Fatigue from grief
SAMHSA’s National Helpline | SAMHSA
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.
Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders.
This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative. Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs. In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems. Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.
Addresses concerns of children of parents with substance use/abuse problems.It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt. Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse. Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.
For additional resources, please visit the SAMHSA Store.
Last Updated: 08/30/2022
SAMHSA Behavioral Health Treatment Services Locator
HomeWelcome to the Behavioral Health Treatment Services Locator, a confidential and anonymous source of information for persons seeking treatment facilities in the United States or U.S. Territories for substance use/addiction and/or mental health problems.
PLEASE NOTE: Your personal information and the search criteria you enter into the Locator is secure and anonymous. SAMHSA does not collect or maintain any information you provide.
Please enter a valid location.
please type your address
-
FindTreatment.
 gov
gov Millions of Americans have a substance use disorder. Find a treatment facility near you.
-
988 Suicide & Crisis Lifeline
Call or text 988
Free and confidential support for people in distress, 24/7.
-
National Helpline
1-800-662-HELP (4357)
Treatment referral and information, 24/7.

-
Disaster Distress Helpline
1-800-985-5990
Immediate crisis counseling related to disasters, 24/7.
- Overview
- Locator OverviewLocator Overview
- Locator OverviewLocator Overview
- Finding Treatment
- Find Facilities for VeteransFind Facilities for Veterans
- Find Facilities for VeteransFind Facilities for Veterans
- Facility Directors
- Register a New FacilityRegister a New Facility
- Register a New FacilityRegister a New Facility
- Other Locator Functionalities
- Download Search ResultsDownload Search Results
- Use Google MapsUse Google Maps
- Print Search ResultsPrint Search Results
- Use Google MapsUse Google Maps
- Icon from Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers).
 Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers).
Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers). - Icon from Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers). Find programs providing methadone for the treatment of opioid addiction (heroin or pain relievers).
The Locator is authorized by the 21st Century Cures Act (Public Law 114-255, Section 9006; 42 U.S.C. 290bb-36d). SAMHSA endeavors to keep the Locator current. All information in the Locator is updated annually from facility responses to SAMHSA’s National Substance Use and Mental Health Services Survey (N-SUMHSS). New facilities that have completed an abbreviated survey and met all the qualifications are added monthly. Updates to facility names, addresses, telephone numbers, and services are made weekly for facilities informing SAMHSA of changes. Facilities may request additions or changes to their information by sending an e-mail to [email protected], by calling the BHSIS Project Office at 1-833-888-1553 (Mon-Fri 8-6 ET), or by electronic form submission using the Locator online application form (intended for additions of new facilities).
Updates to facility names, addresses, telephone numbers, and services are made weekly for facilities informing SAMHSA of changes. Facilities may request additions or changes to their information by sending an e-mail to [email protected], by calling the BHSIS Project Office at 1-833-888-1553 (Mon-Fri 8-6 ET), or by electronic form submission using the Locator online application form (intended for additions of new facilities).
Psychological fatigue during the war: what to do
Well-known Ukrainian psychologist Natalia Kholodenko shared proven tips to help cope with psychological fatigue and restore mental balance.
Every news in Ukraine causes psychological fatigue. Fear for today and a lack of understanding of the future drive us into those corners of thought that we have not been to before. I confess: I have already thought more than once that the deceased is a person freed from physical suffering, grief, panic. However, this is a momentary weakness. Next, you need to find a target! It's impossible to keep up without it.
The main purpose of my existence today is to protect children and then to help anyone I can be of service to. If you're broken, you can't do it. And that's how you start to cling to life.
1. Create your own virtual reality. Add with your thoughts to your life everything that you lack the most right now. Lie in the arms of a loved one who is not around, give yourself a fancy bubble bath or whatever. Try to feel pleasure, not pain. Thus, we form a version of another life: everything that exists virtually becomes reality more easily.
2. Remember good things from the past. Take a walk in your favorite park, look at photos from holidays and travels. This is your foundation. If it was good once, then it can be good again.
3. Draw your fortune. As you like and with what you can (pencil, pen, stick in the sand). Draw for as long as you feel relief.
4. Seize the moment! Watch the branch by the window as if you were making a movie about it. Let time freeze for a minute or five minutes. It is very important to hang on one object in one unit of time and see how it lives now.
It is very important to hang on one object in one unit of time and see how it lives now.
Tags: ukraine2022, psychologist's blog, war in Ukraine
Advertising
Popular materials
Lose weight in 7 days: effective and simple workout
National heritage: 5 forgotten dishes of Ukrainian cuisine
Women's Health Annual Checkup Essential List
Featured Materials
People / News
Ukrainians have become more likely to communicate in Ukrainian since the beginning of the full-scale invasion
Relations / Psychology
Emotional numbness: what to do if you feel inner emptiness
Lifestyle / Blog lifestyle
5 modern books about Ukraine that you need to read
People / News
Reload.
 today: chronicle of Ukraine's reboot
today: chronicle of Ukraine's reboot People / News
How Russian invaders turned a Ukrainian village into a concentration camp for residents
People / News
In Ukraine, you can use free services in the treatment of breast cancer
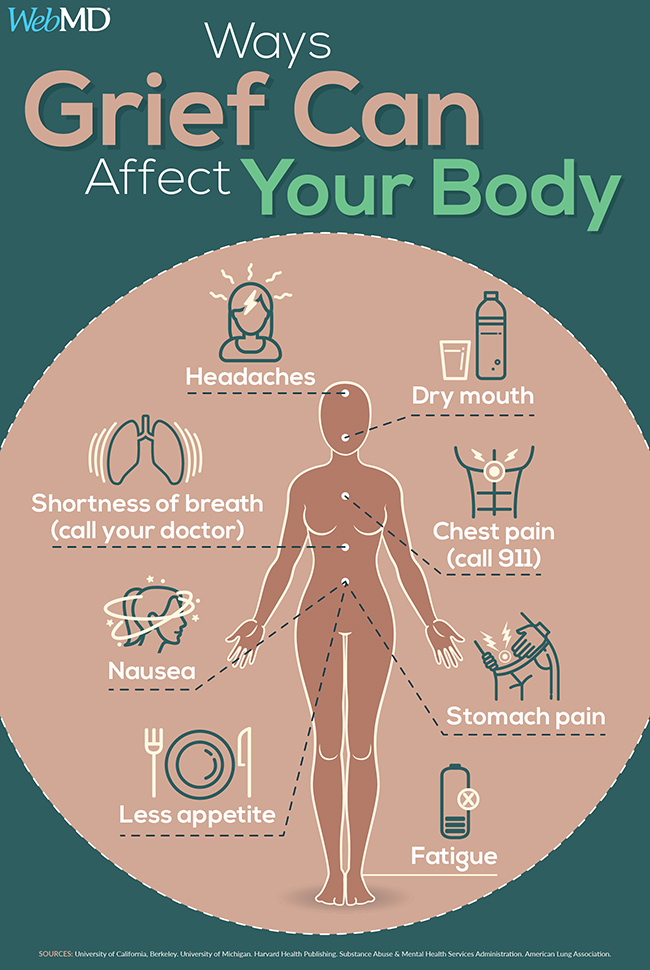
How grief affects our physical condition
By the time of the tragedy, Megan Devine had been working as a psychotherapist for five years. She helped patients cope with the consequences of violence and other traumas, overcome drug addiction, and become emotionally stable.
And then disaster struck: on a summer day, right before Megan's eyes, her loved one, a young, healthy man, drowned. The world has collapsed. All her knowledge and professional experience were inapplicable to such a loss. Recovery took many years. Meghan discovered a community of grieving people that became her support group. Megan then began working with grief as a psychotherapist, and then wrote the book Let's Talk About Loss (Olymp-Business, 2020).
A large section of it is devoted to the story of the physical and mental changes that occur in the process of mourning.
“A person has ceased to be himself and has not yet become someone new,” writes Megan Devine. “All our previous state, both physical and emotional, is losing stability.”
Loss provokes changes in the biochemistry of the brain and affects almost all bodily functions - appetite, digestion, blood pressure, heart rate, breathing, muscle tension and sleep. In addition to physical reactions, cognitive impairment, memory loss, disorientation, and decreased concentration often occur during the early period of grief. Megan talks about these symptoms.
Fatigue and insomnia
Sleep disturbances are often a serious problem: you either don't sleep at all, or your waking up is reduced to small windows between long periods of sleep. When you do sleep, grief seeps into your sleep, no matter how exhausted you may be. Some people continue to regularly wake up the very minute their loved one has died. Others are awakened by the fact that they are trying to grope him in bed, and the place is empty.
Others are awakened by the fact that they are trying to grope him in bed, and the place is empty.
If you have trouble sleeping, you are not alone. Sleep as much as you can, when you can, don't see it as avoidance or denial. In fact, it is recovery and rest. If you can't sleep or wake up from dreams, don't fight it. Rest as and when you can. Discuss ways to get better sleep with doctors you trust.
Dreams and nightmares
Nightmares about your loss may make you want to avoid sleep. Recurring dreams, such as those where you are told news of death, are a healthy, necessary part of grief. Such dreams do not present you with solutions to problems or signs of the future - they mean that your creative, associative mind is trying to navigate the space of loss. This knowledge doesn't make nightmares any more pleasant.
Every system in your body is working hard to help you survive, and nightmares are often part of that process. Note it, but don't dive into it, don't get bogged down in analysis. If you wake up from a nightmare, repeating a simple phrase, such as "My mind is trying to fit it in," can sometimes help calm your mind and nervous system.
If you wake up from a nightmare, repeating a simple phrase, such as "My mind is trying to fit it in," can sometimes help calm your mind and nervous system.
Physical pain
Heart palpitations, headaches, abdominal pain, dizziness, nausea—these symptoms often appear in a person experiencing a difficult event. After the death of Matt (Meghan's husband. - Approx. ed.), I seemed to have inherited his heartburn, sciatica and neck pain. Nothing like that bothered me while he was alive.
Looking through my early grief diaries now, I am amazed at the feeling of fatigue that is described there, and the amount of physical pain: aching muscles, headache, phantom pains in all parts of the body. In the first two years, I ended up in the emergency room at least four times: with severe pain in my stomach and chest, changes in vision, and each time the tests showed nothing.
I think in many ways the body is the vessel that holds all this experience. His breakdowns, failures and other signs of excessive stress become clear when you think about how much he has to endure.