept, your finances, your career, and your relationships.
As you might expect, symptoms look very different depending on whether you’re in a period of hypomania or a period of depression.
Here’s what hypomania symptoms can look like:
- feeling elated or high
- feeling jittery, restless, or irritable
- tackling a large number of projects at the same time
- tumbling, racing thoughts
- speaking with haste
- behaving recklessly with money or sex
- staying up all night without feeling exhausted
Here’s what depression symptoms can look like:
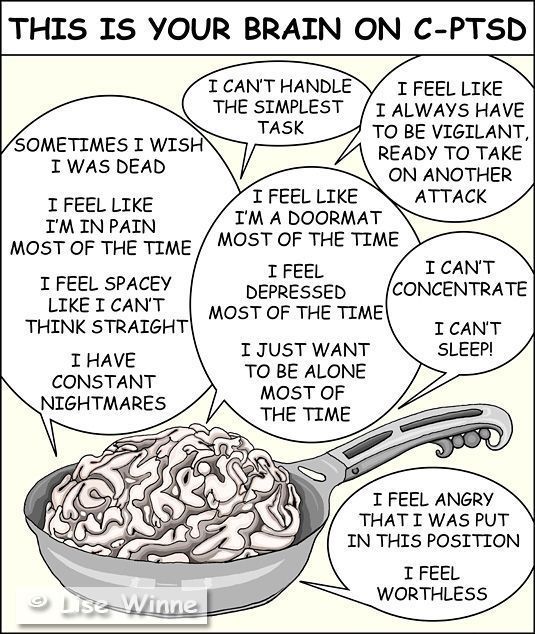
- feeling numb, drained, or “dead” inside
- feeling sorrowful, sad, or hopeless
- having trouble falling asleep or waking up
- sleeping at times of the day when you’re usually active
- losing pleasure in things you usually enjoy, including sex
- losing the ability to focus or concentrate
- having little desire to speak, or speaking slowly
- feeling little or no motivation to act
It’s possible that you could have mixed symptoms in one episode—for example, feeling anxious and jittery, while also feeling unmotivated and drained. How long periods of depression or hypomania last varies from person to person.
How long periods of depression or hypomania last varies from person to person.
People with BPD 2 describe living with the disorder like this:
When I am having an episode of hypomania, I:
- feel as though I don’t need sleep.
- have so many ideas it’s impossible to act on them all.
- talk so fast other people can hardly keep up.
- feel unconquerable, ecstatic, powerful, completely unique.
- drain my bank account.
- complete huge projects in short periods.
- create things feverishly.
- stop eating or eat just enough to keep going.
- sometimes do risky things like having sex with strangers.
- sometimes believe I am hearing directly from God.
When I am having an episode of depression, I:
- can feel lost and invisible.
- cannot seem to find the words to say what’s going on.
- sleep so much — but never feel rested.
- lose all motivation and passion for living,
- can’t seem to do things I know I should do.

- crave unhealthy food.
- eat to try and feel better.
- hide from the people in my life.
- stop performing with my usual vigor at work or school.
- have trouble concentrating.
- feel like a failure.
- am convinced things are hopeless.
- sometimes feel like folding up and dying.
Exactly how you experience the practical and emotional effects of bipolar disorder 2 will be unique to you, but you may recognize some or all of the above effects.
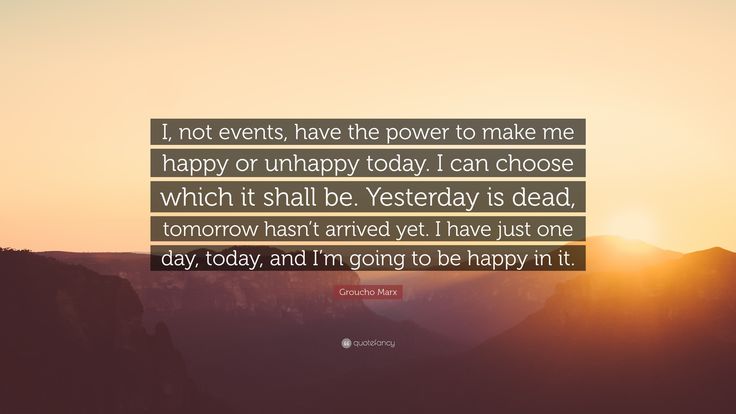
Living with bipolar disorder 2 isn’t just about participating in therapy and taking medication. There are many other ways that you can work toward a more balanced, healthy life.
Become an active part of your treatment team
Bipolar disorder 2 generally requires a combination of medication and therapy for the best results. While your doctor will recommend and prescribe medications and your therapist will guide your therapy sessions, you are an expert on what you’re experiencing. And you can become an expert on bipolar disorder 2 in time.
And you can become an expert on bipolar disorder 2 in time.
To help your treatment team with your care, you can read up on the disorder yourself. Equipped with science-supported information on available treatment, accounts from other people about what they’ve experienced, and what to look for when an episode of hypomania or depression is on the horizon, you’ll be ready to help create a wellness plan that works for you.
What to read if you need more than words
These graphic memoirs capture what it’s like to live with bipolar disorder 2 and some of the other mental health conditions commonly diagnosed at the same time. The combination of art and story may be more telling than words alone.
- Rx by Rachel Lindsay
- Marbles: Mania, Depression, Michaelangelo, and Me by Ellen Forney
- Hyperbole and a Half by Allie Brosh
- Lighter Than My Shadow by Katie Green
Monitor your moods, symptoms, and triggers
Managing a condition like bipolar disorder 2 is not a one-and-done situation. Over time, you will go through periods where stressors in your life, changes in your body, and many other variables will alter how effective your treatment plan is.
Over time, you will go through periods where stressors in your life, changes in your body, and many other variables will alter how effective your treatment plan is.
If you develop a practice of kind and respectful self-monitoring, you may be able to keep symptoms from escalating into a full-blown hypomanic or depressive episode. Here are a few areas to watch:
- Keep track of your feelings. You can use a journal, a mood chart or calendar, an app, or any other method that allows you to take a frequent inventory of your emotions. What are you looking for? Any change in your mood or outlook that feels like a familiar sign of a mood shift. Electronic and digital methods of tracking mood are also increasingly being researched. While there’s no evidence yet that these methods prevent an episode, people do seem to use them faithfully and the apps are valid measures of changing symptoms.
- Notice changes in your desires and habits. Healthy routines, schedules, and structures may feel unfamiliar at first, but they are a key part of maintaining your mental health.
 When desires and habits start to change, it can be an early indicator of a brewing mood shift. You may notice, for example, that you no longer feel like cooking or exercising long before you notice any change in your emotions.
When desires and habits start to change, it can be an early indicator of a brewing mood shift. You may notice, for example, that you no longer feel like cooking or exercising long before you notice any change in your emotions.
- Anticipate your triggers. In time, you may come to recognize that certain kinds of life events — loss of sleep, financial stress, relationship conflicts, or traumatic experiences — can make it more likely that you’ll have a relapse. In a recent study involving people who had experienced a relapse of bipolar symptoms, nearly 70 percent had gone through a stressful life event in the days just before the relapse. Knowing these triggers in advance may help you take extra care of yourself or reach out for extra support at critical times.
- Consider interpersonal and social rhythm therapy (IPSRT). IPSRT equips you with skills to help you maintain the daily routines that protect you from escalating episodes, including sleep schedules, taking your medications daily, sticking to healthy eating and exercise patterns, and responding to stressful situations in healthy ways.
 Studies show that IPSRT reduces anxiety, hypomania, and depression symptoms in people with bipolar disorder.
Studies show that IPSRT reduces anxiety, hypomania, and depression symptoms in people with bipolar disorder.
Create an action plan for when symptoms change
There’s always the possibility that you’ll have breakthrough symptoms or a relapse at some point in your life. If you’ve made a plan to guide how you and those around you will respond, you may be able to minimize the disruption and quickly get the help you need.
The National Alliance on Mental Illness (NAMI) suggests that your plan include these items:
- names and contact information for your healthcare team, including your primary care doctor, psychiatrist, therapist, and any other healthcare professionals you need
- names and contact information for key family members you trust
- phone numbers for local crisis centers and healthcare facilities near you, especially those with respected mental health centers
- a list of your medications and any allergies you may have
- a brief timeline of any other mental health crises, hospitalizations, or suicide attempts
- information about your triggers, special needs, and what has helped in the past
Some people decide to include a psychiatric advance directive, which is a legal document that names a person to make decisions on your behalf if you’re not in a position to make them.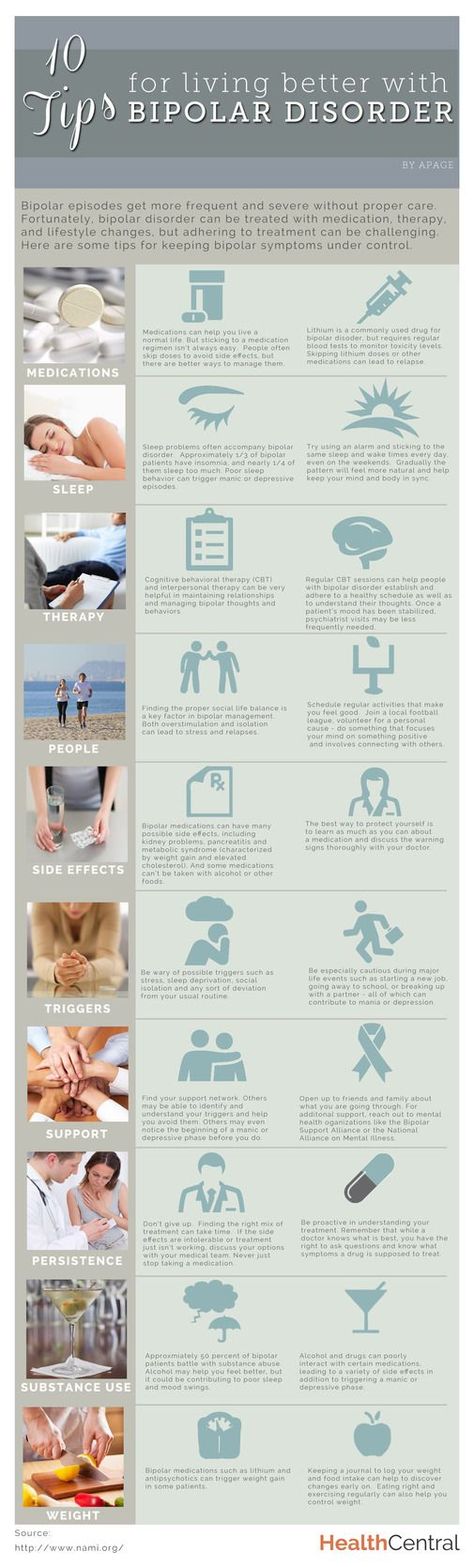
It’s a good idea to let the people you trust know that the plan exists and where they can read it if necessary. You may also want to keep copies of the plan in several easy-to-find locations in your home, as well as in your vehicle and on your phone.
Develop a Wellness Recovery Action Plan (WRAP)
Because healthy routines are so important for maintaining wellness and preventing a crisis, you may want to create a WRAP. They typically include:
- a brief description of what you and your life look like when you are healthy
- an inventory of your wellness tools: people, routines, and resources you need to keep symptoms in check and keep your treatment plan active
- a list of your triggers
- a list of early warning signs that could mean you’re headed for a hypomania or depression episode
- problem-solving strategies, including a list of people you trust to help you devise solutions
- indications that you are in a mental health crisis and need help
Studies show that WRAP plans, especially those that include problem-solving interventions, can help you feel prepared for recovery.
Stay connected to people who support you
When you are not feeling your best, it can be tempting to withdraw from the people who know you and care about your wellbeing. You may start to miss appointments with your therapist or physician. You may skip social events that usually appeal to you. You may avoid conversations with people who can help you.
Studies show that having positive social support can make it easier for you to cope with and manage your emotions. Supportive relationships can also build your resilience during times of recovery.
It’s a good idea to develop a wide, diverse support network. You could connect with professionals in the mental health community, local or virtual support groups, people in volunteer organizations, civic groups, or faith communities, colleagues, family, and friends. At different times, these connections may be able to support in a variety of ways — reminding you that you are much, much more than a diagnosis.
Take good care of your physical health
The health of your body and the health of your mind are related.
- Rest. One of the most important areas to safeguard is your sleep patterns. Research is clear: Loss of sleep can trigger episodes of hypomania and depression. For a closer look at sleep and its effects on bipolar disorder, go here.
- Move. Another important health habit to cultivate is physical exercise. Vigorous physical activity can elevate your mood, relieve depression and hypomania symptoms, and help you sleep better at night.
- Eat well. Your body and mind are more likely to thrive if you’re eating nutritious foods regularly. Researchers say a healthy diet can help lower the risk of mental health problems and improve treatment outcomes for people with bipolar disorder.
Bipolar 2 can be diagnosed by a doctor, psychiatrist, psychiatric nurse, or psychologist. To arrive at a diagnosis, a healthcare professional will ask you about your symptoms and how they affect your life. You’ll also be asked about your family’s medical and mental health history. Your doctor may give you a blood test to rule out other conditions that could destabilize your moods.
Your doctor may give you a blood test to rule out other conditions that could destabilize your moods.
An official diagnosis of bipolar 2 requires that you have experienced at least one episode of hypomania and at least one major depressive episode. The episodes must have significantly disrupted your ability to function. You can find a guide to bipolar disorder diagnosis here.
Bipolar 2 is most often treated with a combination of medication and psychotherapy. Medications could include:
- mood stabilizers
- atypical antipsychotics
- anxiety medications
- medications to help you sleep
The types of psychotherapy most helpful in treating bipolar 2 include:
- interpersonal social rhythm therapy
- cognitive behavioral therapy
- family-focused therapy
- dialectical behavior therapy
- group therapy
How to help someone with bipolar 2
In a 2016 study that examined the unmet needs of people with bipolar disorder, researchers said people in a depression episode most need:
- help to recognize that they’re in a depression period
- encouragement to follow through on treatment
- acceptance, tolerance, and empathy
People with bipolar disorder are likely to feel worried about relapse, fearful of the stigma, and guilty about the impacts the disorder has on other people. As a family member, you also experience considerable stress because of the practical ways the disorder affects everyone in the family. For some people, family therapy may be a good option for increasing support and resolving conflicts.
As a family member, you also experience considerable stress because of the practical ways the disorder affects everyone in the family. For some people, family therapy may be a good option for increasing support and resolving conflicts.
Bipolar disorder is not curable, but treatment can be effective in managing symptoms. If you follow your treatment plan and take care of yourself, you may go for long periods where you have few or no symptoms and your moods are stable. That’s not the case for everyone, of course — some people may have symptoms even when they carefully follow a treatment plan.
Without treatment, the picture looks different. People with untreated bipolar disorder are more likely to have severe mood shifts, and they may be at greater risk of harming themselves.
If you or someone in your life has been diagnosed with bipolar disorder 2, you’re embarking on a new course: one that could help you even out some of the highs and lows that have disrupted your life.
The hypomania and depression that have made your life so hard can be managed with medication, therapy, support, and healthier habits.
It will take time to get your treatment plan in place, and you may need to tweak it from time to time as your body, mind, and life go through changes. But bipolar disorder 2 can usually be treated successfully, and you can find your way to more balanced mental and physical health.
How to live with bipolar disorder | Chita.ru
Manic-depressive psychosis, or simply bipolar: under such names, the people know the disorder, which affects an average of five to eight people out of a thousand. There are many myths about him, including quite ridiculous ones.
On Bipolar Affective Disorder Awareness Day, March 30, journalist Yekaterina Bormotova told E1.RU how to live with this diagnosis.
A few years ago, I was diagnosed with a “fashionable” then already diagnosis - F31. Translated from medical into Russian, this means "bipolar affective disorder. " Many thanks to the doctors for choosing such a pleasant term for the name of my illness, because earlier, back in Soviet times, it was called "manic-depressive psychosis" - you must admit, it's scary.
" Many thanks to the doctors for choosing such a pleasant term for the name of my illness, because earlier, back in Soviet times, it was called "manic-depressive psychosis" - you must admit, it's scary.
But the pleasant term also has a downside: few people take the illness with that name seriously. “Manic-depressive psychosis” sounds impressive, and bipolar is something about teenagers who have not decided on their mood. At least that's how it is perceived by many. And it didn't help at all when I was diagnosed. Not at all.
I was 27 when I first came to the regional psychiatric hospital. She called an ambulance herself: I was at home alone and felt that now I can do something with myself. My consciousness seemed to split in two: some part of me wanted to end this life, but the other part understood that it should not do this. It's very scary. Imagine that you are locked in a room with a killer and must persuade him not to kill you. Now imagine that this room is your mind and the killer is you.
By that time I had already seen a psychiatrist, the doctor thought that I had a recurrent depressive disorder. He was partly right: depression is part of bipolar. But the second part of it is mania.
People often don't understand the difference between depression and bad mood. I have a simple explanation: depression is running in water. You do everything that you do on land, you strain your muscles in the same way, you apply the same efforts, but because of the resistance of the water you cannot get the same result. To follow this analogy, mania is weightlessness. Your efforts are not hindered by gravity, you barely push off the ground and fly, not run.
“It's a nice feeling, but if you wanted to run from point A to point B, then hovering over the surface is not quite the desired result,” Ekaterina Bormotova.
Movie and book protagonists usually say, "I always knew there was something wrong with me." I never thought so. I was convinced that all people live and feel the same way as I do, they are just stronger and cope, and I always do some stupid things and spoil everything. Even in our youth, my future husband said that I needed to see a psychologist. Of course, I didn't think so. Later, when we got married, he started talking about a psychiatrist, but I was convinced that everything was fine with me.
Even in our youth, my future husband said that I needed to see a psychologist. Of course, I didn't think so. Later, when we got married, he started talking about a psychiatrist, but I was convinced that everything was fine with me.
In the end, I went to the doctor only after the divorce, and he found that I was depressed. And a year and a half later, they brought me to the eighth kilometer (Siberian tract, the address of the psychiatric hospital - ed.) .
There were about 20 people in the hospital room. No bedside tables, no TV, no flowers on the windows - only beds with white sheets, I was wearing a hospital nightgown, a toothbrush and slippers from personal things. This is called the "observation chamber", newcomers enter there. It sounds creepy, but when you realize that the alternative is death, the choice is obvious. Then those who are not dangerous for themselves and others are transferred to other wards, where you can already have personal belongings, but you still can’t use the phone or, for example, embroider.
The number of suicides in Russia and the world is decreasing every year, but still remains at a high level
Photo: Infographic: Vitaly Kalistratov / City Portal Network
Share
I left the hospital after a month and a half and told about my illness on social networks. I know some people thought it was overkill, and some people thought I was a hero for coming out with an open face, but let's be honest, I had no choice. At work, they knew what hospital I ended up in, and the journalistic community is compact, one way or another people would know that I was in a madhouse. It was easier to tell myself than to catch meaningful looks and fight rumors when I wanted to change jobs.
Then a new life began. Because of one of the drugs, I gained 20 kg, slept 16 hours a day and did not want to leave the house. I was lucky that I could work remotely, my parents supported me, but even so I was forced to get into debt. I can’t imagine how people with my diagnosis cope with work at this stage, it’s very difficult: due to antipsychotics, absent-mindedness appears, cognitive functions weaken, and communication skills are lost.
I can’t imagine how people with my diagnosis cope with work at this stage, it’s very difficult: due to antipsychotics, absent-mindedness appears, cognitive functions weaken, and communication skills are lost.
“To put it simply, you become very stupid, slow and withdrawn,” Ekaterina Bormotova.
Books and films about bipolar often reveal the problem of accepting treatment - many people find it difficult to come to terms with the fact that they will have to take drugs for the rest of their lives, which also cause side effects. But they don't say anything about losing yourself. Here you live for 27 years and think that certain character traits are characteristic of you, and then you find out that, perhaps, these are not character traits, but a disease.
How to understand where you end and the disease begins? How to understand that it was you who wanted to hitchhike, get a cat, move to another city or get married, and not sick thoughts influenced your decisions? Do you love Aivazovsky in general, or did you just see his canvas in mania, when all feelings are aggravated to the limit? I am in several patient communities, and this is what really worries a lot of people.
Being a person with bipolar disorder is not as hard as living next to such a person
Photo: Illustration: Yuri Orlov / City Portal Network
Share
There is good news: you can live with it. Over time, the body gets used to the drugs and ceases to give very harsh side effects. Some drugs are a thing of the past and are used only during periods of exacerbations, some doctors find a replacement if they complain about unpleasant effects. They picked up a good working scheme for me, with which I can live a full life: work, communicate with people, help loved ones. But, of course, there are exacerbations.
An aggravation does not start all at once, it develops over several days or weeks. It is very important to notice this at the very beginning, otherwise there will be problems - from quarrels with loved ones to losing a job and debts. Debts... Damn money in mania is spent like it's not yours. Even before I was diagnosed, I had to mess with it terribly. You know, I would forbid giving people loans without an examination by a psychiatrist. At the very least, it would save me from a number of problems. Fortunately, I never had large sums or property, so I lost a little.
Even before I was diagnosed, I had to mess with it terribly. You know, I would forbid giving people loans without an examination by a psychiatrist. At the very least, it would save me from a number of problems. Fortunately, I never had large sums or property, so I lost a little.
“Nevertheless, it's a shame to realize that the money I lost due to exacerbations would have been enough for at least the first installment on the mortgage,” Ekaterina Bormotova.
In exacerbations, I offended people, made people fall in love with me, let people down, destroyed important connections, made new dubious ones, behaved disgustingly and defiantly, did things that I regret very much and will regret all my life. And I don't want that ever again. If for this you need to take pills for life, I'm ready.
I am very lucky to have close people. Almost no one abandoned me after I told about my diagnosis, although I know that many patients experience this. It was a little difficult to explain to some close people why I agreed to the treatment - they told me: “You don’t need it, I know you, everything is fine with you, you are normal. ” Relatives and friends often persuade patients to stop taking medications, because with the drugs they become “strangers”. But it's not. I am convinced that with treatment we do not lose ourselves, we find ourselves. It just takes time sometimes. Sometimes this time is measured in years.
” Relatives and friends often persuade patients to stop taking medications, because with the drugs they become “strangers”. But it's not. I am convinced that with treatment we do not lose ourselves, we find ourselves. It just takes time sometimes. Sometimes this time is measured in years.
I think that being a person with bipolar disorder is not as difficult as living with such a person. My loved ones are forced to constantly remember that my behavior may be due to illness. My mother often asks questions that can annoy an adult. I say that I fell in love, baked a cake or hung out at a bar until five in the morning, and I see wariness in her eyes: she is afraid that this is mania, which will invariably be followed by depression. I understand why she is worried. And I am eternally grateful to her for not talking about it. Well, he says, but at least not very often.
People with my diagnosis are forced not only to take pills, but also to keep diaries and follow their every sneeze in order to track the slightest mood swings. It's tiring. But even more tiring external supervision. I think people with bipolar really only need two things: medication and for everyone to get off of it. Oh, and psychotherapy. It is necessary to figure out who still loved Aivazovsky: you or your illness.
It's tiring. But even more tiring external supervision. I think people with bipolar really only need two things: medication and for everyone to get off of it. Oh, and psychotherapy. It is necessary to figure out who still loved Aivazovsky: you or your illness.
Earlier E1.RU published the story of a girl with bipolar disorder. Read an interview with a psychiatrist about how to spot possible disorders in a teenager in time.
From heaven to hell and back: a psychiatrist about bipolar disorder
04/26/2021
Recently, there has been a lot of talk about bipolar disorder, and even more information on the Internet. But, as many of us have seen, it is impossible to believe everything that is in free sources. With the same goal of preventing confusion in our heads, there is an interview with Lyubov Viktorovna Bekeneva, a psychiatrist, head of the male department of the Yakut Republican Psychoneurological Dispensary, Candidate of Medical Sciences, Associate Professor of the Department of Neurology and Psychiatry of the NEFU Medical Institute, and we will start it with a story about the patient :
“A bright, spectacular man, a Yakutian, the owner of a large manufacturing company, he was always successful. Everything seemed to come easy to him. On the day when he flew away on a working visit abroad, and only after getting off the plane, he began to sign contract after contract, assuming multimillion-dollar obligations - no one suspected something strange. After all, he is an entrepreneur with considerable experience ... I wanted to celebrate. Vasily Emelyanovich bought tickets from Yakutsk to "abroad" for his wife and mother, he was waiting for them with great impatience and a sense of pride in the successful transactions. He arrived at the airport in a limousine, with a large bouquet of scarlet roses at the ready, eager to meet his mother and wife right at the plane. Seeing his son, a storm of emotions swept over his mother: “What happened to Vasya? .. Did the same thing happen to him as to Anna, my sister?”
- Bipolar affective disorder is diagnosed most often in people who have a hereditary predisposition to this disease - says Lyubov Viktorovna - external factors, such as living conditions or injuries, neurological diseases, cannot cause the development of bipolar disorder. However, judging by statistics, a child from a mother with bipolar disorder will inherit the disease only in 25% of cases, and if both parents suffer from endogenous diseases, the probability increases by 50%. It is impossible to predict with 100% accuracy whether a child will be sick. As we observe in the case of the patient from history, his mother's sister had the disease, and it was reflected only in Vasily, her nephew.
However, judging by statistics, a child from a mother with bipolar disorder will inherit the disease only in 25% of cases, and if both parents suffer from endogenous diseases, the probability increases by 50%. It is impossible to predict with 100% accuracy whether a child will be sick. As we observe in the case of the patient from history, his mother's sister had the disease, and it was reflected only in Vasily, her nephew.
- What is the average age of patients with bipolar disorder?
- As a rule, the disease is diagnosed in young people, aged approaching 30 years and up to 40 years. Very rare cases when the disease is detected later or earlier than this age.
- What does a patient with bipolar disorder look like?
- The name of the diagnosis speaks for itself - it is a disease that causes polar mood disorders, that is, two completely different conditions. In general terms, the disease can be described as follows: it has two stages - mania and depression.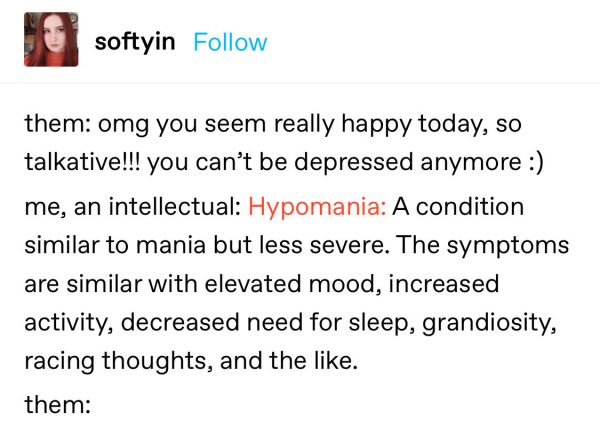 During the period of mania, the patient comes up with ideas of a different nature, including delusional ones, which he tries to translate into reality, no matter what it costs him. In such an excited state, a person becomes very sociable, energetic, tireless. With all its activity, from the side it may seem that a person does not get tired at all. Sleep is disturbed at the same time - people with BAD can sleep for three hours a day, and this will be enough for them to radiate energy and work again the next day. Their speech is very fast, loud, the topic of conversation jumps from one to another, their movements are sharp, during the dialogue they can grab furniture, shift household items from place to place. An episode of mania is followed by a deep, devastating depression, often with suicidal thoughts.
During the period of mania, the patient comes up with ideas of a different nature, including delusional ones, which he tries to translate into reality, no matter what it costs him. In such an excited state, a person becomes very sociable, energetic, tireless. With all its activity, from the side it may seem that a person does not get tired at all. Sleep is disturbed at the same time - people with BAD can sleep for three hours a day, and this will be enough for them to radiate energy and work again the next day. Their speech is very fast, loud, the topic of conversation jumps from one to another, their movements are sharp, during the dialogue they can grab furniture, shift household items from place to place. An episode of mania is followed by a deep, devastating depression, often with suicidal thoughts.
- What can a state of mania be compared to?
- A description of the state of mild alcohol intoxication, a feeling of euphoria, when it seems that everything is possible, is more suitable.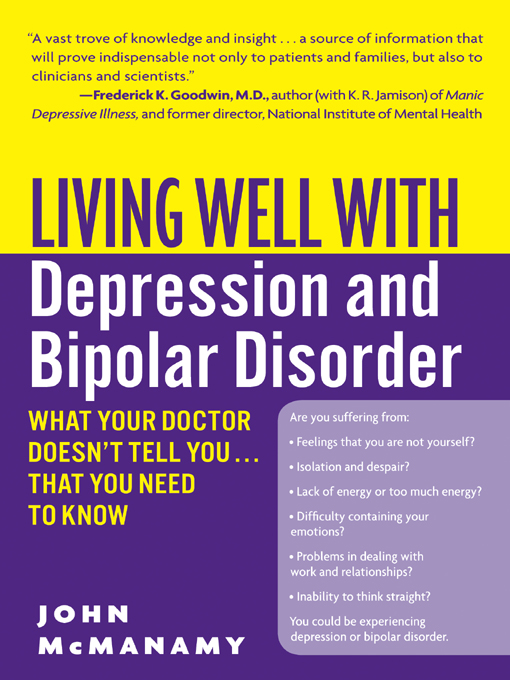 The state of mania is the same in men and women, both sexes feel the same, but among patients with bipolar disorder there are still more females. The state of mania does not begin at once - this is preceded by a state of hypomania, lasting about a month: a person becomes more productive, performs work instead of the usual weekly period - for example, in four days. Further, psychomotor arousal is on the rise: a business that requires work for a month is completed in a week. So a person enters a state of mania, the time to make a decision is rapidly declining, common sense leaves the patient, uncontrollable mania begins, rash acts. The state of mania, furious unrestrained activity, can last about three to four months.
The state of mania is the same in men and women, both sexes feel the same, but among patients with bipolar disorder there are still more females. The state of mania does not begin at once - this is preceded by a state of hypomania, lasting about a month: a person becomes more productive, performs work instead of the usual weekly period - for example, in four days. Further, psychomotor arousal is on the rise: a business that requires work for a month is completed in a week. So a person enters a state of mania, the time to make a decision is rapidly declining, common sense leaves the patient, uncontrollable mania begins, rash acts. The state of mania, furious unrestrained activity, can last about three to four months.
- Are there more cases over time?
- Not. The figures remain at the same level - 1% of the total world population.
- How do people with such a diagnosis live, is it possible to recover from bipolar disorder?
- The exit from the state of bipolar affective disorder also passes gradually, and what is interesting is that those symptoms that appeared last go away first, and what began to bother at the very beginning of mania, for example, sleep disturbance, go last. In the treatment of patients with bipolar disorder, drugs are used that normalize the condition, designed to prevent the transition to a state of mania and subsequent depression. The therapy continues throughout life. Of course, the removal of an acute condition takes place in a hospital. It is impossible for a person in mania to prove his illness, in no way, the persuasion of relatives, relatives and friends does not work here. On average, an acute condition requires a hospital stay of two months. When a patient re-admits, the person already remembers his past condition, and in order to prevent it from happening again, he goes to the hospital with less pronounced symptoms of bipolar disorder, each patient has 1-3 such visits for the entire period after diagnosis, most of the time patients take drugs on an outpatient basis under the supervision of the attending psychiatrist, the need for hospitalization rarely occurs. Intermission is the name of the state in which a patient is treated for bipolar disorder, there are no breakdowns, transitions to mania and back, a person lives calmly, like all ordinary people for years, sometimes even decades.
In the treatment of patients with bipolar disorder, drugs are used that normalize the condition, designed to prevent the transition to a state of mania and subsequent depression. The therapy continues throughout life. Of course, the removal of an acute condition takes place in a hospital. It is impossible for a person in mania to prove his illness, in no way, the persuasion of relatives, relatives and friends does not work here. On average, an acute condition requires a hospital stay of two months. When a patient re-admits, the person already remembers his past condition, and in order to prevent it from happening again, he goes to the hospital with less pronounced symptoms of bipolar disorder, each patient has 1-3 such visits for the entire period after diagnosis, most of the time patients take drugs on an outpatient basis under the supervision of the attending psychiatrist, the need for hospitalization rarely occurs. Intermission is the name of the state in which a patient is treated for bipolar disorder, there are no breakdowns, transitions to mania and back, a person lives calmly, like all ordinary people for years, sometimes even decades.
I note that the most terrible consequences of depression are in patients with bipolar disorder, the stage of depression is often accompanied by suicide attempts, and in most cases such patients bring the decision to the end. In the depressive phase, the patient feels lethargic, apathetic and spends most of the time lying down, showing no interest in anything. Elderly patients who continue treatment for more than a dozen years need the help of their relatives, they are unable to control their condition on their own, and if a person in a depressive episode is not hospitalized, this can turn into a fatal outcome. In my practice, unfortunately, there was a case of indifference of children to the parent - the mother entered a state of depression, and did not get out of it - she had no strength left, bipolar affective disorder destroyed the body, bringing it to complete exhaustion.
- Does it happen that a patient or his relatives suspect bipolar disorder and go to a dispensary?
-Yes, it happens. Basically, people confuse bipolar disorder with cyclothymia, this disease is much easier and does not require hospital treatment. With cyclothymia, mood swings are milder - a person is in hypomania and mild depression. This state is often inherent in people of creative professions, who are easily carried away by new things, but also quickly lose interest. Bipolar affective disorder, as already mentioned, has much more severe symptoms and consequences.
Basically, people confuse bipolar disorder with cyclothymia, this disease is much easier and does not require hospital treatment. With cyclothymia, mood swings are milder - a person is in hypomania and mild depression. This state is often inherent in people of creative professions, who are easily carried away by new things, but also quickly lose interest. Bipolar affective disorder, as already mentioned, has much more severe symptoms and consequences.
- And in conclusion, can I give you some advice on what to do if you feel that your psyche is failing?
- Do not be afraid to go to a psychiatrist for help. This is not a sign of weakness. If you or your loved one needs the help of a psychiatrist, please contact the receptionist of the polyclinic of our Yakut Republican Psychoneurological Dispensary at Lermontov 178/1, telephone 507-899. Assistance is provided free of charge, under the CHI policy. The sooner you begin treatment, the sooner the depressing, life-threatening condition will begin to leave you.