How to deal with pms depression
Premenstrual syndrome (PMS) - Diagnosis and treatment
Diagnosis
There are no unique physical findings or lab tests to positively diagnose premenstrual syndrome. Your doctor may attribute a particular symptom to PMS if it's part of your predictable premenstrual pattern.
To help establish a premenstrual pattern, your doctor may have you record your signs and symptoms on a calendar or in a diary for at least two menstrual cycles. Note the day that you first notice PMS symptoms, as well as the day they disappear. Also be sure to mark the days your period starts and ends.
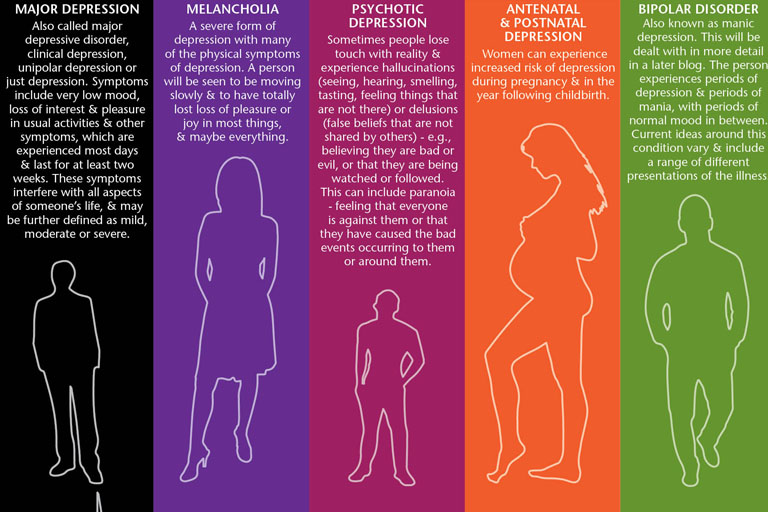
Certain conditions may mimic PMS, including chronic fatigue syndrome, thyroid disorders and mood disorders, such as depression and anxiety. Your health care provider may order tests, such as a thyroid function test or mood screening tests to help provide a clear diagnosis.
Treatment
For many women, lifestyle changes can help relieve PMS symptoms. But depending on the severity of your symptoms, your doctor may prescribe one or more medications for premenstrual syndrome.
The success of medications in relieving symptoms varies among women. Commonly prescribed medications for premenstrual syndrome include:
- Antidepressants. Selective serotonin reuptake inhibitors (SSRIs) — which include fluoxetine (Prozac), paroxetine (Paxil, Pexeva), sertraline (Zoloft) and others — have been successful in reducing mood symptoms. SSRIs are the first line treatment for severe PMS or PMDD. These medications are generally taken daily. But for some women with PMS, use of antidepressants may be limited to the two weeks before menstruation begins.
- Nonsteroidal anti-inflammatory drugs (NSAIDs). Taken before or at the onset of your period, NSAIDs such as ibuprofen (Advil, Motrin IB, others) or naproxen sodium (Aleve) can ease cramping and breast discomfort.
- Diuretics. When exercise and limiting salt intake aren't enough to reduce the weight gain, swelling and bloating of PMS, taking water pills (diuretics) can help your body shed excess fluid through your kidneys. Spironolactone (Aldactone) is a diuretic that can help ease some of the symptoms of PMS.
- Hormonal contraceptives. These prescription medications stop ovulation, which may bring relief from PMS symptoms.
More Information
- Combination birth control pills
- Minipill (progestin-only birth control pill)
Request an Appointment at Mayo Clinic
Lifestyle and home remedies
You can sometimes manage or reduce the symptoms of premenstrual syndrome by making changes in the way you eat, exercise and approach daily life. Try these tips:
Try these tips:
Modify your diet
- Eat smaller, more-frequent meals to reduce bloating and the sensation of fullness.
- Limit salt and salty foods to reduce bloating and fluid retention.
- Choose foods high in complex carbohydrates, such as fruits, vegetables and whole grains.
- Choose foods rich in calcium. If you can't tolerate dairy products or aren't getting adequate calcium in your diet, a daily calcium supplement may help.
- Avoid caffeine and alcohol.
Incorporate exercise into your regular routine
Engage in at least 30 minutes of brisk walking, cycling, swimming or other aerobic activity most days of the week. Regular daily exercise can help improve your overall health and alleviate certain symptoms, such as fatigue and a depressed mood.
Reduce stress
- Get plenty of sleep.
- Practice progressive muscle relaxation or deep-breathing exercises to help reduce headaches, anxiety or trouble sleeping (insomnia).
- Try yoga or massage to relax and relieve stress.
Record your symptoms for a few months
Keep a record to identify the triggers and timing of your symptoms. This will allow you to intervene with strategies that may help to lessen them.
Alternative medicine
Here's what's known about the effectiveness of complementary remedies used to soothe the symptoms of premenstrual syndrome:
- Vitamin supplements. Calcium, magnesium, vitamin E and vitamin B-6 have all been reported to soothe symptoms, but evidence is limited or lacking.
-
Herbal remedies. Some women report relief of PMS symptoms with the use of herbs, such as ginkgo, ginger, chasteberry (Vitex agnus), evening primrose oil and St. John's wort. However, few scientific studies have found that any herbs are effective for relief of PMS symptoms.
Herbal remedies also aren't regulated by the Food and Drug Administration, so there's no record of product safety or effectiveness.
 Talk with your doctor before taking any herbal products, as they may have side effects or interact with other medications you're taking. St. John's wort, for example, reduces the effectiveness of birth control pills.
Talk with your doctor before taking any herbal products, as they may have side effects or interact with other medications you're taking. St. John's wort, for example, reduces the effectiveness of birth control pills. - Acupuncture. A practitioner of acupuncture inserts sterilized stainless steel needles into the skin at specific points on the body. Some women experience symptom relief after acupuncture treatment.
Preparing for your appointment
You're likely to start by seeing your family doctor or primary care provider. However, in some cases when you call to set up an appointment, you may be referred to a doctor who specializes in conditions affecting the female reproductive tract (gynecologist).
Here's some information to help you prepare for your appointment and what to expect from your doctor.
What you can do
- Be aware of any pre-appointment restrictions. At the time you make the appointment, ask if there's anything you need to do in advance to prepare.

- Write down symptoms you're experiencing, including any that may seem unrelated to the reason for which you scheduled the appointment.
- Make a list of your key medical information, including any other conditions for which you're being treated and the names of any medications, vitamins or supplements you're taking.
- Consider questions to ask your doctor and write them down. Bring along notepaper and a pen to jot down information as your doctor addresses your questions.
For premenstrual syndrome, some basic questions to ask your doctor include:
- Is there anything I can do to minimize PMS symptoms?
- Will my PMS symptoms eventually go away on their own?
- Could the symptoms that I'm experiencing indicate a more serious medical condition?
- Do you recommend treatment for PMS symptoms? What treatments are available?
- Is there a generic alternative to the medicine you're prescribing?
- Do you have any brochures or other printed material that I can take with me? What websites do you recommend?
Don't hesitate to ask any other questions that occur to you during your appointment.
What to expect from your doctor
Your doctor is likely to ask you a number of questions, such as:
- How severe are your symptoms?
- On what days during your menstrual cycle are your symptoms at their worst?
- Do you have symptom-free days during your menstrual cycle?
- Can you anticipate when your symptoms are coming on?
- Does anything seem to make your symptoms better or worse?
- Do your symptoms interfere with your daily activities?
- Have you recently felt down, depressed or hopeless?
- Have you or has anyone in your family been diagnosed with a psychiatric disorder?
- What treatments have you tried so far? How have they worked?
By Mayo Clinic Staff
Related
Associated Procedures
Products & Services
Why It Happens, Treatments, and Finding Support
We include products we think are useful for our readers. If you buy through links on this page, we may earn a small commission.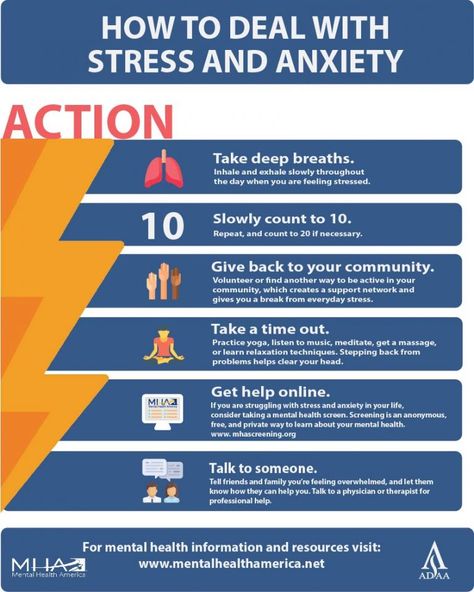 Here’s our process.
Here’s our process.
Healthline only shows you brands and products that we stand behind.
Our team thoroughly researches and evaluates the recommendations we make on our site. To establish that the product manufacturers addressed safety and efficacy standards, we:
- Evaluate ingredients and composition: Do they have the potential to cause harm?
- Fact-check all health claims: Do they align with the current body of scientific evidence?
- Assess the brand: Does it operate with integrity and adhere to industry best practices?
We do the research so you can find trusted products for your health and wellness.
Read more about our vetting process.Is it PMS?
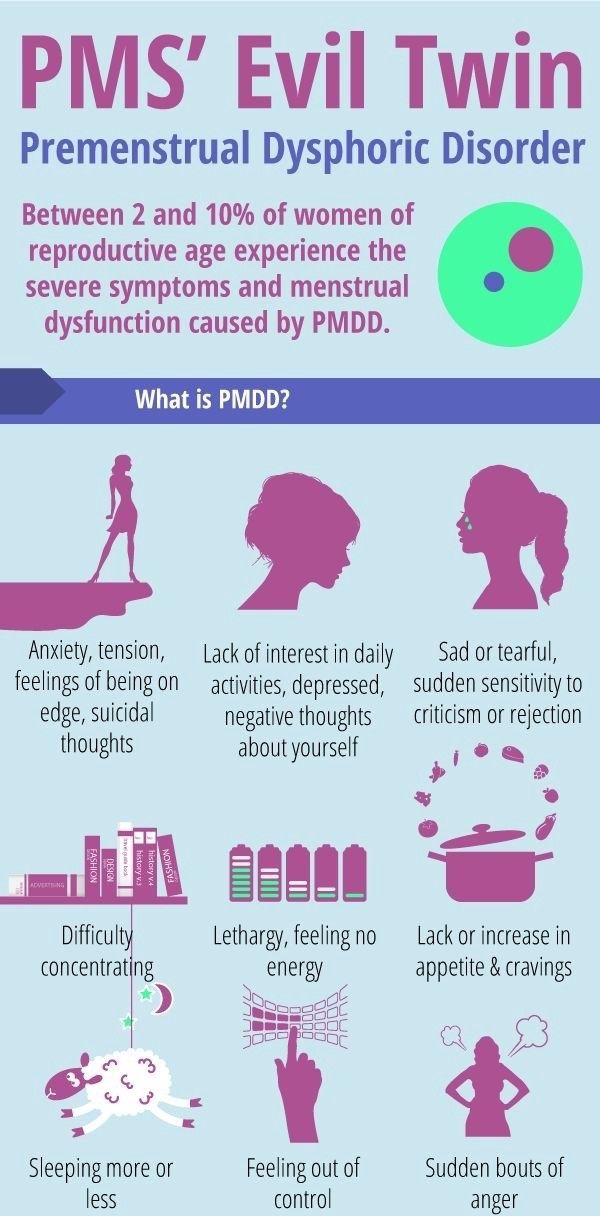
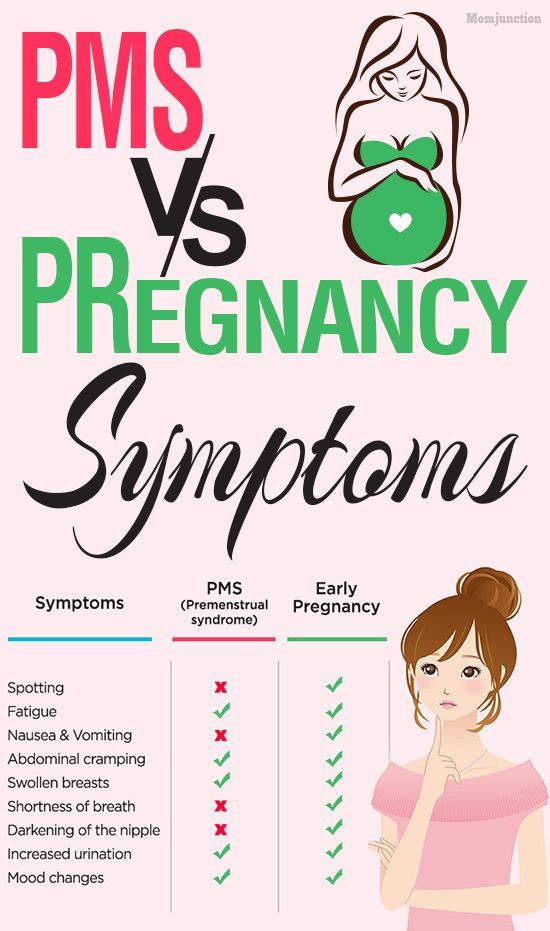
Premenstrual syndrome (PMS) is a collection of physical and emotional symptoms that start a week or so before your period. It makes some people feel more emotional than usual and others bloated and achy.
PMS can also make people feel depressed in the weeks leading up to their period. This may make you feel:
- sad
- irritable
- anxious
- tired
- angry
- teary
- forgetful
- absentminded
- uninterested in sex
- like sleeping too much or too little
- like eating too much or too little
Other reasons you might feel depressed before your period include:
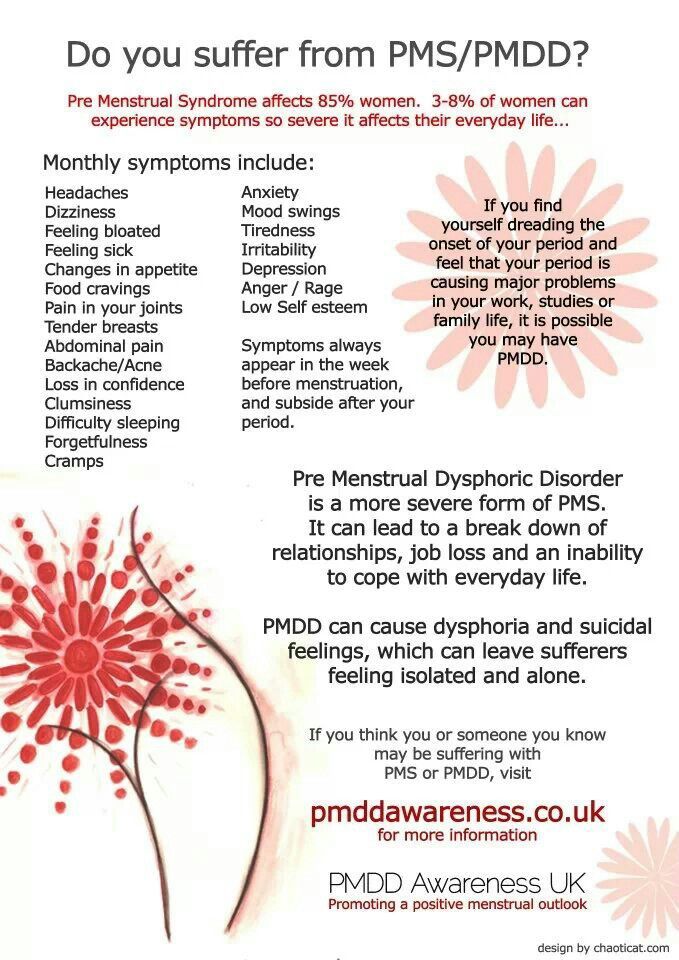
- Premenstrual dysphoric disorder (PMDD). PMDD is very similar to PMS, but its symptoms are more severe. Many people with PMDD report feeling very depressed before their period, some to the point of thinking about suicide. While recent research estimates about 75 percent of women have PMS during their reproductive years, only 3 to 8 percent have PMDD.
- Premenstrual exacerbation. This refers to when symptoms of an existing condition, including depression, become worse in the weeks or days leading up to your period.
 Depression is one of the most common conditions that coexists with PMS. About half of all women who get treated for PMS also have either depression or anxiety.
Depression is one of the most common conditions that coexists with PMS. About half of all women who get treated for PMS also have either depression or anxiety.
Read on to learn more about the connection between PMS and depression.
Experts aren’t sure about the exact cause of PMS, but it’s likely linked to hormonal fluctuations that happen during the second half of the menstrual cycle.
Ovulation happens about halfway through your cycle. During this time, your body releases an egg, causing estrogen and progesterone levels to drop. A shift in these hormones can cause both physical and emotional symptoms.
Changes in estrogen and progesterone levels also influence serotonin levels. This is a neurotransmitter that helps regulate your mood, sleep cycle, and appetite. Low levels of serotonin are linked to feelings of sadness and irritability, in addition to trouble sleeping and unusual food cravings — all common PMS symptoms.
Your symptoms should improve when estrogen and progesterone levels rise again.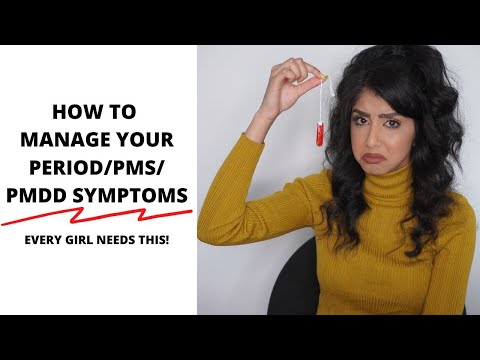 This usually happens a few days after you get your period.
This usually happens a few days after you get your period.
There’s no standard treatment for depression during PMS. But several lifestyle changes and a few medications may help relieve your emotional symptoms.
Track your symptoms
If you don’t already, start keeping track of your menstrual cycle and your emotions throughout its different stages. This will help you confirm that your depression symptoms are indeed linked to your cycle. Knowing that there’s a reason you’re feeling down can also help keep things in perspective and offer some validation.
Having a detailed log of your last few cycles is also handy if you want to bring up your symptoms with your doctor. There’s still some stigma around PMS, and having documentation of your symptoms might help you feel more confident about bringing them up. It can also help your doctor get a better idea of what’s going on.
You can track your cycle and symptoms using period-tracking app on your phone. Look for one that allows you to add your own symptoms.
You can also print out a chart or make your own. Across the top, write the day of the month (1 through 31). List your symptoms down the left side of the page. Put an X in the box next to the symptoms you experience each day. Note whether each symptom is mild, moderate, or severe.
To track depression, make sure to note when you experience any of these symptoms:
- sadness
- anxiety
- crying spells
- irritability
- food cravings or appetite loss
- poor sleep or too much sleep
- trouble concentrating
- lack of interest in your daily activities
- tiredness, lack of energy
Hormonal birth control
Hormonal birth control methods, such as the pill or patch, can help with bloating, tender breasts, and other physical PMS symptoms. For some people, they can also help with emotional symptoms, including depression.
But for others, hormonal birth control can make depression symptoms worse. If you go this route, you might have to try out different types of birth control before you find a method that works for you. If you’re interested in the pill, opt for a continuous one that doesn’t have a week of placebo pills. Continuous birth control pills can eliminate your period, which sometimes helps eliminate PMS, too.
If you’re interested in the pill, opt for a continuous one that doesn’t have a week of placebo pills. Continuous birth control pills can eliminate your period, which sometimes helps eliminate PMS, too.
Natural remedies
A couple of vitamins may help relieve PMS-related symptoms of depression.
A clinical trial found that a calcium supplement helped with PMS-related depression, appetite changes, and tiredness.
Many foods are good sources of calcium, including:
- milk
- yogurt
- cheese
- leafy green vegetables
- fortified orange juice and cereal
You can also take a daily supplement containing 1,200 milligrams of calcium, which you can find on Amazon.
Don’t be discouraged if you don’t see results right away. It can take about three menstrual cycles to see any symptom improvement while taking calcium.
Vitamin B-6 might also help with PMS symptoms.
You can find it in the following foods:
- fish
- chicken and turkey
- fruit
- fortified cereals
Vitamin B-6 also comes in supplement form, which you can find on Amazon. Just don’t take more than 100 milligrams a day.
Just don’t take more than 100 milligrams a day.
Learn about other supplements that can help with PMS symptoms.
Lifestyle changes
Several lifestyle factors also seem to play a role in PMS symptoms:
- Exercise. Try to be active for at least 30 minutes more days of the week than not. Even a daily walk through your neighborhood can improve symptoms of depression, fatigue, and trouble concentrating.
- Nutrition. Try to resist the junk food cravings that can come with PMS. Large amounts of sugar, fat, and salt can all wreak havoc on your mood. You don’t have to cut them out completely, but try to balance out these foods with fruits, vegetables, and whole grains. This will help keep you full throughout the day.
- Sleep. Not getting enough sleep can kill your mood if you’re weeks away from your period. Try to get at least seven to eight hours of sleep a night, especially in the week or two leading up to your period.
 See how not getting enough sleep affects your mind and body.
See how not getting enough sleep affects your mind and body. - Stress. Unmanaged stress can worsen depression symptoms. Use deep breathing exercises, meditation, or yoga to calm both your mind and body, especially when you feel PMS symptoms coming on.
Medication
If other treatment options aren’t helping, taking an antidepressant may help. Selective serotonin reuptake inhibitors (SSRIs) are the most common type of antidepressant used to treat PMS-related depression.
SSRIs block the absorption of serotonin, which increases the amount of serotonin in your brain. Examples of SSRIs include:
- citalopram (Celexa)
- fluoxetine (Prozac and Sarafem)
- paroxetine (Paxil)
- sertraline (Zoloft)
Other antidepressants that work on serotonin might also help treat PMS depression. These include:
- duloxetine (Cymbalta)
- venlafaxine (Effexor)
Work with your doctor to come up with a dosage plan. They might suggest you only take an antidepressant during the two weeks before your symptoms tend to start. In other cases, they might recommend taking them every day.
They might suggest you only take an antidepressant during the two weeks before your symptoms tend to start. In other cases, they might recommend taking them every day.
Your gynecologist might be the first person you turn to for help when PMS depression becomes overwhelming. It’s important that your doctor is someone you trust and who takes your symptoms seriously. If your doctor doesn’t listen to you, search for another provider.
You can also turn to the International Association for Premenstrual Disorders. It offers blogs, online communities, and local resources that can help you find a doctor familiar with PMS and PMDD.
If you or someone you know is having suicidal thoughts — related to PMS depression or not — get help from a crisis or suicide prevention hotline. Try the National Suicide Prevention Lifeline at 800-273-8255.
If you think someone is at immediate risk of self-harm or hurting another person:
- Call 911 or your local emergency number.
- Stay with the person until help arrives.
- Remove any guns, knives, medications, or other things that may cause harm.
- Listen, but don’t judge, argue, threaten, or yell.
Psychological problems and PMS. How to understand what is the difference?
Mood swings are one of the common symptoms attributed to PMS.
PMS itself is poorly understood and is largely attributed to all women in general, and this is one of the stereotypes that needs to be combated, because it attributes negative emotions to female biology, while in fact, far from all women and far from each cycle experience the psychological symptoms of PMS. nine0005
What's more, research suggests that, on average, men and women are equally affected by the same mood swings.
How exactly do hormones affect mental health?
There is no exact answer to this question, but, apparently, the cyclical monthly work of the ovaries plays a key role, producing different amounts of the hormones estradiol and progesterone in each part of the cycle, which, in turn, can affect neurotransmitters, that is, how signals travel through our brains. nine0005
nine0005
Rapidly changing levels of these hormones can affect mood not only before and during menstruation, but also after childbirth and before menopause, leading to a cascade of reactions in the body that cause such hormone-dependent depressive states in predisposed people.
How to distinguish PMS from other psychological problems?
It is important to remember that the stereotypes that surround PMS are similar to those that surround people who have experienced mental health problems, and this stigma needs to be addressed. nine0005
From a psychological point of view, it is important to distinguish whether the symptoms are caused specifically by hormonal changes characteristic of PMS or by some other pre-existing mental state. Both women with and without mental health problems can suffer from PMS. Many women are simply afraid to talk about their mood swings and depression just because they believe that they will simply be written off as PMS and supposedly inevitable female biology, they will be called weak and simply devalued.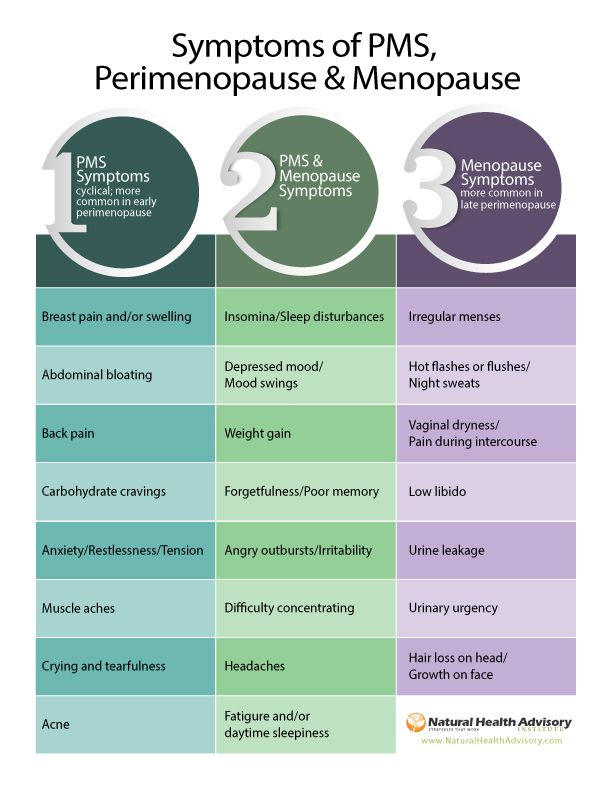 nine0005
nine0005
In rare cases, mood swings and depression can be so severe that they can develop into a serious problem and have a very negative impact on a woman's psychological well-being, which is why it is important to know and be able to recognize the signs that you need qualified help.
PMS and PMDD and their impact on the psychological well-being of women
A severe affective disorder with severe psychological symptoms of PMS is called premenstrual dysphoric disorder. About 3-5% of women suffer from it. PMDD can cause extreme mood swings and intense feelings of hopelessness, deep sadness and depression, and anxiety so severe that it interferes with women's daily lives. nine0005
If you're not sure if your symptoms are normal, you can ask other women how they feel during PMS and compare their answers with your own and analyze the differences.
Remember that PMDD is not fiction, but a condition that must be taken seriously and requires medical attention because it interferes with normal life.

How to deal with PMS and its psychological aspects? nine0014
It is important to be able to recognize and manage the psychological symptoms of PMS and the additional stress it can put on you.
-
Try to maintain physical mobility and lead an active lifestyle: when moving, endorphins are released, and even a short walk can improve your mood a little.
-
It may seem that a huge chocolate cake or an extra portion of fried potatoes will quickly improve your mood if things are really bad, but in fact it is not, especially if such food has a “forbidden fruit” flavor for you and you will scold yourself later for it . In any health condition, it is better to stick to a balanced diet and not to spread rot on yourself if something did not go as planned. nine0005
-
Try to find things that help you relax or calm down. It even makes sense to have a special list of activities and things that make you happy, so that if you are completely sad and at a loss, there is somewhere to look and do something good for yourself.
 Relaxation helps relieve stress and distract from intrusive thoughts, and the ability to properly rest and recover is one of the most important skills in taking care of yourself.
Relaxation helps relieve stress and distract from intrusive thoughts, and the ability to properly rest and recover is one of the most important skills in taking care of yourself.
How do you know if you need help?
Try to mark all symptoms on a special calendar or application to see if they are related to your cycle.
If you find that you regularly experience mood swings, anxiety and depression before and during your period, it is most likely related to PMS.
Take care of yourself, try to recognize such changes and remind yourself that this is a temporary phenomenon that can be dealt with. However, if you notice that this condition does not go away or becomes more intense, and you can not cope, then help is needed. nine0005
Remember that the more you know about what is happening to you, the easier it will be for you to cope with what is bothering you.
PMS and depression - HealthInfo
As you know, there are about 150 symptoms of premenstrual syndrome (PMS). It occurs due to a decrease in the content of the female hormone estrogen on the eve of the onset of "critical days". This unpleasant condition is familiar to approximately 80% of all women (and their families), but only approximately 10% suffer from it for real, often with severe symptoms of depression. nine0088
It occurs due to a decrease in the content of the female hormone estrogen on the eve of the onset of "critical days". This unpleasant condition is familiar to approximately 80% of all women (and their families), but only approximately 10% suffer from it for real, often with severe symptoms of depression. nine0088
Many women habitually associate nervousness, mood swings, depression, aggression with the menstrual cycle. But this relationship does not always exist. Can't changes in a woman's mood be related, for example, to weather conditions or occupation? How do you know when it's time to ask for help?
Depends on the weather…
“When we do research related to PMS, many women report that they generally feel somewhat better in spring and summer (closer to summer), and worse in winter,” says Jean Endicott, PhD, Professor of Clinical Psychology and Psychiatry at Columbia University. “That is, in itself, the connection between the mental state of a woman and the current season clearly exists, although there is no scientific justification for this.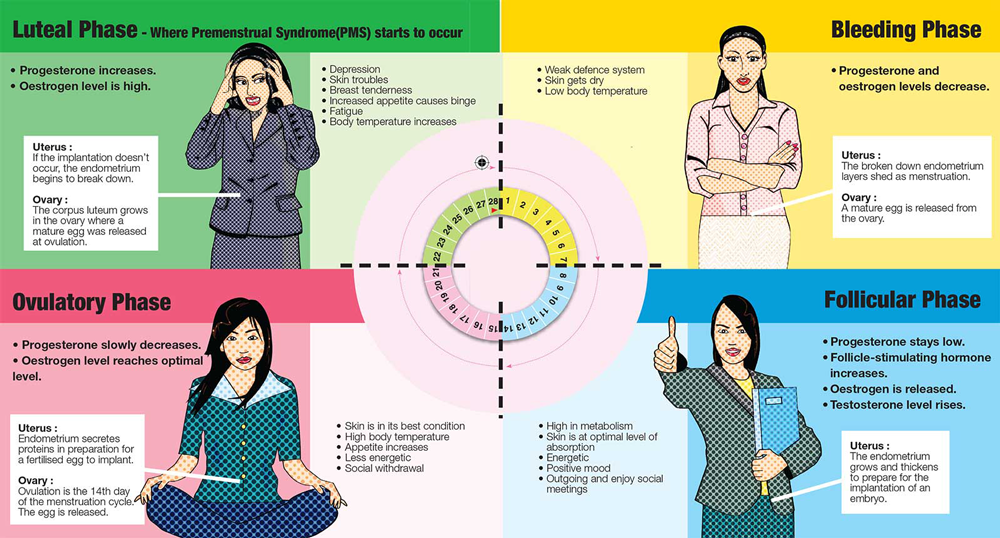 ” nine0005
” nine0005
This may be due to the fact that there are more sunny days in summer, or because this season women have more opportunities to be outdoors and are more physically active, and physical activity is known to be a good remedy for depression. In winter, there are fewer such opportunities. In addition, scientists believe that women who are dependent on seasonality may be partially dependent on circadian rhythms.
Circadian rhythms are biological cycles that repeat every 24 hours and include periods of wake and sleep, activity and rest, hunger and food intake, and fluctuations in hormone levels and body temperature. How strongly all these rhythms affect the condition of a woman, in all likelihood, depends on her individual characteristics. nine0005
PMS, depression… or is that the nature?
Nevertheless, one should not treat one's mood lightly, just as one should not raise a panic ahead of time. It is important to understand why irritability is replaced by tearfulness, and quiet "bright" sadness suddenly turns into "black longing".
If you are prone to mood swings or feel overwhelmed, try keeping a diary for three months in which you record absolutely every change in your mood every day. nine0005
Buy a calendar and chart daily mood swings: up and down, happy, sad, tired, euphoric, angry, irritable. But only this needs to be done every day, without waiting for the mood to deteriorate sharply or only when menstruation approaches.
Time to see a doctor?
If your diary shows that depression is indeed related to your monthly cycle, how do you know if you should seek medical help? Try to answer questions:
- Are you not just irritable at this time, but do you get into conflicts on any occasion with family members and make scandals for them?
- Are you unable to work productively and enjoy family life at this time?
- Do you have difficulty performing your daily functions, change your eating habits or lose your appetite, sleep poorly?
- Do you experience severe anxiety or bouts of self-criticism?
- Do you have thoughts of death or suicide? nine0058
If you answered yes to several of these questions (especially the last one), see your doctor. If your cycle symptoms are really starting to interfere with your work or personal life, it's time to seek professional help.
If your cycle symptoms are really starting to interfere with your work or personal life, it's time to seek professional help.
Combating PMS is a must
There are several options for dealing with depression associated with PMS, which one to choose - the doctor will advise. This, for example, can be a course of cognitive behavioral therapy or light therapy. It is possible that a course of antidepressants or other drugs will be prescribed (on a strictly individual basis). nine0005
Antidepressants
Antidepressants of the SSRI group (selective serotonin reuptake inhibitors) are sometimes prescribed in such cases. They elevate mood by increasing the brain's use of chemicals called serotonin, which are responsible for transmitting impulses between cells (neurotransmitters). SSRIs have become the most popular treatment for depression because they are proven to be highly effective and have fewer side effects. The intake of such drugs begins on the 14th day of the cycle and stops with the onset of menstrual bleeding.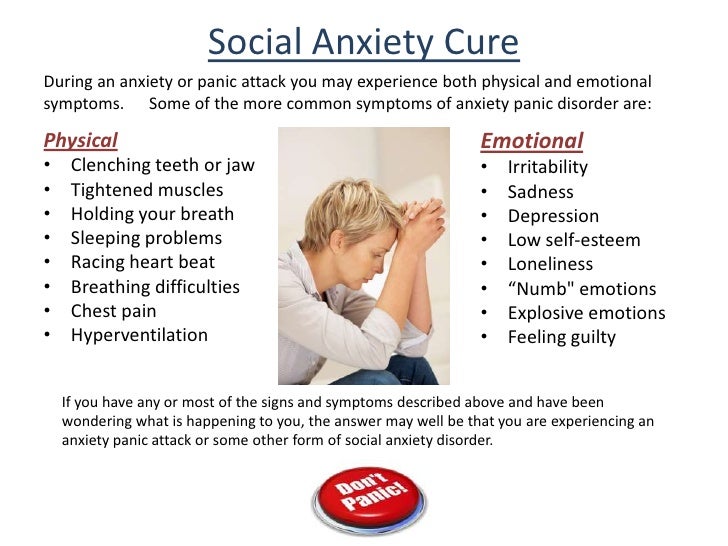 As a rule, several weeks pass before the onset of a lasting effect, but in women suffering from depressive conditions due to PMS, it occurs faster. Remember that only a doctor can give you medicine! nine0005
As a rule, several weeks pass before the onset of a lasting effect, but in women suffering from depressive conditions due to PMS, it occurs faster. Remember that only a doctor can give you medicine! nine0005
Cognitive behavioral therapy
Cognitive behavioral therapy can help develop skills to manage depression and change moods associated with the menstrual cycle. This method is based on ideas, according to which the feelings and behavior of a person are determined not by the situation in which the person finds himself, but by his perception of this situation. This technique can prompt a woman to sometimes very simple methods of correcting her lifestyle and behavior, for example, not to plan difficult work these days, or attend relaxing massage courses and not skip yoga classes. nine0005
It is useful to make a list of things to do and things in advance that are pleasant for you and will really help you to control yourself and cheer you up. Only the list needs to be drawn up in advance, because when the “moment” comes, you will have neither the desire nor the energy for this.