Does sleep help with depression
SAMHSA’s National Helpline | SAMHSA
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.
Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders.
This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative. Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs. In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems. Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.
Addresses concerns of children of parents with substance use/abuse problems.It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt. Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse. Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.
For additional resources, please visit the SAMHSA Store.
Last Updated: 08/30/2022
SAMHSA Behavioral Health Treatment Services Locator
HomeWelcome to the Behavioral Health Treatment Services Locator, a confidential and anonymous source of information for persons seeking treatment facilities in the United States or U.S. Territories for substance use/addiction and/or mental health problems.
PLEASE NOTE: Your personal information and the search criteria you enter into the Locator is secure and anonymous. SAMHSA does not collect or maintain any information you provide.
Please enter a valid location.
please type your address
-
FindTreatment.
 gov
gov Millions of Americans have a substance use disorder. Find a treatment facility near you.
-
988 Suicide & Crisis Lifeline
Call or text 988
Free and confidential support for people in distress, 24/7.
-
National Helpline
1-800-662-HELP (4357)
Treatment referral and information, 24/7.
-
Disaster Distress Helpline
1-800-985-5990
Immediate crisis counseling related to disasters, 24/7.
- Overview
- Locator OverviewLocator Overview
- Locator OverviewLocator Overview
- Finding Treatment
- Find Facilities for VeteransFind Facilities for Veterans
- Find Facilities for VeteransFind Facilities for Veterans
- Facility Directors
- Register a New FacilityRegister a New Facility
- Register a New FacilityRegister a New Facility
- Other Locator Functionalities
- Download Search ResultsDownload Search Results
- Use Google MapsUse Google Maps
- Print Search ResultsPrint Search Results
- Use Google MapsUse Google Maps
- Icon from Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers).
 Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers).
Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers). - Icon from Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers). Find programs providing methadone for the treatment of opioid addiction (heroin or pain relievers).
The Locator is authorized by the 21st Century Cures Act (Public Law 114-255, Section 9006; 42 U.S.C. 290bb-36d). SAMHSA endeavors to keep the Locator current. All information in the Locator is updated annually from facility responses to SAMHSA’s National Substance Use and Mental Health Services Survey (N-SUMHSS). New facilities that have completed an abbreviated survey and met all the qualifications are added monthly. Updates to facility names, addresses, telephone numbers, and services are made weekly for facilities informing SAMHSA of changes. Facilities may request additions or changes to their information by sending an e-mail to [email protected], by calling the BHSIS Project Office at 1-833-888-1553 (Mon-Fri 8-6 ET), or by electronic form submission using the Locator online application form (intended for additions of new facilities).
Updates to facility names, addresses, telephone numbers, and services are made weekly for facilities informing SAMHSA of changes. Facilities may request additions or changes to their information by sending an e-mail to [email protected], by calling the BHSIS Project Office at 1-833-888-1553 (Mon-Fri 8-6 ET), or by electronic form submission using the Locator online application form (intended for additions of new facilities).
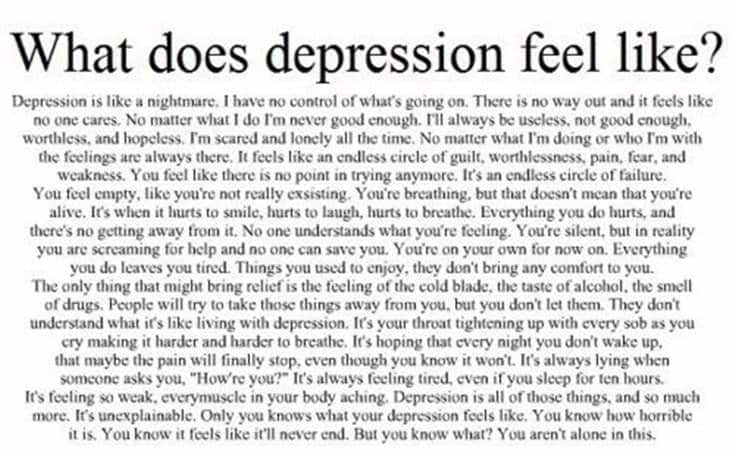
No sleep, no rest for the tormented soul
Sleep is one of the basic needs of the human body, and its lack leads to severe psychological and physical stress: not only mood and cognitive abilities suffer, but also the cardiovascular system and metabolism. Nevertheless, for almost 50 years, sleep deprivation has been trying to treat one of the most difficult and terrible conditions for the human psyche - depression. We set out to explore what forced sleep therapy for psychiatric disorders is, why it can be effective, and why it should be used with caution.
Anyone who has not slept for a long time at least once knows perfectly well what this is fraught with: lethargy appears, attention decreases, mood deteriorates and severe physical fatigue occurs. Available stimulants like caffeine stop working (their mechanism of action is rather limited), and the only way out is to take a break and still rest.
In chronic sleep deprivation and insomnia (we talked about it in detail in the material “Your words rock well”, prepared for World Sleep Day last year), deeper and more serious conditions and diseases are added to superficial symptoms.
For example, the consequences of lack of sleep include cardiovascular disease, nutritional and metabolic problems (from overeating to type 2 diabetes), and various mental disorders. Last but not least, lack of sleep is closely associated with depression, which is surprising in its own way, because sleep deprivation is often used to treat it, and at times quite successfully.
At least that's what the meta-analyses suggest. One, conducted in 2017, focuses on 66 studies published since 1974 to 2016: it states that sleep deprivation is effective in 50 percent of patients in randomized control trials and 45 percent in other studies. The effect did not depend on what experimental technique was used, on what preparations the patient was sitting, and also on his gender and age.
The authors of the study call the effect significant, but given the fact that the side variables that would provide the desired effect could not be found, the result can be called random - of course, if we consider the use of sleep deprivation as a binary variable. In other words, when psychiatrists give patients with depression forced sleep therapy, it can either help or not - as luck would have it.
At the same time, sleep deprivation is still considered a fairly effective way to treat depression, and why this is so (even if it is intuitively clear that lack of sleep is more likely to be harmful) should still be understood.
Intervene experimentally
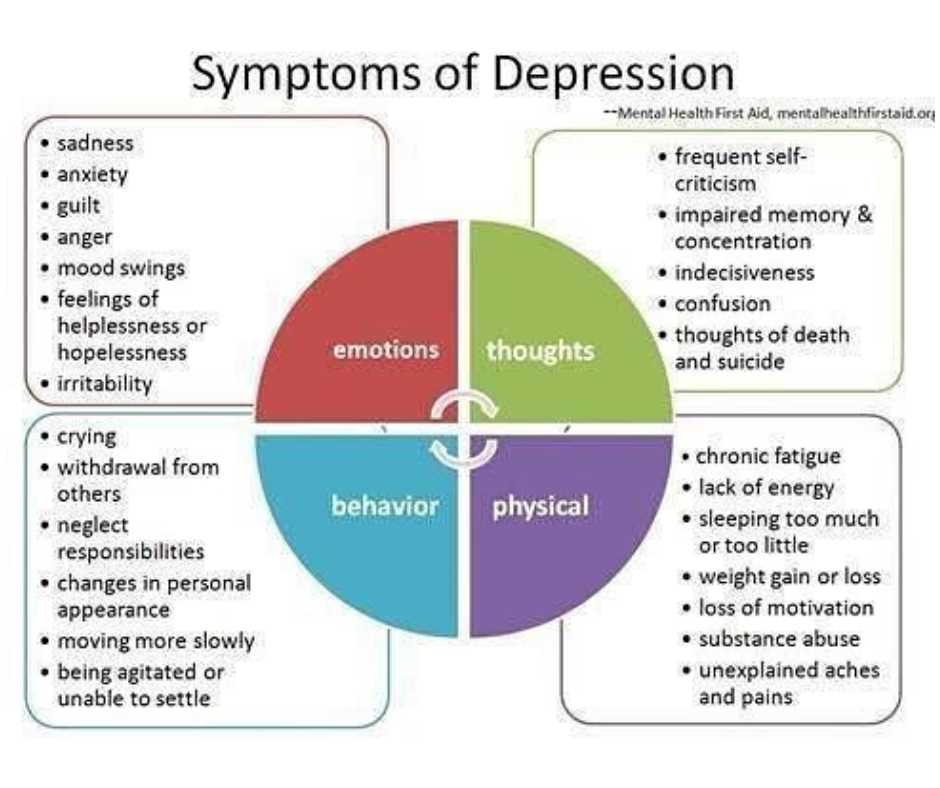
The relationship between sleep quality and mental disorders is complex. First of all, the relationship between them is two-way: insomnia, as well as hypersomnia - excessive sleep duration and daytime sleepiness, are considered both symptoms of depression and factors that largely affect its development.
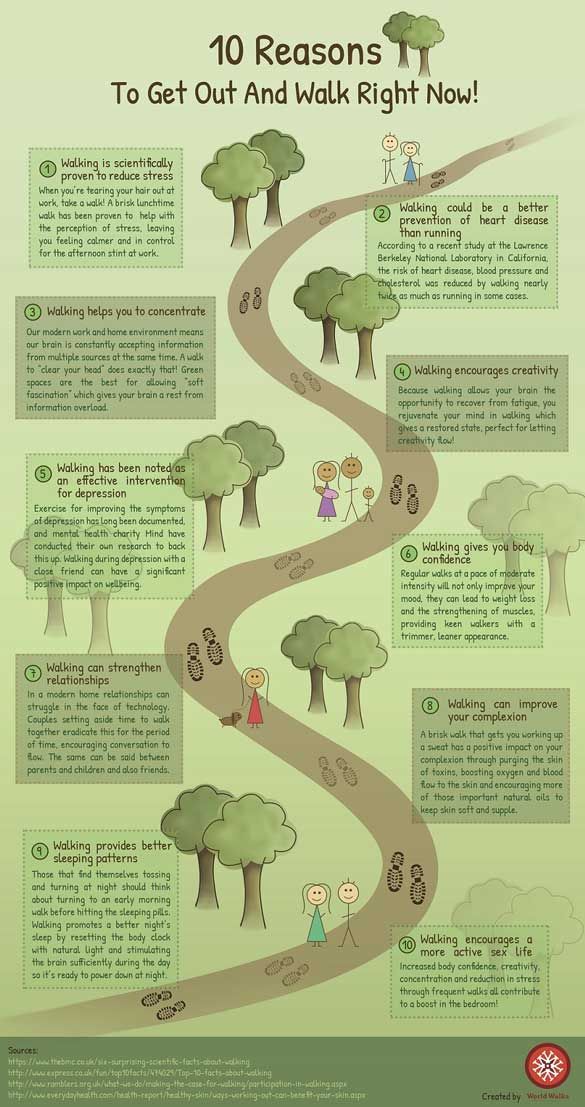
First of all, therefore, in case of depression, it is necessary to restore normal sleep hygiene: do not eat a few hours before going to bed, go to bed at the same time, sleep the number of hours recommended for age (for an adult - about seven to eight hours a day). day) and do not put off rest for the weekend in anticipation of a cumulative effect.
Obviously this can be quite difficult; in this case, patients with depression are prescribed drugs from the group of neuroleptics or other substances with anti-anxiety (trouble, as you know, does not come alone: with depression, the risk of developing anxiety is higher) or sedative effect.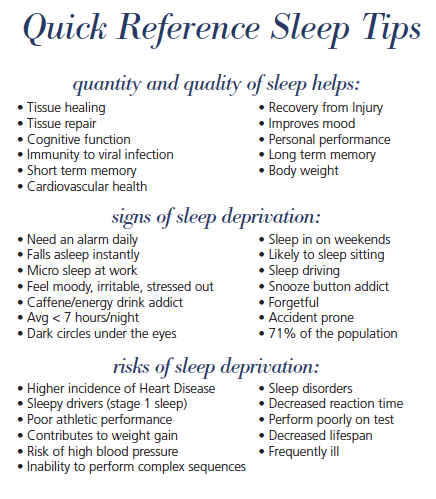
In the early 1970s, the German psychiatrist Walter Schulte discovered and studied that sleep deprivation could have a therapeutic effect on depression. He observed three patients diagnosed with depressive disorder: two teachers and one physician. Each of them reported to Schulte that after a sleepless night at work or playing sports, they feel an improvement in their mental state.
Of course, it is impossible to base an entire psychiatric practice on three cases, so after the first statements about the benefits of sleep deprivation (after Schulte, two more of his colleagues managed to achieve a significant effect in 23 out of 34 patients), scientists began to actively conduct research.
First, it was necessary to determine exactly how many hours of sleep deprivation it takes to achieve at least some effect - and at what time to start the experiment. Usually, sleep deprivation therapy involves a whole day (or even more: sometimes up to 36-40 hours) of forced wakefulness: the patient is woken up at about one in the morning, after which he does not sleep the whole next day and sometimes even the whole next night.
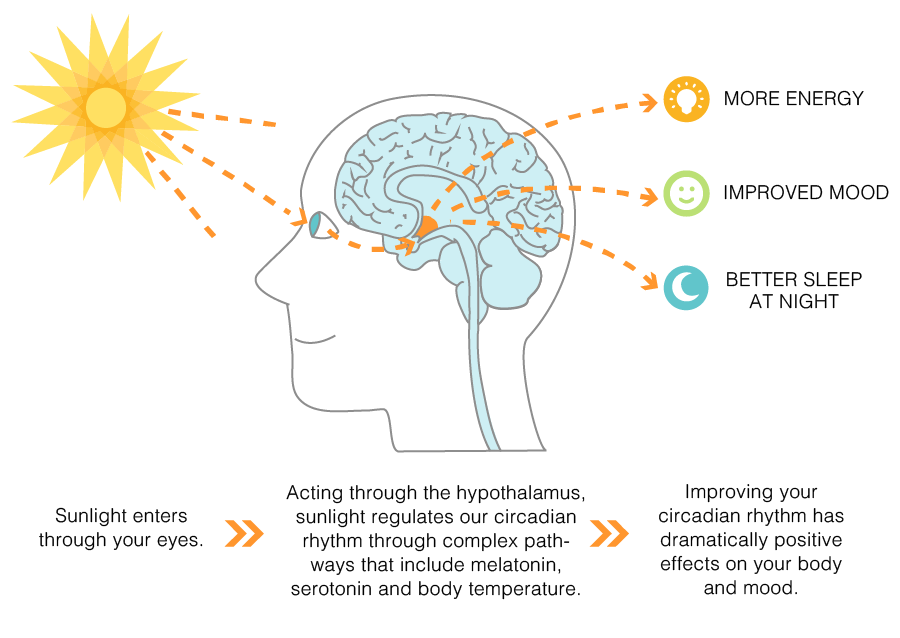
With this therapy, the intake of any CNS stimulants (even coffee) is excluded, and it is also recommended to combine forced insomnia with light therapy (however, both are considered branches of chromotherapy - artificial "tuning" of sleep and wake cycles).
The effect is quite fast: with sleep deprivation in a depressed patient, visible improvements are immediately observed. However, this is a rather deceptive success: studies indicate that in 50-80 percent of patients the state returns to the usual depressive state after they do get some sleep. At the same time, in 10-15 percent of patients, improvements, on the contrary, appear only after sleep following deprivation. In 2-7 percent of patients, the condition may worsen, and symptoms of mania may be added to depression (sleep deprivation, therefore, is not recommended for people with bipolar disorder - even in the depressive phase).
Some vagueness of the effect can be explained by the fact that a day or more without sleep is still quite painful for the body. Therefore, scientists tried to reduce the time of forced wakefulness to a few hours at night. To do this, for example, you can wake up the patient in the middle of the night and keep him awake for a couple of hours. Such a study was conducted in the early 1990s, but forced wakefulness until five in the morning after waking up at three did not give any special effect.
Therefore, scientists tried to reduce the time of forced wakefulness to a few hours at night. To do this, for example, you can wake up the patient in the middle of the night and keep him awake for a couple of hours. Such a study was conducted in the early 1990s, but forced wakefulness until five in the morning after waking up at three did not give any special effect.
Although meta-analyses indicate that there are no precise confounding variables that would provide the desired effect of sleep deprivation, anecdotal studies still state that several conditions must be met for such a method to be effective.
For example, sleep deprivation works best on patients with endogenous depression, rather than depression caused by external factors. In addition, the variation in the patient's mood during the day must also be taken into account: sleep deprivation works most effectively in those who feel better in the evening, rather than during the day.
The mechanism of the therapeutic effect of sleep deprivation has not been fully established.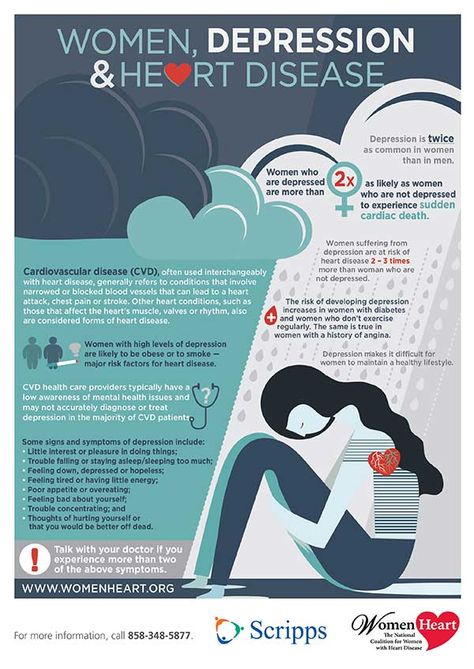 For example, recent research suggests the role of the neurotransmitter adenosine, which accumulates in the brain during the day and is ultimately responsible for making us feel tired and fall asleep.
For example, recent research suggests the role of the neurotransmitter adenosine, which accumulates in the brain during the day and is ultimately responsible for making us feel tired and fall asleep.
Other studies point to the involvement of the serotonergic system, which is central to the pathology of depression, in such therapy. When taking the drug pindolol, which blocks serotonin autoreceptors and improves the effect of antidepressants from the group of selective serotonin reuptake inhibitors, sleep deprivation more effectively improves well-being in depression.
A logical reason for the effectiveness of lack of sleep seems to be its comparison with the use of psychostimulants (eg, amphetamine). Indeed, in the absence of sleep, effects similar to taking psychoactive substances are sometimes observed (you may be familiar with this: sometimes, with a long wakefulness, it seems that there is more strength and energy).
In both cases, the concentration of monoamines in the brain increases (primarily, however, not serotonin, but dopamine), due to which the work of the limbic system stabilizes, and mental well-being improves. Such a theory is consistent with the fact that the effect of sleep deprivation is often unstable and short-lived - like psychostimulants. However, this is still just a theory.
Such a theory is consistent with the fact that the effect of sleep deprivation is often unstable and short-lived - like psychostimulants. However, this is still just a theory.
Use with caution
Despite a fairly long history of study and use in psychiatric practice, sleep deprivation still remains an experimental treatment for depression and is not included in the standard treatment recommendations along with antidepressant drugs and psychotherapy. This is evidenced both by the fact that depression is often treated with sleep deprivation only under controlled conditions (under the supervision of doctors), and by the fact that sleepless nights have many negative consequences.
One of the most serious is the possible increased risk of developing Alzheimer's disease even from one night of sleeplessness. Two proteins play a key role in the development of the disease: beta-amyloid, which forms plaques in the brain, and tau, which contributes to the formation of intracellular neurofibrillary cords.
Studies show that just one sleepless night significantly increases the concentration of beta-amyloid in the brain and tau in the blood. The mechanism of such an action is not fully known in either case, and it is also not clear whether there are actually any negative consequences.
It is also interesting that lack of sleep leads to increased feelings of loneliness and social isolation. Here the effect, however, is more psychological: the lack of sleep makes people look for a variety of ways to escape from the accumulated fatigue, which increases the need for communication. Other people, on the contrary, find a sleepy person more repulsive and do not want to make contact with him.
A rather understandable conflict arises, which makes it difficult to establish communication with others - hence the feeling of loneliness appears. And with depression (unless, of course, it was not there before, since loneliness is one of the common psychological symptoms of a disorder), it is definitely not necessary.
In addition, a recent study showed that a sleepless night reduces the activity of the prefrontal cortex, which is responsible, among other things, for cognitive control. With a decrease in cognitive control, in turn, anxiety increases significantly - and it can significantly worsen the condition of depression.
However, it should be borne in mind that the use of sleep deprivation for the treatment of insomnia and the same technique for behavioral research are two different things. Healthy people without mental disorders take part in the latter; in them, control studies of sleep deprivation therapy show that not getting a night's rest only increases irritability—and doesn't work the way it does for people with depression, even in the short term.
Therefore, it is logical to assume that lack of sleep may not bring negative behavioral and mental aspects to people with depression: review studies also speak about the severity of the presence of mental disorders for the effectiveness of sleep deprivation. But do not forget about the average effectiveness of 50 percent (as well as the fact that the drug treatment of depression has about the same indicators).
But do not forget about the average effectiveness of 50 percent (as well as the fact that the drug treatment of depression has about the same indicators).
So, while sleep deprivation can actually help improve depression, we don't recommend experimenting with your body, brain, and mental state in this way: it's better to have your psychiatrist do it.
Elizaveta Ivtushok
How depression made me an early bird and a new approach to sleep turned me into a superhuman
August 13, 2018Health
Entrepreneur Alicia Liu spoke about her experience of dealing with depression and the unexpected consequences of dealing with depression.
Share
0Alicia Liu
Developer, entrepreneur, vice president of Nava.
Background
For the last six months I have been waking up around 6:30 am, including weekends and holidays. Of course, this is not so early compared to those who get up at five in the morning. But for me, this is a huge change. I literally became a different person. Now I wake up before my alarm and start the day enthusiastically. Before breakfast, I have a whole set of things to do: I meditate, do yoga, ride a bike, read, write, cook oatmeal. It may seem that I am obsessed with my health, but I myself do not quite understand how I came to this.
But for me, this is a huge change. I literally became a different person. Now I wake up before my alarm and start the day enthusiastically. Before breakfast, I have a whole set of things to do: I meditate, do yoga, ride a bike, read, write, cook oatmeal. It may seem that I am obsessed with my health, but I myself do not quite understand how I came to this.
From childhood I was an incorrigible owl, I loved to read until late at night. Before the invention of tablets and e-readers, I took a table lamp to bed and covered myself with a blanket so that my parents would not notice that I was not sleeping. Around 11 p.m., I usually have a surge of creative energy - this persisted even after turning into a lark. Most of the articles and projects in recent years I have done after midnight.
I work at tech start-ups, and they seem to be specifically designed for owls. No one will look at you askance if you come to work after 10 or even after 11. So, although I went to bed at one or two in the morning, I managed to get 7-8 hours of sleep.
Of course, I knew the benefits of getting up early. But it never crossed my mind to try.
Until I changed jobs. I got a job in a company that improves public services. Because of this, I had to travel every month from San Francisco to the company's headquarters in Washington. Frequent jet lag and increased job responsibilities at a fast-growing startup led to stress and insomnia. And then depression crept in.
How I realized that I had depression
This is not the first time I have experienced depression. In addition, I have been meditating for a long time, so it would seem that I should have recognized the signs of an approaching depression in advance. But no. The brain is great at masking problems with rational explanations.
I associated my pessimistic moods with a realistic outlook on life. Convinced myself that optimists are just being deceived. In addition, the world as I knew it was disintegrating before my eyes. Optimizing public services is incredibly difficult, especially when the President and Congress are actively trying to destroy everything you do. At first, I enthusiastically took up this job, but the motivation began to decline sharply. It doesn't look like me at all.
Optimizing public services is incredibly difficult, especially when the President and Congress are actively trying to destroy everything you do. At first, I enthusiastically took up this job, but the motivation began to decline sharply. It doesn't look like me at all.
I was thinking how nice it would be to quit my job and be relieved of my work responsibilities. With difficulty I waited for the end of the working day, already on Tuesday I dreamed about the weekend and thought with fear about work on Sunday evening.
I didn't have the energy to do anything after work. Gradually, I stopped meeting friends and being interested in entertainment. I convinced myself that everything that used to give me joy - traveling, restaurants, photography, writing articles - were just meaningless activities.
Worse, I gave up training because I was constantly feeling tired. And this despite the fact that in a year I have already participated in two sprint triathlons. I began to think that it is not so important whether I live or not. It was then that I finally realized that my brain seemed to be malfunctioning.
I began to think that it is not so important whether I live or not. It was then that I finally realized that my brain seemed to be malfunctioning.
It is a common misconception that depression is a state of being very sad. In fact, you just don't care. Sadness implies that you still care about yourself. During depression, it’s hard to force yourself to work, do your hobbies, go somewhere, see people, because you don’t care about all this.
How depression is related to sleep and how I struggled with it
I went to see a doctor and a psychotherapist. At the appointment, it became clear to me that I had insomnia. This is a sleep disorder in which it is difficult to fall asleep or not wake up for several days. The symptoms of depression and insomnia mutually reinforce each other.
By that time I had been having trouble sleeping for many weeks. Although I went to bed very early, I did not fall asleep for a long time. I was tormented by anxious thoughts about work. I constantly felt tired, and this only exacerbated the depression.
I constantly felt tired, and this only exacerbated the depression.
I knew I had to do something, but I didn't want to take sleeping pills. After sedation, the next day you feel like a zombie. At one time, I worked with a company that was studying the effects of medical marijuana on various conditions, including insomnia. It doesn't have the side effects of sleeping pills. I took advantage of the fact that I live in California and went to the doctor to get permission to buy medical marijuana.
In the US, it is classified as a banned substance, so there is very little reliable information about its properties. I had to experiment to understand how much I need to fall asleep. It's not at all as pleasant as it sounds. I don't smoke, and making tinctures seemed too complicated for me. Therefore, I settled on food products with the addition of marijuana. Their action occurs only after a few hours, so it is very difficult to choose the right time to take and dose. Other food eaten also affects the effect. However, it became easier for me to fall asleep. Only insomnia has not gone away.
However, it became easier for me to fall asleep. Only insomnia has not gone away.
I still woke up around 4 or 5 am and couldn't sleep anymore because of anxious thoughts. Sometimes I managed to fall asleep again, but in the morning I still felt lethargic and tired.
Marijuana inhibits REM sleep, which is essential for memory and other important brain functions. It is suitable as a temporary solution, but does not provide sleep that truly restores the body. I knew that I needed to learn to sleep naturally. It was around this time that I came across information about cognitive behavioral therapy for insomnia (CBT-B).
How CBT works for insomnia
The body has a natural need for sleep. He knows how to sleep. Small children and animals do not suffer from insomnia. Adults have trouble sleeping because they think too much.
According to CBT-B, our thoughts are the main cause of depression and anxiety. And if you replace negative illogical thoughts with positive and realistic ones, mental health will improve. And in order to change your thoughts, you need to change your behavior.
And in order to change your thoughts, you need to change your behavior.
Before that, I thought, like most people: if I don't get enough sleep, then I need to sleep more. I went to bed earlier and stayed in bed longer. CPT-B suggests the opposite approach: to get enough sleep, you need to sleep less than .
Sleep time and just time in bed are not the same thing. The ratio of these two numbers reflects the efficiency of your sleep.
I went to bed at 23 and got up at 8, but slept only 5-6 hours. That is, my sleep efficiency was only 5/9or 55%, and ideally you need more than 90%. No wonder I was so tired.
To change a habit, you first need to observe it. This also applies to sleep. CBT-B specialists advise tracking your sleep two weeks before starting therapy and keeping a special sleep log. In this case, you can not take sleeping pills. I did not want to suffer without sleep for another two weeks, so I immediately began therapy. And I tracked my sleep using the Apple Watch app. This method is not as reliable as handwriting, but it was enough for me.
And I tracked my sleep using the Apple Watch app. This method is not as reliable as handwriting, but it was enough for me.
CBT-B includes improving sleep hygiene and getting rid of negative thoughts about it. It is based on two behavioral strategies: stimulus control and sleep restriction. They can be used individually or combined. I decided to combine. The downside is that you need even less sleep. For almost a month I was very, very tired. This is extremely unpleasant, but you get the result faster.
Stimulus control
It teaches to associate the bed only with sleep. For this:
- Go to bed only when you feel sleepy. Not just when you're tired, but when your eyes close, your head bows and you begin to nod off.
- If you are still awake after 15 to 20 minutes, get up and go to another room until you feel sleepy again.
- Don't do other things in bed: don't read, don't work, don't correspond, don't watch TV. The only exception is sex.

Sleep restriction
This strategy assumes that you need to spend as much time in bed as the body is able to sleep. To do this:
- Determine how much time you sleep using your sleep observations. When I started practicing this method, I got about five hours of sleep per night. This exercise helps you see that we usually sleep longer than we think.
- Calculate what time you need to go to bed. It all depends on how much you sleep and when you need to get up. I wanted to get up at 6:30, it turns out that I needed to go to bed only after one in the morning. Give yourself some time to fall asleep. No matter how tired you are, go to bed only at the calculated time. You should aim for 90 percent efficiency, that is, almost all the time in bed should be occupied by sleep.
- When sleep efficiency exceeds 90% during the week, increase time in bed by 30 minutes. If you get more sleep next week, go to bed another half an hour earlier, and so on.
 But if your sleep efficiency starts to decline, reduce your time in bed again.
But if your sleep efficiency starts to decline, reduce your time in bed again.
Sleep only in bed and nowhere else. Don't take a nap and consume less caffeine. But most importantly, get up at the same time every day, even on weekends. At first it was very difficult: I always liked to lie around longer on non-working days. But since I still didn’t get enough sleep, I decided to try it. I am sure that as a result it helped me to improve the quality of sleep.
Results
The most amazing and important thing I have learned in therapy is not how to sleep more. My sleep time has increased to six and a half hours. But sometimes there were still nights when I slept for 5-6 hours, and this is much less than the recommended 7-8. At the same time, I helped myself in every possible way:
- I did yoga poses, lit scented candles, took a hot bath to relax before going to bed.
- Bought nice cotton sheets, a duvet and linen bed sheets to make her sleep more comfortable.
- I sewed thick curtains myself, because the finished ones for our window are too narrow.
- After consulting a doctor, I bought a special phototherapy lamp that regulates the production of melatonin. I didn't notice any effect. If you have insomnia, do not start treatment with a lamp yourself: improper use can only worsen the symptoms.
- I kept an anxiety diary to organize the thoughts that prevented me from sleeping. Every morning for 10 minutes I wrote down everything that bothered me. You have to write before the time runs out. Try it if you suffer from anxiety.
- Bought glasses with yellow lenses that protect from the blue light of the screens. I put them on every night around nine.
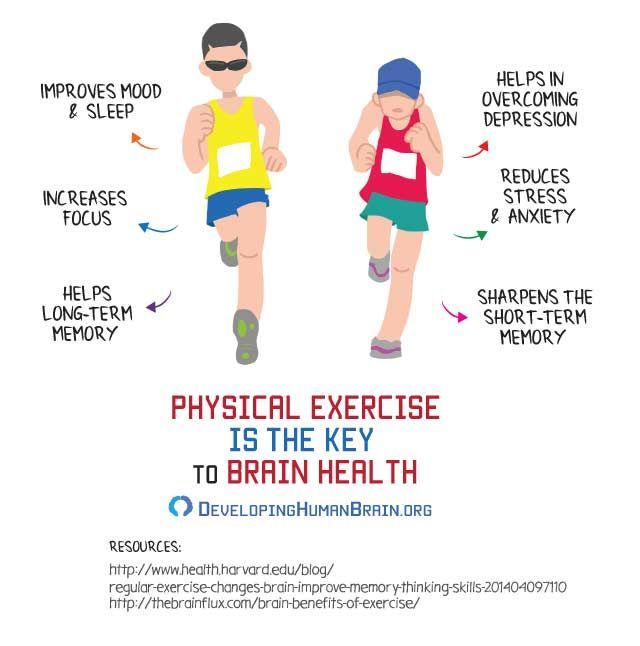
- And the most useful thing is that I started exercising regularly again. I signed up for a triathlon with a friend, it gave me motivation. Exercise itself is effective in treating insomnia and depression.
Even though I've been doing this for half a year, I still get less than seven hours of sleep.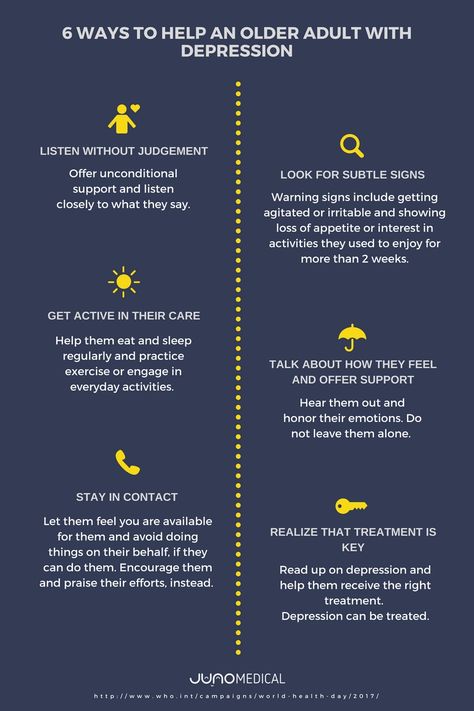 And I feel great! Because, in addition to a change in habits, I also had a change in thinking.
And I feel great! Because, in addition to a change in habits, I also had a change in thinking.
I thought I needed about eight hours of sleep in order to feel good the next day, be productive and energetic - but this is not true.
When I gave up this belief, I began to enjoy life much more. As soon as my anxiety about not sleeping stopped, the depression also went away. This was during the first week of therapy. As I later learned, sleep reduction is used to treat depression along with antidepressants.
Personal findings
As you can see, during this therapy you begin to behave a little strangely. If you wake up in the middle of the night, you need to get out from under the covers and do something boring until you feel sleepy again. But when I realized that the body itself would fall asleep as soon as it was ready, I accepted these oddities. When I was up at night, I listened to podcasts and audiobooks, did household chores, and played with my cats. In order not to suffer so much, getting out of a warm bed, I put on a cozy sweater and slippers.
In order not to suffer so much, getting out of a warm bed, I put on a cozy sweater and slippers.
Difficulties with sleep and insomnia do not come from lack of sleep, but from anxiety about not getting enough sleep.
Since I went to bed late to limit my sleep to the hours I needed, I had extra free time. I watched a lot of TV series and read a lot of management books. Both pleasure and benefit!
If you are not sleeping alone, there are additional difficulties. My husband practically stopped seeing me in bed. I go to bed when he is already fast asleep, and I get up much earlier than him. Be sure to discuss how the new sleep routine will affect your relationship. I hope your partner will notice that you are becoming happier and more energetic, and will treat the changes with understanding. Replace falling asleep together with some other activity that strengthens your bond.
The most noticeable effect of therapy was on my mood. Of course, there are still nights when I wake up too early and can't get back to sleep. But now I do not indulge in anxious thoughts, but benefit from additional free time.
But now I do not indulge in anxious thoughts, but benefit from additional free time.
Ever since I started CBT for insomnia, I feel almost superhuman.
I began to see the meaning in my work again and became much more productive. I'm speaking at two conferences this year, although just recently I thought I wouldn't be able to speak in front of an audience.
I became hypersociable and learned to recharge my energy from interacting with people. I began to value time with friends and conversations with strangers more. I have become a real triathlete and train almost ten hours a week. I took eighth place in my age category in the sprint triathlon and now I am preparing for the Olympic distance. If I used to be intimidated by the thought of swimming 1.5 kilometers, cycling 40 and running 10 more, now I am overwhelmed with enthusiasm.
I started writing articles again after a two-year hiatus. I don't know what to do with the surge of creative energy.