Hit and run ocd help
Hit and Run OCD? Overview, Symptoms and Treatment Options
All types of OCD include obsessions and compulsions. Obsessions are unwanted and intrusive thoughts, feelings, urges and doubts, while compulsions are repetitive physical or mental actions performed in an attempt to relieve distress and anxiety
Obsessive-compulsive disorder (OCD) is a common disorder in which a person experiences intrusive thoughts (obsessions) and engages in ritualistic behaviors (compulsions) to alleviate the distress caused by the intrusive thoughts.
Hit-and-run OCD is a subtype of OCD in which someone experiences obsessions centering on hitting a pedestrian or animal while driving, or feeling as if they already hit a pedestrian or animal and can’t remember the accident. Sometimes, the intrusive thoughts may happen subconsciously, and it’s not until the person is done driving that they realize they were afraid they were going to hit something the entire time.
This can be a less common subtype of OCD, and it may fall under the umbrella of harm OCD, with specific manifestations related to driving. No matter the roots of hit-and-run OCD, it can be an extremely overwhelming disorder to live with. If you feel you may have this form of OCD, read on to learn more about its symptoms and available treatment options.
What are some symptoms of hit-and-run OCD?
Do you fear driving because you worry you’ll hit a cyclist? Do you avoid more congested streets for fear of harming someone with your vehicle? Have you spent time wondering “Did I hit someone while driving?” or, “Are those sirens going by for a person I accidentally hit?” Do you often feel the need to drive back to intersections or other areas to check if you might’ve injured or killed someone with your vehicle?
These are just some of the symptoms you may experience with hit-and-run OCD.
Your intrusive thoughts may be prompted simply by driving at all, or they may be brought on by certain situations, such as:
- Looking down at your radio for a moment
- Running over litter in the road
- Hitting a pothole
- Hearing sirens or brake screeches nearby
- Driving on a busy road or past a cyclist or jogger
- Noticing you zoned out for a moment while driving
Once you have been triggered, a cycle of obsessions will begin that may make you feel convinced you will actually hit someone or an animal or that you already have and can’t remember it. The uncertainty may lead you to engage in compulsions to seek out a sense of clarity or to simply comfort yourself.
The uncertainty may lead you to engage in compulsions to seek out a sense of clarity or to simply comfort yourself.
Compulsions associated with hit-and-run OCD may include:
- Listening to police radio scans
- Going back to where you had been driving to check if there’s an accident/harmed person
- Avoiding driving at night or in crowded areas
- Avoiding driving altogether
- Asking nearby people if they saw someone get hit
- Looking for accident reports in news media
- Driving extra slowly
Oftentimes, your compulsions will only offer temporary relief, and you will find yourself repeating the same obsessive-compulsive cycle with no end in sight. This can be extremely frustrating and may feel as if you’ll never be able to drive peacefully again. Luckily, with treatment, you can gain control over your symptoms and find freedom from the seemingly endless cycle of obsessions and compulsions.
How is hit-and-run OCD treated?
Although this manifestation of OCD may be less common, it can still be treated just as effectively as many other subtypes. The recommended treatment option for all types of OCD is a form of cognitive behavioral therapy called exposure and response prevention (ERP) therapy.
The recommended treatment option for all types of OCD is a form of cognitive behavioral therapy called exposure and response prevention (ERP) therapy.
ERP works by exposing you to the things that trigger your obsessive-compulsive cycles. Your therapist may have you practice driving in situations you tend to avoid or write exposure “scripts” exploring the uncertainty you’ve felt in previous driving situations. By experiencing your intrusive thoughts with guidance from your therapist, you can practice resisting your compulsions. Your therapist will work with you to become more tolerant of the distress your obsessions cause by sitting with the uncertainty.
Over time, you will feel more capable of enduring the uncertainty without the need to engage in your compulsions.
How can I begin treatment of hit-and-run OCD?
Finding the right therapist for you has been made easier than ever thanks to NOCD’s virtual treatment options. Available nationwide, our therapists specialize in the treatment of OCD using ERP therapy, and you can get started today with a free call to our clinical team.
Once we match you with a therapist, you can start sessions quickly and from the comfort of your home. We offer teletherapy options where you can complete ERP sessions virtually over a video or phone call. Over time, you can learn how to resist your compulsions and feel more at peace while driving.
International OCD Foundation | Driven To Distraction: “Hit And Run OCD”
By Fred Penzel, PhD
This article was initially published in the Winter 2015 edition of the OCD Newsletter.
“Doc,” began Don, a 35-year-old school teacher, “I told my wife we should sell my car because I just can’t drive any more. Every time I go anywhere, I keep thinking that I’m hitting people with my car. It could be a jogger, a pedestrian, someone on a bike, or even an animal. I have to stop to get out and check for whoever it was I hit, or else I have to drive around the block twenty times. I keep looking in the rearview mirror so much of the time that I’m afraid I really will get into an accident. I listen to the news and read the paper every day to see if there were any accidents near where I was with my car. If I hear a siren or see a cop car or an ambulance, I think they are going to the spot where I killed someone. It’s like I can never be sure.”
I listen to the news and read the paper every day to see if there were any accidents near where I was with my car. If I hear a siren or see a cop car or an ambulance, I think they are going to the spot where I killed someone. It’s like I can never be sure.”
Don looked as if he was in genuine physical pain. Speaking mostly to the floor, he said, “You must think I’m really insane, and I’m not so sure that it isn’t true.”
Although this was only our first session, it was already apparent that Don was clearly describing a case of OCD. There are many varieties of OCD. People have even given nicknames to some of them. Don’s type specifically is referred to by some as “Hit and Run OCD.”
It is important to understand that OCD can make a person uncertain about the most basic things that they think, see, hear, touch, or experience otherwise. In the nineteenth century, it was known as “The Doubting Disease.” Hit and run obsessions fall under a subgroup of doubts about having harmed others through some kind of negligence. In this particular case, it seems to pick on people’s driving, making them wonder whether they have hit someone or run someone over, even if there is no real evidence that this has happened. Some particular situations can be more challenging than others, including:
In this particular case, it seems to pick on people’s driving, making them wonder whether they have hit someone or run someone over, even if there is no real evidence that this has happened. Some particular situations can be more challenging than others, including:
- Driving on a street with a lot of pedestrians crossing back and forth
- Driving down a poorly lit road at night
- Cruising around a busy parking lot
- Driving over bumps or potholes in the road
- Running over a piece of trash in the street
- Going over a bump or an irregular patch of pavement
- Briefly focusing (even for a second or two) on such things as the car’s instrument panel or entertainment system instead of the road ahead (“I could have hit someone when not paying attention”)
- Driving past a jogger or bicyclist
- Backing out of a driveway or a parking space
- Looking back in the rearview mirror and not seeing someone they thought they just passed
- Hearing the screech of brakes nearby
- Having an animal run in front of or past the car
These types of situations lead to sufferers experiencing typical repetitive obsessional thoughts such as:
- How can I tell if I actually hit someone? Would I see it? Would I hear it or feel it? Maybe I did hit someone.
- How do I know I didn’t kill someone? Would I know it, and how can I be certain?
- If I did hit someone and didn’t stop and take responsibility, will I be charged with leaving the scene of an accident?
- If I’m this doubtful, I must have been driving carelessly and am clearly at fault if I did hit someone.
- What if I go to jail? What will happen to my family? Their suffering will also be my fault.
- How could I ever live with the guilt of having taken a life? I could never forgive myself. My life would be over.
- I just noticed that I may not have been fully paying attention the last few minutes while driving. Maybe this means I hit someone and am not aware of it.
Naturally, when a person is as doubtful as is the case with OCD sufferers, the only solution is to somehow find perfect certainty. This is not easy to do in an uncertain world, meaning sufferers will sometimes go to extraordinary lengths to know for sure whether they have done something bad. Along with this perfectionism can come another hallmark of OCD: guilt (as you can see from the above list of obsessions). Both of these can then lead to compulsions. Compulsions are anything a person does, mentally or physically, to rid themselves of the anxiety caused by the obsessions.
Along with this perfectionism can come another hallmark of OCD: guilt (as you can see from the above list of obsessions). Both of these can then lead to compulsions. Compulsions are anything a person does, mentally or physically, to rid themselves of the anxiety caused by the obsessions.
Types of compulsions often carried out by Hit and Run OCD sufferers include:
- Driving around the block numerous times after backing out of a driveway to see if anyone is lying there
- Repeatedly driving up and down the same stretch of road looking for bodies
- Getting out of the car and checking in bushes or under parked cars along the road in case a victim was flung there
- Constantly checking the rearview mirror while driving to see if anyone is lying in the road
- Asking passengers or bystanders if someone was hit by the driver
- Reading news articles in the next day’s paper after a possible incident, looking for accident reports
- Listening to news reports of accidents
- Calling the local police precinct or hospital to find out if any accidents were reported in a particular area they drove in
- Walking all around and inspecting the car many times after a possible accident looking for dents, bloodstains, etc.
 that would prove that someone was hit
that would prove that someone was hit - Avoiding driving at night or in crowded areas
- Driving extra slowly
- Trying to mentally review each moment of a possible accident event in order to determine what actually happened
- Leaving notes on people’s cars just in case they (the driver) accidentally damaged them
As it turned out, Don had many of the above worries and performed many of the listed compulsions. I explained to Don that there was no running from or canceling out this kind of doubt. Trying to not think about these things would only cause him to think about them more. His attempts to do so had not worked thus far, and it was clear that they never would. I also related that the only way to overcome his fear was to face it — through exposure and response prevention therapy (ERP) — and that this was true of many fears. He told me, “I don’t know if it’s possible. The thoughts seem so real, and this thing seems bigger than me.” I asked him to have a little faith in himself and in the method, which had worked for many people in the past, including those with his symptoms.
“If you do your ERP homework and work patiently,” I said, “we’ll have you driving again.” Luckily, he was willing to give it a try, having run out of any other options. Because his anxiety was so high, I also referred him to a local psychiatrist who prescribed an SSRI-type antidepressant, Lexapro. The purpose of medication in this case was to help Don’s willingness to try the therapy I was proposing.
After making a very detailed list of all of Don’s obsessions and compulsions, we went on to make what is called a “hierarchy.” We did this by making a separate list of all the situations we could think of that related to his OCD that made him anxious. He then rated each one of these situations from 0 to 100 in terms of how anxious they could potentially make him. He had a fairly large range, with some things being as low as a 10 and several rated as 100 — the worst fear he could imagine experiencing.
Once this list was completed, we began the work of ERP therapy, which consisted of giving Don homework assignments starting with the lowest rated items on his hierarchy list. The assignments involved having him face situations that would cause him to confront his fears in a gradual way, and then work his way up to more and more challenging work. The purpose of this was to help him develop a tolerance for the doubt created by his thoughts so as to reduce their impact and thus, reduce the anxiety they caused. It was also for the purpose of learning the truth of what would happen when he didn’t do the compulsion. Further, it helped weaken the habits he had developed around doing his compulsions so that he could more successfully resist them. His assignments included such things as:
The assignments involved having him face situations that would cause him to confront his fears in a gradual way, and then work his way up to more and more challenging work. The purpose of this was to help him develop a tolerance for the doubt created by his thoughts so as to reduce their impact and thus, reduce the anxiety they caused. It was also for the purpose of learning the truth of what would happen when he didn’t do the compulsion. Further, it helped weaken the habits he had developed around doing his compulsions so that he could more successfully resist them. His assignments included such things as:
- Backing out of his driveway and then leaving his block without driving back to check or checking his rearview mirror
- Not seeking reassurance from others
- Resisting inspecting his car after going out for a drive
- Not checking the news for accident reports
- Not calling the police to question them about accident reports
- Driving around crowded streets and parking lots without going back or checking in any way, especially at night when possible
- Never stopping to get out and check for bodies
In addition to changing his behavior, I asked Don to consider responding to his obsessions in his head differently as well. For example:
For example:
- Refraining from reviewing past driving events, agreeing instead that he might have actually hit and killed someone
- Upon hearing sirens, agreeing with the obsession that it was emergency vehicles going to pick up the bodies of those he had hit
- Generally agreeing with any thoughts of having hit people or animals
And finally to go out of his way to actively trigger the obsessions as a way to confront them by:
- Reading articles about hit-and-run drivers being convicted and going to jail
- Watching videos of cars hitting people
- Viewing ads and reading articles on the hazards of distracted driving
It took Don eight months of steady daily work to finally gain control of his symptoms and to drive normally again. There were both good and difficult days along the way. No one gets well perfectly. “I feel like I got my life back,” Don said. “I’m really glad we didn’t sell that car.”
Post-traumatic stress disorder is the only mental disorder whose causes can be traced. PTSD is always triggered by a traumatic event and can be accompanied by symptoms ranging from irritability to amnesia. This disease can last for years and decades, but modern techniques help get rid of traumatic memories and their consequences in just 3 months of psychotherapy. nine0003
PTSD is always triggered by a traumatic event and can be accompanied by symptoms ranging from irritability to amnesia. This disease can last for years and decades, but modern techniques help get rid of traumatic memories and their consequences in just 3 months of psychotherapy. nine0003
Why doesn't everyone develop PTSD?
There is a misconception that post-traumatic stress disorder occurs only in those who have participated in hostilities or terrorist attacks. But PTSD can develop due to any event that poses a real threat to life or the integrity of the psyche. For example, if a person was covered while swimming by a wave, and he almost choked, or because of an attack by bandits in a dark alley, or, for example, as a result of an accident. In war, traumatic situations are quite common, but participation in an accident can cause no less serious damage to the psyche than participation in hostilities. nine0003
For PTSD to occur, there must be an objective threat to a person's life, or at least to his psyche or the integrity of his personality.

For most people, negative events are completely erased from memory. After traumatic situations, PTSD develops in only 3-5% of the world's population. The normal reaction of the brain in such a situation is to stay alert for several hours or days, then make sure that the traumatic situation does not repeat itself, and exit this state. But in 3-5% of people, the brain for some reason forgets to relax and continues to expect a recurrence of the traumatic event. There is a mechanism of constant reminder that a person is in danger. nine0003
For the occurrence of PTSD, there must be an objective threat to a person's life, or at least to his psyche or the integrity of his personality. For example, a situation of uncertainty can violate the integrity of the psyche when a person is taken hostage. He doesn't know what will happen to him, whether he dies or not. PTSD can occur as a result of both immediate and prolonged fear of the unknown. It happens that for a certain period of time in a person's life there are many traumatic situations. For example, such a fear of the unknown may arise in a child who grows up in a family where he is regularly beaten. nine0003
For example, such a fear of the unknown may arise in a child who grows up in a family where he is regularly beaten. nine0003
See also
What is PTSD
How do PTSD symptoms take root?
Manifestations of post-traumatic stress disorder, as a rule, begin to occur with the first traumatic situation. The human brain, like any mammal, reacts to a threat to life according to the principle “fight, run or freeze” - this is the basic evolutionary principle of protection, according to which a living being at the moment of danger on an instinctive unconscious level quickly decides what to do - fight, run away or fall into a stupor. The brain develops this reaction, protecting itself from the events of the external world that threaten life, and this protection is formed at the level of conditioned and unconditioned reflexes. When a dangerous situation passes, the brain does not know that it has passed - it assumes, based on previous events, that similar situations will continue to occur. Because of this, the body is constantly under stress, it is on the alert - and makes it continue to live on the basis of "fight, flight or freeze." In ordinary life, this can manifest itself in the form of symptoms of PTSD, for example, increased irritability or, conversely, excessive closeness and withdrawal into oneself. nine0003
Because of this, the body is constantly under stress, it is on the alert - and makes it continue to live on the basis of "fight, flight or freeze." In ordinary life, this can manifest itself in the form of symptoms of PTSD, for example, increased irritability or, conversely, excessive closeness and withdrawal into oneself. nine0003
Trauma causes a huge surge of negative emotions, but it is this surge that gives rise to an acute desire to live in a person.
There is an assumption that what symptoms of PTSD a person develops directly depends on what kind of reaction he “chooses” during the traumatic event. That is, for example, if during the attack of bandits a person tried to escape from the offenders, there is a high probability that after this situation he will withdraw into himself and in every possible way will avoid dark alleys. Over time, these symptoms get fixed and take root deeper, developing into post-traumatic stress disorder. And if traumatic situations are repeated over and over again, then they further intensify these symptoms and feed the formed emotional and physiological reactions. nine0003
nine0003
See also
Mental norm and pathology
How does trauma become the meaning of life?
As a rule, life before and after a traumatic event is very different. Trauma causes a huge surge of negative emotions, but it is this surge that gives rise to an acute desire to live in a person. Before a traumatic event, a person may simply not think about the importance of life, and the instinct of self-preservation during the trauma focuses his attention on this. When strong emotions recede after a traumatic event, a person returns to everyday life and, against the background of that surge, begins to feel empty. He wants to return to strong emotions again, to feel them again, even though they were extremely negative. That is why many people are not ready to part with their traumatic memories, because returning to them, they feel alive again. nine0003
However, for those who choose to seek treatment for PTSD, the process of symptom relief is short-lived. PTSD can be chronic, advanced, and last 20-30 years, but it can be cured in just a few appointments with a specialist using targeted therapy without the use of drugs.
PTSD can be chronic, advanced, and last 20-30 years, but it can be cured in just a few appointments with a specialist using targeted therapy without the use of drugs.
- Diseases and disorders
Share:
ChRDM COO BEY-BEGI, Anadyr (TIN 870
07), details, extract from the Unified State Register of Legal Entities, address, mail, website, telephone, financial indicatorsRefresh browser
Refresh browser
Opportunities
Integration
About the system
Statistics nine0003
Contacts
CfDJ8HJyMSOWarhLkJBDZs2NT-Gi6_5-gJd2Jw-ogkPHp0zbBWx2cUFyOhKxjvR9ogqgqiTP8rERzeHSYNqKCINCBVbNukr8yWqJak4Cj9Yg8kkJ1rk8HE1Jx73QgkSNhitnoKMyIzOSFgpWUjv
Description of the search engine
search encyclopedia
TIN
OGRN
Sanction lists nine0003
Company search
Head of the organization
Court cases
Affiliation Check
Execution proceedings
Organization details
Information about the beneficiaries
Organization's current account nine0003
Credit risk assessment
Checking the blocking of the current account
Number of employees
Authorized capital of the organization
Bankruptcy check
Date of registration
Checking the counterparty by TIN
checkpoint nine0003
OKPO
Tenders and public procurement
Customer search (B2B)
Legal address
Analysis of the financial condition
Organization founders
Financial statements
OKTMO
OKVED
Company Comparison
Trademark Check
License check
Extract from the Unified State Register of Legal Entities
Competitor analysis
Organization website
OKOPF
Registration Information nine0003
OKFS
Branches and representative offices
OKOGU
OKATO
Register of dishonest suppliers
Company rating
Check yourself and the counterparty
due diligence nine0003
Banking licenses
Scoring of counterparties
Alcohol licenses
Media monitoring
Signs of economic activity
Reputational risks
Compliance
nine0006 DetailsThe full name of the organization
Chukotsk regional children's and youth sports public organization "Bay-Bugi"
English name
ChRDM Soo "Bei-Begi"
Addles
Chukotsky OKR, ul. Stroiteley, 9
Stroiteley, 9
OKFS
Property of public associations
OKOPF
Public organizations
OKOGU
Regional and local public associations
TIN
870
07OGRN
1118700000100
KPP
870
1Chukuto Autonomous District, Anadyr
OKPO
76995652
OKTMO
Chukotka Autonomous Okrug, Urban districts of Chukotka Autonomous Okrug, Anadyr
Phone
E-mail
No information nine0003
Website
No information
Company information
Manager
Rozhiy Ivan Ivanovich, Chairman *Size of the enterprise
Number of employees
Branches
Data without updates available in the SPARK system.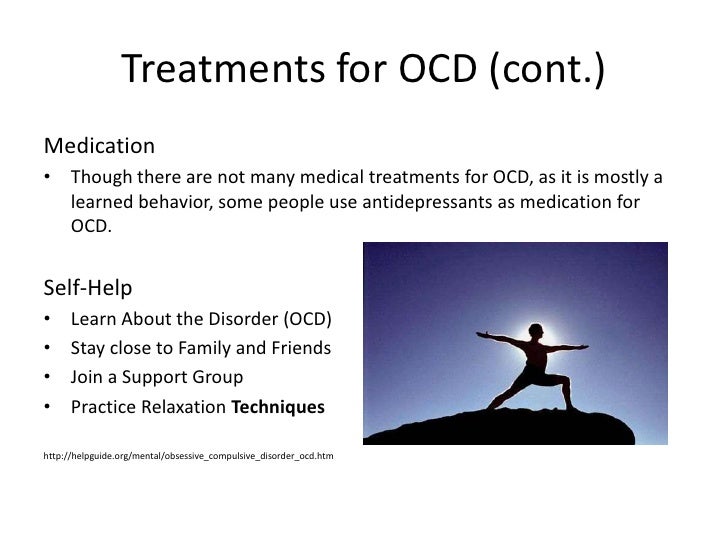
For up-to-date data - . nine0003
Information on state registration
Date of registration
03/30/2011
Registration authority
Federal Tax Service of Russia for Chukotka Autonomous Okrug
Address of the registration authority
689000 Energetikov, 14
Registration authority where the registration file is located
Federal Tax Service Administration for the Chukotka Autonomous Okrug
Types of activity
Main activity according to OKVED
Activities of other public organizations not included in other groups
Description
Company CHRDM SOO BAY-BEGI, address: Chukotka region, Anadyr, st. Stroiteley, d. 9 was registered on 03/30/2011. The organization was assigned TIN 870
07, OGRN 1118700000100, KPP 8701. The main activity is the activity of other public organizations not included in other groups, in total 1 type of activity is registered according to OKVED. There are no connections with other companies. nine0021 Chairman - Rozhiy Ivan Ivanovich.
There are no connections with other companies. nine0021 Chairman - Rozhiy Ivan Ivanovich. CHRD SOO BAY-BEGI did not take part in tenders. 4 enforcement proceedings were initiated against the company. CHRD SOO BAY-BEGI did not participate in arbitration cases.
Requisites CHRD SOO BEY-BEGI, legal address, official website and extract from the Unified State Register of Legal Entities are available in the SPARK system (demo access is free).
Company status
Complete information about the company CHRD SOO BAY-BEGI
SPARK-Risks
One-page report with the most important information from SPARK
299₽
- Company registration data
- Manager and main owners
- Contact information
- Risk factors
- Signs of economic activity
- Key financial indicators in dynamics
- Check according to the registers of the Federal Tax Service
Buy Example
SPARK-Profile
Full information report
from SPARK
999₽ nine0003
Yearly change monitoring enabled
- Company registration data
- History of changes in managers, names, addresses
- Full list of addresses, phone numbers, websites
- Data on co-owners from various sources
- Related companies nine0047 Activity details
- Financial statements for several years
- Financial assessment
Buy Example
Representative
of the company
for free
Your company? nine0284
Increase confidence
SPARK-Risks for 1C
Reliability assessment
and counterparty monitoring
Application for demo access
Applications with corporate email are processed faster.