Lithium and naproxen
The clinical significance of lithium-nonsteroidal anti-inflammatory drug interactions
Save citation to file
Format: Summary (text)PubMedPMIDAbstract (text)CSV
Add to Collections
- Create a new collection
- Add to an existing collection
Name your collection:
Name must be less than 100 characters
Choose a collection:
Unable to load your collection due to an error
Please try again
Add to My Bibliography
- My Bibliography
Unable to load your delegates due to an error
Please try again
Your saved search
Name of saved search:
Search terms:
Test search terms
Email: (change)
Which day? The first SundayThe first MondayThe first TuesdayThe first WednesdayThe first ThursdayThe first FridayThe first SaturdayThe first dayThe first weekday
Which day? SundayMondayTuesdayWednesdayThursdayFridaySaturday
Report format: SummarySummary (text)AbstractAbstract (text)PubMed
Send at most: 1 item5 items10 items20 items50 items100 items200 items
Send even when there aren't any new results
Optional text in email:
Create a file for external citation management software
Review
. 1990 Oct;10(5):350-4.
M Ragheb 1
Affiliations
Affiliation
- 1 Carl T. Hayden Veterans Administration Medical Center, Phoenix, Arizona 85012.
- PMID: 2258452
Review
M Ragheb. J Clin Psychopharmacol. 1990 Oct.
. 1990 Oct;10(5):350-4.
Author
M Ragheb 1
Affiliation
- 1 Carl T. Hayden Veterans Administration Medical Center, Phoenix, Arizona 85012.
- PMID: 2258452
Abstract
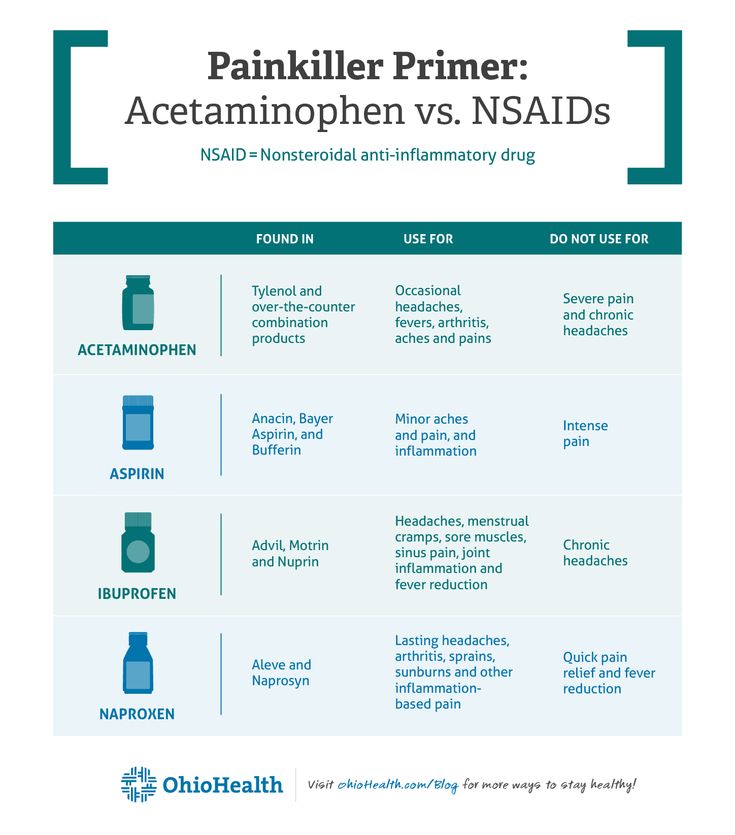
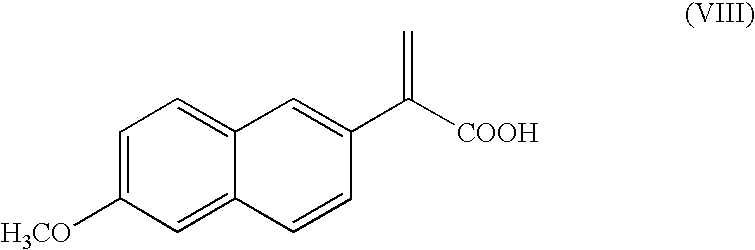
There is conclusive evidence that nonsteroidal anti-inflammatory drugs can increase serum lithium levels, diminish renal lithium clearance, and possibly induce lithium toxicity. Such an interaction has occurred in patients with normal renal function. The effect on serum lithium levels varies greatly among different nonsteroidal anti-inflammatory drugs, indomethacin seeming most potent. On the other hand, there is no convincing evidence that sulindac and aspirin affect serum lithium levels to a clinically significant degree. Ibuprofen and naproxen can significantly increase serum lithium levels, but there is marked interindividual variation. Patients receiving nonsteroidal anti-inflammatory drugs must have their serum lithium levels checked every 4-5 days until the extent of drug interaction is assessed. A reduction in lithium dosage may be needed in some cases.
Such an interaction has occurred in patients with normal renal function. The effect on serum lithium levels varies greatly among different nonsteroidal anti-inflammatory drugs, indomethacin seeming most potent. On the other hand, there is no convincing evidence that sulindac and aspirin affect serum lithium levels to a clinically significant degree. Ibuprofen and naproxen can significantly increase serum lithium levels, but there is marked interindividual variation. Patients receiving nonsteroidal anti-inflammatory drugs must have their serum lithium levels checked every 4-5 days until the extent of drug interaction is assessed. A reduction in lithium dosage may be needed in some cases.
Similar articles
-
Lithium interaction with sulindac and naproxen.
Ragheb M, Powell AL. Ragheb M, et al. J Clin Psychopharmacol. 1986 Jun;6(3):150-4. J Clin Psychopharmacol.
 1986. PMID: 3711365 Clinical Trial.
1986. PMID: 3711365 Clinical Trial. -
Toxic elevation of serum lithium concentration by non-steroidal anti-inflammatory drugs.
Kelly CB, Cooper SJ. Kelly CB, et al. Ulster Med J. 1991 Oct;60(2):240-2. Ulster Med J. 1991. PMID: 1785162 Free PMC article. No abstract available.
-
Two drug interaction studies evaluating the pharmacokinetics and toxicity of pemetrexed when coadministered with aspirin or Ibuprofen in patients with advanced cancer.
Sweeney CJ, Takimoto CH, Latz JE, Baker SD, Murry DJ, Krull JH, Fife K, Battiato L, Cleverly A, Chaudhary AK, Chaudhuri T, Sandler A, Mita AC, Rowinsky EK. Sweeney CJ, et al. Clin Cancer Res. 2006 Jan 15;12(2):536-42. doi: 10.1158/1078-0432.CCR-05-1834.
 Clin Cancer Res. 2006. PMID: 16428497 Clinical Trial.
Clin Cancer Res. 2006. PMID: 16428497 Clinical Trial. -
Adverse drug interactions involving common prescription and over-the-counter analgesic agents.
Hersh EV, Pinto A, Moore PA. Hersh EV, et al. Clin Ther. 2007;29 Suppl:2477-97. doi: 10.1016/j.clinthera.2007.12.003. Clin Ther. 2007. PMID: 18164916 Review.
-
[Untoward interactions between antihypertensives and nonsteroidal anti-inflammatory drugs].
Pavlicević I, Rumboldt M, Rumboldt Z. Pavlicević I, et al. Lijec Vjesn. 2005 Jul-Aug;127(7-8):168-72. Lijec Vjesn. 2005. PMID: 16485829 Review. Croatian.
See all similar articles
Cited by
-
Elektif Non-Kardiyak Cerrahi Geçirecek Erişkinlerin Pre-Operatif Değerlendirme Kılavuzu: Avrupa Anesteziyoloji Derneği’nden Güncellenmiş Önerilerin Özeti: Pre-Operative Evaluation of Adults Undergoing Elective Noncardiac Surgery: Summary of the Updated Guideline From the European Society of Anaesthesiology.
Günaydın B, Kurtipek Ö. Günaydın B, et al. Turk J Anaesthesiol Reanim. 2019 Jun;47(3):244-272. doi: 10.5152/TJAR.2019.150419. Epub 2018 Jun 1. Turk J Anaesthesiol Reanim. 2019. PMID: 31183475 Free PMC article. Turkish. No abstract available.
-
Psychoactive Drugs in Plastic Surgery.
Davison SP, Baglien BD, Hayes KD. Davison SP, et al. Plast Reconstr Surg Glob Open. 2017 Mar 28;5(3):e1282. doi: 10.1097/GOX.0000000000001282. eCollection 2017 Mar. Plast Reconstr Surg Glob Open. 2017. PMID: 28458985 Free PMC article.
-
Prime Drug Interplay in Dental Practice.
Mohan S, Govila V, Saini A, Verma SC. Mohan S, et al. J Clin Diagn Res. 2016 Mar;10(3):ZE07-11. doi: 10.7860/JCDR/2016/16912.
 7434. Epub 2016 Mar 1. J Clin Diagn Res. 2016. PMID: 27135021 Free PMC article. Review.
7434. Epub 2016 Mar 1. J Clin Diagn Res. 2016. PMID: 27135021 Free PMC article. Review. -
Factors associated with chronic pain in patients with bipolar depression: a cross-sectional study.
Failde I, Dueñas M, Agüera-Ortíz L, Cervilla JA, Gonzalez-Pinto A, Mico JA. Failde I, et al. BMC Psychiatry. 2013 Apr 15;13:112. doi: 10.1186/1471-244X-13-112. BMC Psychiatry. 2013. PMID: 23587328 Free PMC article.
-
The incidence and clinical correlates of lithium toxicity: a retrospective review.
Dennison U, Clarkson M, O'Mullane J, Cassidy EM. Dennison U, et al. Ir J Med Sci. 2011 Sep;180(3):661-5. doi: 10.1007/s11845-011-0712-6. Epub 2011 Apr 23. Ir J Med Sci. 2011. PMID: 21516355
See all "Cited by" articles
Publication types
MeSH terms
Substances
Cite
Format: AMA APA MLA NLM
Add to Collections
- Create a new collection
- Add to an existing collection
Name your collection:
Name must be less than 100 characters
Choose a collection:
Unable to load your collection due to an error
Please try again
Send To
Lithium therapy and its interactions
Corrected 12 June 2020. View correction.
View correction.
This is the corrected version of the article.
SUMMARY
Lithium is one of the most effective mood stabilisers for people with a mood disorder. However, many of these patients are also taking other medicines that could potentially interact with lithium.
To minimise the risk of relapse, it is usually necessary to maintain the lithium serum concentration between 0.6 mmol/L and 0.8 mmol/L.
Lithium clearance is easily influenced by drugs that alter renal function such as ACE inhibitors, angiotensin receptor antagonists, diuretics, and non-steroidal anti-inflammatory drugs.
It is therefore prudent for prescribers to monitor and adjust the lithium dose to avoid adverse effects or loss of efficacy.
Introduction
Driven by new research reinforcing the unique benefits of lithium, there has been a worldwide resurgence in the prescription of lithium. In clinical practice it is used predominantly to stabilise mood.1 It remains one of the most effective options for bipolar disorder,2 along with the newer atypical antipsychotics.3 Lithium also serves as an effective adjunctive option for recurrent or resistant major depressive disorder and has anti-suicidal properties which are invaluable in the management of mood disorders.
In clinical practice it is used predominantly to stabilise mood.1 It remains one of the most effective options for bipolar disorder,2 along with the newer atypical antipsychotics.3 Lithium also serves as an effective adjunctive option for recurrent or resistant major depressive disorder and has anti-suicidal properties which are invaluable in the management of mood disorders.
Lithium is simple to administer and is usually well tolerated. Routine management of patients receiving lithium monotherapy is relatively straightforward.4 However, complications can arise when other drugs are added that could potentially interact with lithium.
Regular monitoring of lithium plasma concentrations and other safety parameters is essential. Results should be communicated to the patient and everyone involved in their care. Aids are available to assist prescribers with lithium management, including an Australian tool called the ‘Lithiumeter’.4
Indications for lithium
Patients with classic, episodic and remitting bipolar disorder with a family history and no psychiatric comorbidity are most likely to respond to lithium. Typically, lithium is effective in about a third of patients – with response rates up to two-thirds in those whose relatives have achieved good responses.5 It is likely that people who commence lithium early in the course of their illness may have greater likelihood of response. In major depressive disorder, lithium is used to augment antidepressant drugs.
Typically, lithium is effective in about a third of patients – with response rates up to two-thirds in those whose relatives have achieved good responses.5 It is likely that people who commence lithium early in the course of their illness may have greater likelihood of response. In major depressive disorder, lithium is used to augment antidepressant drugs.
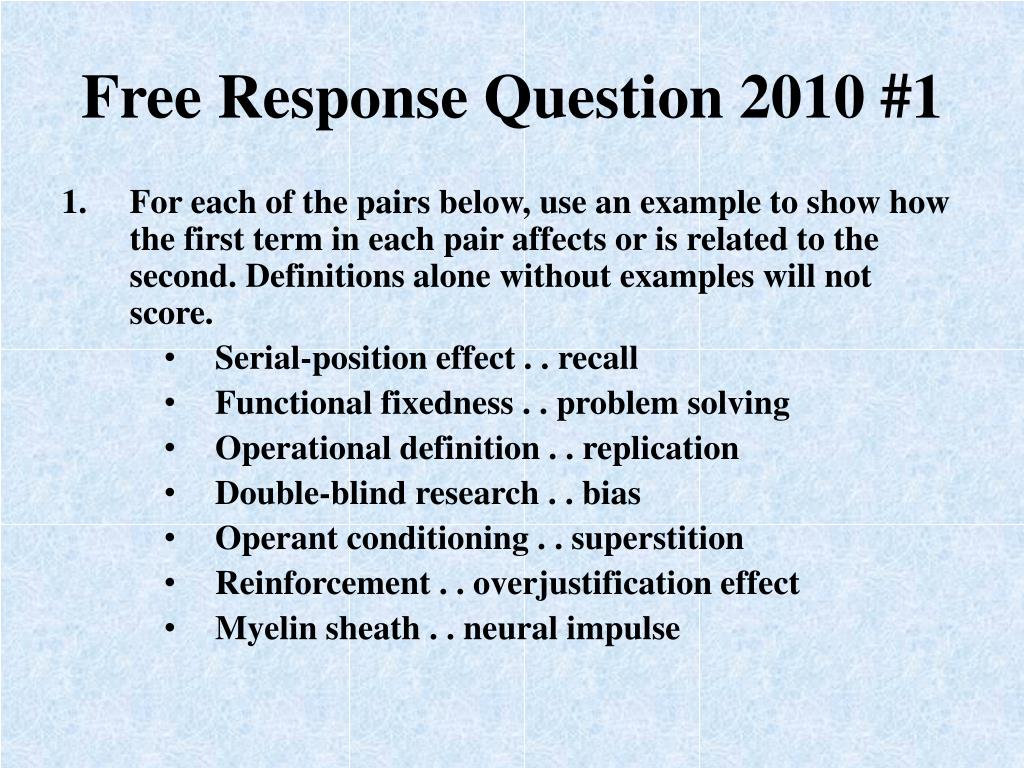
Lithium monitoring
Lithium has a very narrow therapeutic window for maintenance therapy. Too little lithium risks undertreatment of the mood disorder and increases the risk of relapse. Too much lithium increases the risk of both acute and chronic toxicity. Lithium concentrations should always be measured 12 hours after the last dose.
For the maintenance phase of treatment, recent guidelines recommend that patients maintain a serum concentration of 0. 6–0.8 mmol/L to maximise therapeutic benefit.6 For acute treatment in mania, serum concentrations should be increased to 0.6–1.0 mmol/L as tolerated. In depression, concentrations can be in the range of 0.4–0.8 mmol/L. In practice, target concentrations and monitoring practices are often inconsistent. Not all pathology laboratories use the same reference ranges, therefore noting whether the lithium concentration is consistent with the patient’s presentation and the guidelines is essential.
6–0.8 mmol/L to maximise therapeutic benefit.6 For acute treatment in mania, serum concentrations should be increased to 0.6–1.0 mmol/L as tolerated. In depression, concentrations can be in the range of 0.4–0.8 mmol/L. In practice, target concentrations and monitoring practices are often inconsistent. Not all pathology laboratories use the same reference ranges, therefore noting whether the lithium concentration is consistent with the patient’s presentation and the guidelines is essential.
As a part of optimising lithium dosing, clinicians may notice that a specific concentration achieves the most therapeutic benefit during euthymic periods and during manic and depressive episodes. Taking note of this is essential and helps to ensure stability of these patient-specific concentrations over time, particularly during each illness phase.
Maintenance of the therapeutic concentration (and adherence) is the strongest predictor of long-term stability. However, in some patients, stabilising their mood is not always possible with lithium alone. A trial with other mood stabilisers, such as adjunctive sodium valproate or an atypical antipsychotic, is often necessary.
A trial with other mood stabilisers, such as adjunctive sodium valproate or an atypical antipsychotic, is often necessary.
A recommended monitoring schedule for lithium in a patient not taking other drugs is outlined in the Box.4 Drug interactions are more likely to affect patients as they get older because of declining renal function and the accumulation of medical comorbidities. Close monitoring and dose adjustments are therefore often needed as patients get older.
Box - Monitoring schedule for lithium therapy
Baseline assessments and follow-up of patients should be performed:
- during the early maintenance phase (e.g. baseline, 7 days, 14 days and 28 days) then at 3, 6 and 12 months, then annually
and
- when there are any changes in presentation
- following abnormal findings
- when altering the treatment regimen.
Regularly check the following:
- serum lithium concentrations and mood and stability over time
- renal function
- electrolytes, urea, creatinine
- estimated glomerular filtration rate
- thyroid and parathyroid function
- thyroid stimulating hormone
- calcium
- blood and cardiometabolic tests
- full blood count, glucose, lipids, liver function tests
- ECG
- weight, BMI, umbilical girth
- diet and eating behaviour
- exercise and hydration
- other comorbidities
- adverse effects
- cognition
- global functioning
- treatment adherence
Based on reference 4
In patients taking concomitant drugs, extra care should be taken because of the risk of drug interactions.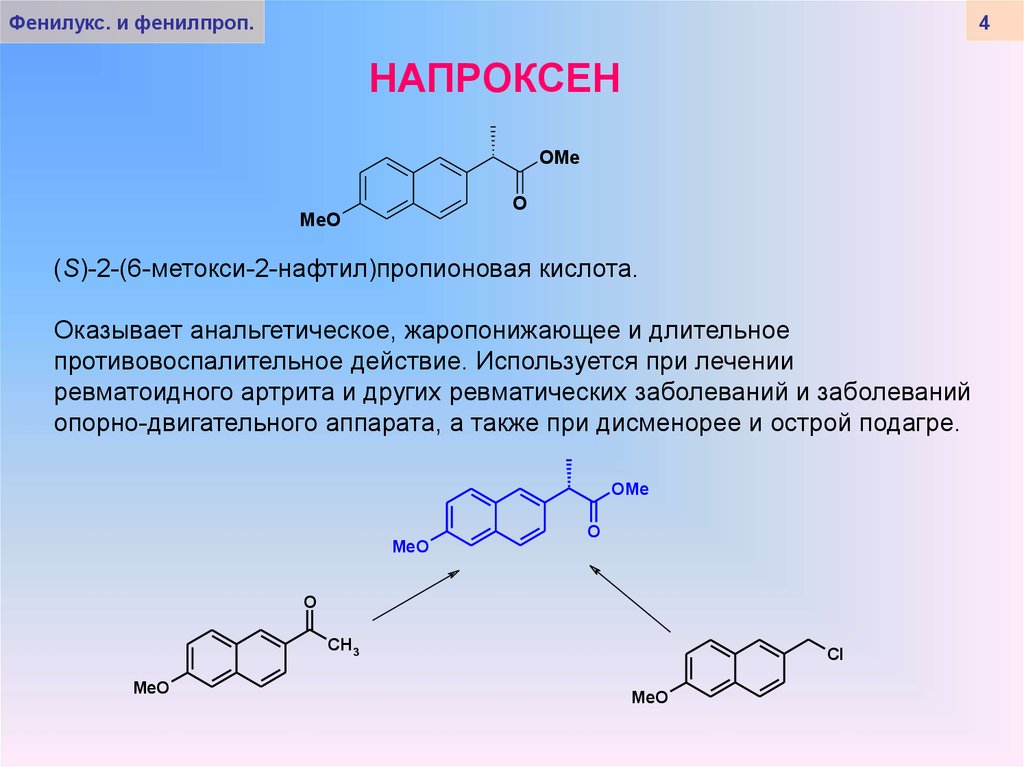 Lithium concentrations should be closely monitored around the time of medication changes – at least just before and when the drugs have reached steady states. Lithium’s half-life is about 24 hours, so a steady state is usually achieved after 5–7 days. A complete list of lithium drug interactions can be found at MIMS Online or Drugs.com.
Lithium concentrations should be closely monitored around the time of medication changes – at least just before and when the drugs have reached steady states. Lithium’s half-life is about 24 hours, so a steady state is usually achieved after 5–7 days. A complete list of lithium drug interactions can be found at MIMS Online or Drugs.com.
Regular monitoring is required until a therapeutic concentration of lithium is reached and maintained, and any time that the patient presents with symptoms of lithium toxicity.7 Conditions leading to haemodynamic and volume changes such as dehydration, febrile illness, gastrointestinal loss, drug interactions, perioperative management and surgery can affect lithium serum concentrations and levels should be rechecked in these circumstances.
Prescribers should contact the treating psychiatrist or consult a medicines information pharmacist if they are unsure how to manage a patient. Having up-to-date serum lithium concentrations at hand will assist.
Adverse effects of lithium
Regular long-term monitoring of lithium concentrations is essential to avoid both acute and chronic toxicity. Physical examinations and laboratory investigations should be performed at baseline and regular intervals after that (see Box).
Common acute adverse effects include tremor, polydipsia, polyuria, dysgeusia, nausea and diarrhoea (see Table). Prescribers can reassure patients that these adverse effects are usually transient after starting treatment. They are often dependent on the serum concentration of lithium and frequently subside within days or weeks. Nephrogenic diabetes insipidus (polyuria and polydipsia) is a common adverse effect of lithium.
Table - Major adverse effects of lithium therapy
|
Toxicity |
Adverse effect |
Action |
|
Acute |
Any acute adverse effect or presentation |
Measure lithium concentration |
|
Headache, fatigue |
Consider stopping lithium |
|
|
Thirst, taste |
Review medication |
|
|
Arrythmias |
Hospitalisation |
|
|
Nausea, vomiting, diarrhoea, polyuria |
Review hydration and consider haemodialysis |
|
|
Tremor |
Monitoring and review medication |
|
|
Chronic |
Cognitive effects, ataxia, agitation, confusion, sluggishness |
Monitor changes, optimise lithium concentrations, neurological referral |
|
Thyroid or parathyroid dysfunction |
Monitor changes, optimise lithium concentrations, endocrinology referral |
|
|
Renal dysfunction |
Monitor changes, optimise lithium concentrations, nephrology referral |
Chronic adverse effects include subjective cognitive effects, thyroid and parathyroid dysfunction, and renal dysfunction (see Table)._1.jpg) Some patients may report more mild neurocognitive effects such as ‘brain fog’, ‘emotional greying’, ‘slowing’, ‘shakiness’, anomia, and ‘reduced creativity’. The higher the lithium concentration, the greater the risk of toxic presentations. In the long term, or with higher blood concentrations or repeated acute fluctuations, lithium leads to end-stage renal failure in 1% of patients (over 15 years treatment).8 However, it should be noted that most patients do not experience renal adverse effects.
Some patients may report more mild neurocognitive effects such as ‘brain fog’, ‘emotional greying’, ‘slowing’, ‘shakiness’, anomia, and ‘reduced creativity’. The higher the lithium concentration, the greater the risk of toxic presentations. In the long term, or with higher blood concentrations or repeated acute fluctuations, lithium leads to end-stage renal failure in 1% of patients (over 15 years treatment).8 However, it should be noted that most patients do not experience renal adverse effects.
Common drug–drug interactions with lithium
The most common and noteworthy drug–drug interactions with lithium are pharmacokinetic in nature. The lithium ion is extensively absorbed in the gastrointestinal tract. The main determinant of serum concentrations is renal excretion, therefore the main drug interactions occur when co-administered drugs alter renal function, specifically modifying glomerular filtration and tubular reabsorption.
The most commonly prescribed drugs that have the potential to interact with lithium are ACE inhibitors, angiotensin II receptor antagonists (sartans), diuretics, and non-steroidal anti-inflammatory drugs (NSAIDs). Combinations of these are frequently used, so prescribers should be aware of their additive effects for a patient taking lithium.
ACE inhibitors and angiotensin II receptor antagonists
Several case reports and hospital admission studies have shown that ACE inhibitors and angiotensin II receptor antagonists can increase lithium serum concentrations and increase the chance of toxicity. Closer monitoring of lithium concentrations is needed when people start either of these drugs and the lithium dose will probably need to be reduced until a stable therapeutic concentration has been achieved. Closer monitoring is also required when these drugs are stopped.
Diuretics
When any diuretic is used, lithium concentrations must be carefully monitored. Thiazide and thiazide-like diuretics increase sodium reabsorption which decreases the clearance of lithium and significantly elevates lithium concentrations in serum. This is enough to fall out of the therapeutic range in many cases. As a rule of thumb, many prescribers halve the lithium dose then up- or down-titrate the dose with monitoring. Other prescribers avoid thiazide diuretics altogether.
This is enough to fall out of the therapeutic range in many cases. As a rule of thumb, many prescribers halve the lithium dose then up- or down-titrate the dose with monitoring. Other prescribers avoid thiazide diuretics altogether.
Amiloride is recommended as a diuretic because it blocks entry of lithium through the epithelial sodium channel in the collecting duct. This reduces lithium accumulation and may improve kidney function in patients on long-term treatment.9
Other diuretics such as the osmotic methylxanthine (e.g. theophylline) and loop (e.g. furosemide (frusemide)) and potassium-sparing (e.g. spironolactone) diuretics may also alter lithium concentrations.
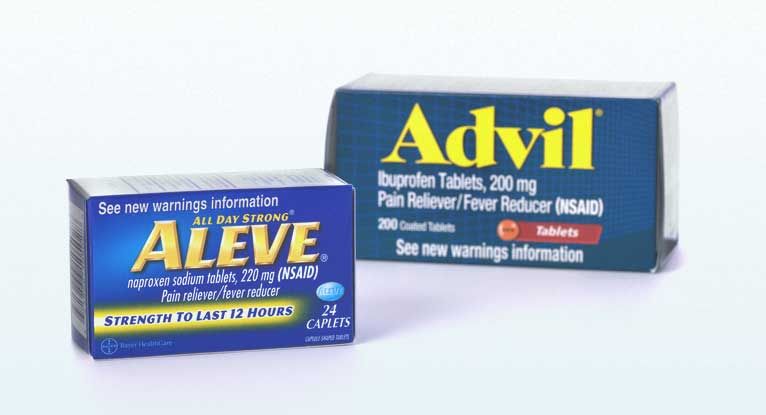
Non-steroidal anti-inflammatory drugs
Patients on lithium therapy should be advised to avoid NSAIDs. Regular use is more problematic than episodic use. NSAIDs differentially alter lithium concentrations by multiple mechanisms, and one of these is to reduce prostaglandin E2 by inhibiting cyclo-oxygenase. This reduces vasodilation of the afferent arteriole which decreases blood flow to the glomerulus. This decreases glomerular filtration and consequently lithium excretion. If NSAIDs are indicated, they should be used under medical guidance with closer monitoring of lithium concentrations. Lower lithium doses may be required.
This reduces vasodilation of the afferent arteriole which decreases blood flow to the glomerulus. This decreases glomerular filtration and consequently lithium excretion. If NSAIDs are indicated, they should be used under medical guidance with closer monitoring of lithium concentrations. Lower lithium doses may be required.
Other drugs
Acetazolamide for intraocular pressure, glaucoma and epilepsy has been shown to significantly increase lithium clearance.
Conclusion
Lithium has an important role in the treatment of mood disorders. Prescribers need to be mindful of its potential drug interactions and the impact they can have on patients. Improved knowledge of and confidence with monitoring will contribute to better patient outcomes.
Gin Malhi has received grant or research support from the National Health and Medical Research Council, Australian Rotary Health, NSW Health, Ramsay Health, American Foundation for Suicide Prevention, Ramsay Research and Teaching Fund, Elsevier, AstraZeneca and Servier; has been a speaker for AstraZeneca, Janssen-Cilag, Lundbeck, Otsuka and Servier; and has been a consultant for AstraZeneca, Janssen Cilag, Lundbeck, Otsuka and Servier.
Michael Berk is supported by a National Health and Medical Research Council Senior Principal Research Fellowship (1059660 and APP1156072).
References
- Grande I, Berk M, Birmaher B, Vieta E. Bipolar disorder. Lancet 2016;387:1561-72.
- Vieta E, Berk M, Schulze TG, Carvalho AF, Suppes T, Calabrese JR, et al. Bipolar disorders. Nat Rev Dis Primers 2018;4:18008.
- Ng F, Mammen OK, Wilting I, Sachs GS, Ferrier IN, Cassidy F, et al. The International Society for Bipolar Disorders (ISBD) consensus guidelines for the safety monitoring of bipolar disorder treatments. Bipolar Disord 2009;11:559-95.

- Malhi GS, Gershon S, Outhred T. Lithiumeter: Version 2.0. Bipolar Disord 2016;18:631-41.
- Grof P, Duffy A, Cavazzoni P, Grof E, Garnham J, MacDougall M, et al. Is response to prophylactic lithium a familial trait? J Clin Psychiatry 2002;63:942-7.
- Malhi, GS, Bassett D, Boyce P, Bryant R, Fitzgerald PB, Fritz K, et al. Royal Australian and New Zealand College of Psychiatrists clinical practice guidelines for mood disorders. Aust N Z J Psychiatry 2015;49:1087–206.
- Ott M, Stegmayr B, Salander Renberg E, Werneke U. Lithium intoxication: Incidence, clinical course and renal function - a population-based retrospective cohort study. J Psychopharmacol 2016;30:1008-19.
- Azab AN, Shnaider A, Osher Y, Wang D, Bersudsky Y, Belmaker RH.
 Lithium nephrotoxicity. Int J Bipolar Disord 2015;3:13.
Lithium nephrotoxicity. Int J Bipolar Disord 2015;3:13. - Batlle DC, von Riotte AB, Gaviria M, Grupp M. Amelioration of polyuria by amiloride in patients receiving long-term lithium therapy. N Engl J Med 1985;312:408-14.
Lithium
Lithium is one of the most well studied and commonly used drugs for the treatment of patients suffering from bipolar disorders - mental illness characterized by alternating periods of depression and mania. Lithium is often referred to as a "mood stabilizer" and is usually given to patients who do not respond to other medications. It is a relatively slow-acting drug, sometimes it can take several months before it stabilizes the mental state. The amount of the drug should be sufficient to create a stable concentration of lithium in the blood, necessary for a therapeutic effect. This dosage for each patient is individual and depends on age, general health and other medications. The lithium level should be checked regularly: if it is too low, the treatment will be ineffective, and if it is too high, it is dangerous for poisoning with nausea, vomiting, diarrhea, clouding of consciousness and trembling. Very high concentrations of lithium can lead to stupor, heart attacks, and even death. Lithium intake can cause hypothyroidism. Therefore, when taking lithium preparations, regular monitoring of thyroid function is necessary. nine0005
This dosage for each patient is individual and depends on age, general health and other medications. The lithium level should be checked regularly: if it is too low, the treatment will be ineffective, and if it is too high, it is dangerous for poisoning with nausea, vomiting, diarrhea, clouding of consciousness and trembling. Very high concentrations of lithium can lead to stupor, heart attacks, and even death. Lithium intake can cause hypothyroidism. Therefore, when taking lithium preparations, regular monitoring of thyroid function is necessary. nine0005
Exam Preparation
Blood for lithium testing is usually taken 12-18 hours after the last dose of a lithium-containing drug.
Indications for examination
At the beginning of treatment with drugs containing lithium, or when they are repeated after a break.
Regularly after reaching a sufficient level of lithium in the blood for treatment - to confirm that the required level is maintained.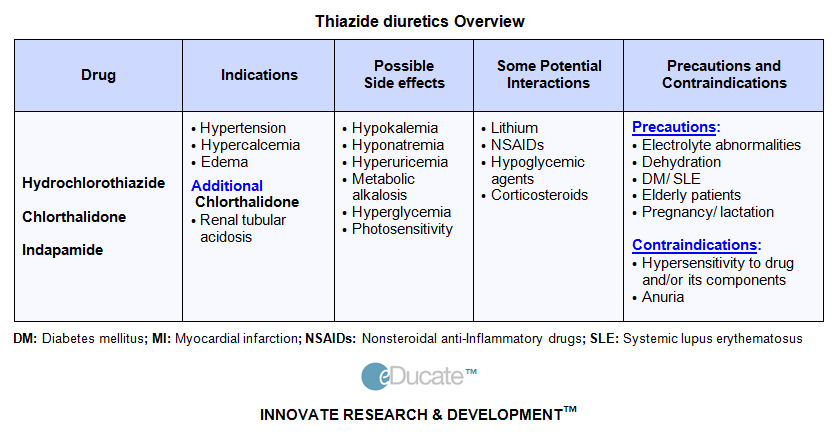 nine0005 When it is necessary to find out the reason for the ineffectiveness of lithium therapy (whether the amount of the drug taken is too low, or the fact is that, for example, the patient does not comply with the prescription for taking lithium).
nine0005 When it is necessary to find out the reason for the ineffectiveness of lithium therapy (whether the amount of the drug taken is too low, or the fact is that, for example, the patient does not comply with the prescription for taking lithium).
With symptoms indicating a toxic effect (drowsiness, weakness, incoordination, slurred speech, nausea, vomiting and diarrhea, clouding of consciousness, trembling).
Interpretation
If the lithium level is within the normal range, then the drug has a therapeutic effect without a toxic effect. nine0006
If the concentration of lithium in the blood is low, then most likely the patient does not receive the right amount of medication, if it is higher and there is a side effect - the dose taken is too high. However, you should not reduce the amount of the drug or stop taking it without consulting a doctor, as this may complicate the disease. Treatment should be prescribed by a doctor: for each person, taking into account individual characteristics, he will select the dose that has the most favorable therapeutic effect. nine0006
nine0006
Results may be affected
Theophylline and caffeine lower lithium levels. Lithium is eliminated from the body primarily through the kidneys, so long-term use of lithium increases the chance of kidney failure, and impaired kidney function can cause elevated lithium levels.
Various medications, as well as some dietary supplements, can affect the concentration of lithium in the blood. Medications that increase lithium levels include anti-inflammatory drugs (ibuprofen, naproxen) and diuretics (hydrochlorothiazide and furosemide). nine0005 Some medications contribute to the side effects of lithium, including neuroleptics (clozapine and olanzapine), blood pressure lowering drugs, and anti-seizure medications (carbamazepines).
Loss of salts and water by the body (as with a salt-free diet, increased sweating, or diseases accompanied by nausea and vomiting) contributes to an increase in the level of lithium in the body and the manifestation of its side effects.
Assigned in combination with
Serum creatinine
Thyroid stimulating hormone (TSH)
Lithium in the blood
Lithium is one of the most well studied and commonly used drugs for the treatment of patients suffering from bipolar disorders.
Synonyms English
Lithium.
Research method
Atomic absorption spectrometry (AAS).
Units
µg/l (micrograms per liter), mmol/l (millimoles per liter). nine0006
What biomaterial can be used for research?
Venous blood.
How to properly prepare for an examination?
- Do not eat for 2-3 hours before the examination, you can drink pure non-carbonated water.
- Do not smoke 30 minutes before the examination.
Overview of the study
Lithium preparations are among the most well studied and widely used in the treatment of bipolar disorder, a mental illness characterized by alternating periods of depression and mania. These periods can last from several days to several months or even years. The patient's condition ranges from apathy to euphoria. Both adults and children are susceptible to bipolar disorder. nine0006
These periods can last from several days to several months or even years. The patient's condition ranges from apathy to euphoria. Both adults and children are susceptible to bipolar disorder. nine0006
Lithium is often referred to as a "mood stabilizer" and is commonly prescribed for patients not responding to other medications. It is a relatively slow-acting drug, sometimes it can take several months before it stabilizes the mental state.
The amount of the drug must be sufficient to create a stable concentration of lithium in the blood, necessary for a therapeutic effect. This dosage for each patient is individual and depends on age, general health and other medications. nine0006
Lithium levels should be checked regularly: if it is too low, treatment will be ineffective, and if it is too high, it can cause poisoning with nausea, vomiting, diarrhoea, confusion and trembling. Very high concentrations of lithium can lead to stupor, heart attacks, and even death.
What is research used for?
- To control whether the lithium level is sufficient for treatment.

- To determine the necessary concentration of lithium in the blood at the beginning of taking medications. nine0090
- To monitor fluctuating lithium levels.
- To find out how a patient's medications affect lithium levels.
- If lithium toxicity is suspected.
When is the test ordered?
- At the beginning of treatment with drugs containing lithium, or when they are taken again after a break.
- Regularly after reaching a sufficient level of lithium in the blood for treatment - to confirm that the required level is maintained. nine0090
- When it is necessary to find out the reason for the failure of lithium therapy (whether the amount of the drug taken is too low, or the fact is that, for example, the patient does not comply with the prescription for taking lithium).
- For symptoms suggestive of a toxic effect (drowsiness, weakness, incoordination, slurred speech, nausea, vomiting and diarrhea, clouding of consciousness, trembling).
What do the results mean?
Reference values
Concentration: 0.7 - 84 µg/l.
Therapeutic concentration: 0.6 - 1.2 mmol/l.
If the lithium level is within the normal range, then the drug has a therapeutic effect without a toxic effect.
If the concentration of lithium in the blood is low, then most likely the patient does not receive the right amount of medication, if it is higher and there is a side effect - the dose taken is too high. However, you should not reduce the amount of the drug or stop taking it without consulting a doctor, as this may complicate the disease. Treatment should be prescribed by a doctor: for each person, taking into account individual characteristics, he will select the dose that has the most favorable therapeutic effect. nine0006
What can influence the result?
Theophylline and caffeine lower lithium levels.
Important Notes
- Lithium is eliminated primarily through the kidneys, so long-term use increases the chance of kidney failure, and kidney dysfunction can cause elevated lithium levels.