Ocd depression anger
OCD and Anger: Causes, Treatment, and How to Deal
OCD and anger often go hand in hand. Here’s how to channel your frustration in healthy ways — or help a loved one.
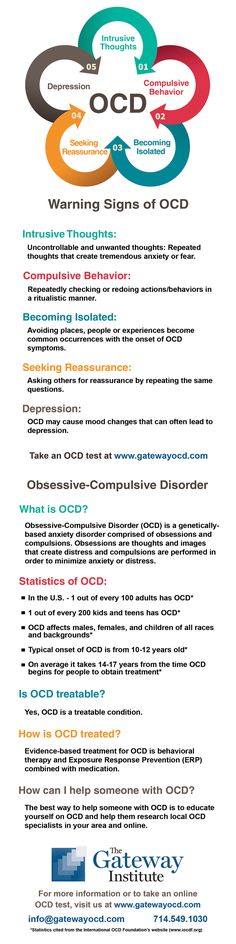
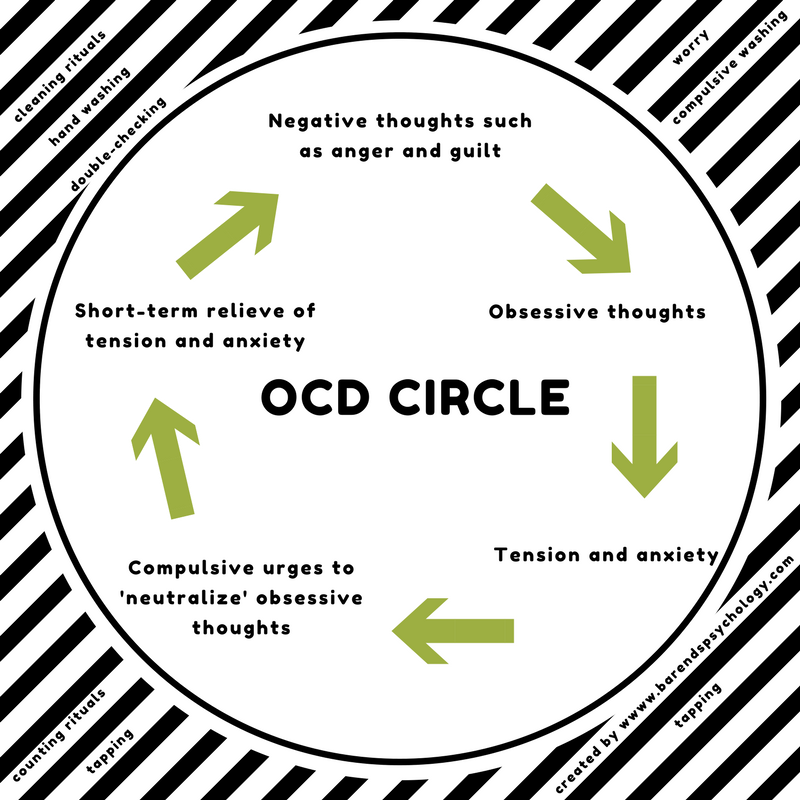
People with obsessive-compulsive disorder (OCD) have unrelenting, invasive thoughts (obsessions) and can act in ways they feel unable to control (compulsions).
For example, they might worry obsessively about having secured their house safely or turned off their stove. They might feel compelled to perform certain rituals in the same order or pray excessively to prevent harm.
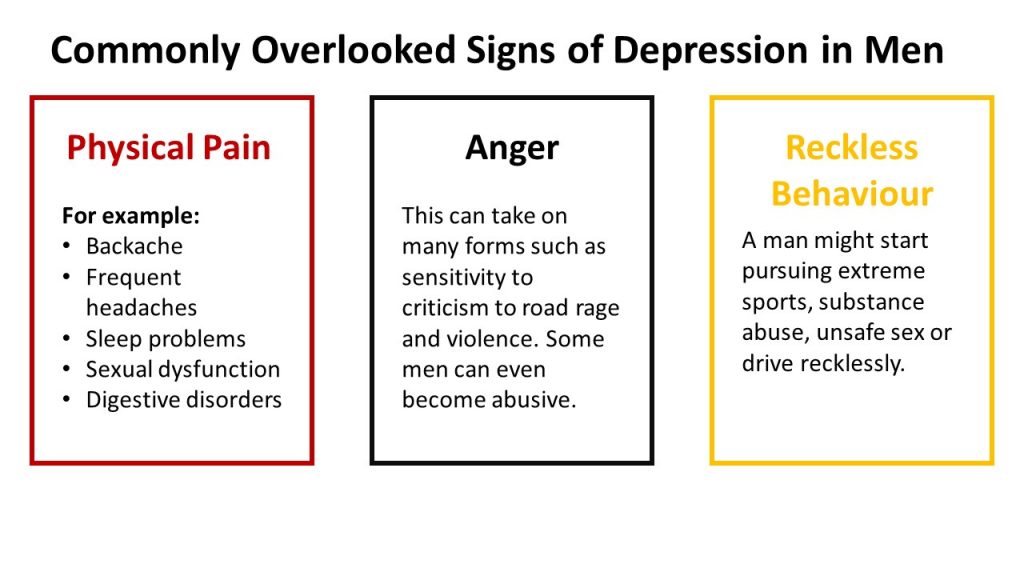
People with OCD can also experience episodes of anger. OCD is a chronic, distressing condition, so feeling angry makes sense. In fact, anger is a common human emotion that everyone experiences.
But intense anger, particularly when it turns into aggression, can be distressing for people with OCD and their loved ones.
The good news is that you can absolutely manage out-of-control anger in healthy ways, and you can support a loved one by managing it, too. Here’s how.
Some research suggests that anger episodes may be more common in OCD. For example, this 2011 study found that out of 42 adults with OCD attending an outpatient clinic, 21 reported experiencing angry outbursts in which they:
- yelled at others
- threatened to hurt others
- acted aggressively
- threatened to leave
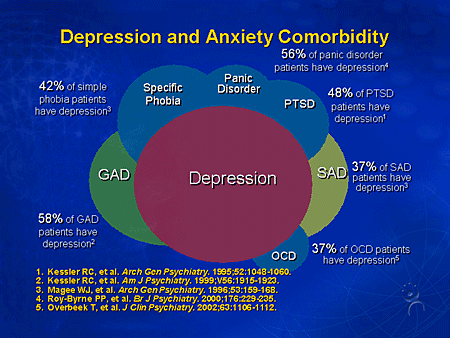
In the same study, people who experienced anger episodes also experienced more panic attacks and had more severe depression.
This 2019 study of 90 Chinese people with OCD found that around 31% had experienced at least one anger outburst in the past week. In this 2020 German study, people living with OCD also reported more anger than people without the disorder.
Anger may also occur in children with OCD.
For example, this 2012 study found that anger attacks were relatively common in children ages 6 to 16 with OCD. Researchers also found that anger attacks were associated with more severe symptoms and impairment.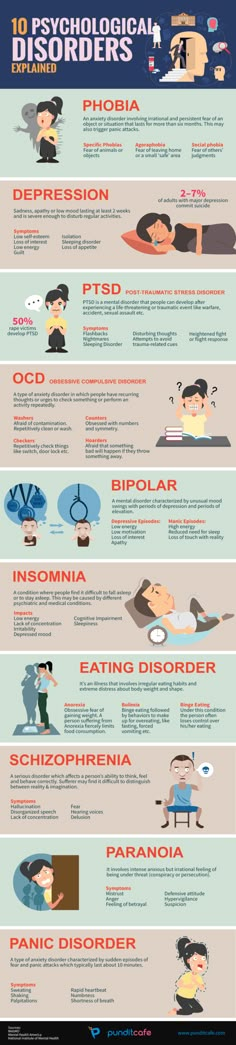
This 2015 study found similar results with increased anger in children with OCD and more intense symptoms. According to the study, the anger also took a toll on caregivers and led to poorer relationships with parents, siblings, relatives, and peers.
The link between OCD and anger is complicated and multilayered. Some people with OCD may become angry at having to live with such a difficult disorder. Others may experience anger as part of their obsessions or compulsions.
If you live with OCD and experience intrusive violent thoughts, it’s important to remember that there’s no such thing as a thought crime, and just because you think it doesn’t mean it’s going to happen.
A wide range of factors can spark anger outbursts in adults and children with OCD. These can include:
- loved ones not accommodating compulsive behaviors, which can also lead to profound fear
- others not understanding or minimizing what it’s like to have OCD
- interruptions that prevent performing rituals or performing them perfectly
- frustration with having OCD
- having to suppress feelings of anger
- negative reactions to medication
- symptoms of OCD, such as having to perform compulsions perfectly and constantly having unwanted, upsetting thoughts
- prolonged levels of anxiety and stress
- PANDAS, which stands for ‘pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections’ — a strep infection in children that triggers or worsens OCD by causing mood changes and irritability
OCD can affect people of every race, from children to adults.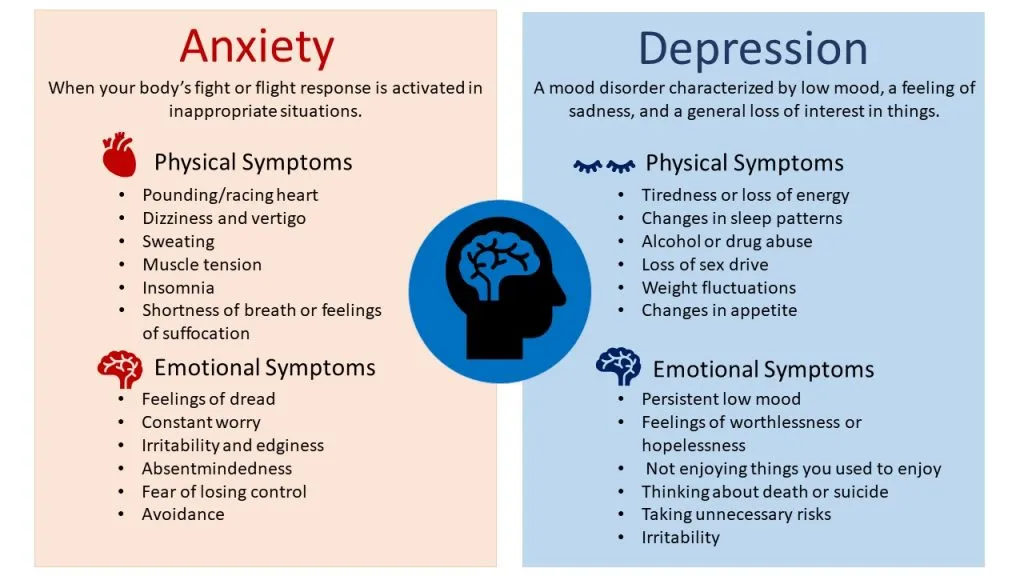 While both diagnosis and treatment options are widely available, there can be disparities in what people experience.
While both diagnosis and treatment options are widely available, there can be disparities in what people experience.
Barriers to treatment are an especially significant challenge for African Americans and other historically marginalized groups who, according to research, are less likely to access psychological and psychiatric services and are less likely to receive effective treatment for OCD.
Affordable options, available mental health professionals, and community education are noted as obstacles.
In OCD, the level, intensity, and specific behaviors of an anger episode can vary from person to person. Some people may express anger in destructive ways, while others internalize their anger instead. Some may do both.
During an anger episode, adults or children with OCD may:
- yell
- swear
- make hurtful remarks
- throw things
- hurt themselves
- hurt others
Often, people with OCD turn their anger inward, which may include:
- having thoughts of self-harm or suicide
- having feelings of self-hatred or worthlessness
- withdrawing from loved ones
If you’re witnessing an angry outburst, it can understandably be concerning. However, it can be helpful to remember that a person with OCD is dealing with a lot.
However, it can be helpful to remember that a person with OCD is dealing with a lot.
So, even though they’re directing their anger toward you, their frustration may really stem from what they’re experiencing.
Of course, this doesn’t make it OK for anyone to become violent. If that happens, consider the below resources for immediate help.
Everyone experiences anger from time to time. Again, anger is a natural — even necessary — emotion. For example, anger tells you when someone is crossing your boundaries. Anger is also a signal that you may need to make some important changes.
To better understand the link between your OCD and anger, consider these questions:
- On a daily basis, when do I feel the most frustration?
- When do I feel the least frustration?
- In the last month or week, why did I get angry with someone?
- Were there early signs that my anger was building?
- What emotions or experiences might be underlying my anger, such as loneliness, shame, or sadness?
- How was my anger related to my recurring thoughts or behaviors?
In general, when dealing with anger, the key is to prevent it from escalating into aggression. Consider trying these practices to effectively channel your anger and minimize anger episodes:
Consider trying these practices to effectively channel your anger and minimize anger episodes:
- Get treatment for OCD. Your anger may decrease once your symptoms are successfully managed.
- Pinpoint what is specifically triggering your anger and brainstorm solutions that address each trigger.
- Figure out your personal early warning signs so you can practice some relaxation techniques before your anger gets out of hand.
- Use a meditation app to help you relax and become more mindful.
- Make yoga part of your day, such as trying this 20-minute yoga for anxiety video.
- Identify the positive ways you’d like others to support you.
- Journal about your feelings regularly.
- During an outburst, take a time-out by leaving the room until you cool off.
- Consider an anger management course.
If your loved one has OCD, it can be difficult to know how to help them through an anger outburst. In general, it’s important to create a supportive environment, manage your own emotions, and set boundaries to maintain your own safety.
Here are some specific actions that may help:
- Acknowledge that living with OCD is difficult, and their anger is warranted.
- Avoid pressuring them to stop being angry or criticizing them for feeling frustrated.
- Recognize their improvements, big or small.
- Gently encourage them to try calming practices, which you might take on together.
- Regularly check-in to see how they’re feeling, encouraging them to share their frustrations.
- Listen fully to what they share, without judging or interrupting them and becoming defensive.
- Avoid comparing them to other people with OCD or comparing their progress from day to day.
- Learn to effectively manage your own anger and frustration.
- Consider attending family therapy or working with your own therapist.
- Create a family contract of clearly defined goals for reducing OCD symptoms and getting on the same page.
- Identify what you need to feel safe and advocate for it.

Anger attacks getting out of hand?
If you believe you’re in danger
If someone is being violent, or you’re concerned about the possibility of violence, immediate help is available. You can contact the National Domestic Violence Hotline online, or call or text “START” to 800-799-SAFE (7233). This resource is completely confidential.
If your loved one is in immediate danger of self-harm or suicide
- Remove objects from their reach that they could use to harm themselves, such as pills, weapons, or sharp objects.
- Stay with them and seek professional help right away.
- Call your local emergency room (or 911, if you feel it’s safe for you). Tell the operator that it’s for a medical emergency, so they can direct you to the right support.
Additional crisis hotlines
- Call a crisis hotline, such as the National Suicide Prevention Lifeline at 800-273-8255.
- Text “HOME” to the Crisis Text Line at 741741.

- Call the Veterans Crisis Line at 800-273-8255, text 838255, or chat online 24-7.
- Visit Befrienders Worldwide. It’s an international crisis helpline network that can help you find a local helpline.
- Call the Deaf Crisis Line at 321-800-DEAF (3323) or text “HAND” at 839863.
For many adults and children, OCD and anger often go hand in hand. The relationship between the two is complex.
Overall, living with OCD and dealing with its symptoms can leave people feeling frustrated, confused, and angry. Feeling misunderstood and having rituals interrupted can also heighten anger.
While anger is a normal, natural emotion, in some cases, it can turn into aggressive, violent behavior. When that happens, it’s important to make sure everyone is safe and seek help.
To maintain a safe, healthy environment, it’s also important to develop an action plan that everyone understands and supports. Your plan might include a list of shared goals, appropriate and inappropriate behavior, and consequences.
Ultimately, give yourself grace. Give your loved ones grace. Check out these OCD resources, and consider working with a therapist who specializes in OCD.
OCD is highly treatable, and your entire family can thrive.
OCD and Anger: Causes, Treatment, and How to Deal
OCD and anger often go hand in hand. Here’s how to channel your frustration in healthy ways — or help a loved one.
People with obsessive-compulsive disorder (OCD) have unrelenting, invasive thoughts (obsessions) and can act in ways they feel unable to control (compulsions).
For example, they might worry obsessively about having secured their house safely or turned off their stove. They might feel compelled to perform certain rituals in the same order or pray excessively to prevent harm.
People with OCD can also experience episodes of anger. OCD is a chronic, distressing condition, so feeling angry makes sense. In fact, anger is a common human emotion that everyone experiences.
But intense anger, particularly when it turns into aggression, can be distressing for people with OCD and their loved ones.
The good news is that you can absolutely manage out-of-control anger in healthy ways, and you can support a loved one by managing it, too. Here’s how.
Some research suggests that anger episodes may be more common in OCD. For example, this 2011 study found that out of 42 adults with OCD attending an outpatient clinic, 21 reported experiencing angry outbursts in which they:
- yelled at others
- threatened to hurt others
- acted aggressively
- threatened to leave
In the same study, people who experienced anger episodes also experienced more panic attacks and had more severe depression.
This 2019 study of 90 Chinese people with OCD found that around 31% had experienced at least one anger outburst in the past week. In this 2020 German study, people living with OCD also reported more anger than people without the disorder.
Anger may also occur in children with OCD.
For example, this 2012 study found that anger attacks were relatively common in children ages 6 to 16 with OCD. Researchers also found that anger attacks were associated with more severe symptoms and impairment.
Researchers also found that anger attacks were associated with more severe symptoms and impairment.
This 2015 study found similar results with increased anger in children with OCD and more intense symptoms. According to the study, the anger also took a toll on caregivers and led to poorer relationships with parents, siblings, relatives, and peers.
The link between OCD and anger is complicated and multilayered. Some people with OCD may become angry at having to live with such a difficult disorder. Others may experience anger as part of their obsessions or compulsions.
If you live with OCD and experience intrusive violent thoughts, it’s important to remember that there’s no such thing as a thought crime, and just because you think it doesn’t mean it’s going to happen.
A wide range of factors can spark anger outbursts in adults and children with OCD. These can include:
- loved ones not accommodating compulsive behaviors, which can also lead to profound fear
- others not understanding or minimizing what it’s like to have OCD
- interruptions that prevent performing rituals or performing them perfectly
- frustration with having OCD
- having to suppress feelings of anger
- negative reactions to medication
- symptoms of OCD, such as having to perform compulsions perfectly and constantly having unwanted, upsetting thoughts
- prolonged levels of anxiety and stress
- PANDAS, which stands for ‘pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections’ — a strep infection in children that triggers or worsens OCD by causing mood changes and irritability
OCD can affect people of every race, from children to adults. While both diagnosis and treatment options are widely available, there can be disparities in what people experience.
While both diagnosis and treatment options are widely available, there can be disparities in what people experience.
Barriers to treatment are an especially significant challenge for African Americans and other historically marginalized groups who, according to research, are less likely to access psychological and psychiatric services and are less likely to receive effective treatment for OCD.
Affordable options, available mental health professionals, and community education are noted as obstacles.
In OCD, the level, intensity, and specific behaviors of an anger episode can vary from person to person. Some people may express anger in destructive ways, while others internalize their anger instead. Some may do both.
During an anger episode, adults or children with OCD may:
- yell
- swear
- make hurtful remarks
- throw things
- hurt themselves
- hurt others
Often, people with OCD turn their anger inward, which may include:
- having thoughts of self-harm or suicide
- having feelings of self-hatred or worthlessness
- withdrawing from loved ones
If you’re witnessing an angry outburst, it can understandably be concerning. However, it can be helpful to remember that a person with OCD is dealing with a lot.
However, it can be helpful to remember that a person with OCD is dealing with a lot.
So, even though they’re directing their anger toward you, their frustration may really stem from what they’re experiencing.
Of course, this doesn’t make it OK for anyone to become violent. If that happens, consider the below resources for immediate help.
Everyone experiences anger from time to time. Again, anger is a natural — even necessary — emotion. For example, anger tells you when someone is crossing your boundaries. Anger is also a signal that you may need to make some important changes.
To better understand the link between your OCD and anger, consider these questions:
- On a daily basis, when do I feel the most frustration?
- When do I feel the least frustration?
- In the last month or week, why did I get angry with someone?
- Were there early signs that my anger was building?
- What emotions or experiences might be underlying my anger, such as loneliness, shame, or sadness?
- How was my anger related to my recurring thoughts or behaviors?
In general, when dealing with anger, the key is to prevent it from escalating into aggression. Consider trying these practices to effectively channel your anger and minimize anger episodes:
Consider trying these practices to effectively channel your anger and minimize anger episodes:
- Get treatment for OCD. Your anger may decrease once your symptoms are successfully managed.
- Pinpoint what is specifically triggering your anger and brainstorm solutions that address each trigger.
- Figure out your personal early warning signs so you can practice some relaxation techniques before your anger gets out of hand.
- Use a meditation app to help you relax and become more mindful.
- Make yoga part of your day, such as trying this 20-minute yoga for anxiety video.
- Identify the positive ways you’d like others to support you.
- Journal about your feelings regularly.
- During an outburst, take a time-out by leaving the room until you cool off.
- Consider an anger management course.
If your loved one has OCD, it can be difficult to know how to help them through an anger outburst. In general, it’s important to create a supportive environment, manage your own emotions, and set boundaries to maintain your own safety.
Here are some specific actions that may help:
- Acknowledge that living with OCD is difficult, and their anger is warranted.
- Avoid pressuring them to stop being angry or criticizing them for feeling frustrated.
- Recognize their improvements, big or small.
- Gently encourage them to try calming practices, which you might take on together.
- Regularly check-in to see how they’re feeling, encouraging them to share their frustrations.
- Listen fully to what they share, without judging or interrupting them and becoming defensive.
- Avoid comparing them to other people with OCD or comparing their progress from day to day.
- Learn to effectively manage your own anger and frustration.
- Consider attending family therapy or working with your own therapist.
- Create a family contract of clearly defined goals for reducing OCD symptoms and getting on the same page.
- Identify what you need to feel safe and advocate for it.
Anger attacks getting out of hand?
If you believe you’re in danger
If someone is being violent, or you’re concerned about the possibility of violence, immediate help is available. You can contact the National Domestic Violence Hotline online, or call or text “START” to 800-799-SAFE (7233). This resource is completely confidential.
If your loved one is in immediate danger of self-harm or suicide
- Remove objects from their reach that they could use to harm themselves, such as pills, weapons, or sharp objects.
- Stay with them and seek professional help right away.
- Call your local emergency room (or 911, if you feel it’s safe for you). Tell the operator that it’s for a medical emergency, so they can direct you to the right support.
Additional crisis hotlines
- Call a crisis hotline, such as the National Suicide Prevention Lifeline at 800-273-8255.
- Text “HOME” to the Crisis Text Line at 741741.

- Call the Veterans Crisis Line at 800-273-8255, text 838255, or chat online 24-7.
- Visit Befrienders Worldwide. It’s an international crisis helpline network that can help you find a local helpline.
- Call the Deaf Crisis Line at 321-800-DEAF (3323) or text “HAND” at 839863.
For many adults and children, OCD and anger often go hand in hand. The relationship between the two is complex.
Overall, living with OCD and dealing with its symptoms can leave people feeling frustrated, confused, and angry. Feeling misunderstood and having rituals interrupted can also heighten anger.
While anger is a normal, natural emotion, in some cases, it can turn into aggressive, violent behavior. When that happens, it’s important to make sure everyone is safe and seek help.
To maintain a safe, healthy environment, it’s also important to develop an action plan that everyone understands and supports. Your plan might include a list of shared goals, appropriate and inappropriate behavior, and consequences.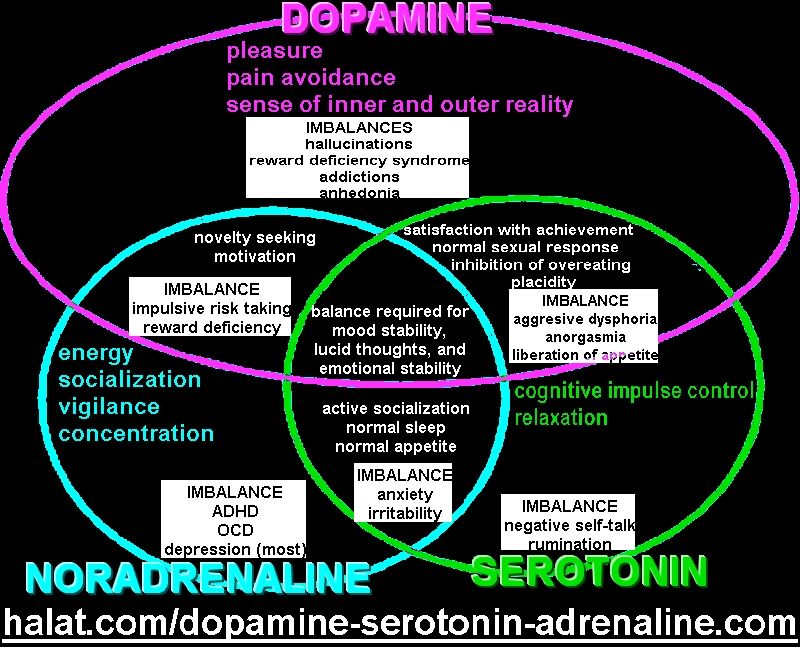
Ultimately, give yourself grace. Give your loved ones grace. Check out these OCD resources, and consider working with a therapist who specializes in OCD.
OCD is highly treatable, and your entire family can thrive.
Depressive obsessive-compulsive disorder //Psychological newspaper
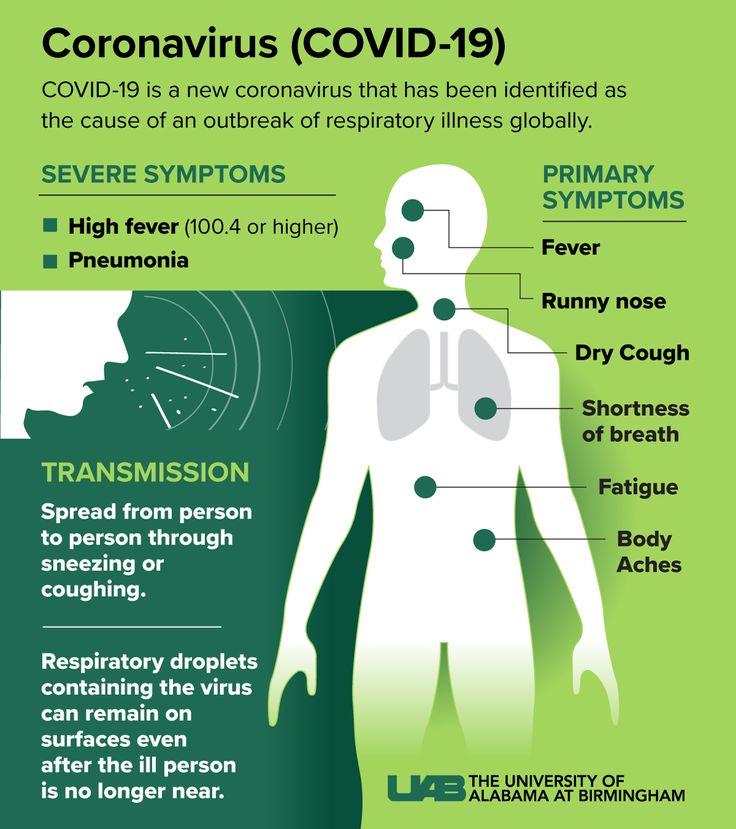
Obsessive-compulsive disorder presents a particular difficulty in diagnosis. This is because the main, root causes of this disease can be quite different. The main issue is associated with the so-called register-dependent obsessive symptoms (obsessive thoughts and actions), which qualitatively vary depending on the course of the main disease. That is, for example, if obsessions are caused by a personality disorder, then personality disorders will be paramount, and obsessions or compulsions will be secondary. If obsessive thoughts are caused by neurosis, then psychotrauma is considered as the main problem, and obsessive symptoms are only an “echo”, a secondary component. There is reason to believe that obsessions also appear during depression, and obsessions and compulsions in this case will acquire special qualitative colors. nine0003
nine0003
The depressive register of OCD, or OCD depression, is relatively poorly understood from the point of view of the general theory of obsessive thoughts. As follows from the definition of mild depression, to diagnose it, it is enough to define the “Beck triad”: a negative image of oneself, a negative image of the world and a negative image of the future. With more serious degrees of depression, one has to take into account the diversity of the depressive syndrome. In this case, melancholic and suicidal thoughts, apathy, depressed mood, "powerlessness" with manifestations of asthenia, vegetative reactions with anxiety are often observed. The main question that arises when analyzing the mental state of such people is an attempt to understand why the depressive process is self-sufficient and stable. Particular attention is also drawn to the hypothesis that the course of thought processes in this disease becomes excessively cyclical. At the same time, previously normal thoughts begin to undergo various transformations, and also change a number of their qualities - they become obsessive. nine0003
nine0003
It is assumed that there are a number of still little-known mechanisms that can change the register of obsessions, and can also significantly complicate the course and treatment of obsessions and compulsions. This can be explained by the example of the “transition” of neurotic obsessive thoughts into depressive ones. For example, a person cannot overcome any difficult life situation, and this leads him to extreme stress. After some time, certain changes seem to occur, life is gradually getting better, but memories of the crisis form obsessive unpleasant memories that are distinguished by egodistonism (contrary to the ego). This is the neurotic register of obsessive thoughts. Let us assume that further various crisis situations are repeated in the above-mentioned person, there are more and more psychotraumas. And looped egodistonism (not accepting any failures in the past) begins to transform into a generalized negative image of the outside world. That is, the usual egodyston process evolved not only into non-acceptance of oneself, but also into an obsessive rejection of the whole picture of reality. One of the components of Beck's depressive triad appears. The subsequent attachment of ego-synthonicity in relation to one's own negative image gives rise to self-accusations (the second component of the triad is a negative image of oneself). Attempts to predict the future under such circumstances lead to obsessive thoughts that even after a long period of time nothing will change for the better. The result of this whole process is the transition of obsessions from the neurotic to the depressive register, with qualitative changes both in the repetition cycles and in the semantic plots themselves. In other words, the entire Beck triad listed above can be considered depressive intrusive thoughts in OCD depression. nine0003
One of the components of Beck's depressive triad appears. The subsequent attachment of ego-synthonicity in relation to one's own negative image gives rise to self-accusations (the second component of the triad is a negative image of oneself). Attempts to predict the future under such circumstances lead to obsessive thoughts that even after a long period of time nothing will change for the better. The result of this whole process is the transition of obsessions from the neurotic to the depressive register, with qualitative changes both in the repetition cycles and in the semantic plots themselves. In other words, the entire Beck triad listed above can be considered depressive intrusive thoughts in OCD depression. nine0003
Thus, the understanding of the phenomena of melancholia, depression, self-accusation and suicidality itself becomes systemic, and, therefore, several methodological levels can already be distinguished (Beck's theory and the general theory of obsessive thoughts) at which these processes can be analyzed, slowed down or stopped.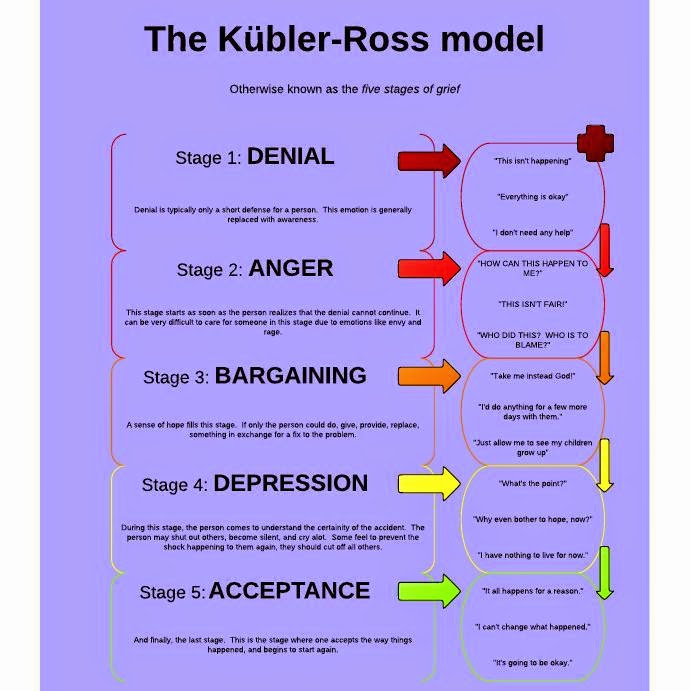 It is important to understand obsessions as unique mechanisms inherent in all mental disorders or illnesses, the main purpose of which is seen as ensuring the stability of unbalanced pathological processes .
It is important to understand obsessions as unique mechanisms inherent in all mental disorders or illnesses, the main purpose of which is seen as ensuring the stability of unbalanced pathological processes .
That is, for the psyche and streams of consciousness (thoughts), the primary task will not be to ensure complete recovery, but fixation (looping) on a more or less stable functional state. All this happens to prevent further complications of various mental illnesses.
Depressive OCD or OCD depression is characterized by a number of specific features. In particular, the characteristics of the course of different syndromes may indicate several registries of mental illness. For example, an anxious and depressive background will most likely indicate disturbances in the work of the autonomic nervous system, as well as depression itself (“two registers work” - vegetative and depressive). In this case, in addition to the obsessive Beck triad, panic attacks can also appear.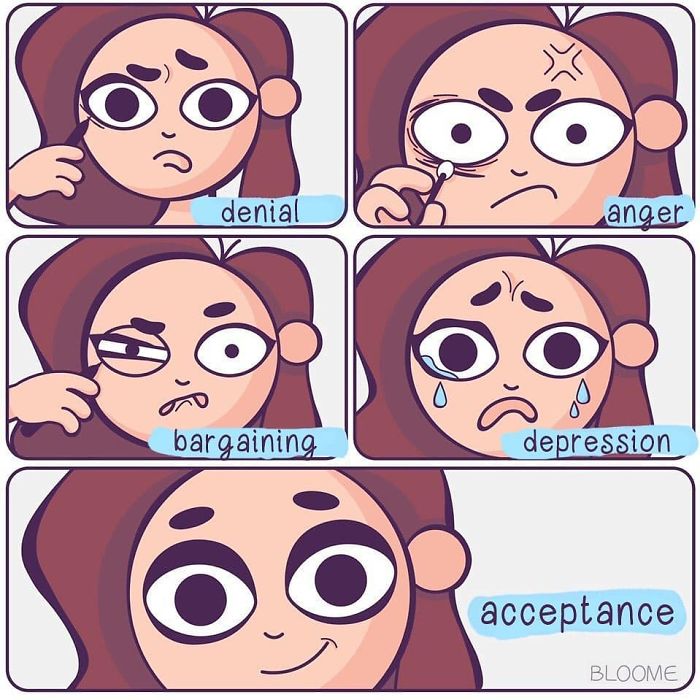 But the most common combination can be considered a neurosis and a depressive episode (two registers - neurotic and depressive). In this situation, intrusive memories will reinforce the obsessions of self-accusation, self-abasement and other melancholic obsessions. What is especially interesting, in the framework of the register analysis of obsessions and compulsions, we can assume that the neurotic register of obsessive thoughts can turn into a depressive one, or two registers will be observed in the clinical picture at once (respectively, we will observe signs of a depressive-neurotic syndrome). nine0003
But the most common combination can be considered a neurosis and a depressive episode (two registers - neurotic and depressive). In this situation, intrusive memories will reinforce the obsessions of self-accusation, self-abasement and other melancholic obsessions. What is especially interesting, in the framework of the register analysis of obsessions and compulsions, we can assume that the neurotic register of obsessive thoughts can turn into a depressive one, or two registers will be observed in the clinical picture at once (respectively, we will observe signs of a depressive-neurotic syndrome). nine0003
As mentioned above, depressive obsessions can be recognized not only by syndromatic signs. Depression transforms the neurotic obsession into egodystonic and egosynthonic elements. In particular, selfishness is associated with self-accusations (a person does not even have reasonable self-criticism that he is not really to blame for all his troubles and troubles in the world - the disease itself forms a strong sense of guilt), and selfishness manifests itself in a negative image of the outside world (not accepting and not understanding a number of his instincts, drives, needs and motives, a person begins to consider the external environment as something alien, hostile, strange). The above reflections and conclusions speak in favor of the fact that the obsessions of any register, including the depressive one, quite strongly affect the "ego", "id" and "superego" of the individual. nine0003
The above reflections and conclusions speak in favor of the fact that the obsessions of any register, including the depressive one, quite strongly affect the "ego", "id" and "superego" of the individual. nine0003
Quite relevant is the question of how good the level of awareness of depressive obsessions and compulsions will be in comparison with their other varieties. Here we should pay attention to the fact that neurotic obsessions are reflected much better, since in this case the personality, as it were, is fighting against itself. In depressive OCD, the situation is aggravated by the fact that adequate self-criticism is suppressed here by various cognitive distortions, in particular, catastrophization, as well as strong emotions of guilt. Sometimes the individual himself defends his own irrational conclusions about his own worthlessness, the absolute negativity of the world around him and the supposedly “gloomy future”. Beck's triad as a special obsessive formation makes a person return to melancholic thoughts again and again and does not allow switching to more constructive strategies.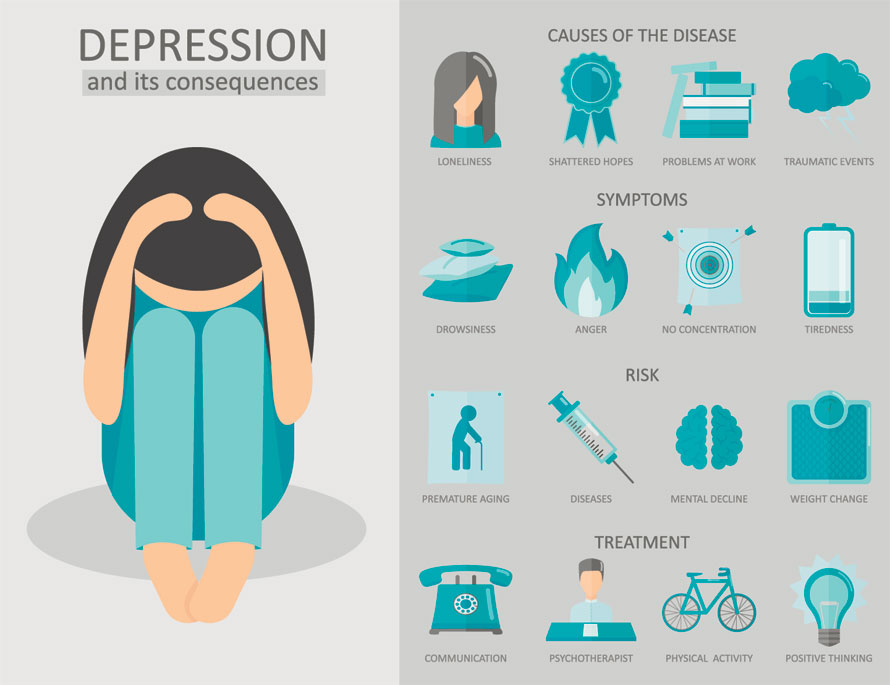 Moreover, the presence of a vegetative register of obsessions in addition to the depressive one can contribute to more serious risks of developing suicides. nine0003
Moreover, the presence of a vegetative register of obsessions in addition to the depressive one can contribute to more serious risks of developing suicides. nine0003
Like neurotic intrusive memories, depressive obsessions organize themselves into steady and stable recurring cycles. Therefore, the chronicity of OCD neurosis and OCD depression is quite high. However, the pace of the stream of consciousness is different here. With obsessive psychotraumatic experiences, thoughts can arise quickly, their very appearance is often illogical and non-associative. At the same time, obsessions of the depressive register may not be of high intensity, but they slowly fetter consciousness, reduce attention and memory. Slow "mental stirrers" and "mental chewing gums" - ruminations - can become commonplace here. nine0003
You can also notice certain differences at the level of psychosomatics. Disturbing neurotic memories can cause various autonomic disorders (excessive sweating, tachycardia, frequent urination, nervous functional gastritis, cholecystitis, etc. ). In turn, depressive obsessions can often be accompanied by asthenia, “powerlessness”, increased fatigue, etc. Quite complex and specially structured psychosomatics can be observed with the simultaneous presence of both neurotic and depressive obsessions. Among the sensory phenomena characteristic of OCD-depressions, it is possible to single out absent-mindedness, a decrease in attention with intensified attempts to stabilize it, and consciousness, as it were, loses its “focus”. It should also be taken into account that a neurotic obsession is a traumatic emotional experience or memory invading consciousness. In turn, depressive obsession is a cyclical repetition of destructive attitudes, which are based on the Beck triad. In both cases, getting rid of this kind of thoughts on your own can be quite difficult. nine0003
). In turn, depressive obsessions can often be accompanied by asthenia, “powerlessness”, increased fatigue, etc. Quite complex and specially structured psychosomatics can be observed with the simultaneous presence of both neurotic and depressive obsessions. Among the sensory phenomena characteristic of OCD-depressions, it is possible to single out absent-mindedness, a decrease in attention with intensified attempts to stabilize it, and consciousness, as it were, loses its “focus”. It should also be taken into account that a neurotic obsession is a traumatic emotional experience or memory invading consciousness. In turn, depressive obsession is a cyclical repetition of destructive attitudes, which are based on the Beck triad. In both cases, getting rid of this kind of thoughts on your own can be quite difficult. nine0003
The above features of depressive obsessions help to better understand the phenomenon of depression. At this stage, we can not only study melancholia and depression at the level of Beck's cognitive-behavioral theories, but also connect both syndromatic (psychiatric) and register theoretical developments of the general theory of obsessive thoughts (medical psychology). Combining all of the above approaches into a single analytical framework can contribute to a better understanding of the nature of depression. nine0003
Combining all of the above approaches into a single analytical framework can contribute to a better understanding of the nature of depression. nine0003
It should also point out the potential for a new look at psychotherapeutic interventions for depressive episodes and OCDs. The most interesting and relevant direction may be the rethinking of cognitive behavioral therapy, taking into account the fact that obsessive thoughts in several registers require special, innovative approaches for correction. In itself, the interaction of several diseases - neurosis and depression, as well as neurotic disorders with vegetative ones - these are systemic aspects that have not yet been studied enough in psychology and psychiatry. Therefore, the ability to distinguish between different obsessions can be a serious help for the study of new preventive and therapeutic methodologies, methods and techniques. nine0003
- International Statistical Classification of Diseases and Related Health Problems.
 In 3 vols. T. 1. - Tenth revision. - Geneva: World Health Organization, 1995. - 697 p.
In 3 vols. T. 1. - Tenth revision. - Geneva: World Health Organization, 1995. - 697 p. - Diagnostic and manual statistical of mental disorders (DSM-IV). — Forth Edition. - Washington: American Psychiatric Association, 1994. - 915 p.
- Diagnostic and manual statistical of mental disorders. Text revision (DSM-IV-TR). — Forth Edition. - Washington: American Psychiatric Association, 2000. - 943 p.
- Diagnostic and manual of mental disorders : DSM-5. — Fifth edition. - Washington: American Psychiatric Association, 2013. - 970 p.
OCD: what is obsessive-compulsive mental disorder, diagnosis, treatment
In our time, obsessive-compulsive mental disorder is faced by those who knew this disease only by hearsay. Surprisingly, psychologists note that many OCD patients can find advantages in their illness. Still, it is better to diagnose the disease and try to cope with it. The statistics are disappointing - up to 3% of the world's population is faced with a violation. nine0003
nine0003
What is OCD (obsessive compulsive disorder)?
OCD, or obsessive-compulsive disorder, is a mental disorder characterized by obsessive thoughts (obsessions) and actions (compulsions). Striking examples include the desire for perfect cleanliness, the fear of catching various diseases, a manic attachment to certain rituals (for example, pressing the doorbell three times, washing hands after each handshake, etc.).
Often, the manifestation of obsessive-compulsive disorder is accompanied by bodily harm to oneself or other people. It is important to diagnose the disease in time so that it does not develop into a pathology. nine0003
Obsessive-compulsive disorder is also called obsessive-compulsive disorder. The disease can be chronic, episodic or progressive. Equally, the disease is present in both men and women. Sometimes the patient himself understands that his thoughts in their manifestation are absurd, and the behavior that follows them is very ineffective. But resisting them is useless. Suppressing these actions only increases the anxiety state.
But resisting them is useless. Suppressing these actions only increases the anxiety state.
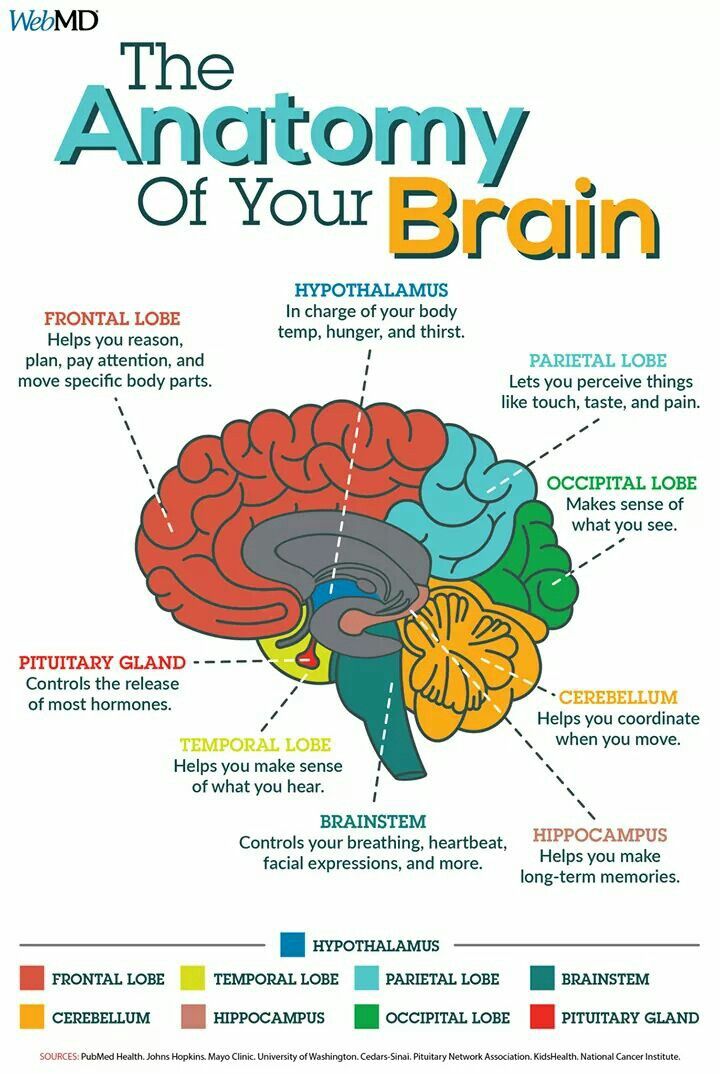
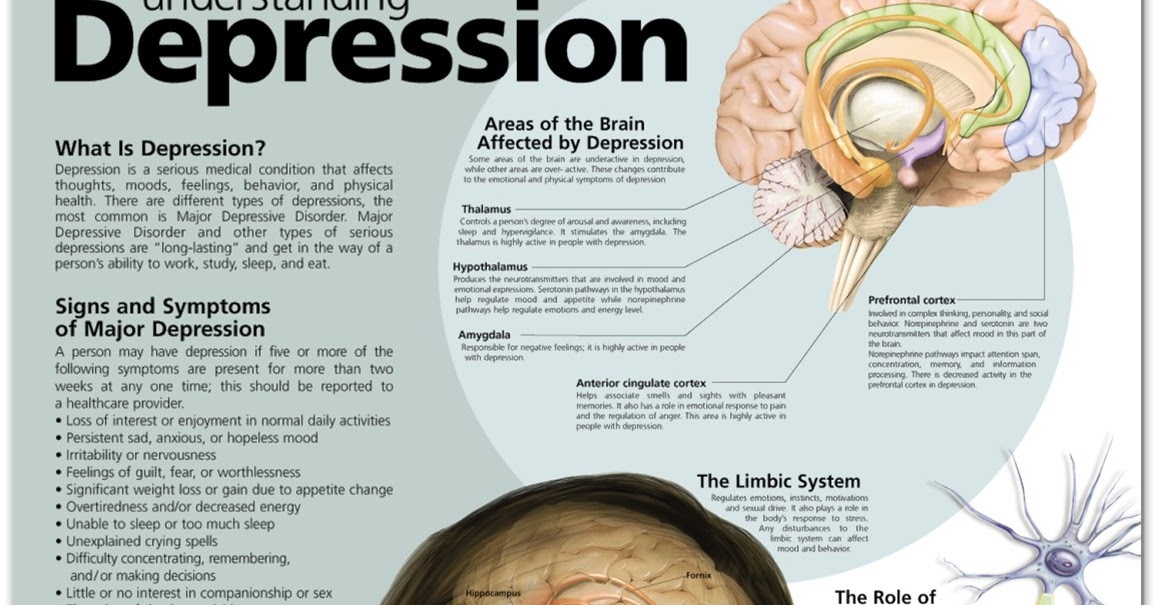
If we consider the disease from the side of physiology, then it leads to functional disorders in the following parts of the brain: nine0003
- basal ganglia;
- frontal part;
- caudate nucleus;
- amygdala.
The severity of obsessive-compulsive personality disorder in patients can vary and most often depends on the presence of stressful situations in a person's life. Violation can change life for the worse, reduce communication with society. A distinctive feature of obsession can be considered the absence of rationalism, and compulsions - that they cannot be abandoned. nine0003
Patients, realizing their situation, are afraid to go crazy, they begin to worry about their relatives, about their own and their safety. In practice, such neuroses do not lead to serious consequences or mental disorders, and aggressive thoughts do not lead to subsequent actions.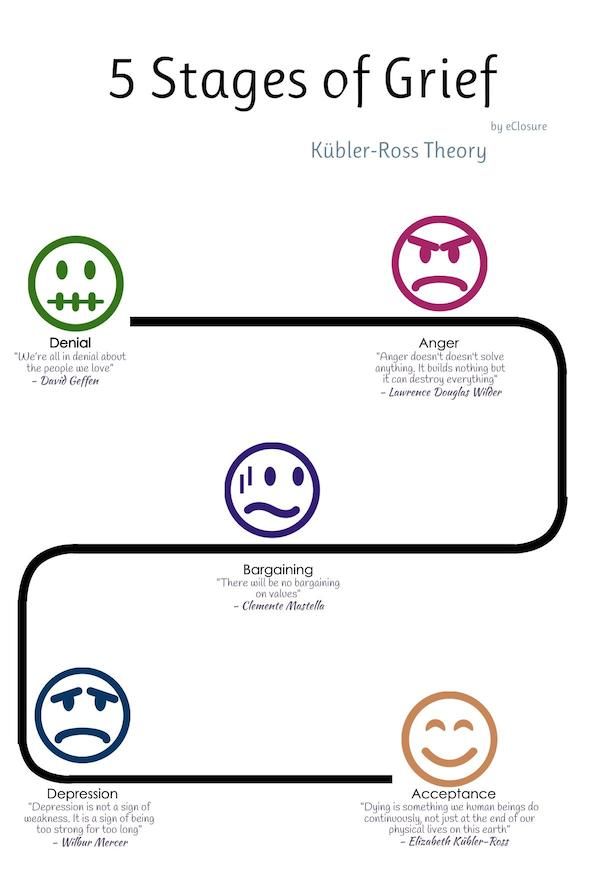
This is what distinguishes a person with OCD from mentally deranged or hallucinating patients. A patient with OCD has the following symptoms:
- high intelligence;
- adequate thinking;
- conscientiousness and anxiety;
- high sense of responsibility;
- pedantry;
- desire to be the best.
Symptoms of obsessive-compulsive disorder
The most obvious symptoms include the obsessive and compulsive disorders already mentioned, that is, obsessive thoughts and a manic desire to perform any action. Thoughts can manifest as images, delusional ideas, inexplicable drives. Obsessive-compulsive disorder and its symptoms are observed in the form of the inability to make decisions regarding everyday situations. nine0003
Of the main signs of OCD, the following can be distinguished: obsessive-compulsive disorder:
- intrusive thoughts;
- anxiety and various fears;
- the same rituals that a person performs daily.
Among the mental symptoms in patients, the following are observed:
- fear of catching an infection;
- causeless anxiety;
- maniacal desire for order and cleanliness; nine0030
- excessive superstition.
With OCD, the patient appropriates all incoming thoughts, in contrast to the disease of a split personality, when a person hears "foreign" voices.
These actions themselves do not bring pleasure to a person, but they can reduce the level of anxiety and stress. This does not last long and after a while the obsession returns, a phobia sets in and everything starts in a circle. Outwardly, compulsions can resemble ordinary work, for example, a person lays out things, constantly cleans the house, although the house can be perfectly clean anyway. nine0003
Sometimes the manifestation of obsessive-compulsive disorder manifests itself physically. A person does not sleep well, he has headaches, heartaches, blinking becomes more frequent, nervous tics and convulsions occur, pressure rises, appetite is disturbed, and sexual desire decreases.
The manifestations of obsessive-compulsive disorder are constant and manic in nature, they cause inconvenience to a person.
Causes of obsessive-compulsive disorder nine0043
Scientists are still conducting various studies to establish the exact causes of the violation. But there are no exact data in this area. Despite this, it is customary to single out several areas that can cause obsessive-compulsive disorder syndrome, the reasons are:
- Psychological. OCD occurs when a person develops aggression towards an object. It also includes stressful situations that provoke a violation. The state appears as an exit of emotions, as a marker of anxiety. nine0030
- Biological.
 The disorder is the result of a disease of the brain or nervous system. It can be provoked by various kinds of injuries, hormonal disorders or anatomical features.
The disorder is the result of a disease of the brain or nervous system. It can be provoked by various kinds of injuries, hormonal disorders or anatomical features. - Genetic. The disease can be inherited.
- Sociological. They arise as a response of the body to external factors.
- Exogenous. They manifest themselves in the form of traumatic situations that can happen at work or in personal life. nine0061
- "Mental chewing gum" or rumination.
 When a person sets himself unsolvable questions and tasks.
When a person sets himself unsolvable questions and tasks. - Arrhythmia. Obsession, which is manifested by the constant re-reading of various objects.
- Intrusive reproduction. It manifests itself in the painful formation of a person to remember everything that is not related to a given period of time, event or conversation. nine0030
- Onomatomania. An obsessive desire to remember all the words, titles and names.
- Misunderstanding. At this stage, intrusive thoughts are mild. A person feels a violation of the habitual consciousness, anxiety, cannot understand the nature of the occurrence of manic impulses.
- Understanding. Accompanied by a visit to a specialist. The patient understands that disturbances are present, but cannot yet realize the changes. Often at this stage there is hope that the state will change and life will return to its previous course.
- Adoption. The patient comes to terms with the mental disorder, agrees to treatment. He ceases to regard obsession and compulsion as a temporary condition.
 At this stage, it is important to fully interact with the attending physician, to obtain comprehensive information about the disease. nine0030
At this stage, it is important to fully interact with the attending physician, to obtain comprehensive information about the disease. nine0030 - Suicidal behavior. In a severe stage, the patient may commit suicide or try to cause physical harm to another person.
- From constant contact with soap and detergents that a person uses so actively, dermatitis can develop.
- Possible problems in the social sphere. Inability to communicate with society. A person falls out of society - he does not have a hobby, he is afraid to appear in public places, he cannot concentrate on work.
 nine0030
nine0030 - There are conflicts with relatives and friends. Some people with OCD are unable to start a family and have difficulty raising children.
- The patient has intrusive thoughts. The frequency of their appearance in this case exceeds the permissible norm for two weeks.
- Obsessive thoughts and actions qualitatively worsen the life of the patient. nine0030
- The implementation of obsessions and compulsions causes discomfort in the patient.
- Actions and thoughts occur regularly and frighten the patient with their frequency.
- There is no specificity in thoughts and actions, their nature is associated with anxiety, generates stress in a person, internal tension.
- Primary. A person learns about a genetic predisposition, corrects his behavior with the help of a specialist, uses various methods to prevent the occurrence of a violation. Primary prevention also includes educational methods.
- Secondary. Used to prevent recurrence of OCD. In this case, you will also need the help of a specialist to correct behavior, calm and sufficient sleep, abstinence from alcoholic beverages and drugs. You can also follow a special diet that is aimed at producing serotonin.
 nine0030
nine0030 - Erich Fromm, "The human soul, its capacity for good and evil"
- Karen Horney, Neurosis and Personal Growth: The Struggle for Self-Realization
- Goldsmith G.N. Approaches to the treatment of narcissistic disorders: Kohut and Kernberg nine0030
- Otto Friedmann Kernberg, “Severe personality disorders. Psychotherapy Strategies»
- Dadasheva K.N. 1 , Agafonov B.V. 2 , Dadasheva M.N. 1 , Podrezova L.A. GBUZ MO MONIKI them. M.F. Vladimirsky, Moscow - neurasthenic syndrome in general medical practice. The possibilities of therapy.
- McWilliams N., reflections on schizoid dynamics
- T.A. Solokhina, prof. V.S. Yastrebov, L.S. Shevchenko - A model of organizing socio-psychological care for patients with schizophrenia.

Disease pathogenesis
Despite various theories of the occurrence of OCD, the pathogenesis of obsessive-compulsive disorder has a well-defined nature of occurrence, although not fully understood. These structures of the body interact with each other through serotonin. The lack of this hormone is due to the heightened effect of neurons on the cerebral cortex. This provokes a blockage of the nerve impulse, which does not reach the next neuron.
Classification and stage of development of ROC nine0043
Obsessive-compulsive disorder has different degrees of severity and manifests itself in the following stages:
There are several variants of manifestation. For example, they can be expressed in simple symbolic actions. The patient can put a certain prohibition on performing actions, for example, counting steps for failure or success. They can also be expressed in physical actions aimed at self-harm: pulling out body hair and eating it. As a rule, an accurate diagnosis requires complete immersion in the disease in order to understand whether it is different from other mental disorders. nine0003
The manifestation of obsessive-compulsive disorder is equally observed in both men and women. It is much less common in children, although it is believed that the first signs may appear before the age of 11 years.
It is much less common in children, although it is believed that the first signs may appear before the age of 11 years.
Obsessive-compulsive disorder is most common in adolescents. Studies have shown that the disorder affects mainly adolescents aged 11-17 years. Up to 85% of all patients are adolescents.
Each person, as a rule, goes through three stages that are inherent in OCD: nine0003
The obsessive-compulsive disorder scale was introduced to determine the stage of the disorder. It's called the Yale-Brown scale. It was developed at Yale University under the direction of Wayne Goodman. This manual is accepted throughout the world as a traditional method for identifying the stage of OCD.
Complications of obsessive-compulsive disorder
In obsessive-compulsive disorder, the consequences can be irreversible and cover completely different areas of life: nine0003
When to see a doctor?
At the slightest suspicion of the listed symptoms, you should immediately contact a specialist. Often a person with OCD is not able to independently realize and accept that his behavior and way of thinking has changed.
If you have problems with society and loved ones, then you should listen to their advice and make an appointment with a doctor. nine0003
Diagnostics
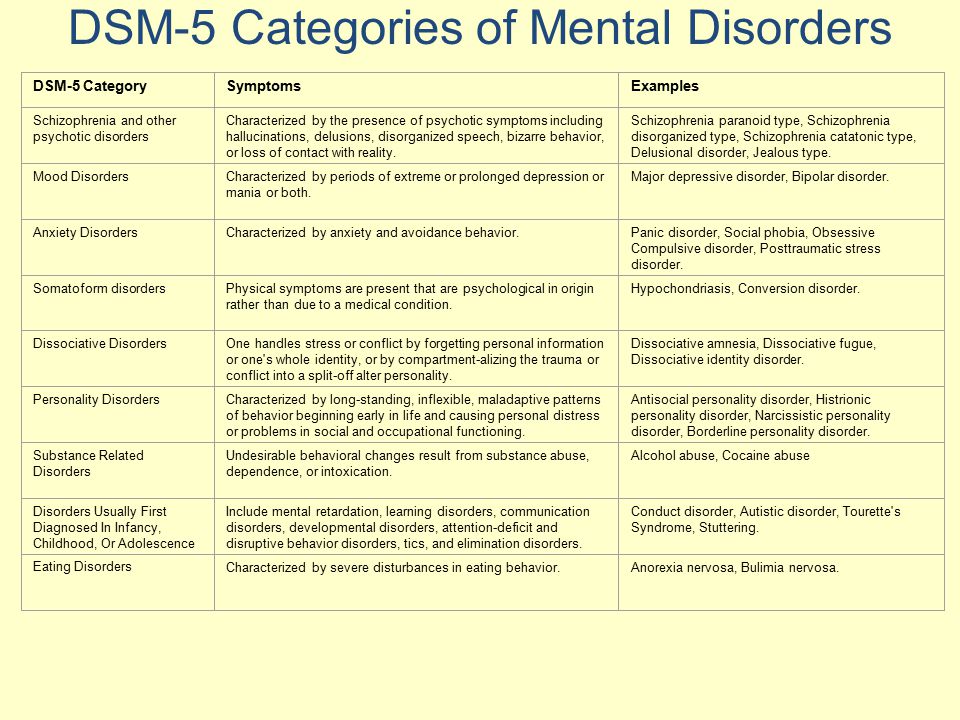
The violation is included in the International Classification of Diseases (ICD-10). Diagnosis of obsessive-compulsive disorder includes a mandatory visit to a specialist with subsequent diagnosis.
When making a diagnosis, the doctor relies on the following criteria:
The diagnosis is made if the patient has obsessive thoughts or ideas. They adopt an image that prompts them to impulsively perform some kind of action. nine0003
There is a mixed form of the disorder where the patient is equally haunted by obsessive thoughts and there is a manic execution of compulsions.
Treatment
Comprehensive treatment of obsessive-compulsive disorder includes an individual visit to a psychotherapist - a specialist identifies the causes of the disease, helps to recognize the signs of an obsessive-compulsive disorder, and accepts that the patient has OCD.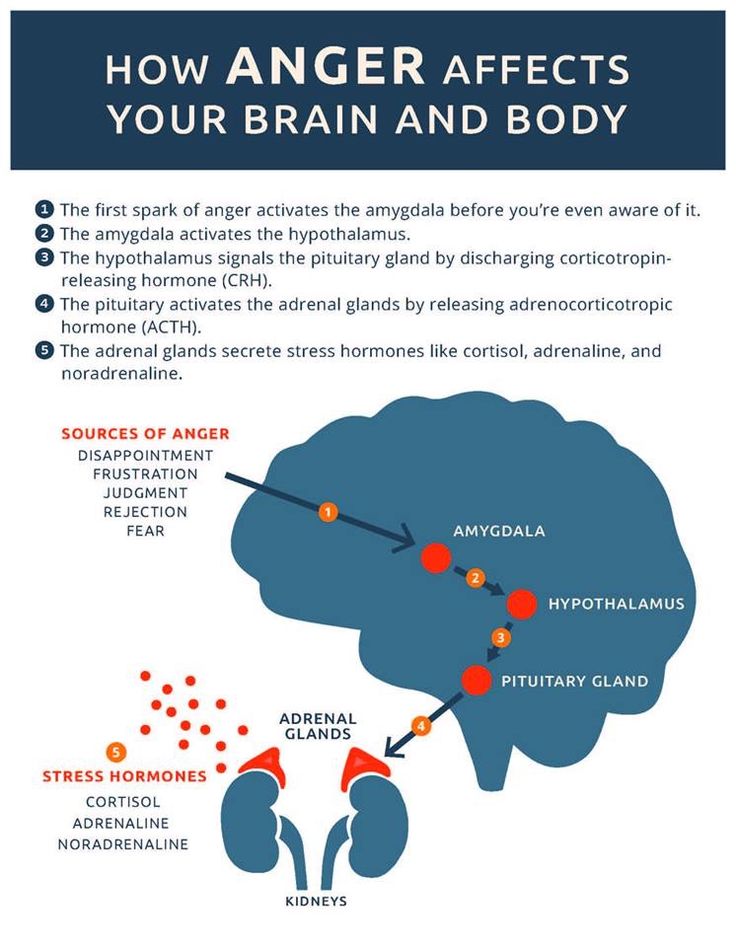 The next step is the CBT method (Cognitive Behavioral Therapy). The psychotherapist teaches the patient to monitor the appearance of OCD, find ways to change negative thoughts, displace them and change them into optimistic actions. Medications in this case are prescribed with the consent of the patient. nine0003
The next step is the CBT method (Cognitive Behavioral Therapy). The psychotherapist teaches the patient to monitor the appearance of OCD, find ways to change negative thoughts, displace them and change them into optimistic actions. Medications in this case are prescribed with the consent of the patient. nine0003
Antidepressants and anxiolytics (drugs that relieve anxiety) are prescribed as medicines. Treatment with sedatives is also possible, which helps relieve depressive thoughts, remove depressed mood.
Therapy for obsessive-compulsive disorder may include biofeedback therapy. Sensors are installed on the patient, with the help of which breathing, muscle work and heart rate are controlled. This technique helps to control the condition and further cope with emerging obsessive thoughts and negative emotions. nine0003
You can get treatment from private practitioners, but it is better to choose clinics that specialize in the treatment of mental disorders. Such institutions employ doctors with many years of experience who have been practicing and treating obsessive-compulsive disorder for many years.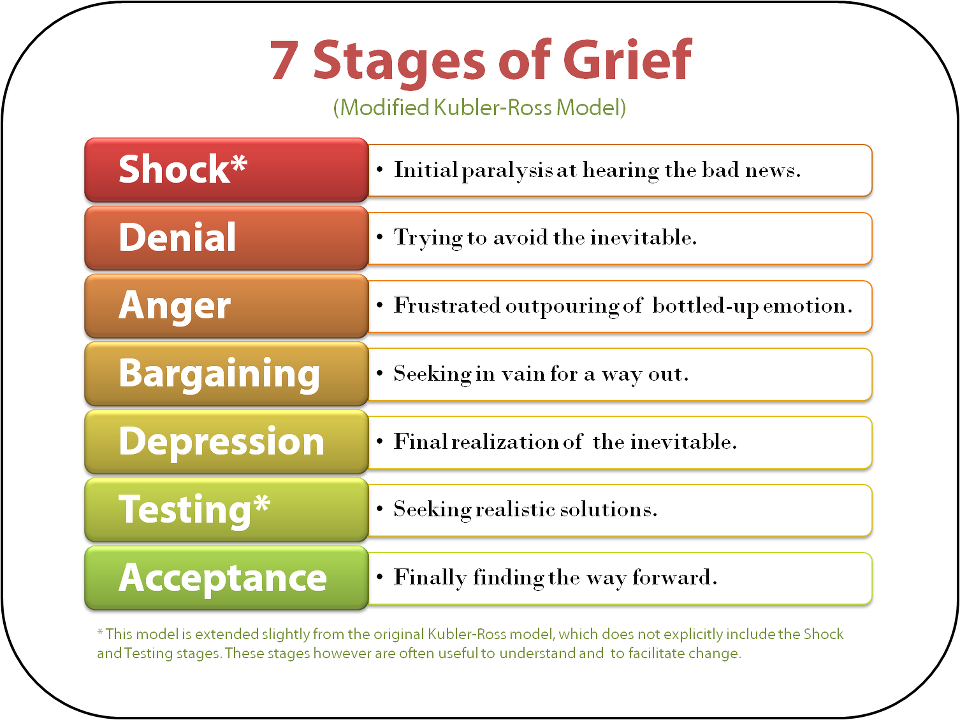
+7 (495) 121-48-31
Prevention and recommendations for illness
OCD is typical for people who have any other mental disorders. Also, with a stable calm state of patients diagnosed with OCD, its recurrence is possible. Since the specific cause of the violation has not been established, then prevention is advisory in nature. nine0003
For obsessive-compulsive disorder, recommendations in terms of prevention can be primary and secondary:
If any signs appear, it is better to consult a doctor, and not try to come to terms with unfamiliar conditions. It is useful to get comprehensive information about OCD from people who have suffered this violation.
References: