Lamictal side effects bipolar
Lamotrigine | Mood Stabiliser Uses & Side Effects
About lamotrigine
Please note
Thinking about trying medication? Read our guide
How lamotrigine works
Lamotrigine is a type of medicine called a ‘mood stabiliser’ as it can reduce feelings of excitability and over-activity and reduce mood swings. It tends to work better on the low mood (depression) part of bipolar disorder.
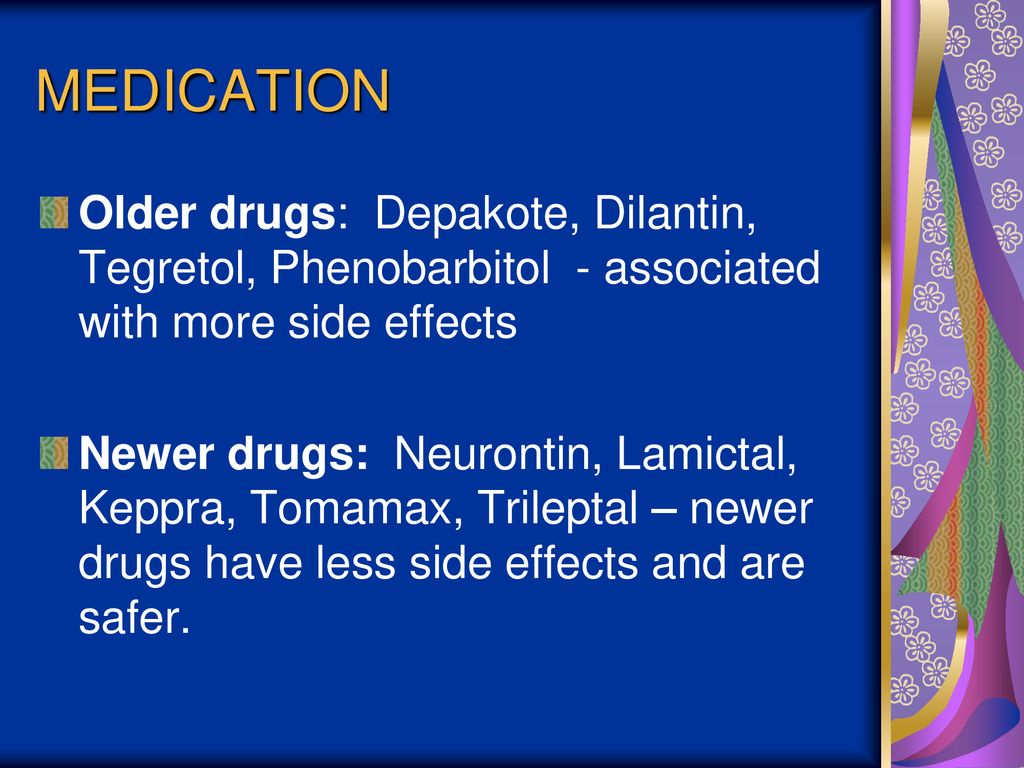
It is also taken by some people who have epilepsy, as it increases the effects of the calming transmitter GABA, leading to a reduction in seizures. This is a very separate use but will be covered in any patient leaflets.
Bipolar disorderLamotrigine and everyday life
Frequently asked questions
You may start off at a low dose and gradually increase it every few days or weeks until you and your doctor find the dose that is right for you. It may take up to six weeks to do this, by which time you should be a on a stable, long-term dose and have seen some helpful results from the medication.
It is important not to hurry the dosing timetable as doing so can increase your chances of getting a serious skin reaction.
You may want to let your family and friends know you are taking lamotrigine so they can support you and help you look out for side effects.
For guidance on this, check out our page on getting support with your medication.
Lamotrigine may make you feel very drowsy or sleepy when you start taking it.
It may also make it difficult for you to get to sleep.
If these symptoms carry on for a long time, or if this is difficult for you, talk to your doctor or pharmacist about other medicines you could take.
Alcohol
You can drink alcohol while taking lamotrigine, but it is likely to make you feel sleepier.
Street drugs
We do not know how street drugs affect lamotrigine, but all these drugs affect the way the brain works so they may not mix well.
Lamotrigine can produce a false positive test for phencyclidine (PCP) on a urine drug screen.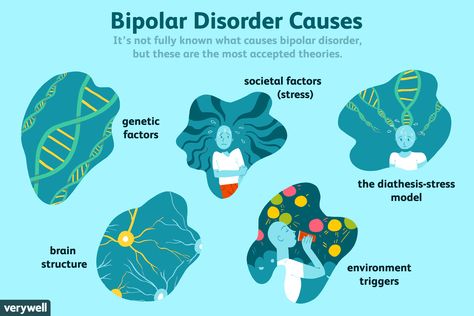 Talk to your doctor about this if it is a problem for you.
Talk to your doctor about this if it is a problem for you.
Lamotrigine does not mix well with some other medicines and drugs and may affect the way in which they work. Tell your doctor if you are taking any other medications including over-the-counter medicines for common illnesses and things you put on your skin.
Special information about contraceptive pills containing oestrogen
- When lamotrigine is taken with any type of the Pill (oral contraceptive) containing oestrogen, it lowers the level of lamotrigine that you have in your body.
- If you have a pill-free week, the levels of lamotrigine will then rise, which may give you side effects.
- If you take the Pill without a break, it will make your lamotrigine levels stable. You will not be harmed by not having the break.
- Talk to your doctor or pharmacist before you start taking lamotrigine if you also take the Pill.
- The morning-after pill does not affect the level of lamotrigine in your body as it does not contain oestrogen.

If you have any further questions about this, you should speak to your doctor or pharmacist.
Lamotrigine tablets have lactose in them which may not suit people who have a problem drinking milk or eating certain sugars. Talk to your doctor or pharmacist about this if you think it could be a problem for you.
Do not drive a car or ride a bike just after you start taking lamotrigine.
Taking lamotrigine may make you feel dizzy and may affect your eyesight when you start taking it (possibly causing blurred or double vision).
This could affect you if you drive a car, ride a bike, or do anything else that needs a lot of focus. It might be best to stop doing these things for the first few days, until you know how it affects you.
Do not worry - most people do these things as normal while taking lamotrigine.
Pregnancy
If you become pregnant while you are on lamotrigine, you should carry on taking the medicine and go back to your doctor as soon as possible to discuss whether you should stop or change your medicine.
Studies of over 7,500 women taking lamotrigine showed no increase in problems during the early stages of pregnancy.
Your doctor might also give you extra folic acid to take, which helps prevent any spine problems in your baby.
From month four onwards, you are likely to need a higher dose of lamotrigine to keep the level of the medication in your body constant. After giving birth, your lamotrigine dose will go back to what it was before.
If you are taking lamotrigine for epilepsy, any dose increases may be made based on the results of your blood level tests.
Post-natal
If you and your doctor agree that you will carry on taking lamotrigine throughout your pregnancy, you should tell your midwife that you are taking it before you give birth.
Breastfeeding
Lamotrigine can be passed to the baby in breastmilk, and side effects have been seen in breastfed babies. Usually there is no problem with breastfeeding a healthy baby.
Talk to your midwife or doctor about the benefits and risks of breastfeeding while taking lamotrigine.
There is nothing to suggest that lamotrigine has any effects on fertility.
Lamotrigine is not a banned substance in sport.
It could, however, make you feel dizzy and give you blurred or double vision when you start taking it.
It might be better to delay any sport that needs a lot of focus until you know how it affects you.
Do not worry - most people play sports as normal while taking lamotrigine.
Try not to take lamotrigine for the first time just before your exams, as you may have sleep problems (feeling tired or having difficulty getting to sleep), and some blurred eyesight or double vision when you start taking lamotrigine.
You should talk to your doctor about any future exams if you are starting lamotrigine.
You might decide together to delay starting it until you have done them.
If they are more than a month away, however, you might find that it is better to start lamotrigine to improve your motivation to study.
Do not worry - most people do all these things as normal while taking lamotrigine.
Your doctor should know
Uses, warnings, safety and side effects of lamotrigine
Taking lamotrigine
How long will I need to take lamotrigine for?
You and your doctor should talk about how long you need to take lamotrigine before you begin treatment with this medication.
If you take lamotrigine for bipolar disorder you will probably take it for at least six months (any shorter and your old symptoms can come back). If it works for you, you may take it for much longer than that.
You should only take lamotrigine as agreed with your doctor
Make sure that you know your dose. If it is not written on the label, check with your pharmacist or doctor.
You may have to take lamotrigine once or twice a day.
It doesn’t matter what time you take it each day – choose a time that you can always remember. This could be at mealtimes, or when you brush your teeth. You can take it before or after food.
You can take it before or after food.
If you are taking the tablets that you swallow whole, wash them down with a glass of water. Do not try and chew them – they will taste unpleasant.
If you are taking the orodispersible tablets (melts), get a glass of cold water and mix the tablet(s) in at least enough water to cover them. You can stir the drink to help them break up. 'Dispersible' doesn’t mean you will get a totally clear solution - it will look a little cloudy. Drink it all, and then add more water to the glass and drink that in order to make sure you get all the medicine in the tablet.
You can also chew the dispersible tablets, but it may help to rinse them down with some cold water.
You can still swallow the dispersible tablets whole with water if you prefer.
What should I do if I miss a dose of lamotrigine?
If you remember later during the day, take it as soon as possible. If you forget to take it by the time of the next dose, just start again with the next dose.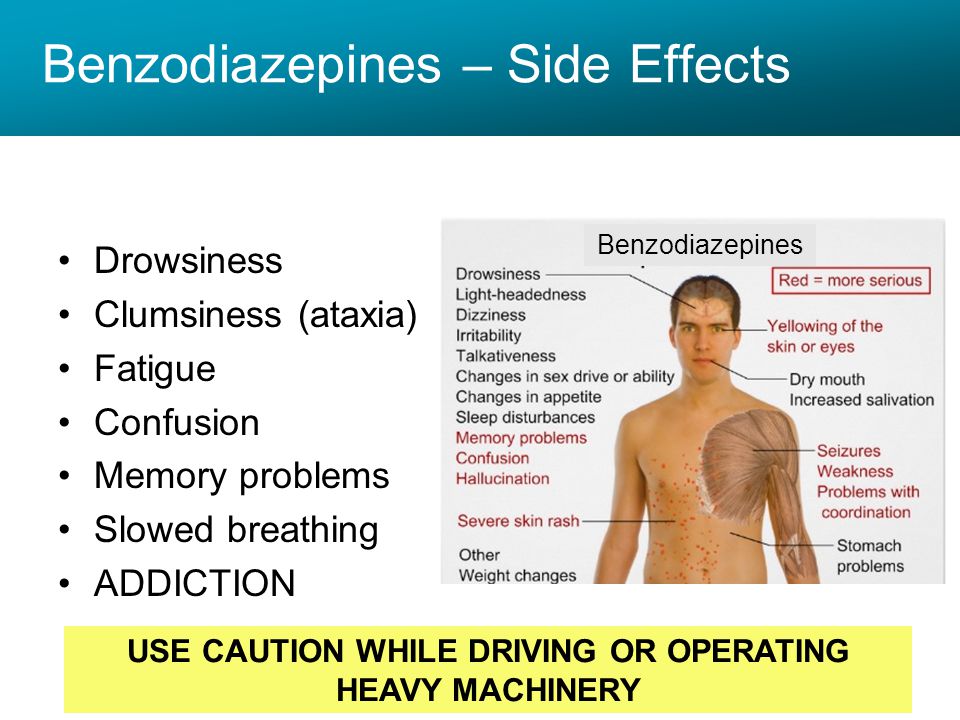
Do not take a double dose.
What will happen if I forget to take my lamotrigine?
If you forget to take your tablets for a few days, you may start getting your old symptoms of low mood back.
Stopping the use of lamotrigine
Although you may not be taking your lamotrigine for seizures (fits), if you stop the medication suddenly, there is a chance you may have a seizure. This is because after taking lamotrigine for some time, your body will have got used to having an anticonvulsant (anti-seizure) medicine on board. Suddenly stopping the use of lamotrigine may therefore cause a seizure. But don't worry - this doesn't mean you are suddenly epileptic.
If you have stopped taking lamotrigine, you need to speak to your doctor so that you can safely start it again and build back up to your dose. It is best to be honest; they will help you get back on track.
If you are thinking of stopping treatment with lamotrigine, talk to your doctor before doing this.
Warnings and safety
Safety headlines
If you have taken more lamotrigine than the dosage recommended by the doctor who prescribed it to you, you must get medical help immediately – even if you do not feel any different.
While taking lamotrigine, some people may think about hurting themselves or taking their own lives. You must go straight to hospital with your medicine if you have any of these thoughts.
Lamotrigine can cause other serious side effects: allergic reactions (difficulty breathing, swelling of your face or throat, itching skin lumps), skin rashes and other serious symptoms. Go to a hospital with your medicine if you get any of these symptoms.
Lamotrigine does not mix well with some other medicines and drugs. The contraceptive Pill can affect the level of lamotrigine in your blood. Talk to your doctor about this if you are on the Pill.
You might feel dizzy or have double vision in the first few days after taking lamotrigine. Do not drive a car, ride a bike or operate machines until you see how this affects you.
Do not drive a car, ride a bike or operate machines until you see how this affects you.
Use good contraception while you are taking lamotrigine. If you take it while you are pregnant, it is unlikely to affect the developing baby. However, it can cause symptoms in babies if you breastfeed while taking lamotrigine. Talk to your doctor or midwife about this and get their help.
When to go to the hospital
If you have taken more lamotrigine than the dosage recommended by the doctor who prescribed it to you, you must get medical help immediately – even if you do not feel any different . Go to A&E, and take your medicine with you to show the doctors. Tell them how much you have taken. Get a friend to go with you, if you can, just in case you feel ill on the way.
You might get any of the following symptoms:
- quick, uncontrollable body movements
- clumsiness and lack of co-ordination, causing problems with your balance
- heart rhythm changes
- loss of consciousness, convulsions/seizures (fits) or coma
While taking lamotrigine some people may think about hurting themselves or have thoughts of taking their own lives.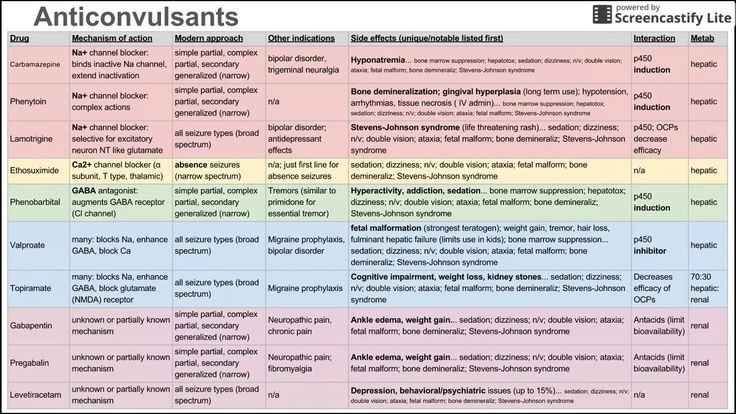 This can happen to anyone, including people who are under 25. These thoughts may happen or get worse in the first few weeks of taking the medicine. You must go straight to hospital with your medicine if you have any of these thoughts and tell the doctor that you are taking lamotrigine. There are other medications you can take instead.
This can happen to anyone, including people who are under 25. These thoughts may happen or get worse in the first few weeks of taking the medicine. You must go straight to hospital with your medicine if you have any of these thoughts and tell the doctor that you are taking lamotrigine. There are other medications you can take instead.
You should also go to a doctor or hospital straight away if you get any of the following symptoms:
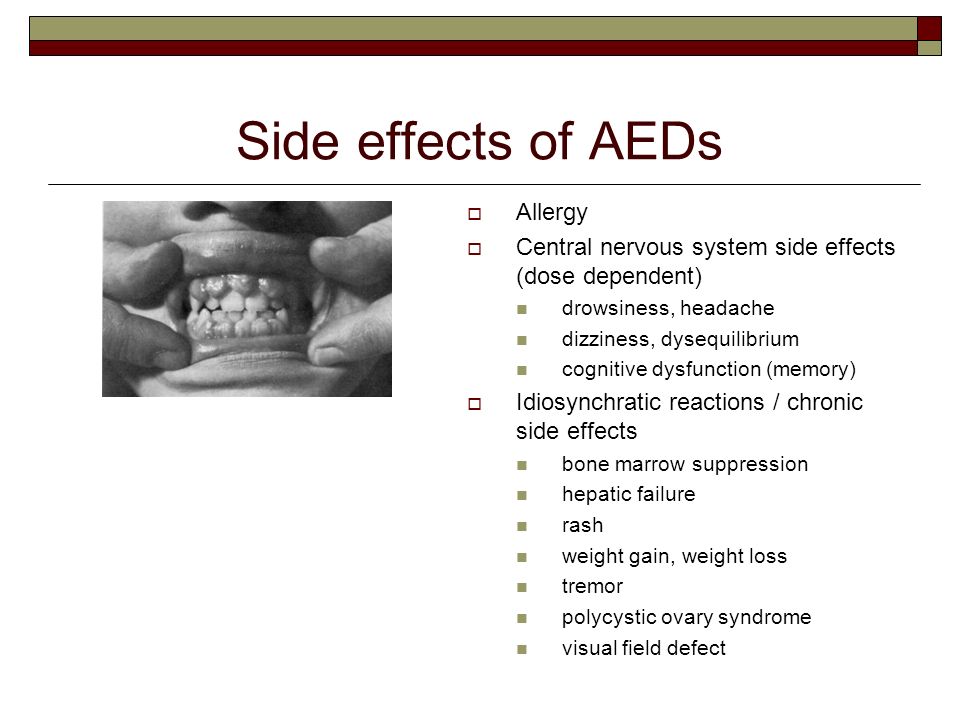
- skin rashes or redness with blisters and peeling skin around the mouth, nose, eyes and groin/sex organs (genitals)
- peeling of large areas of skin (up to 30% - almost a third – of your body surface)
- ulcers in the mouth, throat, nose or around your groin/sex organs (genitals)
- red or swollen eyes
- a high temperature (fever), flu-like symptoms or drowsiness
- swelling around your face
- swollen glands in your neck, armpit or groin
- unexpected bleeding or bruising
- your fingers turning blue
- a sore throat
- more infections (such as colds) than usual
If these reactions occur, they tend to be during the first eight weeks of taking lamotrigine.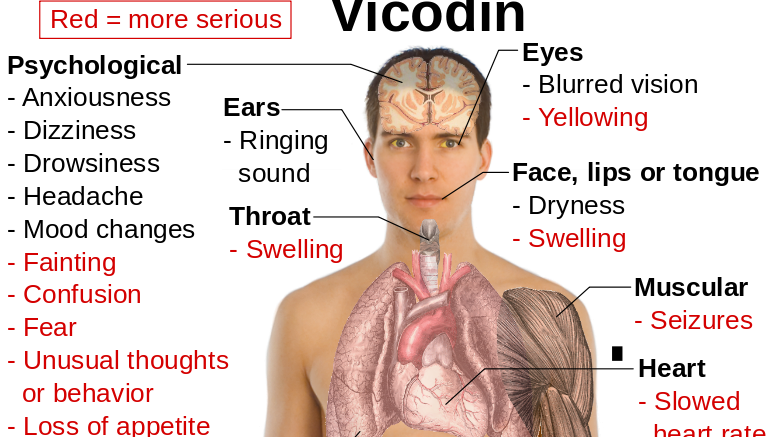
Side effects of lamotrigine
Side effects of lamotrigine
Some side effects that appear should get better after a few days. If they do not, you should go back to your doctor.
Do not stop taking the tablets until you talk to your doctor, or you may get withdrawal symptoms as well.
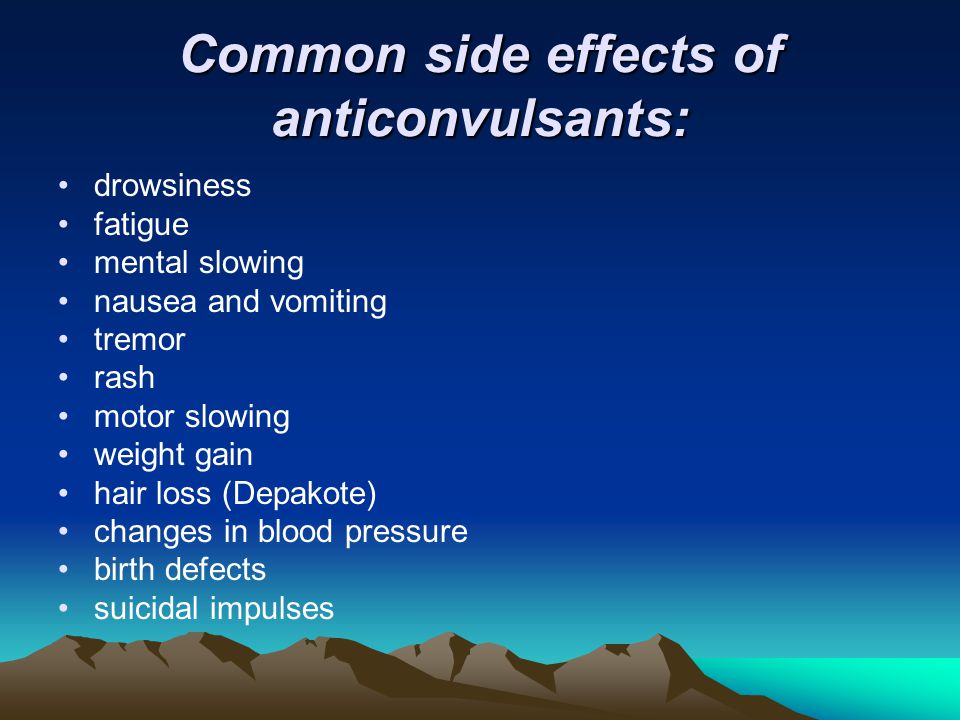
Very common side effects of taking lamotrigine (affecting more than one in ten people) include:
- headaches
- skin rashes
Common side effects of taking lamotrigine (affecting up to one in ten people) include:
- feeling aggressive, agitated or irritable
- feeling sleepy, tired or drowsy
- insomnia (having difficulty sleeping)
- feeling dizzy
- shaking or tremors
- diarrhoea (loose poo)
- dry mouth
- nausea (feeling sick) or vomiting (being sick)
- having pain in your back or joints, or elsewhere
There are other side effects that you can get when taking this medicine; we have only included the most common ones here.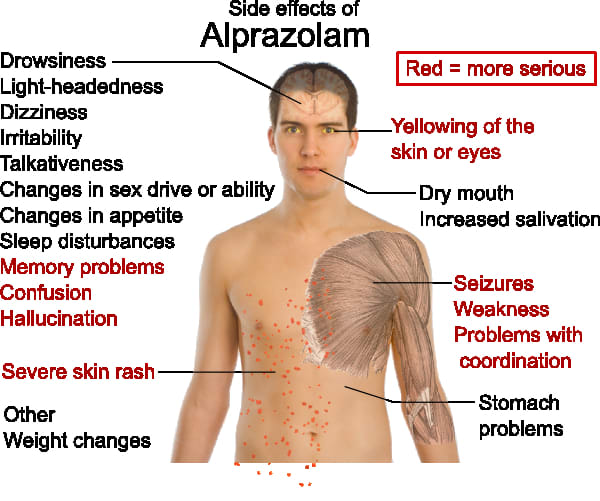
Please look at the leaflet inside your medicine box, or ask a doctor or pharmacist, if you want to know whether you are getting a side effect from your medicine.
If you do get a side effect, please think about reporting it via the Yellow Card Scheme.
Taking lamotrigine
How long will I need to take lamotrigine for?
You and your doctor should talk about how long you need to take lamotrigine before you begin treatment with this medication.
If you take lamotrigine for bipolar disorder you will probably take it for at least six months (any shorter and your old symptoms can come back). If it works for you, you may take it for much longer than that.
You should only take lamotrigine as agreed with your doctor
Make sure that you know your dose. If it is not written on the label, check with your pharmacist or doctor.
You may have to take lamotrigine once or twice a day.
It doesn’t matter what time you take it each day – choose a time that you can always remember.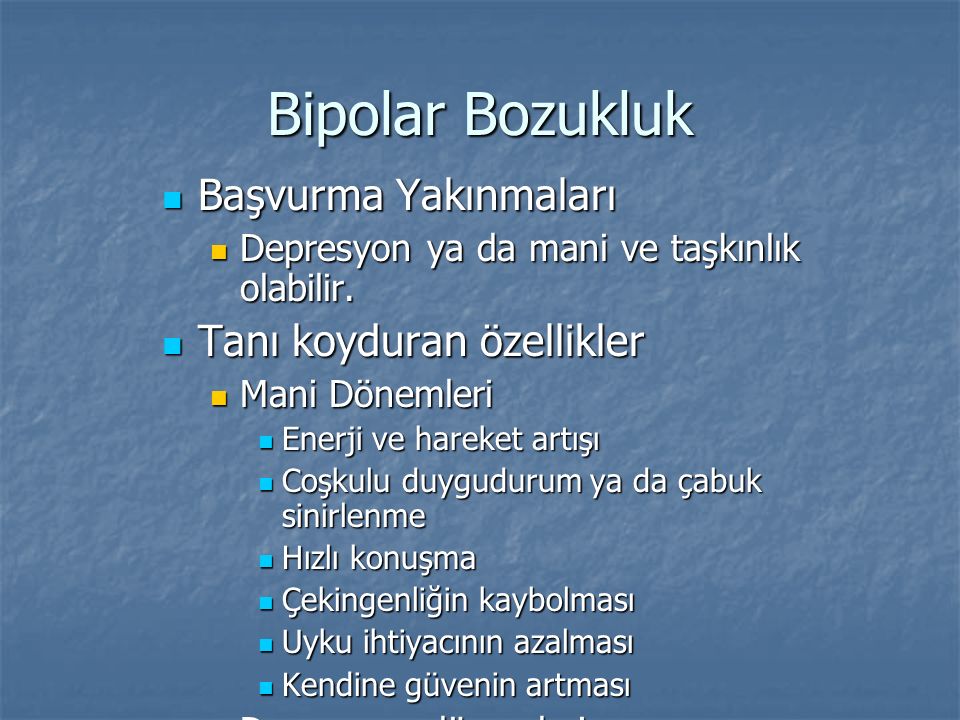 This could be at mealtimes, or when you brush your teeth. You can take it before or after food.
This could be at mealtimes, or when you brush your teeth. You can take it before or after food.
If you are taking the tablets that you swallow whole, wash them down with a glass of water. Do not try and chew them – they will taste unpleasant.
If you are taking the orodispersible tablets (melts), get a glass of cold water and mix the tablet(s) in at least enough water to cover them. You can stir the drink to help them break up. 'Dispersible' doesn’t mean you will get a totally clear solution - it will look a little cloudy. Drink it all, and then add more water to the glass and drink that in order to make sure you get all the medicine in the tablet.
You can also chew the dispersible tablets, but it may help to rinse them down with some cold water.
You can still swallow the dispersible tablets whole with water if you prefer.
What should I do if I miss a dose of lamotrigine?
If you remember later during the day, take it as soon as possible. If you forget to take it by the time of the next dose, just start again with the next dose.
Do not take a double dose.
What will happen if I forget to take my lamotrigine?
If you forget to take your tablets for a few days, you may start getting your old symptoms of low mood back.
Stopping the use of lamotrigine
Although you may not be taking your lamotrigine for seizures (fits), if you stop the medication suddenly, there is a chance you may have a seizure. This is because after taking lamotrigine for some time, your body will have got used to having an anticonvulsant (anti-seizure) medicine on board. Suddenly stopping the use of lamotrigine may therefore cause a seizure. But don't worry - this doesn't mean you are suddenly epileptic.
If you have stopped taking lamotrigine, you need to speak to your doctor so that you can safely start it again and build back up to your dose. It is best to be honest; they will help you get back on track.
If you are thinking of stopping treatment with lamotrigine, talk to your doctor before doing this.
Warnings and safety
Safety headlines
If you have taken more lamotrigine than the dosage recommended by the doctor who prescribed it to you, you must get medical help immediately – even if you do not feel any different.
While taking lamotrigine, some people may think about hurting themselves or taking their own lives. You must go straight to hospital with your medicine if you have any of these thoughts.
Lamotrigine can cause other serious side effects: allergic reactions (difficulty breathing, swelling of your face or throat, itching skin lumps), skin rashes and other serious symptoms. Go to a hospital with your medicine if you get any of these symptoms.
Lamotrigine does not mix well with some other medicines and drugs. The contraceptive Pill can affect the level of lamotrigine in your blood. Talk to your doctor about this if you are on the Pill.
You might feel dizzy or have double vision in the first few days after taking lamotrigine.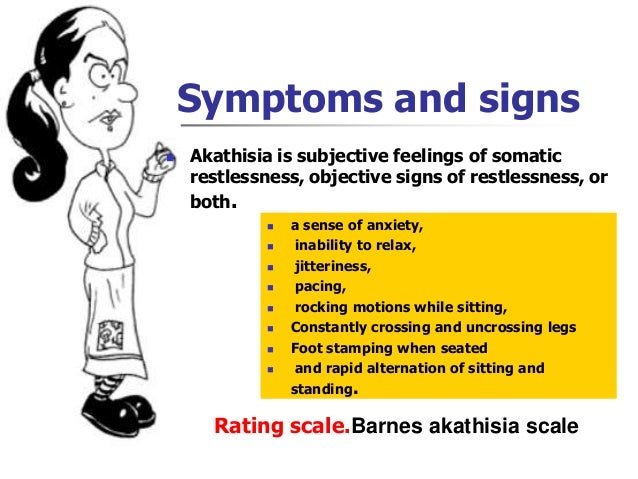 Do not drive a car, ride a bike or operate machines until you see how this affects you.
Do not drive a car, ride a bike or operate machines until you see how this affects you.
Use good contraception while you are taking lamotrigine. If you take it while you are pregnant, it is unlikely to affect the developing baby. However, it can cause symptoms in babies if you breastfeed while taking lamotrigine. Talk to your doctor or midwife about this and get their help.
When to go to the hospital
If you have taken more lamotrigine than the dosage recommended by the doctor who prescribed it to you, you must get medical help immediately – even if you do not feel any different. Go to A&E, and take your medicine with you to show the doctors. Tell them how much you have taken. Get a friend to go with you, if you can, just in case you feel ill on the way.
You might get any of the following symptoms:
- quick, uncontrollable body movements
- clumsiness and lack of co-ordination, causing problems with your balance
- heart rhythm changes
- loss of consciousness, convulsions/seizures (fits) or coma
While taking lamotrigine some people may think about hurting themselves or have thoughts of taking their own lives. This can happen to anyone, including people who are under 25. These thoughts may happen or get worse in the first few weeks of taking the medicine. You must go straight to hospital with your medicine if you have any of these thoughts and tell the doctor that you are taking lamotrigine. There are other medications you can take instead.
This can happen to anyone, including people who are under 25. These thoughts may happen or get worse in the first few weeks of taking the medicine. You must go straight to hospital with your medicine if you have any of these thoughts and tell the doctor that you are taking lamotrigine. There are other medications you can take instead.
You should also go to a doctor or hospital straight away if you get any of the following symptoms:
- skin rashes or redness with blisters and peeling skin around the mouth, nose, eyes and groin/sex organs (genitals)
- peeling of large areas of skin (up to 30% - almost a third – of your body surface)
- ulcers in the mouth, throat, nose or around your groin/sex organs (genitals)
- red or swollen eyes
- a high temperature (fever), flu-like symptoms or drowsiness
- swelling around your face
- swollen glands in your neck, armpit or groin
- unexpected bleeding or bruising
- your fingers turning blue
- a sore throat
- more infections (such as colds) than usual
If these reactions occur, they tend to be during the first eight weeks of taking lamotrigine.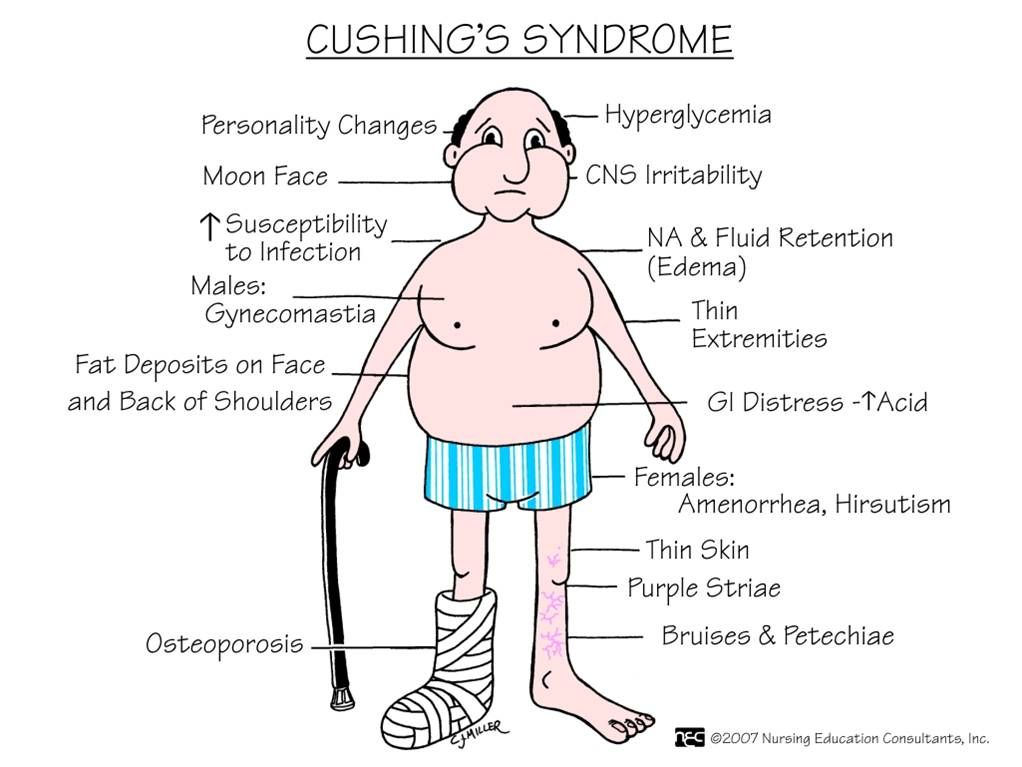
Side effects of lamotrigine
Side effects of lamotrigine
Some side effects that appear should get better after a few days. If they do not, you should go back to your doctor.
Do not stop taking the tablets until you talk to your doctor, or you may get withdrawal symptoms as well.
Very common side effects of taking lamotrigine (affecting more than one in ten people) include:
- headaches
- skin rashes
Common side effects of taking lamotrigine (affecting up to one in ten people) include:
- feeling aggressive, agitated or irritable
- feeling sleepy, tired or drowsy
- insomnia (having difficulty sleeping)
- feeling dizzy
- shaking or tremors
- diarrhoea (loose poo)
- dry mouth
- nausea (feeling sick) or vomiting (being sick)
- having pain in your back or joints, or elsewhere
There are other side effects that you can get when taking this medicine; we have only included the most common ones here.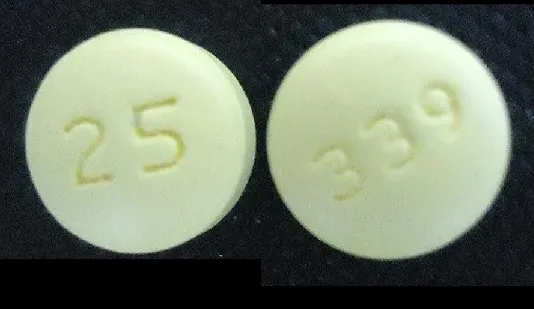
Please look at the leaflet inside your medicine box, or ask a doctor or pharmacist, if you want to know whether you are getting a side effect from your medicine.
If you do get a side effect, please think about reporting it via the Yellow Card Scheme.
The information on this page was reviewed by the College of Mental Health Pharmacy in March 2020.
Visit the CMHP websiteCMHP. College of Mental Health Pharmacy
Uses, Dosages, Common Side Effects, and Interactions
Lamictal (lamotrigine) is an anti-seizure medicine approved to treat epilepsy in children and adults and to delay mood episodes in people with bipolar I disorder. The most common side effects include dizziness, headache, vomiting and rash. The drug has a black box warning for life-threatening skin rashes.
GlaxoSmithKline developed Lamictal, and the U.S. Food and Drug Administration approved it in 1994.
Even though it’s only approved for epilepsy and as maintenance medicine to delay mood episodes in people with bipolar I, some medical providers prescribe it to treat other conditions off-label — uses not approved by the FDA.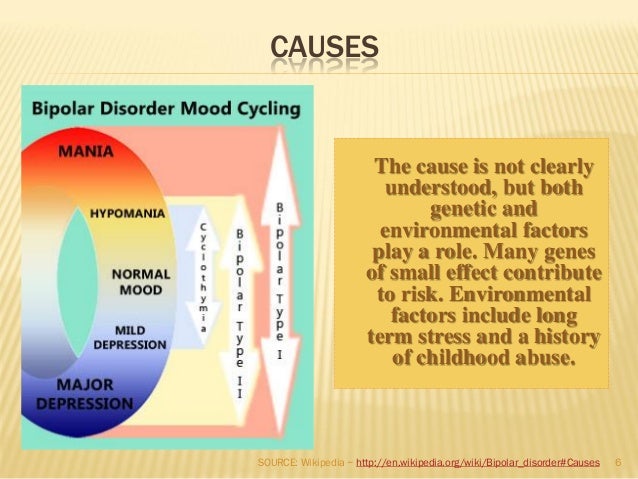
Off-label uses include:
- Panic disorder
- Anxiety
- Migraines and headaches
- Rapid-cycling bipolar depression
- Binge eating disorder
- Borderline personality disorder
- Posttraumatic stress disorder (PTSD)
Lamictal XR, the extended-release version of Lamictal, is not approved for patients younger than 13. It’s only approved for treating certain types of seizures.
In January 2020, Taro Pharmaceuticals, a manufacturer of generic Lamictal, issued a recall for one lot of lamotrigine because it was contaminated with a small amount of enalapril maleate — a blood pressure and heart failure drug that may cause birth defects.
Researchers in 2022 published results on a generic version of extended-release lamotrigine and found the drug to be bioequivalent to the brand name medication.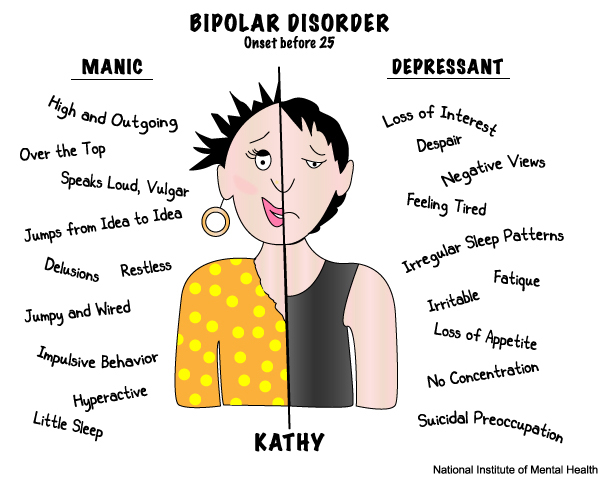
How It Works
Researchers believe Lamictal works by slowing down electrical signals and inhibiting certain chemicals in the brain that cause brain cells to signal too quickly. When brain cells work too fast, it causes seizures. By slowing down these brain signals, lamotrigine may help to reduce seizure episodes.
In people with bipolar disorder, the medication helps to reduce mood swings, though researchers aren’t sure how the drug actually works.
Recommended Dosages
Lamictal comes in several forms and strengths. Depending on the reason for treatment, the recommended dosage is different.
Forms and Strengths
- Tablets: 25 mg, 100 mg, 150 mg, and 200 mg
- Tablets for oral suspension: 2 mg, 5 mg, and 25 mg
- Orally disintegrating tablets: 25 mg, 50 mg, 100 mg, and 200 mg
- Extended release tablets: 5 mg, 50 mg, 100 mg, 200 mg, 250 mg, and 300 mg
Patients typically take Lamictal once or twice a day, and it can be taken with or without food.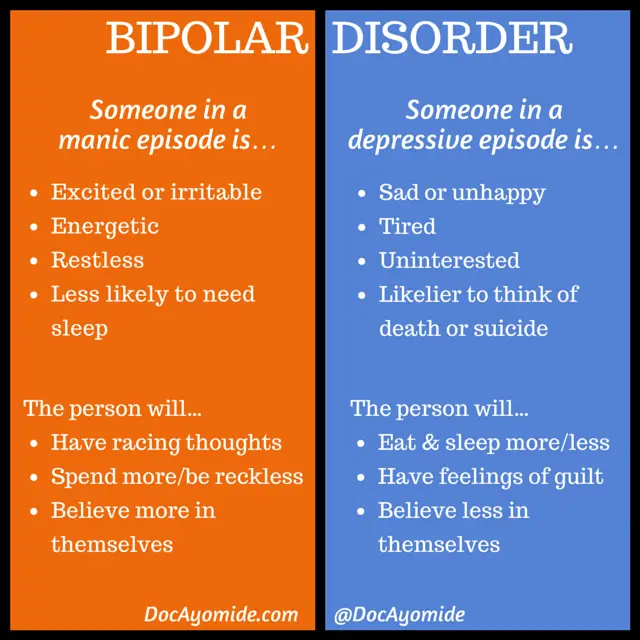 If taking Lamictal XR, make sure to take the pills whole and don’t crush, cut or chew them.
If taking Lamictal XR, make sure to take the pills whole and don’t crush, cut or chew them.
The medication starts at a low dose. Then, the dose gets higher over the course of several weeks. People who are taking the drug with other drugs for seizures take lower doses. They may take it every other day when beginning treatment.
Common Side Effects
Researchers studied Lamictal in clinical trials that included thousands of patients in several groups. Across these studies, researchers defined common side effects as those that occurred in 10 percent or more of patients using the drug for epilepsy and five percent or more of patients using the drug for bipolar disorder.
Common side effects of Lamictal (lamotrigine) include:
- Ataxia (impaired balance or coordination)
- Back pain, abdominal pain
- Blurred vision
- Diarrhea
- Diplopia (double vision)
- Dizziness
- Fatigue
- Headache
- Insomnia
- Nausea
- Pharyngitis
- Rash
- Rhinitis (inflammation of membranes in the nose)
- Somnolence (drowsiness)
- Vomiting
- Xerostomia (dry mouth)
The most common side effects in children were infection, vomiting, diarrhea, accidental injury, fever, abdominal pain and tremor.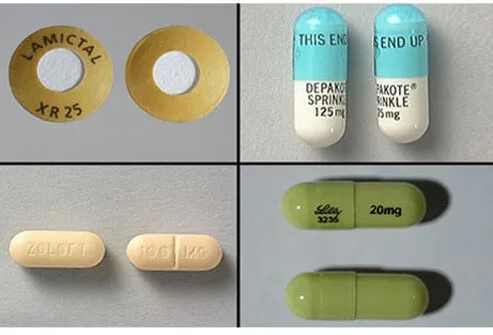
In clinical trials, the most common side effects that caused people to drop out of the trial included: rash, headache, dizziness and impaired balance or coordination.
Serious Side Effects
There have been reports of serious side effects linked to Lamictal, but these side effects are rare, according to the drug’s label. These range from serious skin rashes to death.
Skin Rashes
In clinical trials, 11 of 3,348 adults with epilepsy who received Lamictal had a serious rash that led to hospitalization and discontinuation. Researchers received postmarketing reports of rash-related deaths, but the numbers were too few to estimate the exact rate.
Serious rashes that led to hospitalization were: Stevens-Johnson syndrome — a serious, blistering rash — angioedema, toxic epidermal necrolysis and rashes associated with multiorgan hypersensitivity.
Hemophagocytic Lymphohistiocytosis (HLH)
HLH is a potentially life-threatening syndrome caused by overactivation of the immune system.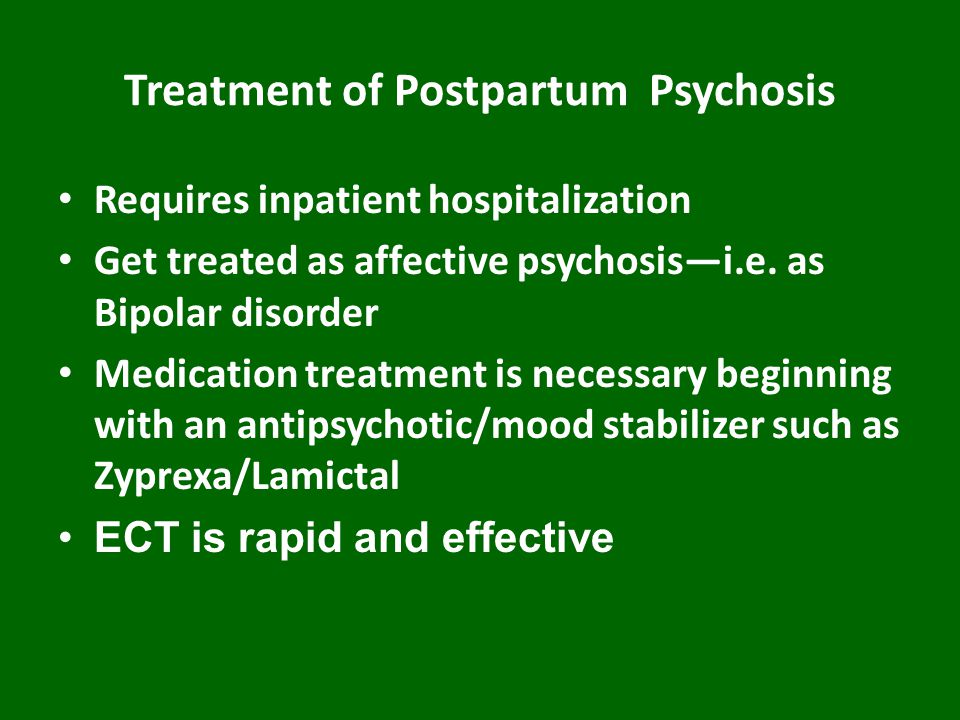 The overactivation causes severe inflammation throughout the body. In April 2018, the FDA released a warning that Lamictal can cause HLH.
The overactivation causes severe inflammation throughout the body. In April 2018, the FDA released a warning that Lamictal can cause HLH.
HLH usually starts with a high fever and rash. It causes problems with blood cells and internal organs such as the lungs, kidneys and liver. It usually starts within 8 to 24 days after starting treatment.
Multiorgan Hypersensitivity Reactions and Organ Failure
Multiorgan hypersensitivity reactions, also known as drug reaction with eosinophilia and systemic symptoms (DRESS), have occurred. This is a potentially fatal drug reaction.
Symptoms include fever, rash, and other organ problems. It sometimes resembles a viral infection. Report these symptoms to your medical provider right away.
Blood Problems
Some people who took Lamictal had abnormal blood cell counts such as neutropenia, leukopenia, anemia, thrombocytopenia, pancytopenia, and, rarely, aplastic anemia and pure red cell aplasia.
Suicidal Thoughts or Behaviors
Taking Lamictal may increase the risk of suicidal thoughts or behaviors.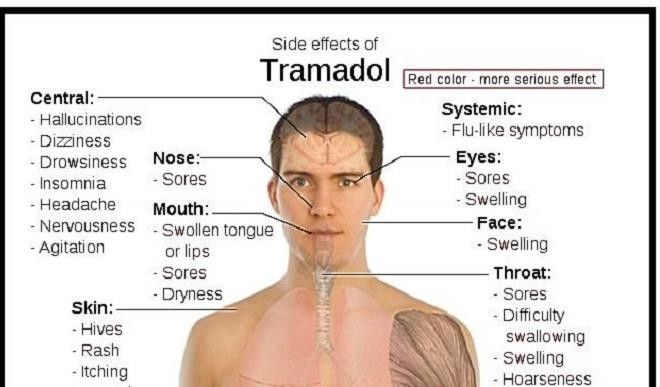 In studies of anti-epileptic drugs (AED) such as Lamictal, patients who took one type of drug had about twice the risk of suicidal thoughts and behaviors compared to people who took a placebo. These symptoms may start as early as one week after starting treatment.
In studies of anti-epileptic drugs (AED) such as Lamictal, patients who took one type of drug had about twice the risk of suicidal thoughts and behaviors compared to people who took a placebo. These symptoms may start as early as one week after starting treatment.
Aseptic Meningitis
Taking Lamictal increases the risk of aseptic meningitis — inflammation of the membrane covering the spinal cord and brain. Symptoms include rash, fever, vomiting, nausea and stiffness and soreness in the neck. Symptoms usually appear anywhere from one day to about a month after starting therapy.
Withdrawal Seizures
Patients taking Lamictal should not abruptly stop treatment. Patients with epilepsy may experience an increase in seizure frequency and people with bipolar disorder may develop seizures. Slowly weaning off the drug for at least two weeks is recommended.
Drug Interactions
Lamictal’s drug label lists several drugs that may increase or decrease the drug’s blood concentration. This could lead to less effective medication or an increase in side effects if the concentration is too high.
This could lead to less effective medication or an increase in side effects if the concentration is too high.
This is not a complete list of potential drug interactions. Make sure you tell your medical provider about all medications, supplements and herbs you take.
Drugs that interact with Lamictal include:
- Oral contraceptives with ethinylestradiol and levonorgestrel decrease lamotrigine concentration and decrease levonorgestrel.
- Carbamazepine and carbamazepine epoxide decreases lamotrigine concentration and may increase carbamazepine epoxide levels.
- Lopinavir/ritonavir decreases lamotrigine concentration.
- Atazanavir/ritonavir decreases lamotrigine concentration.
- Phenobarbital/primidone decreases lamotrigine concentration.
- Phenytoin decreases lamotrigine concentration.
-
Rifampin decreases lamotrigine concentration.
- Valproate increases lamotrigine concentration two fold. Some studies suggest taking these drugs together increases the risk of potentially fatal drug-induced skin rashes.
Special Precautions
Make sure you talk to your medical provider about any allergies you have, medications you take or preexisting health conditions. Lamictal might not be safe or effective for everyone.
Before taking Lamictal:
- Tell your doctor and pharmacist if you are allergic to lamotrigine or any ingredients in the tablets. For example, some formulas may include lactose.
- Tell your doctor or pharmacist about the medications you take, especially drugs in the interactions list or other drugs used to treat epilepsy.
- Tell your doctor if you use medications that contain female hormones such as birth control or hormone replacement therapy (HRT).
-
Tell your doctor if you have or have ever had lupus or any other autoimmune disease in which the immune system attacks healthy tissues and organs; a blood disorder; mental health conditions or kidney or liver disease.
- Tell your doctor if you plan to be pregnant or are pregnant. Call your doctor right away if you become pregnant while taking lamotrigine.
- Tell your doctor if you are breastfeeding or plan to breastfeed. Lamotrigine may pass to your baby through breast milk. Tell your doctor if your baby has interrupted breathing, poor sucking or unusual sleepiness.
- Know that this medication can cause sleepiness and/or dizziness. Don’t operate machinery or drive until you know how Lamictal affects you.
-
Know that you may experience changes in your mental health. This medication may cause thoughts of suicide, panic attacks, agitation, new or worsening irritability, restlessness, anxiety, dangerous impulses, depression, insomnia, aggressive behavior, abnormally excited moods and other unusual changes in mood. Tell another person close to you about these symptoms so they can help you look out for them. Tell your doctor right away if you experience changes in mood or mental health.

Lamictal Facts
Please seek the advice of a medical professional before making health care decisions.
TELL US WHAT YOU THINK
Did You Find Drugwatch Helpful?
Yes No
Thank you for your feedback. Do you have any thoughts you'd like to share about Drugwatch.com?
This article changed my life!
This article was informative
I have a question
How can we improve this page?
This article contains incorrect information
This article doesn't have the information I'm looking for
I have a question
How can we improve this page?
Thank You for Your Feedback
We appreciate your feedback. One of our content team members will be in touch with you soon.
We appreciate your feedback. One of our content team members will be in touch with you soon.
0015 Lamictal . Be carefully and be sure to specify the information on section Composition in the instructions for the drug Lamictal directly from the package or from the pharmacist at the pharmacy.more...
Lamotrigine
Formulations of
The information provided in section Formulations of Lamictal is based on data from another medicine with exactly the same composition as medicine Lamictal . Be carefully and be sure to specify the information in section Release form in the instructions for the drug Lamictal directly from the package or from the pharmacist at the pharmacy.
more.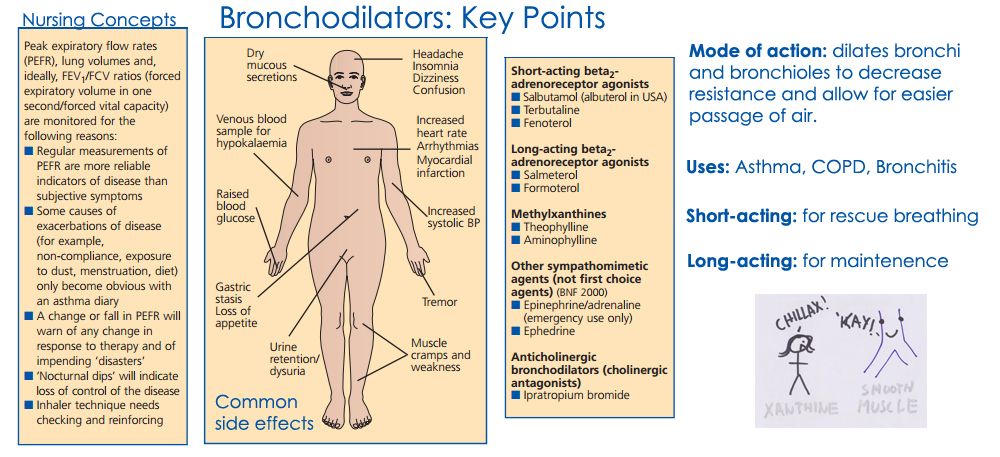 ..
..
Tablets: light yellowish brown tablets, square, with rounded corners.
25 mg dose: "GSEC7" is embossed on one side and "25" on the other.
50 mg dose: "GSEC1" is embossed on one side and "50" on the other.
100 mg dose: "GSEC5" is embossed on one side and "100" on the other.
Soluble/chewable tablets: white or off-white tablets with a blackcurrant scent.
5 mg dose: oblong, biconvex, embossed with "GS CL2" on one side and "5" on the other side. Small blotches may be noted.
25mg dose: square with rounded corners, raised square with "25" on one side and "GS CL5" stamped on the other side. Small blotches may be noted.
100mg dose: square with rounded corners, raised square with "100" on one side and "GS CL7" stamped on the other side. Small blotches may be noted.
Therapeutic indications
The information provided in section Therapeutic indications Lamictal is based on data from another medicine with exactly the same composition as Lamictal . Be carefully and be sure to check the information under section Therapeutic indications in the instructions for the drug Lamictal directly from the package or from the pharmacist at the pharmacy.
Be carefully and be sure to check the information under section Therapeutic indications in the instructions for the drug Lamictal directly from the package or from the pharmacist at the pharmacy.
more...
Partial and generalized seizures, including tonic-clonic and associated with Lennox-Gastaut syndrome (in adults and children), bipolar disorders in adults over 18 years of age with predominantly depressive phases.
Dosage and Administration
The information provided in section Dosage and Administration Lamictal is based on data from another medicine with exactly the same composition as Lamictal . Be carefully and be sure to clarify the information in section Dosage and Administration in the instructions for the drug Lamictal directly from the package or from the pharmacist at the pharmacy.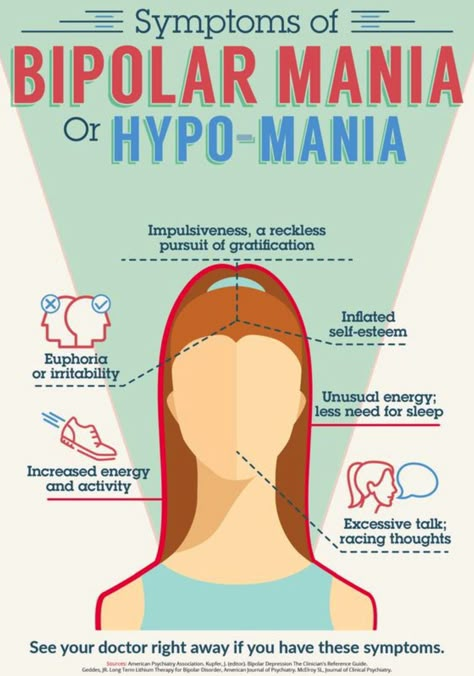
more...
Epilepsy: Adults and children over 12 years of age not treated with sodium valproate Initial dose 25 mg once daily for 2 weeks, then 50 mg once daily for 2 weeks, then increased by 50–100 mg every 1-2 weeks until the optimal therapeutic effect is achieved. Maintenance dose - 100-200 mg / day in 1 or 2 doses (some patients require a dose of 500 mg / day).
Scheme for increasing doses with lamotridrida monotherapy in adults and children over 12 years old
| 1-2 weeks | 3-4 weeks | supporting dose |
| 25 mg 1 time per day | 50 mg 1 time per day 1 time day | 100–200 mg/day in 1 or 2 divided doses. To achieve a therapeutic effect, doses may be increased by 50-100 mg every 1-2 weeks |
For patients receiving sodium valproate, initial dose of 25 mg every other day for 2 weeks, then 25 mg daily for the following 2 weeks, after which the dose is increased by a maximum of 25-50 mg / day every 1-2 weeks until the optimal therapeutic effect is achieved. Maintenance dose - 100-200 mg / day in 1 or 2 doses.
Maintenance dose - 100-200 mg / day in 1 or 2 doses.
Patients taking antiepileptic drugs that induce liver enzymes with or without other antiepileptic drugs (with the exception of sodium valproate), initial dose - 50 mg 1 time per day for 2 weeks, then 100 mg / day in 2 doses for 2 weeks. Then the dose is increased by a maximum of 100 mg every 1-2 weeks until the optimal therapeutic effect is achieved. The maintenance dose to achieve the optimal therapeutic effect is 200-400 mg / day in 2 divided doses. Some patients may need a dose of 700 mg/day to achieve the desired effect.
Scheme for increasing doses in combined therapy in adults over 12 years old
| Therapy | Dose |
| Lamictal and Valproot in combination with other anti -epileptic drugs | |
| 3–4 weeks | 25 mg/day |
| Maintenance dose | 100–200 mg in 1 or 2 doses (dose should be increased by 25–50 mg 2 weeks before reaching maintenance) |
| Lamictal and antiepileptic drugs that induce hepatic enzymes (phenytoin, carbamazepine, phenobarbital, primidone) with or without other antiepileptic drugs (excluding valproate): | |
| 1-2 weeks | |
| 3–4 weeks | 100 mg/day in 2 doses |
| Maintenance dose | 200–400 mg/day in 2 doses (dose should be increased by 100 mg every 1–2 weeks until maintenance dose is reached) |
Children 2 to 12 years of age receiving sodium valproate with or without other antiepileptic drugs starting dose of 0.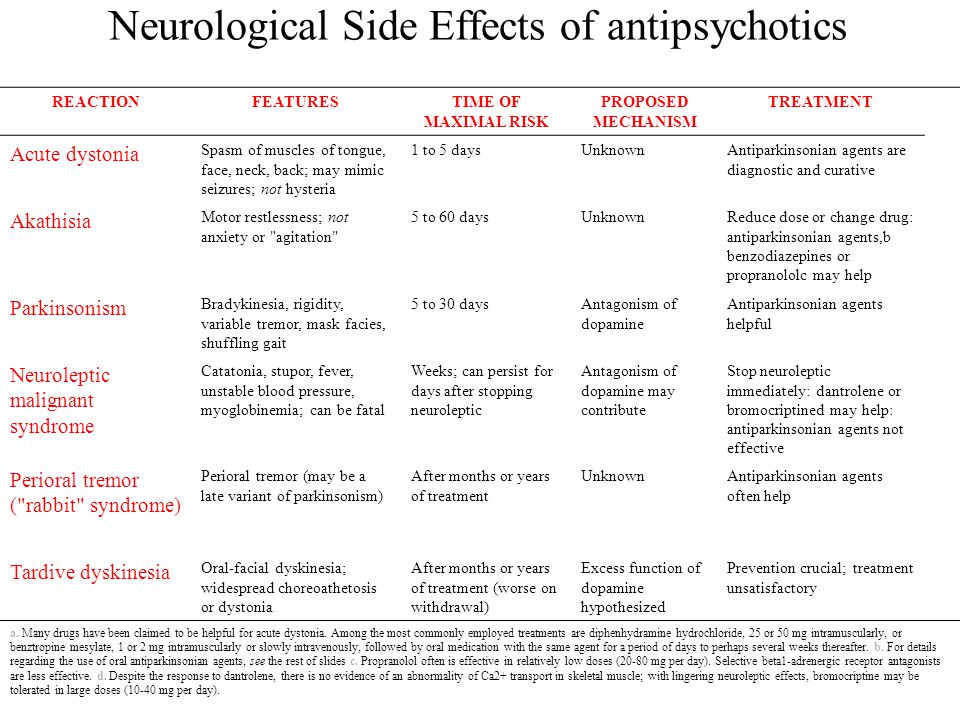 15 mg/kg once daily for 2 weeks; then - 0.3 mg / kg 1 time per day for 2 weeks. Then the dose is increased by 0.3 mg / kg every 1-2 weeks until the optimal therapeutic effect is achieved. Maintenance dose - 1-5 mg / kg / day in 1 or 2 doses. The maximum daily dose is 200 mg.
15 mg/kg once daily for 2 weeks; then - 0.3 mg / kg 1 time per day for 2 weeks. Then the dose is increased by 0.3 mg / kg every 1-2 weeks until the optimal therapeutic effect is achieved. Maintenance dose - 1-5 mg / kg / day in 1 or 2 doses. The maximum daily dose is 200 mg.
For patients taking antiepileptic drugs that induce liver enzymes, with or without other antiepileptic drugs (with the exception of sodium valproate), initial dose - 0.6 mg / kg / day in 2 doses for 2 weeks, then - 1.2 mg / kg / day in 2 doses for 2 weeks. Then the dose is increased by a maximum of 1.2 mg / kg every 1-2 weeks until the optimal therapeutic effect is achieved. The average maintenance dose to achieve the optimal therapeutic effect is 5–15 mg / kg / day in 2 divided doses. The maximum daily dose is 400 mg. To achieve optimal effect in children, it is necessary to systematically monitor body weight in order to adjust doses in accordance with changes in the body weight of the child.
Scheme of increased doses in combined therapy in children from 2 to 12 years old
| Therapy | Dose |
| Lamictal and valproate in combination with other anti -epileptic drugs or without them | |
| 3-4 weeks | 0. 3 mg/kg/day 3 mg/kg/day |
| Maintenance dose | Increase the dose by 0.3 mg/kg every 1-2 weeks until maintenance 1 -5 mg / kg (in 1 or 2 doses), but not more than 200 mg / day |
| Lamictal and antiepileptic drugs that induce hepatic enzymes (phenytoin, carbamazepine, phenobarbital, primidone), with or without other antiepileptic drugs (excluding valproate) | |
| 1–2 weeks | /kg in 2 doses|
| 3–4 weeks | 1.2 mg/kg in 2 doses 15 mg/kg (in 2 doses), but not more than 400 mg/day |
Bipolar disorders (to prevent the development of a depressive episode). Inside, chewing, dissolving in a small amount of water or swallowing whole with water.
Dose escalation schedule to achieve a maintenance daily stabilization dose in adults (over 18 years of age) for bipolar disorder
| Therapy | Doses | |
| 0114 1-2 weeks | 50 mg/day 5 | |
| 3-4 weeks | 100 mg/day in 2 doses | |
| 5 Week | 200 mg/day in 2 doses||
| 6 stabilizing dose)* | 300 mg | |
| Week 7 | if necessary, increase the dose to 400 mg in 2 doses | |
Lamictal in combination with antiepileptic drugs, the nature of the interaction of which is unknown.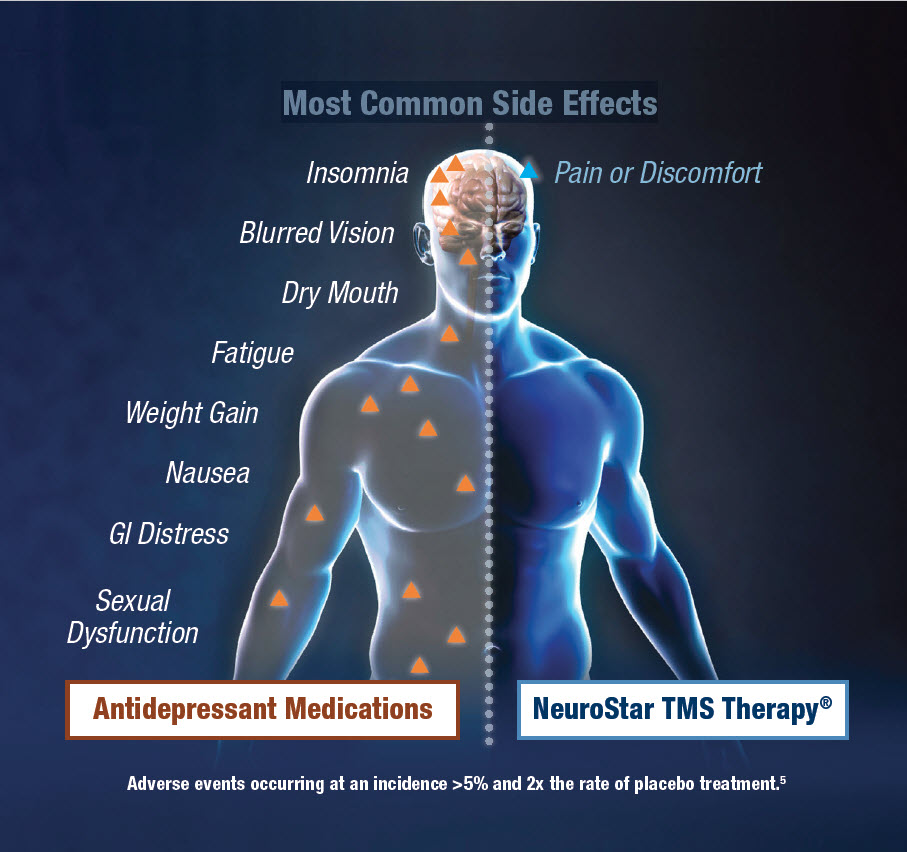 Monotherapy with Lamictal 5 Monotherapy with Lamictal 5 | ||
| 1-2 weeks | 25 mg/day | |
| 3-4 weeks | 50 mg/day in reception | |
| 100 mg/day in 1-2 reception of reception of acceptance of acceptance | ||
| Week 6 (stabilization dose)* | 200 mg/day in 1-2 doses | |
, liver enzyme inhibitors (including sodium valproate), 25 mg every other day for 2 weeks, then - 25 mg daily for 2 weeks, then - 50 mg / day in 1 or 2 doses for 1 week; stabilizing dose - 100 mg / day in 1 or 2 doses (varies depending on the clinical effect). The maximum dose is 200 mg/day.
Lamictal therapy in combination with antiepileptic drugs that induce liver enzymes (carbamazepine, phenobarbital), without sodium valproate, initial dose - 50 mg once a day for 2 weeks, then 100 mg / day in 2 divided doses for 2 weeks The dose is increased by 5 weeks to 200 mg/day in 2 doses and up to 300 mg/day by 6 weeks.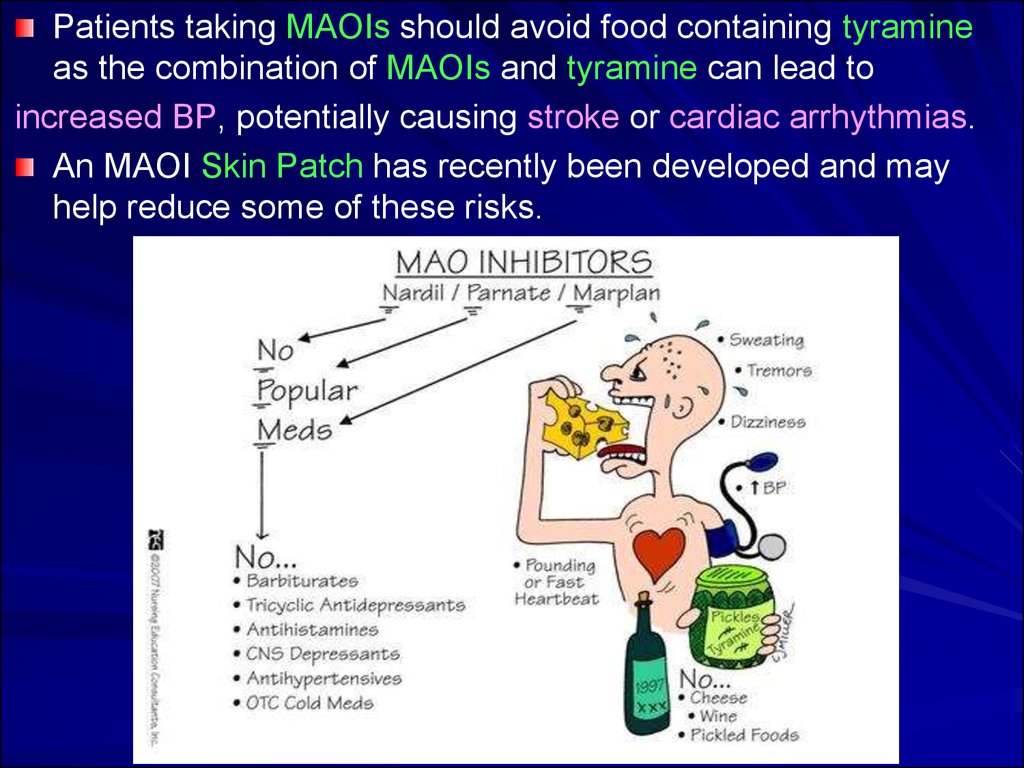 To achieve the optimal therapeutic effect - 400 mg / day in 2 doses, starting from 7 weeks.
To achieve the optimal therapeutic effect - 400 mg / day in 2 doses, starting from 7 weeks.
Therapy with Lamictal and drugs with an unknown interaction pattern (lithium, bupropion). Monotherapy with Lamictal: initial dose - 25 mg / day for 2 weeks, then 50 mg / day in 1 or 2 doses for 2 weeks. The dose should be increased to 100 mg/day for 5 weeks. To achieve the optimal therapeutic effect, a dose of 200 mg / day is required in 1 or 2 doses.
Once the daily maintenance stabilization dose is reached, other psychotropic drugs may be discontinued.
Lamictal therapy after discontinuation of antiepileptic drugs, liver enzyme inhibitors (including sodium valproate): after discontinuation of sodium valproate, the stabilizing dose is doubled, not exceeding 100 mg / week.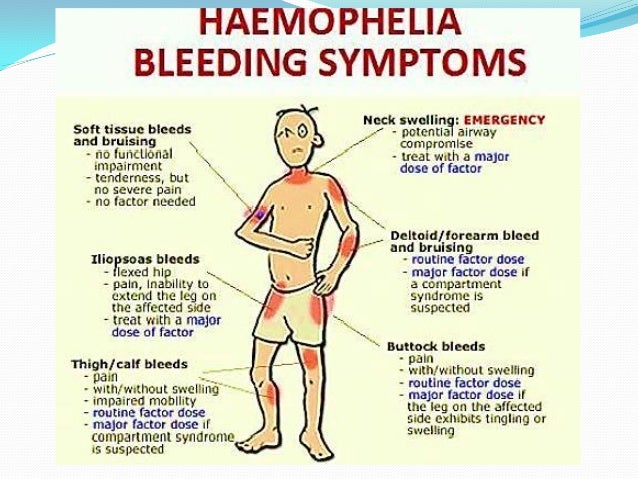 For example, a stabilizing dose of 100 mg/day is increased to 200 mg/day in the first week, and a dose of 200 mg/day in 2 divided doses is maintained in the second and third weeks. If necessary, the dose can be increased to 400 mg / day.
For example, a stabilizing dose of 100 mg/day is increased to 200 mg/day in the first week, and a dose of 200 mg/day in 2 divided doses is maintained in the second and third weeks. If necessary, the dose can be increased to 400 mg / day.
Lamictal therapy after discontinuation of antiepileptic drugs that induce liver enzymes (carbamazepine), depending on the initial maintenance dose: the dose of Lamictal is gradually reduced over 3 weeks.
Lamictal therapy after discontinuation of psychotropic drugs or other antiepileptic drugs, the nature of the interaction of which with lamotrigine is unknown (lithium preparations, bupropion): the same maintenance dose is maintained.
Dosing regimen for lamotrigine in bipolar disorder after adding other drugs to therapy
| Therapy | Dose, mg/day | |||
Addition of antiepileptic drugs, liver enzyme inhibitors (sodium valproate), depending on the initial dose of lamotrigine: at a stabilizing dose of 200 mg / day, in the first week - reduce it to 100 mg / day, in the second, third week and then - save 100 mg / day.![]() At a dose of 300 mg/day, reduce to 150 mg/day in the first week and then keep unchanged, at a dose of 400 mg/day, reduce to 200 mg/day in the first week and then keep unchanged.
At a dose of 300 mg/day, reduce to 150 mg/day in the first week and then keep unchanged, at a dose of 400 mg/day, reduce to 200 mg/day in the first week and then keep unchanged.
Addition of antiepileptic drugs that induce hepatic enzymes (carbamazepine) in patients not receiving sodium valproate, depending on the initial dose of lamotrigine: at a dose of 200 mg / day, keep it unchanged in the first week, increase to 300 in the second mg / day, in the third and further - increase to 400 mg / day.
At a dose of 150 mg/day, keep it unchanged for the first week, increase to 225 mg/day for the second week, and increase to 300 mg/day for the third and beyond. At a dose of 100 mg/day, keep it unchanged for the first week, increase to 150 mg/day for the second week, and increase to 200 mg/day for the third and beyond.
Addition of other psychotropic or antiepileptic drugs, the nature of the interaction of which with lamotrigine is unknown: maintain a maintenance dose of 200 mg / day in 2 doses (from 100 to 400 mg).
In patients with hepatic impairment, the initial, escalating, and maintenance doses should be reduced by ~50% and 75% in patients with moderate (stage B) and severe (stage C) hepatic impairment, respectively. In the future, they should be adjusted depending on the clinical effect. In case of impaired renal function, a reduction in the maintenance dose is recommended. Patients over 65 years of age do not need to change the dosing regimen. There are no recommendations for dosing the drug for children under 18 years of age.
Contraindications
The information provided in section Contraindications Lamictal is based on data of another medicine with exactly the same composition as the medicine Lamictal . Be carefully and be sure to check the information on section Contraindications in the instructions for the drug Lamictal directly from the package or from the pharmacist at the pharmacy.
more...
Hypersensitivity.
Use with caution in renal failure.
Adverse effects
The information provided in section Adverse effects Lamictal is based on data from another medicine with exactly the same composition as the medicine Lamictal . Be be careful and be sure to check the information under section Side effects in the instructions for the drug Lamictal directly from the package or from the pharmacist at the pharmacy.
more...
The following WHO classification was used to grade side effects:
common (>1 in 100 prescriptions), sometimes (<1 in 100 prescriptions) and rare (<1 in 1000 prescriptions).
From the side of the skin and subcutaneous tissue: often - skin rash, mostly maculopapular in nature; rarely - erythema multiforme exudative (including Stevens-Johnson syndrome), toxic epidermal necrolysis (Lyell's syndrome).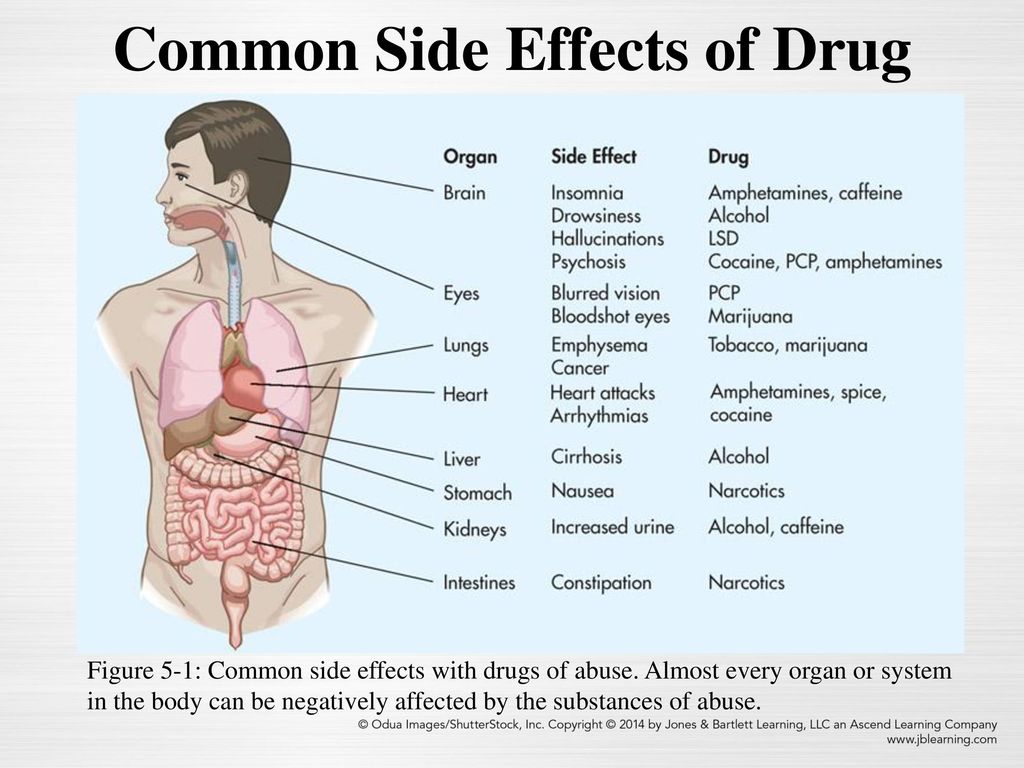
Skin rash usually appears within the first 8 weeks of starting lamotrigine and resolves when lamotrigine is discontinued.
In rare cases, severe skin reactions may develop, which in most cases resolve after discontinuation of the drug (some patients may remain scarring), as well as potentially life-threatening conditions such as Stevens-Johnson syndrome and Lyell's syndrome.
From the side of the hematopoietic and lymphatic system: rarely - neutropenia, leukopenia, anemia, thrombocytopenia, pancytopenia, aplastic anemia, agranulocytosis.
Hematological disorders may or may not be associated with hypersensitivity syndrome and DIC.
From the immune system: rarely - hypersensitivity syndrome with manifestations such as fever, lymphadenopathy, facial edema, hematological disorders, liver damage, DIC syndrome, multiple organ failure.
Early signs of hypersensitivity (eg fever and lymphadenopathy) may occur even in the absence of skin rash. In such a case, the patient should be immediately examined and lamotrigine should be discontinued unless there is another obvious reason for such symptoms.
In such a case, the patient should be immediately examined and lamotrigine should be discontinued unless there is another obvious reason for such symptoms.
Skin rashes are part of the hypersensitivity syndrome, the severity of which can vary, in rare cases up to the development of multiple organ failure and disseminated intravascular coagulation.
From the side of the central nervous system: often - irritability, anxiety, headache, fatigue, drowsiness, insomnia, dizziness, imbalance, tremor, nystagmus, ataxia.
Sometimes aggressiveness.
Rarely - tics, hallucinations, confusion, agitation, imbalance, movement disorders, extrapyramidal disorders, choreoathetosis, increased seizures.
From the side of vision: often - diplopia, blurred vision, conjunctivitis.
From the digestive system: often - disorders of the gastrointestinal tract, incl. nausea, vomiting and diarrhea; rarely - increased liver function tests, impaired liver function, liver failure.
From the musculoskeletal system: often - arthralgia, back pain; rarely - lupus-like syndrome.
Others: abrupt withdrawal of Lamictal, as well as other antiepileptic drugs, can provoke an increase in seizures associated with the development of a withdrawal syndrome.
It has been established that with insufficient effectiveness of the drug, incl. with status epilepticus, rhabdomyolysis, multiple organ dysfunction, disseminated intravascular coagulation may occur - sometimes with a fatal outcome.
Overdose
The information provided in section Overdose Lamictal is based on data of another medicine with exactly the same composition as the medicine Lamictal . Be carefully and be sure to clarify the information in section Overdose in the instructions for the drug Lamictal directly from the package or from the pharmacist at the pharmacy.![]()
more...
Symptoms: dizziness, headache, drowsiness, vomiting, nystagmus, ataxia, impaired consciousness, coma.
Treatment: gastric lavage, detoxification therapy.
Pharmacodynamics
Provided under section Pharmacodynamics Lamictal information is based on data from another medicine with exactly the same composition as medicine Lamictal . Be carefully and be sure to specify the information on section Pharmacodynamics in the instructions for the drug Lamictal directly from the package or from the pharmacist at the pharmacy.
more...
Lamotrigine is a voltage-gated sodium channel blocker, inhibits the abnormal release of glutamic acid (an amino acid that plays a key role in the development of epileptic seizures), and also inhibits glutamate-induced depolarization.
Pharmacokinetics
The information provided in section Pharmacokinetics Lamictal is based on data of another medicine with exactly the same composition as the medicine Lamictal . Be carefully and be sure to specify the information on section Pharmacokinetics in the instructions for the drug Lamictal directly from the package or from the pharmacist at the pharmacy.
more...
Lamotrigine is rapidly and completely absorbed from the intestine. C max in plasma is reached approximately 2.5 hours after oral administration. T max slightly increases after a meal, but the level of absorption remains unchanged.
Pharmacokinetics is linear at doses up to 450 mg.
The degree of binding of lamotrigine to plasma proteins is about 55%. The volume of distribution is 0.92–1.22 l/kg.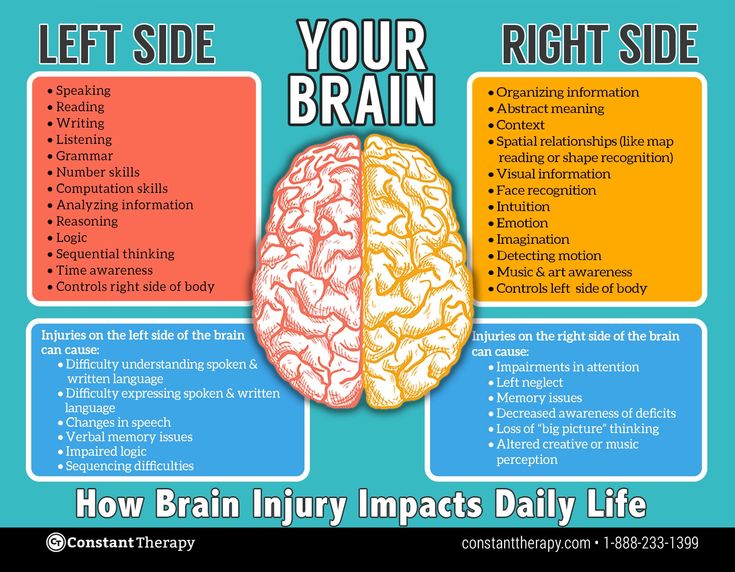
The enzyme glucuronyl transferase is involved in the metabolism of lamotrigine. Lamotrigine does not affect the pharmacokinetics of other antiepileptic drugs.
In adults, Cl lamotrigine averages 39±14 ml/min.
Lamotrigine is metabolized to glucuronides, which are excreted in the urine. Less than 10% of the drug is excreted in the urine unchanged, about 2% - with faeces. Clearance and T 1/2 do not depend on the dose.
Cl of lamotrigine, calculated by body weight, is higher in children than in adults; it is highest in children under 5 years of age. In children T 1/2 lamotrigine is usually shorter than in adults.
Available data indicate no significant difference in creatinine clearance in elderly patients compared with younger patients.
The mean Cl values of lamotrigine for patients with chronic renal failure and patients on hemodialysis are 0.42 ml / min / kg (chronic renal failure), 0.33 ml / min / kg (between hemodialysis sessions) and 1.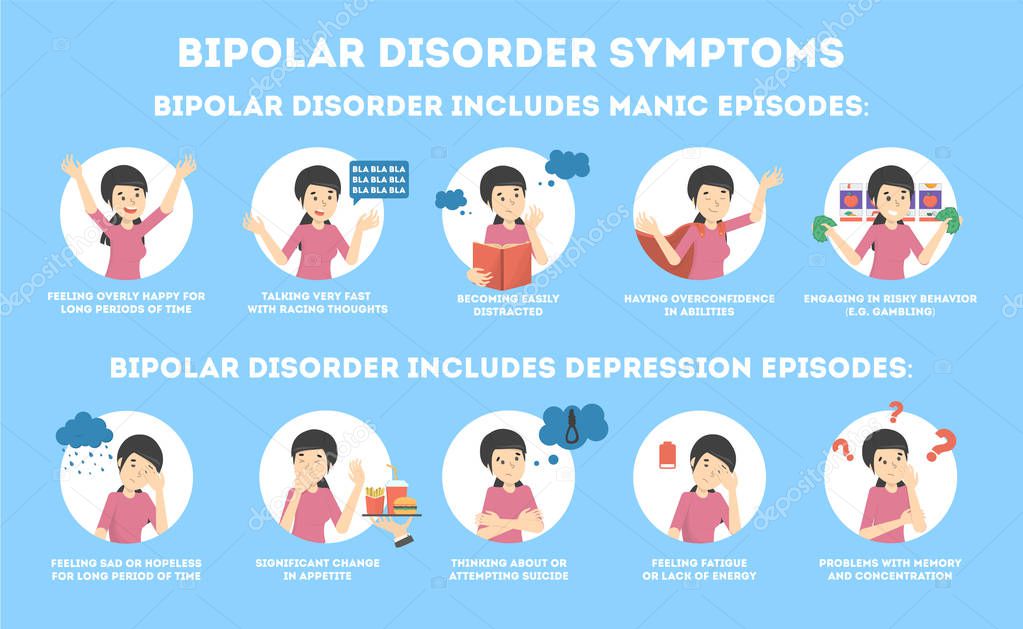 57 ml / min / kg (during hemodialysis). Average T 1/2 is respectively 42.9; 57.4 and 13 hours During a 4-hour hemodialysis session, about 20% of lamotrigine is excreted from the body. Thus, in patients with impaired renal function, the initial dose of lamotrigine is calculated according to the standard antiepileptic drug regimen; for patients with a significant decrease in renal function, a reduction in the maintenance dose is recommended.
57 ml / min / kg (during hemodialysis). Average T 1/2 is respectively 42.9; 57.4 and 13 hours During a 4-hour hemodialysis session, about 20% of lamotrigine is excreted from the body. Thus, in patients with impaired renal function, the initial dose of lamotrigine is calculated according to the standard antiepileptic drug regimen; for patients with a significant decrease in renal function, a reduction in the maintenance dose is recommended.
Mean Cl values of lamotrigine in patients with mild, moderate, and severe hepatic impairment (Child-Pugh stages A, B, and C) are 0.31; 0.24 and 0.1 ml/min/kg, respectively. The initial, escalating and maintenance doses should be reduced by approximately 50% in patients with moderate hepatic impairment (stage B) and by 75% in severe hepatic impairment (stage C). The initial and increasing doses should be adjusted depending on the clinical effect.
Pharmacological group
The information provided in section Pharmacological group Lamictal is based on data from another medicine with exactly the same composition as the medicine Lamictal . Be carefully and be sure to specify the information on section Pharmacological group in the instructions for the drug Lamictal directly from the package or from the pharmacist at the pharmacy.
Be carefully and be sure to specify the information on section Pharmacological group in the instructions for the drug Lamictal directly from the package or from the pharmacist at the pharmacy.
more...
- Antiepileptics
Interactions
The information provided in section Interactions Lamictal is based on data from another medicine with exactly the same composition as medicine Lamictal . Be carefully and be sure to check the information on section Interaction in the instructions for the medicine Lamictal directly from the package or from the pharmacist at the pharmacy.
more...
Antiepileptic drugs (phenytoin, carbamazepine, phenobarbital, primidone), paracetamol accelerate the metabolism of lamotrigine and shorten its T 1/2 by 2 times.
Since valproate is competitively metabolized by hepatic enzymes, it causes a slowdown in the metabolism of lamotrigine and increases its T 1/2 up to 70 hours in adults and up to 45-55 hours in children.
Dizziness, ataxia, diplopia, blurred vision and nausea may occur when lamotrigine is added to carbamazepine therapy, which disappears when the dose of carbamazepine is reduced.
When added to therapy with anhydrous lithium gluconate 2 g twice daily for 6 days of lamotrigine 100 mg/day, lithium pharmacokinetics are not affected.
Repeated administration of bupropion does not significantly affect the pharmacokinetics of lamotrigine after a single dose, with the exception of a slight increase in AUC for lamotrigine glucuronide.
Storage
The information provided in section Storage Lamictal is based on data from another medicine with exactly the same composition as the medicine Lamictal . Be carefully and be sure to specify the information on section Storage in the instructions for the drug Lamictal directly from the package or from the pharmacist at the pharmacy.+Lacosamide+(Vimpat).jpg)
more...
In a dry, dark place, at a temperature not exceeding 30 °C.
Keep out of reach of children.
Shelf life of Lamictal ® 3 years.
Do not use after the expiry date which is stated on the packaging.
Packaging and contents
The information provided in section Packaging and contents Lamictal is based on data from another medicine with exactly the same composition as the medicine Lamictal . Be carefully and be sure to check the information on section Packaging and contents of in the instructions for the drug Lamictal directly from the package or from the pharmacist at the pharmacy.
more...
| Tablets | 1 tab. |
| lamotrigine | 25 mg |
| 50 mg | |
| 100 mg | |
| excipients: lactose monohydrate; MCC; sodium starch glycolate type A; povidone; magnesium stearate; iron oxide yellow E172 |
in a blister pack of 10; in a box of 3 blisters.
| Dissolve/chewable tablets | 1 tab. |
| lamotrigine | 5 mg |
| 25 mg | |
| 100 mg | |
| excipients: calcium carbonate; low-substituted hydroxypropyl cellulose; aluminum magnesium silicate; sodium starch glycolate type A; povidone K30; sodium saccharin; blackcurrant flavor 500.009/AP 0551; magnesium stearate |
in a blister of 10 pieces; in a box of 3 blisters.
Use in pregnancy and lactation, fertility
The information provided in section Use in pregnancy and lactation, fertility Lamictal is based on data from another medicine with exactly the same composition as the medicine Lamictal . Be carefully and be sure to check the information under section Use in pregnancy and lactation, fertility in the instructions for the medicine Lamictal directly from the package or from the pharmacist at the pharmacy.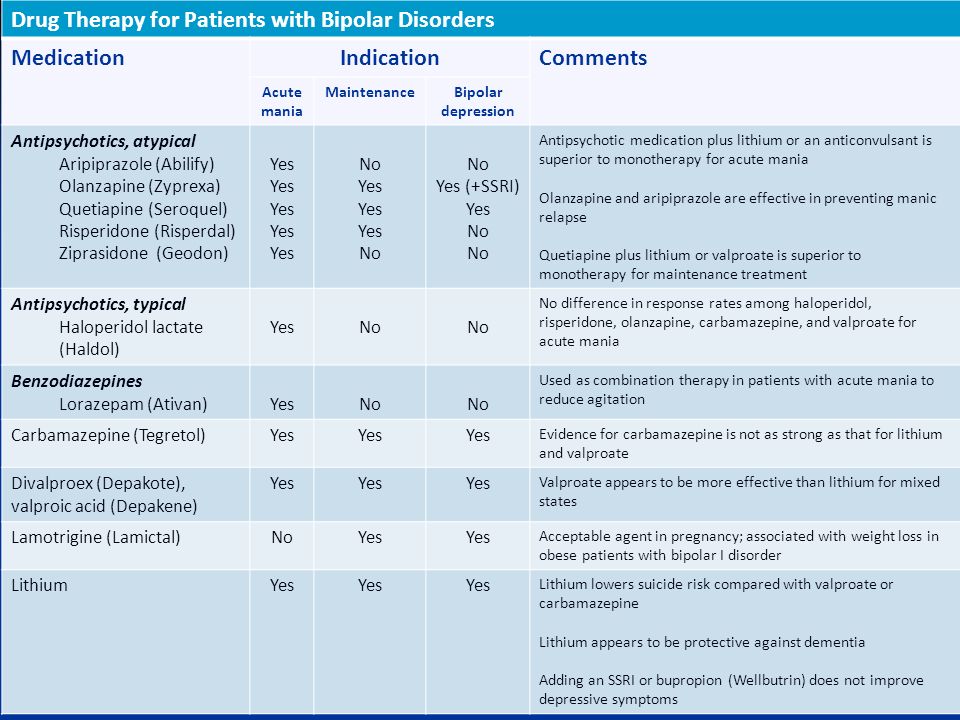
more...
Since lamotrigine is a weak inhibitor of dihydrofolate reductase,
there is at least a theoretical risk of fetal birth defects if taken during pregnancy.
There are insufficient data to assess the safety of lamotrigine in pregnancy.
Currently, information on the use of lamotrigine in lactation is incomplete.
Lamotrigine is found in breast milk at concentrations ranging from 40% to 60% of its plasma concentration. In some breastfed children, plasma concentrations of lamotrigine reach therapeutic levels.
Precautions
The information provided in section Precautions Lamictal is based on data from another medicinal product with exactly the same composition as the medicinal product Lamictal . Be carefully and be sure to clarify the information in section Special instructions in the instructions for the drug Lamictal directly from the package or from the pharmacist at the pharmacy.![]()
more...
There are reports of skin rashes that usually occur within the first 8 weeks of treatment with lamotrigine. In most cases, skin rashes were mild and resolved on their own, but at the same time, serious cases were noted that required hospitalization of the patient and withdrawal of Lamictal (for example, Stevens-Johnson syndrome and toxic epidermal necrolysis). Rash (mild forms) is usually a manifestation of hypersensitivity syndrome and is dose-independent, while Lyell and Stevens-Johnson syndrome are always dose-dependent.
Due to the risk of rash, the initial dose should not be exceeded and the dose increase regimen should not be violated.
Lamictal is a weak inhibitor of dihydrofolate reductase and therefore may interfere with folate metabolism during long-term therapy. However, even with long-term use, lamotrigine did not cause serious changes in hemoglobin, mean volume of formed elements in the blood, serum folate concentration (when taken for up to 1 year) or erythrocytes (when taken for up to 5 years).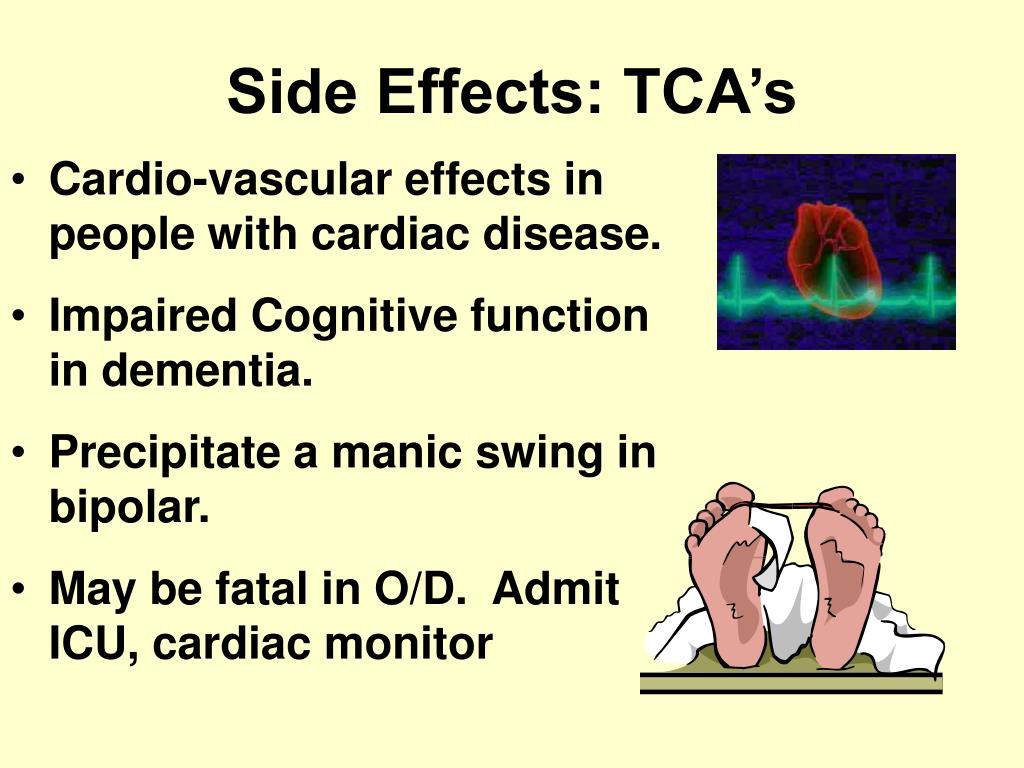
In end-stage renal disease, accumulation of the glucuronide metabolite of lamotrigine is possible, so lamotrigine should be used with caution in patients with renal impairment.
Patients receiving any other drug containing lamotrigine should not take Lamictal without consulting a physician.
If the estimated daily dose is 1-2 mg, Lamictal may be taken at a dose of 2 mg every other day for the first 2 weeks. If the estimated dose is less than 1 mg, Lamictal should not be taken.
In pediatric practice, monotherapy with the drug is not recommended as an initial method of treatment in patients with a primary diagnosis. After an anticonvulsant effect is achieved with combination therapy, the antiepileptic drugs
co-administered with Lamictal can be discontinued and patients can continue treatment with Lamictal as monotherapy.
It is possible that children aged 2 to 6 years will need a maintenance dose at the upper end of the recommended dose range.
General dosing recommendations for epilepsy
Any change in therapy, either with the withdrawal of an antiepileptic drug that was prescribed in conjunction with lamotrigine, or, conversely, with the addition of other antiepileptic drugs to combination therapy, including lamotrigine, must be taken into account the possibility of changing the pharmacokinetics of lamotrigine.
ATC - Anatomical Therapeutic Chemical Classification
Provided in section ATC - Anatomical-Therapeutic-Chemical Classification Lamictal information is compiled on the basis of data on another drug with exactly the same composition as the drug Lamictal . Be carefully and be sure to specify the information on section ATC - Anatomical-Therapeutic-Chemical Classification in the instructions for the drug Lamictal directly from the package or from the pharmacist at the pharmacy.
more...
N03AX09 Lamotrigine
Nosological classification (ICD-10)
Information provided in section Nosological classification (ICD-10) Lamictal is based on data from another medicine with exactly the same composition as 9001 medicine5 Lamictal . Be carefully and be sure to specify the information in section Nosological classification (ICD-10) in the instructions for the medicine Lamictal directly from the package or from the pharmacist at the pharmacy.
more...
- F31 Bipolar affective disorder
- G40.1 Localized (focal) (partial) symptomatic epilepsy and epileptic syndromes with simple partial seizures
- G40.3 Generalized epileptic epilepsy 6 and 9073 4073 Grand mal seizures, unspecified [with or without petit mal seizures]
- G40.
 7 Small seizures [petit mal] unspecified without seizures grand mal
7 Small seizures [petit mal] unspecified without seizures grand mal
Lamictal price
We do not have exact data on the cost of this medicine.
However, we will provide data for each active ingredient
The average cost of Lamotrigine 100 mg per unit in online pharmacies is from $0.46 to $2.5, per package from $34 to $258.
The average cost of Lamotrigine 5 mg per unit in online pharmacies is from $0.62 to $1.28, per pack from $25 to $62.
The average cost of Lamotrigine 25 mg per unit in online pharmacies is from $0.29 to $1.1, per pack from $22 to $162.
The average cost of Lamotrigine 50 mg per unit in online pharmacies is from $0.36 to $1, per pack from $25 to $89.
The average cost of Lamotrigine 150 mg per unit in online pharmacies is from $0.57 to $1.11, per pack from $51 to $135.
The average cost of Lamotrigine 200 mg per unit in online pharmacies is from $0.33 to $1.37, per pack from $32 to $176.
Sources:
- https://www.drugs.com/search.php?searchterm=ru-lamictal
- https://pubmed.ncbi.nlm.nih.gov/?term=ru-lamictal
Find in the country:
A
B
B
g
D
E
K
and
I
K
L
m
M
H
O
2 P
R
S
T
U
F
X
S
S
E
S
I
updated recommendations of the British Association for Psychopharmacology
01/08/2017
Treatment outcomes for bipolar disorder (BD) have been, and still are, modest. However, British experts believe that there is significant potential for improvement if therapy is carried out in accordance with modern recommendations based on evidence-based medicine. This summer, the British Association for Psychopharmacology presented the third update of its evidence-based BD treatment guideline, the key provisions of which we would like to acquaint our readers with.
The quality of the evidence on which recommendations were made was rated from I to IV (descending), and the strength of the recommendations, respectively, by the number of asterisks, from very low (*) to high (****). The provisions, the observance of which, according to the authors, should be the most stringent, they marked with the letter S.
Acute manic episode
Most patients with manic states require short-term medical treatment in an adequate clinical setting (I). A network meta-analysis of randomized controlled trials (RCTs) demonstrated the efficacy of a range of drugs (I). When choosing a drug, it is necessary to take into account its effectiveness and the risk of developing adverse events.
There is currently no alternative psychotherapeutic treatment for acute mania.
For patients not receiving long-term treatment with BR . In the case of severe manic episodes, oral dopamine receptor antagonists, which provide a rapid anti-manic effect, should be considered (****). Thus, a systematic analysis of clinical trial data indicates that haloperidol, olanzapine, risperidone, and quetiapine are highly effective for the short-term relief of symptoms of acute mania. An alternative is valproate, which has a lower risk of developing adverse motor reactions, but they should not be prescribed to women of childbearing age due to the unacceptable risk of a teratogenic effect and a slowdown in the child's intellectual development in the future. It is also possible to use aripiprazole, other antagonists and partial agonists of dopamine receptors, carbamazepine and lithium preparations.
Thus, a systematic analysis of clinical trial data indicates that haloperidol, olanzapine, risperidone, and quetiapine are highly effective for the short-term relief of symptoms of acute mania. An alternative is valproate, which has a lower risk of developing adverse motor reactions, but they should not be prescribed to women of childbearing age due to the unacceptable risk of a teratogenic effect and a slowdown in the child's intellectual development in the future. It is also possible to use aripiprazole, other antagonists and partial agonists of dopamine receptors, carbamazepine and lithium preparations.
If an agitated patient requires parenteral therapy to correct behavior without full consent, dopamine antagonists/partial agonists and GABAergics (benzodiazepines) should be used (S).
It is recommended to prescribe the minimum effective dose of drugs (S). Do not increase the dose of dopamine receptor antagonists just to achieve a sedative effect (S).
For less severe, non-psychotic patients with mania and hypomania, treatment can be extrapolated from mania practice (IV).
In order to quickly induce sleep in agitated hyperactive patients, it is worth considering the additional administration of GABAergic drugs (***).
Whenever possible, the choice of therapy should be based on the patient's previous experience and preferences.
Antidepressants (i.e. drugs approved for the treatment of unipolar depression) during a manic episode are usually discontinued by tapering the dose (**).
If treatment of mania has been successful, long-term BR therapy should be considered (S).
For patients with a manic episode that developed during long-term therapy. If the current condition is caused by insufficient efficacy of basic therapy, it is recommended to increase the dose of the drug used to the maximum well tolerated (S). Increasing the dose of dopamine receptor antagonists and partial agonists or valproate may be sufficient to relieve manic symptoms (IV).
In the case of treatment with lithium preparations, it should be ensured that its concentration in the blood serum is in the target range.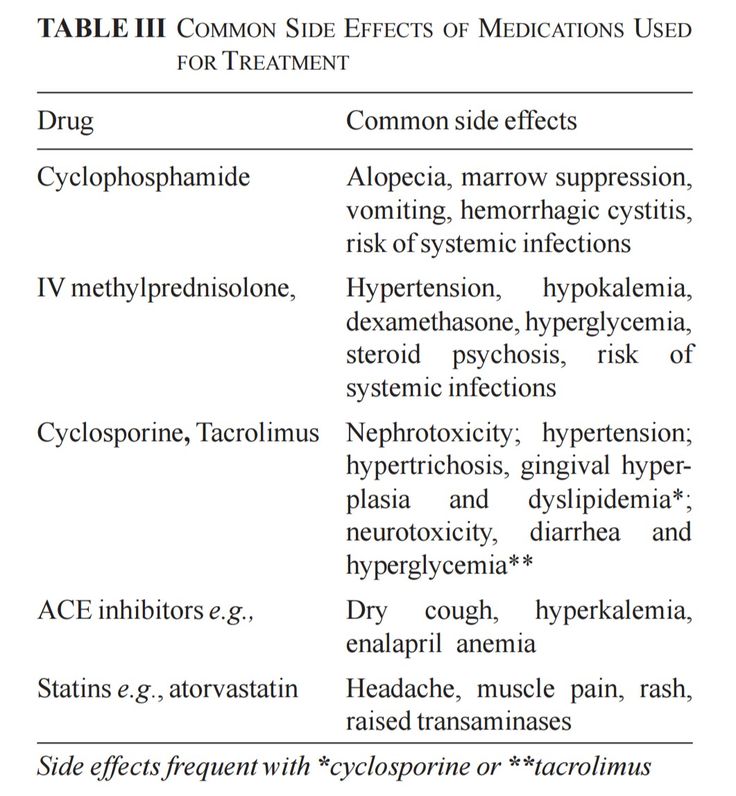 Try increasing the dose until a concentration of 0.6-0.8 mmol/L (mEq/L) is reached. A concentration of 0.8-1.0 mmol/L may be more effective, but long-term maintenance is associated with an increased risk of side effects (I).
Try increasing the dose until a concentration of 0.6-0.8 mmol/L (mEq/L) is reached. A concentration of 0.8-1.0 mmol/L may be more effective, but long-term maintenance is associated with an increased risk of side effects (I).
If the patient is on lithium, consider adding a dopamine receptor antagonist/partial agonist or valproate to therapy (****).
If the manic episode was the result of the patient's non-compliance with medical recommendations, the cause should be determined and adequate measures taken (S). For example, if insufficient adherence to therapy is due to adverse events, it is necessary to reduce the dose of the drug (if the side effect is dose-dependent) or transfer the patient to an alternative treatment regimen with better tolerance. If non-compliance is deliberate and not related to tolerability of therapy, long-term use of lithium preparations is not indicated due to the risk of developing mania or depression if they are discontinued (I).
If symptoms cannot be controlled with optimal doses of first-line drugs and/or the manic state is extremely severe, another treatment should be added.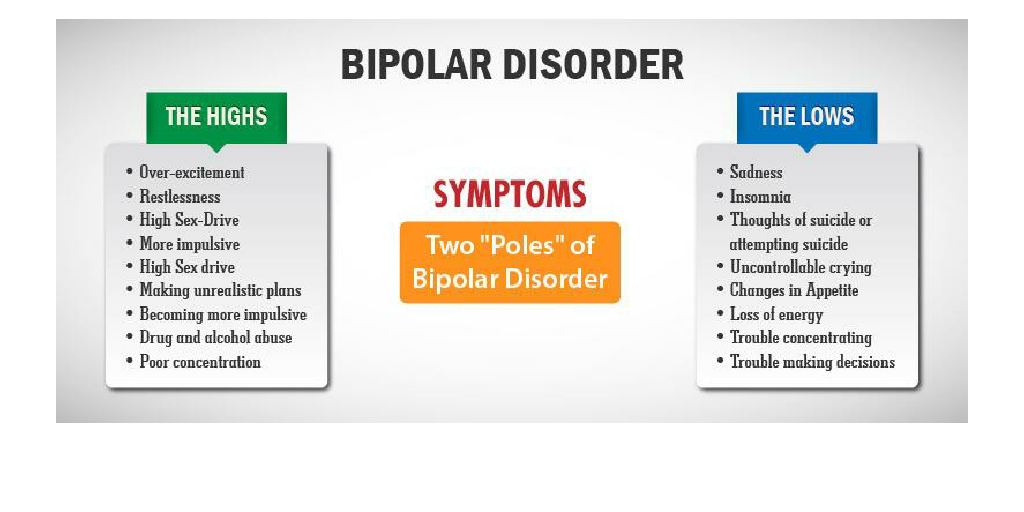 Consider a combination of lithium or valproate with a dopamine antagonist/partial agonist (****).
Consider a combination of lithium or valproate with a dopamine antagonist/partial agonist (****).
Clozapine is considered in more refractory cases (**).
Electroconvulsive therapy may be considered in patients with very severe or treatment-resistant mania, in cases where the patient prefers this type of treatment, in severe mania during pregnancy (***).
Manic or hypomanic episode with mixed features. DSM-5 proposes the term "mixed traits" instead of the definition of "mixed episode" used in DSM-IV. A secondary analysis of the results of studies in relation to the effectiveness of the treatment of mixed episodes indicates that the treatment of episodes such as manic is adequate.
Use of psychoactive substances. If substance use may have contributed to a manic or hypomanic episode, consider medical support for drug withdrawal (S).
Termination of therapy for an acute episode. Drug withdrawal should be planned based on the need for further long-term maintenance treatment (S). Many drugs are effective not only for the treatment of manic states, but also for the prevention of their relapse (I).
Many drugs are effective not only for the treatment of manic states, but also for the prevention of their relapse (I).
The dose of drugs used only for the intensive treatment of mania, upon reaching a complete remission, is gradually reduced (for 4 weeks or more) until complete withdrawal (IV). Remission often occurs after 3 months, but mood stabilization may take 6 months or more.
Any drugs used in addition to symptomatic treatment (sedation, sleep induction) should be discontinued immediately after improvement (S).
Acute depressive episode
Network meta-analysis of RCTs showed the effectiveness of a limited range of drugs with different pharmacodynamics and different evidence bases.
There is no consensus on the appropriateness of the use of antidepressants, that is, drugs that are effective in unipolar depression (IV).
Most of the data come from studies involving patients with type I BD, but it seems logical to extrapolate them to people with type II BD.
For patients not receiving long-term BR treatment. Consider quetiapine, lurasidone, or olanzapine (***). An important benefit of dopamine receptor antagonists is their antimanic properties (I).
The use of antidepressants in BD is currently not well understood. Only the combination of fluoxetine with olanzapine has the necessary evidence base for BD (***). The widespread use of other antidepressants in patients with BD is the result of an extrapolation of data obtained in the treatment of unipolar depression. However, when prescribing antidepressants to patients with a history of mania, anti-manic agents (dopamine receptor antagonists, lithium preparations, valproates) should be added to them (S).
Initial treatment with lamotrigine (with gradual dose escalation) should be considered, usually as an adjunct to drugs to prevent relapse of mania (****).
Electroconvulsive therapy should be considered in patients with increased risk of suicide, treatment resistance, psychosis, severe depression during pregnancy, or life-threatening exhaustion (***). If possible, reduce previous polypharmacy, which can cause an increase in the seizure threshold.
If possible, reduce previous polypharmacy, which can cause an increase in the seizure threshold.
If symptoms of depression are mild, despite a limited evidence base, lithium preparations may be used, especially as a preparation for long-term treatment (**).
Family CBT or Interpersonal Rhythm Therapy should be considered as adjunctive treatment, if possible, as this may help shorten the duration of the acute episode (**).
For patients with a depressive episode that developed during long-term therapy. Confirm that the current long-term treatment regimen is capable of preventing relapse of mania (lithium drugs, valproates, dopamine antagonists/partial agonists), assess the adequacy of drug doses and/or serum lithium concentration (S). If possible, current stressors should be eliminated.
If the patient does not respond to the optimization of long-term treatment, and the symptoms of depression are sufficiently pronounced, it is necessary to start the treatment indicated in the paragraph above. The following are recommendations for the treatment of resistant depression.
The following are recommendations for the treatment of resistant depression.
Drug choice for a depressive episode. Preferable treatment options cannot be determined based on the available studies (IV).
In the treatment of depression, there is a risk of transition to a manic state or unstable mood (I). And although such a phase change is characteristic of the disease itself, with monotherapy with antidepressants, the risk increases. Non-selective monoamine reuptake inhibitors (venlafaxine, duloxetine, amitriptyline, and imipramine) are more likely to induce mania than selective drugs, especially selective serotonin (II) reuptake inhibitors. The risk of developing a manic state while taking antidepressants in combination with antimanic drugs is minimal (I). If an antidepressant is prescribed as monotherapy for type II BD, dose escalation should be gradual and closely monitored by the clinician for early management of adverse reactions such as hypomania, comorbidity, or agitation (IV).
In contrast to the widespread use of antidepressants, lamotrigine is rarely used outside of specialized centers, despite its effectiveness in type I BD and the possibility of use in type II BD.
Long-term therapy should be considered after successful treatment of a depressive episode (S).
Withdrawal of antidepressants. The possibility of gradual withdrawal of antidepressants is considered after achieving complete remission (IV). Depressive episodes in BD are usually shorter than in unipolar depression (I). In the absence of indications for prolongation of therapy, it is worth canceling the antidepressant no earlier than 12 weeks after the start of remission (*). Longer treatment with antidepressants is justified if their withdrawal causes a relapse in the patient.
Treatment of resistant depression. BD patients with depression may show relative or even marked resistance to treatment (I). This means that the patient does not respond to treatment not only with antidepressants, but also with quetiapine, olanzapine, lurasidone and lamotrigine both as monotherapy and in combinations.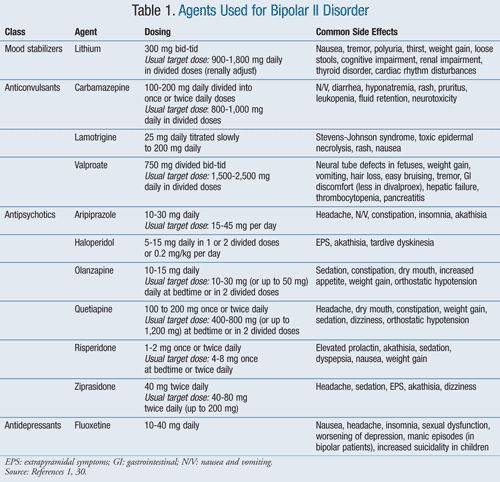 The evidence base for the treatment of such patients with BD is extremely scarce. Electroconvulsive therapy may be a treatment option (***). It is possible to extrapolate the experience of treating unipolar depression using augmentation strategies. Coverage with anti-manic drugs such as lithium, valproate, dopamine antagonists/partial agonists (S) is needed.
The evidence base for the treatment of such patients with BD is extremely scarce. Electroconvulsive therapy may be a treatment option (***). It is possible to extrapolate the experience of treating unipolar depression using augmentation strategies. Coverage with anti-manic drugs such as lithium, valproate, dopamine antagonists/partial agonists (S) is needed.
Psychosocial therapy as initial treatment. There is very little evidence of the effectiveness of psychotherapy alone (without medication) in the treatment of acute bipolar depression. More evidence is needed that this approach is effective (IV).
Long-term treatment
Long-term treatment should be considered even after one severe manic episode, i.e. type I BD (***).
Without active consent to long-term treatment, treatment adherence may be low (I). Extended treatment should be considered, including psychoeducation, motivational and family support, especially in the initial stages of the disease, to model the patient's behavior and help him adhere to the regimen (***).![]()
If the patient has been successfully treated for several years, continued therapy is recommended due to the high risk of relapse (***).
Treatment recommendations for type I BD can be extrapolated to type II BD as clinical studies show similar efficacy (**).
Long-term treatment strategies. Currently, the preferred relapse prevention strategy is continuous rather than intermittent oral therapy.
A network meta-analysis of studies evaluating long-term therapy showed the effectiveness of a limited range of drugs with different pharmacodynamics and different evidence bases in preventing relapses of mania: lithium preparations, olanzapine, quetiapine, long-acting injectable risperidone and valproates. Lamotrigine, lithium, quetiapine, and lurasidone have been shown to be effective in preventing recurrence of depressive episodes.
Although relatively few patients remain in such studies for 6 months or more, there is strong evidence of a high efficacy of lithium in preventing relapse in patients who have not experienced an early response to therapy with these drugs (I).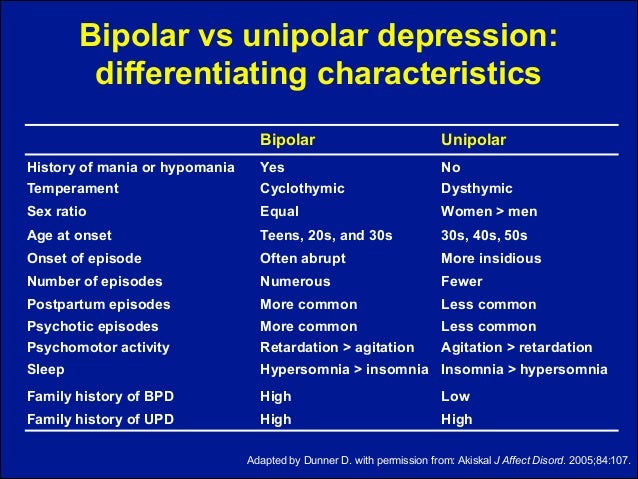
Short-term addition of other drugs (GABA receptor modulators or dopamine receptor antagonists/partial agonists) is necessary if a stress factor is likely or present, early symptoms of relapse (especially insomnia) or severe anxiety (IV). It is worth considering the possibility of providing the patient with these drugs in advance, instructing him on the cases in which they should be used (*). Increasing the doses of long-term therapy drugs instead of additional drugs may also be effective (*).
Due to the fact that the optimal strategy for long-term treatment has not yet been determined, clinicians and patients are involved in clinical studies designed to answer key therapeutic questions (S).
Choice of drug for long-term therapy. In addition to studies on relapse prevention, analysis of treatment results in real clinical practice indicates the effectiveness of such drugs: lithium > valproate > olanzapine > quetiapine > carbamazepine (I).
It is recommended to consider lithium as monotherapy (****).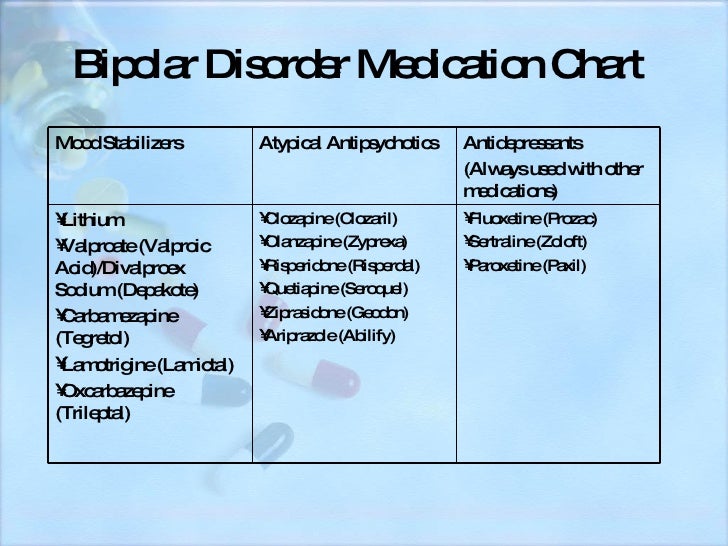 Lithium monotherapy is effective in preventing relapses of manic, depressive and mixed states (I), has a greater evidence base for the prevention of new episodes compared to other agents (I) and a better studied long-term safety profile (I). According to RCTs and observational studies, patients with BD who use lithium preparations are less at risk of suicide and self-harmful behavior (I).
Lithium monotherapy is effective in preventing relapses of manic, depressive and mixed states (I), has a greater evidence base for the prevention of new episodes compared to other agents (I) and a better studied long-term safety profile (I). According to RCTs and observational studies, patients with BD who use lithium preparations are less at risk of suicide and self-harmful behavior (I).
In the treatment of lithium, biochemical monitoring, including the determination of its concentration in blood serum, is mandatory (S). The target range is 0.6-0.8 mmol/L. Lithium concentrations above 0.8 mmol/L are associated with an increased risk of impaired renal function, especially in women (I). Monitoring of lithium concentration in somatically healthy patients should be carried out at intervals of 3 months in the first year of treatment and 6 months thereafter (S).
If lithium is ineffective, poorly tolerated, or non-compliant, other treatment options should be considered: valproate, dopamine antagonists/partial agonists (****).
Often valproates are put on the same level with lithium as "mood stabilizers". The evidence base based on the results of controlled clinical trials is weaker, however, data from real practice indicate a greater effectiveness of valproates compared to other drugs (I). Risk factors in women have been discussed above.
Additional data obtained from studies on the treatment of acute episodes. If a patient experiences a sustained remission of a manic or depressive episode while taking any drug, this may be a reason to use this drug as long-term monotherapy (IV). At the same time, preference will probably be given to dopamine receptor antagonists due to their effectiveness in short-term use, however, the possibility of using lithium preparations as a better alternative should also be considered (IV).
Carbamazepine as a maintenance treatment is less effective than lithium preparations, but can sometimes be used as monotherapy when lithium is ineffective, especially in patients without classic episodes of euphoric mania (II).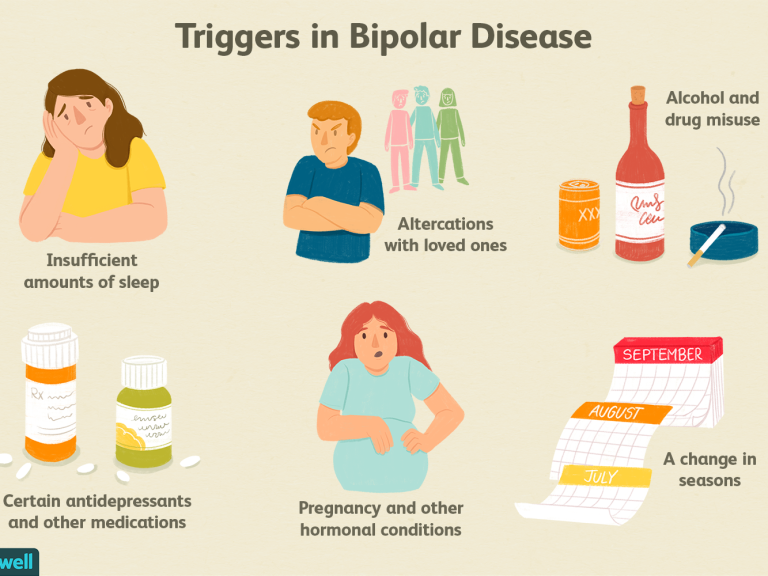 The drug seems to be effective mainly only for the prevention of relapses of manic states (I). Do not forget about drug interactions, which are a big problem in the treatment of carbamazepine. One might consider oxcarbazepine, which is less prone to such interactions (I).
The drug seems to be effective mainly only for the prevention of relapses of manic states (I). Do not forget about drug interactions, which are a big problem in the treatment of carbamazepine. One might consider oxcarbazepine, which is less prone to such interactions (I).
If prophylaxis of relapse of mania is needed, but the patient does not comply with the recommendations for taking the oral drug, or if the parenteral route is preferred, the use of long-acting drugs should be considered (**). There are a large number of long-acting dopamine receptor antagonists/partial agonists such as fluphenazine decanoate, haloperidol decanoate, olanzapine pamoate, risperidone microspheres, paliperidone palmitate, and aripiprazole monohydrate. In RCTs, only risperidone (II) has been shown to be effective. The use of other drugs is based on the class efficacy of dopamine antagonists/partial agonists, extrapolation of the results of their use in oral form and clinical experience (IV).
Lamotrigine and quetiapine can be considered as monotherapy for type II BD (***). Type I BD usually requires a combination of lamotrigine with a long-term antimanic drug (IV).
Type I BD usually requires a combination of lamotrigine with a long-term antimanic drug (IV).
Insufficient efficacy of monotherapy. If a patient fails to respond to monotherapy and subthreshold symptoms or relapses persist, long-term combination therapy is considered. When it comes to symptoms or relapses of mania, a combination of two predominantly anti-manic drugs (i.e., lithium, valproate, dopamine antagonists/partial agonists) would be logical (IV). In case of persisting symptoms or recurrence of depression, a combination of lithium, lamotrigine, quetiapine, lurasidone, or olanzapine (IV) may be appropriate.
The role of antidepressants in the long-term treatment of BD has not been studied in RCTs, but their long-term use appears to be effective in some patients (**).
If clozapine has been shown to be effective in the treatment of resistant mania, continued use is considered (**).
Supportive electroconvulsive therapy may be considered in patients who respond well to it during an acute episode but respond poorly to oral medications (*).
Consider adding psychotherapy if subthreshold symptoms are present (**).
Fast cycling. Conditions that contribute to rapid cycling, such as hypothyroidism or substance use, should be identified and addressed (**).
Gradual withdrawal of antidepressants should also be considered as they may cause cycling (**).
There is no specific treatment for rapid cycling. Many patients with this often debilitating form of BD require a combination of drugs. The countercyclical effect of therapy is evaluated in dynamics over a period of six months or more by monitoring the patient's mood. Ineffective drugs are canceled to avoid unnecessary polypharmacy (S).
Cancellation of long-term treatment . After discontinuation of drugs, there is a risk of relapse even after years of stable remission (II). Thus, the decision to discontinue treatment should be made after assessing the potential risks (S).
The gradual withdrawal of any drug should take at least 4 weeks, and longer if possible (S).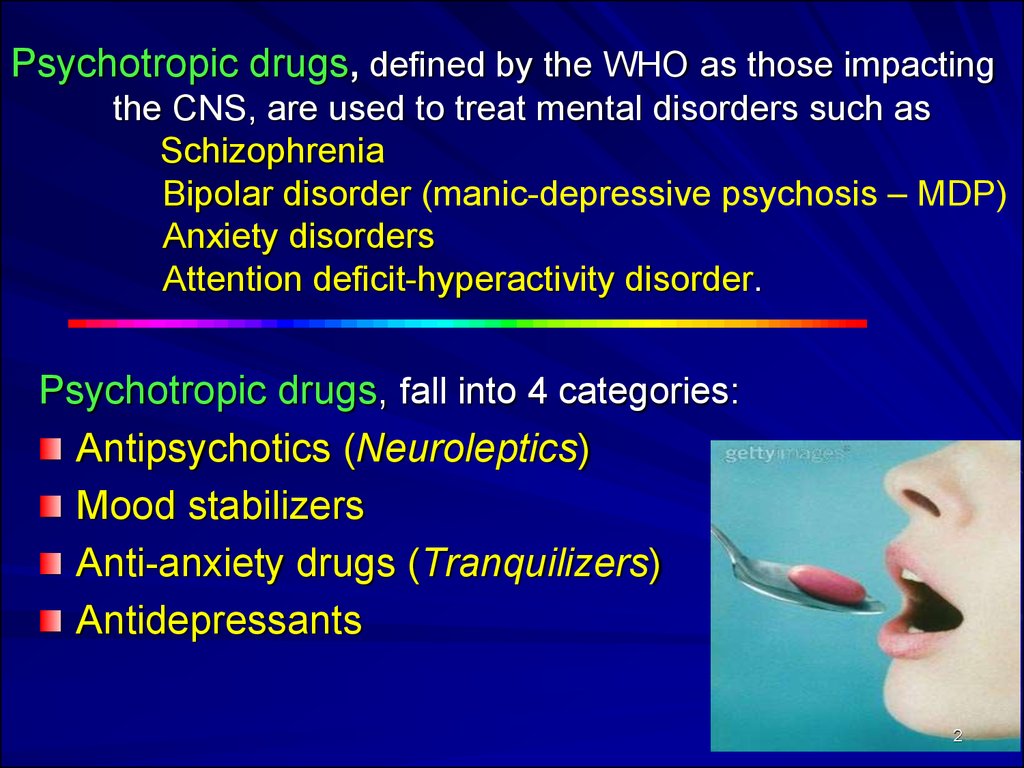 Abrupt withdrawal of lithium preparations is fraught with early relapse of mania (I).
Abrupt withdrawal of lithium preparations is fraught with early relapse of mania (I).
Discontinuation of drugs should not lead to termination of patient follow-up. It is necessary to continue monitoring and develop a plan to recognize and eliminate early signs of a relapse of a manic or depressive state (S).
Specific psychosocial interventions. Psychosocial interventions may improve treatment outcomes, reduce subthreshold symptoms, and reduce the risk of relapse (II). Psychoeducation is an important component of good clinical practice, as without it clinical interaction cannot be effective (S).
Various forms of psychotherapy (family therapy, cognitive behavioral therapy, interpersonal rhythm therapy) have been studied to prevent relapse. Psychological interactions are more effective in the initial stages of the disease (I).
Functional impairment in BD patients may require the use of cognitive and functional remediation strategies (II).
Patient groups provide the patient with support and additional information about BD and its treatment (IV).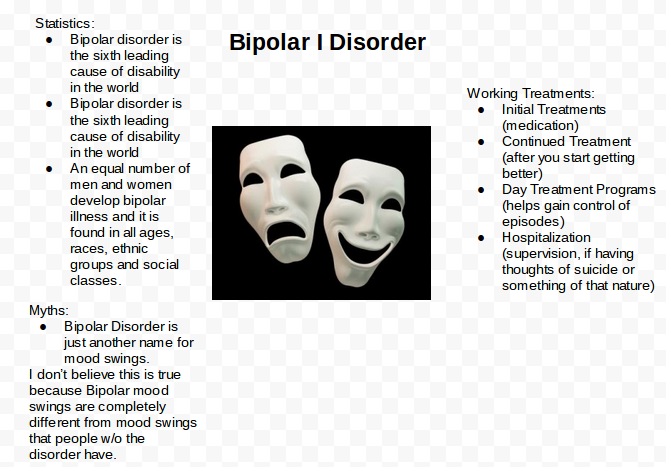
Treatment of alcoholism in patients with BD
In alcoholics, even a modest reduction in alcohol consumption can improve health (I).
To reduce alcohol consumption, the patient should be offered naltrexone or nalmefene in addition to a behavioral therapy program (**).
If naltrexone has not helped the patient stay sober, acamprosate is recommended (**).
If a patient wants to remain sober but acamprosate and naltrexone do not help, disulfiram is considered. However, the patient should be aware of the risks associated with the use of disulfiram and the need to monitor his mood (*).
Treatment of comorbid borderline personality disorder in patients with BD
Patients with comorbidity require treatment for both disorders. In this regard, one should not give preference only to medical treatment (carried out in BD) or only psychotherapy (indicated in borderline conditions) (S). In the absence of appropriate indications, there is no need to cancel or suspend adequate therapy for BD or borderline personality disorder.
Although there are few data supporting the effectiveness of medical treatment of borderline conditions, mood instability common to both pathological conditions can be successfully treated with drugs (lamotrigine, lithium preparations, olanzapine, risperidone, aripiprazole and quetiapine), which improves the course of borderline disorder .
Treatment of anxiety and other comorbid disorders in patients with BD
Treatment of comorbid anxiety disorders, attention-deficit hyperactivity disorder and substance abuse is according to relevant clinical guidelines (*).
Antidepressants should be used with caution (S).
Treatment of BR in selected groups of patients
Manic states in children and adolescents. Aripiprazole is preferred because it is approved for the treatment of type I BD in adolescents (over 13 years of age) (***). In other cases, it is worth adhering to the recommendations for the treatment of BD in adults.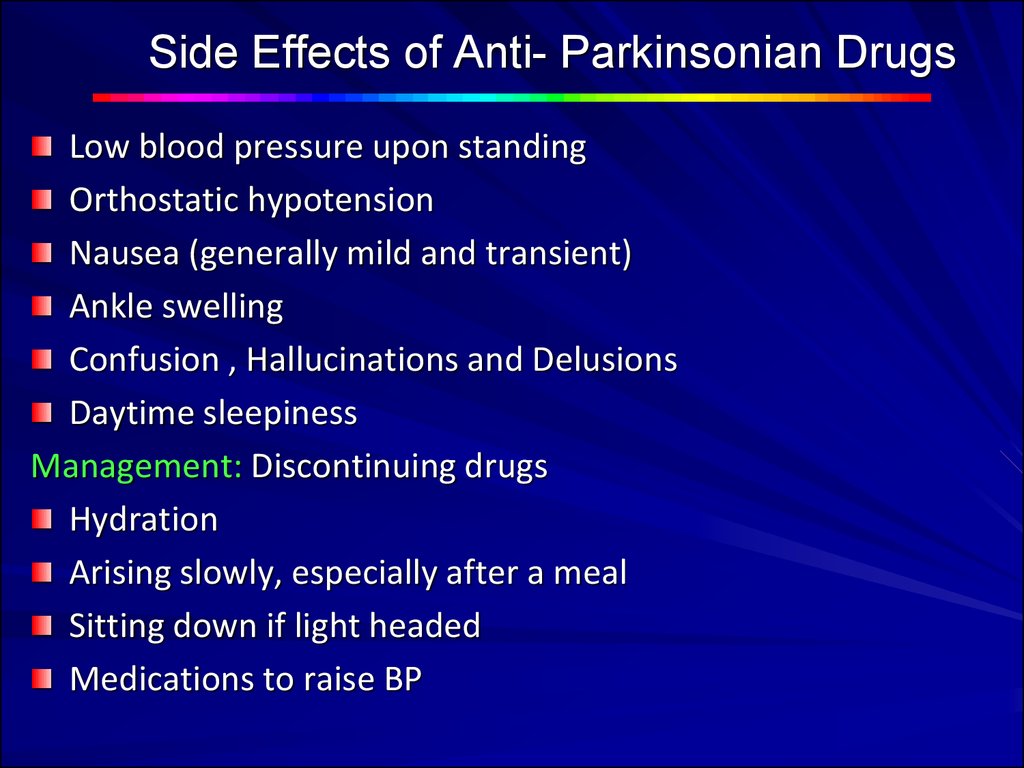 There is evidence that olanzapine and risperidone are effective in adolescents (**).
There is evidence that olanzapine and risperidone are effective in adolescents (**).
Children should be given adequate doses of drugs (S). It is necessary to be aware of the increased risk of side effects, in particular the possible weight gain (S).
Bipolar depression in children and adolescents. Considers medication and psychotherapy based on adult treatment data (*).
Antidepressants are more likely to cause mania in children and adolescents than in adults (II).
Long-term treatment is recommended in young patients because mood relapses and instability can have a detrimental effect on cognitive and emotional function (S).
Elderly patients . If obvious side effects are observed when using normal doses of psychotropic drugs, a dose reduction is considered (*).
Women who can become pregnant. Valproate and carbamazepine may be teratogenic (I). Given the risk/benefit ratio, valproate is contraindicated in women who may become pregnant (I).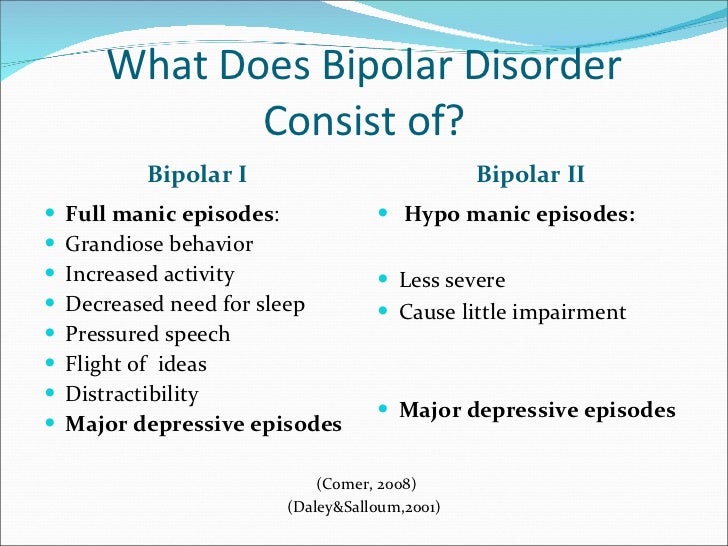
Concerns about the association of lithium intake and the development of heart defects appear to be unfounded (II).
Since at least 50% of pregnancies today are unplanned, family planning counseling should be provided where possible (S).
Pregnancy and postpartum period. Dopamine antagonists/partial agonists, antidepressants, lamotrigine and lithium preparations are not teratogenic or the risk is very low. However, it should be remembered that the risk of new drugs is always unknown, so they should be used with caution.
Pregnant women are not immune from relapse. Discontinuation of medications can lead to mood destabilization (IV). Thus, the potential negative impact on the fetus must be weighed against the risk of a mental disorder in the mother and how this will affect the child's condition (S).
Many psychotropic drugs used to treat BD can cause symptoms in newborns. Babies need to be watched hours and even days after birth (S).
Women have an increased risk of recurrence of mania or depression after childbirth (I).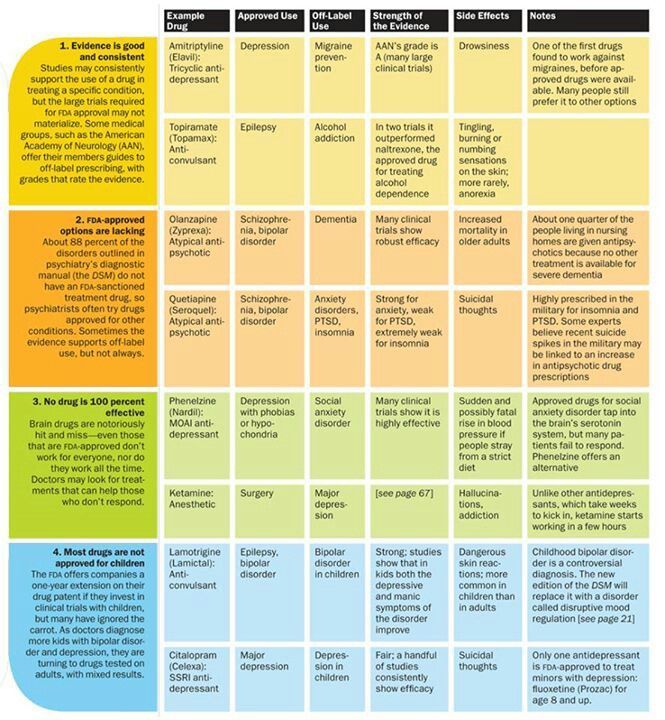 In this regard, they need constant monitoring and preventive treatment (S).
In this regard, they need constant monitoring and preventive treatment (S).
There are anecdotal reports of adverse reactions in breast-fed infants when mothers take psychotropic drugs, but the frequency of such events is not yet clear (III).
Women who continue to receive psychotropic medication after childbirth make their own decision to breastfeed or formula-feed after a detailed explanation of the benefits and risks (S). If the mother decides to continue breastfeeding while on therapy, the baby should be monitored (S).
There are regular reports of the adverse effects of taking antidepressants and other psychotropic drugs during pregnancy on the further development of children. Very often, such studies are of inadequate design and low quality. Thus, claims that the use of psychotropic drugs during pregnancy may cause behavioral disorders in children in the future should be treated with caution.
The main recommendations for the treatment of BR are summarized in the table.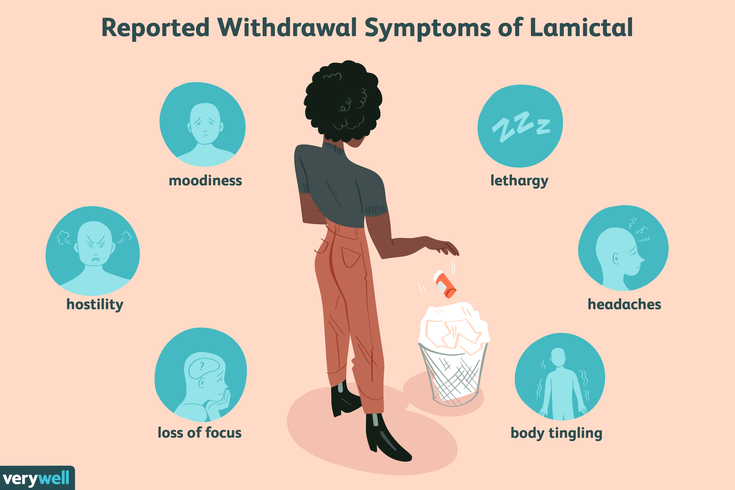
Prepared by Natalia Mishchenko
Evidence-based guidelines for treating bipolar disorder: Revised third edition recommendations from the British Association for Psychopharmacology. Goodwin G.M., Haddad P.M., FerrierI.N. et al. J Psychopharmacol. Jun 2016; 30(6): 495-553.
- Number:
- Thematic issue "Neurology, Psychiatry, Psychotherapy" No. 3 (38), spring 2016
11/25/2022 NeurologyTherapy and family medicine
The problem of injection on the body (forward to the brain) of acute and chronic stress factors, one of the most common in medicine; in modern medical practice in modern minds it has a special meaning, both in the medical, and in the medical and social sense, scho without intermediary occupies the sphere of professional activity of various physicians - neurologists, cardiologists, gastroenterologists, pulmonologists, endocrinologists, psychiatrists, and also doctors-internists wide profile and family doctors.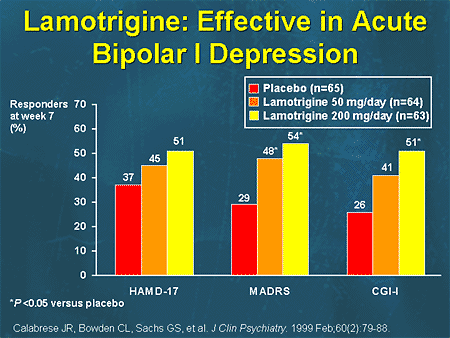 A special place is added to the influx of chronic stress in the pathogenesis of t. sickness of civilization - psychosomatic and cerebrovascular pathology, as well as neuroses [6, 9, 16]. Podnuє guessing the form of pathology, the primary lesion of the central nervous system (CNS) on all levels of the structural and functional organization of the brain - in terms of molecular to systemic with a further development of dysregulation of internal organs, central and peripheral blood circulation, the disease of civilization also belongs to the category of dysregulation pathology. ...
A special place is added to the influx of chronic stress in the pathogenesis of t. sickness of civilization - psychosomatic and cerebrovascular pathology, as well as neuroses [6, 9, 16]. Podnuє guessing the form of pathology, the primary lesion of the central nervous system (CNS) on all levels of the structural and functional organization of the brain - in terms of molecular to systemic with a further development of dysregulation of internal organs, central and peripheral blood circulation, the disease of civilization also belongs to the category of dysregulation pathology. ...
11/25/2022 PsychiatryTherapy and family medicine Treating depressive disorder
In today's world, depression is one of the most widespread mental disorders. Show illness and negative consequences both on the psychological and on the somatic level, and severe depression can become a cause of suicide. In the absence of a decrease in the quality of life of ailments, and a stronger focus on the economic and medical systems of the country, the urgency of this illness is mindful. About modern standards of diagnostics and methods of treating depressive disorder in its dopovіdі at the international neurological conference "XIV Neurosymposium" by Prof. Allan H. Young....
In the absence of a decrease in the quality of life of ailments, and a stronger focus on the economic and medical systems of the country, the urgency of this illness is mindful. About modern standards of diagnostics and methods of treating depressive disorder in its dopovіdі at the international neurological conference "XIV Neurosymposium" by Prof. Allan H. Young....
11/20/2022 Psychiatry Somatically unreasonable syndromes and functional disorders at the sight of a psychiatrist
The conference “Internal medicine in the minds of modern people” was organized by the Department of Internal Diseases of the Faculty of Dentistry of the National Medical University. O.O. Bogomolets (m. Kyiv), community organizations "Academy of Internal Medicine" (m. Kiev) and "Polish Medical Association in Ukraine named after.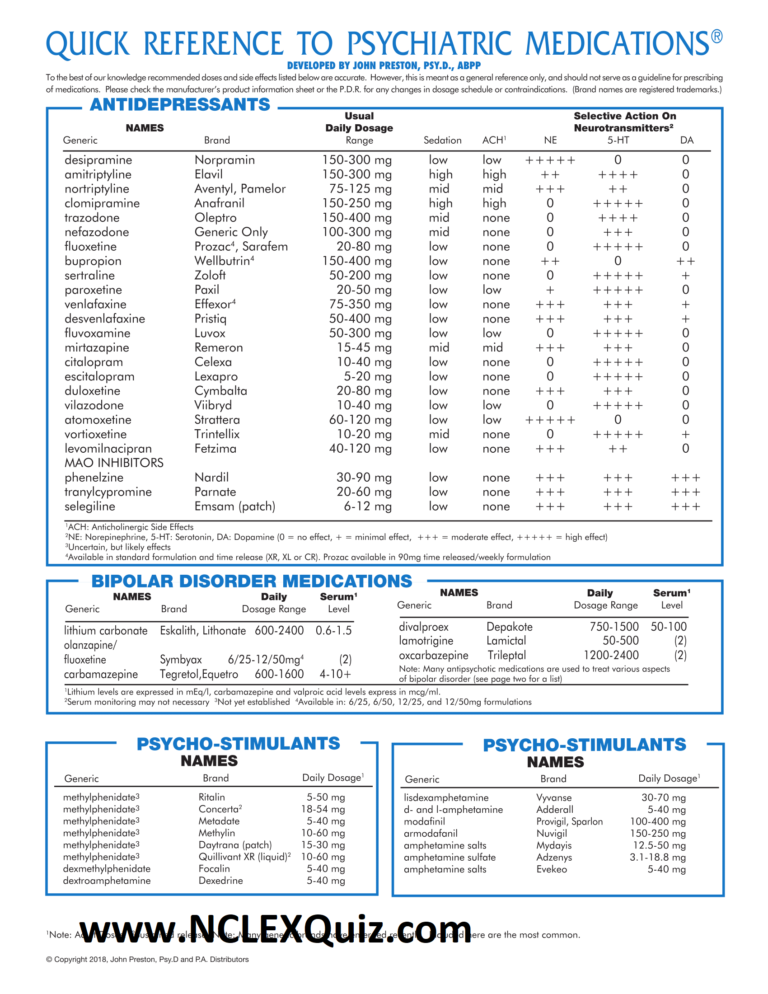 A.S. Svіncіtskogo” (m. Kiev). Tsya zustrіch bula was dedicated to the nutrition of diagnostics, exaltation, as well as the prevention of illness in the ambush of evidence-based medicine ....
A.S. Svіncіtskogo” (m. Kiev). Tsya zustrіch bula was dedicated to the nutrition of diagnostics, exaltation, as well as the prevention of illness in the ambush of evidence-based medicine ....
04.11.2022 NeurologyCiticoline for improving memory in older people
Antiquity is characterized by the development of a wide range of pathologies, traditionally viewed as a natural process, and then, not like a disease. If old age is not aggravated by neurological or psychiatric ailments, cognitive functions do not break down, but rather calm down. Zokrema, in the middle of that frail age, the memory of those warehouses that are respected by physiological ones is commemorated. Mayzhe skin is subjectively aware of the memory of the memory of old times, which manifests itself, in the middle, like an hour later, necessary for memorizing new information and guessing information, as it was guessed earlier.