Is pacing a sign of anxiety
Psychomotor Agitation: Symptoms, Treatment, and More
Psychomotor Agitation: Symptoms, Treatment, and MoreMedically reviewed by Elaine K. Luo, M.D. — By Annamarya Scaccia — Updated on April 25, 2017
Overview
Psychomotor agitation is a symptom related to a wide range of mood disorders. People with this condition engage in movements that serve no purpose. Examples include pacing around the room, tapping your toes, or rapid talking.
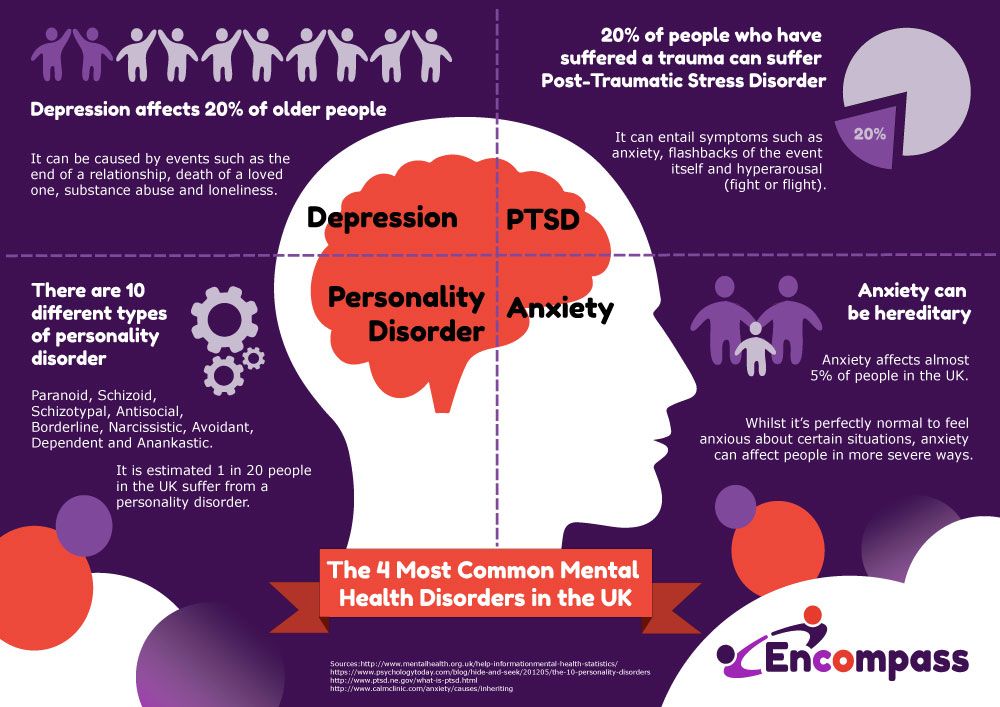
Psychomotor agitation often occurs with mania or anxiety. It’s seen most often in people with bipolar disorder. Psychomotor agitation can be caused by other conditions, too, such as posttraumatic stress disorder or depression.
People with psychomotor agitation can’t stay still or remain calm. They use movement to release tension and anxiety. If you have psychomotor agitation, you may regularly fidget, move fast, or move with no reason or purpose.
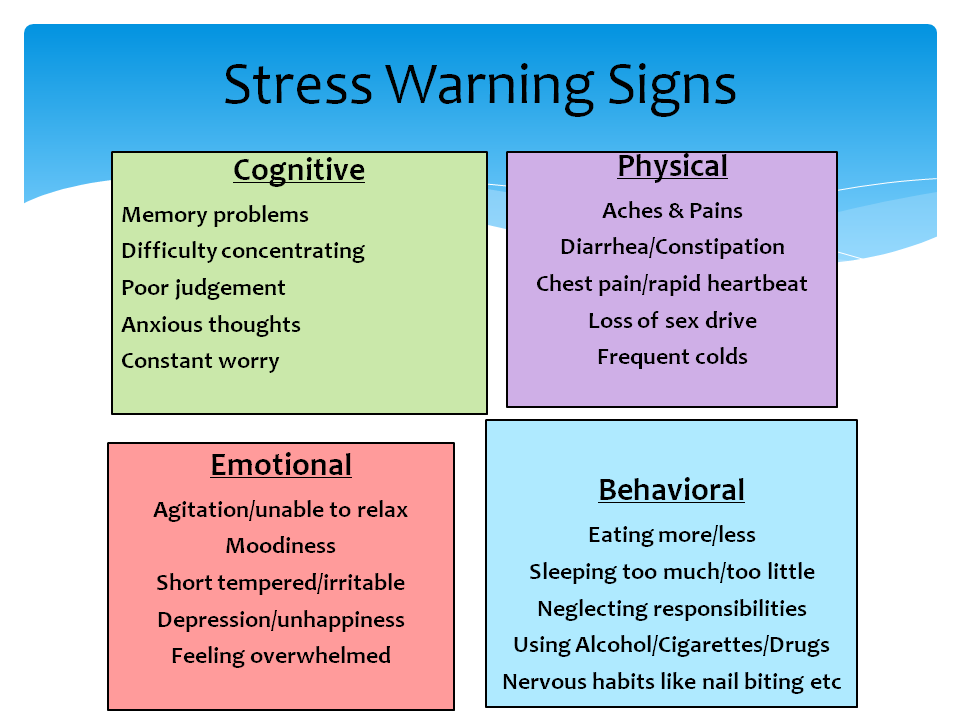
The most common signs of psychomotor agitation include:
- emotional distress
- restlessness
- tapping
- starting and ending tasks abruptly
- fidgeting
- pacing
- hand-wringing
- fast talking
- racing thoughts
- crowded thoughts
- moving objects for no reason
People who have psychomotor agitation will display a set of behaviors, including:
- pacing back and forth in a room
- taking off clothing, then putting it back on
- twisting their hands
- tapping their feet on the floor
- tapping their fingers on any surface
- picking up and moving objects around the room for no reason
In severe cases, psychomotor agitation can lead to self-inflicted harm. People may rip, chew, or pull at the skin near their lips, fingernails, or other body parts until they bleed.
Psychomotor agitation is often seen in people with bipolar disorder. It’s also less commonly seen in people with other conditions, including:
- panic attacks
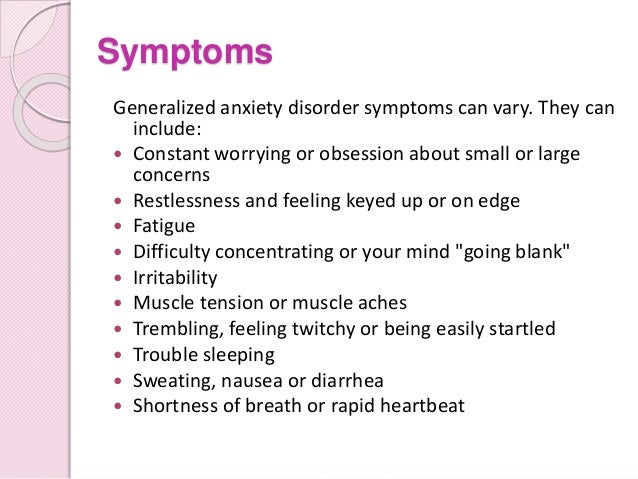
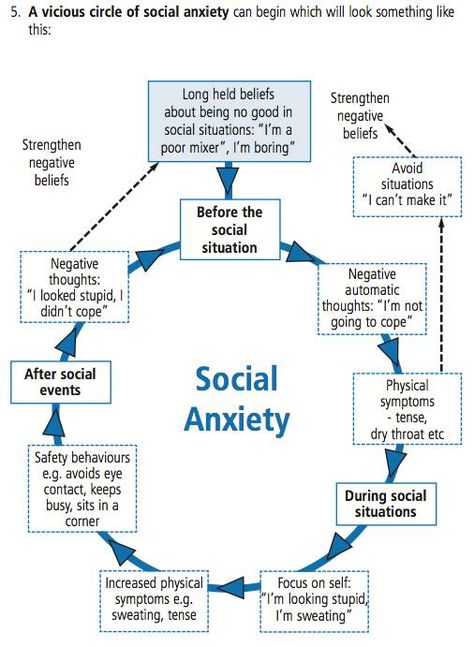
- anxiety disorder
- depression
- posttraumatic stress disorder
- traumatic brain injury (TBI)
- claustrophobia
- Parkinson’s disease
- alcohol withdrawal
- drug overdose or withdrawal
- dementia
- schizophrenia
- severe major depressive disorder
- effects of certain antipsychotic medications
- substance abuse
Researchers have also found a link between akathisia and psychomotor agitation in people with TBI. Akathisia is a movement disorder marked by restlessness.
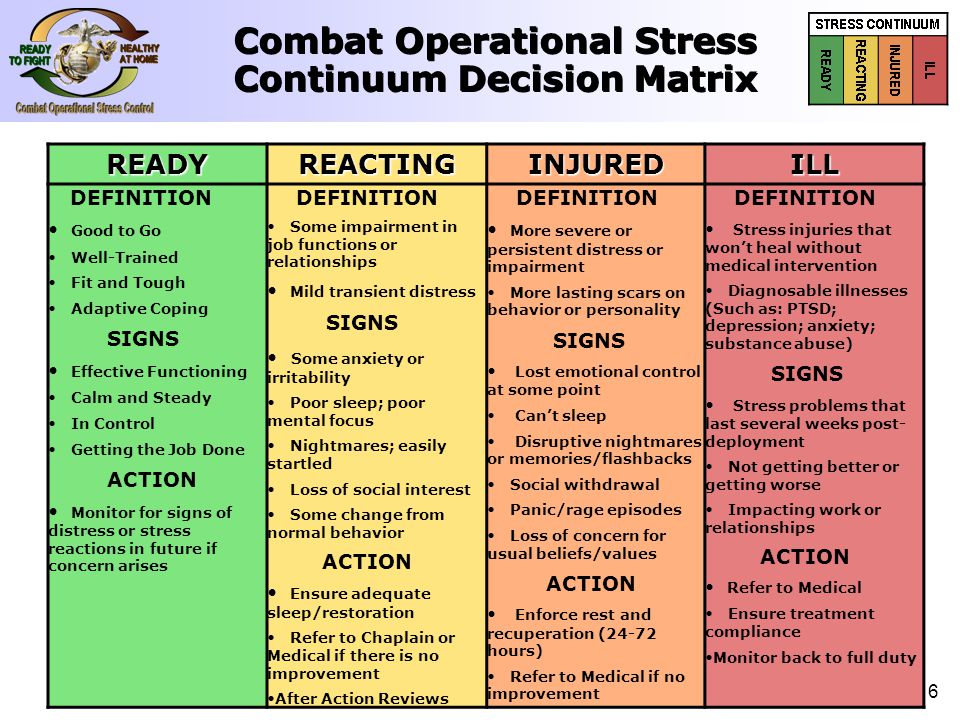
Psychomotor agitation is a common symptom of bipolar depression. It mostly occurs during manic episodes, but it’s also seen during depressive episodes.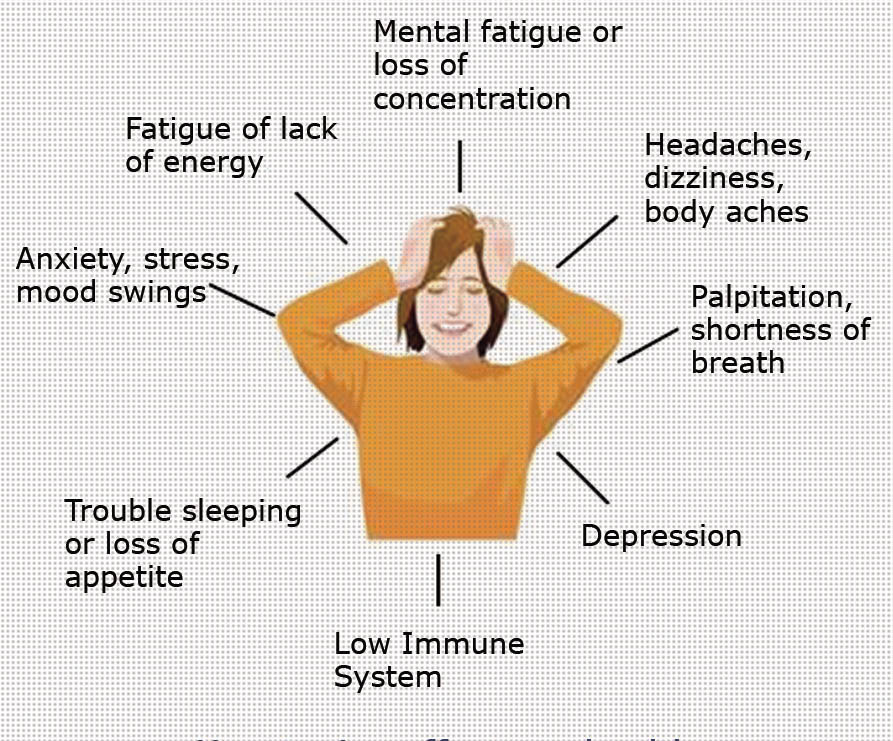 It’s often linked with other noneuphoric hypomanic symptoms and suicidal thoughts. Signs of noneuphoric hypomania include:
It’s often linked with other noneuphoric hypomanic symptoms and suicidal thoughts. Signs of noneuphoric hypomania include:
- crying
- trouble sleeping
- racing thoughts
- trouble making decisions
- confusion
- false belief someone is out to harm you
- inflated feelings of self-importance
- hearing sounds or voices that aren’t there
Psychomotor symptoms differ depending on whether they occur during a manic episode, mixed affective episode (depression and mania), or depressive episode. During a manic episode, a person is more like to move aimlessly. For example, they may pace, wring their hands, or tap their fingers.
During a mixed affective or depressive episode, movements will be used to reduce tension and stress. The person may feel anxious, upset, irritable, and restless.
See your doctor as soon as you first notice signs of psychomotor agitation. Your doctor will be able to determine if your symptoms are caused by bipolar disorder or another mental health condition. They will also help you decide on the best treatment plan to help you manage your symptoms.
They will also help you decide on the best treatment plan to help you manage your symptoms.
You should also see your doctor if you notice changes in your psychomotor agitation symptoms. Changes in motor activity may indicate changes or progression of the underlying cause of the condition.
Your doctor will ask you questions and review your medical history. They will also run some tests and perform a physical exam. Your test results will be used to rule out causes of psychomotor agitation.
Once you receive a diagnosis, you and your doctor can work out a treatment plan to manage your symptoms.
Treatment depends on the underlying cause of your symptoms. For example, if your doctor finds that antidepressants or anti-anxiety pills are causing psychomotor agitation, they may switch your medication.
If psychomotor agitation is related to manic or depressive episodes, your doctor may prescribe mood stabilizers or antipsychotic drugs. A 2013 study found that the anti-anxiety drug class benzodiazepines can help treat types of psychosis-induced agitation.
You may be able to manage psychomotor agitation using relaxations techniques that help people with anxiety. Try these:
- See a talk therapist once or twice per week.
- Practice yoga and meditation often.
- Exercise most days.
- Use deep breathing exercises.
Learn more: Alternative treatments for anxiety »
You should use these techniques in addition to medication or other treatments recommended by your doctor. It may be difficult to manage psychomotor agitation with relaxation techniques alone.
Psychomotor agitation can be managed with the right treatment. It’s important to pay attention to the signs and symptoms. Sharing what you experience with your doctor can help them make a diagnosis.
Last medically reviewed on April 25, 2017
How we reviewed this article:
Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
- Benazzi, F. (2002, November 15). Psychomotor changes in melancholic and atypical depression: Unipolar and bipolar-II subtypes [Abstract]. Psychiatry Research, 112(3), 211-20
ncbi.nlm.nih.gov/pubmed/12450630 - FDA requiring Boxed Warning updated to improve safe use of benzodiazepine drug class. (2020).
fda.gov/drugs/drug-safety-and-availability/fda-requiring-boxed-warning-updated-improve-safe-use-benzodiazepine-drug-class - Gillies, D., Sampson, S., Beck, A., & Rathbone, J. (2013, April 30). Benzodiazepines for psychosis-induced aggression or agitation. Cochrane Database of Systematic Reviews, 4
onlinelibrary.wiley.com/doi/10.1002/14651858.CD003079.pub3/abstract - Koenig, A. M., Arnold, S. E., & Streim, J. E. (2016, January).
 Agitation and irritability in Alzheimer’s disease: Evidenced-based treatments and the black-box warning [Abstract]. Current Psychiatry Reports, 18(3)
Agitation and irritability in Alzheimer’s disease: Evidenced-based treatments and the black-box warning [Abstract]. Current Psychiatry Reports, 18(3)
link.springer.com/article/10.1007%2Fs11920-015-0640-7 - Leventhal, A. M., & Zimmerman, M. (2010, June). The relative roles of bipolar disorder and psychomotor agitation in substance dependence. Psychology of Addictive Behaviors, 24(2), 360-365
ncbi.nlm.nih.gov/pmc/articles/PMC3150706/ - Mann, J. J., Brown, R. P., Halper, J. P., Sweeney, J. A., Kocsis, J. H., Stocker, P. E., & Bilezikian, J. P. (1985, September 19). Reduced sensitivity of lymphocyte beta-adrenergic receptors in patients with endogenous depression and psychomotor agitation [Abstract]. The New England Journal of Medicine, 313, 715-720
nejm.org/doi/full/10.1056/NEJM198509193131202 - Manzo, C., Gareri, P. & Castagna, A. (2017, March 4). Psychomotor agitation following treatment with hydroxychloroquine.
 Drug Safety - Case Reports, 4, 6
Drug Safety - Case Reports, 4, 6
link.springer.com/article/10.1007/s40800-017-0048-x - Narita, Z., Takano, H., & Sumiyoshi, T. (2017, March 13). Successful treatment for psychomotor agitation in neuromyelitis optica spectrum disorder with trazodone-risperidone combination: A case report. Neuropsychiatric Disease and Treatment, 2017(13), 775-777
dovepress.com/successful-treatment-for-psychomotor-agitation-in-neuromyelitis-optica-peer-reviewed-fulltext-article-NDT - Piguet C., Dayer, A., Kosel, M. Desseillies, M., Vullieumier, P., & Bertschy, G. (2010, March). Phenomenology of racing and crowded thoughts in mood disorders: A theoretical reappraisal [Abstract]. Journal of Affective Disorders, 121(3), 189-198
ncbi.nlm.nih.gov/pubmed/19515428 - Piguet, C., Desseilles, M., Cojan, Y., Sterpenich, V., Dayer, A., Bertschy, G., & Vuilleumier, P. (2014, November 17). Neural correlates of generation and inhibition of verbal association patterns in mood disorders.
 Social Cognitive and Affective Neuroscience, 10(7), 978–986.
Social Cognitive and Affective Neuroscience, 10(7), 978–986.
doi.org/10.1093/scan/nsu146 - Snyderman, D. & Rovner, B. (2009, October 15). Mental status exam in primary care: A review [Abstract]. American Family Physician, 80(8), 809-814
ncbi.nlm.nih.gov/pubmed/19835342?dopt=Abstract - Wielenga-Boiten, J. E. & Ribbers, G. M. (2012, November 9). Akathisia—rare cause of psychomotor agitation in patients with traumatic brain injury: Case report and review of literature. Journal of Rehabilitation Research & Development, 49(9), 1349-1354
dx.doi.org/10.1682/JRRD.2011.10.0202
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.
Current Version
Apr 26, 2017
Written By
Annamarya Scaccia
Edited By
Yvette Brazier
Apr 25, 2017
Medically Reviewed By
Elaine K.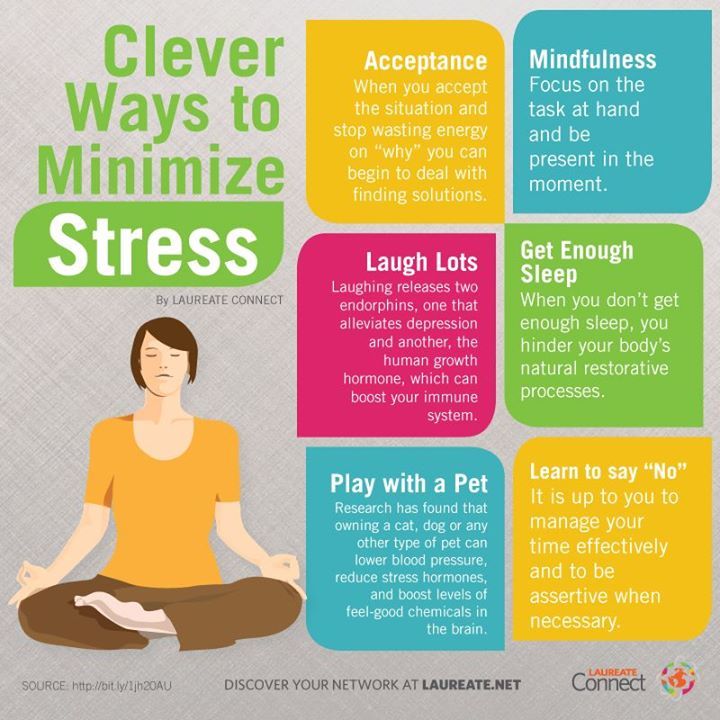 Luo, MD
Luo, MD
Share this article
Medically reviewed by Elaine K. Luo, M.D. — By Annamarya Scaccia — Updated on April 25, 2017
Read this next
What’s Causing My Agitation?
Agitation is a feeling of aggravation, annoyance, or restlessness brought on by provocation or, in some cases, little to no provocation.
READ MORE
What You Need to Know About Catatonia
Medically reviewed by Timothy J. Legg, PhD, PsyD
Catatonia affects a person’s ability to move in a normal way. Explore types and risk factors. Also learn about diagnosis, prevention, and much more.
READ MORE
How to Balance Staying Informed and Not Being Overwhelmed By Stressful News
From a global pandemic, and now an escalation to war in Ukraine, turning on the news may feel like mental torture at this point.
 If you have been…
If you have been…READ MORE
What’s Resilience? Benefits and Tips for ‘Bouncing Back’ After Hardship
Resilience describes your ability to bounce back from life's difficulties. Here's how this skill can benefit your mental health and tips to boost it.
READ MORE
The Top 9 Online Psychiatry Services for 2023
If you’re considering meeting with a psychiatrist but prefer remote visits, online psychiatry may be right for you. Here are our top picks for online…
READ MORE
Therapy for Every Budget: How to Access It
Medically reviewed by Karin Gepp, PsyD
Finding a therapist is a huge step in caring for your mental health. To help get you started, here’s a list of affordable mental health care options.
READ MORE
A 2023 Review of BetterHelp for Online Therapy
BetterHelp is an online therapy service that allows you to text-chat with a licensed therapist.
 Learn how it works, what to consider, and whether it’s…
Learn how it works, what to consider, and whether it’s…READ MORE
Harmful Content on Eating Disorders, Suicide Can Pop Up in Minutes on New TikTok Account, Study Finds
TikTok recommends potentially harmful content related to self-harm and eating disorders to some young teenagers within minutes of them creating an…
READ MORE
What is it, symptoms, and causes
Psychomotor agitation: What is it, symptoms, and causes- Health Conditions
- Health Conditions
- Alzheimer's & Dementia
- Anxiety
- Arthritis
- Asthma & Allergies
- Breast Cancer
- Cancer
- Cardiovascular Health
- COVID-19
- Dermatology & Skincare
- Diabetes
- Environment & Sustainability
- Exercise & Fitness
- Eye Health
- Headache & Migraine
- Health Equity
- HIV & AIDS
- Human Biology
- Inflammatory Bowel Disease
- Leukemia
- LGBTQIA+
- Men's Health
- Mental Health
- Multiple Sclerosis (MS)
- Nutrition
- Parkinson's Disease
- Psoriasis
- Sexual Health
- Women's Health
- Health Conditions
- Health Products
- Health Products
- Nutrition & Fitness
- Vitamins & Supplements
- CBD
- Sleep
- Mental Health
- At-Home Testing
- Men’s Health
- Women’s Health
- Health Products
- Discover
- News
- Latest News
- Original Series
- Medical Myths
- Honest Nutrition
- Through My Eyes
- New Normal Health
- Podcasts
- How Viagra became a new 'tool' for young men
- What makes breast cancer come back?
- How to understand chronic pain
- What is behind vaccine hesitancy?
- The amazing story of hepatitis C, from discovery to cure
- New directions in dementia research
- News
- Tools
- General Health
- Drugs A-Z
- Health Hubs
- Health Tools
- BMI Calculators and Charts
- Blood Pressure Chart: Ranges and Guide
- Breast Cancer: Self-Examination Guide
- Sleep Calculator
- Quizzes
- RA Myths vs Facts
- Type 2 Diabetes: Managing Blood Sugar
- Ankylosing Spondylitis Pain: Fact or Fiction
- General Health
- Connect
- About Medical News Today
- Who We Are
- Our Editorial Process
- Content Integrity
- Conscious Language
- Newsletters
- Sign Up
- Follow Us
- About Medical News Today
Medically reviewed by Nicole Washington, DO, MPH — By Lana Burgess — Updated on March 9, 2022
Psychomotor agitation is a feeling of anxious restlessness that causes a person to make movements without meaning to.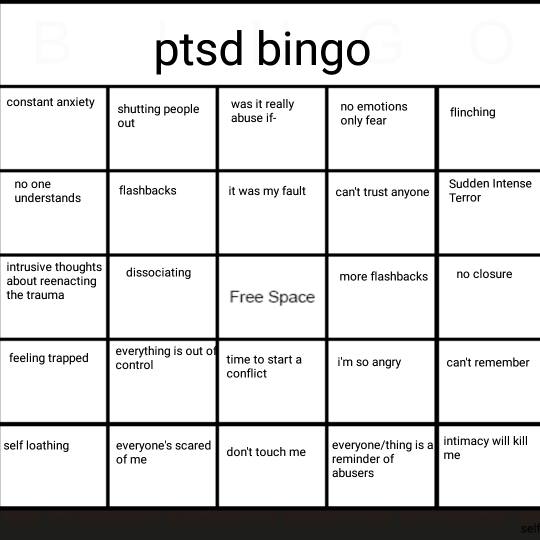
Psychomotor agitation often affects people with bipolar disorder, but it is also associated with other conditions that affect mental health or neurological function. It is a physical expression of anxiety and mental tension.
This article explores the ways of feeling, moving, and behaving that could be symptoms of psychomotor agitation. It also looks at what mood disorders are associated with psychomotor agitation.
Psychomotor agitation can be distressing for people who experience it and may also cause concern to others around them.
The condition can cause behavioral, physical, and mental symptoms, including:
- sudden, unexplainable movements
- inability to sit still
- muscle tension
- hyperactivity to stimulus
- physical tremors
- inability to relieve tension
- sudden weakness
- anxiety
- frustration
- sweating
- disorientation
- tachycardia
- dyspnea
This anxious tension may lead a person to:
- pace around a room
- wring their hands
- tap their fingers
- tap their feet
- fidget
- start and stop tasks abruptly
- talk very quickly
- move objects around for no reason
People with psychomotor agitation and mental health conditions such as bipolar disorder and schizophrenia may feel uneasy, nervous, or that there is no hope of controlling their agitations.
Someone experiencing psychomotor agitation may display these behaviors in a way that seems uncontrolled or erratic. This can often place them and others around them at risk of physical harm.
People with severe psychomotor agitation may:
- bite their lips until they bleed
- pull skin off from around their lips
- pull skin off from around their nails
- chew the inside of their cheek
Typically, psychomotor agitation will not have a single cause. A person may experience the condition due to a combination of psychological and environmental factors, including stress, trauma, and substance withdrawal.
Associated conditions
Psychomotor agitation has associations with the following mental health conditions:
- bipolar disorder
- post-traumatic stress disorder (PTSD)
- panic attacks
- generalized anxiety disorder
- depression
- schizophrenia
- alcohol withdrawal
- claustrophobia
- Parkinson’s disease
- dementia
Psychomotor agitation is particularly prevalent among people with bipolar disorder. People diagnosed with bipolar disorder can experience three different episodes called manic, mixed, and depressive.
People diagnosed with bipolar disorder can experience three different episodes called manic, mixed, and depressive.
Psychomotor agitation is a symptom of all three types of episode. However, the nature of psychomotor agitation can change, depending on which type is occurring:
- Manic episode: Alongside psychomotor agitation, a person may experience racing thoughts. Feeling overwhelmed by these can cause people to move without meaning to and to talk rapidly. Movements resulting from psychomotor agitation in a manic episode may appear chaotic.
- Mixed affective episode: This is a particularly vulnerable state when a person experiences a mixture of depressive and manic symptoms. As well as feeling very low, they may feel agitated and irritable.
- Depressive episode: In a depressive episode, people may feel extremely low, hopeless, and tearful. They may make some movements that are signs of psychomotor agitation.
Learn more about bipolar disorder here.
If a person is experiencing psychomotor agitation or knows someone who is, they should speak with a doctor. A doctor can determine the cause of psychomotor agitation and advise how to manage it.
This may include changes to medication programs or psychotherapy and drug treatments to treat underlying mental health conditions.
Management plans can include:
- treating the underlying cause of psychomotor agitation
- learning de-escalation and coping strategies
- minimizing stressful stimuli
- managing drug and alcohol withdrawal, if relevant
- medications such as antipsychotics, benzodiazepines
Learn about the treatments for bipolar disorder here.
Psychomotor agitation can often cause distress. However, a person can manage it with the right treatment.
Seeking treatment for psychomotor agitation can help a person identify and manage conditions or environmental factors that may contribute to their agitation.
Starting treatment early for psychomotor agitation can help reduce its impact and associated conditions on someone’s life.
Last medically reviewed on March 9, 2022
- Bipolar
- Mental Health
- Anxiety / Stress
How we reviewed this article:
Medical News Today has strict sourcing guidelines and draws only from peer-reviewed studies, academic research institutions, and medical journals and associations. We avoid using tertiary references. We link primary sources — including studies, scientific references, and statistics — within each article and also list them in the resources section at the bottom of our articles. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
- Benzodiazepine drug information. (2020).
https://www.fda.gov/drugs/information-drug-class/benzodiazepine-drug-information - Pompili, M.
 , et al. (2021). The management of psychomotor agitation associated with schizophrenia or bipolar disorder: A brief review.
, et al. (2021). The management of psychomotor agitation associated with schizophrenia or bipolar disorder: A brief review.
https://www.ncbi.nlm.nih.gov/labs/pmc/articles/PMC8074323/ - San, L., et al. (2016). State of acute agitation at psychiatric emergencies in Europe: The STAGE study.
https://www.ncbi.nlm.nih.gov/labs/pmc/articles/PMC5084082/ - Vieta, E., et al. (2017). Protocol for the management of psychiatric patients with psychomotor agitation.
https://www.ncbi.nlm.nih.gov/labs/pmc/articles/PMC5591519/
Share this article
Medically reviewed by Nicole Washington, DO, MPH — By Lana Burgess — Updated on March 9, 2022
Related Coverage
What to know about bipolar disorder
Medically reviewed by Janet Brito, Ph.D., LCSW, CST
Bipolar disorder causes shifts in a person's mood and energy levels. It is usually manageable with a correct diagnosis and suitable treatment and…
READ MORE
Bipolar type definitions
Medically reviewed by Timothy J.
 Legg, PhD, PsyD
Legg, PhD, PsyDThere are five categories of bipolar disorder. Bipolar I and II occur most frequently, while other types are less common. Learn more about the…
READ MORE
How can physical therapy help?
Medically reviewed by Lauren Jarmusz, PT, DPT, OCS
Physical therapy aims to help people maintain, recover, or improve their physical ability. Learn more.
READ MORE
Parkinson's disease early signs and causes
Medically reviewed by Seunggu Han, MD
Parkinson’s disease is a neurological condition that affects movement and thinking. Here, learn about the early signs and why it happens.
READ MORE
PTSD: What you need to know
Medically reviewed by Timothy J. Legg, PhD, PsyD
PTSD is a mental health condition that can happen after a traumatic event.
 Find out how to recognize the symptoms, what to expect, and how to get help…
Find out how to recognize the symptoms, what to expect, and how to get help…READ MORE
Why do dogs imitate sexual behavior?
Most owners are not surprised when their dog climbs on top of another dog, a pillow, or wraps around a stranger's leg. But you might be wondering why females show this behavior too? This is especially true for those who were sterilized as a puppy.
Harmless imitation of sexual behavior by males and females is normal in all dog breeds, but it is important to know when this needs to be corrected.
What is normal behavior?
Whatever you call it - imitation of sexual behavior or mating - it is natural for males and females. Some dogs behave this way because they are excited. For others, this may be an attempt to establish their dominant position and show who is in charge in the house.
Such behavior towards other pets, people or even the sofa in the living room once or twice a day is not considered excessive.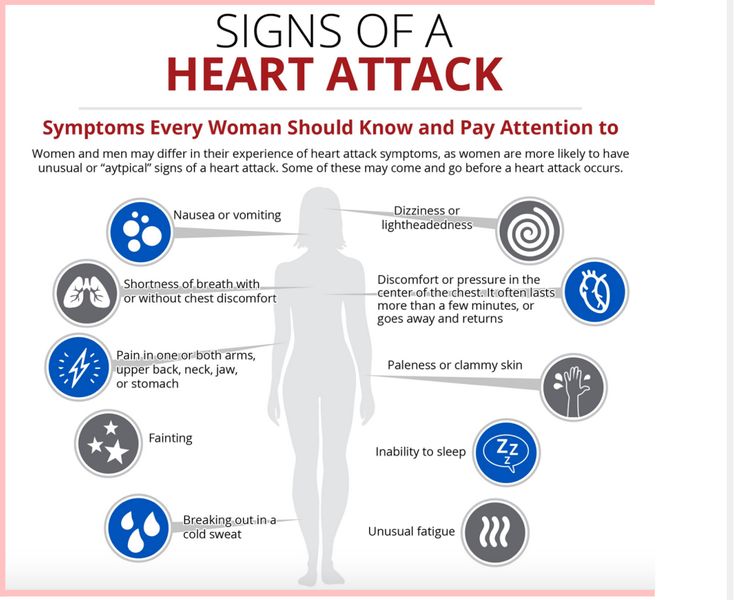 But if you or your family members are concerned about your dog's behavior, there are a few things you can do to correct the situation or eliminate it altogether. nine0003
But if you or your family members are concerned about your dog's behavior, there are a few things you can do to correct the situation or eliminate it altogether. nine0003
How can I prevent sexual imitation?
Pet owners often notice that their dog begins to imitate sexual behavior when they are in their first estrus. Many veterinarians recommend spaying or neutering the dog before this point to eliminate this unwanted behavior. Neutering can also help prevent unexpected litters of puppies and reduce your pet's risk of developing testicular or breast cancer. But even spayed and neutered dogs can mimic mating from time to time. nine0003
The ASPCA (American Society for the Prevention of Cruelty to Animals) recommends teaching dogs the "no" command ahead of time so they don't touch prohibited items. Once your dog has learned this command, you can warn him to move away from furniture, other dogs, or guests. If you see her getting ready to climb onto an object (rubbing, licking it, whining plaintively), you can give the “no” command and distract your four-legged friend with a toy or more interesting activity. Although this command may take some time to learn, it is the easiest way to prevent unwanted behavior. nine0003
Although this command may take some time to learn, it is the easiest way to prevent unwanted behavior. nine0003
When should I be concerned about a dog imitating sexual behavior?
Although this behavior is normal, it can sometimes indicate serious problems. Carefully observe the dog: what actions it performs before it starts rubbing against the object and during this process. This way you can determine if you have cause for concern.
- Is imitation a sign of boredom? If your dog is lying on the floor or pacing around the room and then seems to start rubbing against things, he may just be bored and want to play. nine0028
- Maybe your dog is trying to get rid of the itch? Sexual imitation and excessive genital licking can be a sign that your dog has a health problem, such as skin allergies or a urinary tract infection. If you notice that this behavior is accompanied by the dog licking the back of the body, urinating frequently, having trouble urinating, or showing signs of dehydration, you should make an appointment with your veterinarian as recommended by the ASPCA.
 nine0028
nine0028 - Is your dog stressed? According to the ASPCA, males and females may mimic sexual behavior to relieve stress. Do you have a new pet in the house or a new baby? Or have you recently changed your work schedule? Sometimes small changes in your pet's daily routine can cause stress. Every dog reacts to stressful situations differently. Try to figure out what might be causing her anxiety and do your best to get her into the new routine. If stress-induced sexual behavior continues for too long, it can become a habit that is extremely difficult to break, and you may need to resort to professional training. nine0028
- Behavior become just a bad habit? If you've ruled out all other causes and can't wean your dog from the unwanted behavior, it might be time to start training it. You may need to try new methods, such as group socializing sessions, individual training with a professional dog handler, or even time outs. If you and your veterinarian have ruled out a medical reason for the simulation, heed your doctor's advice on how best to proceed.
 nine0028
nine0028
Why do dogs imitate sexual behavior? There are many reasons! We hope that now that you have received several answers to this question, your dog will show less "obscene" behavior and you will have more joyful moments with him.
Author
Chrissy Klinger
The child walks in his sleep - why does the child crawl in his sleep at night on the bed
21.09.0003
6–9 months 9–18 months 1.5–3 years
Author of the article
Tatyana Chkhikvishvili
Tatyana Chkhikvishvili
Head of online programs, psychologist, consultant on sleep and breastfeeding
Mother of two children tells about the reasons why the baby crawls in a dream, what causes sleepwalking, and what parents should do in such situations so that the baby’s sleep does not worsen.
Calendar of child crises
Leaps of development
The first year of a baby's life is a time of incredibly rapid change.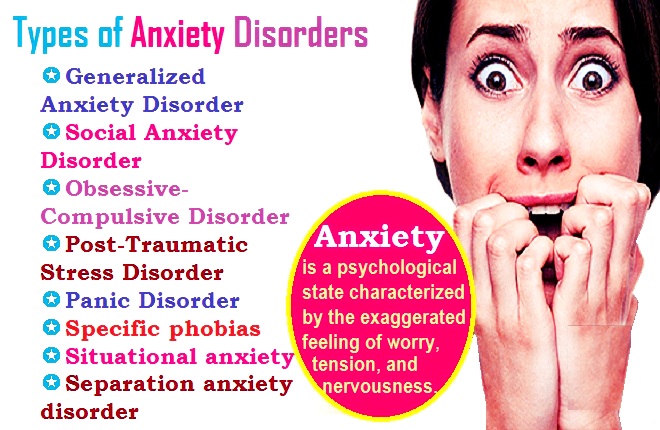 The baby is going through one developmental leap after another - and often this takes the form of crises. But the child develops not only intellectually - his physical development is also very rapid. He learns to sit down, crawl, stand up, move on two straight legs! - new skills affect the nervous system of the baby, excite and may even frighten him. This in itself can affect how well he sleeps.
The baby is going through one developmental leap after another - and often this takes the form of crises. But the child develops not only intellectually - his physical development is also very rapid. He learns to sit down, crawl, stand up, move on two straight legs! - new skills affect the nervous system of the baby, excite and may even frighten him. This in itself can affect how well he sleeps.
Often during such periods, the baby's sleep worsens, becomes more sensitive and restless, he wakes up more often and sleeps less. The child sits up in a dream, then wakes up and begins to cry, because he still does not know how to lie down from such a position. Gradually, he gets used to new opportunities, calms down, begins to sleep normally. nine0003
Practice around the clock
Until the child gets used to his new skills, he constantly trains them. Sometimes at the wrong time for such training. Including night. Between cycles and sometimes phases of sleep, the child has brief awakenings.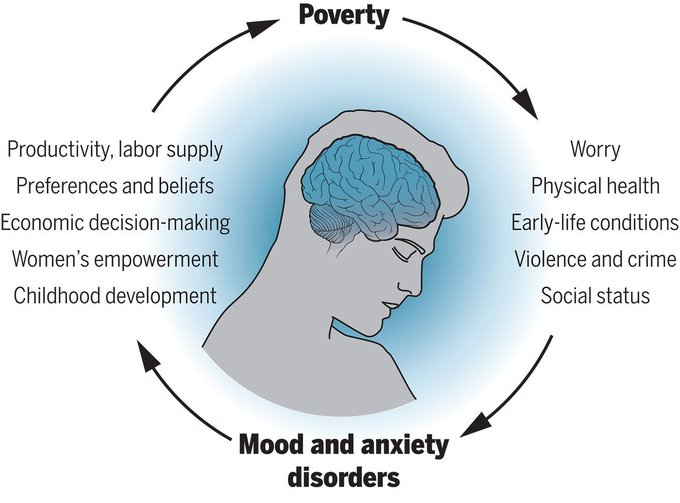 They are needed to control the situation and one's condition, and are also due to the large proportion of the REM phase necessary for brain growth.
They are needed to control the situation and one's condition, and are also due to the large proportion of the REM phase necessary for brain growth.
In moments of such awakenings, the baby may begin to practice a new skill. He instantly sits up, begins to crawl or jumps up in bed. After that, he finally wakes up and cries, not understanding what happened, why he does not lie. And where is mom anyway? nine0003
What to do?
- Practice as many new skills as you can while you are awake so that they quickly become habitual and stop being so exciting to your baby. Stretch out your arms to encourage your child to sit up. Let him crawl freely on the floor, creating a safe environment. Show him how to get up and walk on his own with the help of a support, such as a sofa or table.
- It is important to teach your baby to lie down from new positions. Often he can already sit down or stand up, but still does not understand how to return back to the lying position - and begins to cry.
 Show how to lie down from a sitting and standing position, train during active wakefulness. nine0028
Show how to lie down from a sitting and standing position, train during active wakefulness. nine0028 - Remember - this is temporary, soon your child will get used to new skills and calm down. Babies get used to their new abilities from 3-5 days to 2-6 weeks.
Constant sleepwalking
If you notice that your child sleepwalks regularly and talks without waking up, this may be a symptom of sleepwalking (somnambulism). Don't be afraid.
It is believed that somnambulism occurs in approximately 2.5% of people. In a systematic form among children - in 1-5%. One-time cases of walking in a dream in childhood were noted in about 30% of people. This happens more often with boys. nine0003
Sleepwalking usually resolves by age 15. Only about 1% of people continue to sleepwalk as adults. Most often, sleepwalking first appears at the age of 3-4 years. And the peak of somnambulism in children falls on the age of 5-10 years.
The sleepwalker often looks like he is awake. Right during a very deep sleep, the child suddenly gets up and goes somewhere. He can say something, go to the toilet, and not even always where it needs to be done. After that, he can fall asleep somewhere in an unusual place or return to his bed and go to bed again as if nothing had happened. In the morning he does not remember at all what he did at night. nine0003
Right during a very deep sleep, the child suddenly gets up and goes somewhere. He can say something, go to the toilet, and not even always where it needs to be done. After that, he can fall asleep somewhere in an unusual place or return to his bed and go to bed again as if nothing had happened. In the morning he does not remember at all what he did at night. nine0003
Causes of sleepwalking in children
Somnambulism occurs due to the fact that the process of inhibition of the central nervous system during deep sleep does not affect the areas of the brain responsible for the coordination of movement. If inhibition sit on the bed or say something.
Sleepwalking should not always be regarded as a sign of illness. So far, scientists are not completely sure what exactly is the cause of somnambulism. But it is believed that the factors influencing the appearance of sleepwalking are the immaturity of the nervous system, periods of developmental leaps, a state of tension, anxiety, stress. It has been proven that somnambulism is influenced by heredity. But it can also be associated with congenital pathologies, epilepsy, chronic diseases, craniocerebral injuries, neuroinfections, poisoning with worm poisons. nine0003
It has been proven that somnambulism is influenced by heredity. But it can also be associated with congenital pathologies, epilepsy, chronic diseases, craniocerebral injuries, neuroinfections, poisoning with worm poisons. nine0003
You have a little somnambulist in your house: what to do
- If your child has regular sleepwalking, a doctor should be consulted.
- Supervise the child during sleepwalking to protect him from injury. Make sure that he cannot leave the apartment, block access to the window. It is better to put locking devices on the windows so that the child cannot open them himself. Remove fragile, cutting, piercing, flammable objects from free access.
- Gently hug and guide your baby to bed. In extreme cases, you can wake up, but you need to do this very gently, in an affectionate calm voice. nine0028
- A psychologist or psychotherapist can help. As a rule, sedatives are prescribed for treatment. Sometimes there is a need for medical treatment.

- Minimize conflicts in the family and the burden on the child. Do not allow evening scandals, overexcitation of the child by the end of the day (including positive emotions). Maintain a trusting relationship with your child so that in the evening in bed he can share with you his experiences and impressions of the day. nine0028
- You can use soothing teas, herbs, aromatic oils.
- Pay attention to whether bathing before bedtime relaxes or excites your baby. If it turns you on, you should take a bath early so that you have enough time to completely calm down before going to bed.
Why sleepwalking is dangerous
Somnambulism is not a disease or a dangerous condition and does not require special treatment. In itself, walking at night without waking up is dangerous only with possible injuries. Remember the precautions. If you are not at home overnight and are not sure about the complete safety of the space, you can put wet towels on the floor near the bed. A child who has begun to walk in the middle of the night will wake up from an unusual sensation of moisture and lie back down or call you for help. nine0003
A child who has begun to walk in the middle of the night will wake up from an unusual sensation of moisture and lie back down or call you for help. nine0003
There are dangerous diseases in which sleepwalking can act as one of the symptoms. It is primarily about epilepsy. In this case, the patient in the waking state has convulsions, and in the "off state" the child walks and often seems to be swallowing something. In addition to epilepsy, sleepwalking can accompany some mental disorders, such as neurosis (85% of all sleepwalkers) and hysteria. In addition to restless nights, neurotics are distinguished by increased impressionability, excitability, tearfulness, fatigue, and complaints of headaches. In these cases, it is necessary to treat, of course, the root cause. nine0003
When to worry
You should consult a neurologist if:
- sleepwalking has its own fixed clock time;
- during episodes of somnambulism, the child behaves aggressively;
- episodes last longer than 15 minutes;
- there are other problems: stuttering, enuresis, frequent nightmares, tossing about in bed, oddities in daytime behavior.