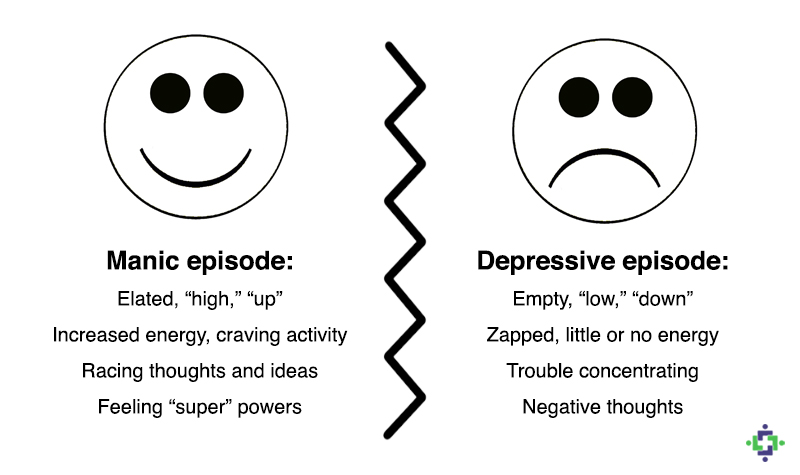
How to tell if someone is manic
Symptoms - Bipolar disorder - NHS
Bipolar disorder is characterised by extreme mood swings. These can range from extreme highs (mania) to extreme lows (depression).
Episodes of mania and depression often last for several weeks or months.
Depression
During a period of depression, your symptoms may include:
- feeling sad, hopeless or irritable most of the time
- lacking energy
- difficulty concentrating and remembering things
- loss of interest in everyday activities
- feelings of emptiness or worthlessness
- feelings of guilt and despair
- feeling pessimistic about everything
- self-doubt
- being delusional, having hallucinations and disturbed or illogical thinking
- lack of appetite
- difficulty sleeping
- waking up early
- suicidal thoughts
Mania
The manic phase of bipolar disorder may include:
- feeling very happy, elated or overjoyed
- talking very quickly
- feeling full of energy
- feeling self-important
- feeling full of great new ideas and having important plans
- being easily distracted
- being easily irritated or agitated
- being delusional, having hallucinations and disturbed or illogical thinking
- not feeling like sleeping
- not eating
- doing things that often have disastrous consequences – such as spending large sums of money on expensive and sometimes unaffordable items
- making decisions or saying things that are out of character and that others see as being risky or harmful
Patterns of depression and mania
If you have bipolar disorder, you may have episodes of depression more regularly than episodes of mania, or vice versa.
Between episodes of depression and mania, you may sometimes have periods where you have a "normal" mood.
The patterns are not always the same and some people may experience:
- rapid cycling – where a person with bipolar disorder repeatedly swings from a high to a low phase quickly without having a "normal" period in between
- mixed state – where a person with bipolar disorder experiences symptoms of depression and mania together; for example, overactivity with a depressed mood
If your mood swings last a long time but are not severe enough to be classed as bipolar disorder, you may be diagnosed with a mild form of bipolar disorder called cyclothymia.
Living with bipolar disorder
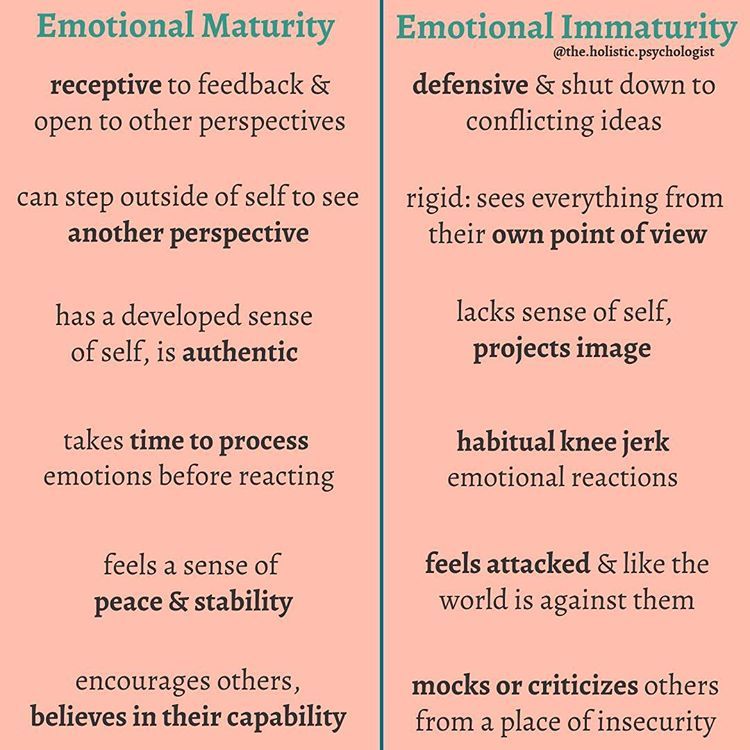
Bipolar disorder is a condition of extremes. A person with bipolar disorder may be unaware they're in the manic phase.
After the episode is over, they may be shocked at their behaviour. But at the time, they may believe other people are being negative or unhelpful.
Some people with bipolar disorder have more frequent and severe episodes than others.
The extreme nature of the condition means staying in a job may be difficult and relationships may become strained. There's also an increased risk of suicide.
During episodes of mania and depression, someone with bipolar disorder may experience strange sensations, such as seeing, hearing or smelling things that are not there (hallucinations).
They may also believe things that seem irrational to other people (delusions). These types of symptoms are known as psychosis or a psychotic episode.
Find out more about living with bipolar disorder
Page last reviewed: 14 March 2019
Next review due: 14 March 2022
What Is It, Causes, Triggers, Symptoms & Treatment
Overview
What is mania?
Mania is a condition in which you have a period of abnormally elevated, extreme changes in your mood or emotions, energy level or activity level. This highly energized level of physical and mental activity and behavior must be a change from your usual self and be noticeable by others.
This highly energized level of physical and mental activity and behavior must be a change from your usual self and be noticeable by others.
What's considered an “abnormal,” extreme change in behavior and what does it look like?
Abnormal manic behavior is behavior that stands out. It’s over-the-top behavior that other people can notice. The behavior could reflect an extreme level of happiness or irritation. For example, you could be extremely excited about an idea for a new healthy snack bar. You believe the snack could make you an instant millionaire but you’ve never cooked a single meal in your life, don’t know a thing about how to develop a business plan and have no money to start a business. Another example might be that you strongly disagree with a website “influencer” and not only write a 2,000 word post but do an exhaustive search to find all the websites connected to the influencer so you can post your letter there too.
Although these examples may sound like they could be normal behavior, a person with mania will expend a great deal of time and energy including many sleepless nights working on projects such as these.
What is a manic episode?
A manic episode is a period of time in which you experience one or more symptoms of mania and meet the criteria for manic episode (see “symptoms” and “diagnosis” sections). In some cases, you may need to be hospitalized.
Can I have a manic episode as its own condition or is it always part of another mental health condition?
Technically if you have a manic episode, you have a mental health condition. Mania can be a part of several mental health conditions including:
- Bipolar I disorder (most common condition for mania to occur).
- Seasonal affective disorder.
- Postpartum psychosis.
- Schizoaffective disorder.
- Cyclothymia.
What is bipolar I disorder?
Bipolar I disorder is a mental health illness in which a person has major high and low swings in mood, activity, energy and ability to think clearly. To be diagnosed with bipolar I disorder, you have to have at least one episode of mania that lasts for at least seven days or have an episode that is so severe that it requires hospitalization.
Most people have both episodes of both mania and depression, but you don’t have to have depression to be diagnosed with mania. Many people with a bipolar I disorder diagnosis have recurring, back-to-back manic episodes with very few episodes of depression.
What are the triggers of manic episodes?
Manic episode triggers are unique to each person. You’ll have to become a bit of a detective and monitor your mood (even keeping a “mood diary”) and start to track how you feel before an episode and when it occurs. Ask family and close friends who you trust and have close contact with to help identify your triggers. As outside observers, they may notice changes from your usual behavior more easily than you do.
Knowing your triggers can help you prepare for an episode, lessen the effect of an episode or prevent it from happening at all.
Common triggers to be aware of include:
- A highly stimulating situation or environment (for example, lots of noise, bright lights or large crowds).
- A major life change (such as divorce, marriage or job loss).
- Lack of sleep.
- Substance use, such as recreational drugs or alcohol.
What happens after a manic episode?
After a manic episode you may:
- Feel happy or embarrassed about your behavior.
- Feel overwhelmed by all the activities you’ve agreed to take on.
- Have only a few or unclear memories of what happened during your manic episode.
- Feel very tired and need sleep.
- Feel depressed (if your mania is part of bipolar disorder).
Symptoms and Causes
What are the symptoms of mania?
Symptoms of a manic episode
- Having an abnormally high level of activity or energy.
- Feeling extremely happy or excited — even euphoric.
- Not sleeping or only getting a few hours of sleep but still feeling rested.
- Having an inflated self-esteem, thinking you’re invincible.
- Being more talkative than usual.
 Talking so much and so fast that others can’t interrupt.
Talking so much and so fast that others can’t interrupt. - Having racing thoughts — having lots of thoughts on lots of topics at the same time (called a “flight of ideas”).
- Being easily distracted by unimportant or unrelated things.
- Being obsessed with and completely absorbed in an activity.
- Displaying purposeless movements, such as pacing around your home or office or fidgeting when you’re sitting.
- Showing impulsive behavior that can lead to poor choices, such as buying sprees, reckless sex or foolish business investments.
Psychotic symptoms of a manic episode
- Delusions. Delusions are false beliefs or ideas that are incorrect interpretations of information. An example is a person thinking that everyone they see is following them.
- Hallucinations. Having a hallucination means you see, hear, taste, smell or feel things that aren’t really there. An example is a person hearing the voice of someone and talking to them when they’re not really there.

How long does a manic episode last?
Early signs (called “prodromal symptoms”) that you’re getting ready to have a manic episode can last weeks to months. If you’re not already receiving treatment, episodes of bipolar-related mania can last between three and six months. With effective treatment, a manic episode usually improves within about three months.
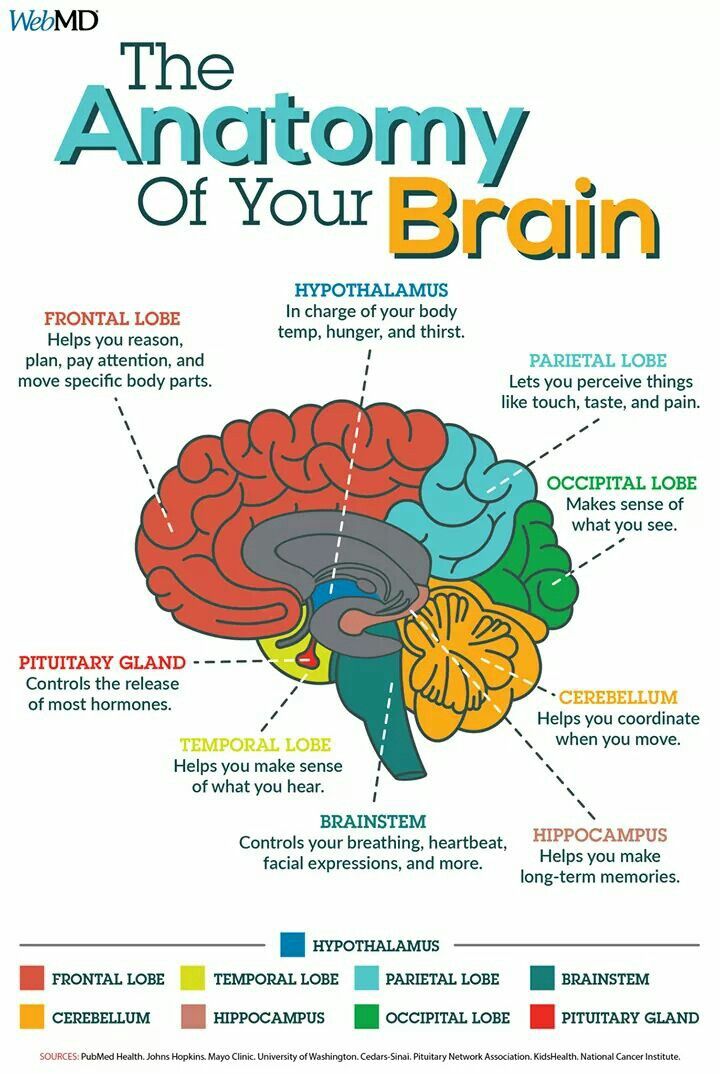
What causes mania?
Scientists aren’t completely sure what causes mania. However, there are several factors that are thought to contribute. Causes differ from person to person.
Causes may include:
- Family history. If you have a family member with bipolar illness, you have an increased chance of developing mania. This isn't definite though. You may never develop mania even if other family members have.
- A chemical imbalance in the brain.
- A side effect of a medication (such as some antidepressants), alcohol or recreational drugs.
- A significant change in your life, such as a divorce, house move or death of a loved one.
- Difficult life situations, such as trauma or abuse, or problems with housing, money or loneliness.
- A high level of stress and an inability to manage it.
- A lack of sleep or changes in sleep pattern.
- As a side effect of mental health problems including seasonal affective disorder, postpartum psychosis, schizoaffective disorder or other physical or neurologic condition such as brain injury, brain tumors, stroke, dementia, lupus or encephalitis.
Diagnosis and Tests
How is mania diagnosed?
Your healthcare provider will ask about your medical history, family medical history, current prescriptions and non-prescription medications and any herbal products or supplements you take. Your provider may order blood tests and body scans to rule out other conditions that may mimic mania. One such condition is hyperthyroidism. If other diseases and conditions are ruled out, your provider may refer you to a mental health specialist
To be diagnosed with mania, your mental health specialist may follow the criteria of the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders, DSM-5. Their criteria for manic episode is:
Their criteria for manic episode is:
- You have an abnormal, long-lasting elevated expression of emotion along with a high degree of energy and activity that lasts for at least one week and is present most of the day, nearly every day.
- You have three or more symptoms to a degree that they’re a noticeable change from your usual behavior (four symptoms if mood is only irritable). (See the symptoms section of this article for a list of the symptoms used as criteria.)
- The mood disturbance is severe enough to cause significant harm to your social, work or school functioning or there’s a need to hospitalize you to prevent you from harming yourself or others, or you have psychotic features, such as hallucinations or delusions.
- The manic episode can’t be caused by the effects of a substance (medications or drug abuse) or another medical condition.
Management and Treatment
How is mania treated?
Mania is treated with medications, talk therapy, self-management and family and friends support.
Medications
If you have mania only, your healthcare provider may prescribe an antipsychotic medication, such as ariprazole (Abilify®), lurasidone (Latuda®), olanzapine (Zyprexa®), quetiapine (Seroquel®) or risperridone (Risperdal®).
If you have mania as part of a mood disorder, your provider may add a mood stabilizer. Some examples include lithium, valproate (Depakote®) and carbamazepine (Tegretol®). (If you’re pregnant or plan to become pregnant, let your provider know. Valproate can increase the chance of birth defects and learning disabilities and shouldn’t be prescribed to individuals who are able to become pregnant.)
Sometimes antidepressants are also prescribed.
Talk therapy (psychotherapy)
- Psychotherapy involves a variety of techniques. During psychotherapy, you’ll talk with a mental health professional who'll help you identify and work through factors that may be triggering your mania and/or depression (if you’re diagnosed with bipolar I disorder).
- Cognitive behavioral therapy can be useful in helping you change inaccurate perceptions that you have about yourself and the world around you.
- Family therapy is important since it’s very helpful for your family members to understand your behavior and what they can do to help.
Ask your provider for contact information for local support groups. You might find it helpful to talk with other people who have similar medical experiences and share problems, ideas for coping and strategies for living and caring for yourself.
Other treatments
Electroconvulsant therapy (ECT) may be considered in rare cases in individuals who have severe mania or depression (if bipolar). ECT involves applying brief periods of electric current to your brain.
Prevention
What steps can I take to better cope with or manage my mania?
Although episodes of mania can’t always be prevented, you can make a plan to better manage your symptoms and prevent them from getting worse when you feel a manic episode may be starting.
Some ideas to try during this time include:
- Avoid stimulating activities and environment – such as loud or busy places or bright places. Instead choose calm and relaxing activities and environments.
- Stick to routines. Go to bed at a set time, even if you’re not tired. Also, stick to the same times for eating meals, taking medications and exercising.
- Limit the number of social contacts to keep you from getting too stimulated and excited.
- Postpone making any major life decisions and big purchases.
- Avoid people and situations that might tempt you to make poor or risky choices, such as taking recreational drugs or drinking alcohol.
- Consider selecting someone to manage your finances during a manic episode.
If you ever have thoughts of harming yourself, tell family or friends, call you healthcare provider or contact the National Suicide Prevention Lifeline at 800-273-(TALK) (1-800-273-8255). Counselors are available 24/7.
Outlook / Prognosis
What outcome can I expect if I’ve been diagnosed with mania?
If your mania is related to a diagnosis of bipolar I disorder, this is a lifelong disease. Although there’s no cure for mania, medication and talk therapy (psychotherapy) can manage your condition in most cases.
Living With
How can I involve family and friends in understanding my mania?
It’s important to have an honest conversation with your family and closest friends.
- Let your family and friends know what you do and don’t find helpful. For example, if you’d appreciate a friendly reminder about taking your daily medications or a question about if you are getting enough sleep, let them know. On the other hand, if you don’t like always being asked if your current state of happiness is a sign you’re having a manic episode, discuss this.
- Ask your family and friends if they can help identify your triggers if you can’t. They may be able to spot triggers that you can’t spot yourself.
 Ask what they’ve noticed or any patterns they may see around the times of your episodes. As soon as you recognize an early sign, make an appointment to see your healthcare provider. You may or may not need a medication adjustment. However, it’s good to be on the alert since your symptoms could rapidly change.
Ask what they’ve noticed or any patterns they may see around the times of your episodes. As soon as you recognize an early sign, make an appointment to see your healthcare provider. You may or may not need a medication adjustment. However, it’s good to be on the alert since your symptoms could rapidly change. - Describe how your symptoms feel to you. Your family and friends will have a better understanding of your condition.
- Let family and friends know what type of help you’d like from them and when you’d like it. There may be times when you feel you can cope on your own. Knowing the difference will be helpful for everyone.
Frequently Asked Questions
What is acute mania?
Acute mania is the manic phase of bipolar I disorder. It is defined as an extremely unstable euphoric or irritable mood along with excess activity or energy level, excessively rapid thought and speech, reckless behavior and feeling of invincibility.
What is unipolar mania?
Unipolar mania is a disorder in which only excitement, excess activity or energy level and euphoric symptoms are seen. This is a rare condition.
What’s the difference between mania and hypomania?
Hypomania is a less severe form of mania. The criteria that healthcare professionals use to make the diagnosis of either hypomania or mania is what sets them apart. The differences between these two conditions is as follows:
| Mania | Hypomania | |
|---|---|---|
| How long the episode lasts. | At least one week. | At least four consecutive days. |
| Severity of episode. | Causes severe impact on social or work/school functioning. | Not severe enough to significantly affect social or work/school functioning. |
| Need for hospitalization. | Possibly. | No. |
| Psychotic symptoms present (delusions or hallucinations). | Is among possible symptoms. | Can’t be present for a diagnosis of hypomania. |
Can my diagnosis change between bipolar I disorder and bipolar II disorder?
No. Once you have a diagnosis of bipolar I disorder — even if you never have another manic episode or a psychotic event (delusions or hallucinations) — your diagnosis can never be changed to bipolar II disorder. You’ll always have a bipolar I disorder diagnosis.
A note from Cleveland Clinic
Problems can develop in your social life, work/school functioning and home life when you have symptoms of mania, which include mood swings and an abnormal level of energy and activity. You may require hospitalization if you have severe hallucinations or delusions, or to prevent you from harming yourself or others. It’s important to have a good understanding of mania, mania symptoms, your particular triggers and ways to better manage your manic episodes. Medications, talk therapy and support groups as well as support from your family and friends can help manage your mania. Stay in close contact with all your healthcare providers, especially during times of manic episodes. Your provider will want to see you and may need changes to your medications or dose.
Stay in close contact with all your healthcare providers, especially during times of manic episodes. Your provider will want to see you and may need changes to your medications or dose.
What is mania and hypomania. how to understand that you have a bipolar disorder
The statistics are relentless: every year there are more and more people with mental disorders. You should not be afraid, since most conditions can be corrected with modern medicines. One of these disorders is manic syndrome, which most often coexists with depressive phases within the framework of bipolar disorder, whose obsolete name is manic-depressive psychosis. nine0003
Irina Ivashkova
Manic episodes may last a week or more, and manic episodes may be punctuated by periods of depression during which you may feel tired, sad, and hopeless. While manic episodes are most common in people with bipolar disorder, there are other causes for these extreme changes in behavior and mood.
Article content
What is mania? nine0012
A manic episode is characterized by a prolonged period of abnormally elevated or irritable mood, intense energy, racing thoughts, and other extreme and exaggerated behaviors. People may also experience psychoses, including hallucinations and delusions, which indicate a disconnect from reality.
People may also experience psychoses, including hallucinations and delusions, which indicate a disconnect from reality.
In addition to the "pure" variant of the manic syndrome, there are variants in which one of the signs is less or more pronounced. For example, hypomania is a condition in which all three symptoms are present, but do not reach the level of a disorder, that is, they do not disrupt the behavior and social functioning of a person and are not combined with psychotic disorders. nine0003
Symptoms of mania
Recognizing the symptoms of mania is not only important for diagnosis. Symptoms of a manic episode can be a medical emergency, as can symptoms of shortness of breath, chest pain, or bleeding from other illnesses.
When attempting to identify a possible manic episode, it is important to consider the person's typical behavior because an important element of mania is that it represents a change from normal behavior. This will allow you to seek medical help as soon as possible. nine0003
This will allow you to seek medical help as soon as possible. nine0003
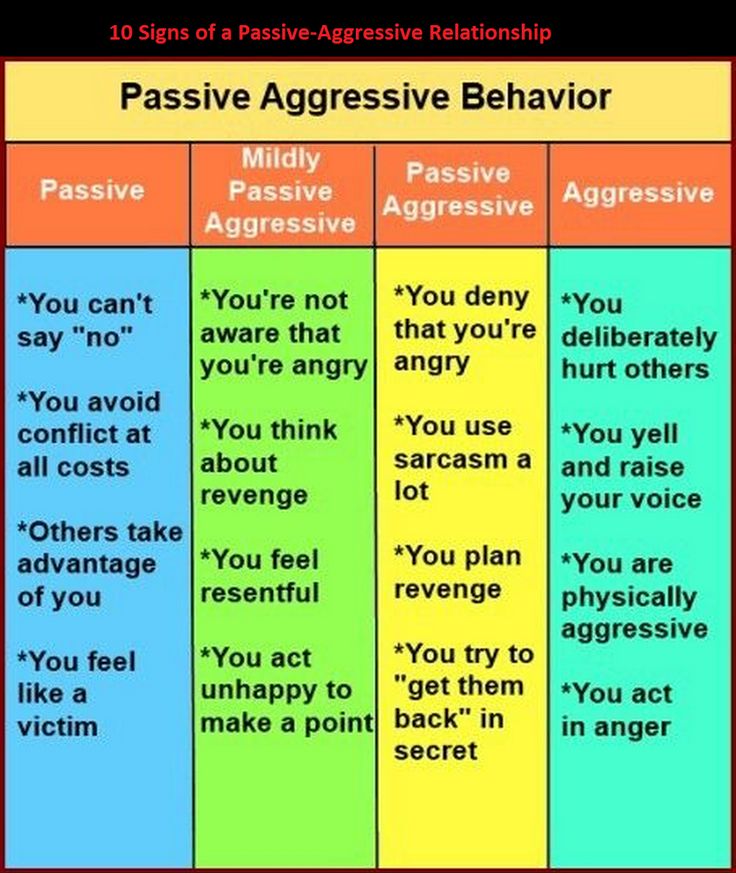
A manic episode is illustrated by such manifestations as:
Reduced need for sleep (went to bed at 4, woke up at 8 full strength) is often observed when symptoms of mania appear. Sleep problems and bipolar disorder can feed off each other, with manic episodes leading to sleep problems and vice versa.
Many activities at the same time. During a manic episode, you may be restless looking for ways to release excess energy. People often take on multiple projects or experience a performance spike that goes beyond what they would normally achieve over a given period of time. nine0003
Talks a lot, quickly and aggressively. This is a common symptom at the onset of a manic or hypomanic episode. It is important to note that in order to be classified in this category, speech must represent a deviation from ordinary human speech. Some people always speak faster than others.
Some people always speak faster than others.
Hypersexuality is a common manic or hypomanic symptom and can manifest itself in uncharacteristic or risky sexual behavior such as seeking out sex workers, watching porn, etc. nine0003
Increase in risk behaviors. A person experiencing a manic episode may suddenly begin to overspend and gamble.
Quick thinking. Notice if your friend or family member complains that his thoughts are racing around uncontrollably. Outwardly, a person with bipolar disorder may appear to be speaking smoothly and pleasantly, while on the inside they have repetitive, restless thoughts. Don't be afraid to ask what they mean if they say their mind is racing. nine0003
Flight of ideas. For a person entering the manic phase of bipolar disorder, the flight of ideas can be difficult to follow. If you find it difficult to logically comprehend the course of the discussion, pay attention to it. It might sound something like this: “I wonder what the weather will be like tomorrow. What is the purpose of life? Oh, I forgot to feed the cat." We all have moments when our words form an illogical sequence. It's important to notice changes in how your loved one communicates their ideas. nine0003
It might sound something like this: “I wonder what the weather will be like tomorrow. What is the purpose of life? Oh, I forgot to feed the cat." We all have moments when our words form an illogical sequence. It's important to notice changes in how your loved one communicates their ideas. nine0003
Grandeur . Be on the lookout if your friend or loved one develops megalomaniacs, such as making statements like "Justin Bieber is sending me love letters" or "We're supposed to move to Yemen this weekend, I've been named president there." Grandiosity is often experienced by people with bipolar disorder during the manic or hypomanic phase. It is important to note that megalomania is absent in hypomania, but grandiose thinking such as "I'm going to quit my job and write a novel" is a possible symptom of hypomania. Context matters. If this comment is made by a novice writer, it may be quite normal. But the very same words spoken by someone who doesn't like to write and has never talked about writing a novel before are suspicious. nine0003
nine0003
Hostility and/or irritability. Beware of these manifestations, be careful and seek help if your loved one suddenly began to behave this way. Don't try to handle the situation on your own.
Suicidal thoughts. In some cases, a manic episode can lead to feelings of hopelessness or worthlessness, as well as thoughts of death or suicide.
Excessive religiosity. Increased religious zeal or involvement may be another manic symptom. Pay attention to this if you see it. nine0003
Bright clothes. During a manic or hypomanic episode, a person is more likely to wear bright and even flashy clothing. Of course, most people who wear bright colors do not experience a manic or hypomanic episode. But clothing can be a subtle clue if the choice of something bright is matched by others. Changes in clothing style, such as a preference for more revealing clothing, may also reflect other symptoms such as hypersexuality.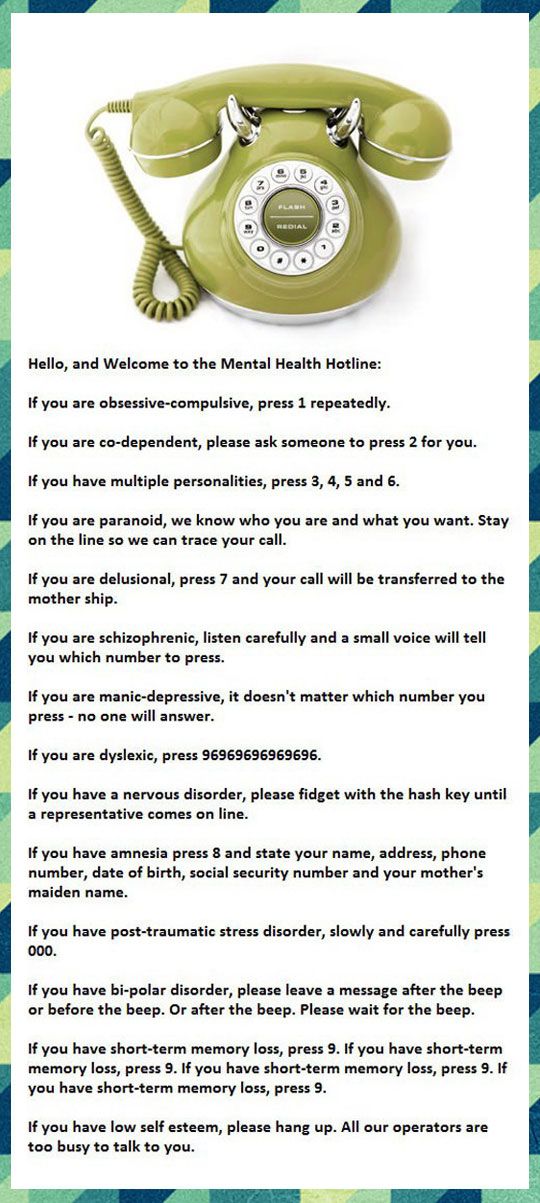 nine0003
nine0003
To summarize: For bipolar disorder to be diagnosed with a manic episode, a person must have a sustained and abnormally elevated, expansive, or irritable mood for at least one week and at least three of the following symptoms.
Causes of mania and hypomania
Manic episodes are often found in people with BIPO -wil but they can also be caused by other factors and health conditions, including:
- Childbirth (postpartum psychosis),
- Brain injury,
Psychotherapy with a qualified therapist can help you identify when your mood changes and the triggers that lead to manic episodes.
 They can also teach medication rules and skills to manage these episodes and improve quality of life.
They can also teach medication rules and skills to manage these episodes and improve quality of life. Support is an important part of managing manic episodes, so you might consider joining a support group for people with bipolar disorder if you lack the resources of friends and family. nine0003
In addition to medication and therapy, a few relatively simple lifestyle changes can help manage a manic episode and prevent more. Talk to your healthcare provider about other complementary methods that may be right for you.
- Make time for exercise. Do your best to get some physical activity every day.
- Eat a balanced diet and avoid skipping meals. nine0084
- Focus on good sleep hygiene, including maintaining a consistent sleep-wake cycle (even on weekends).
Do you have signs of mental disorders?
How to recognize a mental disorder by the way you communicate
April 4, 2021 Health
Be attentive to the little things: sometimes a person's strange behavior is nothing but the symptoms of a disease.
Depression
According to WHO, depression is the most common mental illness, affecting more than 300 million people worldwide. With depression, there is a persistent decrease in mood and self-esteem, loss of interest in life and former hobbies, pessimism, sleep and appetite disorders. nine0003
The speech of a depressed person has its own characteristics:
- Quiet voice.
- Lack of desire to carry on a conversation.
- Long thought before answering, lethargy, careful choice of words.
- Frequent use of words with a negative connotation ("lonely", "sad", "unhappy"), the pronoun "I" and words expressing totality ("always", "nothing", "entirely").
In addition, there is the concept of masked depression, when a person hides his problems and tries to appear happy. Recognizing the disorder in this case is not easy: the interlocutor will always deny all life's difficulties. Can make jokes about suicide. nine0003
Lyutsina Lukyanova
psychotherapist, chief physician of the medical center "Shchastia"
Masked depression is harder to recognize.
 Such patients will try not to touch on topics that are problematic for them in the dialogue, to emphasize that everything is fine in their life. But as soon as we start talking about the areas where they are experiencing difficulties, we will see despondency on their faces and hear phrases: “Where should I hurry? I can do everything, I have my whole life ahead of me.”
Such patients will try not to touch on topics that are problematic for them in the dialogue, to emphasize that everything is fine in their life. But as soon as we start talking about the areas where they are experiencing difficulties, we will see despondency on their faces and hear phrases: “Where should I hurry? I can do everything, I have my whole life ahead of me.” Bipolar affective disorder (BAD)
Bipolar affective disorder, or manic-depressive psychosis, is another mental illness associated with mood changes. It affects about 60 million people in the world. The life of such people goes in two modes: mania (or hypomania - its mild form) and depression. The duration of each period is individual and unpredictable, it can range from several days to several months.
Alexandra Shvets
Candidate of Medical Sciences, Neurologist at the Ekaterininskaya Clinic
A characteristic feature is the change of phases: increased mood or desire to move, do something, create, commit and depression, apathy, despondency, impotence, indifference.
 The moment when the phase change will come is impossible to predict.
The moment when the phase change will come is impossible to predict. The manic phase is characterized by an incredible rise in mood and strength, increased activity, including sexual activity. There is so much energy that a person stops sleeping and eating, he is busy all the time. The speech of the patient in the manic phase is characterized by the following features:
- Excessive talkativeness. The person is agitated, jumping from one thought to another.
- Bragging, confidence in oneself and in the feasibility of one's plans. The person says that he is ready to move mountains and complete many different projects.
- Delusional ideas (appear in special cases). For example, the patient may say that everyone envy him and want to harm him.
The depressive phase is accompanied by a decline in strength, self-esteem, sexual desire, loss of interest in former hobbies and life in general. The person is depressed, inhibited, does not want to communicate with anyone.
 In severe cases, he plans suicide. nine0003
In severe cases, he plans suicide. nine0003 Generalized anxiety disorder
One third of the world's population is affected by this disease. A person constantly experiences anxiety and anxiety, suffers from unpleasant sensations in the body: trembling, sweating, dizziness, discomfort in the solar plexus area. Anxiety is usually caused by a variety of fears related to the future.
Among the features of communication:
- Stories about their own fears. A person is afraid to either fly on an airplane, or sit in an elevator, or communicate, or go into unfamiliar places. nine0084
- Constant indignation and complaints, including about the state of health.
Often these are lonely people who have not achieved success in their personal life and work. Often they are outraged by something: the leadership of the country or the company where they work, the situation in the state or at home - everything that they encounter in life.
Lyutsina Lukyanova
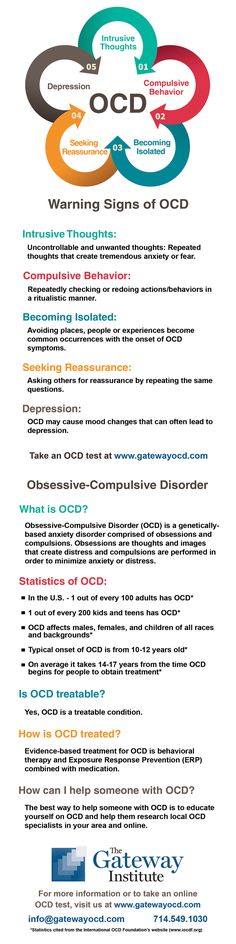
Obsessive Compulsive Disorder (OCD)
Another disease associated with anxiety.
 With it, the patient has obsessive frightening thoughts that he is not able to fight. To get rid of anxiety, a person performs some kind of ritual: spits over his left shoulder, checks all the locks in the house, washes his hands, and so on. These actions may seem pointless, but they help the patient to relieve the condition for a short time. nine0003
With it, the patient has obsessive frightening thoughts that he is not able to fight. To get rid of anxiety, a person performs some kind of ritual: spits over his left shoulder, checks all the locks in the house, washes his hands, and so on. These actions may seem pointless, but they help the patient to relieve the condition for a short time. nine0003 A person with OCD can be recognized by the same signs in speech as those with generalized anxiety disorder. These are complaints, suspiciousness, repeated talk about fears. However, it will be much more effective to observe his behavior, to track the ritual. A typical OCD patient is the American inventor Howard Hughes, about whose life the movie The Aviator was made. He constantly washed his hands because he was afraid of catching an infection.
OCD patients are very difficult to identify by phrases in speech, the exception is if the person himself wants to tell you about what worries him. It is not difficult to notice them if you watch people in the park, for example.
 nine0003
nine0003 Lutsina Lukyanova
Post-traumatic stress disorder (PTSD)
The disorder may occur after a traumatic situation, most often associated with a threat to life. Those who become ill are victims of sexual or other violence, terrorist attacks, participants in hostilities. They try to avoid conversations, places and situations that may remind them of the events they have experienced, but the memories keep returning them there. In especially severe cases, the patient can force the event out of memory, as if to forget. nine0003
Patients with PTSD suffer from both depressive and anxiety symptoms, so their speech can contain the same signs as those of patients with depression or anxiety disorder.
It is difficult to notice something from their statements, because they try not to communicate with anyone, living in their experiences. But if the dialogue does take place, then you will not hear a word about happiness, joy or love. An interlocutor with PTSD will either be laconic, or devote his story to the misfortune that happened to him.
 nine0003
nine0003 Lutsina Lukyanova
Schizophrenia
According to WHO, 23 million people worldwide suffer from schizophrenia. This is a serious mental illness, which is accompanied by a violation of thinking, perception of reality, emotions, speech and behavior. Patients do not have a critical attitude to their condition, in most cases they are sure that they are healthy. A typical example is the mathematician and Nobel laureate in economics John Nash, about whose life the film A Beautiful Mind was made.
Schizophrenia can be recognized by the following features:
- Suspiciousness and paranoia. A person can be sure that he is being persecuted or they want to harm him.
- Grandiose ideas and plans.
- Crazy ideas. The patient may think that the world has long been captured by aliens.
- Inability to engage in dialogue and formulate thoughts. They either break off somewhere in the middle of a sentence (sperrung), or consist of a random collection of words (verbal okroshka).