Average length of manic episode
What Is It, Causes, Triggers, Symptoms & Treatment
Overview
What is mania?
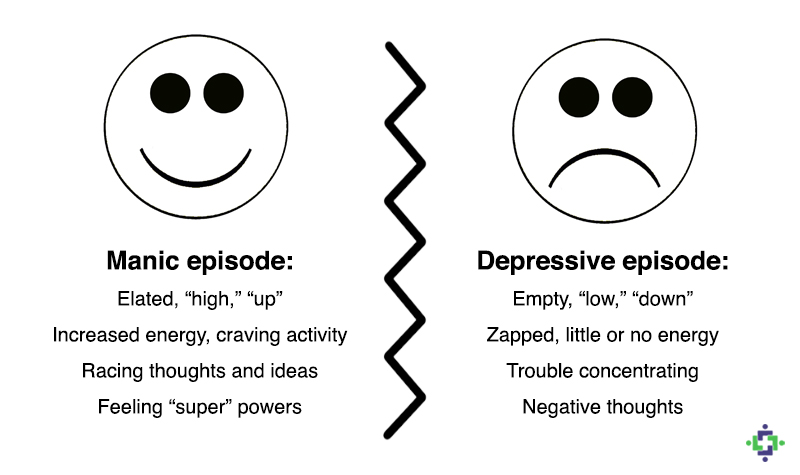
Mania is a condition in which you have a period of abnormally elevated, extreme changes in your mood or emotions, energy level or activity level. This highly energized level of physical and mental activity and behavior must be a change from your usual self and be noticeable by others.
What's considered an “abnormal,” extreme change in behavior and what does it look like?
Abnormal manic behavior is behavior that stands out. It’s over-the-top behavior that other people can notice. The behavior could reflect an extreme level of happiness or irritation. For example, you could be extremely excited about an idea for a new healthy snack bar. You believe the snack could make you an instant millionaire but you’ve never cooked a single meal in your life, don’t know a thing about how to develop a business plan and have no money to start a business. Another example might be that you strongly disagree with a website “influencer” and not only write a 2,000 word post but do an exhaustive search to find all the websites connected to the influencer so you can post your letter there too.
Although these examples may sound like they could be normal behavior, a person with mania will expend a great deal of time and energy including many sleepless nights working on projects such as these.
What is a manic episode?
A manic episode is a period of time in which you experience one or more symptoms of mania and meet the criteria for manic episode (see “symptoms” and “diagnosis” sections). In some cases, you may need to be hospitalized.
Can I have a manic episode as its own condition or is it always part of another mental health condition?
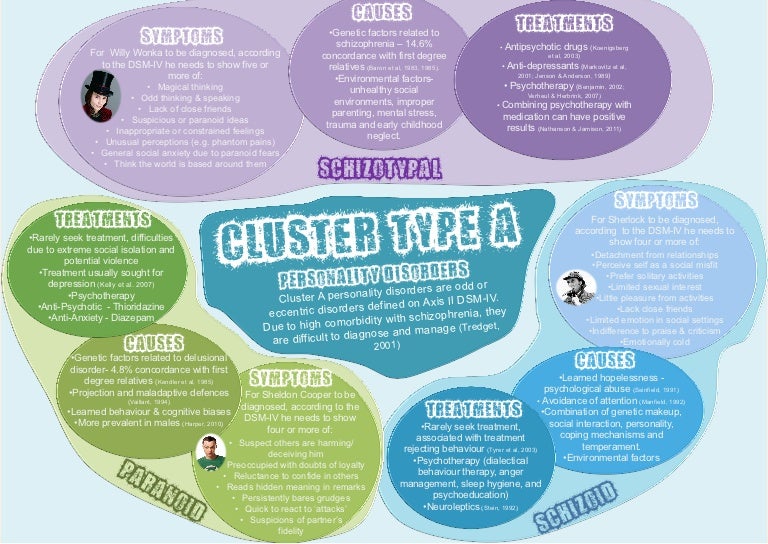
Technically if you have a manic episode, you have a mental health condition. Mania can be a part of several mental health conditions including:
- Bipolar I disorder (most common condition for mania to occur).
- Seasonal affective disorder.
- Postpartum psychosis.
- Schizoaffective disorder.
- Cyclothymia.
What is bipolar I disorder?
Bipolar I disorder is a mental health illness in which a person has major high and low swings in mood, activity, energy and ability to think clearly. To be diagnosed with bipolar I disorder, you have to have at least one episode of mania that lasts for at least seven days or have an episode that is so severe that it requires hospitalization.
To be diagnosed with bipolar I disorder, you have to have at least one episode of mania that lasts for at least seven days or have an episode that is so severe that it requires hospitalization.
Most people have both episodes of both mania and depression, but you don’t have to have depression to be diagnosed with mania. Many people with a bipolar I disorder diagnosis have recurring, back-to-back manic episodes with very few episodes of depression.
What are the triggers of manic episodes?
Manic episode triggers are unique to each person. You’ll have to become a bit of a detective and monitor your mood (even keeping a “mood diary”) and start to track how you feel before an episode and when it occurs. Ask family and close friends who you trust and have close contact with to help identify your triggers. As outside observers, they may notice changes from your usual behavior more easily than you do.
Knowing your triggers can help you prepare for an episode, lessen the effect of an episode or prevent it from happening at all.
Common triggers to be aware of include:
- A highly stimulating situation or environment (for example, lots of noise, bright lights or large crowds).
- A major life change (such as divorce, marriage or job loss).
- Lack of sleep.
- Substance use, such as recreational drugs or alcohol.
What happens after a manic episode?
After a manic episode you may:
- Feel happy or embarrassed about your behavior.
- Feel overwhelmed by all the activities you’ve agreed to take on.
- Have only a few or unclear memories of what happened during your manic episode.
- Feel very tired and need sleep.
- Feel depressed (if your mania is part of bipolar disorder).
Symptoms and Causes
What are the symptoms of mania?
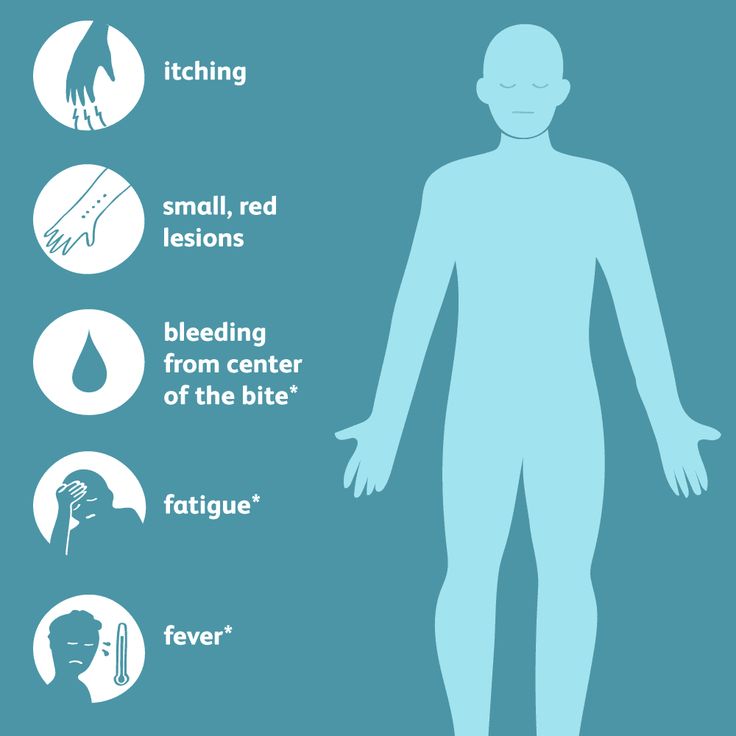
Symptoms of a manic episode
- Having an abnormally high level of activity or energy.
- Feeling extremely happy or excited — even euphoric.
- Not sleeping or only getting a few hours of sleep but still feeling rested.
- Having an inflated self-esteem, thinking you’re invincible.
- Being more talkative than usual. Talking so much and so fast that others can’t interrupt.
- Having racing thoughts — having lots of thoughts on lots of topics at the same time (called a “flight of ideas”).
- Being easily distracted by unimportant or unrelated things.
- Being obsessed with and completely absorbed in an activity.
- Displaying purposeless movements, such as pacing around your home or office or fidgeting when you’re sitting.
- Showing impulsive behavior that can lead to poor choices, such as buying sprees, reckless sex or foolish business investments.
Psychotic symptoms of a manic episode
- Delusions. Delusions are false beliefs or ideas that are incorrect interpretations of information. An example is a person thinking that everyone they see is following them.
- Hallucinations. Having a hallucination means you see, hear, taste, smell or feel things that aren’t really there.
 An example is a person hearing the voice of someone and talking to them when they’re not really there.
An example is a person hearing the voice of someone and talking to them when they’re not really there.
How long does a manic episode last?
Early signs (called “prodromal symptoms”) that you’re getting ready to have a manic episode can last weeks to months. If you’re not already receiving treatment, episodes of bipolar-related mania can last between three and six months. With effective treatment, a manic episode usually improves within about three months.
What causes mania?
Scientists aren’t completely sure what causes mania. However, there are several factors that are thought to contribute. Causes differ from person to person.
Causes may include:
- Family history. If you have a family member with bipolar illness, you have an increased chance of developing mania. This isn't definite though. You may never develop mania even if other family members have.
- A chemical imbalance in the brain.
- A side effect of a medication (such as some antidepressants), alcohol or recreational drugs.
- A significant change in your life, such as a divorce, house move or death of a loved one.
- Difficult life situations, such as trauma or abuse, or problems with housing, money or loneliness.
- A high level of stress and an inability to manage it.
- A lack of sleep or changes in sleep pattern.
- As a side effect of mental health problems including seasonal affective disorder, postpartum psychosis, schizoaffective disorder or other physical or neurologic condition such as brain injury, brain tumors, stroke, dementia, lupus or encephalitis.
Diagnosis and Tests
How is mania diagnosed?
Your healthcare provider will ask about your medical history, family medical history, current prescriptions and non-prescription medications and any herbal products or supplements you take. Your provider may order blood tests and body scans to rule out other conditions that may mimic mania. One such condition is hyperthyroidism. If other diseases and conditions are ruled out, your provider may refer you to a mental health specialist
To be diagnosed with mania, your mental health specialist may follow the criteria of the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders, DSM-5. Their criteria for manic episode is:
Their criteria for manic episode is:
- You have an abnormal, long-lasting elevated expression of emotion along with a high degree of energy and activity that lasts for at least one week and is present most of the day, nearly every day.
- You have three or more symptoms to a degree that they’re a noticeable change from your usual behavior (four symptoms if mood is only irritable). (See the symptoms section of this article for a list of the symptoms used as criteria.)
- The mood disturbance is severe enough to cause significant harm to your social, work or school functioning or there’s a need to hospitalize you to prevent you from harming yourself or others, or you have psychotic features, such as hallucinations or delusions.
- The manic episode can’t be caused by the effects of a substance (medications or drug abuse) or another medical condition.
Management and Treatment
How is mania treated?
Mania is treated with medications, talk therapy, self-management and family and friends support.
Medications
If you have mania only, your healthcare provider may prescribe an antipsychotic medication, such as ariprazole (Abilify®), lurasidone (Latuda®), olanzapine (Zyprexa®), quetiapine (Seroquel®) or risperridone (Risperdal®).
If you have mania as part of a mood disorder, your provider may add a mood stabilizer. Some examples include lithium, valproate (Depakote®) and carbamazepine (Tegretol®). (If you’re pregnant or plan to become pregnant, let your provider know. Valproate can increase the chance of birth defects and learning disabilities and shouldn’t be prescribed to individuals who are able to become pregnant.)
Sometimes antidepressants are also prescribed.
Talk therapy (psychotherapy)
- Psychotherapy involves a variety of techniques. During psychotherapy, you’ll talk with a mental health professional who'll help you identify and work through factors that may be triggering your mania and/or depression (if you’re diagnosed with bipolar I disorder).

- Cognitive behavioral therapy can be useful in helping you change inaccurate perceptions that you have about yourself and the world around you.
- Family therapy is important since it’s very helpful for your family members to understand your behavior and what they can do to help.
Ask your provider for contact information for local support groups. You might find it helpful to talk with other people who have similar medical experiences and share problems, ideas for coping and strategies for living and caring for yourself.
Other treatments
Electroconvulsant therapy (ECT) may be considered in rare cases in individuals who have severe mania or depression (if bipolar). ECT involves applying brief periods of electric current to your brain.
Prevention
What steps can I take to better cope with or manage my mania?
Although episodes of mania can’t always be prevented, you can make a plan to better manage your symptoms and prevent them from getting worse when you feel a manic episode may be starting.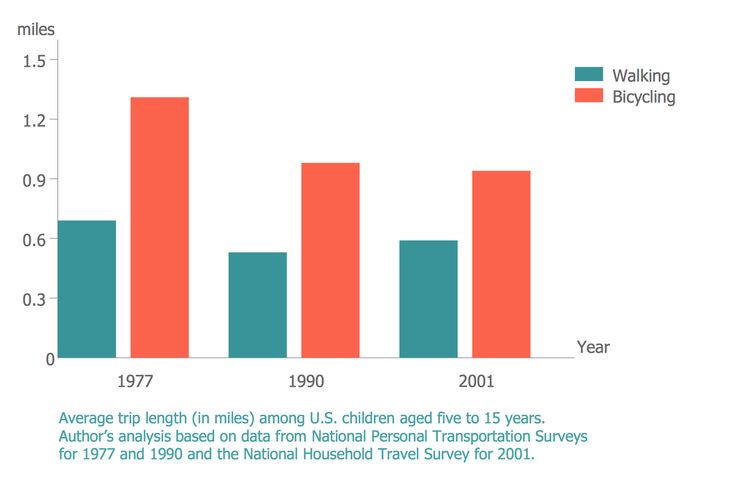
Some ideas to try during this time include:
- Avoid stimulating activities and environment – such as loud or busy places or bright places. Instead choose calm and relaxing activities and environments.
- Stick to routines. Go to bed at a set time, even if you’re not tired. Also, stick to the same times for eating meals, taking medications and exercising.
- Limit the number of social contacts to keep you from getting too stimulated and excited.
- Postpone making any major life decisions and big purchases.
- Avoid people and situations that might tempt you to make poor or risky choices, such as taking recreational drugs or drinking alcohol.
- Consider selecting someone to manage your finances during a manic episode.
If you ever have thoughts of harming yourself, tell family or friends, call you healthcare provider or contact the National Suicide Prevention Lifeline at 800-273-(TALK) (1-800-273-8255). Counselors are available 24/7.
Outlook / Prognosis
What outcome can I expect if I’ve been diagnosed with mania?
If your mania is related to a diagnosis of bipolar I disorder, this is a lifelong disease. Although there’s no cure for mania, medication and talk therapy (psychotherapy) can manage your condition in most cases.
Living With
How can I involve family and friends in understanding my mania?
It’s important to have an honest conversation with your family and closest friends.
- Let your family and friends know what you do and don’t find helpful. For example, if you’d appreciate a friendly reminder about taking your daily medications or a question about if you are getting enough sleep, let them know. On the other hand, if you don’t like always being asked if your current state of happiness is a sign you’re having a manic episode, discuss this.
- Ask your family and friends if they can help identify your triggers if you can’t. They may be able to spot triggers that you can’t spot yourself.
 Ask what they’ve noticed or any patterns they may see around the times of your episodes. As soon as you recognize an early sign, make an appointment to see your healthcare provider. You may or may not need a medication adjustment. However, it’s good to be on the alert since your symptoms could rapidly change.
Ask what they’ve noticed or any patterns they may see around the times of your episodes. As soon as you recognize an early sign, make an appointment to see your healthcare provider. You may or may not need a medication adjustment. However, it’s good to be on the alert since your symptoms could rapidly change. - Describe how your symptoms feel to you. Your family and friends will have a better understanding of your condition.
- Let family and friends know what type of help you’d like from them and when you’d like it. There may be times when you feel you can cope on your own. Knowing the difference will be helpful for everyone.
Frequently Asked Questions
What is acute mania?
Acute mania is the manic phase of bipolar I disorder. It is defined as an extremely unstable euphoric or irritable mood along with excess activity or energy level, excessively rapid thought and speech, reckless behavior and feeling of invincibility.
What is unipolar mania?
Unipolar mania is a disorder in which only excitement, excess activity or energy level and euphoric symptoms are seen. This is a rare condition.
What’s the difference between mania and hypomania?
Hypomania is a less severe form of mania. The criteria that healthcare professionals use to make the diagnosis of either hypomania or mania is what sets them apart. The differences between these two conditions is as follows:
| Mania | Hypomania | |
|---|---|---|
| How long the episode lasts. | At least one week. | At least four consecutive days. |
| Severity of episode. | Causes severe impact on social or work/school functioning. | Not severe enough to significantly affect social or work/school functioning. |
| Need for hospitalization. | Possibly. | No. |
| Psychotic symptoms present (delusions or hallucinations). | Is among possible symptoms. | Can’t be present for a diagnosis of hypomania. |
Can my diagnosis change between bipolar I disorder and bipolar II disorder?
No. Once you have a diagnosis of bipolar I disorder — even if you never have another manic episode or a psychotic event (delusions or hallucinations) — your diagnosis can never be changed to bipolar II disorder. You’ll always have a bipolar I disorder diagnosis.
A note from Cleveland Clinic
Problems can develop in your social life, work/school functioning and home life when you have symptoms of mania, which include mood swings and an abnormal level of energy and activity. You may require hospitalization if you have severe hallucinations or delusions, or to prevent you from harming yourself or others. It’s important to have a good understanding of mania, mania symptoms, your particular triggers and ways to better manage your manic episodes. Medications, talk therapy and support groups as well as support from your family and friends can help manage your mania.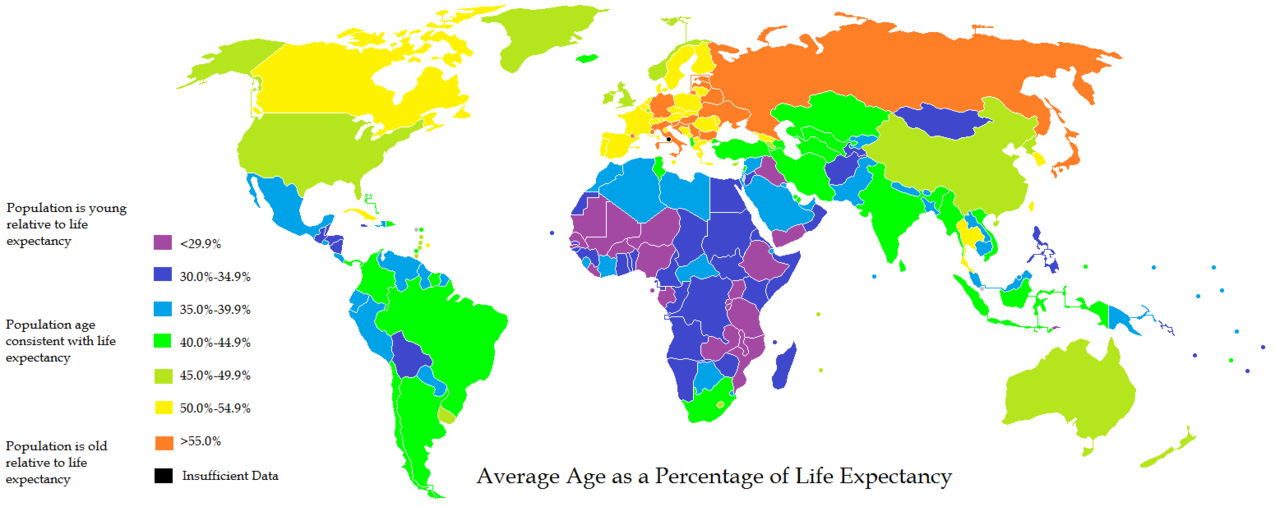 Stay in close contact with all your healthcare providers, especially during times of manic episodes. Your provider will want to see you and may need changes to your medications or dose.
Stay in close contact with all your healthcare providers, especially during times of manic episodes. Your provider will want to see you and may need changes to your medications or dose.
How Long Will a Bipolar Manic Episode Last?
Bipolar disorder includes manic, and sometimes also depressive, episodes. Here’s how long symptoms of mania and its derivatives can last, depending on your type of bipolar disorder.
People with bipolar disorder experience manic episodes, as well as depressive episodes, of varying lengths. Hypomania is different from mania, and a third type of bipolar disorder can manifest with symptoms of hypomania.
When you’re experiencing a manic episode, you may find that you have more energy and an abnormally elevated mood — be it good or irritable. Your inhibitions may also be lowered. You may often struggle to sleep or relax during these episodes.
While you can’t predict exactly how long a manic episode will last, remembering that it won’t last forever can help you get through it.
The length of manic or hypomanic symptoms depends on the type of bipolar disorder you have, according to the National Institute of Mental Health. The length can also vary from person to person. If you’re undergoing treatment, the manic episode might be shorter or less intense.
Generally speaking, these are the durations:
You can learn all the facts on bipolar disorder here.
As mentioned above, symptoms of mania differ by disorder.
A manic episode is characterized by these outward signs:
- hyperactivity
- problems sleeping or resting
- rapid speech
- restlessness, fidgeting
- heightened irritability
- extreme happiness and excitement
During periods of mania, you may make decisions that can result in long-term consequences. You might also create elaborate plans or start new business ventures.
The difference between mania and hypomania is that hypomania is less intense and shorter in duration.
Cyclothymia features only symptoms of hypomania, which is why it’s often underdiagnosed and misdiagnosed.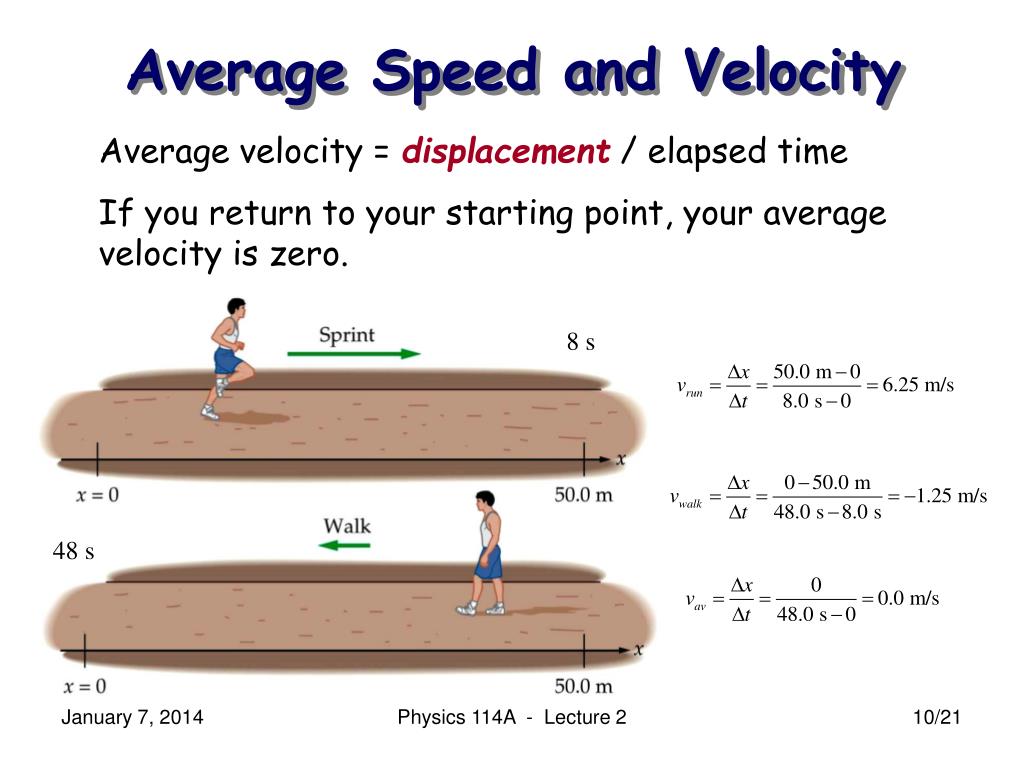
If you’re currently experiencing a manic episode, there are a few things you can do.
- Reach out to your treatment team. Your doctor, psychiatrist, or therapist can help you navigate your episode. They may recommend that you start or change medication.
- Avoid mind-altering substances like alcohol or recreational drugs. Becoming intoxicated can worsen your manic episode or interfere with your medication management.
- Get plenty of sleep. It might be hard to sleep during a manic episode, but try to go to bed and wake up at a regular time. You might find that certain sleep hygiene practices help.
- Eat according to a regular schedule. Hunger can destabilize your mood. Reduce your consumption of caffeine and sugary foods, as these can also affect your mood.
- Spend time with others. If you attend a support group, this might be helpful. Spending time with people close to you and your condition can help you feel more validated and less isolated.
- Stay consistent with meds. No matter whether you’re experiencing a manic episode or not, it’s important to consistently take medication that’s been prescribed to you according to your doctor’s directions. Setting a reminder on your phone might help you during episodes.
Experiencing a manic episode can be difficult and stressful. The good news is that, with the help of your therapist and doctor, you can navigate your manic episode well. During manic episodes, it’s important to keep taking your medication and maintaining a regular and healthy schedule.
Want to learn more about creating a routine to manage bipolar disorder? You can get tips here.
Bipolar affective disorder (BAD) - causes, symptoms, treatment
Bipolar affective disorder (BAD) is a severe mental illness characterized by mood and energy swings with recurring episodes of depression followed by episodes of mania or hypomania. BD is highly heritable. Early onset, chronic course and lack of optimal treatment make it one of the most disabling diseases. The lifetime prevalence of bipolar disorder across the spectrum is estimated at 2–4% of the general population and is the sixth leading cause of disability worldwide. nine0003
The lifetime prevalence of bipolar disorder across the spectrum is estimated at 2–4% of the general population and is the sixth leading cause of disability worldwide. nine0003
The average age at onset of bipolar affective disorder varies. According to epidemiological studies, the peak period is 20 years. It is also reported that approximately 20% of all patients show some signs of the disease in adolescence, about 50% by 30 years and 99% by 60 years.
Overall, the data indicate that bipolar disorder is more common in women, but the disease is also widespread among men. Currently, no relationship has been found between incidence and belonging to any social class. By comparison, there is a clear downward social drift among schizophrenic patients. nine0003
BAR types
The current diagnostic classification describes two main subtypes: bipolar I disorder and bipolar II disorder, which are distinguished by the absence of full-blown manic episodes in type II bipolar disorder. Type I bipolar disorder can be diagnosed on the basis of a single manic episode, but depressive episodes occur in most cases. Type II bipolar disorder is diagnosed if at least one hypomanic and one depressive episode has occurred. Hypomanic episodes are, by definition, clinically less severe than manic episodes, potentially of shorter duration, not markedly impaired in social or occupational functioning, and do not require hospitalization; the appearance of any psychotic symptoms qualifies the episode as manic. nine0003
Type I bipolar disorder can be diagnosed on the basis of a single manic episode, but depressive episodes occur in most cases. Type II bipolar disorder is diagnosed if at least one hypomanic and one depressive episode has occurred. Hypomanic episodes are, by definition, clinically less severe than manic episodes, potentially of shorter duration, not markedly impaired in social or occupational functioning, and do not require hospitalization; the appearance of any psychotic symptoms qualifies the episode as manic. nine0003
Causes of BAD
The mechanisms of the development of the disease are complex, multifaceted and not fully established. Among them, there are genetic predisposition, disturbances in the metabolism of neurotransmitters at the level of the brain, endocrine causes, environmental factors, and others.
Psychiatric genetic research has led to the understanding that bipolar affective disorder and its associated diagnoses undoubtedly have a genetic basis, however, they are not caused by a single abnormal gene, but rather have a highly polygenic structure that is not specific to a particular diagnosis.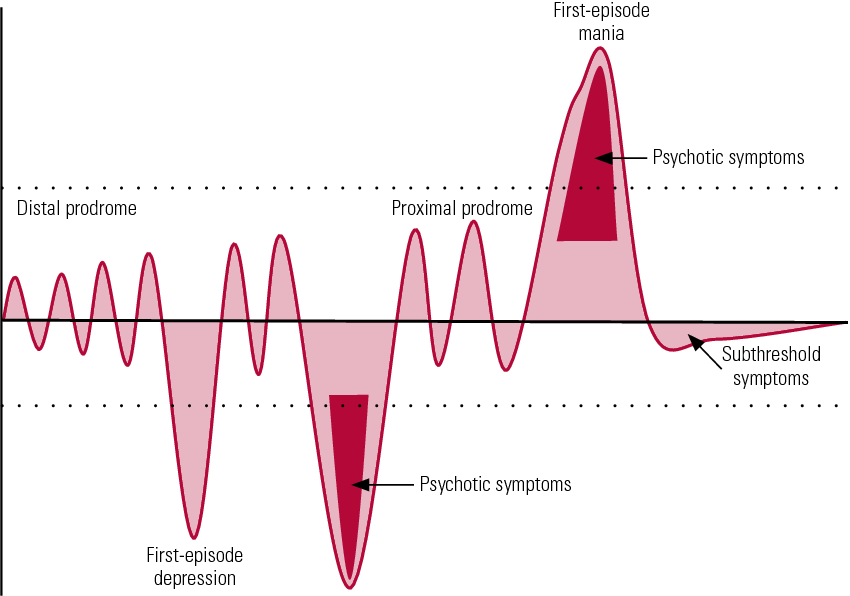 Large pedigree studies show that BAD accumulates in families. The relative risk for immediate family members of patients with bipolar affective disorder is ~7–10%. It is also known that bipolar I disorder tends to aggregate more in families than bipolar type Ⅱ disorder. BAD runs in families with related diagnoses such as major depressive disorder and schizophrenia. At the same time, schizophrenia is more often associated with BAD type Ⅰ compared to BAD type Ⅱ, and major depressive disorder is clearly not combined with a specific BAD subtype. nine0003
Large pedigree studies show that BAD accumulates in families. The relative risk for immediate family members of patients with bipolar affective disorder is ~7–10%. It is also known that bipolar I disorder tends to aggregate more in families than bipolar type Ⅱ disorder. BAD runs in families with related diagnoses such as major depressive disorder and schizophrenia. At the same time, schizophrenia is more often associated with BAD type Ⅰ compared to BAD type Ⅱ, and major depressive disorder is clearly not combined with a specific BAD subtype. nine0003
In the 1960s, the instrumental possibilities for conducting experiments with brain samples expanded. It became realistic to evaluate their response to the introduction of certain drugs. The results of such experiments, combined with clinical observations, have generated many hypotheses about a single neurotransmitter responsible for the development of a particular mental illness. The catecholamine theory of the occurrence of bipolar affective disorder is popular. Its central principle is that the two clinical poles of bipolar disorder - mania and depression - arise as a result of functional changes in the activity of catecholamines, while low activity causes a depressive state, and high activity causes a manic state. There is currently strong evidence that the clinical symptoms of BAD can be mimicked and alleviated by pharmacological modulation of the catecholamine system, but there is no direct evidence that the catecholamine system is involved in the pathogenesis of BAD. The same conclusion has been drawn from contemporary evaluations of other influential hypotheses, such as the dopamine hypothesis of schizophrenia. nine0003
The influence of environmental factors is not studied as widely as the influence of genes. However, some reviews show the role of childhood adversity in the development of bipolar disorder, as well as the role of perinatal complications, maternal influenza infection during pregnancy, exposure to maternal smoking in utero, older paternal age at conception, and others.
Although stressful life events in and of themselves are not considered a cause of bipolar disorder, they can be a trigger for relapse. nine0003
Clinical picture
Bipolar affective disorder refers to mood disorders. It manifests itself in different types of episodes - manic, depressive, mixed, which can be expressed in mild, moderate and severe degrees.
In the case of a depressive syndrome, this can range from subclinical depression to a severe condition that patients perceive as the worst thing that happened in their life. The addition of psychotic symptoms to a severe depressive episode is also likely. These may be delusional ideas of sinfulness, imminent poverty and other misfortunes, for which, according to the patient, he himself is responsible. Auditory hallucinations insult and humiliate, accuse a person, and olfactory hallucinations are most often represented by the smell of sewage. The patient perceives his life as a series of tragic mistakes. Psychomotor retardation can develop up to stupor. Severe depression at least deprives a person of the opportunity to work and maintain social relationships, and in the worst case can lead to suicide. nine0003
Psychomotor retardation can develop up to stupor. Severe depression at least deprives a person of the opportunity to work and maintain social relationships, and in the worst case can lead to suicide. nine0003
Patients with a mild or even moderate depressive episode certainly experience a reluctance to engage in daily activities, but they usually do not stop functioning fully. They have a significant decrease in mood, loss of interest in the surrounding reality, anhedonia - an inability to enjoy, they feel weak, fatigued. Other symptoms include a decrease in the ability to concentrate, low self-esteem, ideas of one's own insignificance, gloomy ideas about the future, sleep disturbances, and a decrease in appetite. nine0003
For a definite diagnosis of depression in bipolar affective disorder, the duration of an episode must be at least two weeks.
Manic syndrome can also be expressed in varying degrees: from hypomania to severe mania with psychotic symptoms.
During the period of hypomania, patients are more socially adapted than in mania. However, in both cases, an important detail is missing - criticism of one's own condition, awareness of oneself as sick. nine0003
However, in both cases, an important detail is missing - criticism of one's own condition, awareness of oneself as sick. nine0003
The manic stage of bipolar disorder is subjectively more pleasant than the depressive stage. Classical mania, the so-called "jolly mania", is characterized by a typical triad of symptoms: increased mood, ideational-psychic excitement, desire for activity. Patients are in a great mood, they love the whole world, they love themselves. They do not have the slightest doubt in their own abilities, in their own genius, and in addition they have a large supply of energy: many sacrifice sleep for the sake of activity, sleep an hour a day, while not feeling overwhelmed. A person in mania has a false sense of being productive, but new ideas come to him so quickly that old ones remain unfulfilled. nine0003
The danger lies in the many rash actions performed by a person on the rise. To give away property, to collect loans, to have questionable sexual contacts, leaving the family and children - a patient with bipolar affective disorder is capable of all this, and he will later have to regret all this.
In addition to classical mania, angry, dysphoric mania also takes place in the structure of the disease. The patient becomes irritable and aggressive beyond measure, especially towards those who do not support his ideas. nine0003
The mixed episode combines seemingly incompatible manifestations: melancholy with significant motor arousal, excellent mood simultaneously with stupor, many ideas in parallel with suicidal thoughts. A person is extremely emotionally unstable, which may be a harbinger of an unfavorable outcome of the course of BAD.
The German psychiatrist Emil Kraepelin noted as early as the 19th century that states of manic arousal can vary greatly in duration from weeks to months, and that more severe forms of mania with marked arousal and psychotic features tend to have relatively long episodes. He also believed that melancholic (depressive) states are usually longer than manic episodes, can sometimes persist for years, and tend to become more pronounced than mania at older ages. Modern research confirms these ancient ideas. nine0003
Modern research confirms these ancient ideas. nine0003
Diagnostics
Bipolar disorder of both types (BAD type Ⅰ and BAD type Ⅱ) is difficult to accurately diagnose in clinical practice, especially in the early stages. Only 20% of patients with bipolar disorder who have had a depressive episode are diagnosed within the first year after seeking treatment, and the average delay between onset and diagnosis is 5–10 years. The main reason for the difficulty in diagnosis is to differentiate bipolar type I or II disorder from unipolar depression, a disease characterized by recurrent depressive episodes, especially in patients who present directly during a depressive episode and in those who do not have a clear history. mania or hypomania. Unipolar depression has been reported to be a common misdiagnosis in patients with bipolar disorder, especially in bipolar II disorder, since patients with this disorder, by definition, never experience major manic episodes. nine0003
In recent years, the diagnostic criteria for bipolar disorder have been revised to address this problem to include both mood changes and activity or energy changes. New rating scales for self-administration and clinical use have been developed to help improve the early detection of clinical signs suggestive of a diagnosis of bipolar disorder in people with a history of depressive episodes.
New rating scales for self-administration and clinical use have been developed to help improve the early detection of clinical signs suggestive of a diagnosis of bipolar disorder in people with a history of depressive episodes.
As with most mental illnesses, physicians are forced to focus only on a carefully collected history and observation of the clinical picture, due to the lack of laboratory or instrumental studies that could help establish the diagnosis of bipolar disorder. It requires an analysis of subjective - collected from the words of the patient, as well as objective - collected from the words of the immediate environment, anamnestic data, isolating information about affective episodes, the nature, duration and severity of their course. nine0003
Features of the course of bipolar disorder in women
There is not much difference between the sexes in lifetime prevalence of bipolar affective disorder. However, there are several clinical characteristics that distinguish men and women with bipolar disorder.
Women have a later age of onset than men. They are more likely to debut during the fifth decade. Women with bipolar disorder are more likely to experience an episode of depression followed by mania, while men with bipolar disorder are either as likely or more likely to experience episodes of mania followed by depression. nine0003
A bimodal peak in psychiatric hospitalizations in spring and autumn is observed in women with bipolar disorder compared to a unimodal peak in men in the spring.
Some studies have shown gender differences in the long-term outcome of bipolar disorder. Women face significantly greater disruption to social/recreational and family life. This, apparently, is due to their irritability, increased self-confidence, talkativeness, windiness and excessive financial extravagance, since such behavior on the part of a woman is more condemned in society than on the part of a man. nine0003
Women are hospitalized much more often than men because they feel worse and tend to seek medical attention more often.
Complications
The most formidable complication of the disease, of course, is the possible suicide of the patient. The determination of suicidal risk is carried out at the very first diagnostic stage of the survey. It includes clarification of anamnestic data related to previous suicide attempts (if any), as well as an assessment of risk factors. There are special questionnaires that can help with this, for example, the Columbia Suicidal Intention Severity Scale. nine0003
Loss of connection with reality during the period of mania, in turn, can also lead to a person causing harm of varying degrees of severity to both himself and others.
BAD treatment
Medical therapy
Due to advances in research on pharmacological and psychosocial treatments for bipolar disorder, recommendations for the treatment of the disorder are frequently revised.
According to recent data, there are several types of treatment for acute mania: mood stabilizers (such as lithium and valproic acid) are widely used in combination with atypical antipsychotics (quetiapine, olanzapine, aripiprazole, risperidone, asenapine, paliperidone, and cariprazine). Typical neuroleptics are also effective in mania, although there is a risk of it switching to depression. nine0003
Typical neuroleptics are also effective in mania, although there is a risk of it switching to depression. nine0003
On the other hand, treatment options for acute bipolar depression are relatively limited. There is evidence supporting the efficacy of quetiapine and olanzapine, as well as the combination of olanzapine and fluoxetine, an antidepressant from the group of selective serotonin reuptake inhibitors. In the depressive phase, it is also possible to prescribe lithium.
Widely available and common tricyclic antidepressants can cause rapid episode cycling and manic reversal, so they should not be used in bipolar disorder, even when combined with mood stabilizers. nine0003
Ketamine, which has a rapid antidepressant effect on treatment-resistant depression, can also be used to treat bipolar depression.
Neuromodulation
Electroconvulsive therapy finds its use in therapeutically resistant depression in bipolar disorder.
Transcranial magnetic stimulation is effective in unipolar depression and mania, but its effectiveness in bipolar depression has not yet been proven. nine0003
nine0003
Other drugs and supplements
Some research suggests a possible beneficial effect of N-acetylcysteine, an antioxidant, on bipolar depression and ramelteon, a melatonin agonist, on mood stability. A meta-analysis found that omega-3 fatty acids are effective for bipolar depression but not for mania. Clinical trials of nutritional supplements that improve mitochondrial function are currently ongoing.
Psychosocial treatments
In the treatment of bipolar disorder, pharmacological and psychosocial approaches must work closely together.
With regard to psychosocial treatment, psychoeducation is paramount and should be carried out for all patients, as this significantly reduces the number of relapses.
Various types of psychotherapy are used in the treatment of bipolar disorder: interpersonal and social rhythm therapy (IPSRT) - a modified version of interpersonal therapy specifically designed for the treatment of bipolar disorder, family therapy, cognitive behavioral therapy (CBT). nine0003
nine0003
Prognosis and prevention
Primary prevention of mental illness, the causes of which are not fully understood, is a difficult task. It seems rational to periodically screen the risk group - children of parents with an established diagnosis of bipolar disorder, the attentive attitude of doctors to the presence of an anxiety disorder in them, to subclinical symptoms of mood changes.
All patients with bipolar affective disorder are recommended to prescribe normothymic drugs in order to prevent relapses and maintain the euthymic period. nine0003
The prognosis depends on the frequency and duration of attacks and intermissions. The constant intake of maintenance therapy individually selected by the doctor allows patients to be in a stable condition and feel the joy of life.
Not Found (#404)
hide menu
Issues of the current year
-
7-8 (136)
-
5-6 (135)
-
3-4 (134)
-
2 (133)
-
1 (132)
7-8 (136)
Issue content 7-8 (136), 2022
-
War Wikis: help in crisis situations
-
Ethical and legal problems of mental health: Ukraine at the focus of international respect
Yu.
Learn more