Hallucinations lyme disease
Musical hallucinations in patients with Lyme disease
Case Reports
. 2003 Jul;96(7):711-5.
doi: 10.1097/01.SMJ.0000053458.21691.2E.
Raphael B Stricker 1 , Edward E Winger
Affiliations
Affiliation
- 1 Department of Medicine, California Pacific Medical Center, 450 Sutter Street, Suite 1504, San Francisco, CA 94108, USA. [email protected]
- PMID: 12940329
- DOI: 10.1097/01.SMJ.0000053458.21691.2E
Case Reports
Raphael B Stricker et al. South Med J. 2003 Jul.
. 2003 Jul;96(7):711-5.
doi: 10.1097/01.SMJ.0000053458.21691.2E.
Authors
Raphael B Stricker 1 , Edward E Winger
Affiliation
- 1 Department of Medicine, California Pacific Medical Center, 450 Sutter Street, Suite 1504, San Francisco, CA 94108, USA. [email protected]
- PMID: 12940329
- DOI: 10.1097/01.SMJ.0000053458.21691.2E
Abstract
Musical hallucinations are poorly understood auditory hallucinations that occur in patients with otologic or neurologic diseases.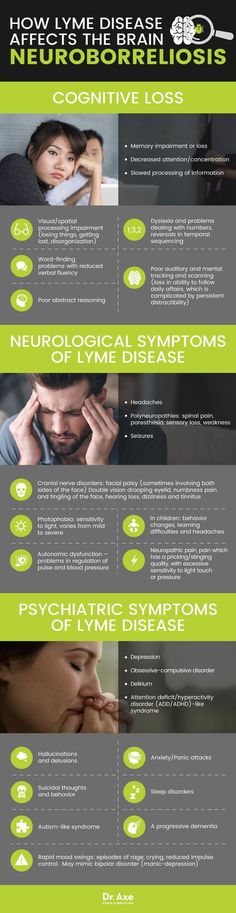 We report the first cases of musical hallucinations in two patients with neurologic Lyme disease. Both subjects were women with clinical and laboratory evidence of chronic Lyme disease, progressive neurologic dysfunction, and abnormal magnetic resonance imaging of the brain. There was no evidence of hearing loss in either case. Musical hallucinations had a sudden onset and took the form of patriotic or operatic music. The auditory hallucinations disappeared with intravenous (i.v.) antibiotic therapy in both patients, but the hallucinations recurred when i.v. antibiotic therapy was discontinued in one case. Response to therapy was accompanied by an increase in the CD57 lymphocyte subset in one patient, whereas recurrent hallucinations were associated with persistently low CD57 levels in the other case. We conclude that musical hallucinations may be associated with neurologic Lyme disease. These auditory hallucinations appear to respond to i.v. antibiotic therapy. Patients with musical hallucinations of unknown cause should be tested for infection with the Lyme disease spirochete.
We report the first cases of musical hallucinations in two patients with neurologic Lyme disease. Both subjects were women with clinical and laboratory evidence of chronic Lyme disease, progressive neurologic dysfunction, and abnormal magnetic resonance imaging of the brain. There was no evidence of hearing loss in either case. Musical hallucinations had a sudden onset and took the form of patriotic or operatic music. The auditory hallucinations disappeared with intravenous (i.v.) antibiotic therapy in both patients, but the hallucinations recurred when i.v. antibiotic therapy was discontinued in one case. Response to therapy was accompanied by an increase in the CD57 lymphocyte subset in one patient, whereas recurrent hallucinations were associated with persistently low CD57 levels in the other case. We conclude that musical hallucinations may be associated with neurologic Lyme disease. These auditory hallucinations appear to respond to i.v. antibiotic therapy. Patients with musical hallucinations of unknown cause should be tested for infection with the Lyme disease spirochete.
Similar articles
-
Lyme neuroborreliosis presenting as Alice in Wonderland syndrome.
Binalsheikh IM, Griesemer D, Wang S, Alvarez-Altalef R. Binalsheikh IM, et al. Pediatr Neurol. 2012 Mar;46(3):185-6. doi: 10.1016/j.pediatrneurol.2012.01.001. Pediatr Neurol. 2012. PMID: 22353296
-
Minds on replay: musical hallucinations and their relationship to neurological disease.
Golden EC, Josephs KA. Golden EC, et al. Brain. 2015 Dec;138(Pt 12):3793-802. doi: 10.1093/brain/awv286. Epub 2015 Oct 7. Brain. 2015. PMID: 26446167
-
Severe neuroborreliosis: The benefit of prolonged high-dose combination of antimicrobial agents with steroids--an illustrative case.
Massengo SA, Bonnet F, Braun C, Vital A, Beylot J, Bastard J. Massengo SA, et al. Diagn Microbiol Infect Dis. 2005 Feb;51(2):127-30. doi: 10.1016/j.diagmicrobio.2004.04.022. Diagn Microbiol Infect Dis. 2005. PMID: 15698718
-
Clinical aspects of neuroborreliosis and post-Lyme disease syndrome in adult patients.
Pfister HW, Rupprecht TA. Pfister HW, et al. Int J Med Microbiol. 2006 May;296 Suppl 40:11-6. doi: 10.1016/j.ijmm.2005.12.003. Epub 2006 Mar 9. Int J Med Microbiol. 2006. PMID: 16524775 Review.
-
Lyme disease associated with sudden sensorineural hearing loss: case report and literature review.
Peeters N, van der Kolk BY, Thijsen SF, Colnot DR. Peeters N, et al. Otol Neurotol.
 2013 Jul;34(5):832-7. doi: 10.1097/MAO.0b013e31827c9f93. Otol Neurotol. 2013. PMID: 23303170 Review.
2013 Jul;34(5):832-7. doi: 10.1097/MAO.0b013e31827c9f93. Otol Neurotol. 2013. PMID: 23303170 Review.
See all similar articles
Cited by
-
Neurological Pain, Psychological Symptoms, and Diagnostic Struggles among Patients with Tick-Borne Diseases.
Maxwell SP, Brooks C, McNeely CL, Thomas KC. Maxwell SP, et al. Healthcare (Basel). 2022 Jun 23;10(7):1178. doi: 10.3390/healthcare10071178. Healthcare (Basel). 2022. PMID: 35885705 Free PMC article.
-
The Emerging Role of Microbial Biofilm in Lyme Neuroborreliosis.
Di Domenico EG, Cavallo I, Bordignon V, D'Agosto G, Pontone M, Trento E, Gallo MT, Prignano G, Pimpinelli F, Toma L, Ensoli F. Di Domenico EG, et al.
 Front Neurol. 2018 Dec 3;9:1048. doi: 10.3389/fneur.2018.01048. eCollection 2018. Front Neurol. 2018. PMID: 30559713 Free PMC article. Review.
Front Neurol. 2018 Dec 3;9:1048. doi: 10.3389/fneur.2018.01048. eCollection 2018. Front Neurol. 2018. PMID: 30559713 Free PMC article. Review. -
Neuropsychiatric Lyme Borreliosis: An Overview with a Focus on a Specialty Psychiatrist's Clinical Practice.
Bransfield RC. Bransfield RC. Healthcare (Basel). 2018 Aug 25;6(3):104. doi: 10.3390/healthcare6030104. Healthcare (Basel). 2018. PMID: 30149626 Free PMC article. Review.
-
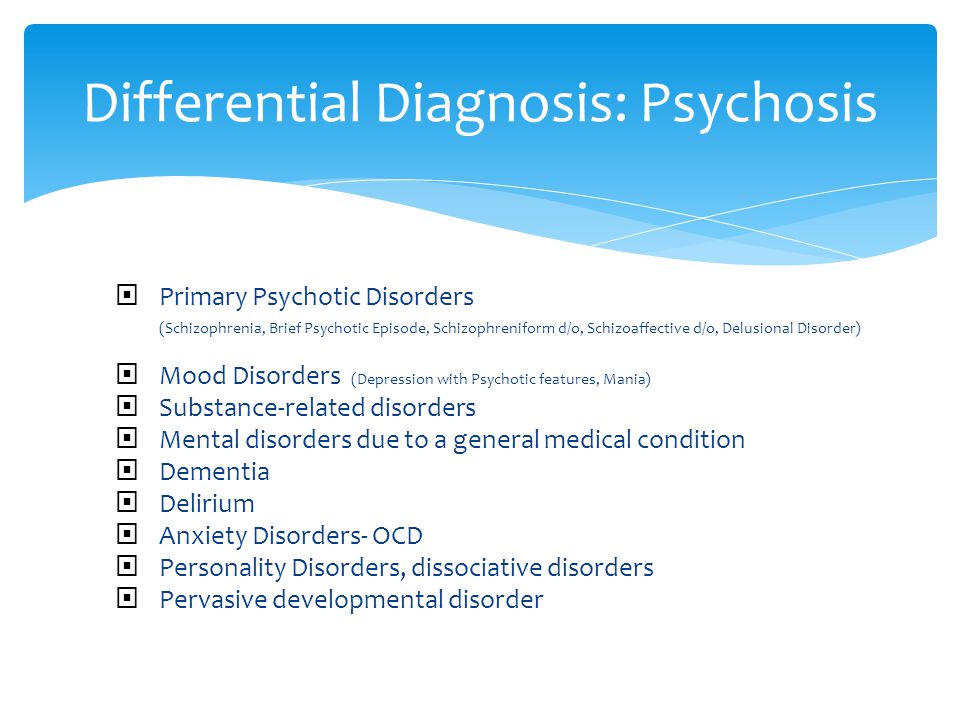
Diagnostic pitfalls in a young Romanian ranger with an acute psychotic episode.
Nagy EE, Rácz A, Urbán E, Terhes G, Berki T, Horváth E, Georgescu AM, Zaharia-Kézdi IE. Nagy EE, et al. Neuropsychiatr Dis Treat. 2016 May 3;12:961-7. doi: 10.2147/NDT.S103300. eCollection 2016.
 Neuropsychiatr Dis Treat. 2016. PMID: 27217753 Free PMC article.
Neuropsychiatr Dis Treat. 2016. PMID: 27217753 Free PMC article. -
Musical hallucinations: review of treatment effects.
Coebergh JA, Lauw RF, Bots R, Sommer IE, Blom JD. Coebergh JA, et al. Front Psychol. 2015 Jun 16;6:814. doi: 10.3389/fpsyg.2015.00814. eCollection 2015. Front Psychol. 2015. PMID: 26136708 Free PMC article. Review.
See all "Cited by" articles
Publication types
MeSH terms
Substances
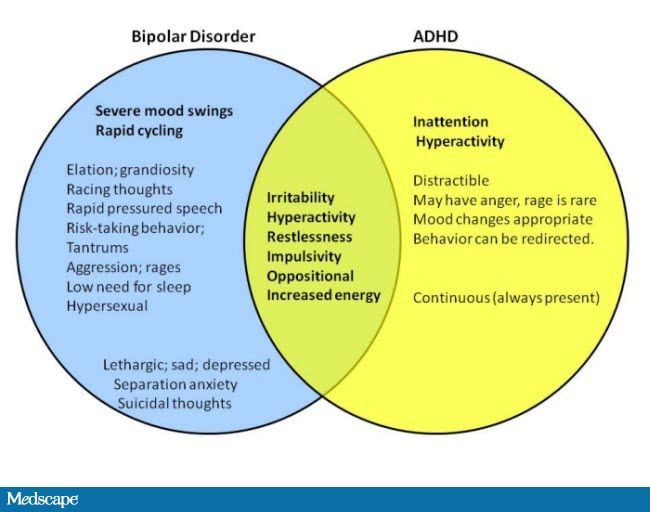
Association of Lyme Disease and Schizoaffective Disorder, Bipolar Type: Is it Inflammation Mediated?
1. Centers for Disease Control and Prevention. AtlantaLyme Disease Data. [Last accessed on Jan 2]. Available from: http://www.cdc.gov/Lyme/stats/
Centers for Disease Control and Prevention. AtlantaLyme Disease Data. [Last accessed on Jan 2]. Available from: http://www.cdc.gov/Lyme/stats/
2. Torrey EF, Bowler A. Geographical distribution of insanity in America: Evidence for an urban factor. Schizophr Bull. 1990;16:591–604. [PubMed] [Google Scholar]
3. Brown JS., Jr Geographic correlation of schizophrenia to ticks and tick-borne encephalitis. Schizophr Bull. 1994;20:755–75. [PubMed] [Google Scholar]
4. Bar KJ, Jochum T, Hager F, Meissner W, Sauer H. Painful hallucinations and somatic delusions in a patient with the possible diagnosis of neuroborreliosis. Clin J Pain. 2005;21:362–3. [PubMed] [Google Scholar]
5. Pasareanu AR, Mygland A, Kristensen Ø. A woman in her 50s with manic psychosis. Tidsskr Nor Laegeforen. 2012;132:537–9. [PubMed] [Google Scholar]
6. Hess A, Buchmann J, Zettl UK, Henschel S, Schlaefke D, Grau G, et al. Borreliaburgdorferi central nervous system infection presenting as an organic schizophrenialike disorder.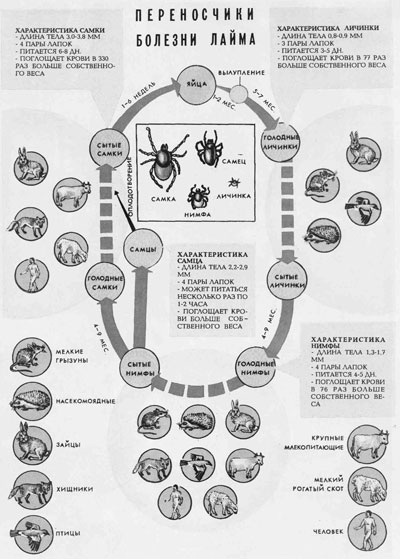 Biol Psychiatry. 1999;45:795. [PubMed] [Google Scholar]
Biol Psychiatry. 1999;45:795. [PubMed] [Google Scholar]
7. Earl AK, Sullivan KM, Warfel D, Feldman SM, Richardson CM, Vyas G, et al. Lyme disease and schizophrenia: Case studies from an adjunctive minocycline study. Schizophr Bull. 2013;39(Suppl 1):62–3. [Google Scholar]
8. Fallon BA, Nields JA. Lyme disease: A neuropsychiatric illness. Am J Psychiatry. 1994;151:1571–83. [PubMed] [Google Scholar]
9. Fallon BA, Nields JA, Parsons B, Liebowitz MR, Klein DF. Psychiatric manifestations of lymeborreliosis. J Clin Psychiatry. 1993;54:263–8. [PubMed] [Google Scholar]
10. Pfister HW, Preac-Mursic V, Wilske B, Rieder G, Förderreuther S, Schmidt S, et al. Catatonic syndrome in acute severe encephalitis due to Borreliaburgdorferi infection. Neurology. 1993;43:433–5. [PubMed] [Google Scholar]
11. Roelcke U, Barnett W, Wilder-Smith E, Sigmund D, Hacke W. Untreated neuroborreliosis: Bannwarth's syndrome evolving into acute schizophrenia-like psychosis. A case report. J Neurol.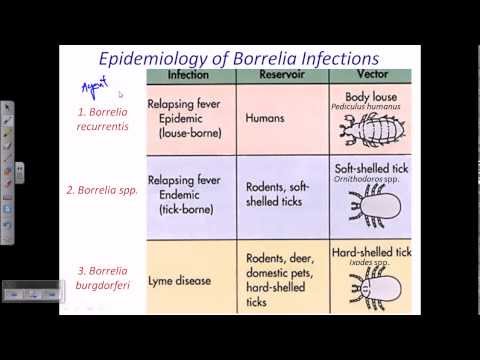 1992;239:129–31. [PubMed] [Google Scholar]
1992;239:129–31. [PubMed] [Google Scholar]
12. Diringer MN, Halperin JJ, Dattwyler RJ. Lyme meningoencephalitis: Report of a severe, penicillin-resistant case. Arthritis Rheum. 1987;30:705–8. [PubMed] [Google Scholar]
13. Reik L, Jr, Smith L, Khan A, Nelson W. Demyelinating encephalopathy in lyme disease. Neurology. 1985;35:267–9. [PubMed] [Google Scholar]
14. Burrascand J. Hartford, Conneticut: Lyme Disease Foundation; 1993. Lyme disease presenting as organic psychosis. Sixth annual Lyme disease scientific conference. [Google Scholar]
15. Schutzer S, editor. Cold Spring Harbor, NY: Cold Spring Harbor Laboratory Press; 1992. Lyme disease: Molecular and Immunologic Approaches. [Google Scholar]
16. Omasits M, Seiser A, Brainin M. Recurrent and relapsing course of borreliosis of the nervous system. Wien KlinWochenschr. 1990;102:4–12. [PubMed] [Google Scholar]
17. Pachner AR, Duray P, Steere AC. Central nervous system manifestations of lyme disease. Arch Neurol. 1989;46:790–5. [PubMed] [Google Scholar]
1989;46:790–5. [PubMed] [Google Scholar]
18. Bransfield RC. The psychoimmunology of lyme/tick-borne diseases and its association with neuropsychiatric symptoms. Open Neurol J. 2012;6:88–93. [PMC free article] [PubMed] [Google Scholar]
19. Falcone T, Carlton E, Franco K, Janigro D. Inflammation, psychosis, and the brain. Psychiatr Times. 2009;26:1–6. [Google Scholar]
20. Potvin S, Stip E, Sepehry AA, Gendron A, Bah R, Kouassi E. Inflammatory cytokine alterations in schizophrenia: A systematic quantitative review. Biol Psychiatry. 2008;63:801–8. [PubMed] [Google Scholar]
21. Miller BJ, Buckley P, Seabolt W, Mellor A, Kirkpatrick B. Meta-analysis of cytokine alterations in schizophrenia: Clinical status and antipsychotic effects. Biol Psychiatry. 2011;70:663–71. [PMC free article] [PubMed] [Google Scholar]
22. Gao HM, Hong JS. Why neurodegenerative diseases are progressive: Uncontrolled inflammation drives disease progression. Trends Immunol. 2008;29:357–65. [PMC free article] [PubMed] [Google Scholar]
23. Stertz L, Magalhães PV, Kapczinski F. Is bipolar disorder an inflammatory condition? The relevance of microglial activation. CurrOpin Psychiatry. 2013;26:19–26. [PubMed] [Google Scholar]
Stertz L, Magalhães PV, Kapczinski F. Is bipolar disorder an inflammatory condition? The relevance of microglial activation. CurrOpin Psychiatry. 2013;26:19–26. [PubMed] [Google Scholar]
24. Kirkpatrick B, Miller BJ. Inflammation and schizophrenia. Schizophr Bull. 2013;39:1174–9. [PMC free article] [PubMed] [Google Scholar]
25. Girgis RR, Kumar SS, Brown AS. The cytokine model of schizophrenia: Emerging therapeutic strategies. Biol Psychiatry. 2014;75:292–9. [PMC free article] [PubMed] [Google Scholar]
26. Dean OM, Data-Franco J, Giorlando F, Berk M. Minocycline: Therapeutic potential in psychiatry. CNS Drugs. 2012;26:391–401. [PubMed] [Google Scholar]
27. Keller WR, Kum LM, Wehring HJ, Koola MM, Buchanan RW, Kelly DL. A review of anti-inflammatory agents for symptoms of schizophrenia. J Psychopharmacol. 2013;27:337–42. [PMC free article] [PubMed] [Google Scholar]
28. Kelly DL, Vyas G, Richardson CM, Koola M, McMahon RP, Buchanan RW, et al. Adjunct minocycline to clozapine treated patients with persistent schizophrenia symptoms.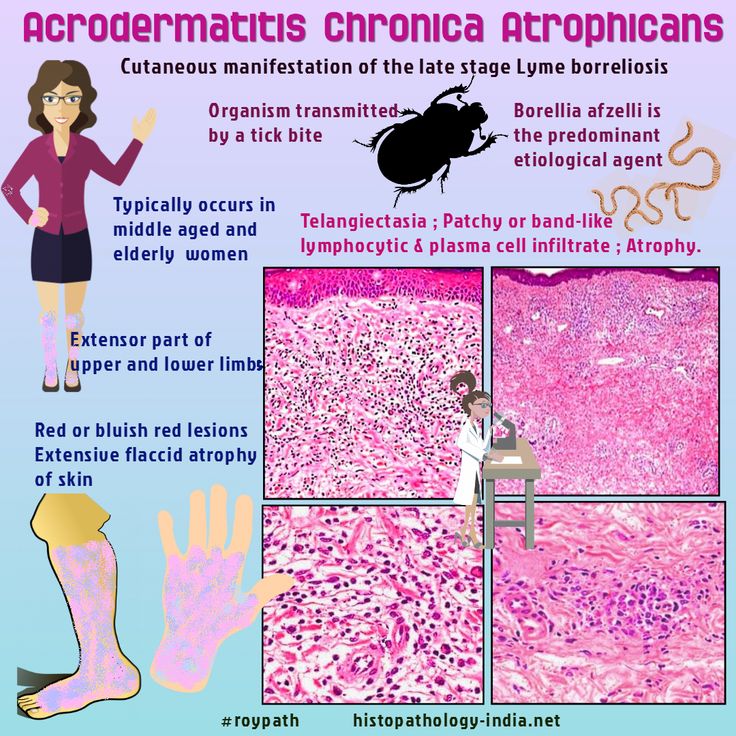 Schizophr Res. 2011;133:257–8. [PubMed] [Google Scholar]
Schizophr Res. 2011;133:257–8. [PubMed] [Google Scholar]
29. Hassett AL, Radvanski DC, Buyske S, Savage SV, Sigal LH. Psychiatric comorbidity and other psychological factors in patients with “chronic lyme disease” Am J Med. 2009;122:843–50. [PMC free article] [PubMed] [Google Scholar]
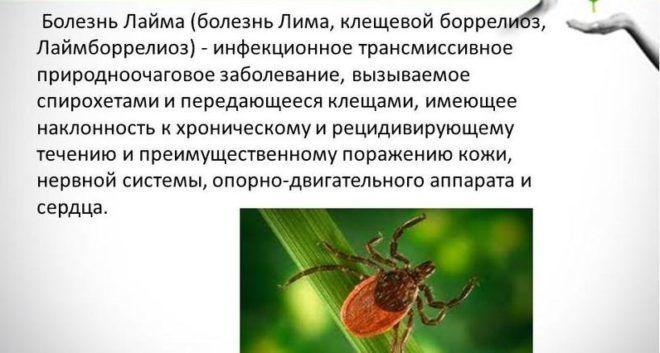
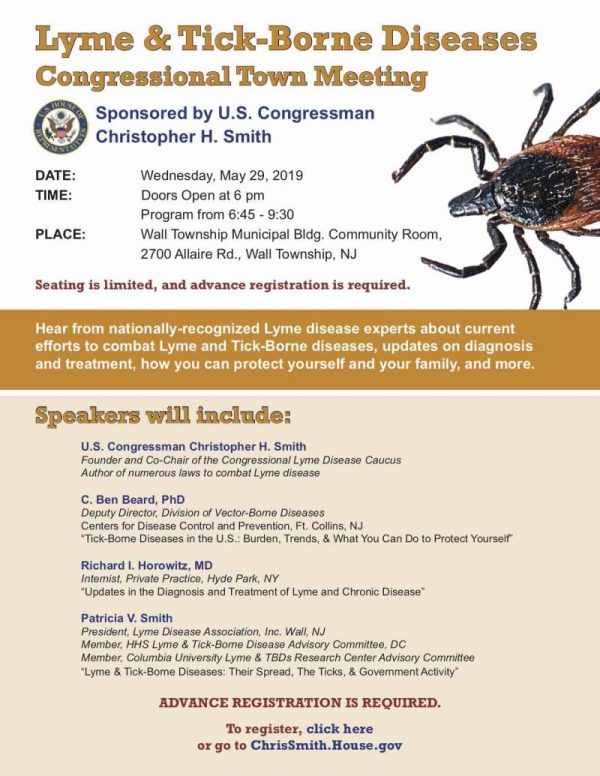
Lyme disease - treatment, symptoms, causes, diagnosis
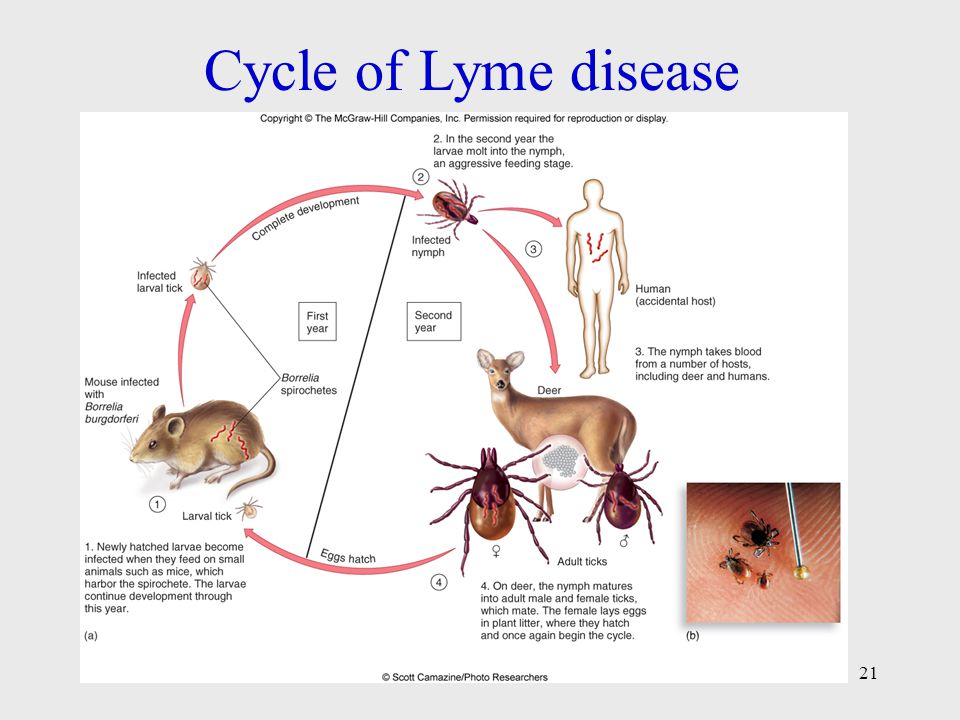
Lyme disease is a bacterial infection affecting all organs and systems caused by the spirochete borrelia burgdorferi. The microorganism was named after Willy Burgdorfer, a researcher of this disease, and the town of Lyme in the United States. Studies have shown that this infection has existed in the US for at least 100 years. The natural focus of infection is wild animals, in whose body this bacterium persists and is transmitted to other animals with tick bites. Humans and pets become infected with this bacterium through accidental bites. Unfortunately, a strong immunity to this infection does not develop, and it is possible to re-infect with accidental tick bites.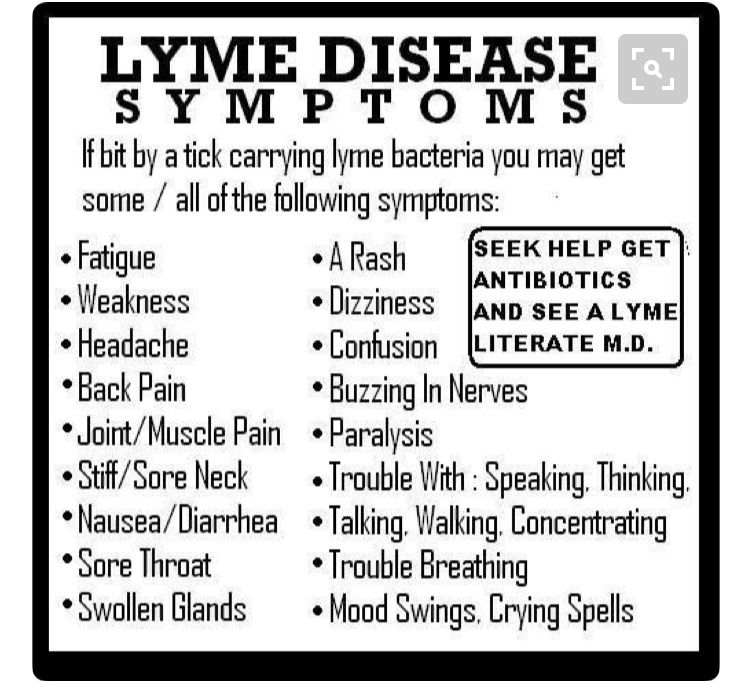 Lyme disease is transmitted through the bite of a tick.
Lyme disease is transmitted through the bite of a tick.
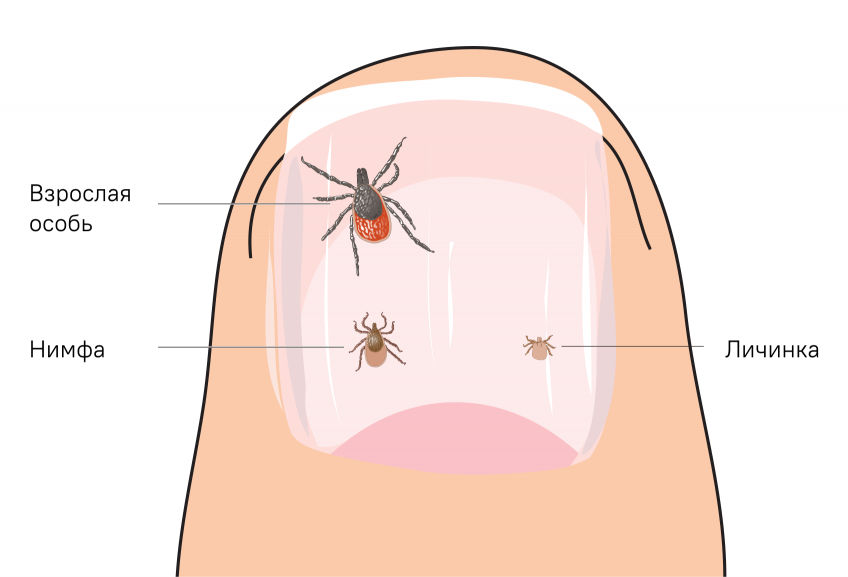
Ticks develop through four life stages: egg, larva, nymph, and adult. The transition from one stage to another is accompanied by a molting process that requires building material (blood). When a tick bites an animal infected with a microbe, it becomes infected, and the infection persists in the tick's body throughout the entire life cycle of the insect. But an adult tick does not transmit the infection to the next generations. Transmitters of infection in the USA are ticks from the Ixodes family (Ixodes pacificis, Ixodes scapularis, Ixodes dammini, etc.).
Other types of ticks play a minor role in the existence of natural foci of borreliosis, since recirculation between animals does not include humans. For example, we are talking about wood rat mites (Ixodes neotomae) and rabbit mites (Haemaphysalis leporispalustris), in which Lyme disease bacteria may be present, but they are not transmitted to humans. This is explained by the fact that ticks feed only on the blood of these animals.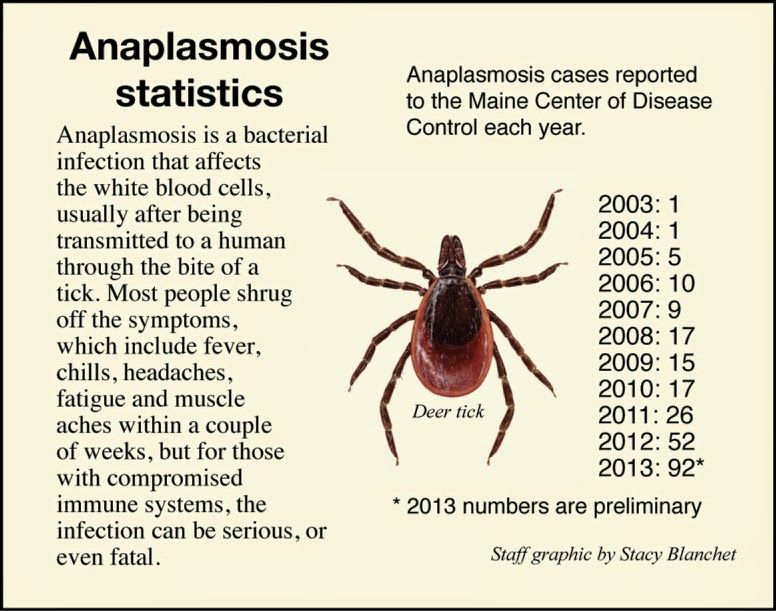
In other parts of the world, other ticks are involved in the transmission of borreliosis (in Europe it is the sheep tick (Ixodes ricinus), and in Asia the taiga tick (Ixodes persculcatus). These ticks are found everywhere (in the forest, on the seashore and even in courtyards of residential buildings)
While a tick can bite at any time of the year, the peak season for tick bites is April-September. Ticks can survive in a variety of weather conditions as long as there is sufficient moisture
Symptoms of Lyme disease.
The early symptoms of Lyme disease are similar to those of influenza: headache, fever, muscle pain, fatigue, stiff neck. Approximately 60% of fair-skinned patients develop a characteristic rash called erythema migrans (usually a few days after a tick bite). In patients with dark skin, these rashes look like a bruise.
The rash may appear within a day of the bite or a month later. This rash may look like a half-inch red spot raised above the skin surface in the form of a ring (normally colored skin in the center). But sometimes the rash can be large and occupy, for example, the entire back. It is necessary to distinguish small rashes from other possible skin lesions. As a rule, local skin damage is a reaction to trauma and usually disappears after a few days without causing general symptoms.
But sometimes the rash can be large and occupy, for example, the entire back. It is necessary to distinguish small rashes from other possible skin lesions. As a rule, local skin damage is a reaction to trauma and usually disappears after a few days without causing general symptoms.
Symptoms of disseminated infection.
Often, the patient does not notice the first signs of the disease, and there comes a period of involvement of internal organs in the infectious process. But the symptoms of dissemination are not specific to Lyme disease and are seen in other diseases as well.
General symptoms
General weakness, severe headache, fever severe muscle pain.
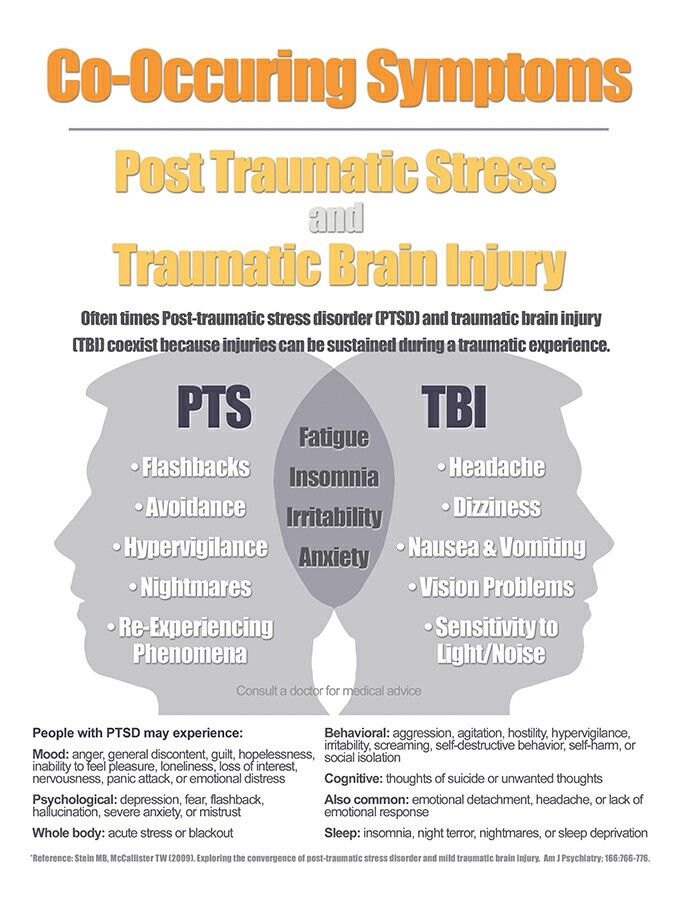
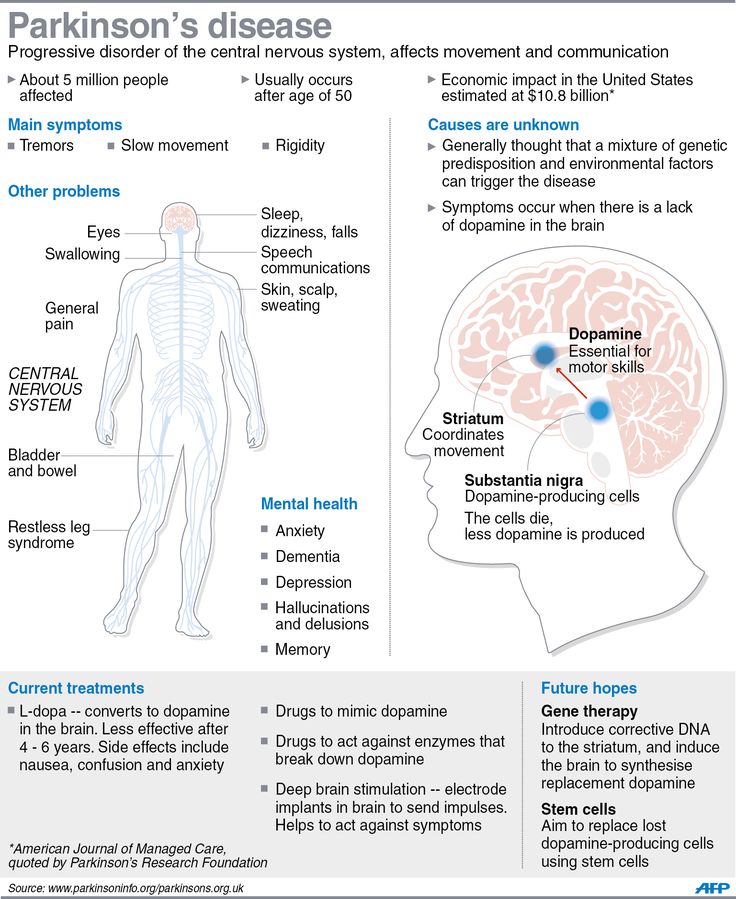
CNS symptoms
Signs of nerve conduction disorders (weakness / paresis in the limbs, loss of reflexes, sensory disturbances, peripheral neuropathy), severe headaches, neck stiffness, meningitis, cranial nerve disorders ( for example, smell/taste changes Difficulty chewing, swallowing, or speaking Dysphonia or problems in the vocal cords Bell's palsy Facial palsy Dizziness/fainting Shoulders droop Inability to turn the head Light or sound sensitivity.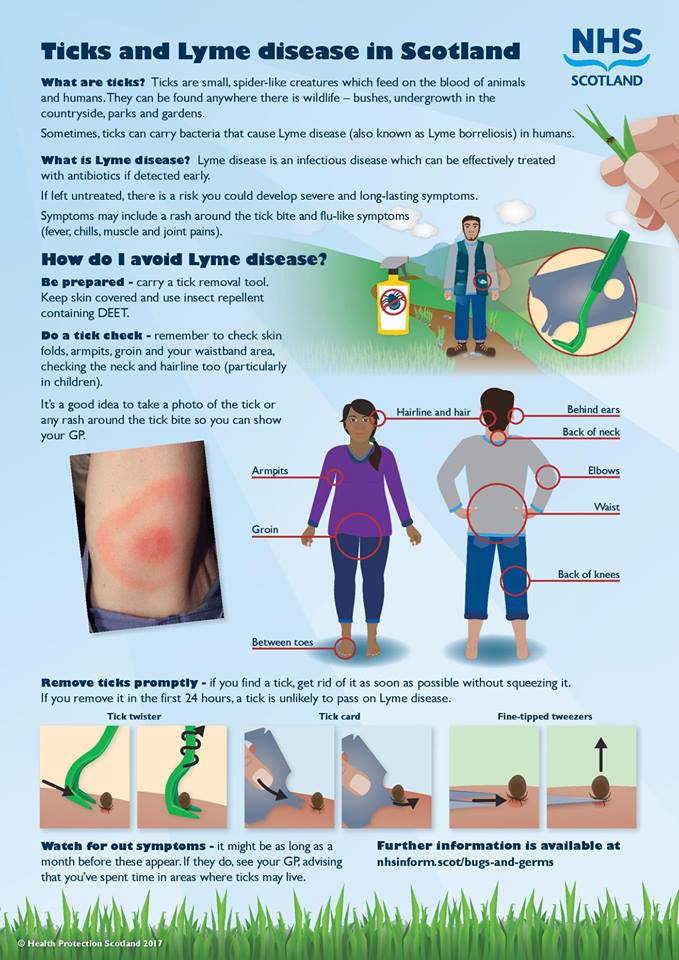 hearing changes are also possible, deviation of the eyeball, ptosis of the eyelid, stroke, sleep disturbances, intellectual-mnestic disorders (impaired fixation memory, concentration of attention, performing simple arithmetic actions), behavioral disorders (depression, personality change).0003
hearing changes are also possible, deviation of the eyeball, ptosis of the eyelid, stroke, sleep disturbances, intellectual-mnestic disorders (impaired fixation memory, concentration of attention, performing simple arithmetic actions), behavioral disorders (depression, personality change).0003
In addition, other mental changes are described in the literature: anxiety attacks, disorientation, hallucinations, paranoia, and other schizophrenia-like changes.
Eyes
Visual impairment including blindness, retinal damage, optic nerve atrophy, eye redness, conjunctivitis, "spots" before the eyes, inflammation of various parts of the eye, pain, diplopia.
Skin
Eruption not on side of bite. Skin rashes vary in both shape and color, usually ring-shaped, and can range in color from red to purple. The rashes may be hot to the touch or itchy or hard to the touch. In addition, other skin manifestations are possible:
- Lyphocytoma, which is a benign nodule or tumor, and
- Acrodermatitis chronic atrophicus, which is usually discoloration/degeneration of the skin of the hands or feet.
Cardiovascular system
Cardiac arrhythmias, conduction disturbances in the myocardium, myocarditis, pain in the heart area, vasculitis.
Joints
Arthritis in Lyme disease is manifested by pain, both transient and persistent. Joint lesions are usually not symmetrical, sometimes there are swelling in the joints..
Liver
Moderate liver dysfunction.
Light . Respiratory disorders sometimes pneumonia.
Muscles. Muscle pain, inflammation, decreased tone.
Gastrointestinal tract bowel dysfunction (diarrhea), appetite disorders, anorexia
Effect on pregnancy
Spontaneous abortion, premature birth, stillbirth are possible with Lyme disease. In addition, cases of congenital Lyme disease have been described. In such cases, the bacteria may pass from the mother to the fetus through the placenta.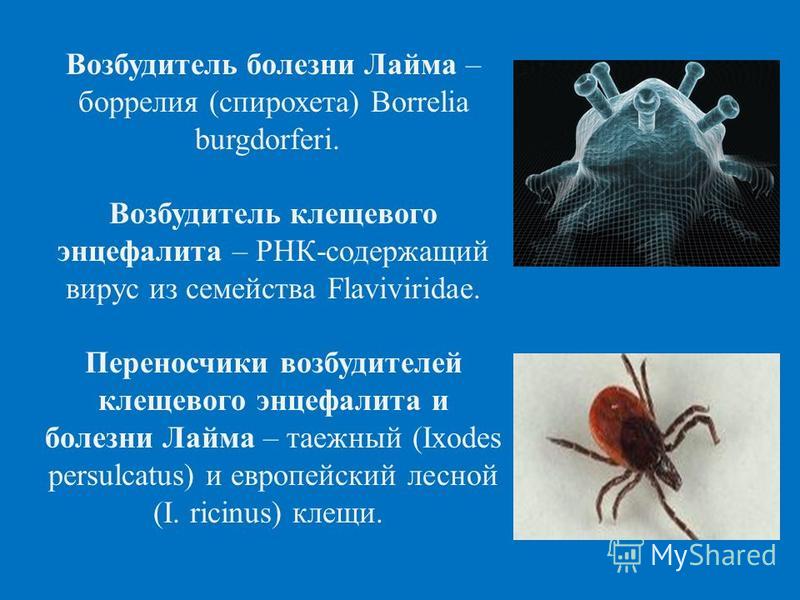 In addition, it is not excluded that the infection can be transmitted through breast milk.
In addition, it is not excluded that the infection can be transmitted through breast milk.
Diagnosis
Unfortunately, there are no tests that reliably confirm that the patient is currently infected with borreliosis bacteria and then confirm the absence of bacteria (the small size of spirochetes and the number does not allow you to see these bacteria in a living organism). The diagnosis is exposed on the basis of symptoms of a clinical picture and an epidemiological history.
Laboratory diagnostic methods
Indirect tests (antibody tests )
Antibodies are proteins produced by immune cells to bind infectious agents and neutralize microorganisms. Both the general level of antibodies in the blood and specific antibodies to the bacterium that causes Lyme disease are determined. False negative tests may be due to too low levels of antibodies to spirochetes, the presence of a small number of freely circulating spirochetes and, therefore, a low level of immune response (use of antibiotics, mutation of spirochetes). False-positive tests may be in other diseases (eg, syphilis, periodontal disease, rheumatoid arthritis). Types of Tests (antibody titer, Western blotting, antibodies to Lyme C6 peptide).
False-positive tests may be in other diseases (eg, syphilis, periodontal disease, rheumatoid arthritis). Types of Tests (antibody titer, Western blotting, antibodies to Lyme C6 peptide).
- Antigen detection - These tests detect a unique Bb protein in the fluid (eg urine) of patients. This may be useful for diagnosing Lyme disease in patients taking antibiotics or during a sudden flare-up.
- Polymerase chain reaction (PCR) - This assay enhances the detection of the Bb protein.
- Cultivation - Growing bacteria in media is labor intensive and time consuming (sometimes taking months).
Biopsy and microscopy are not very successful due to the fact that there are not many circulating spirochetes in the blood. Therefore, at present there are no clear protocols for the treatment of this disease. Antibiotics are only effective in the early stages of Lyme disease. When internal organs are involved in the infectious process, antibiotic treatment should be long-term and in sufficient dosage.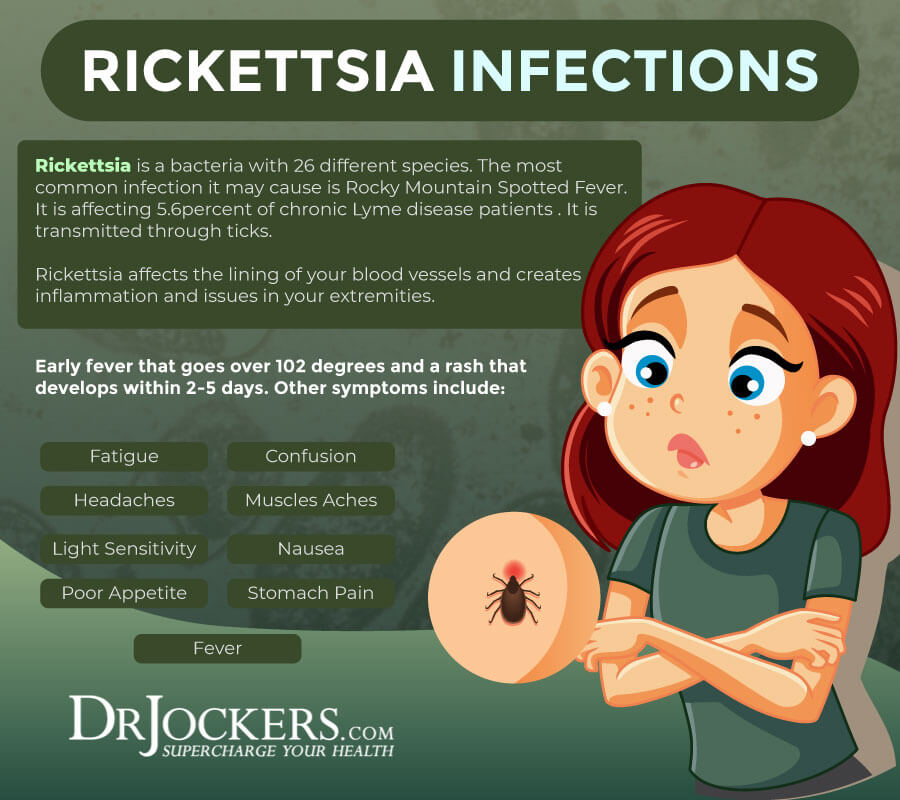 Other drug and non-drug treatments are symptomatic.
Other drug and non-drug treatments are symptomatic.
Infections transmitted by ixodid ticks | GAUZ TO "City Polyclinic No. 3"
Infections transmitted by ixodid ticks
The ixodid tick is a carrier of a huge number of diseases. He hides in thickets of grass, in branches of bushes, trees
They cling to animal hair, human clothes, and then move to the skin, biting through it, drinking blood. Together with saliva, bacteria and viruses enter the human body, livestock, which can cause a number of diseases.
Lyme disease
Lyme disease is one of the most common tick-borne diseases. Its other name is tick-borne borreliosis. The disease is caused by the spirochete Borrelia, which enters the human body when an insect bites along with its saliva, less often with feces through wounds.
Children are more often infected. The peak incidence occurs in the summer season. There is a high risk of infection when caring for animals, visiting forest park areas.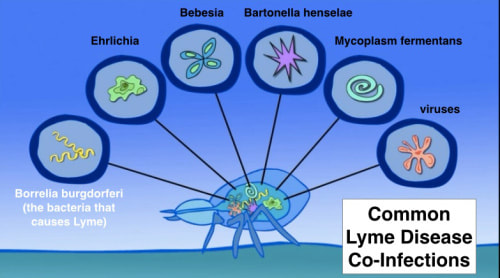 Lyme disease develops more often if the ixodid tick is not removed within 24 hours. The severity of the course of the disease directly depends on the amount of infection that has entered the wound.
Lyme disease develops more often if the ixodid tick is not removed within 24 hours. The severity of the course of the disease directly depends on the amount of infection that has entered the wound.
Tick-borne borreliosis refers to natural focal systemic diseases with complex pathogenesis. First, the skin is affected, then the musculoskeletal system, cardiovascular, nervous system. Lyme disease develops gradually.
Conventionally, its course is divided into three stages:
- Stage 1: bacteria penetrate the wound, causing an allergic reaction;
- stage 2: after a few weeks, the infection spreads through the lymph and blood throughout the body;
- Stage 3: internal organs, brain membranes are affected.
The main pronounced symptom of the disease is round redness, outlined by a bright red border. There is itching, the temperature rises to 39º and above, there is vomiting, headache. With the progression of Lyme disease, external manifestations disappear, other symptoms appear, depending on the organ of the lesion.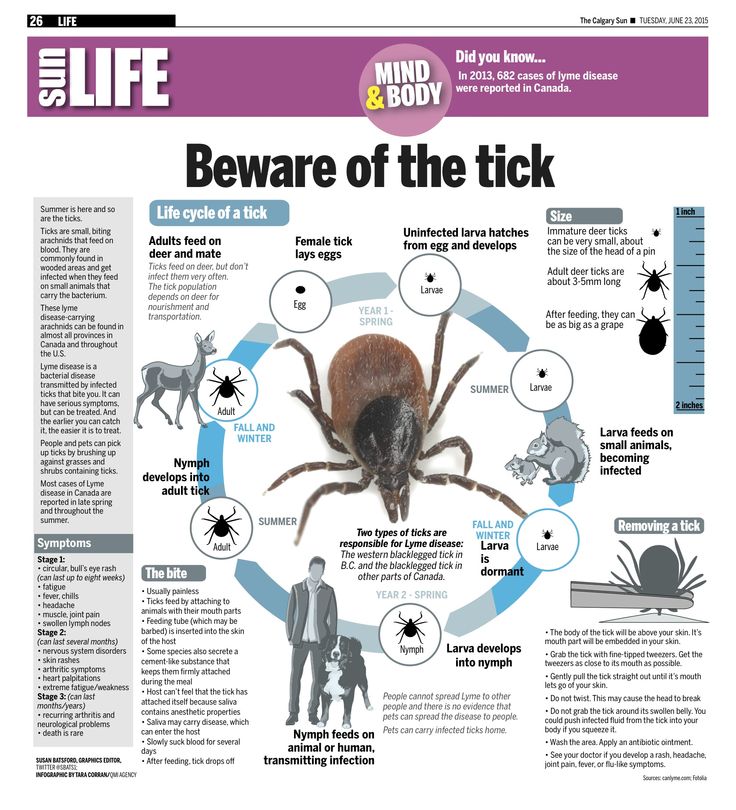 Lack of treatment leads to paralysis, the development of dementia, loss of vision, hearing, heart attack.
Lack of treatment leads to paralysis, the development of dementia, loss of vision, hearing, heart attack.
Human monocytic ehrlichiosis (MEH)
Monocytic ehrlichiosis is considered rare. Pathology is caused by bacteria belonging to the Ehrlichi family. They enter the bloodstream with the saliva of the ixodid tick.
Reservoirs for infection are animals: deer, roe deer, dogs, rats, hamsters, voles, fish.
A few weeks after infection (tick bite), symptoms of MEC disease appear:
- sudden rise in temperature;
- chills;
- weakness;
- muscle pain;
- causeless fatigue.
Laboratory blood tests indicate a decrease in the number of platelets and white blood cells. Changes occur in the liver, due to which bouts of vomiting and diarrhea become frequent. A dramatic weight loss begins. With severe development of human monocytic ehrlichiosis, the brain suffers, meningitis, pulmonary bleeding, and renal failure develop.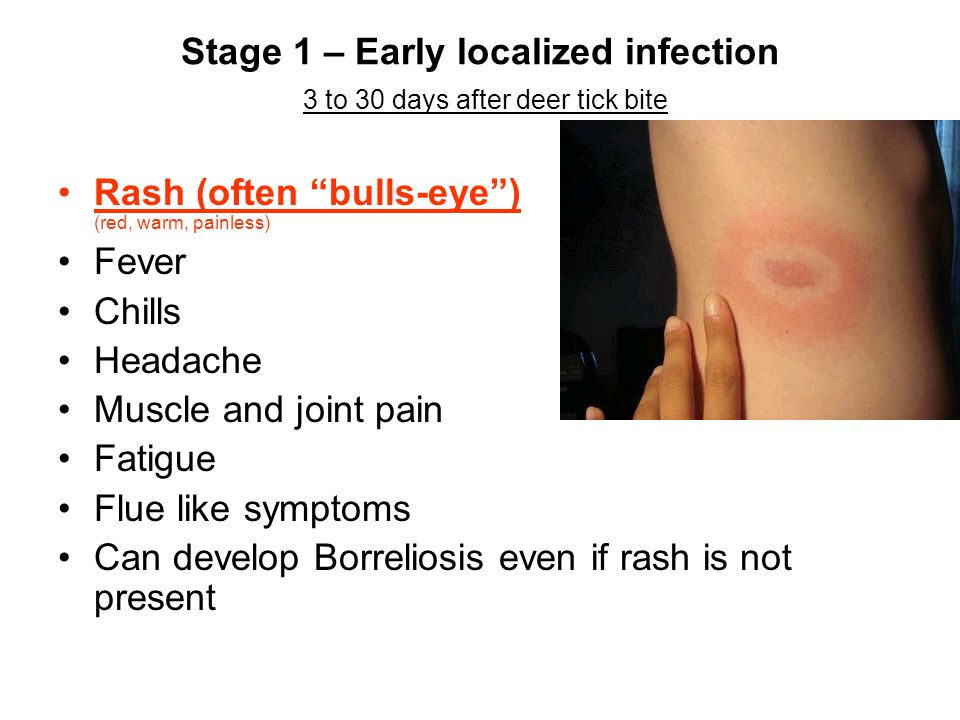 Mortality reaches 3-10% of all cases of infection.
Mortality reaches 3-10% of all cases of infection.
Human granulocytic anaplasmosis (HGA)
Infections transmitted by ixodid ticks are ubiquitous. In 1991, a disease of human granulocytic anaplasmosis was detected, the carriers of which turned out to be notorious insects. The disease is caused by anaplasma bacteria. After the bite of a blood-sucking insect infected with anaplasmas, the pathogen enters the bloodstream. Destroys white blood cells, causing inflammation in the body. At the initial stage of the disease, the symptoms of HAS resemble the flu. There is a high temperature, headache. They are supplemented by weakness, chills, muscle pain.
Among the rare signs of the disease, doctors note:
- decrease in blood pressure;
- sore throat;
- rash over body;
- cough;
- vomiting;
- pain in the right hypochondrium.
During diagnostics, tests, a high amount of liver enzymes, a decrease in the number of platelets and leukocytes are detected.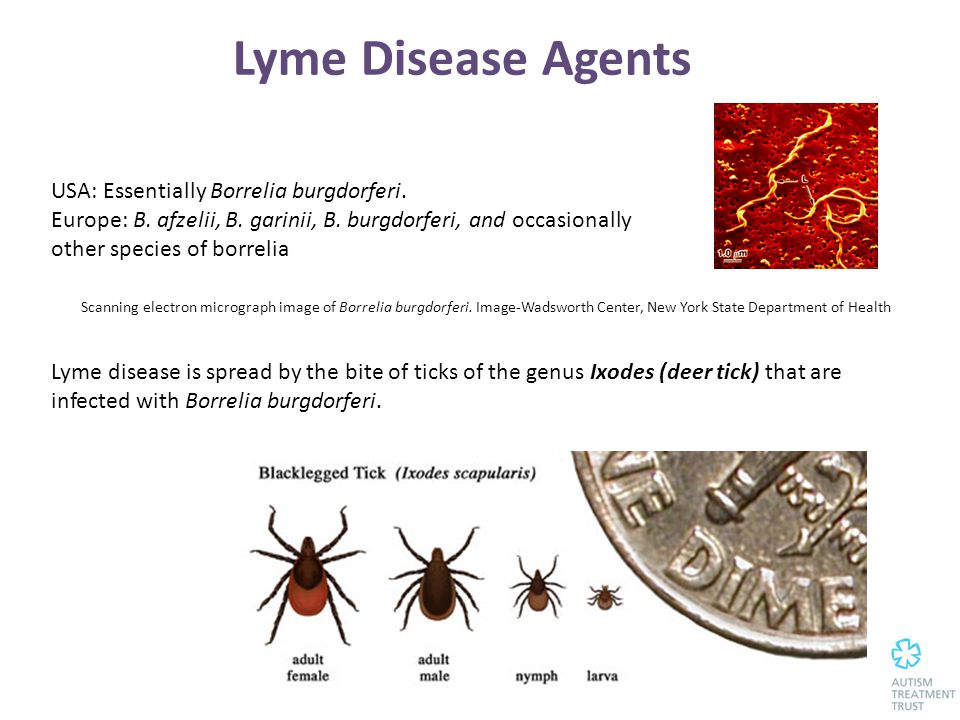 Many patients tolerate the disease without complications. In 1% of cases, a fatal outcome is observed with kidney failure or the development of meningoencephalitis.
Many patients tolerate the disease without complications. In 1% of cases, a fatal outcome is observed with kidney failure or the development of meningoencephalitis.
Tick-borne encephalitis
Tick-borne encephalitis develops when bitten by ixodid ticks infected with flaviviruses. In addition to humans, it affects livestock (goats, cows), so infection occurs when raw milk, meat that has not undergone heat treatment is consumed.
The disease is common in Mongolia, China, in Russian regions: the Far East, Siberia. Less common in Scandinavia, Eastern Europe.
Tick-borne encephalitis occurs in different ways. There are three forms of the disease:
- feverish;
- meningeal;
- focal.
Getting into wounds or intestines, the virus instantly multiplies, quickly spreads through the organs. The deterioration of the condition is sharply noticed: convulsions, muscle aches, headache appear. The temperature rises, chills are observed. The face and neck turn red, the vessels on the sclera increase. The fever manifests itself in attacks. This state lasts up to 10 days. Gradually, the symptoms subside.
The temperature rises, chills are observed. The face and neck turn red, the vessels on the sclera increase. The fever manifests itself in attacks. This state lasts up to 10 days. Gradually, the symptoms subside.
In the meningeal form, the membranes of the brain are affected, which causes headache, severe vomiting. There is a fear of light, asthenia, a decline in strength and mood is felt.
In the focal form, the temperature rises to 40º, breathing is disturbed, and consciousness disorders appear. Often, tick-borne encephalitis is accompanied by hallucinations, muscle paralysis, and the development of sciatica. Possible death in the absence of timely assistance.
Disease prevention
Prevention of infections transmitted by ixodid ticks can prevent the unpredictable consequences of infectious diseases. Everyone can protect themselves, pets from parasite bites. It is necessary to plan in advance trips to the forest, to the lake, fishing, hunting, in order to prepare protective clothing, and vaccinate if necessary.
Preventive measures include:
- Vaccination.
Vaccination includes three doses of the vaccine on a 0-1-12 schedule or an accelerated schedule of 0-14 days-1 year. For vaccination, the domestically produced vaccine "Encevir" is used for adults and children from 3 years old, for the vaccination of children from 3 to 17 years old "Encevir-Neo". Vaccination of adults is carried out free of charge at the expense of the budget for decreed contingents (for persons performing: agricultural, hydro-reclamation, construction, excavation and movement of soil, procurement, trade, geological, prospecting, forwarding, deratization and pest control types of work, as well as logging work , clearing and landscaping of forests, recreation and recreation areas for the population, persons working with live cultures of the tick-borne encephalitis pathogen). It is also possible to vaccinate at the expense of personal funds. To do this, you need to contact the clinic at the place of residence.