Is invega an atypical antipsychotic
Paliperidone (Invega) | NAMI: National Alliance on Mental Illness
Brand names:
- Invega®
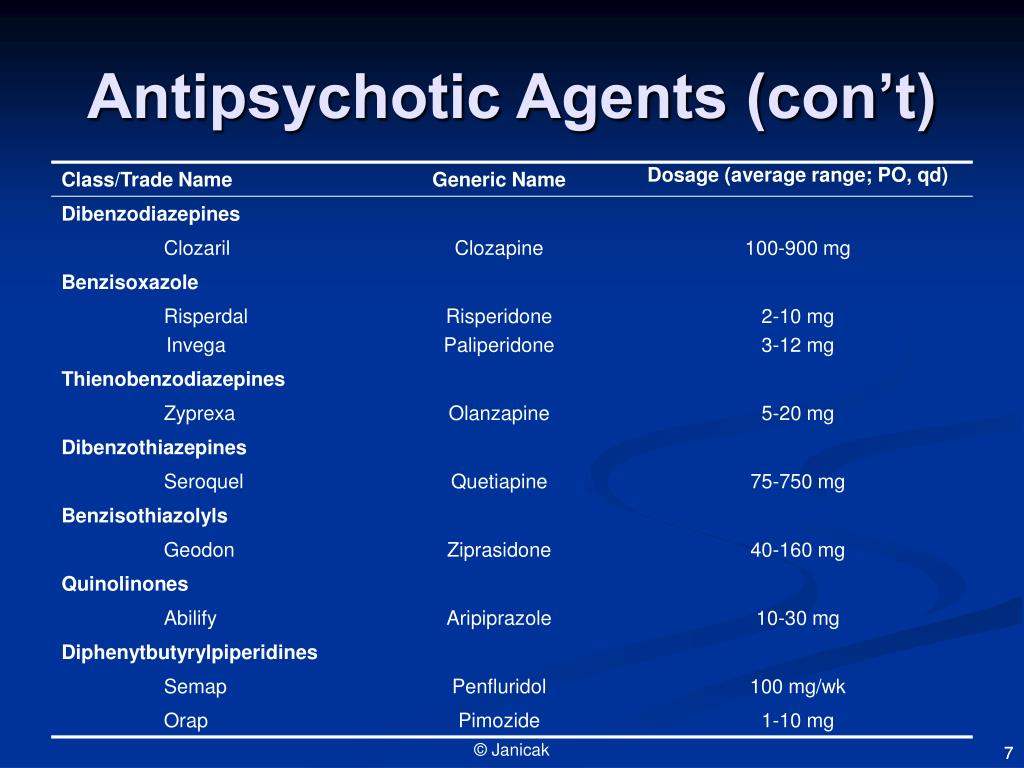
- Extended-release oral tablet: 1.5 mg, 3 mg, 6 mg, 9 mg
- Invega Sustenna®
- Extended-release intramuscular suspension: 39 mg, 78 mg, 117 mg, 156 mg, 234 mg
- Invega Trinza®
- Extended-release intramuscular suspension: 273mg, 410mg, 546mg, 819mg
- Invega Hafyera™
- Extended-release intramuscular suspension: 1,092 mg, 1,560 mg
Generic name: paliperidone (pal ee PER i done)
- Paliperiodone
- Extended-release oral tablet: 1.5 mg, 3 mg, 6 mg, 9 mg
All FDA black box warnings are at the end of this fact sheet. Please review before taking this medication.
What Is Paliperidone And What Does It Treat?
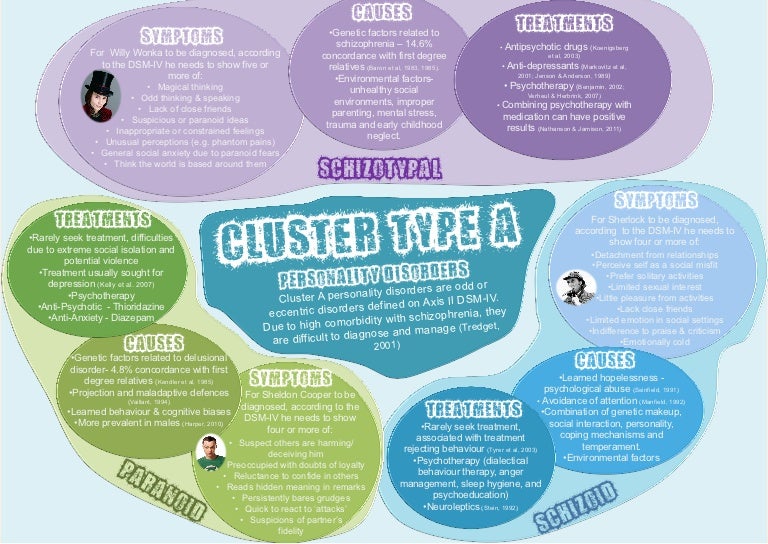
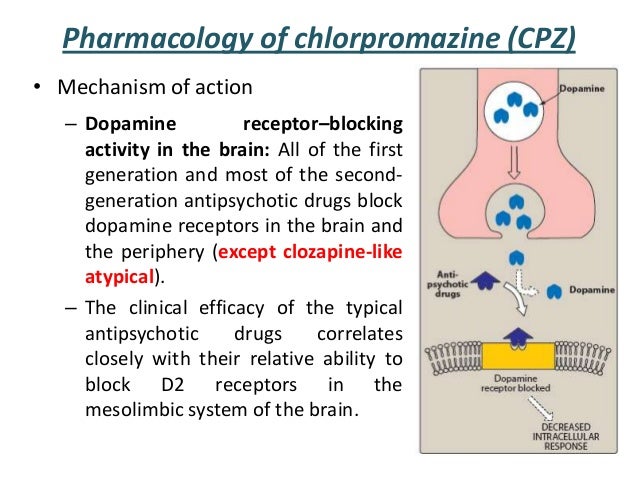
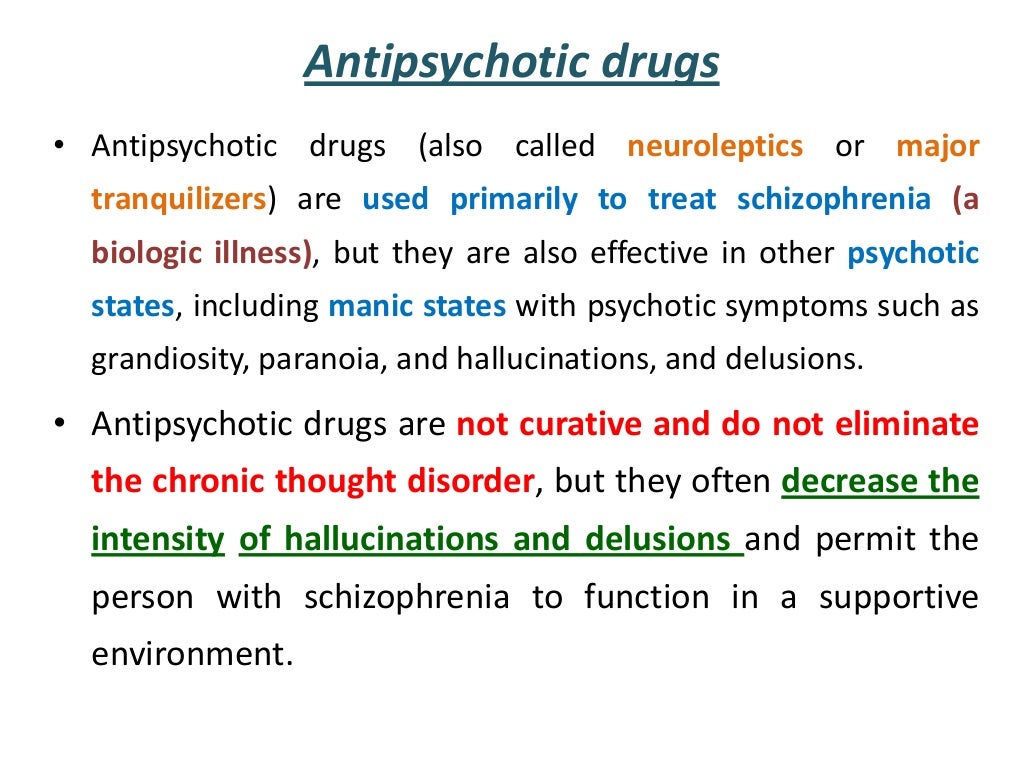
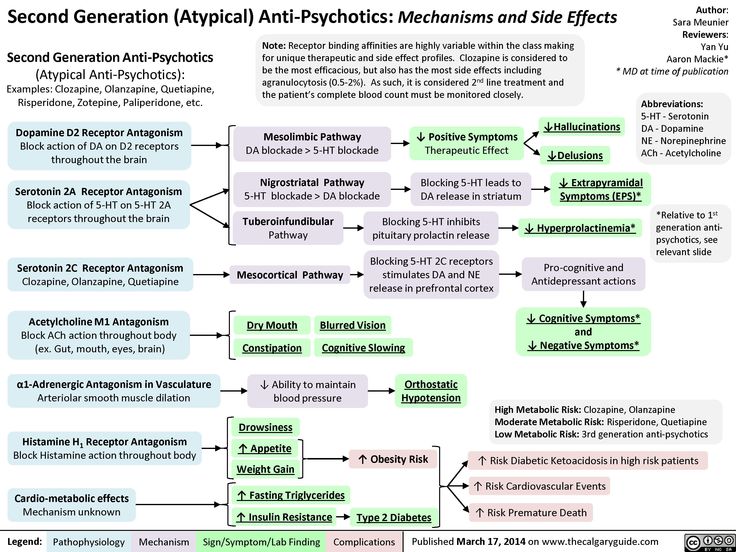
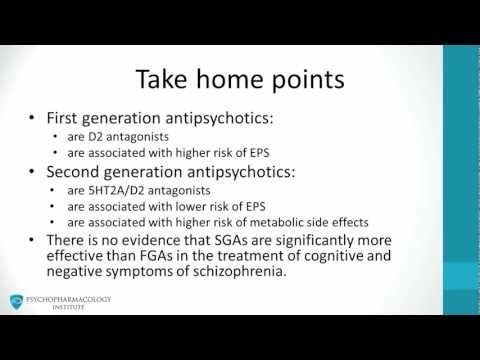
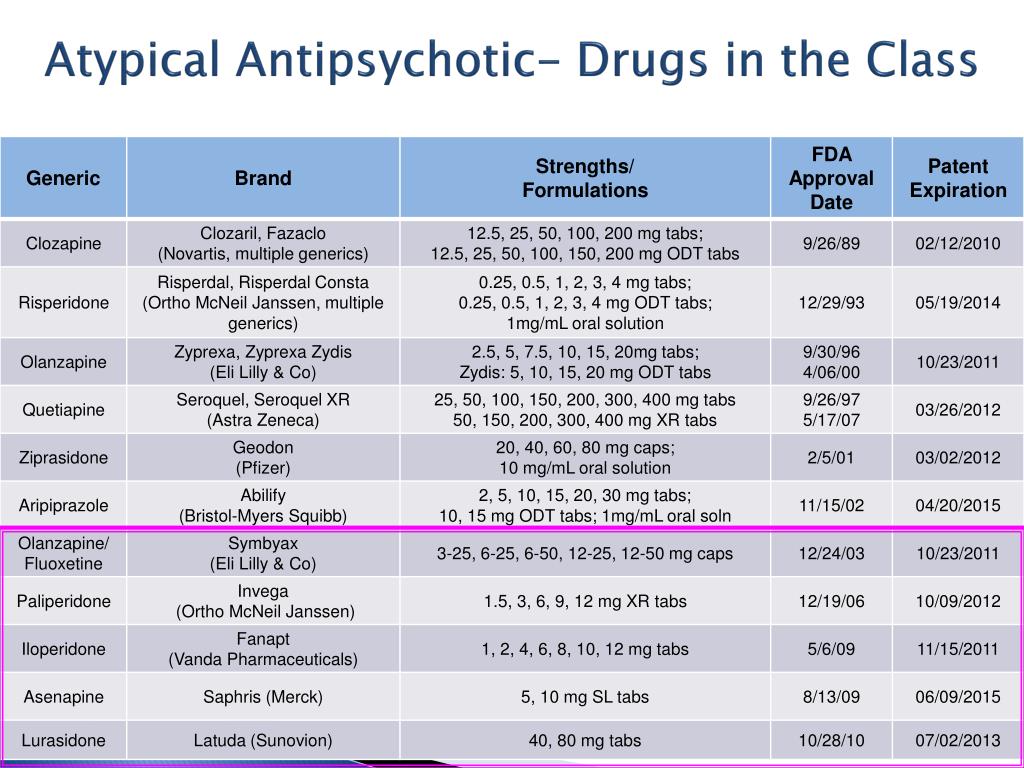
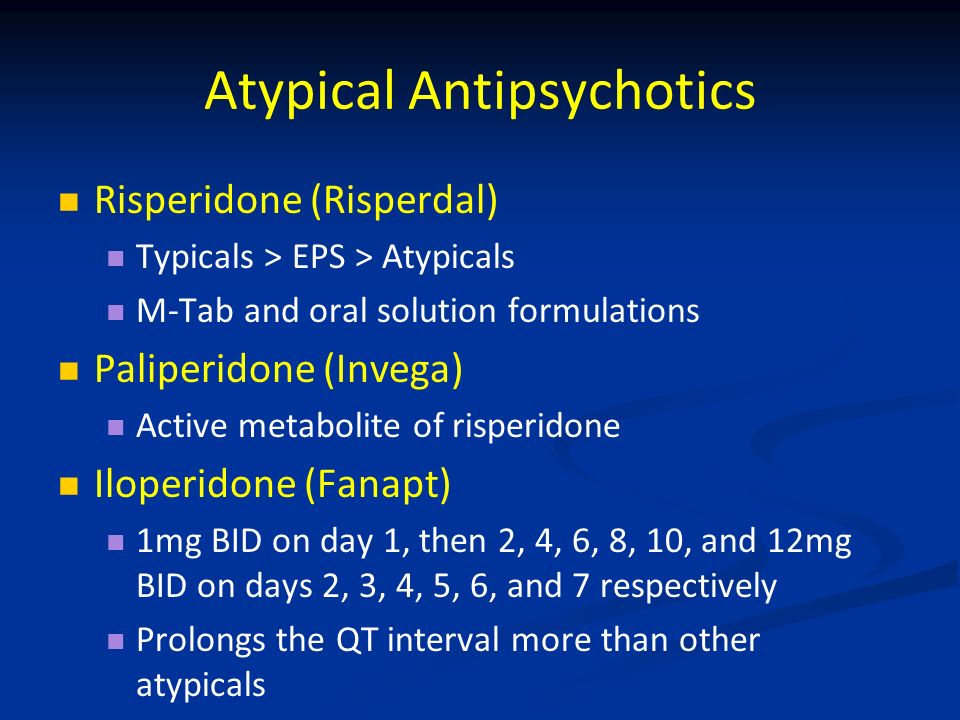
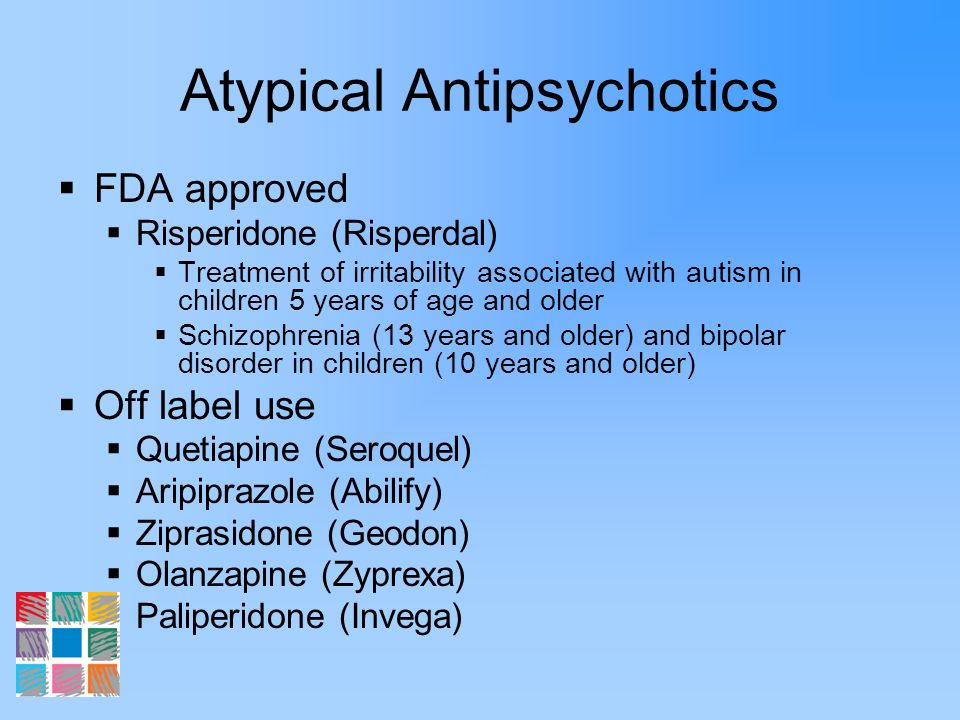
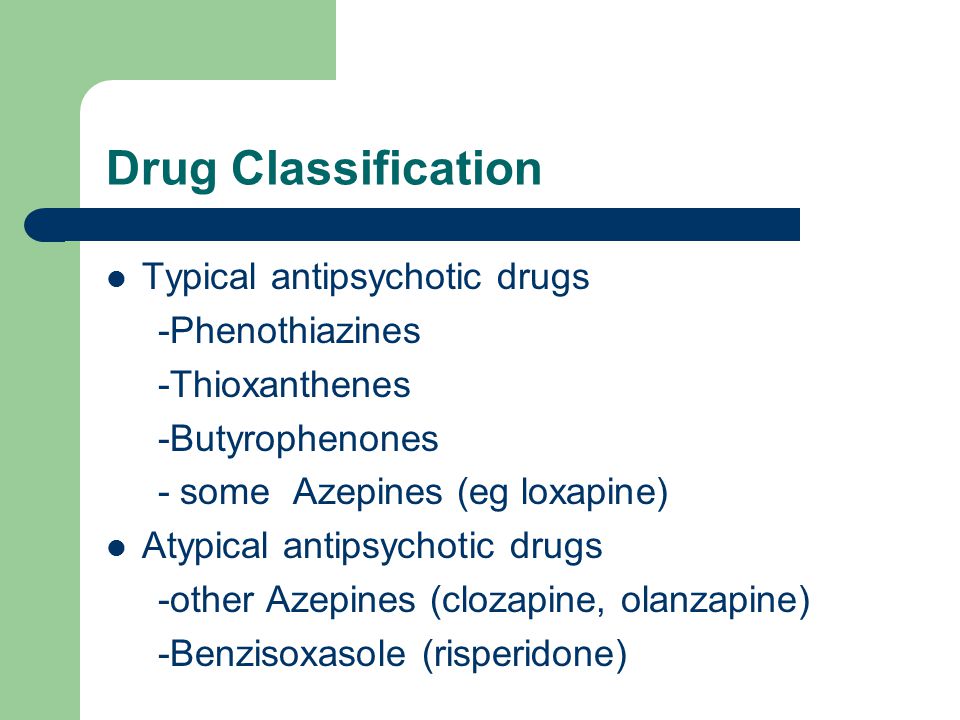
Paliperidone is a medication that works in the brain to treat schizophrenia and schizoaffective disorder. It is also known as a second generation antipsychotic (SGA) or atypical antipsychotic. Paliperidone rebalances dopamine and serotonin to improve thinking, mood, and behavior.
Symptoms of schizophrenia include:
- Hallucinations – imagined voices or images that seem real
- Delusions - beliefs that are not true (e.g., other people are reading your thoughts)
- Disorganized thinking or trouble organizing your thoughts and making sense
- Little desire to be around other people
- Trouble speaking clearly
- Lack of motivation
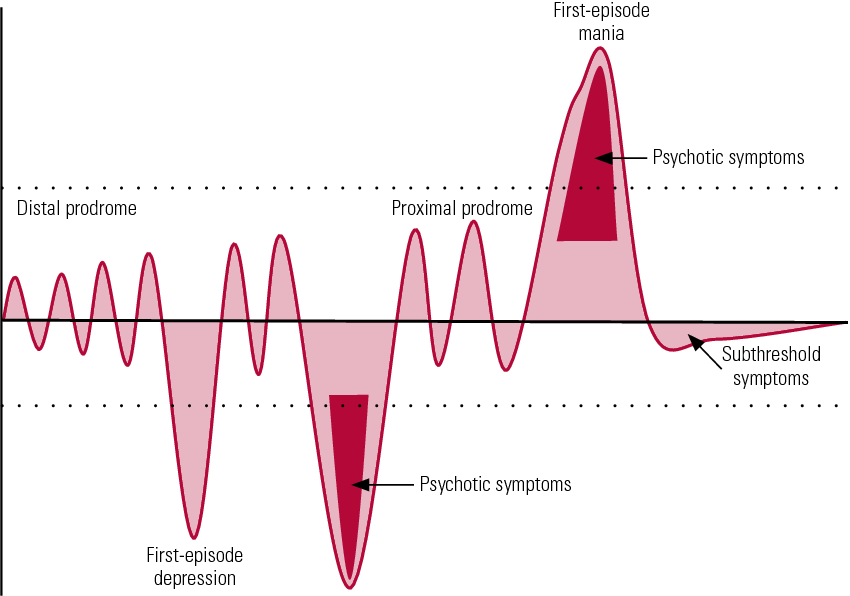
Schizoaffective disorder is an illness that includes symptoms of schizophrenia as well as abnormal moods (elevated and/or depressed mood).
Mood symptoms include:
- Depressed mood – feeling sad, empty, or tearful
- Feeling worthless, guilty, hopeless, or helpless
- Loss of interest or pleasure in normal activities
- Sleep and eat more or less than usual (for most people it is less)
- Low energy, trouble concentrating, or thoughts of death (suicidal thinking)
- Psychomotor agitation (‘nervous energy’)
- Psychomotor retardation (feeling like you are moving in slow motion)
- Feeling irritable or ‘high”
- Having increased self esteem
- Feeling like you don’t need to sleep
- Feeling the need to continue to talk
- Feeling like your thoughts are too quick (racing thoughts)
- Feeling distracted
- Getting involved in activities that are risky or could have bad consequences (e.
 g., excessive spending)
g., excessive spending)
Paliperidone may help some or all of these symptoms.
This medication sheet will focus primarily on schizophrenia. You can find more information about schizoaffective disorder here.
Paliperidone may also be helpful when prescribed “off-label” for manic or mixed episodes of bipolar disorder. “Off-label” means that it hasn’t been approved by the Food and Drug Administration for this condition. Your mental health provider should justify his or her thinking in recommending an “off-label” treatment. They should be clear about the limits of the research around that medication and if there are any other options.
What Is The Most Important Information I Should Know About Paliperidone?
Schizophrenia requires long-term treatment. Do not stop taking paliperidone, even when you feel better.
With input from you, your health care provider will assess how long you will need to take the medication.
Missing doses of paliperidone may increase your risk for a relapse in your symptoms.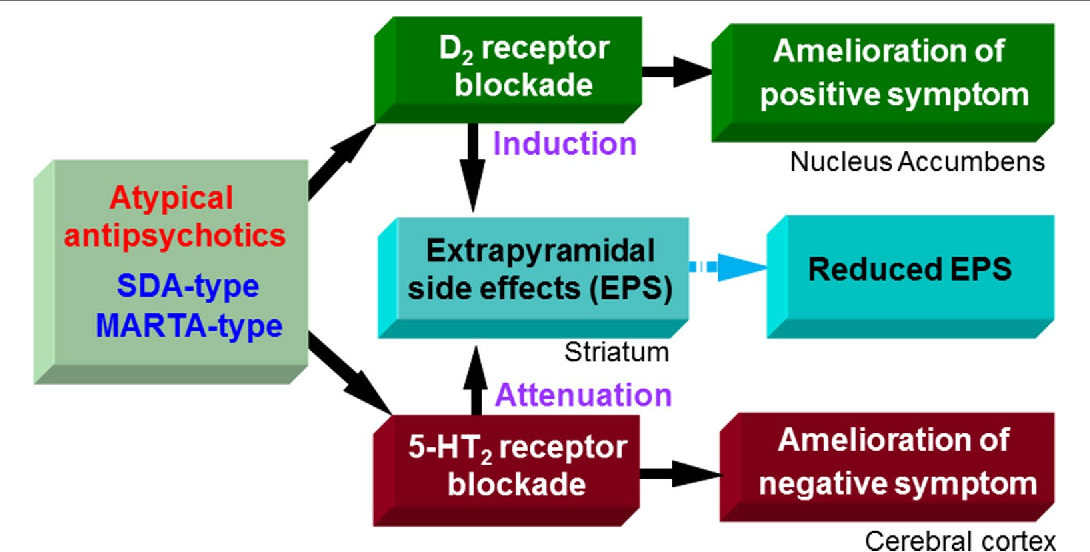
Do not stop taking paliperidone or change your dose without talking with your health care provider first.
For paliperidone to work properly, it should be taken every day as ordered by your health care provider.
Are There Specific Concerns About Paliperidone And Pregnancy?
If you are planning on becoming pregnant, notify your health care provider to best manage your medications. People living with schizophrenia who wish to become pregnant face important decisions. This is a complex decision since untreated schizophrenia has risks to the fetus, as well as the mother. It is important to discuss the risks and benefits of treatment with your doctor and caregivers.
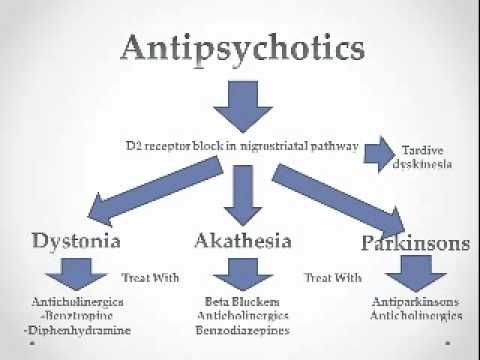
Antipsychotic use during the third trimester of pregnancy has a risk for abnormal muscle movements (extrapyramidal symptoms [EPS]) and/or withdrawal symptoms in newborns following delivery. Symptoms in the newborn may include agitation, feeding disorder, hypertonia, hypotonia, respiratory distress, somnolence, and tremor; these effects may be self-limiting or require hospitalization.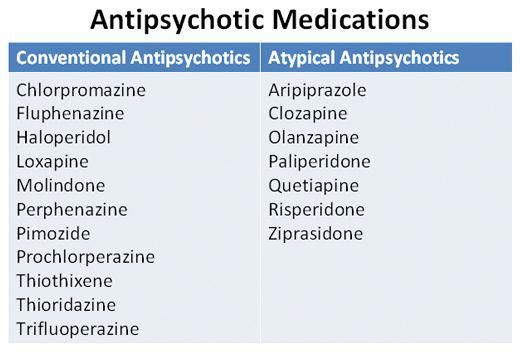
Caution is advised with breastfeeding since paliperidone does pass into breast milk.
What Should I Discuss With My Healthcare Provider Before Taking Paliperidone?
- Symptoms of your condition that bother you the most
- If you have thoughts of suicide or harming yourself
- Medications you have taken in the past for your condition, whether they were effective or caused any adverse effects
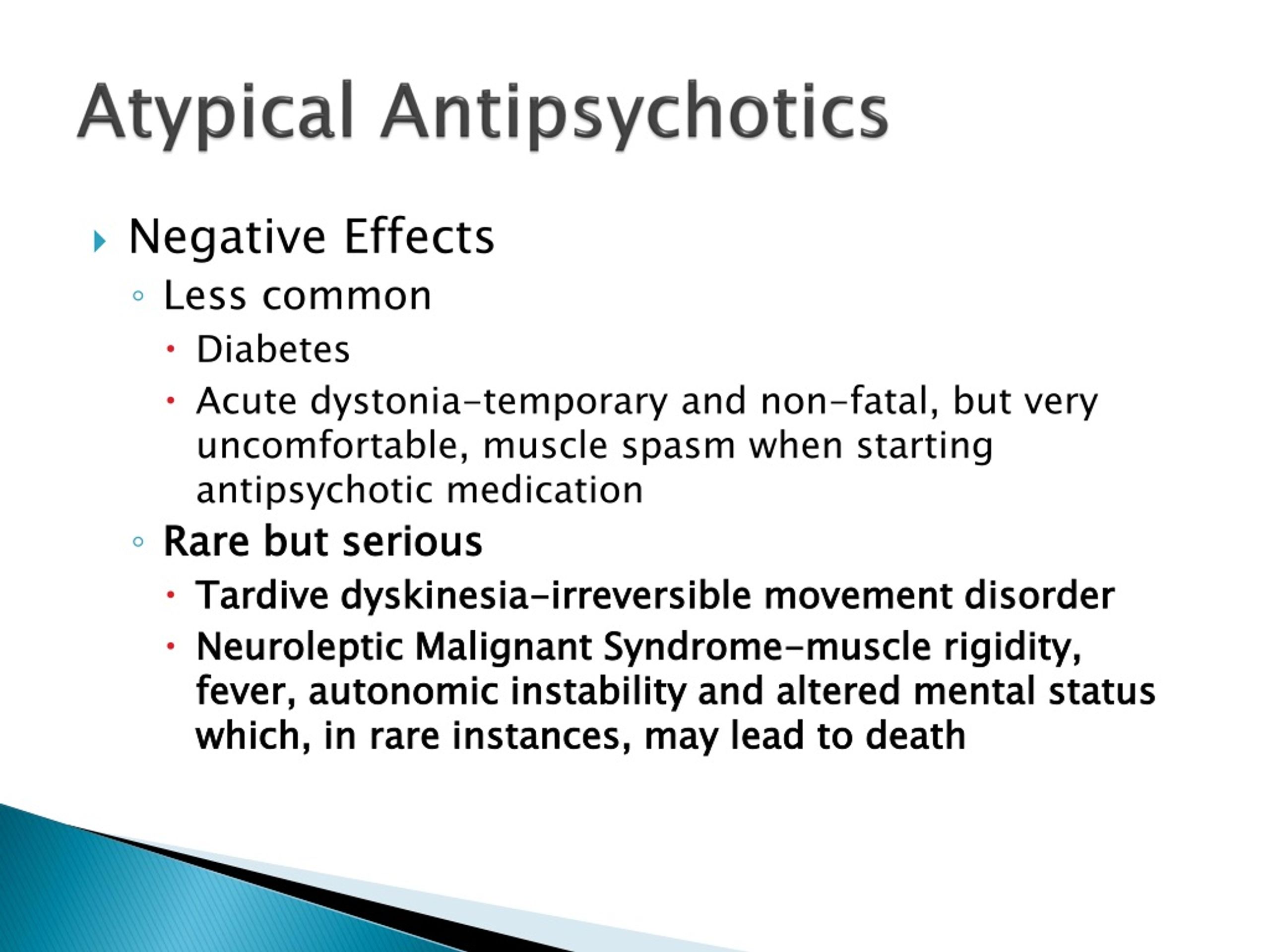
- If you ever had muscle stiffness, shaking, tardive dyskinesia, neuroleptic malignant syndrome, or weight gain caused by a medication
- If you experience side effects from your medications, discuss them with your provider. Some side effects may pass with time, but others may require changes in the medication.
- Any psychiatric or medical problems you have, such as heart rhythm problems, long QT syndrome, heart attacks, diabetes, high cholesterol, or seizures
- If you have a family history of diabetes or heart disease
- All other medications you are currently taking (including over the counter products, herbal and nutritional supplements) and any medication allergies you have
- Other non-medication treatment you are receiving, such as talk therapy or substance abuse treatment.
 Your provider can explain how these different treatments work with the medication.
Your provider can explain how these different treatments work with the medication. - If you are pregnant, plan to become pregnant, or are breastfeeding
- If you smoke, drink alcohol, or use illegal drugs
How Should I Take Paliperidone?
Paliperidone tablets are usually taken 1 time per day with or without food.
Typically patients begin at a low dose of medication and the dose is increased slowly over several weeks.
The dose of the tablets usually ranges from 3 mg to 12 mg. The dose of the Sustenna brand of long-acting paliperidone injection formulation usually ranges from 78 mg to 234 mg every month. The dose of the Trinza brand long-acting paliperidone injection formulation ranges from 273mg to 819mg every 3 months. Only your health care provider can determine the correct dose for you.
The tablets should be swallowed whole. They should not be chewed, crushed, or broken.
Use a calendar, pillbox, alarm clock, or cell phone alert to help you remember to take your medication.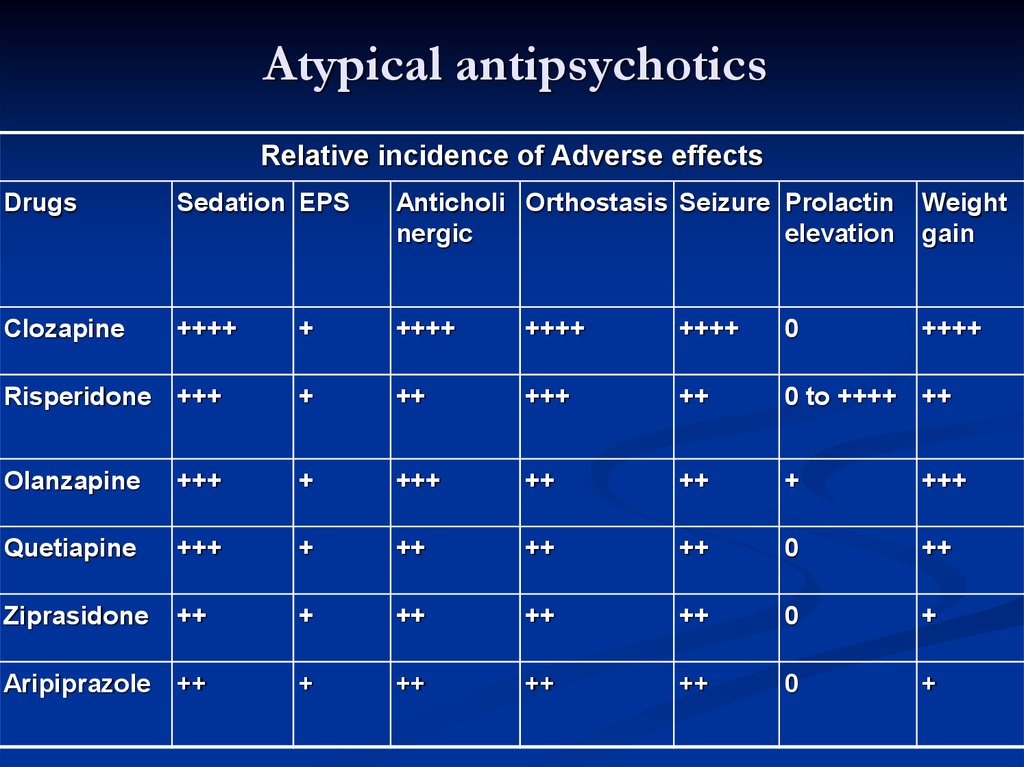 You may also ask a family member or friend to remind you or check in with you to be sure you are taking your medication.
You may also ask a family member or friend to remind you or check in with you to be sure you are taking your medication.
The Sustenna brand of long-acting injection paliperidone is administered twice in the first 8 days of treatment, then every 4 weeks. Your health care provider will administer these injections.
The Trinza brand of long-acting injection paliperidone is administered every 3 months. Your health care provider will administer these injections.
The Hafyera brand of long-acting injection paliperidone is administered every 6 months. Your health care provider will administer these injections.
What Happens If I Miss A Dose Of Paliperidone?
If you miss a dose of paliperidone, take it as soon as you remember, unless it is closer to the time of your next dose. Do not double your next dose or take more than what is prescribed. If you miss an injection, call your doctor or pharmacist right away. Discuss this with your healthcare provider.
What Should I Avoid While Taking Paliperidone?
Avoid drinking alcohol or using illegal drugs while you are taking paliperidone.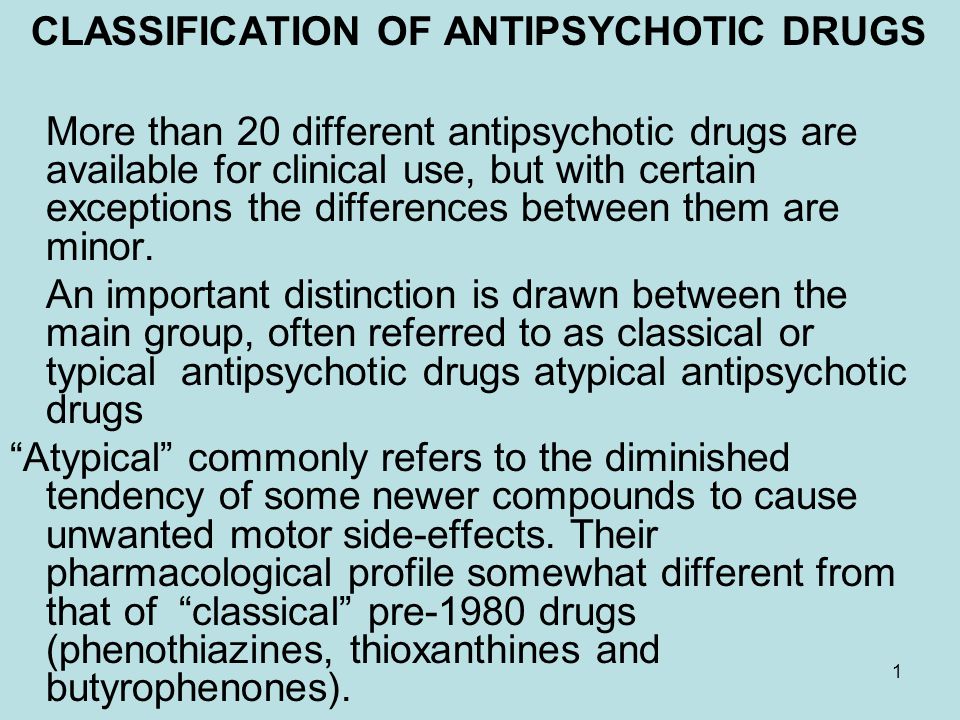 They may decrease the benefits (e.g., worsen your confusion) and increase adverse effects (e.g., sedation) of the medication.
They may decrease the benefits (e.g., worsen your confusion) and increase adverse effects (e.g., sedation) of the medication.
What Happens If I Overdose With Paliperidone?
If an overdose occurs call your doctor or 911. You may need urgent medical care. You may also contact the poison control center at 1-800-222-1222.
A specific treatment to reverse the effects of paliperidone does not exist.
What Are Possible Side Effects Of Paliperidone?
Common side effects
Rapid heartbeat, drowsiness, extrapyramidal symptoms, restlessness, headache, increased prolactin, weight gain, cholesterol abnormalities, increased glucose, vomiting, tremor, anxiety
Injections may cause localized reactions such as redness or swelling at the site of injection
Rare/serious side effects
Paliperidone may increase the blood levels of a hormone called prolactin. Side effects of increased prolactin levels include females losing their period, production of breast milk and males losing their sex drive or possibly experiencing erectile problems.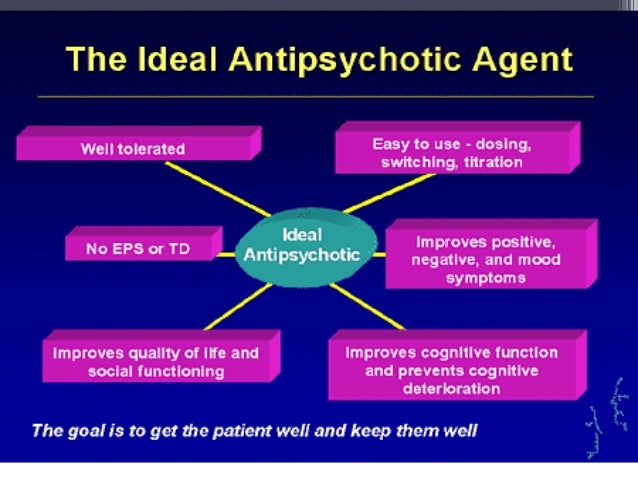 Long term (months or years) elevated prolactin levels can lead to osteoporosis, or increased risk of bone fractures.
Long term (months or years) elevated prolactin levels can lead to osteoporosis, or increased risk of bone fractures.
Some people may develop muscle related side effects while taking paliperidone. The technical terms for these are “extrapyramidal symptoms” (EPS) and “tardive dyskinesia” (TD). Symptoms of EPS include restlessness, tremor, and stiffness. TD symptoms include slow or jerky movements that one cannot control, often starting in the mouth with tongue rolling or chewing movements.
Temperature regulation: Impaired core body temperature regulation may occur; caution with strenuous exercise, heat exposure, and dehydration.
Second generation antipsychotics (SGAs) increase the risk of weight gain, high blood sugar, and high cholesterol. This is also known as metabolic syndrome. Your health care provider may ask you for a blood sample to check your cholesterol, blood sugar, and hemoglobin A1c (a measure of blood sugar over time) while you take this medication.
- Information on healthy eating and adding exercise to decrease your chances of developing metabolic syndrome may be found at the following sites:
- http://www.
 helpguide.org/articles/healthy-eating/healthy-eating.htm
helpguide.org/articles/healthy-eating/healthy-eating.htm - http://www.helpguide.org/home-pages/exercise-fitness.htm
- http://www.
SGAs have been linked with higher risk of death, strokes, and transient ischemic attacks (TIAs) in elderly people with behavior problems due to dementia.
All antipsychotics have been associated with the risk of sudden cardiac death due to an arrhythmia (irregular heart beat). To minimize this risk, antipsychotic medications should be used in the smallest effective dose when the benefits outweigh the risks. Your doctor may order an EKG to monitor for irregular heartbeat.
Neuroleptic malignant syndrome is a rare, life threatening adverse effect of antipsychotics which occurs in <1% of patients. Symptoms include confusion, fever, extreme muscle stiffness, and sweating. If any of these symptoms occur, contact your health care provider immediately.
All antipsychotics can cause sedation, dizziness, or orthostatic hypotension (a drop in blood pressure when standing up from sitting or lying down).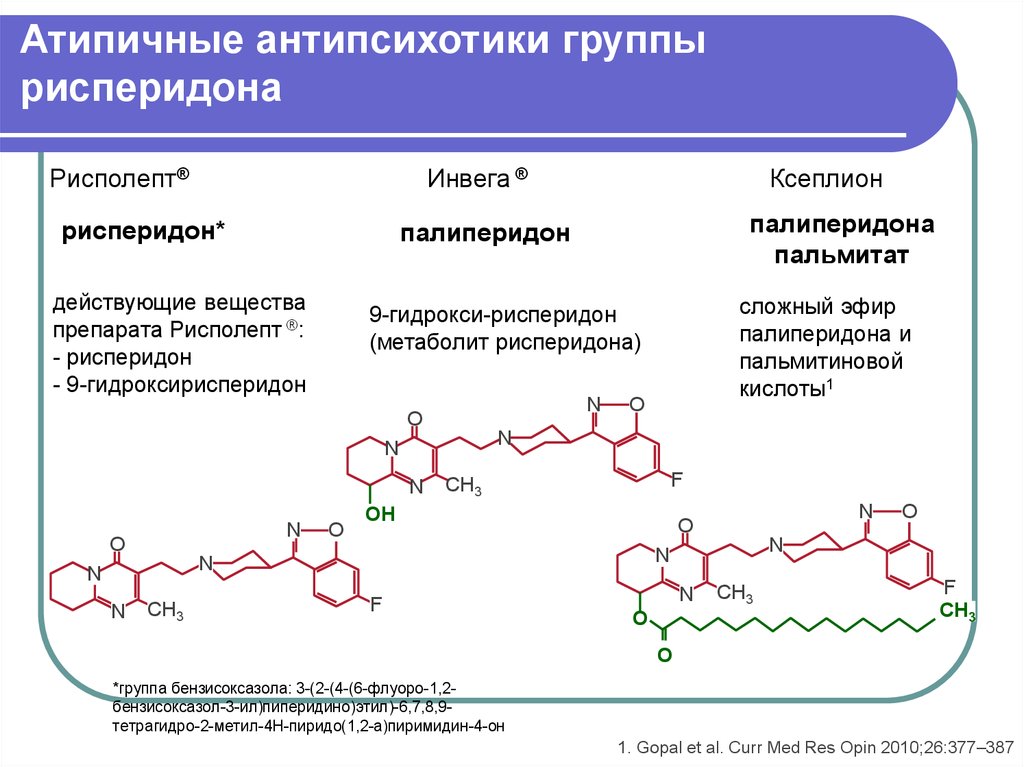 These side effects may lead to falls which could cause bone fractures or other injuries. This risk is higher for people with conditions or other medications that could worsen these effects. If falls or any of these symptoms occur, contact your health care provider.
These side effects may lead to falls which could cause bone fractures or other injuries. This risk is higher for people with conditions or other medications that could worsen these effects. If falls or any of these symptoms occur, contact your health care provider.
Are There Any Risks For Taking Paliperidone For Long Periods Of Time?
Tardive dyskinesia (TD) is a side effect that develops with prolonged use of antipsychotics. Medications such as paliperidone have been shown to have a lower risk of TD compared to older antipsychotics, such as Haldol® (haloperidol). If you develop symptoms of TD, such as grimacing, sucking, and smacking of lips, or other movements that you cannot control, contact your health care provider immediately. All patients taking either first or second generation antipsychotics should have an Abnormal Involuntary Movement Scale (AIMS) completed regularly by their health care provider to monitor for TD.
Second generation antipsychotics (SGAs) increase the risk of diabetes, weight gain, high cholesterol, and high triglycerides. (See “Serious Side Effects” section for monitoring recommendations).
(See “Serious Side Effects” section for monitoring recommendations).
What Other Medications May Interact With Paliperidone?
Paliperidone may block the effects of agents used to treat Parkinson’s disease such as levodopa (Sinemet®), bromocriptine, pramipexole (Mirapex®), ropinirole (Requip®), and others.
Paliperidone may lower your blood pressure. Medications used to lower blood pressure may increase this effect and increase your risk of falling. Propranolol (Inderal®) is an example of this type of medication.
The following medications may increase the risk of heart problems when used with paliperidone.
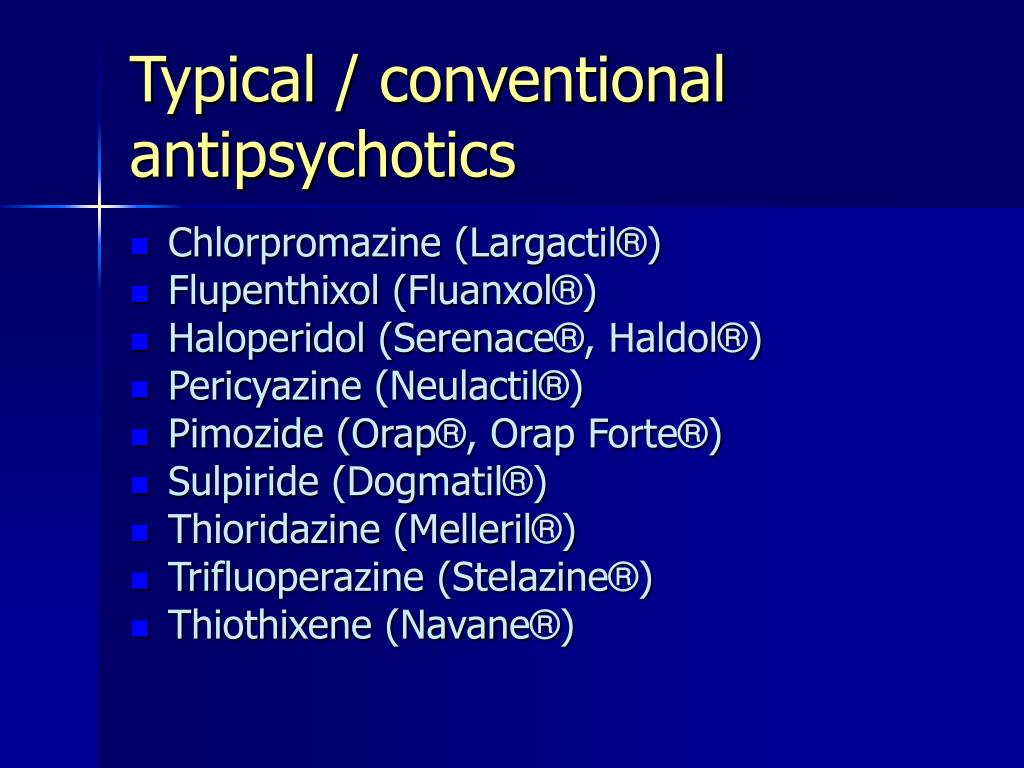
- Antipsychotics including chlorpromazine (Thorazine®), thioridizine (Mellaril®), iloperidone (Fanapt®), asenapine (Saphris®), quetiapine (Seroquel®), and ziprasidone (Geodon®).
- Antiarrhymics (heart rhythm medications), including procainamide, quinidine, amiodarone (Cordarone®), dronedarone (Multaq®), and sotalol (Betapace®).
The following medications may increase the levels and effects of paliperidone: divalproex sodium (Depakote®).
The following medications may decrease the levels and effects of paliperidone: carbamazepine (Tegretol®, Equatro®), rifampin, St. John’s Wort.
How Long Does It Take For Paliperidone To Work?
It is very important to tell your doctor how you feel things are going during the first few weeks after you start taking paliperidone. It will probably take several weeks to see big enough changes in your symptoms to decide if paliperidone is the right medication for you.
Antipsychotic treatment is generally needed lifelong for persons with schizophrenia. Your doctor can best discuss the duration of treatment you need based on your symptoms and illness.
- Hallucinations, disorganized thinking, and delusions may improve in the first 1-2 weeks
- Sometimes these symptoms do not completely go away
- Motivation and desire to be around other people can take at least 1-2 weeks to improve
- Symptoms continue to get better the longer you take paliperidone
- It may take 2-3 months before you get the full benefit of paliperidone
Summary of FDA Black Box Warnings
Increased mortality in elderly patients with dementia related psychosis
- Both first generation (typical) and second generation (atypical) antipsychotics are associated with an increased risk of mortality in elderly patients when used for dementia related psychosis.
- Although there were multiple causes of death in studies, most deaths appeared to be due to cardiovascular causes (e.g., sudden cardiac death) or infection (e.g., pneumonia).
- Antipsychotics are not indicated for the treatment of dementia related psychosis.
Provided by
(November 2022)
©2022 The College of Psychiatric and Neurologic Pharmacists (CPNP) and the National Alliance on Mental Illness (NAMI). CPNP and NAMI make this document available under the Creative Commons Attribution-No Derivatives 4.0 International License. Last Updated: January 2016.
This information is being provided as a community outreach effort of the College of Psychiatric and Neurologic Pharmacists. This information is for educational and informational purposes only and is not medical advice. This information contains a summary of important points and is not an exhaustive review of information about the medication. Always seek the advice of a physician or other qualified medical professional with any questions you may have regarding medications or medical conditions. Never delay seeking professional medical advice or disregard medical professional advice as a result of any information provided herein. The College of Psychiatric and Neurologic Pharmacists disclaims any and all liability alleged as a result of the information provided herein.
Always seek the advice of a physician or other qualified medical professional with any questions you may have regarding medications or medical conditions. Never delay seeking professional medical advice or disregard medical professional advice as a result of any information provided herein. The College of Psychiatric and Neurologic Pharmacists disclaims any and all liability alleged as a result of the information provided herein.
What You Need to Know About Invega (paliperidone)
What is Invega?
Invega is a medication known as a second generation (atypical) antipsychotic that is used to treat symptoms of schizophrenia and schizoaffective disorder.
When did the U.S. Food and Drug Administration (FDA) approve the medication?
Invega was first approved by the FDA in 2006.
Is there a generic version of Invega?
Yes, paliperidone is the generic version of Invega and is available in the United States.
Are there any major differences between Invega and other antipsychotics used to treat Invega?
Invega belongs to the class of medications known as atypical antipsychotics, or second generation antipsychotics.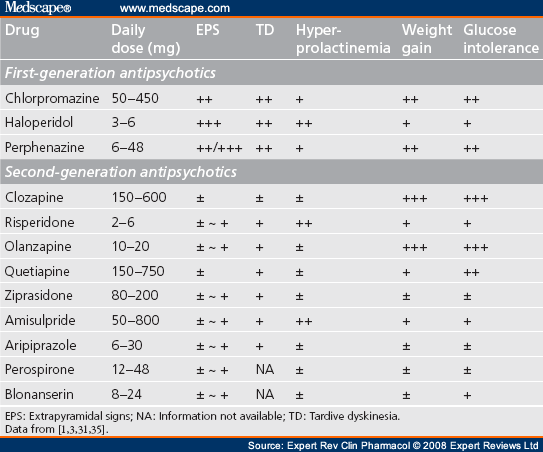 Talk to your doctor about what might work best for you and the costs and benefits of taking the medication. Some people may need to try several different antipsychotics before they find the most effective treatment with the fewest side effects.
Talk to your doctor about what might work best for you and the costs and benefits of taking the medication. Some people may need to try several different antipsychotics before they find the most effective treatment with the fewest side effects.
Can children take Invega?
In general, there are limited data for young children but the efficacy of Invega for treating children 12 and older has been established. However, children and adolescents taking atypical antipsychotics can be at higher risk for side effects such as weight gain. Talk to your child’s doctor about the risks of using the medication.
Are there potential interaction issues for people taking Invega and any other drugs?
There are hundreds of other drugs which are known to interact with Invega in major, moderate, or mild ways, so let your doctor know what other medications you are taking before you begin taking the medication. Some of these include antidepressants, antibiotics, other antipsychotics, cisapride, carbidopa/levodopa, anxiety medications, blood pressure medications, heart medications including procainamide, quinidine, sotalol, sedatives, and sleep medications.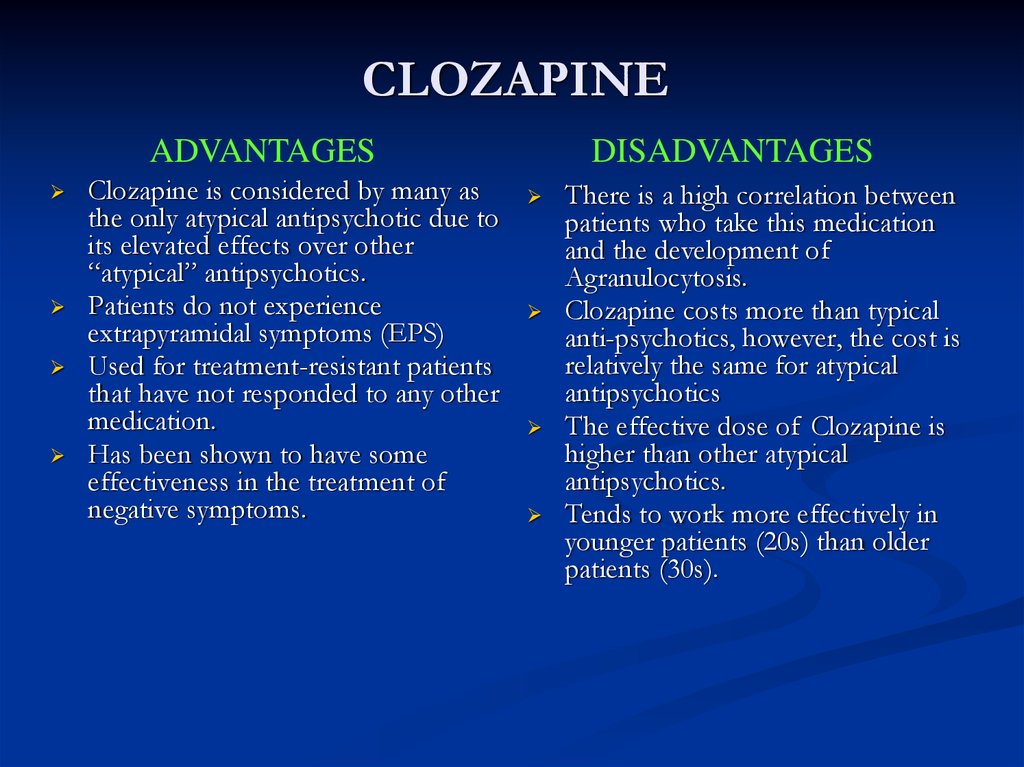 Also let your doctor know if you have an allergic reaction to Invega, Risperdal, or any other medications.
Also let your doctor know if you have an allergic reaction to Invega, Risperdal, or any other medications.
Are there any other medical conditions that would make someone ineligible for Invega therapy?
Talk to your doctor about other medical conditions before you take Invega, such as dementia, heart issues, seizures, stroke, brain tumor, Parkinson’s disease, diabetes, breast cancer, stomach conditions, inflammatory bowel disease, kidney disease, or liver disease. Also, talk to your doctor if you have a history of substance abuse or any other mental health issues.
What is the typical starting dose that would be prescribed to someone taking Invega?
The recommended initial adult dosage for oral Invega Extended-Release tablets is 6 mg taken once daily in the morning. Some patients may benefit from a higher or lower dosage, but a dosage above 12 mg daily is not recommended.
What do I do if I miss a dose?
Take the dose of Invega when you remember, but skip the missed dose if it it’s almost time for your next dose.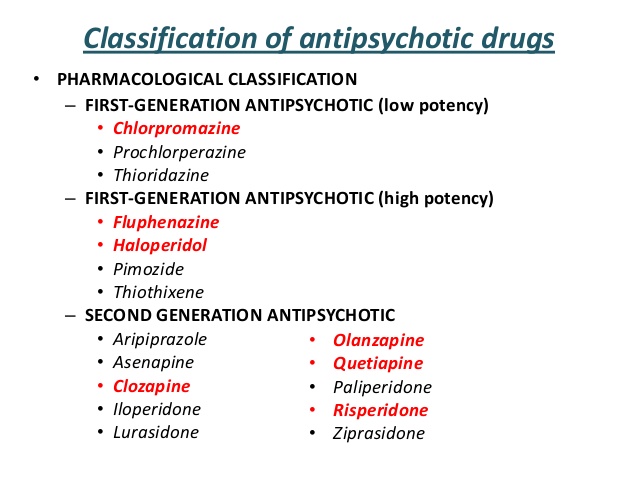 You should never take extra doses of the medication to make up for missed doses.
You should never take extra doses of the medication to make up for missed doses.
What common side effects can Invega cause?
Common side effects of Invega can include:
Doctors recommend that you not drink alcohol while on the medication. It also is recommended that you wait to drive or operate machinery until you know how the medication affects you. Report major side effects to your doctor immediately, which can include fever, sweating, confusion, irregular or fast heartbeat, muscle pain, restlessness, slow or stiff movements, uncontrollable movement of face or body, and painful erections that last for hours. You can also report side effects to the FDA at 1-800-FDA-1088 or online.
What are the potential long-term effects of taking Invega?
Your doctor should monitor for progression of potential long-term side effect of Invega, which can include tardive dyskinesia (abnormal muscle movement and jerks) and metabolic adverse effects such as weight gain, high blood sugar, and high cholesterol.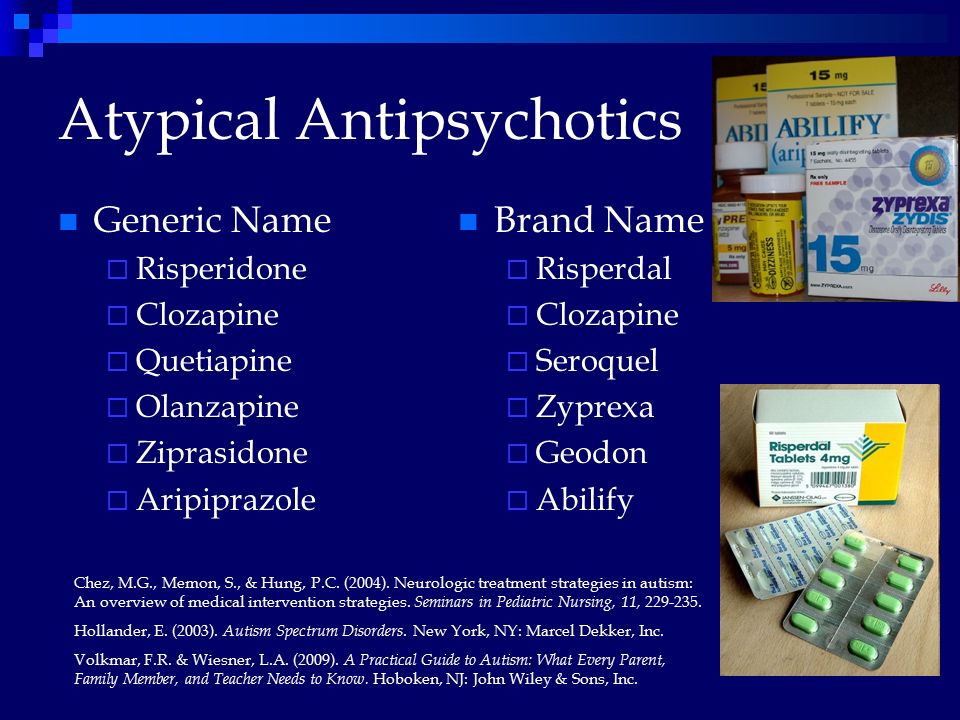
Is it safe for a woman who is pregnant, about to become pregnant, or nursing to take Invega?
There have been no controlled human pregnancy studies on the effects of Invega. The drug may be transferred via human breast milk and potentially harm a baby. Therefore, before taking Invega, talk to your doctor if you are pregnant, planning to become pregnant, or are nursing.
Can symptoms occur if Invega is discontinued?
It’s important not to stop taking the drug if you feel better. Maintain contact with your doctor and seek medical attention if necessary when discontinuing the drug. Talk to your doctor about how to mitigate potential withdrawal symptoms.
What should I do if I overdose on Invega?
Seek immediate help or call the Poison Help Line at 1-800-222-1222 if you overdose, as it can be fatal. Symptoms may include drowsiness, unsteadiness, restlessness, increased heartbeat, slow or stiff movement, and uncontrollable movement of face or body.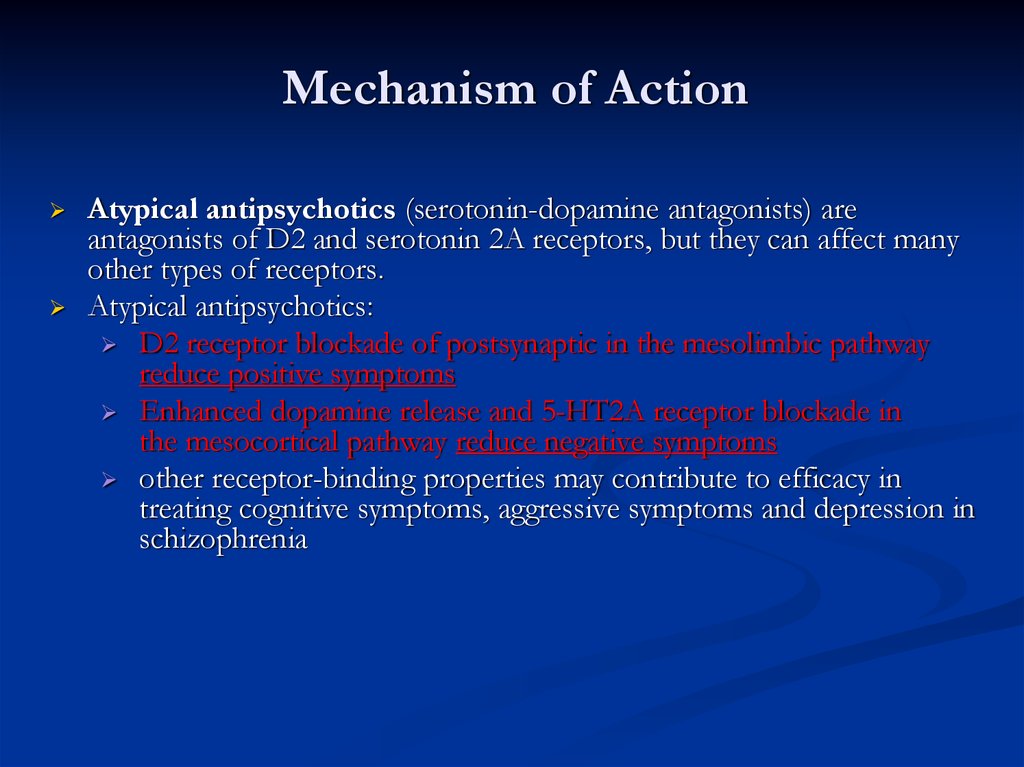
Is Invega habit-forming?
Invega has no habit-forming potential, but it is not recommended that you discontinue use of the drug before talking with your doctor, as withdrawal symptoms can occur.
How much does Invega cost?
According to goodrx.com, 30 tablets of 6 mg Invega cost approximately $1,000. Thirty tablets of 6 mg generic paliperidone cost approximately $800.
Are there any disadvantages to Invega?
The biggest disadvantages of Invega are the potential long-term side effects, which can include increased blood sugar, increased cholesterol, weight gain and, rarely, tardive dyskinesia.
DISCLAIMER: The information contained herein should NOT be used as a substitute for the advice of an appropriately qualified and licensed physician or other health care provider. This article mentions drugs that were FDA-approved and available at the time of publication and may not include all possible drug interactions or all FDA warnings or alerts.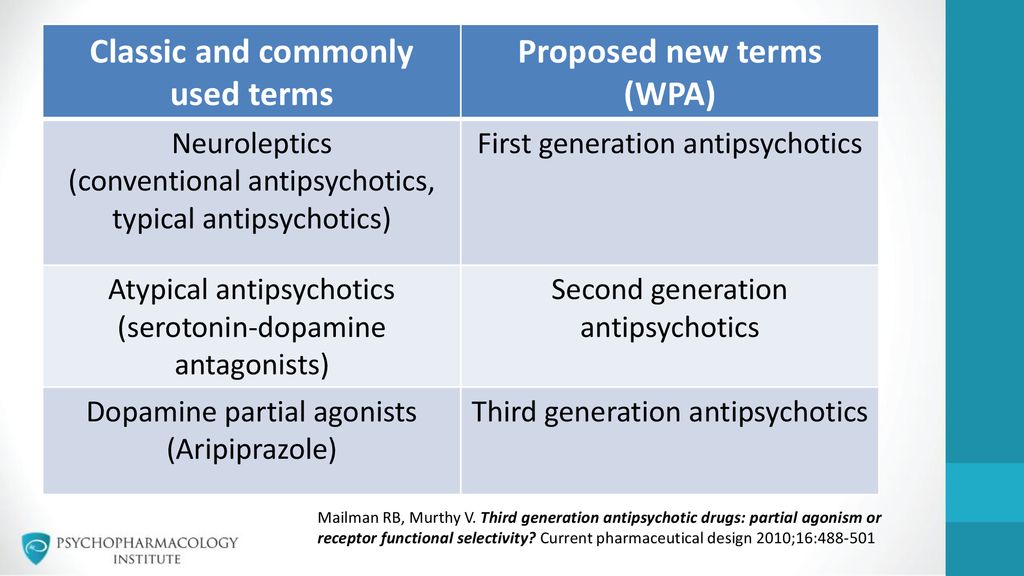 The author of this page explicitly does not endorse this drug or any specific treatment method. If you have health questions or concerns about interactions, please check with your physician or go to the FDA site for a comprehensive list of warnings.
The author of this page explicitly does not endorse this drug or any specific treatment method. If you have health questions or concerns about interactions, please check with your physician or go to the FDA site for a comprehensive list of warnings.
- FDA – Highlights of Prescribing Information - Invega
- U.S. National Library of Medicine - Paliperidone
- NAMI – Paliperidone
Notes: This article was originally published January 2, 2017 and most recently updated August 31, 2022.
Not Found (#404)
hide menu
Issues of the current year
-
7-8 (136)
-
5-6 (135)
-
3-4 (134)
-
2 (133)
-
1 (132)
7-8 (136)
Issue content 7-8 (136), 2022
- nine0009
War Wikis: help in crisis situations
-
Ethical and legal problems of mental health: Ukraine at the focus of international respect
Yu.
 A. Kramar
A. Kramar -
Screening, diagnosis and treatment of diabetic sensorimotor polyneuropathy: consensus recommendations
-
Influx of mass information on delinquent behavior
R. І. Isakov
-
Stopping programs for rukhovo's rehabilitation for the normalization of the psychoemotional sphere of patients with Parkinson's disease
N.P. Voloshin, I.V. Bogdanova, I.K. Voloshin-Gaponov, S.V. Fedosiev, L.P. Tereshchenko, T.V. Bogdanova
-
Trauma management algorithm
-
Type of neuropathic pain according to the International classification of orofacial pain
-
Management of patients with dementia: key provisions for diagnosis, examination and observation for example of life
-
Significant Pre-Raphaelism: John Ruskin and Effi Gray
5-6 (135)
3-4 (134)
2 (133)
1 (132)
Other projects of the Health of Ukraine publishing house
Specialization medical portal
nine0009 Child doctorMedical aspects of women's health
Clinical Immunology, Allergology, Infectology
Rational pharmacotherapy
nine0000 Second generation injectable antipsychotics in clinical practice Second generation injectable antipsychotics in clinical practice Website of the publishing house "Media Sfera"
contains materials intended exclusively for healthcare professionals.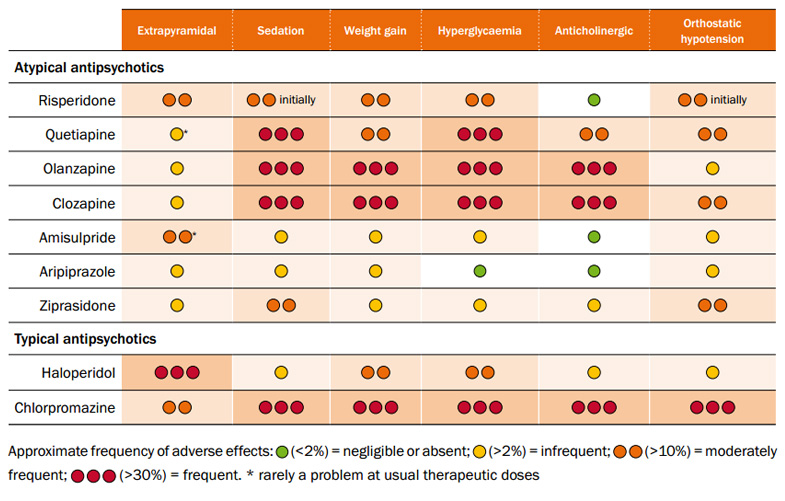 By closing this message, you confirm that you are a registered medical professional or student of a medical educational institution.
By closing this message, you confirm that you are a registered medical professional or student of a medical educational institution.
St. Petersburg State University
Grigoryeva E.V.
Moscow State University of Medicine and Dentistry named after A.I. A.I. Evdokimov” of the Ministry of Health of Russia
Injectable antipsychotics-prolongs of the second generation in clinical practice
Authors:
Petrova N.N., Grigoryeva E.V.
More about the authors
Magazine: Journal of Neurology and Psychiatry. S.S. Korsakov. 2022;122(2): 115-123 nine0004
DOI: 10.17116/jnevro2022122021115
How to quote:
Petrova N.N., Grigoryeva E.V. Injectable antipsychotics-prolongs of the second generation in clinical practice. Journal of Neurology and Psychiatry. S.S. Korsakov. 2022;122(2):115-123.
Petrova NN, Grigorieva EV. Second-generation long-acting injectable antipsychotics in clinical practice.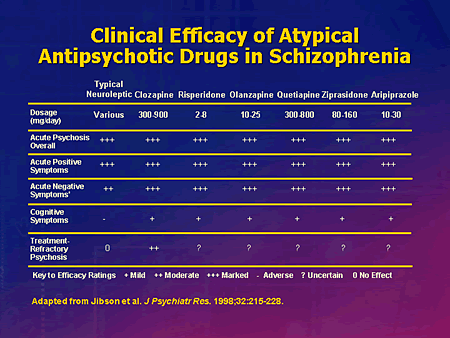 nine0145 Zhurnal Nevrologii i Psikhiatrii imeni S.S. Korsakova. 2022;122(2):115-123. (In Russ.).
nine0145 Zhurnal Nevrologii i Psikhiatrii imeni S.S. Korsakova. 2022;122(2):115-123. (In Russ.).
https://doi.org/10.17116/jnevro2022122021115
Close metadata
The article discusses 5 clinical cases of paranoid schizophrenia in patients at different stages of the development of the disease, shows the therapeutic tactics of using drugs from the group of injectable prolong antipsychotics of the second generation to solve problems that arise during anti-relapse therapy. The data of studies substantiating these approaches are presented. Various options for combination therapy are discussed, including at the stage of drug replacement and the appointment of a second-generation long-acting injectable antipsychotic. nine0004
Keywords:
schizophrenia
anti-relapse therapy
injectable antipsychotics prolongs of the second generation
clinical practice
Authors:
Petrova N.N.
St. Petersburg State University
Grigoryeva E.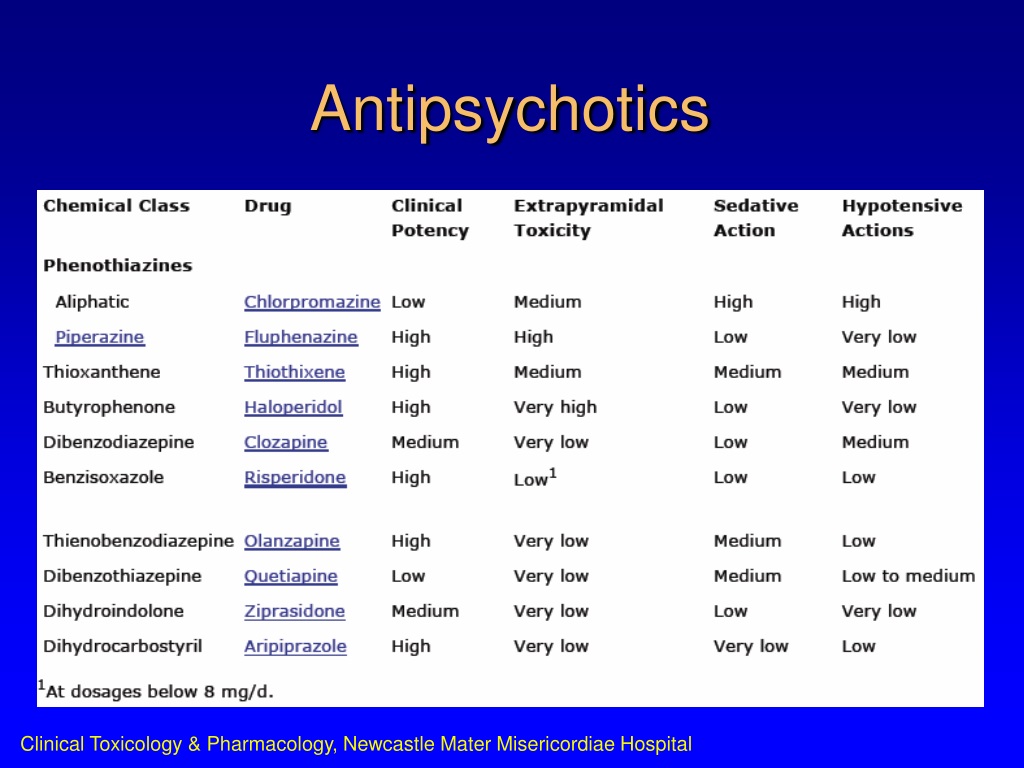 V.
V.
Moscow State University of Medicine and Dentistry named after A.I. A.I. Evdokimov" of the Ministry of Health of Russia
References:
- Mathews M, Gopal S, Singh A, et al. Comparison of Relapse Prevention with 3 Different Paliperidone Formulations in Patients with Schizophrenia Continuing versus Discontinuing Active Antipsychotic Treatment: A Post-Hoc Analysis of 3 Similarly Designed Randomized Studies. Neuropsychiatr Dis Treat. 2020;16:1533-1542. https://doi.org/10.2147/NDT.S221242
- Stahl SM. Stahl's Essential Psychopharmacology: Case studies. Vol. 2. Cambridge university press, 2015.
- Tiihonen J, Mittendorfer-Rutz E, Majak M, et al. Real-World Effectiveness of Antipsychotic Treatments in a Nationwide Cohort of 29,823 Patients with Schizophrenia. JAMA Psychiatry. 2017;74:686-693.
- Taipale H, Mittendorfer-Rutz E, Alexanderson K, et al. Antipsychotics and mortality in a nationwide cohort of 29,823 patients with schizophrenia. Schizophr Res.
 2018;197:274-280. Epub 2017 Dec 21. https://doi.org/10.1016/j.schres.2017.12.010
2018;197:274-280. Epub 2017 Dec 21. https://doi.org/10.1016/j.schres.2017.12.010 - Si T, Li N, Lu H, et al. Impact of paliperidone palmitate one-month formulation on relapse prevention in patients with schizophrenia: A post-hoc analysis of a one-year, open-label study stratified by medication adherence. Jof Psychopharmacology (Oxford, England). 2018;32(6):691-701. https://doi.org/10.1177/0269881118772449
- Brissos S, Veguilla MR, Taylor D, Balanza-Martinez V. The role of long-acting injectable antipsychotics in schizophrenia: a critical appraisal. Ther Adv Psychopharmacol. 2014;4(5):198-219.
- Correll CU, Citrome L, Haddad PM, et al. The use of long-acting injectable antipsychotics in schizophrenia: evaluating the evidence. JClin Psychiatry. 2016;77(suppl 3):1-24.
- Barnes TR, Shingleton-Smith A, Paton C. Antipsychotic long-acting injections: prescribing practice in the UK. Br J Psychiatry Suppl. 2009;52:37-42.
- Patel MX, Taylor M, David AS.
 Antipsychotic long-acting injections: mind the gap. Br J Psychiatry Suppl. 2009;52:1-4.
Antipsychotic long-acting injections: mind the gap. Br J Psychiatry Suppl. 2009;52:1-4. - Skodlar B, Tomori M, Parnas J. Subjective experience and suicidal ideation in schizophrenia. Compr Psychiatry. 2008;4:482-488.
- Barret EA, Mork E, Færden A, et al. The development of insight and its relationship with suicidality over one year follow-up in patients with first episode psychosis. Schizophr Res. 2015;162:97-102. nine0011
- Petrova N.N., Vishnevskaya O.A. Clinical features of depression in remission of paranoid schizophrenia. Journal of Neurology and Psychiatry. S.S. Korsakov. 2013;11:34-41.
- Siris SG. Suicide and schizophrenia. J Psychopharmacol. 2001;15(2):127-135. https://doi.org/10.1177/026988110101500209
- Ventriglio A, Gentile A, Bonfitto I, et al. Suicidal behavior in the debut of schizophrenia. Suicidology. 2017;8(2):20-28.
- Pompili M, Orsolini L, Lamis DA, et al. Suicide Prevention in Schizophrenia: Do Long-Acting Injectable Antipsychotics (LAIs) have a Role? CNS Neurol Disord Drug Targets.
 2017;16(4):454-462. https://doi.org/10.2174/1871527316666170223163629
2017;16(4):454-462. https://doi.org/10.2174/1871527316666170223163629 - Tiihonen J, Walhbeck K, Lonnqvist J., et al. Effectiveness of antipsychotic treatments in a nationwide cohort of patients in community care after fi rst hospitalization due to schizophrenia and schizoaffective disorder: observational follow-up study. Br Med J. 2006;333:224-229.
- Johnson DA, Pasterski G, Ludlow JM, et al. The discontinuance of maintenance neuroleptic therapy in chronic schizophrenic patients: drug and social consequences. Acta Psychiatr Scand. 1983;67:339-352.
- Möller HJ, Llorca PM, Sacchetti E, et al. Efficacy and safety of direct transition to risperidone long-acting injectable in patients treated with various antipsychotic therapies. International Clinical Psychopharmacology. 2005;20(3):121-130.
- Citrome L. Paliperidone palmitate: review of the efficacy, safety, and cost of a new second-generation depot antipsychotic medication. Int J Clin Pract. 2010;64:216-239.
- Martinuzzi E, Barbosa S, Daoudlarian D, et al. Stratification and prediction of remission in first-episode psychosis patients: the OPTiMiSE cohort study. Translational Psychiatry. 2019;9:20. https://doi.org/10.1038/s41398-018-0366-5
- Murmantsev K.V., Khasanova D.T. A modern view on the use of antipsychotic drugs in the practice of a hospital doctor. effective pharmacotherapy. Neurology and psychiatry. 2020;16(4):36-38. Murmantsev KV, Khasanova DT. A modern view on the use of antipsychotic drugs in the practice of a hospital doctor. effective pharmacotherapy. Neurology and psychiatry. 2020;16(4):36-38. (In Russ.).
- Karson C, Duffy RA, Eramo A. Long-term outcomes of antipsychotic treatment in patients with first-episode schizophrenia: a systematic review. Neuropsychiatr Dis Treat. 2016;12:57-67. eCollection 2016. https://doi.org/10.2147/NDT.S96392
- Chhumakov EM, Petrova NN, Limankin OV. Characteristics of the response to treatment in outpatients with the first episode of schizophrenia spectrum disorders.
 Vestnik of Saint Petersburg University. medicine. 2019;14:3:216-225.
Vestnik of Saint Petersburg University. medicine. 2019;14:3:216-225. - Petrova N.N., Tsyrenova K.A. Assessment of adherence to antipsychotic therapy in patients with the first episode of schizophrenia. Modern therapy of mental disorders. 2019;3:12-17. https://doi.org/10.21265/PSYPH.2019.49.35972
- Caseiro O, Pérez-Iglesias R, Mata I, et al. Predicting relapse after a first episode of non-affective psychosis: a three-year follow-up study. J Psychiatr Res. 2012;46(8):1099-1105.
- Emsley R, Chiliza B, Asmal L, et al. Long-acting injectable antipsychotics in early psychosis: a literature review. Early Interv. Psychiatry. 2013;7(3):247-254.
- Emsley R, Hargarter L, Bergmans P. Once-monthly paliperidone palmitate in early stage schizophrenia — a retrospective, non-interventional 1-year study of patients with newly diagnosed schizophrenia. Neuropsychiatr Dis Treat. 2017;13:2261-2269.
- Nasrallah HA, Gopal S, et al. A controlled, evidence-based trial of paliperidone palmitate, a long-acting injectable antipsychotic, in schizophrenia.
 Neuropsychopharmacol. 2010;35(10):2072-2082. nine0011
Neuropsychopharmacol. 2010;35(10):2072-2082. nine0011 - Patel C, Emond B, Lafeuille M-H, et al. Real-World Analysis of Switching Patients with Schizophrenia from Oral Risperidone or Oral Paliperidone to Once-Monthly Paliperidone Palmitate. Drugs Real World Outcomes. 2020;7(1):19-29. https://doi.org/10.1007/s40801-019-00172-9
- Llorca PM, Abbar M, Courtet P, et al. Guidelines for the use and management of long-acting injectable antipsychotics in serious mental illness. BMC Psychiatry. 2013;13:340. https://doi.org/10.1186/1471-244X-13-340
- Marder SR, Conley R, Ereshefsky L, et al. Clinical guidelines: dosing and switching strategies for long-acting risperidone. JClin Psychiatry. 2003;64(suppl 16):41-46.
- Keith SJ, Kane JM, Turner M, et al. Academic highlights: guidelines for the use of long-acting injectable atypical antipsychotics. JClin Psychiatry. 2004;65(1):120-131.
- Correll CU, Rubio JM, Kane JM. What is the risk-benefit ratio of long-term antipsychotic treatment in people with schizophrenia? World Psychiatry.
 2018;17(2):149-160. https://doi.org/10.1002/wps.20516
2018;17(2):149-160. https://doi.org/10.1002/wps.20516 - Porcelli S, Bianchini O, De GG, et al. Clinical related factors to schizophrenia relapse. Int J Psychiatry Clin Pract. 2016;20(2):54-69.
- Hiemke C, Bergemann N, Clement HW, et al. Consensus guidelines for therapeutic drug monitoring in neuropsychopharmacology: update 2017. Pharmacopsychiatry. 2018;51(1-02):9-62. Epub 2017 Sep 14. https://doi.org/10.1055/s-0043-116492
- Citrome L. New second-generation long-acting injectable antipsychotics for the treatment of schizophrenia. Expert Rev Neurother. 2013;13(7):767-783. nine0011
- Janssen Pharmaceuticals Inc. Invega Trinza (paliperidone palmitate) extended-release injectable suspension, for intramuscular use. Titusville, NJ: Janssen Pharmaceuticals Inc.; March 2018.
- Janssen Pharmaceuticals Inc. Invega Sustenna (paliperidone palmitate) extended-release injectable suspension, for intramuscular use. Titusville, NJ: Janssen Pharmaceuticals Inc.; March 2018.
- Correll CU, Rubio JM, Inczedy-Farkas G, et al. Efficacy of 42 pharmacological cotreatment strategies added to antipsychotic monotherapy in schizophrenia: systematic overview and quality appraisal of the meta-analytic evidence. JAMA Psychiatry. 2017;74(7):675-684. nine0011
- Galling B, Roldan A, Hagi K, et al. Antipsychotic augmentation vs. monotherapy in schizophrenia: systematic review, metaanalysis and meta-regression analysis. World Psychiatry. 2017;16(1):77-89.
- Correll CU, Sliwa JK, Najarian DM, Saklad SR. Practical considerations for managing breakthrough psychosis and symptomatic worsening in patients with schizophrenia on long-acting injectable antipsychotics. CNS Spectr. 2019;24(4):354-370. https://doi.org/10.1017/S1092852918001098
- Morris MT, Tarpada SP. Long-Acting Injectable Paliperidone Palmitate: A Review of Efficacy and Safety. Psychopharmacol Bull. 2017;47(2):42-52. PMCID: PMC5472171.
- Berwaerts J, Liu Y, Gopal S, et al. Efficacy and safety of the 3-month formulation of paliperidone palmitate vs placebo for relapse prevention of schizophrenia: a randomized clinical trial.
Learn more