How to overcome fear of sleeplessness
Putting the Fear of Sleeplessness to Rest
Fear can be a powerful disincentive to change. It was one of several factors that kept me from undergoing cognitive-behavioral therapy for insomnia (CBT-I) for over a decade.
Not that I wasn’t eager to trade in my bad nights for better nights. I’d struggled with bouts of sleeplessness since my teens. Stress at work or anticipation of a challenging day ahead could keep me wound up until 2 or 3 in the morning, and occasionally all night. A few bad nights could usher in a cycle of insomnia lasting three or four weeks.
But knowing in advance what CBT-I would entail — restricting my sleep every night — was a deal-breaker for me. Subject myself to a series of short nights that were sure to make my daytime symptoms worse? Prolong my exhaustion, my bad mood, and my trouble thinking, on the slim chance that sleep restriction would turn my problem around?
The prospect was not just distasteful. It was also scary. What if during my sleep period the Sandman never showed up? The fear of it tied my stomach in knots. While CBT-I might help others, it was not for me.
But I laid my apprehensions aside and decided to try it as part of my research for a book about insomnia. CBT-I was every bit as difficult as I’d anticipated. Restricting my time in bed turned me into a zombie the first few days. I shuffled along with mush for brains, forgetting where I put my keys and barely able to compose a paragraph. Which made me cross: why such punishment to achieve something that should be effortless?
But it was at night when the sleep issue came to a head, forcing me to confront my fear of sleeplessness face to face. How else to explain the freak show those early nights of treatment became? No matter that I had to march myself around the house to stay awake until 12:30, my designated bedtime. As I was heading to the bedroom, fear ambushed me in the doorway. I panicked at the thought of not sleeping and how rotten I’d feel the next day. I was much too aroused to fall asleep.
Treatment protocol required that I avoid the bedroom until I felt sleepy, so I turned away and sat down to read until I felt myself drifting off again. But when I went to the bedroom to lie down, fear seized me again, and then a third time, and a fourth. I got up, I lay down. Lay down, got up. How long would the torture last?
But when I went to the bedroom to lie down, fear seized me again, and then a third time, and a fourth. I got up, I lay down. Lay down, got up. How long would the torture last?
I battled my fears for three nights and slogged through three miserable days. If I hadn’t been determined to see the thing through for the sake of my research, I might easily have given up. But at 12:30 on the fourth night I collapsed and slept until the alarm woke me at 5:15. I’d been shot cleanly through the goalposts without a moment’s wakefulness.
That was the beginning of the end of my protracted bouts of insomnia. I still had miles to go: adding time in bed as sleep became more solid, tweaking bed and wake times, modifying my bedtime routine. But staying the course with CBT-I eventually led to sounder, more regular sleep. It didn’t “cure” my insomnia; I’m still susceptible to stress-related sleep disturbance. But now it takes a bigger challenge to throw my sleep off course, and when it goes off course I can right the ship in days rather than weeks.
CBT-I was also an exposure therapy for me, routing my fear of sleeplessness. Before treatment, the mere sight of the sun setting or the thought of a bad night ahead could make my stomach clench.
But no longer. By forcing me to confront my fear while priming me to sleep by means of sleep restriction, it effectively extinguished that fear. As the days went by, I found myself sleepier and sleepier at bedtime and often fell asleep within minutes of lying down. I was less fatigued and my thoughts were clearer during the day. As bedtime approached, I began to expect that I would sleep. Eventually my fear of sleeplessness all but faded away: a great boon after having lived with the fear for so many years.
But CBT-I as I experienced it was not a gentle or systematic desensitization. It was scary to contemplate and scarier still to follow through with. During an interview in September 2011, I told sleep investigator Michael Perlis that it was like staring at a big spider in front of my nose.
Perlis, associate professor of psychology and director of the Behavioral Sleep Medicine Program at the University of Pennsylvania, acknowledged my point. “I never said that sleep restriction was kind and gentle, and you’re right to say that it’s not systematic. There are other forms of therapy that are implosive,” he said, “where they throw you in a bin with snakes” in an attempt to change a response or behavior very quickly. The mechanism that enables CBT-I to work as effectively as it does — a dose of sleep restriction sufficient to enable the rapid and overwhelming buildup of sleep drive — would be lost if therapy were administered in attenuated doses. An already disagreeable treatment would only be further drawn out.
But as Perlis and I were discussing why the response rate to CBT-I is only 70 to 80 percent*, I returned to the scare factor. Not everyone with chronic insomnia develops fear of sleeplessness. I wondered aloud if the insomniacs who do — whose fear would tend to manifest as trouble getting to sleep at the beginning of the night, or “sleep onset insomnia” — might be more likely than others to drop out of therapy.
CBT-I works equally well for all three subtypes of insomnia patients, Perlis replied: people with sleep-onset insomnia, people prone to middle-of-the-night awakenings, and those who awaken too early. But if a study were done to ascertain who across the subtypes tended to suffer the most during treatment and drop out, Perlis thought I might be right. “It’s all the onset folks, because [with sleep restriction] you’ve just done the meanest thing you can do.” Not only have you set them up to experience sleep deprivation; you’ve also forced them to face down a monster in their bed.
My fear of sleeplessness is water over the dam. But the thought of having to face it was part of what kept me from trying CBT-I many years before I did, and I regret it. Those years would no doubt have been better without the tormenting bouts of insomnia I experienced so often and at such great length.
My concern is now for others like me, who, struggling with fear of sleeplessness, shy away from CBT-I or get overwhelmed early in treatment and drop out. As the sleep community looks for ways to deliver therapy to more patients, addressing the anxieties of this group of insomniacs early on might make a difference. Talking about fear of sleeplessness when presenting CBT-I as an option, or at the start of sleep restriction, might encourage more sleep onset insomniacs to try it and stick with it long enough to reap the benefits.
As the sleep community looks for ways to deliver therapy to more patients, addressing the anxieties of this group of insomniacs early on might make a difference. Talking about fear of sleeplessness when presenting CBT-I as an option, or at the start of sleep restriction, might encourage more sleep onset insomniacs to try it and stick with it long enough to reap the benefits.
Reference
Morin, C.M., et al. (1999). Nonpharmacologic treatment of chronic insomnia. An American Academy of Sleep Medicine review. Sleep, 22(8), 1134-1156.
How to Handle the Fear of Sleep
These strategies may help take the dread out of going to sleep.
Written by Winnie Yu
Every night, for the last 10 years, Traci Coulter has struggled to sleep. Minutes tick by, then hours. Coulter begins to fret about her to-do list the next day and all her responsibilities as a public relations executive. To make matters worse, she knows a garbage truck is coming by at 3 a. m. and will wake her up - a thought that only makes her more anxious.
m. and will wake her up - a thought that only makes her more anxious.
“It’s an ongoing cycle of not getting the rest that I need, and it causes such anxiety for me,” says Coulter, 38, who lives in New York City. “I have nights where I sit and stew without any sleep at all.” Some nights, she’s afraid to go to bed.
Going to sleep might seem like a natural act, but for some people, sleep is a source of dread. Becoming anxious about sleep is actually a form of performance anxiety, says Alexander Obolsky, MD, a psychiatrist who specializes in trauma and stress, and assistant professor of clinical psychiatry at Northwestern University Medical School in Chicago.
Some older adults for instance, get worried because the amount of sleep they get diminishes. “They get anxious because they think they’re not sleeping enough,” Obolsky says.
Tossing and Turning
Often, dreading sleep is the result of a sleep disorder. "Sleep dread is extremely common," says Matthew Edlund, MD, director of the Center for Circadian Medicine in Sarasota, Fla. , and author of The Power of Rest.
, and author of The Power of Rest.
Insomnia, which affects as many as 40% of Americans at one time or another, is the most common cause of this fear. When people don’t get the sleep they need, they become concerned.
But worrying about it only worsens the insomnia, Edlund says. “We’ve turned sleep into a job,” he says. “We think, ‘Oh my gosh, I have to have enough sleep to make everything work.’ They’re worried about sleep, so they can’t sleep.”
Stalked by Chronic Nightmares
Chronic nightmares are another troublesome sleep disorder that can cause fear, says Shelby Harris, PsyD, CBSM, director of the Behavioral Sleep Medicine Program at the Montefiore Medical Center’s Sleep-Wake Disorders Center in New York City. Children are especially vulnerable, but adults - especially those who suffer from post-traumatic stress disorder -- experience nightmares, too.
Joni Aldrich, 57, of Winston-Salem, N.C., began to dread sleep after she lost her husband to brain cancer four years ago. After he had a seizure, she had to make the difficult decision to suspend treatment, an experience that traumatized her.
After he had a seizure, she had to make the difficult decision to suspend treatment, an experience that traumatized her.
Every night, she had nightmares of him begging her to help him, but she couldn’t. She would awaken shaking. Aldrich finally got help from a counselor and began taking an anti-anxiety medication to help her sleep. “I still take the anti-anxiety medication in a very low dose, because I fear the results otherwise,” says Aldrich, CEO of Cancer Lifeline Publications. “Even one of those nightmares wouldn't be worth it. And, I still go to bed later than I should just to make sure that I'm really tired.”
Fears Related to Sleep Apnea
Still others are fretful about sleep because they have health conditions. People who have sleep apnea for example, sometimes fear that they’ll stop breathing in their sleep.
Harris says that fear is rare, but may occur when someone first learns that he or she has sleep apnea and is waiting for a CPAP (continuous positive airway pressure) device to treat the condition.
“Once the apnea is under control, people sleep better knowing they’re not waking up multiple times a night,” Harris says.
So what can you do to eliminate the fear of sleep? Here’s what experts suggest:
Change Your Thinking.
Like many anxieties, dread of sleep is all about perspective. Rather than dwell on the negative effects of sleeplessness, remind yourself that it’s perfectly normal to have occasional bad nights and that occasional nighttime awakenings are to be expected.
If you’re anxious because you’re anticipating a disruption, tell yourself to expect it. “I knew an internist who was on call and couldn’t sleep because he was always expecting a call,” Edlund says. “I told him just to expect calls and not worry about it, and he slept much better after that.”
Practice Good Sleep Hygiene.
The basics:
- Go to bed at the same time every night and wake up at the same time every morning.
- Don’t eat or drink any caffeine in the four to five hours before bed.

- Resist the urge to nap.
- Avoid exercise two hours before bed.
- Keep your bedroom cool and dark.
- Limit your bedroom activities to sleep and sex.
If you can’t sleep, get up and do something boring. “Keep a boring book on your bed table,” Obolsky says.
Also, create a restful routine. Prime your body for bed by doing the doing the same things every night. A restful routine that involves a warm bath, listening to music, or deep breathing can be especially helpful if you have insomnia, Edlund says.
Consider Getting Medical Help.
If you have a sleep disorder that doesn’t let up, such as insomnia or chronic nightmares, talk to a sleep specialist.
Insomnia can be treated with cognitive behavioral therapy or sleep medications. Chronic nightmares may require imagery rehearsal therapy that involves rewriting and rehearsing a new version of the nightmare during the day. It can also be treated with various prescription medications. You should also talk to your doctor if you think you have sleep apnea or another condition that’s disrupting your sleep.
For Coulter, training for a marathon in 2008 provided a temporary break from the sleeplessness. She also gets some relief by taking a sleep medication, though she says it doesn’t always work. She is now considering seeing a sleep specialist and in the meantime, has started running again. “Running does help,” she says. “I think I shift my anxiety to doing a good run or doing well in a race.”
How to overcome the fear of sleep (somniphobia)?
Some people have a strong and deep fear of objects, beings, circumstances, events that others seem relatively harmless. For example, a person may be pathologically afraid of spiders, clowns, heights, or something else that in itself does not pose any threat and therefore does not cause unlimited, uncontrollable and unreasonable fear in other people.
Such strong fears of seemingly neutral objects or situations are called specific (isolated) phobias. Some of the specific phobias can significantly affect our daily life. One of them is somniphobia, it is also hypnophobia or clinophobia. People suffering from somniphobia are afraid to fall asleep - just the thought that they will have to sleep at night terrifies them.
People suffering from somniphobia are afraid to fall asleep - just the thought that they will have to sleep at night terrifies them.
The mere thought of sleep terrifies a person with somniphobia
If for most of us a cozy bed and a warm blanket is an opportunity to relax, get away from problems and fall asleep peacefully, then for those suffering from somniphobia, the upcoming night's rest is not a reward, but a punishment tantamount to execution. No wonder they are terrified of falling asleep. The result is a chronic lack of sleep, which negatively affects the quality of life, psyche and physical health - memory is disturbed, immunity weakens, weight increases, and a number of other serious problems arise.
Fear of sleep - what is it? How to understand that you have somniphobia and how it can be caused?
Fear of sleep - what is it?
A somniphobic sufferer experiences extreme anxiety at the mere thought of sleep. Since the process of going to sleep and sleep itself is associated with fear, stress, horror, such a person falls asleep with great difficulty, even if he is very tired. And if he still manages to get some sleep, the rest turns out to be fragmented and of poor quality.
And if he still manages to get some sleep, the rest turns out to be fragmented and of poor quality.
A person cannot fall asleep, even if he is very tired
Signs and symptoms
Symptoms and manifestations of fear of sleep are usually divided into psychological and physical.
Psychological symptoms of somniphobia:
- Increasing distress as bedtime approaches.
- Feeling of anxiety and fear at the thought of sleep.
- Panic attacks occurring at the time when it is necessary to go to bed.
- Memory deterioration.
- Irritability or mood swings.
- Difficulty concentrating on anything other than worrying about sleep.
These obsessive thoughts and stressful conditions, combined with lack of sleep, have a strong negative effect on the body.
Physical symptoms of somniphobia:
- Nausea resulting from and against stress.
- Palpitations and oppression of the chest at the thought of sleep.
- Sweating, hyperventilation (rapid breathing) or chills at the thought of sleeping.
- Increased levels of stress hormones such as cortisol.
- In children - crying, refusal to sleep.
- Chronic fatigue and daytime sleepiness.
Daytime sleepiness and chronic fatigue are a consequence of chronic lack of sleep in somniphobia
Many of the above symptoms are very similar to those of panic disorder. The key difference between panic disorders and phobias is that panic disorders are not as closely related to a specific object or situation. Like the manifestations of any specific phobia, the symptoms of somniphobia appear only in a situation that causes fear, or when approaching it.
Why might a person be afraid to fall asleep?
Experts don't know exactly why people develop phobias. Including the mechanism of development of somniphobia is not completely clear.
Phobias in general are believed to arise from a combination of genetic and acquired factors. They usually develop during childhood. The likelihood of their occurrence may be higher if close family members also suffer from phobias - due to hereditary predisposition or due to common life experience. Phobias are more common in women and may exist alongside other anxiety disorders.
They usually develop during childhood. The likelihood of their occurrence may be higher if close family members also suffer from phobias - due to hereditary predisposition or due to common life experience. Phobias are more common in women and may exist alongside other anxiety disorders.
Most experts say that somniphobia is not related to sleep itself - a person is afraid of something that might happen during a night's rest. Fear of sleep and falling asleep can be caused by various factors and is often the result of the problems listed below.
Chronic nightmares
Most of us sometimes have bad dreams, but some people have them quite often. Night terrors can feel so real that the person does not want to go to bed for fear of having similar dreams again. In particular, because of the fear of nightmares, children are often afraid to go to bed.
Nightmares often cause somniphobia in a child
Depression and anxiety
People who suffer from an anxiety or depressive disorder may also develop somniphobia. Such a person often experiences a general fear of sleep and at night, he may have difficulty falling asleep, nightmares. In the daytime, it is easier for him to switch from negative thoughts to solving work or household tasks, communication. There are fewer distractions at night than during the day, so his anxiety increases at night.
Such a person often experiences a general fear of sleep and at night, he may have difficulty falling asleep, nightmares. In the daytime, it is easier for him to switch from negative thoughts to solving work or household tasks, communication. There are fewer distractions at night than during the day, so his anxiety increases at night.
Increased symptoms of depression and anxiety at night
In addition, people with anxiety and depressive disorders often worry about the fact that they will not be able to control themselves during sleep.
Traumatic incidents
Fear of sleep may develop after a psychotrauma. For example, after the death of a loved one, a physical attack, or any other experience that leads to PTSD (post-traumatic stress disorder).
The tendency of people with PTSD to develop somniphobia has objective reasons - this disorder is often accompanied by nightmares, sleepwalking or other sleep disturbances, which may be accompanied by a general fear of sleep.
The loss of a loved one is a powerful psychotraumatic factor
Symptoms of post-traumatic stress disorder often flare up at night - fear of recurrence of episodes of exacerbations and increased vulnerability due to lack of control over one's thoughts during sleep also become causes of hypnophobia.
Sleepwalking
Sleepwalking or somnambulism is the most common parasomnia, in which a person, continuing to sleep, gets up and walks. When traveling at night, somnambulists are not aware of their actions, so the disease is usually first detected by a family member, loved one, or even a random roommate (for example, in a sanatorium or hotel). When a sleepwalker learns about his problem, he usually feels embarrassed about what he did during sleep. He is also worried that this will happen again in the future. In this regard, a person suffering from sleepwalking is afraid to go to bed.
Sleepwalkers may develop somniphobia
Some somnambulists are injured during unconscious night wanderings, sometimes so severe that they have to be hospitalized. The fear of getting seriously injured can also develop into a fear of sleep, especially if a person lives alone.
The fear of getting seriously injured can also develop into a fear of sleep, especially if a person lives alone.
Fear of death
Some people are afraid to fall asleep and never wake up again. Even in the absence of any reason whatsoever to die in a dream, the fear of death can cause somniphobia.
If you have obstructive sleep apnea (OSA), you may also be afraid of dying at night. For example, sleep apnea sufferers sometimes have an unreasonable fear that their CPAP machine will fail, causing them to stop breathing and never resume.
A person with OSAS may be afraid that the CPAP machine will break, they will suffocate and die in their sleep.
Sleep paralysis
Sleep paralysis is a sleep disorder in which a person wakes up and cannot move, as if paralyzed: the mind is awake, but the body is at rest and "does not obey the orders" of the brain. Although doctors emphasize that these episodes of immobility are harmless, they can be very frightening for people experiencing them.
In addition, such patients often report seeing or hearing strange, frightening hallucinations during an attack. It also provokes the appearance of fear before falling asleep, which can lead to the development of anxiety during sleep, awakening and fear of falling asleep again.
Sleep talk
Sleep talk is common and usually harmless. When talking at night, people usually say something incomprehensible or meaningless. However, if you are keeping a secret or worrying about revealing something intimate while unconscious, this can lead to a phobia.
Horror movies
Watching a scary movie, especially before going to bed, can make your mind run through potential dangers that could happen during the night. These fears range from being attacked by fictional monsters to more realistic scenarios such as burglary.
Watching a horror movie at night is the path to somniphobia
Possible consequences of somniphobia
Like any other phobia, the fear of sleep affects the behavior and personality of a person, negatively affects his social activity. However, the effects of somniphobia are not limited to this. Chronic sleep deprivation significantly impairs quality of life by causing:
However, the effects of somniphobia are not limited to this. Chronic sleep deprivation significantly impairs quality of life by causing:
Daytime sleepiness . Not getting enough sleep at night, you will inevitably feel tired the next day, you will constantly be sleepy.
Chronic fatigue . The longer you live with this phobia, the more likely you are to develop chronic fatigue syndrome.
Mood swings . Lack of sleep negatively affects mood, making us irritable and quick-tempered.
Problems with memory, attention, coordination . Without proper sleep, the brain does not have time to process the information received and “place it on the shelves”. As a result, cognitive abilities are impaired, including memory impairment, the ability to perceive and analyze new information. In addition, dizziness and difficulty concentrating may occur.
Violation of attention and decreased reaction due to chronic sleep deprivation can provoke an accident
Treatment
Not every phobia needs treatment, but they should be taken seriously. If you do not pay due attention to your unreasonable obsessive fears, they can limit your life, up to the development of extreme anxiety and deep depression.
If you do not pay due attention to your unreasonable obsessive fears, they can limit your life, up to the development of extreme anxiety and deep depression.
It is especially important to get rid of a phobia if it leads to a lack of sleep. Sleep is vital for brain health, heart function, weight control, and lack of it can seriously affect your well-being. If you manage to take the right steps to overcome somniphobia and improve your sleep, this will ultimately lead to better overall health.
Mild somniphobia can be started with home treatments.
Improve your sleep hygiene
Your sleep problems may be due to poor sleep hygiene. Improve it by following simple rules:
- Always keep a schedule - go to bed at the same time. This will help your "internal clock" run smoothly and make it easier to fall asleep.
- Do not drink coffee before bed.
- Try to make your bedroom as comfortable and associated with sleep as possible. Remove all irritants from it - TV, computer, smartphone, other sources of noise, light, entertainment.
 Curtain the window with blackout curtains, change the uncomfortable bed and bedding. Adjust the air temperature - you should not be cold or hot.
Curtain the window with blackout curtains, change the uncomfortable bed and bedding. Adjust the air temperature - you should not be cold or hot. - Try calming yourself before bed with a ritual such as drinking herbal tea, reading a book, or taking a bath.
Regular drinking of herbal tea before bed can help get rid of fear of sleep
Unfortunately, improving sleep hygiene alone is unlikely to cure somniphobia.
Avoid "treatment" with alcohol or drugs
Experts advise against overcoming the fear of falling asleep and sleeping with alcohol and drugs. Their effect is very short-lived, incomplete and incorrect. As a result, you will shave a bad habit, the problem will not go away, and your health will be undermined.
Keep a diary
Write down your dreams and feelings during sleep, as well as thoughts, feelings, and other factors that increase or decrease anxiety in a diary. This will help you find the sources of your fear and how to deal with them.
Write down your feelings before bed and during sleep in a diary - this will help to cope with a phobia
You are not alone
You may be ashamed of your phobia, feel like an outcast. It is important to remember that you are not alone. First, there are other people who, just like you, struggle with the fear of sleep. Second, a trusted friend or family member can be a great source of support if you tell them about your condition.
The support of a loved one can help reduce the fear of sleep
Use relaxation techniques
Deep breathing, muscle relaxation, or guided imagery can help relieve anxiety before bed.
- If you've tried to manage your sleep anxiety on your own and haven't gotten better, it may be time to seek professional help from your doctor. He will conduct the necessary diagnostics and determine how best to solve your problem.
Is there a cure for somniphobia?
There are no specific drugs for the treatment of phobias, but some drugs can reduce anxiety and improve sleep. As a rule, medication in the treatment of fear of sleep is combined with various psychotherapeutic methods.
As a rule, medication in the treatment of fear of sleep is combined with various psychotherapeutic methods.
Psychotherapeutic methods of dealing with fear of sleep
Exposure therapy . The principle “look into the eyes of your fear” is used - in a controlled environment, a situation is simulated that causes an attack of hypnophobia. The duration of this situation (exposure) is determined individually and can range from 40 to 90 minutes. The result of such long-term immersion in your fear under the supervision of a psychotherapist while working on reducing the level of anxiety is a gradual getting rid of the fear of sleep.
In the treatment of somniphobia, psychotherapeutic methods are used
Cognitive Behavioral Therapy (CBT) . This psychotherapeutic technique focuses on changing the relationship between your thoughts, feelings and behavior. Numerous studies show that, through the use of cognitive rewiring techniques (identifying unwanted thoughts, eliminating them, and generating beneficial ones) and changing behavior, CBT is effective in helping people reduce anxiety, fear, and panic. Although cognitive behavioral therapy is not a first-line treatment for specific phobias, it can be a safe and effective option for adults or children struggling with somniphobia.
Although cognitive behavioral therapy is not a first-line treatment for specific phobias, it can be a safe and effective option for adults or children struggling with somniphobia.
Frequently asked questions
What causes somniphobia?
Like all other specific phobias, somniphobia is caused either by a genetic predisposition or by a traumatic “triggering” event.
Are sleep phobias related to insomnia?
Yes, these two phenomena are connected. Fear of sleep can lead to insomnia.
What causes untreated somniphobia and its consequence - lack of sleep?
Prolonged lack of sleep can lead to serious health problems, including increased risk of:
- depression;
- diabetes;
- heart attack;
- hypertension;
- obesity;
- stroke.
Why am I afraid to sleep alone?
Perhaps this is due to the nightmares that haunt you at night. Or you may feel fear if you used to sleep with a partner, and now you have to sleep alone. Similar problems occur in people who are forced to fall asleep in a new place - the so-called "first night effect", when one half of the brain is resting, while the other "remains alert."
Or you may feel fear if you used to sleep with a partner, and now you have to sleep alone. Similar problems occur in people who are forced to fall asleep in a new place - the so-called "first night effect", when one half of the brain is resting, while the other "remains alert."
Do children have somniphobia and what can be done about it?
Children, like adults, may experience sleep anxiety, such as fear of the dark or imaginary monsters. Take action - make your child feel safe and secure:
- do not allow him to watch scary TV shows, cartoons and movies;
- read good bedtime stories to your baby;
- put a night light in the nursery with a soft, dim light or slightly open the door of the room to the illuminated corridor;
- Allow your child to sleep with something comfortable, soothing, such as a favorite soft toy.
If the problem persists, contact a child psychologist or psychotherapist.
Insomnia is not terrible - the fear of it is dangerous | Kovrov G.
 V., Posokhov S.I.
V., Posokhov S.I. Sleep disturbance is one of the most common and important problems of modern medicine. Sleep dissatisfaction occurs in 45% of the population. Poor sleep is the cause of a poor quality of life; many diseases develop during sleep, and disturbed sleep modifies their course. It is these facts that make it more efficient to develop sleep medicine. The most striking manifestation of sleep disorders is insomnia [1]. Insomnia is defined as a problem of falling asleep, maintaining sleep, with nocturnal or early awakenings, combined with feelings of lack of recovery after sleep, with a violation of the functional state of a person during the daytime (increased drowsiness, decreased performance, attention and memory, etc.).
The close relationship between poor sleep and the somatic state of the body today is beyond doubt. Previously, it was shown [2] that a high (up to 73.7%) prevalence of sleep disorders was found in patients undergoing inpatient treatment in the city clinical hospital. Sleep disorders in patients with various diseases are also combined with depressive syndrome [3] and autonomic disorders, and more severe sleep disorders are observed in patients of older age groups. Currently, much attention is paid to the diagnosis of sleep disorders in cardiovascular pathology, endocrine diseases, pain syndrome and other neurological and somatic disorders.
Sleep disorders in patients with various diseases are also combined with depressive syndrome [3] and autonomic disorders, and more severe sleep disorders are observed in patients of older age groups. Currently, much attention is paid to the diagnosis of sleep disorders in cardiovascular pathology, endocrine diseases, pain syndrome and other neurological and somatic disorders.
Despite the fact that the principles of diagnosis and treatment of insomnia are described in detail in the literature, in outpatient and inpatient practice, the doctor faces several problems in diagnosing and prescribing treatment.
The main problem is the identification of hidden sleep disorders, which usually occur against the background of somatic and neuropsychiatric diseases [4]. In a situation where the patient actively complains about poor sleep, there are no diagnostic problems. But what to do with those patients who believe that poor sleep is associated with poor health, and sees no point in reporting this to the doctor. But dissatisfaction with the quality of sleep in patients who do not complain about sleep may not differ from that of those who complain [4]. Undoubtedly, the task of the physician is to actively identify symptoms of poor sleep efficiency in such patients. High activity of complaints about poor sleep quality in patients may indicate that dysfunctional beliefs about their sleep have been formed or are being formed, which, from the point of view of psychologists, have a negative impact on treatment [5, 6]. Patients are generally convinced that all their psychological and somatic problems are due to poor sleep. This causes an increase in the level of anxiety, the development of fear of bed and the night in general. This is where patients' fear of insomnia does more harm than insomnia itself, leading to "bed anxiety." This is a very difficult category of patients.
But dissatisfaction with the quality of sleep in patients who do not complain about sleep may not differ from that of those who complain [4]. Undoubtedly, the task of the physician is to actively identify symptoms of poor sleep efficiency in such patients. High activity of complaints about poor sleep quality in patients may indicate that dysfunctional beliefs about their sleep have been formed or are being formed, which, from the point of view of psychologists, have a negative impact on treatment [5, 6]. Patients are generally convinced that all their psychological and somatic problems are due to poor sleep. This causes an increase in the level of anxiety, the development of fear of bed and the night in general. This is where patients' fear of insomnia does more harm than insomnia itself, leading to "bed anxiety." This is a very difficult category of patients.
And others believe that their poor sleep is not so bad as to complain. Thus, patients protect themselves from the appearance of negative thoughts, calming themselves at the same time, without giving any information to the doctors. This is especially important when a general practitioner is treating, for example, arterial hypertension, and the absence of active complaints about poor sleep leads to ignoring the issue of sleep correction. It is still necessary to improve the quality of sleep if there are at least some manifestations of his disorder. The literature describes cases of improvement in the course of the underlying disease with the correction of insomnia. In particular, it is known that the use of hypnotics (zopiclone, melatonin) leads to a decrease in blood pressure against the background of improved sleep [3, 7, 8].
This is especially important when a general practitioner is treating, for example, arterial hypertension, and the absence of active complaints about poor sleep leads to ignoring the issue of sleep correction. It is still necessary to improve the quality of sleep if there are at least some manifestations of his disorder. The literature describes cases of improvement in the course of the underlying disease with the correction of insomnia. In particular, it is known that the use of hypnotics (zopiclone, melatonin) leads to a decrease in blood pressure against the background of improved sleep [3, 7, 8].
So, if there is minimal suspicion of poor sleep quality in patients with any disease, it is necessary to clarify the nature of the violations and take measures to improve sleep, even if not all causes of insomnia are immediately clear.
To clarify the causes of insomnia, it is first of all important to assess the patient's psychological state (levels of anxiety, depression, dysfunctional beliefs). Such diagnostics makes it possible not only to choose the appropriate treatment, but also to predict the effectiveness of curation. How many times have we met with patients who come to the doctor with ready-made attitudes and “recipes” for how they should be treated? Ready-made "recipes from patients" are sometimes useful, because they allow you to take into account the positive or negative experience of previous treatment, and sometimes they interfere greatly, especially when patients insist on their concepts and do not want to listen to the doctor.
Such diagnostics makes it possible not only to choose the appropriate treatment, but also to predict the effectiveness of curation. How many times have we met with patients who come to the doctor with ready-made attitudes and “recipes” for how they should be treated? Ready-made "recipes from patients" are sometimes useful, because they allow you to take into account the positive or negative experience of previous treatment, and sometimes they interfere greatly, especially when patients insist on their concepts and do not want to listen to the doctor.
The appointment of polysomnography performed in sleep centers, in particular, when making a diagnosis of insomnia, does not make sense at all, since the diagnosis of "insomnia" is a clinical concept. But in case of differential diagnosis with other forms of sleep disorders, clinically unclear causes of sleep disorders, long course and poor curability, the question of objectifying sleep disorders by polysomnography should be raised [9].
In the treatment of insomnia, regardless of the causes that caused it, the method of cognitive behavioral therapy is the most promising today [6, 10]. Of course, full-fledged psychotherapeutic assistance is difficult to implement. However, in outpatient practice at the reception, a number of simple but effective rules can be proposed:
1. Go to bed later. This recommendation is due to the fact that patients with insomnia, due to fear of not falling asleep, try to go to bed early, sometimes even at 21.00, in order to get ready for bed and fall asleep at 23–24.00, which violates the principles of sleep hygiene and leads to an increase in the time spent in bed.
2. Wake up earlier (waking up late is associated with patients' desire for sleep, but is also harmful, although early rise may be associated with increased anxiety in patients).
3. Do not go to bed and do not sleep during the day.
It is important to note that the high therapeutic effect of these simple recommendations will be significant only if they are regularly followed for a long time. And not always, unfortunately, there is compliance or mutual understanding between the doctor and the patient, in the absence of which the effectiveness of the above methods can be significantly reduced [10].
And not always, unfortunately, there is compliance or mutual understanding between the doctor and the patient, in the absence of which the effectiveness of the above methods can be significantly reduced [10].
When starting to prescribe drugs to correct sleep disorders, the doctor is faced with two extremes: either the patient has never taken sleeping pills, despite the chronic course of insomnia, or he has tried everything that is produced by pharmaceutical companies.
In the first case, treatment should begin with the safest preparations, in particular, with herbal remedies containing sedatives (valerian, motherwort, mint, esholcia, etc.). It is necessary to use phytotherapeutic preparations during the day in the morning and for a long time. It is very important to explain to the patient that drugs with a calming effect, although they are used to improve sleep, it is advisable to take them not only at night, but also during the daytime to relieve increased excitability and reduce anxiety.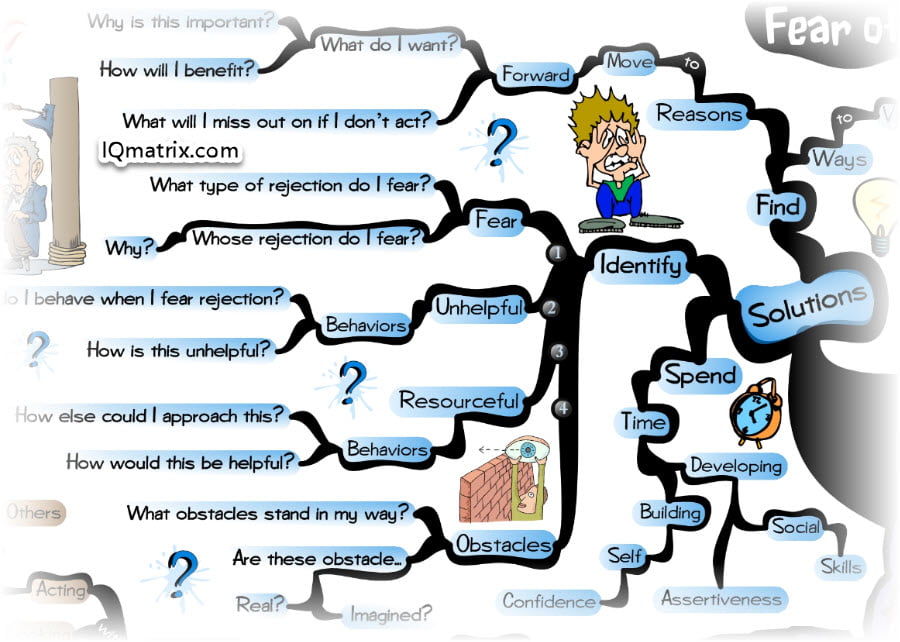 At the age of over 55, melatonin is widely used for the treatment of insomnia [11]. Its safety and effectiveness have been shown in various studies. Recent studies have demonstrated its greatest effectiveness in patients with a low level of anxiety - both in patients with concomitant somatic pathology (hypertension, gastric ulcer, etc.), and without any diseases.
At the age of over 55, melatonin is widely used for the treatment of insomnia [11]. Its safety and effectiveness have been shown in various studies. Recent studies have demonstrated its greatest effectiveness in patients with a low level of anxiety - both in patients with concomitant somatic pathology (hypertension, gastric ulcer, etc.), and without any diseases.
Prescribing other sleeping pills may have a number of limitations due to possible side effects. But their high efficiency in relation to "sleep" psychologically is undoubtedly higher. This can sometimes be important for a patient who, while taking sleeping pills, seems to him to have a real dream. All these drugs cannot be prescribed for a long time, but sometimes it is important to get a short-term effect in order to gain time to clarify the features of insomnia, while the patient does not develop fear of bed (one of the important and unpleasant symptoms of insomnia).
Known sleeping pills in most cases are GABA-ergic drugs that affect the course of slow sleep and reduce nocturnal awakenings. Unfortunately, there is not enough information in the literature to predict the effect of a hypnotic drug on the sleep-wake cycle, depending on the individual characteristics of the organism or the presence of a concomitant disease. This significantly complicates the problem of choosing a drug, and doctors have to rely only on their experience in this matter.
Unfortunately, there is not enough information in the literature to predict the effect of a hypnotic drug on the sleep-wake cycle, depending on the individual characteristics of the organism or the presence of a concomitant disease. This significantly complicates the problem of choosing a drug, and doctors have to rely only on their experience in this matter.
But among all sleeping pills there is a drug that is fundamentally different in its mechanism of action - Donormil [12, 13]. Being a blocker of histamine receptors, it does not activate the sleep system, but depresses the wakefulness system. This fundamental difference from most hypnotic drugs allows Donormil to be more widely used in the correction of insomnia both as monotherapy and in combination with other hypnotic drugs (the mechanism of the hypnotic effect of which does not intersect) to cancel or replace an ineffective drug. This makes it a versatile sleep aid of its kind. Of course, Donormil also has a number of disadvantages due to the presence of contraindications and rarely insufficient effectiveness.
In the event that a physician is faced with difficult-to-treat patients who have "tried everything", it is extremely important to determine the presence or absence of serious mental disorders. In practice, however, it turns out that such patients either were treated by psychiatrists (who, according to the patients, did not help or helped partially), or do not want to go to psychiatrists even for a consultation. In this difficult situation, it is still necessary to try to refer such patients to psychiatrists. Treating "insomnia" on your own can become a heavy burden. And if you can still work with patients who have a schizoid mentality, then with patients who have severe depression, the treatment of "insomnia" even with the help of antidepressants can be simply dangerous because of the risk of suicide.
Thus, it is possible to introduce the principle of sleep medicine "healthy sleep - a healthy body" into general medical practice only using the basics of sleep hygiene and other approaches of cognitive-behavioral psychotherapy.