Effects of add
Adult attention-deficit/hyperactivity disorder (ADHD) - Symptoms and causes
Overview
Adult attention-deficit/hyperactivity disorder (ADHD) is a mental health disorder that includes a combination of persistent problems, such as difficulty paying attention, hyperactivity and impulsive behavior. Adult ADHD can lead to unstable relationships, poor work or school performance, low self-esteem, and other problems.
Though it's called adult ADHD, symptoms start in early childhood and continue into adulthood. In some cases, ADHD is not recognized or diagnosed until the person is an adult. Adult
ADHD symptoms may not be as clear as ADHD symptoms in children. In adults, hyperactivity may decrease, but struggles with impulsiveness, restlessness and difficulty paying attention may continue.
Treatment for adult ADHD is similar to treatment for childhood ADHD. Adult ADHD treatment includes medications, psychological counseling (psychotherapy) and treatment for any mental health conditions that occur along with ADHD.
Products & Services
- Book: Mayo Clinic Family Health Book, 5th Edition
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Symptoms
Some people with ADHD have fewer symptoms as they age, but some adults continue to have major symptoms that interfere with daily functioning. In adults, the main features of ADHD may include difficulty paying attention, impulsiveness and restlessness. Symptoms can range from mild to severe.
Symptoms can range from mild to severe.
Many adults with ADHD aren't aware they have it — they just know that everyday tasks can be a challenge. Adults with ADHD may find it difficult to focus and prioritize, leading to missed deadlines and forgotten meetings or social plans. The inability to control impulses can range from impatience waiting in line or driving in traffic to mood swings and outbursts of anger.
Adult ADHD symptoms may include:
- Impulsiveness
- Disorganization and problems prioritizing
- Poor time management skills
- Problems focusing on a task
- Trouble multitasking
- Excessive activity or restlessness
- Poor planning
- Low frustration tolerance
- Frequent mood swings
- Problems following through and completing tasks
- Hot temper
- Trouble coping with stress
What's typical behavior and what's ADHD?
Almost everyone has some symptoms similar to ADHD at some point in their lives. If your difficulties are recent or occurred only occasionally in the past, you probably don't have ADHD. ADHD is diagnosed only when symptoms are severe enough to cause ongoing problems in more than one area of your life. These persistent and disruptive symptoms can be traced back to early childhood.
If your difficulties are recent or occurred only occasionally in the past, you probably don't have ADHD. ADHD is diagnosed only when symptoms are severe enough to cause ongoing problems in more than one area of your life. These persistent and disruptive symptoms can be traced back to early childhood.
Diagnosis of ADHD in adults can be difficult because certain ADHD symptoms are similar to those caused by other conditions, such as anxiety or mood disorders. And many adults with ADHD also have at least one other mental health condition, such as depression or anxiety.
When to see a doctor
If any of the symptoms listed above continually disrupt your life, talk to your doctor about whether you might have ADHD.
Different types of health care professionals may diagnose and supervise treatment for ADHD. Seek a provider who has training and experience in caring for adults with ADHD.
Request an Appointment at Mayo Clinic
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health.
To provide you with the most relevant and helpful information, and understand which
information is beneficial, we may combine your email and website usage information with
other information we have about you. If you are a Mayo Clinic patient, this could
include protected health information. If we combine this information with your protected
health information, we will treat all of that information as protected health
information and will only use or disclose that information as set forth in our notice of
privacy practices. You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
Causes
While the exact cause of ADHD is not clear, research efforts continue. Factors that may be involved in the development of ADHD include:
- Genetics. ADHD can run in families, and studies indicate that genes may play a role.
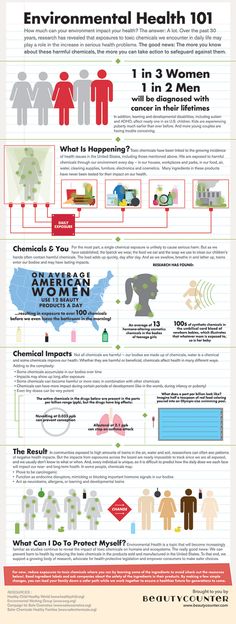
- Environment. Certain environmental factors also may increase risk, such as lead exposure as a child.
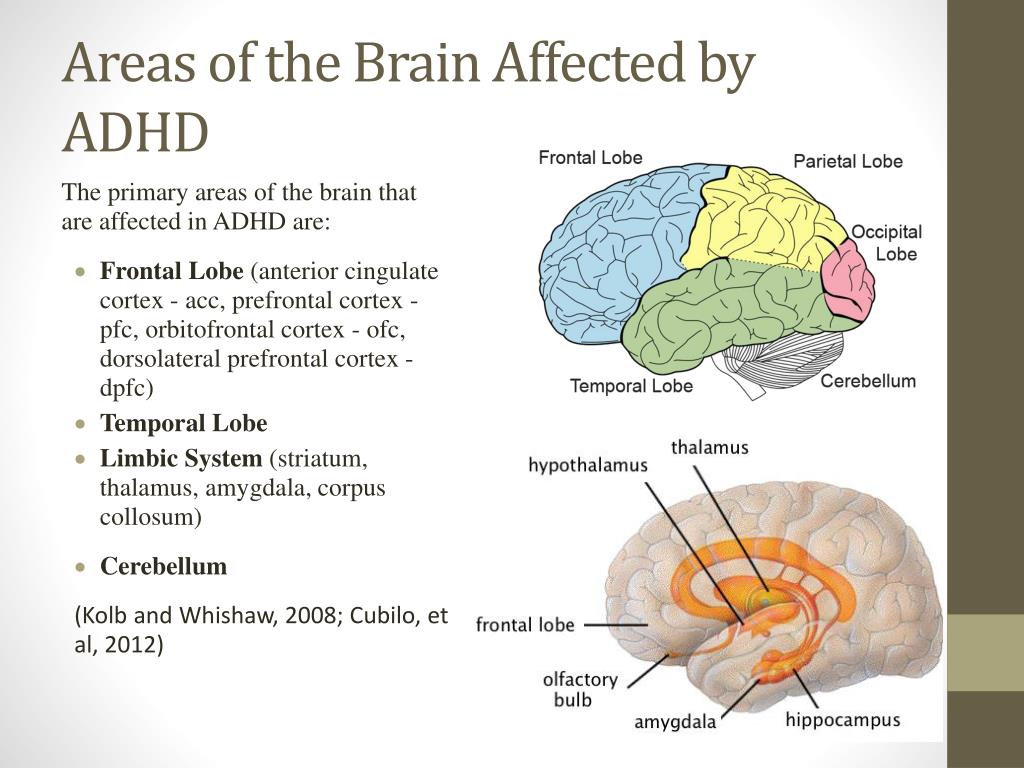
- Problems during development. Problems with the central nervous system at key moments in development may play a role.
Risk factors
Risk of ADHD may increase if:
- You have blood relatives, such as a parent or sibling, with ADHD or another mental health disorder
- Your mother smoked, drank alcohol or used drugs during pregnancy
- As a child, you were exposed to environmental toxins — such as lead, found mainly in paint and pipes in older buildings
- You were born prematurely
Complications
ADHD can make life difficult for you. ADHD has been linked to:
ADHD has been linked to:
- Poor school or work performance
- Unemployment
- Financial problems
- Trouble with the law
- Alcohol or other substance misuse
- Frequent car accidents or other accidents
- Unstable relationships
- Poor physical and mental health
- Poor self-image
- Suicide attempts
Coexisting conditions
Although ADHD doesn't cause other psychological or developmental problems, other disorders often occur along with ADHD and make treatment more challenging. These include:
- Mood disorders. Many adults with ADHD also have depression, bipolar disorder or another mood disorder. While mood problems aren't necessarily due directly to ADHD, a repeated pattern of failures and frustrations due to ADHD can worsen depression.
- Anxiety disorders. Anxiety disorders occur fairly often in adults with ADHD. Anxiety disorders may cause overwhelming worry, nervousness and other symptoms. Anxiety can be made worse by the challenges and setbacks caused by ADHD.
- Other psychiatric disorders. Adults with ADHD are at increased risk of other psychiatric disorders, such as personality disorders, intermittent explosive disorder and substance use disorders.
- Learning disabilities. Adults with ADHD may score lower on academic testing than would be expected for their age, intelligence and education. Learning disabilities can include problems with understanding and communicating.
By Mayo Clinic Staff
Related
Associated Procedures
Products & Services
The effect of ADHD on the life of an individual, their family, and community from preschool to adult life
Article Text
Article menu
- Article
Text - Article
info - Citation
Tools - Share
- Rapid Responses
- Article
metrics - Alerts
Original articles
The effect of ADHD on the life of an individual, their family, and community from preschool to adult life
- V A Harpin
- Correspondence to:
Dr V A Harpin
Ryegate Children’s Centre, Sheffield Children’s NHS Trust, Tapton Crescent Road, Sheffield S10 5DD, UK; Val. Harpinsheffch-tr.trent.nhs.uk
Harpinsheffch-tr.trent.nhs.uk
Abstract
Attention deficit/hyperactivity disorder (ADHD) may affect all aspects of a child’s life. Indeed, it impacts not only on the child, but also on parents and siblings, causing disturbances to family and marital functioning. The adverse effects of ADHD upon children and their families changes from the preschool years to primary school and adolescence, with varying aspects of the disorder being more prominent at different stages. ADHD may persist into adulthood causing disruptions to both professional and personal life. In addition, ADHD has been associated with increased healthcare costs for patients and their family members.
- CHQ, Child Health Questionnaire
- ODD, oppositional defiant disorder
http://dx.doi.org/10.1136/adc.2004.059006
Statistics from Altmetric.com
Request Permissions
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
You will be able to get a quick price and instant permission to reuse the content in many different ways.
- CHQ, Child Health Questionnaire
- ODD, oppositional defiant disorder
Attention deficit/hyperactivity disorder (ADHD) is a chronic, debilitating disorder which may impact upon many aspects of an individual’s life, including academic difficulties,1 social skills problems,2 and strained parent-child relationships.3 Whereas it was previously thought that children eventually outgrow ADHD, recent studies suggest that 30–60% of affected individuals continue to show significant symptoms of the disorder into adulthood.4 Children with the disorder are at greater risk for longer term negative outcomes, such as lower educational and employment attainment.5 A vital consideration in the effective treatment of ADHD is how the disorder affects the daily lives of children, young people, and their families. Indeed, it is not sufficient to merely consider ADHD symptoms during school hours—a thorough examination of the disorder should take into account the functioning and wellbeing of the entire family.
As children with ADHD get older, the way the disorder impacts upon them and their families changes (fig 1⇓). The core difficulties in executive function seen in ADHD7 result in a different picture in later life, depending upon the demands made on the individual by their environment. This varies with family and school resources, as well as with age, cognitive ability, and insight of the child or young person. An environment that is sensitive to the needs of an individual with ADHD and aware of the implications of the disorder is vital. Optimal medical and behavioural management is aimed at supporting the individual with ADHD and allowing them to achieve their full potential while minimising adverse effects on themselves and society as a whole.
Figure 1
Stages of ADHD. Adapted from Kewley G (1999).6
The aim of this paper is to follow the natural history of this complex disorder through preschool years, school life, and adulthood and to consider its effect on the family, the community, and society as a whole. In addition, comorbidities and healthcare costs are examined.
In addition, comorbidities and healthcare costs are examined.
THE PRESCHOOL CHILD
Poor concentration, high levels of activity, and impulsiveness are frequent characteristics of normal preschool children. Consequently, a high level of supervision is the norm. Even so, children with ADHD may still stand out. In this age group there is often unusually poor intensity of play and excessive motor restlessness.8,9 Associated difficulties, such as delayed development, oppositional behaviour, and poor social skills, may also be present. If ADHD is a possibility, it is vital to offer targeted parenting advice and support. Even at this early stage parental stress may be huge when a child does not respond to ordinary parental requests and behavioural advice.9 Targeted work with preschool children and their carers has been shown to be effective in improving parent child interaction and reducing parental stress.10,11 A useful review of the available evidence and methods is provided by Barkley. 12
12
PRIMARY SCHOOL YEARS
The primary school child with ADHD frequently begins to be seen as being different as classmates start to develop the skills and maturity that enable them to learn successfully in school. Although a sensitive teacher may be able to adapt the classroom to allow an able child with ADHD to succeed, more frequently the child experiences academic failure, rejection by peers, and low self esteem (fig 2⇓). Comorbid problems, such as specific learning difficulties, may also start to impact on the child, further complicating diagnosis and management. Assessment by an educational psychologist may help to unravel learning strengths and difficulties, and advise on necessary support in the classroom.
Figure 2
Emotional and family functioning in children with ADHD compared with controls.13 *Higher scores indicative of greater functioning. CHQ, Child Health Questionnaire.13
Frequently, difficulties at home or on outings with carers (for example, when shopping, out in the park, or visiting other family members) also become more apparent at this age. Parents may find that family members refuse to care for the child, and that other children do not invite them to parties or out to play. Many children with ADHD have very poor sleep patterns, and although they appear not to need much sleep, daytime behaviour is often worse when sleep is badly affected. As a result, parents have little time to themselves; whenever the child is awake they have to be watching them. Not surprisingly, family relationships may be severely strained, and in some cases break down, bringing additional social and financial difficulties.14 This may cause children to feel sad or even show oppositional or aggressive behaviour.
Parents may find that family members refuse to care for the child, and that other children do not invite them to parties or out to play. Many children with ADHD have very poor sleep patterns, and although they appear not to need much sleep, daytime behaviour is often worse when sleep is badly affected. As a result, parents have little time to themselves; whenever the child is awake they have to be watching them. Not surprisingly, family relationships may be severely strained, and in some cases break down, bringing additional social and financial difficulties.14 This may cause children to feel sad or even show oppositional or aggressive behaviour.
Assessing the quality of life of the child suffering from ADHD is difficult. Behavioural assessments are usually carried out by parents, teachers, or healthcare professionals, and it can usually only be inferred how the child must feel. However, data from self evaluations indicate that children with ADHD view their most problematic behaviour as less within their control and more prevalent than children without ADHD. 15 Participation in a school based, nurse led support group was associated with an increase in self worth in pre-adolescents with ADHD.16
15 Participation in a school based, nurse led support group was associated with an increase in self worth in pre-adolescents with ADHD.16
Johnston and Mash reviewed the evidence of the effect of having a child with ADHD on family functioning.14 They concluded that the presence of a child with ADHD results in increased likelihood of disturbances to family and marital functioning, disrupted parent-child relationships, reduced parenting efficacy, and increased levels of parent stress, particularly when ADHD is comorbid with conduct problems.
In a survey of the mothers and fathers of 66 children, parents of children with ADHD combined and inattentive subtypes expressed more role dissatisfaction than parents of control children.17 Furthermore, ADHD in children was reported to predict depression in mothers.18 Pelham et al reported that the deviant child behaviours that represent major chronic interpersonal stressors for parents of ADHD children are associated with increased parental alcohol consumption.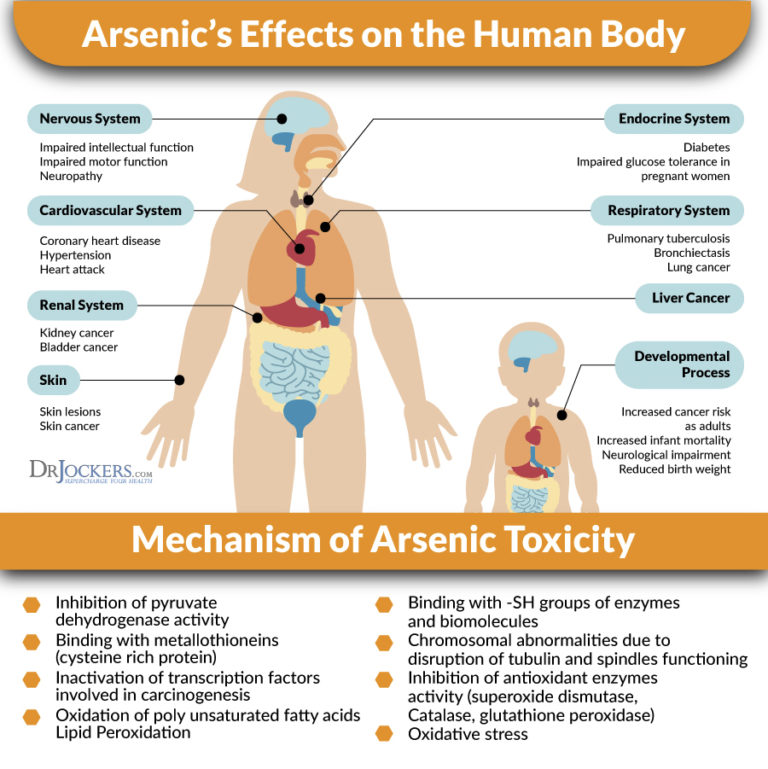 19
19
Limited attention has been given to sibling relationships in families with ADHD children. While it has been reported that siblings of children with ADHD are at increased risk for conduct and emotional disorders,20 a more recent study presenting sibling accounts of ADHD identified disruption caused by symptoms and behavioural manifestations of ADHD as the most significant problem.21 This disruption was experienced by siblings in three primary ways: victimisation, caretaking, and sorrow and loss. Siblings reported feeling victimised by aggressive acts from their ADHD brothers through overt acts of physical violence, verbal aggression, and manipulation and control. In addition, siblings reported that parents expected them to care for and protect their ADHD brothers because of the social and emotional immaturity associated with ADHD. Furthermore, as a result of the ADHD symptoms and consequent disruption, many siblings described feeling anxious, worried, and sad.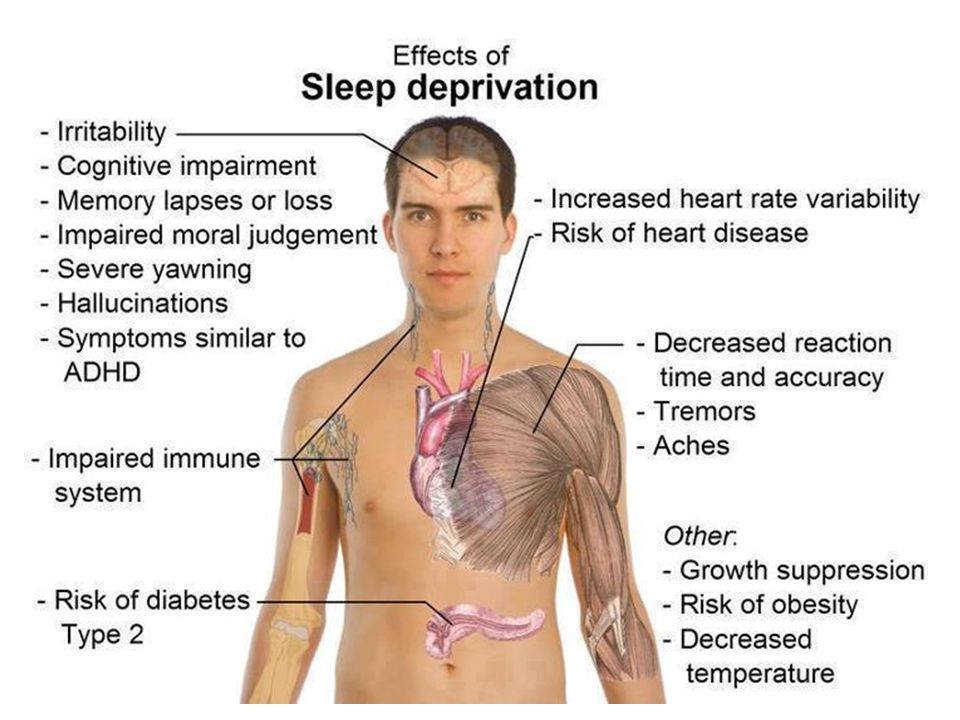 21
21
Broader social and family functioning has been assessed using the Child Health Questionnaire (CHQ), a parent rated health outcome scale that measures physical and psychosocial wellbeing.22–,24 The studies demonstrated that treatment of ADHD with atomoxetine, a new non-stimulant medication for ADHD, resulted in improved perception of quality of life, with improvements being apparent in social and family functioning, and self esteem. Further research assessing the ongoing quality of life for the child and their family following multimodal input is urgently needed.
ADHD IN YOUNG PEOPLE
Adolescence may bring about a reduction in the overactivity that is often so striking in younger children, but inattention, impulsiveness, and inner restlessness remain major difficulties. A distorted sense of self and a disruption of the normal development of self has been reported by adolescents with ADHD.25 Furthermore, excessively aggressive and antisocial behaviour may develop, adding further problems (fig 3⇓). A study by Edwards et al27 examined teenagers with ADHD and oppositional defiant disorder (ODD), which is defined by the presence of markedly defiant, disobedient, provocative behaviour and by the absence of more severe dissocial or aggressive acts that violate the law or the rights of others. These teenagers rated themselves as having more parent-teen conflict than did community controls. Increased parent-teen conflict was also reported when parents of teenagers with ADHD carried out the rating exercise. In addition, a survey of 11–15 year olds showed that those with hyperkinesis were twice as likely as the overall population to have “a severe lack of friendship”.28
A study by Edwards et al27 examined teenagers with ADHD and oppositional defiant disorder (ODD), which is defined by the presence of markedly defiant, disobedient, provocative behaviour and by the absence of more severe dissocial or aggressive acts that violate the law or the rights of others. These teenagers rated themselves as having more parent-teen conflict than did community controls. Increased parent-teen conflict was also reported when parents of teenagers with ADHD carried out the rating exercise. In addition, a survey of 11–15 year olds showed that those with hyperkinesis were twice as likely as the overall population to have “a severe lack of friendship”.28
Figure 3
Antisocial behaviour in adolescents with ADHD.26 Data primarily represents outcomes in those with conduct disorder as teenagers.
Young people with ADHD are at increased risk of academic failure, dropping out of school or college, teenage pregnancy, and criminal behaviour (fig 4A⇓ and B). Driving poses an additional risk. Individuals with ADHD are easily distracted from concentrating on driving when going slowly, but while driving fast may also be dangerous. It has been shown that, compared with age matched controls, drivers with ADHD are at increased risk of traffic violations, especially speeding, and are considered to be at fault in more traffic accidents, including fatal ones (fig 5⇓).30 The risk of such events was increased further by the presence of concomitant ODD.29 However, it has been suggested that treatment may have a positive effect on driving skills.31
Driving poses an additional risk. Individuals with ADHD are easily distracted from concentrating on driving when going slowly, but while driving fast may also be dangerous. It has been shown that, compared with age matched controls, drivers with ADHD are at increased risk of traffic violations, especially speeding, and are considered to be at fault in more traffic accidents, including fatal ones (fig 5⇓).30 The risk of such events was increased further by the presence of concomitant ODD.29 However, it has been suggested that treatment may have a positive effect on driving skills.31
Figure 4
Impact of ADHD in adolescence. Data from Barkley RA;26 (A) Impact at school; (B) impact on health, social, and psychiatric wellbeing.
Figure 5
Driving-related offences in young adults with ADHD and controls. NS, not significant. Data from Barkley RA et al. 29
29
ADULT LIFE
As many as 60% of individuals with ADHD symptoms in childhood continue to have difficulties in adult life.32,33 Adults with ADHD are more likely to be dismissed from employment and have often tried a number of jobs before being able to find one at which they can succeed.5 They may need to choose specific types of work and are frequently self employed. In the workplace, adults with ADHD experience more interpersonal difficulties with employers and colleagues. Further problems are caused by lateness, absenteeism, excessive errors, and an inability to accomplish expected workloads. At home, relationship difficulties and break-ups are more common. The risk of drug and substance abuse is significantly increased in adults with persisting ADHD symptoms who have not been receiving medication.34 The genetic aspects of ADHD mean that adults with ADHD are more likely to have children with ADHD. This in turn causes further problems, especially as the success of parenting programmes for parents of children with ADHD is highly influenced by the presence of parental ADHD. 35 Thus, ADHD in parents and children can lead to a cycle of difficulties.
35 Thus, ADHD in parents and children can lead to a cycle of difficulties.
COMORBIDITIES
Comorbid disorders may impact on individuals with ADHD throughout their lives. It is estimated that at least 65% of children with ADHD have one or more comorbid conditions.36 The reported incidence of some of the most frequent comorbidities is shown in figure 6⇓, with neurodevelopmental problems, such as dyslexia and developmental coordination disorder, being particularly common. Many children with ADHD also suffer from tic disorders (not related to stimulant medication). In addition, around 60% of children with Tourette’s Syndrome fulfil criteria for ADHD,38,39 and autistic spectrum disorder is increasingly recognised with comorbid ADHD.39 Initially, excessive hyperactivity may mask the features of autistic spectrum disorder until the child receives medication. Conduct disorder and ODD coexist with ADHD in at least 30%, and in some reports up to 90%, of cases. 36 These most frequently occurring comorbidities can, however, be considered more as complications of ADHD, with adversity in their psychological environment possibly determining whether children at risk make the transition to antisocial conduct.40
36 These most frequently occurring comorbidities can, however, be considered more as complications of ADHD, with adversity in their psychological environment possibly determining whether children at risk make the transition to antisocial conduct.40
Figure 6
ADHD and comorbidity in Swedish school age children.37 MR, mental retardation; RWD, reading/writing disorder; DC, developmental coordination; ODD, oppositional defiant disorder.
PROBLEMS ASSOCIATED WITH TREATMENT
Growth deficits in children receiving stimulant treatment for ADHD have long been the subject of scientific discussion. Conflicting results have been reported with some authors indicating that stimulants do indeed affect growth in children,41–,43 but that this only occurs during active treatment phase and does not compromise final height.44 Other studies, however, have not found any evidence to suggest that stimulants influence growth. 45,46 Taken together, the results suggest that clinicians should monitor the growth of hyperactive children receiving stimulants, and consider dose reduction in individual cases should evidence of growth suppression occur.
45,46 Taken together, the results suggest that clinicians should monitor the growth of hyperactive children receiving stimulants, and consider dose reduction in individual cases should evidence of growth suppression occur.
Another frequently quoted concern about treatment of ADHD with stimulant medications is that it could lead to drug addiction in later life. Young people with ADHD are by nature impulsive risk takers, and there is clear evidence that untreated ADHD—especially with concomitant conduct disorder—is associated with a three- to fourfold increase in the risk of substance misuse.47,48 In contrast, patients medicated with stimulants have a similar risk of substance misuse to controls.49 These data therefore provide strong evidence in favour of careful treatment and support for young people with ADHD.
HEALTHCARE COSTS
Healthcare costs for individuals with ADHD in the UK have not been fully estimated, but evidence from the USA suggests that they are increased compared with age matched controls. A population based, historical cohort study followed 4880 individuals from 1987 to 1995 and compared the nine year median medical cost per person: ADHD medical costs were US$4306, whereas non-ADHD medical costs were US$1944 (p<0.01).50 These findings are likely to reflect increased injury following accidents and a rise in use of substance abuse services and other outpatient facilities, although poor ability to comply with advice on medication (for example, asthma management) may also be implicated. A study of the injuries to children with ADHD established that children with ADHD were more likely to be injured as pedestrians or bicyclists than children not suffering from ADHD. They were more likely to sustain injuries to multiple body regions, head injuries, and to be severely injured.51 ADHD has been found to represent a risk factor for substance abuse,47,52 and an investigation of prevalence of ADHD among substance abusers has established that ADHD was significantly overrepresented among inpatients with psychoactive substance use disorder.
A population based, historical cohort study followed 4880 individuals from 1987 to 1995 and compared the nine year median medical cost per person: ADHD medical costs were US$4306, whereas non-ADHD medical costs were US$1944 (p<0.01).50 These findings are likely to reflect increased injury following accidents and a rise in use of substance abuse services and other outpatient facilities, although poor ability to comply with advice on medication (for example, asthma management) may also be implicated. A study of the injuries to children with ADHD established that children with ADHD were more likely to be injured as pedestrians or bicyclists than children not suffering from ADHD. They were more likely to sustain injuries to multiple body regions, head injuries, and to be severely injured.51 ADHD has been found to represent a risk factor for substance abuse,47,52 and an investigation of prevalence of ADHD among substance abusers has established that ADHD was significantly overrepresented among inpatients with psychoactive substance use disorder. 53 Increased use of health services is also seen in the relatives of individuals with ADHD. A study has shown that direct and indirect medical costs were twice as high as those of family members of a control group.54 The difference in these costs was primarily due to a higher incidence of mental health problems in the family members of ADHD patients, which reflects the increased stresses and demands of living with an adult or child with ADHD. Indeed, ADHD related family stress has been linked to increased risk of parental depression and alcohol related disorders.55–,57
53 Increased use of health services is also seen in the relatives of individuals with ADHD. A study has shown that direct and indirect medical costs were twice as high as those of family members of a control group.54 The difference in these costs was primarily due to a higher incidence of mental health problems in the family members of ADHD patients, which reflects the increased stresses and demands of living with an adult or child with ADHD. Indeed, ADHD related family stress has been linked to increased risk of parental depression and alcohol related disorders.55–,57
It is vital to consider the role of treatment of ADHD in decreasing the individual’s risk of adverse outcomes. A number of studies on the effect of treatment of ADHD on the risk of substance abuse encouragingly demonstrate a fall in risk to that of the normal population.58–,60
CONCLUSION
Mannuzza’s review of the long term prognosis in ADHD concludes that childhood ADHD does not preclude high educational and vocational achievements (for example, Master’s degree or medical qualification). 61 However, ADHD is a disorder that may affect all aspects of a child’s life. Careful assessment is paramount, and if this demonstrates significant impairment as a result of ADHD, there is clear evidence that treatment of ADHD should be instituted.62,63 Current treatment focuses mainly on the short term relief of core symptoms, mainly during the school day. This means that important times of the day, such as early mornings before school and evening to bedtime, are frequently unaffected by current treatment regimes. This can negatively impact on child and family functioning and fail to optimise self esteem and long term mental health development.
61 However, ADHD is a disorder that may affect all aspects of a child’s life. Careful assessment is paramount, and if this demonstrates significant impairment as a result of ADHD, there is clear evidence that treatment of ADHD should be instituted.62,63 Current treatment focuses mainly on the short term relief of core symptoms, mainly during the school day. This means that important times of the day, such as early mornings before school and evening to bedtime, are frequently unaffected by current treatment regimes. This can negatively impact on child and family functioning and fail to optimise self esteem and long term mental health development.
In 2003, the American Academy of Pediatrics recommended that clinicians should work with children and their families to monitor the success (or failure) of treatment, using certain criteria to assess specific areas of difficulty and quality of life as a whole.64 There has been a reluctance in the UK to treat ADHD with medication, fuelled by concerns about possible over-prescription in the USA. In addition, newspaper and media coverage of ADHD is often negative and stigmatising. The evidence of potentially severe difficulties for the child, the family, and, in some cases, for society as a whole, means that coordinated multi-agency effort to support the child and family is essential. Moreover, healthcare professionals have an important role in providing balanced and supportive information about ADHD and meeting the needs of affected individuals and their families.
In addition, newspaper and media coverage of ADHD is often negative and stigmatising. The evidence of potentially severe difficulties for the child, the family, and, in some cases, for society as a whole, means that coordinated multi-agency effort to support the child and family is essential. Moreover, healthcare professionals have an important role in providing balanced and supportive information about ADHD and meeting the needs of affected individuals and their families.
REFERENCES
- ↵
Faraone SV, Biederman J, Monuteaux MC, et al. A psychometric measure of learning disability predicts educational failure four years later in boys with ADHD. J Atten Disord2001;4:220–30.
- ↵
Bagwell CL, Molina BS, Pelham WE, et al. ADHD and problems in peer relations: Predictions from childhood to adolescence. J Am Acad Child Adolesc Psychiatry2001;40:1285–92.
- ↵
Johnston C, Mash EJ.
 Families of children with ADHD: review and recommendations for future research. Clin Child Fam Psychol Rev2001;4:183–207.
Families of children with ADHD: review and recommendations for future research. Clin Child Fam Psychol Rev2001;4:183–207. - ↵
Weiss G, Hechtman L. Hyperactive children grown up: ADHD in children, adolescents and adults. New York: Guildford, 1993.
- ↵
Mannuzza S, Klein RG, Bessler A, et al. Adult outcome of hyperactive boys. Educational achievement, occupational rank and psychiatric status. Arch Gen Psychiatry1993;50:565–76.
- ↵
Kewley GD. Attention deficit hyperactivity disorder: Recognition, reality and resolution. London: David Fulton Publishers, 1999.
- ↵
Barkley RA. Behavioral inhibition, sustained attention, and executive functions: constructing a unifying theory of ADHD. Psychol Bull1997;121:65–94.
- ↵
Alessandri SM. Attention, play, and social behaviour in ADHD preschoolers.
 J Abnorm Child Psychol1992;20:289–302.
J Abnorm Child Psychol1992;20:289–302. - ↵
DuPaul GJ, McGoey KE, Eckert TL, et al. Preschool children with attention-deficit/hyperactivity disorder: impairments in behavioural, social, and school functioning. J Am Acad Child Adolesc Psychiatry2001;40:508–15.
- ↵
Sonuga-Barke EJ, Daley D, Thompson M, et al. Parent-based therapies for preschool attention-deficit/hyperactivity disorder: a randomised, controlled trial with a community sample. J Am Acad Child Adolesc Psychiatry2001;40:402–8.
- ↵
Barton J. PhD Thesis. The effect of modifying maternal expressed emotion on outcome of preschool hyperactivity. University of Glasgow 2002.
- ↵
Barkley R. Psychosocial treatments for attention-deficit/hyperactivity disorder in children. J Clin Psychiatry2002;63:36–43.
- ↵
Landgraf JM, Abetz L, Ware JE.
 The CHQ User’s Manual, 2nd edition. Boston: HealthAct, 1999.
The CHQ User’s Manual, 2nd edition. Boston: HealthAct, 1999. - ↵
Johnston C, Mash EJ. Families of children with attention-deficit/hyperactivity disorder: review and recommendations for future research. Clin Child and Fam Psychol Rev2001;4:183–207.
- ↵
Kaidar I, Wiener J, Tannock R. The attributions of children with attention-deficit/hyperactivity disorder for their problem behaviors. J Atten Disord2003;6:99–109.
- ↵
Frame K, Kelly L, Bayley E. Increasing perceptions of self-worth in preadolescents diagnosed with ADHD. J Nurs Scholarsh3003;35:225–9.
- ↵
Podolski CL, Nigg JT. Parent stress and coping in relation to child ADHD severity and associated child disruptive behaviour problems. J Clin Child Psychol2001;30:503–13.
- ↵
Faraone SV, Biederman J, Chen WJ, et al. Genetic heterogeneity in attention-deficit hyperactivity disorder (ADHD): gender, psychiatric comorbidity, and maternal ADHD.
 J Abnorm Psychol1995;104:334–45.
J Abnorm Psychol1995;104:334–45. - ↵
Pelham WE Jr, Lang AR. Can your children drive you to drink? Stress and parenting in adults interacting with children with ADHD. Alcohol Res Health2999;23:292–8.
- ↵
Szatmari P, Offord DR, Boyle MH. Ontario Child Health Study: prevalence of attention deficit disorder with hyperactivity. J Child Psychol Psychiatry1989;30:219–30.
- ↵
Kendall J, Siblings accounts of attention deficit hyperactivity disorder. Family Proc1999;38:117–36.
- ↵
Michelson D, Faries D, Wernicke J, et al. Atomoxetine in the treatment of children and adolescents with attention-deficity/hyperactivity disorder: a randomised, placebo-controlled, dose response study. Pediatrics2001;108:1–9.
Barton J, Prasad S, Buitelaar JK, et al. 10-week, open-label, acute treatment with atomoxetine in non-North American children with ADHD.
 Poster presented at the Royal College of Psychiatrists Annual General Meeting. Edinburgh, UK, 30 June–3 July 2003.
Poster presented at the Royal College of Psychiatrists Annual General Meeting. Edinburgh, UK, 30 June–3 July 2003.- ↵
Harpin V. Changes in quality of life in patients with attention-deficit-hyperactivity disorder after atomoxetine treatment. Paper presented at the meeting of the European Academy of Childhood Disability (EACD). Norway: Oslo, 2–4 October, 2003.
- ↵
Krueger M, Kendall J. Descriptions of self: an exploratory study of adolescents with ADHD. J Child Adolesc Psychiatr Nurs2001;14:61–72.
- ↵
Barkley RA. Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment, 2nd edition. New York: Guildford Press, 1998.
- ↵
Edwards G, Barkley RA, Laneri M, et al. Parent–adolescent conflict in teenagers with ADHD and ODD. J Abnormal Child Psychology2001;29:557–72.
- ↵
Meltzer H, Gatward R, Goodman R, et al.
 The mental health of children and adolescents in Great Britain. Office for National Statistics, London: The Stationery Office, 2000.
The mental health of children and adolescents in Great Britain. Office for National Statistics, London: The Stationery Office, 2000. - ↵
Barkley RA, Guevremont DC, Anastopoulos AD, et al. Driving-related risks and outcomes of attention deficit hyperactivity disorder in adolescents and young adults: A 3 to 5 year follow up survey. Pediatrics1993;92:212–18.
- ↵
Barkley RA, Murphy KR, Kwasnik D. Motor vehicle driving competencies and risks in teens and young adults with attention deficit hyperactivity disorder. Pediatrics1996;98:1089–95.
- ↵
Cox DJ, Merkel RL, Penberthy JK, et al. Impact of methylphenidate delivery profiles on driving performance of adolescents with attention-deficit/hyperactivity disorder: a pilot study. J Am Acad Child Adolesc Psychiatry2004;43:269–75.
- ↵
Weiss G, Hechtman L, Milroy T, et al.
 Psychiatric status of hyperactives as adults: a controlled prospective 15-year follow-up of 63 hyperactive children. J Am Acad Child Psychiatry1985;24:211–20.
Psychiatric status of hyperactives as adults: a controlled prospective 15-year follow-up of 63 hyperactive children. J Am Acad Child Psychiatry1985;24:211–20. - ↵
Weiss M, Hechtman L, Weiss G. ADHD in Adulthood—A guide to current theory, diagnosis and treatment. Baltimore: Johns Hopkins University Press, 1999.
- ↵
Biederman J, Wilens TE, Mick E, et al. Does attention-deficit hyperactivity disorder impact the development course of drug and alcohol abuse and dependence? Biol Psychiatry1998;44:269–73.
- ↵
Sonuga-Barke EJ, Daley D, Thompson M. Does maternal ADHD reduce the effectiveness of parent training for preschool children’s ADHD? J Am Acad Child Adolesc Psychiatry2002;41:696–702.
- ↵
Biederman J, Newcom J, Sprich S. Comorbidity of attention deficit hyperactivity disorder with conduct, depressive, anxiety and other disorders.
 Am J Psychiatry1991;148:564–77.
Am J Psychiatry1991;148:564–77. - ↵
Kadesjo B, Gillberg C. The comorbidity of ADHD in the general population of Swedish school-age children. J Child Psychol Psychiatry2001;42:487–92.
- ↵
Freeman RD, Fast DK, Burd L, et al. An international perspective on Tourette syndrome: selected findings from 3,500 individuals in 22 countries. Dev Med Child Neurol2000;42:436–47.
- ↵
Gillberg C, Gillberg IC, Rasmussen P, et al. Co-existing disorders in ADHD—implications for diagnosis and intervention. Eur Child Adolesc Psychiatry2004;13 (Suppl 1) :I80–92.
- ↵
Taylor E. Clinical foundations of hyperactivity research. Behav Brain Res1998;94:11–24.
- ↵
Mattes JA, Gittelman R. Growth of hyperactive children on maintenance regimen of methylphenidate. Arch Gen Psychiatry1983;40:317–21.
Lisska MC, Rivkees SA. Daily methylphenidate use slows the growth of children: a community based study. J Pediatr Endocrinol Metab2003;16:711–18.
- ↵
Poulton A, Cowell CT. Slowing of growth in height and weight on stimulants: a characteristic pattern. J Paediatr Child Health3003;39:180–5.
- ↵
Klein RG, Mannuzza S. Hyperactive boys almost grown up. III. Methylphenidate effects on ultimate height. Arch Gen Psychiatry1988;45:1131–4.
- ↵
Spencer T, Biederman J, Wilens T. Growth deficits in children with attention deficit hyperactivity disorder. Pediatrics1998;102:501–6.
- ↵
Biederman J, Faraone SV, Monuteaux MC, et al. Growth deficits and attention-deficit/hyperactivity disorder revisited: impact of gender, development, and treatment. Pediatrics2003;111:1010–16.
- ↵
Biederman J, Wilens TE, Mick E, et al.
 Does attention-deficit hyperactivity disorder impact the developmental course of drug and alcohol abuse and dependence? Biol Psychiatry1998;44:269–73.
Does attention-deficit hyperactivity disorder impact the developmental course of drug and alcohol abuse and dependence? Biol Psychiatry1998;44:269–73. - ↵
Wilens TE. Impact of ADHD and its treatment on substance abuse in adults. J Clin Psychiatry2004;65 (Suppl 3) :38–45.
- ↵
Biederman J, Wilens T, Mick E, et al. Pharmacotherapy of attention-deficit/hyperactivity disorder reduces risk for substance use disorder. Pediatrics1999;104:e20.
- ↵
Leibson CL, Katusic SK, Barbaresi WJ, et al. Use and costs of medical care for children and adolescents with and without attention-deficit/hyperactivity disorder. JAMA2001;285:60–6.
- ↵
DiScala C, Lescohier I, Barthel M, et al. Injuries to children with attention deficit hyperactivity disorder. Pediatrics1998;102:1415–21.
- ↵
Sullivan MA, Rudnik-Levin F.
 Attention deficit/hyperactivity disorder and substance abuse. Diagnostic and therapeutic considerations. Ann N Y Acad Sci2001;931:251–70.
Attention deficit/hyperactivity disorder and substance abuse. Diagnostic and therapeutic considerations. Ann N Y Acad Sci2001;931:251–70. - ↵
Schubiner H, Tzelepis A, Milberger S, et al. Prevalence of attention-deficit/hyperactivity disorder and conduct disorder among substance abusers. J Clin Psychiatry2000;61:244–51.
- ↵
Swensen AR, Birnbaum HG, Secnik K, et al. Attention-deficit/hyperactivity disorder: increased costs for patients and their families. J Am Acad Child Adolesc Psychiatry2003;42:1415–23.
- ↵
Cunningham CE, Benness BB, Siegel LS. Family functioning, time allocation, and parental depression in the families of normal and ADHD children. J Clin Child Psychol1988;17:169–77.
Brown RT, Pacini JN. Perceived family functioning, marital status, and depression in parents of boys with attention deficit disorder.
 J Learn Disabil1989;22:581–7.
J Learn Disabil1989;22:581–7.- ↵
Hankin CS. ADHD and its impact on the family. Drug Benefit Trends2001;13 (Suppl C) :15–16.
- ↵
Huss M, Lehmkuhl U. Methylphenidate and substance abuse: a review of pharmacology, animal and clinical studies. J Atten Disord2002;6 (Suppl 1) :S65–71.
Faraone SV, Wilens T. Does stimulant treatment lead to substance use disorders? J Clin Psychiatry2003;64 (Suppl 1) :9–13.
- ↵
Mannuzza S, Klein RG, Moulton JL 3rd. oes stimulant treatment place children at risk for adult substance abuse? A controlled, prospective follow-up study. J Child Adolesc Psychopharmacol2003;13:273–82.
- ↵
Mannuzza S, Klein RG. Long-term prognosis in attention-deficit/hyperactivity disorder. Child Adolesc Psychiatr Clin N Am2000;9:711–26.
- ↵
National Institute for Clinical Excellence (NICE).
 Guidance on the use of methylphenidate (Ritalin, Equasym) for attention deficit/hyperactivity disorder (ADHD) in childhood. Health Technology Assessment No 13. October 2000.
Guidance on the use of methylphenidate (Ritalin, Equasym) for attention deficit/hyperactivity disorder (ADHD) in childhood. Health Technology Assessment No 13. October 2000. - ↵
The MTA Cooperative Group. A 14-month randomised clinical trial of treatment strategies for attention-deficit/hyperactivity disorder. Arch Gen Psychiatry1999;56:1073–86.
- ↵
American Academy of Pediatrics, Reiff MI, Tippins S. ADHD—A Complete and Authoritative Guide. Chicago: Independent Publishers Group, 2003.
Linked Articles
Read the full text or download the PDF:
Subscribe
Log in using your username and password
For personal accounts OR managers of institutional accounts
Username *
Password *
Forgot your log in details?Register a new account?
Forgot your user name or password?
Adding or changing an effect for a pattern
Excel for Microsoft 365 Word for Microsoft 365 Outlook for Microsoft 365 PowerPoint for Microsoft 365 Project Online Desktop Client Excel for Microsoft 365 for Mac Word for Microsoft 365 for Mac PowerPoint for Microsoft 365 for Mac Excel 2021 Word 2021 Outlook 2021 PowerPoint 2021 Microsoft® Project Professional 2021 Microsoft Project Standard 2021 Excel 2021 for Mac Word 2021 for Mac PowerPoint 2021 for Mac Excel 2019Word 2019 Outlook 2019 PowerPoint 2019 Project Professional 2019 Project Standard 2019 Excel 2019 for Mac Word 2019 for Mac PowerPoint 2019 for Mac Excel 2016 Word 2016 Outlook 2016 PowerPoint 2016 Project Professional 2016 Project Standard 2016 Excel 2016 for Mac Word 2016 for Mac PowerPoint 2016 for Mac Excel 2013 Word 2013 Outlook 2013 PowerPoint 2013 Project Professional 2013 Project Standard 2013 Excel 2010 Word 2010 Outlook 2010 PowerPoint 2010 Excel for Mac 2011 Word for Mac 2011 PowerPoint for Mac 2011 More. ..Less
..Less
To make a drawing more attractive, you can add effects such as shadows, glows, reflections, anti-aliasing, embossing, and 3-D rotation.
You can also add an artistic effect or change the brightness, contrast, or sharpness of a picture.
Adding an effect to a pattern
-
Select the pattern for which you want to add or change an effect.
Note: To add the same effect to multiple patterns, click the first pattern, and then press and hold the CTRL key while clicking other patterns. If you're using Word, you'll need to copy the pictures to the canvas if they're not already there. Click the Insert tab, click the Shapes icon and select New Canvas .
 (After adding or changing an effect, you need to move the drawings back to their original place in the document.)
(After adding or changing an effect, you need to move the drawings back to their original place in the document.) -
On the Picture Tools panel , on the Format tab, in the Picture Styles group, click Picture Effects .
-
Hover over one of the Picture Effects options to display a menu of different ways to apply each effect. When you hover over one of the effects in the menu, it appears as a preview picture in the document.
Notes:
-
To adjust the added effect, press the Parameters button at the bottom of each effect menu.
 For example, on menu Shadow , click Shadow Options to make custom settings for the shadow effect.
For example, on menu Shadow , click Shadow Options to make custom settings for the shadow effect. -
If the Picture Tools or Format tab is not visible, double-click the picture to make sure it is selected. If you see the words [Compatibility Mode] next to the file name at the top of the program window, save your document in DOCX or XLSX format (instead of the old DOC or XLS file format) and try again.
-
Deleting an effect from a drawing
For each effect category picture
For example, to remove the shadow, on the pointer to item Effects for picture > Shadow > No shadow .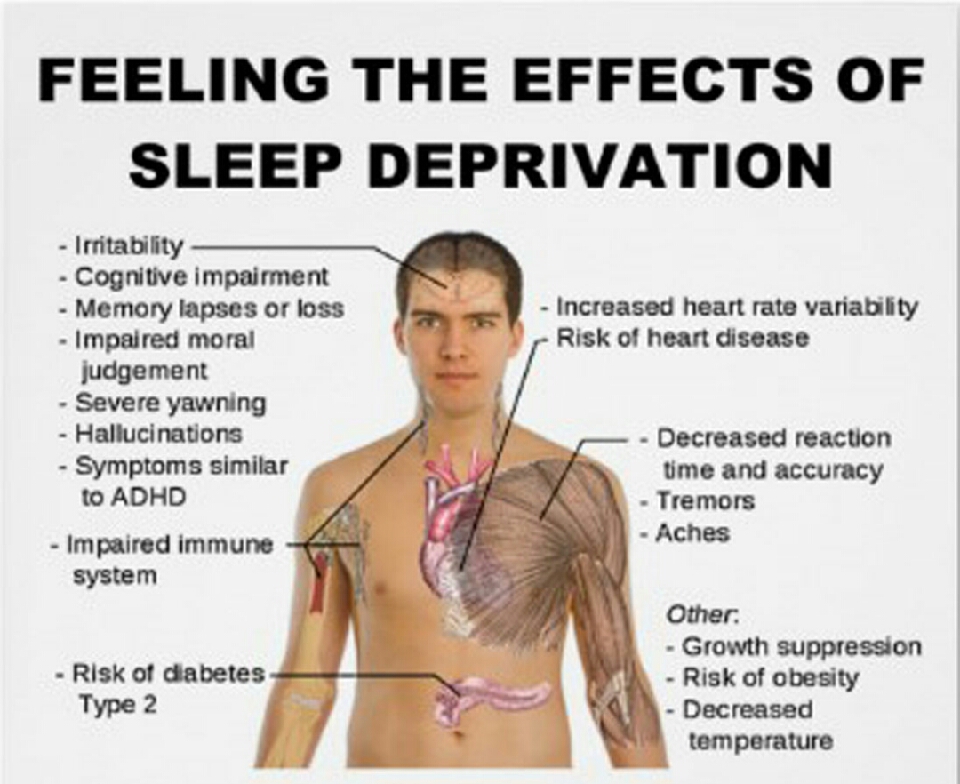
-
Select the pattern for which you want to remove the effect.
-
In the Picture Tools group on the Format tab, in the Picture Styles group, select Picture Effects .
-
Select the Effects category for the picture you want to delete. In the menu, the first option is No
(for example, No Shadow or No Reflection). Select this option to remove these effects from the picture.
Important: Office 2010 is no longer supported by .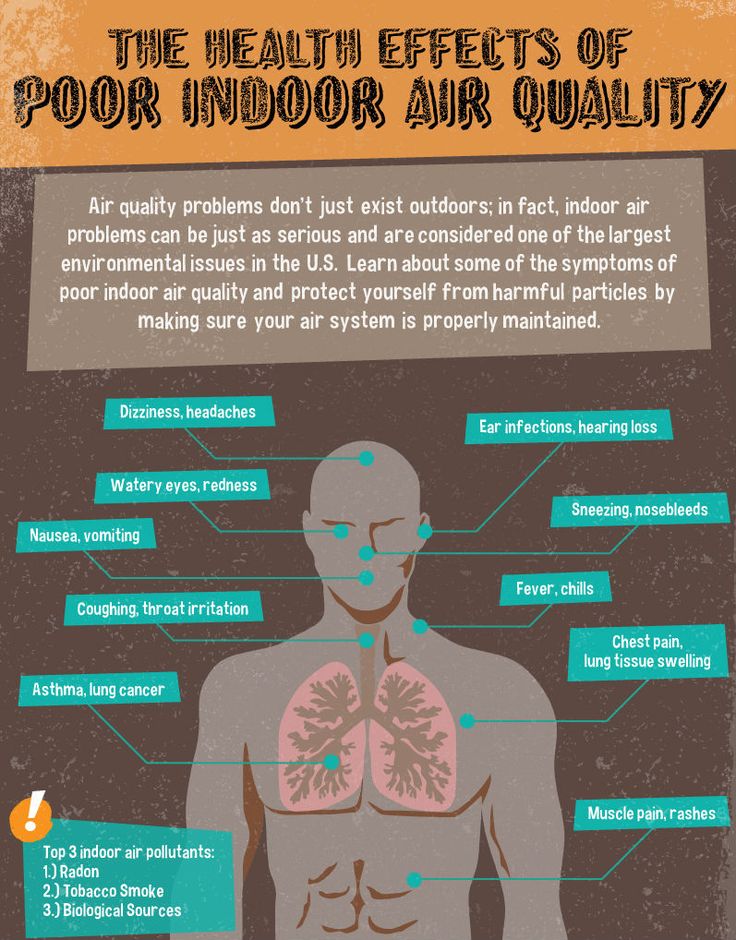 Move to Microsoft 365 to work remotely from any device and continue to receive support.
Move to Microsoft 365 to work remotely from any device and continue to receive support.
Update
To make a drawing more attractive, you can add effects such as shadows, glows, reflections, anti-aliasing, embossing, and 3-D rotation.
You can also add an artistic effect or change the brightness, contrast, or sharpness of a picture.
-
Click the picture for which you want to add or change an effect.
Note: To add the same effect to multiple patterns, click the first pattern, and then press and hold the CTRL key while clicking other patterns. When using Word, you need to copy the drawings to the canvas if they are not already there. Click the Insert tab, click the Shapes icon and select New Canvas .
 (After adding or changing an effect, you need to move the drawings back to their original place in the document.)
(After adding or changing an effect, you need to move the drawings back to their original place in the document.) -
On the Picture Tools panel , on the Format tab, in the Picture Styles group, click Picture Effects .
If the Picture Tools or Format tab is not visible, double-click the picture to make sure it is selected. If the words 9 are displayed next to the file name at the top of the program window0015 [Compatibility mode] , save the document in DOCX or XLSX format (instead of the old DOC or XLS file format) and try again.
-
Do one or more of the following:
-
Hover over Preset 9 to add or modify a built-in combination of effects0016 and then click the desired effect.
To set the inline effect, click Volume Options and change the settings as needed.
-
To add or modify a shadow, point to Shadow and then click the desired shadow.
Click 9 to adjust the shadow0015 Shade Options and change the options as needed.
-
To add or modify a reflection, point to Reflection and then click the desired reflection option.
To configure reflection, click Reflection options and change the required settings.
-
To add or modify a glow, point to Glow and then click the desired glow option.
To customize the glow colors, select the command Other glow colors , and then select the desired color. To change a color that is not included in Theme Colors, select the Additional Colors command, and then select the desired color on the 9 tab0015 Standard or create your own color on the tab Spectrum . Custom colors and colors on the Standard tab are not updated when the document theme is subsequently changed.
To set glow options, click Glow Options and change the settings as needed.
-
Click 9 to add or change smoothing0015 Smoothing , and then select the amount of smoothing you want.
To adjust smoothing, click Smoothing Options and change the settings as needed.
-
To add or modify a relief, point to Relief and then click the desired relief.
To adjust the relief, click Volume Options and change the required settings.
-
To add or change a 3-D rotation, point to 3-D Rotation and then click the desired rotation option.
To set up the rotation, select the command Rotation options for 3-D figure and change the required parameters.
Notes:
-
For more information about the options in these at the top of the dialog box Format picture.
-
-
Removing effect from pattern
For each effect category picture
For example, to remove the shadow, pointer to Effects for Picture > Shadow > No shadow .
-
Select the pattern for which you want to remove the effect.
-
In the Picture Tools group on the Format tab, in the Picture Styles group, select Picture Effects .
-
Select the Effects category for the picture you want to delete. In the menu, the first option is No
(for example, No shadow or No reflection). Select this option to remove these effects from the picture.
Do any of the following.
Quick style application
-
Click the picture and open the Picture Format tab.
-
Press the Quick Styles button and select the desired style.
Add or modify a shadow, reflection, glow, edge, wraparound, or three-degree rotation
-
Click the picture and open the Picture Format tab.
-
Click Picture Effects , hover over the effect type and select the desired effect.
-
To adjust the effect, press the button Parameters at the bottom of the effect menu.
Additional information
Inserting pictures
Important: Microsoft Office for Mac 2011 is no longer supported by . Move to Microsoft 365 to work remotely from any device and continue to receive support.
Update
Do any of the following.
Applying and changing style
-
Click the picture and open the Picture Format tab.
-
Under Picture Styles , select the desired style.
To see more styles, hover over the element of interest and click .
Add or modify a shadow, reflection, glow, bevel, or 3D rotation
-
Click the picture and open the Picture Format tab.
-
In section Picture Styles click the button Effects , hover over the effect type and select the desired option.
-
To fine-tune the effect, in Picture Styles , click the Effects button, hover over the effect type, and select Options [effect name] .
Accessories
Change color, transparency, or recolor a picture
Removing the background of a picture
Edit pictures in the Photos app in Windows 10
Add Lighting Effects in Photoshop
User's Guide Cancel
Search
Last update Dec 13, 2021 06:59:03 PM GMT
- Photoshop User Guide
- Introduction to Photoshop
- Dream about it.
 Do it.
Do it. - What's New in Photoshop
- Editing the first photo
- Create documents
- Photoshop | Frequently Asked Questions
- Photoshop System Requirements
- Transferring presets, operations and settings
- Introduction to Photoshop
- Dream about it.
- Photoshop and other Adobe products and services
- Working with Illustrator artwork in Photoshop
- Working with Photoshop files in InDesign
- Substance 3D Materials for Photoshop
- Photoshop and Adobe Stock
- Working with the built-in Capture extension in Photoshop
- Creative Cloud Libraries
- Creative Cloud Libraries in Photoshop
- Working in Photoshop using the Touch Bar
- Net and guides
- Creating transactions
- Cancellation and transaction history
- Photoshop on iPad
- Photoshop on iPad | General questions
- Work environment introduction
- System requirements | Photoshop on iPad
- Creating, opening and exporting documents
- Adding photos
- Working with layers
- Drawing and painting with brushes
- Selecting areas and adding masks
- Retouch compositions
- Working with Adjustment Layers
- Adjusting the key of a composition using the Curves layer
- Applying transform operations
- Trimming and rotating compositions
- Rotate, pan, zoom and restore the canvas
- Working with text layers
- Working with Photoshop and Lightroom
- Getting missing fonts in Photoshop on iPad
- Japanese text in Photoshop on iPad
- Application settings management
- Touch shortcuts and gestures
- Key combinations
- Image resizing
- Live stream your creative process in Photoshop on iPad
- Fix imperfections with the Healing Brush
- Creating brushes in Capture and using them in Photoshop
- Working with Camera Raw files
- Creating and using smart objects
- Adjusting the exposure of images with the Dodge and Burn tools
- Photoshop Web Application Beta
- Frequently Asked Questions | Photoshop Web App Beta
- Work environment overview
- System requirements | Photoshop Web App Beta
- Keyboard shortcuts | Photoshop Web App Beta
- Supported file formats | Photoshop Web Application Beta
- Opening and working with cloud documents
- Collaboration with stakeholders
- Limited editing options for cloud documents
- Cloud Documents
- Photoshop Cloud Documents | FAQ
- Photoshop Cloud Documents | Workflow Questions
- Working with and managing cloud documents in Photoshop
- Cloud storage update for Photoshop
- Unable to create or save cloud document
- Troubleshooting Photoshop cloud documents
- Collecting cloud document sync logs
- Sharing and editing cloud documents
- File Sharing and Commenting in Application
- Work environment
- Work environment basics
- Learn faster with the What's New panel in Photoshop
- Create documents
- Working in Photoshop using the Touch Bar
- Tool Gallery
- Performance settings
- Using tools
- Touch gestures
- Touch gestures and customizable workspaces
- Overview versions of technology
- Metadata and comments
- Default key combinations
- Touch gestures and customizable workspaces
- Putting Photoshop images in other applications
- Installations
- Default key combinations
- Rulers
- Show or hide non-printing auxiliaries
- Specifying columns for the image
- Cancellation and transaction history
- Panels and menus
- File placement
- Positioning elements with reference
- Positioning with the ruler tool
- Presets
- Customizing keyboard shortcuts
- Net and guides
- Web, screen, and application content development
- Photoshop for design
- Artboards
- View on device
- Copy CSS from layers
- Dividing web pages into fragments
- HTML options for snippets
- Changing the arrangement of fragments
- Working with web graphics
- Create web photo galleries
- Understanding images and working with color
- Resizing images
- Working with raster and vector images
- Image size and resolution
- Importing images from cameras and scanners
- Creating, opening and importing images
- Image viewer
- "Invalid JPEG marker" error | Opening images
- Viewing multiple images
- Customizing color palettes and color swatches
- HDR images
- Image color matching
- Converting between color modes
- Color modes
- Erase image fragments
- Blend modes
- Choice of colors
- Making changes to indexed color tables
- Image information
- Distortion filters not available
- Color details
- Color and monochrome corrections with channels
- Selecting colors in the Color and Swatches panels
- Sample
- Color mode (or picture mode)
- Shade
- Adding a color mode change to an operation
- Add swatches from HTML 9 CSS and SVG files0024
- Bit depth and settings
- Layers
- Understanding Layers
- Reversible editing
- Create and manage layers and groups
- Selecting, grouping and linking layers
- Putting images into frames
- Opacity and layering
- Layer masks
- Applying smart filters
- Layer compositions
- Move, arrange and lock layers
- Masking layers with vector masks
- Managing layers and groups
- Effects and Layer Styles
- Editing layer masks
- Extract resources
- Display layers with clipping masks
- Generation of graphic resources from layers
- Working with smart objects
- Blend modes
- Combining several fragments into one image
- Combining Images with Auto Layers
- Alignment and distribution of layers
- Copy CSS from layers
- Load selections based on layer boundaries or layer masks
- See-through to show the contents of other layers
- Layer
- Mixing
- Composite images
- Background
- Selections
- Select and Mask workspace
- Quick Scoping
- Getting Started with Selections
- Selecting with the Marquee toolbox
- Selecting with the Lasso tools
- Selecting a color range in an image
- Pixel highlight setting
- Convert between paths and selection boundaries
- Channel Basics
- Moving, copying and deleting selected pixels
- Creating a temporary quick mask
- Save selections and alpha channel masks
- Selecting focus areas in an image
- Duplication, splitting and merging of channels
- Channel calculation
- Extraction
- Bounding box
- Image corrections
- Perspective distortion
- Reducing blur due to camera movement
- Healing Brush Tool Examples
- Export color lookup tables
- Image sharpening and blur correction
- Understanding color grading
- Applying the Brightness/Contrast setting
- Shadow and Highlight Detail Correction
- "Levels" correction
- Hue and saturation correction
- Juiciness Correction
- Adjusting the color saturation in image areas
- Quick tone correction
- Applying special color effects to images
- Improving the image by adjusting the color balance
- HDR images
- View histograms and pixel values
- Image color matching
- Crop and straighten photographs
- Converting a color image to black and white
- Adjustment and fill layers
- Curves adjustment
- Blend modes
- Target Imaging for Press
- Color and tone correction with Levels and Curves eyedroppers
- HDR exposure and toning compensation
- Filter
- Blur
- Lighten or darken areas of an image
- Selective Color Correction
- Replacing object colors
- Adobe Camera Raw
- Camera Raw system requirements
- What's New in Camera Raw
- Introduction to Camera Raw
- Creation of panoramas
- Supported lenses
- Vignetting, graininess, and haze removal in Camera Raw
- Default key combinations
- Automatic perspective correction in Camera Raw
- Reversible editing in Camera Raw
- Camera Raw Radial Filter Tool
- Manage Camera Raw settings
- Processing, saving and opening images in Camera Raw
- Image enhancements with Camera Raw's improved Spot Remover
- Rotating, cropping and modifying images
- Camera Raw color correction
- Feature Overview | Adobe Camera Raw | Issues for 2018
- Overview of new features
- Processing versions in Camera Raw
- Making local adjustments in Camera Raw
- Fixing and restoring images
- Removing objects from photos using Content-Aware Fill
- Content-aware patching and relocation
- Retouching and fixing photos
- Image Distortion and Noise Correction
- Basic troubleshooting steps to solve most problems
- Image transformation
- Object transformation
- Crop, rotate and canvas adjustment
- Crop and straighten photographs
- Creating and editing panoramic images
- Deforming images, shapes and contours
- Perspective
- Using the Liquify filter
- Content-aware scale
- Transforming images, shapes and paths
- Deformation
- Transformation
- Panorama
- Drawing and painting
- Drawing symmetrical ornaments
- Options for drawing a rectangle and changing the stroke
- Drawing details
- Drawing and editing shapes
- Paint tools
- Creating and modifying brushes
- Blend modes
- Adding color to outlines
- Edit contours
- Painting with mix brush
- Brush Presets
- Gradients
- Gradient interpolation
- Fill and stroke selections, layers, and paths
- Drawing with the pen tool group
- Pattern making
- Creating a pattern with the Pattern Builder filter
- Loop control
- Managing pattern libraries and presets
- Drawing with pen tablet
- Creating textured brushes
- Adding dynamic elements to brushes
- Gradient
- Draw stylized strokes with the Artistic Archive Brush
- Drawing with pattern
- Synchronizing presets across multiple devices
- Text
- Adding and editing text
- Universal text editor
- Working with OpenType SVG fonts
- Character formatting
- Paragraph formatting
- Creating text effects
- Text editing
- Leading and letter spacing
- Font for Arabic and Hebrew
- Fonts
- Troubleshooting fonts
- Asian text
- Creating text
- Text Engine error when using Photoshop's Type tool | Windows 8
- Adding and editing text
- Video and animation
- Video editing in Photoshop
- Editing video and animation layers
- Introduction to video and animation
- Video and animation preview
- Drawing frames in video layers
- Import video files and image sequences
- Creating frame animations
- Creative Cloud 3D Animation (Preview)
- Creating timeline animations
- Creating images for videos
- Filters and effects
- Using the Liquify filter
- Using Blur Gallery group effects
- Filter basics
- Filter effects reference
- Adding lighting effects
- Using the Adaptive Wide Angle filter
- Oil Paint Filter
- Effects and Layer Styles
- Applying specific filters
- Image area feathering
- Saving and exporting
- Saving files in Photoshop
- Export files to Photoshop
- Supported file formats
- Saving files in other graphic formats
- Move projects between Photoshop and Illustrator
- Saving and exporting video and animation
- Saving PDF files
- Digimarc copyright protection
- Saving files in Photoshop
- Printing
- Printing 3D objects
- Printing with Photoshop
- Printing and color management
- Checklists and PDF presentations
- Print photos in a new image layout
- Spot color printing
- Duplexes
- Printing images on a printing press
- Photoshop Color Enhancement
- Printing troubleshooting | Photoshop
- Automation
- Create activities
- Creating data-driven images
- Scenarios
- File batch processing
- Operation playback and management
- Adding conditional operations
- About actions and the Actions panel
- Recording tools in operations
- Adding a color mode change to an operation
- Photoshop UI Development Kit for Plugins and Scripts
- Color Management
- Understanding Color Management
- Accurate color assurance
- Color settings
- Working with color profiles
- Color management of documents for viewing on the web
- Color management for document printing
- Color management of imported images
- Proofing
- Content authenticity
- Learn more about content credentials
- Identity and origin of NFT tokens
- Connecting accounts for creative attribution
- 3D objects and technical images
- 3D in Photoshop | Common questions about deprecated 3D features
- Creative Cloud 3D Animation (Preview)
- Printing 3D objects
- 3D drawing
- 3D Panel Enhancement | Photoshop
- 3D Concepts and Tools
- Rendering and saving 3D objects
- Creating 3D objects and animations
- Image stacks
- 3D graphics workflow
- Measurements
- DICOM files
- Photoshop and MATLAB
- Counting objects in an image
- Merging and transforming 3D objects
- Editing 3D textures
- HDR Exposure and Toning Compensation
- 3D panel settings
Lighting effects filter allows you to create various lighting effects in RGB images. Provided also the ability to apply textures obtained from grayscale image files (they are called bump maps ) to create volumetric effects, and save your own styles for use in other images.
Provided also the ability to apply textures obtained from grayscale image files (they are called bump maps ) to create volumetric effects, and save your own styles for use in other images.
The Lighting Effects filter in Photoshop only works on 8-bit RGB images. You must have a supported graphics card to use lighting effects. See Frequently Asked Questions for more information.
-
Select "Filter" > Render > Lighting Effects.
-
Select a style from the Presets menu in the upper left corner.
-
In the browser, select the individual lights to be adjusted. Then, on the top half of the properties panel, do one of the following:
- Select the source type (directional, infinite or point) from the top menu.
- Adjust the color, intensity and size of the light center.
-
In the lower half of the properties panel, set up the entire set of lights with the following options:
Toning
Click to tint all lighting.
exposition
Controls highlight and dark area information.
Gloss
Determines how many surfaces reflect light.
Metal
Determines which color is more present in reflected light: the color of the incident light or the color of the object it hits.
Wednesday
Diffuses light as if it were mixed with other (sun or fluorescent) light in the room. To use only the light source, choose 100, and to remove it, choose -100.
Texture
Applies the texture channel.
Quickly master the dedicated lighting effects workspace. This tutorial by Dan Moughamian provides step by step instructions.
Also see the Lighting Effects overview video by Matt Kloskowski.
Several types of light sources can be selected.
Dot
Illumination in all directions directly above the image, like a light bulb.
Endless
Illumination of the whole plane, like the sun.
dotted
Emits an elliptical beam of light. The line in the viewport defines the direction and angle of the light, and the handles define the edges of the ellipse.
-
From the top menu of the properties panel, select Point.
-
Adjust the light source in the viewer window.
- To move the light, drag it anywhere on the canvas.
- To change the spread of the light (reflecting the light coming in or out), drag the white section of the intensity ring in the center.
An intensity value of 100 produces the brightest illumination, normal illumination is around 50, negative intensity values move the light source further away, and a value of –100 produces no illumination.

-
Select Infinite from the top menu of the properties panel.
-
Adjust the light.
- To change direction, drag the marker at the end of the line.
- To change the brightness, drag the white section of the intensity ring in the center of the light controls.
- To change direction, drag the marker at the end of the line.
-
At the top of the properties panel, select Directional.
-
Adjust the light source in the viewer window.
- To move the light, drag within the outer ellipse.
- To rotate the light, drag outside the outer ellipse.
- To change the angle of the light center, drag the edge of the inner ellipse.
- To stretch or shrink the ellipse, drag one of the four outer handles.
- To change the area of the ellipse filled with light, drag the white section of the intensity ring in the center.

The Presets menu in the Lighting Effects workspace allows you to choose from 17 lighting styles. You can also create your own sets by setting additional lights in the "Default" option. The Lighting Effects filter requires at least one light source to be applied. At one point in time, it is allowed to edit the characteristics of only one light source, but all additionally entered ones are used to create the effect.
Spotlight at 2 o'clock
Yellow spotlight with medium (17) intensity and wide (91) focus.
blue light bulb
Blue top lamp with and without full (85) intensity focus.
circle of light
Four projectors. White has full (100) intensity and concentrated (8) focus. Yellow has strong intensity (88) and concentrated (3) focus. Red has medium (50) intensity and concentrated (0) focus. Blue has full (100) intensity and medium (25) focus.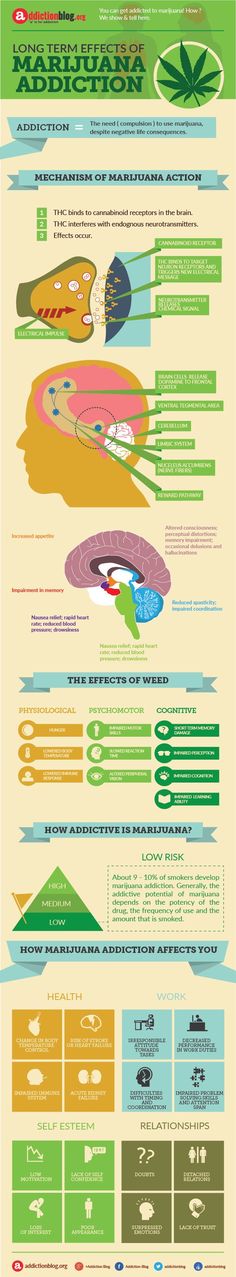
crosshair
White spotlight with medium (35) intensity and wide (69) focus.
crosshair down
Two white spotlights with medium (35) intensity and wide (100) focus.
Default
Medium intensity white spotlight (35) with wide focus (69).
Five lights down/five lights up
Five spotlights pointing down or up, full (100) intensity and wide (60) focusing.
Torch
Yellow bulb with medium (46) intensity.
flood light
White Medium (35) Wide (69) focus.
Parallel directed
Directional blue daylight with full (98) intensity and no focus.
RGB Light Sources
Red, blue and green light sources which emit light with an average (60) intensity and broad (96) focus.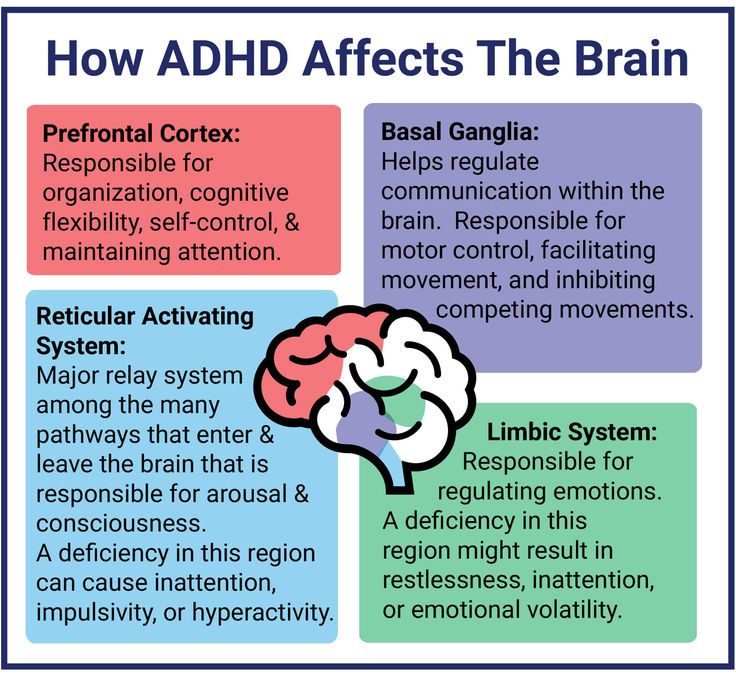
Soft directional light
Two directional light sources, white and blue, not focused. The white light source has a weak (20) intensity. The blue light source has a medium (67) intensity.
soft bulb
Soft bulb with medium (50) intensity.
soft spotlight
White full (98) intensity and wide (100) spotlight focus.
Three down
Three white spotlights with low (35) intensity and wide (96) focusing.
triple spotlight
Three spotlights with low (35) intensity and wide (100) focus.
-
In the Lighting Effects workspace, do one of the following:
- In the upper left corner, click the light icons to add point, directional, and infinity lights. Repeat this operation if necessary (maximum 16 light sources are allowed).
- In the Lights panel (located in the lower right corner by default), drag a light onto the trash icon to remove it.
- In the upper left corner, click the light icons to add point, directional, and infinity lights. Repeat this operation if necessary (maximum 16 light sources are allowed).
-
In the Lighting Effects dialog box, do one of the following:
- To create a preset, select Custom from the Preset menu and click the light icons to add point, directional, and infinity lights. Repeat this operation if necessary (maximum 16 light sources are allowed).
- To save the set, click Save, name the style, and then click OK. Saved presets include all settings for each light source and appear in the Preset menu each time an image is opened.
- To delete a set, select it and then click the Delete button.
In the Lighting Effects workspace, the Texture channel lets you control lighting effects using grayscale images (called "bump maps"). Bump maps are added to the image as alpha channels. You can add any grayscale image as an alpha channel to an image, or create a new alpha channel and add a texture to it. To create an embossed text effect, use a channel with white text on a black background (or vice versa).