Friend with schizophrenia
Helping Someone with Schizophrenia - HelpGuide.org
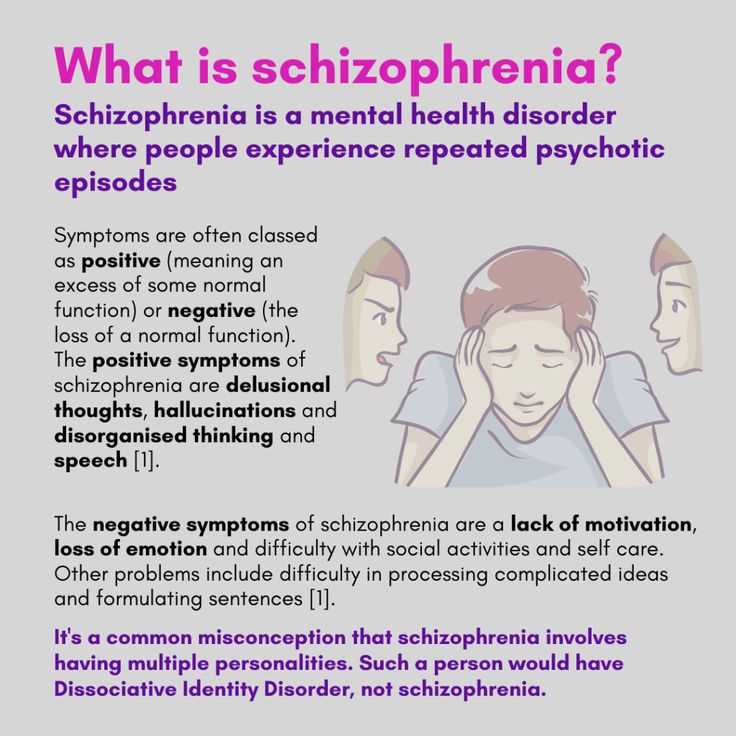
schizophrenia
Have a loved one with schizophrenia? Your support can make a huge difference by helping them find the right treatment, cope with symptoms, and build a rich, satisfying life.
When a loved one has schizophrenia
The love and support of family and friends plays an important role in schizophrenia treatment and recovery. If you have a loved one with schizophrenia, you may be struggling with any number of difficult emotions, including fear, guilt, anger, and frustration. You may feel helpless in the face of your loved one’s symptoms, worried about the stigma of schizophrenia, or confused and embarrassed by their strange behaviors. You may even be tempted to hide your loved one’s illness from others.
But it’s important to remember that a diagnosis of schizophrenia is not a life-sentence. Recovery is possible, especially with your love and support. To help someone with schizophrenia, it’s crucial you:
- Accept the illness and its difficulties.
- Not buy into the myth that someone with schizophrenia can't get better or live a full and meaningful life.
- Do your best to help your loved one feel better and enjoy life.
- Pay attention to your own needs.
- Maintain your sense of humor and remain hopeful.
While dealing with a loved one’s schizophrenia can be challenging, the following strategies can help you guide your loved one on the road to recovery without losing sight of your own hopes and dreams.
Tips for helping a loved one with schizophrenia
Educate yourself. Learning about schizophrenia and its treatment will allow you to make informed decisions about how best to cope with symptoms, encourage your loved one to pursue self-help strategies, handle setbacks, and work towards recovery.
Reduce stress. Stress can cause schizophrenia symptoms to flare up, so it's important to create a structured and supportive environment for your loved one.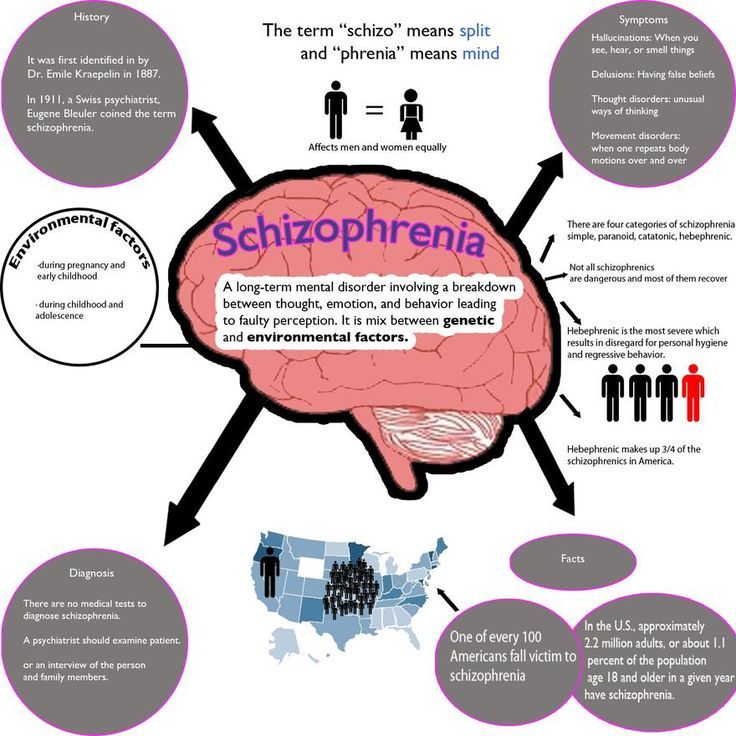
Set realistic expectations. It's important to be realistic about the challenges of schizophrenia. Help your loved one set and achieve manageable goals, and be patient with the pace of recovery.
Empower your loved one. Be careful that you're not taking over and doing things for your loved one that they are capable of doing. Support your loved one while still encouraging as much independence and self-help as possible.
Helping someone with schizophrenia tip 1: Encourage treatment and self-help
Encouraging treatment and self-help is a cornerstone of helping a loved one with schizophrenia. While medication is an important element of schizophrenia treatment, your loved one's recovery depends on other factors as well. Self-help strategies such as changing to a healthy diet, managing stress, exercising, and seeking social support can have a profound effect on your loved one's symptoms, feelings, and self-esteem. And the more someone does for themselves, the less hopeless and helpless they'll feel, and the more likely their doctor will be able to reduce their medication. Your encouragement and support can be crucial to your loved one starting and continuing a program of self-help.
Your encouragement and support can be crucial to your loved one starting and continuing a program of self-help.
[Read: How to Help Someone with Mental Illness Accept Treatment]
Starting treatment
Often, the first challenge of treatment is convincing the person with schizophrenia to see a doctor. To people experiencing delusions, hallucinations, and paranoia, there is no need for medical intervention because the voices and conspiracy theories are real.
If a loved one with schizophrenia is reluctant to see a doctor, try to:
Provide options. Your loved one may be more willing to see a doctor if he or she has some control over the situation. If your relative appears suspicious of you, suggest that another person accompany them to the appointment. You can also give your loved one a choice of doctors.
Focus on a particular symptom. Someone with schizophrenia may resist seeing a doctor out of fear of being judged or labeled “crazy. ” You can make the doctor less threatening by suggesting a visit in order to deal with a specific symptom such as insomnia or lack of energy.
” You can make the doctor less threatening by suggesting a visit in order to deal with a specific symptom such as insomnia or lack of energy.
Tips for supporting a loved one's schizophrenia treatment
Seek help right away. Early intervention makes a difference in the course of schizophrenia, so help your loved one find a good doctor and start treatment.
Be collaborative. When your loved one has a voice in their own treatment, they will be more motivated to work towards recovery.
Encourage self-help. Since schizophrenia is often episodic, periods of remission from the severest symptoms can provide an opportunity for your loved one to employ self-help strategies that may limit the length and frequency of future episodes.
Tip 2: Build your support network
To better support and care for someone with schizophrenia, you need to find help, encouragement, and understanding from others. The more support you have, the better it will be for both you and your loved one.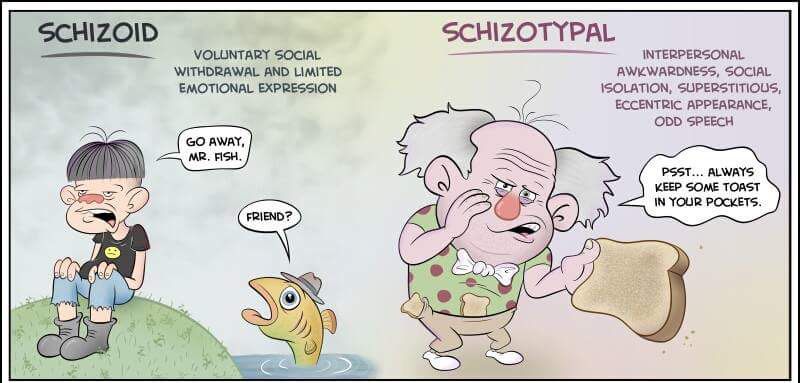
Recognize your own limits. Be realistic about the level of support and care you can provide. You can't do it all, and you won't be much help to a loved one if you're exhausted, so seek help where you can.
Join a support group. Meeting others who know first-hand what you're going through can help reduce feelings of isolation and fear. Support groups provide an invaluable venue for the relatives of people with schizophrenia to share experiences, advice, and information.
Turn to trusted friends and family members. Ask loved ones if you can call on them for support. Most people will be flattered by your request.
Seek out new friends. If you don't feel that you have anyone to turn to, it's never too late to build new friendships and improve your support network.
Take advantage of support services. Ask your loved one's doctor or therapist about respite services and other support available in your area, or contact local hospitals and mental health clinics.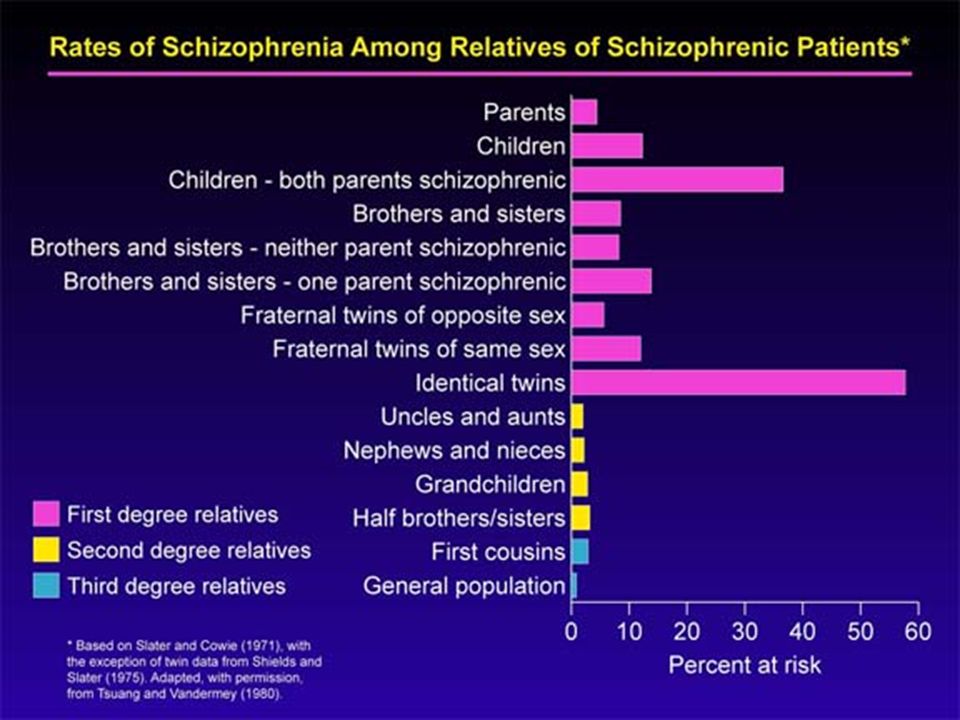
With over 25,000 licensed counselors, BetterHelp has a therapist that fits your needs. Sign up today and get matched.
GET 20% OFF
Tip 3: Monitor medication
Once in treatment, careful monitoring can ensure that your loved one stays on track and gets the most out of medication.
Take side effects seriously. Many people with schizophrenia stop taking their medication because of side effects. Bring any distressing side effects to the attention of the doctor, who may be able to reduce the dose, switch to another antipsychotic, or add medication to counter the side effect.
Encourage your loved one to take medication regularly. Even with side effects under control, some people with schizophrenia refuse medication or have trouble remembering their daily dose. Medication reminder apps, weekly pillboxes, and calendars can help. Some medications are available as long-lasting weekly or monthly injections instead of daily pills.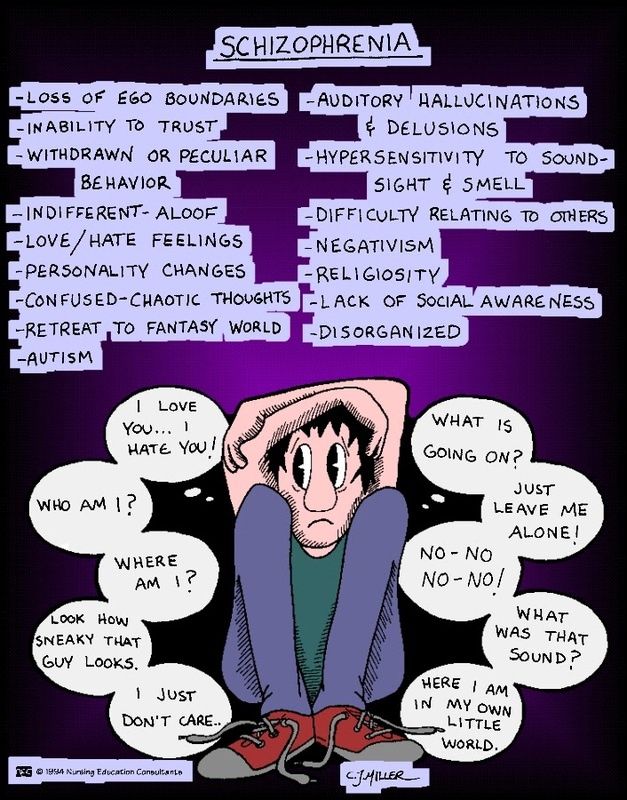
Be careful to avoid drug interactions. Help your loved one avoid any dangerous drug interactions by giving the doctor a complete list of the drugs and supplements they're taking. Mixing alcohol or illegal drugs with schizophrenia medication is harmful, so talk to the doctor if your relative has a substance abuse problem.
Track your family member's progress. A mood-tracking app, journal, or diary is a good way to track changes in your family member's behavior, outlook, and other symptoms in response to medication.
Stopping medication is the most frequent cause of relapse in schizophrenia, so it's extremely important that your family member continues to take all medication as directed. While relapse can occur even if a person is taking medication as prescribed, you may be able to prevent a full-blown crisis by recognizing the warning signs and taking immediate steps.
Common warning signs of schizophrenia relapse
- Insomnia
- Social withdrawal
- Deterioration of personal hygiene
- Increasing paranoia
- Hostility
- Confusing or nonsensical speech
- Strange disappearances
- Hallucinations
If you notice any warning signs of relapse or other indications that your family member's symptoms of schizophrenia are getting worse, call the doctor right away.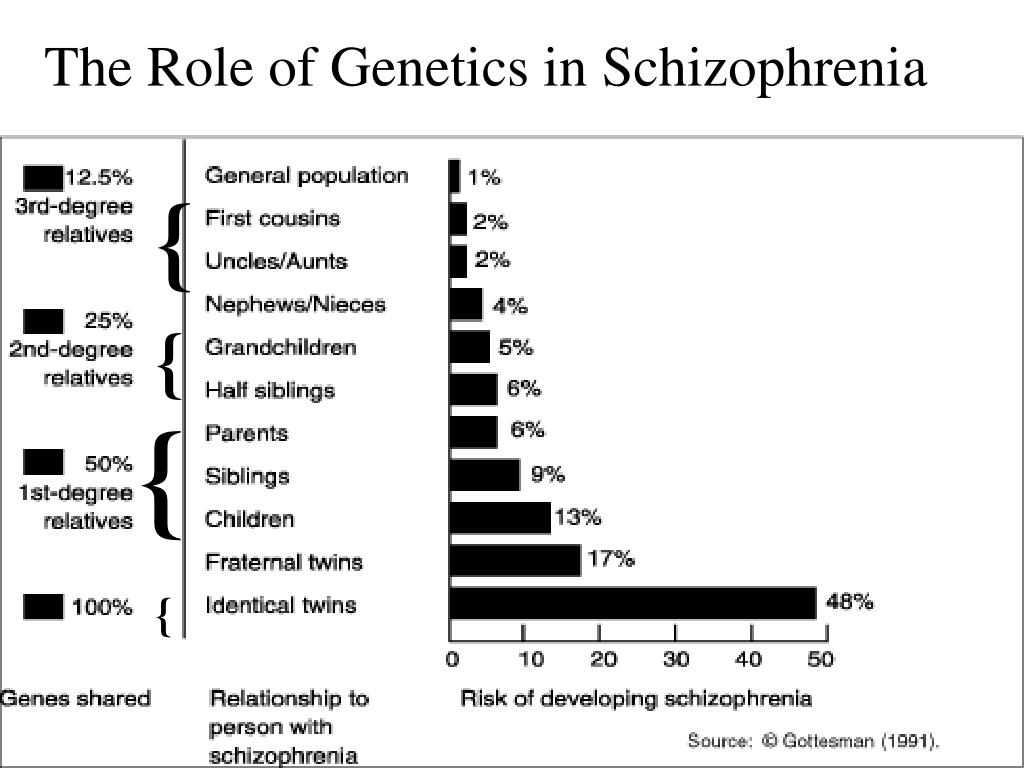
Tip 5: Prepare for crisis situations
Despite your best efforts to prevent relapse, there may be times when your loved one's condition deteriorates rapidly and hospitalization is required to keep them safe. Having an emergency plan ready for an acute psychotic episode will help you handle the crisis safely and quickly. A good emergency plan for someone with schizophrenia includes:
- Emergency contact information for your loved one's doctor and therapists.
- The address and phone number of the hospital you will go to for psychiatric admission.
- Friends or relatives who will take care of other children or dependents while you deal with the crisis.
It's also wise to go over the emergency plan with your family member. The crisis situation may be less frightening to your loved one if they know what to expect during an emergency.
10 tips for handling a schizophrenia crisis
- Remember that you cannot reason with acute psychosis.
- The person may be terrified by their own feelings of loss of control.
- Don't express irritation or anger.
- Speak quietly and calmly, do not shout or threaten the person.
- Don't use sarcasm as a weapon.
- Decrease distractions by turning off the TV, computer, any fluorescent lights that hum, etc.
- Ask any casual visitors to leave—the fewer people the better.
- Avoid direct, continuous eye contact.
- Avoid touching the person.
- Sit down and ask the person to sit down as well.
Tip 6: Explore housing options
Someone with schizophrenia needs a stable, supportive place to live, but finding the right living situation can be challenging.
- Can your loved one care for themselves?
- How much support do they need with daily activities?
- Does your loved one have a drug or alcohol problem?
- How much treatment supervision does your loved one require?
Living with family
Living with family can be a good option for someone with schizophrenia if their family members understand the illness well, have a strong support system of their own, and are able to provide whatever assistance is needed.
At-home arrangements are less likely to be successful if the person with schizophrenia uses drugs or alcohol, resists taking medication, or is aggressive or uncooperative.
| Choosing the Right Housing Option for Someone with Schizophrenia |
| Living with family works best if: |
|
| Living with family is not advised if: |
|
Try not to feel guilty if you are unequipped to house someone with schizophrenia. If you can't look after your own needs or those of other family members while caring for your loved one, they will be better off elsewhere.
Residential options outside the family home
If an at-home living arrangement isn't the right fit, explore the residential facilities in your community.
Options in your area may include:
Residential treatment facilities or 24-hour care homes. A more structured living environment for those requiring greater assistance or suffering an acute psychotic episode.
Transitional group home. An intensive program that helps individuals transition back into society and avoid relapse after a crisis or hospitalization.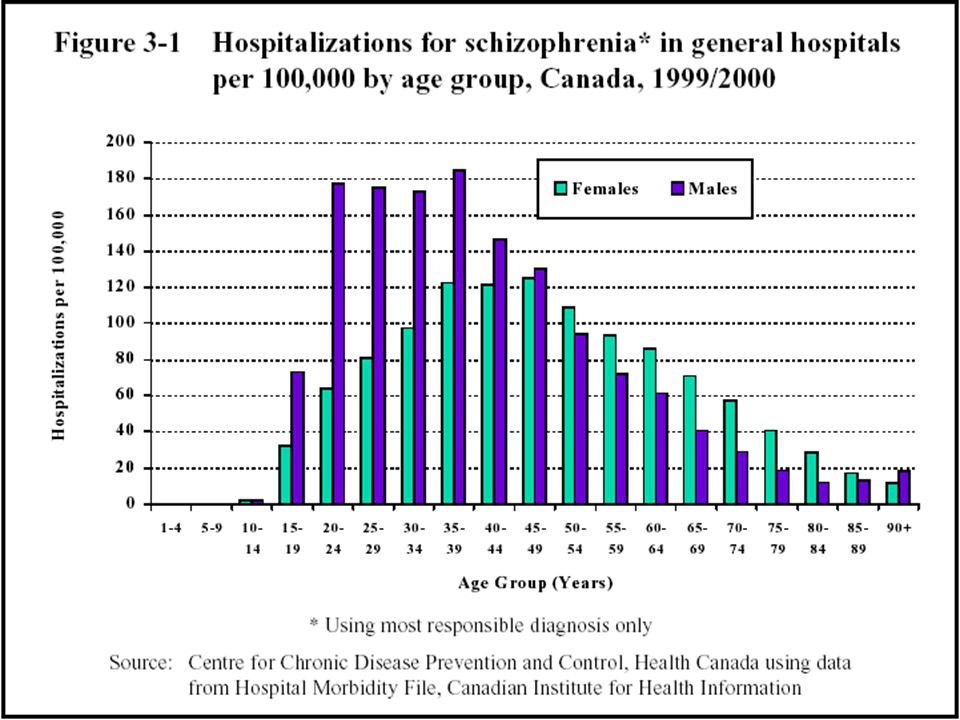
Foster or boarding homes. A group living situation offering a degree of independence, while providing meals and other basic necessities.
Supervised apartments. Residents live alone or share an apartment, with staff members available on-site to provide assistance and support.
Tip 7: Take care of yourself
Taking care of yourself isn't selfish. In fact, it's just as important for your loved one with schizophrenia that you look after your own health needs.
Schizophrenia can place an incredible amount of stress on the family. It can take over your life and burn you out. And if you're stressed, you'll make the person with schizophrenia stressed and trigger or exacerbate their symptoms.
Since adopting healthy lifestyle habits is also important for your loved one in managing schizophrenia symptoms, by taking care of your own health you can act as a role model. You may even be able to pursue some of these steps together, helping to motivate and encourage each other.
Connect with others. Social interaction with someone who cares about you is the most effective way to relieve stress. It's important for both you and the person with schizophrenia to have other people you can connect with face-to-face—someone you can talk to for an uninterrupted period of time, someone who will listen without judging or continually becoming distracted. That person may be a friend, family member, clergy member, or professional therapist.
Get regular exercise. Physical activity reduces stress and releases endorphins, powerful chemicals in your brain that energize your spirits and make you feel good. Whether you exercise alone, with a friend, or with your loved one with schizophrenia, aim for 30 minutes of activity on most days, or if it's easier, three 10-minute sessions.
Eat a healthy diet. What you eat has a direct impact on the way you feel. Minimize sugar and refined carbs, foods that quickly lead to a crash in mood and energy.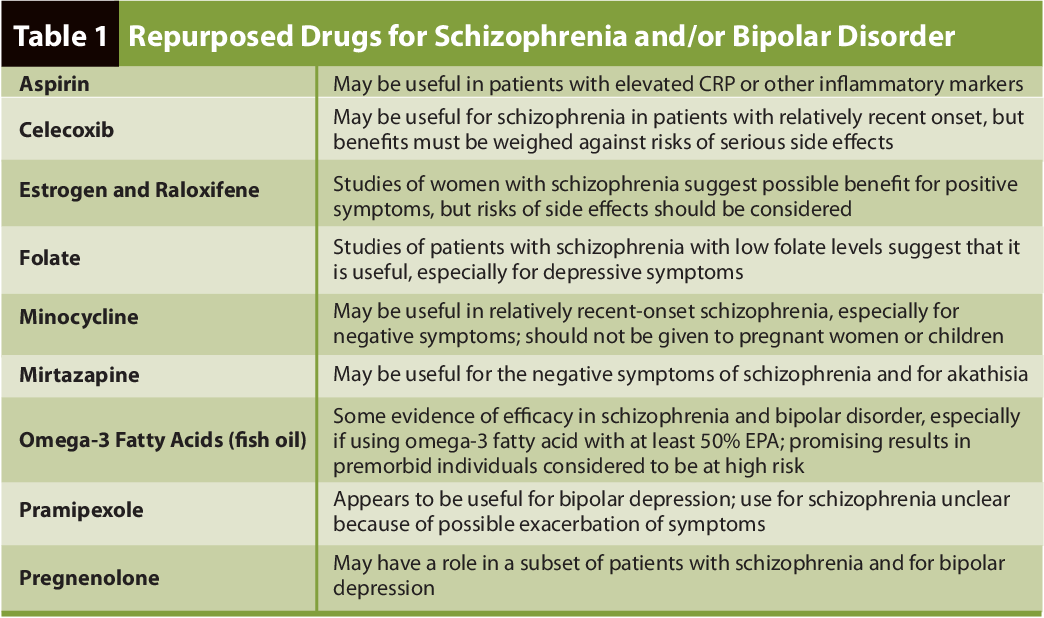 Boost your intake of Omega-3 fatty acids from fatty fish, fish oil, walnuts, and flaxseeds to help improve your focus, energy, and outlook. The same diet tips can help manage your loved one's symptoms, too.
Boost your intake of Omega-3 fatty acids from fatty fish, fish oil, walnuts, and flaxseeds to help improve your focus, energy, and outlook. The same diet tips can help manage your loved one's symptoms, too.
Practice acceptance. Instead of dwelling on the unfairness of your loved one's diagnosis, accept your feelings, even the negative ones. It can make a huge difference in your ability to manage stress and balance your moods. See HelpGuide's Emotional Intelligence Toolkit for more.
Seek out joy. Making time for fun isn't indulgent—it's necessary. Schedule time into your day for things you enjoy, whether it's spending time in nature, visiting friends, or reading a good book. Encourage your loved one with schizophrenia to do the same.
Look after your health. Neglecting your health will only add to the stress in your life. Get enough sleep and stay on top of any medical conditions.
Use relaxation techniques.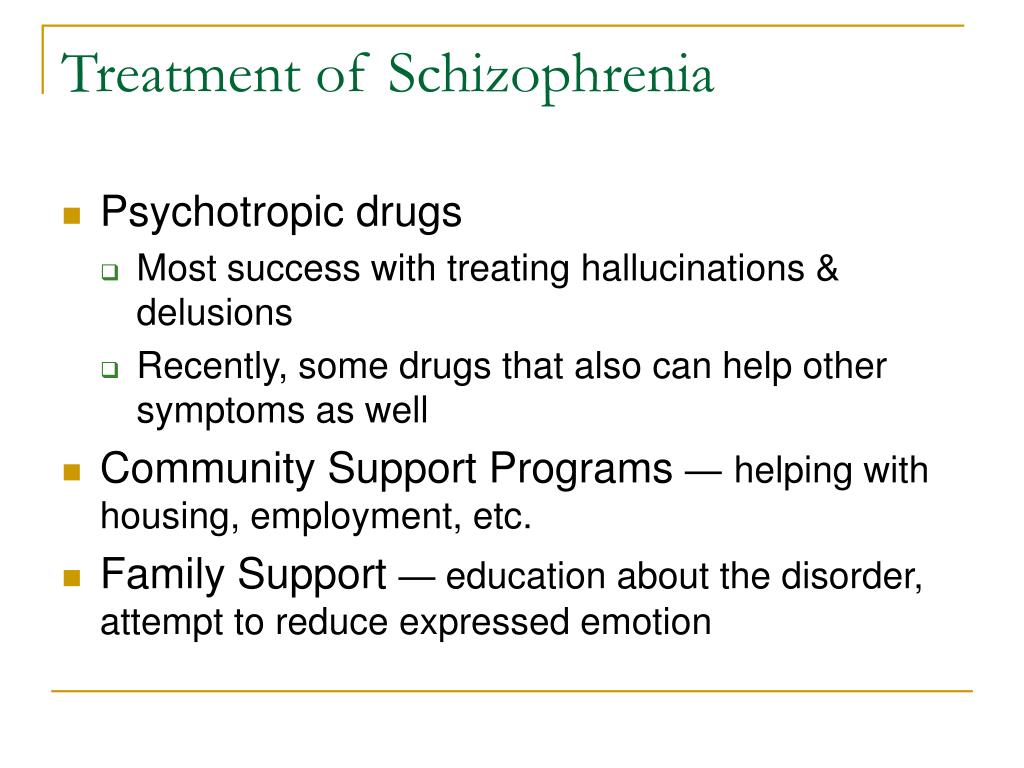 Techniques such as meditation, deep breathing, yoga, or progressive muscle relaxation can put the brakes on stress and bring your mind and body back into balance.
Techniques such as meditation, deep breathing, yoga, or progressive muscle relaxation can put the brakes on stress and bring your mind and body back into balance.
Authors: Melinda Smith, M.A., Lawrence Robinson, and Jeanne Segal, Ph.D.
- References
Schizophrenia Spectrum and Other Psychotic Disorders. (2013). In Diagnostic and Statistical Manual of Mental Disorders. American Psychiatric Association. https://doi.org/10.1176/appi.books.9780890425787.x02_Schizophrenia_Spectrum
Pilling, S., P. Bebbington, E. Kuipers, P. Garety, J. Geddes, G. Orbach, and C. Morgan. “Psychological Treatments in Schizophrenia: I. Meta-Analysis of Family Intervention and Cognitive Behaviour Therapy.
 ” Psychological Medicine 32, no. 5 (July 2002): 763–82. https://doi.org/10.1017/s0033291702005895
” Psychological Medicine 32, no. 5 (July 2002): 763–82. https://doi.org/10.1017/s0033291702005895Lloyd, Joanne, Helen Lloyd, Ray Fitzpatrick, and Michele Peters. “Treatment Outcomes in Schizophrenia: Qualitative Study of the Views of Family Carers.” BMC Psychiatry 17, no. 1 (July 21, 2017): 266. https://doi.org/10.1186/s12888-017-1418-8
Ganguly, Pronab, Abdrabo Soliman, and Ahmed A. Moustafa. “Holistic Management of Schizophrenia Symptoms Using Pharmacological and Non-Pharmacological Treatment.” Frontiers in Public Health 6 (2018): 166. https://doi.org/10.3389/fpubh.2018.00166
Knight, Edward L. “Self-Help and Serious Mental Illness.” Medscape General Medicine 8, no. 1 (March 15, 2006): 68. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1681955/
“Self-Management: The Experiences and Views of Self-Management of People with a Diagnosis of Schizophrenia – Social Care Online.” Accessed November 2, 2021. https://www.scie-socialcareonline.org.uk/self-management-the-experiences-and-views-of-self-management-of-people-with-a-diagnosis-of-schizophrenia/r/a11G00000017tP5IAI
Stępnicki, Piotr, Magda Kondej, and Agnieszka A.
 Kaczor. “Current Concepts and Treatments of Schizophrenia.” Molecules: A Journal of Synthetic Chemistry and Natural Product Chemistry 23, no. 8 (August 20, 2018): 2087. https://doi.org/10.3390/molecules23082087
Kaczor. “Current Concepts and Treatments of Schizophrenia.” Molecules: A Journal of Synthetic Chemistry and Natural Product Chemistry 23, no. 8 (August 20, 2018): 2087. https://doi.org/10.3390/molecules23082087Patel, Krishna R., Jessica Cherian, Kunj Gohil, and Dylan Atkinson. “Schizophrenia: Overview and Treatment Options.” Pharmacy and Therapeutics 39, no. 9 (September 2014): 638–45. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4159061/
Biagianti, Bruno, Sophia H. Quraishi, and Danielle A. Schlosser. “Potential Benefits of Incorporating Peer-to-Peer Interactions Into Digital Interventions for Psychotic Disorders: A Systematic Review.” Psychiatric Services 69, no. 4 (April 1, 2018): 377–88. https://doi.org/10.1176/appi.ps.201700283
Schizophrenia: The Journey to Recovery (PDF) – Family guide to schizophrenia assessment and treatment. (Schizophrenia Society of Canada)
60 Tips for Helping People who have Schizophrenia – Tips for communicating with someone who has schizophrenia, handling a crisis, and avoiding relapses.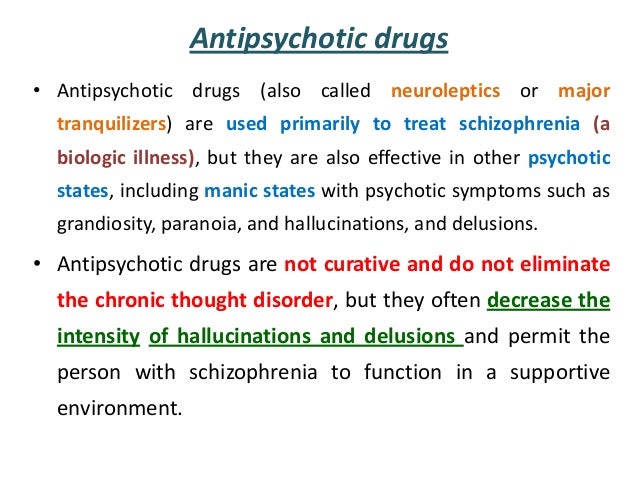 (Schizophrenia.com)
(Schizophrenia.com)
Finding a Good Residential Option for Someone with Severe Mental Illness – Provides suggestions for choosing the right living arrangement for someone with schizophrenia. (Schizophrenia.com)
Helplines and support
In the U.S.: Call 1-800-950-6264 or visit NAMI.org
UK: Call 0300 5000 927 or visit Rethink: Schizophrenia
Australia: Call 1800 18 7263 or visit Sane Australia
Canada: Visit Schizophrenia Society of Canada for links to regional societies that offer helplines and local services
India: Call the Vandrevala Foundation Helpline at 1860 2662 345 or 1800 2333 330
Last updated: December 5, 2022
How to Help Someone with Schizophrenia: 10 Do’s and Don’ts
Schizophrenia is a mental health condition that involves a disconnect from reality.
Along with symptoms that affect concentration and memory, people living with schizophrenia experience psychosis, which includes hallucinations and delusions.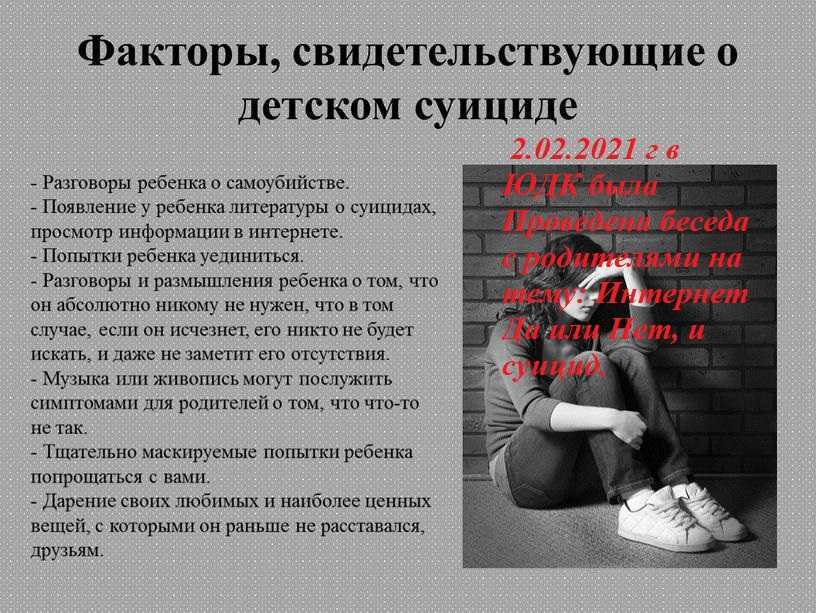
They might lose interest in their usual activities, struggle with self-care, and withdraw from loved ones.
These symptoms can have a far-reaching impact. Not only do they often make daily life difficult and contribute to emotional distress, they can also lead to isolation, sleep problems, or substance use — any of which can affect well-being and complicate treatment.
If your loved one lives with schizophrenia, you might wonder how you can best offer support. Here’s a look at seven ways to help, along with some tips on what to avoid.
When you recognize and understand the symptoms of schizophrenia, your loved one’s behavior may seem less confusing or frightening.
There’s a lot of stigma around schizophrenia, much of which relates to key symptoms of psychosis:
- Delusions, or beliefs not supported by factual evidence. They might believe someone is poisoning their food, that they have special powers, or that some outside organization controls their behavior.
- Hallucinations, or seeing, hearing, and feeling things no one else can. They might hear music, voices that say cruel things, or see (and touch) animals that aren’t really there.
- Cognitive symptoms, including trouble concentrating, speaking clearly, or answering questions. They might use words or phrases that don’t make sense, say things you can’t understand, or repeat the same phrases.
Someone with schizophrenia might believe they’re really a celebrity or a historic or religious figure.
Called a delusion of grandeur, this isn’t the same as dissociative identity disorder, where someone has a separate, additional personality.
They might also make unusual or jerky motions and move restlessly. And they might seem agitated or upset.
It’s a myth, though, that schizophrenia automatically makes someone violent or dangerous.
Explore schizophrenia symptoms in more detail.
When your loved one describes their hallucinations or delusions, you might feel uncertain about how to respond.
It’s normal to not know what to say, but you can still validate their confusion, frustration, and fear — even when you don’t fully understand their experience.
Instead of dismissing these symptoms as lies or stories, remember the things they see, hear, and believe are completely real to them.
Consider how you’d feel, and how you’d want others to support you, if you firmly believed something that everyone else denied.
What to say
To avoid dismissing their experience, try something like:
- “Seeing a strange figure in your house must be so frightening. Is there anything I can do to help you feel safer?”
- “I understand not wanting to go out when you feel someone watching you. Would you have an easier time running errands if I kept you company?”
They might seem disinterested in talking and offer “flat” responses, but difficulty expressing emotion is a common schizophrenia symptom.
You might also notice their speech patterns seem unusual or unfamiliar, and you might not always understand what they’re trying to say.
All the same, give them time to express themselves in their own way. Let them talk without trying to finish their sentences or fill in blank spaces. It may take more time to have a conversation, but making the effort can help them feel supported and connected.
You might want to do whatever you can to make things easier for your loved one. Maybe you have plenty of suggestions or advice for changes they can make to improve their well-being.
They’re still their own person, though, and they might not need or want you to take complete charge.
Instead, ask, “What can I do to help you out?”
Or try making suggestions that still leave them in control:
- “I noticed you don’t have many clean clothes left in the closet. Would it help if I threw in a load of laundry for you?”
- “Do you need groceries? I can take you to the store today.”
- “I was thinking we could make dinner together, but why don’t we do the dishes first?”
If they say they don’t need help, it’s best to respect that — as long as their safety isn’t at risk.
You might think getting some fresh air or tidying up would do wonders for their health. When you insist they do something they don’t want to do, though, they might feel frustrated and pull back instead.
Self-isolation and social withdrawal are often early signs of schizophrenia. Your loved one might lose interest in things they used to enjoy: work or school, hobbies, and spending time with you and other loved ones.
Keeping in contact provides your loved with important social and emotional support. Staying connected also gives you the opportunity to encourage them if they seem reluctant to get support or continue treatment.
How to check in
- Make a habit of checking in regularly, even just to ask if they need anything. They may always turn down offers of help, but that doesn’t mean you have to stop asking.
- Send a text or give them a quick call to say, “I was thinking about you. How are you doing today?”
- Suggest activities to do together, like watching a movie, taking a walk, or playing a game.
- Offer encouragement when they reach out first. “I’m so glad to hear from you. Thanks for calling!”
Once they appear, schizophrenia symptoms can come and go throughout life. Creating a plan for what to do when this happens can make it easier to manage symptoms if they return or get worse.
This plan might include things like:
- key signs of a schizophrenia episode
- numbers for their psychiatrist, therapist, and other professionals
- strategies for coping with distress, including stretches, physical movement, or deep breathing
- phone numbers for emergency contacts
- their preferred first steps to getting help, such as checking in with their therapist or heading to the emergency room
- a list of current medications, allergies, and other important health information
- who should take care of their children or pets and look after their house
If you feel comfortable doing so, put your own number on the list and let them know they can call you in a crisis.
Also include numbers for crisis helplines that can provide immediate help and support, like:
- Crisis Text Line by texting HOME to 741741
- National Suicide Prevention Lifeline by calling 1-800-273-8255
- The International Association for Suicide Prevention website for crisis helplines and other resources outside the United States
People with schizophrenia typically need long-term treatment and support from mental health professionals.
Medication for schizophrenia can improve symptoms and sometimes help keep them from coming back.
Therapy, on the other hand, can help people living with schizophrenia learn to recognize signs of an episode and explore strategies to manage symptoms and the distress they cause.
You can ask about treatment and offer support in positive, supportive ways without making them feel criticized or helpless.
Do’s
- “How is therapy going? Has your therapist been helpful?”
- “I remember you mentioned having a hard time remembering to take your medication.
 Would it help to set a reminder on your phone?”
Would it help to set a reminder on your phone?” - “Can I give you a ride to therapy or take you to pick up your prescription this week?”
Don’ts
- “Are you still going to therapy?”
- “Did you take your medication today?”
- “You know you can’t stop treatment even if you feel better, right?”
Family therapy can also provide the opportunity for family members to get more information about treatment plans and productive ways to offer support.
Schizophrenia doesn’t just make it difficult to concentrate and stay focused at work or school. It can also affect motivation and ability to handle daily tasks, including:
- chores
- self-care
- interaction with loved ones
Pushing them to make changes they aren’t ready for, like returning to full-time work, generally won’t help.
Instead, encourage them to work toward small goals, especially things you can do together. You might try:
- helping them stay physically active by hiking together on weekends
- encouraging them to eat regular meals by preparing dinner together
- brainstorming a nighttime routine that helps them get to sleep easier
- helping them list off relaxing hobbies to try, like yoga, watercolor painting, or gardening
- encouraging healthy coping skills, like listening to music or practicing mindfulness meditation
Many people have trouble accessing community support with finding work or living arrangements.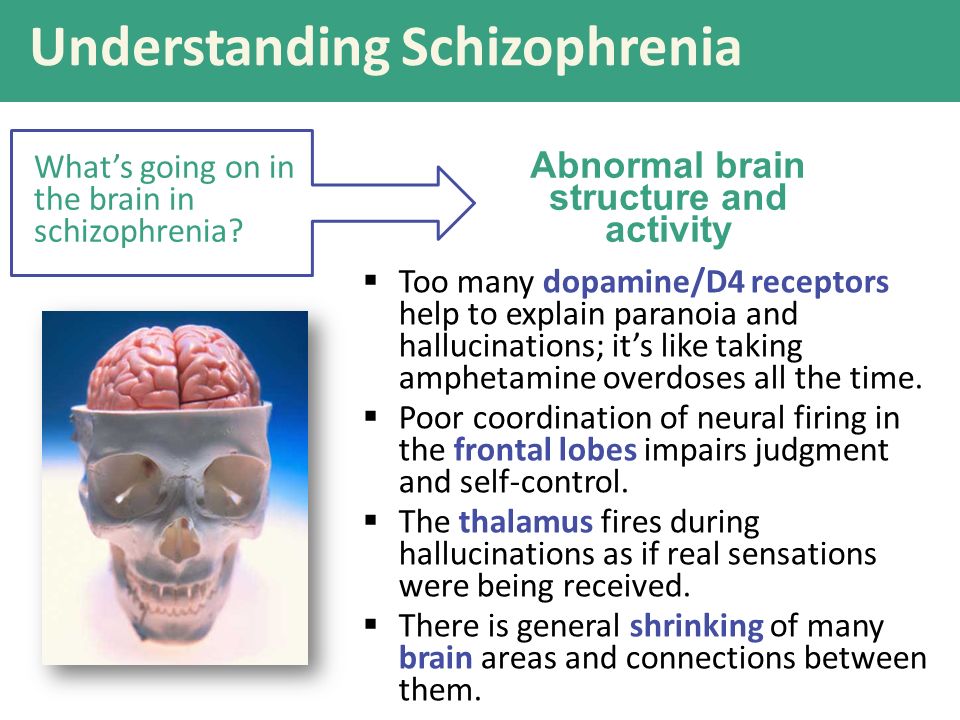 With their permission, you can also offer support by acting as their advocate and making phone calls on their behalf.
With their permission, you can also offer support by acting as their advocate and making phone calls on their behalf.
If you’re not able to offer that support, you could offer to contact someone else they trust instead.
There are plenty of ways to show support for someone with schizophrenia, but there are a few things you’ll want to avoid doing.
Challenging or denying hallucinations and delusions
Many people think it’s best to gently counter hallucinations or delusions by saying something like, “That’s not real, or I would see it, too.”
Yet these symptoms are very real to them, and denying their reality often just ends up driving them away.
They may decide they can’t trust or confide in you since you don’t believe them. A lack of trust can make it more difficult to support them and encourage them to get help for symptoms.
Offering support doesn’t mean pretending to believe in the hallucinations or delusions. You can simply say:
- “It must feel so upsetting to hear those voices.
 ”
” - “That sounds so confusing and stressful.”
Doing everything for them
When your loved one is unable to do chores, errands, or daily tasks, you might try to help by taking over those responsibilities.
But it’s often more helpful to encourage them to take steps toward doing these things themselves and offering support when needed.
You can also ask if there’s anything specific getting in the way of tasks:
- If they haven’t done laundry because they ran out of laundry soap and feel afraid of leaving the house, you could offer to do a grocery run.
- If they can’t prepare meals because a voice threatens them whenever they pick up a knife, you might help them chop a few days’ worth of vegetables in advance.
You can also offer to help them plan and schedule out weekly responsibilities when you spend time together.
Blaming or judging
Your loved one can’t help having schizophrenia, and they can’t control the symptoms they experience. Even with medication and therapy, hallucinations, delusions, and other symptoms may never go away completely.
Even with medication and therapy, hallucinations, delusions, and other symptoms may never go away completely.
Offering compassion and respect is the best way to support them and maintain your connection, even when their behavior confuses or frustrates you.
If you feel overwhelmed or burned out, it’s always OK to help them reach out to another support person or professional.
If your loved one talks about suicide or dying or has serious symptoms of psychosis, help them get immediate care.
Signs of a severe episode of psychosis might include:
- not recognizing their surroundings or loved ones
- not knowing who they are
- saying things that don’t make sense
- talking about hurting themselves or others
- engaging in behaviors that put them in danger, like trying to drive or go outside while disoriented
Check their crisis plan for emergency contact numbers and their preferred approach to treatment. Stay with them, if possible, or contact another support person to keep them company.
If you can’t find their crisis plan and they seem very distressed, it may be time to call 911 or the nearest psychiatric hospital. Explain that your loved one has schizophrenia and that you believe they’re having an episode of psychosis.
In the meantime:
- Give them space.
- Avoid touching them without asking first.
- Speak in a calm, quiet voice.
- Keep any directions simple, clear, and easy to follow.
- Narrate your actions, like, “I’m going to make a phone call now” and “Is it all right if I come sit next to you?”
Schizophrenia is a mental health condition that may never fully go away.
Professional treatment and support can go a long way toward helping your loved one get relief from symptoms and build coping skills.
Don’t forget, though, that your compassionate support can also make a big difference by motivating them to seek help for symptoms and keep up with their treatment plan.
Crystal Raypole has previously worked as a writer and editor for GoodTherapy.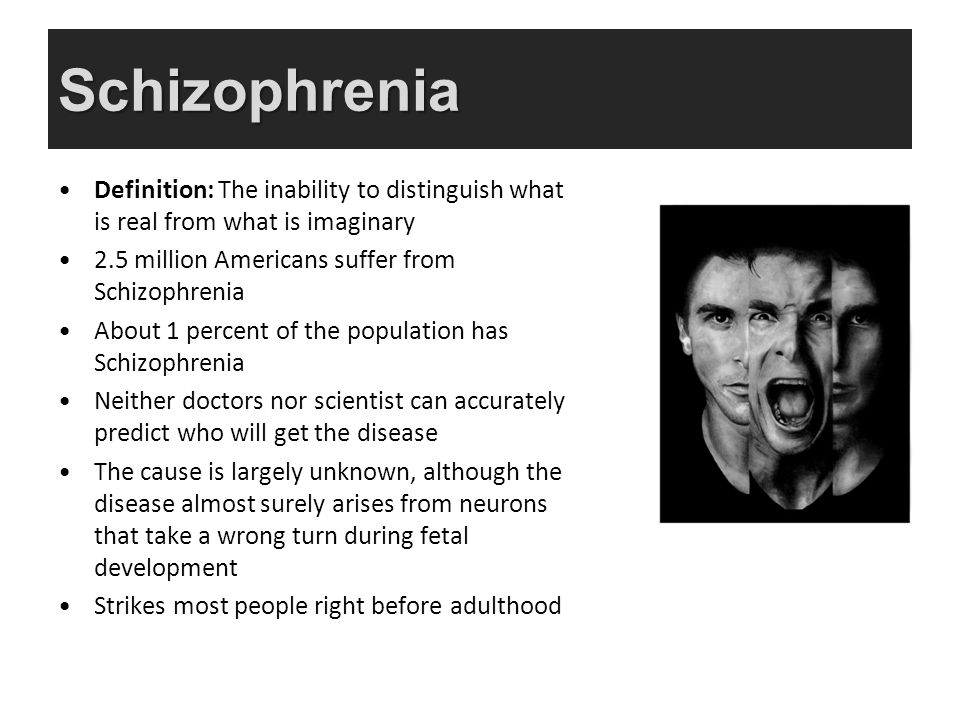 Her fields of interest include Asian languages and literature, Japanese translation, cooking, natural sciences, sex positivity, and mental health. In particular, she’s committed to helping decrease stigma around mental health issues.
Her fields of interest include Asian languages and literature, Japanese translation, cooking, natural sciences, sex positivity, and mental health. In particular, she’s committed to helping decrease stigma around mental health issues.
Schizophrenia
Schizophrenia- Healthcare issues »
- A
- B
- B
- G
- D
- E
- and
- 9000 About
- P
- P
- With
- T
- in
- F
- x
- 9 h
- K.
- S
- B
- E
- S
- I
- Popular Topics
- Air pollution
- Coronavirus disease (COVID-19)
- Hepatitis
- Data and statistics »
- News bulletin
- The facts are clear
- Publications
- Find country »
- A
- B
- C
- g
- D
- E
- and
- th
- K
- L
- 9000 N
- 9000
- in
- Ф
- x
- C hours
- Sh
- Sh.

- K
- E 9000 WHO in countries »
- Reporting
- Regions »
- Africa
- America
- Southeast Asia
- Europe
- Eastern Mediterranean
- Western Pacific
- Media Center
- Press releases
- Statements
- Media messages
- Comments
- Reporting
- Online Q&A
- Developments
- Photo reports
- Questions and answers
- Update
- Emergencies "
- News "
- Disease Outbreak News
- WHO Data »
- Dashboards »
- COVID-19 Monitoring Dashboard
- Basic moments "
- About WHO »
- CEO
- About WHO
- WHO activities
- Where does WHO work?
- Governing Bodies »
- World Health Assembly
- Executive committee
- Main page/
- Media Center /
- Newsletters/
- Read more/
- Schizophrenia
Key Facts
- Schizophrenia is a severe mental disorder that affects approximately 24 million people, or 1 in 300 people worldwide.

- Schizophrenia causes psychosis, is associated with severe disability, and can negatively affect all areas of life, including personal, family, social, academic and work life.
- People with schizophrenia are often subject to stigma, discrimination and human rights violations.
- Worldwide, more than two thirds of people with psychosis do not receive specialized mental health care.
- There are a number of effective care options for patients with schizophrenia that can lead to a complete recovery of at least one in three patients.
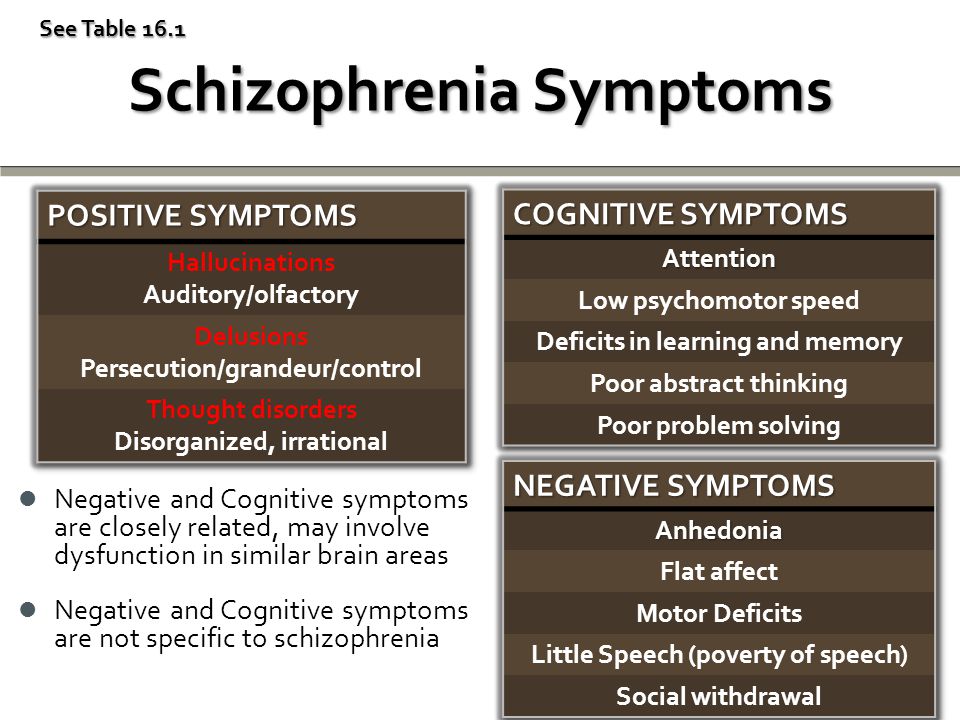
Symptoms
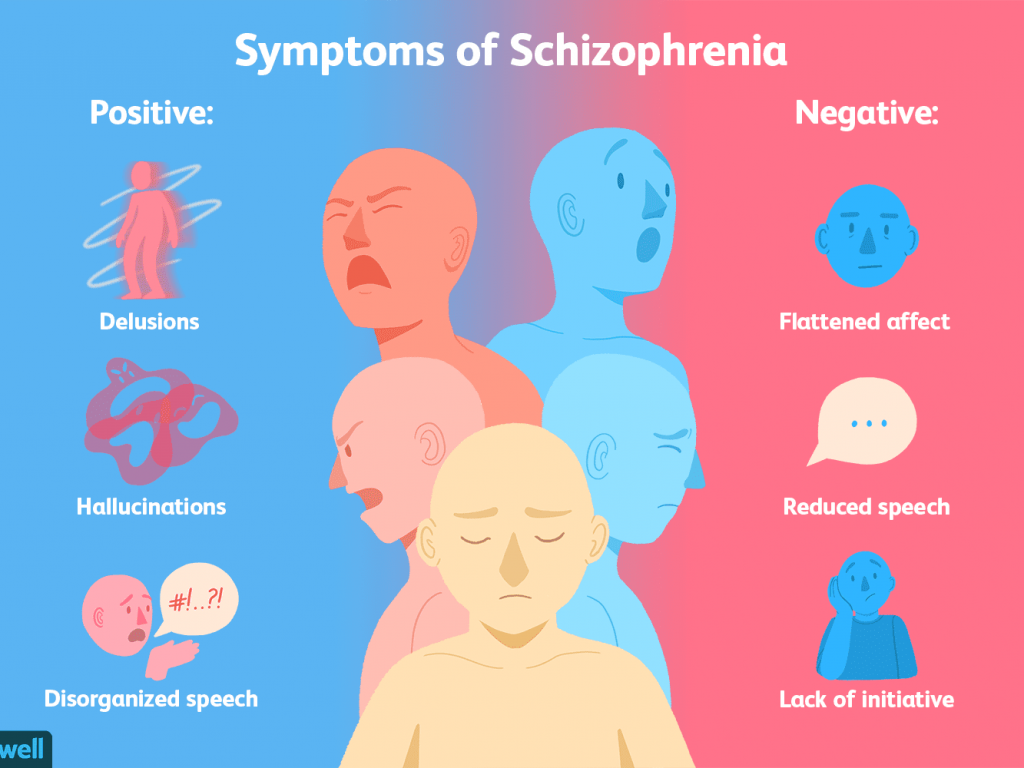
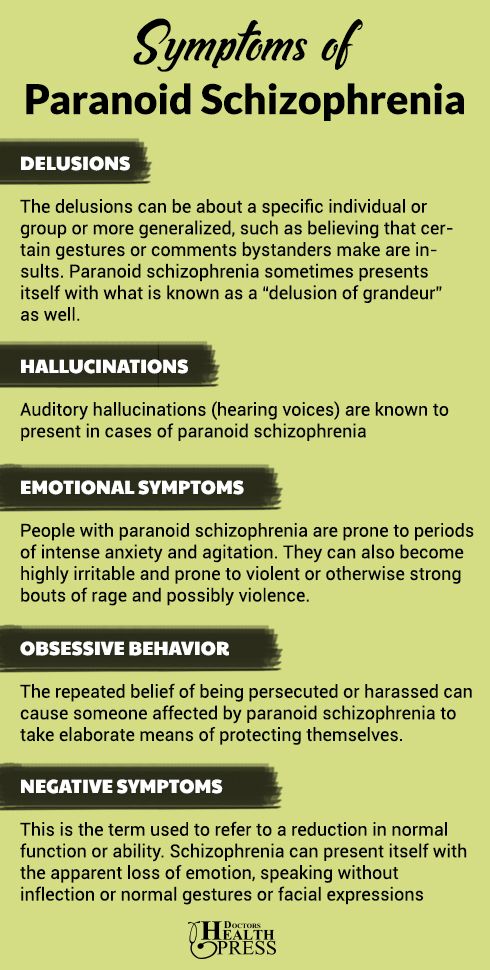
Schizophrenia is characterized by significant disturbances in perception of reality and behavioral changes such as:
- persistent delusions: the patient has a persistent belief in the truth of certain things, despite evidence to the contrary;
- persistent hallucinations: the patient hears, sees, touches non-existent things and smells non-existent smells;
- feeling of external influence, control or passivity: the presence in the patient of the feeling that his feelings, impulses, actions or thoughts are dictated from outside, put in or disappear from consciousness at the will of others, or that his thoughts are broadcast to others;
- disorganized thinking, often expressed in incoherent or pointless speech;
- Significant disorganization of behavior, which is manifested, for example, by the patient performing actions that may seem strange or meaningless, or in an unpredictable or inappropriate emotional reaction that does not give the patient the opportunity to organization of their behavior;
- "negative symptoms" such as extreme poverty of speech, smoothness of emotional reactions, inability to feel interest or pleasure, social autism; and/or
- Extreme agitation or, on the contrary, slowness of movements, freezing in unusual postures.

People with schizophrenia often also experience persistent cognitive or thinking problems that affect memory, attention, or problem-solving skills.
At least one third of patients with schizophrenia experience complete remission of symptoms (1). In some, periods of remission and exacerbation of symptoms follow each other throughout life, in others there is a gradual increase in symptoms.
Scope and impact
Schizophrenia affects approximately 24 million people, or 1 in 300 people (0.32%) worldwide. Among adults, the rate is 1 in 222 (0.45%) (2). Schizophrenia is less common than many other mental disorders. Onset is most common in late adolescence and between the ages of 20 and 30; while women tend to have a later onset of the disease.
Schizophrenia is often accompanied by significant stress and difficulties in personal relationships, family life, social contacts, studies, work or other important areas of life.
Individuals with schizophrenia are 2-3 times more likely to die early than the population average (2). It is often associated with physical illnesses such as cardiovascular disease, metabolic disease, and infectious disease.
It is often associated with physical illnesses such as cardiovascular disease, metabolic disease, and infectious disease.
Patients with schizophrenia often become the object of human rights violations both within the walls of psychiatric institutions and in everyday life. Significant stigmatization of people with this disease is a widespread phenomenon that leads to their social isolation and has a negative impact on their relationships with others, including family and friends. This creates grounds for discrimination, which in turn limits access to health services in general, education, housing and employment.
Humanitarian emergencies and health crises can cause intense stress and fear, disrupt social support mechanisms, lead to isolation and disruption of health services and supply of medicines. All these shocks can have a negative impact on the lives of people with schizophrenia, in particular by exacerbating existing symptoms of the disease. People with schizophrenia are more vulnerable during emergencies to various human rights violations and, in particular, face neglect, abandonment, homelessness, abuse and social exclusion.
Causes of schizophrenia
Science has not established any one cause of the disease. It is believed that schizophrenia may be the result of the interaction of a number of genetic and environmental factors. Psychosocial factors may also influence the onset and course of schizophrenia. In particular, heavy marijuana abuse is associated with an increased risk of this mental disorder.
Assistance services
At present, the vast majority of people with schizophrenia do not receive mental health care worldwide. Approximately 50% of patients in psychiatric hospitals are diagnosed with schizophrenia (4). Only 31.3% of people with psychosis get specialized mental health care (5). Much of the resources allocated to mental health services are inefficiently spent on the care of patients admitted to psychiatric hospitals.
Available scientific evidence clearly indicates that hospitalization in psychiatric hospitals is not an effective treatment for mental disorders and is regularly associated with the violation of the basic rights of patients with schizophrenia. Therefore, it is necessary to ensure the expansion and acceleration of work on the transfer of functions in the field of mental health care from psychiatric institutions to the level of local communities. Such work should begin with the organization of the provision a wide range of quality community-based mental health services. Options for community-based mental health care include integrating this type of care into primary health care and hospital care. general care, setting up community mental health centres, outpatient care centres, social housing with nursing care and social home care services. Involvement in the care process is important the patient with schizophrenia, his family members and members of local communities.
Therefore, it is necessary to ensure the expansion and acceleration of work on the transfer of functions in the field of mental health care from psychiatric institutions to the level of local communities. Such work should begin with the organization of the provision a wide range of quality community-based mental health services. Options for community-based mental health care include integrating this type of care into primary health care and hospital care. general care, setting up community mental health centres, outpatient care centres, social housing with nursing care and social home care services. Involvement in the care process is important the patient with schizophrenia, his family members and members of local communities.
Schizophrenia management and care
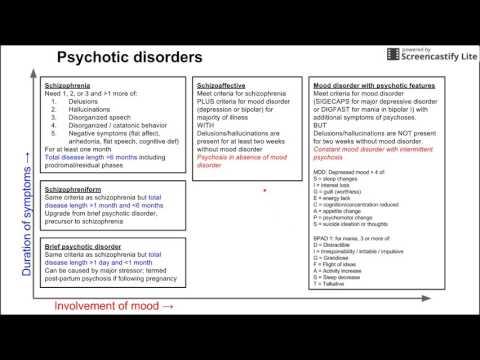
There are a number of effective approaches to treating people with schizophrenia, including medication, psychoeducation, family therapy, cognitive behavioral therapy, and psychosocial rehabilitation (eg, life skills education).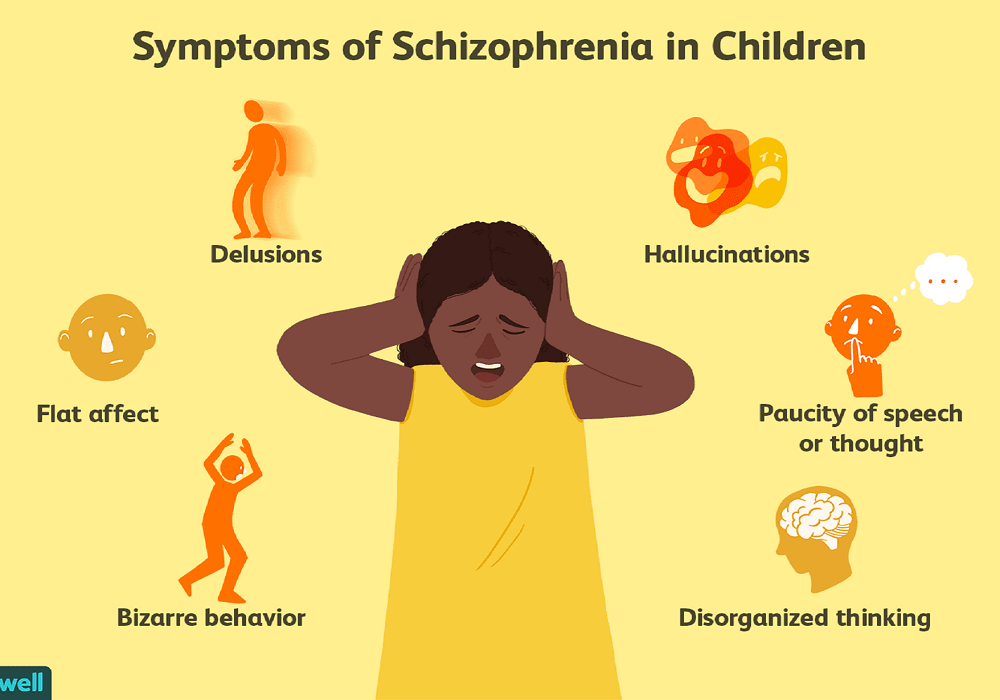 The most important interventions for helping people with schizophrenia are assisted living, special housing and employment assistance. It is extremely important for people with schizophrenia and their families and/or caregivers to a recovery-centered approach that empowers people to participate in decisions about their care.
The most important interventions for helping people with schizophrenia are assisted living, special housing and employment assistance. It is extremely important for people with schizophrenia and their families and/or caregivers to a recovery-centered approach that empowers people to participate in decisions about their care.
WHO action
steps are in place to ensure that appropriate services are provided to people with mental disorders, including schizophrenia. One of the key recommendations The action plan is to transfer the function of providing assistance from institutions to local communities. WHO Special Mental Health Initiative aims to further progress towards the goals of the Comprehensive Plan mental health action 2013–2030 by ensuring that 100 million more people have access to quality and affordable mental health care.
The WHO Mental Health Gap Action Program (mhGAP) is working to develop evidence-based technical guidelines, tools and training packages to scale up services in countries, especially in low-resource settings.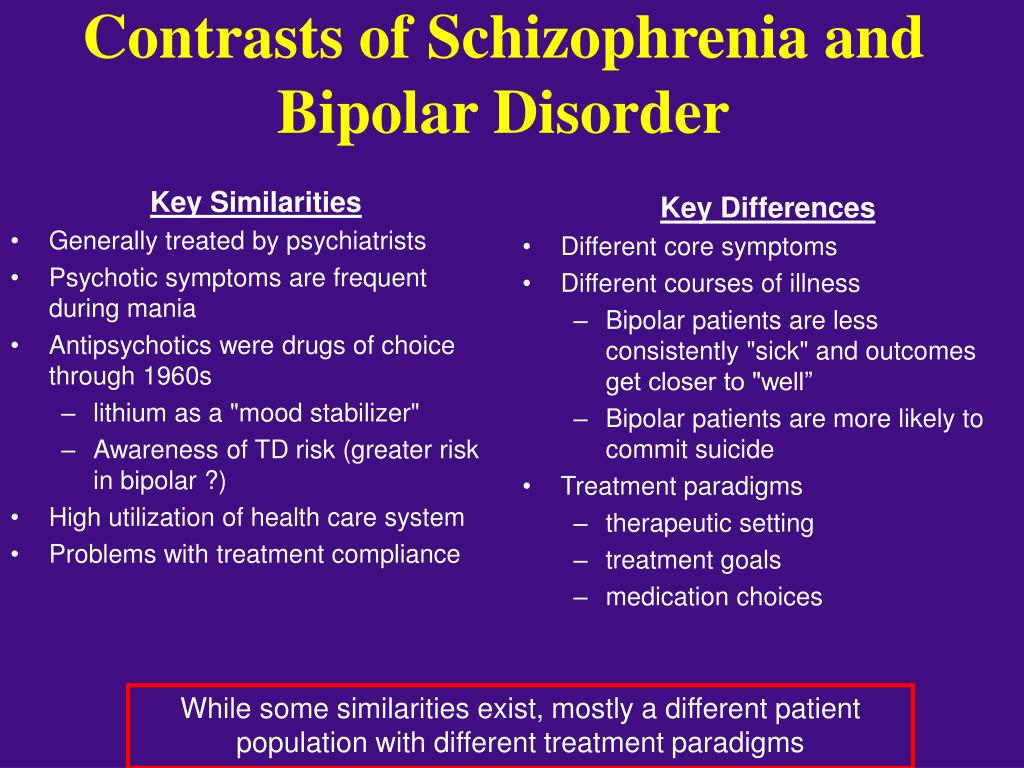 The program focuses on a priority list of mental health disorders, including psychosis, and aims to strengthen the capacity of non-specialized health workers in as part of an integrated approach to mental health care at all levels of care. To date, the mhGAP Program has been implemented in more than 100 WHO Member States.
The program focuses on a priority list of mental health disorders, including psychosis, and aims to strengthen the capacity of non-specialized health workers in as part of an integrated approach to mental health care at all levels of care. To date, the mhGAP Program has been implemented in more than 100 WHO Member States.
The WHO QualityRights project aims to improve the quality of care and better protect human rights in mental health and social care settings and to expand opportunities of various organizations and associations to defend the rights of persons with mental disorders and psychosocial disabilities.
The WHO guidelines on community mental health services and human rights-based approaches provide information for all stakeholders who intend to develop or transform mental health systems and services. health in accordance with international human rights standards, including the UN Convention on the Rights of Persons with Disabilities.
Bibliography
(1) Harrison G, Hopper K, Craig T, Laska E, Siegel C, Wanderling J. Recovery from psychotic illness: a 15- and 25-year international follow-up study. Br J Psychiatry 2001;178:506-17.
Recovery from psychotic illness: a 15- and 25-year international follow-up study. Br J Psychiatry 2001;178:506-17.
(2) Institute of Health Metrics and Evaluation (IHME). Global Health Data Exchange (GHDx). http://ghdx.healthdata.org/gbd-results-tool?params=gbd-api-2019-permalink/27a7644e8ad28e739382d31e77589dd7 (accessed 25 September 2021)
(3) LaursenTM, Nordentoft M, Mortensen PB. Excess early mortality in schizophrenia. Annual Review of Clinical Psychology , 2014;10, 425-438.
(4) WHO. Mental health systems in selected low- and middle-income countries: a WHO-AIMS cross-national analysis. WHO: Geneva, 2009
(5) Jaeschke K et al. Global estimates of service coverage for severe mental disorders: findings from the WHO Mental Health Atlas 2017 Glob Ment Health 2021;8:e27.
10 questions about schizophrenia - Gazeta.Ru
Are people with schizophrenia dangerous? Are they boisterous? Hear voices? Are they isolated from society? "Gazeta.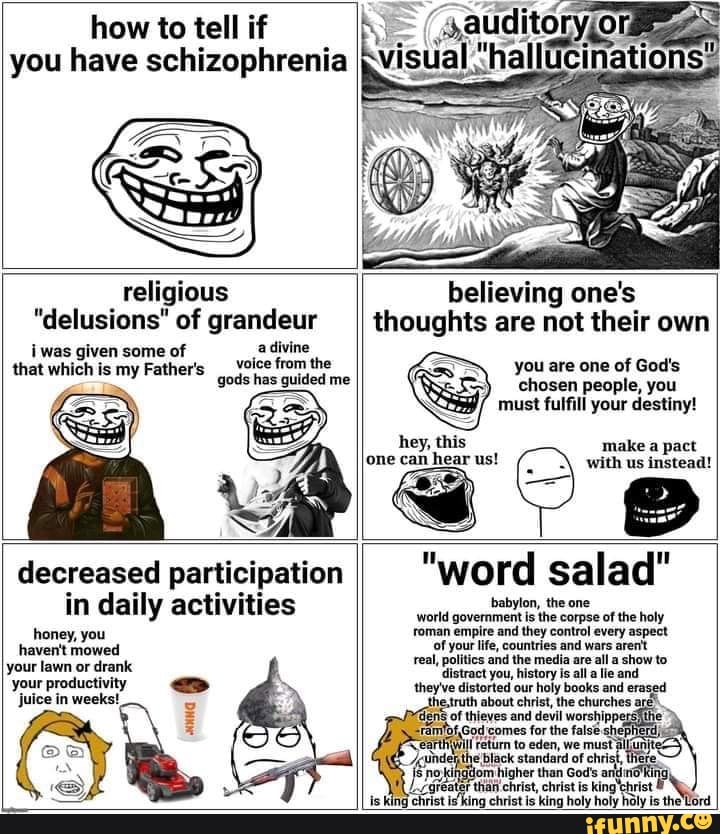 Ru" answers questions that are formed by common myths about schizophrenia. This material is conceived as an educational program with the aim of destigmatizing the diagnosis of schizophrenia. With its help, we would like to convey the thesis that the diagnosis of schizophrenia is not a final verdict, and ordinary life is possible with it.
Ru" answers questions that are formed by common myths about schizophrenia. This material is conceived as an educational program with the aim of destigmatizing the diagnosis of schizophrenia. With its help, we would like to convey the thesis that the diagnosis of schizophrenia is not a final verdict, and ordinary life is possible with it.
1. Who is to blame if a person develops schizophrenia?
Medicine does not yet know what causes the disorder. It is assumed that this is a coincidence of genetic factors, violations of chemical processes in the brain and environmental influences.
Scientists cannot examine and evaluate the processes that take place in the brain of people diagnosed with schizophrenia. But the studies that are already available have shown that in this disease there are problems in the work of neurotransmitters, mainly dopamine. These are substances through which impulses are transmitted from one nerve cell to another. The brain and central nervous system are also somewhat altered in this disorder. But how these changes affect and when they develop is still unknown.
But how these changes affect and when they develop is still unknown.
2. Is there any way I can tell if I or a loved one has schizophrenia?
Diagnosing schizophrenia in oneself is quite difficult: people with a mental disorder most often do not realize that something is wrong with them. Relatives and friends of the sick person who notice changes in behavior, thinking, habits, and reactions often turn to specialists.
The first signs of the disease can not always be recognized precisely as pathological. A person can joke strangely, move away from people and the professional community. He can talk about unusual feelings and experiences, share unusual ideas and try to implement them. In general terms, his behavior can be described as follows: a closed eccentric, convinced of his inventions. Perhaps this is just a temporary state caused by some kind of experience or stress. But sometimes schizophrenia begins with such non-obvious symptoms.
3. How do people behave when they definitely have schizophrenia?
The disease manifests itself differently in everyone, in different combinations of symptoms and complaints. If relatives or the person himself notice that his (her) condition has signs of a mental disorder, then you need to contact a specialist - only he can diagnose and distinguish one disease from another with similar symptoms.
If relatives or the person himself notice that his (her) condition has signs of a mental disorder, then you need to contact a specialist - only he can diagnose and distinguish one disease from another with similar symptoms.
In general, symptoms of schizophrenia may include:
- Delirium. A person begins to think that something is happening that has something to do with him or the world around him: as if someone is watching him, persecuting him, trying to harm him, slander, offend him. It may seem to a patient with schizophrenia that someone has written down thoughts, conversations, texts, tasks in his head and made him think about it, pronounce it, decide it. He is sure that others also hear what is going on in his head, and tries to communicate on this topic. For some, information “appears” that something tragic, dangerous is about to happen in the country, in the world, on Earth. The most important thing is that a person sincerely believes in the reality of all this.
- Hallucinations. These are false auditory, tactile, visual sensations. A person with schizophrenia lives them, for him they are real.
- Negative symptoms. What is listed above is called productive symptoms - they were brought by the disease, this is its product. Negative symptoms are those that the disease takes away, minus from the life of the sick person. The liveliness of movements, energy, will, desire to do something, to communicate disappear. A patient with schizophrenia may not want anything, he (she) is not interested in anything, he (she) ceases to take care of himself and observe the simplest hygiene.
- Disorders of thought and speech. For others, they look like a "salad of thoughts and words." The sick person may ask questions to himself or receive them from others, begin to answer and get confused in words.
- Unusual behavior. A person becomes characterized by childishness, antics, frozen postures, or, conversely, fussy and meaningless movements, which often do not fit either with the situation, or with the environment, or with the tasks.
4. So, if my friend has these symptoms, then he (she)…?
Not always. Yes, and one symptom from this description, and a combination of several, may indicate schizophrenia, but in the same way they can be disguised as manifestations of a completely different disorder.
close
100%
A non-specialist should not suspect schizophrenia in a person. Even experienced professionals conduct many examinations and tests before making a diagnosis. Therefore, the best tactic in this case is to convince to visit a specialist.
5. It seems that this happened to my loved one. Will he be sent to a psychiatric hospital now?
Optional. Schizophrenia can proceed in different ways, many are successfully treated only at home, on an outpatient basis. If the behavior of your loved one has changed and has become a concern, then do not invent diagnoses, and even more so do not voice the assumption to outsiders. Talk to the person himself, find out what he feels and what worries him. And together with him sign up for a specialist if you understand that he:
And together with him sign up for a specialist if you understand that he:
- has become suspicious, listens to something, checks something;
- suddenly loses thought or thread of conversation, breaks off speech in mid-sentence or does not complete business;
- has problems with social adaptation (cannot perform the simplest actions - for example, buy groceries in a store).
Unfortunately, the circumstances of the disease develop in such a way that from the very beginning the sick person needs help and support from relatives and friends. And it starts with the need to convince him to go to a specialist.
You may have seen the movie A Beautiful Mind. It was created based on the life story of a real-life American mathematician, scientist and Princeton University professor John Nash. He had schizophrenia, which caused his strange behavior, but did not lead to the loss of the ability to think scientifically. The film shows well how the support of loved ones helped John Nash.
This is, of course, a separate example, but it shows that it is wrong to equate schizophrenia with complete loss of reason. The disease can proceed in different ways, the treatment can be so effective that a person will live almost the same as before.
6. Registration
It's not a shame. This is right and necessary: everyone should receive treatment for their disease. Help for schizophrenia is provided by a specialist, and accounting is a diary of monitoring the course of the disease. It has long been understood abroad that only treatment and control help many people with schizophrenia avoid difficult life situations (vagrancy, alcohol or drug abuse), notice a relapse (return of symptoms) in time, and return to remission.
7. So now you are on pills all your life?
That would be perfect! If loved ones can convince a person with schizophrenia to take prescribed medications and come to check-ups on time, then symptoms can be controlled and a relapse can be prevented.
8. What does “under control” mean? Don't pills cure?
Control means with the help of medicines and additional methods (psychotherapy, for example) to make the symptoms of the disease affect life as little as possible. This is called remission. With a favorable course of the disease, remission on medications can be such that a person will remain in society, will live almost the same as before the diagnosis.
close
100%
Some people with this condition manage to take control of their medication and treatment. But still, most need support from loved ones, compassion without obsession and excessive anxiety. In practice, this can be a donated pill box, in which the desired drug is pre-filled. Or creating a calm environment in the house and a joint visit to a psychotherapist. Or daily walks and organizing participation in household chores so that a person does not feel excluded from family life and does not concentrate on experiences.
9. When can a person be considered healthy?
There is no cure for schizophrenia yet. And there are many diseases that can only be brought into remission with the help of drugs: for example, diabetes mellitus or hypertension - people have to take drugs all their lives, but no one considers them to be defective.
And there are many diseases that can only be brought into remission with the help of drugs: for example, diabetes mellitus or hypertension - people have to take drugs all their lives, but no one considers them to be defective.
And, of course, the scientific world is looking for, developing, testing drugs that can work as efficiently as possible. For example, in Russia there is a drug from the pharmaceutical company Gideon Richter, which can help fight productive and negative symptoms and make it possible to live more harmoniously in society.
10. They say that people with such a diagnosis can suddenly attack, try to kill, do they become strong like animals?
There are factors that can lead to an outbreak of aggression. But this does not mean that the sick are just waiting for someone to attack. If you had to deal with this, then protect the patient (close the windows, turn off the gas, take away knives and matches, etc.), yourself, family members, animals and call an ambulance, telling what is happening.