Am i a schizophrenic
Diagnosis - Schizophrenia - NHS
There's no single test for schizophrenia and the condition is usually diagnosed after assessment by a specialist in mental health.
If you're concerned you may be developing symptoms of schizophrenia, see a GP as soon as possible. The earlier schizophrenia is treated, the better.
The GP will ask about your symptoms and check they're not the result of other causes, such as recreational drug use.
Community mental health team
If a diagnosis of schizophrenia is suspected, the GP should refer you to your local community mental health team (CMHT).
CMHTs are made up of different mental health professionals who support people with complex mental health conditions.
A member of the CMHT team, usually a psychiatrist or a specialist nurse, will carry out a more detailed assessment of your symptoms. They'll also want to know your personal history and current circumstances.
To make a diagnosis, most mental healthcare professionals use a diagnostic checklist.
Schizophrenia can usually be diagnosed if:
- you've experienced 1 or more of the following symptoms most of the time for a month: delusions, hallucinations, hearing voices, incoherent speech, or negative symptoms, such as a flattening of emotions
- your symptoms have had a significant impact on your ability to work, study or perform daily tasks
- all other possible causes, such as recreational drug use or bipolar disorder, have been ruled out
Related illnesses
Sometimes it might not be clear whether someone has schizophrenia. If you have other symptoms at the same time, a psychiatrist may have reason to believe you have a related mental illness, such as:
- bipolar disorder – people with bipolar disorder swing from periods of elevated moods and extremely active, excited behaviour (mania) to periods of deep depression; some people also hear voices or experience other kinds of hallucinations, or may have delusions
- schizoaffective disorder – this is often described as a form of schizophrenia because its symptoms are similar to schizophrenia and bipolar disorder, but schizoaffective disorder is a mental illness in its own right; it may occur just once in a person's life, or come and go and be triggered by stress
You may also be assessed for post-traumatic stress disorder, depression, anxiety and substance misuse.
Getting help for someone else
As a result of their delusional thought patterns, people with schizophrenia may be reluctant to visit their GP if they believe there's nothing wrong with them.
It's likely someone who has had acute schizophrenic episodes in the past will have been assigned a care co-ordinator. If this is the case, contact the person's care co-ordinator to express your concerns.
If someone is having an acute schizophrenic episode for the first time, it may be necessary for a friend, relative or another loved one to persuade them to visit their GP.
In the case of a rapidly worsening schizophrenic episode, you may need to go to the accident and emergency (A&E) department, where a duty psychiatrist will be available.
If a person who is having an acute schizophrenic episode refuses to get help, their nearest relative can request that a mental health assessment is carried out. The social services department of your local authority can advise how to do this.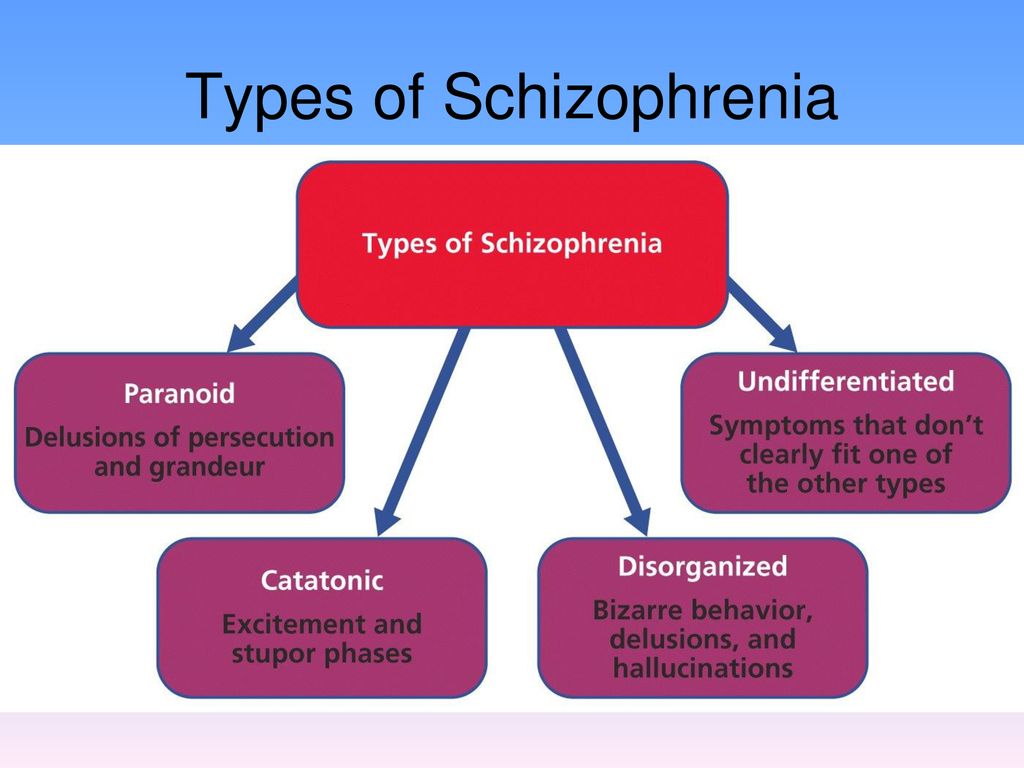 Find your local authority.
Find your local authority.
In severe cases, people can be compulsorily detained in hospital for assessment and treatment under the Mental Health Act (2007).
After diagnosis
If you or a friend or relative are diagnosed with schizophrenia, you may feel anxious about what will happen. You may be worried about the stigma attached to the condition, or feel frightened and withdrawn.
It's important to remember that a diagnosis can be a positive step towards getting good, straightforward information about the illness and the kinds of treatment and services available.
Diagnosing children and young people
Children and young people with a first episode of schizophrenia should be referred urgently to a specialist mental health service.
This should be either children and young people's mental health services (CYPMHHS) for those aged up to 17, or an early intervention service for those aged 14 years or over, that includes a consultant psychiatrist with training in children and young people's mental health.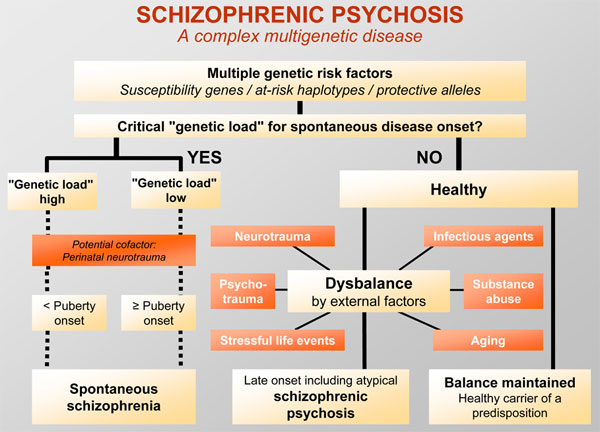
For more information, see the National Institute for Health and Care Excellence (NICE) guidelines on psychosis and schizophrenia in children and young people.
Page last reviewed: 11 November 2019
Next review due: 11 November 2022
Schizophrenia Test
Medically reviewed by Tiffany Taft, PsyD — By Psych Central Staff — Updated on February 4, 2021
Schizophrenia is a chronic mental health condition that affects a person’s thoughts, feelings, and behaviors.
It’s characterized by several symptoms, the most common being hallucinations or delusions that have no connection to reality, but feel real to the person experiencing them.
This schizophrenia quiz is for anyone who wants to see if they may have symptoms commonly associated with schizophrenia or a related condition. It takes most people less than 2 minutes to complete and will provide instant results.
Instructions
Answer the questions below honestly based on how you currently feel or have felt in the past month.
This quiz cannot replace diagnosis by a healthcare provider. If you believe you have symptoms of schizophrenia or another condition after taking this test, reach out to a qualified healthcare professional for a full evaluation.
This online screening is not a diagnostic tool. Only a trained medical professional, like a doctor or mental health professional, can help you determine the next best steps for you.
Common symptoms of schizophrenia
You may be diagnosed with schizophrenia if you experience 2 or more of the following symptoms for at least 1 month:
- delusions
- hallucinations
- incoherent speech, or speech that quickly switches from topic to topic with no thread between them
- severely disorganized or catatonic behavior
- any of the negative symptoms of schizophrenia
Schizophrenia has two main types of symptoms: positive and negative.
Delusions and hallucinations are the main characteristics of schizophrenia. These are positive symptoms.
These are positive symptoms.
A delusion is a fixed belief that doesn’t change, even when a person is given evidence the belief isn’t based in reality. An example of a delusion is that “everyone is out to get me.”
Hallucinations involve seeing, hearing, or feeling things that aren’t there. Examples include hearing voices that aren’t your own, or seeing people that aren’t actually in the room.
Hallucinations and delusions are called positive symptoms because they represent additional behaviors not generally seen in people without the condition. Negative symptoms can be seen as behaviors that are missing or underdeveloped.
Negative symptoms include:
- lack of emotional expression
- an inability to experience happiness
- difficulties planning or sticking with an activity like grocery shopping
- social withdrawal
Check out more about the symptoms of schizophrenia.
How is schizophrenia treated?
Schizophrenia is often managed with a combination of treatments, including medications and psychotherapy.
Symptoms of schizophrenia are often effectively treated with antipsychotic medications. Since there are many types of these drugs, you should reach out to your doctor about your options, their pros and cons, and how to manage any side effects that may occur.
Psychosocial treatment is also often recommended. This includes talk therapy and social skills training.
You may want to reach out to your doctor about programs in your area, and assistance in getting enrolled. Most insurance companies, if you have insurance, will cover some of these services.
Support groups can be another great way to get started and learn about additional resources. For example, the National Alliance on Mental Illness (NAMI) has a weekly support group for people with mental health conditions. You can find a group in your area on the NAMI homepage.
Learn more about the treatment options and approaches to schizophrenia.
What causes schizophrenia?
Schizophrenia is a complex mental health condition.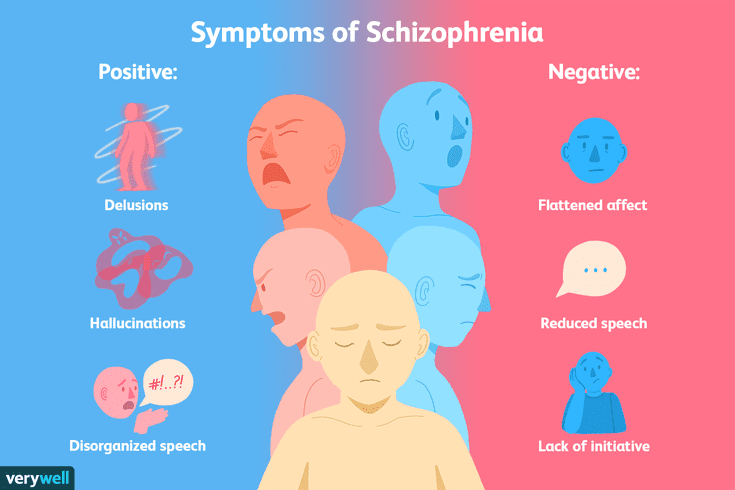 Its exact causes are unknown, but several things may play a role, including:
Its exact causes are unknown, but several things may play a role, including:
- genetics
- environmental triggers
- structural or chemical brain changes
- complications before or during birth
Most people develop schizophrenia in their late teens or early 30s.
Ready to start therapy? Our Find a Therapist resource may help.
Schizophrenia
Schizophrenia- Popular Topics
- Air pollution
- Coronavirus disease (COVID-19)
- Hepatitis
- Data and statistics »
- News bulletin
- The facts are clear
- Publications
- Find Country »
- A
- B
- C
- D
- E
- e
- ё 9000
- x
- C
- h
- Sh
9000 WHO in countries » - Reporting
- Regions »
- Africa
- America
- Southeast Asia
- Europe
- Eastern Mediterranean
- Western Pacific
- Media Center
- Press releases
- Statements
- Media messages
- Comments
- Reporting
- Online Q&A
- Developments
- Photo reports
- Questions and answers
- Update
- Emergencies "
- News "
- Disease Outbreak News
- WHO data »
- Dashboards »
- COVID-19 Monitoring Dashboard
- Basic moments "
- About WHO »
- CEO
- About WHO
- WHO activities
- Where does WHO work?
- Governing Bodies »
- World Health Assembly
- Executive committee
- Main page/
- Media Center /
- Newsletters/
- Read more/
- Schizophrenia
Key Facts
- Schizophrenia is a severe mental disorder that affects approximately 24 million people, or 1 in 300 people worldwide.
- Schizophrenia causes psychosis, is associated with severe disability, and can negatively affect all areas of life, including personal, family, social, academic and work life.
- People with schizophrenia are often subject to stigma, discrimination and human rights violations.
- Globally, more than two thirds of people with psychosis do not receive specialized mental health care.
- There are a number of effective care options for patients with schizophrenia that can lead to a complete recovery of at least one in three patients.
Symptoms
Schizophrenia is characterized by significant disturbances in perception of reality and behavioral changes such as:
- persistent delusions: the patient has a persistent belief in the truth of certain things, despite evidence to the contrary;
- persistent hallucinations: the patient hears, sees, touches non-existent things and smells non-existent smells;
- sensation of external influence, control or passivity: the presence in the patient of the sensation that his feelings, impulses, actions or thoughts are dictated from outside, put in or disappear from consciousness by someone else's will, or that his thoughts are broadcast to others;
- disorganized thinking, often expressed in incoherent or pointless speech;
- Significant disorganization of behavior, which manifests itself, for example, in the performance by the patient of actions that may seem strange or meaningless, or in an unpredictable or inappropriate emotional reaction that does not give the patient the opportunity to organization of their behavior;
- "negative symptoms" such as extreme poverty of speech, smoothness of emotional reactions, inability to feel interest or pleasure, social autism; and/or
- Extreme agitation or, on the contrary, slowness of movements, freezing in unusual postures.
People with schizophrenia often also experience persistent cognitive or thinking problems that affect memory, attention, or problem-solving skills.
At least one third of patients with schizophrenia experience complete remission of symptoms (1). In some, periods of remission and exacerbation of symptoms follow each other throughout life, in others there is a gradual increase in symptoms.
Scope and impact
Schizophrenia affects approximately 24 million people, or 1 in 300 people (0.32%) worldwide. Among adults, the rate is 1 in 222 (0.45%) (2). Schizophrenia is less common than many other mental disorders. Onset is most common in late adolescence and between the ages of 20 and 30; while women tend to have a later onset of the disease.
Schizophrenia is often accompanied by significant stress and difficulties in personal relationships, family life, social contacts, studies, work or other important areas of life.
Individuals with schizophrenia are 2-3 times more likely to die early than the population average (2). It is often associated with physical illnesses such as cardiovascular disease, metabolic disease, and infectious disease.
It is often associated with physical illnesses such as cardiovascular disease, metabolic disease, and infectious disease.
Patients with schizophrenia often become the object of human rights violations both within the walls of psychiatric institutions and in everyday life. Significant stigmatization of people with this disease is a widespread phenomenon that leads to their social isolation and has a negative impact on their relationships with others, including family and friends. This creates grounds for discrimination, which in turn limits access to health services in general, education, housing and employment.
Humanitarian emergencies and health crises can cause intense stress and fear, disrupt social support mechanisms, lead to isolation and disruption of health services and supply of medicines. All these shocks can have a negative impact on the lives of people with schizophrenia, in particular by exacerbating existing symptoms of the disease. People with schizophrenia are more vulnerable during emergencies to various human rights violations and, in particular, face neglect, abandonment, homelessness, abuse and social exclusion.
Causes of schizophrenia
Science has not established any one cause of the disease. It is believed that schizophrenia may be the result of the interaction of a number of genetic and environmental factors. Psychosocial factors may also influence the onset and course of schizophrenia. In particular, heavy marijuana abuse is associated with an increased risk of this mental disorder.
Assistance services
At present, the vast majority of people with schizophrenia do not receive mental health care worldwide. Approximately 50% of patients in psychiatric hospitals are diagnosed with schizophrenia (4). Only 31.3% of people with psychosis get specialized mental health care (5). Much of the resources allocated to mental health services are inefficiently spent on the care of patients admitted to psychiatric hospitals.
Available scientific evidence clearly indicates that hospitalization in psychiatric hospitals is not an effective treatment for mental disorders and is regularly associated with the violation of the basic rights of patients with schizophrenia. Therefore, it is necessary to ensure the expansion and acceleration of work on the transfer of functions in the field of mental health care from psychiatric institutions to the level of local communities. Such work should begin with the organization of the provision a wide range of quality community-based mental health services. Options for community-based mental health care include integrating this type of care into primary health care and hospital care. general care, setting up community mental health centres, outpatient care centres, social housing with nursing care and social home care services. Involvement in the care process is important the patient with schizophrenia, his family members and members of local communities.
Therefore, it is necessary to ensure the expansion and acceleration of work on the transfer of functions in the field of mental health care from psychiatric institutions to the level of local communities. Such work should begin with the organization of the provision a wide range of quality community-based mental health services. Options for community-based mental health care include integrating this type of care into primary health care and hospital care. general care, setting up community mental health centres, outpatient care centres, social housing with nursing care and social home care services. Involvement in the care process is important the patient with schizophrenia, his family members and members of local communities.
Schizophrenia management and care
There are a number of effective approaches to treating people with schizophrenia, including medication, psychoeducation, family therapy, cognitive behavioral therapy, and psychosocial rehabilitation (eg life skills education). The most important interventions for helping people with schizophrenia are assisted living, special housing and employment assistance. It is extremely important for people with schizophrenia and their families and/or caregivers to a recovery-centered approach that empowers people to participate in decisions about their care.
The most important interventions for helping people with schizophrenia are assisted living, special housing and employment assistance. It is extremely important for people with schizophrenia and their families and/or caregivers to a recovery-centered approach that empowers people to participate in decisions about their care.
WHO activities
steps are in place to ensure that appropriate services are provided to people with mental disorders, including schizophrenia. One of the key recommendations The action plan is to transfer the function of providing assistance from institutions to local communities. WHO Special Mental Health Initiative aims to further progress towards the goals of the Comprehensive Plan mental health action 2013–2030 by ensuring that 100 million more people have access to quality and affordable mental health care.
The WHO Mental Health Gap Action Program (mhGAP) is working to develop evidence-based technical guidelines, tools and training packages to scale up services in countries, especially in low-resource settings. The program focuses on a priority list of mental health disorders, including psychosis, and aims to strengthen the capacity of non-specialized health workers in as part of an integrated approach to mental health care at all levels of care. To date, the mhGAP Program has been implemented in more than 100 WHO Member States.
The program focuses on a priority list of mental health disorders, including psychosis, and aims to strengthen the capacity of non-specialized health workers in as part of an integrated approach to mental health care at all levels of care. To date, the mhGAP Program has been implemented in more than 100 WHO Member States.
The WHO QualityRights project aims to improve the quality of care and better protect human rights in mental health and social care settings and to expand opportunities of various organizations and associations to defend the rights of persons with mental disorders and psychosocial disabilities.
The WHO guidelines on community mental health services and human rights-based approaches provide information for all stakeholders who intend to develop or transform mental health systems and services. health in accordance with international human rights standards, including the UN Convention on the Rights of Persons with Disabilities.
Bibliography
(1) Harrison G, Hopper K, Craig T, Laska E, Siegel C, Wanderling J. Recovery from psychotic illness: a 15- and 25-year international follow-up study. Br J Psychiatry 2001;178:506-17.
Recovery from psychotic illness: a 15- and 25-year international follow-up study. Br J Psychiatry 2001;178:506-17.
(2) Institute of Health Metrics and Evaluation (IHME). Global Health Data Exchange (GHDx). http://ghdx.healthdata.org/gbd-results-tool?params=gbd-api-2019-permalink/27a7644e8ad28e739382d31e77589dd7 (accessed 25 September 2021)
(3) LaursenTM, Nordentoft M, Mortensen PB. Excess early mortality in schizophrenia. Annual Review of Clinical Psychology , 2014;10, 425-438.
(4) WHO. Mental health systems in selected low- and middle-income countries: a WHO-AIMS cross-national analysis. WHO: Geneva, 2009
(5) Jaeschke K et al. Global estimates of service coverage for severe mental disorders: findings from the WHO Mental Health Atlas 2017 Glob Ment Health 2021;8:e27.
A schizophrenic's story: how the disease changed my whole life
Subscribe to our newsletter "Context": it will help you understand the events.
Alice Evans was a student when she developed symptoms of schizophrenia. She spent the next 10 years at her parents' house. Here is her story.
I first felt really bad when I was 20 years old. At that time I was studying at the university.
When I entered, I was uncomfortable being away from home, but gradually I made friends. I enjoyed studying, especially the drama course. Although during this period I was visited by many depressive thoughts.
I worked three jobs to pay my rent. Together with studies, this lifestyle at some point became unbearable.
I almost completely stopped sleeping. That's when the problems started.
It seemed to me that the surrounding world had lost its colors. This is how I can describe my state of mind at the time. Everything became gray and dull.
Thoughts and phrases began to elude me. I started to think about something and lost the thread. Plus, I couldn't speak. The words just didn't physically come out of my mouth.
Plus, I couldn't speak. The words just didn't physically come out of my mouth.
Constant fears appeared. It was especially scary when I started to hear extraneous voices on the radio or on TV. I did not understand what was happening, and did not realize how seriously I was ill.
One weekend my uncle and aunt visited me. We were walking around the city, and suddenly I saw that everything around was empty, people disappeared, and buildings collapsed. I walked completely alone through a deserted, abandoned city.
Of course, it was not so, but during a psychic attack, the vision is your reality. And you can't snap your fingers to make it all go back. It's impossible.
As if in a fog
This period of my life passed like in a fog. I was confused all the time, I felt exhausted and scared, so I don’t remember very much about those times.
Due to speech disorders, I could not tell my relatives and friends about how serious my condition was. I don't think I fully realized it myself. A person suffering from psychosis is most often afraid to admit it.
I don't think I fully realized it myself. A person suffering from psychosis is most often afraid to admit it.
Image copyright, AliceEvans
Photo caption,Alice was 20 years old when she began to show signs of schizophrenia
One day I left the house with no idea where I was going. I wandered the streets alone and lost. She got into some buses to get home, but did not know which route they were taking. There was no one around to help.
Somehow, I still don't know how, I was picked up by my friends and taken to my parents in Devon.
After that, I didn't leave my parents' house for 10 years.
My parents took me to a psychiatrist who spoke to me very kindly and prescribed drugs to relieve the symptoms of schizophrenia. These symptoms were expressed in hallucinations, various manias and mental confusion.
Side effects
When I heard my diagnosis - schizophrenia - I was even delighted. At least I understood what I was dealing with and could start fighting for the future.
At least I understood what I was dealing with and could start fighting for the future.
The medicines worked almost immediately, but I wanted to have a course of therapy in which I could talk about my illness. At that time, this kind of treatment was very poorly funded. And today, mentally ill people face the same problem.
Skip the Podcast and continue reading.
Podcast
What was that?
We quickly, simply and clearly explain what happened, why it's important and what's next.
episodes
The End of the Story Podcast
While taking medication, I began to slowly move towards healing. Gradually, speech began to return, I began to wash myself and serve myself at an elementary level. Those who say that mental disorders do not affect the physical state are wrong. In my case, my body also failed.
Unfortunately, my drugs had side effects and I gained over 60 kilograms in about a year of treatment.
Excess weight has been a problem for me since my school days, although now, looking back, I understand that then I had nothing to worry about. Such a powerful weight gain aggravated my condition. I felt unattractive, didn't want to see my friends, and my fear of going out made it impossible to play sports.
Then I found my first job in many years: washing dishes in a local pub. I put on headphones, turned on my favorite music and worked the whole shift like that, I even liked it. But, unfortunately, my health made itself felt, and I could not have a permanent job. It was kind of a vicious circle.
To a new life
But one day a miracle happened, thanks to which I found new friends. I have always liked music and art, long before my illness. And my mom convinced me to join the local drama club. I was terrified at the prospect of being in the company of strangers and playing on stage, but I was very well received there, and I got a role in a production that was being worked on.
I was terrified at the prospect of being in the company of strangers and playing on stage, but I was very well received there, and I got a role in a production that was being worked on.
Image copyright AliceEvans
Image captionAlice was unable to speak for a long time
It was very difficult for me to memorize the text, but it did not annoy anyone. The guys had a good reaction and a sense of humor, they always saved the situation if I forgot the words.
Most of the group I became friends with Tristan. He supported me in everything, and one day I told him about my schizophrenia. He also had some mental disorders, and it was easy for me to talk to him about it, knowing that he understood me.
One day he announced that he decided to enter the university and suggested that I also apply. I was horrified, but his strength and support, coupled with my own inner self-belief, did the trick. I applied and to my great surprise was accepted into the Chelsea Institute of Art.
And then my life began.
Photo credit: BBC World Service
Photo captionOne of the symptoms of schizophrenia is withdrawing into oneself, disconnecting from reality
A few facts about schizophrenia:
- One in every hundred people in Britain suffers schizophrenia
- Usually the disease manifests itself at about 20 years of age
- Symptoms of the disease are divided into positive and negative. The positive ones are hallucinations and manias, the negative ones are the lack of motivation, self-isolation, lack of interest in the surrounding life. Negative symptoms tend to be longer lasting and more difficult to treat.
Two years ago, my situation "sank" a little again. Being overweight prevented my body from effectively dealing with a lung infection, and I spent 10 days in intensive care with symptoms of asthma.
Image caption, Luckily, I made a full recovery and was allowed to undergo weight loss surgery—another major chapter in my healing story.
Luckily, I made a full recovery and was allowed to undergo weight loss surgery—another major chapter in my healing story. This is what Alice looks like now
I volunteered for a local mental health charity. There I gained a lot of experience and useful skills. They also referred me to speech therapy, which also played a huge role in my return to normal life. Unfortunately, funding for the foundation was cut significantly, and the department I worked in was forced to close, to the disappointment of both staff and patients.
However, I was very lucky. Before closing, the staff of this department helped me apply for a master's degree at the Royal Institute of Arts. Gradually, I began to engage in teaching activities myself, helping others to discover their artistic talents. I am currently pursuing a professor's degree.
It took me 20 years to get to where I am now and I still have seizures. Living with schizophrenia is very difficult and I am very fortunate to have such incredible support from my family and friends.