Ocd help for children
Helping a child with obsessive-compulsive disorder
If your child has obsessive-compulsive disorder (OCD), you know that this condition affects not only your child but also your entire family. The guidance that follows can help parents gain a better understanding of OCD, learn helpful strategies to support their children, and ease distress all around.
What is obsessive-compulsive disorder?
OCD typically includes uncontrollable, recurring thoughts (obsessions) and behaviors (compulsions or rituals) that a child feels an urgent need to repeat again and again. For example, your child may repeat a grooming routine until he feels “just right.”
A child may engage in compulsions or rituals to temporarily reduce distress. A child also may complete a compulsion because she imagines that doing so will prevent a scary outcome. For example, a child may tap a countertop three times at the start of every hour to prevent a parent from dying in a car crash. Even though the child logically may know that the two behaviors are not linked, the distress caused by having such obsessions can make the likelihood of the car crash seem possible if the child does not perform the ritual.
Unfortunately, compulsions strengthen obsessions in the long run. This sets up a vicious cycle of obsessions, distress, and compulsions.
How does OCD affect the family?
OCD does not just affect children who have the disorder. It can have an impact on the entire family, resulting in frequent conflicts. For example, the insistence on completing compulsions at specified times and places — such as, at 9:00 AM at home — may make you late for work and your children late for school. OCD also may dictate which family members cannot touch certain objects or say certain phrases, which may make family members feel uncomfortable in their own home.
Parents and siblings understandably can feel resentful for the ways in which OCD can interfere with their daily lives. Parents also can feel guilty about not being able to support their child sufficiently.
How can you support a child with OCD?
Looking for help from an experienced mental health professional is a good way to start. Strategies used to treat OCD go against maternal and paternal instincts, so it is important for children and their parents to be involved in treatment to learn how to manage OCD. The tips below may help.
Strategies used to treat OCD go against maternal and paternal instincts, so it is important for children and their parents to be involved in treatment to learn how to manage OCD. The tips below may help.
- Pursue cognitive behavioral therapy. Cognitive behavioral therapy (CBT) is a specialized psychotherapy that helps people learn the links among thoughts, feelings, and behaviors, and develop tools to address unhelpful patterns. A special type of CBT that focuses on exposure and response prevention (ERP) is considered the gold standard treatment for OCD. This evidence-based treatment helps a child gradually resist engaging in compulsions while learning that the outcome is not as bad as expected — or, at least, can be tolerated. If your child’s symptoms are consuming more than an hour daily, creating distress for your child or family, and interfering with activities, your child may benefit from CBT with ERP. You can ask your pediatrician for a referral, or search for a provider or a program through the International OCD Foundation.
- Try not to accommodate. As a parent, your instinct is to support and protect your child. Unfortunately, OCD feeds on attention and accommodation. For example, if your child asks you to open a door to avoid coming in contact with germs, you inadvertently strengthen OCD each time you open the door. This is because your child’s brain learns that the door handle is something to fear and cannot be handled by him. Try to resist participating in rituals, even if it feels awful to refrain. Giving OCD an inch only encourages it to demand a mile. Resisting accommodation may make symptoms worse before they get better. Think of OCD as a bully who demands lunch money. A bully usually will not accept “no” as an initial answer. Instead, he’ll try to up the ante until he gets the money. However, the bully will learn over time that it is not worth the effort to get no attention and no money. The situation can improve if you remain consistent.
- Understand that your child is probably not trying to be oppositional.
 If you view your child as defying you on purpose, you may feel angry. This can prompt you to engage in a futile battle of wills. Try to shift perspectives for a moment. Think about something that terrifies you — maybe entering a cage with a hungry tiger. Your human instinct is to escape, and you might do whatever it takes to do so. Now imagine someone trying to force you to stay in the cage. That is what it can feel like for a child to be told that she needs to stop a ritual. Obsessions elicit tremendous distress. Your child may worry that she will not be able to tolerate the outcome of an incomplete compulsion. Remind yourself that OCD is a very convincing bully. You are angering OCD, not your child. It is not your child trying to disrupt the family; it is the OCD.
If you view your child as defying you on purpose, you may feel angry. This can prompt you to engage in a futile battle of wills. Try to shift perspectives for a moment. Think about something that terrifies you — maybe entering a cage with a hungry tiger. Your human instinct is to escape, and you might do whatever it takes to do so. Now imagine someone trying to force you to stay in the cage. That is what it can feel like for a child to be told that she needs to stop a ritual. Obsessions elicit tremendous distress. Your child may worry that she will not be able to tolerate the outcome of an incomplete compulsion. Remind yourself that OCD is a very convincing bully. You are angering OCD, not your child. It is not your child trying to disrupt the family; it is the OCD.
Seek support for yourself
As noted above, OCD can affect the whole family. Ask your pediatrician or a mental health professional about OCD peer support groups for parents in your community. The National Alliance on Mental Illness (NAMI) may guide you to one.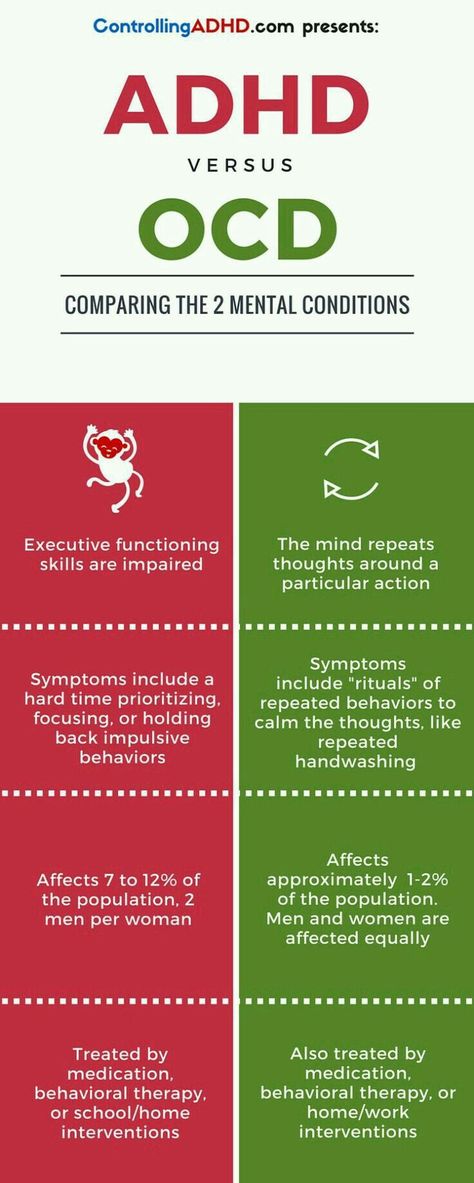 Some clinicians trained in CBT and CBT with ERP for children with obsessive-compulsive disorder also provide parent guidance. You deserve support, too, and to learn that you are not alone as you help your child manage OCD.
Some clinicians trained in CBT and CBT with ERP for children with obsessive-compulsive disorder also provide parent guidance. You deserve support, too, and to learn that you are not alone as you help your child manage OCD.
As a service to our readers, Harvard Health Publishing provides access to our library of archived content. Please note the date of last review or update on all articles.
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.
The Parents' Role in OCD Treatment
When you’re the parent of an anxious child, you assume that your role is to provide reassurance, comfort, and a sense of safety. Of course you want to support and protect a child who is distressed and, as much as possible, avert her suffering. But in fact, when it comes to a child with an anxiety disorder like obsessive compulsive disorder, trying to shield her from things that trigger her fears can be counterproductive for the child. By doing what comes naturally to a parent, you are inadvertently accommodating the disorder, and allowing it to take over your child’s life.
By doing what comes naturally to a parent, you are inadvertently accommodating the disorder, and allowing it to take over your child’s life.
That’s why parents have a surprisingly important role in treating anxiety disorders in children. The gold standard in pediatric OCD treatment is a form of cognitive-behavioral therapy called exposure and response prevention. The therapy involves “exposing” the child to her anxieties in a gradual and systematic way, so she no longer fears and avoids those objects or situations; “response prevention” means she is not allowed to perform a ritual to manage fears. Because parents become so involved in their children’s OCD, research has shown that including parents in treatment and assigning them as “co-therapists” improves effectiveness.
The fear hierarchy
In therapy the child, parents, and therapist create a “fear hierarchy” in which they collaboratively identify all of the feared situations, rate them on a scale of 0-10, and tackle them one at a time. For example, a child with fears about germs and getting sick would repeatedly confront “contaminated” situations and objects until her fear subsides and she can tolerate the activity. The child would start with a low-level anxiety item, such as touching clean towels, and build to more difficult items such as holding half-eaten food from the trash.
For example, a child with fears about germs and getting sick would repeatedly confront “contaminated” situations and objects until her fear subsides and she can tolerate the activity. The child would start with a low-level anxiety item, such as touching clean towels, and build to more difficult items such as holding half-eaten food from the trash.
Response prevention involves preventing the child from performing the behavior that serves to decrease the anxiety. For example, a boy with a fear of germs would have to abstain from washing his hands after touching the doorknob, or the garbage. Through gradual exposure he learns that what he “fears” usually does not come true, so that new learning can take place. It also teaches him that he can tolerate uncomfortable feelings.
Practice at homeMuch of the work in CBT involves practice outside of sessions, requiring parents to participate in the treatment. Children are assigned “homework” and asked to continue practicing facing their fears in a variety of settings. Since exposure and response prevention evokes anxiety and requires considerable follow-up, family involvement and support is essential.
Since exposure and response prevention evokes anxiety and requires considerable follow-up, family involvement and support is essential.
For a child with a fear of contamination, the parents may encourage him to do the dishes, or to become a “human vacuum cleaner,” which is what clinicians call picking up small scraps of garbage from the carpet. A child with fears of vomiting might write a comic about “Vomit Man” in session with his therapist, and then practice reciting it aloud to his parents.
The problem with reassurance
But parents have a bigger role than backup when it comes to practicing exposures at home. Since OCD can be a crippling disorder for children, relatives often become excessively involved in a child’s symptoms in order to help the child function. For instance, many children with OCD, as well as other anxiety disorders, seek constant reassurance from family members. Reassurance-seeking is used by children to manage fears, and many parents provide it, even though it’s excessive, in order to make their child feel better in the moment.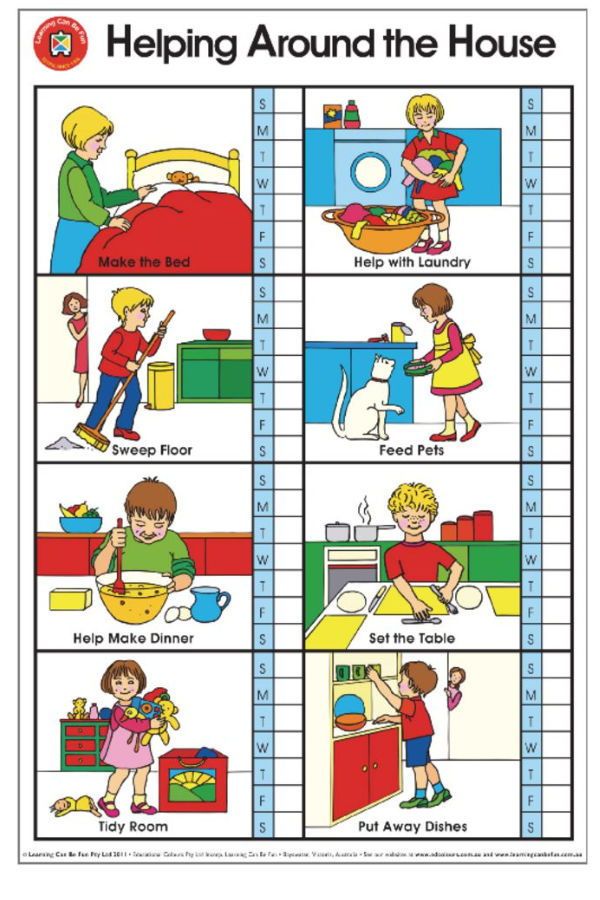
Reassurance-seeking is one of the many forms of “family accommodation.” This phenomenon refers to the manner in which family members participate in the rituals the child uses to manage his anxiety, as well as how they modify personal and family routines in order to accommodate him.
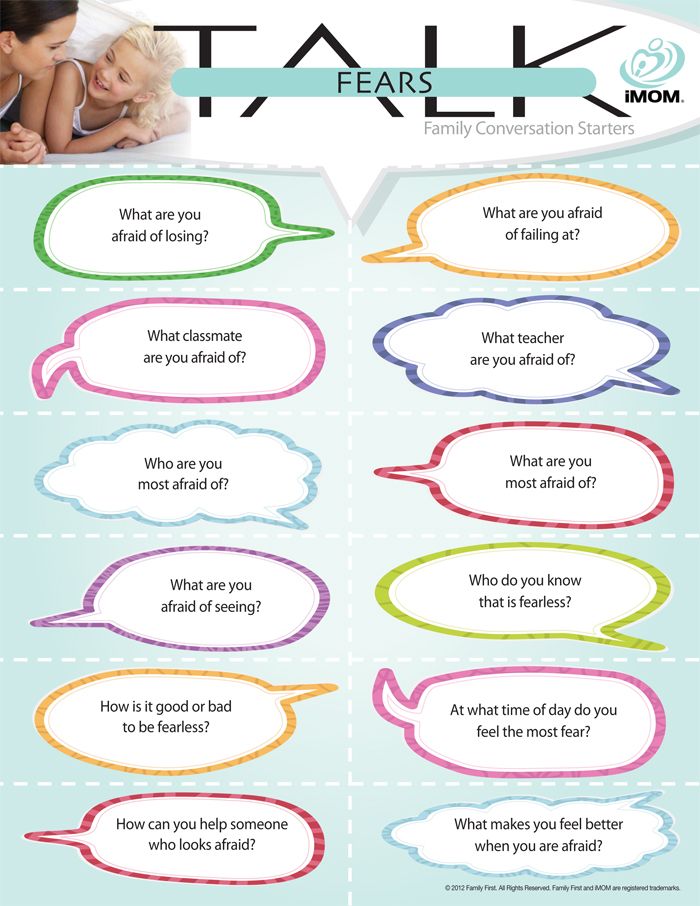
Many children suffering from OCD are unable to tolerate uncertainty, and they ask their parents to provide them with definitive answers. For example, it is not uncommon to hear an anxious child ask their parent “Am I going to get sick from eating this?” or “Is everything going to be okay?” although the answer may have already been provided several times.
Parents can easily become frustrated because they feel like no matter how many times their child’s questions are answered, they are never satisfied. Answering their child’s questions becomes an endless cycle, and the child never learns that he can indeed tolerate the uncertainty.
Accommodating fears
There are many other forms of accommodation. Families may stop taking vacations, going out to restaurants, or even change the way they speak in order to avoid anxiety-provoking situations for their child. They may avoid particular names, numbers, colors, and sounds that trigger anxiety.
Families may stop taking vacations, going out to restaurants, or even change the way they speak in order to avoid anxiety-provoking situations for their child. They may avoid particular names, numbers, colors, and sounds that trigger anxiety.
“OCD can be very overwhelming to families and can really interfere with how families can normally function,” says Jerry Bubrick, PhD, a clinical psychologist at the Child Mind Institute who specializes in anxiety and OCD. “The family decisions are made to accommodate the anxiety, rather than the best interests of the family.”
To the family of a patient we’ll call John, a 12-year old boy who was treated at the Child Mind Institute for OCD, this is all too familiar. John had fears about contamination and gaining weight and thus he avoided any food that was considered “unhealthy,” took up to seven showers a day, and didn’t play with his siblings or hug his parents in the belief that they were contaminated.
“We didn’t go out to a restaurant for months,” said John’s mother. “He didn’t have any friends come over. We didn’t have any of our friends come over. Our house was a safe place.”
“He didn’t have any friends come over. We didn’t have any of our friends come over. Our house was a safe place.”
But accommodating John’s anxiety didn’t stop it from taking over more and more of his life. John’s mother described the peak of his OCD as an extremely challenging time for her family. “It was really hard because it’s like we had lost our son. He was so trapped in the OCD. We couldn’t physically touch him. There was no spontaneity anymore. We couldn’t even sit across the table and talk anymore.”
While the parents who accommodate their child are well intentioned, family accommodation is known to reinforce their child’s symptoms. Since anxiety is maintained through avoidance, family members who accommodate their child are causing the symptoms to become even more fixed.
“Before I knew what accommodation was, I thought I was helping,” said John’s mother. “I was heartbroken when I found out the definition of accommodation. I was devastated to know I was feeding the OCD instead of helping John. ”
”
Naming the child’s OCD is one way to reduce the stigma associated with it, and makes the child feel like the anxiety is not who she is. For example, a child may name her OCD “The Bully” or “The Witch.” John’s mother continues: “Divorcing the OCD from John has been huge. Now the family has a common enemy, everyone is in on the battle. Before it was an unnamed invader. Now we know who we’re fighting.”
Building coping skills
Through treatment, parents learn new ways to respond when their children get “stuck” and how to encourage their child to rely on coping skills or to “boss back” their anxiety, instead of relying on their parents to help them through it. The children eventually become much more independent, and the parents may start to realize that anxiety is no longer in charge of their families.
Grandparents and siblings can also become involved in family accommodation, although they are not typically included in treatment as regularly as parents are.
“Since grandparents and siblings are more a part of the child’s outside world, they may be more likely to accommodate because they want to maintain peace,” said Dr. Bubrick. “They should be a involved in the treatment so they don’t undermine it.”
Helping kids face fears
Through treatment, family members learn to help their children face their fears instead of avoiding them. Instead of comforting the child, it becomes the parent’s job to remind him of the skills he has developed in treatment and to use them in the moment.
“Now I’m helping John and I’m not feeding the OCD,” said John’s mom. A lot of that is letting John know that he has strength to fight the OCD. Reminding him of the strategies instead of making the world better for him.”
Frequently Asked Questions
How do I help a child with OCD at home?You help a child with OCD at home by participating in their therapy. Their therapist can help you make a plan for reinforcing their treatment by exposing them to their fears and supporting them while you do it. For example, if your child has a fear of contamination, you can encourage them to clean the dishes or pick up garbage from the floor.
For example, if your child has a fear of contamination, you can encourage them to clean the dishes or pick up garbage from the floor.
OCD in children - causes, symptoms and treatment in Moscow at the Family Doctor clinic
Doctors
Clinic doctors
Obsessive-compulsive disorder (OCD) or obsessive-compulsive disorder is common in children. It is characterized by repetitive obsessive thoughts and actions that do not go away on their own. To eliminate unpleasant symptoms, you need the help of a child psychiatrist or psychotherapist. He knows how to help a child with OCD. The disease is being treated. A person outwardly will not be any different from the rest.
Obsessions and compulsions are familiar to Leonardo DiCaprio, Sharon Stone, Daniel Radcliffe, but this does not prevent them from performing in public, living with interest and not suffering from illness, as they keep the situation under control.
How common is neurosis
In young children, the disease is rarely diagnosed, parents take the symptoms for the characteristics of the baby, and are in no hurry to consult a doctor. Later, the frequency of neurosis increases and OCD occurs in 2 out of 100 adolescents aged 13-18.
Obsessive-compulsive disorder in children. Symptoms
The child is anxious, asks to confirm that everything is fine, that there is nothing to worry about. He cannot sleep alone or falls asleep for a long time, often comes to his parents at night.
Performs stereotypical actions that look illogical, constantly washes hands, shifts things, double-checks objects. Can put things in order in any free minute or litter the room, accumulating unnecessary things.
He says that he is disturbed by bad or terrible thoughts that he cannot get rid of. Seeks to avoid some places or situations, words.
Sometimes parents try to interrupt compulsive movements or rituals, but this only makes the situation worse by causing nervousness. Children become withdrawn, hide their experiences, withdraw and the disease is aggravated.
Children become withdrawn, hide their experiences, withdraw and the disease is aggravated.
Teenagers show signs of OCD. Without treatment, the disease is almost always complicated by an anxiety-depressive disorder, manifested by gloom, lack of interest in any activity, depression, and a desire for loneliness. In advanced cases, social disadaptation occurs, the child thinks about suicide, injures himself: scratches the skin, burns it.
All symptoms of neurosis are usually divided into two large groups: obsessions and compulsions.
Obsessive-compulsive disorder in children: obsessions
Obsessions are called ridiculous obsessive thoughts, images that appear against the will of a person. Usually they scare, as they are associated with health, well-being, the life of parents and other loved ones. The obsessive child is aware of the absurdity of thoughts, but cannot get rid of them.
Table 2. Main types of childhood obsessions
| Obsessions | Features |
| obsessive thoughts | Constantly pondering different questions, sometimes completely ridiculous, for example: "Man is a robot. |
| obsessive score | Continuous counting of everything that is possible: met red cars, steps taken, birds, dogs met. |
| obsessive fears | Very different: get sick, choke, get infected, meet a monster, be left without parents. |
| haunting memories | Painfully remind of an unpleasant event, which is accompanied by a sense of shame. |
| obsessive attraction | A constant desire to do something, more often condemned or unworthy: to spit at a person, insult him, say a swear word. In this case, thoughts are never realized. |
| obsessive doubts | He double-checks a hundred times: whether he turned off the light, whether he put the book in his briefcase. |
Compulsions help the patient to get rid of obsessions.
Obsessive-compulsive disorders in children: compulsions
Compulsions are called certain actions that help get rid of obsessions. Rituals reduce anxiety, stress. They do not last long, so without treatment, compulsive children perform rituals almost continuously.
Table 3. Examples of rituals
| Compulsions | What fear is associated with |
| Constantly thoroughly washes his hands, constantly cleans the room. | Infections, feelings of uncleanliness. |
| Endlessly sends SMS, calls, reads prayers, whispers spells. | To be left without parents or a significant person. |
| Often double-checks whether the tap is closed, the drawer of the table, whether the backpack is packed. | Do something wrong. |
| Folds things in a special way, wears the same clothes. | Fear of the realization of a bad event. |
| Accumulates rubbish in the room. | Fear of losing what the future may require. |
Causes of OCD
The causes of the disease are unknown. Scientists talk about biological and mental factors associated with the development of obsessive-compulsive disorder.
- Biological factors: structural features of the central nervous system, impaired metabolism of neurotransmitters, genetic characteristics, infection.
- Mental factors: development of an internal personality conflict, violation of interpersonal relationships.
Table 4. Theories of the emergence of neurosis
| Theory | Essence |
| Psychoanalytic | Conflict of internal and external installations. |
| Pavlova I.P. | Neurosis develops in people of a mental and artistic warehouse. |
| genetic | The disease develops in people with certain characterological features. |
| psychological trauma | Severe stress affects the functioning of the brain. |
| Social impact | Excessive severity and restrictions in any manifestation. |
Parents should be aware that OCD is caused by an imbalance of chemicals in the brain. The disease does not occur as a result of poor parenting or exposure to stress. You can not blame the child for bad behavior, lack of willpower - he cannot control himself.
Compulsions significantly disrupt the normal behavior of a person, turn him off from social life, and do not allow him to reveal his creative, intellectual potential. In adults, continuous compulsions can lead to disability.
In adults, continuous compulsions can lead to disability.
Diagnosis
The diagnosis is established by a pediatric psychiatrist on the basis of conversations with parents and the child, filling out questionnaires, testing, interpreting drawings, observing in the game and other methods that allow to determine the characterological personality traits, behavior and reactions, and identify problems. The presence of a more serious pathology, manifested by similar symptoms, including schizophrenia, is excluded.
Table 5. Diseases and conditions that may resemble OCD
| Disease or condition | Features |
| Normal Rituals | All ordinary children have rituals. So, before falling asleep, the child washes, brushes his teeth, puts on pajamas, listens to his mother reading a book, turns off the light. |
| ASD - autism spectrum disorders | Violations of socialization and intellect are added to the rituals. |
| Tourette syndrome | The main manifestation is tics, but their cause is not OCD. |
| Anorexia | All obsessive thoughts are related to food, a person avoids food, considering it to be dirt that stains the body. May be combined with OCD. |
| Schizophrenia | The patient perceives thoughts and actions as imposed from outside. He hears voices ordering him to do something. |
Treatment methods for OCD at the Family Doctor Clinic
When OCD is confirmed in children, complex treatment is carried out, consisting of two blocks.
- Psychotherapy. Different types of influence are used. The doctor teaches the patient to identify erroneous and illogical thoughts, to replace them with constructive ones.
- Drug therapy allows you to quickly stop the vivid manifestations of obsessions and compulsions. Certain types of antidepressants and antipsychotics are prescribed.
It is important to understand that the treatment lasts a long time, requires careful adherence to the recommendations of a specialist. Only in this case is it possible to completely get rid of OCD.
To make an appointment with a child and adolescent psychotherapist and clarify the cost of a doctor’s appointment, contact the Family Doctor clinic by calling the unified contact center in Moscow +7 (495) 775 75 66, use the online doctor appointment service or contact the clinic’s receptionist.
Information verified and confirmed by a pediatric psychotherapist at the Family Doctor clinic
Psychotherapists
About the doctor Record
Maksim Alekseevich Makhov
psychiatrist, psychotherapist
Clinic on Ozerkovskaya
About the doctor
Clinic on Novoslobodskaya
leave feedback
Treatment of childhood obsessive-compulsive disorder OCD in Israel
Obsessive-compulsive disorder (OCD) is also known as obsessive-compulsive disorder.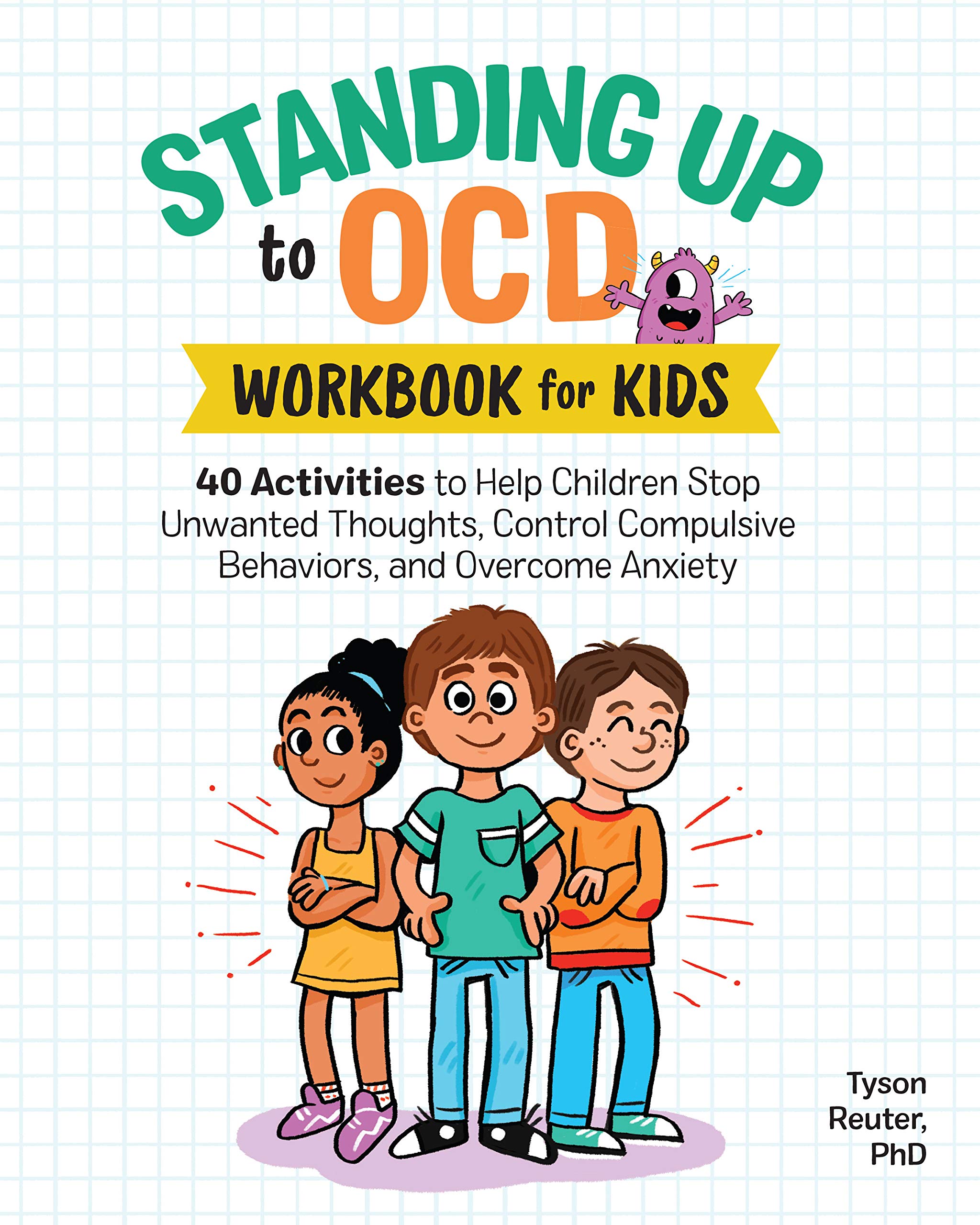 This disorder affects 1% to 4% of children. About half of cases begin in childhood and continue into adulthood.
This disorder affects 1% to 4% of children. About half of cases begin in childhood and continue into adulthood.
Anxiety is observed in children suffering from OCD, which manifests itself in a pronounced need to organize the world around them in a special way. They ask to retell what they have already been told many times, or to play the same game many times.
[SLIDER=1661]
R&D includes 2 components:
-
Obsessions or obsessions. The child constantly pronounces the same thought, returns to the same memories - both in the form of visual images and in the form of inner speech. The child may be constantly disturbed by the obsessive thought of pollution. He constantly wants to wash, avoid dirty places. He may require strict order in the house, symmetry in the arrangement of objects. If something is disturbed in his habits, this causes increased anxiety. The child may also be concerned about their own health and the health of their loved ones.
-
Compulsive actions or obsessive behavior is the second component of the syndrome. We are talking about repetitive behavioral rituals, which must be observed strictly in a strict order, otherwise, according to the patient, something bad may happen. Such rituals include constantly washing hands, touching certain things in a certain order with the hands, and much more. It should be noted that children, unlike adult patients, try to tell their parents about their rituals, which increases the chances of recovery. Unfortunately, parents do not always listen to children's experiences, and this contributes to the further development of the disorder.
When diagnosing obsessive-compulsive disorder, the Matspen Center conducts a comprehensive study of the patient's mental state to identify or exclude another concomitant disease. A complete physical examination of the patient is also carried out in order to determine contraindications to certain medications, as well as to establish possible physical prerequisites for the development of OCD.
 " Sometimes the last phrase you read or heard begins to spin endlessly in your head.
" Sometimes the last phrase you read or heard begins to spin endlessly in your head. 

 Rituals can be accompanied by, for example, children's games, collecting toys. Such rituals are useful, they contribute to adaptation and socialization. It is important that they change over time, exactly meet the needs of a particular age.
Rituals can be accompanied by, for example, children's games, collecting toys. Such rituals are useful, they contribute to adaptation and socialization. It is important that they change over time, exactly meet the needs of a particular age.