Indicators of adhd
Symptoms and Diagnosis of ADHD
COVID-19: Information for parenting children with ADHD
Learn more
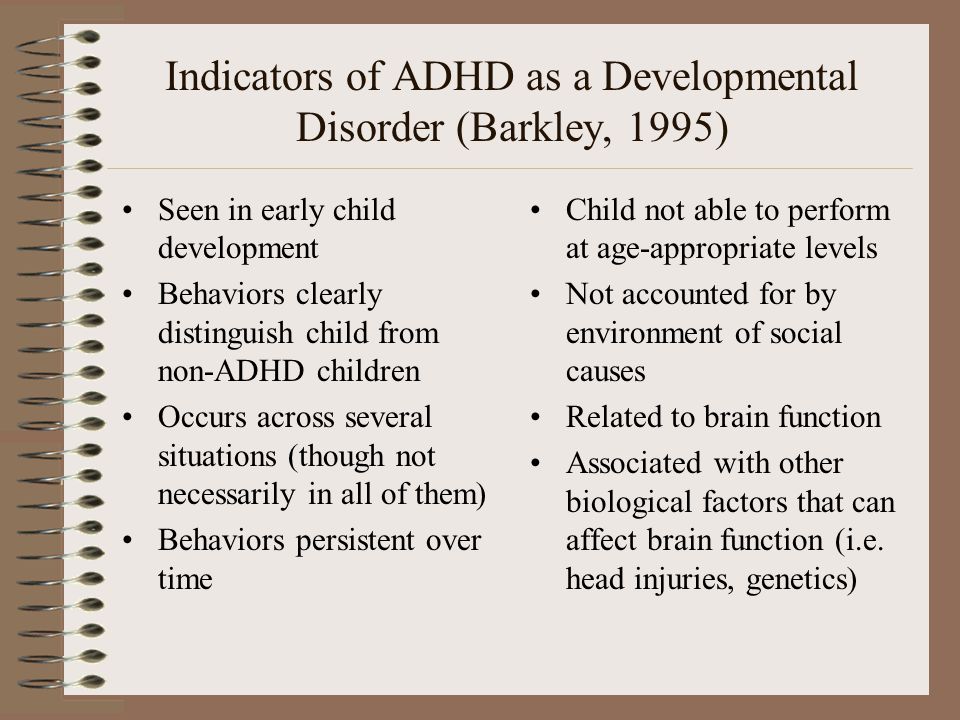
Deciding if a child has ADHD is a process with several steps. This page gives you an overview of how ADHD is diagnosed. There is no single test to diagnose ADHD, and many other problems, like sleep disorders, anxiety, depression, and certain types of learning disabilities, can have similar symptoms.
If you are concerned about whether a child might have ADHD, the first step is to talk with a healthcare provider to find out if the symptoms fit the diagnosis. The diagnosis can be made by a mental health professional, like a psychologist or psychiatrist, or by a primary care provider, like a pediatrician.
The American Academy of Pediatrics (AAP) recommends that healthcare providers ask parents, teachers, and other adults who care for the child about the child’s behavior in different settings, like at home, school, or with peers. Read more about the recommendations.
The healthcare provider should also determine whether the child has another condition that can either explain the symptoms better, or that occurs at the same time as ADHD. Read more about other concerns and conditions.
Why Family Health History is Important if Your Child has Attention and Learning Problems
How is ADHD diagnosed?
Healthcare providers use the guidelines in the American Psychiatric Association’s Diagnostic and Statistical Manual, Fifth edition (DSM-5)1, to help diagnose ADHD. This diagnostic standard helps ensure that people are appropriately diagnosed and treated for ADHD. Using the same standard across communities can also help determine how many children have ADHD, and how public health is impacted by this condition.
Here are the criteria in shortened form. Please note that they are presented just for your information. Only trained healthcare providers can diagnose or treat ADHD.
Get information and support from the National Resource Center on ADHD
DSM-5 Criteria for ADHD
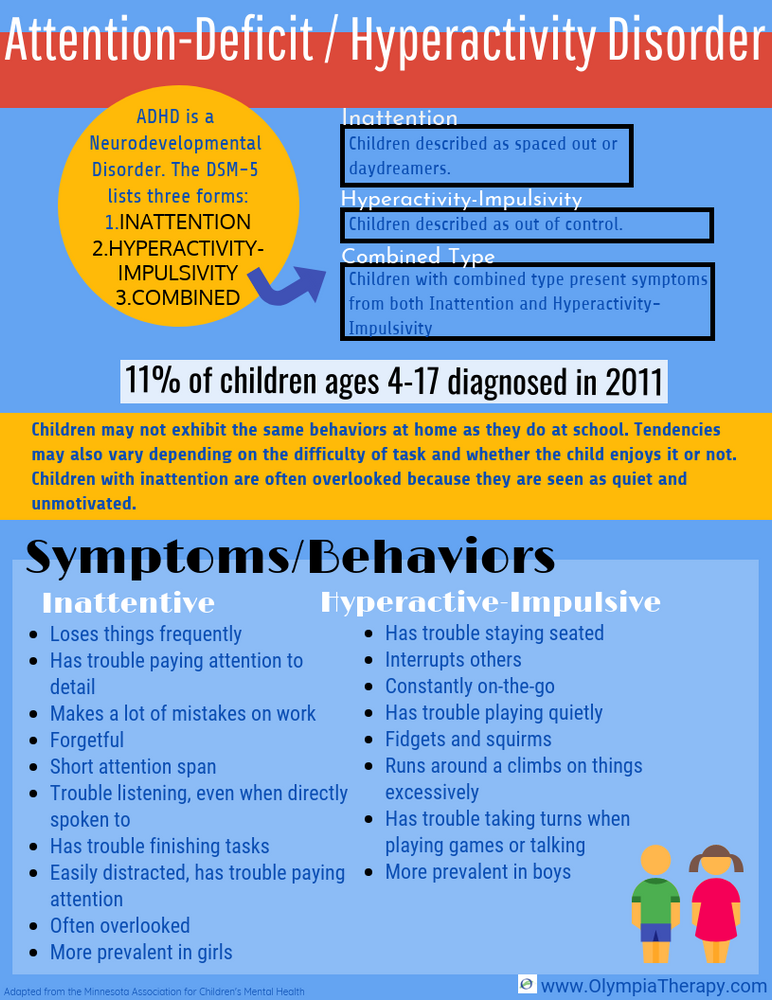
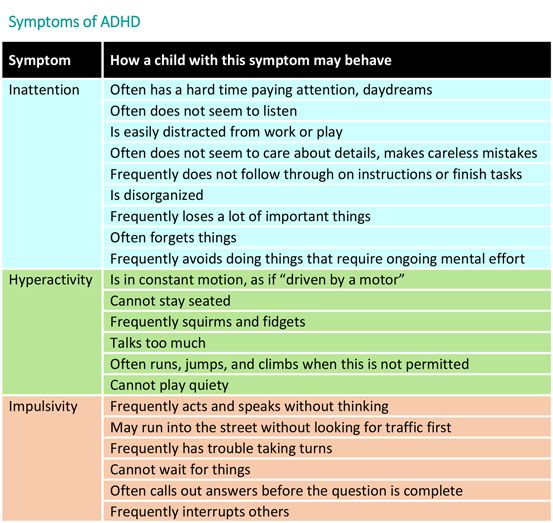
People with ADHD show a persistent pattern of inattention and/or hyperactivity–impulsivity that interferes with functioning or development:
- Inattention: Six or more symptoms of inattention for children up to age 16 years, or five or more for adolescents age 17 years and older and adults; symptoms of inattention have been present for at least 6 months, and they are inappropriate for developmental level:
- Often fails to give close attention to details or makes careless mistakes in schoolwork, at work, or with other activities.
- Often has trouble holding attention on tasks or play activities.
- Often does not seem to listen when spoken to directly.
- Often does not follow through on instructions and fails to finish schoolwork, chores, or duties in the workplace (e.g., loses focus, side-tracked).
- Often has trouble organizing tasks and activities.
- Often avoids, dislikes, or is reluctant to do tasks that require mental effort over a long period of time (such as schoolwork or homework).
- Often loses things necessary for tasks and activities (e.g. school materials, pencils, books, tools, wallets, keys, paperwork, eyeglasses, mobile telephones).
- Is often easily distracted
- Is often forgetful in daily activities.
- Often fails to give close attention to details or makes careless mistakes in schoolwork, at work, or with other activities.
- Hyperactivity and Impulsivity: Six or more symptoms of hyperactivity-impulsivity for children up to age 16 years, or five or more for adolescents age 17 years and older and adults; symptoms of hyperactivity-impulsivity have been present for at least 6 months to an extent that is disruptive and inappropriate for the person’s developmental level:
- Often fidgets with or taps hands or feet, or squirms in seat.
- Often leaves seat in situations when remaining seated is expected.
- Often runs about or climbs in situations where it is not appropriate (adolescents or adults may be limited to feeling restless).
- Often unable to play or take part in leisure activities quietly.
- Is often “on the go” acting as if “driven by a motor”.
- Often talks excessively.
- Often blurts out an answer before a question has been completed.
- Often has trouble waiting their turn.
- Often interrupts or intrudes on others (e.g., butts into conversations or games)
- Often fidgets with or taps hands or feet, or squirms in seat.
In addition, the following conditions must be met:
- Several inattentive or hyperactive-impulsive symptoms were present before age 12 years.
- Several symptoms are present in two or more settings, (such as at home, school or work; with friends or relatives; in other activities).
- There is clear evidence that the symptoms interfere with, or reduce the quality of, social, school, or work functioning.
- The symptoms are not better explained by another mental disorder (such as a mood disorder, anxiety disorder, dissociative disorder, or a personality disorder). The symptoms do not happen only during the course of schizophrenia or another psychotic disorder.
Based on the types of symptoms, three kinds (presentations) of ADHD can occur:
- Combined Presentation: if enough symptoms of both criteria inattention and hyperactivity-impulsivity were present for the past 6 months
- Predominantly Inattentive Presentation: if enough symptoms of inattention, but not hyperactivity-impulsivity, were present for the past six months
- Predominantly Hyperactive-Impulsive Presentation: if enough symptoms of hyperactivity-impulsivity, but not inattention, were present for the past six months.
Because symptoms can change over time, the presentation may change over time as well.
Diagnosing ADHD in Adults
ADHD often lasts into adulthood. To diagnose ADHD in adults and adolescents age 17 years or older, only 5 symptoms are needed instead of the 6 needed for younger children. Symptoms might look different at older ages. For example, in adults, hyperactivity may appear as extreme restlessness or wearing others out with their activity.
To diagnose ADHD in adults and adolescents age 17 years or older, only 5 symptoms are needed instead of the 6 needed for younger children. Symptoms might look different at older ages. For example, in adults, hyperactivity may appear as extreme restlessness or wearing others out with their activity.
For more information about diagnosis and treatment throughout the lifespan, please visit the websites of the National Resource Center on ADHD and the National Institutes of Mental Health.
Reference
American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, 5th edition. Arlington, VA., American Psychiatric Association, 2013.
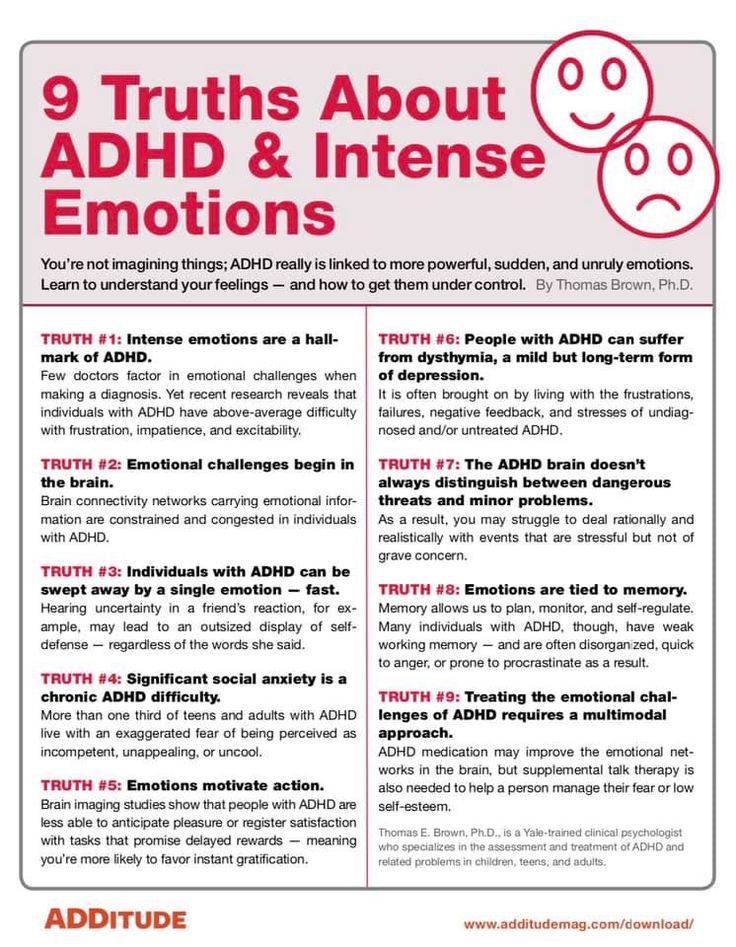
Other Concerns and Conditions with ADHD
- Behavior or Conduct Problems
- Learning Disorder
- Anxiety and Depression
- Difficult Peer Relationships
- Risk of Injuries
- Oral Health
- Health Risks
ADHD often occurs with other disorders. Many children with ADHD have other disorders as well as ADHD, such as behavior or conduct problems, learning disorders, anxiety and depression1,2.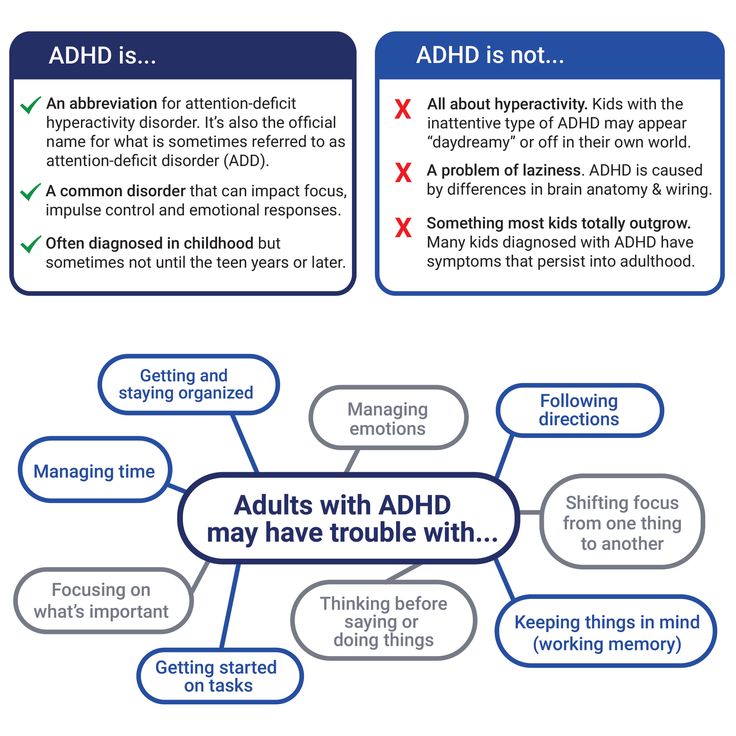
Learn about how many children with ADHD have another disorder
The combination of ADHD with other disorders often presents extra challenges for children, parents, educators, and healthcare providers. Therefore, it is important for healthcare providers to screen every child with ADHD for other disorders and problems. This page provides an overview of the more common conditions and concerns that can occur with ADHD. Talk with your healthcare provider if you have concerns about your child’s symptoms.
Every child with ADHD should be screened for other disorders and problems.
Read more about the recommendations here.
Behavior or Conduct Problems
Children occasionally act angry or defiant around adults or respond aggressively when they are upset. When these behaviors persist over time, or are severe, they can become a behavior disorder. Children with ADHD are more likely than other children to be diagnosed with a behavior disorder such as Oppositional Defiant Disorder or Conduct Disorder.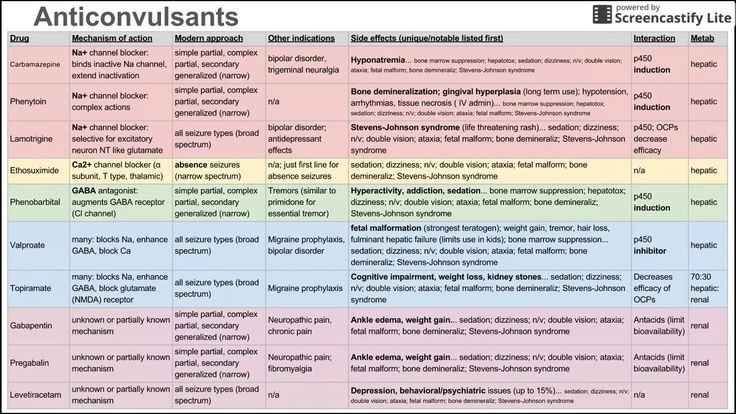
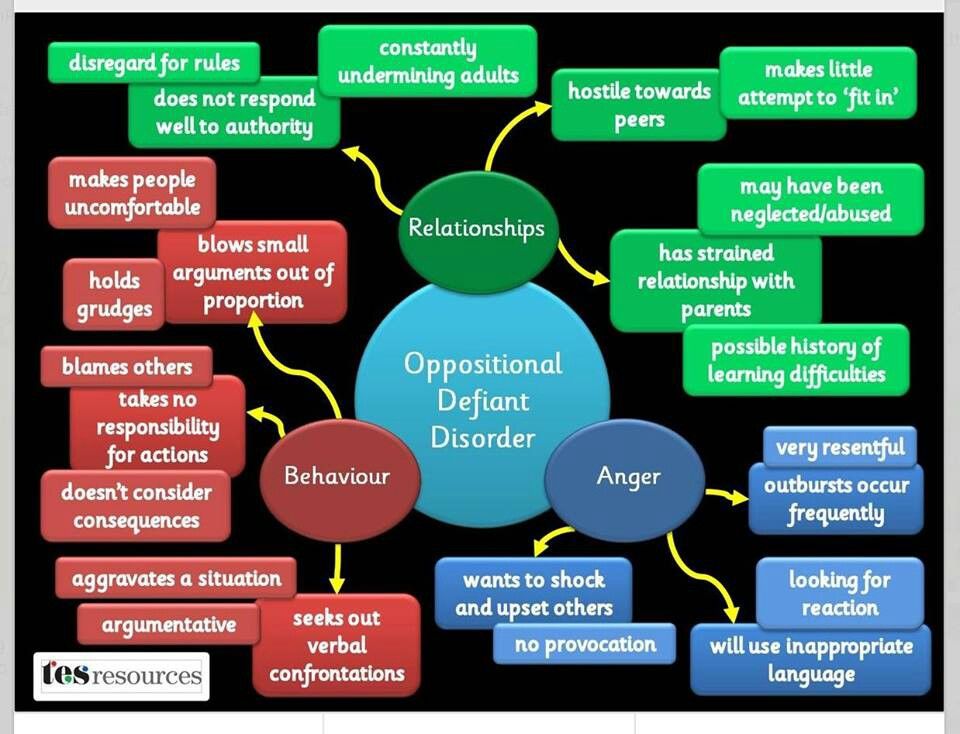
Oppositional Defiant Disorder
When children act out persistently so that it causes serious problems at home, in school, or with peers, they may be diagnosed with Oppositional Defiant Disorder (ODD). ODD is one of the most common disorders occurring with ADHD. ODD usually starts before 8 years of age, but can also occur in adolescents. Children with ODD may be most likely to act oppositional or defiant around people they know well, such as family members or a regular care provider. Children with ODD show these behaviors more often than other children their age.
Examples of ODD behaviors include
- Often losing their temper
- Arguing with adults or refusing to comply with adults’ rules or requests
- Often getting angry, being resentful, or wanting to hurt someone who they feel has hurt them or caused problems for them
- Deliberately annoying others; easily becoming annoyed with others
- Often blaming other people for their own mistakes or misbehavior
Conduct Disorder
Conduct Disorder (CD) is diagnosed when children show a behavioral pattern of aggression toward others, and serious violations of rules and social norms at home, in school, and with peers. These behaviors can lead to breaking the law and being jailed. Having ADHD makes a child more likely to be diagnosed with CD. Children with CD are more likely than other children to get injured, and to have difficulties getting along with peers.
These behaviors can lead to breaking the law and being jailed. Having ADHD makes a child more likely to be diagnosed with CD. Children with CD are more likely than other children to get injured, and to have difficulties getting along with peers.
Examples of CD behaviors include
- Breaking serious rules, such as running away, staying out at night when told not to, or skipping school
- Being aggressive in a way that causes harm, such as bullying, fighting, or being cruel to animals
- Lying and stealing, or damaging other people’s property on purpose
Treatment for disruptive behavior disorders
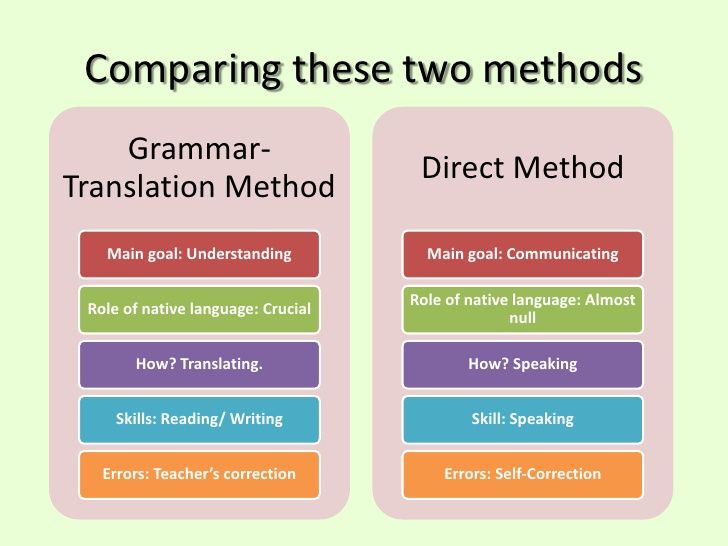
Starting treatment early is important. Treatment is most effective if it fits the needs of the child and family. The first step to treatment is to have a comprehensive evaluation by a mental health professional. Some of the signs of behavior problems, such as not following rules, are also signs of ADHD, so it is important to get a careful evaluation to see if a child has both conditions. For younger children, the treatment with the strongest evidence is behavioral parent training, where a therapist helps the parent learn effective ways to strengthen the parent-child relationship and respond to the child’s behavior. For school-age children and teens, an often-used effective treatment is combination training and therapy that includes the child, the family, and the school. Sometimes medication is part of the treatment.
For younger children, the treatment with the strongest evidence is behavioral parent training, where a therapist helps the parent learn effective ways to strengthen the parent-child relationship and respond to the child’s behavior. For school-age children and teens, an often-used effective treatment is combination training and therapy that includes the child, the family, and the school. Sometimes medication is part of the treatment.
Learn more about disruptive behavior disorders
Top of Page
Learning Disorder
Why Family Health History is Important if Your Child has Attention and Learning Problems
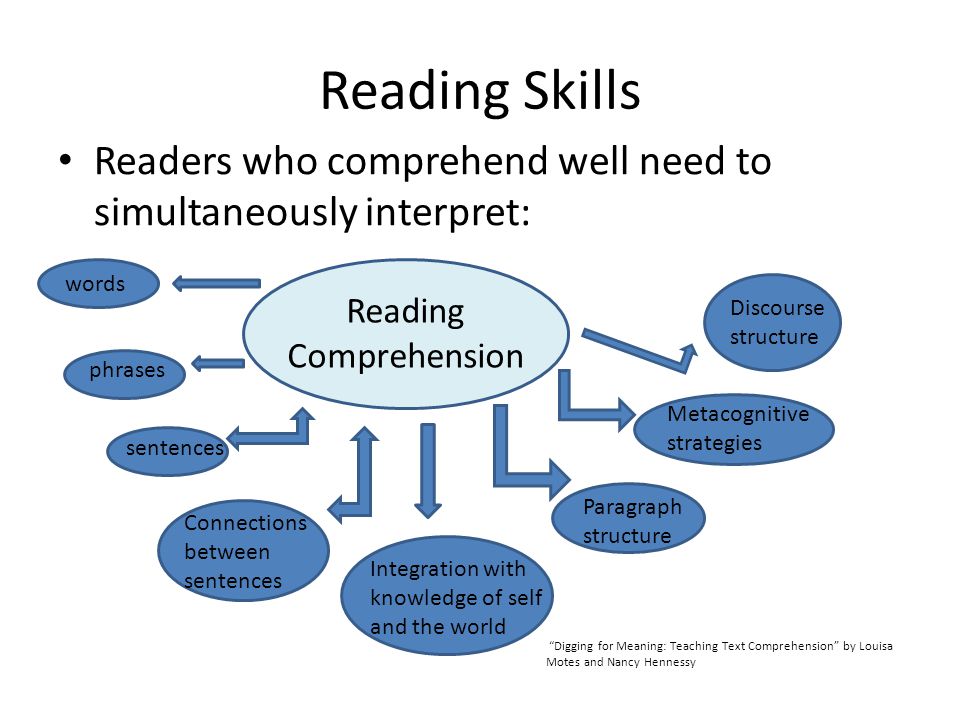
Many children with ADHD also have a learning disorder (LD). This is in addition to other symptoms of ADHD, such as difficulties paying attention, staying on task, or being organized, which can also keep a child from doing well in school.
Having a learning disorder means that a child has a clear difficulty in one or more areas of learning, even when their intelligence is not affected. Learning disorders include
Learning disorders include
- Dyslexia – difficulty with reading
- Dyscalculia – difficulty with math
- Dysgraphia – difficulty with writing
The combination of problems caused by having ADHD and LD can make it particularly hard for a child to succeed in school. Properly diagnosing each disorder is an important part of getting the right kind of help for the child.
Treatment for learning disorders
Children with learning disorders often need extra help and instruction that is specialized for them. Having a learning disorder can qualify a child for special education services in school. Because children with ADHD often have difficulty in school, the first step is a careful evaluation to see if the problems are also caused by a learning disorder. Schools usually do their own testing to see if a child needs intervention. Parents, healthcare providers, and the school can work together to find the right referrals and treatment.
Learn more about learning disorder
Top of Page
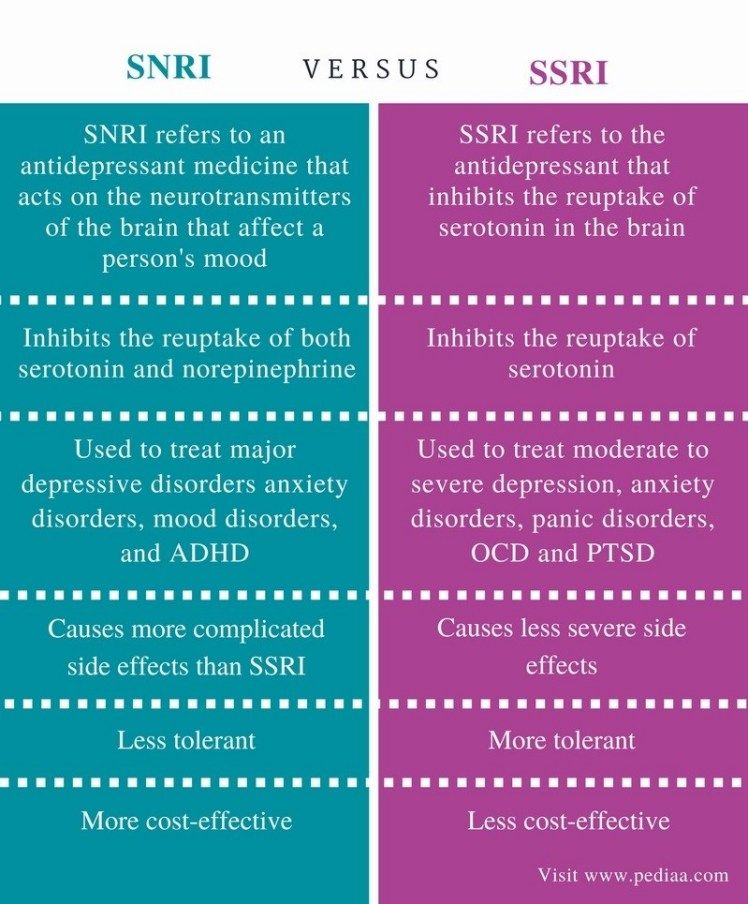
Anxiety and Depression
Anxiety
Many children have fears and worries. However, when a child experiences so many fears and worries that they interfere with school, home, or play activities, it is an anxiety disorder. Children with ADHD are more likely than those without to develop an anxiety disorder.
However, when a child experiences so many fears and worries that they interfere with school, home, or play activities, it is an anxiety disorder. Children with ADHD are more likely than those without to develop an anxiety disorder.
Examples of anxiety disorders include
- Separation anxiety – being very afraid when they are away from family
- Social anxiety – being very afraid of school and other places where they may meet people
- General anxiety – being very worried about the future and about bad things happening to them
Depression
Occasionally being sad or feeling hopeless is a part of every child’s life. When children feel persistent sadness and hopelessness, it can cause problems. Children with ADHD are more likely than children without ADHD to develop childhood depression. Children may be more likely to feel hopeless and sad when they can’t control their ADHD symptoms and the symptoms interfere with doing well at school or getting along with family and friends.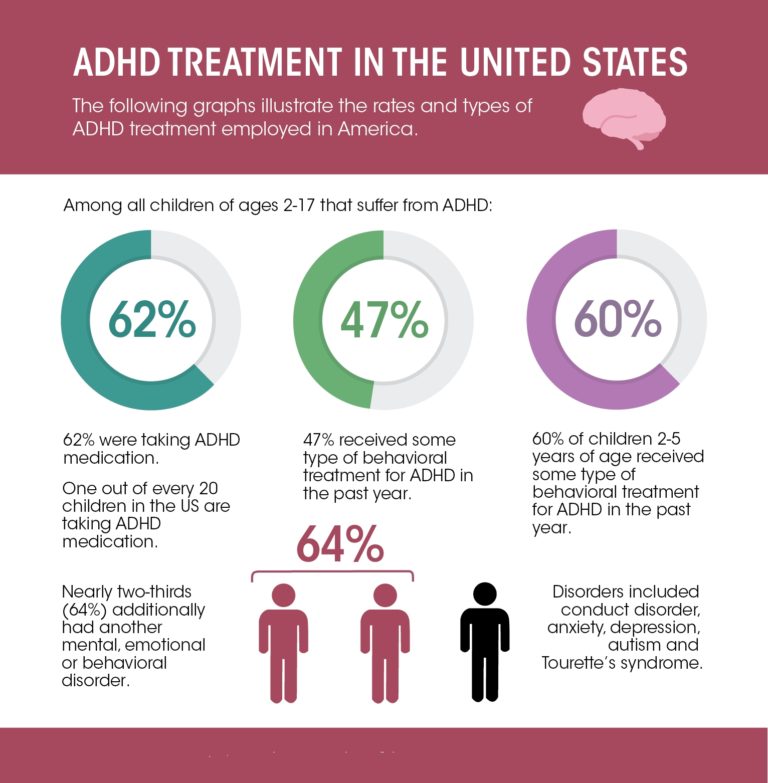
Examples of behaviors often seen when children are depressed include
- Feeling sad or hopeless a lot of the time
- Not wanting to do things that are fun
- Having a hard time focusing
- Feeling worthless or useless
Children with ADHD often have a hard time focusing on things that are not very interesting to them. Depression can make it hard to focus on things that are normally fun. Changes in eating and sleeping habits can also be a sign of depression. For children with ADHD who take medication, changes in eating and sleeping can also be side-effects from the medication rather than signs of depression. Talk with your healthcare provider if you have concerns.
Extreme depression can lead to thoughts of suicide. Read more about suicide prevention.
Treatment for anxiety and depression
The first step to treatment is to talk with a healthcare provider to get an evaluation. Some signs of depression, like having a hard time focusing, are also signs of ADHD, so it is important to get a careful evaluation to see if a child has both conditions.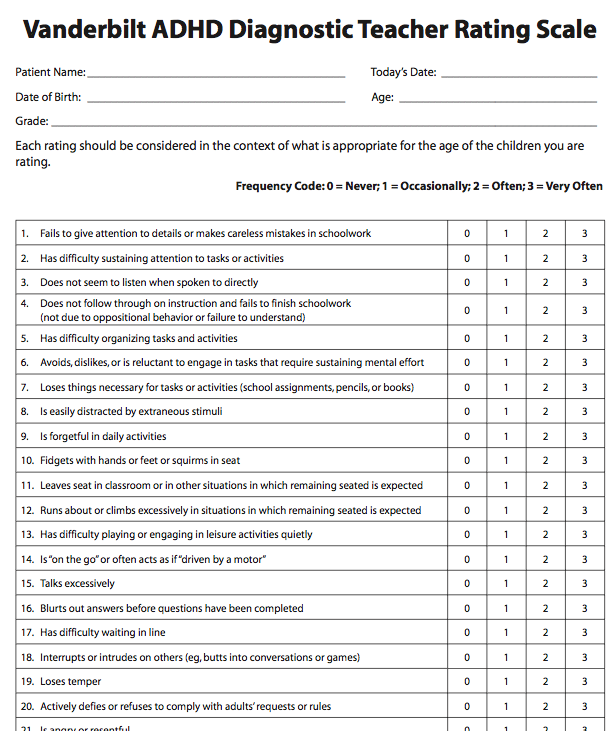 A mental health professional can develop a therapy plan that works best for the child and family. Early treatment is important, and can include child therapy, family therapy, or a combination of both. The school can also be included in therapy programs. For very young children, involving parents in treatment is very important. Cognitive behavioral therapy is one form of therapy that is used to treat anxiety or depression, particularly in older children. It helps the child change negative thoughts into more positive, effective ways of thinking. Consultation with a health provider can help determine if medication should also be part of the treatment.
A mental health professional can develop a therapy plan that works best for the child and family. Early treatment is important, and can include child therapy, family therapy, or a combination of both. The school can also be included in therapy programs. For very young children, involving parents in treatment is very important. Cognitive behavioral therapy is one form of therapy that is used to treat anxiety or depression, particularly in older children. It helps the child change negative thoughts into more positive, effective ways of thinking. Consultation with a health provider can help determine if medication should also be part of the treatment.
Learn more about anxiety and depression
Learn about the FDA’s warning when using antidepressants with young people
Top of Page
Difficult Peer Relationships
ADHD can make peer relationships or friendships very difficult. Having friends is important to children’s well-being and may be very important to their long-term development.
Although some children with ADHD have no trouble getting along with other children, others have difficulty in their relationships with their peers; for example, they might not have close friends, or might even be rejected by other children. Children who have difficulty making friends might also more likely have anxiety, behavioral and mood disorders, substance abuse, or delinquency as teenagers.
How does ADHD interfere with peer relationships?
Exactly how ADHD contributes to social problems is not fully understood. Children who are inattentive sometimes seem shy or withdrawn to their peers. Children with symptoms of impulsivity/hyperactivity may be rejected by their peers because they are intrusive, may not wait their turn, or may act aggressively. In addition, children with ADHD are also more likely than those without ADHD to have other disorders that interfere with getting along with others.
Having ADHD does not mean a child won’t have friends.
Not everyone with ADHD has difficulty getting along with others. For those children who do have difficulty, many things can be done to help them with relationships. The earlier a child’s difficulties with peers are noticed, the more successful intervention may be. Although researchers don’t have definitive answers on what works best for children with ADHD, some things parents might consider as they help their child build and strengthen peer relationships are:
For those children who do have difficulty, many things can be done to help them with relationships. The earlier a child’s difficulties with peers are noticed, the more successful intervention may be. Although researchers don’t have definitive answers on what works best for children with ADHD, some things parents might consider as they help their child build and strengthen peer relationships are:
- Pay attention to how children get along with peers. These relationships can be just as important as grades to school success.
- Regularly talk with people who play important roles in your child’s life (such as teachers, school counselors, after-school activity leaders, healthcare providers, etc.). Keep updated on your child’s social development in community and school settings.
- Involve your child in activities with other children. Talk with other parents, sports coaches and other involved adults about any progress or problems that may develop with your child.
- Peer programs can be helpful, particularly for older children and teenagers.
 Social skills training alone has not shown to be effective, but peer programs where children practice getting along with others can help. Schools and communities often have such programs available. You may want to talk to your healthcare provider and someone at your child’s school about programs that might help.
Social skills training alone has not shown to be effective, but peer programs where children practice getting along with others can help. Schools and communities often have such programs available. You may want to talk to your healthcare provider and someone at your child’s school about programs that might help.
Top of Page
Risk of Injuries
Children and adolescents with ADHD are likely to get hurt more often and more severely than peers without ADHD. Research indicates that children with ADHD are significantly more likely to
- Get injured while walking or riding a bicycle
- Have head injuries
- Injure more than one part of their body
- Be hospitalized for unintentional poisoning
- Be admitted to intensive care units or have an injury resulting in disability
More research is needed to understand why children with ADHD get injured, but it is likely that being inattentive and impulsive puts children at risk. For example, a young child with ADHD may not look for oncoming traffic while riding a bicycle or crossing the street, or may do something dangerous without thinking of the possible consequences. Teenagers with ADHD who drive may take unnecessary risks, may forget rules, or may not pay attention to traffic.
Teenagers with ADHD who drive may take unnecessary risks, may forget rules, or may not pay attention to traffic.
There are many ways to protect children from harm and keep them safe. Parents and other adults can take these steps to protect children with ADHD.
- Always have your child wear a helmet when riding a bike, skateboard, scooter, or skates. Remind children as often as necessary to watch for cars and to teach them how to be safe around traffic.
- Supervise children when they are involved in activities or in places where injuries are more likely, such as when climbing or when in or around a swimming pool.
- Keep potentially harmful household products, medications, and tools out of the reach of young children.
- Teens with ADHD are at extra risk when driving. They need to be extra careful to avoid distractions like driving with other teens in the car, talking on a cell phone, texting, eating, or playing with the radio. Like all teens, they need to avoid alcohol and drug use, and driving when drowsy.
- Parents should discuss rules of the road, why they are important to follow, and consequences for breaking them with their teens. Parents can create parent-teen driving agreements that put these rules in writing to set clear expectations and limits. Learn more about what parents can do from CDC’s Parents Are the Key campaign.
- For more injury prevention tips, visit CDC’s Injury Center.
Top of Page
Oral Health
Children with ADHD have increased risk of injury to the mouth and teeth, as well as cavities (also known as caries or tooth decay). Learn about protecting children’s oral health.
Health Risks
The core symptoms of ADHD, like impulsivity and inattention, might lead children to behave in ways that can put their health at risk or cause them to forget healthy and protective behaviors. Over time, if not addressed, these risks can lead to injury, disease, or even an earlier-than-expected death. In addition to injuries, children with ADHD are at increased risk for being overweight or having obesity. Healthy habits for children include:
Healthy habits for children include:
- Developing healthy eating habits, such as eating plenty of fruits, vegetables, and whole grains, and choosing lean protein sources.
- Participating in daily physical activity based on age.
- Limiting the amount of daily screen time from TVs, computers, phones, and other electronics.
- Getting the recommended amount of sleep each night based on age.
Learn more about protecting the health of children with ADHD
Top of Page
References
Danielson, M. L., Bitsko, R.H., Ghandour, R.M, Holbrook, J.R., Kogan, M.D., & Blumberg, S.J. (2018). Prevalence of parent-reported ADHD diagnosis and associated treatment among U.S. children and adolescents, 2016. Journal of Clinical Child & Adolescent Psychology, 47(2): 199-212.
DuPaul, G. J., Gormley, M.J., & Laracy, S.D. (2013). Comorbidity of LD and ADHD: Implications of DSM-5 for assessment and treatment. Journal of Learning Disabilities, 46(1): 43-51.
Strine, T.W., Lesesne, C.A., Okoro, C.A., McGuire, L.C., Chapman, D.P., Balluz, L.S., & Mokdad, A.H. (2006). Emotional and behavioral difficulties and impairments in everyday functioning among children with a history of attention-deficit/hyperactivity disorder. Prevention of Chronic Disorders, 3(2):A52. Epub 2006 Mar 15.
Jerome, L., Segal, A., & Habinski, L. (2006). What we know about ADHD and driving risk: A literature review, meta-analysis and critique. Journal of the Canadian Academy of Child and Adolescent Psychiatry, 15(3), 105-125.
- Children’s Mental Health
- Child Development
- Positive Parenting Tips
- Injury, Violence, and Safety
- Safe and Healthy Kids and Teens
- A-Z Index of Birth Defects, Blood Disorders & Disabilities
ADHD and Genetics | Encyclopedia of early childhood development
Philip Asherson, PhD
King's College, London, UK
(English). Translation: November 2015
Translation: November 2015
Attention-deficit/hyperactivity disorder (ADHD) is a common disorder that first appears in childhood and often continues into adulthood and is associated with the development of cognitive and functional deficits and comorbid disorders. This disorder is often familial, with multiple twin studies demonstrating a high degree of heritability for ADHD and also suggesting a predominant influence of genes on the etiology of the disease. Although such studies do not exclude the importance of environmental factors, they suggest that in most cases the latter interact with genetic factors; although exceptional external conditions such as early severe deprivation, 1 or exceptional genetic risk factors such as rare copy number variants (CNV), 2 can in some cases have a significant impact on the risk of developing the disease.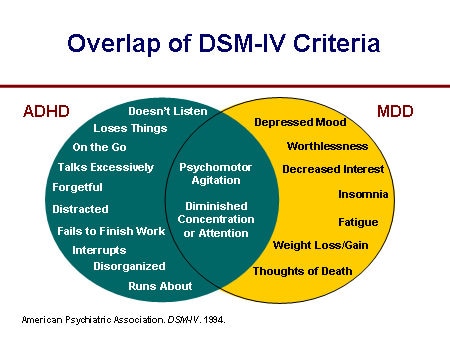 The nature of the genetic influence on the development of ADHD remains largely unknown, although it is believed to be largely determined by the additive and interactive effects of common genetic variations.
The nature of the genetic influence on the development of ADHD remains largely unknown, although it is believed to be largely determined by the additive and interactive effects of common genetic variations.
Subject
Genetic research on ADHD is relevant for two reasons. First, quantitative genetic studies allow us to explore the extent of the influence of genetic factors on ADHD and the degree of commonality of genetic variability in ADHD and its associated cognitive disorders, brain dysfunction and comorbid disorders and traits. Second, molecular genetic studies make it possible to identify specific risk factors for the development of ADHD, providing a detailed understanding of the molecular and neurobiological mechanisms involved. nine0008
Key questions
What is the genetic influence of genes on ADHD, and what mechanisms mediate their effect on behavior? How do genetic and environmental factors interact in the etiology of ADHD and associated behavioral and cognitive traits?
Recent research results
Family and twin studies give an idea of ADHD as a family disease, the risk of developing which in the closest relatives of probands with ADHD is 5-10 times higher than the population.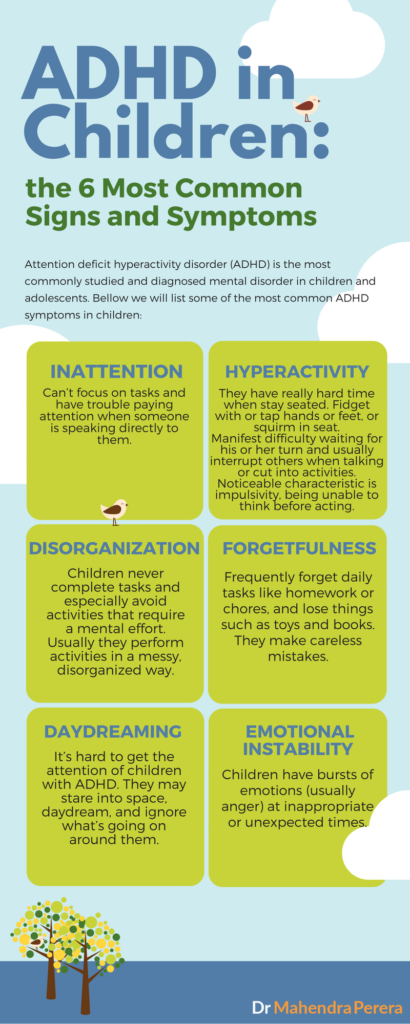 nine0014 3.4 Approximately 76% of the variance in the manifestation of ADHD is explained by genetic factors (heritability). 5 An analysis of the frequency of this syndrome among twins and sibling probands with ADHD has shown that genetics influences the level of ADHD in the population, and that, in essence, ADHD is an extreme manifestation of one or more quantitative traits. 3 Genetic factors influencing the two domains of ADHD symptoms, inattention and hyperactivity-impulsivity, overlap to a large extent but not completely, suggesting that they are based on both unique and shared genetic and neurobiological processes. nine0014 6 Other studies have examined the degree of commonality of genetic influences for ADHD and related disorders and traits. These studies have shown that ADHD, especially attention deficit symptoms, and dyslexia have common genetic factors, 7 hyperactivity-impulsivity has a genetic commonality with educational difficulties, 8 and ADHD with symptoms of autism spectrum disorders.
nine0014 3.4 Approximately 76% of the variance in the manifestation of ADHD is explained by genetic factors (heritability). 5 An analysis of the frequency of this syndrome among twins and sibling probands with ADHD has shown that genetics influences the level of ADHD in the population, and that, in essence, ADHD is an extreme manifestation of one or more quantitative traits. 3 Genetic factors influencing the two domains of ADHD symptoms, inattention and hyperactivity-impulsivity, overlap to a large extent but not completely, suggesting that they are based on both unique and shared genetic and neurobiological processes. nine0014 6 Other studies have examined the degree of commonality of genetic influences for ADHD and related disorders and traits. These studies have shown that ADHD, especially attention deficit symptoms, and dyslexia have common genetic factors, 7 hyperactivity-impulsivity has a genetic commonality with educational difficulties, 8 and ADHD with symptoms of autism spectrum disorders. 9 It is believed that these symptoms manifest the pleiotropic effect of genes that affect several disorders simultaneously. nine0008
9 It is believed that these symptoms manifest the pleiotropic effect of genes that affect several disorders simultaneously. nine0008
Recently, two familial influences on cognition have been identified through overlapping familial influences on ADHD and cognitive impairment. 10 A more significant factor explaining 85% of ADHD familial variance pooled all familial influences on mean reaction time and reaction time variability on accelerated reaction time tasks, while a less significant factor explaining 12.5% of ADHD familial variance pooled all familial influences on errors resulting from skipping an action, and 60% of familial influences on errors resulting from violation of instructions in tasks go/no-go task .* In addition, cognitive factors were found to be independent of genetic influences common to ADHD and IQ. 11 Thus, these two cognitive factors appear to be indicators of most familial influences on ADHD, and are thought to be due mainly to genetic factors.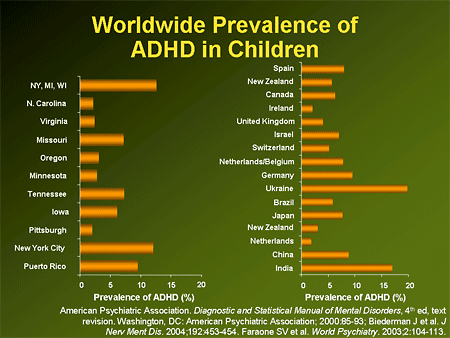 As such, there is currently a need for further study of the problem to describe the genetic factors that underlie these two familial cognitive factors and the neurobiological processes involved, and whether these factors are a link between genetic influences and behavior or they are the result of the pleiotropic action of genes. nine0008
As such, there is currently a need for further study of the problem to describe the genetic factors that underlie these two familial cognitive factors and the neurobiological processes involved, and whether these factors are a link between genetic influences and behavior or they are the result of the pleiotropic action of genes. nine0008
Molecular genetic research on ADHD began with association studies of candidate genes in the mid-1990s. Associations were first found with variants of the dopamine receptor D4 (DRD4) genes of the dopamine transporter (DAT1). Then came the association of ADHD with a microsatellite marker near the dopamine receptor D5 (DRD5) gene. Numerous replicated studies have been conducted since then, but only a small proportion have independently reproduced results. However, a meta-analysis of the available data supports an association with DRD4 and DRD5, which remains significant at the genome-wide level in the study by Li et al.0014 12 although there are several potential sources of heterogeneity that could explain this.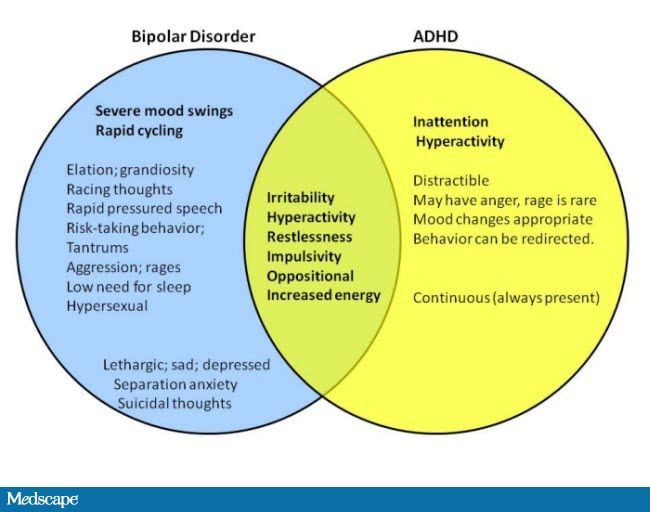 These include specific association with ADHD that is not comorbid with conduct disorder, 13 association with specific haplotypes (certain sets of linked genetic variants), 14.15 and interaction with environmental variables such as maternal smoking during pregnancy. 16-18 The results of these candidate gene studies are important because they provide the first direct evidence that neurotransmission regulatory genes, namely dopamine regulators, directly affect the risk of developing ADHD, and because they confirm the hypothesis put forward earlier, according to which suggested that the rapid and noticeable effect of stimulants on ADHD symptoms depends on the change in the availability of dopamine at neuronal synapses under the influence of these stimulants. nine0008
These include specific association with ADHD that is not comorbid with conduct disorder, 13 association with specific haplotypes (certain sets of linked genetic variants), 14.15 and interaction with environmental variables such as maternal smoking during pregnancy. 16-18 The results of these candidate gene studies are important because they provide the first direct evidence that neurotransmission regulatory genes, namely dopamine regulators, directly affect the risk of developing ADHD, and because they confirm the hypothesis put forward earlier, according to which suggested that the rapid and noticeable effect of stimulants on ADHD symptoms depends on the change in the availability of dopamine at neuronal synapses under the influence of these stimulants. nine0008
There have been many studies of other candidate genes, focusing mainly on the dopamine, serotonin and norepinephrine systems. Based on a meta-analysis of these works in a recent review by Gizer et al.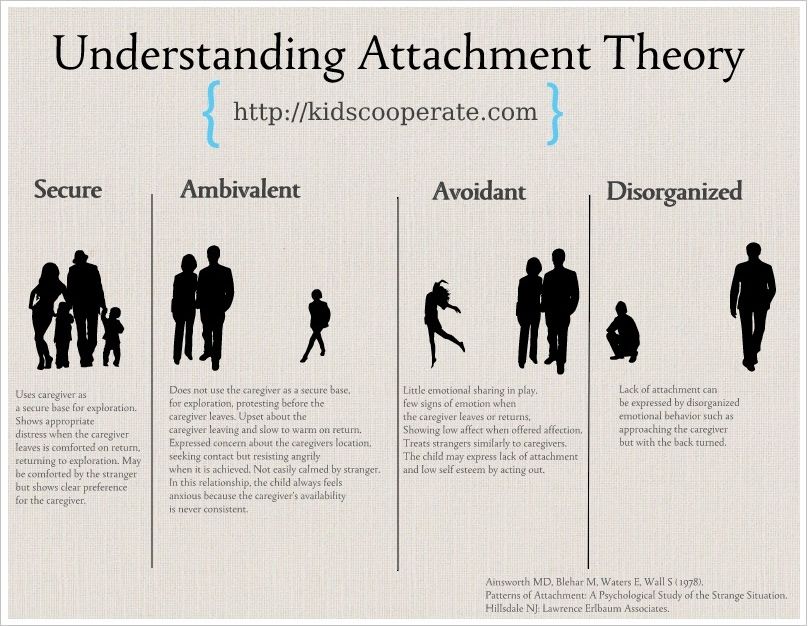 , 19 there are significant associations for several genes (DRD4, DAT1, DRD5, DBH, ADRA2A, 5HTT, TPh3, MAOA, and SNAP25). An earlier estimate of the overall effect size for the most consistently reproducible genetic studies was about 3.3% of the variance due to the combined contribution of the above genes, which explains 4.3% of the total genetic variability in ADHD, which has a heritability rate of 76%. nine0014 20 More work is certainly needed to explain the rest of the genetic influence on ADHD.
, 19 there are significant associations for several genes (DRD4, DAT1, DRD5, DBH, ADRA2A, 5HTT, TPh3, MAOA, and SNAP25). An earlier estimate of the overall effect size for the most consistently reproducible genetic studies was about 3.3% of the variance due to the combined contribution of the above genes, which explains 4.3% of the total genetic variability in ADHD, which has a heritability rate of 76%. nine0014 20 More work is certainly needed to explain the rest of the genetic influence on ADHD.
In subsequent studies, the single nucleotide polymorphism (SNP) panel method was successfully used, which allows the genotyping of genetically informative markers throughout the human genome. Depending on density, SNP panels can cover 80% or more of the common genetic variants. In the case of ADHD, it remains only to establish associations at the genome level, since not a single NP (SNP) has yet been found, the significance of which would reach the genome-wide level.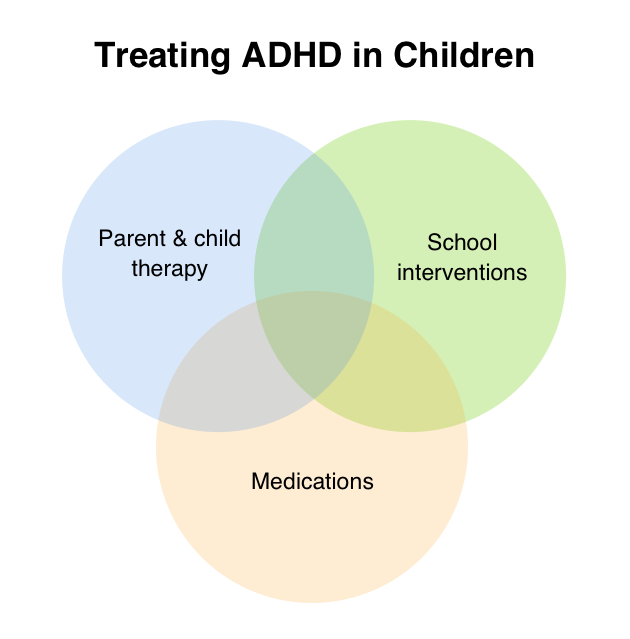 The problem is that due to the very large number of independent haplotypes (correlated sequences of correlated genetic variability) at the generally accepted significance level of 0.05 - 0.001, a lot of random associations of OP will be revealed. As a result, in order to compensate for the high frequency of “false alarms” when identifying initial associations in genome-wide analysis, it is recommended to use higher significance levels (in the region of 5 x 10 -8 ). 21 Since in almost all cases of association of individual alleles with the development of common multifactorial diseases, the increase in risk is small and the odds ratio is about 1.1 - 1.4 or less, a genome-wide study requires a sample of 12,000 or more individuals in order to reliably identify multiple associated OPs. The first PPA in the study of ADHD included the analysis of 438,784 EPs in 958 parent-proband triplets with a combined type of ADHD. No genes were found with a medium or large effect, 22 and none of the associations reached genome-wide significance.
The problem is that due to the very large number of independent haplotypes (correlated sequences of correlated genetic variability) at the generally accepted significance level of 0.05 - 0.001, a lot of random associations of OP will be revealed. As a result, in order to compensate for the high frequency of “false alarms” when identifying initial associations in genome-wide analysis, it is recommended to use higher significance levels (in the region of 5 x 10 -8 ). 21 Since in almost all cases of association of individual alleles with the development of common multifactorial diseases, the increase in risk is small and the odds ratio is about 1.1 - 1.4 or less, a genome-wide study requires a sample of 12,000 or more individuals in order to reliably identify multiple associated OPs. The first PPA in the study of ADHD included the analysis of 438,784 EPs in 958 parent-proband triplets with a combined type of ADHD. No genes were found with a medium or large effect, 22 and none of the associations reached genome-wide significance.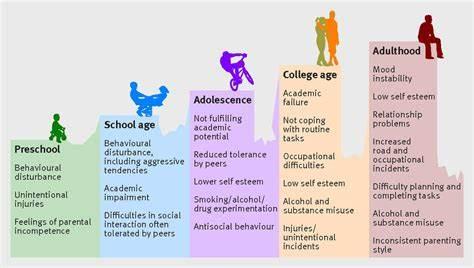 However, a study of a group of 51 candidate genes, mainly related to the dopamine, norepinephrine, and serotonin neurotransmitter systems, revealed a significant group association of the analyzed OPs. Similar results were subsequently obtained in an analysis using PPA data from several studies.
However, a study of a group of 51 candidate genes, mainly related to the dopamine, norepinephrine, and serotonin neurotransmitter systems, revealed a significant group association of the analyzed OPs. Similar results were subsequently obtained in an analysis using PPA data from several studies.
Of particular interest is the cadherin gene (CDh23), which has been found to be associated with ADHD in several PPAs and also lies within the only region that has reached the level of genome-wide significance according to a meta-analysis study of ADHD linkage groups. nine0014 23-25 These and other findings from PPA suggest that genes involved in cell division, cell adhesion and neuronal migration and plasticity may also influence the risk of developing ADHD. 26
Overall, much work remains to be done to characterize the specific genetic factors that explain the high heritability of this disorder. However, this is a common occurrence in the study of widespread disorders, and several possible explanations for the so-called "dark matter" of heredity have been put forward. Possible causes include: numerous genes with very small individual effects; genetic heterogeneity, when many genes and (allelic) variants in genes are responsible for the risk of developing a disease; a high degree of interaction between genes and the environment and etiological heterogeneity. In addition, we still do not understand the contribution of copy number variations (CNVs) or other rare genetic variations to ADHD, although recent evidence suggests that in a few cases CNVs may be the primary cause of the disorder. nine0014 2
Possible causes include: numerous genes with very small individual effects; genetic heterogeneity, when many genes and (allelic) variants in genes are responsible for the risk of developing a disease; a high degree of interaction between genes and the environment and etiological heterogeneity. In addition, we still do not understand the contribution of copy number variations (CNVs) or other rare genetic variations to ADHD, although recent evidence suggests that in a few cases CNVs may be the primary cause of the disorder. nine0014 2
Finally, attention in most genetic studies has turned to the identification of intermediate phenotypes - neurobiological indicators that mediate the influence of genes on ADHD and are more closely associated with them. For example, as shown in several fMRI studies, for a number of traits, the association with individual genetic variants has a statistical effect of a larger size. 27.28 If a similar state of affairs were found for cognitive variables sharing a common genetic variability with ADHD, then genetic studies of intermediate phenotypes would identify genetic variants associated with ADHD. Research on intermediate phenotypes should focus primarily on the processes underlying two familial cognitive factors, which are expressed in impaired functioning resulting in slower and unstable reaction times, and increased skipping and instruction errors in performance of cognitive assessment tasks. functions, 10 because these cognitive impairments in ADHD are primarily associated with genetic factors.
Research on intermediate phenotypes should focus primarily on the processes underlying two familial cognitive factors, which are expressed in impaired functioning resulting in slower and unstable reaction times, and increased skipping and instruction errors in performance of cognitive assessment tasks. functions, 10 because these cognitive impairments in ADHD are primarily associated with genetic factors.
Interestingly, the most commonly reproducible association with cognitive function criteria in ADHD is a negative association between cognitive function and the DRD4 allele responsible for ADHD risk. Among children with ADHD, the DRD4-7R seven repeat allele associated with a high risk of ADHD is associated with less cognitive impairment than alleles that do not increase the risk of ADHD. nine0014 29 The same unexpected results were obtained for the ZNF804A gene and schizophrenia. 30 It is possible that this pattern of association may be inherent in various neuropsychiatric disorders.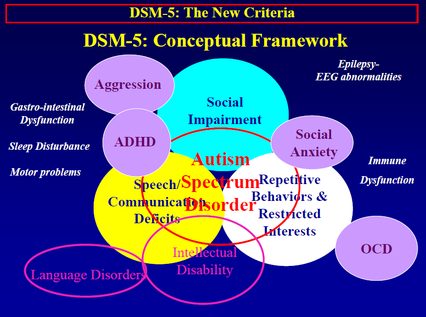 These data suggest that cognition points to an important source of heterogeneity, with the less impaired group showing a distinct mechanism of molecular pathogenesis.
These data suggest that cognition points to an important source of heterogeneity, with the less impaired group showing a distinct mechanism of molecular pathogenesis.
Unexplored areas
Going forward, both common and rare genetic variants responsible for the heritability of ADHD need to be identified using very large sample sizes and whole genome sequencing technologies. Neuroscience research needs to focus on measures that are genetically correlated with ADHD and use genetic association data to determine the nature of the cognitive, neuronal, and cellular processes that mediate genetic risk and behavior. Genetic research on ADHD in adults is just beginning, but it is expected that some genetic factors will be found that are responsible for the persistence and remission of the disorder during the transition years from childhood to adulthood. Finally, more research is needed to identify environmental risks that accompany or interact with genetic risk for developing ADHD.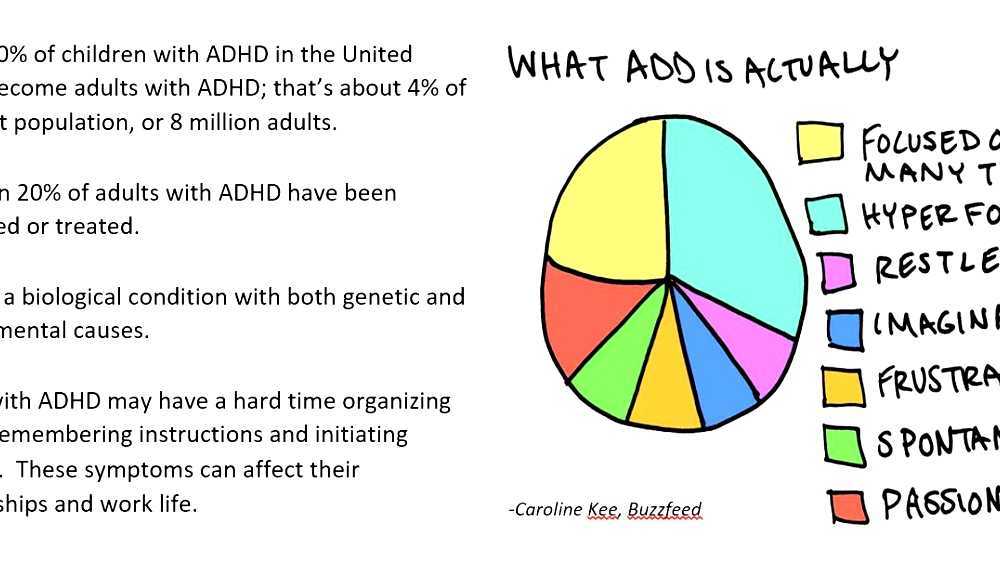 nine0008
nine0008
Conclusions
ADHD is a highly inherited disorder that begins in childhood and often continues into adulthood. Quantitative genetic studies help us understand the etiological links that exist between ADHD and comorbid personality disorders, as well as reveal the cognitive processes that mediate between genetic influences and behavior. Further research is needed to understand the processes underlying ADHD-associated cognitive deficits, manifested in reaction time and errors of skipping action and instruction violations. In the etiology of ADHD, genes encoding the dopamine system, in particular DRD4 and DRD5, play a role, as well as other genes that regulate neurotransmission and development of the nervous system, such as SNAP-25 and CDh23, as evidenced by the PPA results. Previous studies have identified rare copy number variations as a major risk factor for ADHD, but they appear to affect only a few cases. Further research is needed to explain the dark matter of heritability by linking it to genetic variations associated with ADHD.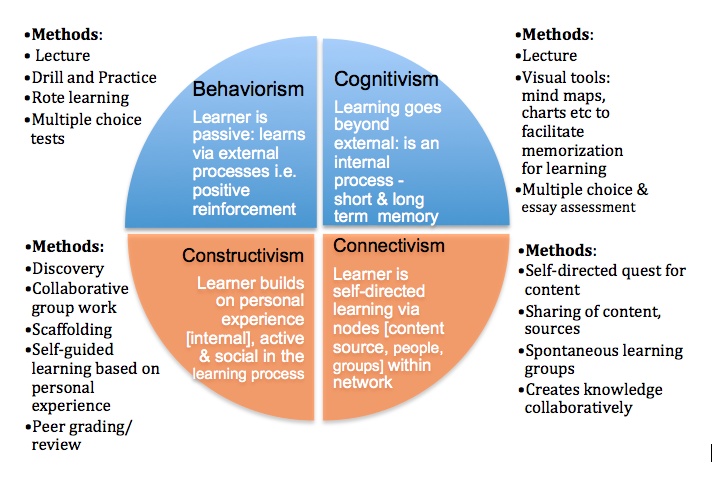 nine0008
nine0008
Recommendations
Studies of families, twins, and adoptive relatives have had a significant impact on the perception of ADHD, and this, in turn, has influenced clinical decision making. We know that heredity plays a significant role in this disorder, and that genetic influences are responsible for the stability of ADHD over time. In addition, genetic studies have helped to understand the development of comorbid disorders. In the future, research will use genetic data to identify subgroups of different etiologies in order to improve the prediction of clinical outcome and develop new strategies for targeted intervention to treat this disorder and prevent its progression during adulthood. The development of such strategies is necessary because of the significant personal and social costs associated with ADHD, including problems with education and employment, a high incidence of accidents, and a high risk of developing anxiety, depression, drug and alcohol addictions, and antisocial behavior. nine0008
nine0008
Literature
- Stevens SE, Sonuga-Barke EJ, Kreppner JM, Beckett C, Castle J, Colvert E, Groothues C, Hawkins A, Rutter M. Inattention/overactivity following early severe institutional deprivation: presentation and associations in early adolescence. Journal of Abnormal Child Psychology 2008;36(3):385-98.
- Elia J, Gai X, Xie HM, Perin JC, Geiger E, Glessner JT, D'arcy M, deBerardinis R, Frackelton E, Kim C, Lantieri F, Muganga BM, Wang L, Takeda T, Rappaport EF, Grant SF , Berrettini W, Devoto M, Shaikh TH, Hakonarson H, White PS. Rare structural variants found in attention-deficit hyperactivity disorder are preferentially associated with neurodevelopmental genes. nine0054 Molecular Psychiatry 2010;15(6):637-46.
- Chen W, Zhou K, Sham P, Franke B, Kuntsi J, Campbell D, Fleischman K, Knight J, Andreou P, Arnold R, Altink M, Boer F, Boholst MJ, Buschgens C, Butler L, Christiansen H, Fliers E, Howe-Forbes R, Gabriëls I, Heise A, Korn-Lubetzki I, Marco R, Medad S, Minderaa R, Müller UC, Mulligan A, Psychogiou L, Rommelse N, Sethna V, Uebel H, McGuffin P, Plomin R , Banaschewski T, Buitelaar J, Ebstein R, Eisenberg J, Gill M, Manor I, Miranda A, Mulas F, Oades RD, Roeyers H, Rothenberger A, Sergeant J, Sonuga-Barke E, Steinhausen HC, Taylor E, Thompson M , Faraone SV, Asherson P.
 DSM-IV combined type ADHD shows familial association with sibling trait scores: a sampling strategy for QTL linkage. nine0054 American Journal of Medical Genetic Part B-Neuropsychiatric Genetic 2008;147B(8): 1450-60.
DSM-IV combined type ADHD shows familial association with sibling trait scores: a sampling strategy for QTL linkage. nine0054 American Journal of Medical Genetic Part B-Neuropsychiatric Genetic 2008;147B(8): 1450-60. - Faraone SV, Biederman J, Monuteaux MC. Toward guidelines for pedigree selection in genetic studies of attention deficit hyperactivity disorder. Genetic Epidemiology 2000;18(1):1-16.
- Faraone SV, Perlis RH, Doyle AE, Smoller JW, Goralnick JJ, Holmgren MA, Sklar P. Molecular genetics of attention-deficit/hyperactivity disorder. Biological Psychiatry 2005;57(11):1313-23.
- McLoughlin G, Ronald A, Kuntsi J, Asherson P, Plomin R. Genetic support for the dual nature of attention deficit hyperactivity disorder: substantial genetic overlap between the inattentive and hyperactive-impulsive components. Journal of Abnormal Child Psychology 2007;35(6):999-1008.
- Paloyelis Y, Rijsdijk F, Wood AC, Asherson P, Kuntsi J.
 The genetic association between ADHD symptoms and reading difficulties: The role of inattentiveness and IQ. nine0054 Journal of Abnormal Child Psychology 2010;38(8):1083-95.
The genetic association between ADHD symptoms and reading difficulties: The role of inattentiveness and IQ. nine0054 Journal of Abnormal Child Psychology 2010;38(8):1083-95. - Wood AC, Rijsdijk F, Asherson P, Kuntsi J. Hyperactive-impulsive symptom scores and oppositional behaviors reflect alternate manifestations of a single liability. Behavior Genetics 2009;39(5):447-60.
- Ronald A, Simonoff E, Kuntsi J, Asherson P, Plomin R. Evidence for overlapping genetic influences on autistic and ADHD behaviors in a community twin sample. Journal of Child Psychology and Psychiatry 2008;49(5):535-42.
- Kuntsi J, Wood AC, Rijsdijk F, Johnson KA, Andreou P, Albrecht B, Arias-Vasquez A, Buitelaar JK, McLoughlin G, Rommelse NN, Sergeant JA, Sonuga-Barke EJ, Uebel H, van der Meere JJ, Banaschewski T, Gill M, Manor I, Miranda A, Mulas F, Oades RD, Roeyers H, Rothenberger A, Steinhausen HC, Faraone SV, Asherson P. Separation of cognitive impairments in attention hyper deficitactivity disorder into two familial factors.
 Archives of General Psychiatry 2010;67(11):1159-67.
Archives of General Psychiatry 2010;67(11):1159-67. - Wood AC, Rijsdijk F, Johnson KA, Andreou P, Albrecht B, Arias-Vasquez A, Buitelaar JK, McLoughlin G, Rommelse NN, Sergeant JA, Sonuga-Barke EJ, Uebel H, van der Meere JJ, Banaschewski T, Gill M, Manor I, Miranda A, Mulas F, Oades RD, Roeyers H, Rothenberger A, Steinhausen HC, Faraone SV, Asherson P, Kuntsi J. The relationship between ADHD and key cognitive phenotypes is not mediated by shared familial effects with IQ. Psychological Medicine 2010:1-11.
- Li D, Sham PC, Owen MJ, He L. Meta-analysis shows significant association between dopamine system genes and attention deficit hyperactivity disorder (ADHD). nine0054 Human Molecular Genetics 2006;15(14):2276-84.
- Zhou K, Chen W, Buitelaar J, Banaschewski T, Oades RD, Franke B, Sonuga-Barke E, Ebstein R, Eisenberg J, Gill M, Manor I, Miranda A, Mulas F, Roeyers H, Rothenberger A, Sergeant J , Steinhausen HC, Lasky-Su J, Taylor E, Brookes KJ, Xu X, Neale BM, Rijsdijk F, Thompson M, Asherson P, Faraone SV.
 Genetic heterogeneity in ADHD: DAT1 gene only affects probands without CD. American Journal of Medical Genetic Part B-Neuropsychiatry Genetic 2008;147B(8):1481-7.
Genetic heterogeneity in ADHD: DAT1 gene only affects probands without CD. American Journal of Medical Genetic Part B-Neuropsychiatry Genetic 2008;147B(8):1481-7. - Asherson P, Brookes K, Franke B, Chen W, Gill M, Ebstein RP, Buitelaar J, Banaschewski T, Sonuga-Barke E, Eisenberg J, Manor I, Miranda A, Oades RD, Roeyers H, Rothenberger A, Sergeant J , Steinhausen HC, Faraone SV. Confirmation that a specific haplotype of the dopamine transporter gene is associated with combined-type ADHD. American Journal of Psychiatry 2007;164(4):674-7.
- Brookes KJ, Xu X, Anney R, Franke B, Zhou K, Chen W, Banaschewski T, Buitelaar J, Ebstein R, Eisenberg J, Gill M, Miranda A, Oades RD, Roeyers H, Rothenberger A, Sergeant J, Sonuga -Barke E, Steinhausen HC, Taylor E, Faraone SV, Asherson P. Association of ADHD with genetic variants in the 5'-region of the dopamine transporter gene: evidence for allelic heterogeneity. nine0054 American Journal of Medical Genetic Part B-Neuropsychiatry Genetic 2008;147B(8):1519-23.
- Brookes KJ, Mill J, Guindalini C, Curran S, Xu X, Knight J, Chen CK, Huang YS, Sethna V, Taylor E, Chen W, Breen G, Asherson P. A common haplotype of the dopamine transporter gene associated with attention-deficit/hyperactivity disorder and interacting with maternal use of alcohol during pregnancy. Archives of General Psychiatry 2006;63(1):74-81.
- Becker K, El-Faddagh M, Schmidt MH, Esser G, Laucht M. Interaction of dopamine transporter genotype with prenatal smoke exposure on ADHD symptoms. nine0054 Journal of Pediatrics 2008;152(2):263-9.
- Kahn RS, Khoury J, Nichols WC, Lanphear BP. Role of dopamine transporter genotype and maternal prenatal smoking in childhood hyperactive-impulsive, inattentive, and oppositional behaviors. Journal of Pediatrics 2003;143(1):104-10.
- Gizer IR, Ficks C, Waldman ID. Candidate gene studies of ADHD: a meta-analytic review. Human Genetics 2009;126(1):51-90.
- Kuntsi J, Neale BM, Chen W, Faraone SV, Asherson P.
 The IMAGE project: methodological issues for the molecular genetic analysis of ADHD. nine0054 Behavioral and Brain Function 2006;2:27.
The IMAGE project: methodological issues for the molecular genetic analysis of ADHD. nine0054 Behavioral and Brain Function 2006;2:27. - Dudbridge F, Gusnanto A. Estimation of significance thresholds for genomewide association scans. Genetic Epidemiology 2008;32(3):227-34.
- Neale BM, Lasky-Su J, Anney R, Franke B, Zhou K, Maller JB, Vasquez AA, Asherson P, Chen W, Banaschewski T, Buitelaar J, Ebstein R, Gill M, Miranda A, Oades RD, Roeyers H , Rothenberger A, Sergeant J, Steinhausen HC, Sonuga-Barke E, Mulas F, Taylor E, Laird N, Lange C, Daly M, Faraone SV. Genome-wide association scan of attention deficit hyperactivity disorder. nine0054 American Journal of Medical Genetics Part B-Neuropsychiatric Genetics 2008;147B(8):1337-1344.
- Zhou K, Dempfle A, Arcos-Burgos M, Bakker SC, Banaschewski T, Biederman J, Buitelaar J, Castellanos FX, Doyle A, Ebstein RP, Ekholm J, Forabosco P, Franke B, Freitag C, Friedel S, Gill M , Hebebrand J, Hinney A, Jacob C, Lesch KP, Loo SK, Lopera F, McCracken JT, McGough JJ, Meyer J, Mick E, Miranda A, Muenke M, Mulas F, Nelson SF, Nguyen TT, Oades RD, Ogdie MN, Palacio JD, Pineda D, Reif A, Renner TJ, Roeyers H, Romanos M, Rothenberger A, Schäfer H, Sergeant J, Sinke RJ, Smalley SL, Sonuga-Barke E, Steinhausen HC, van der Meulen E, Walitza S , Warnke A, Lewis CM, Faraone SV, Asherson P.
 Meta-analysis of genome-wide linkage scans of attention deficit hyperactivity disorder. nine0054 American Journal of Medical Genetics Part B-Neuropsychiatric Genetics 2008;147B(8):1392-8.
Meta-analysis of genome-wide linkage scans of attention deficit hyperactivity disorder. nine0054 American Journal of Medical Genetics Part B-Neuropsychiatric Genetics 2008;147B(8):1392-8. - Lasky-Su J, Neale BM, Franke B, Anney RJ, Zhou K, Maller JB, Vasquez AA, Chen W, Asherson P, Buitelaar J, Banaschewski T, Ebstein R, Gill M, Miranda A, Mulas F, Oades RD , Roeyers H, Rothenberger A, Sergeant J, Sonuga-Barke E, Steinhausen HC, Taylor E, Daly M, Laird N, Lange C, Faraone SV.. Genome-wide association scan of quantitative traits for attention deficit hyperactivity disorder identifies novel associations and confirm candidate gene associations. nine0054 American Journal of Medical Genetics Part B-Neuropsychiatric Genetics 2008;147B(8):1345-54.
- Lesch KP, Timmesfeld N, Renner TJ, Halperin R, Röser C, Nguyen TT, Craig DW, Romanos J, Heine M, Meyer J, Freitag C, Warnke A, Romanos M, Schäfer H, Walitza S, Reif A, Stephan DA, Jacob C. Molecular genetics of adult ADHD: converging evidence from genome-wide association and extended pedigree linkage studies.
 Journal of Neural Transmission 2008;115(11):1573-85. nine0128 Franke B, Neale BM, Faraone SV. Genome-wide association studies in ADHD. Human Genetics 2009;126(1):13-50.
Journal of Neural Transmission 2008;115(11):1573-85. nine0128 Franke B, Neale BM, Faraone SV. Genome-wide association studies in ADHD. Human Genetics 2009;126(1):13-50. - Munafo MR, Brown SM, Hariri AR. Serotonin transporter (5-HTTLPR) genotype and amygdala activation: a meta-analysis. Biological Psychiatry 2008;63(9):852-7.
- Green AE, Munafò MR, DeYoung CG, Fossella JA, Fan J, Gray JR. Using genetic data in cognitive neuroscience: from growing pains to genuine insights. Nature Reviews Neuroscience 2008;9:710-720.
- Kebir O, Tabbane K, Sengupta S, Joober R. Candidate genes and neuropsychological phenotypes in children with ADHD: review of association studies. Journal of Psychiatry and Neuroscience 2009;34(2):88-101.
- Walters JT, Corvin A, Owen MJ, Williams H, Dragovic M, Quinn EM, Judge R, Smith DJ, Norton N, Giegling I, Hartmann AM, Möller HJ, Muglia P, Moskvina V, Dwyer S, O'Donoghue T , Morar B, Cooper M, Chandler D, Jablensky A, Gill M, Kaladjieva L, Morris DW, O'Donovan MC, Rujescu D, Donohoe G.
 Psychosis susceptibility gene ZNF804A and cognitive performance in schizophrenia. nine0054 Archives of General Psychiatry 2010;67(7):692-700.
Psychosis susceptibility gene ZNF804A and cognitive performance in schizophrenia. nine0054 Archives of General Psychiatry 2010;67(7):692-700.
*Note: Go/no-go task is a type of task in which the participant must respond to some stimulus while ignoring other stimuli.
RUDN doctors found changes in the amino acid balance in children with ADHD
Cookies
This site uses cookies. The information collected by a cookie cannot identify you, but it can help us improve our site. By continuing to use the site, you consent to the processing of cookies. nine0008
Good
Read more
Nauka
August 19, 2021
RUDN University doctors discovered changes in the amino acid composition of blood serum in children with attention deficit hyperactivity disorder (ADHD). The results obtained will help to better understand the mechanism of the disorder and develop new treatment strategies.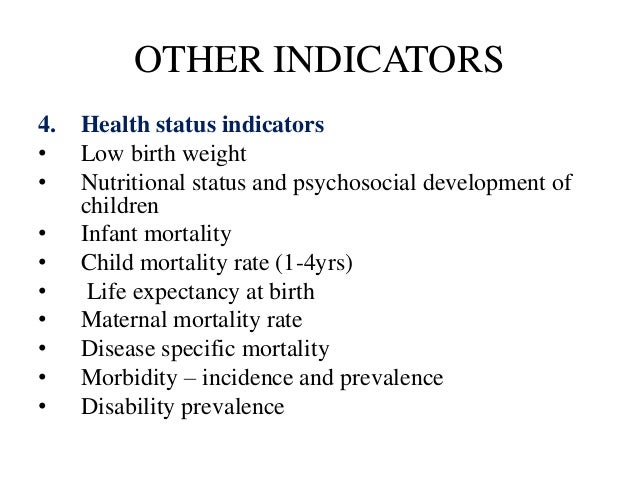
Attention deficit hyperactivity disorder (ADHD) is a developmental disorder that begins in childhood. Children with ADHD have difficulty concentrating and managing impulsivity. It is known that ADHD also manifests itself at the neurochemical level - for example, the work of the neurotransmitters dopamine and norepinephrine is disrupted. However, there is still no unambiguous data on how the balance of amino acids that are responsible for brain function changes in ADHD. Although at the same time, drugs consisting of amino acids are often used to treat ADHD. Scientists from the Peoples' Friendship University of Russia have found out how the amino acid composition of blood serum differs in children with ADHD. nine0008
“Amino acids play an important role in brain development and function. In particular, it is well known that certain amino acids or their precursors are involved in the transmission of nerve impulses. Accordingly, impaired amino acid metabolism leads to significant neurological disorders, especially in childhood.
Uncovering the potential mechanisms of ADHD related to amino acid balance is important to improve our understanding of this disorder and further development of treatment strategies,” said Anatoly Skalny, MD, Head of the Department of Medical Elementology at RUDN University. nine0008
102 children aged 7 to 14 years old took part in the medical study. 71 of them were diagnosed with ADHD, the rest of the participants in the experiment were neurotypical, that is, without diagnosed disorders. The level of amino acids in blood serum was measured using liquid chromatography. Then the data obtained in children with ADHD and neurotypical children were compared by statistical methods.
It turned out that the amino acid composition of blood serum in children with ADHD differs from neurotypical children. The levels of histidine, glutamine and proline were lower by 29%, 10% and 20% respectively. Aspartic acid and glutamate turned out to be 7% more, hydroxyproline — 42%. Accordingly, the ratio of glutamine to glutamate in children with ADHD is 28% less than normal, and the ratio of proline to hydroxyproline is 29%.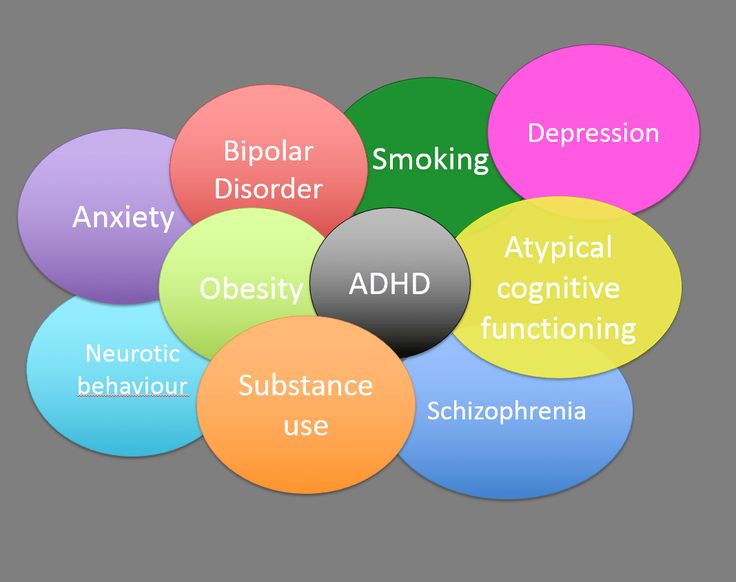 The first ratio serves as one of the indicators of the transmission of nerve impulses, and the second can be a marker of impaired collagen metabolism and connective tissue function. Associated conditions are sometimes considered comorbid ADHD.
The first ratio serves as one of the indicators of the transmission of nerve impulses, and the second can be a marker of impaired collagen metabolism and connective tissue function. Associated conditions are sometimes considered comorbid ADHD.
“The observed changes in the levels and ratios of proline to hydroxyproline and glutamine to glutamate are likely related to comorbid connective tissue pathology and changes in neurotransmission in ADHD. However, further studies in vivo and in vitro are needed to study in detail the mechanisms that link amino acid metabolism with the pathogenesis of ADHD,” Anatoly Skalny commented.
Study published in Biomedical Reports. nine0008
Previous news
August 18, 2021
RUDN University doctors found out the role of macrophages in liver regeneration
Next news
August 20, 2021
RUDN linguist found out that aspirated consonants can contribute to the spread of COVID-19
PFUR ecologists have found a vulnerability in the calculation of the content of organic matter in arable soils according to Earth remote sensing data
RUDN ecologists have shown that one of the methods by which the content of organic matter in the soil is determined turns out to be ineffective after precipitation. Studies have shown that the impact of rain on the open surface of arable soils leads to a decrease in the accuracy of modeling the content of organic matter up to 70%. RUDN University environmentalists also suggested how to compensate for this negative phenomenon and increase the accuracy of calculations up to 84%.
Studies have shown that the impact of rain on the open surface of arable soils leads to a decrease in the accuracy of modeling the content of organic matter up to 70%. RUDN University environmentalists also suggested how to compensate for this negative phenomenon and increase the accuracy of calculations up to 84%.
RUDN Institute of Ecology became the winner of the "Green Prize" of the Russian environmental operator
The Institute of Ecology became a laureate in the nomination "Educational Activities" with the project "Development of an educational and methodological complex" Fundamentals and principles of a circular economy. Creation of a sustainable system for handling municipal solid waste.” The authors are Elena Savenkova, Doctor of Economics, Director of the RUDN Institute of Ecology, and Anna Kurbatova, Candidate of Biological Sciences, Associate Professor of the Department of Environmental Safety and Product Quality Management of the RUDN Institute of Ecology.