How long does it take antidepressants to start working
Overview - Antidepressants - NHS
Antidepressants are a type of medicine used to treat clinical depression.
They can also be used to treat a number of other conditions, including:
- obsessive compulsive disorder (OCD)
- generalised anxiety disorder
- post-traumatic stress disorder (PTSD)
Antidepressants are also sometimes used to treat people with long-term (chronic) pain.
Read more about when antidepressants are used.
How antidepressants work
It's not known exactly how antidepressants work.
It's thought they work by increasing levels of chemicals in the brain called neurotransmitters. Certain neurotransmitters, such as serotonin and noradrenaline, are linked to mood and emotion.
Neurotransmitters may also affect pain signals sent by nerves, which may explain why some antidepressants can help relieve long-term pain.
While antidepressants can treat the symptoms of depression, they do not always address its causes. This is why they're usually used in combination with therapy to treat more severe depression or other mental health conditions.
How effective are antidepressants?
Research suggests that antidepressants can be helpful for people with moderate or severe depression.
They're not usually recommended for mild depression, unless other treatments like talking therapy have not helped.
Doses and duration of treatment
Antidepressants are usually taken in tablet form. When they're prescribed, you'll start on the lowest possible dose thought necessary to improve your symptoms.
Antidepressants usually need to be taken for 1 or 2 weeks (without missing a dose) before the benefit starts to be felt. It's important not to stop taking them if you get some mild side effects early on, as these effects usually wear off quickly.
If you take an antidepressant for 4 weeks without feeling any benefit, speak to your GP or mental health specialist. They may recommend increasing your dose or trying a different medicine.
A course of treatment usually lasts for at least 6 months after you start to feel better. Some people with recurrent depression may be advised to take them indefinitely.
Read more about antidepressant dosages.
Side effects
Different antidepressants can have a range of different side effects. Always check the information leaflet that comes with your medicine to see what the possible side effects are.
The most common side effects of antidepressants are usually mild. Side effects should improve within a few days or weeks of treatment, as the body gets used to the medicine.
Read more about:
- possible side effects of antidepressants
- cautions and interactions of antidepressants
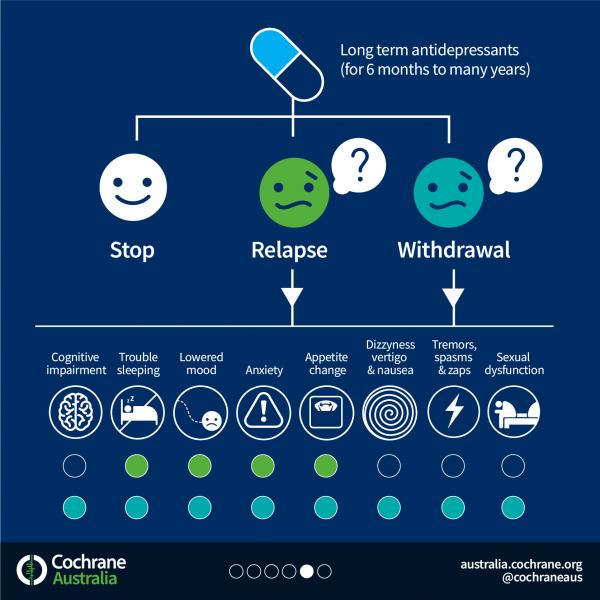
Coming off antidepressants
Talk to your doctor before you stop taking antidepressants. It's important that you do not stop taking antidepressants suddenly.
Once you're ready to come off antidepressants, your doctor will probably recommend reducing your dose gradually over several weeks – or longer, if you have been taking them for a long time.
This is to help prevent any withdrawal symptoms you might get as a reaction to coming off the medicine.
Read more about stopping or coming off antidepressants.
Types of antidepressants
There are several different types of antidepressants.
Selective serotonin reuptake inhibitors (SSRIs)
SSRIs are the most widely prescribed type of antidepressants. They're usually preferred over other antidepressants, as they cause fewer side effects. An overdose is also less likely to be serious.
Fluoxetine is probably the best known SSRI (sold under the brand name Prozac). Other SSRIs include citalopram (Cipramil), escitalopram (Cipralex), paroxetine (Seroxat) and sertraline (Lustral).
Serotonin-noradrenaline reuptake inhibitors (SNRIs)
SNRIs are similar to SSRIs. They were designed to be a more effective antidepressant than SSRIs. However, the evidence that SNRIs are more effective in treating depression is uncertain. It seems that some people respond better to SSRIs, while others respond better to SNRIs.
It seems that some people respond better to SSRIs, while others respond better to SNRIs.
Examples of SNRIs include duloxetine (Cymbalta and Yentreve) and venlafaxine (Efexor).
Noradrenaline and specific serotonergic antidepressants (NASSAs)
NASSAs may be effective for some people who are unable to take SSRIs. The side effects of NASSAs are similar to those of SSRIs, but they're thought to cause fewer sexual problems. However, they may also cause more drowsiness at first.
The main NASSA prescribed in the UK is mirtazapine (Zispin).
Tricyclic antidepressants (TCAs)
TCAs are an older type of antidepressant. They're no longer usually recommended as the first treatment for depression because they can be more dangerous if an overdose is taken. They also cause more unpleasant side effects than SSRIs and SNRIs.
Exceptions are sometimes made for people with severe depression that fail to respond to other treatments. TCAs may also be recommended for other mental health conditions, such as OCD and bipolar disorder.
TCAs may also be recommended for other mental health conditions, such as OCD and bipolar disorder.
Examples of TCAs include amitriptyline, clomipramine, dosulepin, imipramine, lofepramine and nortriptyline.
Some types of TCAs, such as amitriptyline, can also be used to treat chronic nerve pain.
Serotonin antagonists and reuptake inhibitors (SARIs)
SARIs are not usually the first choice of antidepressant, but they may be prescribed if other antidepressants have not worked or have caused side effects.
The main SARI prescribed in the UK is trazodone (Molipaxin).
Monoamine oxidase inhibitors (MAOIs)
MAOIs are an older type of antidepressant that are rarely used nowadays.
They can cause potentially serious side effects so should only be prescribed by a specialist doctor.
Examples of MAOIs include tranylcypromine, phenelzine and isocarboxazid.
Other treatments for depression
Other treatments for depression include talking therapies such as cognitive behavioural therapy (CBT).
People with moderate to severe depression are usually treated using a combination of antidepressants and CBT. Antidepressants work quickly in reducing symptoms, whereas CBT takes time to deal with causes of depression and ways of overcoming it.
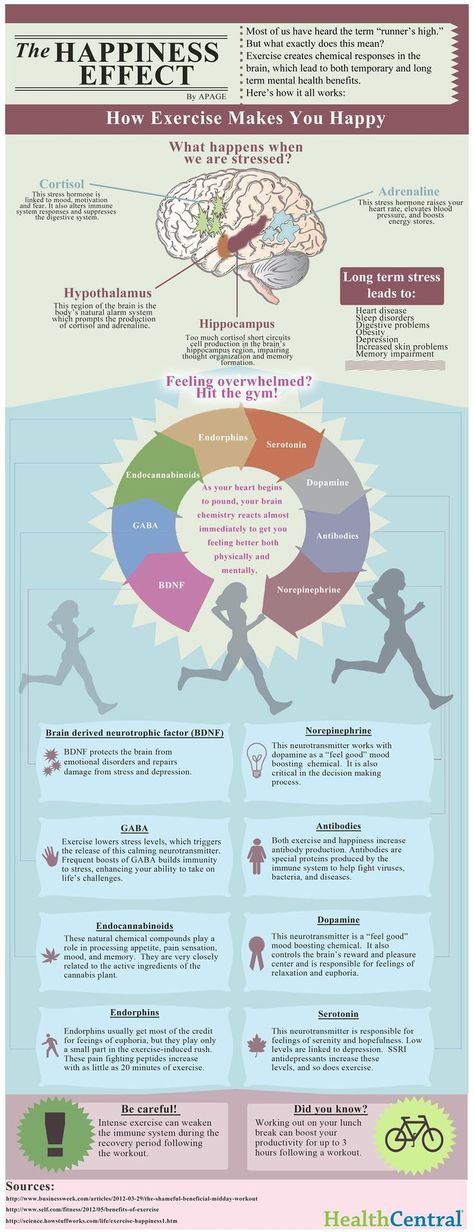
Regular exercise has also been shown to be useful for those with mild depression.
Read more about alternatives to antidepressants.
Yellow Card Scheme
The Yellow Card Scheme allows you to report suspected side effects from any type of medicine you're taking. It's run by a medicines safety watchdog called the Medicines and Healthcare products Regulatory Agency (MHRA).
It's run by a medicines safety watchdog called the Medicines and Healthcare products Regulatory Agency (MHRA).
See the Yellow Card Scheme website for more information.
Community content from HealthUnlockedHow Long Does It Take for Antidepressants to Work?
Skip to contentPublished: March 9, 2022 Updated: October 27, 2022
Published: 03/09/2022 Updated: 10/27/2022
The timing of a drug’s antidepressant effects depends on many factors including the patient’s symptoms, biological individuality, and life stressors. Overall, a person can expect an antidepressant to work anywhere from four to eight weeks after the first dose.1 Some may notice wanted differences much sooner, while others will never note the desired effects.
Online Psychiatry and Medication Management Covered By Insurance
Talkiatry offers psychiatric appointments with real doctors within a week. They’re in-network with every major insurer and offer medication management. Take the assessment and meet your new psychiatrist.
They’re in-network with every major insurer and offer medication management. Take the assessment and meet your new psychiatrist.
Choosing Therapy is compensated for marketing by Talkiatry.
Free Assessment
What Are Antidepressants & How Do They Work?
Antidepressants are a large and diverse group of medications for depression that aim to reduce the signs and symptoms of any depressive disorder. The goal of an antidepressant is to peel away the effects of depression, so the person will begin to think, feel, and behave in ways that are no longer influenced by the condition, and they require a prescription.2
There are many types of antidepressants, many of which act differently on the body and the brain. The main types of antidepressants are:3
- Selective serotonin reuptake inhibitors (SSRIs). These medications work by systematically blocking neurons’ ability to reabsorb serotonin, so more of the wanted neurotransmitter is available to neighboring neurons.
 Some SSRI options include fluoxetine (Prozac), paroxetine (Paxil), sertraline (Zoloft), citalopram (Celexa) and escitalopram (Lexapro).
Some SSRI options include fluoxetine (Prozac), paroxetine (Paxil), sertraline (Zoloft), citalopram (Celexa) and escitalopram (Lexapro). - Serotonin and norepinephrine reuptake inhibitors (SNRIs). Rather than only blocking the reabsorption of serotonin, SNRIs impact norepinephrine as well. SNRIs include duloxetine (Cymbalta), venlafaxine (Effexor), desvenlafaxine (Pristiq) and levomilnacipran (Fetzima).
- Atypical antidepressants. These drugs are a group of medications that do not work like SSRIs or SNRIs, but still have impact on the serotonin and norepinephrine systems. Trazodone, vortioxetine (Trintellix), vilazodone (Viibryd) and bupropion (Wellbutrin) are examples of atypical antidepressants.
Additionally, there are some older antidepressants that are used less often due to a greater risk of severe side effects. They are as effective in the treatment of depression. These antidepressant classes include:1
- Tricyclic antidepressants (TCAs) like imipramine (Tofranil), nortriptyline (Pamelor), amitriptyline, and doxepin.
- Tetracyclics like mirtazapine (Remeron) and maprotiline (Ludiomil).
- Monoamine oxidase inhibitors (MAOIs) like tranylcypromine (Parnate), phenelzine (Nardil) and isocarboxazid (Marplan).
Antidepressants can treat much more than major depressive disorder or other types of depression. Prescribers may recommend many antidepressants for anxiety, OCD, chronic pain, or sleep problems.1
*These medications have a black box warning, the most serious warning from the FDA for the risk of suicidal thoughts and behaviors in certain people. Before starting any of these medications, you should talk with your doctor about these risks.
Do Antidepressants Work Immediately?
Experts in the field commonly believe that antidepressants do not work immediately. Instead, they need a period of about four to six weeks to begin producing the desired result.1,2,3
Another school of thought states that antidepressants do work immediately, but the person will not be able to notice the early differences most of the time. Even from the first day someone takes an antidepressant, the medication is active in the brain. Researchers have found that some patients have found some antidepressant effects even a few hours after using medications.4
Even from the first day someone takes an antidepressant, the medication is active in the brain. Researchers have found that some patients have found some antidepressant effects even a few hours after using medications.4
It is likely that both schools of thought have some merit. Antidepressants work in different manners at the neurotransmitter level and this may explain why effects can be seen in different timetables.
How Long Does It Take for Antidepressants to Work?
When starting a new medication, depression symptoms could alleviate in a matter of days, weeks, or months. In the more undesirable situations, they may never get better with that medication, and the person will have to trial others to get the wanted results.
Farrokh Alemi, PhD, Professor at George Mason University explains, “Symptom remission is usually defined as 50% reduction in symptoms of depression on the Hamilton scale. However, it’s unclear which symptom (if any) gets resolved first.
”
Here is a general timeline outlining when you might expect to see results from antidepressants: 1,4,5,6
- 1 Day – On the first day of taking an antidepressant medication, most people will feel nothing at all. Some will notice side effects like nausea or vomiting that could be mild.
- 1 Week – One week in, people are more likely to note some other side effects like sleeping problems, diarrhea, dry mouth, and sexual problems. The patient may not see any desired effects yet.
- 2 Weeks – After 14 days of treatment, people may see their initial side effects dissipate. They may notice some changes in their symptoms like changing energy levels or improving moods, or other people may see the differences first.
- 1 Month – When someone completes their first month of treatment more significant symptom reduction could occur. They might be inspired and more motivated.

- 3 Months – At 90 days into treatment, the full effects of the antidepressant will be active, so if the targeted symptoms are low, they should stay low. Three months in, people may also notice some weight gain, which could be a side effect or a sign that one’s appetite has returned.
- 6 Months – Nothing new is likely at six months, but if symptoms remain well-treated and this is the person’s first bout of depression, the prescriber could consider ending the medication.
- 1 Year – Just like at the six month mark, no new changes are expected at one year. It is another good opportunity to reevaluate the treatment to see if the plan should be adjusted or left unchanged.
- After 1 Year – The typical length of treatment with an antidepressant is one year, but many people use them longer. Some may feel like the medication has lost its effectiveness over time, but many could remain on the same dose for long periods.
This is a typical timeline, but there are always exceptions to the rule. People should always stay patient, be alert, and maintain communication with their prescriber to ensure safety.
Do Any Antidepressants Work Quicker than Others?
Researchers seeking better ways to treat depression are always looking for medications that work quicker in the body. Finding medications that have a rapid onset of antidepressant action (ROAA) is a worthwhile pursuit.
Some medications that might work faster than others include:5
- Escitalopram (Lexapro) and citalopram (Celexa) show decreased symptoms as early as two weeks into treatment.
- Olanzapine – Fluoxetine Combination. By combining fluoxetine (Prozac) with an antipsychotic medication, olanzapine (Zyprexa), patients could report relief within two weeks. This is not likely a medication that would be used as a first line treatment for mild or moderate cases of depression due to its higher side effect burden.
- Mirtazapine (Remeron). Compared to SSRIs, Remeron helped improve sleep, anxiety, and movement issues during the first two weeks of treatment.
One encouraging treatment with a ROAA is esketamine. Esketamine (Spravato) can help people feel better after just a single treatment. A patient is likely to report lower symptoms within two hours with results lasting as long as two week.5 Rather than a pill you take, esketamine is given as a nasal spray or IV invulsion. At this time, esketamine has to be administered in a physician’s office.
Researchers and clinicians continue seeking the best ways to manage depression. For this reason, they experiment with brain stimulation, like transcranial magnetic stimulation (TMS)) and (electroconvulsive therapy (ECT)), sleep deprivation, and hormone changes.5 Depending on the patient’s symptoms, these treatments may be viable.
*These medications have a black box warning, the most serious warning from the FDA for the risk of suicidal thoughts and behaviors in certain people. Before starting any of these medications, you should talk with your doctor about these risks.
Before starting any of these medications, you should talk with your doctor about these risks.
Popular Choices For Online Psychiatry
Talkiatry – In-network insurance with every major insurer. Free Assessment
Hims / Hers – Best For Affordability. Free Assessment
Brightside – Best For Anxiety and Depression. Free Assessment
Talkspace – Accepts Optum, Cigna, Aetna, and UnitedHealthCare. Learn More
According to 18 Best Online Psychiatrists of 2022 (updated on 8/5/2022), Choosing Therapy partners with leading mental health companies and is compensated for referrals by Talkiatry, Hims / Hers, Brightside, and Talkspace.
When to Expect Initial Improvement When Starting Antidepressants
As soon as one starts taking their medication, they should increase their awareness to notice any changes, including side effects or desired results. They should make their loved ones aware of their antidepressant, so that their friends and family can pay attention to any differences as well.
They should make their loved ones aware of their antidepressant, so that their friends and family can pay attention to any differences as well.
Some signs your antidepressants have started working may include:7
- Decreased feeling of hopelessness
- Better mood and irritability levels
- More balanced sleep and appetite
- More focus and better concentration
- Increased self-worth
- Fewer thoughts of self-harm and a decrease in suicidal ideation
- Higher energy and motivation
If all goes well, a person can expect these results between a few weeks and a few months after starting the medication.
When to Expect Maximum Benefits from Antidepressants
The maximum benefit from a medication is expected by two months of use. At that point, the full impact of the antidepressant will be experienced.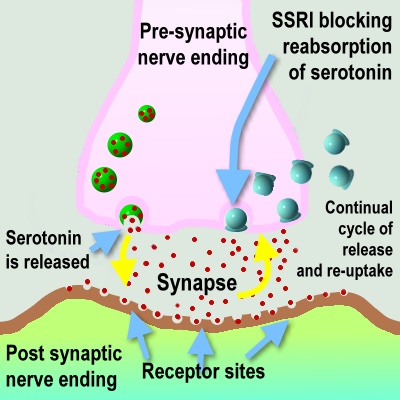
If a person is still not happy with the result, the treatment provider could decide to raise the dose, change the medication, or add another medication to boost the effects. The total time needed to find the best medication and the best dose can sometimes take months or years, so patience is always needed.
In fact, Alemi adds, “The majority of patients who receive antidepressants for the first time do not benefit from these medications.” He also notes that if this is the case, “You should not make sudden changes in medications or stop taking a medication unless advised by your clinician that it is safe to do so.”
Side Effects of Antidepressants
Some people experience side effects before depression relief, and many will feel no unwanted effects at all. Some side effects will quickly fade after a few days, and others will persist. Whatever the case, people should always consult with their prescriber about their effects and side effects of the antidepressant. Remember, the effects of depression could be much greater than the side effects of medication.1
Remember, the effects of depression could be much greater than the side effects of medication.1
Some common, early side effects of antidepressants include:1,3
- Nausea and vomiting
- Weight gain
- Diarrhea
- Being unable to fall asleep
- Sexual problems, like lower sexual interest and an inability to have sex
- Dry mouth
- Headaches
The side effects are often mild and tend to disappear as the patient’s body adapts.3 Younger people may experience some more troubling side effects of antidepressants.
Those under the age of 25 may notice increased depression and thoughts of suicide in the days or weeks after starting a new antidepressant.1 If you or someone you love is experiencing these troubling side effects, seek emergency medical services immediately or call 9-1-1.
What Causes Variability in Individual Response Time?
Much of antidepressant use is a mystery. No one is exactly sure how antidepressants work, why they don’t work for some people, and why they work slower in some than others.
In the simplest terms, the ways a person’s body absorbs and processes the medication will dictate the speed and level of effect. A person may not be able to change this, but exploring options with pharmacogenetic testing may offer insights.
How to Get the Most Out of Your Antidepressant Medication
Effective treatment for depression is multifaceted. If someone wants the best results, they will need to follow through with new routines, lifestyle changes, and all recommendations.
Alemi states that first and foremost, you should “Begin by making sure that you are taking the right medication. The Health Informatics Program of George Mason University has created a free site to help individuals learn more about potential antidepressants that could be right for them. ” This should always be discussed with a prescribing doctor, but may be helpful for some.
” This should always be discussed with a prescribing doctor, but may be helpful for some.
Additionally, Alemi adds two other ways to make sure you’re getting the most out of your antidepressants; “Make sure your medication consistently and do not stop until passage of time or the medications lead to remission of symptoms. Then exercise. Exercise has been shown to be as effective as antidepressants for some patients.”
Some additional ways to ensure you’re getting the most out of your antidepressant medication include:3
- Stay patient and realize it will take some time for your body to feel the full results of the medication
- Take the correct dose of your medication around the same time each day
- The side effects may get better over time, so wait out the mild symptoms
- Talk about dose or medication changes with your prescriber to know what the next step is
- Start or increase therapy and try using options like cognitive behavioral therapy (CBT) for depression
- Avoid alcohol and other drugs while using your antidepressant to avoid distorting the results
- Boost your physical health with better diet, exercise, and sleep routines
You can take all the right steps and your antidepressant may not work well for you. It doesn’t mean there is anything wrong with you. It only means that you have not found your best match yet.
It doesn’t mean there is anything wrong with you. It only means that you have not found your best match yet.
How Long Should You Take Antidepressants?
You should plan to take a new antidepressant for at least two month to study the effects and wanted results. You may only stop before this time if distressing or dangerous side effects emerge, and you should always consult with your doctor prior to doing so.
The duration of treatment will last at least six months and could go on indefinitely if you feel happy with the outcomes. Always discuss possible medication changes with your prescriber to understand the risks and benefits of changes.1
When Antidepressants Are Prescribed for Other Issues
Many people will use antidepressants to address depression, anxiety, or a combination of depression and anxiety. Whether you are using the medication for anxiety, for depression, or for other needs, the timeline will be consistent. Most effects will be noted between four to six weeks after the first dose.
Most effects will be noted between four to six weeks after the first dose.
Questions to Ask Your Health Team About Antidepressants
You never want to take medication without a good understanding of what it is and how it works in your system. Having this basic information can help make you aware of the risks and perceptive of any changes.
Questions to ask your care team about depression treatment and antidepressants include:1,3
- How do you know which antidepressant is right for me?
- How long will it take to work?
- What changes can I expect and what happens if I don’t notice any changes?
- What common side effects should I look out for?
- Can I mix different medications?
- Can I use alcohol or other drugs with this medication?
- What happens if I miss a dose?
- How much will this drug cost?
- Can I use this medication if I am pregnant or breastfeeding?
Asking questions and listening intently is always helpful, but your prescriber might not know all the answers.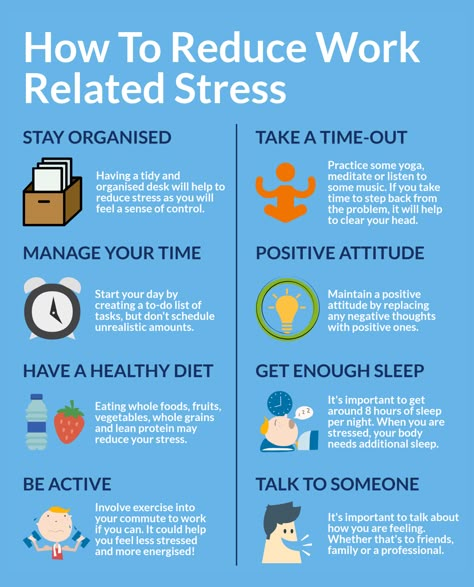 The science of antidepressants is not exact, and one of the most important and helpful questions to ask, Alemi says, is, “What is the evidence that this medication will work for me.”
The science of antidepressants is not exact, and one of the most important and helpful questions to ask, Alemi says, is, “What is the evidence that this medication will work for me.”
Final Thoughts
Seeing immediate improvement in your symptoms from an antidepressant is rare, but be patient and aware of your condition to study the changes. Even if the process takes some trial and error, the benefits of an antidepressant could be life-changing.
Additional Resources
Education is just the first step on our path to improved mental health and emotional wellness. To help our readers take the next step in their journey, Choosing Therapy has partnered with leaders in mental health and wellness. Choosing Therapy may be compensated for referrals by the companies mentioned below.
Brightside Health (Online Psychiatry) – If you’re struggling with serious mental health issues, finding the right medication can make a difference. Brightside Health treatment plans start at $95 per month. Cigna and Aetna accepted. Following a free online evaluation and receiving a prescription, you can get FDA approved medications delivered to your door. Free Assessment
Brightside Health treatment plans start at $95 per month. Cigna and Aetna accepted. Following a free online evaluation and receiving a prescription, you can get FDA approved medications delivered to your door. Free Assessment
Hims / Hers (Online Psychiatry) – If you’re living with anxiety, depression, OCD, or PTSD finding the right medication match may make all the difference. Get FDA approved medication prescribed by your dedicated Hims / Hers Healthcare Provider and delivered right to your door. Plans start at $25 per month (first month). Get Started
BetterHelp (Online Therapy) – BetterHelp has over 20,000 licensed therapists who provide convenient and affordable online therapy. BetterHelp starts at $60 per week. Complete a brief questionnaire and get matched with the right therapist for you. Get Started
Choosing Therapy partners with leading mental health companies and is compensated for referrals by Brightside, Hims / Hers, and BetterHelp
7 sources
Choosing Therapy strives to provide our readers with mental health content that is accurate and actionable. We have high standards for what can be cited within our articles. Acceptable sources include government agencies, universities and colleges, scholarly journals, industry and professional associations, and other high-integrity sources of mental health journalism. Learn more by reviewing our full editorial policy.
We have high standards for what can be cited within our articles. Acceptable sources include government agencies, universities and colleges, scholarly journals, industry and professional associations, and other high-integrity sources of mental health journalism. Learn more by reviewing our full editorial policy.
-
MedlinePlus. (2022, January 31.) Antidepressants. Retrieved from https://medlineplus.gov/antidepressants.html
-
UNC Health Talk. (2020, June 23.). 8 Things You Might Not Know About Antidepressants. Retrieved from https://healthtalk.unchealthcare.org/8-things-you-might-not-know-about-antidepressants/
-
Mayo Clinic. 2019, December 31). Antidepressants: Selecting one that’s right for you. Retrieved from https://www.mayoclinic.org/diseases-conditions/depression/in-depth/antidepressants/ART-20046273?p=1
-
Harmer, C., Favaron, E., et al. (2009, September). Effect of Acute Antidepressant Administration on Negative Affective Bias in Depressed Patients.
 American Journal of Psychiatry. Retrieved from https://ajp.psychiatryonline.org/doi/full/10.1176/appi.ajp.2009.09020149
American Journal of Psychiatry. Retrieved from https://ajp.psychiatryonline.org/doi/full/10.1176/appi.ajp.2009.09020149 -
Machado-Vieira, R., Baumann, J., Wheeler-Castillo, C., Latov, D., Henter, I. D., Salvadore, G., & Zarate, C. A. (2010). The Timing of Antidepressant Effects: A Comparison of Diverse Pharmacological and Somatic Treatments. Pharmaceuticals. Retrieveved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3991019/
-
Posternak, M.A. (2005, October). How Quickly Do Antidepressants Begin to Work? Psychiatric Times. Retrieved from https://www.psychiatrictimes.com/view/how-quickly-do-antidepressants-begin-work
-
American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders (5th ed.). Arlington, VA.
If you are in need of immediate medical help:
Medical
Emergency
911
Suicide Hotline
800-273-8255
Guide to antidepressants: how do they work?
Treatment
Depression of the Health Guardian Guest
Davydovspid.
 p.Center
p.Center 13 JULY 2022
200421
AIDS
"Species Center" is nervous about depression, and, unfortunately, for many of our readers this is a pressing problem. This time, with the help of Maria Danina, Candidate of Psychological Sciences, our authors have compiled a short guide to antidepressants. Their types, principles of operation and device. All basic concepts in one text.
Depression is quite common: according to WHO, more than 300 million people of all ages and genders suffer from it worldwide.
As defined by the American Psychiatric Association, this serious illness can take many forms, vary in severity from person to person, and coexist with other conditions that cause similar symptoms, such as anxiety disorders.
Since the causes of depression are associated with disorders of the brain, it is useless to call on patients with depression to "pull themselves together" - its symptoms cannot be overcome by willpower, just as it is impossible to influence the brain by willpower.
“Mood is our subjective experience, that is, what we can become aware of and what we can give an account of. At the heart of any psychological phenomenon are complex and multi-level processes that take place in our nervous system. In particular, neurochemical ones,” explains Maria Danina, senior researcher at the Laboratory of the Scientific Foundations of Psychotherapy, Candidate of Psychological Sciences.
According to her, according to the monoamine theory, three different monoamine neurotransmitters contribute to depressive symptoms. Moreover, neurotransmitters do not "trigger" the disease by themselves, but affect certain processes, which, in fact, lead to depression.
First, it is dopamine, which is involved in the motivation system. A lack of dopamine can lead to anhedonia—that is, the inability to experience pleasure.
Secondly, it is norepinephrine. It is involved in the regulation of our daily activities. Its deficiency is associated with psychomotor retardation (when a person begins to move and speak more slowly than usual).
And thirdly, serotonin. Which is involved in the control of the sensitivity of the pain system, suppresses pain signals and negative emotions.
Lack of serotonin leads to increased pain, negative emotions and anxiety. In addition, due to a lack of serotonin, obsessive states develop, associated with constantly recurring thoughts about the past and the causes of one's current state, which are difficult to get rid of - psychiatrists call this rumination.
“In addition to lowering the level of neurotransmitters, other groups of biologically active substances, such as glucocorticoids, can contribute to depression,” notes Maria Danina. - Let's say that the level of the famous "stress hormone" cortisol also increases with depression - and this in turn leads to a lack of dopamine. Monoamine levels can be affected by thyroid hormones and the sex hormones estrogen and progesterone.”
However, many factors can trigger clinical depression, such as hereditary predisposition, low self-esteem, difficult life circumstances, severe stress, and chronic diseases. And therefore, we cannot “shift all the blame” only on violations in the brain, emphasizes Maria Danina.
And therefore, we cannot “shift all the blame” only on violations in the brain, emphasizes Maria Danina.
Life in the “serotonin pit”
An alternative to the monoamine theory, which from the point of view of many scientists can no longer be considered the main one, is the biopsychosocial model of depression. In accordance with it, the development of the disease is influenced not only by biological, but also by psychological factors.
“A person may experience loss (grief) or severe frustration of their needs (stress). As a result, his neurochemistry also changes,” explains Danina. “But this is the so-called normal “mourning process.” Doctors talk about reactive depression only if, even after months, a person continues to experience all the same unpleasant sensations, and over time, his condition only worsens.
In some people, however, the functional characteristics of their neurons make them more prone to depression. Such patients "start" the process does not require external circumstances. And their depression has a non-reactive "endogenous" character.
Such patients "start" the process does not require external circumstances. And their depression has a non-reactive "endogenous" character.
In both cases, in addition to psychotherapy, doctors prescribe antidepressants, that is, drugs that can affect neurotransmitters in the brain, as a medical aid.
There are five classes in total. Each of which affects the brain in its own way.
1. Selective serotonin reuptake inhibitors (SSRIs).
SSRI drugs increase serotonin levels. This helps to more accurately regulate mood and gradually overcome moderate to severe depression. These drugs do their job by "forbidding" neurons to absorb serotonin from the synaptic gap between neurons. As a result, neurons are able to communicate better.
SSRIs have fewer side effects than other classes of antidepressants. For example, in case of an overdose, they do not disrupt cardiac conduction and do not lead to convulsions.
However, the side effects are still there and quite serious - from increased suicidal thoughts to sexual dysfunction, drowsiness, dry mouth, dizziness and headache.
In addition, all drugs that increase the level of serotonin in the brain can cause serotonin syndrome - a situation where the neurotransmitter becomes too much.
Serotonin and signal transmission through nerve cells.In serotonin syndrome, the person becomes overexcited, restless, sweats and has an increased heart rate. That is why being treated simultaneously with two antidepressants that increase serotonin levels is dangerous to life and health.
2. Selective serotonin and norepinephrine reuptake inhibitors (SNRIs).
SNRIs work in much the same way as SSRIs, with one difference. Drugs “forbid” neurons to absorb not only serotonin, but also norepinephrine, a neurotransmitter that is involved in the regulation of emotions and thought processes.
And since norepinephrine works in close conjunction with serotonin and dopamine, SNRIs are thought to increase attention, focus, and improve memory.
The indications and side effects of SNRIs are very similar to those of SSRIs. There are few advantages of this class of drugs over SSRIs, but for some patients they are better suited.
There are few advantages of this class of drugs over SSRIs, but for some patients they are better suited.
3. Atypical antidepressants.
This class includes drugs with different modes of action that have only one thing in common - these drugs are not like SSRIs and SNRIs.
Although some drugs in this class also "prohibit" neurons from taking up serotonin, like reuptake inhibitors, some of them can act on receptors for other neurotransmitters. This allows you to fine-tune the sensitivity of neurons to one or another substance.
It is worth noting that the components of some atypical antidepressants - say, bupropion - are listed in the note to the list of psychotropic substances subject to control in the Russian Federation. And although this tool is approved by reputable international medical organizations - for example, the US Food and Drug Administration (FDA), it cannot be legally purchased in Russia.
The side effects of this class of drugs depend on the specific drug. For example, some atypical antidepressants make you sleepy, while others, on the contrary, invigorate. To choose the right medicine, the doctor must take into account the peculiarities of the legislation, individual symptoms and the patient's health status.
For example, some atypical antidepressants make you sleepy, while others, on the contrary, invigorate. To choose the right medicine, the doctor must take into account the peculiarities of the legislation, individual symptoms and the patient's health status.
4. Tricyclic antidepressants (TCAs).
All drugs in this class are thought to increase the levels of norepinephrine and serotonin in the brain, much like SNRIs do.
But TCAs have a very important difference - they are able to act on brain receptors that bind to other substances. In overdose, this leads to severe side effects, such as seizures and complete heart block. And although TCAs are quite effective, drugs from this group today are trying to use as little as possible.
5. Monoamine oxidase inhibitors (MAOIs).
This class of drugs "turns off" monoamine oxidase, an enzyme that breaks down norepinephrine, serotonin, and dopamine in the brain. As a result, neurotransmitters are not destroyed and remain in the synaptic cleft for a long time.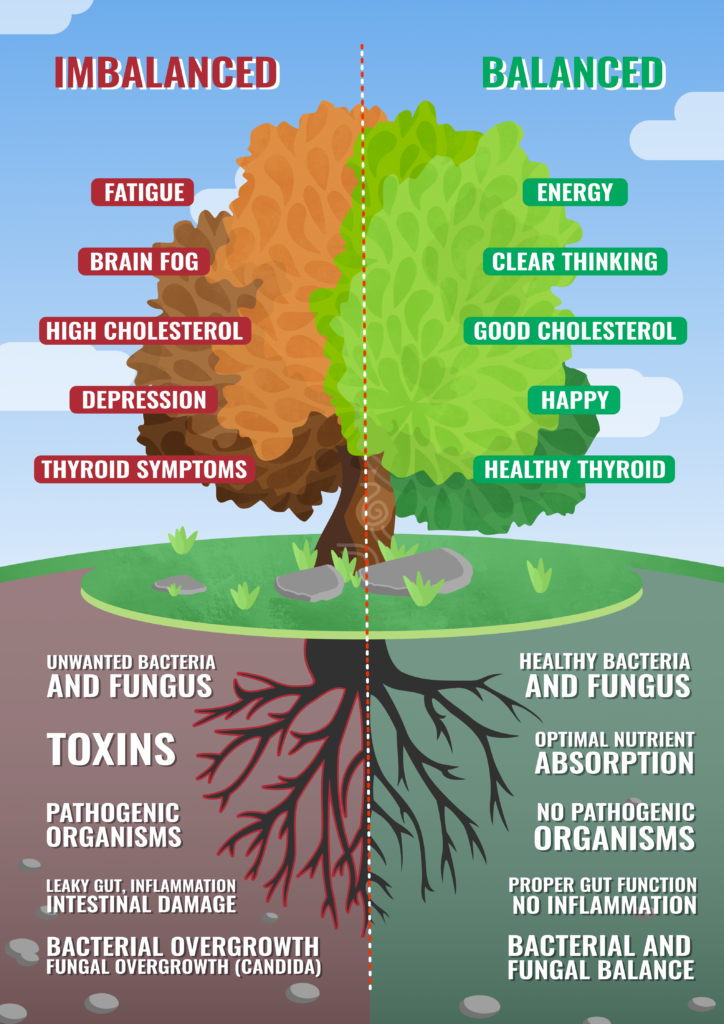
Unfortunately, MAOIs have many side effects, including high blood pressure, weight gain, swelling, sexual dysfunction, and suicidal ideation. So today, drugs of this class are used only under strict medical supervision and as a last resort - if other antidepressants have not helped.
Is it possible to do without antidepressants?
In medicine, there is the concept of a balance of benefits and harms. This is exactly what the old medical saying about medicines says, which "cure one thing - cripple another." When deciding to prescribe an antidepressant (or any other powerful drug), the doctor always thinks about whether it will benefit a particular patient.
related
Society
"You will burn in paradise!" Is depression really permanent?
- DepressionMedicineRussia
Of course, antidepressants are drugs with serious side effects, the abuse of which will not lead to anything good. However, this does not mean that the life of a person with depression without antidepressants will be any better.
However, this does not mean that the life of a person with depression without antidepressants will be any better.
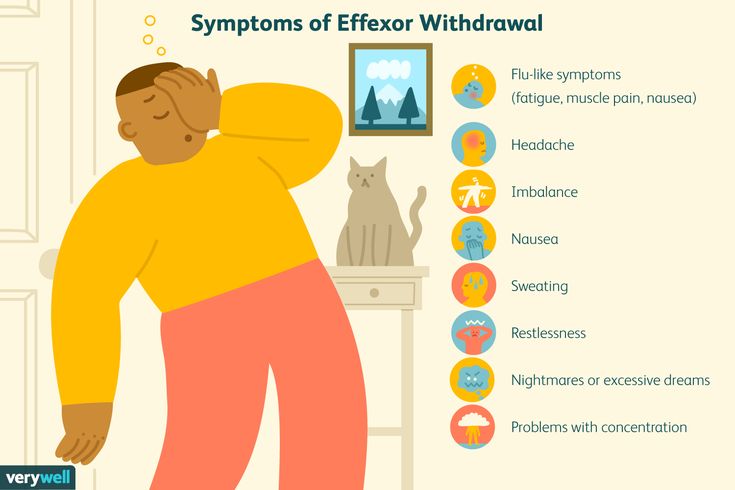
What happens if you stop taking the antidepressants prescribed by your doctor? The biggest risk is the return of depression. Moreover, 80% of patients who abruptly stop taking antidepressants develop a withdrawal syndrome. This condition appears within a few days after discontinuation and can last up to two weeks.
From a medical point of view, it is not too dangerous, but the sensations can be quite unpleasant.
Withdrawal symptoms can be divided into four groups:
- gastrointestinal: nausea, vomiting, diarrhea and abdominal cramps;
- somatic: headaches, lethargy and sweating;
- sleep-related: insomnia or excessive sleepiness, nightmares;
- affective: restlessness, agitation and bad mood.
To avoid withdrawal syndrome, the physician should gradually reduce the dose of antidepressants. This may take several weeks or even several months.
This may take several weeks or even several months.
Moreover, not only giving up antidepressants on your own, but also “prescribing” them to yourself without consulting a specialist is harmful.
“If you have symptoms of depression that do not go away for more than two weeks, this is a reason to consult a psychiatrist. The sooner the better, because early treatment gives a better prognosis,” Maria Danina sums up.
Doctors sometimes have to try several different antidepressants to find the right one for you. But it will not be possible to do without a specialist: only during a personal examination, the doctor can confirm the diagnosis and prescribe treatment, she emphasizes.
Where to go for depression?
There are several exits:
- neuropsychiatric dispensary at the place of residence (free of charge),
- psychiatric hospital (free of charge),
- private clinic (extra charge),
- private doctor (for a fee).
Of all the options described for the treatment of depression, the last three options are preferred.
Also, whether you have a confirmed diagnosis of depression, are on medication, or only suspect you have an illness, you may need support - informational or emotional.
At the time of publication of the article for people who suspect depression, there are:
- 24-hour hotline of the Moscow Service for Psychological Assistance to the Population: from a landline for Moscow residents - 051, free of charge; from a mobile phone - 8-495-051 *, only the services of a telecom operator are paid according to the tariff plan.
- Emergency medical and psychological assistance in crisis situations - (495) 205-05-50.
- Emergency psychological help - (495) 575-87-70.
- Hotline of the Psychological Assistance Ministry of Emergencies of Russia - (499) 216-50-50.
Subscribe to the AIDS.Center channel in Yandex.Zen
DepressionHealthcareSciencelet's be friends?
- read
- read
- join
- read
read also
Stop Communication for Mental Health Society.
 Understanding when to break up
Understanding when to break up - PsychologyHarm reduction
SocietyWon't my mother leave me?: how women deal with HIV stigma
- HIVPrEPDiscriminationWomenN=NPrevention
EpidemicDigest: what discoveries in the field of HIV were reported by the scientific media at the beginning of November what used to be punitive psychiatry. In fact, psychiatry is a deep science with a rich history. The article talks about drugs that can save our mental health, as well as today's views on what human mental health is and why we can improve it with the help of pharmacological drugs.
Part one, in which we look with amazed children's eyes and do not understand anything at all
There have always been many questions about antidepressants. Unlike "ordinary" medicines, they cannot be understood with the mind, you just need to believe. For example, all antidepressants begin to work only by the second week of taking. Traditionally, guidelines explain this by saying that "during this time, the drug accumulates." But what does "accumulate" mean? After all, the drug either works immediately or does not work at all. All other psychotropic substances act almost immediately. Sleeping pills act immediately. Tranquilizers act immediately. Antipsychotics, mood stabilizers, anticonvulsants, stimulants - they all begin to act quickly. And "stubborn" antidepressants - only after two weeks. The question is why?
Traditionally, guidelines explain this by saying that "during this time, the drug accumulates." But what does "accumulate" mean? After all, the drug either works immediately or does not work at all. All other psychotropic substances act almost immediately. Sleeping pills act immediately. Tranquilizers act immediately. Antipsychotics, mood stabilizers, anticonvulsants, stimulants - they all begin to act quickly. And "stubborn" antidepressants - only after two weeks. The question is why?
For an explanation of some terms from the field of psychopharmacology, see the Glossary at the end of the article. - Ed.
Figure 1 Advertisement for Thorazine (US trade name for chlorpromazine) recommends the drug for schizophrenic delusions and hallucinations.
Antidepressants improve the emotional background of patients with depression and do not affect the mood of healthy people. This not normal. If a substance has a psychoactive effect, it has the same effect on both pathological and physiological processes. If a sleeping pill is given to a person suffering from insomnia, he will fall asleep. And if you give sleeping pills to a healthy person, he will fall asleep in the same way. If an anxious and agitated patient is given a benzodiazepine tranquilizer, then the person will calm down and calm down. What if it's for an ordinary person? The same thing - a person will calm down and calm down. The "evil old" classic antipsychotics (the same chlorpromazine - "Aminazine") are still indispensable in acute psychoses: in fact, they have a carpet bombing effect on the rebellious brain, stopping mental activity through a break in dopamine transmission.
If a sleeping pill is given to a person suffering from insomnia, he will fall asleep. And if you give sleeping pills to a healthy person, he will fall asleep in the same way. If an anxious and agitated patient is given a benzodiazepine tranquilizer, then the person will calm down and calm down. What if it's for an ordinary person? The same thing - a person will calm down and calm down. The "evil old" classic antipsychotics (the same chlorpromazine - "Aminazine") are still indispensable in acute psychoses: in fact, they have a carpet bombing effect on the rebellious brain, stopping mental activity through a break in dopamine transmission.
And if a healthy person is bound and stabbed with antipsychotics, then the same thing will happen to his mental processes - the brain will turn into a scorched desert. But with antidepressants, the picture is completely different. They have an effect on a depressive mood background, but not on a normal one. A healthy person will only experience side effects, but no change in consciousness. So how does the pill know which person is depressed and which is not?
So how does the pill know which person is depressed and which is not?
A key symptom of depression is decreased mood. This in itself is not a problem: there are a lot of substances that quickly and guaranteed to improve mood - for example, a 40% solution of ethyl alcohol or psychostimulants, and they will not work in two weeks, but from the very first dose. Why then does medicine not use them? The fact is that they absolutely do not help with depression: neither alcohol nor amphetamines have an antidepressant effect, no matter what people say. And antidepressants - such as serotonin reuptake inhibitors Prozac, Zoloft, Paxil, Cipramil - help. Why?
Molecular basis of psychoses
An increase in the flow of dopamine and, to a lesser extent, serotonin is associated with the development of psychoses. According to the dopamine hypothesis of schizophrenia, the antipsychotic effect of antipsychotics is due to their ability to block dopamine receptors. However, since there are many varieties of these receptors in the brain and they perform a wide variety of functions, it is impossible to completely drown them out, as classic antipsychotics do (chlorpromazine, haloperidol, chlorprothixene and others), - there will be a lot of unpleasant side effects. Therefore, modern atypical antipsychotics selectively block some types of dopamine and serotonin receptors, and they have much fewer side effects.
Therefore, modern atypical antipsychotics selectively block some types of dopamine and serotonin receptors, and they have much fewer side effects.
Symptoms of depression
The main symptom of clinical depression (or major depressive disorder ) is a persistent decrease in emotional background, not just a "bad mood" that any person can have. Clinical depression is a disease that has clear criteria and is described by a whole bunch of symptoms. Depression manifests itself in a decrease in mood, feelings of guilt and hopelessness, loss of interest and pleasure, a decrease in energy, and as a result in increased fatigue and a decrease in activity, all of which should persist for at least two weeks.
Monoamine oxidase (MAO)
This is an enzyme involved in the destruction of monoamines (more precisely, the catabolism of monoamines by oxidative deamination). Monoamines include a mass of endogenous hormones and neurotransmitters, including all of which we are interested in: dopamine, adrenaline, norepinephrine, serotonin and histamine; as well as exogenous psychoactive substances (for example, phenylethylamine and narcotic substances derived from it).
MAO is one of the key enzymes of the human brain, and there are about forty related proteins in the family of monoamine receptors. If you block MAO, monoamines will stop being destroyed and begin to accumulate in the synaptic transmission system, which is not always good. Therefore, even modern selective MAO inhibitors - very powerful antidepressants - are quite dangerous to use and are allowed only in a hospital setting, where there is constant monitoring and control over the patient's condition.
Part two, in which we ask for advice from the spirits of our ancestors, but instead listen to boring old man's tales about the affairs of bygone days
Where did psychopharmacology come from? It dates back to 1876, when BASF invented methylene blue. This is the first substance from the group of phenothiazines, but then this was not yet suspected. Methylene blue is a very popular molecule. For example, pyoctannin - a 1-2% solution of methylene blue - is known to us as medical blue, although it has now been replaced by brilliant green, yellow iodine and colorless hydrogen peroxide. Even methylene blue was once treated for malaria, carbon monoxide poisoning, insecticides were obtained from it and used to treat worms in veterinary medicine. In 1883, phenothiazine itself was obtained from diphenylamine. Phenothiazine is the biblical Adam, from which twelve tribes of various useful substances have grown. Since the beginning of the 20th century, its derivatives have been used in veterinary medicine as an anthelmintic. Since the 30s, they began to try it as an anti-allergic agent, and in 19In 1947, promethazine was invented - one of the first antihistamines, along with Dimedrol discovered in 1943. These medicines are still used today.
Even methylene blue was once treated for malaria, carbon monoxide poisoning, insecticides were obtained from it and used to treat worms in veterinary medicine. In 1883, phenothiazine itself was obtained from diphenylamine. Phenothiazine is the biblical Adam, from which twelve tribes of various useful substances have grown. Since the beginning of the 20th century, its derivatives have been used in veterinary medicine as an anthelmintic. Since the 30s, they began to try it as an anti-allergic agent, and in 19In 1947, promethazine was invented - one of the first antihistamines, along with Dimedrol discovered in 1943. These medicines are still used today.
Promethazine had a pronounced sedative, suppressive effect, and surgeons began to use it in cocktails for anesthesia. In an attempt to enhance the inhibitory effect, in 1950 chlorpromazine was obtained, and in 1951 it fell into the hands of psychiatrists. Thus began the era of psychopharmacology: chlorpromazine is now known to us under the name of chlorpromazine. This is the very first neuroleptic, the gold standard of antipsychotic effect. Until now, the potency of all antipsychotics is measured through the "chlorpromazine equivalent", just like the potency of all tranquilizers is measured through the diazepam equivalent.
This is the very first neuroleptic, the gold standard of antipsychotic effect. Until now, the potency of all antipsychotics is measured through the "chlorpromazine equivalent", just like the potency of all tranquilizers is measured through the diazepam equivalent.
Parallel to this, in 1952, iproniazid, a drug for the treatment of tuberculosis, was invented. At that time, an open form of tuberculosis almost always meant a death sentence. Naturally, the prospect of imminent death caused some depression and sadness in patients. The situation was aggravated by the fact that the drugs did not help much, but the observation of phthisiatricians was all the more paradoxical that patients under the influence of iproniazid become inadequately happy. Iproniazid was the first ever antidepressant from the group of monoamine oxidase inhibitors; it is currently not used due to difficulties with its application in medical practice.
At the same time, in the 1950s, they began to actively look for other psychotropic drugs like chlorpromazine. So, in 1955, imipramine appeared - a tricyclic benzozepine analogue of chlorpromazine. It did not have an antipsychotic effect, but it turned out by chance that imipramine has an antidepressant effect. Thus began the era of tricyclic antidepressants, which before the advent of Prozac were by far the dominant group in their class, and now find the widest use. In 1961, a derivative of imipramine was registered under the name amitriptyline - the greatest antidepressant of all times and peoples. At 19In 1955, the first bezodiazepine tranquilizer, chlordiazepoxide (Elenium), was found by random selection, and in 1963 diazepam (Valium, Sibazon, Seduxen, Relanium) was obtained from it. So, quite by chance, the "big trinity" of psychopharmacology has developed - chlorpromazine, amitriptyline and diazepam. Antipsychotic, antidepressant and tranquilizer.
So, in 1955, imipramine appeared - a tricyclic benzozepine analogue of chlorpromazine. It did not have an antipsychotic effect, but it turned out by chance that imipramine has an antidepressant effect. Thus began the era of tricyclic antidepressants, which before the advent of Prozac were by far the dominant group in their class, and now find the widest use. In 1961, a derivative of imipramine was registered under the name amitriptyline - the greatest antidepressant of all times and peoples. At 19In 1955, the first bezodiazepine tranquilizer, chlordiazepoxide (Elenium), was found by random selection, and in 1963 diazepam (Valium, Sibazon, Seduxen, Relanium) was obtained from it. So, quite by chance, the "big trinity" of psychopharmacology has developed - chlorpromazine, amitriptyline and diazepam. Antipsychotic, antidepressant and tranquilizer.
Figure 2. In One Flew Over the Cuckoo's Nest, one of the main literary works of the beatnik and hippie culture, the action takes place in an American psychiatric hospital.
As for depression, before the first psychopharmacological revolution they were treated with drugs. Opiates were used until the late 50s, amphetamines until the mid-60s. Then amitriptyline and the company came into our world, and drugs gradually faded into the shadows due to their obvious side effects. Since the late 50s, it has become known about biogenic amines - norepinephrine, dopamine, serotonin. Since the late 1960s, there have been strong suspicions that serotonin is responsible for the development of depressive states. In the 70s, a biological theory was formed, according to which, during depression, the concentration of certain mediators in the synapse decreases in the brain. At 1977 fluoxetine was synthesized, but it passed the tests only by 1987, and went on sale in 1991 under the name "Prozac" (14 years from synthesis to the counter - compare with a year or two that took 50-60 -e). Thus, the world's first selective serotonin reuptake inhibitor appeared, which unleashed the second pharmacological revolution and made the Eli-Lilly company rich. Figure 3 shows a brief history of the development of antidepressants.
Figure 3 shows a brief history of the development of antidepressants.
Figure 3. A brief history of the development of antidepressants. The past decade has not brought revolutions in antidepressants. Although it is worth noting that licenses for all important drugs expired in the 2000s, and they began to be produced in generics and began to be widely used in Russian medicine. Meanwhile, a lot of things happened with the “neighbors” in the pharmacological reference book: “zero” is a revolution in atypical antipsychotics. Risperidone, Seroquel, Zyprexa - these names are not as well known to the general public as Prozac, but for the treatment of psychosis (primarily schizophrenia) this is a very big step.
Part three, in which we continue to not understand a single thing, but not in the way we used to understand, but in a different way, but then a diagram and a table appear in the narrative, which, as you know, calms down and increases the rating of trust in the text
Together, a number of reasons have been formulated for which depression develops. For example, the monoamine hypothesis postulates that a deficiency of certain neurotransmitters (primarily serotonin, but also norepinephrine and dopamine) is responsible for the characteristic psychiatric disturbances in depression.
For example, the monoamine hypothesis postulates that a deficiency of certain neurotransmitters (primarily serotonin, but also norepinephrine and dopamine) is responsible for the characteristic psychiatric disturbances in depression.
But the further facts did not fit into the theory. Many varieties of serotonin receptors - 7 types, 13 subtypes - made it difficult to explain why drugs with the same biochemical activity have a different effect on the patient's consciousness. The 5-HT receptor blocker 2A mirtazapine (rimeron) is an antidepressant, and the blocker of the same 5-HT 2A quetiapine (seroquel) is an atypical antipsychotic. But if serotonin receptor blockers are antidepressants, is it reasonable to assume that agonists will be depressants? No matter how. Many bad things can be said about serotonin receptor agonists - mescaline, psilocybin, LSD and the like - but they do not cause depression, that's for sure.
Serotonin receptors have a huge number of functions. Through them, a huge number of drugs and drugs realize their effect. And all this could somehow be ignored, if not for the fact that serotonin is not particularly involved in the formation of mood at all. The main excitatory neurotransmitter in the human brain is the amino acid glutamate. The main inhibitor is γ-aminobutyric acid (GABA), which is obtained from the same glutamate. Serotonin, dopamine, norepinephrine and other hormones perform auxiliary modulating function.
Through them, a huge number of drugs and drugs realize their effect. And all this could somehow be ignored, if not for the fact that serotonin is not particularly involved in the formation of mood at all. The main excitatory neurotransmitter in the human brain is the amino acid glutamate. The main inhibitor is γ-aminobutyric acid (GABA), which is obtained from the same glutamate. Serotonin, dopamine, norepinephrine and other hormones perform auxiliary modulating function.
By the mid-2000s, some mechanisms for the formation of emotions began to be clarified, and the monoamine theory began to quickly lose ground. At the same time, as can be seen from the table of biological theories of the development of depression, there is still no single view of the problem.
| Theory | Arguments for | Arguments against |
|---|---|---|
| Distribution of glutamate gear | The level of glutamate and glutamine in the prefrontal cortex reduced intravenous administration of ketamin (nmda receptors antagonist) causes antidepressant effects of dopamine receptor | |
| Reduced GABA transmission | Decreased GABA levels in plasma, cerebrospinal fluid, prefrontal and occipital cortex Antidepressants affect GABA transmission | GABA works at >30% of synapses in the brain, implying nonspecific action |
| Circadian rhythm disorder | Sleep deprivation and sleep light therapy have an antidepressant effect Many patients with depression suffer from depression body temperature and neuroendocrine secretion | Association between " clock genes" and depression is not detected |
| Endogenous opioid dysfunction | Agonists Δ-opioid receptors have an antidepressant effect on primates and increase the level of neurotrophin in the brain | Large-scale studies confirming such a relationship |
as well as: District nervous nervinomin, citizen , violation of thyroxine functions, disruption of the work of some “circuits” of the brain, etc. | ||
0219 neuroplastic theory , which has practically superseded the theory of biogenic amines at the present time. Its main postulate is that the formation of the emotional background (and, accordingly, all its pathological deviations) is not determined by the level of individual neurotransmitters, but is formed as a result of the combined activity of various parts of the brain. The interaction of these neuronal complexes is regulated by long-term potentiation (sustained increase in synaptic transmission between neurons), synaptic plasticity (change in the strength of interneuronal transmission) and excitotoxicity (damage and death of nerve endings during overactivation of glutamate receptors). It has been proven that during prolonged depression, the gray matter of the brain (the layer where the actual nerve cells are located) becomes thinner, the connectivity and branching of nerve endings decrease.
It turned out that all this functions, is regulated and maintained by special neurotrophin proteins (growth factors that ensure the development and viability of brain cells). There are many neurotrophins, but in the aspect of this article, we are mainly interested in neurotrophic growth factor (aka BDNF), which is involved in the formation of new connections between neurons; it is also effective in disorders characteristic of depressive and anxiety disorders. And its synthesis, in turn, is regulated by serotonin receptors. Therefore, serotonin-active antidepressants are effective in both depressive and anxiety states (Fig. 4).
There are many neurotrophins, but in the aspect of this article, we are mainly interested in neurotrophic growth factor (aka BDNF), which is involved in the formation of new connections between neurons; it is also effective in disorders characteristic of depressive and anxiety disorders. And its synthesis, in turn, is regulated by serotonin receptors. Therefore, serotonin-active antidepressants are effective in both depressive and anxiety states (Fig. 4).
Figure 4. Beyond the Monoamine Hypothesis , according to which the main cause of depression is a violation of serotonin or norepinephrine signaling in the brain. Serotonin (5-hydroxytryptamine, 5-HT; left half of the figure) and norepinephrine (right half of the figure), the main mediators of monoamine transmission, are secreted by presynaptic neurons. Serotonin is synthesized in them from tryptophan, and norepinephrine is synthesized from tyrosine with the participation of the corresponding hydroxylase enzymes. Both of these substances are stored in vesicles (vesicles) near the presynaptic membrane of the neuron, and when a signal arrives, they are secreted into the synaptic cleft. The normal interruption of the action of mediators in the gap between neurons occurs due to the reuptake of serotonin and norepinephrine by the corresponding transporter proteins, as well as through feedback (regulatory receptors that monitor the level of serotonin are involved here (receptors 5-HT 1A and 5-HT 1B ) or norepinephrine (α 2 -noradrenoreceptors)). In addition, monoamine oxidase A (MAO-A) works in the presynaptic neuron, which breaks down neurotransmitters and, consequently, regulates the number of synaptic vesicles.
Both of these substances are stored in vesicles (vesicles) near the presynaptic membrane of the neuron, and when a signal arrives, they are secreted into the synaptic cleft. The normal interruption of the action of mediators in the gap between neurons occurs due to the reuptake of serotonin and norepinephrine by the corresponding transporter proteins, as well as through feedback (regulatory receptors that monitor the level of serotonin are involved here (receptors 5-HT 1A and 5-HT 1B ) or norepinephrine (α 2 -noradrenoreceptors)). In addition, monoamine oxidase A (MAO-A) works in the presynaptic neuron, which breaks down neurotransmitters and, consequently, regulates the number of synaptic vesicles.
In a postsynaptic neuron, serotonin and norepinephrine each bind to their own type of G-protein coupled receptors that trigger adenylate cyclase (AC) and phospholipase C (PL-C). Both of these enzymes initiate signaling cascades involving cyclic adenosine monophosphate (cAMP) and inositol triphosphate (IF 3 ), respectively, multiplying the signal from the receptors and transmitting it to the cell nucleus.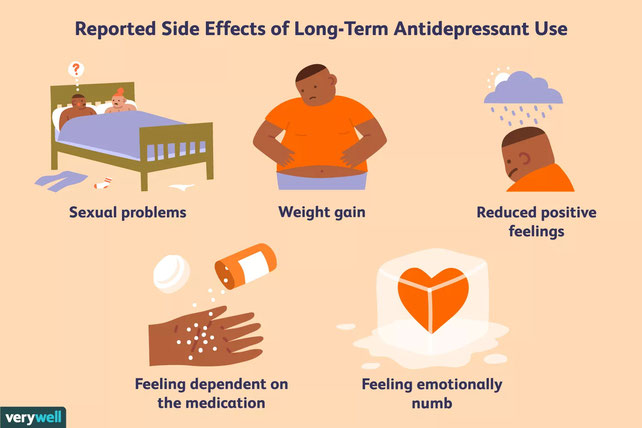
In support of the monoamine hypothesis, the following observations made in patients suffering from depression speak: 1) inhibition of tryptophan or tyrosine hydroxylases or exclusion of a source of tryptophan from the diet leads to a return of depression; 2) an increased frequency of mutations in the gene for the brain form of tryptophan hydroxylase; 3) an increase in the affinity of MAO-A to its substrates; 4) disruption of the "feedback" receptors 5-HT 1A and 5-HT 1B ; 5) serotonin transporter polymorphism; 6) disruption of postsynaptic GPCR receptors; and 7) decreased levels of cAMP, IF 3 , and nuclear factor COE (cAMP response element).
Antidepressants in various ways increase the release of serotonin (some also norepinephrine and dopamine) into the synaptic cleft, where it acts on serotonin receptors. The subsequent cascade of signaling reactions, amplifying many times, reaches the cell nucleus, where it activates the CEF transcription factor (cAMP response element-binding, CREB). COE triggers the expression of genes responsible for the synthesis of the neurotrophic factor, and the cell begins to produce BDNF, which then acts on its own TrkB receptor (type B tyrosine kinase receptor), which triggers the processes of synaptic plasticity, differentiation and resistance to damaging effects that we need so much.
COE triggers the expression of genes responsible for the synthesis of the neurotrophic factor, and the cell begins to produce BDNF, which then acts on its own TrkB receptor (type B tyrosine kinase receptor), which triggers the processes of synaptic plasticity, differentiation and resistance to damaging effects that we need so much.
It is possible that, in addition to the above, depression in the nervous tissue increases the concentration of pro-inflammatory cytokines that trigger neurotoxic processes (similar to autoimmune ones). And their activity is also suppressed by neurotrophic factors.
This is not a quick matter, and thus the long period of unfolding of the therapeutic effect of the antidepressant can be explained. Of course, this explanation is also lame, but it looks much more convincing.
Part four, in which the author supposed to tear off the covers and completely expose black magic, but it turned out as always
In 2009, an interesting article was published under the title “Why do antidepressants work with such a delay? Cognitive neuropsychological model of the action of antidepressants. The authors of this article express the paradoxical idea that antidepressants do not affect a person's mood at all. Through the release of neurotrophins and the suppression of interleukins, antidepressants restore the normal functioning of the limbic system and the prefrontal cortex. (It is these parts of the brain that are responsible for the formation of emotions, the balance of positive and negative emotional responses, for assessments and evaluative distortions / errors, as well as for the correlation of emotional and cognitive processes.) Research data are given that changes were observed in patients with depression from the first days the first week, i.e. much earlier than the effect of treatment was clinically manifested and the background of mood was restored. At this “pre-clinical” stage, a change in activity on fMRI was already detected, patients achieved better results in a battery of tests for face recognition (where it is proposed to interpret different expressions - neutral / happy / unhappy), and they had a decrease in the frequency and magnitude of cognitive distortions (such as the tendency to to negative thinking).
The authors of this article express the paradoxical idea that antidepressants do not affect a person's mood at all. Through the release of neurotrophins and the suppression of interleukins, antidepressants restore the normal functioning of the limbic system and the prefrontal cortex. (It is these parts of the brain that are responsible for the formation of emotions, the balance of positive and negative emotional responses, for assessments and evaluative distortions / errors, as well as for the correlation of emotional and cognitive processes.) Research data are given that changes were observed in patients with depression from the first days the first week, i.e. much earlier than the effect of treatment was clinically manifested and the background of mood was restored. At this “pre-clinical” stage, a change in activity on fMRI was already detected, patients achieved better results in a battery of tests for face recognition (where it is proposed to interpret different expressions - neutral / happy / unhappy), and they had a decrease in the frequency and magnitude of cognitive distortions (such as the tendency to to negative thinking).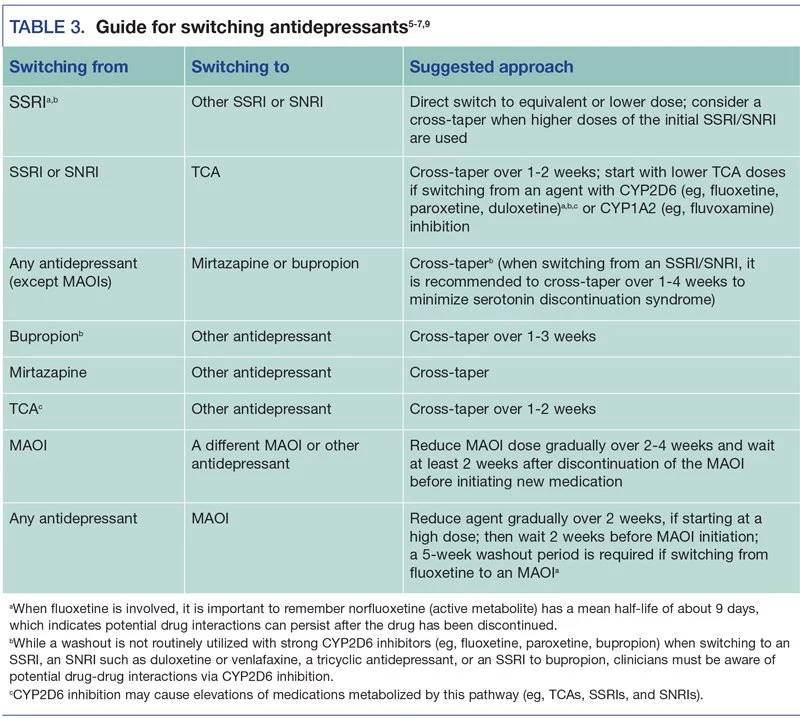 An improved understanding of the effect of antidepressants is shown in Figure 5.
An improved understanding of the effect of antidepressants is shown in Figure 5.
Figure 5. Scheme of action of antidepressants. , It turns out that not raising the mood leads to a decrease in emotional distortions (as is drawn on top of ). Everything is just the opposite - this reduction in emotional-cognitive distortions entails the restoration of mood ( at the bottom of ).
Why is the cognitive neuropsychological theory expressed in the article good? It is fully consistent with the biological views of the neuroplastic model and with the psychotherapeutic approach, since it explains at what point psychology and the drug come together, and why psychotherapy works as well (if not better) than pharmacotherapy. It resolves the "paradox of two weeks" because, according to these views, antidepressants are exactly the same drugs as all the others, and they begin their action immediately, from the very first doses. This concept also explains why drugs help the sick and do not affect the healthy. These ideas give insight into why different patients show different and difficult to predict responses to the same drug, because mood improvement is a distant and by no means necessary side effect.
These ideas give insight into why different patients show different and difficult to predict responses to the same drug, because mood improvement is a distant and by no means necessary side effect.
There is, however, one slippery place, which the authors of the mentioned article quickly slip through. The fact is that there is no reason to think that our abstract verbal thinking is somehow able to influence the neuronal processes of deep-lying parts of the brain. Rather, there are reasons to think that no, thinking does not affect emotions. But let's leave that for future researchers.
Epilogue, in which, if someone does not understand, we will summarize that there will be no answer, because this problem has no solution
There is still no absolute and generally accepted answer to the question of how and why antidepressants work. And more importantly, why they often don't work. And why are the reactions so individual and, at first glance, drugs that are identical in mechanism may or may not work. We are constantly narrowing the circle, and every time the answer seems to be found, it slips away again. Today we know more than yesterday, and yesterday we knew more than the day before yesterday. And still, the final decision is still very far away.
We are constantly narrowing the circle, and every time the answer seems to be found, it slips away again. Today we know more than yesterday, and yesterday we knew more than the day before yesterday. And still, the final decision is still very far away.
The article was originally published on the author's personal blog.
Glossary
- Psychopharmacology
- branch of medicine dealing with psychotropic drugs. Strictly speaking, the first were lithium preparations, which appeared in the 40s. But the generally accepted beginning of the era of psychopharmacology is the discovery of chlorpromazine (chlorpromazine).
- Antidepressants
- medicines used for depression and anxiety disorders. The best-known groups of them are tricyclic antidepressants (for example, amitriptyline) and selective serotonin reuptake inhibitors (for example, Prozac).
- Amitriptyline
- is the most popular and famous antidepressant. A classic representative of the group of tricyclic antidepressants.
 It is still in use.
It is still in use. - Fluoxetine (Prozac)
- the first selective serotonin reuptake inhibitor (SSRI). This name has become a household name and entered into mass use. Prozac is good, first of all, not even with high efficiency (in this regard, the old tricyclic antidepressants still surpass it), but with good tolerability. SSRIs have made treatment available to the mass outpatient. Of course, this immediately led to a lot of excesses and abuses.
- Antipsychotics
- drugs with antipsychotic activity. With reservations, A. can be considered a synonym for the word "neuroleptic", however, neuroleptics are a very clearly defined class, among them there is a so-called. "small antipsychotics" (they are also "behavior correctors"), which actually have antipsychotic activity to a very moderate extent.
- Antipsychotics
- potent antipsychotics.
- Aminazine
- the very first and most famous antipsychotic, the "gold standard".
 According to the strength of action, all other antipsychotics are measured in "chlorpromazine equivalent".
According to the strength of action, all other antipsychotics are measured in "chlorpromazine equivalent". - Phenothiazine
- is a heterocyclic compound whose derivatives are widely used in medicine as neuroleptics, antihistamines and antiarrhythmics.
- Normotimics
- drugs that stabilize the emotional state and mood, remove mood swings and return behavior to the boundaries of the norm (for example, lithium preparations).
- Psychotropic substances
- any chemical compound that affects mental processes. This phrase is often used as a synonym for drugs , but this is not entirely true. Psychopharmacological drugs are psychotropic substances. Caffeine (aka theine) is also a psychotropic substance.
- Stimulants
- Substances with psychostimulant effects, practically all of which are prohibited. The classic representative is amphetamine.
- Tranquilizers
- psychotropic drugs with sedative, inhibitory, depressant and hypnotic effects.
 In the classical sense, "major tranquilizers" are neuroleptics, but now tranquilizers are almost always understood as "small tranquilizers", that is, anti-anxiety, sedative and hypnotic drugs - first of all, this is a group of benzodiazepines (the most popular of which are phenazepam and diazepam) .
In the classical sense, "major tranquilizers" are neuroleptics, but now tranquilizers are almost always understood as "small tranquilizers", that is, anti-anxiety, sedative and hypnotic drugs - first of all, this is a group of benzodiazepines (the most popular of which are phenazepam and diazepam) . - Chlordiazepoxide (Elenium)
- the first benzodiazepine tranquilizer. At present, it is practically not used, since it has been supplanted by subsequent drugs.
- Diazepam
- is the most popular benzodiazepine. The most popular tranquilizer and psychotropic drug in general. A classic beznodiazepine tranquilizer, with all the pros and cons of its class.
- Acute psychoses
- rapidly developing disorders of mental activity. "Madness" or "madness" in the philistine sense.
- GABA (γ-aminobutyric acid)
- major human inhibitory neurotransmitter.
- fMRI (functional magnetic resonance imaging)
- made it possible to study the activity of living nervous tissue.
 The introduction of fMRI technologies has determined the progress of neuroscience in the last decade.
The introduction of fMRI technologies has determined the progress of neuroscience in the last decade. - The monoamine theory of the action of antidepressants
- suggests that their drug effect is achieved through a specific blockade of certain receptors for monoamines - serotonin, norepinephrine, dopamine. The neuroplastic model does not cross out the monoamine one, but evolutionarily develops and supplements it.
- Neuroplastic model
- is one of the hypotheses of the mechanisms of action of antidepressants. He suggests that their medicinal effect is achieved by influencing the processes of synaptic plasticity and the growth of neuronal endings.
- Megan E. Kozisek, David Middlemas, David B. Bylund. (2008). Brain-derived neurotrophic factor and its receptor tropomyosin-related kinase B in the mechanism of action of antidepressant therapies. Pharmacology & Therapeutics . 117 , 30-51;
- Eero Castrn, Tomi Rantamki.
 (). Neurotrophins in Depression and Antidepressant Effects. Novartis Foundation Symposium . 43-59;
(). Neurotrophins in Depression and Antidepressant Effects. Novartis Foundation Symposium . 43-59; - R.H. Belmaker, Galila Agam. (2008). Major Depressive Disorder. N Engl J Med . 358 , 55-68;
- Francesca Calabrese, Raffaella Molteni, Giorgio Racagni, Marco A. Riva. (2009). Neuronal plasticity: A link between stress and mood disorders. Psychoneuroendocrinology . 34 , S208-S216;
- Eero Castrén, Tomi Rantamäki. (2010). The role of BDNF and its receptors in depression and antidepressant drug action: Reactivation of developmental plasticity. Devel Neurobio . 70 , 289-297;
- Eero Castrén, Tomi Rantamäki. (2010). Role of Brain-Derived Neurotrophic Factor in the Aetiology of Depression. CNS Drugs . 24 , 1-7;
- C. J. Harmer, G. M. Goodwin, P. J.