How to treat dissociative identity disorder
Dissociative disorders - Diagnosis and treatment
Diagnosis
Diagnosis usually involves assessment of symptoms and ruling out any medical condition that could cause the symptoms. Testing and diagnosis often involves a referral to a mental health professional to determine your diagnosis.
Evaluation may include:
- Physical exam. Your doctor examines you, asks in-depth questions, and reviews your symptoms and personal history. Certain tests may eliminate physical conditions — for example, head injury, certain brain diseases, sleep deprivation or intoxication — that can cause symptoms such as memory loss and a sense of unreality.
- Psychiatric exam. Your mental health professional asks questions about your thoughts, feelings, and behavior and discusses your symptoms. With your permission, information from family members or others may be helpful.
- Diagnostic criteria in the DSM-5. Your mental health professional may compare your symptoms to the criteria for diagnosis in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), published by the American Psychiatric Association.
For diagnosis of dissociative disorders, the DSM-5 lists these criteria.
Dissociative amnesia
For dissociative amnesia:
- You've had one or more episodes in which you couldn't remember important personal information — usually something traumatic or stressful — or you can't remember your identity or life history. This memory loss is too extensive to be explained by ordinary forgetfulness.
- Your episodes of memory loss don't occur only during the course of another mental health disorder, such as post-traumatic stress disorder. Also, your symptoms are not due to alcohol or other drugs, and they're not caused by a neurological or other medical condition, such as amnesia related to head trauma.
- You may also experience dissociative fugue, where you purposefully travel or experience confused wandering that involves amnesia — inability to remember your identity or other important personal information.
- Your symptoms cause you significant stress or problems in your relationships, work or other important areas of your life.
Dissociative identity disorder
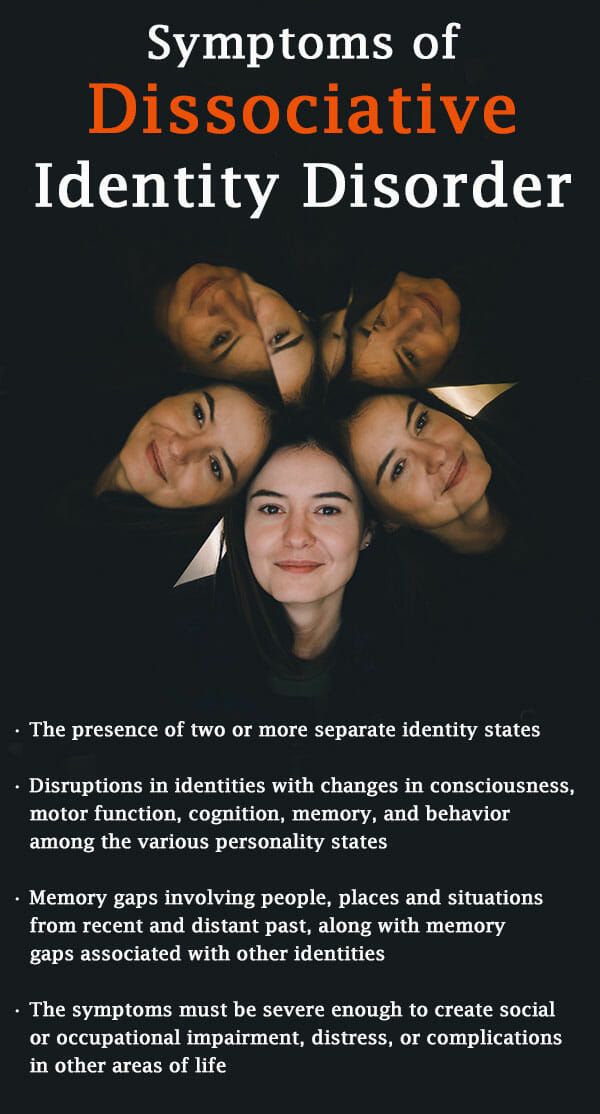
For dissociative identity disorder:
- You display, or others observe, two or more distinct identities or personalities, which may be described in some cultures as possession that is unwanted and involuntary. Each identity has its own pattern of perceiving, relating to and thinking about yourself and the world.
- You have recurrent gaps in memory for everyday events, skills, important personal information and traumatic events that are too extensive to be explained by ordinary forgetfulness.
- Your symptoms are not a part of broadly accepted cultural or religious practice.
- Your symptoms are not due to alcohol or other drugs, or a medical condition. In children, symptoms are not due to imaginary playmates or other fantasy play.
- Your symptoms cause you significant stress or problems in your relationships, work or other important areas of your life.
Depersonalization-derealization disorder
For depersonalization-derealization disorder:
- You have persistent or recurrent experiences of feeling detached from yourself, as if you're an outside observer of your thoughts, sensations, actions or your body (depersonalization).
 Or you feel detached or experience a lack of reality for your surroundings as if you're in a dream or the world is distorted (derealization).
Or you feel detached or experience a lack of reality for your surroundings as if you're in a dream or the world is distorted (derealization). - While you're experiencing an episode of depersonalization or derealization, you're aware the experience is not reality.
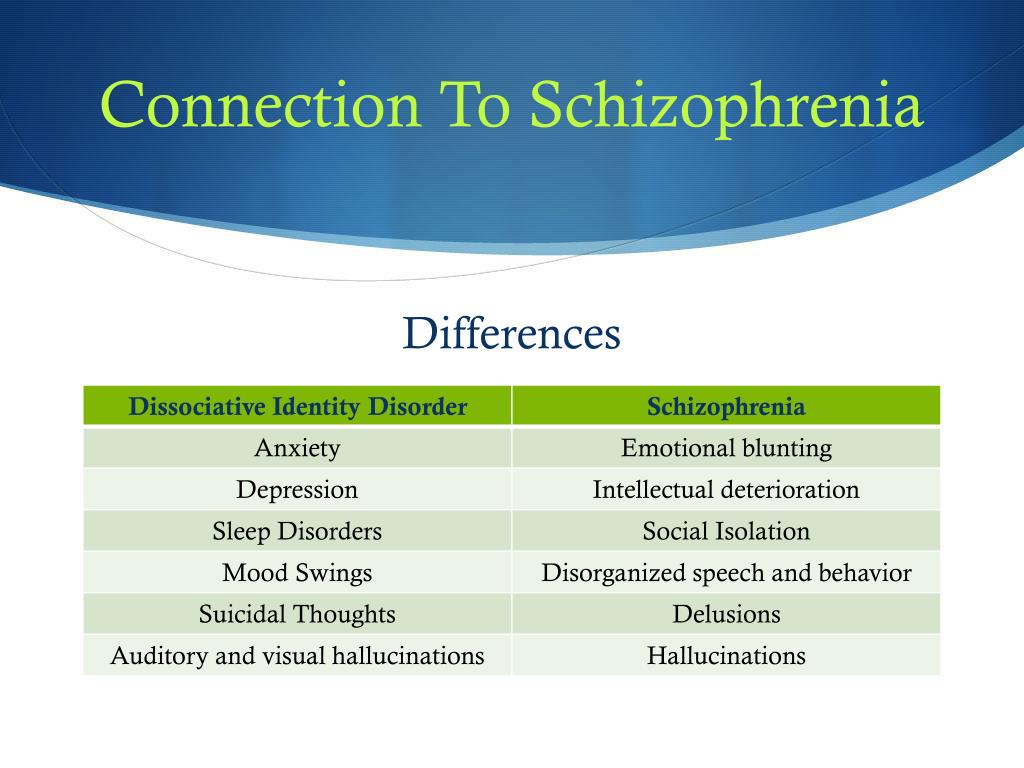
- Your symptoms do not occur only during the course of another mental disorder, such as schizophrenia or panic disorder, or during another dissociative disorder. Your symptoms are also not explained by the direct effects of alcohol or other drugs, or a medical condition, such as temporal lobe epilepsy.
- Your symptoms cause you significant stress or problems in your relationships, work or other important areas of your life.
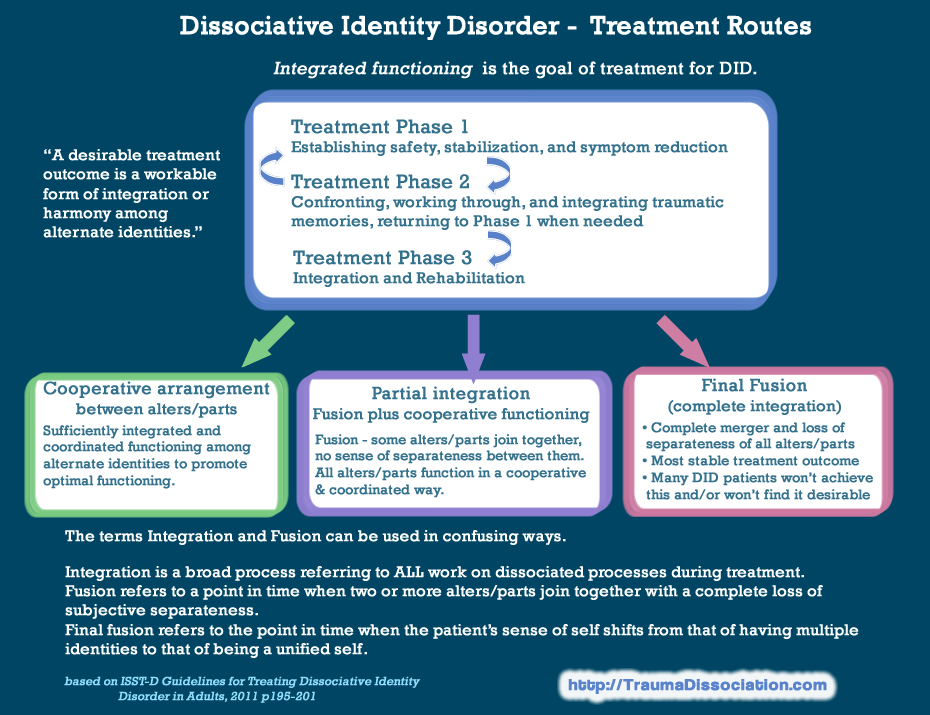
Treatment
Dissociative disorders treatment may vary based on the type of disorder you have, but generally include psychotherapy and medication.
Psychotherapy
Psychotherapy is the primary treatment for dissociative disorders. This form of therapy, also known as talk therapy, counseling or psychosocial therapy, involves talking about your disorder and related issues with a mental health professional. Look for a therapist with advanced training or experience in working with people who have experienced trauma.
Look for a therapist with advanced training or experience in working with people who have experienced trauma.
Your therapist will work to help you understand the cause of your condition and to form new ways of coping with stressful circumstances. Over time, your therapist may help you talk more about the trauma you experienced, but generally only when you have the coping skills and relationship with your therapist to safely have these conversations.
Medication
Although there are no medications that specifically treat dissociative disorders, your doctor may prescribe antidepressants, anti-anxiety medications or antipsychotic drugs to help control the mental health symptoms associated with dissociative disorders.
More Information
- Cognitive behavioral therapy
- Hypnosis
- Psychotherapy
Request an Appointment at Mayo Clinic
Preparing for your appointment
As a first step, your doctor may ask you to come in for a thorough exam to rule out possible physical causes of your symptoms. However, in some cases you may be referred immediately to a psychiatrist. You may want to take a family member or friend along, if possible, to help you remember information.
However, in some cases you may be referred immediately to a psychiatrist. You may want to take a family member or friend along, if possible, to help you remember information.
Here's some information to help you prepare for your appointment, and what to expect from your doctor.
What you can do
Before your appointment, make a list of:
- Any symptoms you're experiencing, including any recent behavior that caused confusion or concern for you or your loved ones.
- Key personal information, including any major stresses or recent life changes. Also note events from your past, including your childhood, that caused physical or emotional trauma. If you can't recall some periods of your life, note the time frame and anything you can remember about the period leading up to your amnesia.
- Your medical information, including other physical or mental health conditions you have. Include any medications, vitamins, herbs or other supplements you're taking, and the dosages.
- Questions to ask your doctor to make the most of your time together
Some questions to ask your doctor may include:
- What's likely causing my symptoms or condition?
- What are other possible causes?
- How will you determine my diagnosis?
- Is my condition likely temporary or long term (chronic)?
- What treatments do you recommend for this disorder?
- How much can I expect my symptoms to improve with treatment?
- How will you monitor my progress?
- I have these other health conditions. How can I best manage them together?
- Should I see a specialist?
- Are there any brochures or other printed material that I can have?
- What websites do you recommend?
Don't hesitate to ask other questions during your appointment.
What to expect from your doctor
Your doctor is likely to ask you a number of questions. Be ready to answer them to reserve time to go over any points you want to focus on.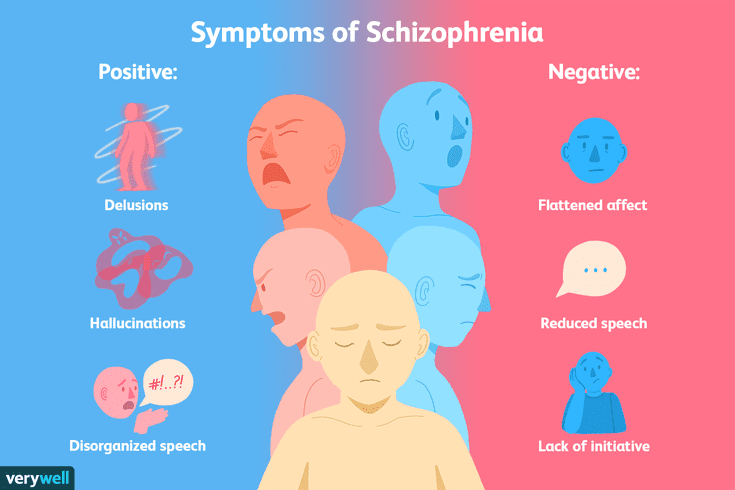 Your doctor may ask:
Your doctor may ask:
- What symptoms concern you or your loved ones?
- When did you or your loved ones first notice your symptoms?
- Are there periods of time in your life that you don't remember?
- Have you ever found yourself some distance away from your home or work, and not known how you got there?
- Do you ever feel as if you're outside of your body, observing yourself?
- Do you feel as though there is more than one person, or maybe many people, living inside your head?
- What other symptoms or behaviors are causing you or your loved ones distress?
- How often do you feel anxious or depressed?
- Have your symptoms caused problems in your work or your personal relationships?
- Have you ever thought about harming yourself or others?
- Do you drink alcohol or use recreational drugs?
- Do you now or have you ever served in the military?
- Have you ever been touched against your will?
- Were you physically abused or neglected as a child?
- Was anyone in your family abused during your childhood?
- Are you currently being treated for any other medical conditions, including mental health disorders?
By Mayo Clinic Staff
Related
Associated Procedures
Products & Services
Causes, Symptoms, Types & Treatment
Overview
What is delusional disorder?
Delusional disorder is a type of psychotic disorder.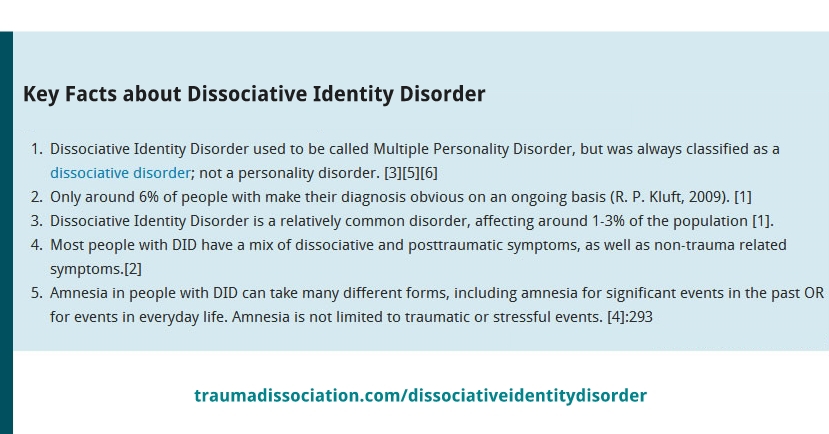 Its main symptom is the presence of one or more delusions.
Its main symptom is the presence of one or more delusions.
A delusion is an unshakable belief in something that’s untrue. The belief isn’t a part of the person’s culture or subculture, and almost everyone else knows this belief to be false.
People with delusional disorder often experience non-bizarre delusions. Non-bizarre delusions involve situations that could possibly occur in real life, such as being followed, deceived or loved from a distance. These delusions usually involve the misinterpretation of perceptions or experiences. In reality, these situations are either untrue or are highly exaggerated.
Non-bizarre delusions are different from bizarre delusions, which include beliefs that are impossible in our reality, such as believing someone has removed an organ from your body without any physical evidence of the procedure.
People with delusional disorder often continue to socialize and function well, apart from the subject of their delusion. Generally, they don’t behave in an odd or unusual manner. This is unlike people with other psychotic disorders, who might also have delusions as a symptom. In some cases, however, people with delusional disorder might become so preoccupied with their delusions that their lives are disrupted.
This is unlike people with other psychotic disorders, who might also have delusions as a symptom. In some cases, however, people with delusional disorder might become so preoccupied with their delusions that their lives are disrupted.
What are the types of delusional disorder?
There are different types of delusional disorder, which are determined based on the main theme of the delusions the person experiences. The types of delusional disorder include:
- Erotomanic: People with this type of delusional disorder believe that another person, often someone important or famous, is in love with them. They may attempt to contact the person of the delusion and engage in stalking behavior.
- Grandiose: People with this type of delusional disorder have an overinflated sense of self-worth, power, knowledge or identity. They may believe they have a great talent or have made an important discovery.
- Jealous: People with this type of delusional disorder believe that their spouse or sexual partner is unfaithful without any concrete evidence.
- Persecutory: People with this type of delusional disorder believe someone or something is mistreating, spying on or attempting to harm them (or someone close to them). People with this type of delusional disorder may make repeated complaints to legal authorities.
- Somatic: People with this type of delusional disorder believe that they have a physical issue or medical problem, such as a parasite or a bad odor.
- Mixed: People with this type of delusional disorder have two or more of the types of delusions listed above.
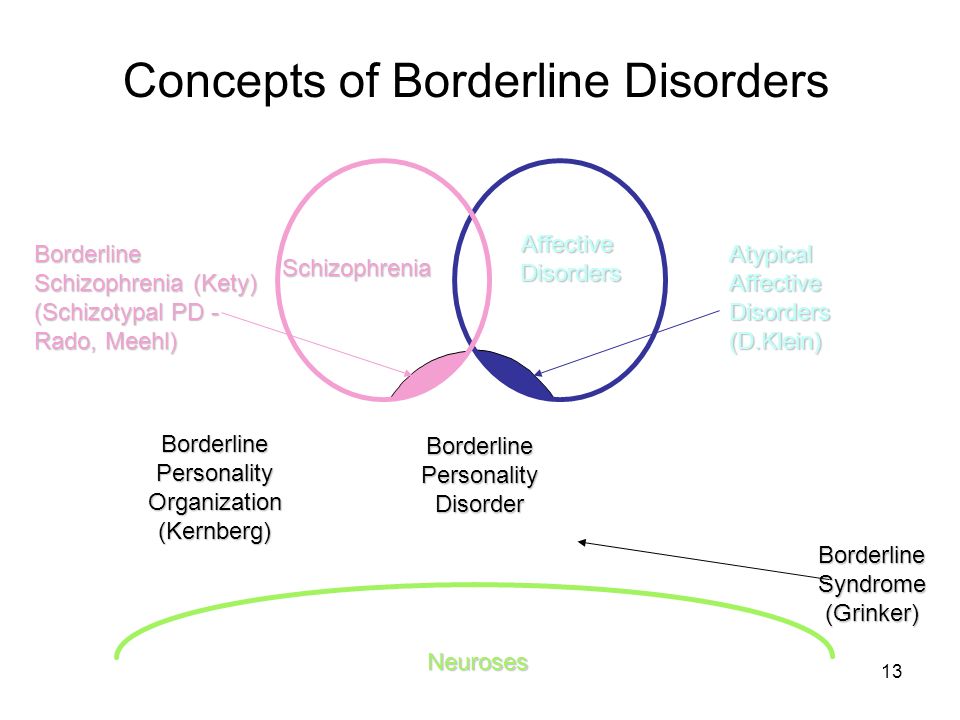
What is the difference between delusional disorder and schizophrenia?
Schizophrenia is a spectrum (or range) of conditions that involve psychotic symptoms, which include:
- Disorganized speech or behavior.
- Negative symptoms (a decrease in emotion in a person’s facial expressions and motivation).
Delusional disorder is different from schizophrenia because there aren’t any other psychotic symptoms other than delusions.
In addition, in contrast to schizophrenia, delusional disorder is relatively rare, and daily functioning isn’t as impaired as it is in schizophrenia.
Who does delusional disorder affect?
Delusional disorder most often occurs in middle to late life, with the average age of onset being 40 years.
The persecutory and jealous types of delusional disorder are more common in people assigned male at birth (AMAB), and the erotomanic type is more common in people assigned female at birth (AFAB).
People who tend to be socially isolated are more likely to develop delusional disorder. These populations include:
- Immigrants who have language barriers.
- People who are deaf.
- People who are visually impaired.
- Elderly people.
How common is delusional disorder?
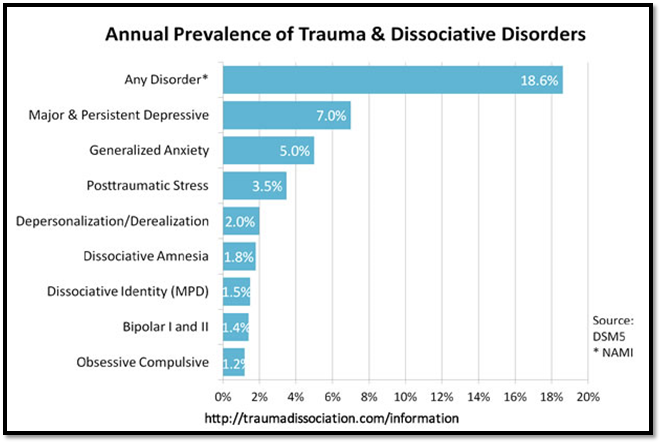
Although delusions might be a symptom of more common disorders, such as schizophrenia, delusional disorder itself is rather rare. Approximately 0.05% to 0.1% of the adult population has delusional disorder.
What is the most common type of delusional disorder?
The most common type of delusional disorder is the persecutory type — when someone believes others are out to harm them despite evidence to the contrary.
Symptoms and Causes
What are the signs and symptoms of delusional disorder?
The presence of delusions is the most obvious sign of delusional disorder, which vary based on the type.
Another characteristic of this condition is that the person often lacks self-awareness that their delusions are problematic. They’re unable to accept that their delusions are irrational or inaccurate, even if they recognize that other people would describe their delusions this way.
Anger and violent behavior may be present if someone is experiencing persecutory, jealous or erotomanic delusions.
People with delusional disorder may also develop anxiety and/or depression as a result of the delusions.
Early symptoms of delusional disorder may include:
- Feelings of being exploited.
- Preoccupation with the loyalty or trustworthiness of friends.
- A tendency to read threatening meanings into benign remarks or events.
- Persistently holding grudges.
- A readiness to respond and react to perceived slights.
What causes delusional disorder?
As with many other psychotic disorders, researchers don’t yet know the exact cause of delusional disorder. Researchers are, however, looking at the role of various factors that may contribute to the development of the condition, including:
- Genetic factors: The fact that delusional disorder is more common in people who have family members with delusional disorder or schizophrenia suggests there might be a genetic factor involved. Researchers believe that, as with other mental disorders, a tendency to develop delusional disorder might be passed on from parents to their biological children.
- Biological factors: Researchers are studying how abnormalities of certain areas of your brain might be involved in the development of delusional disorder.
 An imbalance of certain chemicals in your brain, called neurotransmitters, has been linked to the formation of delusional symptoms.
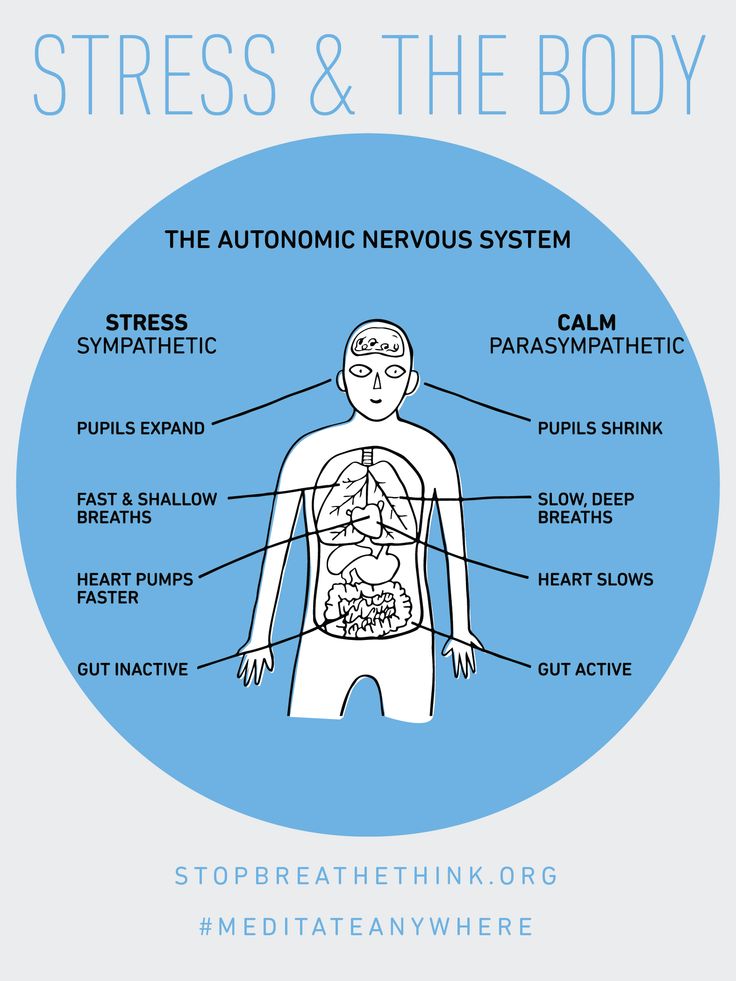
An imbalance of certain chemicals in your brain, called neurotransmitters, has been linked to the formation of delusional symptoms. - Environmental and psychological factors: Evidence suggests that delusional disorder can be triggered by stress. Alcohol use disorder and substance use disorder might contribute to the condition. Hypersensitivity and ego defense mechanisms like reaction formation, projection and denial are some psychodynamic theories for the development of delusional disorder. Social isolation, envy, distrust, suspicion and low self-esteem are also some psychological factors that may lead to a person seeking an explanation for these feelings and, thus, forming a delusion as a solution.
Diagnosis and Tests
How is delusional disorder diagnosed?
Healthcare providers — mainly mental health professionals — diagnose delusional disorder when a person has one or more delusions for one month or more that can’t be explained by any other condition.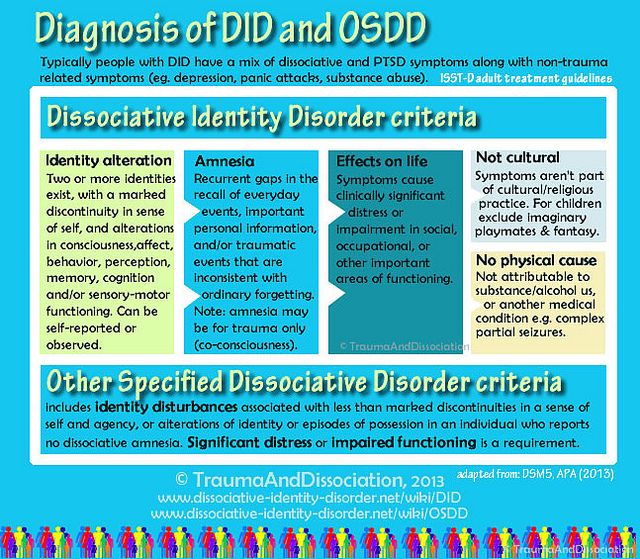 The person must also not have the characteristic symptoms of other psychotic disorders, such as schizophrenia.
The person must also not have the characteristic symptoms of other psychotic disorders, such as schizophrenia.
If someone is experiencing signs and symptoms of delusional disorder, a healthcare provider will perform a complete medical history and physical examination. Although there aren’t any laboratory tests to diagnose delusional disorder, their healthcare provider might use various diagnostic tests — such as imaging tests, a urine drug screen and blood tests — to rule out any physical conditions, medications or substances that could be causing the symptoms.
If their healthcare provider finds no physical reason for the symptoms, a consultation with a psychiatrist or psychologist will likely be made. Psychiatrists and psychologists use specially designed interview and assessment tools to evaluate a person for a psychotic disorder. They’ll ask questions about the delusions and assess the person’s mental status.
The psychiatrist or psychologist may also interview family members and friends so they can provide further details about the person’s delusions and a timeline of the symptoms.
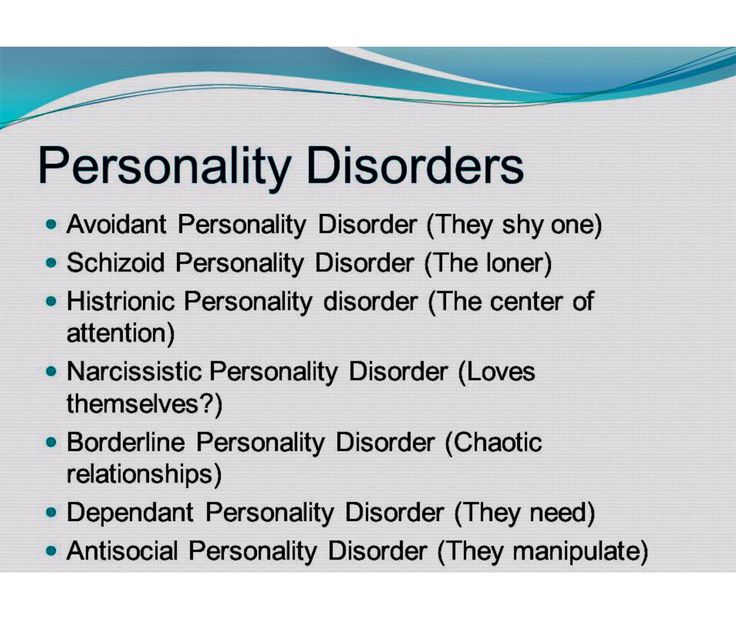
As other mental health conditions can cause delusions, mental health professionals carefully assess the person for other symptoms. Delusional disorder can be misdiagnosed as any of the following conditions:
- Obsessive-compulsive disorder.
- Schizophrenia.
- Delirium/major neurocognitive disorder.
- Bipolar disorder.
- Personality disorders, especially borderline personality disorder and paranoid personality disorder.
Management and Treatment
How is delusional disorder treated?
Treatment for delusional disorder most often includes psychotherapy (talk therapy) and medication, but delusional disorder is highly resistant to treatment with medication alone.
People with delusional disorder often don’t seek treatment for the condition on their own because most people with delusional disorder don’t realize their delusions are problematic or incorrect. It’s more likely they’ll seek help due to other mental health conditions such as depression or anxiety.
People with severe symptoms or who are at risk of hurting themselves or others might need to be admitted to the hospital until the condition is stabilized.
Psychotherapy for delusional disorder
Psychotherapy is a term for a variety of treatment techniques that aim to help people identify and change troubling emotions, thoughts and behaviors. Working with a mental health professional, such as a psychologist or psychiatrist, can provide support, education and guidance to the person and their family.
Through therapy, people with delusional disorder can learn to manage their symptoms, identify early warning signs of relapse and develop relapse prevention plans. Types of psychotherapy include:
- Individual psychotherapy: This type of therapy can help a person recognize and correct the underlying thinking that has become distorted.
- Cognitive behavioral therapy (CBT): This is a structured, goal-oriented type of therapy.
 A mental health professional helps people take a close look at their thoughts and emotions. They’ll come to understand how their thoughts affect their actions. Through CBT, they can unlearn negative thoughts and behaviors and learn to adopt healthier thinking patterns and habits.
A mental health professional helps people take a close look at their thoughts and emotions. They’ll come to understand how their thoughts affect their actions. Through CBT, they can unlearn negative thoughts and behaviors and learn to adopt healthier thinking patterns and habits. - Family-focused therapy: This therapy can help people with delusional disorder and their families. This treatment involves psychoeducation regarding delusional disorder, communication improvement training and problem-solving skills training.
Medications for delusional disorder
The primary medications used to help treat delusional disorder are called antipsychotics (neuroleptics). Medications include the following:
- First-generation (“typical”) antipsychotics: Healthcare providers have used these medications to treat mental health conditions since the mid-1950s. These medicines work by blocking dopamine receptors in your brain. Dopamine is a neurotransmitter believed to be involved in the development of delusions.
 First-generation antipsychotics include chlorpromazine (Thorazine®), fluphenazine (Prolixin®), haloperidol (Haldol®), thiothixene (Navane®), trifluoperazine (Stelazine®), perphenazine (Trilafon®) and thioridazine (Mellaril®).
First-generation antipsychotics include chlorpromazine (Thorazine®), fluphenazine (Prolixin®), haloperidol (Haldol®), thiothixene (Navane®), trifluoperazine (Stelazine®), perphenazine (Trilafon®) and thioridazine (Mellaril®). - Second-generation (“atypical”) antipsychotics: These newer antipsychotics are also effective in treating the symptoms of delusional disorder. They work by blocking dopamine and serotonin receptors in your brain. These drugs include risperidone (Risperdal®), clozapine (Clozaril®), quetiapine (Seroquel®), ziprasidone (Geodon®) and olanzapine (Zyprexa®). These medications are usually better tolerated than first-generation antipsychotics.
Other medications that healthcare providers might prescribe to treat delusional disorder include anxiolytics and antidepressants. Anxiolytics might help if the person has a very high level of anxiety and/or problems sleeping. Antidepressants can help treat depression, which often occurs in people with delusional disorder.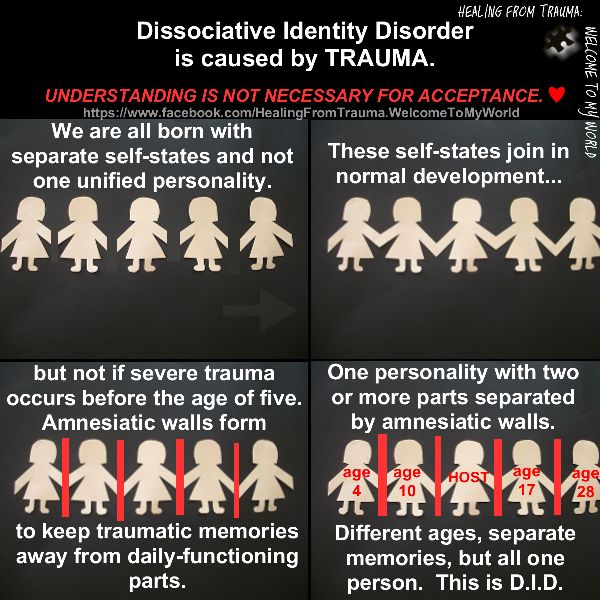
Prevention
Can delusional disorder be prevented?
There’s no known way to prevent delusional disorder. However, early diagnosis and treatment can help decrease the disruption to the person’s life, family and friendships.
Outlook / Prognosis
What is the prognosis (outlook) for delusional disorder?
The prognosis (outlook) for people with delusional disorder varies depending on a few factors, including:
- The type of delusional disorder.
- The severity of the delusions.
- The person’s life circumstances, including the availability of support and a willingness to stick with treatment.
Delusional disorder doesn’t usually significantly affect a person’s daily functioning, but the severity of the delusion may gradually get worse. Most people with delusional disorder can remain employed as long as their work doesn’t involve things related to their delusions.
The prognosis of delusional disorder is better if the person sticks to their treatment plan. Almost 50% of people have a full recovery, more than 20% of people report a decrease in symptoms and less than 20% of people report minimal to no change in symptoms.
Almost 50% of people have a full recovery, more than 20% of people report a decrease in symptoms and less than 20% of people report minimal to no change in symptoms.
Unfortunately, many people with this condition don’t seek help. It’s often difficult for people with mental health conditions to recognize they’re not well. They also might be too embarrassed or afraid to seek treatment. Without treatment, delusional disorder can be a life-long condition.
What are the possible complications of delusional disorder?
If left untreated, delusional disorder might lead to:
- Depression, often as a consequence of difficulties associated with the delusions.
- Social isolation.
- Legal issues — for example, stalking or harassing the person involved with the delusion could lead to arrest.
- Self-harm or harm to others. This is more common in the jealous and persecutory types.
Living With
How can I help someone with delusional disorder?
If you know someone with delusional disorder, you can help by providing support and encouragement for them to seek help and treatment.
People with delusional disorder who feel pressured or repeatedly criticized by others will likely experience stress, which may worsen their symptoms. Because of this, a positive approach may be more helpful and effective.
The friends and family members of people with delusional disorder often experience stress, depression, grief and isolation. It’s important to take care of your mental health and seek help if you’re experiencing these symptoms.
A note from Cleveland Clinic
It’s important to remember that delusional disorder is a mental health condition. As with all mental health conditions, seeking help as soon as symptoms appear can help decrease the disruptions to life. Mental health professionals can offer treatment plans that can help manage thoughts and behaviors.
Treatment of dissociative personality disorder in St. Petersburg
- Main
- Psychiatry
- Treatment of dissociative disorder
Dissociative personality disorder is a rather rare disease in our country. However, interest in this personality disorder is reflected not only in the Western European community of psychiatrists and psychotherapists, but also in modern cinema (for example, in the film Split, which was released in domestic cinemas in 2016). The disease itself is not associated with schizophrenia, as many still mistakenly believe, and the diagnosis (F44.8 according to ICD-10, 6B64 according to ICD-11) as such appeared in the International Classification of Diseases already in the 80s of the last century. nine0011
Since 1984, psychiatrists and psychotherapists have begun to form associations for the study of dissociative identity disorder. By 1995, more than 40,000 patients were diagnosed with this disease, previously defined as a subspecies of hysterical neurosis. To date, the treatment of dissociative personality disorder has been successfully carried out with the help of pharmacotherapy and psychotherapeutic treatment.
By 1995, more than 40,000 patients were diagnosed with this disease, previously defined as a subspecies of hysterical neurosis. To date, the treatment of dissociative personality disorder has been successfully carried out with the help of pharmacotherapy and psychotherapeutic treatment.
Dissociative personality disorder is one of the psychological defense mechanisms that occurs after a trauma suffered in childhood. The mechanism helps to cope with stress and, in most cases, represses memories of psychological or sexual abuse. The presence of any factors that contribute to the emergence of painful memories activates the alter ego (“other self”). Depending on the case, there may be several “other selves”. At the same time, the person himself does not know and does not remember what these “other selves” said and did after he comes to his senses. nine0011
In childhood, dissociative identity disorder may look like a kind of game and, as a rule, goes unnoticed not only by parents, but also by peers (for example, at school). However, entering adulthood, a person with a dissociative disorder begins to experience difficulties in communicating with other people and in family life. However, today there are examples of happy families with many children, where one of the spouses is diagnosed with a dissociative disorder.
However, entering adulthood, a person with a dissociative disorder begins to experience difficulties in communicating with other people and in family life. However, today there are examples of happy families with many children, where one of the spouses is diagnosed with a dissociative disorder.
Consultation of a doctor on the treatment of dissociative disorder:
+7 (812) 407-18-00
Thank you for your trust!
- Psychosocial personality correction
- Anonymous treatment without registration
- Assistance to family and relatives
| Service | Price | |
|---|---|---|
| Outpatient treatment | ||
| Psychiatric consultation | 5 000 ₽ | |
| Psychotherapist appointment | 5 000 ₽ | |
Reception of the chief physician Bocharov A.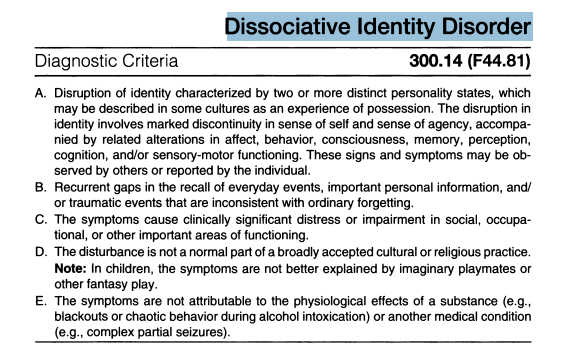 V. (Associate Professor, PhD) V. (Associate Professor, PhD) | 6 000 ₽ | |
| Psychiatric consultation at home | 6 000 ₽ | |
| Treatment in a hospital | ||
| Delivery to hospital | Is free | |
| Standard Chamber | nine0046 | 8 900 ₽ |
| 3-bed superior room | 12 000 ₽ | |
| 2-bed superior room | 15 000 ₽ | |
| 1 local VIP room | 19 500 ₽ | |
| Doctor's appointment 2 weeks after discharge | Is free | |
Signs of dissociative personality disorder
Treatment of dissociative identity disorder
Help for family and relatives
Resources
Expert Q&A: dissociative disorders — https://psychiatry.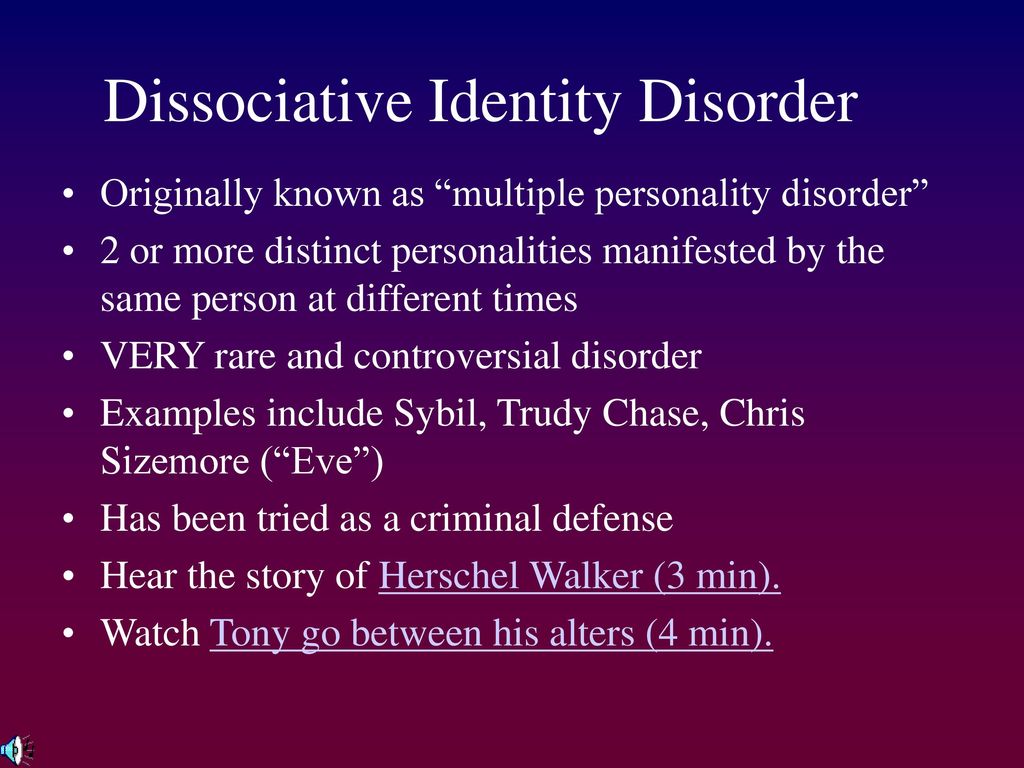 org
org
Clinical handling of patients with dissociative disorders — https://pubmed.ncbi.nlm.nih.gov
Dissociative identity disorder (multiple personality disorder) — https://www.webmd.com
Update date: 10/12/2022
- Depersonalization and derealization
- Suicidal behavior
- Anxiety disorder
Make an appointment
Date and time: (not set)
Make an appointment with a psychiatrist
Make an appointment with a psychiatrist
Select the date and time of your appointment
Tomorrow
December 28
Thursday
December 29
Friday
Dec 30
Sunday
January 01
Monday
January 02
Tuesday
January 03
Wednesday
04 January
Thursday
05 January
Friday
January 06
Saturday
07 January
Sunday
January 08
Monday
January 09
Tuesday
January 10
Wednesday
January 11
Thursday
January 12
Friday
January 13
Saturday
January 14
Sunday
January 15
Monday
January 16
Tuesday
January 17
Wednesday
January 18
Thursday
January 19
Friday
January 20
Saturday
January 21
Sunday
January 22
Monday
January 23
Tuesday
January 24
Wednesday
January 25
Thursday
January 26
Friday
January 27
Saturday
January 28
Sunday
January 29
Monday
January 30
Tuesday
January 31
Treatment for dissociative disorder
Bocharov Alexey
Viktorovich
Psychiatrist, psychotherapist
Head physician of clinic
Experience 41 years
Psychiatrist, psychotherapist, sexologist, child psychiatrist
Experience 41 years
Sinenchenko Andrey
Georgievich
Psychiatrist, psychotherapist
PhD
Experience 22 years
Psychiatrist, psychotherapist, narcologist
Work experience 22 years
Zun Sergey
Andreevich
Psychiatrist, narcologist
PhD
Experience 33 years
Psychiatrist, narcologist, psychotherapist
Work experience 33 years
Lisitsyna Elena
Alekseevna
Psychiatrist
Top category
Experience 33 years
Psychiatrist
Work experience 33 years
nine0010 Buchelnikova VictoriaViktorovna
Psychiatrist
Head of amb.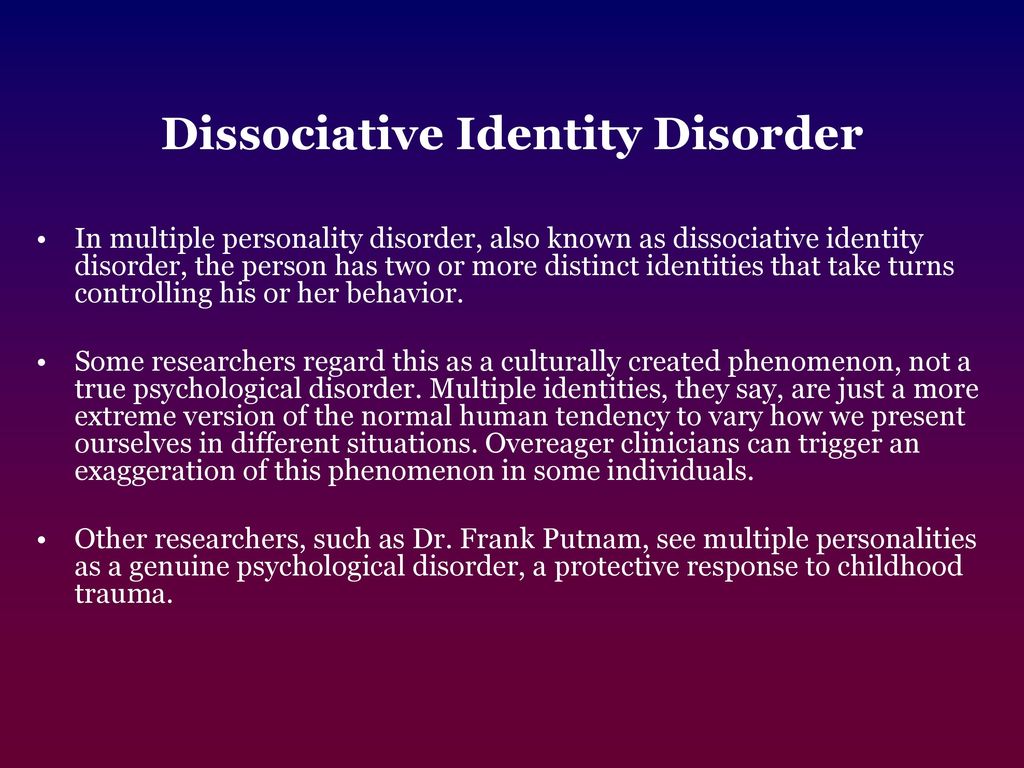 branch
branch
Work experience 15 years
Psychiatrist
Work experience 15 years
Voronina Elvira
Vladimirovna
Psychiatrist
First category
Experience 27 years
Psychiatrist
Work experience 27 years
Efimova Evgenia
Vladimirovna
Second category
Work experience 19 years
Psychiatrist
Work experience 19 years
Gorobets Elena
Vasilievna
Psychiatrist
First category
Work experience 16 years
Psychiatrist
Work experience 16 years
Travnikova Oksana
Mikhailovna
Psychiatrist
First category
Experience 21 years
Psychiatrist
Work experience 21 years
Kurochkina Nadezhda
Pavlovna
Psychiatrist
First category
Work experience 19 years
Psychiatrist
Work experience 19years
Suslennikova Elena
Viktorovna
Psychiatrist, psychotherapist
First category
Experience 25 years
Psychiatrist, psychotherapist
Work experience 25 years
Chuban Olga
Ivanovna
Psychiatrist, psychotherapist
First category
Work experience 13 years
Psychiatrist, psychotherapist, psychologist
Work experience 13 years
nine0010 Popov AndreyPetrovich
Psychiatrist
Top category
Experience 35 years
Psychiatrist
Experience 35 years
Stetsiv Ludmila
Gennadievna
Psychiatrist, psychotherapist
PhD
Experience 31 years
Psychiatrist, psychotherapist
Work experience 31 years
Prokhorchev Konstantin
Sergeevich
Psychiatrist, psychotherapist
First category
Work experience 12 years
Psychiatrist, psychotherapist
Work experience 12 years
Gulevsky Roman
Alexandrovich
Head of hospital
Experience 25 years
Psychiatrist, narcologist
Experience 25 years
Konoplin Dmitry
Alekseevich
Narcologist, psychiatrist
PhD
Work experience 24 years
Narcologist, psychiatrist
Work experience 24 years
Stavitskaya Svetlana
Yurievna
Psychiatrist
Top category
Work experience 24 years
Psychiatrist
Work experience 24 years
Pylskaya Anna
Nikolaevna
Psychiatrist
Second category
Experience 7 years
Psychiatrist
Work experience 7 years
Trofimova Alexandra
Olegovna
Psychiatrist, child psychiatrist
First category
Experience 28 years
Psychiatrist, child psychiatrist
Experience 28 years
Zhelobetskaya Maria
Sergeevna
Psychiatrist, psychotherapist
Top category
Experience 22 years
Psychiatrist, psychotherapist
Work experience 22 years
nine0010 Endrzheevskaya DianaVadimovna
Psychiatrist, psychotherapist
Second category
Work experience 14 years
Psychiatrist, child psychiatrist, psychotherapist
Work experience 14 years
nine0010 Ivanov AlexanderNikolaevich
Psychiatrist, narcologist
Top category
Experience 20 years
Psychiatrist, narcologist
Experience 20 years
Semenov Andrey
Nikolaevich
Psychiatrist, narcologist
Leading specialist of clinic
Work experience 24 years
Psychiatrist, narcologist, transfusiologist
Work experience 24 years
Leave a request for a call:
+7 (812) 407-18-00
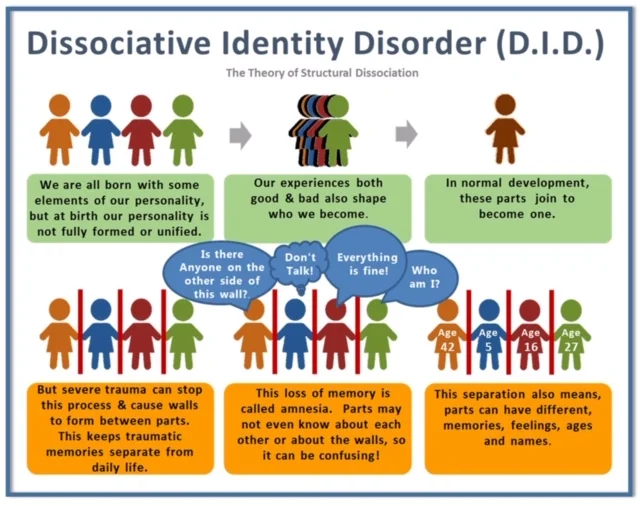
nine0000 What is Dissociative Identity Disorder? Dissociative identity disorder is a mental disorder characterized by either having two or more personalities, or a state of disconnection from the outside world, one's identity, and an inability to remember certain daily life events and important personal information.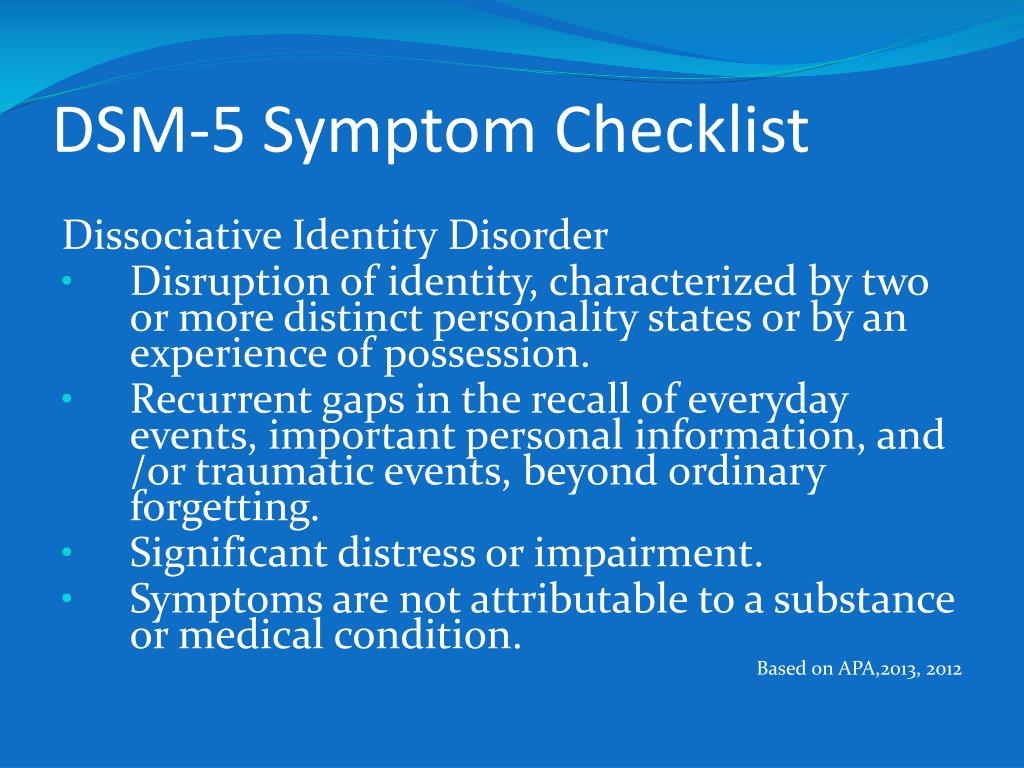 This disorder is often mistaken for depression, anxiety, or psychosis. Long before our days, this condition was called possession, and it was treated with exorcism. In the 19th century, this disorder was called hysteria, and in the 20th century it was called multiple personality disorder or multiple personality disorder. nine0011
This disorder is often mistaken for depression, anxiety, or psychosis. Long before our days, this condition was called possession, and it was treated with exorcism. In the 19th century, this disorder was called hysteria, and in the 20th century it was called multiple personality disorder or multiple personality disorder. nine0011
Types of dissociative identity disorder
There are several types of dissociative disorders, which are characterized by different symptoms and manifestations. One of them is dissociative fugue, a disorder in which a person can find himself in a completely unfamiliar place and not remember how he got there. In this case, a person may forget some important information about himself and not even remember his name. At the same time, memory for some information, such as literature, science, and other things, can be preserved. In a state of fugue, a person assumes a different personality and identity with a different character, mannerisms and behavior. While in this identity, a person can lead an outwardly normal life. A dissociative fugue can last for hours or years. After that, a person may find himself in a completely unfamiliar place and at the same time not remember anything that happened to him in a state of fugue. nine0011
While in this identity, a person can lead an outwardly normal life. A dissociative fugue can last for hours or years. After that, a person may find himself in a completely unfamiliar place and at the same time not remember anything that happened to him in a state of fugue. nine0011
A person who has a dissociative disorder is actually suffering a lot from their condition.
Another type of dissociative disorder is the presence of several personalities in which a person finds himself in turn or simultaneously. At such moments, he disconnects from himself and stops feeling his own body, and also cannot see himself from the outside. Personalities within a person can have different ages, genders, nationalities, mental abilities, temperaments, and behave in completely different ways. Often these personalities can even have different physiological manifestations. For example, while in one personality, a person can see poorly and wear glasses, and in another, have excellent vision and walk without glasses or lenses (or think that he sees perfectly and does without glasses). Just as in the case of dissociative fugue, when switching, one person cannot remember what happened to the person during immersion in another. nine0011
Just as in the case of dissociative fugue, when switching, one person cannot remember what happened to the person during immersion in another. nine0011
Manifestations of dissociative identity disorder
This disease affects both children (adolescents) and adults and presents with similar symptoms. However, dissociative disorder with multiple personalities in adolescents is quite rare. In old age, dissociation practically does not develop. When a specialist suspects a person of dissociative identity disorder, he usually asks if it happened that the person suddenly found himself in some place and did not understand how he got there. Also, the patient may suddenly speak in a completely different voice, he may have a different handwriting. For example, a person who has one of his personalities as a child may suddenly begin to write in a child's handwriting. Such phenomenal manifestations can be evoked in a patient suffering from dissociative personality disorder, and in a state of hypnosis.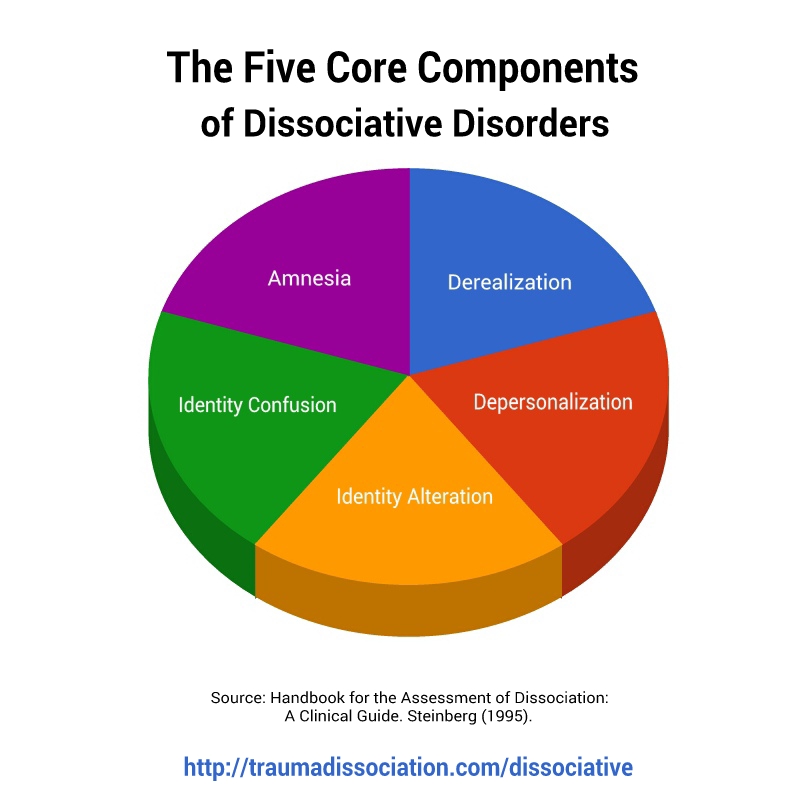 That is why the French psychiatrist Jean-Martin Charcot at one time mistakenly believed that hypnosis is a pathological condition that causes hysteria and the manifestation of multiple personalities. However, later it turned out that hypnosis is only superficially similar to dissociative personality disorder, but does not cause it, and the disease itself develops without any connection with hypnosis. nine0011
That is why the French psychiatrist Jean-Martin Charcot at one time mistakenly believed that hypnosis is a pathological condition that causes hysteria and the manifestation of multiple personalities. However, later it turned out that hypnosis is only superficially similar to dissociative personality disorder, but does not cause it, and the disease itself develops without any connection with hypnosis. nine0011
See also
Myths about hypnosis
A person who has a dissociative disorder is, in fact, very distressed by his condition. He sees the negative or dismissive attitude of those around him: they look at him strangely, they reject him, no one finds a common language with him, because of him the family can collapse, and so on. At the moment of a dissociative state, a person does not have the opportunity to critically look at himself and his own behavior. That is, in a situation where one of the alternative personalities appears, he is in an inadequate state. nine0011
nine0011
The main theory about the origin of this disease is based on the fact that in childhood such people experienced a traumatic situation, usually bullying or violence.
Dissociation is one of three conditions in which the patient is exempt from criminal liability, along with psychosis and mental retardation. There were cases when people in a dissociative state committed murder and rape. In such situations, even taking into account the severity of the crimes, patients are not sent to prison, but are sent to a psychiatric hospital or, in extreme cases, to a special ward of the psychiatric department of the prison. nine0011
Causes of dissociative identity disorder
Scientists have not yet found the genetic causes of dissociative identity disorder. The main theory about the origin of this disease is based on the fact that in childhood such people experienced a traumatic situation, usually bullying or violence. However, even this theory does not explain all 100% of cases of dissociative states.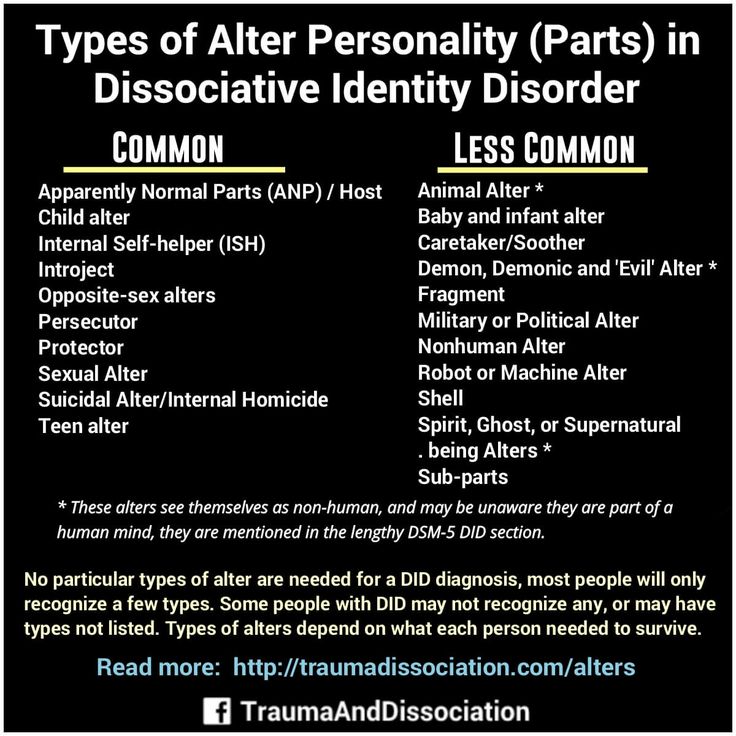 There are patients who, without an overt or identified traumatic situation in childhood, suffer from dissociative personality disorder. With regard to the physiological manifestations of this disorder, there is an assumption that in such patients certain areas of the brain stop working and others turn on. However, none of the theories suggesting physiological causes of dissociation currently explains all cases of the disease. nine0011
There are patients who, without an overt or identified traumatic situation in childhood, suffer from dissociative personality disorder. With regard to the physiological manifestations of this disorder, there is an assumption that in such patients certain areas of the brain stop working and others turn on. However, none of the theories suggesting physiological causes of dissociation currently explains all cases of the disease. nine0011
Diagnosis of dissociative identity disorder
Diagnosis of dissociative identity disorder is made through clinical interviews with several specialists. Sometimes the diagnosis requires not one, but several meetings with psychologists and psychiatrists, so that they have the opportunity to identify different aspects of the disorder, look at the patient's condition from several points of view and assemble a consultation. However, the specialist who identifies this disorder must have a great deal of experience and qualifications, since this disease can often be confused with others.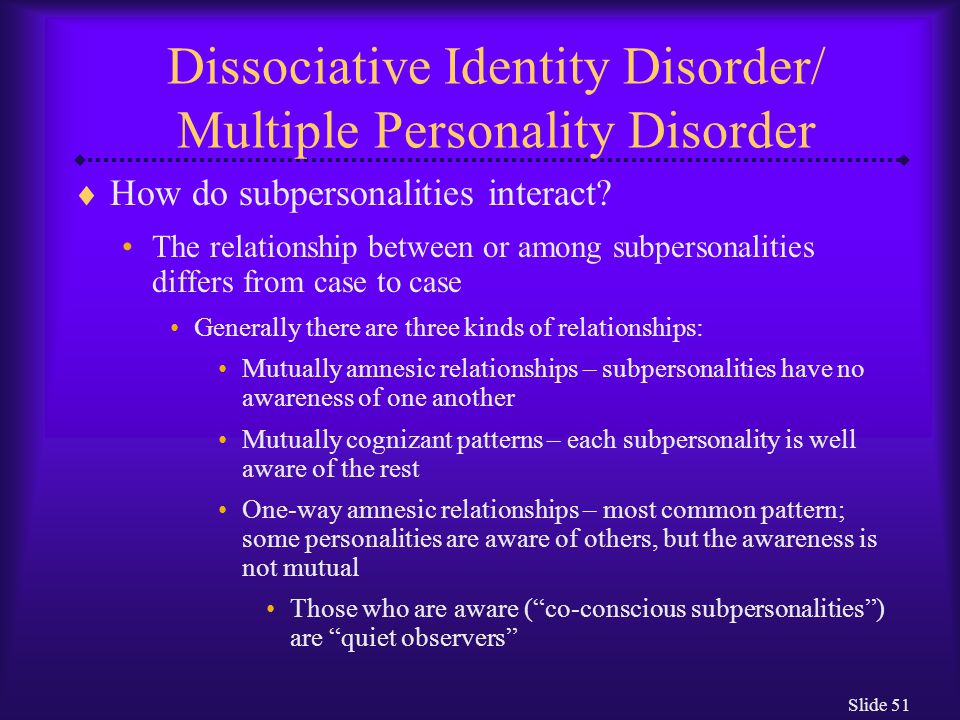 In its manifestations, it can be similar to depression, anxiety or psychosis. It is also common for patients with dissociative identity disorder to be diagnosed with schizophrenia. Dissociation is a rare disorder and not every mental health professional can diagnose this disorder. nine0011
In its manifestations, it can be similar to depression, anxiety or psychosis. It is also common for patients with dissociative identity disorder to be diagnosed with schizophrenia. Dissociation is a rare disorder and not every mental health professional can diagnose this disorder. nine0011
Medications do not cure dissociative identity disorder, but only relieve some of the symptoms.
See also
Mental norm and pathology
A separate task for a specialist in the process of diagnosing dissociation in a child is to distinguish diseases from the presence of imaginary friends in a child, which very often appear in perfectly healthy children at a certain age. To do this, a specialist must be highly qualified in the field of developmental psychology and clearly be able to recognize a dissociative disorder not only in adults, but also in children. nine0011
Treatment of dissociative identity disorder
The main treatment for dissociative identity disorder is hypnosis.