Does weed cause psychosis
Is there a link between marijuana use and psychiatric disorders?
National Institutes of Health
Research Report
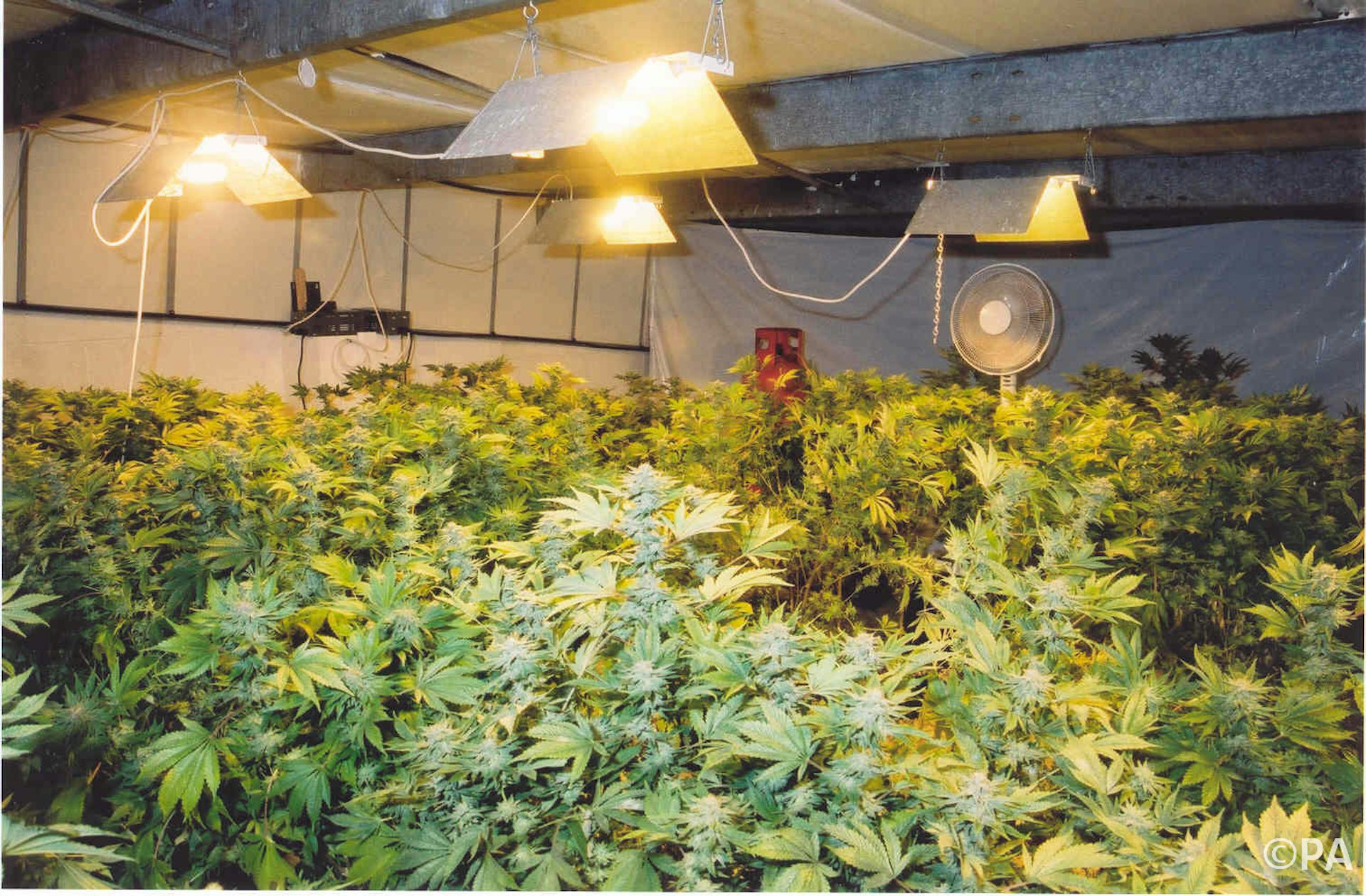
Several studies have linked marijuana use to increased risk for psychiatric disorders, including psychosis (schizophrenia), depression, anxiety, and substance use disorders, but whether and to what extent it actually causes these conditions is not always easy to determine.32 Recent research suggests that smoking high-potency marijuana every day could increase the chances of developing psychosis by nearly five times compared to people who have never used marijuana.113 The amount of drug used, the age at first use, and genetic vulnerability have all been shown to influence this relationship. The strongest evidence to date concerns links between marijuana use and psychiatric disorders in those with a preexisting genetic or other vulnerability. 61
Research using longitudinal data from the National Epidemiological Survey on Alcohol and Related Conditions examined associations between marijuana use, mood and anxiety disorders, and substance use disorders. After adjusting for various confounding factors, no association between marijuana use and mood and anxiety disorders was found. The only significant associations were increased risk of alcohol use disorders, nicotine dependence, marijuana use disorder, and other drug use disorders.62
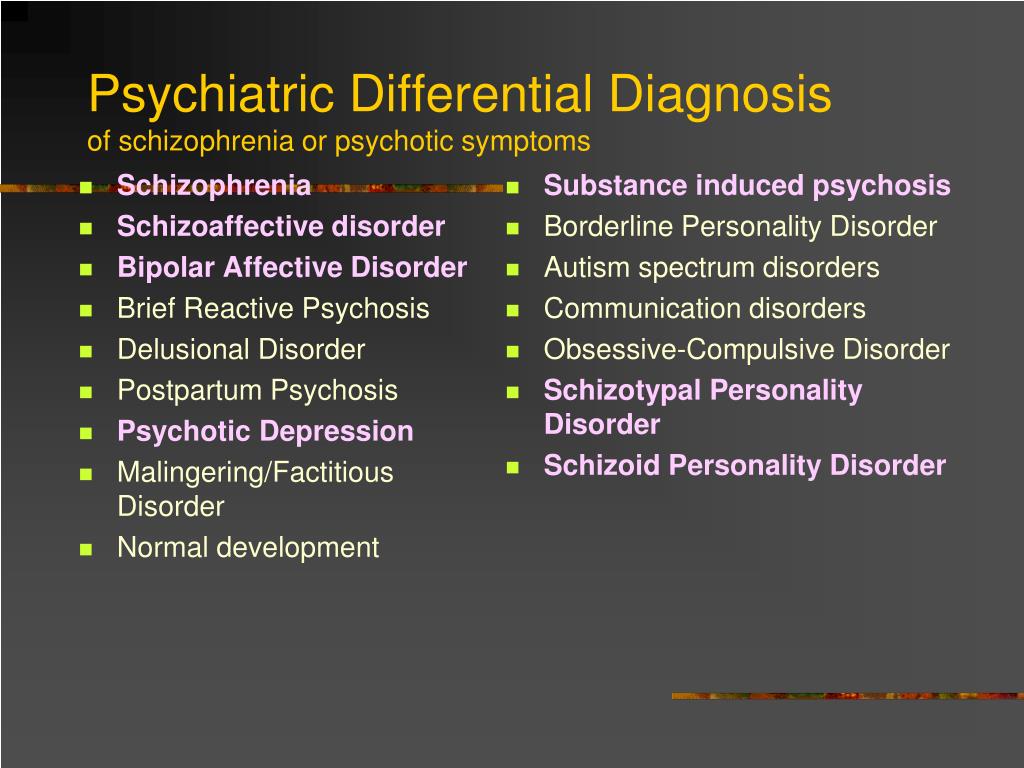
Recent research (see "AKT1 Gene Variations and Psychosis") has found that people who use marijuana and carry a specific variant of the AKT1 gene, which codes for an enzyme that affects dopamine signaling in the striatum, are at increased risk of developing psychosis. The striatum is an area of the brain that becomes activated and flooded with dopamine when certain stimuli are present. One study found that the risk of psychosis among those with this variant was seven times higher for those who used marijuana daily compared with those who used it infrequently or used none at all.63
Image
Source: Di Forti et al. Biol Psychiatry. 2012.
Whether adolescent marijuana use can contribute to developing psychosis later in adulthood appears to depend on whether a person already has a genetically based vulnerability to the disorder.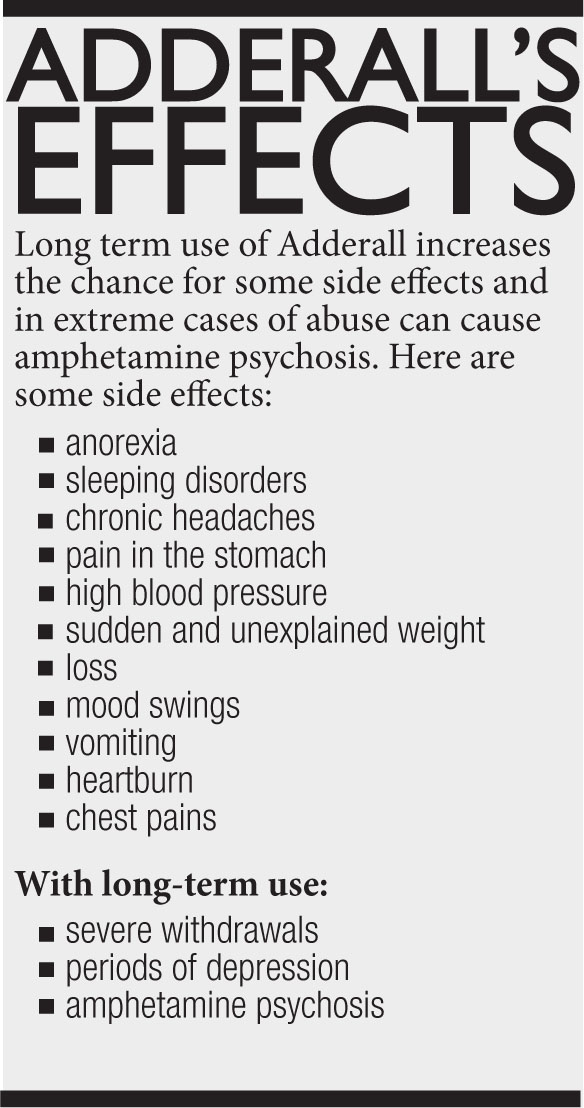 The AKT1 gene governs an enzyme that affects brain signaling involving the neurotransmitter dopamine. Altered dopamine signaling is known to be involved in schizophrenia. AKT1 can take one of three forms in a specific region of the gene implicated in susceptibility to schizophrenia: T/T, C/T, and C/C. Those who use marijuana daily (green bars) with the C/C variant have a seven times higher risk of developing psychosis than those who use it infrequently or use none at all. The risk for psychosis among those with the T/T variant was unaffected by whether they used marijuana.
The AKT1 gene governs an enzyme that affects brain signaling involving the neurotransmitter dopamine. Altered dopamine signaling is known to be involved in schizophrenia. AKT1 can take one of three forms in a specific region of the gene implicated in susceptibility to schizophrenia: T/T, C/T, and C/C. Those who use marijuana daily (green bars) with the C/C variant have a seven times higher risk of developing psychosis than those who use it infrequently or use none at all. The risk for psychosis among those with the T/T variant was unaffected by whether they used marijuana.Another study found an increased risk of psychosis among adults who had used marijuana in adolescence and also carried a specific variant of the gene for catechol-O-methyltransferase (COMT), an enzyme that degrades neurotransmitters such as dopamine and norepinephrine
64 (see "Genetic Variations in COMT Influences the Harmful Effects of Abused Drugs"). Marijuana use has also been shown to worsen the course of illness in patients who already have schizophrenia. As mentioned previously, marijuana can produce an acute psychotic reaction in non-schizophrenic people who use marijuana, especially at high doses, although this fades as the drug wears off.
As mentioned previously, marijuana can produce an acute psychotic reaction in non-schizophrenic people who use marijuana, especially at high doses, although this fades as the drug wears off.
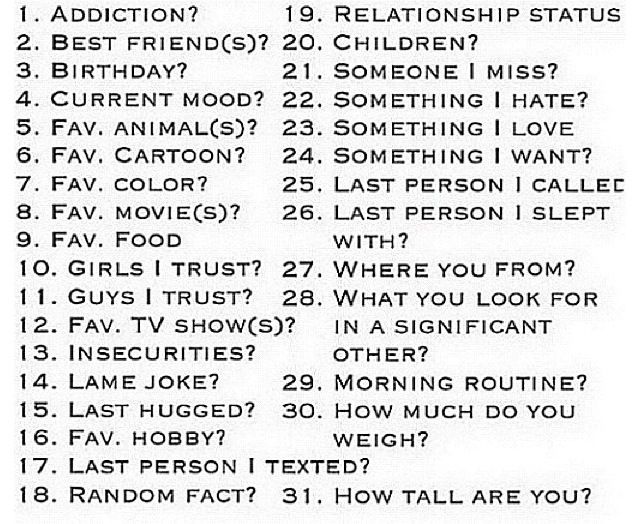
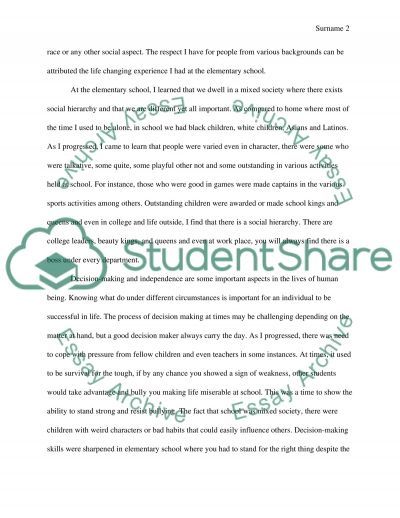
Image
Source: Di Forti et al. Biol Psychiatry. 2012.
The influence of adolescent marijuana use on adult psychosis is affected by genetic variables. This figure shows that variations in a gene can affect the likelihood of developing psychosis in adulthood following exposure to cannabis in adolescence. The COMT gene governs an enzyme that breaks down dopamine, a brain chemical involved in schizophrenia. It comes in two forms: "Met" and "Val." Individuals with one or two copies of the Val variant have a higher risk of developing schizophrenic-type disorders if they used cannabis during adolescence (dark bars). Those with only the Met variant were unaffected by cannabis use.Inconsistent and modest associations have been reported between marijuana use and suicidal thoughts and attempted suicide among teens.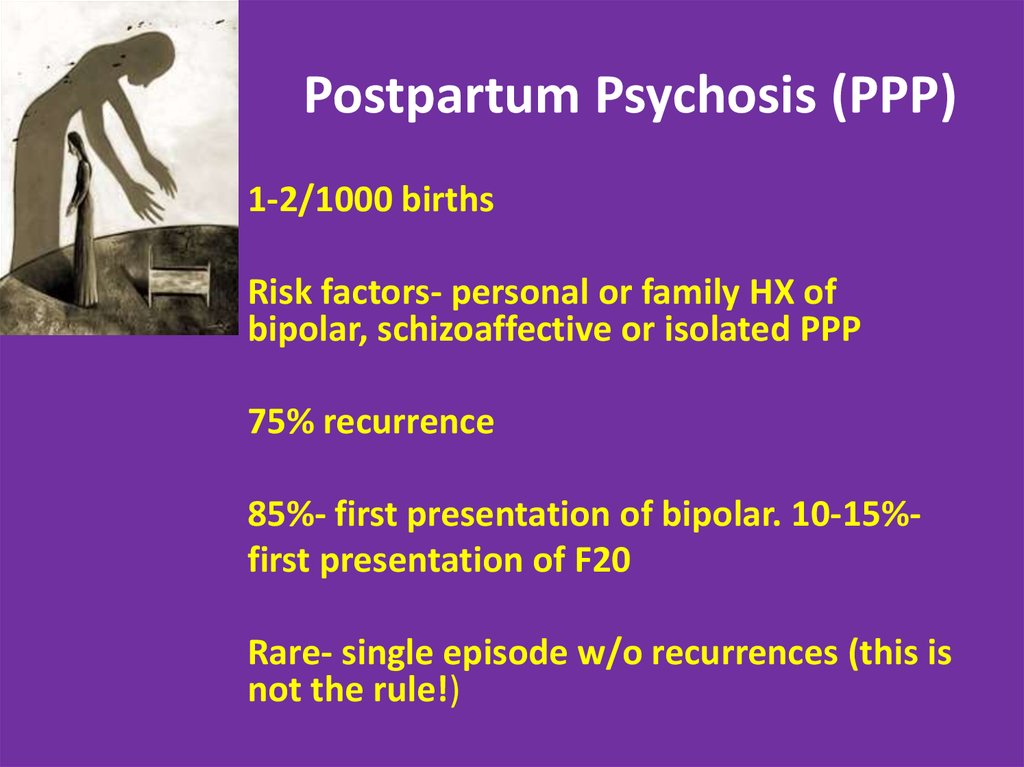 65,66 Marijuana has also been associated with an amotivational syndrome, defined as a diminished or absent drive to engage in typically rewarding activities. Because of the role of the endocannabinoid system in regulating mood and reward, it has been hypothesized that brain changes resulting from early use of marijuana may underlie these associations, but more research is needed to verify that such links exist and better understand them.
65,66 Marijuana has also been associated with an amotivational syndrome, defined as a diminished or absent drive to engage in typically rewarding activities. Because of the role of the endocannabinoid system in regulating mood and reward, it has been hypothesized that brain changes resulting from early use of marijuana may underlie these associations, but more research is needed to verify that such links exist and better understand them.
Image
Photo by ©getttyimages.com/Fuse
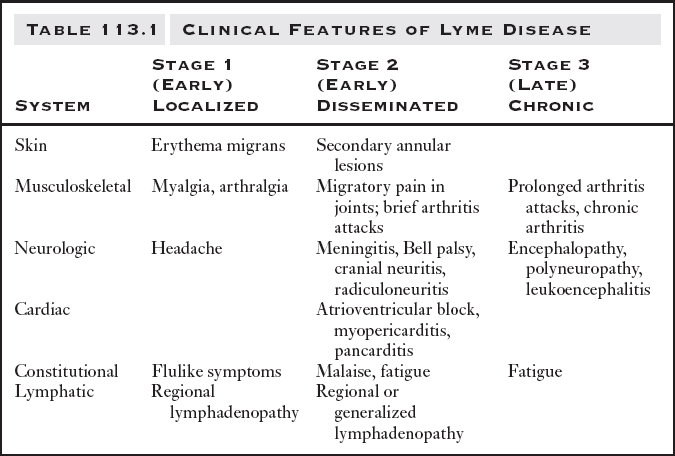
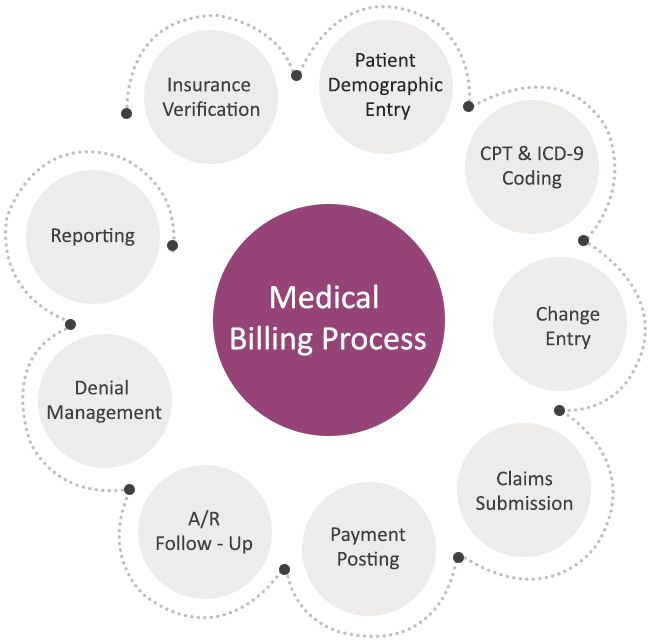
Acute (present during intoxication)
- Impaired short-term memory
- Impaired attention, judgment, and other cognitive functions
- Impaired coordination and balance
- Increased heart rate
- Anxiety, paranoia
- Psychosis (uncommon)
Persistent (lasting longer than intoxication, but may not be permanent)
- Impaired learning and coordination
- Sleep problems
Long-term (cumulative effects of repeated use)
- Potential for marijuana addiction
- Impairments in learning and memory with potential loss of IQ*
- Increased risk of chronic cough, bronchitis
- Increased risk of other drug and alcohol use disorders
- Increased risk of schizophrenia in people with genetic vulnerability**
*Loss of IQ among individuals with persistent marijuana use disorder who began using heavily during adolescence
**These are often reported co-occurring symptoms/disorders with chronic marijuana use.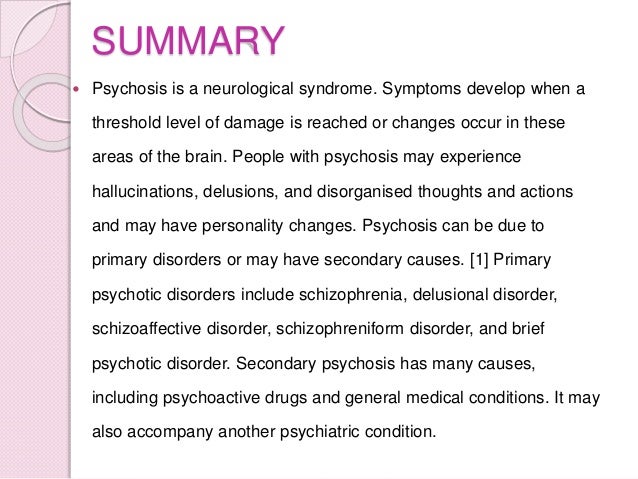 However, research has not yet determined whether marijuana is causal or just associated with these mental problems.
However, research has not yet determined whether marijuana is causal or just associated with these mental problems.
Cannabis and psychosis: Neurobiology - PMC
1. Varma LP. Cannabis psychosis. Indian J Psychiatry. 1972;14:241–55. [Google Scholar]
2. Baldacchino A, Blair H, Scherbaum N, Grosse-Vehne E, Riglietta M, Tidone L, et al. Drugs and Psychosis Project: A multi-centre European study on comorbidity. Drug Alcohol Rev. 2009;28:379–89. [PubMed] [Google Scholar]
3. Moore TH, Zammit S, Lingford-Hughes A, Barnes TR, Jones PB, Burke M, et al. annabis use and risk of psychotic or affective mental health outcomes: A systematic review. Lancet. 2007;370:319–28. [PubMed] [Google Scholar]
4. Chen CY, Lin KM. Health consequences of illegal drug use. Curr Opin Psychiatry. 2009;22:287–92. [PubMed] [Google Scholar]
5. Gregg L, Barrowlough C, Haddock G. Reasons for increased substance use in psychosis. Clin Psychol Rev. 2007;27:494–510. [PubMed] [Google Scholar]
Clin Psychol Rev. 2007;27:494–510. [PubMed] [Google Scholar]
6. Barrigón ML, Gurpegui M, Ruiz-Veguilla M, Diaz FJ, Anguita M, Sarramea F, et al. Temporal relationship of first-episode non-affective psychosis with cannabis use: A clinical verification of an epidemiological hypothesis. J Psychiatr Res. 2010;44:413–20. [PubMed] [Google Scholar]
7. de la Serna E, Mayoral M, Baeza I, Arango C, Andrés P, Bombin I, et al. Cognitive functioning in children and adolescents in their first episode of psychosis: Differences between previous cannabis users and nonusers. J Nerv Ment Dis. 2010;198:159–62. [PubMed] [Google Scholar]
8. Compton MT, Kelley ME, Ramsay CE, Pringle M, Goulding SM, Esterberg ML, et al. Association of pre-onset cannabis, alcohol, and tobacco use with age at onset of prodrome and age at onset of psychosis in first-episode patients. Am J Psychiatry. 2009;166:1251–7. [PMC free article] [PubMed] [Google Scholar]
9. Corcoran CM, Kimhy D, Stanford A, Khan S, Walsh J, Thompson J, et al.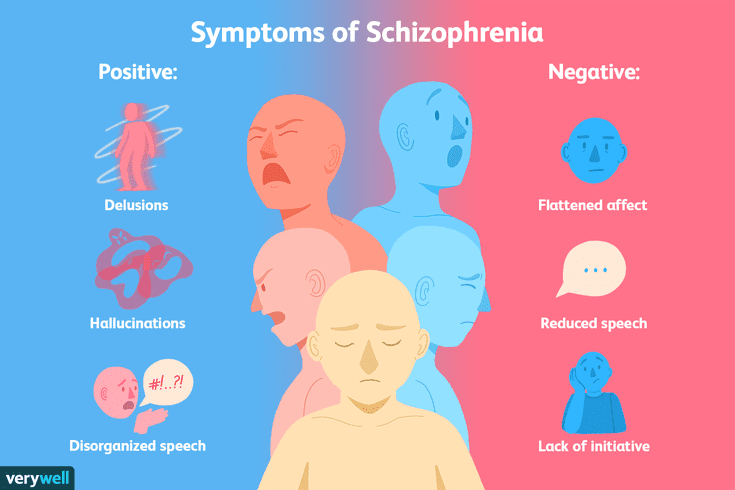 Temporal association ofcannabisuse with symptoms in individuals at clinical high risk for psychosis. Schizophr Res. 2008;106:286–93. [PMC free article] [PubMed] [Google Scholar]
Temporal association ofcannabisuse with symptoms in individuals at clinical high risk for psychosis. Schizophr Res. 2008;106:286–93. [PMC free article] [PubMed] [Google Scholar]
10. Sewell RA, Skosnik PD, Garcia-Sosa I, Ranganathan M, D’Souza DC. Behavioral, cognitive and psychophysiological effects of cannabinoids: Relevance to psychosis and schizophrenia. Rev Bras Psiquiatr. 2010;32(Suppl 1):S15–30. [PubMed] [Google Scholar]
11. Baker AL, Hides L, Lubman DI. Treatment of cannabis use among people with psychotic or depressive disorders: A systematic review. J Clin Psychiatry. 2010;71:247–54. [PubMed] [Google Scholar]
12. Winter-van Rossum I, Boomsma MM, Tenback DE, Reed C, van Os J. The influence ofcannabison the course of bipolar disorder: A longitudinal analysis. Tijdschr Psychiatr. 2010;52:287–98. [PubMed] [Google Scholar]
13. Schubart CD, Sommer IE, van Gastel WA, Goetgebuer RL, Kahn RS, Boks MP. Cannabis with high cannabidiol content is associated with fewerpsychoticexperiences. Schizophr Res. 2011;130:216–21. [PubMed] [Google Scholar]
Schizophr Res. 2011;130:216–21. [PubMed] [Google Scholar]
14. Wiley JL, Kendler SH, Burston JJ, Howard DR, Selley DE, Sim-Selley LJ. Antipsychotic-induced alterations in CB1 receptor-mediated G-protein signaling and in vivo pharmacology in rats. Neuropharmacology. 2008;55:1183–90. [PMC free article] [PubMed] [Google Scholar]
15. Morrison PD, Zois V, McKeown DA, Lee TD, Holt DW, Powell JF, et al. The acute effects of synthetic intravenous Delts9-tetrahydrocannabinol on psychosis, mood and cognitive functioning. Psychol Med. 2009;31:1607–16. [PubMed] [Google Scholar]
16. D’Souza DC, Perry E, MacDougall L, Ammerman Y, Cooper T, Wu YT, et al. The psychotomimetic effects of intravenous delta-9-tetrahydrocannabinol in healthy individuals: Implications for psychosis. Neuropsychopharmacology. 2004;29:1558–72. [PubMed] [Google Scholar]
17. D’Souza DC, Sewell RA, Ranganathan M. Cannabis and psychosis/schizophrenia: Human studies. Eur Arch Psychiatry Clin Neurosci. 2009;259:413–31. [PMC free article] [PubMed] [Google Scholar]
2009;259:413–31. [PMC free article] [PubMed] [Google Scholar]
18. Le BecPY, Fatséas M, Denis C, Lavie E, Auriacombe M. Cannabis and psychosis: Search of a causal link through a critical and systematic review. Encephale. 2009;35:377–85. [PubMed] [Google Scholar]
19. McLaren JA, Silins E, Hutchinson D, Mattick RP, Hall W. Assessing evidence for a causal link between cannabis and psychosis: A review of cohort studies. Int J Drug Policy. 2010;21:10–9. [PubMed] [Google Scholar]
20. Kuepper R, van Os J, Lieb R, Wittchen HU, Höfler M, Henquet C. Continued cannabis use and risk of incidence and persistence of psychotic symptoms: 10 year follow-up cohort study. BMJ. 2011;342:d738. [PMC free article] [PubMed] [Google Scholar]
21. Malik AR, D’Souza DC. Gone to pot: The association between cannabis and psychosis. Psychiatric Times. 2006;23 [Google Scholar]
22. Hambrecht M, Häfner H. Cannabis, vulnerability, and the onset of schizophrenia: An epidemiological perspective. Aust N Z J Psychiatry. 2000;34:468–75. [PubMed] [Google Scholar]
Aust N Z J Psychiatry. 2000;34:468–75. [PubMed] [Google Scholar]
23. Hall W, Degenhardt L, Teesson M. Cannabis use and psychotic disorders: An update. Drug Alcohol Rev. 2004;23:433–43. [PubMed] [Google Scholar]
24. Andréasson S, Allebeck P, Rydberg U. Schizophrenia in users and nonusers of cannabis: A longitudinal study in Stockholm County. Acta Psychiatr Scand. 1989;79:505–10. [PubMed] [Google Scholar]
25. van Os J, Bak M, Hanssen M, Bijl RV, de Graaf R, Verdoux H. Cannabis use and psychosis: A longitudinal population-based study. Am J Epidemiol. 2002;156:319–27. [PubMed] [Google Scholar]
26. Verdoux H, Gindre C, Sorbara F, Tournier M, Swendsen JD. Effects of cannabis and psychosis vulnerability in daily life: An experience sampling test study. Psychol Med. 2003;33:23–32. [PubMed] [Google Scholar]
27. Mathers DC, Ghodse AH. Cannabis and psychotic illness. Br J Psychiatry. 1992;161:648–53. [PubMed] [Google Scholar]
28. Wilson RI, Nicoll RA. Endocannabinoid signaling in the brain.![]() Science. 2002;296:678–82. [PubMed] [Google Scholar]
Science. 2002;296:678–82. [PubMed] [Google Scholar]
29. Degenhardt L. The link between cannabis use and psychosis: Furthering the debate. Psychol Med. 2003;33:3–6. [PubMed] [Google Scholar]
30. Henquet C, Di Forti M, Morrison P, Kuepper R, Murray RM. Gene-environment interplay between cannabis and psychosis. Schizophr Bull. 2008;34:1111–21. [PMC free article] [PubMed] [Google Scholar]
31. Mechoulam R, Gaoni Y. A total synthesis of DL-delta-1-tetrahydrocannabinol, the active constituent of hashish. J Am Chem Soc. 1965;87:3273–5. [PubMed] [Google Scholar]
32. Manrique-Garcia E, Zammit S, Dalman C, Hemmingsson T, Andreasson S, Allebeck P. Cannabis, schizophrenia and other non-affective psychoses: 35 years of follow-up of a population-based cohort. Psychol Med. 2012;42:1321–8. [PubMed] [Google Scholar]
33. Malone DT, Hill MN, Rubino T. Adolescent cannabis use and psychosis: Epidemiology and neurodevelopment models. Br J Pharmacol. 2010;160:511–22. [PMC free article] [PubMed] [Google Scholar]
34. Rubino T, Parolaro D. Long lasting consequences of cannabis exposure in adolescence. Mol Cell Endocrinol. 2008;286(1-2 Suppl 1):S108–13. [PubMed] [Google Scholar]
Rubino T, Parolaro D. Long lasting consequences of cannabis exposure in adolescence. Mol Cell Endocrinol. 2008;286(1-2 Suppl 1):S108–13. [PubMed] [Google Scholar]
35. Vigano D, Guidali C, Petrosino S, Realini N, Rubino T, Di Marzo V, et al. Involvement of the endocannabinoid system in phencyclidine-induced cognitive deficits modelling schizophrenia. Int J Neuropsychopharmacol. 2009;12:599–614. [PubMed] [Google Scholar]
36. Bhattacharyya S, Morrison PD, Fusar-Poli P, Martin-Santos R, Borgwardt S, Winton-Brown T, et al. Opposite effects of delta-9-tetrahydrocannabinol and cannabidiol on human brain function and psychopathology. Neuropsychopharmacology. 2010;35:764–74. [PMC free article] [PubMed] [Google Scholar]
37. Malone DT, Jongejan D, Taylor DA. Cannabidiol reverses the reduction in social interaction produced by low dose Delta (9)-tetrahydrocannabinol in rats. Pharmacol Biochem Behav. 2009;93:91–6. [PubMed] [Google Scholar]
38. DeRosse P, Kaplan A, Burdick KE, Lencz T, Malhotra AK. Cannabis use disorders in schizophrenia: Effects on cognition and symptoms. Schizophr Res. 2010;120:95–100. [PMC free article] [PubMed] [Google Scholar]
Cannabis use disorders in schizophrenia: Effects on cognition and symptoms. Schizophr Res. 2010;120:95–100. [PMC free article] [PubMed] [Google Scholar]
39. Hernández ML, García-Gil L, Berrendero F, Ramos JA, Fernández-Ruiz JJ. Delta 9-Tetrahydrocannabinol increases activity of tyrosine hydroxylase in cultured fetal mesencephalic neurons. J Mol Neurosci. 1997;8:83–91. [PubMed] [Google Scholar]
40. El Marroun H, Tiemeier H, Steegers EA, Roos-Hesselink JW, Jaddoe VW, Hofman A, et al. A prospective study on intrauterine cannabis exposure and fetal blood flow. Early Hum Dev. 2010;86:231–6. [PubMed] [Google Scholar]
41. Lafourcade M, Elezgarai I, Mato S, Bakiri Y, Grandes P, Manzoni OJ. Molecular components and functions of the endocannabinoid system in mouse prefrontal cortex. PLoS One. 2007;2:e709. [PMC free article] [PubMed] [Google Scholar]
42. Wang X, Dow-Edwards D, Anderson V, Minkoff H, Hurd YL. In utero marijuana exposure associated with abnormal amygdala dopamine D2 gene expression in the human fetus. Biol Psychiatry. 2004;56:909–15. [PubMed] [Google Scholar]
Biol Psychiatry. 2004;56:909–15. [PubMed] [Google Scholar]
43. Harkany T, Guzmán M, Galve-Roperh I, Berghuis P, Devi LA, Mackie K. The emerging functions of endocannabinoid signalling during CNS development. Trends Pharmacol Sci. 2007;28:83–92. [PubMed] [Google Scholar]
44. Huizink AC, Mulder EJ. Maternal smoking, drinking or cannabis use during pregnancy and neurobehavioral and cognitive functioning in human offspring. Neurosci Biobehav Rev. 2006;30:24–41. [PubMed] [Google Scholar]
45. Harkany T, Keimpema E, Barabás K, Mulder J. Endocannabinoid functions controlling neuronal specification during brain development. Mol Cell Endocrinol. 2008;286(1-2 Suppl 1):S84–90. [PubMed] [Google Scholar]
46. Stokes PR, Egerton A, Watson B, Reid A, Lappin J, Howes OD, et al. History of cannabis use is not associated with alterations in striatal dopamine D2/D3 receptor availability. J Psychopharmacol. 2012;26:144–9. [PubMed] [Google Scholar]
47. Solowij N, Michie PT. Cannabis and cognitive dysfunction: Parallels with endophenotypes of schizophrenia? J Psychiatry Neurosci. 2007;32:30–52. [PMC free article] [PubMed] [Google Scholar]
2007;32:30–52. [PMC free article] [PubMed] [Google Scholar]
48. Hurd YL, Wang X, Anderson V, Beck O, Minkoff H, Dow-Edwards D. Marijuana impairs growth in mid-gestation fetuses. Neurotoxicol Teratol. 2005;27:221–9. [PubMed] [Google Scholar]
49. Puighermanal E, Marsicano G, Busquets-Garcia A, Lutz B, Maldonado R, Ozaita A. Cannabinoid modulation of hippocampal long-term memory is mediated by mTOR signaling. Nat Neurosci. 2009;12:1152–8. [PubMed] [Google Scholar]
50. Katona I, Freund TF. Endocannabinoid signaling as a synaptic circuit breaker in neurological disease. Nat Med. 2008;14:923–30. [PubMed] [Google Scholar]
51. Arseneault L, Cannon M, Poulton R, Murray R, Caspi A, Moffitt TE. Cannabis use in adolescence and risk for adult psychosis: Longitudinal prospective study. BMJ. 2002;325:1212–3. [PMC free article] [PubMed] [Google Scholar]
52. Dekker N, Schmitz N, Peters BD, van Amelsvoort TA, Linszen DH, de Haan L. Cannabis use and callosal white matter structure and integrity in recent-onset schizophrenia. Psychiatry Res. 2010;181:51–6. [PubMed] [Google Scholar]
Psychiatry Res. 2010;181:51–6. [PubMed] [Google Scholar]
53. Campolongo P, Trezza V, Ratano P, Palmery M, Cuomo V. Developmental consequences of perinatal cannabis exposure: Behavioral and neuroendocrine effects in adult rodents. Psychopharmacology (Berl) 2011;214:5–15. [PMC free article] [PubMed] [Google Scholar]
54. Zammit S, Thomas K, Thompson A, Horwood J, Menezes P, Gunnell D, et al. Maternal tobacco, cannabis and alcohol use during pregnancy and risk of adolescent psychotic symptoms in offspring. Br J Psychiatry. 2009;195:294–300. [PubMed] [Google Scholar]
55. Fadda P, Robinson L, Fratta W, Pertwee RG, Riedel G. Differential effects of THC- or CBD-rich cannabis extracts on working memory in rats. Neuropharmacology. 2004;47:1170–9. [PubMed] [Google Scholar]
56. Williamson S, Jackson L, Skeoch C, Azzim G, Anderson R. Determination of the prevalence of drug misuse by meconium analysis. Arch Dis Child Fetal Neonatal Ed. 2006;91:F291–2. [PMC free article] [PubMed] [Google Scholar]
57. Jutras-Aswad D, DiNieri JA, Harkany T, Hurd YL. Neurobiological consequences of maternal cannabis on human fetal development and its neuropsychiatric outcome. Eur Arch Psychiatry Clin Neurosci. 2009;259:395–412. [PubMed] [Google Scholar]
Jutras-Aswad D, DiNieri JA, Harkany T, Hurd YL. Neurobiological consequences of maternal cannabis on human fetal development and its neuropsychiatric outcome. Eur Arch Psychiatry Clin Neurosci. 2009;259:395–412. [PubMed] [Google Scholar]
58. Zavitsanou K, Wang H, Dalton VS, Nguyen V. Cannabinoid administration increases 5HT1A receptor binding and mRNA expression in the hippocampus of adult but not adolescent rats. Neuroscience. 2010;169:315–24. [PubMed] [Google Scholar]
59. Verweij KJ, Zietsch BP, Lynskey MT, Medland SE, Neale MC, Martin NG, et al. Genetic and environmental influences on cannabis use initiation and problematic use: A meta-analysis of twin studies. Addiction. 2010;105:417–30. [PMC free article] [PubMed] [Google Scholar]
60. Hartman CA, Hopfer CJ, Haberstick B, Rhee SH, Crowley TJ, Corley RP, et al. The association between cannabinoid receptor 1 gene (CNR1) and cannabis dependence symptoms in adolescents and young adults. Drug Alcohol Depend. 2009;104:11–6. [PMC free article] [PubMed] [Google Scholar]
[PMC free article] [PubMed] [Google Scholar]
61. Huizink AC, Levälahti E, Korhonen T, Dick DM, Pulkkinen L, Rose RJ, et al. Tobacco, cannabis, and other illicit drug use among Finnish adolescent twins: Causal relationship or correlated liabilities? J Stud Alcohol Drugs. 2010;71:5–14. [PMC free article] [PubMed] [Google Scholar]
62. Jentsch JD, Andrusiak E, Tran A, Bowers MB, Roth RH. Delta9-tetrahydrocannabinol increases prefrontal cortical catecholaminergic utilization and impairs spatial working memory in the rat: Blockade of dopaminergic effects with HA966. Neuropsychopharmacology. 1997;16:426–32. [PubMed] [Google Scholar]
63. McGrath J, Welham J, Scott J, Varghese D, Degenhardt L, Hayatbakhsh MR, et al. Association between cannabis use and psychosis-related outcomes using sibling pair analysis in a cohort of young adults. Arch Gen Psychiatry. 2010;67:440–7. [PubMed] [Google Scholar]
64. Pelayo-Terán JM, Pérez-Iglesias R, Mata I, Carrasco-Marín E, Vázquez-Barquero JL, Crespo-Facorro B.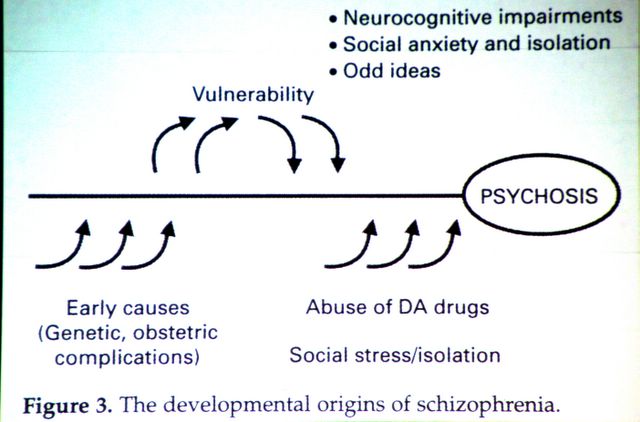 Catechol-O-Methyltransferase (COMT) Val158Met variations and cannabis use in first-episode non-affective psychosis: Clinical-onset implications. Psychiatry Res. 2010;179:291–6. [PubMed] [Google Scholar]
Catechol-O-Methyltransferase (COMT) Val158Met variations and cannabis use in first-episode non-affective psychosis: Clinical-onset implications. Psychiatry Res. 2010;179:291–6. [PubMed] [Google Scholar]
65. Bhattacharyya S, Crippa JA, Martin-Santos R, Winton-Brown T, Fusar-Poli P. Imaging the neural effects of cannabinoids: Current status and future opportunities for psychopharmacology. Curr Pharm Des. 2009;15:2603–14. [PubMed] [Google Scholar]
66. Jager G, Block RI, Luijten M, Ramsey NF. Cannabis use and memory brain function in adolescent boys: A cross-sectional multicenter functional magnetic resonance imaging study. J Am Acad Child Adolesc Psychiatry. 2010;49:561–72. [PMC free article] [PubMed] [Google Scholar]
67. Delisi LE, Bertisch HC, Szulc KU, Majcher M, Brown K, Bappal A, et al. A preliminary DTI study showing no brain structural change associated with adolescent cannabis use. Harm Reduct J. 2006;3:17. [PMC free article] [PubMed] [Google Scholar]
68. Bolla KI, Eldreth DA, Matochik JA, Cadet JL.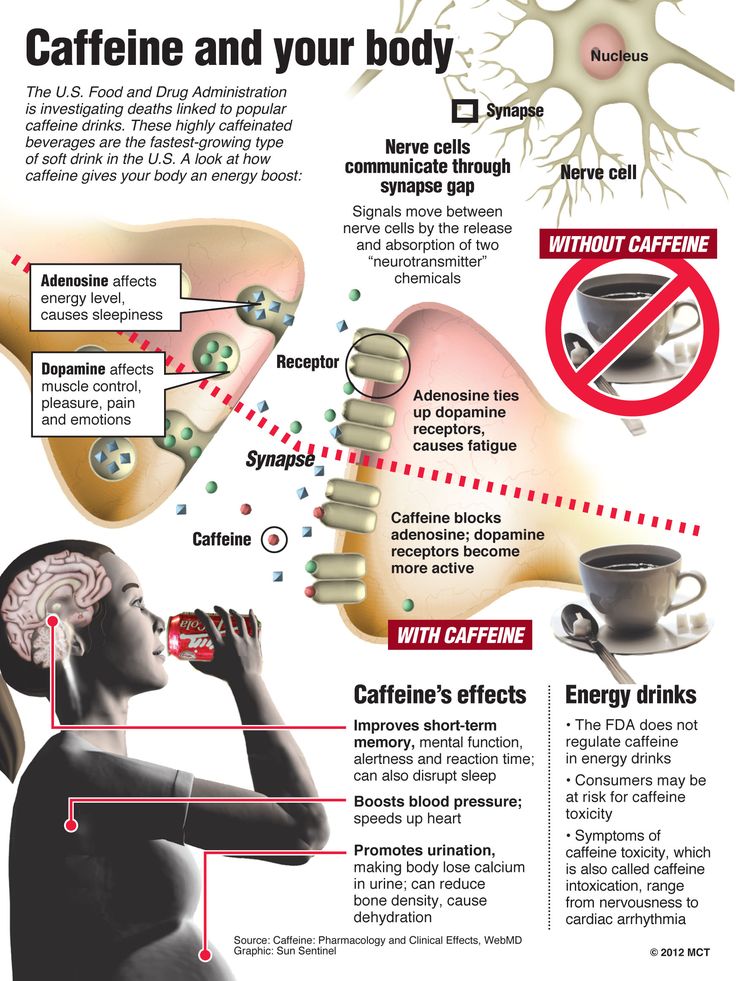 Neural substrates of faulty decision-making in abstinent marijuana users. Euroimage. 2005;26:480–92. [PubMed] [Google Scholar]
Neural substrates of faulty decision-making in abstinent marijuana users. Euroimage. 2005;26:480–92. [PubMed] [Google Scholar]
69. Arnone D, Barrick TR, Chengappa S, Mackay CE, Clark CA, Abou-Saleh MT. Corpus callosum damage in heavy marijuana use: Preliminary evidence from diffusion tensor tractography and tract-based spatial statistics. Neuroimage. 2008;41:1067–74. [PubMed] [Google Scholar]
70. van Os J, Kenis G, Rutten BP. The environment and schizophrenia. Nature. 2010;468:203–12. [PubMed] [Google Scholar]
71. Yücel M, Solowij N, Respondek C, Whittle S, Fornito A, Pantelis C, et al. Regional brain abnormalities associated with long-term heavy cannabis use. Arch Gen Psychiatry. 2008;65:694–701. [PubMed] [Google Scholar]
72. Peters BD, Blaas J, de Haan L. Diffusion tensor imaging in the early phase of schizophrenia: What have we learned? J Psychiatr Res. 2010;44:993–1004. [PubMed] [Google Scholar]
73. Pierre JM. Psychosis associated with medical marijuana: Risk vs.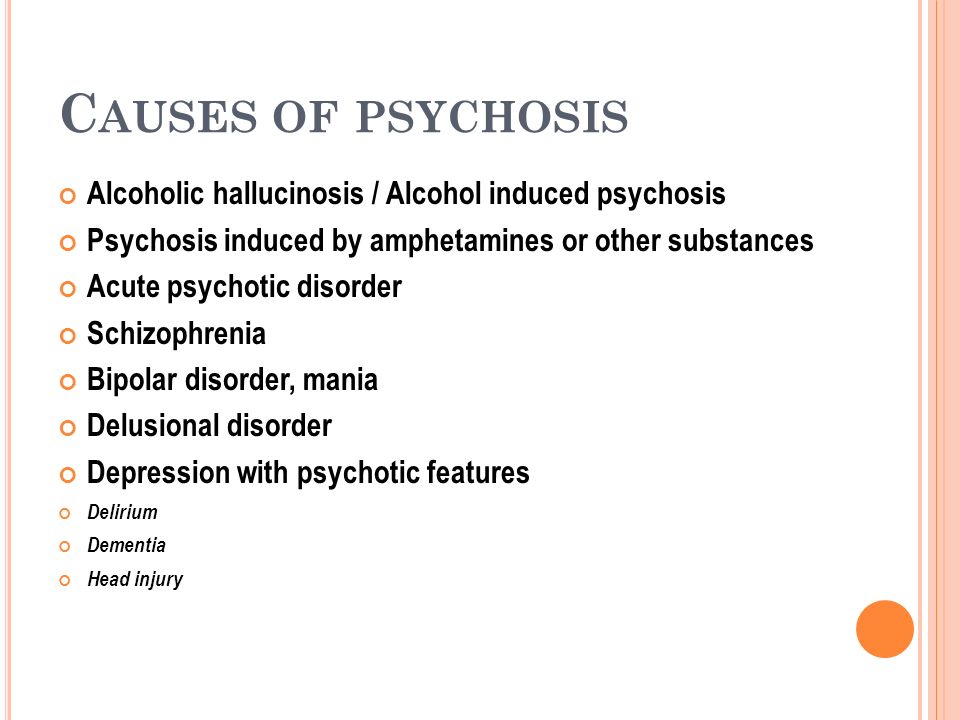 benefits of medicinal cannabis use. Am J Psychiatry. 2010;167:598–9. [PubMed] [Google Scholar]
benefits of medicinal cannabis use. Am J Psychiatry. 2010;167:598–9. [PubMed] [Google Scholar]
74. Kuepper R, Morrison PD. Does dopamine mediate the psychosis-inducing effects of cannabis. A review and integration of findings across disciplines? Schizophr Res. 2010;121:107–17. [PubMed] [Google Scholar]
75. Jockers-Scherübl MC, Rentzsch J, Danker-Hopfe H, Radzei N, Schürer F, Bahri S, et al. Adequate antipsychotic treatment normalizes serum nerve growth factor concentrations in schizophrenia with and without cannabis or additional substance abuse. Neurosci Lett. 2006;400:262–6. [PubMed] [Google Scholar]
76. Stefanis NC, Delespaul P, Henquet C, Bakoula C, Stefanis CN, Van Os J. Early adolescent cannabis exposure and positive and negative dimensions of psychosis. Addiction. 2004;99:1333–41. [PubMed] [Google Scholar]
77. Martin-Santos R, Fagundo AB, Crippa JA, Atakan Z, Bhattacharyya S, Allen P, et al. Neuroimaging in cannabis use: A systematic review of the literature. Psychol Med. 2010;40:383–98. [PubMed] [Google Scholar]
Psychol Med. 2010;40:383–98. [PubMed] [Google Scholar]
78. Linszen D, van Amelsvoort T. Cannabis and psychosis: An update on course and biological plausible mechanisms. Curr Opin Psychiatry. 2007;20:116–20. [PubMed] [Google Scholar]
79. Fadda P, Scherma M, Spano MS, Salis P, Melis V, Fattore L, et al. Cannabinoid self-administration increases dopamine release in the nucleus accumbens. Neuroreport. 2006;17:1629–32. [PubMed] [Google Scholar]
80. Bossong MG, van Berckel BN, Boellaard R, Zuurman L, Schuit RC, Windhorst AD, et al. Delta9-tetrahydrocannabinol induces dopamine release in the human striatum. Neuropsychopharmacology. 2009;34:759–66. [PubMed] [Google Scholar]
81. Welch KA, McIntosh AM, Job DE, Whalley HC, Moorhead TW, Hall J, et al. The impact of substance use on brain structure in people at high risk of developing schizophrenia. Schizophr Bull. 2011;37:1066–76. [PMC free article] [PubMed] [Google Scholar]
82. Battisti RA, Roodenrys S, Johnstone SJ, Respondek C, Hermens DF, Solowij N. Chronic use of cannabis and poor neural efficiency in verbal memory ability. Psychopharmacology (Berl) 2010;209:319–30. [PubMed] [Google Scholar]
Chronic use of cannabis and poor neural efficiency in verbal memory ability. Psychopharmacology (Berl) 2010;209:319–30. [PubMed] [Google Scholar]
83. Shrivastava A, Johnston M, Tsuang M. Cannabis use and cognitive dysfunction. Indian J Psychiatry. 2011;53:187–91. [PMC free article] [PubMed] [Google Scholar]
84. Cougnard A, Marcelis M, Myin-Germeys I, De Graaf R, Vollebergh W, Krabbendam L, et al. Does normal developmental expression of psychosis combine with environmental risk to cause persistence of psychosis. A psychosis proneness-persistence model? Psychol Med. 2007;37:513–27. [PubMed] [Google Scholar]
85. Hayatbakhsh MR, Najman JM, Jamrozik K, Mamun AA, O’Callaghan MJ, Williams GM. Childhood sexual abuse and cannabis use in early adulthood: Findings from an Australian birth cohort study. Arch Sex Behav. 2009;38:135–42. [PubMed] [Google Scholar]
86. Harley M, Kelleher I, Clarke M, Lynch F, Arseneault L, Connor D, et al. Cannabis use and childhood trauma interacts additively to increase the risk of psychotic symptoms in adolescence. Psychol Med. 2010;40:1627–34. [PubMed] [Google Scholar]
Psychol Med. 2010;40:1627–34. [PubMed] [Google Scholar]
87. Kelly BD, O’Callaghan E, Waddington JL, Feeney L, Browne S, Scully PJ, et al. Schizophrenia and the city: A review of literature and prospective study of psychosis and urbanicity in Ireland. Schizophr Res. 2010;116:75–89. [PubMed] [Google Scholar]
88. Dekker N, Linszen DH, De Haan L. Reasons for cannabis use and effects of cannabis use as reported by patients with psychotic disorders. Psychopathology. 2009;42:350–60. [PubMed] [Google Scholar]
89. Roffman JL, Weiss AP, Goff DC, Rauch SL, Weinberger DR. Neuroimaging-genetic paradigms: A new approach to investigate the pathophysiology and treatment of cognitive deficits in schizophrenia. Harv Rev Psychiatry. 2006;14:78–91. [PubMed] [Google Scholar]
90. Zammit S, Allebeck P, Andreasson S, Lundberg I, Lewis G. Self reported cannabis use as a risk factor for schizophrenia in Swedish conscripts of 1969: Historical cohort study. BMJ. 2002;325:1199. [PMC free article] [PubMed] [Google Scholar]
91. Rodríguez de Fonseca F, Cebeira M, Fernández-Ruiz JJ, Navarro M, Ramos JA. Effects of pre- and perinatal exposure to hashish extract on the ontogeny of brain dopaminergic neurons. Neuroscience. 1991;43:713–23. [PubMed] [Google Scholar]
Rodríguez de Fonseca F, Cebeira M, Fernández-Ruiz JJ, Navarro M, Ramos JA. Effects of pre- and perinatal exposure to hashish extract on the ontogeny of brain dopaminergic neurons. Neuroscience. 1991;43:713–23. [PubMed] [Google Scholar]
92. Ellgren M, Artmann A, Tkalych O, Gupta A, Hansen HS, Hansen SH, et al. Dynamic changes of the endogenous cannabinoid and opioid mesocorticolimbic systems during adolescence: THC effects. Eur Neuropsychopharmacol. 2008;18:826–34. [PMC free article] [PubMed] [Google Scholar]
How marijuana affects mental health and is it possible for people with mental disorders to smoke - Knife
Scientists warn of an increased risk of developing severe mental disorders such as psychosis, mania and even paranoid schizophrenia. At the same time, other researchers believe that it is too early to talk about a causal relationship, and the brain of heavy smokers is completely restored in just a month after the start. There are still others who even suggest using weed for the treatment of mental disorders. We understand what to fear.
We understand what to fear.
How marijuana affects the brain
Marijuana is the most widespread drug and the fourth most common way to slightly poison your body (immediately after alcohol, tobacco and coffee). Its effect on the body is complex: the active substances mj do not directly disrupt its work, but indirectly affect many vital processes.
Cannabis resin contains more than 80 active substances (cannabinoids), but the characteristic effect of smoking is caused by a combination of two main ones, the action of which is opposite.
1. Tetrahydrocannabinol ( THC )
Causes euphoria, revitalization and pleasant excitement, and also increases anxiety, restlessness and agitation.
2. Cannabidiol (CBD)
Has an inhibitory effect, reduces anxiety, calms.
The interaction of these two substances explains the excitatory effect from small doses (THC is a more active substance) and the subsequent inhibitory effect from large doses (CBD is larger in volume).
Cannabinoids simultaneously affect several parts of the brain and processes in the body:
- the limbic system, which is responsible for emotions, which can cause both euphoria and fear;
- the hippocampus that controls memory and attention: memory becomes weaker, attention becomes scattered, thinking becomes chaotic. Consumers may describe these sensations as intuition and insight, but in reality it is a chaotic wandering of thoughts and emotions;
- the prefrontal cortex of the brain, which begins to react sharply to external sensations: sounds, colors seem brighter;
- affect the feeling of hunger, increasing appetite;
- enhance the release of dopamine, which explains positive emotions.
Experiments on mice described the "popcorn effect": under the influence of marijuana, nimble rodents became quiet and lethargic. But at the same time, their nerves were overexcited: they literally bounced in place from sounds and touches.

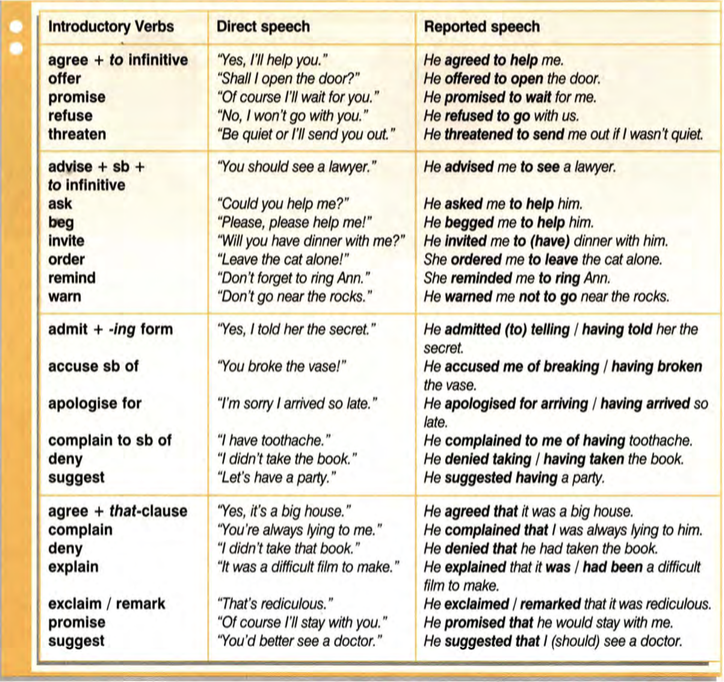
In different plant varieties, the content of THC varies significantly: from 1% to 20%. In some, it is so high that it can provoke a real psychosis. The average buyer, of course, is usually not aware of the specifics of the chemical composition. On average, the joints that were smoked in the hippie era are weaker than those sold now. For example, a popular variety called "skunk": it is grown in greenhouses or hydroponically, it acts on the brain quickly and, along with euphoria, can cause nervousness, panic attacks and vomiting.
Is there an addiction to marijuana
Contrary to popular belief, there is an addiction to cannabis. But the risk of its development is lower than from hard drugs, tobacco or alcohol. Marijuana causes addiction in about 9% of users (for alcohol and cocaine users, this risk is higher, 15%). For those who consume several times a week, the risk of addiction reaches 30%.
In the US, marijuana addiction is listed as a mental disorder and affects more than four million people, and in England there are hotlines and support groups for addicts - you can check yourself right now, answering 12 questions about marijuana use.

The state of the addict is described as a "motivational syndrome": weakening and slowing down of mental abilities, decreased interest in the outside world, passivity, lack of ambition and motivation, fatigue, shaky mood. But scientists are still arguing whether such a “vegetable” state is caused by years of abuse, or by an overly relaxed lifestyle itself.
An experiment with students (volunteers smoked 11 joints a day and were still paid for it) showed that their learning abilities recovered when the experiment ended. So far, no irreversible changes in the brain directly caused by marijuana have been identified. Science says that if you quit, on average, after a month, mental abilities will return to normal. But this is not accurate: research is ongoing, and there is already evidence (still requiring clarification) that some consumers, even months later, are less able to make informed decisions and are more prone to risk and impulsivity.
Despite rumors, there is a withdrawal syndrome when using marijuana: a person on withdrawal may lose appetite, experience nausea, sweating, restless sleep with nightmares, emotional swings.
What negative effects are observed when using marijuana
The effects of marijuana are very individual and depend not only on the type of grass, but also on the reactions of a particular organism. So it is almost impossible to predict it in advance.
In various studies, from 5 to 20% of mj users experienced panic attacks, anxiety, depression, obsessive thoughts, loss of energy, apathy.
A survey in a community of young people with mental health problems found that almost 15% of participants (out of 120 respondents) admitted to experiencing negative effects from smoking weed, ranging from irritability to panic attacks.
J: “Smoked a couple of times to relieve depression and seemed to help. But then, against the background of use, anxiety began to go off scale, up to painful spasms from fear, so I don’t want to continue the experiments.”
He also showed that the "pipe" is indeed a common means of self-medication of the psyche among teenagers and young people: 50 out of 120 (that is, almost one in two) admitted that they had an experience of using it.
L.: “I sat on the grass for six months. I found that after getting up, the depressive phase always begins, and it is harder than it usually happens. At the same time, the usual antidepressants do not remove it.”
These phenomena are unpleasant, but temporary. Nevertheless, cannabis can provoke mental disorders that can stay with us for life. Diseases of "big psychiatry" are considered incurable: a person can stay in remission for many years - but at any moment he can be overwhelmed by a new attack.
Can marijuana cause psychosis? A large dose of cannabis (or a small one, but with a high content of THC) can cause acute psychosis - a mental disorder in which a person loses touch with reality and the ability to behave adequately, he can see hallucinations, hear voices, and express crazy ideas.
In medicine, there is a special term "hashish psychosis" ( Cannabis induced psychosis) . It is accompanied by bouts of fear (they are caused by terrible hallucinations) and aggression (a person tries to protect himself from them).
Even a twilight disorder of consciousness may occur, in which the patient runs, aimlessly, not reacting to those around him, and after hours he does not remember at all what happened to him. The risk of getting such an experience, according to various studies, is from 1.5% to 5%, and it is higher the higher the dose you took. Usually after a few hours the patient fully recovers. But there may be long-term consequences as well.
Is there a link between cannabis use and schizophrenia
Hundreds of studies involving tens of thousands of people have been devoted to the relationship between marijuana abuse and schizophrenia, and most of them have concluded that there is such a connection, and quite strong.
One of the largest studies was conducted in Finland: for 15 years, doctors examined 18,000 patients with acute psychosis caused by drugs or alcohol, which eventually developed from single psychotic attacks into schizophrenia.
46% of cannabis-induced psychotic patients developed some form of schizophrenia within 8 years.
In most cases, the disease manifested itself in the first three years after the first hospitalization.
Danish researchers led by Mikkel Arendt came to similar conclusions (published in the British Journal of Psychiatry). Of the patients with hashish psychosis they examined, almost a third eventually fell ill with one of the most severe forms of schizophrenia - paranoid. With this disease, the level of intelligence is preserved, but consciousness is completely captured by hallucinations and delusional ideas.
Adolescents addicted to cannabis and adolescents suffering from schizophrenia showed similar brain features: hyperactivity of the centers of vision and hearing. It is with this feature that the symptoms of anxious listening to non-existent sounds (for example, voices in the head), frightening obsessive images, hallucinations are associated.
But correlation does not mean causation: just because cannabis increases the risk of schizophrenia does not mean that it causes the disease.

Psychosis, and even more so manifestations of schizophrenia, are observed only in a relatively small part of active marijuana users, so the scientists made a cautious conclusion: cannabis abuse provokes an accelerated development of the disease and its more severe and more frequent attacks, provided that the initial predisposition: in cannabis users symptoms of schizophrenia appear earlier by an average of 2.7 years.
Schizophrenia itself develops quite slowly. Changes in the psyche can take up to 10-15 years before the first psychotic episode occurs. The narcotic substance can act as a trigger that starts the active phase of the disease.
What is a predisposition to a mental disorder
First of all, this is a hereditary predisposition - that is, an innate hypersensitivity to certain substances, a violation of the metabolism of neurotransmitters in the brain.
There is no one gene for schizophrenia that will surely drive you crazy if you were born with it, but there are many genes that each slightly increase your chances of getting the disease.
Second, difficult social conditions. Belonging to economically and socially disadvantaged sections of society, constant stress, experienced violence - all this increases the risk of a “roof congress”. Finally, personal psychological characteristics. For example, highly pronounced anxiety traits can develop into a full-fledged anxiety disorder.
Each of these factors in itself is not a sentence: a trigger is often needed to “trigger” a disease. It may never appear, but often it becomes a drug.
It cannot be ruled out that people predisposed to schizophrenia use the herb as a self-medication to get rid of constant mental discomfort. People with mental disorders are indeed more prone to different types of chemical addictions.
There is another view on the relationship between these two phenomena. Doctors from King's College came to the conclusion that the same combination of genes causes susceptibility to both schizophrenia and marijuana addiction.

Large studies have been criticized for not always taking into account the effects of other harmful substances, since a significant proportion of users are not limited to cannabis. It is quite possible that marijuana itself would not have had such an effect.
The fact that the incidence of schizophrenia has practically not changed over the years, while marijuana has experienced a real boom in the last 30 years: the number of users in many countries, in particular in the USA, Canada and France, has exceeded 10% - but while the number of patients with schizophrenia in society remains at the level of 1%.
Can marijuana make mania worse? But several recent studies have shown that cannabis use in adolescence is a risk factor for the development of bipolar disorder (BD) at an older age.
A team at Warwick Medical School found that teens who use marijuana at least 2-3 times a week are more likely to show symptoms of hypomania (a mild form of mania), one of the manifestations of bipolar disorder, later on.
Smokers with bipolar disorder, like those with schizophrenia, often justify themselves by saying that the herb helps them cope with the most severe symptoms: anxiety, depression. But the scientists did not take their word for it and found that patients usually use grass not when they feel bad, but when the mood is already upbeat to increase euphoria. This is just fraught with an attack of mania.
Moreover, it turned out that people with BAD who abuse marijuana are more likely to attempt suicide . In addition, the disease starts at a younger age than in "teetotalers". This is bad, because bipolar disorder, which began in adolescence, is more severe and more dangerous than in adults.
For cannabis to cause mania or the onset of bipolar disorder, there must also be a hereditary predisposition. It was even possible to establish the genes that are responsible for it. If you have a certain variant of the AKT1 gene, your risk of manic psychosis is higher. “If you have bipolar disorder and use marijuana to relieve symptoms, ask your doctor to refer you for genetic testing,” the study authors thoughtfully suggest.
“If you have bipolar disorder and use marijuana to relieve symptoms, ask your doctor to refer you for genetic testing,” the study authors thoughtfully suggest.
What other troubles are associated with marijuana
There are other mental disorders that are more common among cannabis users. First of all, these are anxiety and depressive states.
Studies show that regular marijuana smokers are 4 to 6 times more likely to have depressive episodes. In Australia, 1,600 schoolchildren were followed for seven years using cannabis at 14-15 years old. Those who smoked daily during this period of their lives were five times more likely to suffer from depression and anxiety in adulthood. In addition, the active substances in cannabis often provoke attacks of paranoia: a person feels that he is being followed, or he is being pursued, wanting to cause harm.
Who is at risk of developing mental illness when smoking mj
A portrait of a person in the “risk group” is formed from various studies. That is, someone who is at great risk of paying for a relaxed mental health.
That is, someone who is at great risk of paying for a relaxed mental health.
1. You have a predisposition to mental disorders.
The catch is that you can’t know for sure about this in advance: schizophrenia usually starts before the age of 25, bipolar disorder before 35. If you are young and feel great, you may not be healthy, but the disease has not yet had time to manifest itself - and taking drugs substances you "help" him to do this. If you already have people with mental disorders in your family, it’s definitely not worth the risk.
2. You have pronounced schizoid character traits (withdrawal, vulnerability, extravagance). Marijuana exacerbates not only schizophrenia, but also schizoid disorder - not so severe, but also unpleasant.
3. You started using early (especially before the age of 16, when the psyche is still being formed).
4. You have experienced an episode of psychosis.
5. You use a lot and often. The larger and more regular the dosage, the higher the likelihood of psychosis and its further development into schizophrenia.

Can marijuana treat mental disorders
Speaking of marijuana and the psyche, one cannot ignore the opposite point of view: that the herb can heal.
Almost all drugs in the 19th-20th centuries were used as medicines and produced for this very purpose. Until it became obvious that the side effects were far worse than the disease itself.
In psychiatry, LSD can be called a hit. Several generations of psychiatrists and psychologists experimented with the effects of psychedelics on their patients, from Carl Gustav Jung in 1930s to Timothy Leary in the 1960s. Leary, the psychedelic guru, was arrested in a scandal, and drug experimentation is banned in most countries. But that doesn't mean they don't exist.
Not so long ago, a book was published about how underground psychiatrists treat patients whom official medicine considered hopeless (that is, resistant to known drugs) with the help of the same LSD, amphetamines and, to a lesser extent, marijuana. It’s definitely not worth repeating their methods at home, even if they really help someone: there is a big difference between using a purified substance under medical supervision and an incomprehensible mixture at your own peril and risk.
It’s definitely not worth repeating their methods at home, even if they really help someone: there is a big difference between using a purified substance under medical supervision and an incomprehensible mixture at your own peril and risk.
There is also a completely legal industry for the production of marijuana for medical purposes in those countries where it is legal (for example, in Canada - since 2001). According to the National Institute on Drug Abuse (NIDA), cannabis-based drugs can be used as pain relievers, against nausea and loss of appetite. For example, Marinol is prescribed to cancer patients to improve their weak appetite: these drugs do not get high, they just contain small dosages of cannabinoids purified from impurities.
The practice of using marijuana in psychiatry is relatively small, and there are even fewer studies proving its effectiveness. But, as we have already found out, a huge number of patients use it as a self-medication, so the question is more than relevant.

Psychiatrist Julie Holland, author of a fairly popular book on marijuana, says marijuana relieves military veterans suffering from post-traumatic stress disorder.
A 2016 study published in the Clinical Psychology Review found that cannabis can also improve the condition of people with depression and social anxiety. True, it soon became clear that these scientists received funding from Canadian marijuana producers, so there is reason to doubt their objectivity.
(Our other article is devoted to the scientifically proven therapeutic effects of marijuana)
Weed smokers are six times more likely to get schizophrenia
Weed smokers are six times more likely to get schizophrenia - Rossiyskaya gazetaFresh issue
WG-Week 9002 Homeland
Thematic applications
Union
Fresh issue
04/04/2019 20:12
Heading:
Society
Weed smokers are six times more likely to get schizophrenia
Vladimir Bogdanov
Canadian doctors, together with colleagues from the United Kingdom and the United States, analyzed data from observations of more than 23,000 marijuana users.![]() Conclusion: there is a relationship between the consumption of "weed" in adolescence and depressive disorder in adults.
Conclusion: there is a relationship between the consumption of "weed" in adolescence and depressive disorder in adults.
Experts are convinced that smoking marijuana is the gateway to heroin addiction or other hard drugs. According to foreign studies over the past 15 years, over 20 million people annually use marijuana. In the United States, marijuana addiction is listed as a mental disorder and affects more than four million people.
Meanwhile, it has been scientifically proven that schizophrenia occurs 6 times more often in marijuana users. Cannabis provokes bouts of paranoia. These people are constantly lowering the psychological barrier against hard drugs. Smoking cannabis causes the greatest harm to the respiratory organs: the dangerous substances contained in the smoke cause lung cancer. In medicine, there is a special term "hashish psychosis". It is accompanied by bouts of fear, terrible hallucinations. One of the largest studies was conducted in Finland: for a long time, doctors examined 18,000 patients with acute psychosis caused by narcotic substances: 46% of these patients fell ill with one form or another of schizophrenia.
Rossiyskaya gazeta - Federal issue: No. 75(7833)
Share:
HealthFight against drugs
14:06Sports
President of the Russian Tennis Federation and IOC member Shamil Tarpishchev knows the reason for the many surprises at the 2022 World Cup
14:03Culture
"Children should not be given sausage": Non/fiction hosted a meeting with Gennady Onishchenko
13:53Economy
Europe will drop the requirement to switch smartphones to airplane mode on board an aircraft
13: 40 Kinocracy
Viktor Sukhorukov explained the popularity of the film "Brother"
13: 35 Plastity
What rare flowers can be seen in the Caucasian reserve in winter
9000 13: 27 PacetorshipIn St. Petersburg, a multimedia digital technology show
9000 13: 19000 13: 19000 13: 19000 13: 19000 13: 19000 13: 19000 13Heavy metal legend "Master" celebrates 35th anniversary with a tour of Russia
13:02 Kinocracy
Actor Quentin Oliver Lee died at 34
12:55Kinokratiya
"Soviet Demis Roussos" Harald Simanis died
12:54Culture
The first Internet journalist and brilliant "matchmaker".