Conduct disorder adolescents
Conduct Disorder
Conduct Disorder
No. 33; Updated June 2018
"Conduct disorder" refers to a group of repetitive and persistent behavioral and emotional problems in youngsters. Children and adolescents with this disorder have great difficulty following rules, respecting the rights of others, showing empathy, and behaving in a socially acceptable way. They are often viewed by other children, adults and social agencies as "bad" or delinquent, rather than mentally ill. Many factors may lead to a child developing conduct disorder, including brain damage, child abuse or neglect, genetic vulnerability, school failure, and traumatic life experiences.
Children or adolescents with conduct disorder may exhibit some of the following behaviors:
Aggression to people and animals
- bullies, threatens or intimidates others
- delights in being cruel and mean to others
- starts physical fights
- has used a weapon that could cause serious physical harm to others (e.
g. a bat, brick, broken bottle, knife or gun)
- is physically cruel to people or animals
- steals from a victim while hurting them
- forces someone into sexual activity
- shows no genuine remorse after an aggressive episode
Destruction of Property
- deliberately engaged in fire setting with the intention to cause damage
- deliberately destroys other's property
Deceitfulness, lying, or stealing
- has broken into someone else's building, house, or car
- lies to obtain goods, or favors or to avoid obligations
- steals items without confronting a victim (e.g. shoplifting, but without breaking and entering)
Serious violations of rules
- often stays out at night despite parental objections
- runs away from home
- often stays away from
Children who exhibit these behaviors should receive a comprehensive evaluation by an experience mental health professional.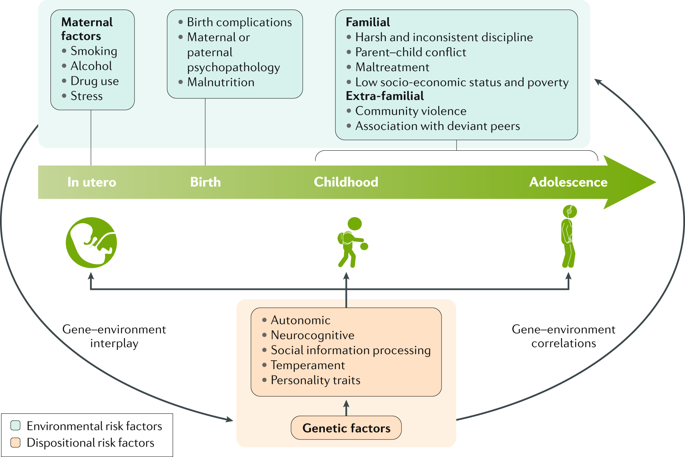 Many children with a conduct disorder may have coexisting conditions such as mood disorders, anxiety, PTSD, substance abuse, ADHD, learning problems, or thought disorders which can also be treated. Research shows that youngsters with conduct disorder are likely to have ongoing problems if they and their families do not receive early and comprehensive treatment. Without treatment, many youngsters with conduct disorder are unable to adapt to the demands of adulthood and continue to have problems with relationships and holding a job.
Many children with a conduct disorder may have coexisting conditions such as mood disorders, anxiety, PTSD, substance abuse, ADHD, learning problems, or thought disorders which can also be treated. Research shows that youngsters with conduct disorder are likely to have ongoing problems if they and their families do not receive early and comprehensive treatment. Without treatment, many youngsters with conduct disorder are unable to adapt to the demands of adulthood and continue to have problems with relationships and holding a job.
Treatment of children with conduct disorder can be complex and challenging. Treatment can be provided in a variety of different settings depending on the severity of the behaviors. Adding to the challenge of treatment are the child's uncooperative attitude, fear and distrust of adults. In developing a comprehensive treatment plan, a child and adolescent psychiatrist may use information from the child, family, teachers, community (including the legal system) and other medical specialties to understand the causes of the disorder.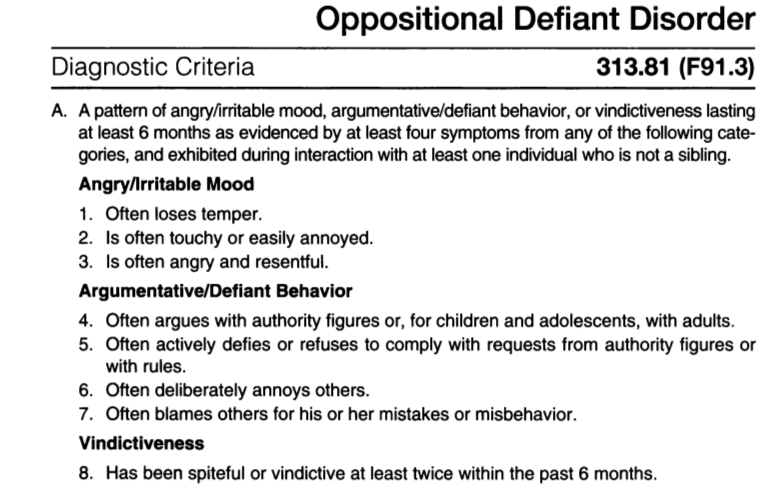
Behavior therapy and psychotherapy are usually necessary to help the child appropriately express and control anger. Special education may be needed for youngsters with learning disabilities. Parents often need expert help to develop and carry out special management and educational programs in the home and at school. Home-based treatment programs such as Multisystemic Therapy (MST) are effective for helping both the child and family.
Treatment may also include medication in some youngsters who may have difficulty paying attention, impulse problems, or depression.
Treatment is rarely brief since establishing new attitudes and behavior patterns takes time. However, early treatment offers a child a better chance for considerable improvement and hope for a more successful future.
If you find Facts for Families© helpful and would like to make good mental health a reality, consider donating to the Campaign for America’s Kids. Your support will help us continue to produce and distribute Facts for Families, as well as other vital mental health information, free of charge.
Your support will help us continue to produce and distribute Facts for Families, as well as other vital mental health information, free of charge.
You may also mail in your contribution. Please make checks payable to the AACAP and send to Campaign for America’s Kids, P.O. Box 96106, Washington, DC 20090.
The American Academy of Child and Adolescent Psychiatry (AACAP) represents over 10,000 child and adolescent psychiatrists who are physicians with at least five years of additional training beyond medical school in general (adult) and child and adolescent psychiatry.
Facts for Families© information sheets are developed, owned and distributed by AACAP. Hard copies of Facts sheets may be reproduced for personal or educational use without written permission, but cannot be included in material presented for sale or profit. All Facts can be viewed and printed from the AACAP website (www.aacap.org). Facts sheets may not be reproduced, duplicated or posted on any other website without written consent from AACAP. Organizations are permitted to create links to AACAP's website and specific Facts sheets. For all questions please contact the AACAP Communications Manager, ext. 154.
Organizations are permitted to create links to AACAP's website and specific Facts sheets. For all questions please contact the AACAP Communications Manager, ext. 154.
If you need immediate assistance, please dial 911.
Copyright © 2022 by the American Academy of Child and Adolescent Psychiatry.
Symptoms, Causes, Diagnosis and Treatment
What are Conduct Disorders?
Conduct disorder refers to a group of behavioral and emotional problems characterized by a disregard for others. Children with conduct disorder have a difficult time following rules and behaving in a socially acceptable way. Their behavior can be hostile and sometimes physically violent.
In their earlier years, they may show early signs of aggression, including pushing, hitting and biting others. Adolescents and teens with conduct disorder may move into more serious behaviors, including bullying, hurting animals, picking fights, theft, vandalism and arson.
Children with conduct disorder can be found across all races, cultures and socioeconomic groups. They often have other mental health issues as well that may contribute to the development of the conduct disorder. The disorder is more prevalent in boys than girls.
What Symptoms Should Parents Look for?
There are four basic types of behavior that characterize conduct disorder:
- Physical aggression (such as cruelty toward animals, assault or rape).
- Violating others’ rights (such as theft or vandalism).
- Lying or manipulation.
- Delinquent behaviors (such as truancy or running away from home).
Conduct disorder is characterized by aggression toward others and a callous disregard for their rights and needs. Adolescents and teens with conduct disorder can find acts of aggression, deceit and coercion to be gratifying. Your child may meet the criteria for conduct disorder if you find them engaging in several of the below behaviors:
- Bullying or threatening behavior
- Physical aggression
- Cruelty toward people or animals
- Fire-setting
- Breaking curfew
- Truancy from home or school
- Trespassing
- Lying
- Cheating
- Stealing
- Vandalism
- Emotionally or physically abusive behaviors (such as wielding a deadly weapon or forcing sex)
Many young people with conduct disorder will have trouble:
- Feeling and expressing empathy or remorse.
- Showing emotion toward others.
- Performing well in the school or community and blaming others for poor performance.
They often misinterpret the actions of others as being hostile or aggressive. They respond by escalating the situation into verbal or physical conflict.
In adolescents and teens, conduct disorder may be associated with other difficulties, including:
- Substance use.
- Risk-taking behavior.
- School problems.
- Physical injury from accidents or fights.
In younger children, it can be more of a challenge to distinguish signs of conduct disorder from more typical “acting out".
At times, these same symptoms can be seen in children without the disorder. The difference is frequency, intensity, and duration, as well as to what extent it impacts their functioning. In children with conduct disorder, these behaviors happen much more frequently.
What Causes Conduct Disorder in Children?
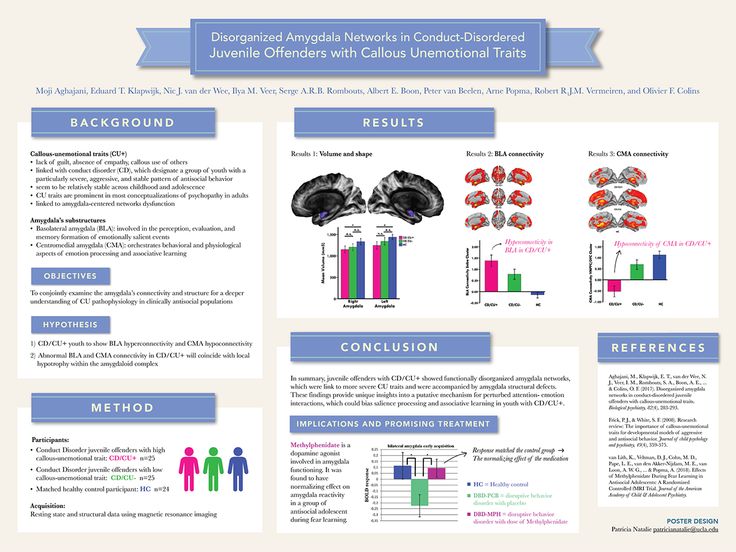
Many factors seem to contribute to this disorder.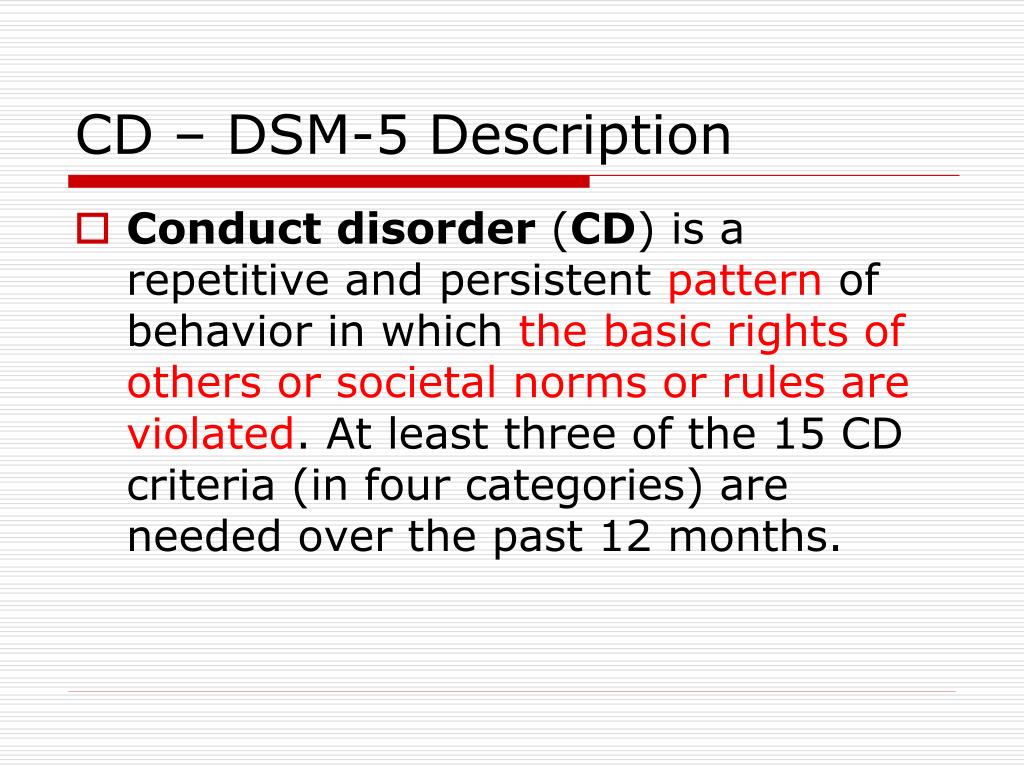 Research has found that children and teens with conduct disorder seem to have an impairment in the frontal lobe of the brain. This interferes with their ability to plan, avoid harm, and learn from negative experiences.
Research has found that children and teens with conduct disorder seem to have an impairment in the frontal lobe of the brain. This interferes with their ability to plan, avoid harm, and learn from negative experiences.
In addition, these factors seem to put children and teens at a higher risk to develop conduct disorder:
- Having experienced abuse, parental rejection or neglect.
- Being diagnosed with other psychiatric disorders.
- Biological parents diagnosed with ADHD, alcohol use disorder, depression, bipolar disorder, or schizophrenia.
- Poor nutrition.
- Living in poverty.
- Maternal psychopathology.
- Poor parenting / lack of parental involvement.
- Inconsistent, overly harsh, or otherwise ineffective discipline.
- Exposure to violence.
- Peer delinquency.
- Having been subjected to physical, sexual, and/or emotional abuse.
- Lack of adequate parental or other adult supervision.
How is Conduct Disorder Diagnosed and Treated?
A child psychiatrist, psychologist, or other qualified mental health professional usually diagnoses conduct disorders in children and teens by completing:
- A detailed history of the child's behavior, as well as relevant biological, psychological, social, and cultural factors, which are identified during a clinical interview with the child and caregiver(s).
- A review of historical data such as school records, court/child welfare records, past treatment records, and interviews with collaterals.
- Additional information can also be obtained via the following:
- Observations of the child's behavior.
- Psychological testing.
Treatment can be complex and challenging. And it can last for several months. Children with conduct disorder tend to be uncooperative with others. They often fear and distrust adults. And adding to the complication is the fact that conduct disorder is often (but not always) diagnosed along with a number of other psychological conditions.
Treatment for conduct disorder may include:
- Multisystemic therapy: Intensive, often home- or community-based interventions to promote positive behavior change in the youth’s environment. Treatment relies heavily on family and school involvement.
- Family therapy.
- Medication.
Conduct disorder can be difficult to overcome. But it is manageable. The earlier the treatment is started after symptoms appear, the more successful it is likely to be.
As with many psychiatric disorders, early intervention is key.
State Autonomous Institution of Social Services of the Sverdlovsk Region "Social and Rehabilitation Center for Minors of the Verkhnesaldinskiy District"
February 25, 2020 at 09:26
The next meeting of the parent club "Rostok" with the parents of foster families was held on February 20, during which the topic was touched upon behavioral disorders in children and adolescents. The meeting, which was held in the form of a psychological and pedagogical training, was attended by parents and teenagers.
The meeting, which was held in the form of a psychological and pedagogical training, was attended by parents and teenagers.
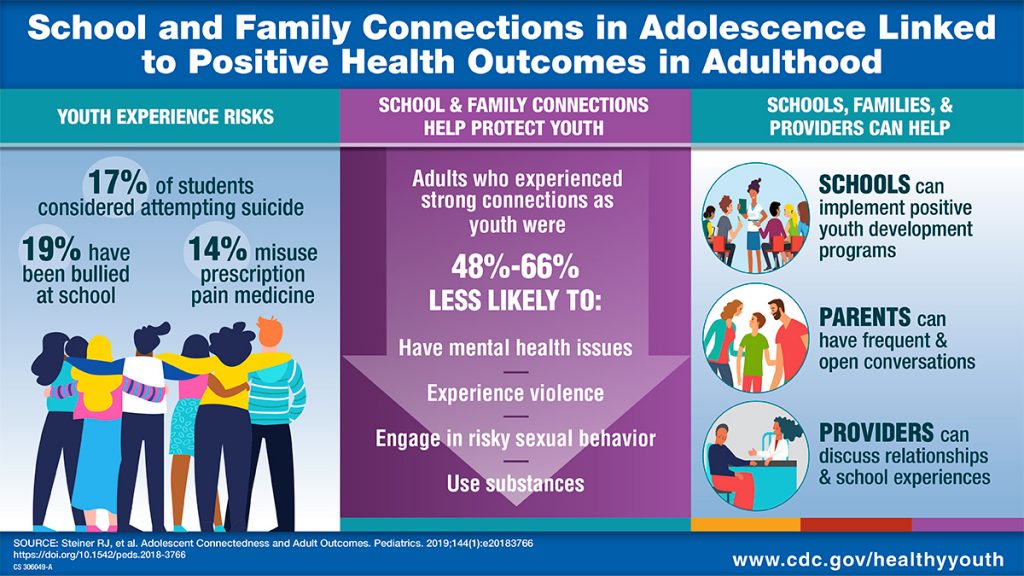
The purpose of the training: improving the psychological and pedagogical parental competence, the use of effective methods and techniques in raising children aimed at correcting their behavioral disorders. The game exercise "ABC of Moods" helped the club members to talk about their feelings and emotions that they were experiencing at the moment. The psychologist provided information that conduct disorder is a syndrome that manifests itself in a persistent inability to control one's behavior, adjusting it to the norms and rules accepted in a given society. This is one of the forms of disorganization of activity, which is most often limited only in the family. Psychologists distinguish 3 degrees of conduct disorder: Weak. Aggressive signs appear only in one area of life - at home or at school. Medium. Negative symptoms appear in several areas (at home, at school, in kindergarten). Strong. The child behaves violently and angrily almost always, in any situation and with different people. But not all disobedience can be attributed to a behavior disorder, these are normal parts of a child’s development, and as they grow older, with proper upbringing, such behavior fades away. Until now, the emotional processes in children with conduct disorder have not been studied enough. But it is known that they often have low self-esteem, a sad mood. Particularly active communication between parents and adolescents was caused by information about the symptoms, signs of conduct disorder. Both parents, relatives, teachers and other adults can provoke the formation of a personality disorder of behavior in children. Younger children show signs of oppositional defiant disorder. This disorder is correctable, so parents can protect the child from its development. Working in groups, parents and adolescents expressed their opinion about the causes of conduct disorder, determined which reactions of behavioral disorganization and at what age are more common.
Strong. The child behaves violently and angrily almost always, in any situation and with different people. But not all disobedience can be attributed to a behavior disorder, these are normal parts of a child’s development, and as they grow older, with proper upbringing, such behavior fades away. Until now, the emotional processes in children with conduct disorder have not been studied enough. But it is known that they often have low self-esteem, a sad mood. Particularly active communication between parents and adolescents was caused by information about the symptoms, signs of conduct disorder. Both parents, relatives, teachers and other adults can provoke the formation of a personality disorder of behavior in children. Younger children show signs of oppositional defiant disorder. This disorder is correctable, so parents can protect the child from its development. Working in groups, parents and adolescents expressed their opinion about the causes of conduct disorder, determined which reactions of behavioral disorganization and at what age are more common. On their personal examples, they were convinced that both the immediate environment - family, relatives, and the wider environment - school, society, peers, have a huge impact on conduct disorder in children and adolescents. Parents were asked to identify methods and techniques aimed at correcting behavior, discuss them, the most effective use in the upbringing and education of children.
On their personal examples, they were convinced that both the immediate environment - family, relatives, and the wider environment - school, society, peers, have a huge impact on conduct disorder in children and adolescents. Parents were asked to identify methods and techniques aimed at correcting behavior, discuss them, the most effective use in the upbringing and education of children.
To create an atmosphere of psychological comfort, emancipation, good mood, specialists of the escort department organized a tea party with sweets. The psychological and pedagogical training ended with the exchange of parents' impressions about relevant information, holding an event, determining their emotional well-being using symbol cards. Parents expressed their desire to meet more often, discuss problem situations together, thanked for the organized event.
Psychologist TSZP.
Mental disorders of adolescence
Posted by: 03.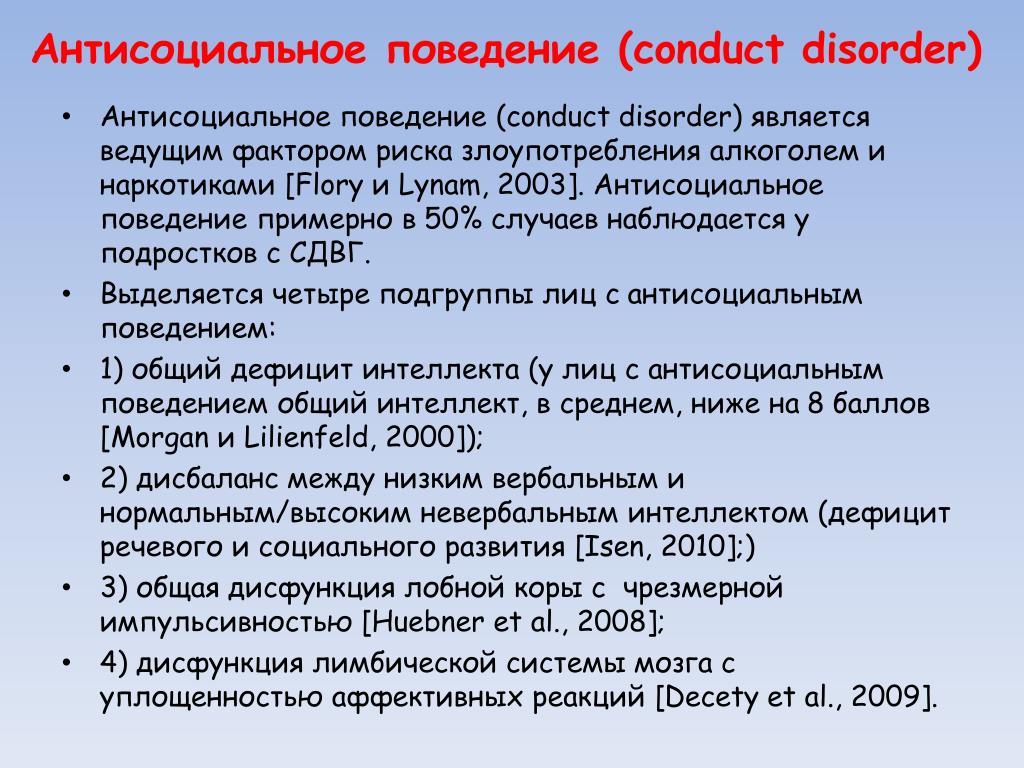 12.2021
12.2021
According to the registration of citizens’ appeals to neuropsychiatric dispensaries and psychiatric hospitals in Moscow in 2018, a psychiatric diagnosis was first established 3,679children under the age of 14. At the same time, a specific weight falls on the share of borderline mental disorders (neurotic reactions, depression, eating disorders, etc.), which require, in contrast to schizophrenia spectrum disorders, more qualified and accurate psychiatric diagnosis.
Mental disorders research data
children and adolescents
The priority of early diagnosis and treatment of mental disorders in adolescence is primarily confirmed by epidemiological studies. In particular, according to current WHO indicators, mental health disorders account for 16% of the global burden of disease and injury among people aged 10-19years. Of particular importance in the light of the increase in the growth rate of borderline mental pathology in the puberty period is the timely detection and treatment of adolescent depression, one of the leading causes of morbidity and disability among minors worldwide, according to current WHO statistics.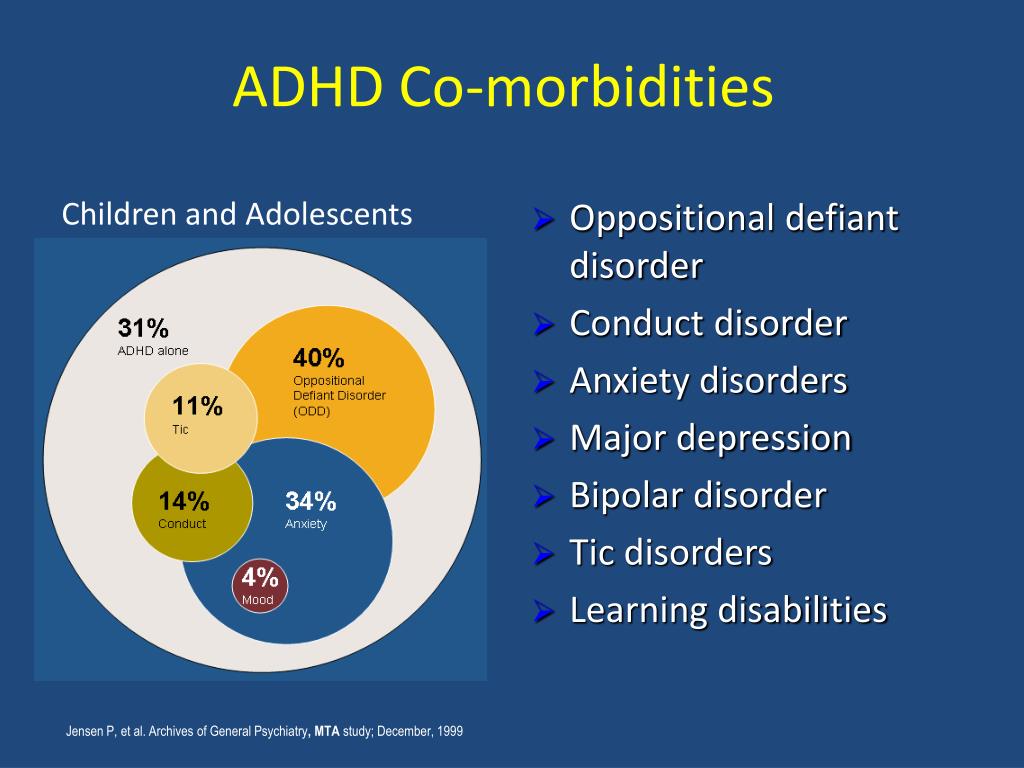 Completed suicides, as a natural outcome of severe depression, are the third leading cause of death in the 15-19 age group.
Completed suicides, as a natural outcome of severe depression, are the third leading cause of death in the 15-19 age group.
Types of mental disorders in adolescents
The spectrum of adolescent mental pathology, primarily requiring the help of a psychiatrist, includes the following nosological units:
- personality disorders
- psychosomatic and affective disorders
- specific behavioral disorders
- anorexia and bulimia nervosa
Personality disorders (in obsolete terminology - psychopathy)
persistent, occurring in childhood and adolescence and remaining in the period of maturity, severe violations of the character and behavior of the individual, accompanied by social and / or educational maladaptation. The reason for contacting a specialist in personality disorders, as a rule, is polymorphic anxiety, depressive and asthenic reactions secondary to the disorder of social and educational adaptation.
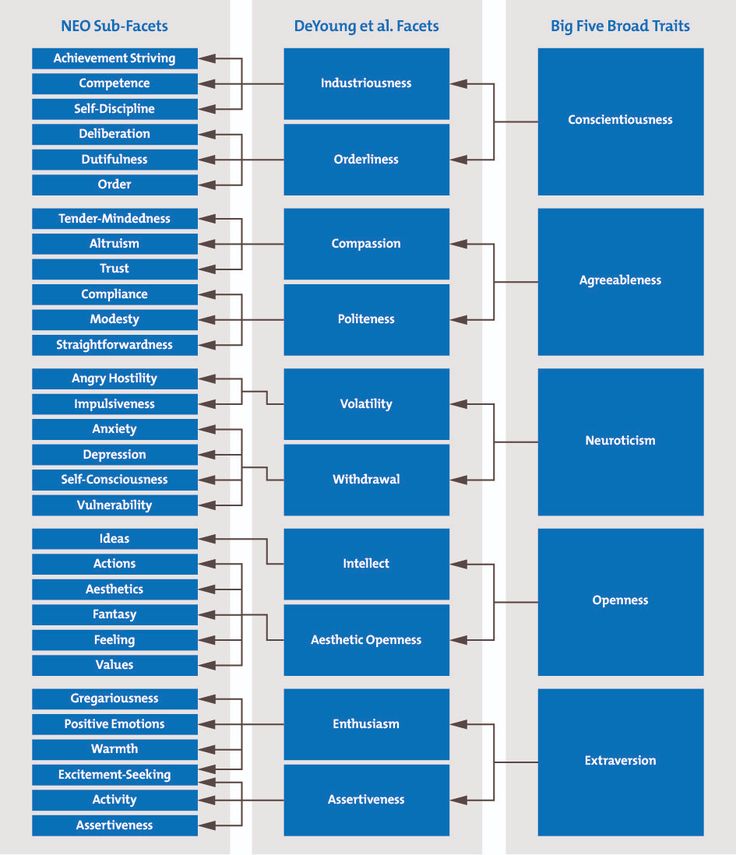
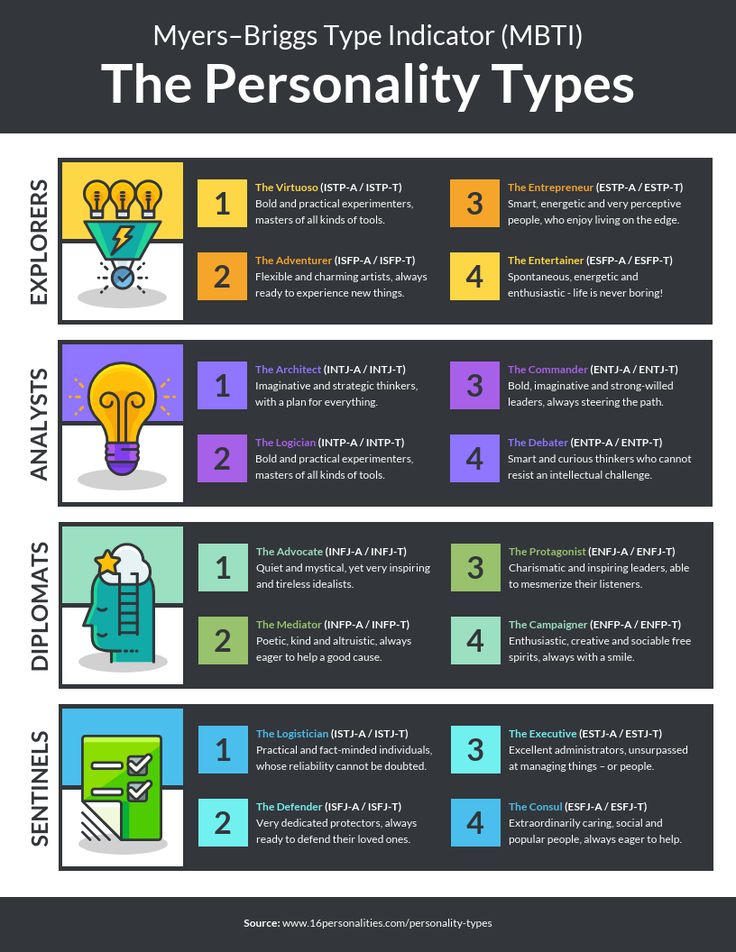
According to the modern diagnostic manual DSM-V, personality disorders are divided into 3 main clusters according to the dominant type of characterological disorders - A, B, C. , emotional coldness, social isolation and / or originality of thinking, eccentricity (in some cases - a distinct eccentricity) of behavior and hobbies.
Cluster B (borderline, hysterical, narcissistic) with a predominance of heightened thirst for recognition, demonstrativeness, emotional instability, irresponsibility and lack of volitional control of behavior (recklessness, infantilism and egocentrism of actions).
Cluster C (avoidant, dependent, obsessive-compulsive PD) is determined by persistent personality disorders such as painful anxiety, shyness, insolvency, a tendency to avoid minimal life difficulties with dependence on the control and guardianship of relatives, and / or pathological perfectionism, regimentation with ease of occurrence fears and fears.
For the diagnosis of personality disorders in clinical practice, the clinical criteria stated in modern diagnostic guidelines (ICD, DSM) are used - in particular:
- Lack of adaptation is persistent, rigid and stable
- Severe impairment or dysfunction due to maladaptive behavior
- Relative stability and early onset of a non-adaptive behavior pattern
Psychosomatic disorders (somatoform/somatized and hypochondriacal disorders)
Includes a wide range of mental pathologies that mimic diseases of the somatic range (cardiopathology, disorders of the gastrointestinal tract, vegetative-vascular dystonia, prolonged fever to subfebrile values, urticaria, etc.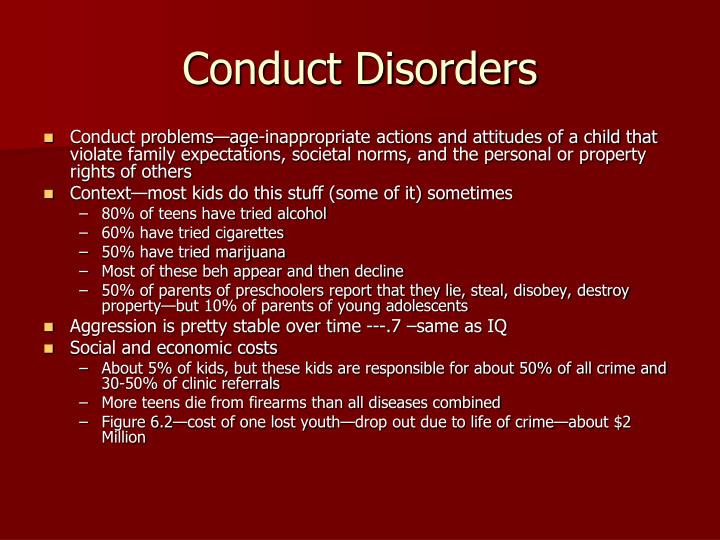 ), and are accompanied by persistent anxiety about one's own health and conviction in the organic nature of suffering.
), and are accompanied by persistent anxiety about one's own health and conviction in the organic nature of suffering.
A distinctive feature is persistent, prolonged and painful bodily sensations localized in a certain system of the body, which, according to functional diagnostics, do not reveal real somatic disorders.
Regardless of the specifics of bodily sensations, the essence of psychosomatic disorders lies in the form of a neurotic hypochondriacal reaction with fixation on one’s own illness, disproportionate intensity of perception of pain phenomena, limitation of life by “behavior in illness” (systematic appeal to doctors; distrust of the data of analyzes that refute the presence of the alleged diseases, refusal of educational and / or daily activities).
The classic variants of somatoform disorders of adolescence include: irritable bowel syndrome, psychogenic flatulence, bladder neurosis, thermoneurosis, cranioalgia (tension headaches), pseudo-allergies, neurogenic psoriasis.
Affective pathology
Depressive disorders are the most common type of affective pathology in adolescence. The urgent need for early diagnosis and specialized treatment is determined by the high suicidal risk of this group of patients.
In modern clinical practice, a depressive disorder is defined as a chronic state of depressed mood, accompanied by a decrease in vitality, apathy, fatigue, sleep and appetite disorders.
In the foreground in the mental status of patients are depression, melancholy with a feeling of heaviness in the chest, apathy and anxiety. The specificity of the option of lowering the mood is determined by the clinical form of the depressive disorder (anxious, apathetic, melancholy, and other depressions). Patients lose their former vivacity, become tired, vulnerable and susceptible to minimal emotional provocateurs - their educational productivity decreases, previously uncharacteristic tearfulness, isolation, a tendency to painful self-flagellation and the formation of ideas of their own insolvency and low value appear. There are sleep disorders such as insomnia and difficulty waking up. Appetite is reduced, or, in the case of anxiety depressions, is modified in the form of compulsive overeating.
There are sleep disorders such as insomnia and difficulty waking up. Appetite is reduced, or, in the case of anxiety depressions, is modified in the form of compulsive overeating.
It is necessary to take into account the fact that depression is officially recognized as a mental illness, the etiology of which is neurotransmitter disorders, in connection with which it is mandatory to require timely medical treatment. Psychotherapeutic correction in the treatment of depressive disorders acts as a significant, however, to a greater extent an auxiliary tool, and cannot be an equivalent replacement for psychopharmacotherapy. Ignoring the need to take specialized medications is fraught with an increase in the severity of depressive symptoms and an increase in suicidal risk.
Behavioral disorders
adolescents are distinguished by particular variability and polymorphism of manifestations. The most common variant of PR, especially maladaptive adolescents at the social and educational level, is the so-called heboid syndrome, characterized by a painful sharpening and distortion of the emotional and volitional characteristics of the personality characteristic of puberty (pathological pubertal crisis).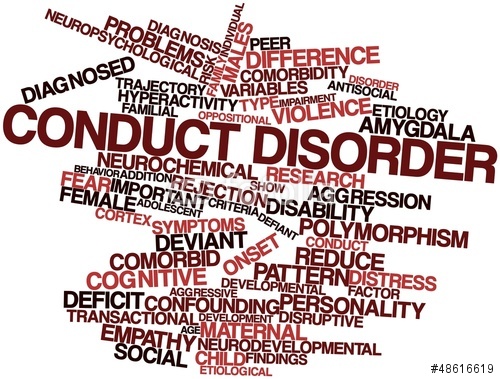
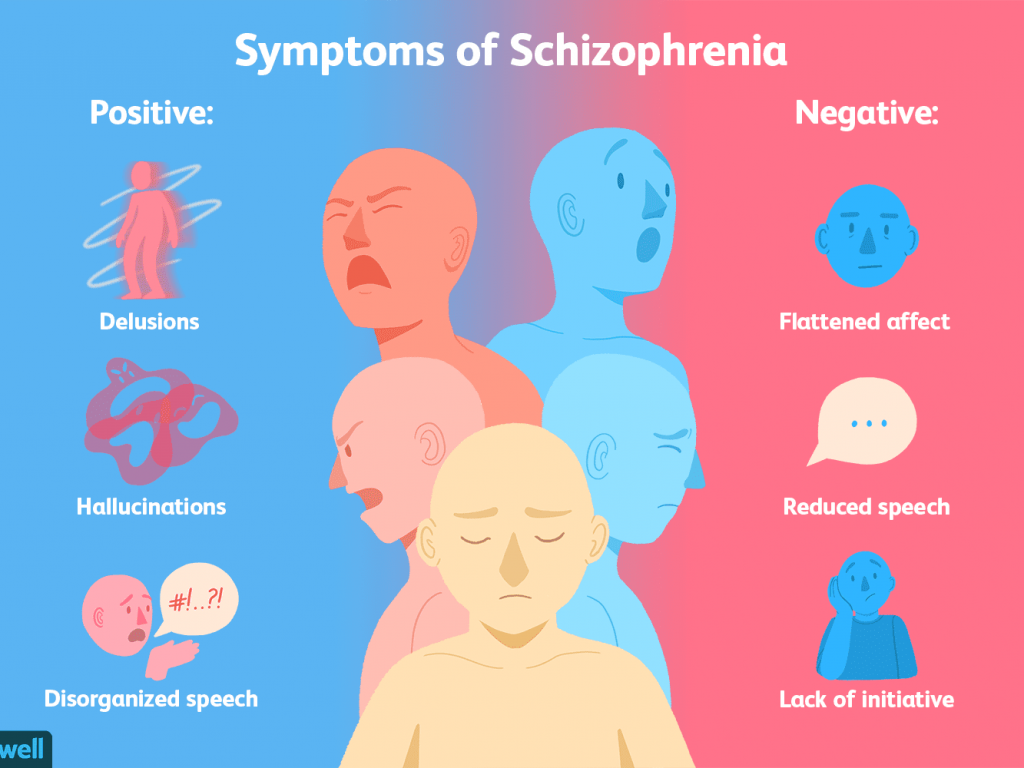
The clinical picture of the heboid syndrome is determined by gross behavioral disorders that do not correspond to the innate nature of the adolescent, with the appearance of rudeness, hostility, intolerance, a tendency to asocial and antisocial actions, pronounced disinhibition and perversion of primitive drives (sexual emancipation, alcoholism, drug addiction, etc.), loss or weakening of the highest moral principles (loss of taboos, social distance, perversion of understanding the boundaries of good and evil).
Heboid syndrome occurs primarily in the initial or manifest periods of schizophrenia and schizophrenia spectrum disorders, as a result of which it requires mandatory observation and treatment by a psychiatrist.
Anorexia nervosa and bulimia nervosa
are considered within the boundaries of eating disorders. In this case, despite this, the axial symptom is the phenomenon of dysmorphophobia - a pathological belief in one's own ugliness, a steady dissatisfaction with one's own appearance with a loss of criticism of an objective assessment.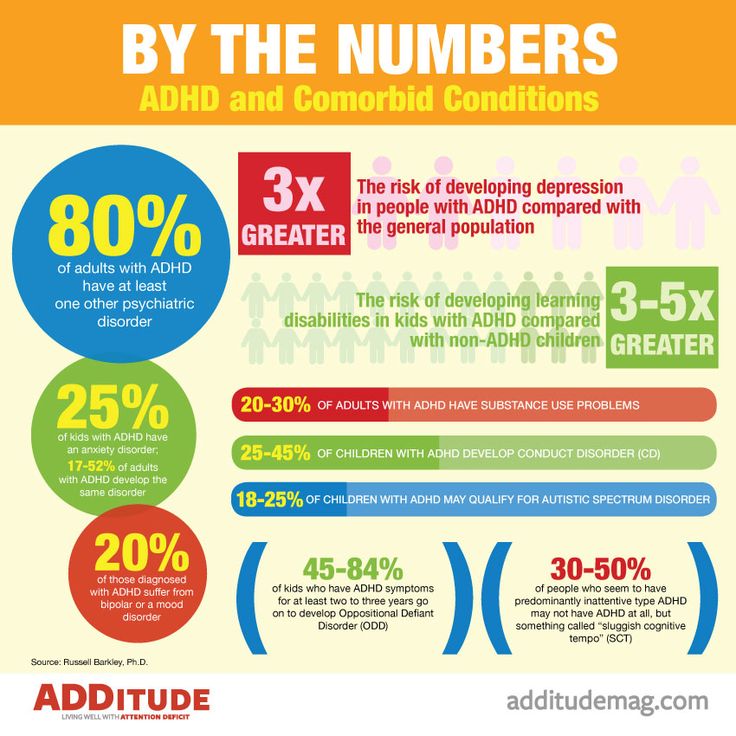
Anorexia nervosa is characterized by an overvalued desire for thinness, a painful stras of obesity, with inadequate food restriction in relation to the established norm. Patients are obsessed with weight issues, ignoring the painful consequences of diets (amenorrhea, alopecia, etc.), parents' beliefs and doctors' recommendations.
Bulimia nervosa often appears in the form of anorexia dynamics at the stage of the formation of an overpowering hunger. As an independent disorder, NB is determined by successive episodes of compulsive overeating followed by gastrointestinal cleansing procedures (provoked vomiting, abuse of laxatives and diuretics). Patients systematically absorb excessive amounts of high-calorie food, cannot stop, eat up until the onset of pain. Compulsive overeating is replaced by obsessive fears of weight gain, a pathological sense of guilt with ideas of self-flagellation and self-abasement.
Eating disorders are non-specific syndromic formations, and therefore can be included in the structure of a whole spectrum of mental illnesses - personality disorders, depression, schizophrenia spectrum disorders.