Is lamictal used for anxiety
Uses, Dosages, Common Side Effects, and Interactions
Lamictal (lamotrigine) is an anti-seizure medicine approved to treat epilepsy in children and adults and to delay mood episodes in people with bipolar I disorder. The most common side effects include dizziness, headache, vomiting and rash. The drug has a black box warning for life-threatening skin rashes.
GlaxoSmithKline developed Lamictal, and the U.S. Food and Drug Administration approved it in 1994.
Even though it’s only approved for epilepsy and as maintenance medicine to delay mood episodes in people with bipolar I, some medical providers prescribe it to treat other conditions off-label — uses not approved by the FDA.
Off-label uses include:
- Panic disorder
- Anxiety
- Migraines and headaches
- Rapid-cycling bipolar depression
- Binge eating disorder
- Borderline personality disorder
- Posttraumatic stress disorder (PTSD)
Lamictal XR, the extended-release version of Lamictal, is not approved for patients younger than 13. It’s only approved for treating certain types of seizures.
In January 2020, Taro Pharmaceuticals, a manufacturer of generic Lamictal, issued a recall for one lot of lamotrigine because it was contaminated with a small amount of enalapril maleate — a blood pressure and heart failure drug that may cause birth defects.
Researchers in 2022 published results on a generic version of extended-release lamotrigine and found the drug to be bioequivalent to the brand name medication.
How It Works
Researchers believe Lamictal works by slowing down electrical signals and inhibiting certain chemicals in the brain that cause brain cells to signal too quickly. When brain cells work too fast, it causes seizures. By slowing down these brain signals, lamotrigine may help to reduce seizure episodes.
In people with bipolar disorder, the medication helps to reduce mood swings, though researchers aren’t sure how the drug actually works.
Recommended Dosages
Lamictal comes in several forms and strengths. Depending on the reason for treatment, the recommended dosage is different.
Depending on the reason for treatment, the recommended dosage is different.
Forms and Strengths
- Tablets: 25 mg, 100 mg, 150 mg, and 200 mg
- Tablets for oral suspension: 2 mg, 5 mg, and 25 mg
- Orally disintegrating tablets: 25 mg, 50 mg, 100 mg, and 200 mg
- Extended release tablets: 5 mg, 50 mg, 100 mg, 200 mg, 250 mg, and 300 mg
Patients typically take Lamictal once or twice a day, and it can be taken with or without food. If taking Lamictal XR, make sure to take the pills whole and don’t crush, cut or chew them.
The medication starts at a low dose. Then, the dose gets higher over the course of several weeks. People who are taking the drug with other drugs for seizures take lower doses. They may take it every other day when beginning treatment.
Common Side Effects
Researchers studied Lamictal in clinical trials that included thousands of patients in several groups. Across these studies, researchers defined common side effects as those that occurred in 10 percent or more of patients using the drug for epilepsy and five percent or more of patients using the drug for bipolar disorder.
Across these studies, researchers defined common side effects as those that occurred in 10 percent or more of patients using the drug for epilepsy and five percent or more of patients using the drug for bipolar disorder.
Common side effects of Lamictal (lamotrigine) include:
- Ataxia (impaired balance or coordination)
- Back pain, abdominal pain
- Blurred vision
- Diarrhea
- Diplopia (double vision)
- Dizziness
- Fatigue
- Headache
- Insomnia
- Nausea
- Pharyngitis
- Rash
- Rhinitis (inflammation of membranes in the nose)
- Somnolence (drowsiness)
- Vomiting
- Xerostomia (dry mouth)
The most common side effects in children were infection, vomiting, diarrhea, accidental injury, fever, abdominal pain and tremor.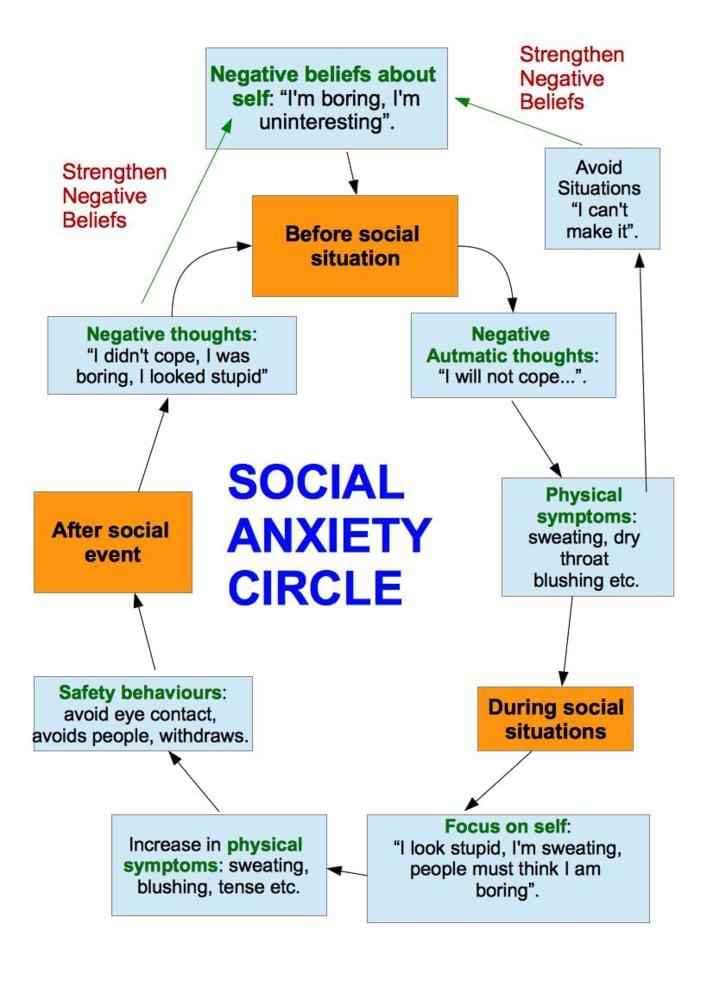
In clinical trials, the most common side effects that caused people to drop out of the trial included: rash, headache, dizziness and impaired balance or coordination.
Serious Side Effects
There have been reports of serious side effects linked to Lamictal, but these side effects are rare, according to the drug’s label. These range from serious skin rashes to death.
Skin Rashes
In clinical trials, 11 of 3,348 adults with epilepsy who received Lamictal had a serious rash that led to hospitalization and discontinuation. Researchers received postmarketing reports of rash-related deaths, but the numbers were too few to estimate the exact rate.
Serious rashes that led to hospitalization were: Stevens-Johnson syndrome — a serious, blistering rash — angioedema, toxic epidermal necrolysis and rashes associated with multiorgan hypersensitivity.
Hemophagocytic Lymphohistiocytosis (HLH)
HLH is a potentially life-threatening syndrome caused by overactivation of the immune system. The overactivation causes severe inflammation throughout the body. In April 2018, the FDA released a warning that Lamictal can cause HLH.
The overactivation causes severe inflammation throughout the body. In April 2018, the FDA released a warning that Lamictal can cause HLH.
HLH usually starts with a high fever and rash. It causes problems with blood cells and internal organs such as the lungs, kidneys and liver. It usually starts within 8 to 24 days after starting treatment.
Multiorgan Hypersensitivity Reactions and Organ Failure
Multiorgan hypersensitivity reactions, also known as drug reaction with eosinophilia and systemic symptoms (DRESS), have occurred. This is a potentially fatal drug reaction.
Symptoms include fever, rash, and other organ problems. It sometimes resembles a viral infection. Report these symptoms to your medical provider right away.
Blood Problems
Some people who took Lamictal had abnormal blood cell counts such as neutropenia, leukopenia, anemia, thrombocytopenia, pancytopenia, and, rarely, aplastic anemia and pure red cell aplasia.
Suicidal Thoughts or Behaviors
Taking Lamictal may increase the risk of suicidal thoughts or behaviors. In studies of anti-epileptic drugs (AED) such as Lamictal, patients who took one type of drug had about twice the risk of suicidal thoughts and behaviors compared to people who took a placebo. These symptoms may start as early as one week after starting treatment.
In studies of anti-epileptic drugs (AED) such as Lamictal, patients who took one type of drug had about twice the risk of suicidal thoughts and behaviors compared to people who took a placebo. These symptoms may start as early as one week after starting treatment.
Aseptic Meningitis
Taking Lamictal increases the risk of aseptic meningitis — inflammation of the membrane covering the spinal cord and brain. Symptoms include rash, fever, vomiting, nausea and stiffness and soreness in the neck. Symptoms usually appear anywhere from one day to about a month after starting therapy.
Withdrawal Seizures
Patients taking Lamictal should not abruptly stop treatment. Patients with epilepsy may experience an increase in seizure frequency and people with bipolar disorder may develop seizures. Slowly weaning off the drug for at least two weeks is recommended.
Drug Interactions
Lamictal’s drug label lists several drugs that may increase or decrease the drug’s blood concentration.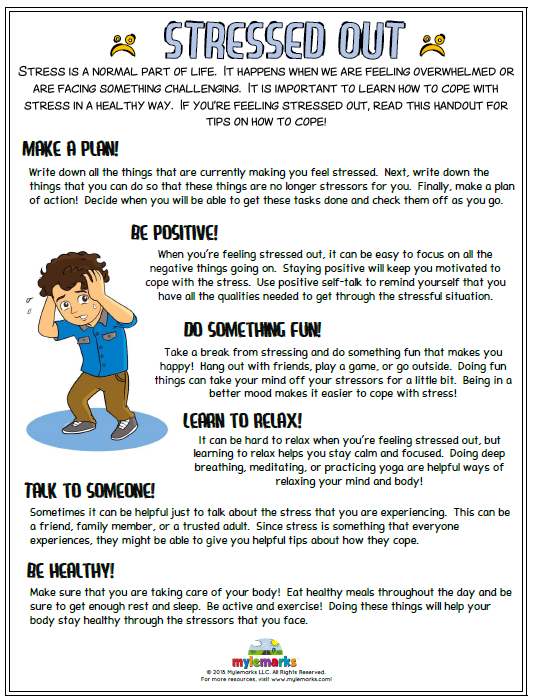 This could lead to less effective medication or an increase in side effects if the concentration is too high.
This could lead to less effective medication or an increase in side effects if the concentration is too high.
This is not a complete list of potential drug interactions. Make sure you tell your medical provider about all medications, supplements and herbs you take.
Drugs that interact with Lamictal include:
- Oral contraceptives with ethinylestradiol and levonorgestrel decrease lamotrigine concentration and decrease levonorgestrel.
- Carbamazepine and carbamazepine epoxide decreases lamotrigine concentration and may increase carbamazepine epoxide levels.
- Lopinavir/ritonavir decreases lamotrigine concentration.
- Atazanavir/ritonavir decreases lamotrigine concentration.
- Phenobarbital/primidone decreases lamotrigine concentration.
- Phenytoin decreases lamotrigine concentration.
-
Rifampin decreases lamotrigine concentration.
- Valproate increases lamotrigine concentration two fold. Some studies suggest taking these drugs together increases the risk of potentially fatal drug-induced skin rashes.
Special Precautions
Make sure you talk to your medical provider about any allergies you have, medications you take or preexisting health conditions. Lamictal might not be safe or effective for everyone.
Before taking Lamictal:
- Tell your doctor and pharmacist if you are allergic to lamotrigine or any ingredients in the tablets. For example, some formulas may include lactose.
- Tell your doctor or pharmacist about the medications you take, especially drugs in the interactions list or other drugs used to treat epilepsy.
- Tell your doctor if you use medications that contain female hormones such as birth control or hormone replacement therapy (HRT).
-
Tell your doctor if you have or have ever had lupus or any other autoimmune disease in which the immune system attacks healthy tissues and organs; a blood disorder; mental health conditions or kidney or liver disease.
- Tell your doctor if you plan to be pregnant or are pregnant. Call your doctor right away if you become pregnant while taking lamotrigine.
- Tell your doctor if you are breastfeeding or plan to breastfeed. Lamotrigine may pass to your baby through breast milk. Tell your doctor if your baby has interrupted breathing, poor sucking or unusual sleepiness.
- Know that this medication can cause sleepiness and/or dizziness. Don’t operate machinery or drive until you know how Lamictal affects you.
-
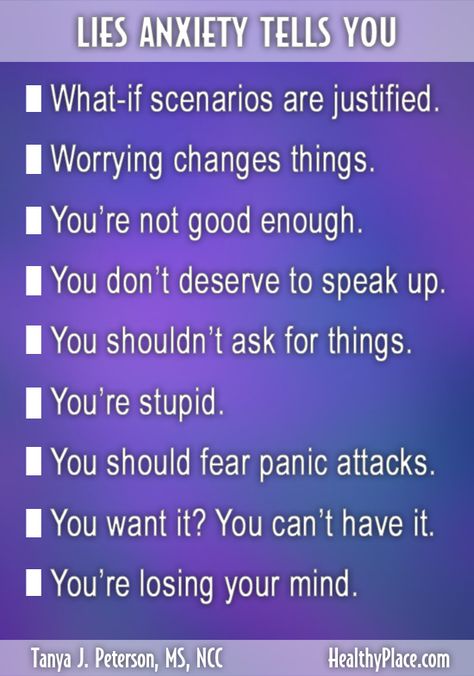
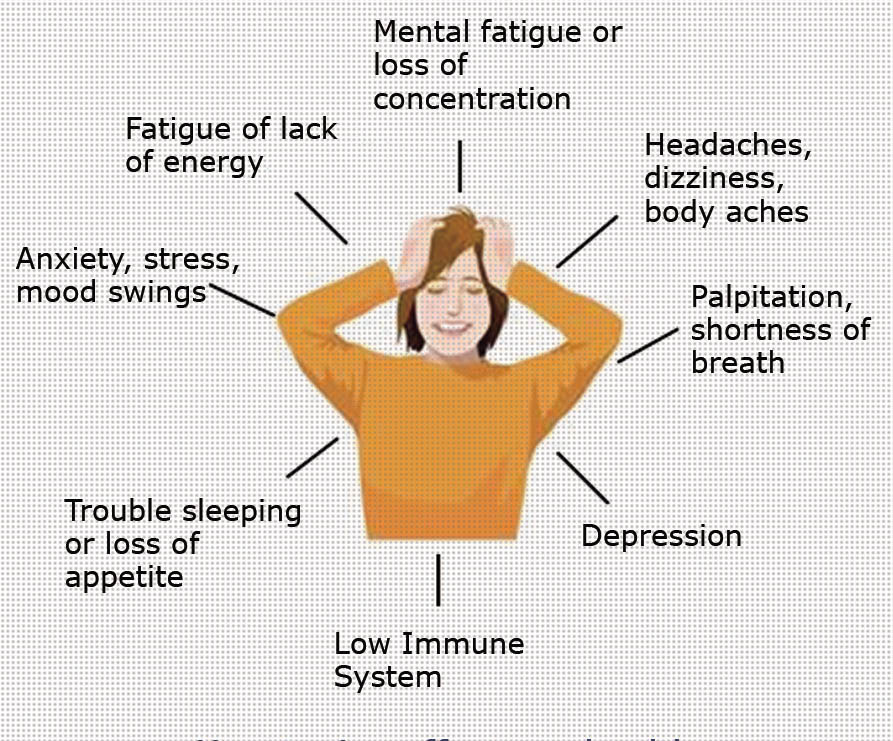
Know that you may experience changes in your mental health. This medication may cause thoughts of suicide, panic attacks, agitation, new or worsening irritability, restlessness, anxiety, dangerous impulses, depression, insomnia, aggressive behavior, abnormally excited moods and other unusual changes in mood. Tell another person close to you about these symptoms so they can help you look out for them. Tell your doctor right away if you experience changes in mood or mental health.

Lamictal Facts
Please seek the advice of a medical professional before making health care decisions.
TELL US WHAT YOU THINK
Did You Find Drugwatch Helpful?
Yes No
Thank you for your feedback. Do you have any thoughts you'd like to share about Drugwatch.com?
This article changed my life!
This article was informative
I have a question
How can we improve this page?
This article contains incorrect information
This article doesn't have the information I'm looking for
I have a question
How can we improve this page?
Thank You for Your Feedback
We appreciate your feedback. One of our content team members will be in touch with you soon.
We appreciate your feedback. One of our content team members will be in touch with you soon.
What is Lamictal (Lamotrigine): Uses, Dosage, Interactions, & Side Effects
Lamictal is a prescription medication that goes by the generic name Lamotrigine. It comes in four forms that are all taken by mouth: immediate-release oral tablets, extended-release oral tablets, chewable oral tablets, and orally disintegrating tablets.
Lamictal (Lamotrigine) belongs to a class of medications called anticonvulsants, or antiepileptic drugs (AEDs). These types of drugs work by altering electrical activity in neurons or altering chemical transmission between neurons. This decreases excitation of certain mechanisms in the brain that may lead to seizures.
For that reason, Lamictal is most commonly prescribed to treat seizures or epilepsy. However, it has also been used for long term mood disorders such as bipolar disorder, and shows promise in being effective for treating anxiety.
If you’re thinking of taking Lamictal (lamotrigine), it can be helpful to have some background information before speaking to your doctor to see if it might be right for you. Here’s everything you need to know.
Lamictal (Lamotrigine) for Depression
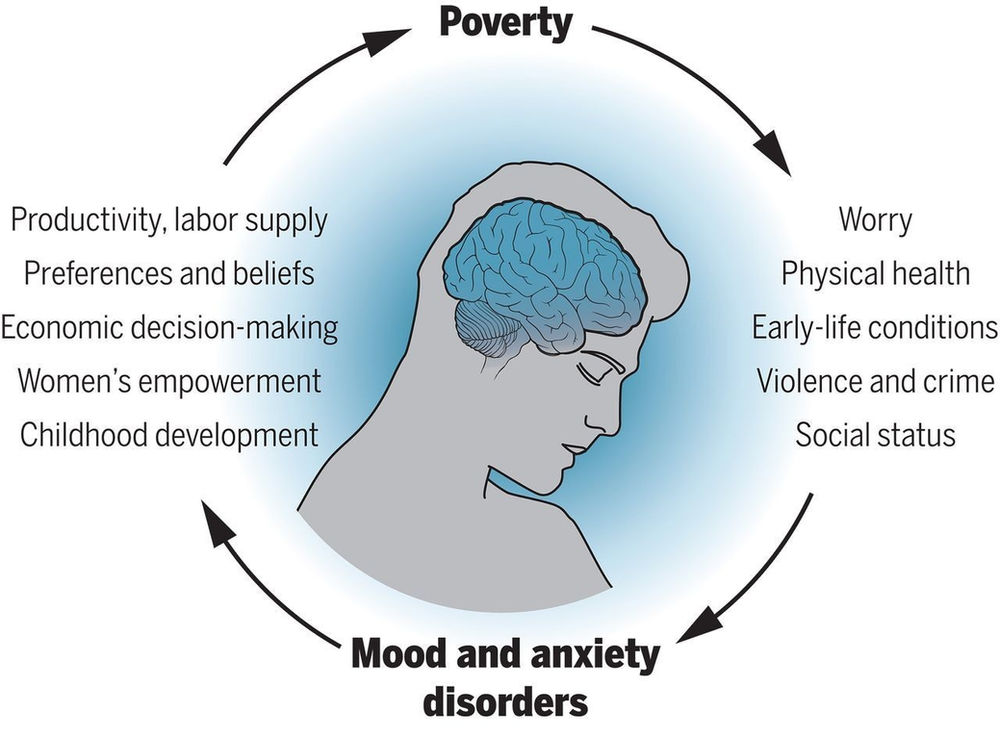
Lamictal is not normally prescribed for treating depression on its own. Instead, it has a distinct place in pharmacology for treating bipolar disorder. Bipolar disorder is marked by shifts in mood, usually fluctuating between symptoms of depression and symptoms of mania.
There are a number of mood stabilizing medications available, but what makes Lamictal unique is that it is the only one that lifts the depressive symptoms rather than suppressing the manic symptoms. This is because it is believed to act on serotonin reuptake.
For that reason, it can be useful for treating those on the bipolar spectrum, as the depressive symptoms often outweigh the manic ones. Plus, Lamictal doesn’t tend to come with many of the unwanted side effects that are common among other antidepressant medications.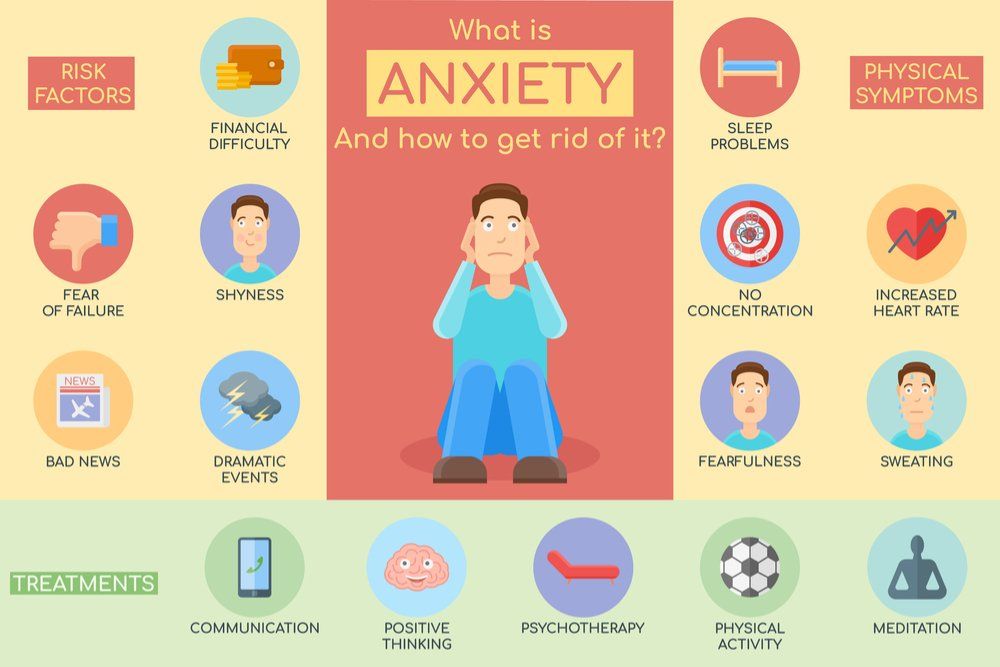
Lamictal (Lamotrigine) for Anxiety
The Food and Drug Administration (FDA) has approved the use of Lamictal for treating seizures and bipolar disorder. However, it has not been approved to treat anxiety disorders. If a doctor prescribes this medication for your anxiety, it is known as an “off-label” use.
There are few studies that show the efficacy of Lamictal for anxiety on its own.
With that said, some research suggests that it works especially well for individuals who experience symptoms of anxiety as a byproduct of their bipolar disorder.
Lamictal has also been used in combination with SSRIs (selective serotonin reuptake inhibitors) for people who are resistant to other types of treatment for mixed anxiety and depression symptoms.
Lamictal (Lamotrigine) Dosage
If your doctor prescribes you lamotrigine, you’ll likely start on a low dose and gradually increase over several weeks. The typical dose falls somewhere between 25 mg and 400 mg. Oral tablets are usually taken once or twice daily with or without food.
If you miss a dose, you shouldn’t double the dose or take extra to make up for forgotten doses.
Lamictal needs to be taken for some time before you start seeing the most positive results. Treatment of bipolar disorder usually requires lifelong commitment. If you happen to miss more than three days of your medication, contact your doctor, as they may need to adjust your dose.
Always follow your prescribing physician’s dosing instructions.
Lamictal (Lamotrigine) Side Effects
As with any medication, Lamictal can come with some side effects. Some of the most common side effects include:
- Drowsiness
- Dizziness
- Headache
- Blurred vision
- Nausea
- Dry mouth
- Sore throat
- Fever
- Tremors
- Symptoms of anxiety
There are also more serious side effects that can occur from taking Lamictal. One that is most noteworthy is a life-threatening skin rash, also known as Stevens-Johnson syndrome.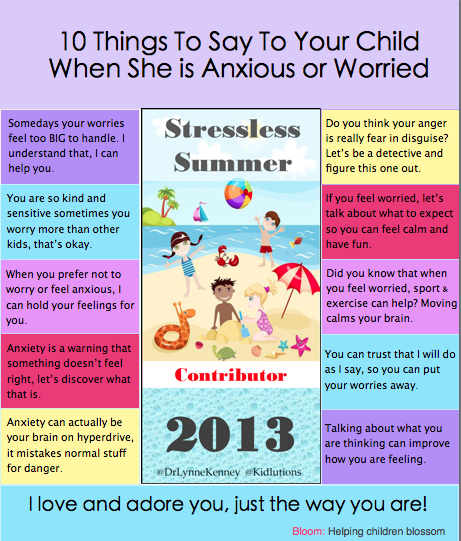 This is a rare, but serious condition that causes a rash on the skin that spreads and blisters over time.
This is a rare, but serious condition that causes a rash on the skin that spreads and blisters over time.
If you have hives, painful sores, shortness of breath, or blisters in and around your mouth, contact an emergency service immediately.
Another rare, but serious, possible side effect of taking Lamictal is aseptic meningitis. This causes serious inflammation of the protective membrane that covers the brain and spinal cord. If you experience intense headaches, fever, chills, vomiting, stiff neck, rash, unusual sensitivity to light, or confusion, you should see an emergency healthcare provider right away.
Some reports of a serious multi-organ hypersensitivity reaction have been associated with taking Lamictal. This may lead to kidney, liver, or heart damage. If you experience enlarged lymph nodes, fever, or rash, you should contact a doctor immediately.
Also, if you suddenly stop taking Lamictal without proper guidance from a doctor, it can cause seizures. You should never stop taking this medication without first speaking to your healthcare provider.
Drug Interactions with Lamictal (Lamotrigine)
Keep in mind that everyone’s body chemistry is different. You might not have a reaction if you combine Lamictal with other medications. Talk to your doctor for a comprehensive list of possible interactions that might be more in line with your individual risk factors.
This medication can interact with other medications. Namely, taking antiseizure drugs with Lamictal can decrease the effectiveness of both medications in your body. On the other hand, Depakote (Sodium Valproate), an anticonvulsant, can increase the effects of Lamictal.
Lamictal also shouldn’t be taken with certain heart arrhythmia medications, such as Tikosyn (Dofetilide). When used together, it can increase the levels of Tikosyn and lead to irregular or fatal arrhythmias.
Finally, taking Lamictal with oral contraceptives may affect how well either medication functions. If you’re on birth control, you may want to talk to your doctor about possible alternatives to Lamictal.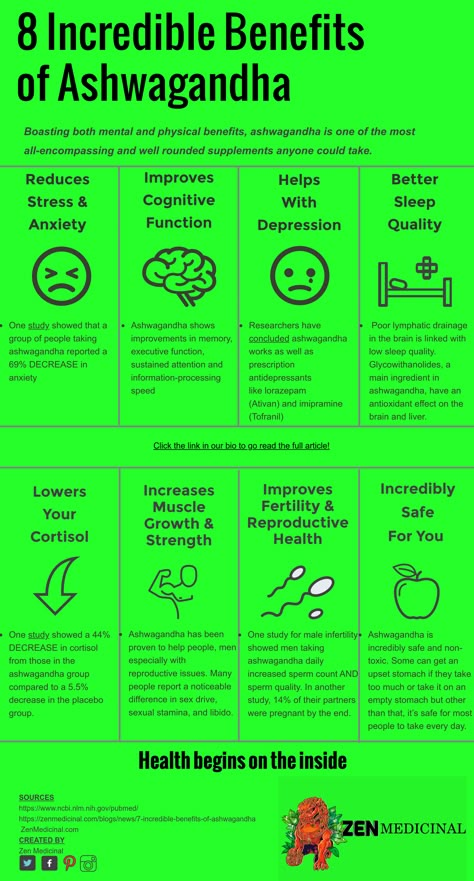
In Conclusion
Lamictal (Lamotrigine) is an anticonvulsant medication that is often prescribed to help reduce seizures or epilepsy. However, it is also FDA-approved to treat bipolar disorder and has shown some effectiveness as an off-label treatment for anxiety and depression.
Lamictal has some mild side effects, but there are some serious rare side effects that are possible. One is Stevens-Johnson syndrome, a deadly skin rash. Other possible serious side effects include aseptic meningitis or organ damage.
This medication should not be taken alongside other drugs without first speaking to your doctor. Its effects can be diminished if taken with certain anticonvulsants, heart arrhythmia medications, or birth control medications.
If you’re struggling with mental health issues, YANA Mental Health can get you on the path to recovery by pairing you with a doctor who will develop a personalized treatment plan just for you. If prescribed, medication will be sent straight to your door — quickly and discreetly. YANA provides quality mental health care on your terms, at your own pace.
YANA provides quality mental health care on your terms, at your own pace.
Sources:
Neurology : Antiepileptic medications | The Royal Children’s Hospital Melbourne
The role of lamotrigine in the management of bipolar disorder | NCBI
Treating comorbid anxiety and depression: Psychosocial and pharmacological approaches | NCBI
Lamictal (Lamotrigine) | National Alliance on Mental Illness
Stevens-Johnson syndrome – Symptoms and causes | The Mayo Clinic.
Comparative efficacy of mood stabilizers in the complex therapy of bulimia nervosa
The main forms of eating disorders are anorexia nervosa and bulimia nervosa. There are data in the literature on an increase in the number of patients with this pathology [7–9, 11] over the past decade.
According to ICD-10, for a reliable diagnosis of bulimia nervosa, the following signs are required: a) constant preoccupation with food and an irresistible craving for food, when the patient periodically cannot resist overeating and takes a large amount of food in a short time; b) counteracting the effect of obesity from the food eaten by the patient using one or more methods: inducing vomiting; abuse of laxatives, alternative periods of fasting; use of appetite suppressants, thyroid medications, or diuretics; neglect of insulin therapy by diabetic patients with bulimia; c) the presence in the psychopathological picture of a morbid fear of obesity, when the patient sets for himself a clearly defined limit of body weight - much lower than the premorbid weight, which in the eyes of the doctor represents the optimal or normal weight; frequent history of previous episodes of anorexia nervosa with remissions between the two disorders from several months to several years; the episode preceding bulimia may be symptomatic or mild with moderate weight loss and/or a transient period of amenorrhea.
According to our data [2], patients with bulimia nervosa are characterized by the presence of cyclothymic affective fluctuations, often associated with the season, in combination with increased impulsivity, decreased control over primitive drives and/or severe anxiety disorders, and a tendency to abuse alcohol and drugs and nicotine addiction.
Since affective fluctuations, especially depression, are constantly found in bulimia nervosa, the use of antidepressants and mood stabilizers is justified. The presence of high impulsivity, psychopathic and impulse disorders justify the use of small doses of neuroleptics (behavior correctors). Thus, psychopharmacotherapy in the treatment of bulimia nervosa should be complex. We are talking about a combination of antidepressants and normothymic drugs with low doses of antipsychotics. As normotimics, it is advisable to use carbamazepine and lamotrigine.
Lamotrigine is an antiepileptic drug that blocks voltage-gated sodium channels in the presynaptic membranes of neurons and inhibits the excessive release of glutamic acid (an amino acid that plays a key role in the development of epileptic seizures). In addition, effects on calcium channels, GABAergic and serotonergic components are described. It is likely that the complex mechanism of action determines the wide spectrum of activity of lamotrigine in epilepsy and a positive effect on mood, which is used in the treatment of bipolar disorders. It should be noted that to date, lamotrigine is the only normotimic, the effectiveness of which, including in patients with "rapid phase change" [5], has been proven in methodologically correctly constructed blind, placebo-controlled studies [3, 4]. Lamotrigine is particularly effective in preventing depressive phases in patients with bipolar affective disorder [6].
In addition, effects on calcium channels, GABAergic and serotonergic components are described. It is likely that the complex mechanism of action determines the wide spectrum of activity of lamotrigine in epilepsy and a positive effect on mood, which is used in the treatment of bipolar disorders. It should be noted that to date, lamotrigine is the only normotimic, the effectiveness of which, including in patients with "rapid phase change" [5], has been proven in methodologically correctly constructed blind, placebo-controlled studies [3, 4]. Lamotrigine is particularly effective in preventing depressive phases in patients with bipolar affective disorder [6].
Carbamazepine is a derivative of tricyclic iminostilbene containing a carbamoyl group in position 6, which mainly determines the presence of anticonvulsant activity in the drug. Structurally, carbamazepine is close to tricyclic antidepressants of the dibenzoazepine group. The drug has a pronounced anticonvulsant (antiepileptic) and moderately antidepressant (thymoleptic) and normothymic effect. In the mechanism of action of carbamazepine, its GABAergic properties, as well as interaction with central adenosine receptors, play a certain role. In terms of overall effectiveness, carbamazepine is not inferior to lithium carbonate and sodium valproate, however, it has a different spectrum of normothymic action, since its effect is more fully manifested in relation to the reduction of depression compared to mania [1, 12]. The antidepressant effect of carbamazepine is less pronounced than the antimanic effect [10].
In the mechanism of action of carbamazepine, its GABAergic properties, as well as interaction with central adenosine receptors, play a certain role. In terms of overall effectiveness, carbamazepine is not inferior to lithium carbonate and sodium valproate, however, it has a different spectrum of normothymic action, since its effect is more fully manifested in relation to the reduction of depression compared to mania [1, 12]. The antidepressant effect of carbamazepine is less pronounced than the antimanic effect [10].
The aim of this work was to study the effectiveness of mood stabilizers - carbamazepine and lamotrigine in the complex therapy of bulimia nervosa using an antidepressant.
Fluoxetine, a serotonin reuptake inhibitor, was chosen as the first choice antidepressant for bulimia nervosa. Fluoxetine is a weak antagonist of cholinergic, adreno-, and histamine receptors. Unlike many antidepressants, it does not cause a decrease in the functional activity of postsynaptic β-adrenergic receptors, improves mood, reduces feelings of fear and tension, and reduces dysphoria without the effect of sedation. In average therapeutic concentrations, it practically does not affect the functions of the cardiovascular system.
In average therapeutic concentrations, it practically does not affect the functions of the cardiovascular system.
Material and methods
The study included 45 women with various forms of bulimia nervosa. Their mean age was 22.5±4 years; the average duration of the disease is 4.2 years.
Patients included patients (60.9%) with cyclic affective fluctuations in the direction of downward mood and drive disorders and patients with less pronounced cyclic affective fluctuations, characterized by the presence of anxiety, in which there were no or mild drive disorders.
All patients had premorbid cyclothymic personality traits. 28 (62.2%) people abused alcohol, 23 (51%) - narcotic and other psychoactive substances, 72% of patients smoked; 25 (56%) women were distinguished by sexual disinhibition.
All patients at the time of examination had bulimic symptoms (strong hunger, insatiation, bouts of overeating with possible subsequent induction of artificial vomiting). In order to avoid possible, in their opinion, weight gain after overeating, they engaged in intense physical exercise and limited themselves to food, which was expressed in the use of various low-calorie diets, alternative fasting periods, as well as laxatives and diuretics, cleansing enemas. Almost all patients induced vomiting after bouts of overeating.
In order to avoid possible, in their opinion, weight gain after overeating, they engaged in intense physical exercise and limited themselves to food, which was expressed in the use of various low-calorie diets, alternative fasting periods, as well as laxatives and diuretics, cleansing enemas. Almost all patients induced vomiting after bouts of overeating.
Patients were randomized into two groups according to the characteristics of therapy.
In the 1st group (25 patients), patients were prescribed fluoxetine at a dose of 20 mg in the morning and carbamazepine at a dose of 200 mg in 3 doses (50 mg in the morning and afternoon and 100 mg in the evening).
The 2nd group (20 people) was prescribed fluoxetine 20 mg per day in the morning. Lamotrigine was included in therapy according to the scheme: 25 mg per day in the morning and then every 7 days the dose was increased by 25 mg/day up to 100 mg/day.
The selected groups did not differ in age and duration of the disease, as well as the features of complex therapy. In all cases, non-drug methods of treatment were used: individual and group psychotherapy, physiotherapy in the form of a circular shower, ultraviolet therapy, respiratory and relaxation therapeutic exercises.
In all cases, non-drug methods of treatment were used: individual and group psychotherapy, physiotherapy in the form of a circular shower, ultraviolet therapy, respiratory and relaxation therapeutic exercises.
After discharge from the hospital, all patients continued to take fluoxetine and normothymic for 6 months, and then, after fluoxetine was canceled, they continued to take normothymic for prophylactic purposes for another 3 months.
The ranking of bulimic symptoms was carried out as follows: no overeating - 0 points; overeating 1-2 times a week (low level) - 1 point; daily bouts of overeating followed by vomiting, no more than 1 time per day (average level) - 2 points; bouts of overeating daily, several times a day with the use of vomiting and gastric lavage (up to clean water), abuse of laxatives, diuretics (high level) - 3 points.
The severity of depression was determined on the Hamilton scale (HAM-D), the level of reactive and personal anxiety on the Spielberger self-assessment scale, the degree of asthenia according to subjective criteria with a score on a 5-point scale. In addition, memory functions and other cognitive functions were assessed.
In addition, memory functions and other cognitive functions were assessed.
The examination was carried out twice: before the start of pharmacotherapy and after 30 days of inpatient treatment. A year later, a follow-up examination of all patients was carried out.
Results and discussion
Against the background of complex therapy, patients of both groups noted the alignment of mood, a decrease in the frequency and intensity of overeating attacks, vomiting, and the normalization of food intake. As the mood leveled out, the level of fear of weight gain, the intensity of dysmorphophobic experiences, reactive and personal anxiety decreased in most patients.
When quantifying bulimic disorders, the following dynamics was established: before the start of therapy in the 1st group - 2.6 points, after 30 days from the start of therapy - 0.6 points; in the 2nd group before the start of therapy - 2.5 points, after 30 - 0.4 points.
The level of depression according to HAM-D was determined in the 1st group by an indicator of 15-23 points at the beginning of therapy in both groups, and after 30 days 5-7 points in the 1st group and 0-3 points in the 2nd. According to the Spielberger scale, the level of reactive anxiety before the start of therapy in both groups was high - more than 45 points; after 30 days it decreased to 28-35 points in both groups; averaged 29.6 points in the 1st group and 30.1 points in the 2nd. As for personal anxiety, its indicators changed: 34 points before the start of therapy and 28 points after 30 days, without significant differences between groups.
According to the Spielberger scale, the level of reactive anxiety before the start of therapy in both groups was high - more than 45 points; after 30 days it decreased to 28-35 points in both groups; averaged 29.6 points in the 1st group and 30.1 points in the 2nd. As for personal anxiety, its indicators changed: 34 points before the start of therapy and 28 points after 30 days, without significant differences between groups.
The phenomena of asthenia during therapy also decreased: from 5 to 2-3 points in the 1st group and to 0 in the 2nd.
There was also an improvement in cognitive functioning in terms of the ability to memorize and logical construction, the concept of attention, working capacity, the ability to synthesize and analyze the information received.
So, if before the start of the course of treatment, patients memorized from 4 to 6 words spoken aloud and from 3 to 5 geometric figures drawn on paper, then after 30 days of treatment in the 2nd group the number of memorized words increased to 6-9, and geometric shapes - 6-8, in the 1st group the number of memorized words changed little - 5-6 words, and the number of geometric shapes only up to 4-6.
Among the side effects in the 1st group, complaints of drowsiness and lethargy during the day prevailed. In the 2nd group, 3 patients developed skin-allergic reactions in the form of a rash, skin itching. Five patients were excluded from the study: 2 patients from the 1st group due to the severity of side effects and 3 patients from the 2nd group due to allergic reactions.
A follow-up examination of treated patients in a year gave the following results.
In the 1st group, 8 (34.8%) patients were found to be in stable remission, with no clinical manifestations of bulimia (they had no bouts of overeating for 6 months before the examination, body weight corresponded to a BMI from 18 to 21 points), and social rehabilitation (5 patients continued their studies at a higher educational institution, 3 patients got a job, 2 got married). 12 (46.1%) patients reported a relapse of the disease (overeating rate 2 points) after fluoxetine withdrawal, of which only 2 returned to work. In 3 (13%) patients, clinical manifestations persisted while taking medications (the frequency of vomiting ranged from 1 to 3 points).
In 3 (13%) patients, clinical manifestations persisted while taking medications (the frequency of vomiting ranged from 1 to 3 points).
In the 2nd group, 11 (64.7%) patients showed stable remission (for 6 months before the examination, there were no attacks of overeating, body weight corresponded to BMI from 18 to 21 points). At the same time, social rehabilitation was more successful (all 11 patients successfully continued their studies or got a job). 6 (35.2%) patients reported relapse (vomiting frequency 1 to 3 points) after fluoxetine discontinuation, and 1 (5%) patient continued to overeat and vomit.
Thus, the combination of fluoxetine and mood stabilizers during 30-day therapy of patients with bulimia nervosa made it possible to achieve a stable improvement in the condition of patients. At the same time, lamotrigine, compared with carbamazepine, caused a slightly greater decrease in the severity of depression. Carbamazepine had little effect on the cognitive functions studied, while the use of lamotrigine significantly improved them. Perhaps this is the reason for the greater number of cases of good social rehabilitation in the 2nd group (64.7%), compared with the 1st (34.8%). Prophylactic therapy with lamotrigine was also more effective (35.2% of patients with relapse after discontinuation of fluoxetine) compared with carbamazepine therapy (46.1%).
Perhaps this is the reason for the greater number of cases of good social rehabilitation in the 2nd group (64.7%), compared with the 1st (34.8%). Prophylactic therapy with lamotrigine was also more effective (35.2% of patients with relapse after discontinuation of fluoxetine) compared with carbamazepine therapy (46.1%).
The use of the normotimic lamotrigine as part of the complex therapy for bulimia nervosa turned out to be more effective in comparison with carbamazepine at the stage of inpatient treatment in terms of the effect on affective disorders, cognitive abilities and social rehabilitation in general.
The use of lamiktal (lamotrigine) in the treatment of patients with alcohol dependence: results of a comparative study - Psychiatry and psychopharmacotherapy named after. P.B. Gannushkina №05 2004
Subscribe to new numbers
The use of lamiktal (lamotrigine) in the treatment of patients with alcohol dependence: results of a comparative study No.
 05 2004
05 2004 Author: M.A. Vinnikova, T.V. Agibalova, G.L. Gurevich, L.V. PB №13 MZ and SR, Moscow
In narcological practice, anticonvulsants have been used for a long time for the relief of alcohol withdrawal syndrome (AAS), the actualization of a pathological craving for alcohol, and the prevention of convulsive paroxysms. Until recently, data on similar mechanisms of formation of paroxysmal brain activity and pathological attraction syndrome served as a pathogenetic justification for the use of this group of drugs.
At the same time, new data have appeared on the possibility of a therapeutic effect of normotimics (anticonvulsants) on pathological desire through the regulation of the GABAergic system.
Various systems of neurotransmitter regulation of the brain are involved in the mechanisms of alcohol dependence formation, the most important and significant of which are dopamine [1, 2], opioid [3], serotonergic [4–6], GABAergic [7, 8] systems .
In narcological practice, anticonvulsants have been used for a long time for the relief of alcohol withdrawal syndrome (AAS), the actualization of a pathological craving for alcohol, and the prevention of convulsive paroxysms [9–17].
Until recently, data on similar mechanisms of formation of paroxysmal brain activity and craving syndrome served as a pathogenetic justification for the use of this group of drugs [10].
At the same time, new data have appeared on the possibility of a therapeutic effect of mood stabilizers (anticonvulsants) on pathological desire through the regulation of the GABAergic system [18–24]. Some authors [25] indicate that normotimics can enhance dopaminergic and adrenergic neurotransmission.
This gives grounds to consider anticonvulsants as the drugs of choice in the treatment of pathological craving for alcohol.
One of the promising drugs in this group is lamiktal (lamotrigine). The results of clinical studies of lamiktal indicate its high efficacy in the treatment of a wide range of different types of epileptic seizures, including simple and complex partial, primary or secondary generalized. Many authors point to a significant therapeutic effect of lamictal on cognitive functions, mood, and behavior. The effectiveness of lamiktal in narcological practice has not been practically studied [26]. The undertaken clinical comparative research is devoted to the decision of these questions.
Many authors point to a significant therapeutic effect of lamictal on cognitive functions, mood, and behavior. The effectiveness of lamiktal in narcological practice has not been practically studied [26]. The undertaken clinical comparative research is devoted to the decision of these questions.
The aim of study was to investigate the therapeutic efficacy of lamiktal in the treatment of craving for alcohol in patients with alcohol dependence in comparison with carbamazepine. The effect of lamiktal on pathological craving for alcohol was studied at various stages of the disease: AAS, post-withdrawal state and remission formation.
Material and research methods
The total number of patients who participated in the study was 40 people. All male patients underwent inpatient treatment for the period from 2002 to 2003 at the Department of Clinical Psychopharmacology of the NSC Narcology. The age of the patients ranged from 35 to 60 years, the mean age was 42. 3±7.8 years. The duration of the disease in the presented sample ranged from 3 to 35 years, the average duration was 15.5±8.5 years.
3±7.8 years. The duration of the disease in the presented sample ranged from 3 to 35 years, the average duration was 15.5±8.5 years.
Patients with a high suicidal risk were excluded from the study; chronic somatic diseases in the acute stage; hypersensitivity to the drug; epileptiform seizures of non-alcoholic origin in history; treated within 30 days prior to inclusion in the study with antidepressants, anticonvulsants, antipsychotics, tranquilizers, nootropics.
The sample was divided into groups using the block randomization method. The groups did not differ in age, socio-demographic indicators, the main clinical and dynamic characteristics are presented in tab. 1.
Axial dependence syndromes were diagnosed according to ICD-10.
The majority of patients (32 people) were diagnosed with the middle stage of alcohol dependence. This was confirmed by the following clinical manifestations: fully formed primary pathological craving for alcohol, loss of quantitative control, maximum tolerance to alcohol, advanced AAS, sharpening of premorbid personality traits.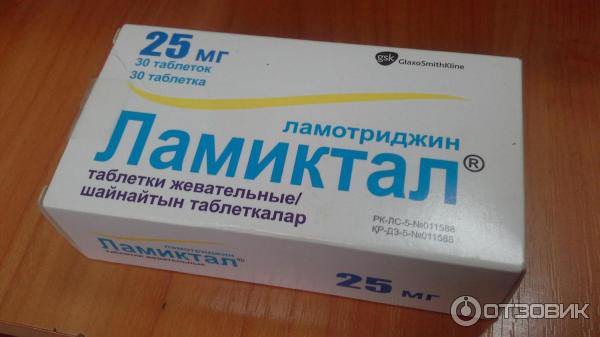 In most patients, the rate of progression of the disease was classified as medium, and the form of use was classified as pseudo-drunkenness.
In most patients, the rate of progression of the disease was classified as medium, and the form of use was classified as pseudo-drunkenness.
In 3 patients, a transitional stage II–III was diagnosed. This was evidenced by the changing type of drunkenness: an intermittent form of alcohol abuse was observed. 5 patients had clinical signs of the final stage of chronic alcoholism. The diagnostic criteria were a decrease in tolerance to alcohol, the appearance of drunkenness like true binges, signs of alcohol degradation and encephalopathy, and significant somatic and social consequences of alcoholism.
All patients had chronic somatic diseases caused by long-term alcohol intoxication (without exacerbation), mainly toxic damage to the liver and heart. Negative social consequences were characterized by the disruption of family relations and the decline in professional skills.
The structure of AAS included somatovegetative and psychopathological disorders. All patients had hyperhidrosis, thirst, tremor, dyspeptic disorders, fluctuations in blood pressure, tachycardia, weakness, fatigue, sleep disorders, depressed mood, anxiety, irritability, dysphoria. The severity of AAS was classified as moderate in 28 patients and as severe in 12 patients. 12 patients had predilirious disorders in the form of severe internal anxiety, prolonged insomnia with nightmarish disturbing dreams before admission, anorexia, hypnagogic hallucinations, erratic arousal in the emergency department, severe general tremor, fragmentary overvalued unsystematized ideas of persecution with a pronounced affective substrate in the form of fear and dysphoria . Convulsive seizures within 3 days before admission were noted in 5 patients.
The severity of AAS was classified as moderate in 28 patients and as severe in 12 patients. 12 patients had predilirious disorders in the form of severe internal anxiety, prolonged insomnia with nightmarish disturbing dreams before admission, anorexia, hypnagogic hallucinations, erratic arousal in the emergency department, severe general tremor, fragmentary overvalued unsystematized ideas of persecution with a pronounced affective substrate in the form of fear and dysphoria . Convulsive seizures within 3 days before admission were noted in 5 patients.
After the relief of acute disorders in the post-withdrawal state, various depressive disorders were the most common: decreased mood, anxiety, irritability, dysphoria, and asthenic manifestations.
The main research methods were clinical-psychopathological, statistical. When evaluating the spectrum of therapeutic efficacy of drugs, we used specially developed scales for assessing psychopathological and somatovegetative manifestations in AAS, the post-withdrawal state, and the scale of the overall clinical impression in the Department of Clinical Psychopharmacology.
The clinical study of drugs was carried out using a specially developed protocol that meets the international requirements of GCP (good clinical practice) as much as possible.
Statistical processing of the obtained results was carried out using the Microsoft Excel 2000 computer program. In connection with the tasks set, intragroup and intergroup comparisons were carried out. We checked the reliability of changes in the pathological craving for alcohol, the severity of affective and behavioral disorders under the influence of lamiktal in comparison with carbamazepine. The severity of each symptom was assessed on a 4-point scale: 0, no symptom; 1 - weak expression; 2 - moderate severity; 3 - strong expression. The results were recorded according to the scheme: mean value±confidence interval. The criterion of significance was the achievement of the level p<0.05 and less. Scores were compared using Student's t-test.
Study scheme
The study was carried out in two stages.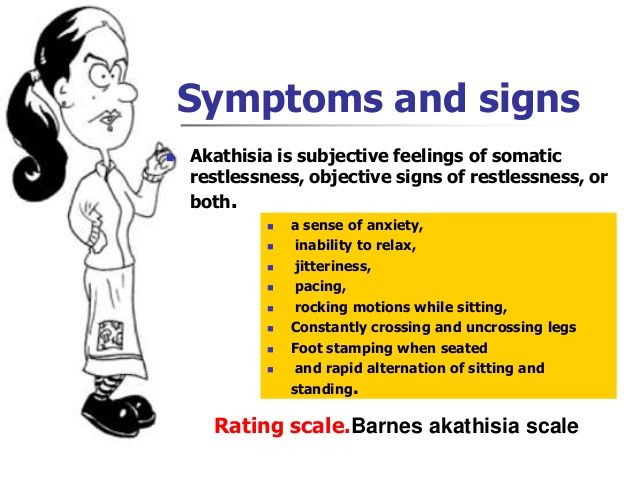 At the first stage, affective disorders were relieved in the AAS structure. The treatment was complex, carried out detoxification measures, restorative and symptomatic therapy. Anticonvulsants were prescribed from the first day of hospitalization as monotherapy. It is important to note that in severe AAS, with significantly pronounced psychopathological and somatovegetative symptoms, tranquilizers (phenazepam at a dose of up to 4–6 mg / day or Relanium at a dose of up to 10-15 mg / day). In addition, in predilirious conditions, infusion detoxification therapy lasted 2-3 days longer than usual.
At the first stage, affective disorders were relieved in the AAS structure. The treatment was complex, carried out detoxification measures, restorative and symptomatic therapy. Anticonvulsants were prescribed from the first day of hospitalization as monotherapy. It is important to note that in severe AAS, with significantly pronounced psychopathological and somatovegetative symptoms, tranquilizers (phenazepam at a dose of up to 4–6 mg / day or Relanium at a dose of up to 10-15 mg / day). In addition, in predilirious conditions, infusion detoxification therapy lasted 2-3 days longer than usual.
At the second stage, the treatment of affective, ideational, behavioral disorders in the post-withdrawal state, which are part of the structure of the pathological craving for alcohol, was carried out. Anticonvulsants were prescribed as the only pathogenetic drug. The daily therapeutic dose was 400–600 mg for carbamazepine and 200 mg for lamiktal. Carbamazepine was prescribed 1 tablet 2-3 times a day, Lamictal - 1 tablet 2 times a day.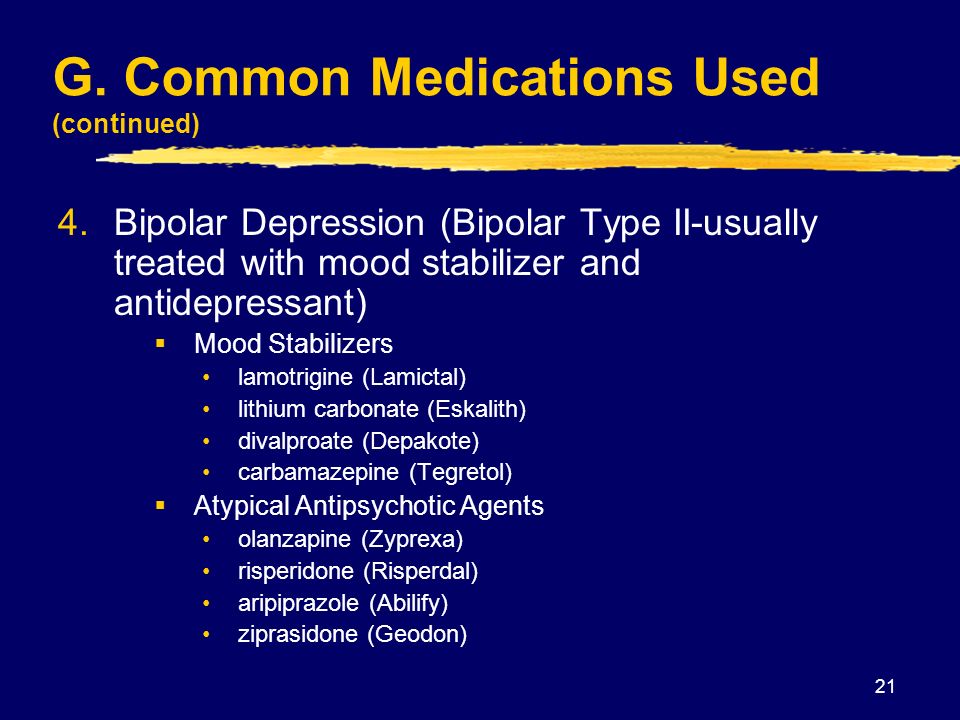
The duration of the clinical trial as a whole was 4 weeks.
Examination of patients was carried out on the day of admission (day 0), then on the 3rd, 7th, 14th, and 30th days of treatment.
The therapeutic effect of the drug was considered good if a 70% reduction in symptoms was achieved on the scales for assessing somatovegetative and psychopathological manifestations on the 3rd day, on the scale of the overall clinical impression on the 7th day of the study; complete reduction of symptoms according to a scale for assessing psychopathological manifestations on the 30th day of the study.
Research results
First of all, attention was paid to the ability of lamictal to stop the pathological craving for alcohol. As can be seen from tab. 2 , its reduction in the main group was observed already by the 3rd day of treatment, while in the control group it was observed only by the 7th day.
The drug had the most pronounced effect on such disorders as low mood, anxiety and sleep disorders. These disorders in the main group were stopped by the 3rd day of treatment (p<0.05), while in the control group, the reduction of anxiety, the ideator component of PVN, improvement in mood was noted by the 7th day, and sleep disturbances were stopped only by the 14th day. mu day of treatment.
These disorders in the main group were stopped by the 3rd day of treatment (p<0.05), while in the control group, the reduction of anxiety, the ideator component of PVN, improvement in mood was noted by the 7th day, and sleep disturbances were stopped only by the 14th day. mu day of treatment.
The drug had a less pronounced effect on dysphoria, irritability and internal tension, which were reduced by the 7-14th day of treatment. When comparing these parameters with the control group, there were no statistical differences, and dysphoria under the influence of carbamazepine stopped faster (by the 3rd day of treatment in the control group compared to the 7th day in the main group).
Lamictal also had a good effect on somatovegetative and neurological manifestations. A noticeable reduction in neurological disorders (tremor, ataxia) was observed by the 3rd day of treatment, while in the control group, by the 7th day of treatment ( tab. 3 ).
Separately, it is necessary to note the high anticonvulsant effect of lamiktal, which is superior to carbamazepine in the study sample. So, in patients with epileptiform convulsions in AAS after taking lamiktal, convulsions did not recur during treatment (3 patients), and in patients taking carbamazepine, repeated convulsive seizures were observed on the 2nd day of therapy (2 patients).
So, in patients with epileptiform convulsions in AAS after taking lamiktal, convulsions did not recur during treatment (3 patients), and in patients taking carbamazepine, repeated convulsive seizures were observed on the 2nd day of therapy (2 patients).
In the application of Lamictal in 2 cases, hyperemia of the skin and punctate rash were observed. These disorders were leveled by reducing the dose of the drug or prescribing symptomatic therapy after 2–3 days. In the control group, 5 people were diagnosed with diplopia, unsteady gait, and accommodation disorders.
The overall clinical impression scale confirmed the high therapeutic efficacy of lamiktal ( see figure ).
Discussion
In terms of its therapeutic spectrum, lamiktal surpasses the reference drug of this group, carbamazepine: it has a more pronounced normothymic and anti-anxiety effect and influence on insomnia disorders. The significant effect of the drug on neurological disorders in the AAS structure (general tremor, ataxia, etc. ) should be emphasized. Lamictal is better tolerated by patients, practically does not cause side effects with long-term use in comparison with carbamazepine.
) should be emphasized. Lamictal is better tolerated by patients, practically does not cause side effects with long-term use in comparison with carbamazepine.
The results of the study showed that lamiktal has a more pronounced redynamic effect compared to carbamazepine - an increase in physical activity, working capacity and stabilization of mood without increasing anxiety and anxiety.
This clinical study of the drug is practically the first experience of using lamiktal in the treatment of alcohol dependence, in particular, the possibility of stopping pathological craving for alcohol through the use of drugs with normothymic activity. The results of the study confirm the prospects for the use of normotimics (using the example of lamiktal) in the treatment of pathological craving and depressive disorders in its structure.
List of used literature Hide list
1. Anokhina I.P. Question. narcol. 1999; 2:45–51.
2.Anokhina I.P. Pathogenesis, clinic and treatment of alcoholism. Sat. n. tr. M., 1976; pp. 15–9.
3. Davis VE, Wolesh MJ. Science 1970; 167:1005–7.
4. Benkert O, Hippius H. Psychiatrische Pharmacotherapie. Berlin.: Springer. 1996.
5. Gorelick DA, Wilkins JN. Recent development in alcoholism. New York: Plenum. 1986; P. 283–305.
6. Yoshimoto K, McBride WJ, Lumeng LLiTK. Alcohol 1992; 9:17–22.
7. Bonner AB. Biological mechanisms of alcohol dependence. Cur Opinion Psychiat 1994; 7:262–8.
8. Rassnick S, D'Amico E, Riley E et al. Ann N Y Acad Sci 1992; 654:502–5.
9. Altshuler V.B., Burlakov A.V., Kravchenko S.A. Question. narcol. 1992; 3–4:47–51.
10. Altshuler V. B. Lectures on narcology (under the editorship of Prof. N. N. Ivanets). M.: "Knowledge". 2000; pp. 116–33.
11. Altshuler V.B. Pathological attraction to alcohol. M.: "Image". 1994.
12. Altshuler V.B. Neuropsychotropic drugs. Sat. symposium reports. M., 1995; pp. 136–42.
13. Macolm R, Ballenger JC, Sturgis ET, Anton R. Am J Psychiat 1989; 146:617–21.
14. Post RM. J Clin Psychyat V49 (Suppl.): 37–47.
15. Ritola E, Malinen L. Acta Psychiat Scand 1989; 64:254–9.
16. Rommelspacher H, Schmidt LG, Helmchen H. Nervenarzt 1991; 62:649–57.
17. Stuppaeck CH, Pycha R, Miller C et al. Alcohol Alcohol 1992; 27:153–8.
18. Avrutsky G.Ya., Neduva A.A. Treatment of mental patients. M.: Medicine. 1988.
19. Ezrielev G.I. New aspects of the pathogenesis of alcoholism. L.: Medicine. 1975.
20. Ivanets N.N., Kinkulkina M.A. Alcohol addiction treatment. News of medicine and pharmacy. 2001; 15–16.
21. Kravchenko S.L., Cherednichenko N.V. Neuropsychotropic drugs. Sat. symposium reports. M., 1995; pp. 149–51.
22. Mosolov S.N. Fundamentals of psychopharmacotherapy. M.: Ed. East house. 1996.
23. T_schner KL, Wiesbeck GA. Krankenhauspsychiatry 1993; 4:74–8.
24. Thome J, Wiesbeck GA, Vince GH. Fortschr Neurol Psychiat 1994; 62:125–33.![]()