Does the sweating from wellbutrin go away
Full List of Bupropion (Wellbutrin, Zyban) Side Effects
Sold under the brand name Wellbutrin®, bupropion is a medication that’s commonly prescribed in the treatment of depression. Sold under the brand name Wellbutrin XL®, it’s also used to treat seasonal affective disorder (SAD) and, when sold as Zyban®, as a medication to help people quit smoking.
Although bupropion is less likely to cause certain side effects than other antidepressants, there are still numerous side effects that you should be aware of if you currently use bupropion or are considering this medication.
Below, we’ve listed the side effects you may experience while using bupropion, with information on how frequently each side effect occurs, what you can do to manage it and your best options if any particular side effect persists.
Common Bupropion (Wellbutrin, Zyban) Side EffectsBupropion is an antidepressant medication used to help treat the symptoms of depression. Its most common side effects are similar to those of many other medications prescribed to treat depression. As with other antidepressants, most side effects that are associated with bupropion occur in the first few weeks of treatment and go away over time.
Common side effects of bupropion include:
Agitation
Dry mouth
Insomnia
Headache or migraine
Nausea and vomiting
Constipation
Tremor
Dizziness
Excessive sweating
Blurred vision
Tachycardia
Confusion
Rash
Hostility
Cardiac arrhythmia (irregular heartbeat)
Weight loss
Auditory disturbance
Of these, the most common side effects reported in clinical trials of bupropion were constipation, dizziness, dry mouth, headaches/migraines, nausea/vomiting, excessive sweating, agitation and tremor, which were all reported by more than 20 percent of users.
AgitationAgitation was the most common side effect reported in clinical trials of Wellbutrin, a medication containing bupropion prescribed to treat major depressive disorder (MDD) and seasonal affective disorder. According to data from the FDA, 31.9 percent of people reported agitation while using bupropion.
According to data from the FDA, 31.9 percent of people reported agitation while using bupropion.
Other side effects associated with agitation include insomnia, which affected about 18 percent of bupropion users in clinical trials.
If you feel agitated after using bupropion and don’t notice this side effect improving in the first few weeks of treatment, talk to your healthcare provider. They may adjust your bupropion dosage or recommend other changes to manage this side effect.
Try to exercise regularly. Other techniques that may help include deep-breathing exercises and yoga. If you continue to feel agitated while using bupropion, you may also want to talk to your healthcare provider about using medication to help you relax or switching to a different antidepressant.
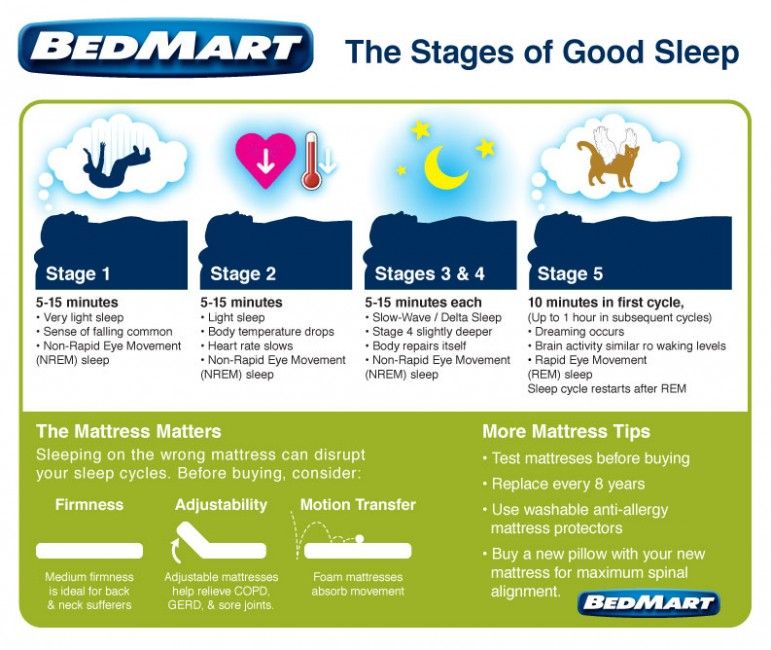
If you find it difficult to sleep after taking bupropion, avoid taking your medication close to your bedtime. Using bupropion earlier in the day will mean that a lower dose of the medication will be in your bloodstream at bedtime, which may make it easier for you to fall asleep.
And vice versa, if you find yourself saying, “Boy, Wellbutrin makes me tired” it may be worth talking to your healthcare provider about taking it at night, closer to bedtime.
Dry MouthBupropion and other antidepressants may cause xerostomia, or dry mouth. This side effect was reported by 27.6 percent of people who were prescribed bupropion in clinical trials, making it the second-most common side effect after agitation.
Dry mouth is a common side effect of many antidepressants, not only bupropion. It may be due to changes in your salivary glands caused by the medication. This side effect is generally more common with older antidepressants, such as tricyclic antidepressants (TCAs).
If you get dry mouth while using bupropion that doesn’t improve over the course of a few weeks, it’s best to talk to your healthcare provider. You can also try chewing sugarless or CPP-ACP gum to stimulate saliva production, which may help to loosen mucus and keep your mouth moist.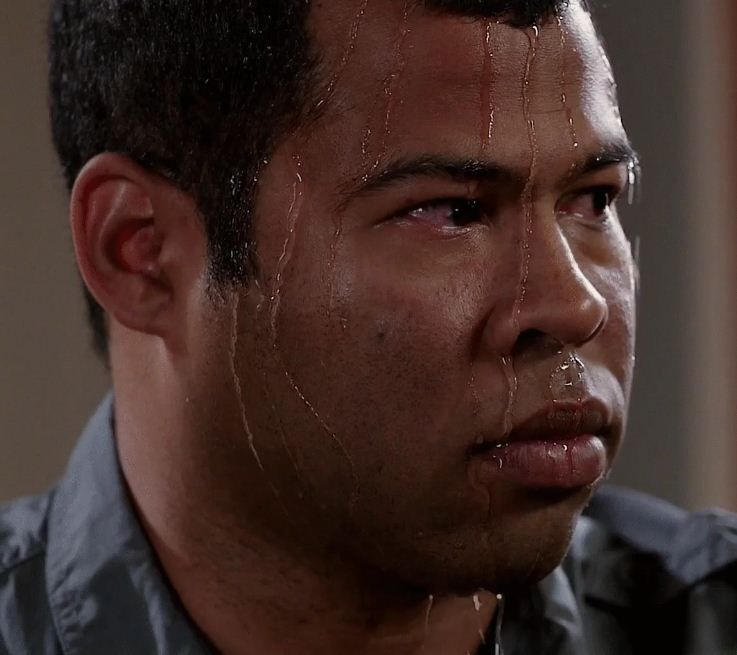
online counseling
the best way to try counseling
Headache/MigraineHeadaches and migraines are a fairly common side effect of bupropion, affecting 25.7 percent of people in clinical trials (versus 22.2 percent of people given a non-therapeutic placebo).
Like dry mouth, headaches are a common side effect of antidepressants. Interestingly, a 2012 study found that headaches were less common in bupropion users than in people prescribed SSRIs and other antidepressants.
As with other side effects of bupropion, your headaches may become less severe or go away completely as your body gets used to the medication. If you get persistent headaches, it’s best to talk to your healthcare provider.
Nausea/VomitingNausea and vomiting are common side effects of bupropion, reported by 22.9 percent of people in clinical trials.
As with many other side effects of bupropion, nausea and vomiting are common side effects of many antidepressants. Nausea caused by bupropion may get better or disappear completely over time as you become more used to the effects of the medication.
Nausea caused by bupropion may get better or disappear completely over time as you become more used to the effects of the medication.
If you often feel nauseous after using bupropion, try to take your medication with food, eat small and frequent meals and make sure that you stay hydrated. You can also try an over-the-counter antacid such as Pepto-Bismol® to provide temporary relief.
If you have persistent nausea or vomiting that doesn’t get better over time or with treatment, it’s best to talk to your healthcare provider.
ConstipationAccording to clinical trial data, 26 percent of people who use bupropion experience constipation as a side effect.
Like many other side effects of bupropion, constipation is a common side effect of medications used to treat major depression or the symptoms of depression. It’s particularly common with older antidepressants such as tricyclic antidepressants, as these medications can affect digestive function.
If you feel constipated after using bupropion or are experiencing Wellbutrin stomach pain, try increasing your intake of fiber-rich foods or use an over-the-counter fiber supplement. Other techniques that may help include drinking plenty of water and exercising regularly.
Other techniques that may help include drinking plenty of water and exercising regularly.
If you have severe, persistent or painful constipation after you start using bupropion, talk to your healthcare provider. They may recommend a non-prescription stool softener such as docusate sodium to ease your symptoms and make going to the toilet easier.
DizzinessDizziness is a relatively common side effect of bupropion, reported by 22.3 percent of people in clinical trials.
In addition to bupropion, several other antidepressants can cause dizziness. You may feel dizzy when you first start taking bupropion, or notice occasional dizziness when you stand up from a seated position or make other sudden movements.
To avoid dizziness, try avoiding caffeine, tobacco and alcohol while you use bupropion or other antidepressants. It can also help to avoid driving or operating machinery and practice standing up slowly when you need to get up. If necessary, you can use other items for support.
If you feel dizzy during the daytime, you can also talk to your healthcare provider about taking Wellbutrin at night, which may help to reduce the severity of this side effect.
Excessive SweatingAnother relatively common side effect of bupropion users, 22.3 percent of people in clinical trials experienced excessive sweating — a significantly larger percentage than those given a non-therapeutic placebo.
Sweating is a common side effect of antidepressants. It’s referred to as antidepressant-induced excessive sweating, or ADIES, and is estimated to affect between four and 22 percent of people who use antidepressants overall.
Excessive sweating from antidepressants usually affects the scalp, face, neck and chest areas, with symptoms often developing in bursts.
If you notice yourself sweating excessively or uncomfortably after you start using bupropion, it’s best to talk to your healthcare provider. They may prescribe medication to treat the sweating or switch you to new antidepressant or different dosage of bupropion.
Tremors — involuntary muscle contractions that usually affect your hands, limbs, head, face or eyes — is a common side effect of bupropion, affecting 21.1 percent of people in clinical trials.
Like other bupropion side effects, tremor is a common side effect of antidepressants, including selective serotonin reuptake inhibitors (SSRIs) and tricyclic antidepressants. It’s referred to as drug or medication-induced tremor (MIT) and can also occur with other medications.
If you get tremors after you start using bupropion, talk to your healthcare provider. Medication-induced tremors as usually treated by ending treatment with the medication that causes the tremors. They may also recommend adjusting your dosage or using a different type of antidepressant.
Bupropion and Sexual Side EffectsAntidepressants are often associated with sexual side effects, such as decreased sexual desire, erection problems, reduced sexual excitement and difficulty ejaculating.
These adverse effects are a particularly common occurrence in people who use selective serotonin reuptake inhibitors (SSRIs) and serotonin norepinephrine reuptake inhibitors (SNRIs).
In a 2000 article, researchers found that 30 to 40 percent of patients prescribed antidepressants developed some degree of sexual dysfunction. Other research has found that between 25 and 73 percent of SSRI and SNRI users reported sexual side effects.
Interestingly, although some bupropion users report experiencing a decrease in sexual function, research tends to show that bupropion is less likely to cause sexual side effects than other antidepressants, and may even help to reverse antidepressant-related sexual issues.
In a 2008 review, researchers noted there’s robust evidence that bupropion tends to cause less sexual dysfunction than SSRIs.
A separate study from 2004 also found that a sustained-release version of bupropion increased sexual desire and frequency of sexual activity in people with SSRI-induced sexual dysfunction.
In other words, bupropion may not cause the same sexual side effects as other antidepressants, or at least not cause them as often or severely. Still, if you notice any changes in your interest in sex or sexual performance after starting bupropion, it’s best to talk to your healthcare provider.
Bupropion and Changes in WeightAntidepressants are commonly associated with weight gain. This association is so strong that many people who are prescribed antidepressants stop using them either due to weight gain or concerns about weight gain during treatment.
Although there’s some evidence that you may gain weight after you start using antidepressants, the link isn’t as strong as many people think.
According to a study published in JAMA Psychiatry, most people who use antidepressants only gain a small amount of weight over 12 months — for most medications, an increase of less than one percent of their original, pre-treatment body mass index (BMI).
Unlike other antidepressants, bupropion typically doesn’t cause weight gain. For example, in the study above, the researchers found that people who used bupropion experienced fluctuations of less than 0.25 percent of their original BMI over the course of 12 months of treatment.
For example, in the study above, the researchers found that people who used bupropion experienced fluctuations of less than 0.25 percent of their original BMI over the course of 12 months of treatment.
Clinical trials of bupropion have also found that it typically doesn’t cause weight loss. In trials for Wellbutrin, a popular brand of bupropion, only 9.4 percent of people gained weight compared to 35 percent of people who received tricyclic antidepressants. Additionally, 28 percent of bupropion users actually lost more than five pounds.
Other studies have also found that bupropion causes mild weight loss when used over the long term.
In short, bupropion doesn’t appear to cause weight gain, at least not to the same extent as other common antidepressants. Most studies show the opposite — that bupropion either produces little change in weight or a small amount of weight loss.
Serious Side Effects of BupropionAlthough uncommon, bupropion may cause a range of more serious adverse effects, including adverse reactions that may require medical attention. We’ve listed these below and provided information on each potential side effect, as well as what you can do if you’re affected.
We’ve listed these below and provided information on each potential side effect, as well as what you can do if you’re affected.
Like other types of antidepressant medication, bupropion carries a “black box” warning from the FDA stating that it, as well as other medications in this category, may produce an increased risk of suicidal thoughts and behavior in children, adolescents and young adults.
Clinical trials of antidepressants do not show this risk in people over the age of twenty-four. Despite this, the FDA recommends monitoring for signs of suicidal thoughts or behavior in anyone prescribed an antidepressant.
This warning is common to antidepressants and also appears on the packaging of most SSRIs, SNRIs and other medications prescribed to treat depression and major depressive disorder. A less severe warning is used on the packaging of Zyban, a form of bupropion prescribed for smoking cessation.
If you experience suicidal thoughts, worsened depression or other abnormal thoughts after you start using bupropion, contact your healthcare provider as soon as you can. Call 911 if you think you are having a medical emergency.
Call 911 if you think you are having a medical emergency.
Bupropion may cause seizures. Use of bupropion is associated with seizures in approximately 0.4 percent of people at typical dosages of 450mg or less per day, making this a rare side effect. Seizures are significantly more common at dosages higher than 450mg per day.
The risk of seizures in people using bupropion is dose-related and is typically higher in people with conditions such as bulimia or anorexia, people who have quit using certain drugs or alcohol recently and people affected by seizure disorders.
Other conditions, such as metabolic disorders, head injury, prescription drug use or illegal drug use, may also increase your risk of seizures while using bupropion.
Hypertension (High Blood Pressure)Bupropion may contribute to an increase in blood pressure and hypertension (overly high blood pressure). Your healthcare provider may ask that you monitor your blood pressure periodically while using bupropion to stay aware of any increases or changes.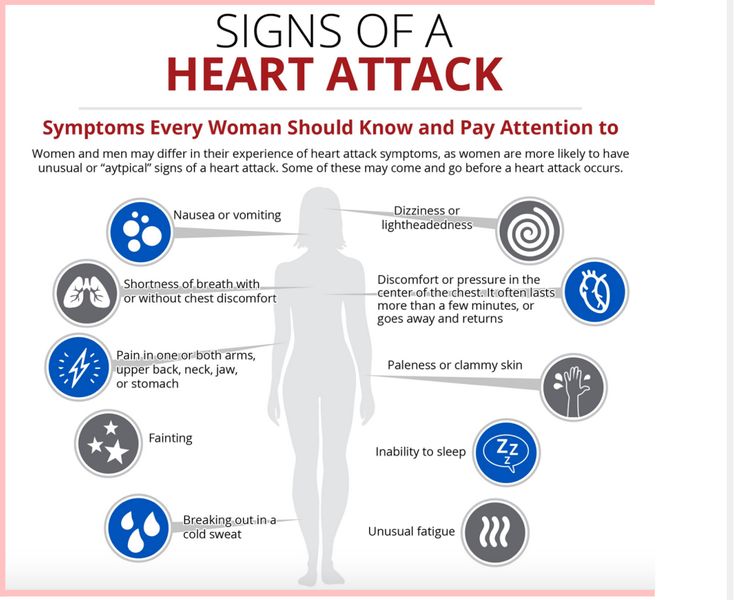
If you currently have hypertension, or have a history of cardiovascular health issues, your healthcare provider may adjust your dosage of bupropion, recommend careful monitoring of your blood pressure or prescribe a different medication.
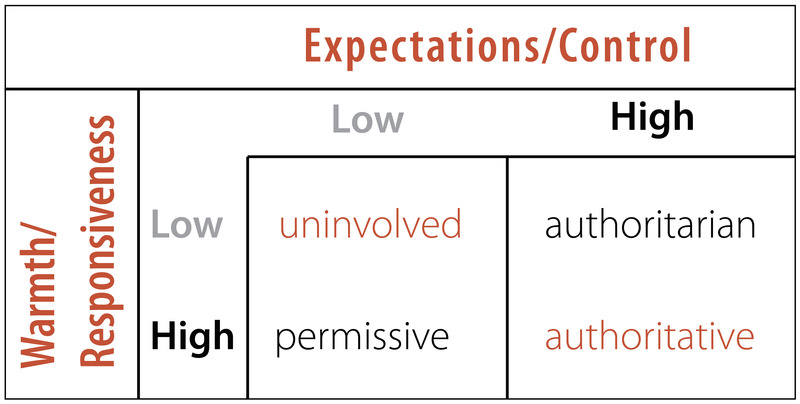
Activation of Mania/HypomaniaTreatment with antidepressants such as bupropion is associated with an increased risk of manic and hypomanic episodes, particularly in people who have risk factors for bipolar disorder or who have been diagnosed with bipolar disorder.
Bupropion is currently not approved by the FDA for treating bipolar depression. If you have bipolar disorder or display risk factors for bipolar disorder, your healthcare provider may recommend using another type of medication to treat your symptoms.
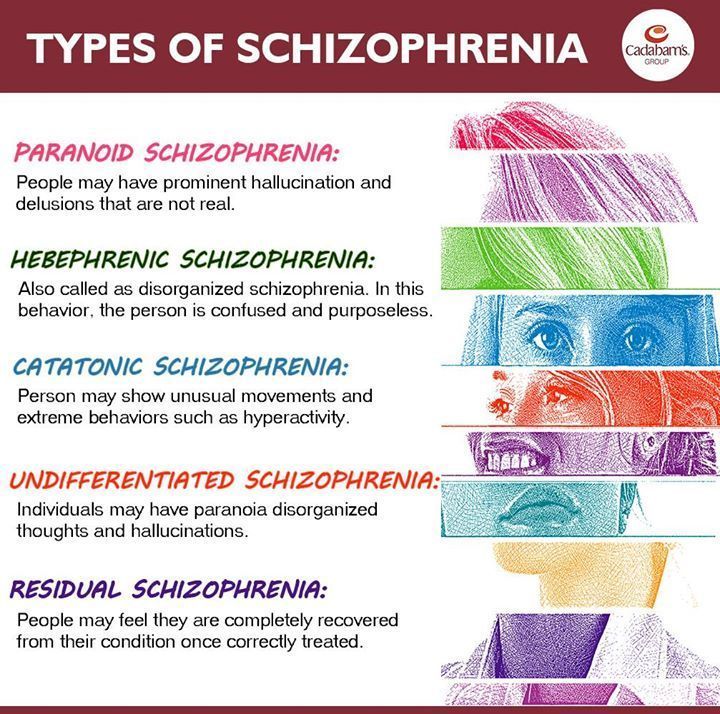
Psychosis and Other Neuropsychiatric SymptomsThere have been several reported cases of psychosis and other neuropsychiatric symptoms in patients treated with bupropion for depression. Several of these involved people who had previously used illicit drugs, while others involved patients diagnosed with bipolar disorder.
If you or a loved one experience any delusions, hallucinations, psychosis, paranoia, confusion or concentration disturbance while using bupropion, contact your healthcare provider.
Hypersensitivity ReactionsAlthough rare, bupropion may cause anaphylactoid/anaphylactic reactions. If you develop any symptoms of an allergic reaction, such as hives, skin rash, shortness of breath, edema, pruritus (itchy skin) or chest pain, contact your healthcare provider.
Drug InteractionsBupropion also may interact with other medications in ways that could cause some potential side effects.
If you’ve used monoamine oxidase inhibitors (MAOIs) within 14 days of starting bupropion, tell your healthcare immediately, as these drug interactions may be severe.
Potential drug interactions with bupropion also include other antidepressants like SSRIs, SNRIs and TCAs, as well as medications like antipsychotics, beta-blockers, blood thinners, corticosteroids and others.
As with other antidepressants, bupropion may cause withdrawal symptoms if you abruptly stop taking it as prescribed. This is known as antidepressant discontinuation syndrome, and is a common issue for people who suddenly end their usage of antidepressants.
Bupropion may be less likely to cause severe withdrawal symptoms than other antidepressants, such as SSRIs and SNRIs. However, if you’re prescribed bupropion and want to stop taking it, it’s still important to talk to your healthcare provider first.
To reduce your risk of experiencing bupropion withdrawal symptoms, your healthcare provider may recommend tapering your dosage gradually over time. We’ve explained this in more detail in our guide to bupropion withdrawal.
online psychiatrist prescriptions
talk to a psychiatry provider. it’s never been easier
Learn More About BupropionBupropion can help in the treatment of depression and make it easier for you to deal with nicotine cravings while quitting smoking. Our full guide to bupropion goes into more detail on how this medication works, common dosages, frequently asked questions and more.
Our full guide to bupropion goes into more detail on how this medication works, common dosages, frequently asked questions and more.
This article is for informational purposes only and does not constitute medical advice. The information contained herein is not a substitute for and should never be relied upon for professional medical advice. Always talk to your doctor about the risks and benefits of any treatment. Learn more about our editorial standards here.
Excessive Sweating Caused by Antidepressants: Measurement and Treatment With Glycopyrrolate (AIDES-G) - Full Text View
Sweating is a common and bothersome adverse effect of treatment with antidepressants. Tricyclics and selective serotonin reuptake inhibitors (SSRIs) have both been clearly shown to cause sweating. Increased sweating has been reported with venlafaxine (Pierre and Guze, 2000) and bupropion (Feighner et al. 1984) as well. It is unclear to what extent tolerance develops to antidepressant-induced sweating. It may continue to be a problem even after 6 or more months on the antidepressant (e.g., Mavissakalian et al., 2002).
It may continue to be a problem even after 6 or more months on the antidepressant (e.g., Mavissakalian et al., 2002).
The prevalence of sweating with SSRIs is estimated to be between 7% and 19% depending on the drug (Ashton & Weinstein 2002). According to the Physician's Desk Reference, excessive sweating occurs in 3-11% patients in clinical trials of SSRIs. Considering the fairly high prevalence of excessive sweating during antidepressant use and its consequences of patient distress and treatment noncompliance, it is important that more intensive efforts be made to understand the phenomenon and to systematically study potential treatments for it.
The mechanism of antidepressant-induced sweating has not been clearly elucidated and there is no generally accepted treatment for it. Initially, a reduction in the dose may be attempted to resolve antidepressant-induced sweating. However, a reduction of dose may not always be helpful (Leeman, 1990; Ashton & Weinstein 2002) as it has been noted that the presence of sweating is not a clear dose-related symptom. As well, reducing the dose of the antidepressant may lead to a worsening of depression and therefore be an unrealistic alternative.
As well, reducing the dose of the antidepressant may lead to a worsening of depression and therefore be an unrealistic alternative.
Antiadrenergic drugs like clonidine and terazosin (Feder, 1995; Mago and Monti, 2007; Mago et al., 2009) may be effective for the treatment of antidepressant-induced excessive sweating because the nervous system control of sweating is initially mediated by adrenergic receptors. However, antiadrenergic treatment may be associated with a decrease in blood pressure in some patients, which may lead to dizziness, especially on standing up. Also, the improvement in excessive sweating may not be complete.
Therefore, additional approaches are needed. Sweat glands are innervated by nerve fibers that release acetylcholine. Anticholinergic medications could be used as a potential treatment for the excessive sweating. In case reports, the anticholinergic drug benztropine has been successfully used to treat antidepressant-induced excessive sweating (Garber and Gregory, 1997; Feder and Guze, 2000). However, this has not been confirmed in a clinical trial. Also, benztropine readily crosses the blood-brain barrier; therefore, in addition to its desired effect peripherally on the sweat glands, it tends to cause cognitive side effects through its central effects.
However, this has not been confirmed in a clinical trial. Also, benztropine readily crosses the blood-brain barrier; therefore, in addition to its desired effect peripherally on the sweat glands, it tends to cause cognitive side effects through its central effects.
Glycopyrrolate is an anticholinergic medication that is preferred for a variety of clinical uses because it does not cross the blood-brain barrier to a great extent. It has been used for many years by anesthesiologists to dry secretions during surgical procedures. In a case series based on chart review (Tran et al., 2009), it was found to be effective for antidepressant-induced excessive sweating.
What does armpit sweating say - armpits sweat a lot, what to do, how to get rid of sweating forever
{{if type === 'partner-stocks'}}
{{/if}}
{{/if}} {{each list}}${this} {{if isGorzdrav}}
Delete
{{/if}}
{{/each}} {{/if}} Search by drug, disease, substance: DERMAKOSMETIKA, Nyureksan, Durex, From pain, VoltarenHome
Articles
What does sweating say
Sweat glands are located throughout the human body. They secrete a liquid that, when evaporated, helps to cool the body. This is how thermoregulation works. Sometimes the amount of sweat increases several times, this condition is called hyperhidrosis. Excessive sweating can be localized and affect only the armpits or palms. Sometimes this condition extends to the whole body. In this case, the causes are most often associated with various pathologies.
They secrete a liquid that, when evaporated, helps to cool the body. This is how thermoregulation works. Sometimes the amount of sweat increases several times, this condition is called hyperhidrosis. Excessive sweating can be localized and affect only the armpits or palms. Sometimes this condition extends to the whole body. In this case, the causes are most often associated with various pathologies.
What is hyperhidrosis
There are 2 types of sweat glands in humans, which differ in their functions and regulation mechanisms:
- fibers, where the main substance is adrenaline. They begin to function in adolescence, produce a secret with pheromones - an individual smell, under stress the function increases, but they do not participate in thermoregulation.
- Eccrine glands - the largest number - in the armpits, on the feet and palms, secrete the liquid part of sweat. The main regulator of the function is acetylcholine. The glands are involved in thermoregulation and sweating during stress.
The work of the vegetative unequal system that controls the sweat glands is not controlled by consciousness. Therefore, it is impossible to cause increased sweating on its own, it increases in response to an increase in body temperature during illness, in hot weather or after exercise. Sweating increases with excitement, emotional stress, which leads to the release of adrenaline.
But the state of hyperhidrosis is different from normal sweat production. The glands work actively when a person is calm and does not overheat. It is often associated with various pathologies. Allocate diffuse hyperhidrosis, in which sweating increases throughout the body. The disease is often associated with pathology of the nervous system. Local, or focal hyperhidrosis, affects only one area of the body. This form is the most common.
Sweating may be seasonal and occurs only during the hot season, but in most people with the pathology, it does not depend on the season.
Causes of excessive sweating
Dermatologists are most often visited by patients with a primary form of pathology, in which it is impossible to determine the cause. The first symptoms of hyperhidrosis appear during puberty. In girls and boys, this is due to an increase in the activity of the hormone testosterone and cortisol, the immaturity of the nervous system. Daily sweating becomes strong, activity increases in all types of sweat glands. Therefore, in adolescents, body odor increases.
The first symptoms of hyperhidrosis appear during puberty. In girls and boys, this is due to an increase in the activity of the hormone testosterone and cortisol, the immaturity of the nervous system. Daily sweating becomes strong, activity increases in all types of sweat glands. Therefore, in adolescents, body odor increases.
It is believed that primary hyperhidrosis in 30-50% of patients is associated with hereditary factors. But the first symptoms can appear at the age of 20-30 years. They are provoked by chronic stress, hormonal changes and other reasons. The secondary form of increased armpit sweating is associated with the following conditions:
- excitability and high activity of the autonomic nervous system;
- endocrine pathologies, most often the state of hyperthyroidism, insulin resistance in diabetes mellitus;
- diseases of the cardiovascular system, accompanied by a violation of the heart rhythm, palpitations;
- certain types of malignant and benign tumors;
- metabolic disorders and overweight;
- overdose or side effects of drugs that affect the autonomic nervous system.
It is not always possible to determine the cause of heavy sweating. But it helps to effectively fight sweating.
Armpit sweating in women
In the female body, the release of a large amount of sweat depends on the hormonal background. When it changes, the interaction of various parts of the autonomic nervous system changes. This process is most pronounced during menopause.
With a decrease in ovarian function in women, their stimulation by pituitary hormones - follicle-stimulating and luteinizing - increases. But due to physiological characteristics, at the same time, the release of thyroid-stimulating hormone increases, which increases blood flow in the thyroid gland. Most often, this process starts in the evening or at night. It manifests itself in the form of hot flashes - the appearance of a feeling of heat in the upper body and head. The woman begins to sweat profusely. The duration of such an attack is several minutes.
You are more likely to experience heavy sweating if you are overweight. Violations of thermoregulation appear with arterial hypertension. These diseases also often progress after age 50. Hyperhidrosis in this case is secondary. It does not pose a danger to life, but it causes discomfort.
Violations of thermoregulation appear with arterial hypertension. These diseases also often progress after age 50. Hyperhidrosis in this case is secondary. It does not pose a danger to life, but it causes discomfort.
Armpit sweating in men
The male body is regulated by the hormone testosterone. It performs an anabolic function, speeds up metabolism. Men are also more sensitive to adrenaline. Therefore, small bursts of this hormone increase the heart rate, increase the reaction rate and lead to armpit sweating.
A man may sweat more than usual if he prefers hot and spicy food. Sweating of the armpits and the whole body increases greatly when drinking alcoholic beverages. In this case, hyperhidrosis is associated with metabolic processes, so the body removes toxic substances after the utilization of ethanol. Nicotine is a direct stimulant. It increases the synthesis of acetylcholine, which enhances the work of the sweat glands. Therefore, in men who smoke, sweating is a natural phenomenon.
Sweating occurs with severe nervous strain. The work of men is more likely than that of women to be associated with stress or hazardous activities.
Men are prone to obesity, metabolic disorders and arterial hypertension. The risk group includes those who lead an inactive lifestyle, have a large waist circumference at the age of 45-50. These disorders affect the tone of the sympathetic nervous system and sweating.
When to see a doctor
If a person begins to sweat during exercise, hot weather, or a lot of excitement, there is no cause for concern. Health problems are indicated by sweating, which occurs against the background of complete calm or is accompanied by additional symptoms.
Slightly elevated body temperature accompanied by night or evening sweats may be a sign of a chronic infection. Sometimes this is manifested by pulmonary tuberculosis, immune disorders, the initial stages of oncological diseases.
A dangerous symptom is the appearance of weakness, dizziness, loss of consciousness against the background of increased sweating. This may be a sign of low glucose levels - hypoglycemia. The condition is life-threatening and therefore requires emergency medical attention. Hyperhidrosis is cured only after normalization of the level of glucose .
This may be a sign of low glucose levels - hypoglycemia. The condition is life-threatening and therefore requires emergency medical attention. Hyperhidrosis is cured only after normalization of the level of glucose .
Older women who have menstrual irregularities and the first symptoms of approaching menopause require special treatment. Without special means ( Klimadinon , etc.), the condition may gradually worsen, menopause will be difficult.
Increased sweat secretion is one of the signs of thyrotoxicosis. This disease is accompanied by an increase in thyroid function and the release of elevated doses of hormones into the blood. At the same time, the heartbeat increases, heart rhythm disturbances appear, a person quickly loses body weight, despite the preservation of the nature of nutrition.
Treatments for excessive sweating
To get rid of excessive sweating, it is necessary to eliminate provoking factors. They start with simple measures:
They start with simple measures:
- eat warm food, refuse spicy food;
- exclude alcohol from the diet;
- stop smoking;
- avoid stress or learn to control emotions.
Antiperspirant deodorants can help with mild cases. Vichy contains aluminum chloride and dimethicone to help regulate perspiration. Similar lineup in Dry Control Extra forte deodorant . For those who are allergic to deodorants, special Elfarma liners , which are also available in black, will help prevent clothing from soaking later.
Folk remedies help cure sweating. At home, prepare a decoction of mint, chamomile flowers, oak bark. In the solution, moisten a napkin, which wipe the problem areas. Baths with the addition of infusion on sage leaves are effective. But it is necessary to carry out therapeutic bathing no more than 1 time per week.
A cold compress can be used as an emergency remedy for excessive sweating. It does not cure the cause of the disease, but helps to narrow the blood vessels and reduce manifestations.
It does not cure the cause of the disease, but helps to narrow the blood vessels and reduce manifestations.
The use of anticholinergics helps to manage excessive sweating. But this method has many shortcomings, drugs act simultaneously on the entire sympathetic nervous system, therefore:
- salivation decreases;
- dry mouth appears;
- concerned about visual impairment;
- pupils dilate;
- may disturb the rhythm of the heart.
Treat hyperhidrosis with botulinum toxin injections. This tool belongs to the group of neurotoxins. After the introduction of the drug into the armpit, the innervation of the sweat glands is disturbed, they stop producing sweat in large quantities. But this is a temporary method of treating the disease, which is valid for 5 months. In the secondary form of hyperhidrosis, it is necessary to treat the underlying disease that causes excessive sweating.
Botox injections for underarm sweating
On the eve of summer, many people remember such a problem as hyperhidrosis. This is excessive sweating that occurs due to physiological, nervous or endocrine problems in the body. In the hot months, the problem escalates, and becomes a serious obstacle to self-confidence. Women are embarrassed by stains on clothes and an unpleasant smell, all this interferes with the normal pace of life, fetters and causes complexes. Modern cosmetology is able to solve the issue of hyperhidrosis using botulinum toxin from sweat.
This is excessive sweating that occurs due to physiological, nervous or endocrine problems in the body. In the hot months, the problem escalates, and becomes a serious obstacle to self-confidence. Women are embarrassed by stains on clothes and an unpleasant smell, all this interferes with the normal pace of life, fetters and causes complexes. Modern cosmetology is able to solve the issue of hyperhidrosis using botulinum toxin from sweat.
Features of the procedure
Using fine needles, the doctor injects underarm botulinum toxin under the skin. To prevent sweating of the armpits, I use botulinum toxin type A. The pre-treated area is anesthetized, and insulin syringes are used for injections. They have such thin needles that damage is minimal and numerous punctures are well tolerated.
Anti-sweat Botox injections are injected directly under the skin, but nothing enters the sweat glands. Before the procedure, the drug is diluted with saline, which allows the substance to be distributed even to those areas in which injections were not made. Punctures are carried out in a checkerboard pattern, and as a result, the entire area is covered. An injection in the armpits from sweat is an absolutely safe method to get rid of an unpleasant problem with sweat, and the procedure itself takes 10-15 minutes.
Punctures are carried out in a checkerboard pattern, and as a result, the entire area is covered. An injection in the armpits from sweat is an absolutely safe method to get rid of an unpleasant problem with sweat, and the procedure itself takes 10-15 minutes.
Botox anti-sweat injection disrupts the neuromuscular transmission in the treated areas, resulting in excessive sweating, odor and discomfort. The effect lasts for 8 months on average.
What areas are treated
Hyperhidrosis does not only appear in the armpits, the heels, palms, skin folds, back or forehead can also be problematic areas. Theoretically, any zone is subject to treatment, here it is more a question of portability. If we are talking about the back, then it is first necessary to consult a doctor and try to find the primary cause of such sweating, since it is not recommended to treat an area that is too large.
Botox against sweating in the heels is also used, but before the session it is necessary to do a thorough pedicure and treat the feet to remove the stratum corneum. The procedure not only removes sweating, but also reduces the risk of fungus, which develops just because of excess moisture.
The procedure not only removes sweating, but also reduces the risk of fungus, which develops just because of excess moisture.
Often the face is also prone to sweating, then sweat injections are injected into the forehead, which simultaneously solves two problems at once - sweating and the primary signs of aging. Botulinum toxin can slow down the appearance of mimic wrinkles.
Preparing for the procedure
Those wishing to undergo Botox injections for sweating will first have to pass a special test - iodine and starch are applied to the problem area, due to a chemical reaction, the mixture changes color, becomes dark blue. The brightness of the color indicates the presence of sweat glands, and in the future, during the session, the doctor will pay special attention to these areas.
Preparation includes getting rid of hair by any method and avoiding antiperspirants. Botox from sweat requires only one thing: no mechanical damage to the skin, obvious redness, irritation, swelling or scratches. If you have damaged the skin during epilation, you will have to wait until all the symptoms have passed.
If you have damaged the skin during epilation, you will have to wait until all the symptoms have passed.
After epilation, Botox injections for sweating can be carried out after 5-7 days, and laser hair removal can be continued 2 weeks after Botox injection, but remember that temperature effects reduce the duration of the effect of injections.
Many beauticians use local anesthesia to avoid pain. For example, an anesthetic cream that is applied in a thin layer to the treated area for 15-20 minutes. During this time, he begins to act, and you can start injections.
After the procedure, there is no pain, patients feel well and can immediately return to normal life. Papules dissolve in 2-3 days, and the armpits acquire an aesthetic appearance.
Will the sweat glands become blocked?
This is a common myth, but it has no basis. Underarm botulinum toxin is injected under the skin, not into the sweat glands, so there can be no blockage. The effect is achieved due to the peculiarities of Botox, which disrupts the neuromuscular connections in the treatment area, sweat simply stops being produced, and therefore the gland will not be affected.
The procedure is completely safe and has a cosmetic effect, relieving the discomfort and problems associated with hyperhidrosis. Compared to injections, conventional antiperspirant is much more dangerous if used frequently.
How to prolong the effect?
Your task is to reduce the effects of temperature as much as possible. During the first 7 days, you should not visit the sauna, bath and solarium. For the same period, it is important to limit physical activity and activity so as not to increase body temperature and not reduce the effectiveness of Botox.
It is also forbidden to drink any alcohol for at least three days after the first session. This is due to the fact that Botox injections for sweating develop their effectiveness gradually, and the effect of alcohol slows this process down.
Sweat injections in the area of the palms can partially reduce the sensitivity of the muscles for some time, therefore it is recommended to be careful when driving.