How long does luvox take to work
Fluvoxamine (Luvox) | NAMI: National Alliance on Mental Illness
Brand names:
- Luvox®
- Tablets (immediate release): 25 mg, 50 mg, 100 mg
- Luvox CR®
- Capsules (extended release): 100 mg, 150 mg
Generic name: fluvoxamine (floo VOKS a meen)
All FDA black box warnings are at the end of this fact sheet. Please review before taking this medication.
What Is Fluvoxamine And What Does It Treat?
Fluvoxamine is an antidepressant medication that works in the brain. It is approved for the treatment of obsessive compulsive disorder (OCD) in adults and children ages 8 and older.
Obsessive Compulsive Disorder (OCD) occurs when a person experiences the following symptoms at the same time:
- Obsessions (unwanted, recurrent, and disturbing thoughts)
- Compulsions (repetitive, ritualized behaviors that the person feels driven to perform in order to lessen the anxiety produced by the obsessions)
Fluvoxamine may also be helpful when prescribed “off-label” for major depressive disorder (MDD), social phobia (also known as social anxiety disorder), posttraumatic stress disorder (PTSD), panic disorder, and eating disorders including bulimia nervosa and binge-eating disorder. “Off-label” means that it hasn’t been approved by the Food and Drug Administration for this condition. Your mental health provider should justify his or her thinking in recommending an “off-label” treatment. They should be clear about the limits of the research around that medication and if there are any other options.
Symptoms of depression include:
- Depressed mood - feeling sad, empty, or tearful
- Feeling worthless, guilty, hopeless, and helpless
- Loss of interest or pleasure in your usual activities
- Sleep and eat more or less than usual (for most people it is less)
- Low energy, trouble concentrating, or thoughts of death (suicidal thinking)
- Psychomotor agitation (‘nervous energy’)
- Psychomotor retardation (feeling like you are moving and thinking in slow motion)
- Suicidal thoughts or behaviors
Social phobia (also known as social anxiety disorder) is a fear of situations where one may feel as if they are being judged by others. Symptoms include:
Symptoms include:
- Blushing
- Difficulty talking
- Nausea
- Sweating
- Shaking
What Is The Most Important Information I Should Know About Fluvoxamine?
Do not stop taking fluvoxamine, even when you feel better. With input from you, your health care provider will assess how long you will need to take the medicine.
Missing doses of fluvoxamine may increase your risk for relapse in your symptoms.
Stopping fluvoxamine abruptly may result in one or more of the following withdrawal symptoms: irritability, nausea, dizziness, vomiting, nightmares, headache, and/or paresthesias (prickling, tingling sensation on the skin).
Depression is also a part of bipolar illness. People with bipolar disorder who take antidepressants may be at risk for "switching" from depression into mania. Symptoms of mania include "high" or irritable mood, very high self-esteem, decreased need for sleep, pressure to keep talking, racing thoughts, being easily distracted, frequently involved in activities with a large risk for bad consequences (for example, excessive buying sprees).
Medical attention should be sought if serotonin syndrome is suspected. Please refer to serious side effects for signs/symptoms.
Are There Specific Concerns About Fluvoxamine And Pregnancy?
If you are planning on becoming pregnant, notify your health care provider to best manage your medications. People living with MDD who wish to become pregnant face important decisions. Untreated MDD has risks to the fetus, as well as the mother. It is important to discuss the risks and benefits of treatment with your doctor and caregivers. For women who take antidepressant medications during weeks 13 through the end of their pregnancy (second and third trimesters), there is a risk that the baby can be born before it is fully developed (before 37 weeks).
For mothers who have taken SSRIs during their pregnancy, there appears to be less than a 1% chance of infants developing persistent pulmonary hypertension. This is a potentially fatal condition that is associated with use of the antidepressant in the second half of pregnancy. However, women who discontinued antidepressant therapy were five times more likely to have a depression relapse than those who continued their antidepressant. If you are pregnant, please discuss the risks and benefits of antidepressant use with your health care provider.
However, women who discontinued antidepressant therapy were five times more likely to have a depression relapse than those who continued their antidepressant. If you are pregnant, please discuss the risks and benefits of antidepressant use with your health care provider.
Caution is advised with breastfeeding since fluvoxamine does pass into breast milk.
What Should I Discuss With My Health Care Provider Before Taking Fluvoxamine?
- Symptoms of your condition that bother you the most
- If you have thoughts of suicide or harming yourself
- Medications you have taken in the past for your condition, whether they were effective or caused any adverse effects
- If you experience side effects from your medications, discuss them with your provider. Some side effects may pass with time, but others may require changes in the medication.
- Any other psychiatric or medical problems you have, including a history of bipolar disorder
- All other medications you are currently taking (including over the counter products, herbal and nutritional supplements) and any medication allergies you have
- Other non-medication treatment you are receiving, such as talk therapy or substance abuse treatment.
 Your provider can explain how these different treatments work with the medication.
Your provider can explain how these different treatments work with the medication. - If you are pregnant, plan to become pregnant, or are breastfeeding
- If you drink alcohol or use drugs
How Should I Take Fluvoxamine?
Fluvoxamine is usually taken two times per day with or without food. The extended release formulation may be taken one time per day with or without food.
Typically patients begin at a low dose of medicine and the dose is increased slowly over several weeks.
The dose usually ranges from 50 mg to 300 mg. Only your health care provider can determine the correct dose for you.
Consider using a calendar, pillbox, alarm clock, or cell phone alert to help you remember to take your medication. You may also ask a family member or friend to remind you or check in with you to be sure you are taking your medication.
The extended-release forms should be swallowed whole. They should not be chewed, crushed, or broken.
What Happens If I Miss A Dose Of Fluvoxamine?
If you miss a dose of fluvoxamine, take it as soon as you remember, unless it is closer to the time of your next dose. Discuss this with your health care provider. Do not double your next dose or take more than what is prescribed.
Discuss this with your health care provider. Do not double your next dose or take more than what is prescribed.
What Should I Avoid While Taking Fluvoxamine?
Avoid drinking alcohol or using illegal drugs while you are taking antidepressant medications. They may decrease the benefits (e.g., worsen your condition) and increase adverse effects (e.g., sedation) of the medication.
What Happens If I Overdose With Fluvoxamine?
If an overdose occurs, call your doctor or 911. You may need urgent medical care. You may also contact the poison control center at 1-800-222-1222.
A specific treatment to reverse the effects of fluvoxamine does not exist.
What Are The Possible Side Effects Of Fluvoxamine?
Common side effects
Headache, nausea, diarrhea, dry mouth, dizziness, increased sweating, feeling nervous, restless, fatigued, or having trouble sleeping (insomnia). These will often improve over the first week or two as you continue to take the medication.
Sexual side effects, such as problems with orgasm or ejaculatory delay, often do not diminish over time.
Rare/serious side effects
Low sodium blood levels (symptoms of low sodium levels may include headache, weakness, difficulty concentrating and remembering), teeth grinding, angle closure glaucoma (symptoms of angle closure glaucoma may include eye pain, changes in vision, swelling or redness in or around eye), serotonin syndrome (symptoms may include shivering, diarrhea, confusion, severe muscle tightness, fever, seizures, and death), seizure
SSRI antidepressants including fluvoxamine may increase the risk of bleeding events. Combined use of aspirin, nonsteroidal anti-inflammatory drugs (e.g., ibuprofen, naproxen), warfarin, and other anti-coagulants may increase this risk. This may include symptoms such as gums that bleed more easily, nose bleed, or gastrointestinal bleeding. Some cases have been life threatening.
Are There Any Risks For Taking Fluvoxamine For Long Periods Of Time?
To date, there are no known problems associated with long term use of fluvoxamine. It is a safe and effective medication when used as directed.
It is a safe and effective medication when used as directed.
What Other Medications May Interact With Fluvoxamine?
Fluvoxamine should not be taken with or within 6 weeks of taking monoamine oxidase inhibitors (MAOIs). These include phenelzine (Nardil®), tranylcypromine (Parnate®), isocarboxazid (Marplan®), rasagiline (Azilect®), and selegiline (Emsam®).
Although rare, there is an increased risk of serotonin syndrome when fluvoxamine is used with other medications that increase serotonin, such as other antidepressants, migraine medications called “triptans” (e.g., Imitrex®), some pain medications (e.g., tramadol (Ultram®), amphetamines, and the antibiotic linezolid (Zyvox®).
Fluvoxamine may increase the levels and effects of:
- Warfarin (Coumadin®)
- Theophylline (Theo-Dur®)
- Certain anticonvulsants: carbamazepine (Tegretol®, Equetro®), phenytoin (Dilantin®)
- Beta blockers, such as propranolol (Inderal®), metoprolol (Lopressor®, Toprol XL®)
- Benzodizapines, such as alprazolam (Xanax®), diazepam (Valium®)
- Certain antipsychotics, such as olanzapine (Zyprexa®), clozapine (Clozaril®), aripiprazole (Abilify®), quetiapine (Seroquel®)
- Mexiletine (Mexitil®)
- Omeprazole (Prilosec®)
- Methadone (Dolophine®)
- Tricyclic antidepressants, such as amitriptyline (Elavil®)
- Warfarin (Coumadin®)
- Theophylline (Theo-Dur®)
- Certain anticonvulsants: carbamazepine (Tegretol®, Equetro®), phenytoin (Dilantin®)
- Beta blockers, such as propranolol (Inderal®), metoprolol (Lopressor®, Toprol XL®)
- Benzodizapines, such as alprazolam (Xanax®), diazepam (Valium®)
- Certain antipsychotics, such as olanzapine (Zyprexa®), clozapine (Clozaril®), aripiprazole (Abilify®), quetiapine (Seroquel®)
- Mexiletine (Mexitil®)
- Omeprazole (Prilosec®)
- Methadone (Dolophine®)
- Tricyclic antidepressants, such as amitriptyline (Elavil®)
Fluvoxamine may decrease the effects of clopidogrel (Plavix®).
Fluvoxamine may increase the effects of other medications that can cause bleeding (e.g., ibuprofen (Advil®, Motrin®), warfarin (Coumadin®), and aspirin).
Combining fluvoxamine with ramelteon (RozeremTM), tizanidine (Zanaflex®), thioridazine (Mellaril®), pimozide, or alosetron (Lotronex®) is not recommended.
How Long Does It Take For Fluvoxamine To Work?
Sleep, energy, or appetite may show some improvement within the first 1-2 weeks. Improvement in these physical symptoms can be an important early signal that the medication is working. Depressed mood and lack of interest in activities may need up to 6-8 weeks to fully improve.
Summary of FDA Black Box Warnings
Suicidal thoughts or actions in children and adults
Depression and certain other psychiatric disorders are themselves associated with increases in the risk of suicide. Patients with major depressive disorder (MDD), both adult and pediatric, may experience worsening of their depression and/or the emergence of suicidal ideation and behavior (suicidality) or unusual changes in behavior, whether or not they are taking antidepressant medications. This risk may persist until significant remission occurs.
This risk may persist until significant remission occurs.
In short-term studies, antidepressants increased the risk of suicidality in children, adolescents, and young adults when compared to placebo. Short-term studies did not show an increase in the risk of suicidality with antidepressants compared to placebo in adults beyond age 24. Adults age 65 and older taking antidepressants have a decreased risk of suicidality. Patients, their families, and caregivers should be alert to the emergence of anxiety, restlessness, irritability, aggressiveness and insomnia. If these symptoms emerge, they should be reported to the patient’s prescriber or health care professional. All patients being treated with antidepressants for any indication should watch for and notify their health care provider for worsening symptoms, suicidality and unusual changes in behavior, especially during the first few months of treatment.
Provided by
(December 2020)
©2020 The College of Psychiatric and Neurologic Pharmacists (CPNP) and the National Alliance on Mental Illness (NAMI). CPNP and NAMI make this document available under the Creative Commons Attribution-No Derivatives 4.0 International License. Last Updated: January 2016.
CPNP and NAMI make this document available under the Creative Commons Attribution-No Derivatives 4.0 International License. Last Updated: January 2016.
This information is being provided as a community outreach effort of the College of Psychiatric and Neurologic Pharmacists. This information is for educational and informational purposes only and is not medical advice. This information contains a summary of important points and is not an exhaustive review of information about the medication. Always seek the advice of a physician or other qualified medical professional with any questions you may have regarding medications or medical conditions. Never delay seeking professional medical advice or disregard medical professional advice as a result of any information provided herein. The College of Psychiatric and Neurologic Pharmacists disclaims any and all liability alleged as a result of the information provided herein.
How Long Does Luvox Take to Work?
Date: 2018-09-17 17:28
By: Health Community Member
Luvox (fluvoxamine maleate) is an antidepressant indicated for the treatment of obsessions and compulsions in adult and pediatric patients with obsessive-compulsive disorder (OCD). It can also be used to treat major depressive episode, panic disorder, social anxiety disorder, post-traumatic stress disorder (PTSD), and bulimia nervosa. Antidepressants are known to have a delayed onset of action. Fluvoxamine may start to work within two to four weeks. Some studies suggested that it is possible to achieve clinical improvement by the end of the first week of treatment.
It can also be used to treat major depressive episode, panic disorder, social anxiety disorder, post-traumatic stress disorder (PTSD), and bulimia nervosa. Antidepressants are known to have a delayed onset of action. Fluvoxamine may start to work within two to four weeks. Some studies suggested that it is possible to achieve clinical improvement by the end of the first week of treatment.
This antidepressant is available in a 25mg, 50mg, and 100mg tablet. If you are suffering from OCD, your doctor may prescribe an initial dose of 50mg tablet to be taken at bedtime. The maximum dose for fluvoxamine is 300mg per day. If side effects are well tolerated, your dose may be increased every four to seven days. Daily doses exceeding 100mg must be divided throughout the day.
Luvox onset of action
Fluvoxamine belongs to the group of antidepressants called selective serotonin reuptake inhibitors (SSRI). In the history of antidepressive agents, none has reached the same level of popularity as SSRIs. The approval of Prozac (fluoxetine) in 1987 brought antidepressants in the limelight. One out of six Americans take daily psychiatric drugs, according to a study published in the Journal of American Medical Association. About 12% of these medications are antidepressants. Despite the development of newer antidepressive agents, the conventional wisdom on its delayed onset of action remains. The National Institute for Health and Clinical Excellence (NICE) has issued a statement for prescribers that patients must be informed about the delay in onset of effect when taking antidepressants.
The approval of Prozac (fluoxetine) in 1987 brought antidepressants in the limelight. One out of six Americans take daily psychiatric drugs, according to a study published in the Journal of American Medical Association. About 12% of these medications are antidepressants. Despite the development of newer antidepressive agents, the conventional wisdom on its delayed onset of action remains. The National Institute for Health and Clinical Excellence (NICE) has issued a statement for prescribers that patients must be informed about the delay in onset of effect when taking antidepressants.
It was believed that it takes two to three weeks before an antidepressant medication shows pertinent effects. Taylor and colleagues challenged this idea in a systematic review and meta-analysis of randomized trials, which aims to establish if an early response to SSRI treatment is possible. The authors found 28 trials with 3,618 participants who received SSRIs and 2,254 who were given a placebo. Using data from week one to six, the authors found that symptomatic improvement in the SSRI group occurs by week one and continues for the following weeks, albeit at a declining rate. The authors concluded that early response to this group of antidepressants might represent a true response and not just a placebo effect.
Using data from week one to six, the authors found that symptomatic improvement in the SSRI group occurs by week one and continues for the following weeks, albeit at a declining rate. The authors concluded that early response to this group of antidepressants might represent a true response and not just a placebo effect.
Why antidepressants take time to work
There is no consensus on why the antidepressive effects of these drugs take some time to become apparent. In the case of SSRIs, the most widely used class of antidepressants, increasing the synaptic levels of 5-hydroxytryptamine (5HT) or serotonin only takes hours or days, but therapeutic response is delayed by weeks or months. Blocking the reuptake of 5HT causes the downregulation of 5HT1A receptors through negative feedback. This process takes time since downregulation of the said receptors is an adaptive response. However, newer drugs that act on 5HT4 receptors have shown rapid antagonistic effect in animal models. Even at postsynaptic level, 5HT4 receptor inhibition lead to rapid and significant response. Another study by Mendez-David and colleagues have shown that 5HT4 activation is important in fluoxetine’s anxiolytic and anti-depressant-like effects. This proves that acting on these receptors for a rapid onset of therapeutic effect could be the next target of novel antidepressants.
Even at postsynaptic level, 5HT4 receptor inhibition lead to rapid and significant response. Another study by Mendez-David and colleagues have shown that 5HT4 activation is important in fluoxetine’s anxiolytic and anti-depressant-like effects. This proves that acting on these receptors for a rapid onset of therapeutic effect could be the next target of novel antidepressants.
What to expect when taking Luvox?
Fluvoxamine was the first SSRI to be approved for the treatment of obsessive-compulsive disorder in children. Low levels of 5HT have been associated with depression and anxiety, as well as panic disorder, OCD, and other mood disorders. In the gut, low levels of serotonin may cause irritable bowel syndrome, bone problems, and even cardiovascular disease. As its name implies, SSRI prevents the reuptake or reabsorption of serotonin back into the nerve endings. Compared to other antidepressants, it has little effect on dopamine and norepinephrine uptake systems. Simply put, SSRI increases the levels of serotonin in the brain, which in return, provides a “feel good” effect. Yet the effects of antidepressants like Luvox is not immediate. While it’s possible for some patients to notice improvement of symptoms in the first week of treatment, it may take weeks or months for other people to respond to the medication. That’s why it’s important to stick with your meds with or without symptom improvement. There are valid evidence supporting the claims that SSRIs have better safety profiles than other class of antidepressants, such as MAO inhibitors and TCAs. But your doctor will most likely put you in a low starting dose to prevent side effects, and more importantly, to avoid discontinuance.
Simply put, SSRI increases the levels of serotonin in the brain, which in return, provides a “feel good” effect. Yet the effects of antidepressants like Luvox is not immediate. While it’s possible for some patients to notice improvement of symptoms in the first week of treatment, it may take weeks or months for other people to respond to the medication. That’s why it’s important to stick with your meds with or without symptom improvement. There are valid evidence supporting the claims that SSRIs have better safety profiles than other class of antidepressants, such as MAO inhibitors and TCAs. But your doctor will most likely put you in a low starting dose to prevent side effects, and more importantly, to avoid discontinuance.
Fluvoxamine - description of the substance, pharmacology, use, contraindications, formula
Contents
- Structural formula
- Russian name
- English name
- Latin name of the substance Fluvoxamine
- Chemical name nine0007 Gross formula
- Pharmacological group of substance Fluvoxamine
- Nosological classification
- CAS code
- Pharmacological action
- Characteristic
- Pharmacology nine0007 Application of substance Fluvoxamine
- Contraindications
- Restrictions for use
- Use in pregnancy and lactation
- Side effects of the substance Fluvoxamine
- Interaction
- Overdose nine0007 Route of administration and doses
- Precautions
- Trade names with the active substance Fluvoxamine
Structural formula
Russian name
Fluvoxamine
English name
Fluvoxamine
Latin name of the substance0005
Chemical name
(E)-5-Methoxy-1-[4-(trifluoromethyl)phenyl]-1-pentanone-0-(2-aminoethyl)oxime (as maleate)
General formula
C 15 H 21 F 3 N 2 O 2
Pharmacological group of the substance Fluvoxamine
Antidepressants
Nosological classification
ICD-10 code list
- F32 Depressive episode
- F42 Obsessive-compulsive disorder
CAS code
54739-18-3
Pharmacological action
Pharmacological action - nine0065 antidepressant .
Characteristics
Antidepressant of the SSRI group.
Fluvoxamine maleate is a white or almost white, odorless crystalline powder. Let's well dissolve in ethyl alcohol and chloroform, we will badly dissolve in water, it is practically insoluble in diethyl ether. Lipophilen.
Pharmacology
Selectively inhibits the reuptake of neuronal serotonin from the synaptic cleft by blocking the membrane pump of the presynaptic membrane. Helps to increase serotonergic transmission and reduce the circulation of serotonin. Blocks the reuptake of serotonin in platelets. Slightly affects the reuptake of dopamine and norepinephrine. Does not affect histaminergic, alpha- and beta-adrenergic, m-cholinergic, dopaminergic, 5-HT 1 - and 5-HT 2 receptors. There is evidence of the effectiveness of fluvoxamine in obsessive-compulsive disorders, incl. in children and adolescents (8–17 years).
Well absorbed from the gastrointestinal tract. Bioavailability does not depend on food intake and is about 53% (due to the "first pass" effect through the liver). When taken for 10 days at doses of 100, 200 and 300 mg / day, the equilibrium concentration in the blood is reached after about 1 week. max "> C max in the equilibrium state is achieved within 3-8 hours after administration and is 88, 283 and 546 ng / ml, respectively. There is no correlation between plasma concentration and efficacy. Plasma protein binding is about 80% (mainly with albumin).The volume of distribution is high - 25 l / kg. In the liver, it undergoes demethylation and deamination; nine inactive metabolites (fluvoxamic acid, fluvoxethanol, etc.) have been identified. Inhibits cytochrome P450 isoenzymes: CYP1A2, CYP3A4, CYP2C9, has a weaker effect on CYP2D6. T 1/2 - 15-20 hours 94% is excreted in the urine for 71 hours (2-3% unchanged).
Bioavailability does not depend on food intake and is about 53% (due to the "first pass" effect through the liver). When taken for 10 days at doses of 100, 200 and 300 mg / day, the equilibrium concentration in the blood is reached after about 1 week. max "> C max in the equilibrium state is achieved within 3-8 hours after administration and is 88, 283 and 546 ng / ml, respectively. There is no correlation between plasma concentration and efficacy. Plasma protein binding is about 80% (mainly with albumin).The volume of distribution is high - 25 l / kg. In the liver, it undergoes demethylation and deamination; nine inactive metabolites (fluvoxamic acid, fluvoxethanol, etc.) have been identified. Inhibits cytochrome P450 isoenzymes: CYP1A2, CYP3A4, CYP2C9, has a weaker effect on CYP2D6. T 1/2 - 15-20 hours 94% is excreted in the urine for 71 hours (2-3% unchanged).
In the study of the excretion of fluvoxamine in patients with impaired renal function (Cl creatinine 5-45 ml / min), who received it at 50 mg twice a day, no cumulation was noted; with hepatic dysfunction, the excretion of fluvoxamine decreased by 30%. In patients with genetically determined deficiency of the CYP2D6 enzyme (2-10% of the population) max "> C max , AUC and T 1/2 increase by 52%, 200% and 62% respectively. In elderly patients (66-73 years) max "> C max fluvoxamine is 40% higher, excretion is 50% lower compared to younger patients (19-35 years). T 1/2 in the elderly in humans is 17.4 and 25.9 hours after administration at a dose of 50 and 100 mg, respectively (in young people - 13.6 and 15.6 hours).In smokers, the bioavailability of fluvoxamine is reduced due to the induction of its metabolism (by 25%).
In patients with genetically determined deficiency of the CYP2D6 enzyme (2-10% of the population) max "> C max , AUC and T 1/2 increase by 52%, 200% and 62% respectively. In elderly patients (66-73 years) max "> C max fluvoxamine is 40% higher, excretion is 50% lower compared to younger patients (19-35 years). T 1/2 in the elderly in humans is 17.4 and 25.9 hours after administration at a dose of 50 and 100 mg, respectively (in young people - 13.6 and 15.6 hours).In smokers, the bioavailability of fluvoxamine is reduced due to the induction of its metabolism (by 25%).
Animal studies have shown a decrease in body weight and survival of fetuses, an increase in the frequency of intrapartum death when taking fluvoxamine during pregnancy at a dose 2-4 times higher than the MRHD.Concentration in breast milk is 3 times lower than that in plasma (0 .09and 0.31 mg/l, respectively, when taken at a dose of 100 mg/day).
Use of the substance Fluvoxamine
Depression of various origins, obsessive-compulsive disorder.
Contraindications
Hypersensitivity, liver failure, simultaneous use of astemizole, cisapride, terfenadine, MAO inhibitors (including furazolidone, procarbazine, selegiline), breastfeeding, children under 8 years of age.
Restrictions on use
Epilepsy, pregnancy; drug dependence, mania, hypomania, seizures, or a history of myocardial infarction.
Use in pregnancy and lactation
Use with caution during pregnancy, balancing the expected benefit to the mother and the potential risk to the fetus.
FDA fetal category C.
Breast-feeding should be avoided during treatment.
Side effects of the substance Fluvoxamine
Of 1087 patients with obsessive compulsive disorder and depression treated with fluvoxamine in controlled clinical trials in North America, 22% of patients discontinued treatment due to side effects. Among them were noted (in brackets the percentage of occurrence in the placebo group is indicated):
From the side of the nervous system and sensory organs: headache 3% (1%), dizziness 2% (less than 1%), asthenia 2% (less than 1 %), insomnia 4% (1%), drowsiness 4% (less than 1%), nervousness 2% (less than 1%), anxiety 1% (less than 1%), agitation 2% (less than 1%). nine0005
nine0005
From the gastrointestinal tract: nausea 9% (1%), anorexia 1% (less than 1%), dry mouth 1% (less than 1%) dyspepsia 1% (less than 1%), vomiting 2% (less than 1%) %), diarrhea 1% (less than 1%), abdominal pain 1% (0%).
In placebo-controlled trials in patients with obsessive-compulsive disorder who received fluvoxamine at a dose of 100–300 mg/day for 10 weeks and with depression who received fluvoxamine at the same dose for 6 weeks, with a frequency of more than 1 % the following side effects were observed (in brackets the percentage of occurrence in the placebo group is indicated):
From the nervous system and sensory organs: headache 22% (20%), dizziness 11% (6%), asthenia 14% (6%), drowsiness 22% (8%), insomnia 21% (10%) %), nervousness 12% (5%), anxiety 5% (3%), agitation 2% (1%), depression 2% (1%), CNS stimulation 2% (1%), tremor 5% (1% ), taste change 3% (1%), amblyopia 3% (2%).
From the side of the cardiovascular system and blood (blood formation, hemostasis): heartbeat 3% (2%), vasodilation 3% (1%), arterial hypertension 2% (1%). nine0005
nine0005
From the respiratory system: upper respiratory tract infections 9% (5%), dyspnea 2% (1%), yawning 2% (0%).
From the digestive tract: anorexia 6% (2%), dry mouth 14% (10%), dental damage 3% (1%), dysphagia 2% (1%), dyspepsia 10% (5% ), nausea 40% (14%), flatulence 4% (3%), diarrhea 11% (7%), constipation 10% (8%), vomiting 5% (2%).
From the genitourinary system: ejaculation disorder 8% (1%), decreased libido 2% (1%), impotence 2% (1%), anorgasmia 2% (0%), frequent urination 3% (2% ), urinary retention 1% (0%). nine0005
Other: flu-like syndrome 3% (2%), chills 2% (1%), sweating 7% (3%).
Interaction
Incompatible with MAO inhibitors, incl. furazolidone, procarbazine and selegiline (risk of serotonergic syndrome and death). The development of serotonergic syndrome (chills, hyperthermia, muscle rigidity, myoclonus, autonomic lability, hypertensive crisis, agitation, tremor, restlessness, convulsions, diarrhea, hypomanic state) is possible while taking drugs with serotonergic activity (tryptophan, lithium compounds). Increases the plasma concentration of propranolol (5 times), metoprolol and other beta-blockers, indirect anticoagulants, incl. warfarin (for 98%), carbamazepine, clozapine (3 times), tricyclic antidepressants (amitriptyline, clomipramine, imipramine). Taking fluvoxamine concomitantly with antipsychotics of the butyrophenone group, including haloperidol, leads to an increase in their plasma concentration or to a 2-10-fold increase in the content of fluvoxamine. Able to inhibit the biotransformation of drugs metabolized with the participation of CYP1A2, CYP3A4, CYP2C9, CYP2D6 cytochrome P450 isoenzymes (phenytoin, quinidine, theophylline, caffeine, etc.), increasing the risk of adverse reactions. Taking fluvoxamine against the background of astemizole, cisapride or terfenadine can lead to a pronounced prolongation of the QT interval and the appearance of pirouette-type arrhythmias (possible death). When taken simultaneously with diltiazem, bradycardia may develop, with sumatriptan - weakness, hyperreflexia and impaired coordination of movements.
Increases the plasma concentration of propranolol (5 times), metoprolol and other beta-blockers, indirect anticoagulants, incl. warfarin (for 98%), carbamazepine, clozapine (3 times), tricyclic antidepressants (amitriptyline, clomipramine, imipramine). Taking fluvoxamine concomitantly with antipsychotics of the butyrophenone group, including haloperidol, leads to an increase in their plasma concentration or to a 2-10-fold increase in the content of fluvoxamine. Able to inhibit the biotransformation of drugs metabolized with the participation of CYP1A2, CYP3A4, CYP2C9, CYP2D6 cytochrome P450 isoenzymes (phenytoin, quinidine, theophylline, caffeine, etc.), increasing the risk of adverse reactions. Taking fluvoxamine against the background of astemizole, cisapride or terfenadine can lead to a pronounced prolongation of the QT interval and the appearance of pirouette-type arrhythmias (possible death). When taken simultaneously with diltiazem, bradycardia may develop, with sumatriptan - weakness, hyperreflexia and impaired coordination of movements. Reduces the excretion of benzodiazepines (alprazolam, bromazepam, diazepam, midazolam, triazolam), causing their cumulation; does not affect the excretion of lorazepam, oxazepam and temazepam. Enhances the side effects of alcohol. nine0005
Reduces the excretion of benzodiazepines (alprazolam, bromazepam, diazepam, midazolam, triazolam), causing their cumulation; does not affect the excretion of lorazepam, oxazepam and temazepam. Enhances the side effects of alcohol. nine0005
Overdose
Symptoms: dizziness, drowsiness, dry mouth, nausea, vomiting, diarrhea, bradycardia or tachycardia, arterial hypotension, ECG changes, abnormal liver function, mydriasis, tremor, myoclonus, seizures, oliguria, coma. Deaths have been described.
Treatment: induction of vomiting or gastric lavage, administration of activated charcoal, ECG monitoring, maintenance of vital functions, symptomatic therapy. There is no specific antidote. Dialysis and forced diuresis are ineffective (due to the large volume of distribution). nine0005
Method of administration and doses
Inside, adults, without chewing, drinking a small amount of water. The initial dose is 50-100 mg / day once (in the evening), with good tolerance, the dose is increased to 150-200 mg / day in 2-3 doses. The maximum daily dose is 300 mg.
The maximum daily dose is 300 mg.
Precautions
The interval between discontinuation of MAO inhibitors and the start of fluvoxamine, or its withdrawal and the start of MAO inhibitors, must be at least 14 days. Careful monitoring of patients with suicidal tendencies is required, especially at the beginning of treatment. Elderly patients should receive fluvoxamine at a reduced dosage. Use with caution for drivers of vehicles and people whose activities require increased concentration of attention and speed of psychomotor reactions. Alcohol should be avoided during treatment. nine0005
Animal studies have not shown drug dependence. Similar studies have not been conducted in humans. Use with caution in patients with a history of drug dependence or abuse.
Trade names with the active substance Fluvoxamine
Reset filters
Lek. form All lek. substance-powder forms film-coated tablets
Dosage All dosages 100 mg 50 mg No dosage
Manufacturer All manufacturers Mylan Laboratories SAS Rapharma SA Sinton s. r.o. Tula Pharmaceutical Factory OOO Pharmasyntez AO Abbott Biologikalz B.V. Abbott Healthcare SAS Advanced Pharmaceuticals LLC (Advanced Pharma LLC)
r.o. Tula Pharmaceutical Factory OOO Pharmasyntez AO Abbott Biologikalz B.V. Abbott Healthcare SAS Advanced Pharmaceuticals LLC (Advanced Pharma LLC)
Arpimed
Reception of Amitriptyline is possible not earlier than 14 days after discontinuation of MAO inhibitors.
Warnings and precautions
Talk to your doctor or pharmacist before using Amitriptyline. nine0005
Arrhythmias and hypotension may occur with high doses of amitriptyline. This can also occur at regular doses if you suffer from heart disease.
Prolongation of the QT interval
Cardiac pathology called “prolongation of the QT interval” (which is recorded on the electrocardiogram, ECG) and arrhythmia (rapid or irregular heartbeat) was observed with the use of Amitriptyline. Tell your doctor if:
- you have a slow heartbeat,
- you have or have had a problem where your heart is not able to supply the body with the blood it needs (a condition called heart failure),
- are taking other medicines that can cause heart problems, or
- have a disorder that leads to a decrease in the level of potassium or magnesium or an increase in the level of potassium in the blood
- if you are preparing for surgery, as it may be necessary to stop taking amitriptyline before administering anesthetics.
 In case of emergency surgery, the anesthesiologist should be informed about the treatment with amitriptyline. nine0008
In case of emergency surgery, the anesthesiologist should be informed about the treatment with amitriptyline. nine0008 - have an overactive thyroid or are taking thyroid medication.
Suicidal thoughts and worsening of your depressive disorder
If you are depressed, you may sometimes have suicidal thoughts and desire to hurt yourself. These may be increased the first time antidepressants are used, as these drugs take time to develop an effect, about 2 weeks or more. nine0005
This is especially observed in the following categories of patients:
- if you had suicidal thoughts and a desire to harm yourself earlier,
- if you are young. Data from clinical studies have shown that an increased risk of suicidal tendencies occurs in people under the age of 25 with psychiatric disorders treated with antidepressants.
If you have suicidal thoughts and want to hurt yourself, call your doctor or go to the hospital right away. nine0005
nine0005
It may be helpful to tell a relative or close friend that you are depressed and ask them to read this leaflet. You can ask them to tell you if they think your depression or anxiety is getting worse, or if they are worried about changes in your behavior.
Manic episode
Some patients with manic-depressive illness may enter a manic phase. It is characterized by exuberant and rapidly changing ideas, hyperthymia (persistent high spirits), and excessive physical activity. nine0005
Tell your healthcare provider if you have or have recently had health problems, especially if you have
- narrow angle glaucoma (loss of vision due to an abnormal increase in intraocular pressure)
- epilepsy, history of convulsions or seizures
- difficulty urinating
- prostate enlargement
- diseases of the thyroid gland
- bipolar disorder
- schizophrenia nine0007 acute liver disease
- severe heart disease
- pyloric stenosis (narrowing of the opening at the outlet of the stomach) and paralytic ileus (intestinal obstruction)
- diabetes, because you may need to adjust the dose of your diabetes medicine.

If you are using antidepressants such as selective serotonin reuptake inhibitors (SSRIs), your doctor may consider changing the dose of your medicine (see section Other drugs and Amitriptyline and section How to take Amitriptyline). nine0005
Older people are more likely to experience certain side effects, such as dizziness due to orthostatic hypotension (see section Possible side effects).
Children and adolescents
Depression, neuropathic pain, chronic headache of tenzial type and migraine prevention
amitriptylin should not be prescribed for children and adolescents under the age of 18 years old since this age group is for this age group since this age group is for this age group since this age group effectiveness has not been established. nine0005
Bedwetting
- ECG should be performed before initiation of amitriptyline therapy to rule out long QT syndrome
- Medicines in this group should not be taken concomitantly with anticholinergics (see also section Other medicines and Amitriptyline)
- Suicidal thoughts and behavior may also develop during early antidepressant treatment for disorders other than depression; in the treatment of patients with bedwetting, the same precautions should be observed as in the treatment of patients with depression.
 nine0008
nine0008
Other medicines and amitriptyline
Some medicines can affect how other medicines work, and this can sometimes cause serious side effects.
Tell your doctor or pharmacist if you are taking, have recently taken or might take any other medicines such as: (used to treat Parkinson's disease). They should not be taken during a course of treatment with amitriptyline (see section Do not take amitriptyline)
 John's wort - herbal remedy for depression
John's wort - herbal remedy for depression
Also tell your doctor if you are taking, have recently taken or may be taking medicines that can affect your heart rate, including:
- palpitations medicines (including quinidine and sotalol)
- astemizole and terfenadine (used to treat allergic reactions and hay fever)
- medicines used to treat certain mental illnesses (including pimozide and sertindole)
- cisapride (used to treat certain types of stomach disorders)
- halofantrine (used to treat malaria)
- methadone (used for pain relief and drug detox)
- diuretics (including furosemide).

If you are having surgery with general or local anesthetics, you must tell your doctor that you are taking this drug.
You must also tell your dentist that you are taking this drug before you use a local anesthetic.
Amitriptyline with alcohol
It is not recommended to drink alcohol during treatment with this medicine, as this may increase the sedative effect. nine0005
Pregnancy and lactation
If you are pregnant or breastfeeding, think you may be pregnant or are planning to become pregnant, please consult your healthcare professional.
Amitriptyline is not recommended during pregnancy unless you and your doctor have discussed the risks and benefits of using the drug.
If you are taking this drug during the last trimester of pregnancy, you should know that your newborn baby may have the following side effects such as irritability, increased muscle tension, tremors, irregular breathing, not wanting to drink fluids, loud crying, urinary retention and constipation. nine0005
nine0005
Your doctor will tell you to start/continue/stop breastfeeding or stop using this drug based on the benefits of breastfeeding for your baby and the benefits of therapy for you.
Influence on the ability to drive a car and use mechanisms
The drug may cause drowsiness, dizziness, especially at the beginning of treatment. It is unacceptable to drive or work with mechanisms if it negatively affects you. nine0005
Important information about the ingredients of amitriptyline tablets
Amitriptyline tablets contain lactose medicine.
How to take Amitriptyline
Amitriptyline should be taken exactly as directed by your doctor. If you have any doubts, you should consult your doctor or pharmacist. nine0005
Not all dosing regimens are possible with different dosage forms and doses of the drug.
The appropriate formulation and dose of the drug must be selected for starting 3 and subsequent increasing doses.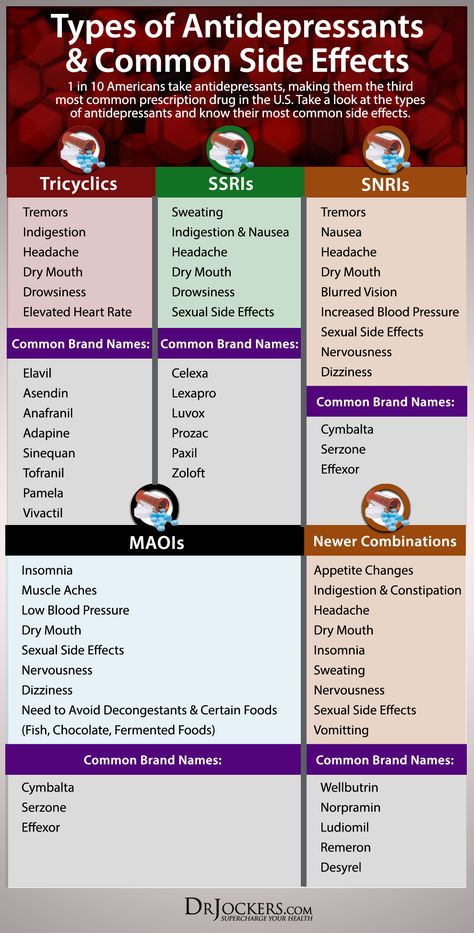
Depression
Adults :
The recommended starting dose is 25 mg twice a day. Depending on the clinical effect, the dose may be increased up to 150 mg/day divided into two doses. nine0005
Elderly patients (over 65 years of age) and patients with cardiovascular disease
The recommended starting dose is 10-25 mg per day. Depending on the clinical effect, the dose may be increased to 100 mg / day, divided into two doses. If you are taking 100mg to 150mg of the drug, you may need to see your doctor more often.
Use in children and adolescents
Amitriptyline is not recommended for children and adolescents to treat depression. See section 2 for more information.
Neuropathic pain, chronic headaches tension-type headaches and migraine prophylaxis
Your doctor will adjust the dose to your treatment according to your symptom and response to your symptoms.
Adults :
The recommended starting dose is 10-25 mg in the evening.
The recommended daily dose is 25-75 mg.
Depending on the clinical effect, the dose may be gradually increased. If you are taking more than 100mg/day, you may need to see your doctor more often. Take the drug once a day or divide the dose into two doses, your doctor will tell you.
Elderly patients (over 65 years of age) and patients with cardiovascular disease
The recommended starting dose is 10-25 mg in the evening.
Depending on the clinical effect of the drug, the dose may be gradually increased.
If you are taking more than 75 mg/day, you may need to see your doctor more often.
Use in children and adolescents
Amitriptyline is not recommended for use in children and adolescents for the treatment of neuropathic pain, chronic tension headache and migraine prophylaxis. For more information, see What you need to know before you use Amitriptyline.
For more information, see What you need to know before you use Amitriptyline.
Bedwetting
Use in children and adolescents
0008
The dose should be increased gradually.
Should be taken 1 to 1.5 hours before bedtime.
Before starting treatment, your healthcare provider should perform an ECG to check for signs of abnormal heartbeat.
Your doctor will re-evaluate your condition after 3 months of treatment and, if necessary, perform a repeat ECG. nine0005
Do not stop taking this medicine without your doctor's advice.
Special Patient Populations
Patients with liver disease or known to be "slow metabolisers" are usually given lower doses.
Your doctor may take blood samples to check your amitriptyline level (see What you need to know before you use amitriptyline).
How and when to take Amitriptyline
The drug should be taken during or after a meal.
Tablets should be swallowed whole with water. Tablets should not be chewed.
Treatment period
Do not change the dose of the drug or stop taking the drug without consulting a doctor.
Depression
As with other drugs used to treat depression, this too can take several weeks before you feel any improvement in your condition. nine0005
In the treatment of depression, the duration of treatment is individual and is usually at least 6 months. The duration of treatment is determined by your doctor.
Continue taking Amitriptyline for as long as your doctor tells you to. The disease may persist for a long time. If you stop treatment too soon, the symptoms of the disease may recur.
Neuropathic pain, chronic headaches tension type and Migraine Prevention
It may take a few weeks for your condition to improve.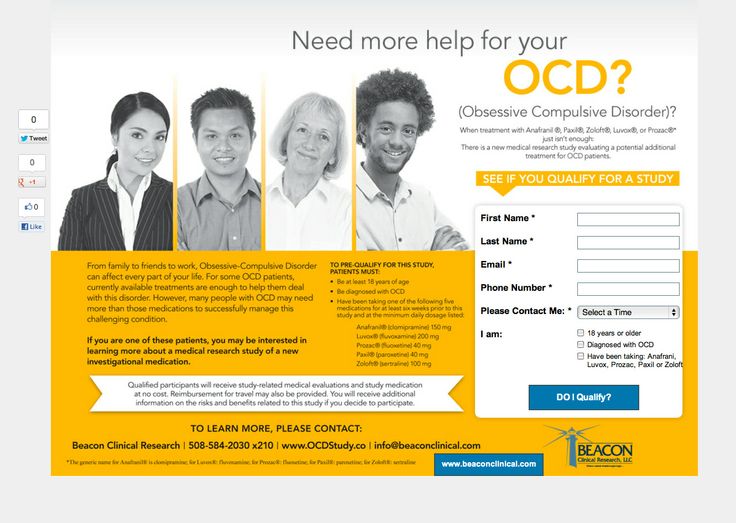
Talk to your doctor about the duration of treatment and continue taking the drug until the doctor stops it.
Bedwetting
Your doctor will determine if you need to continue treatment after 3 months of taking the drug.
If you have taken more Amitriptyline than recommended
If you have taken more Amitriptyline than prescribed by your doctor, contact your doctor or the nearest hospital emergency department immediately, even if you do not experience any discomfort or symptoms of poisoning . Take the medicine package with you if you go to the doctor or hospital.
Overdose symptoms include:
- dilated pupils
- rapid or irregular heartbeat
- difficulty urinating
- dry mouth or tongue
- intestinal obstruction
- seizures
- fever
- anxiety
- confusion
- hallucinations
- involuntary movements
- low blood pressure, weak pulse, pallor
- shortness of breath
- cyanosis of the skin
- Decreased heart rate
- drowsiness
- loss of consciousness
- coma
- various heart diseases such as cardiac conduction block, heart failure, hypotension, cardiogenic shock, metabolic acidosis, hypokalemia.