Dsm 5 alcohol use disorder diagnostic criteria
Alcohol Use Disorder: A Comparison Between DSM–IV and DSM–5
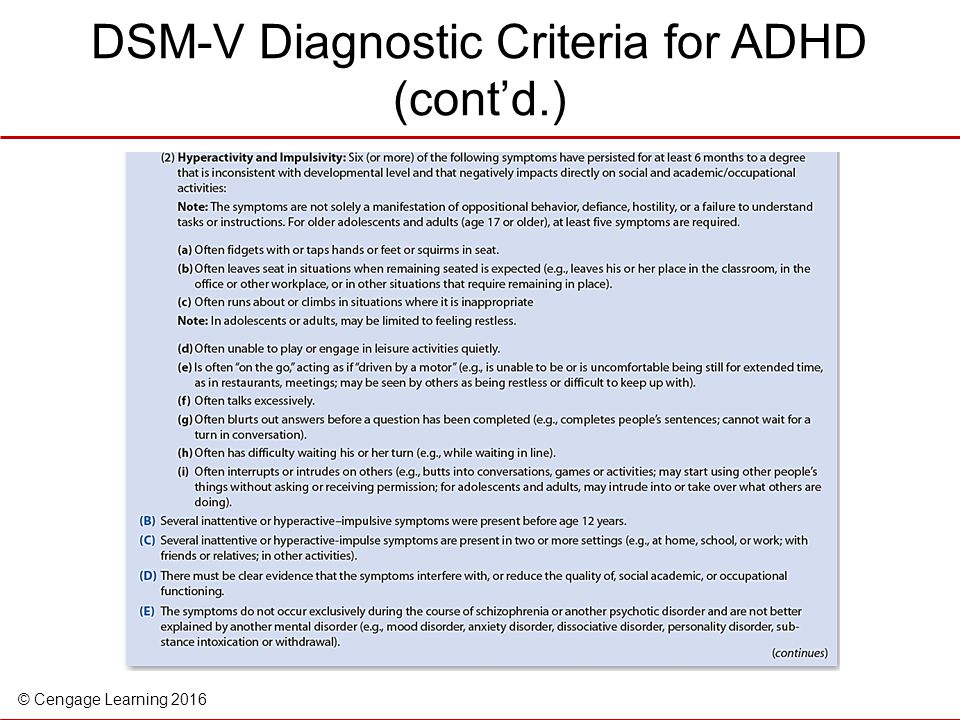
In May 2013, the American Psychiatric Association issued the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM–5). Although there is considerable overlap between DSM–5 and DSM–IV, the prior edition, there are several important differences:
Changes Disorder Terminology
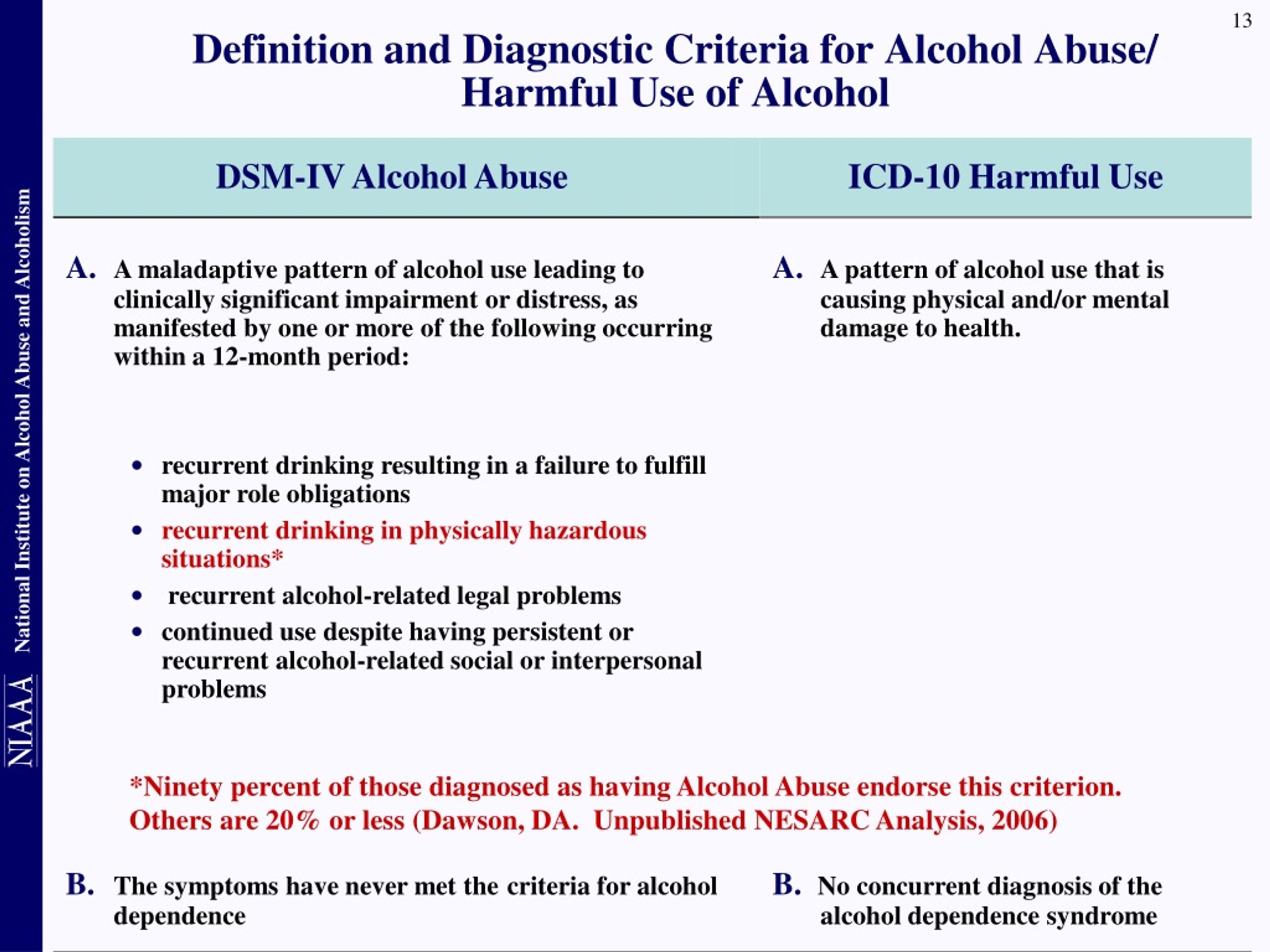
- DSM–IV described two distinct disorders, alcohol abuse and alcohol dependence, with specific criteria for each.
- DSM–5 integrates the two DSM–IV disorders, alcohol abuse and alcohol dependence, into a single disorder called alcohol use disorder (AUD) with mild, moderate, and severe sub-classifications.
Changes Diagnostic Thresholds
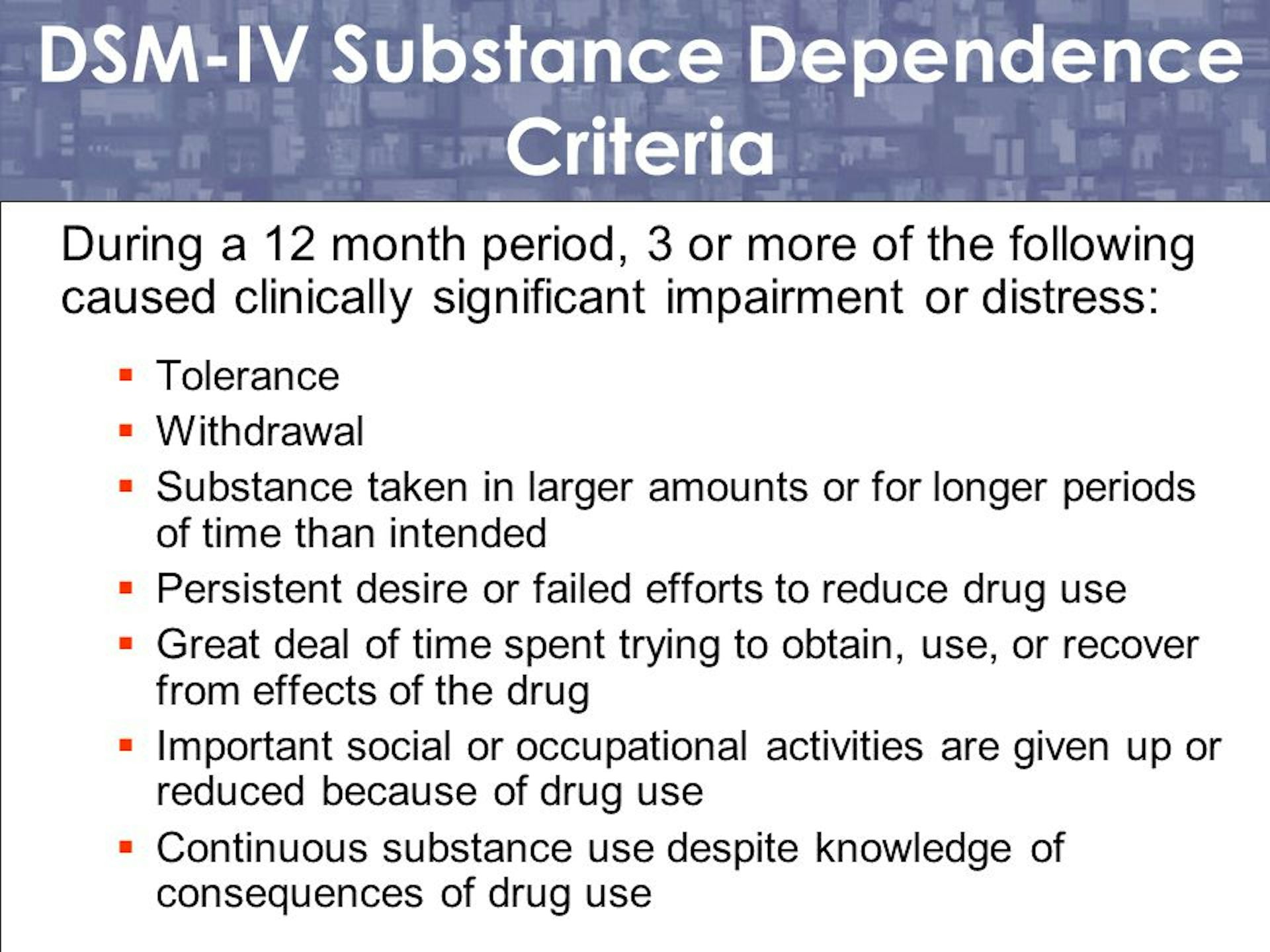
- Under DSM–IV, the diagnostic criteria for abuse and dependence were distinct: anyone meeting one or more of the “abuse” criteria (see items 1 through 4 below) within a 12-month period would receive the “abuse” diagnosis. Anyone with three or more of the “dependence” criteria (see items 5 through 11 below) during the same 12-month period would receive a “dependence” diagnosis.
- Under DSM–5, anyone meeting any 2 of the 11 criteria during the same 12-month period would receive a diagnosis of AUD. The severity of AUD—mild, moderate, or severe—is based on the number of criteria met.
Removes Criterion
- DSM–5 eliminates legal problems as a criterion.
Adds Criterion
- DSM–5 adds craving as a criterion for an AUD diagnosis. It was not included in DSM–IV.
Revises Some Descriptions
- DSM–5 modifies some of the criteria descriptions with updated language.
DSM History and Background
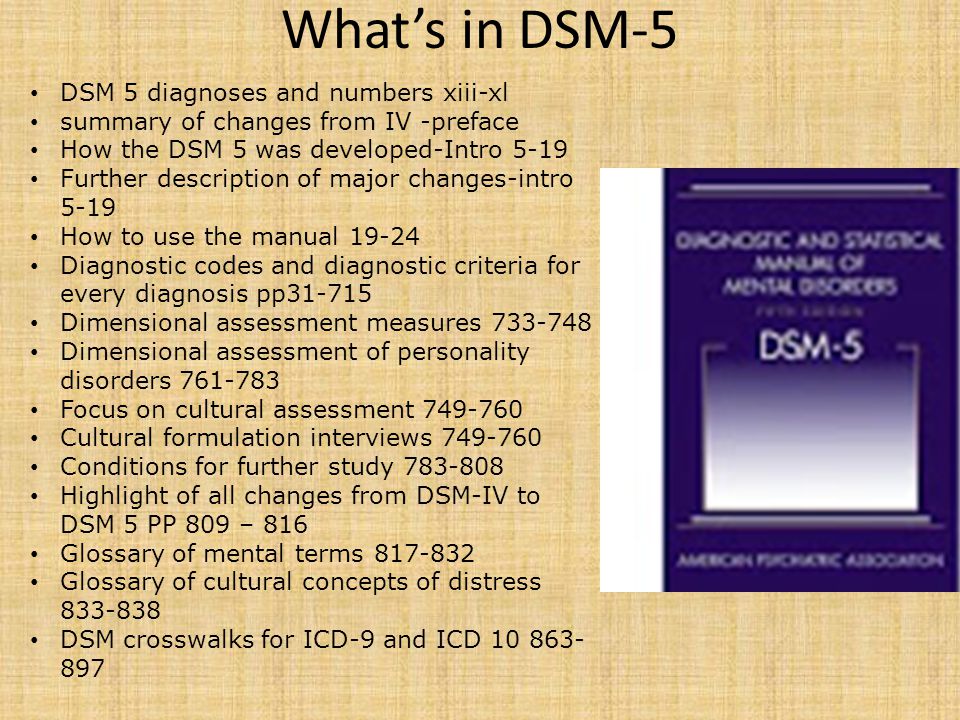
The Diagnostic and Statistical Manual of Mental Disorders (DSM) initially developed out of a need to collect statistical information about mental disorders in the United States. The first attempt to collect information on mental health began in the 1840 census. By the 1880 census, the Bureau of the Census had developed seven categories of mental illness. In 1917, the Bureau of the Census began collecting uniform statistics from mental hospitals across the country.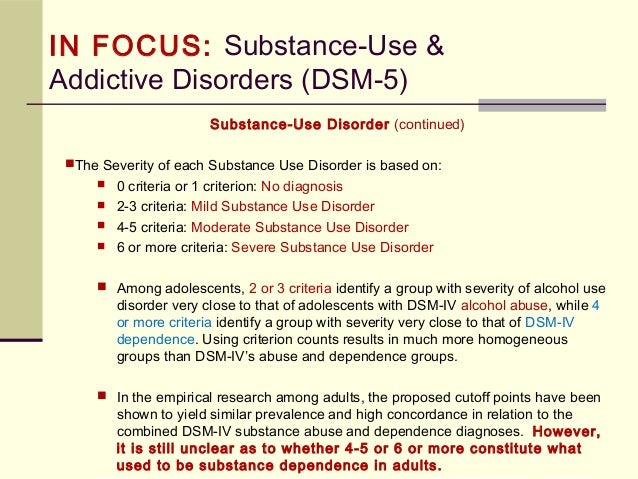
Not long afterward, the American Psychiatric Association and the New York Academy of Medicine collaborated to produce a “nationally acceptable psychiatric nomenclature” for diagnosing patients with severe psychiatric and neurological disorders. After World War I, the Army and Veterans Administration broadened the nomenclature to include disorders affecting veterans.
In 1952, the American Psychiatric Association Committee on Nomenclature and Statistics published the first edition of the Diagnostic and Statistical Manual: Mental Disorders (DSM–I). The DSM–I included a glossary describing diagnostic categories and included an emphasis on how to use the manual for making clinical diagnoses. The DSM–II, which was very similar to the DSM–I, was published in 1968. The DSM–III, published in 1980, introduced several innovations, including explicit diagnostic criteria for the various disorders, that are now a recognizable feature of the DSM. A 1987 revision to the DSM–III, called the DSM–III–R, clarified some of these criteria and also addressed inconsistencies in the diagnostic system.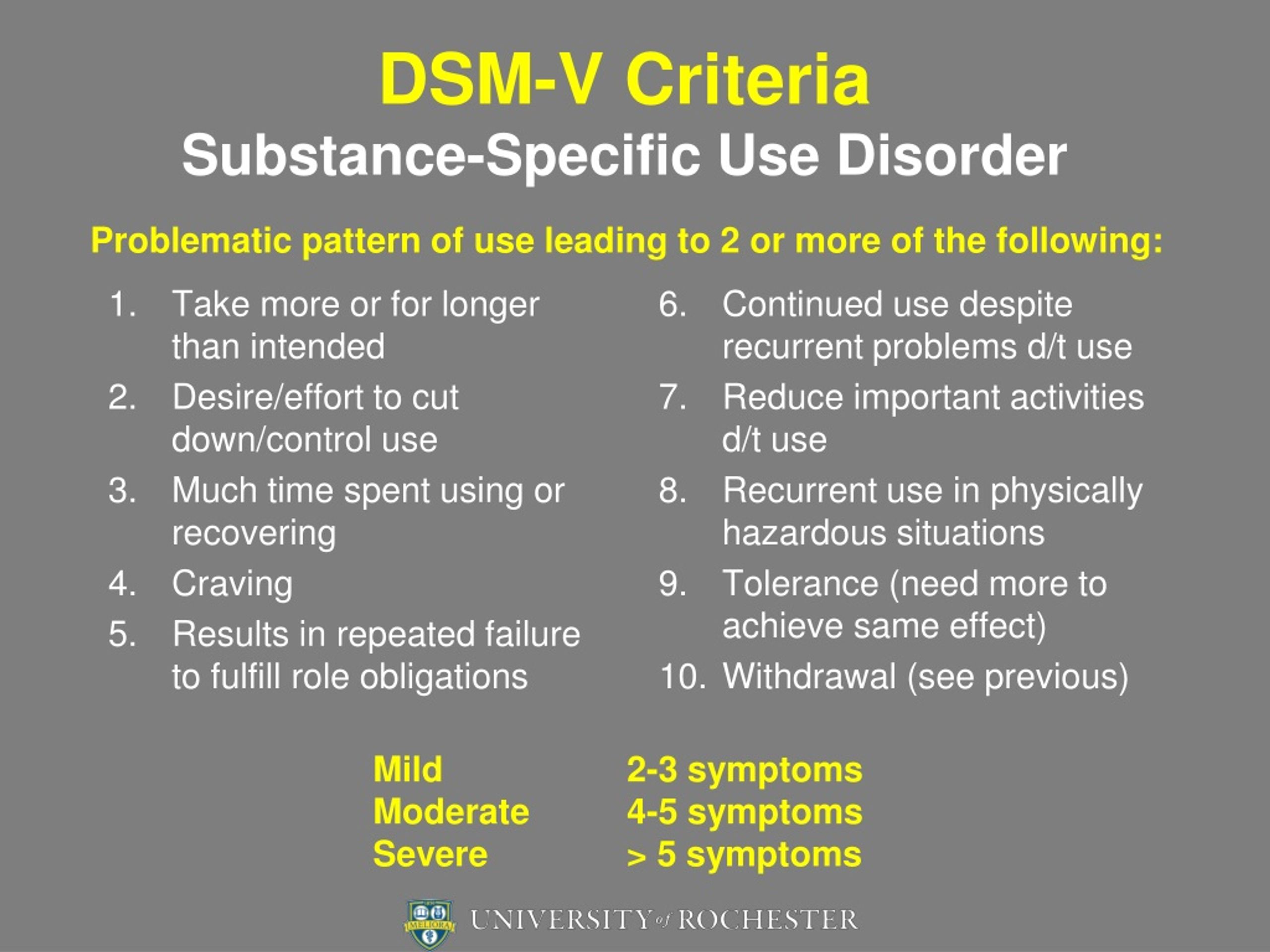 A comprehensive review of the scientific literature strengthened the empirical basis of the next edition, the DSM–IV, which was published in 1994. The DSM–IV–TR, a revision published in 2000, provided additional information on diagnosis. Since 1952, each subsequent edition of the DSM aimed to improve clinicians’ ability to understand and diagnose a wide range of conditions.
A comprehensive review of the scientific literature strengthened the empirical basis of the next edition, the DSM–IV, which was published in 1994. The DSM–IV–TR, a revision published in 2000, provided additional information on diagnosis. Since 1952, each subsequent edition of the DSM aimed to improve clinicians’ ability to understand and diagnose a wide range of conditions.
A Comparison Between DSM–IV and DSM–5
For screen readers, use this accessible text version.
| DSM–IV | |
|---|---|
| In the past year, have you: | |
| Any 1 = ALCOHOL ABUSE | |
| Found that drinking—or being sick from drinking—often interfered with taking care of your home or family? Or caused job troubles? Or school problems? | |
| More than once gotten into situations while or after drinking that increased your chances of getting hurt (such as driving, swimming, using machinery, walking in a dangerous area, or having unsafe sex)? | |
| More than once gotten arrested, been held at a police station, or had other legal problems because of your drinking? | |
| Continued to drink even though it was causing trouble with your family or friends? | |
| Any 3 = ALCOHOL DEPENDENCE | |
| Had to drink much more than you once did to get the effect you want? Or found that your usual number of drinks had much less effect than before? | |
| Found that when the effects of alcohol were wearing off, you had withdrawal symptoms, such as trouble sleeping, shakiness, restlessness, nausea, sweating, a racing heart, or a seizure? Or sensed things that were not there? | |
| Had times when you ended up drinking more, or longer, than you intended? | |
| More than once wanted to cut down or stop drinking, or tried to, but couldn’t? | |
| Spent a lot of time drinking? Or being sick or getting over other aftereffects? | |
| Given up or cut back on activities that were important or interesting to you, or gave you pleasure, in order to drink? | |
| Continued to drink even though it was making you feel depressed or anxious or adding to another health problem? Or after having had a memory blackout? | |
| DSM–5 | |
|---|---|
| In the past year, have you: | |
| The presence of at least 2 of these symptoms indicates Alcohol Use Disorder (AUD). Mild: The presence of 2 to 3 symptoms
| |
| Had times when you ended up drinking more, or longer, than you intended? | |
| More than once wanted to cut down or stop drinking, or tried to, but couldn’t? | |
| Spent a lot of time drinking? Or being sick or getting over other aftereffects? | |
| Wanted a drink so badly you couldn’t think of anything else? | |
| Found that drinking—or being sick from drinking—often interfered with taking care of your home or family? Or caused job troubles? Or school problems? | |
| Continued to drink even though it was causing trouble with your family or friends? | |
| Given up or cut back on activities that were important or interesting to you, or gave you pleasure, in order to drink? | |
| More than once gotten into situations while or after drinking that increased your chances of getting hurt (such as driving, swimming, using machinery, walking in a dangerous area, or having unsafe sex)? | |
| Continued to drink even though it was making you feel depressed or anxious or adding to another health problem? Or after having had a memory blackout? | |
| Had to drink much more than you once did to get the effect you want? Or found that your usual number of drinks had much less effect than before? | |
| Found that when the effects of alcohol were wearing off, you had withdrawal symptoms, such as trouble sleeping, shakiness, restlessness, nausea, sweating, a racing heart, or a seizure? Or sensed things that were not there? | |
All permissions requests regarding the DSM should be directed to the American Psychiatric Association.
Understanding The DSM-5 Criteria For Alcohol Use Disorder (AUD)
- The DSM-5
- DSM-5 AUD Criteria
- DSM History & Background
Given the widespread prevalence of problem drinking, heavy drinking, and binge drinking among young adults and the general public, healthcare providers must rely on a standardized manual for defining alcohol use disorder (AUD).
AUD is a term that encompasses both alcohol abuse and alcohol dependence. It has also colloquially been known as alcoholism.
Today, the manual most commonly used to diagnose alcohol use disorder is the DSM-5.
The Diagnostic & Statistical Manual of Mental Disorders, Fifth EditionThe first step to dealing with any problem in a structured way is to define the problem as clearly as possible.
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) defines the problem by creating a taxonomy, or classification system, for mental health disorders. Conditions range from anxiety disorders and schizophrenia to substance use disorders and many more.
Conditions range from anxiety disorders and schizophrenia to substance use disorders and many more.
With the DSM-5, psychiatry and addiction medicine professionals across the United States can use the same terms, assign the proper ICD-10 medical codes, and administer the best recommended treatments for each case.
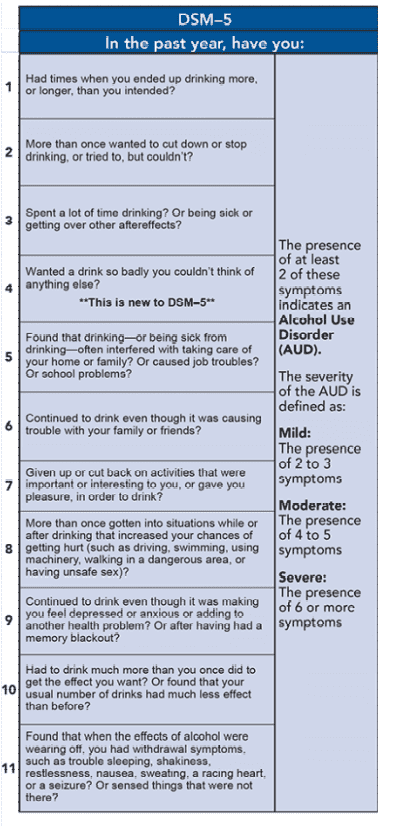
DSM-5 Alcohol Use Disorder CriteriaAccording to the DSM-5, alcohol use disorder is “a problematic pattern of alcohol use leading to clinically significant impairment or distress, as manifested by at least two of the following [criteria], occurring within a 12-month period.”
In other words, if you experienced any two of the symptoms from the following criteria/questionnaire in the past year, you can be diagnosed as having an AUD:
- Alcohol is often taken in larger amounts or over a longer period than was intended. [Do you drink more than you mean to?]
- There is a persistent desire or unsuccessful efforts to cut down or control alcohol use.
 [Do you want to stop, but can’t?]
[Do you want to stop, but can’t?] - A great deal of time is spent in activities necessary to obtain alcohol, use alcohol, or recover from its effects. [Is drinking taking over your life?]
- Craving, or a strong desire or urge to use alcohol. [If you can’t drink, are you thinking about drinking?]
- Recurrent alcohol use resulting in a failure to fulfill major role obligations at work, school, or home. [Is your drinking getting in the way of day-to-day activities?]
- Continued alcohol use despite having persistent or recurrent social or interpersonal problems caused or exacerbated by the effects of alcohol. [Is drinking getting in the way of your relationships?]
- Important social, occupational, or recreational activities are given up or reduced because of alcohol use. [Are you sitting things out because of alcohol?]
- Recurrent alcohol use in situations in which it is physically hazardous. [Are you drinking in risky settings, or doing risky things while drinking?]
- Alcohol use is continued despite knowledge of having a persistent or recurrent physical or psychological problem that is likely to have been caused or exacerbated by alcohol.
 [Do you know drinking isn’t good for you, but you do it anyway?]
[Do you know drinking isn’t good for you, but you do it anyway?] - Tolerance, as defined by either of the following: a need for markedly increased amounts of alcohol to achieve intoxication or desired effect, or a markedly diminished effect with continued use of the same amount of alcohol. [Do you need to drink more than you used to?]
- Withdrawal, as manifested by either of the following: the characteristic withdrawal syndrome for alcohol, or alcohol (or a closely related substance, such as a benzodiazepine) is taken to relieve or avoid alcohol withdrawal symptoms. [Do you feel it when you stop drinking?]
The DSM-5 further classifies AUDs by severity, determined by how many of the eleven diagnostic criteria are met.
- mild AUDs – defined as the presence of 2-3 criteria
- moderate AUDs – defined as the presence of 4-5 criteria
- severe AUDs – defined as the presence of 6 or more criteria
These levels of severity are often used by clinicians when determining risk, eligibility for certain treatment programs, recommended treatment options, and even cost.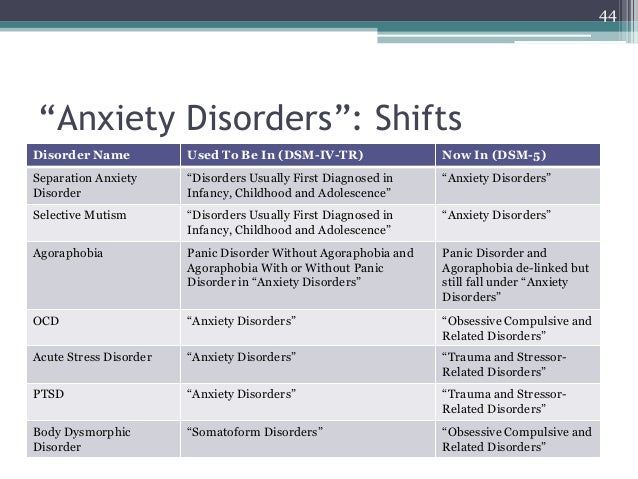
The American Psychiatric Association and the New York Academy of Medicine published the original “Diagnostic and Statistical Manual: Mental Disorders” in 1952 to establish a unified terminology for mental health diagnoses.
The DSM-II, an updated second edition, followed in 1962, and was followed by the DSM-III in 1980, and the DSM-IV in 1994. Each was intended to improve clinicians’ and public health professionals’ ability to understand and properly manage an ever-increasing range of mental-health conditions.
The 5th edition, published in May 2013, is the first “living document” version of the DSM, meaning that it has received and will receive updates and revisions as needed until a sixth edition is eventually released.
Professional Substance Abuse TreatmentChronic or compulsive alcohol consumption and drug use puts you and your loved ones at increased risk for health problems, legal problems, financial jeopardy, and more.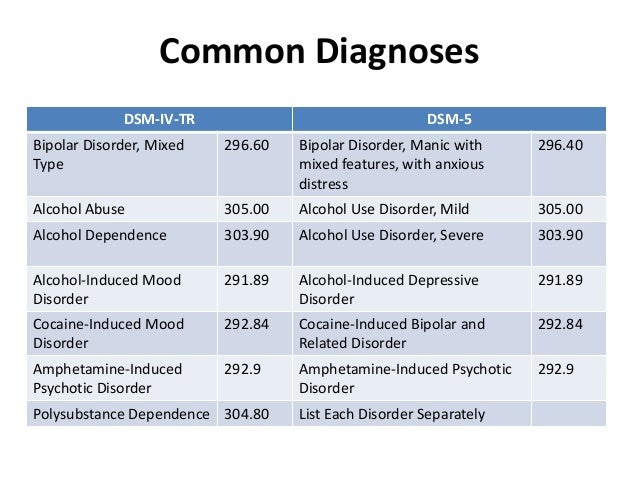 Fortunately, treatment is available.
Fortunately, treatment is available.
Ark Behavioral Health hosts a variety of inpatient and outpatient treatment programs for substance use disorders, as well as other related conditions and comorbidities. To learn if Ark Behavioral Health is the right option for you, please contact a representative today.
Written by Ark Behavioral Health Editorial Team
©2022 Ark National Holdings, LLC. | All Rights Reserved.
This page does not provide medical advice.
Sources
National Institutes of Health (NIH) - Post by Former NIMH Director Thomas Insel: Transforming Diagnosis
National Institute on Alcohol Abuse and Alcoholism (NIAAA) - Alcohol Use Disorder: A Comparison Between DSM–IV and DSM–5
Psychiatry Online - Diagnostic And Statistical Manual of Mental Disorders, Fifth Edition
Ark Behavioral Health offers 100% confidential substance abuse assessment and treatment placement tailored to your individual needs.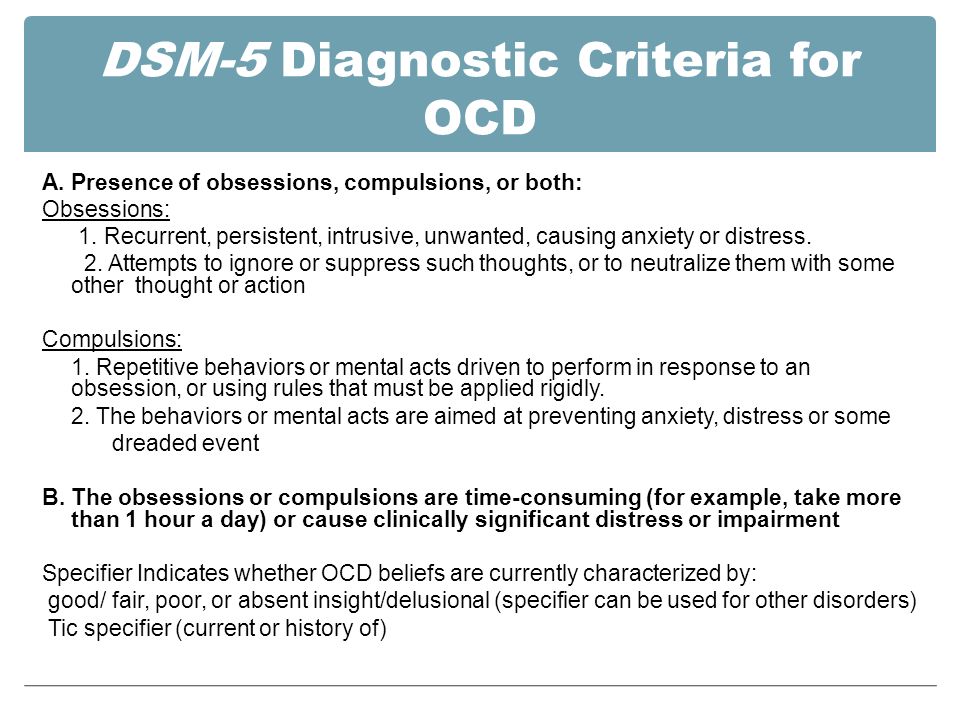 Achieve long-term recovery.
Achieve long-term recovery.
Call Now
100% confidential. We respect your privacy.
Prefer Texting?We've got you covered.
Receive 24/7 text support right away.
There is no obligation and you can opt out at any time.
First Name*
Phone Number*
By submitting this form you agree to the terms of use and privacy policy of the website. Message and data rates may apply. You may receive recourring messages. Text STOP to cancel.
What role do the DSM-5 criteria for substance use and addictive disorders play in diagnosing addiction? | Addiction & Recovery articles | Emotional & Mental Health center
Although the DSM-5 lists numerous different addictions, their diagnostic criteria are very similar - because addictions affect a person's life and behavior in the same way, regardless of substance or behavior. What should you know?
Addiction is an insidious disease that can start with a number of options, but then take over the brain - and depending on what you are addicted to, and sometimes the body.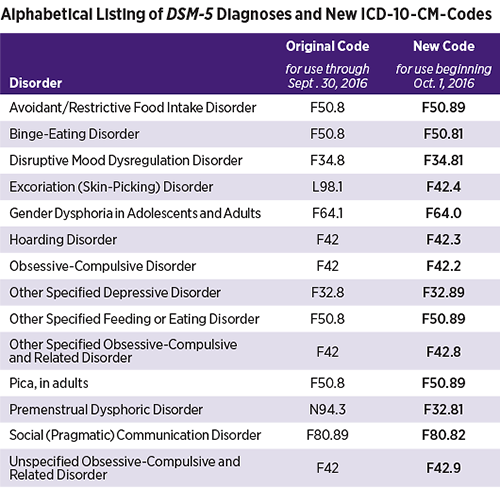 Once you're in the clutches of an addiction, the all-encompassing call for more drugs, alcohol, gambling, shopping, food, sex, or whatever you're used to becomes almost impossible to refuse.
Once you're in the clutches of an addiction, the all-encompassing call for more drugs, alcohol, gambling, shopping, food, sex, or whatever you're used to becomes almost impossible to refuse.
The American Society for Addiction Medicine describes addiction as a chronic and often progressive disease that may include periods of remission and relapse. We now know that becoming an addict is not a moral failing or a permanent choice. Once you are addicted, your addiction robs you of much of your control.
Addiction can be a serious disease, but it is indeed treatable. This treatment can take many forms, but it starts with the decision that you are ready to go into remission. If you're an addict, you've likely tried - and ultimately failed - to stop using the substance or stopped participating in the behavior multiple times and realized that professional help would be needed to break your chains.
This help starts with a diagnosis, and in the US, clinicians will use the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition - DSM-5 for short - to determine if you have an addiction and how severe it is.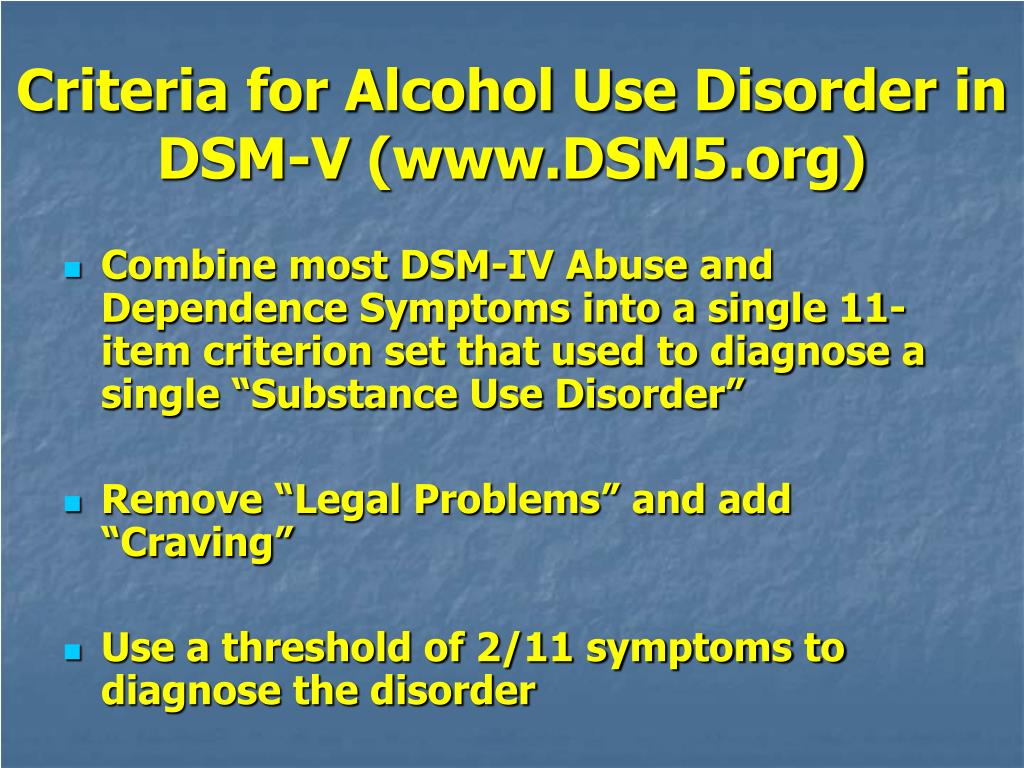
What do drug addicts and their loved ones need to know about the diagnostic criteria for DSM-5 addiction?
The DSM-5 is an incredibly long document filled with diagnostic criteria for many different mental and cognitive disorders, from depression to autism spectrum disorder and schizophrenia to narcissistic personality disorder. Addiction is described in the chapter on Substances and Dependence Disorders. This chapter covers many different addictions, including alcohol, tobacco, opioids, sedatives, sleeping pills, cannabis, and even caffeine. It also includes gambling, but has a strong addiction to psychoactive substances and is rather devoid of behavioral addictions.
DSM-5 includes those passions that were backed by hard science at the time of publication. Not all addictions described in the medical literature, such as addictions to food, shopping, sex, gaming, and Internet use, are official diagnostic categories in the DSM-5. If you are (as you think) addicted to something that is not covered in this document, you can still get the help you need.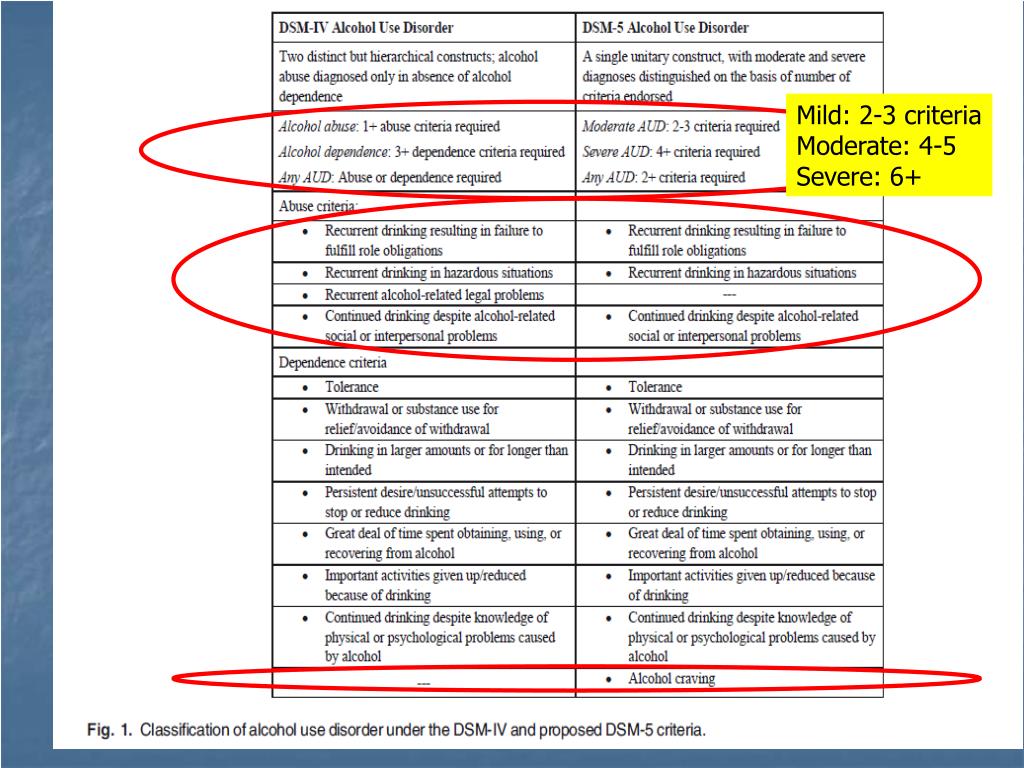 If something is not in the DSM-5, it does not mean that it does not exist.
If something is not in the DSM-5, it does not mean that it does not exist.
Look at the Diagnostic Criteria for Addiction
When you look at the diagnostic criteria for all the different addictions included in the DSM-5, you will begin to realize that they are all pretty similar - no matter what substance or behavior is being discussed in the document. We will make these diagnostic criteria more general so that you can get a general picture of the types of symptoms that signify addiction. Since the DSM-5 mainly deals with substance addiction, we will refer to "substance" - but very similar symptoms will be seen among people suffering from behavioral addictions.
First of all, the DSM-5 will require that at least two of the symptoms be present for one year resulting in significant distress or aggravation:
- The person uses more of the substance, or longer, than they intended.
- The person wants to reduce or stop the use of the substance, but is unsuccessful in these efforts.
- The person spends a lot of time using the substance, getting it, or recovering from it.
- The person experiences a strong craving for the substance.
- The use of a substance causes a person to fail to fulfill their important responsibilities in life.
- Substance use causes or exacerbates interpersonal problems, but does not cause the person to contract or stop.
- A person misses important events due to substance abuse.
- A person uses the substance in situations where it is physically dangerous (for example, while driving or operating heavy machinery).
Then there is tolerance - the person no longer achieves the same effect from using the same amount (or, in the case of a behavioral addiction, for example, from gambling with the same amount of money), or starts using more to return to the same effect . Finally, there is withdrawal symptoms - a person experiences withdrawal symptoms associated with the substance in question when they try to stop using the substance.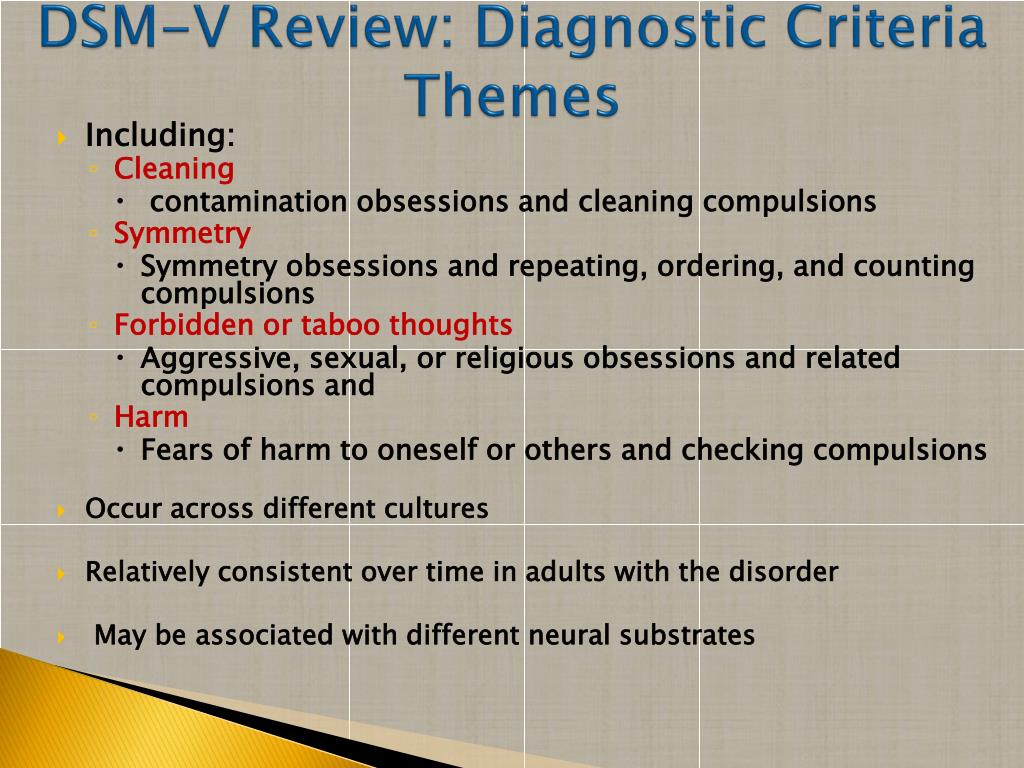
You also need to know that:
- When someone is diagnosed with an addiction, the doctor indicates how serious it is. The presence of two or three of these symptoms typically indicates a milder addiction, a score of four or five for a moderately severe addiction, and a severe addiction is marked by six or more symptoms.
- If you have used within the last year but not within the last three months, you may be diagnosed with early remission. If you have previously met the diagnostic criteria for any addiction but have been abstaining from use for more than a year, you are in stable remission.
While diagnostic criteria form the basis of a diagnosis, anyone an addict turns to for help doesn't just sneak down the list asking if they check the boxes. More “handy” screening tools and questionnaires can be used.
If you think you have an alcohol use disorder (alcoholism) and, for example, contact your family doctor, they may start with questions such as:
- How much do you drink and how often?
- How often do you feel guilty or remorseful after drinking alcohol?
- Have you ever drunk in the morning to be functional?
- How often were you unable to do what was expected of you because you drank?
- Has a relative or doctor expressed concern about your drinking?
- Have you ever been injured because you drank? Is there anyone else?
These questions ultimately try to determine if you meet the diagnostic criteria, but in more practical and specific terms.
Determining whether you are an addict and how addicted you are is only the first step, often a very scary first step. It is, however, a step that will enable addicts to receive the help they need to achieve remission.
DSM-5 PTSD - psyxotrauma - LiveJournal
DSM-V Diagnostic Criteria for PTSD (309.81)
DSM Fifth Revision classifies PTSD as a psychiatric disorder associated with stress and trauma
Below are the DSM-V criteria for PTSD for adults, adolescents, and children over 6 years of age.
Criterion A Exposure to mortal danger or threat of death, receiving or the threat of serious injury, sexual violence or its threat, which may manifest itself in one of the following ways: 90 0203 direct trauma experience.
2. Personal testimony of an event involving others.
3. News of an event that happened to close family members or close friends. In cases of imminent or possible death of a family member or friend, the event must be sudden or unexpected.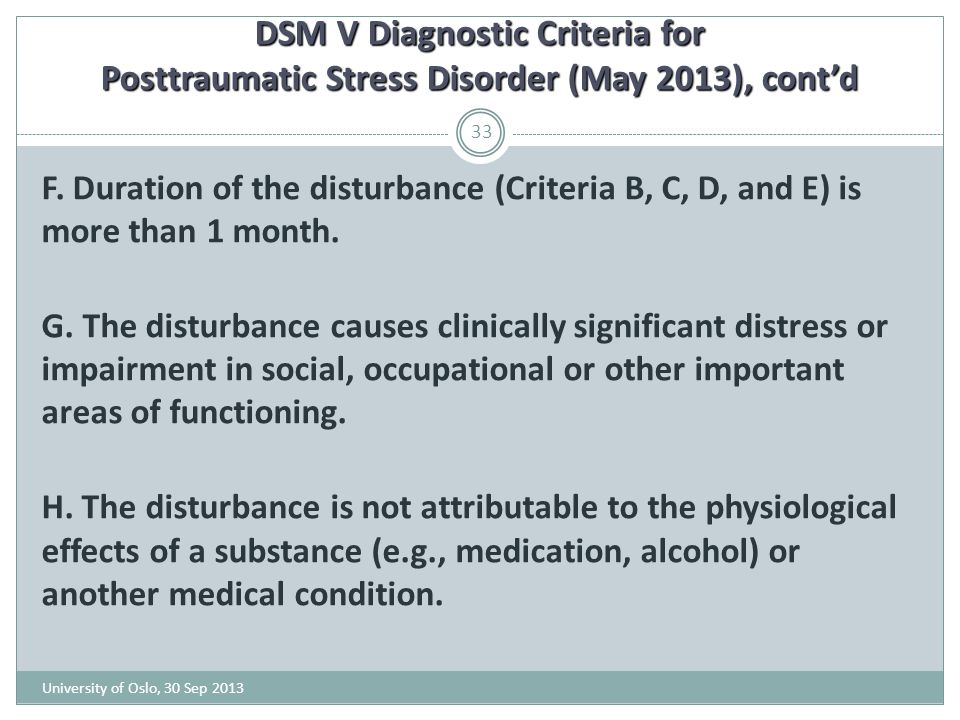
4. Repeated or excessive exposure to some aspect of the traumatic event that causes a strong negative emotional reaction (for example, those who, due to circumstances, were the first to be at the scene of a death and are busy collecting the bodies and remains of the dead; police officers who repeatedly witnessed the immediate consequences of violence over children.)
Note : Paragraph A(4) excludes indirect influence through mass media, television, films, static images in the case, only in cases when it is connected with the performance of professional duties.
Criterion B Presence of one or more intrusion symptoms associated with the traumatic event that appeared after the traumatic event:
1. Repetitive, involuntary, and intrusive memories of a traumatic event that cause distress.
2. Recurring distressing dreams whose content and/or affect is related to the traumatic event.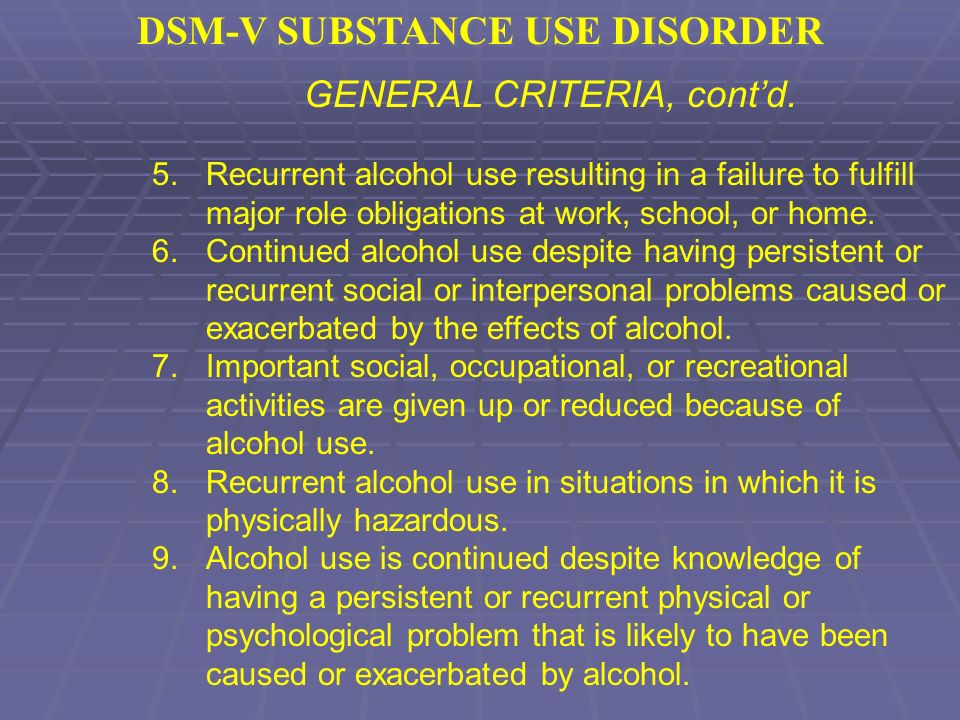
3. Dissociative reactions (eg flashback effects) in which the individual feels or behaves as if a traumatic past event is happening in the present. (Such reactions can be located on a continuum of intensity, the extreme pole of which corresponds to states with a complete loss of contact with the surrounding reality).
4. Severe or prolonged psychological distress when exposed to external or internal stimuli that symbolize or resemble some aspect of the traumatic event.
5. Physiological reactivity to external or internal stimuli that symbolize or resemble some aspect of the traumatic event.
Criterion C Sustained avoidance of trauma-related stimuli after the completion of the traumatic event (at least one of the following):
1. Avoiding or trying to avoid distressing memories, thoughts, or feelings that are directly or closely related to the traumatic event.
2. Avoiding or attempting to avoid external reminders (eg, certain people, places, objects, situations, durations, conversations) that result in distressing memories, thoughts, or feelings related to or closely associated with the traumatic event.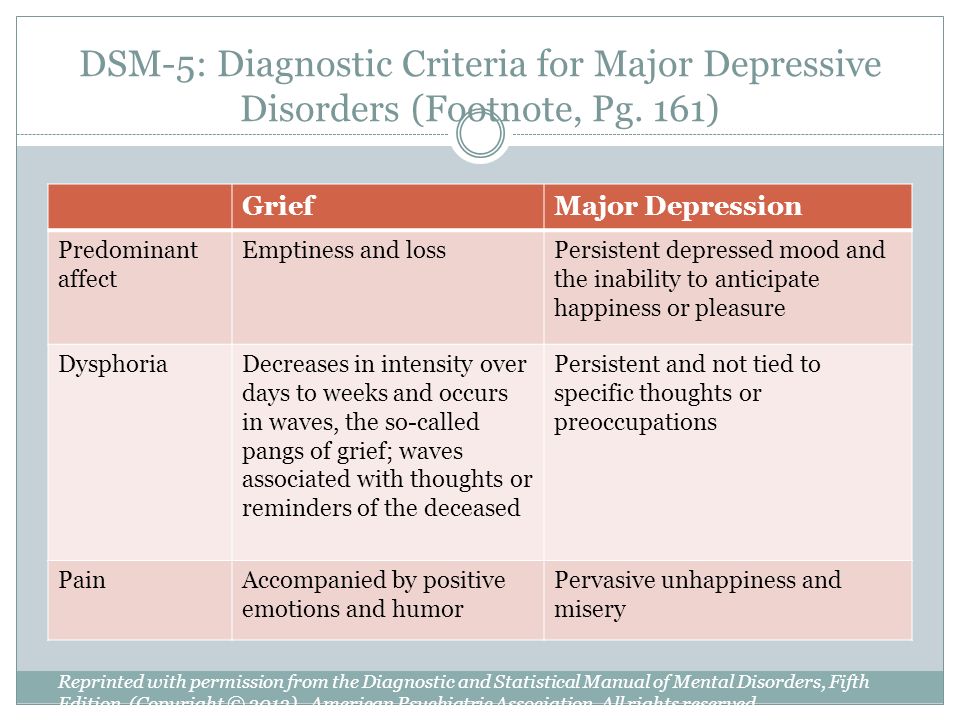
Criterion D Witting cognitive functioning and mood related to the traumatic event, which began after completion of the traumatic event (at least two of the 900,00077
1. Inability to recall important aspects of the traumatic event (mainly due to dissociative amnesia and not related to factors such as traumatic brain injury, alcohol or drug use).
2. Persistent and exaggeratedly distorted beliefs or expectations of a negative nature about oneself or the world around them (For example, "I am bad", "No one can be trusted", "The world is dangerous", "I have lost my soul forever", ""My nervous
3. Persistent and distorted beliefs about the cause or consequences of the traumatic event on which self-blame or blaming others is based. .
5. Marked significant decrease in interest or involvement in activities that were previously significant.
6. Feeling detached and alienated from other people.