How do i support my depressed partner
SAMHSA’s National Helpline | SAMHSA
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.
Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders.
This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative. Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs. In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems. Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.
Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt. Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse. Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.
Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.For additional resources, please visit the SAMHSA Store.
Last Updated: 08/30/2022
Recovery and Recovery Support | SAMHSA
Recovery signals a dramatic shift in the expectation for positive outcomes for individuals who experience mental and substance use conditions or the co-occurring of the two.
SAMHSA's working definition of recovery defines recovery as a process of change through which individuals improve their health and wellness, live self-directed lives, and strive to reach their full potential.
Today, when individuals with mental and/or substance use disorders seek help, they are met with the knowledge and belief that anyone can recover and/or manage their conditions successfully. The value of recovery and recovery-oriented systems of care is widely accepted by states, communities, health care providers, peers, families, researchers, and advocates including the U.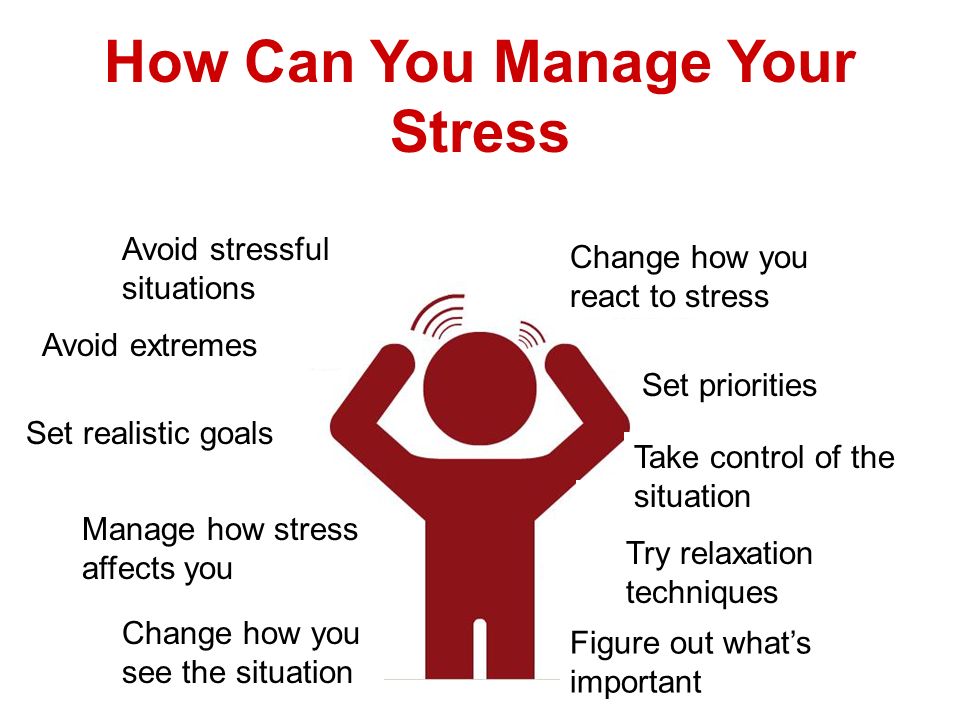 S. Surgeon General, the National Academy of Medicine (NAM), and others.
S. Surgeon General, the National Academy of Medicine (NAM), and others.
Guiding Principles
Hope, the belief that these challenges and conditions can be overcome, is the foundation of recovery. A person’s recovery is built on his or her strengths, talents, coping abilities, resources, and inherent values. It is holistic, addresses the whole person and their community, and is supported by peers, friends, and family members.
The process of recovery is highly personal and occurs via many pathways. It may include clinical treatment, medications, faith-based approaches, peer support, family support, self-care, and other approaches. Recovery is characterized by continual growth and improvement in one’s health and wellness and managing setbacks. Because setbacks are a natural part of life, resilience becomes a key component of recovery.
- Guiding Principles
- The Four Dimensions of Recovery
- The Office of Recovery
- Recovery and Resilience
- Recovery and Relationships
- Recovery Support
- Cultural Awareness and Competency
- The Office of Behavioral Health Equity
The Four Major Dimensions of Recovery
-
Health
Overcoming or managing one’s disease(s) or symptoms, and making informed, healthy choices that support physical and emotional well-being
-
Home
Having a stable and safe place to live
-
Purpose
Conducting meaningful daily activities, such as a job, school volunteerism, family caretaking, or creative endeavors, and the independence, income, and resources to participate in society
-
Community
Having relationships and social networks that provide support, friendship, love, and hope
SAMHSA's Office of Recovery
The Office of Recovery was established to evaluate and initiate policy, programs and services with a recovery focus and ensure the voices of individuals in recovery are represented. The Office will support the growth and expansion of recovery support services across the country.
The Office will support the growth and expansion of recovery support services across the country.
A national clearinghouse and resource for recovery-oriented care across the mental health, substance use, and co-occurring domains, the Office promotes a recovery-oriented system of care working in partnership with recovery community leaders, tracking progress over time and identifying to resolve barriers to system transformation.
Implement recovery-oriented principles and practices in real-world practice settings with diverse groups of people diagnosed with behavioral health conditions.
SAMHSA shares the importance of recovery support and highlights resources that encourage engagement in mental health and substance use treatment.
The goal of this challenge is to identify innovations developed by peer-run or community-based organizations that advance recovery.
This video series is a set of conversations between parents and providers discussing varying topics related to difficult situations parents find themselves in.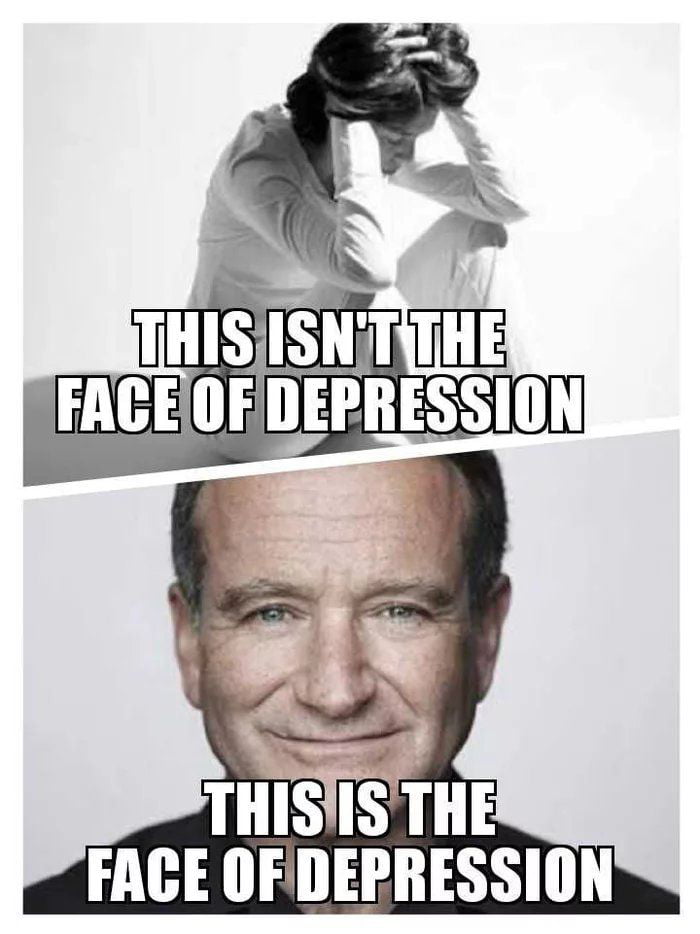
Recovery and Resilience
Resilience refers to an individual’s ability to cope with change and adversity. Resilience develops over time and gives an individual the capacity not only to cope with life’s challenges but also to be better prepared for the next stressful situation. Psychological resilience, the ability to cope with adversity and to adapt to stressful life events, varies widely from person to person and depends on environmental as well as personal factors. It refers to positive adaptation, or the ability to maintain mental and physical health despite participating in stressful situations. Resilience is playing up those protective factors so they can outweigh the risk factors. Optimism and the ability to remain hopeful are essential to resilience and the process of recovery.
Because recovery is a highly individualized process, recovery services and supports must be age appropriate and offered over the life course and flexible enough to ensure cultural relevancy. What may work for adults in recovery may be very different for youth or older adults in recovery. For example, the promotion of resiliency in young people, and the nature of social supports, peer mentors, and recovery coaching for adolescents and transitional age youth are different than recovery support services for adults and older adults.
What may work for adults in recovery may be very different for youth or older adults in recovery. For example, the promotion of resiliency in young people, and the nature of social supports, peer mentors, and recovery coaching for adolescents and transitional age youth are different than recovery support services for adults and older adults.
Recovery and Relationships
The process of recovery is supported through relationships and social networks. This often involves family members who become the champions of their loved one’s recovery. They provide essential support to their family member’s journey of recovery and similarly experience the moments of positive healing as well as the difficult challenges. Families of people in recovery may experience adversities in their social, occupational, and financial lives, as well as in their overall quality of family life.
These experiences can lead to increased family stress, guilt, shame, anger, fear, anxiety, loss, grief, and isolation. The concept of resilience in recovery is also vital for family members who need access to intentional supports that promote their health and well-being. The support of peers and friends is also crucial in engaging and supporting individuals in recovery.
The concept of resilience in recovery is also vital for family members who need access to intentional supports that promote their health and well-being. The support of peers and friends is also crucial in engaging and supporting individuals in recovery.
Peer support assists individuals to engage or stay connected to the recovery process through a shared understanding, respect, and mutual empowerment. Peer support extends beyond the reach of clinical treatment into the everyday environment providing non-clinical, strengths-based support. This relationship can help lay the foundation for SAMHSA’s four dimensions of recovery.
A peer-led national center that provides training and technical assistance related to substance use disorder recovery.
Recovery Support
SAMHSA advanced recovery support systems to promote partnering with people in recovery from mental and substance use disorders and their family members to guide the behavioral health system and promote individual, program, and system-level approaches that foster health and resilience; increase housing to support recovery; reduce barriers to employment, education, and other life goals; and secure necessary social supports in their chosen community.
Recovery support is provided in various settings. Recovery support services help people enter into and navigate systems of care, remove barriers to recovery, stay engaged in the recovery process, and live full lives in communities of their choice.
Recovery support services include culturally and linguistically appropriate services that assist individuals and families working toward recovery from mental and/or substance use problems. They incorporate a full range of social, legal, and other services (PDF | 409 KB). that facilitate recovery, wellness, and linkage to and coordination among service providers, and other supports shown to improve quality of life for people (and their families) in and seeking recovery.
Recovery support services may be provided before, during, or after clinical treatment, or may be provided to individuals who are not in treatment but seek support services.
These services, provided by professionals and peers, are delivered through a variety of community and faith-based groups, treatment providers, schools, and other specialized services. The broad range of service delivery options ensures the life experiences of all people are valued and represented.
The broad range of service delivery options ensures the life experiences of all people are valued and represented.
For example, in the United States there are 34 recovery high schools that help reduce the risk in high school environments for youth with substance use disorders. These schools typically have high retention rates and low rates of students returning to substance use.
Additionally, SAMHSA's Bringing Recovery Supports to Scale Technical Assistance Center Strategy (BRSS TACS) advances effective recovery supports and services for people with mental or substance use disorders and their families.
Find more Publications and Resources on Recovery and Recovery Support.
Cultural Awareness and Competency
Supporting recovery requires that mental health and addiction services:
- Be responsive and respectful to the health beliefs, practices, and cultural and linguistic needs of diverse people and groups
- Actively address diversity in the delivery of services
- Seek to reduce health disparities in access and outcomes
Cultural competence describes the ability of an individual or organization to interact effectively with people of different cultures. To produce positive change, practitioners must understand the cultural context of the community that they serve, and have the willingness and skills to work within this context. This means drawing on community-based values, traditions, and customs, and working with knowledgeable people from the community to plan, implement, and evaluate recovery activities.
To produce positive change, practitioners must understand the cultural context of the community that they serve, and have the willingness and skills to work within this context. This means drawing on community-based values, traditions, and customs, and working with knowledgeable people from the community to plan, implement, and evaluate recovery activities.
Individuals, families, and communities that have experienced social and economic disadvantages are more likely to face greater obstacles to overall health. Characteristics such as race or ethnicity, religion, low socioeconomic status, gender, age, mental health, disability, sexual orientation or gender identity, geographic location, or other characteristics historically linked to exclusion or discrimination are known to influence health status.
SAMHSA is committed to addressing these health disparities by providing culturally and linguistically appropriate mental health, prevention, harm reduction, treatment, and recovery support programs. This commitment is reinforced through the agency’s disparity impact statement that monitors programs and activities to ensure that access, use, and outcomes are equitable across racial, ethnic, and other under resourced populations.
This commitment is reinforced through the agency’s disparity impact statement that monitors programs and activities to ensure that access, use, and outcomes are equitable across racial, ethnic, and other under resourced populations.
Last Updated: 02/16/2023
Depressed partner support
11/22/2019
Depression is one of the most common mental disorders, affecting more than 350 million people of all age groups.
Every year about 150 million people in the world lose their ability to work due to depression
The support of family and friends is essential in the treatment of mental disorders. However, depression can negatively impact relationships and leave loved ones feeling helpless, frustrated, or afraid.
There are ways people can support a partner with depression on their journey to recovery.
Questions to ask about symptoms
To understand the severity of a person's depression, it is helpful to study how these symptoms affect their life.
Asking about symptoms also shows a person that his partner is interested in his feelings and experiences.
Useful questions to ask include:
- Can you help me understand how you feel?
- What activities do you find enjoyable right now?
- Do you enjoy spending time with other people?
- What's wrong with your energy?
- Do you sleep more or less than usual?
- Do you eat more or less than usual?
- Can you focus on things right now?
- Do you have thoughts of death or suicide?
Questions to avoid
Avoid asking questions that seem judgmental or that place blame on the person with depression. They may already be blaming themselves for their symptoms and need support rather than further judgment.
It is also important not to oversimplify depression, which is a serious illness.
Examples of questions to avoid include:
- Why can't you just cheer up?
- Don't I make you happy?
- When will you feel better?
- Don't you understand that it's all in your head?
- Why do you attach such importance to this?
- Do you know that others are in a much worse situation than you?
Partner support
1. Learn about depression
Learn about depression
Learning about depression can make it easier to support those with depression. Learning about symptoms often helps people recognize symptoms in their loved ones.
Symptoms can range from mild to severe and may change over time. However, symptoms must last at least 2 weeks before a doctor can diagnose depression.
Symptoms of depression may include:
- feelings of sadness, worthlessness or guilt
- loss of interest in previously enjoyable activities
- changes in appetite or weight
- changes in sleep habits
- fatigue and loss of energy
- difficulty concentrating or making decisions
- thoughts of death or suicide
2. Understand and acknowledge your partner's feelings
It is important to listen to a person with depression and express empathy, which is the ability to understand and share other people's feelings. One way to show empathy is to mirror what the person is saying.
One way to show empathy is to mirror what the person is saying.
For example, if he says, "I just feel like things will never get better," their partner might reflect this by saying, "that sounds like you're not looking forward to the future."
Constant attempts to cheer up a person are useless, as this devalues his condition and feelings. Phrases like “tomorrow will be better” or “try to cheer up” do not take into account the nature of the disease.
3. Ask your partner what they want from you
To show further understanding and support, ask the person what they need. He may need:
- medication reminders
- company when visiting a doctor or visiting therapy
- homemade dishes
- encouragement to socialize or exercise
- hug or hold the hand
- to sometimes be left alone
Useful questions to ask include:
- How can I help you?
- Would it be helpful if I.
 ..?
..?
4. Encourage your partner to heal
Depression can cause a person to lose their motivation, which can be a barrier to seeking treatment. However, most people with depression need treatment to get better.
Those who support someone with depression can play an important role in their recovery by encouraging them to seek medical help.
To inspire a partner to seek treatment, a person can try:
- joint detection and documentation of your partner's symptoms
- expression of desire to help
- discussion of treatment options such as medication, psychotherapy, and lifestyle changes
- accompaniment to doctor appointments
5. Support your partner during recovery
Recovery from depression can sometimes be difficult. To support a partner in the recovery process:
- help them keep track of their prescriptions and medications
- do some physical exercise together
- plan and prepare healthy meals together
- try to reduce stressors at home
- make your goals small and achievable
- encourage them to socialize with other people
- plan fun activities together
- pay attention to the person's progress towards recovery
- avoid forcing treatment on the person
Let your partner know they are not alone when you say:
- I'm here for you.

- We'll deal with this together.
6. Accept that there will be bad days
People with depression have good days and bad days. To cope with bad days:
- expect them to happen
- understand that this is a normal part of depression
- don't give up love and support at this time
- take some time and do something nice, either alone or with others
- remember that not every day will be like this - there will be good days
7. Take care of yourself
When a person supports a partner with depression, it is very important to take the time to enjoy hobbies and other activities for yourself.
Caring for a partner with depression can be draining, frustrating, and intimidating.
Research shows that having a spouse with depression increases a person's risk of developing depressive symptoms. This risk is especially high when a man is supportive of a depressed woman.
Those caring for someone with a mental illness should also take care of their own mental health. They can do it:
- trying to stay positive
- having realistic expectations about the recovery process
- knowing that they also have the right to be heard and respected
- taking time out and doing pleasurable activities and hobbies
- interacting with people other than their partner
- seeking help from friends or relatives
- doing regular exercise
- eating healthy
- trying to get more sleep and rest
- visiting a psychologist or psychological support groups
Professional support
Professional treatment is an important part of the recovery process. The first step is often to see a doctor, who can recommend treatment, psychotherapy, or both.
For particularly severe depressive symptoms or in life-threatening situations, seek emergency care.
Beginning of form
People with depression may be at risk of suicide. According to the American Foundation for Suicide Prevention, more than half of those who die by suicide suffer from major depression.
Partners of those who suffer from depression should be aware of the warning signs of suicide so that they can take prompt action if necessary. Warning signs include:
- talking about death or suicide
- having a suicide plan
- preparation of means of suicide, e.g. collection of pills
- preparation for death, e.g. by making a will
- distribution of things
- farewell to family and friends
- engaging in risky or reckless behavior
- Extreme changes in mood or personality
- withdrawal from society
If a person suspects that someone is in imminent danger of suicide, they should seek emergency help.
If someone believes that a loved one is contemplating suicide but is not in immediate danger, they should contact the person's doctor and seek support from other family members or a support group.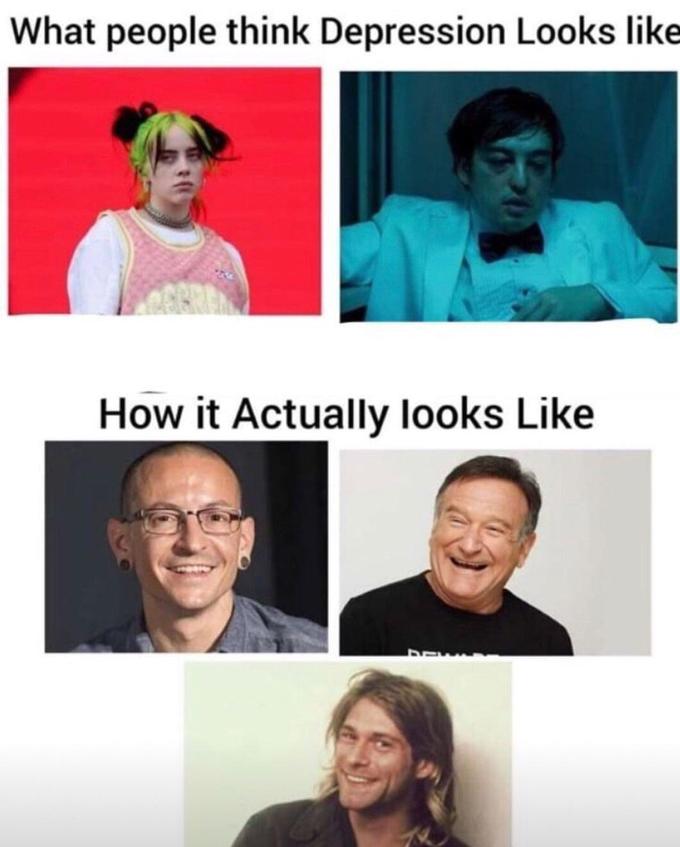
Support for a partner with depression, both emotional and practical, can help speed up the recovery process.
CONTROL AND INSURANCE ORGANIZATIONS
LEGAL INFORMATION
INDEPENDENT QUALITY ASSESSMENT OF MED. SERVICES
ANTI-CORRUPTION
PRICE LIST FOR PAID SERVICES
VACANCIES
How to behave with a person with depression. Instructions - Meduza
Depression is one of the most common mental disorders: according to the World Health Organization as of February 2017, more than 300 million people worldwide suffer from it. The scale of the problem in Russia is harder to assess. Experts talk about almost eight million Russians suffering from depression, but specify that, most likely, there are much more of them - people with depression often do not seek help because of shame or unwillingness to admit the seriousness of their condition.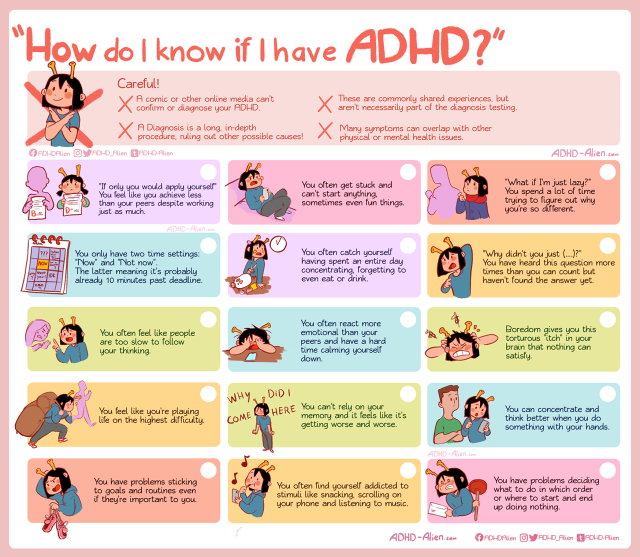 Depression can be underestimated not only by the patients themselves, but also by their relatives. At the request of Meduza, the author of the remain_nameless telegram channel about mental health, Daria Chagina, tells how to properly behave with a person suffering from depression, so as not only not to harm him, but also to help.
Depression can be underestimated not only by the patients themselves, but also by their relatives. At the request of Meduza, the author of the remain_nameless telegram channel about mental health, Daria Chagina, tells how to properly behave with a person suffering from depression, so as not only not to harm him, but also to help.
Recognize the importance of the problem
Pop culture has taught us that depression is a kind of seasonal blues: many of us have heard (or said) "I'm depressed today." Of course, any person experiences bouts of melancholy and depression - due to lack of sleep, problems at work, a quarrel with a loved one, and even bad weather. But as soon as the surrounding circumstances change, everything returns to normal. Depression, on the other hand, is arranged differently: its causes can be deeply hidden, it greatly affects a person’s life, and only in 40% of cases goes away on its own - and even then not completely.
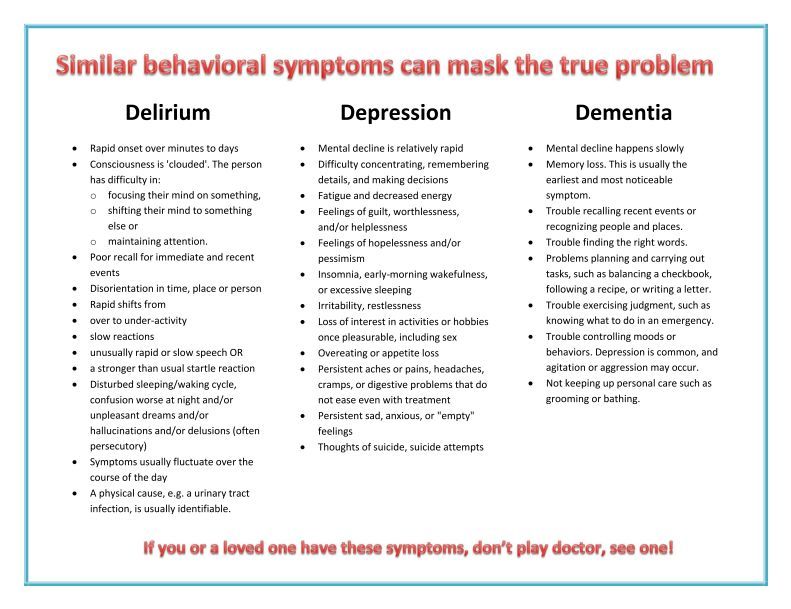
Depression is expressed primarily in a constant depressed state, chronic fatigue and loss of interest in things that used to please. In addition, the disease can be accompanied by various somatic manifestations: a person either suffers from insomnia, or, conversely, constantly wants to sleep. Doesn't want sex. He cannot concentrate on anything and loses his ability to work. Loses appetite or, conversely, begins to overeat. Depression can also lead to a complete loss of interest in life, a suicidal state and suicide. The diagnosis is made if the duration of symptoms is at least two weeks - but depression can last for months or even years, and it must be treated.
In addition, the disease can be accompanied by various somatic manifestations: a person either suffers from insomnia, or, conversely, constantly wants to sleep. Doesn't want sex. He cannot concentrate on anything and loses his ability to work. Loses appetite or, conversely, begins to overeat. Depression can also lead to a complete loss of interest in life, a suicidal state and suicide. The diagnosis is made if the duration of symptoms is at least two weeks - but depression can last for months or even years, and it must be treated.
Risk factors for depression can range from psychological shocks or trauma, dysfunctional family situations or lack of parental love, as well as genetic predisposition or various diseases, as well as alcohol or drug use. Moreover, psychogenic depression (caused, for example, by the death of a loved one, divorce or violence) does not necessarily come immediately - people experience difficult events in different ways, and sometimes the reaction to them comes with a delay.
Show that you are there
Depressed people don't just feel lonely, they often feel ashamed and guilty about their feelings and emotions. For fear of being misunderstood, ridiculed, or rejected, they prefer to remain silent about their experiences, do not seek help, or refuse to acknowledge the seriousness of their situation. Left alone with their feelings, many try to suppress and hide them - and only more convinced of their own "abnormality", worthlessness and uselessness. As studies confirm, it is this feeling of separation from other people that can lead to suicidal thoughts - therefore, the support of relatives and friends is especially important for depressed people. Make it clear that you are there no matter what, the person’s condition does not affect your attitude towards him in any way, you understand the depth of his suffering and are ready to help.
Do not discount the feelings and experiences of a depressed person
If you have never had depression, then you are unlikely to be able to fully understand the state of your loved one. Do not try to compare it to a "bad day" or just a difficult period in life (for example, a session or a job change) and do not offer a person with depression to "pull themselves together" or "tune in to positive." Even if you sincerely want to express support, such advice will only devalue the feelings of a person who is faced with depression, because he knows that everything is not so simple. People in this situation often hear, “Others have worse problems than you”, “It’s all in your head”, “Do something useful”, but all this only causes more shame, guilt or annoyance due to helplessness in the face of illness. Hearing something like this, a person may conclude that you will never understand him, and close up - then it will be much more difficult to help. If you don’t know what to say in such a situation (and this is normal), just hug, say: “I can’t even imagine what you are experiencing right now, but I see that it is very difficult” - and let the person show feelings in the way he it's necessary.
Do not try to compare it to a "bad day" or just a difficult period in life (for example, a session or a job change) and do not offer a person with depression to "pull themselves together" or "tune in to positive." Even if you sincerely want to express support, such advice will only devalue the feelings of a person who is faced with depression, because he knows that everything is not so simple. People in this situation often hear, “Others have worse problems than you”, “It’s all in your head”, “Do something useful”, but all this only causes more shame, guilt or annoyance due to helplessness in the face of illness. Hearing something like this, a person may conclude that you will never understand him, and close up - then it will be much more difficult to help. If you don’t know what to say in such a situation (and this is normal), just hug, say: “I can’t even imagine what you are experiencing right now, but I see that it is very difficult” - and let the person show feelings in the way he it's necessary.
Don't take the words and actions of a depressed person personally
People with depression are generally not able to lead the same active lifestyle as before. For example, they stop responding to messages and calls, refuse offers to go out to dinner or to the movies, they may even miss your birthday or wedding. This looks strange and insulting: after all, quite recently everything was in order, and today a person comes up with reasons to avoid a meeting. And if he nevertheless agrees to it, he can behave indifferently and not even try to pretend that he is interested in listening to you.
It's not about you at all - it's just that in a depressed state, most often there is no strength for anything. Even such simple, ordinary things as getting out of bed, taking a shower and preparing breakfast require a lot of effort. It is all the more difficult to go somewhere where there will be a lot of people. In addition, communication with people itself, even if it is not binding, requires a return, for which a depressed person does not have enough emotional resources. Remember that depressed people feel and appreciate the support of their family and friends, but they simply cannot respond to it in the same way as before.
Remember that depressed people feel and appreciate the support of their family and friends, but they simply cannot respond to it in the same way as before.
Suggest seeking professional help
Depression doesn't often go away on its own, but even if it does, it can come back. According to statistics, 50% of people who have had a depressive episode in their lives have a second one after some time, and 80% of people who have two depressive episodes in their medical history sooner or later have a third. So if you suspect depression, a person should definitely see a specialist - first of all, a psychiatrist who can prescribe drugs if necessary. True, it is also very difficult for many to take this step: going to the doctor is considered something like a “last resort”, an admission of defeat. Antidepressants are also treated with great apprehension, although now there is a large selection of funds - and a competent specialist will be able to choose the right ones in each individual case. Yes, it doesn’t always work right away, but often you can’t do without medication.
Yes, it doesn’t always work right away, but often you can’t do without medication.
Your loved one may be seriously afraid of going to the doctor because of the fear that he will be labeled as "mentally ill", "registered" or even "put in a fool". In fact, psychiatric registration was canceled back in the early 90s, and a person can be placed in a hospital against their will only by a court decision - or if a person poses a threat to himself and is not able to take care of himself. But if your loved one is still haunted by the fear of free medicine, advise him to contact a private specialist - if possible.
Tell the person with depression that more and more people are going to therapy and it really helps. After all, with a fracture, your friend would go to the surgeon - so in this case, you need to see a doctor. Offer help in finding a psychiatrist, offer to give a ride to an appointment or just see them off. But in no case do not shame and do not force.
Help with the simplest things (but in moderation)
When a person close to you cannot do some things due to illness, there is a desire to take everything upon yourself. You really can help, but here you need to know when to stop.
You really can help, but here you need to know when to stop.
If you live together, help with daily chores: waking up and going to bed on time, remembering to take a shower or soak in the bath, eat well, and remember to take medication if prescribed. The correct daily routine helps to maintain some kind of balance even in the most difficult condition. You can try to involve a person in physical exercises - studies confirm that sports help in the treatment and prevention of depression. Moreover, it is the regularity of classes, and not their intensity, that plays the key role - you need to exercise for at least three months and for 45-60 minutes. Workouts on a pulse of 120-130 beats per minute are best suited: running, walking, swimming, cycling, tennis, dancing.
Offer to install useful applications
When depressed, it is useful to monitor how your mood changes over time - there are many paid and free mobile applications in Google Play and the App Store for this. For example, Moodnotes. When creating the application, the developers relied on the method of cognitive behavioral therapy, so in it you can not only note what you think about and how you feel today, but also track what causes certain thoughts and moods. You can also keep a mood diary through the How Are You and MoodPanda apps.
For example, Moodnotes. When creating the application, the developers relied on the method of cognitive behavioral therapy, so in it you can not only note what you think about and how you feel today, but also track what causes certain thoughts and moods. You can also keep a mood diary through the How Are You and MoodPanda apps.
Mindfulness meditation apps can also be useful. It forms the basis of Mindfulness-Based Cognitive Therapy (MBCT), which is now gaining popularity in the United States. The main goal is to help get rid of the tendency to automatically respond to thoughts, emotions and life events. Perhaps the best mobile app for this is Headspace; it's available on both iOS and Android, but it's a paid subscription for $12.99 a month (I must say it's loved by many who don't have a depression problem, too). A free alternative to it could be Stop, Breathe & Think. But, of course, we must remember that neither meditation nor a mood diary can replace treatment, but can only be a help (well, it doesn’t hurt to discuss these practices with your doctor).
Be attentive and patient
The process of treating depression is long and difficult. How much time and effort it will take depends on the severity of depression (mild, moderate, severe), and on the chosen treatment method (only taking pills, only psychotherapy, or both), and on how quickly it turned out to pick up the right pills and their dosage and, finally, whether it was possible to find a suitable psychotherapist. It also happens that a psychotherapist is good, but not suitable. Even if you have done everything you could and the healing process has begun, you should not expect an immediate result. Don't ask, "Are you feeling better?" - It may seem to a depressed person that progress in his treatment does not meet your expectations.
Instead, ask delicately from time to time if he remembers to take his pills, if he misses psychiatric and/or psychotherapist appointments, and if so, try to carefully find out why. For example, in psychotherapy there is such a thing as "resistance" - the patient's subconscious opposition to the process of psychotherapy. This phenomenon is associated with the fear of change, because it is far from always easy and painless to come to a cure. Resistance in psychotherapy can be expressed in many ways, including just missing meetings or refusing to continue psychotherapy in principle. Dealing with this is the work of a psychotherapist, but a careful, confidential conversation with a loved one can also help.
This phenomenon is associated with the fear of change, because it is far from always easy and painless to come to a cure. Resistance in psychotherapy can be expressed in many ways, including just missing meetings or refusing to continue psychotherapy in principle. Dealing with this is the work of a psychotherapist, but a careful, confidential conversation with a loved one can also help.
Take care of yourself
Being around a depressed person can be exhausting. Especially if this is a person close to you, to whose condition you cannot be indifferent. Nevertheless, do not forget the main rule from the instructions for behavior in emergency situations: you must first put on the oxygen mask. You may feel like you have to stay strong for your loved one, but you don't have to sacrifice your comfort and convenience. Don't forget that you have your own worries and feelings. If you make it your goal to get your loved one out of depression at all costs and forget about everything else, there is a risk that you will undermine your own health.