Interventions for obsessive compulsive disorder
International OCD Foundation | How is OCD Treated?
Overview
- Treatment for most OCD patients should involve Exposure and Response Prevention (ERP) and/or medication.
- The majority of people with OCD (about 7 out of 10) will benefit from either medication or ERP.
What Are the Most Effective Treaments for OCD?
The most effective treatments for OCD are Cognitive Behavior Therapy (CBT)
and/or medication. [1] More specifically, the most effective treatments are a type of CBT called Exposure and Response Prevention (ERP), which has the strongest evidence supporting its use in the treatment of OCD, and/or a class of medications called serotonin reuptake inhibitors, or SRIs.
Exposure and Response Prevention is typically done by a licensed mental health professional (such as a psychologist, social worker, or mental health counselor) in an outpatient setting. This means you visit your therapist’s office at a set appointment time once or a few times a week. Click here for help finding the right therapist for you.
Medications can only be prescribed by a licensed medical professionals (such as your physician or a psychiatrist), who would ideally work together with your therapist to develop a treatment plan. Click here to learn more about medications for OCD.
Taken together, ERP and medication are considered the “first-line” treatments for OCD. In other words, START HERE! About 70% of people will benefit from ERP and/or medication for their OCD.
What if Outpatient ERP Hasn’t Worked? Are There More Intensive Options?
Yes. If you or a loved one has tried traditional outpatient therapy and would like to try a more intensive level of care, there are options. The IOCDF keeps a Resource Directory of intensive treatment centers, specialty outpatient clinics, and therapist who provide these various levels of services for OCD. The following lists therapy options from least intensive to most intensive:
The IOCDF keeps a Resource Directory of intensive treatment centers, specialty outpatient clinics, and therapist who provide these various levels of services for OCD. The following lists therapy options from least intensive to most intensive:
- Traditional Outpatient – Patients see a therapist for individual sessions as often as recommended by their therapist generally one or two times a week for 45-50 minutes. (Most Therapists in the Resource Directory as well as “Specialty Outpatient Clinics” offer this type of treatment).
- Intensive Outpatient – Patients may attend groups and one individual session per day several days per week. Clinics designated as “Intensive Treatment Programs” in the Resource Directory offer this level of treatment.
- Day Program – Patients attend treatment during the day (typically group and individual therapy) at a mental health treatment center usually from 9am – 5pm up to five days a week.
 Many clinics designated as “Intensive Treatment Programs” in the Resource Directory offer this level of treatment.
Many clinics designated as “Intensive Treatment Programs” in the Resource Directory offer this level of treatment. - Partial Hospitalization – Same as the Day Program but patients attend the treatment at a mental health hospital. Several clinics designated as “Intensive Treatment Programs” in the Resource Directory offer this level of treatment.
- Residential – Patients are treated while living voluntarily in an unlocked mental health treatment center or hospital. Clinics designated as “Residential” in the Resource Directory offer this level of treatment.
- Inpatient – This is the highest level of care for a mental health condition. Treatment is provided on a locked unit in a mental health hospital on a voluntary or sometimes involuntary basis. Patients are admitted into this level of care if they are unable to care for themselves or are a danger to themselves or others. The goals of inpatient treatment are to stabilize the patient, which generally takes several days to a week, and then transition the patient to a lower level of care.

Additional Treatment Options for OCD
Other recommendations from the APA Practice Guideline,1 cite research showing that ERP delivered in a group format, as well as ERP therapy delivered via videoconferencing (teletherapy), might be effective. Also, there is some promising new research showing that Acceptance and Commitment Therapy may be helpful for OCD. You can search for any of these treatment types in the Resource Directory.
OCD treatment can be difficult, and requires a lot of courage and determination. Having a support network to talk to during treatment can make all the difference. Consider accessing a support group in your area. Click here to learn more about support groups.
Consider accessing a support group in your area. Click here to learn more about support groups.
OCD can be a family affair. Read more here about the impact on families and what family members can do.
When severe OCD proves resistant to standard forms of treatment, there are other options available. However, it should be noted that all of the following procedures are still currently being researched. While there is evidence to suggest that they could potentially be helpful in reducing OCD symptoms, they are not concretely proven to do so. These should be utilized as a last resort when all of the evidence-based treatment methods for OCD (outlined above) have already been accessed:
What about PANDAS?
PANDAS (Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal infections) is a rare type of OCD that occurs in childhood following the immune system’s overreaction to an infection, such as strep throat. PANDAS should be managed with early antibiotic treatment for strep infections. Continued symptoms can be treated with standard OCD treatments such as exposure and response prevention (ERP) therapy and/or SRI medication*. For more information on PANDAS, including diagnosis and treatment, click here.
PANDAS should be managed with early antibiotic treatment for strep infections. Continued symptoms can be treated with standard OCD treatments such as exposure and response prevention (ERP) therapy and/or SRI medication*. For more information on PANDAS, including diagnosis and treatment, click here.
*Closely watching a child's reaction to SRIs is important as they can cause severe behavioral problems, including suicidal thoughts.
Learn More About OCD
International OCD Foundation | Exposure and Response Prevention (ERP)
What is Exposure and Response Prevention?
You may have heard of cognitive behavior therapy (CBT) before. CBT refers to a group of similar types of therapies used by mental health therapists for treating psychological disorders, with the most important type of CBT for OCD being exposure and response prevention (ERP).
The exposure component of ERP refers to practicing confronting the thoughts, images, objects, and situations that make you anxious and/or provoke your obsessions. The response prevention part of ERP refers to making a choice not to do a compulsive behavior once the anxiety or obsessions have been “triggered.” All of this is done under the guidance of a therapist at the beginning — though you will eventually learn to do your own ERP exercises to help manage your symptoms. Over time, the treatment will “retrain your brain” to no longer see the object of the obsession as a threat.
This strategy of purposefully exposing yourself to things that make you anxious may not sound quite right to you.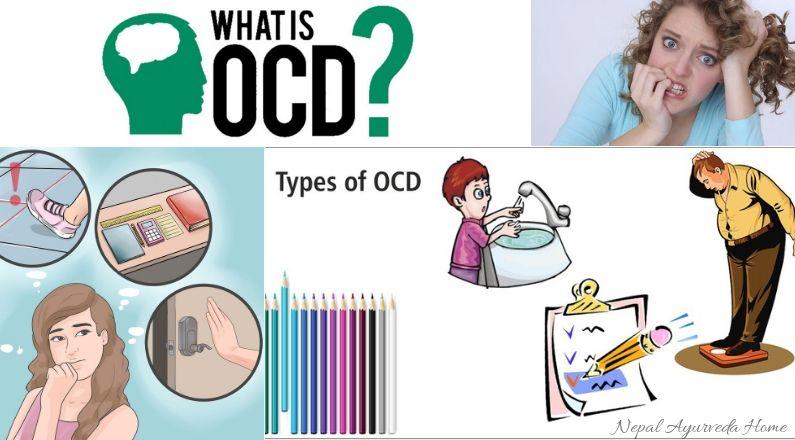 Maybe it sounds difficult. If you have OCD, you have probably tried to confront your obsessions and anxiety only to see that you become very anxious and fearful. With ERP, the difference is that a trained clinician is working with you to develop a plan for exposure. Then, that therapist coaches you through confronting the situation, leaning into the feelings it provokes, sticking with it, and resisting the urge to engage in compulsive behavior.
Maybe it sounds difficult. If you have OCD, you have probably tried to confront your obsessions and anxiety only to see that you become very anxious and fearful. With ERP, the difference is that a trained clinician is working with you to develop a plan for exposure. Then, that therapist coaches you through confronting the situation, leaning into the feelings it provokes, sticking with it, and resisting the urge to engage in compulsive behavior.
Doing ERP is challenging, for sure! But when you do it correctly, the following things happen:
- You will feel an initial increase in anxiety, uncertainty, and obsessional thoughts.
- You will find that these feelings and thoughts are distressing, but also that they can’t hurt you — they are safe and manageable.
- You will find that when you stop fighting the obsessions and anxiety, these feelings will eventually begin to subside.
- This natural drop in anxiety that happens when you stay “exposed” and “prevent” the compulsive “response” is called habituation.
- You will find that your fears are less likely to come true than you thought.
- You will get better at managing “everyday” levels of risk and uncertainty.
A Good Way to Think About OCD and ERP:
Think of anxiety as your body’s alarm system. If your fire alarm goes off, what does it mean? The alarm is there to get your attention and prompt you to take action to protect yourself and your family. But, imagine what would happen if your fire alarm went off every time you burnt a piece of toast or blew out birthday candles? That’s what happens in OCD.
OCD takes over your body’s alarm system so that instead of only warning you of real danger, that alarm system begins to respond to any trigger (no matter how small) as an absolute, terrifying, catastrophic threat.
When your anxiety “goes off” like an alarm system, it communicates information that you are in danger, rather than “pay attention, you might be in danger. ”
”
Unfortunately, with OCD, your brain tells you that you are in danger a lot, even in situations where you “know” that there is a very small likelihood that something bad might happen. This is one of the cruelest parts of this disorder.
Now consider that your compulsive behaviors are your attempts to keep yourself safe when that alarm goes off. What does that mean you are telling your brain when you engage in these behaviors? You are reinforcing the brain’s idea that you must be in danger. Birthday candles are the same as a blazing fire.
In other words, your compulsive behavior fuels that part of your brain that gives out these many unwarranted alarm signals. The bottom line is that in order to reduce your anxiety and your obsessions, you have to make a decision to stop the compulsive behaviors.
However, starting ERP can be a difficult decision to make. It may feel like you are choosing to put yourself in danger. And in the short term, that feels uncomfortable. In the long run, however, you begin to challenge and bring your alarm system (your anxiety) more in line with what is actually happening to you.
How is ERP different from traditional talk therapy (psychotherapy)?
Traditional talk therapy (or psychotherapy) tries to improve a psychological condition by helping you gain “insight” into your problems. Talk therapy can be a very valuable treatment for some disorders, but there is no research evidence that it is effective in treating OCD [1]. While talk therapy may be of benefit at some point in your recovery, it is important to try ERP or medication first, as these are the types of treatment that have been shown through extensive research to be the most effective for treating OCD [2].
- Use the IOCDF’s Resource Directory to find an OCD specialist in your area.
- Read more about medication for OCD.
Sources:
- [1] National Collaborating Centre for Mental Health (UK). Obsessive-Compulsive Disorder: Core Interventions in the Treatment of Obsessive-Compulsive Disorder and Body Dysmorphic Disorder.
 Leicester (UK): British Psychological Society; 2006. (NICE Clinical Guidelines, No. 31.) 5, PSYCHOLOGICAL INTERVENTIONS. Available from: https://www.ncbi.nlm.nih.gov/books/NBK56465/
Leicester (UK): British Psychological Society; 2006. (NICE Clinical Guidelines, No. 31.) 5, PSYCHOLOGICAL INTERVENTIONS. Available from: https://www.ncbi.nlm.nih.gov/books/NBK56465/
↩ - [2] American Psychiatric Association, Koran, L. M., Hanna, G. L., Hollander, E., Nestadt, G., & Simpson, H. B. (2007). Practice guideline for the treatment of patients with obsessive-compulsive disorder. Arlington, VA: American Psychiatric Association, 2007. Available online at http//www.psych.org/psych_pract/treatg/pg/ prac_ guide.cfm ↩
Obsessive-compulsive disorder
A prominent role among mental illnesses is played by syndromes (complexes of symptoms), united in the group of obsessive-compulsive disorder (OCD), which received its name from the Latin terms obsessio and compulsio.
Obsession (lat. obsessio - taxation, siege, blockade).
Compulsions (lat. compello - I force). 1. Obsessive drives, a kind of obsessive phenomena (obsessions).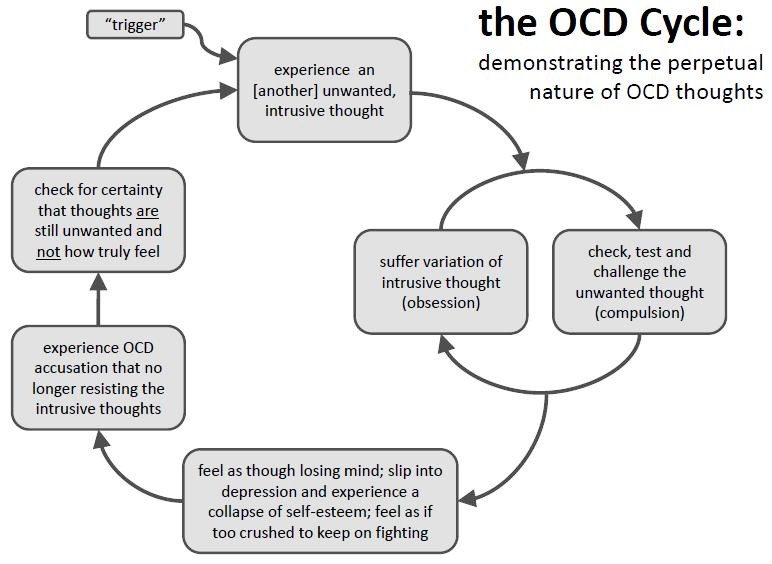 Characterized by irresistible attraction that arises contrary to the mind, will, feelings. Often they are unacceptable to the patient, contrary to his moral and ethical properties. Unlike impulsive drives, compulsions are not realized. These drives are recognized by the patient as wrong and painfully experienced by them, especially since their very appearance, due to its incomprehensibility, often gives rise to a feeling of fear in the patient 2. The term compulsions is also used in a broader sense to refer to any obsessions in the motor sphere, including obsessive rituals.
Characterized by irresistible attraction that arises contrary to the mind, will, feelings. Often they are unacceptable to the patient, contrary to his moral and ethical properties. Unlike impulsive drives, compulsions are not realized. These drives are recognized by the patient as wrong and painfully experienced by them, especially since their very appearance, due to its incomprehensibility, often gives rise to a feeling of fear in the patient 2. The term compulsions is also used in a broader sense to refer to any obsessions in the motor sphere, including obsessive rituals.
In domestic psychiatry, obsessive states were understood as psychopathological phenomena, characterized by the fact that phenomena of a certain content repeatedly appear in the mind of the patient, accompanied by a painful feeling of coercion [Zinoviev PM, 193I]. For N.s. characteristic involuntary, even against the will, the emergence of obsessions with clear consciousness. Although the obsessions are alien, extraneous in relation to the patient's psyche, the patient is not able to get rid of them. They are closely related to the emotional sphere, accompanied by depressive reactions, anxiety. Being symptomatic, according to S.L. Sukhanov [1912], "parasitic", they do not affect the course of intellectual activity in general, remain alien to thinking, do not lead to a decrease in its level, although they worsen the efficiency and productivity of the patient's mental activity. Throughout the course of the disease, a critical attitude is maintained towards obsessions. N.s. conditionally divided into obsessions in the intellectual-affective (phobia) and motor (compulsions) spheres, but most often several of their types are combined in the structure of the disease of obsessions. The isolation of obsessions that are abstract, affectively indifferent, indifferent in their content, for example, arrhythmomania, is rarely justified; An analysis of the psychogenesis of a neurosis often makes it possible to see a pronounced affective (depressive) background at the basis of the obsessive account.
They are closely related to the emotional sphere, accompanied by depressive reactions, anxiety. Being symptomatic, according to S.L. Sukhanov [1912], "parasitic", they do not affect the course of intellectual activity in general, remain alien to thinking, do not lead to a decrease in its level, although they worsen the efficiency and productivity of the patient's mental activity. Throughout the course of the disease, a critical attitude is maintained towards obsessions. N.s. conditionally divided into obsessions in the intellectual-affective (phobia) and motor (compulsions) spheres, but most often several of their types are combined in the structure of the disease of obsessions. The isolation of obsessions that are abstract, affectively indifferent, indifferent in their content, for example, arrhythmomania, is rarely justified; An analysis of the psychogenesis of a neurosis often makes it possible to see a pronounced affective (depressive) background at the basis of the obsessive account. Along with elementary obsessions, the connection of which with psychogeny is obvious, there are “cryptogenic” ones, when the cause of painful experiences is hidden [Svyadoshch L.M., 1959]. N.s. are observed mainly in individuals with a psychasthenic character. This is where apprehensions are especially characteristic. In addition, N.S. occur within the framework of neurosis-like states with sluggish schizophrenia, endogenous depressions, epilepsy, the consequences of a traumatic brain injury, somatic diseases, mainly hypochondria-phobic or nosophobic syndrome. Some researchers distinguish the so-called. "Neurosis of obsessive states", which is characterized by the predominance of obsessive states in the clinical picture - memories that reproduce a psychogenic traumatic situation, thoughts, fears, actions. In genesis play a role: mental trauma; conditioned reflex stimuli that have become pathogenic due to their coincidence with others that previously caused a feeling of fear; situations that have become psychogenic due to the confrontation of opposing tendencies [Svyadoshch A.
Along with elementary obsessions, the connection of which with psychogeny is obvious, there are “cryptogenic” ones, when the cause of painful experiences is hidden [Svyadoshch L.M., 1959]. N.s. are observed mainly in individuals with a psychasthenic character. This is where apprehensions are especially characteristic. In addition, N.S. occur within the framework of neurosis-like states with sluggish schizophrenia, endogenous depressions, epilepsy, the consequences of a traumatic brain injury, somatic diseases, mainly hypochondria-phobic or nosophobic syndrome. Some researchers distinguish the so-called. "Neurosis of obsessive states", which is characterized by the predominance of obsessive states in the clinical picture - memories that reproduce a psychogenic traumatic situation, thoughts, fears, actions. In genesis play a role: mental trauma; conditioned reflex stimuli that have become pathogenic due to their coincidence with others that previously caused a feeling of fear; situations that have become psychogenic due to the confrontation of opposing tendencies [Svyadoshch A. M., 1982]. It should be noted that these same authors emphasize that N.s.c. occurs with various character traits, but most often in psychasthenic personalities.
M., 1982]. It should be noted that these same authors emphasize that N.s.c. occurs with various character traits, but most often in psychasthenic personalities.
Currently, almost all obsessive-compulsive disorders are united in the International Classification of Diseases under the concept of "obsessive-compulsive disorder".
OKR concepts have undergone a fundamental reassessment over the past 15 years. During this time, the clinical and epidemiological significance of OCD has been completely revised. If it was previously thought that this is a rare condition observed in a small number of people, now it is known that OCD is common and causes a high percentage of morbidity, which requires the urgent attention of psychiatrists around the world. Parallel to this, our understanding of the etiology of OCD has broadened: the vaguely formulated psychoanalytic definition of the past two decades has been replaced by a neurochemical paradigm that explores the neurotransmitter disorders that underlie OCD. And most importantly, pharmacological interventions specifically targeting serotonergic neurotransmission have revolutionized the prospects for recovery for millions of OCD patients worldwide.
And most importantly, pharmacological interventions specifically targeting serotonergic neurotransmission have revolutionized the prospects for recovery for millions of OCD patients worldwide.
The discovery that intense serotonin reuptake inhibition (SSRI) was the key to effective treatment for OCD was the first step in a revolution and spurred clinical research that showed the efficacy of such selective inhibitors.
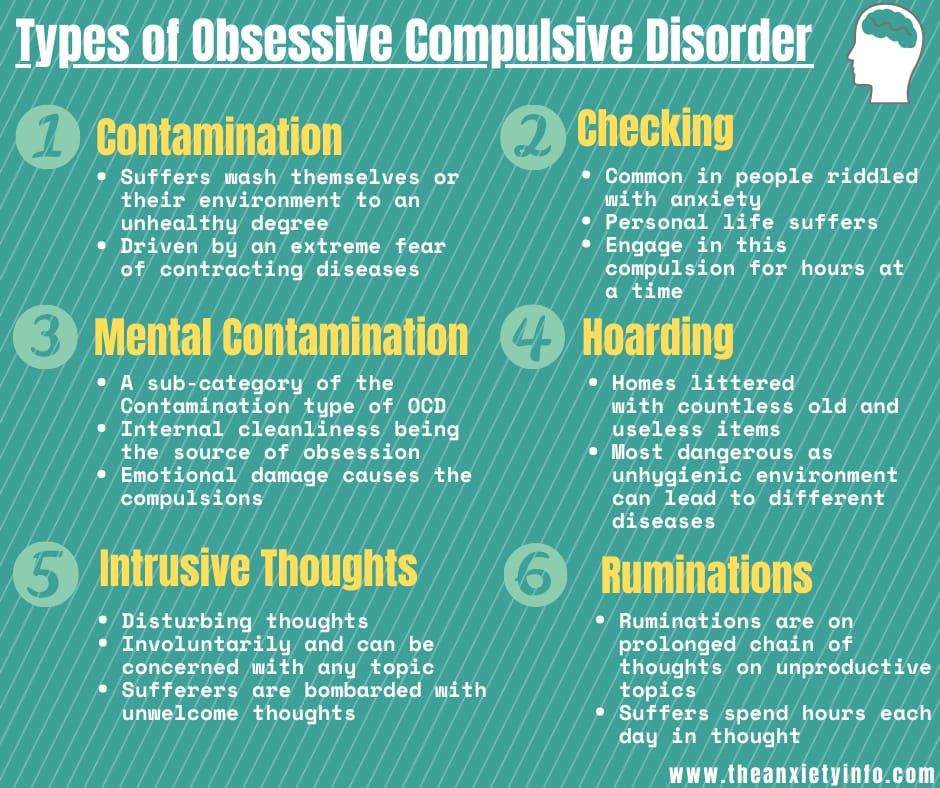
As described in ICD-10, the main features of OCD are repetitive intrusive (obsessive) thoughts and compulsive actions (rituals).
In a broad sense, the core of OCD is the syndrome of obsession, which is a condition with a predominance in the clinical picture of feelings, thoughts, fears, memories that arise in addition to the desire of patients, but with awareness of their pain and a critical attitude towards them. Despite the understanding of the unnaturalness, illogicality of obsessions and states, patients are powerless in their attempts to overcome them. Obsessional impulses or ideas are recognized as alien to the personality, but as if coming from within. Obsessions can be the performance of rituals designed to alleviate anxiety, such as washing hands to combat "pollution" and to prevent "infection". Attempts to drive away unwelcome thoughts or urges can lead to severe internal struggle, accompanied by intense anxiety.
Obsessional impulses or ideas are recognized as alien to the personality, but as if coming from within. Obsessions can be the performance of rituals designed to alleviate anxiety, such as washing hands to combat "pollution" and to prevent "infection". Attempts to drive away unwelcome thoughts or urges can lead to severe internal struggle, accompanied by intense anxiety.
Obsessions in the ICD-10 are included in the group of neurotic disorders.
The prevalence of OCD in the population is quite high. According to some data, it is determined by an indicator of 1.5% (meaning "fresh" cases of diseases) or 2-3%, if episodes of exacerbations observed throughout life are taken into account. Those suffering from obsessive-compulsive disorder make up 1% of all patients receiving treatment in psychiatric institutions. It is believed that men and women are affected approximately equally.
CLINICAL PICTURE
The problem of obsessive-compulsive disorders attracted the attention of clinicians already at the beginning of the 17th century. They were first described by Platter in 1617. In 1621 E. Barton described an obsessive fear of death. Mentions of obsessions are found in the writings of F. Pinel (1829). I. Balinsky proposed the term "obsessive ideas", which took root in Russian psychiatric literature. In 1871, Westphal coined the term "agoraphobia" to refer to the fear of being in public places. M. Legrand de Sol [1875], analyzing the features of the dynamics of OCD in the form of "insanity of doubt with delusions of touch, points to a gradually becoming more complicated clinical picture - obsessive doubts are replaced by ridiculous fears of" touch "to surrounding objects, motor rituals join, the fulfillment of which is subject to the whole life sick. However, only at the turn of the XIX-XX centuries. researchers were able to more or less clearly describe the clinical picture and give syndromic characteristics of obsessive-compulsive disorders. The onset of the disease usually occurs in adolescence and adolescence. The maximum of clinically defined manifestations of obsessive-compulsive disorder is observed in the age range of 10-25 years.
They were first described by Platter in 1617. In 1621 E. Barton described an obsessive fear of death. Mentions of obsessions are found in the writings of F. Pinel (1829). I. Balinsky proposed the term "obsessive ideas", which took root in Russian psychiatric literature. In 1871, Westphal coined the term "agoraphobia" to refer to the fear of being in public places. M. Legrand de Sol [1875], analyzing the features of the dynamics of OCD in the form of "insanity of doubt with delusions of touch, points to a gradually becoming more complicated clinical picture - obsessive doubts are replaced by ridiculous fears of" touch "to surrounding objects, motor rituals join, the fulfillment of which is subject to the whole life sick. However, only at the turn of the XIX-XX centuries. researchers were able to more or less clearly describe the clinical picture and give syndromic characteristics of obsessive-compulsive disorders. The onset of the disease usually occurs in adolescence and adolescence. The maximum of clinically defined manifestations of obsessive-compulsive disorder is observed in the age range of 10-25 years.
Main clinical manifestations of OCD:
Obsessional thoughts - painful, arising against the will, but recognized by the patient as their own, ideas, beliefs, images, which in a stereotyped form forcibly invade the patient's consciousness and which he tries to resist in some way. It is this combination of an inner sense of compulsive urge and efforts to resist it that characterizes obsessional symptoms, but of the two, the degree of effort exerted is the more variable. Obsessive thoughts may take the form of single words, phrases, or lines of poetry; they are usually unpleasant to the patient and may be obscene, blasphemous, or even shocking.
Obsessional imagery is vivid scenes, often violent or disgusting, including, for example, sexual perversion.
Obsessional impulses are urges to do things that are usually destructive, dangerous or shameful; for example, jumping into the road in front of a moving car, injuring a child, or shouting obscene words while in society.
Obsessional rituals include both mental activities (eg, counting repeatedly in a particular way, or repeating certain words) and repetitive but meaningless acts (eg, washing hands twenty or more times a day). Some of them have an understandable connection with the obsessive thoughts that preceded them, for example, repeated washing of hands - with thoughts of infection. Other rituals (for example, regularly laying out clothes in some complex system before putting them on) do not have such a connection. Some patients feel an irresistible urge to repeat such actions a certain number of times; if that fails, they are forced to start all over again. Patients are invariably aware that their rituals are illogical and usually try to hide them. Some fear that such symptoms are a sign of the onset of insanity. Both obsessive thoughts and rituals inevitably lead to problems in daily activities.
Obsessive rumination (“mental chewing gum”) is an internal debate in which the arguments for and against even the simplest everyday actions are endlessly revised. Some obsessive doubts relate to actions that may have been incorrectly performed or not completed, such as turning off the gas stove faucet or locking the door; others concern actions that could harm other people (for example, the possibility of driving past a cyclist in a car, knocking him down). Sometimes doubts are associated with a possible violation of religious prescriptions and rituals - “remorse of conscience”.
Some obsessive doubts relate to actions that may have been incorrectly performed or not completed, such as turning off the gas stove faucet or locking the door; others concern actions that could harm other people (for example, the possibility of driving past a cyclist in a car, knocking him down). Sometimes doubts are associated with a possible violation of religious prescriptions and rituals - “remorse of conscience”.
Compulsive actions - repetitive stereotypical actions, sometimes acquiring the character of protective rituals. The latter are aimed at preventing any objectively unlikely events that are dangerous for the patient or his relatives.
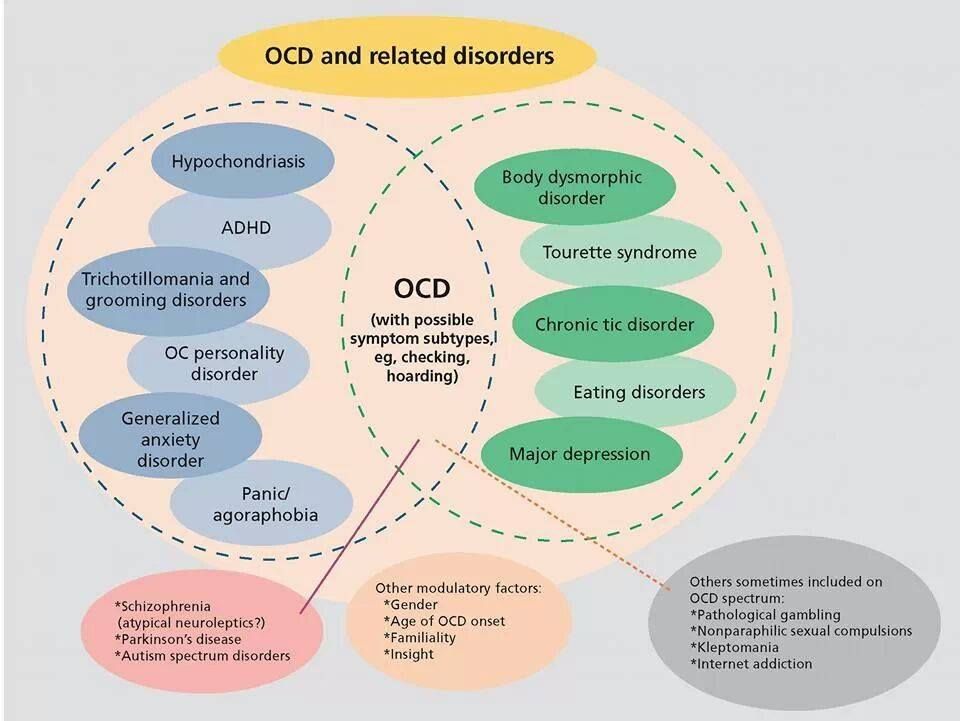
In addition to the above, in a number of obsessive-compulsive disorders, a number of well-defined symptom complexes stand out, and among them are obsessive doubts, contrasting obsessions, obsessive fears - phobias (from the Greek. phobos).
Obsessive thoughts and compulsive rituals may intensify in certain situations; for example, obsessive thoughts about harming other people often become more persistent in the kitchen or some other place where knives are kept.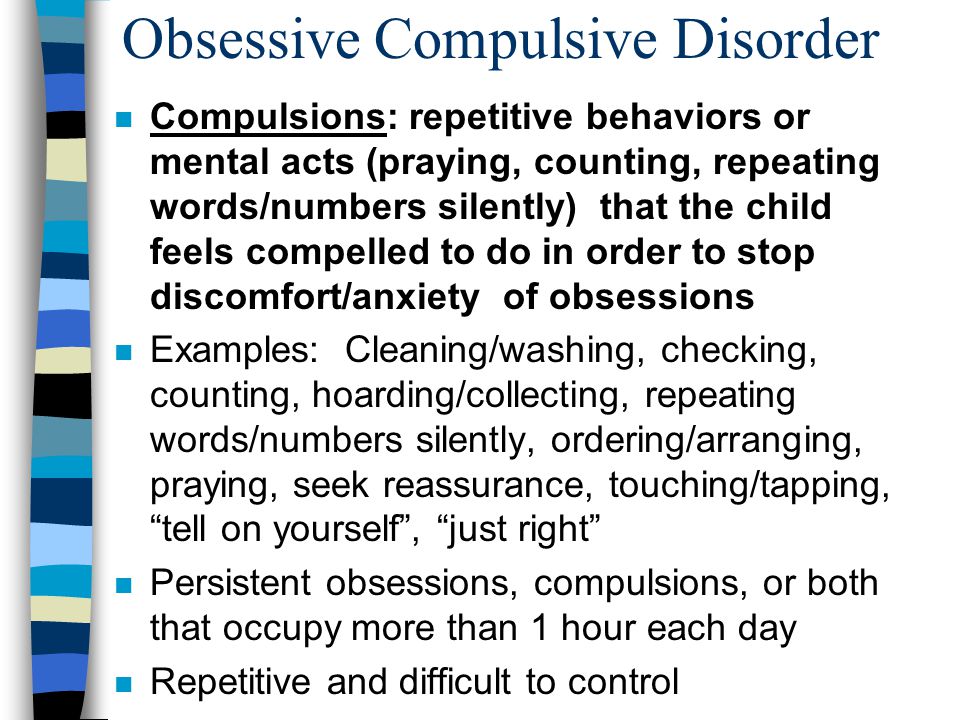 Since patients often avoid such situations, there may be a superficial resemblance to the characteristic avoidance pattern found in phobic anxiety disorder. Anxiety is an important component of obsessive-compulsive disorders. Some rituals reduce anxiety, while after others it increases. Obsessions often develop as part of depression. In some patients, this appears to be a psychologically understandable reaction to obsessive-compulsive symptoms, but in other patients, recurrent episodes of depressive mood occur independently.
Since patients often avoid such situations, there may be a superficial resemblance to the characteristic avoidance pattern found in phobic anxiety disorder. Anxiety is an important component of obsessive-compulsive disorders. Some rituals reduce anxiety, while after others it increases. Obsessions often develop as part of depression. In some patients, this appears to be a psychologically understandable reaction to obsessive-compulsive symptoms, but in other patients, recurrent episodes of depressive mood occur independently.
Obsessions (obsessions) are divided into figurative or sensual, accompanied by the development of affect (often painful) and obsessions of affectively neutral content.
Sensual obsessions include obsessive doubts, memories, ideas, drives, actions, fears, an obsessive feeling of antipathy, an obsessive fear of habitual actions.
Obsessive doubts - intrusively arising contrary to logic and reason, uncertainty about the correctness of committed and committed actions. The content of doubts is different: obsessive everyday fears (whether the door is locked, whether windows or water taps are closed tightly enough, whether gas and electricity are turned off), doubts related to official activities (whether this or that document is written correctly, whether the addresses on business papers are mixed up , whether inaccurate figures are indicated, whether orders are correctly formulated or executed), etc. Despite repeated verification of the committed action, doubts, as a rule, do not disappear, causing psychological discomfort in the person suffering from this kind of obsession.
The content of doubts is different: obsessive everyday fears (whether the door is locked, whether windows or water taps are closed tightly enough, whether gas and electricity are turned off), doubts related to official activities (whether this or that document is written correctly, whether the addresses on business papers are mixed up , whether inaccurate figures are indicated, whether orders are correctly formulated or executed), etc. Despite repeated verification of the committed action, doubts, as a rule, do not disappear, causing psychological discomfort in the person suffering from this kind of obsession.
Obsessive memories include persistent, irresistible painful memories of any sad, unpleasant or shameful events for the patient, accompanied by a sense of shame, remorse. They dominate the mind of the patient, despite the efforts and efforts not to think about them.
Obsessive impulses - urges to commit one or another tough or extremely dangerous action, accompanied by a feeling of horror, fear, confusion with the inability to get rid of it. The patient is seized, for example, by the desire to throw himself under a passing train or push a loved one under it, to kill his wife or child in an extremely cruel way. At the same time, patients are painfully afraid that this or that action will be implemented.
The patient is seized, for example, by the desire to throw himself under a passing train or push a loved one under it, to kill his wife or child in an extremely cruel way. At the same time, patients are painfully afraid that this or that action will be implemented.
Manifestations of obsessive ideas can be different. In some cases, this is a vivid "vision" of the results of obsessive drives, when patients imagine the result of a cruel act committed. In other cases, obsessive ideas, often referred to as mastering, appear in the form of implausible, sometimes absurd situations that patients take for real. An example of obsessive ideas is the patient's conviction that the buried relative was alive, and the patient painfully imagines and experiences the suffering of the deceased in the grave. At the height of obsessive ideas, the consciousness of their absurdity, implausibility disappears and, on the contrary, confidence in their reality appears. As a result, obsessions acquire the character of overvalued formations (dominant ideas that do not correspond to their true meaning), and sometimes delusions.
An obsessive feeling of antipathy (as well as obsessive blasphemous and blasphemous thoughts) - unjustified, driven away by the patient from himself antipathy towards a certain, often close person, cynical, unworthy thoughts and ideas in relation to respected people, in religious persons - in relation to saints or ministers churches.
Obsessive acts are acts done against the wishes of the sick, despite efforts made to restrain them. Some of the obsessive actions burden the patients until they are realized, others are not noticed by the patients themselves. Obsessive actions are painful for patients, especially in those cases when they become the object of attention of others.
Obsessive fears, or phobias, include an obsessive and senseless fear of heights, large streets, open or confined spaces, large crowds of people, the fear of sudden death, the fear of falling ill with one or another incurable disease. Some patients may develop a wide variety of phobias, sometimes acquiring the character of fear of everything (panphobia).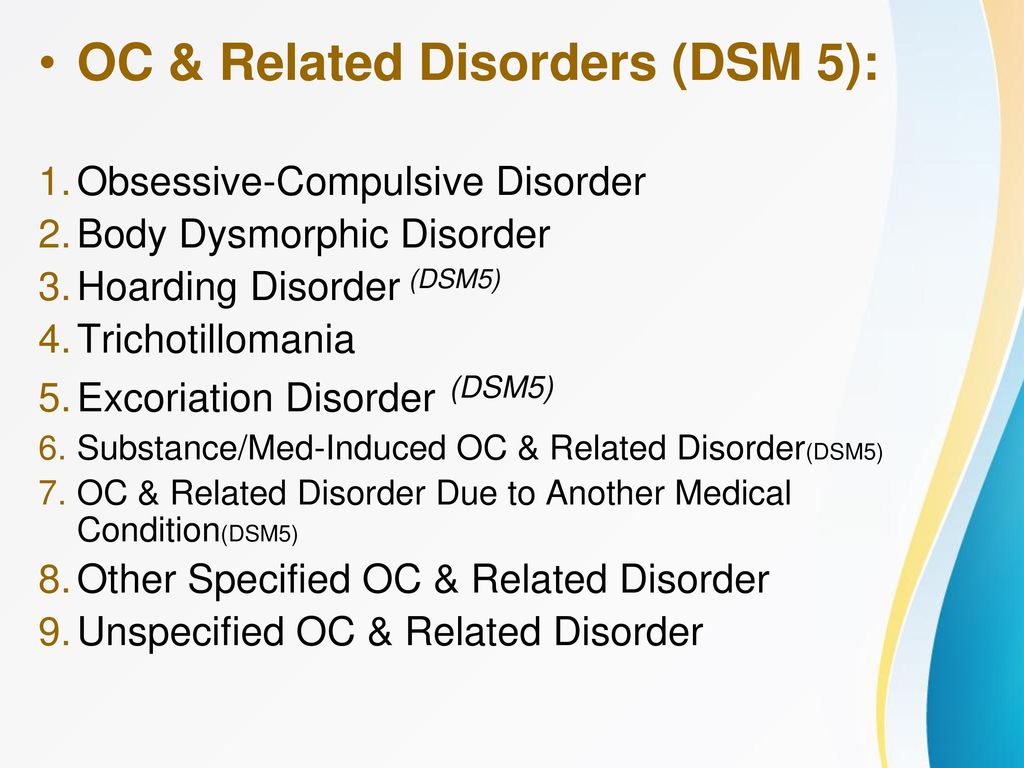 And finally, an obsessive fear of the emergence of fears (phobophobia) is possible.
And finally, an obsessive fear of the emergence of fears (phobophobia) is possible.
Hypochondriacal phobias (nosophobia) - an obsessive fear of some serious illness. Most often, cardio-, stroke-, syphilo- and AIDS phobias are observed, as well as the fear of the development of malignant tumors. At the peak of anxiety, patients sometimes lose their critical attitude to their condition - they turn to doctors of the appropriate profile, require examination and treatment. The implementation of hypochondriacal phobias occurs both in connection with psycho- and somatogenic (general non-mental illnesses) provocations, and spontaneously. As a rule, hypochondriacal neurosis develops as a result, accompanied by frequent visits to doctors and unreasonable medication.
Specific (isolated) phobias - obsessive fears limited to a strictly defined situation - fear of heights, nausea, thunderstorms, pets, treatment at the dentist, etc. Since contact with situations that cause fear is accompanied by intense anxiety, the patients tend to avoid them.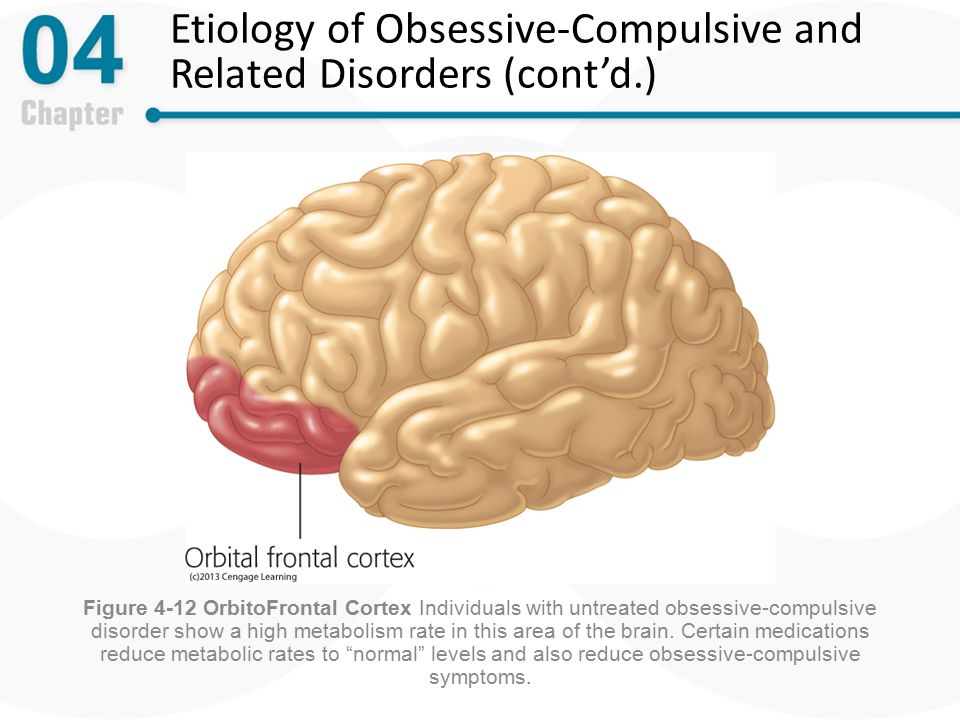
Obsessive fears are often accompanied by the development of rituals - actions that have the meaning of "magic" spells that are performed, despite the critical attitude of the patient to obsession, in order to protect against one or another imaginary misfortune: before starting any important business, the patient must perform some that specific action to eliminate the possibility of failure. Rituals can, for example, be expressed in snapping fingers, playing a melody to the patient or repeating certain phrases, etc. In these cases, even relatives are not aware of the existence of such disorders. Rituals, combined with obsessions, are a fairly stable system that usually exists for many years and even decades.
Obsessions of affectively neutral content - obsessive sophistication, obsessive counting, recalling neutral events, terms, formulations, etc. Despite their neutral content, they burden the patient, interfere with his intellectual activity.
Contrasting obsessions ("aggressive obsessions") - blasphemous, blasphemous thoughts, fear of harming oneself and others. Psychopathological formations of this group refer mainly to figurative obsessions with pronounced affective saturation and ideas that take possession of the consciousness of patients. They are distinguished by a sense of alienation, the absolute lack of motivation of the content, as well as a close combination with obsessive drives and actions. Patients with contrasting obsessions and complain of an irresistible desire to add endings to the replicas they have just heard, giving an unpleasant or threatening meaning to what has been said, to repeat after those around them, but with a touch of irony or malice, phrases of religious content, to shout out cynical words that contradict their own attitudes and generally accepted morality. , they may experience fear of losing control of themselves and possibly committing dangerous or ridiculous actions, injuring themselves or their loved ones. In the latter cases, obsessions are often combined with object phobias (fear of sharp objects - knives, forks, axes, etc.
Psychopathological formations of this group refer mainly to figurative obsessions with pronounced affective saturation and ideas that take possession of the consciousness of patients. They are distinguished by a sense of alienation, the absolute lack of motivation of the content, as well as a close combination with obsessive drives and actions. Patients with contrasting obsessions and complain of an irresistible desire to add endings to the replicas they have just heard, giving an unpleasant or threatening meaning to what has been said, to repeat after those around them, but with a touch of irony or malice, phrases of religious content, to shout out cynical words that contradict their own attitudes and generally accepted morality. , they may experience fear of losing control of themselves and possibly committing dangerous or ridiculous actions, injuring themselves or their loved ones. In the latter cases, obsessions are often combined with object phobias (fear of sharp objects - knives, forks, axes, etc.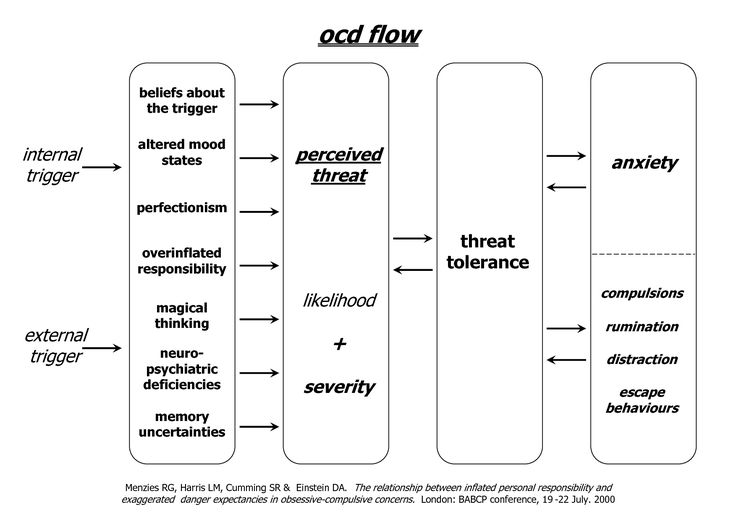 ). The contrasting group also partially includes obsessions of sexual content (obsessions of the type of forbidden ideas about perverted sexual acts, the objects of which are children, representatives of the same sex, animals).
). The contrasting group also partially includes obsessions of sexual content (obsessions of the type of forbidden ideas about perverted sexual acts, the objects of which are children, representatives of the same sex, animals).
Obsessions of pollution (mysophobia). This group of obsessions includes both the fear of pollution (earth, dust, urine, feces and other impurities), as well as the fear of penetration into the body of harmful and toxic substances (cement, fertilizers, toxic waste), small objects (glass fragments, needles, specific types of dust), microorganisms. In some cases, the fear of contamination can be limited, remain at the preclinical level for many years, manifesting itself only in some features of personal hygiene (frequent change of linen, repeated washing of hands) or in housekeeping (thorough handling of food, daily washing of floors). , "taboo" on pets). This kind of monophobia does not significantly affect the quality of life and is evaluated by others as habits (exaggerated cleanliness, excessive disgust). Clinically manifested variants of mysophobia belong to the group of severe obsessions. In these cases, gradually becoming more complex protective rituals come to the fore: avoiding sources of pollution and touching "unclean" objects, processing things that could get dirty, a certain sequence in the use of detergents and towels, which allows you to maintain "sterility" in the bathroom. Stay outside the apartment is also furnished with a series of protective measures: going out into the street in special clothing that covers the body as much as possible, special processing of wearable items upon returning home. In the later stages of the disease, patients, avoiding pollution, not only do not go out, but do not even leave their own room. In order to avoid contacts and contacts that are dangerous in terms of contamination, patients do not allow even their closest relatives to come near them. Mysophobia is also related to the fear of contracting a disease, which does not belong to the categories of hypochondriacal phobias, since it is not determined by fears that a person suffering from OCD has a particular disease.
Clinically manifested variants of mysophobia belong to the group of severe obsessions. In these cases, gradually becoming more complex protective rituals come to the fore: avoiding sources of pollution and touching "unclean" objects, processing things that could get dirty, a certain sequence in the use of detergents and towels, which allows you to maintain "sterility" in the bathroom. Stay outside the apartment is also furnished with a series of protective measures: going out into the street in special clothing that covers the body as much as possible, special processing of wearable items upon returning home. In the later stages of the disease, patients, avoiding pollution, not only do not go out, but do not even leave their own room. In order to avoid contacts and contacts that are dangerous in terms of contamination, patients do not allow even their closest relatives to come near them. Mysophobia is also related to the fear of contracting a disease, which does not belong to the categories of hypochondriacal phobias, since it is not determined by fears that a person suffering from OCD has a particular disease. In the foreground is the fear of a threat from the outside: the fear of pathogenic bacteria entering the body. Hence the development of appropriate protective actions.
In the foreground is the fear of a threat from the outside: the fear of pathogenic bacteria entering the body. Hence the development of appropriate protective actions.
A special place in the series of obsessions is occupied by obsessive actions in the form of isolated, monosymptomatic movement disorders. Among them, especially in childhood, tics predominate, which, unlike organically conditioned involuntary movements, are much more complex motor acts that have lost their original meaning. Tics sometimes give the impression of exaggerated physiological movements. This is a kind of caricature of certain motor acts, natural gestures. Patients suffering from tics can shake their heads (as if checking whether the hat fits well), make hand movements (as if discarding interfering hair), blink their eyes (as if getting rid of a mote). Along with obsessive tics, pathological habitual actions (lip biting, gnashing of teeth, spitting, etc.) are often observed, which differ from obsessive actions proper in the absence of a subjectively painful sense of persistence and experience them as alien, painful.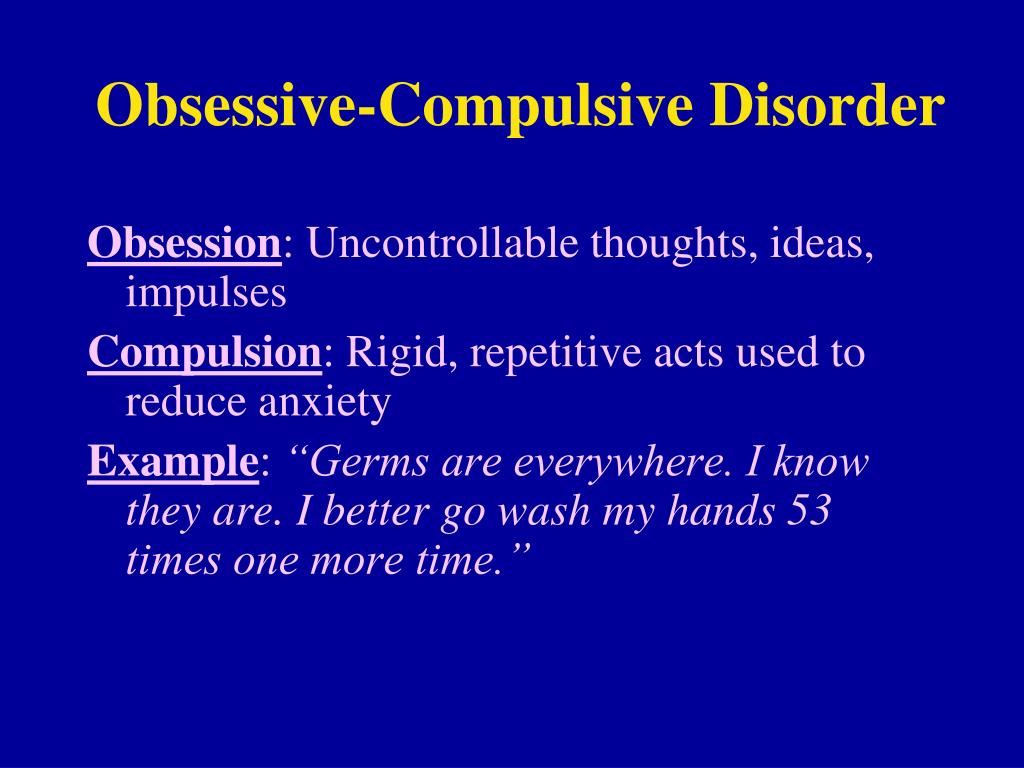 Neurotic states characterized only by obsessive tics usually have a favorable prognosis. Appearing most often in preschool and primary school age, tics usually subside by the end of puberty. However, such disorders can also be more persistent, persist for many years and only partially change in manifestations.
Neurotic states characterized only by obsessive tics usually have a favorable prognosis. Appearing most often in preschool and primary school age, tics usually subside by the end of puberty. However, such disorders can also be more persistent, persist for many years and only partially change in manifestations.
The course of obsessive-compulsive disorder.
Unfortunately, chronization must be indicated as the most characteristic trend in the OCD dynamics. Cases of episodic manifestations of the disease and complete recovery are relatively rare. However, in many patients, especially with the development and preservation of one type of manifestation (agoraphobia, obsessive counting, ritual handwashing, etc.), a long-term stabilization of the condition is possible. In these cases, there is a gradual (usually in the second half of life) mitigation of psychopathological symptoms and social readaptation. For example, patients who experienced fear of traveling on certain types of transport, or public speaking, cease to feel flawed and work along with healthy people. In mild forms of OCD, the disease usually proceeds favorably (on an outpatient basis). The reverse development of symptoms occurs after 1 year - 5 years from the moment of manifestation.
In mild forms of OCD, the disease usually proceeds favorably (on an outpatient basis). The reverse development of symptoms occurs after 1 year - 5 years from the moment of manifestation.
More severe and complex OCDs such as phobias of infection, pollution, sharp objects, contrasting performances, multiple rituals, on the other hand, may become persistent, resistant to treatment, or show a tendency to recur with disorders that persist despite active therapy. Further negative dynamics of these conditions indicates a gradual complication of the clinical picture of the disease as a whole.
DIFFERENTIAL DIAGNOSIS
It is important to distinguish OCD from other disorders that involve compulsions and rituals. In some cases, obsessive-compulsive disorder must be differentiated from schizophrenia, especially when the obsessive thoughts are unusual in content (eg, mixed sexual and blasphemous themes) or the rituals are exceptionally eccentric. The development of a sluggish schizophrenic process cannot be ruled out with the growth of ritual formations, their persistence, the emergence of antagonistic tendencies in mental activity (inconsistency of thinking and actions), and the uniformity of emotional manifestations. Prolonged obsessional states of a complex structure must be distinguished from the manifestations of paroxysmal schizophrenia. Unlike neurotic obsessive states, they are usually accompanied by a sharply increasing anxiety, a significant expansion and systematization of the circle of obsessive associations, which acquire the character of obsessions of "special significance": previously indifferent objects, events, random remarks of others remind patients of the content of phobias, offensive thoughts and thereby acquire in their view a special, menacing significance. In such cases, it is necessary to consult a psychiatrist in order to exclude schizophrenia. It can also be difficult to differentiate between OCD and conditions with a predominance of generalized disorders, known as Gilles de la Tourette's syndrome. Tics in such cases are localized in the face, neck, upper and lower extremities and are accompanied by grimaces, opening the mouth, sticking out the tongue, and intense gesticulation.
Prolonged obsessional states of a complex structure must be distinguished from the manifestations of paroxysmal schizophrenia. Unlike neurotic obsessive states, they are usually accompanied by a sharply increasing anxiety, a significant expansion and systematization of the circle of obsessive associations, which acquire the character of obsessions of "special significance": previously indifferent objects, events, random remarks of others remind patients of the content of phobias, offensive thoughts and thereby acquire in their view a special, menacing significance. In such cases, it is necessary to consult a psychiatrist in order to exclude schizophrenia. It can also be difficult to differentiate between OCD and conditions with a predominance of generalized disorders, known as Gilles de la Tourette's syndrome. Tics in such cases are localized in the face, neck, upper and lower extremities and are accompanied by grimaces, opening the mouth, sticking out the tongue, and intense gesticulation.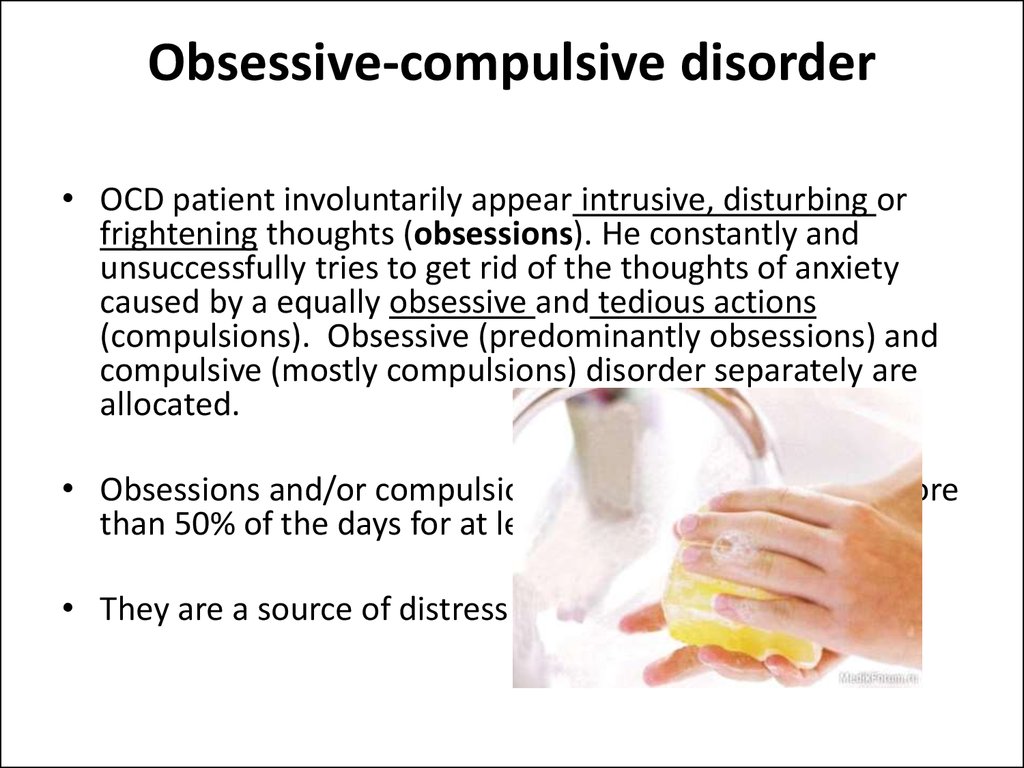 In these cases, this syndrome can be excluded by the coarseness of movement disorders characteristic of it and more complex in structure and more severe mental disorders.
In these cases, this syndrome can be excluded by the coarseness of movement disorders characteristic of it and more complex in structure and more severe mental disorders.
Genetic factors
Speaking about hereditary predisposition to OCD, it should be noted that obsessive-compulsive disorders are found in approximately 5-7% of parents of patients with such disorders. Although this figure is low, it is higher than in the general population. While the evidence for a hereditary predisposition to OCD is still uncertain, psychasthenic personality traits can be largely explained by genetic factors.
FORECAST
Approximately two-thirds of OCD patients improve within a year, more often by the end of this period. If the disease lasts more than a year, fluctuations are observed during its course - periods of exacerbations are interspersed with periods of improvement in health, lasting from several months to several years. The prognosis is worse if we are talking about a psychasthenic personality with severe symptoms of the disease, or if there are continuous stressful events in the patient's life. Severe cases can be extremely persistent; for example, a study of hospitalized patients with OCD found that three-quarters of them remained symptom-free 13 to 20 years later.
Severe cases can be extremely persistent; for example, a study of hospitalized patients with OCD found that three-quarters of them remained symptom-free 13 to 20 years later.
TREATMENT: BASIC METHODS AND APPROACHES
Despite the fact that OCD is a complex group of symptom complexes, the principles of treatment for them are the same. The most reliable and effective method of treating OCD is considered to be drug therapy, during which a strictly individual approach to each patient should be manifested, taking into account the characteristics of the manifestation of OCD, age, gender, and the presence of other diseases. In this regard, we must warn patients and their relatives against self-treatment. If any disorders similar to mental ones appear, it is necessary, first of all, to contact the specialists of the psycho-neurological dispensary at the place of residence or other psychiatric medical institutions to establish the correct diagnosis and prescribe competent adequate treatment.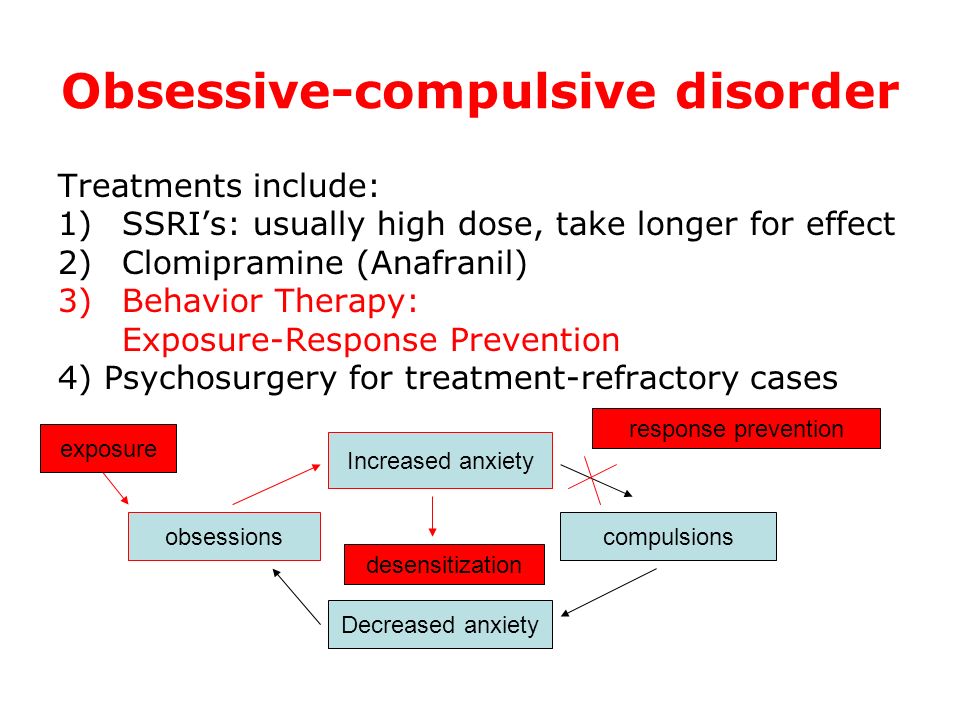 At the same time, it should be remembered that at present a visit to a psychiatrist does not threaten with any negative consequences - the infamous "accounting" was canceled more than 10 years ago and replaced by the concepts of consultative and medical care and dispensary observation.
At the same time, it should be remembered that at present a visit to a psychiatrist does not threaten with any negative consequences - the infamous "accounting" was canceled more than 10 years ago and replaced by the concepts of consultative and medical care and dispensary observation.
When treating, it must be borne in mind that obsessive-compulsive disorders often have a fluctuating course with long periods of remission (improvement). The apparent suffering of the patient often seems to call for vigorous effective treatment, but the natural course of the condition must be kept in mind in order to avoid the typical error of over-intensive therapy. It is also important to consider that OCD is often accompanied by depression, the effective treatment of which often leads to an alleviation of obsessional symptoms.
The treatment of OCD begins with an explanation of the symptoms to the patient and, if necessary, with reassurance that they are the initial manifestation of insanity (a common concern for patients with obsessions). Those suffering from certain obsessions often involve other family members in their rituals, so relatives need to treat the patient firmly, but sympathetically, mitigating the symptoms as much as possible, and not aggravating it by excessive indulgence in the sick fantasies of patients.
Those suffering from certain obsessions often involve other family members in their rituals, so relatives need to treat the patient firmly, but sympathetically, mitigating the symptoms as much as possible, and not aggravating it by excessive indulgence in the sick fantasies of patients.
Drug therapy
The following therapeutic approaches exist for the currently identified types of OCD. Of the pharmacological drugs for OCD, serotonergic antidepressants, anxiolytics (mainly benzodiazepine), beta-blockers (to stop autonomic manifestations), MAO inhibitors (reversible) and triazole benzodiazepines (alprazolam) are most often used. Anxiolytic drugs provide some short-term relief of symptoms, but should not be given for more than a few weeks at a time. If anxiolytic treatment is required for more than one to two months, small doses of tricyclic antidepressants or small antipsychotics sometimes help. The main link in the treatment regimen for OCD, overlapping with negative symptoms or ritualized obsessions, are atypical antipsychotics - risperidone, olanzapine, quetiapine, in combination with either SSRI antidepressants or other antidepressants - moclobemide, tianeptine, or with high-potency benzodiazepine derivatives ( alprazolam, clonazepam, bromazepam).
Any comorbid depressive disorder is treated with antidepressants at an adequate dose. There is evidence that one of the tricyclic antidepressants, clomipramine, has a specific effect on obsessive symptoms, but the results of a controlled clinical trial showed that the effect of this drug is insignificant and occurs only in patients with distinct depressive symptoms.
In cases where obsessive-phobic symptoms are observed within the framework of schizophrenia, intensive psychopharmacotherapy with proportional use of high doses of serotonergic antidepressants (fluoxetine, fluvoxamine, sertraline, paroxetine, citalopram) has the greatest effect. In some cases, it is advisable to connect traditional antipsychotics (small doses of haloperidol, trifluoperazine, fluanxol) and parenteral administration of benzodiazepine derivatives.
Psychotherapy
Behavioral psychotherapy
One of the main tasks of the specialist in the treatment of OCD is to establish fruitful cooperation with the patient. It is necessary to instill in the patient faith in the possibility of recovery, to overcome his prejudice against the "harm" caused by psychotropic drugs, to convey his conviction in the effectiveness of treatment, subject to the systematic observance of the prescribed prescriptions. The patient's faith in the possibility of healing must be supported in every possible way by the relatives of the OCD sufferer. If the patient has rituals, it must be remembered that improvement usually occurs when using a combination of the method of preventing a reaction with placing the patient in conditions that aggravate these rituals. Significant but not complete improvement can be expected in about two-thirds of patients with moderately heavy rituals. If, as a result of such treatment, the severity of rituals decreases, then, as a rule, the accompanying obsessive thoughts also recede. In panphobia, predominantly behavioral techniques are used to reduce sensitivity to phobic stimuli, supplemented by elements of emotionally supportive psychotherapy.
It is necessary to instill in the patient faith in the possibility of recovery, to overcome his prejudice against the "harm" caused by psychotropic drugs, to convey his conviction in the effectiveness of treatment, subject to the systematic observance of the prescribed prescriptions. The patient's faith in the possibility of healing must be supported in every possible way by the relatives of the OCD sufferer. If the patient has rituals, it must be remembered that improvement usually occurs when using a combination of the method of preventing a reaction with placing the patient in conditions that aggravate these rituals. Significant but not complete improvement can be expected in about two-thirds of patients with moderately heavy rituals. If, as a result of such treatment, the severity of rituals decreases, then, as a rule, the accompanying obsessive thoughts also recede. In panphobia, predominantly behavioral techniques are used to reduce sensitivity to phobic stimuli, supplemented by elements of emotionally supportive psychotherapy.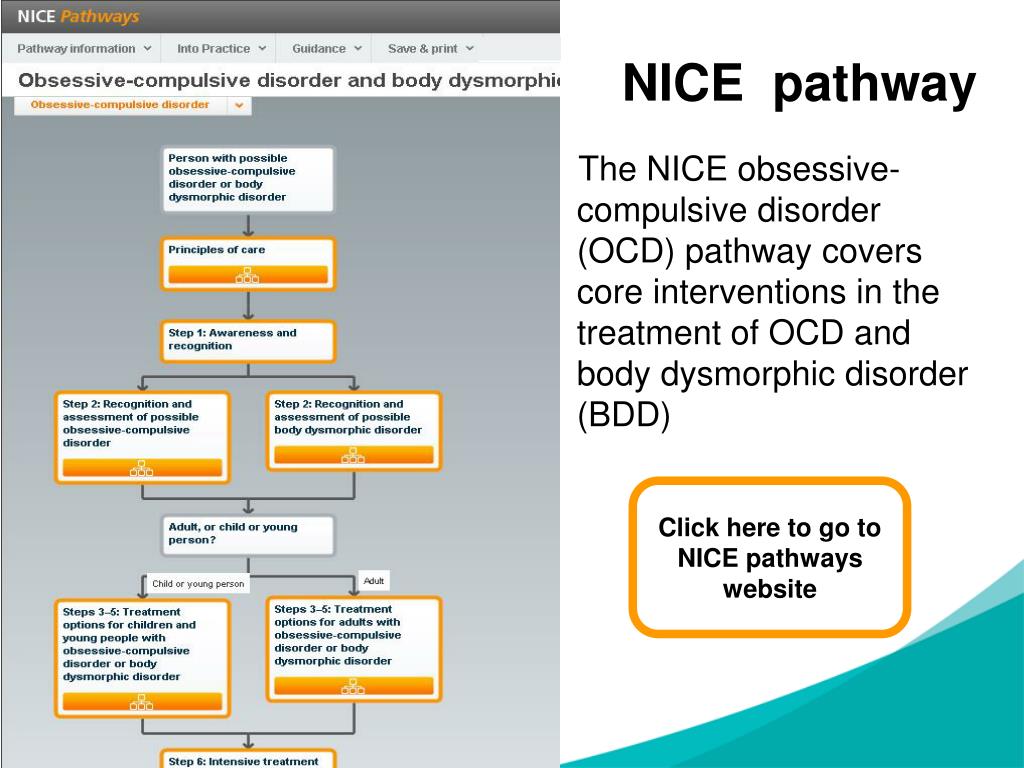 In cases where ritualized phobias predominate, along with desensitization, behavioral training is actively used to help overcome avoidant behavior. Behavioral therapy is significantly less effective for obsessive thoughts that are not accompanied by rituals. Thought-stopping has been used by some experts for many years, but its specific effect has not been convincingly proven.
In cases where ritualized phobias predominate, along with desensitization, behavioral training is actively used to help overcome avoidant behavior. Behavioral therapy is significantly less effective for obsessive thoughts that are not accompanied by rituals. Thought-stopping has been used by some experts for many years, but its specific effect has not been convincingly proven.
Social rehabilitation
We have already noted that obsessive-compulsive disorder has a fluctuating (fluctuating) course and over time the patient's condition may improve regardless of which particular methods of treatment were used. Until recovery, patients can benefit from supportive conversations that provide continued hope for recovery. Psychotherapy in the complex of treatment and rehabilitation measures for patients with OCD is aimed at both correcting avoidant behavior and reducing sensitivity to phobic situations (behavioral therapy), as well as family psychotherapy to correct behavioral disorders and improve family relationships.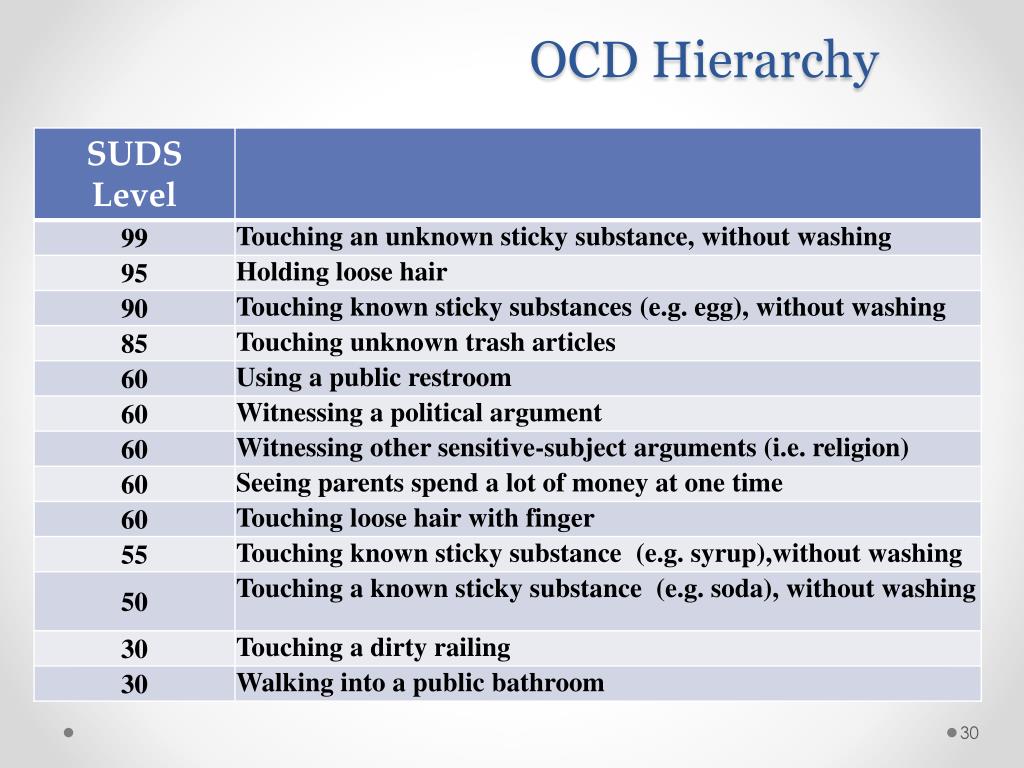 If marital problems exacerbate symptoms, joint interviews with the spouse are indicated. Patients with panphobia (at the stage of the active course of the disease), due to the intensity and pathological persistence of symptoms, need both medical and social and labor rehabilitation. In this regard, it is important to determine adequate terms of treatment - long-term (at least 2 months) therapy in a hospital with subsequent continuation of the course on an outpatient basis, as well as taking measures to restore social ties, professional skills, family relationships. Social rehabilitation is a set of programs for teaching OCD patients how to behave rationally both at home and in a hospital setting. Rehabilitation is aimed at teaching social skills to properly interact with other people, vocational training, as well as skills necessary in everyday life. Psychotherapy helps patients, especially those who experience a sense of their own inferiority, treat themselves better and correctly, master ways to solve everyday problems, and gain confidence in their strength.
If marital problems exacerbate symptoms, joint interviews with the spouse are indicated. Patients with panphobia (at the stage of the active course of the disease), due to the intensity and pathological persistence of symptoms, need both medical and social and labor rehabilitation. In this regard, it is important to determine adequate terms of treatment - long-term (at least 2 months) therapy in a hospital with subsequent continuation of the course on an outpatient basis, as well as taking measures to restore social ties, professional skills, family relationships. Social rehabilitation is a set of programs for teaching OCD patients how to behave rationally both at home and in a hospital setting. Rehabilitation is aimed at teaching social skills to properly interact with other people, vocational training, as well as skills necessary in everyday life. Psychotherapy helps patients, especially those who experience a sense of their own inferiority, treat themselves better and correctly, master ways to solve everyday problems, and gain confidence in their strength.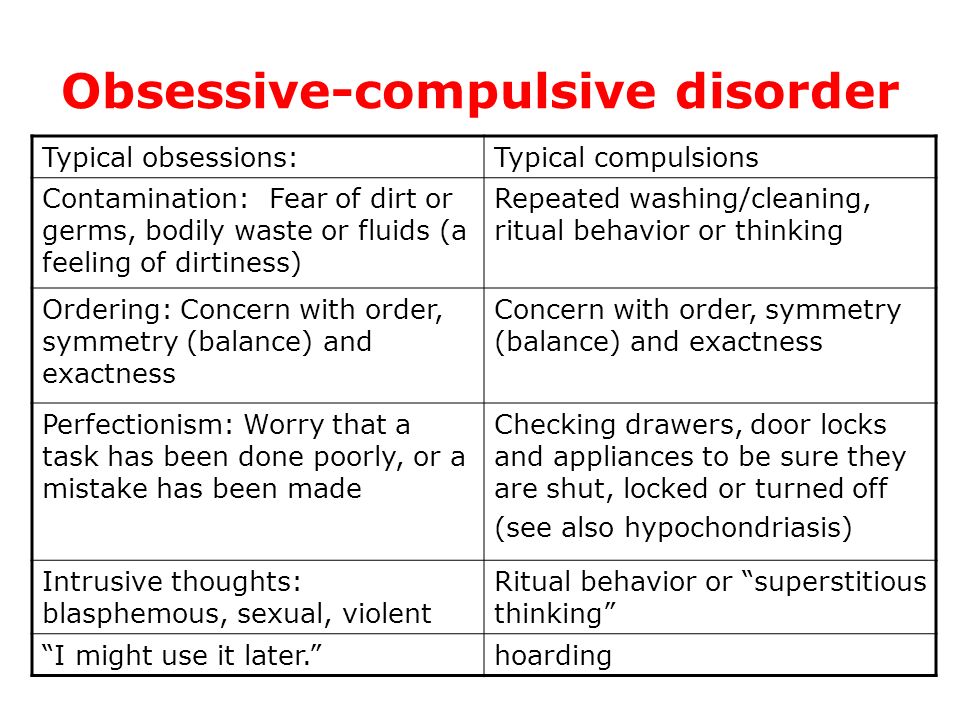
All of these methods, when used judiciously, can increase the effectiveness of drug therapy, but are not capable of completely replacing drugs. It should be noted that explanatory psychotherapy does not always help, and some patients with OCD even worsen because such procedures encourage them to think painfully and unproductively about the subjects discussed in the course of treatment. Unfortunately, science still does not know how to cure mental illness once and for all. OCD often has a tendency to recur, which requires long-term prophylactic medication.
Autism, NJ - Linking Autism and OCD
Debra G. Saltzman, Ph.D., Behavior Therapy Associates, Pennsylvania
Children diagnosed with autism spectrum disorder (ASD) have an increased risk of developing a number of anxiety disorders. In particular, obsessive-compulsive disorder and autism spectrum disorder have a high comorbidity (37% and above). Obsessive-compulsive disorder (OCD) is diagnosed when there are intrusive thoughts (unwanted, intrusive thoughts, images, or urges) that cause significant discomfort and/or compulsions (behaviors) that the person feels urged to do to reduce and/or get rid of the discomfort . obsession.
obsession.
To qualify for OCD, obsessions and/or compulsions must be time consuming or cause noticeable interference with the person's life. Common obsessions include thoughts of infection or illness, fear of harm, fear of losing control, fear of making the wrong decision, doubt that the person did something (bring my books home, turned off the light), and worry about what is happening. In the right place. Common compulsions include washing hands, checking, seeking support from parents and teachers, rereading, erasing and rewriting, repeating actions a certain number of times, saving everything, excessive showering and unpacking.
The impact of OCD on the child and family
This behavior can lead to significant interference with the child and family. Sometimes parents become prisoners of their child's OCD symptoms, doing everything they can to help their child avoid anxiety and avoid a tantrum or a nervous breakdown. Parents and caregivers often struggle to cope with other difficult behaviors, so the addition of comorbid OCD creates more and more problems.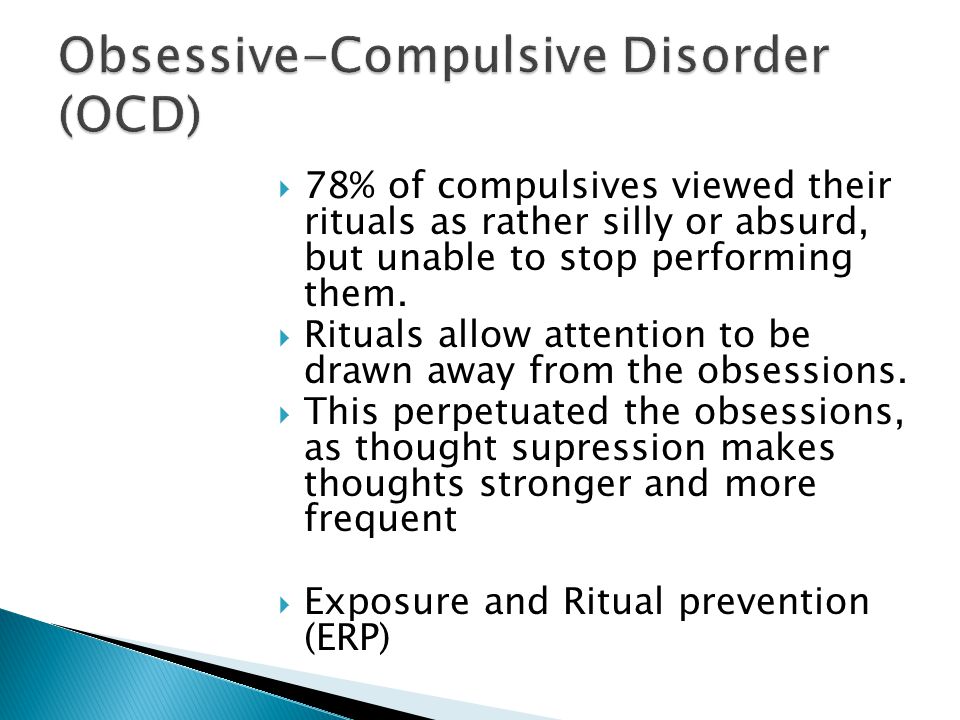 Parents, caregivers, and teachers are doing what comes naturally, which is providing confidence and planning a child's day to avoid OCD triggers. Unfortunately, reassurance and avoidance only serve to maintain OCD and lead to an increase in symptoms over time.
Parents, caregivers, and teachers are doing what comes naturally, which is providing confidence and planning a child's day to avoid OCD triggers. Unfortunately, reassurance and avoidance only serve to maintain OCD and lead to an increase in symptoms over time.
Breaking the cycle of obsessive-compulsive disorder
Treatment to reduce the symptoms of obsessive-compulsive disorder requires just the opposite: to face your fearful scenarios and prevent yourself from being ritualized, and to break the link between obsession and compulsion. This treatment is called exposure and response prevention (ERP). This is done step by step by creating a hierarchy of scary scenarios and complex situations explaining what needs to be done (both parent and child) at each stage. Of course, this requires motivation on the part of the child.
Thus, ERP will have the greatest success among people with high-functioning autism. A child with higher cognitive skills will have a better understanding of the basic functions needed for ERP.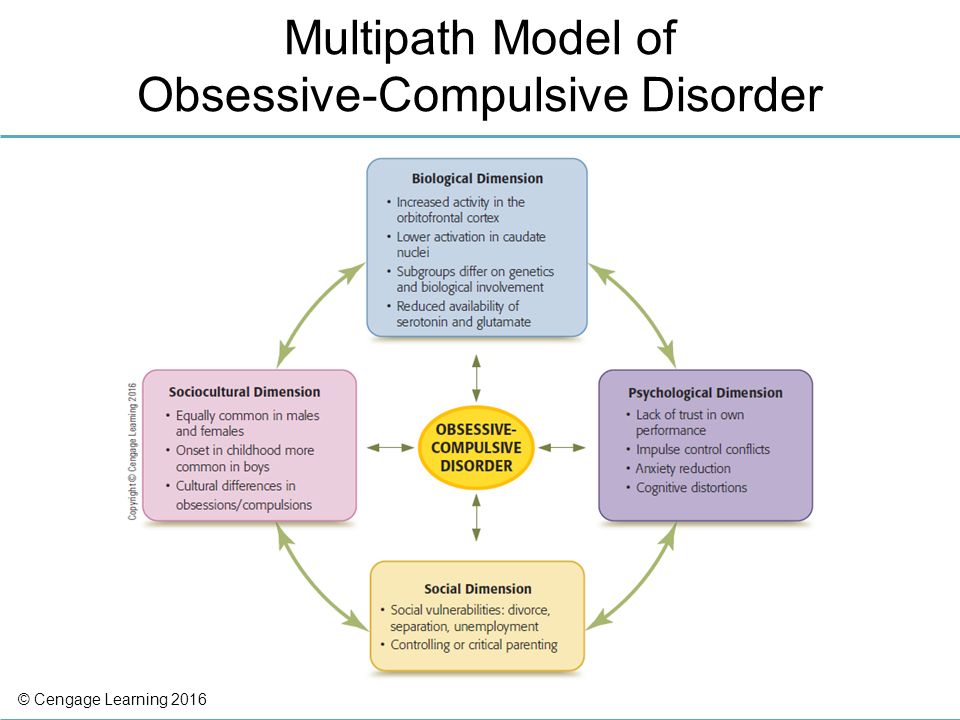 The child agrees to begin treatment that will increase his/her anxiety in the short term, knowing that eventually the anxiety (and OCD) will decrease. Investing anxiety in the short term to live a ritual-free life and no longer be a prisoner of OCD is a challenge, even for children and adults without an ASD diagnosis. The goal is to help a child with a co-diagnosis of ASD understand the benefits of treatment and increase his or her motivation to "fight the OCD monster".
The child agrees to begin treatment that will increase his/her anxiety in the short term, knowing that eventually the anxiety (and OCD) will decrease. Investing anxiety in the short term to live a ritual-free life and no longer be a prisoner of OCD is a challenge, even for children and adults without an ASD diagnosis. The goal is to help a child with a co-diagnosis of ASD understand the benefits of treatment and increase his or her motivation to "fight the OCD monster".
Problems of treatment
There are many problems in the treatment of children with a comorbid diagnosis of ASD and OCD. Motivation is perhaps one of the most difficult tasks. Taking the time to describe how OCD interferes with a child's life and feeling helpless in dealing with the OCD "bully" can help improve motivation. Parents and caregivers may need to stop giving in to OCD in order for the child to feel motivated to work on the problem. Parents who change when they enter the house to help a child who fears infection are not creating an environment for the child to see the need for change.
Knowing that motivation may be reduced, treatment of those with comorbidities may be required at a slower rate. Taking the time to make sure the child fully understands the reasons why we are "face to face with the monster" helps increase motivation. Providing smaller steps to change, which allows the child to better control the pace of treatment, can also increase motivation.
Prevention of exposure and response for people with a comorbid diagnosis of high functioning autism presents a unique challenge, but one that can be overcome. The treatment is very effective and can lead to significant changes in the life of the child and family. Understanding OKRs and the mechanisms that support OKRs are the first steps towards change.
To find mental health professionals in your area, call the Autism New Jersey Helpline at 800.4.AUTISM, [email protected], or visit our online referral database.
Recommendations
Foa, EB, & Wilson, R. (2001). Stop the obsession! New York: Bantam Books.
Stop the obsession! New York: Bantam Books.
Gillihan, S.J., Williams, M.T., Malkoon, E., Yadin, E., and Foa, E.B. (2012). Common Pitfalls in Exposure and Response Prevention (EX/RP) in OCD. Journal of Obsessive-Compulsive and Related Disorders , 1, 251-257.
Levine, A.B., Wood, J.J., Gunderson, S., Murphy, T.K., and Storch, E.A. (2011). Phenomenology of comorbid autism spectrum and obsessive-compulsive disorders in children. Journal of Developmental Disorders and Physical Disabilities , 23(6), 543-553.
Meyer S.M., Petersen L., Shendel D.E., Matthijsen M., Mortensen P.B., Morse O. (2015). Obsessive-compulsive disorder and autism spectrum disorders: longitudinal and offspring risk. PLoS ONE 10(11): e0141703. https://doi.org/10.1371/journal.pone.0141703
Russell, A., Mate-Kols, D., Anson, M., & Murphy, D. (2005). Obsessions and compulsions in Asperger's syndrome and high-functioning autism. British Journal of Psychiatry , 186(6), 525-528.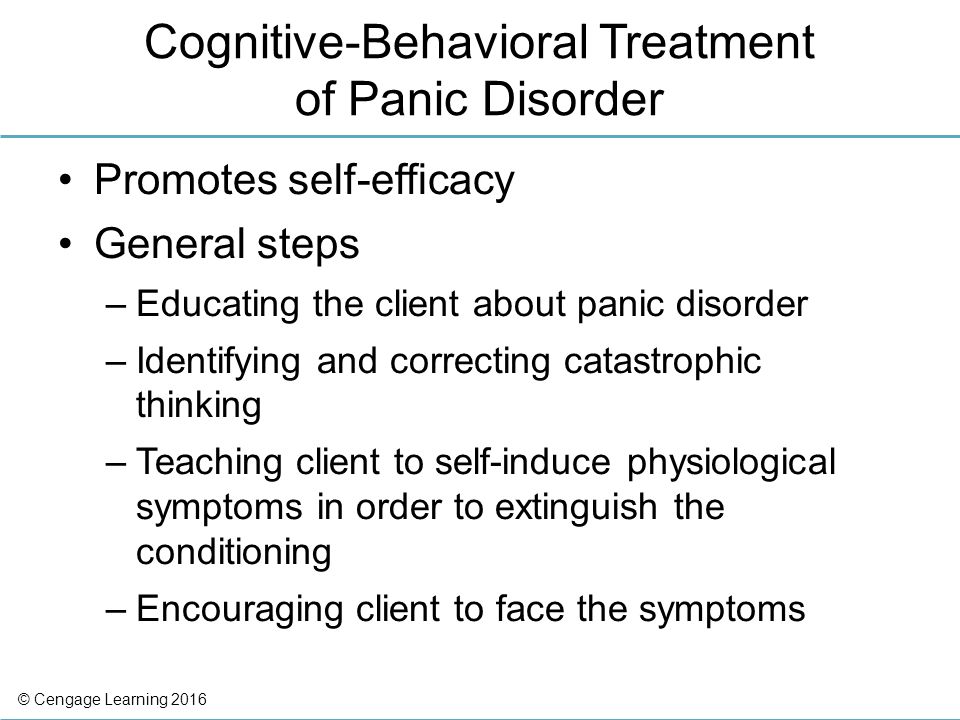
Additional Resources
Freeing Your Child from Anxiety, Revised and Updated Edition: Practical Strategies for Coping with Fears, Anxiety, and Phobias and Preparing for Life - From Toddlers to Teens
Mr. Worry: The Story of OCD
ROC workbook for clinicians, children and adolescents; Actions to Conquer, Control, and Conquer OCD
Up and Down the Hill of Anxiety: A Children's Book on Obsessive Compulsive Disorder and Its Treatment
Responding to OCD: A program that helps children and teens say "no" and tell parents to go
Debra G. Saltzman, Ph.D. is a licensed clinical psychologist at Behavior Therapy Associates, Pennsylvania. Dr. Saltzman has extensive experience in the evaluation and treatment of children, adolescents and adults. Her special interests include anxiety disorders, social skills deficits, past and present childhood sexual abuse, disruptive conduct disorders, depression, coping with trauma, obsessive-compulsive disorder, selective mutism, social phobia, and teaching parents behavior management strategies to improve a child's behavior.