Can you take ativan while pregnant
Is Ativan Safe During Pregnancy?
The U.S. Food and Drug Administration places Ativan in Category D, which means that the drug has the potential to cause birth defects and health problems in developing babies, but that the drug might be required for some women with serious medical problems. Women with severe anxiety that cannot be treated with other medications, for example, might be encouraged to keep taking Ativan during pregnancy, under the close supervision of a doctor.
Treating anxiety during pregnancy can be challenging, especially if the mother has been using psychiatric drugs that could threaten her health or the health of her baby. Ativan, or lorazepam, belongs to a class of tranquilizing medications called benzodiazepines, which are among the most commonly prescribed psychiatric drugs in the US. Ativan is classified Category D drug by the U.S. Food and Drug Administration, which means that although research shows that the medication poses risks to developing infants, it may still be advisable to prescribe the drug to pregnant patients in certain cases.
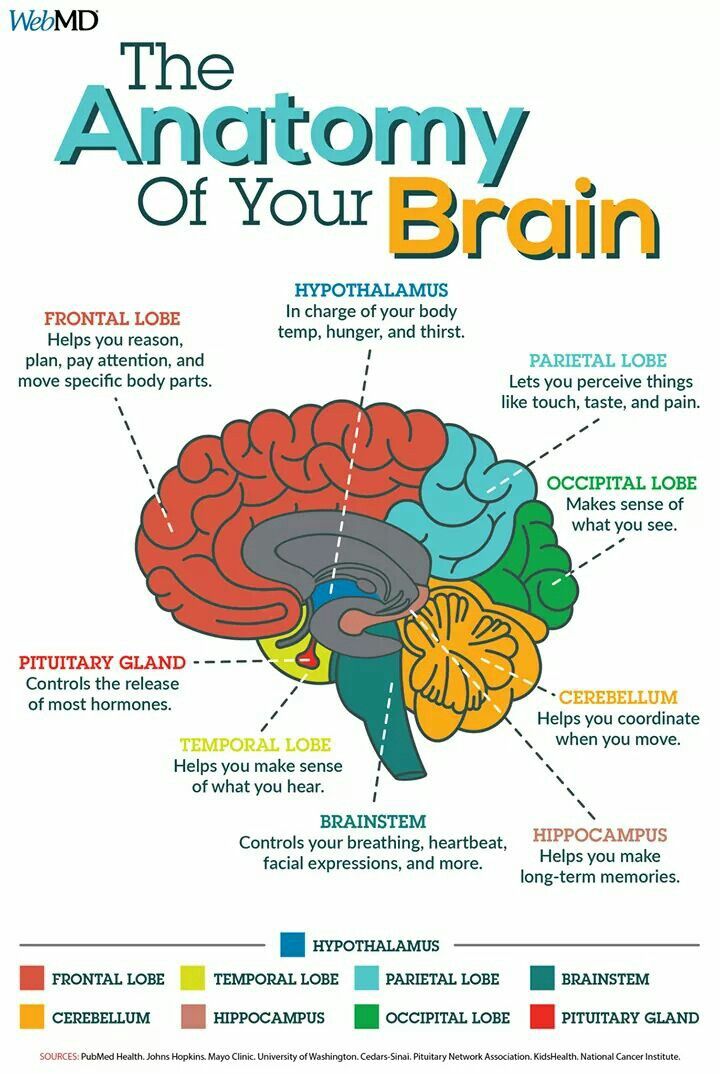
Ativan is a central nervous system depressant that is prescribed to treat several serious conditions of the brain and nerves, including anxiety, insomnia, seizure disorders, muscle spasms, and alcohol withdrawal syndrome.
Ativan is also administered in hospitals or surgical centers to help patients relax before surgery. Like other drugs in the benzodiazepine family ” diazepam (Valium), alprazolam (Xanax), and clonazepam (Klonopin), to name a few ” Ativan has the potential to be addictive. Although Ativan is safe for most adults, use of this medication should be approached with great caution in pregnant women, especially those who have a history of substance abuse or addiction.
Risks vs. Benefits of Ativan
Weighing the risks and benefits of Ativan use in pregnancy should be a collaborative activity involving the physician, the patient, and her partner or spouse. While lorazepam does present the possibility of certain complications and birth defects, leaving anxiety untreated can also have negative repercussions for a pregnant woman and her baby. American Family Physician estimates that approximately half a million pregnant American women suffer from psychiatric disorders during their pregnancy. Many anxiety disorders, including generalized anxiety disorder, panic disorder, social anxiety disorder, and agoraphobia, are more common in women than in men. Pregnancy can trigger anxiety symptoms or make anxiety worse, especially in women who don’t have a strong social support network or who are faced with financial or social stress.
American Family Physician estimates that approximately half a million pregnant American women suffer from psychiatric disorders during their pregnancy. Many anxiety disorders, including generalized anxiety disorder, panic disorder, social anxiety disorder, and agoraphobia, are more common in women than in men. Pregnancy can trigger anxiety symptoms or make anxiety worse, especially in women who don’t have a strong social support network or who are faced with financial or social stress.
If anxiety is not addressed, it may increase the risk of noncompliance with health recommendations or self-destructive behavior, such as smoking and alcohol abuse. Pregnant women struggling with mental illness may be less likely to follow nutritional guidelines, take prenatal vitamins, or attend their prenatal checkups. American Family Physician adds that complications with pregnancy, such as premature delivery and miscarriage, are also more common among pregnant women with anxiety disorders. Finding an alternative to Ativan and other potentially harmful drugs may be the most effective way to ensure a healthy pregnancy.
Finding an alternative to Ativan and other potentially harmful drugs may be the most effective way to ensure a healthy pregnancy.
- Risks During Pregnancy and Breastfeeding
- Health Hazards for Unborn Babies
- Ativan Abuse and Pregnancy
 Because small amounts of Ativan are passed from mother to baby in breast milk, the medication is also not advised for breastfeeding women due to a risk of over-sedation in the infant, notes Drugs.com.Most of the health risks of Ativan affect developing infants and newborn babies. Lorazepam has been associated with a slightly higher than average (0.7 percent) risk of cleft lip and cleft palate in newborns, according to the National Institute on Drug Abuse. This birth defect occurs during the first three months of pregnancy, which indicates that Ativan may be safer for use in the second and third trimesters. However, there is still a risk of drug withdrawal in infants whose mothers have been using Ativan. Some of the most common signs of lorazepam withdrawal in newborn babies include:
Because small amounts of Ativan are passed from mother to baby in breast milk, the medication is also not advised for breastfeeding women due to a risk of over-sedation in the infant, notes Drugs.com.Most of the health risks of Ativan affect developing infants and newborn babies. Lorazepam has been associated with a slightly higher than average (0.7 percent) risk of cleft lip and cleft palate in newborns, according to the National Institute on Drug Abuse. This birth defect occurs during the first three months of pregnancy, which indicates that Ativan may be safer for use in the second and third trimesters. However, there is still a risk of drug withdrawal in infants whose mothers have been using Ativan. Some of the most common signs of lorazepam withdrawal in newborn babies include: - Sedation
- Difficulty breathing
- A slack, floppy quality
- Irritability
In a few cases, seizures have been reported in infants who were withdrawing from the effects of benzodiazepines, but these incidents are rare. Serious signs of Ativan toxicity are more common in babies whose mothers are heavy users of this drug. Women who take Ativan with alcohol, opiates, or street drugs during pregnancy increase the risk of complications with pregnancy, premature delivery, low birth weight, and birth defects even further.
Serious signs of Ativan toxicity are more common in babies whose mothers are heavy users of this drug. Women who take Ativan with alcohol, opiates, or street drugs during pregnancy increase the risk of complications with pregnancy, premature delivery, low birth weight, and birth defects even further.
The 2013 National Survey on Drug Use and Health states that 5.4 percent of pregnant American women were current users of illegal drugs in 2012-2013, while 0.4 percent reported that they were heavy drinkers and 15.4 percent stated that they used tobacco. During pregnancy, women need the support of compassionate professionals who understand that addiction is a disease. Professional detox and rehab programs provide the most effective ways to clear lorazepam and other drugs from a client’s system without endangering her health. Detox programs offer round-the-clock supervision and support to keep clients medically stable as they prepare to take the next steps in rehab.
Safe Treatments for Anxiety
Anxiety can be a serious problem for pregnant women, especially if the disorder is not treated, but not all treatments and medications are safe for pregnant women or their developing babies.
Safe and effective therapeutic modalities for women during pregnancy include:
- Less habit-forming medications with a lower risk of birth defects, such as antidepressants in the SSRI (selective serotonin reuptake inhibitor) category
- Cognitive Behavioral Therapy (CBT), a learning-based approach that helps clients unlearn negative thought patterns and replace them with more positive, self-affirming thoughts and actions
- Holistic therapies such as prenatal massage, meditation, or prenatal yoga, which provide techniques for self-relaxation
- Nutritional counseling to prevent nutrient deficiencies that might contribute to emotional stress or jeopardize the health of the mother and baby
- Psychosocial services to link pregnant women with financial and legal support, access to housing and transportation, and affordable childcare
Pregnancy shouldn’t be a stressful time of life, but for many women, the experiences surrounding pregnancy and childbirth are emotionally trying.
Unfortunately, many pregnant women do not report their symptoms to a healthcare provider or loved one, and many do not receive treatment. Women who are currently abusing prescription drugs like Ativan, or who are at risk of substance abuse, can benefit from active intervention by friends, family members, or healthcare providers.
Is Ativan safe during pregnancy?
Managing anxiety, panic attacks, and anxiety-related conditions can be difficult during any phase of life, but especially during pregnancy. Most of what we know about the safety of common drugs used to treat anxiety in expectant moms is observational, rather than based on well-researched evidence and studies.
This holds true for the class of drugs called benzodiazepines, which are often used to treat intermittent anxiety. Benzodiazepines, like Ativan (lorazepam), are sedating drugs that slow down the function of your central nervous system, according to American Addiction Centers. They have a variety of clinical uses, including treatment of insomnia and substance abuse disorders, but they carry a sizable risk—they are potentially addictive, come with a host of possible side effects, can have severe withdrawal effects, and can be easily abused.
RELATED: What is Ativan?
These risks are heightened when applied to pregnant and nursing women, who not only have to worry about their own health but the health of their babies. Here’s what you should know about taking Ativan during pregnancy or while breastfeeding.
Is Ativan safe to take while pregnant?
Per the U.S. Food and Drug Administration (FDA), Ativan and generic lorazepam is a pregnancy category D drug, which means it carries known risks to pregnant women or their babies and should be avoided during pregnancy. That doesn’t mean the drug never has applications during pregnancy, but that serious considerations should be made between an expectant mother and her provider before taking it.
“There are drugs that are sometimes used in pregnancy that fall into the D category because they’re necessities for a condition that a woman has,” says Felice Gersh, MD, an OB-GYN and director of the Integrative Medical Group of Irvine in Irvine, California. “You have to ask what would happen if this drug wasn’t used, or what will happen if a woman is already on it [and stops taking it]?”
“You have to ask what would happen if this drug wasn’t used, or what will happen if a woman is already on it [and stops taking it]?”
The mental health of an expectant mother is hugely important to the health of her baby; however, Ativan comes with some documented risks to both mother and child.
- Some studies have found that taking Ativan (lorazepam) while pregnant can lead to preterm labor and low birth weight in infants, according to Sherry Ross, MD, an OB-GYN and women’s health expert at Providence Saint John’s Health Center in Santa Monica, California. A 2009 study published in the American Journal of Obstetrics and Gynecology found that benzodiazepines increased a woman’s chances of preterm labor and poor perinatal outcomes, including low birth weight and low Apgar scores.
- Taking Ativan in the first trimester has been associated with a slight increase in birth defects, including cleft lip and cleft palate, says Dr.
 Gersh. (The risk is small but does appear to exist.)
Gersh. (The risk is small but does appear to exist.) - Infants whose mothers used Ativan during pregnancy have a higher risk of neurological impairments. “[Ativan use can] cause floppy infant syndrome, which includes apnea, feeding difficulties, hypothermia, muscle weakness, tremors, jitteriness, respiratory depression, and impaired metabolic response to cold stress,” Dr. Ross says. This may result in a complicated newborn period, including possible intensive care stays for infants.
- Taking Ativan consistently throughout pregnancy or in the later stages of pregnancy can cause addiction and dependence in expectant mothers and even lead to symptoms of withdrawal in newborns after birth.
As with many category D drugs, women trying to conceive or planning to become pregnant often wonder if Ativan can cause infertility or miscarriage. Dr. Ross says there is an increased risk of miscarriage with Ativan use; a 2019 study in JAMA Psychiatry confirms an association between benzodiazepine use and miscarriage, but there are complicating factors (like the insomnia and anxiety the drugs are being used to treat in the first place).
While there’s no evidence that taking Ativan can make it harder to become pregnant, it may still be best to avoid it if you’re hoping to become pregnant soon. And there are certainly safer, more effective medications to take for anxiety during pregnancy.
“Currently there are no studies showing that Ativan can make it more difficult to get pregnant, [but] it’s always best to minimize drugs that could be potentially harmful while trying to conceive,” Dr. Ross explains.
How much Ativan or lorazepam can you take during pregnancy?
Generally speaking, Ativan should be avoided completely during the first trimester, says Dr. Ross, because fetal development is progressing quickly at this stage and the risk of birth defects is higher. Taking it during the second or third trimester should be done under consultation with an experienced provider (psychiatrist with expertise in pregnancy or OB/GYN) to evaluate the risks and benefits. Ideally, once you know you are pregnant, you should work with a provider to determine the safest, most effective treatment for anxiety or panic disorder.
“If the benefits of using this medication outweighs the risks, then it’s best to use it at the lowest dose [for] maximum effect,” says Dr. Ross, who adds that it’s best not to take Ativan for more than two weeks at a time.
What should I do if I’m taking Ativan and suddenly become pregnant?
Although Ativan isn’t safe during pregnancy, you shouldn’t abruptly stop taking it if you find out that you’re expecting. Depending on how much you have been taking or how long you have been using Ativan, you may have developed a dependence on it—and stopping cold turkey could cause serious withdrawal symptoms including seizures.
Instead, advises Dr. Ross, call your provider as soon as you find out you’re pregnant to develop a plan for safely discontinuing your Ativan (lorazepam) use. “It’s best to wean off slowly and with medical supervision…cutting back on the frequency and dose slowly is the safest way to taper off this [risky] medication so withdrawal symptoms don’t develop,” she says.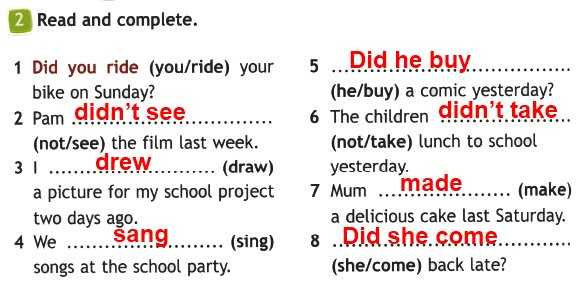
Is Ativan safe to take while breastfeeding?
Many drugs considered unsafe to use during pregnancy may end up being safe to use while breastfeeding, but Ativan’s safety profile doesn’t change. While we don’t have specific information about the connection between Ativan and breastfeeding, Dr. Gersh says the drug definitely passes to the baby through breast milk and can affect your baby’s alertness.
“Ativan suppresses brain function and a baby’s brain is developing rapidly [at this stage],” Dr. Gersh explains. “We know that frequent use of benzodiazepines in adults can lead to problems with cognition—the last thing you want to do is inhibit brain function of your baby.”
In addition to interfering with brain function, Dr. Gersh says the relaxing properties of benzodiazepines like Ativan can inhibit a baby’s ability to suck or feed properly, which could lead to malnutrition. Failure to breastfeed, combined with cognitive side effects, could also interfere with the mother-child bonding process in the newborn phase. Infants exposed to benzodiazepines can also be excessively irritable.
Infants exposed to benzodiazepines can also be excessively irritable.
RELATED: Ativan side effects
How can I safely manage my anxiety while pregnant and breastfeeding?
If you’re living with anxiety while pregnant or postpartum, don’t let the warnings about Ativan scare you away from getting help; while there are no sedatives or benzodiazepines considered safe for use during pregnancy, there are other safer classes of drugs that can be used to treat your symptoms.
In fact, Dr. Gersh says that many doctors are moving away from using Ativan and other sedatives to treat chronic anxiety issues in all patients, pregnant or not. In general, these drugs are not an optimal choice for treatment of chronic anxiety thanks to their high risk of dependency and addiction, a risk that increases with ongoing use. The American College of Obstetricians and Gynecologists (ACOG) recommends that therapy for depression or anxiety during pregnancy be individualized; treatment should incorporate the clinical expertise of the mental health clinician, obstetrician, primary healthcare provider, and pediatrician.
So what does this mean for pregnant or breastfeeding patients with anxiety?
- You should consider receiving therapy from a qualified mental health professional with expertise in pregnancy care. Many anxiety disorders can be managed through cognitive behavioral therapy and mindfulness practices, which a professional can help you with.
- If medication is needed during pregnancy, your doctor can talk to you about pregnancy-safe options. According to Massachusetts General Hospital, Prozac (fluoxetine), selective serotonin reuptake inhibitors, and many tricyclic antidepressants are often considered safe for use during pregnancy. However, tricyclic antidepressants may not be the preferred therapy for depression while pregnant.
- If medication is needed postpartum, while breastfeeding, there are even less restrictions. Zoloft is generally considered the safest anti-anxiety medication to use while nursing, primarily because doctors know the most about its use during breastfeeding.
 But many antidepressants, including SSRIs, are regarded as safe to take while breastfeeding.
But many antidepressants, including SSRIs, are regarded as safe to take while breastfeeding.
Work with your healthcare provider to find the best treatments option for you.
Arpimed
Tell your doctor if you are taking, have recently taken or might take any other medicines. It is especially important to note the following drugs:
If necessary, your doctor will reduce the dose of these drugs before you use lorazepam.
Avoid alcohol while taking lorazepam as this may increase the sedative properties of the drug.
Tell your doctor or pharmacist if you are taking Lorazepam before using any other medicines or when you are hospitalized. nine0003
Some elderly patients may experience dizziness and fainting after taking Lorazepam.
When taking Lorazepam, there is a risk of developing addiction, which can lead to a gradual decrease in effectiveness after several weeks of taking Lorazepam.
Lorazepam has the potential to develop dependence, particularly in patients with a history of alcohol and/or recreational drug abuse.
With the usual regimen of lorazepam, the development of dependence is unlikely, but the risk increases with increasing dose and duration of treatment, as well as in patients with a history of alcohol and / or recreational drug abuse, or in patients with a personality disorder. Therefore, lorazepam should be avoided in patients with a history of alcohol and/or recreational drug abuse. nine0003
Dependence can lead to the development of a withdrawal syndrome, especially when treatment is stopped abruptly. Therefore, it is necessary to cancel the drug gradually.
When taking lorazepam for more than 4 weeks, your doctor should conduct a study of the peripheral blood picture, as well as a biochemical blood test for liver markers, since drugs in this group can lead to impaired liver function.
Long-term use of Lorazepam may lead to the development of drug dependence. Therefore, Lorazepam is usually prescribed in short courses lasting from several days to 4 weeks, including a period of dose reduction and drug withdrawal. This reduces the risk of developing drug dependence or adverse side effects observed when the drug is discontinued. (See section "Cancellation of Lorazepam"). nine0003
This reduces the risk of developing drug dependence or adverse side effects observed when the drug is discontinued. (See section "Cancellation of Lorazepam"). nine0003
The dose of Lorazepam should be increased gradually to avoid side effects.
How to take Lorazepam
Lorazepam should be taken exactly as directed by your doctor. If you have any doubts, then you should consult with your doctor.
When Lorazepam is used to treat anxiety and insomnia, treatment usually lasts from several days to 4 weeks, including a period of dose reduction and drug withdrawal.
The physician should prescribe the lowest effective dose, calculated for the shortest possible period of taking the drug.
Lorazepam tablets should be swallowed with water.
Adults and children over 13 years of age
For anxiety, the daily dose of Lorazepam is 1-4 mg taken in divided doses. Your healthcare provider will determine how often you should take Lorazepam.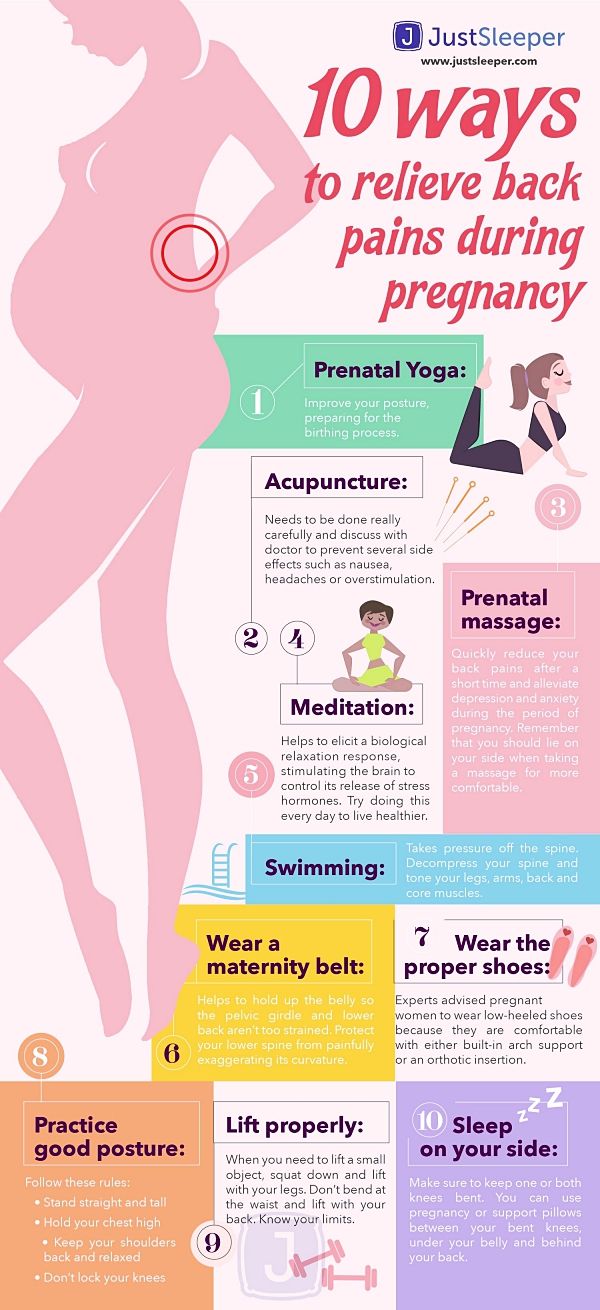 It is not recommended to take Lorazepam to children under 12 years of age with anxiety. nine0003
It is not recommended to take Lorazepam to children under 12 years of age with anxiety. nine0003
For sleep disturbances, 1-2 mg Lorazepam at bedtime is prescribed. Before taking the drug, you must be sure that you can sleep for 7-8 hours.
Lorazepam 2-3 mg is given the night before surgery and 2-4 mg 1-2 hours before surgery.
Children 5 to 13 years old
For surgery, the dose is usually 0.5-2.5 mg (depending on your child's weight) taken one hour before the procedure. nine0003
Lorazepam is not recommended for use in children 5 to 13 years of age for the treatment of anxiety and sleep disorders, and in children under 5 years of age.
Elderly
The physician should prescribe lorazepam to elderly or malnourished patients at low doses.
The drug may be effective at half or even less than the recommended dose in elderly patients, but if necessary, the dose should be adjusted.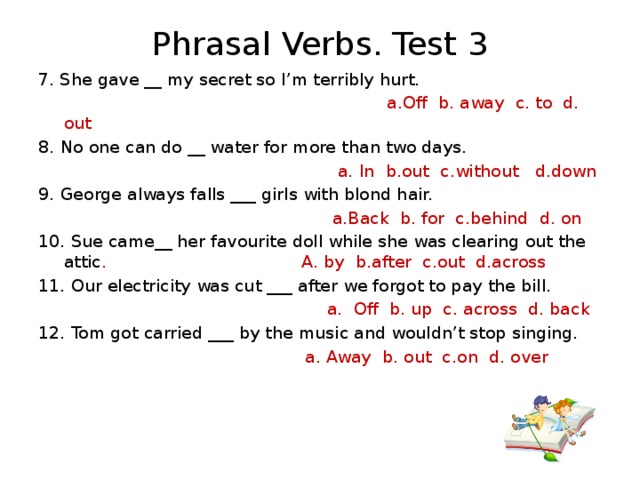 nine0003
nine0003
Patients with renal and hepatic insufficiency
In case of impaired renal function or mild to moderate hepatic insufficiency, Lorazepam is allowed to be taken only in low doses.
Lorazepam is contraindicated in patients with severe hepatic impairment.
If you forget to take Lorazepam
If you forget to take Lorazepam to treat anxiety and if less than 3 hours have passed from your scheduled appointment time, you should take it as soon as you remember. If more than 3 hours have passed from the appointed time, do not worry, take the next dose at the appointed time. Do not take a double dose to make up for a missed one. nine0003
If you forget to take Lorazepam to treat a sleep disorder, take it if you are sure you can sleep for 7-8 hours after taking the drug.
If you have taken more Lorazepam than recommended
If you have taken more Lorazepam than prescribed by your doctor, get medical help right away, call your doctor or go to the nearest hospital. Take the medicine package with you, even if there are no pills left. nine0003
Take the medicine package with you, even if there are no pills left. nine0003
Stopping Lorazepam
After completing the prescribed course of treatment, your doctor will decide whether to continue further treatment.
The dose and frequency of lorazepam should be reduced gradually until the drug is discontinued. This allows your body to adjust to the absence of Lorazepam and reduce the risk of adverse effects when the drug is discontinued. Your doctor will explain to you how to do this. nine0003
If you have any further questions on the use of this medicine, ask your doctor or pharmacist.
Withdrawal
Abrupt discontinuation of Lorazepam may result in withdrawal symptoms such as headaches, muscle pain, anxiety, tension, depression, restlessness, dizziness, nausea, diarrhea, loss of appetite, irritability, confusion, confusion agitation, tremors, abdominal pain, heart rhythm disturbances, short-term memory loss, fever, and sweating. Possible relapse of insomnia. If you have any of these symptoms, contact your doctor. nine0003
Possible relapse of insomnia. If you have any of these symptoms, contact your doctor. nine0003
Do not stop taking Lorazepam suddenly. This can lead to more severe withdrawal symptoms such as loss of sense of reality, feelings of unreality or detachment from everyday life, loss of the ability to feel emotions.
Some patients experience numbness or tingling of the hands or feet, vomiting, ringing in the ears, muscle twitches, hallucinations, seizures, and hypersensitivity to light, sound, and touch. If you have any of these symptoms, contact your doctor immediately. nine0003
Lorazepam - description of the substance, pharmacology, use, contraindications, formula
Contents
- Russian name
- English name
- Latin name of the substance Lorazepam
- Chemical name nine0145 Gross formula
- Pharmacological group of the substance Lorazepam
- Nosological classification
- CAS code
- Pharmacological action
- Characteristic
- Pharmacology nine0145 Use of the substance Lorazepam
- Contraindications
- Restrictions for use
- Use in pregnancy and lactation
- Side effects of the substance Lorazepam
- Interaction
- Overdose nine0145 Dosage and administration
- Precautions
- Special instructions
- Trade names with the active substance Lorazepam
Structural formula
Russian name
Lorazepam
English name
Lorazepam
Latin name of the substance Lorazepam
Lorazepamum ( genus Lorazepami)
Chemical name
7-Chloro-5-(2-chlorophenyl)-1,3-dihydro-3-hydroxy-2H-1,4-benzodiazepin-2-one
Generic formula
C 15 H 10 Cl 2 N 2 O 2
Pharmacological group of the substance Lorazepam 9002
AnxiolyticsNosological classification
ICD-10 code list
- R45.
 1 Anxiety and agitation
1 Anxiety and agitation - F51.0 Insomnia of non-organic etiology
- G47.0 Disorders of falling asleep and maintaining sleep [insomnia]
- F10.5 Alcoholic psychosis
- F91 Conduct disorders
- F30 Manic Episode
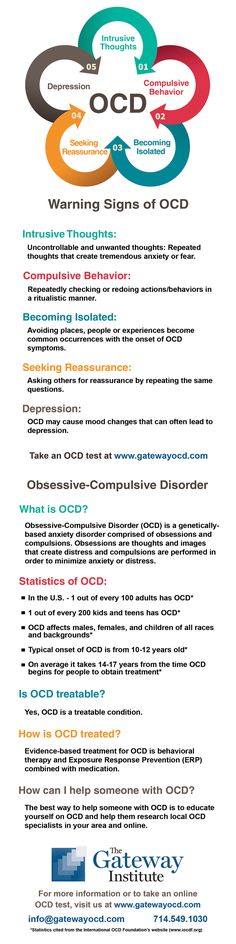
- F42 Obsessive-compulsive disorder
- F25 Schizoaffective disorders
- F41.0 Panic disorder [episodic paroxysmal anxiety]
- Z100* CLASS XXII Surgical practice
- F60 Specific personality disorders
- G44.
 2 Tension headache type
2 Tension headache type - R45.0 Nervousness
- R45.7 State of emotional shock and stress, unspecified
- F32 Depressive episode
- F43.1 Post-traumatic stress disorder
- F40.0 Agoraphobia
- F43.2 Adjustment disorder
- F34.1 Dysthymia
- F41.1 Generalized anxiety disorder
- F43.0 Acute stress reaction
- G40 Epilepsy
- F10.3 Withdrawal state
CAS code
846-49-1
Pharmacological action
Pharmacological action - nine0205 anxiolytic , muscle relaxant , anticonvulsant , sedative , hypnotic , central .:no_upscale()/cdn.vox-cdn.com/uploads/chorus_asset/file/24286525/NightGathering.jpg)
Characteristics
Anxiolytic, benzodiazepine derivative.
Almost white powder, very slightly soluble in water.
Pharmacology
Interacts with specific benzodiazepine receptors of the GABA-benzodiazepine receptor complex, increases the sensitivity of GABA receptors to GABA. As a result, the frequency of opening of transmembrane channels for chloride ions increases, the postsynaptic membrane of the neuron is hyperpolarized, neuronal activity is inhibited, and interneuronal transmission to the CNS is inhibited. The effects are due to the influence on various parts of the central nervous system: the amygdala complex of the limbic system (anxiolytic), the reticular formation of the brain stem and nonspecific nuclei of the thalamus, hypothalamus (sedative and hypnotic), spinal cord (muscle relaxant), hippocampus (anticonvulsant). It reduces the excitability of subcortical formations (limbic system, thalamus, hypothalamus) responsible for the implementation of emotional reactions, and inhibits the interaction of these structures with the cerebral cortex. Stabilizes vegetative functions. nine0003
Stabilizes vegetative functions. nine0003
Suppresses anxiety, fear, reduces psychomotor agitation, emotional stress. It has anti-panic and amnestic (mainly for parenteral use) action. It is effective for insomnia caused by anxiety or a short-term stressful situation: it facilitates the onset of sleep (shortens the period of falling asleep), reduces the number of night awakenings, and increases the duration of sleep. It inhibits polysynaptic spinal reflexes and lowers the tone of skeletal muscles. nine0003
Lorazepam has low toxicity and wide therapeutic range.
An animal reproduction study showed that administration of lorazepam at doses of 40 mg/kg orally and 4 mg/kg or more IV to rabbits resulted in fetal resorption and an increased incidence of fetal death. Causes developmental anomalies in rabbits, regardless of dose. In an 18-month study in rats, no carcinogenic activity was found.
Good but slowly absorbed from the gastrointestinal tract when taken orally, bioavailability is 90%. max "> C max is achieved within 2 hours and is dose dependent: at a dose of 2 mg max"> C max is 20 ng / ml. About 85% binds to plasma proteins. The equilibrium concentration in the blood is usually reached after 2-3 days. Passes through the BBB and the placental barrier. It is rapidly metabolized in the liver by conjugation to form the main inactive metabolite, lorazepam glucuronide. 1/2 "> T 1/2 unconjugated lorazepam - about 12 hours, the main metabolite - 18 hours. Excreted mainly by the kidneys, mainly in the form of glucuronide.
max "> C max is achieved within 2 hours and is dose dependent: at a dose of 2 mg max"> C max is 20 ng / ml. About 85% binds to plasma proteins. The equilibrium concentration in the blood is usually reached after 2-3 days. Passes through the BBB and the placental barrier. It is rapidly metabolized in the liver by conjugation to form the main inactive metabolite, lorazepam glucuronide. 1/2 "> T 1/2 unconjugated lorazepam - about 12 hours, the main metabolite - 18 hours. Excreted mainly by the kidneys, mainly in the form of glucuronide.
When administered intramuscularly, max "> C max is achieved in 60-90 minutes. 1/2"> T 1/2 when administered parenterally is 16 hours. When used for 6 months, no cumulation phenomena are observed. The pharmacokinetic parameters of lorazepam do not change in the elderly.
Application of the substance Lorazepam
Neuroses accompanied by anxiety, agitation, incl. generalized anxiety disorder, post-traumatic stress disorder, phobias, obsessive-compulsive disorder, psychoreactive states, emotional reactive disorders, anxiety in depressive states of various origins (usually in combination with antidepressants), insomnia, psychosomatic disorders (including heart - vascular, gastrointestinal and other diseases), premedication before surgical and diagnostic manipulations (in combination with analgesics), tension headache; nausea and vomiting caused by chemotherapy, epilepsy (as part of combination therapy), alcoholic delirium and withdrawal syndrome in chronic alcoholism (as part of combination therapy). nine0003
nine0003
Contraindications
Hypersensitivity, incl. to other benzodiazepines, myasthenia gravis, angle-closure glaucoma, acute intoxication with CNS depressants, respiratory depression, liver failure, pregnancy (especially the first trimester), breast-feeding, age up to 18 years.
Restrictions on use
Chronic respiratory failure, sleep apnea syndrome, open-angle glaucoma, drug and alcohol dependence, depression (see Precautions), psychosis, severe renal impairment. nine0003
Use during pregnancy and lactation
Contraindicated during pregnancy (especially in the first trimester). At the time of treatment should stop breastfeeding.
Side effects of the substance Lorazepam
From the side of the nervous system and sensory organs: lethargy, fatigue, drowsiness, disorientation, headache, dizziness, depression, ataxia, sleep disturbance, agitation, visual impairment, episodes of amnesia.
From the digestive tract: dry mouth, nausea, vomiting, diarrhoea, change in appetite.
From the side of the skin: erythema, urticaria.
Other: changes in blood composition (leukopenia), increased LDH activity.
May develop addiction, drug dependence, withdrawal syndrome, rebound syndrome (see "Precautions").
Interaction
Lorazepam enhances the effect of CNS depressants, incl. phenothiazines, narcotic analgesics, barbiturates, antidepressants, hypnotics, anticonvulsants, antihistamines with a sedative effect. Potentiates the action of general and local anesthetics, enhances the action of curare-like drugs. With simultaneous use with alcohol, in addition to increasing the inhibitory effect on the central nervous system, paradoxical reactions are possible (psychomotor agitation, aggressive behavior, a state of pathological intoxication). Nicotine inhibits the activity of lorazepam (accelerates its metabolism). nine0003
Overdose
Symptoms: drowsiness, arterial hypotension, confusion, depression of reflexes, coma.
Treatment: induction of vomiting, gastric lavage, intravenous administration of norepinephrine to increase blood pressure, symptomatic therapy, monitoring of vital signs. The introduction of a specific antidote - an antagonist of benzodiazepine receptors flumazenil (in a hospital setting).
Dosage and administration
Inside. nine0206 The dosage regimen and the duration of the course of treatment are set strictly individually.
In neurological practice - 1 mg 2-3 times a day; in psychiatric practice - 4-6 mg / day; with insomnia - 1-2 mg 30 minutes before bedtime. In elderly and debilitated patients, the dose should not exceed 2 mg / day (in divided doses). In patients with liver and / or kidney disease, as well as in patients with cerebral sclerosis, hypotension, heart failure, underweight, dose adjustment is recommended. nine0003
Precautions
Use with caution in depressed patients due to suicidal tendencies. In patients with drug and alcohol dependence, use under close medical supervision.
Side effects are usually observed at the beginning of therapy. The possibility of a more frequent occurrence of side effects in elderly and debilitated patients should be taken into account.
During treatment and for 2 days after its completion, it is necessary to exclude the intake of alcoholic beverages; drivers of vehicles and people whose work requires a quick mental and physical reaction, and is also associated with increased concentration of attention, should not engage in professional activities during this period. nine0003
With prolonged use, addiction and drug dependence may occur (especially when taking high doses). In this regard, lorazepam should not be used for longer than 4-6 weeks. If long-term treatment is necessary, weekly breaks in taking the drug should be periodically taken. With a sharp cessation of treatment, a withdrawal syndrome may occur (tremor, convulsions, abdominal or muscle cramps, vomiting, perspiration), and symptoms similar to those of the disease (anxiety, agitation, irritability, emotional stress, insomnia, convulsions) may also occur.