Does gabapentin help with numbness
Gabapentin | MS Trust
Last updated: 1 December 2020
Other name: Neurontin
Several non branded versions are available.
What is gabapentin used for in MS?
Gabapentin is a drug used in the treatment of nerve pain (neuropathic pain) in multiple sclerosis. It's often used to treat altered sensations (dysaesthesia) like numbness, burning or pins and needles.
The NICE MS Guideline also recommends gabapentin as one of the first drugs to try in the treatment of spasms and spasticity.
Gabapentin is also sometimes used to treat visual problems, like nystagmus where your eyes rapidly flick up and down or from side to side involuntarily.
How do I take gabapentin?
Gabapentin is taken orally as tablets, capsules or a liquid that you drink. It's usually taken three times a day – morning, afternoon and evening. Gabapentin can be taken with or without food.
Your doctor will usually start you on a low dose and build up gradually to find a level that's effective with little or no side effects.
When stopping treatment, the dosage should be gradually reduced over a minimum of a week.
What side effects could I get with gabapentin?
Side effects can include sedation, dizziness, fatigue and weakness. They usually wear off as your body gets used to gabapentin.
Talk to your GP if you're experiencing side effects as they may be able to suggest ways to manage them or they may suggest reducing the dose.
Contraindications
Gabapentin should not be taken during pregnancy or when breastfeeding, unless you are told otherwise by your doctor.
Antacids (used to treat indigestion and heartburn) can reduce the amount of gabapentin that your body absorbs so it doesn’t work as well. It’s therefore recommended that you wait at least two hours after taking an antacid before you take your dose of gabapentin.
If you have a condition that affects your breathing, such as chronic obstructive pulmonary disease (COPD), or you are taking a medicine that affects your breathing, such as an opioid painkiller, then taking gabapentin may cause serious breathing difficulties. If you have concerns about this, discuss them with your doctor.
If you have concerns about this, discuss them with your doctor.
How does gabapentin work?
Gabapentin is an anticonvulsant and anti-epileptic drug. How it works is not fully understood.
From April 2019, the government has announced that gabapentin will be reclassified as a Class C controlled drug under the Misuse of Drugs Act 1971 and be placed in Schedule 3 to the Misuse of Drug Regulations 2001. This follows concerns over the drug being misused. These law changes mean that it will be illegal to possess gabapentin without a prescription and to supply or sell it to others.
What does this mean for me?
Doctors will still be allowed to prescribe gabapentin, however there are a number of rules that you, your doctor and your pharmacist will need to follow from April 2019. NHS England has published a patient leaflet to explain these changes – we also cover some of them below.
- Doctors will only be able to provide 30 days’ supply of gabapentin on one prescription.

- You will need to request a repeat prescription each month from your GP practice.
- Your GP practice may no longer be able to send your prescription electronically to the pharmacy. This means that you or your representative will need to visit the GP practice each month to collect your prescription and take it to the pharmacy.
- If your GP practice uses the electronic prescription service for controlled drugs, your prescription will be sent to the pharmacy electronically. This system has not yet been rolled out in all GP practices.
- You must collect your medicine from the pharmacy within 28 days of the date on the prescription.
- You’ll need to sign and show proof of your identity when you collect your medicine from the pharmacy.
Do speak to your GP practice if you’re unsure about how to get your next prescription.
Research
Various clinical trials have looked at the effectiveness of gabapentin in treating neuropathic pain. A systematic review – which collates and analyses data from a range of studies – found that in people experiencing neuropathic pain after shingles, gabapentin reduced pain by half or more for 3 in 10 people and by a third or more for 5 in 10 people. In people with neuropathic pain caused by diabetes, gabapentin reduced the pain by half or more for 4 in 10 people and by a third or more for 5 in 10 people.
A systematic review – which collates and analyses data from a range of studies – found that in people experiencing neuropathic pain after shingles, gabapentin reduced pain by half or more for 3 in 10 people and by a third or more for 5 in 10 people. In people with neuropathic pain caused by diabetes, gabapentin reduced the pain by half or more for 4 in 10 people and by a third or more for 5 in 10 people.
The systematic review concluded that gabapentin is helpful for some people with chronic neuropathic pain. Unfortunately this review didn’t look at the effectiveness of gabapentin in people with MS, but it does give some idea of the level of pain relief that gabapentin can provide.
Find out more
- Patient Information Leaflet - Neurontin - (EMC website)
- GOV.UK - Pregabalin and gabapentin to be controlled as class C drugs
- GOV.UK - Consultation outcome – pregabalin and gabapentin
- The FDA (US) warns about serious breathing problems with gabapentin and pregabalin - US drug safety agency article from December 2019
-
Cutter NC, et al.
Gabapentin effect on spasticity in multiple sclerosis: a placebo-controlled, randomized trial.
Archives of Physical Medicine & Rehabilitation 2000;81(2):164-169.
Summary (link is external)Mellegers M, et al.
Gabapentin for neuropathic pain: systematic review of controlled and uncontrolled literature.
Clinical Journal of Pain 2001;17:284-295.
Summary (link is external)Wiffen PJ, et al.
Gabapentin for chronic neuropathic pain in adults.
Cochrane Database of Systematic Reviews 2017, Issue 6. Art. No.: CD007938.
Full article (link is external)
Related content
The two main types of pain in multiple sclerosis are nerve (neuropathic) pain and musculoskeletal (nociceptive) pain. Find out more about pain in this A-Z entry.
Spasticity and spasms
Spasticity and spasms are common symptoms of multiple sclerosis that may causes your muscles to feel stiff and heavy, or cause them to move unpredictably.
Questions about MS?
Are you looking for reliable information about MS? Our free MS Enquiry Service helpline, information and resources can answer your questions about multiple sclerosis and life with the condition.
Share this page
Does gabapentin help nerve pain?
Medically reviewed by Carmen Fookes, BPharm. Last updated on Aug 19, 2022.
Gabapentin can help relieve nerve pain in some people with postherpetic neuralgia (nerve pain after shingles) and peripheral diabetic neuropathy (nerve pain in the feet in people with diabetes). A Cochrane review reported that 3 to 4 patients out of every 10 with either of these conditions experienced at least a 50% reduction in pain intensity when prescribed gabapentin at dosages of 1800mg-3600 mg/day (gabapentin encarbil: 1200mg-3600 mg/day). This compared with only 1 or 2 out of every 10 given a placebo (an inactive treatment). People who had an improvement in pain relief with gabapentin are also expected to experience an improvement in sleep, fatigue, and in their mood.
This same Cochrane review reported that over half of those treated with gabapentin did not experience any worthwhile pain relief, but did experience side effects.
What type of nerve pain is gabapentin approved to treat?
Gabapentin is approved to treat nerve pain (neuralgia) that results from nerve damage. Gabapentin may be used to treat:
- Nerve pain caused by a herpes zoster viral infection, also known as shingles. This pain is called post-herpetic neuralgia (PHN), and it can be severe and chronic
- Nerve pain as a result of diabetic neuropathy, which happens when nerves in the feet damaged by diabetes cause chronic burning pain.
How does gabapentin work in nerve pain?
The exact way that gabapentin works to relieve pain is not known. It may change the way the body senses and reacts to pain. Gabapentin is used to manage long-term (chronic) pain, not to be taken for pain as needed. Chronic pain can interfere with sleep and work, and lead to depression.
How quickly does gabapentin work?
Studies show that pain relief may start within one week and reach a maximum effect in about 4 weeks. It can take this long because gabapentin is usually started at a low dose and gradually increased over time until it works.
For treating neuralgia, gabapentin is often started at 300 mg per day and gradually raised by 300 mg per day. One 2017 review of 37 studies found that pain relief usually occurs at a dose of 1,200 mg or more.
The same review compared gabapentin to an inactive medicine (placebo) in almost 6,000 adults with chronic pain from PHN or diabetic neuropathy. Study participants were given either gabapentin or a placebo for 4 to at least 12 weeks. The results showed that 30-40% of people taking gabapentin were able to reduce their pain by half or more, compared to 10-20% of people taking the placebo.
Although some people may get significant relief, others may have side effects without relief of pain. More than half of people taking gabapentin did not get significant relief and had side effects from the drug.
According to the review, about 60% of people taking gabapentin had side effects, including:
- Dizziness
- Sleepiness
- Water retention (edema)
- Clumsiness while walking (ataxia)
It does not typically make pain worse: In trials comparing gabapentin side effects to placebo side effects, only 1% of people reported increased pain, and this was the same for gabapentin and placebo.
Once you find the dose that relieves neuralgia for you, it is important not to stop taking it suddenly. Stopping suddenly can lead to withdrawal symptoms such as:
- Anxiety
- Insomnia
- Nausea
- Pain
- Sweating
- Food and Drug Administration (FDA). Neurontin. October 2017. Available at: https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/020235s064_020882s047_021129s046lbl.pdf [Accessed August 19, 2022].
- National Institutes of Health (NIH).
 Shingles. October 12, 2021. Available at: https://www.nia.nih.gov/health/shingles#long-term. [Accessed August 19, 2022].
Shingles. October 12, 2021. Available at: https://www.nia.nih.gov/health/shingles#long-term. [Accessed August 19, 2022]. - U.S. National Library of Medicine. Gabapentin. Updated May 2, 2022.Available at: https://www.ncbi.nlm.nih.gov/books/NBK493228/. [Accessed August 19, 2022].
- Wiffen PJ, Derry S, Bell RF, Rice ASC, Tölle T, Phillips T, Moore R. Gabapentin for chronic neuropathic pain in adults. Cochrane Database of Systematic Reviews 2017, Issue 6. Art. No.: CD007938. DOI: 10.1002/14651858.CD007938.pub4
Related medical questions
- Lyrica vs Gabapentin: What's the difference?
- Is gabapentin considered a painkiller?
- Does gabapentin cause weight gain?
- How long does gabapentin withdrawal last?
- How long does it take gabapentin to work?
- How does gabapentin make you feel?
- Is gabapentin a controlled substance / narcotic?
- Does gabapentin help you sleep?
- Is gabapentin safe for dogs?
- Does gabapentin cause constipation?
- Is gabapentin safe for cats?
Drug information
- Gabapentin Information for Consumers
- Gabapentin Information for Healthcare Professionals (includes dosage details)
- Side Effects of Gabapentin (detailed)
Related support groups
- Gabapentin (444 questions, 1,966 members)
- Pain (2,102 questions, 11,748 members)
- Neuralgia (116 questions, 388 members)
Medical Disclaimer
Finger numbness, pain in the ribs and changes in smell - is it from the nerves or something more serious? Speak by a neurologist - September 15, 2020
Sometimes low back pain hides a bunch of problems that can not be solved by relaxation techniques alone
Photo: DPA / TASS
Share
Are your fingers and toes numb? Maybe there were pains in the left half of the chest, or "stars" suddenly appeared before the eyes? If you have noticed the appearance of such symptoms in yourself, then this text is for you. We asked the neurologist Elena Krasilova about the possible root causes of these conditions, what is considered normal, how you can try to solve it yourself at the time the problem appears, and which doctor to contact later. Look for your problem and its solution.
Elena Krasilova — neurologist, candidate of medical sciences.
The causes of this condition can be arthrosis or arthritis of the small joints of the legs, an increase in uric acid salts, sometimes damage to the peripheral nerves (part of the nervous system outside the brain and spinal cord. - Author's note .), as well as a lack of trace elements and vitamins (calcium , magnesium, B vitamins and vitamin D).
In the absence of pathology, this condition can be observed in children, because sometimes their nervous system does not keep up with growth, as well as in case of physical overwork.
Tendency to the problem
Overweight people who eat a large amount of foods that increase uric acid, namely chocolate, red meat, alcohol, are most prone to this condition. Those who have elevated blood glucose levels are also at risk. Plays a role and hereditary predisposition to problems in the joints.
Solution
If you experience numbness and pain, you can try to take a comfortable position, conduct self-massage of the legs. If the pain is severe, then a single dose of an anesthetic can help, but you should not abuse the drugs. If this condition recurs or the pain does not go away, you should seek advice from a therapist who, after examination, will either recommend treatment or send you to a specialist (neurologist, orthopedist, rheumatologist) for further treatment.
The root cause of the changes
Sometimes numbness and crawling in the extremities can be caused by rheumatological diseases of the small joints, diseases of the veins or arteries of the lower extremities.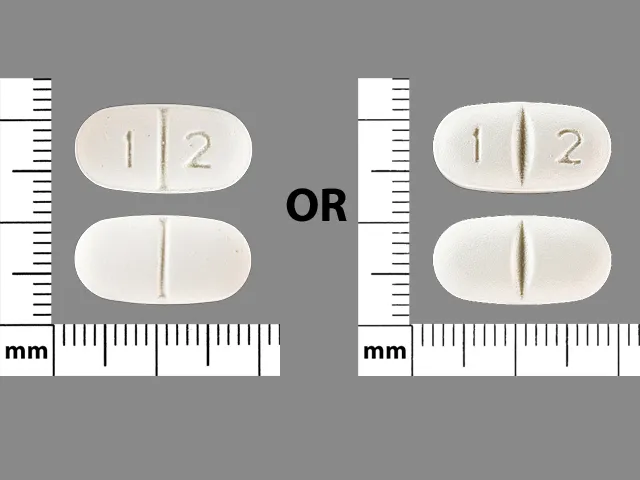 Neurological causes of these conditions are damage or traumatic injury to the peripheral nerves. In addition to injuries, the most common cause of peripheral nerve damage is alcohol abuse, the presence of diabetes mellitus and some other endocrine diseases and diseases of internal organs. In some patients, this condition is associated with nerve compression at the site of its passage in narrow bone-tendon canals (tunnels). The appearance of numbness and goosebumps in the limbs can also be observed in diseases of the spine (numbness in the legs - look for a problem in the lower back, numbness in the hands - in the cervical region), as well as in diseases such as stroke and multiple sclerosis (a disease that occurs in most cases in young people).
Neurological causes of these conditions are damage or traumatic injury to the peripheral nerves. In addition to injuries, the most common cause of peripheral nerve damage is alcohol abuse, the presence of diabetes mellitus and some other endocrine diseases and diseases of internal organs. In some patients, this condition is associated with nerve compression at the site of its passage in narrow bone-tendon canals (tunnels). The appearance of numbness and goosebumps in the limbs can also be observed in diseases of the spine (numbness in the legs - look for a problem in the lower back, numbness in the hands - in the cervical region), as well as in diseases such as stroke and multiple sclerosis (a disease that occurs in most cases in young people).
Can numbness and goosebumps occur in normal limbs?
Yes, this condition can be observed if a person has been in a certain position for a long time, for example, he squatted for a long time or lay with his arm thrown under his head for a long time. This becomes more common with age.
This becomes more common with age.
But if you have this condition after an injury or is permanent, it is not normal, you need to go to the doctor, notes the neurologist.
Tendency to the problem
Limbs are more likely to become numb in people with a sedentary lifestyle, in people with increased body weight, in people whose work is associated with constant stay at the computer, especially if the workplace is not properly organized, in people who whose work is connected with being in a long forced position. Also prone to the problem are those who have a hereditary predisposition to the narrowness of the channels through which the nerve passes.
Decision
Avoid forced awkward positions of the limbs, alcohol abuse, control body weight and blood glucose levels. If this condition occurs after being in an uncomfortable position, self-massage will help to improve blood flow and nourish the nerve. It is necessary to adhere to adequate physical activity, strengthen the muscles of the back and abdominals (if the problem is caused by a disease of the spine).
Who will help?
If numbness or tingling occurs constantly and is not associated with a forced position, then it is necessary to consult a general practitioner or neurologist to determine the cause and prescribe treatment.
The root cause of the changes
According to Elena Krasilova, this problem may be associated with impaired blood circulation in the brain (in particular, with impaired circulation through the vertebral arteries), which can be observed with a stroke, problems in the cervical spine, and sometimes with a disturbance in the work of the heart. Eye diseases (sometimes requiring immediate medical attention) can also be the cause. The reason may be an increase or decrease in blood pressure.
The degree of manifestation is within the normal range
There is no norm here. It is necessary to contact an ophthalmologist, cardiologist or neurologist (depending on the cause of the blurred vision).
Problem susceptibility
Eye disease, cervical spine problems, blood pressure problems, and heart problems.
Solution
Seek professional help. Before visiting a specialist, you can try to normalize blood pressure, try to give your eyes a rest.
Who will help?
Optometrist and neurologist, cardiologist.
The root cause of changes
Nature put us on our feet, but did not think over the protection of the spine. Animals, for example, do not have problems with the spine if there is no injury. Pain can be associated both with problems in the spinal column and with spasm of the muscles surrounding the spine (for example, during hypothermia, during intense physical exertion, diseases of internal organs), there may also be a congenital "weakness" (insufficiency) of the connective tissue (which forms including the linkage).
The degree of manifestation is within the normal range
Pain is not the norm, there should be no discomfort.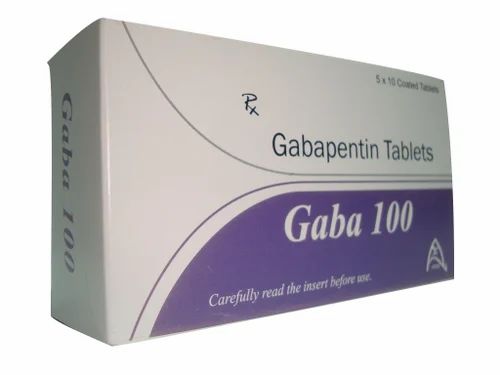
Tendency to the problem
More often back problems are observed in people who lead a sedentary lifestyle, have increased or decreased body weight, whose work is associated with excessive physical exertion. Women have an additional risk factor - pregnancy.
Solution
In some cases, pain medication, massage, therapeutic exercises can help. If the pain bothers you for more than 3-5 days, it is better to contact a specialist for an examination and receive the necessary treatment.
Who will help?
You need to contact a neurologist or a therapist, these specialists, if necessary, can refer you for a consultation with an orthopedist, rheumatologist, gynecologist, and sometimes an endocrinologist.
Neurologist Elena Krasilova
Photo: Timofey Kalmakov
Share
The root cause of the changes
The problem may be related to the lumbar spine, lumbar muscle spasm and problems in the hip joint.
The degree of manifestation is within the normal range
If this happens once, then you should not panic, if the problem recurs, you should consult a doctor.
Solution
Relaxation techniques can be tried to relieve muscle tension.
Where to go?
Neurologists, orthopedists, rheumatologists will help you solve this problem (depending on the cause that caused this condition).
The root cause of changes
Odors change when there are problems in the ENT organs or pathological changes in the brain - tumors, circulatory disorders, craniocerebral injuries. Also, the cause may be irritation of the nasal mucosa with pairs of caustic substances (whiteness, ammonia, etc.). In addition, a change in smells can be a precursor to an epileptic attack and the onset of a migraine attack.
The degree of manifestation is within the normal range
If the odors disappeared for a short time after inhaling caustic vapors or in the presence of nasal diseases, then you should not panic.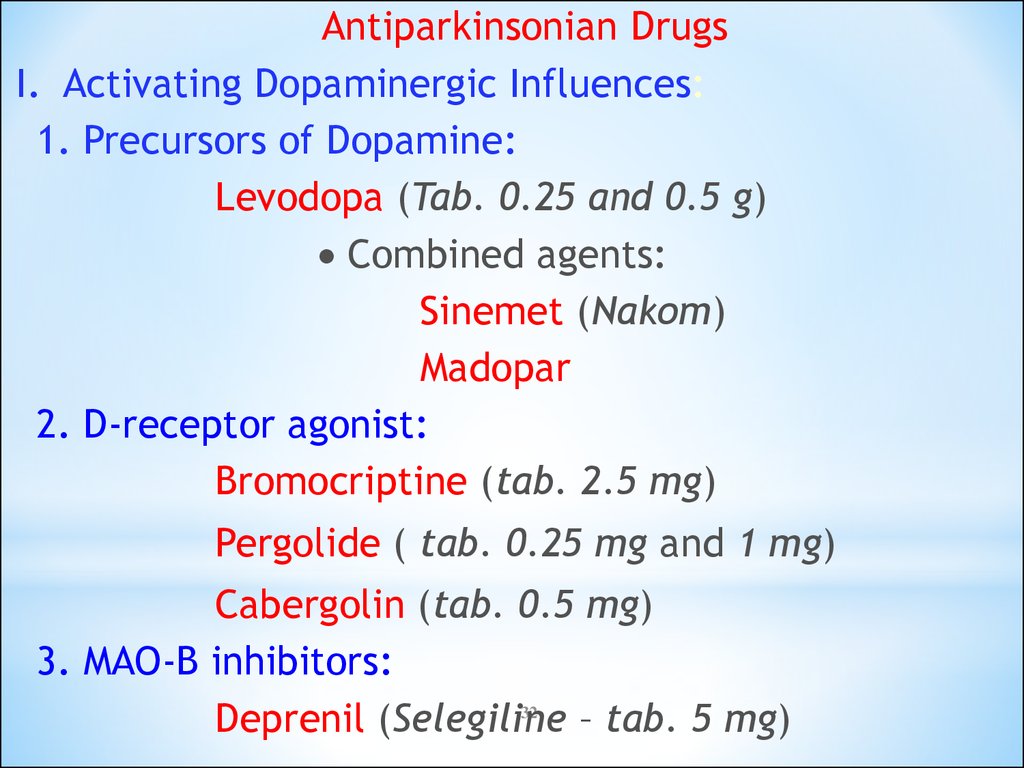 If the odors disappear for no apparent reason or if the smell is persistent, you should contact a specialist.
If the odors disappear for no apparent reason or if the smell is persistent, you should contact a specialist.
Solution
The only thing that can be done before contacting a specialist is to treat the nasal mucosa with a solution of sea water (Aquamaris, Aqualor) or saline.
Where to go?
First, you should contact an ENT doctor, who, if necessary, will refer you to another specialist. If the odors change or disappear before the onset of headaches, or this is followed by a disorientation in the surrounding space, numbness of the torso or convulsions, then immediately go to a neurologist.
The root cause of the changes
Intercostal neuralgia occurs for various reasons. More often, the cause is herpes zoster, inflammation of the intercostal muscles (myositis), injury to the ribs, less commonly, problems in the thoracic spine can also be the cause. But the most dangerous cause of such pain is a myocardial infarction or an angina attack.
The degree of manifestation is within the normal range
Normally, there is no pain in the chest without a reason.
Tendency to the problem
The problem can occur in people who work hard, or in a sedentary lifestyle, with frequent hypothermia, in the presence of diseases of the cardiovascular system (increased blood pressure) or the presence of heart disease.
Solution
If you are sure that this is intercostal neuralgia, and not the heart, you can take a comfortable position, relax, drink an anesthetic, and then consult a specialist. If the pain arose for the first time and is pronounced, does not go away at rest - urgently call an ambulance.
Where to go?
Any pain on the left is an indication for an electrocardiogram to rule out damage to the heart muscle. If everything is fine there, then to neurologists, and in the presence of herpetic eruptions in the intercostal space - to infectious disease specialists.
Chest pain can be a harbinger of a heart attack, so don't delay it, go see a doctor
Photo: Timur Sharipkulov / Ufa1.RU
Share
be diseases of the nervous system, such as essential tremor, Parkinson's disease, multiple sclerosis, damage to the cerebellum (the part of the brain responsible for balance. - approx. aut. ), acquired dementia (dementia), alcoholism, the consequences of tick-borne encephalitis, trauma to the peripheral nerve and some others. Also, this condition can be observed in the pathology of the endocrine system (thyrotoxicosis, diabetes mellitus), poisoning with toxic substances, excessive coffee consumption, vitamin B12 deficiency, stress, excessive physical overexertion.
The degree of manifestation is within the normal range
The norm can be considered if the tremor occurs during excitement (if this does not interfere with a person in his professional and personal life) or after excessive physical exertion.
Tendency to the problem
We must not forget that tremors can manifest themselves in people who abuse alcohol. The tendency to have essential tremor is inherited.
Solution
Find out the cause, if possible, eliminate the provoking factor, take medications prescribed by the doctor.
Where to go?
If you are concerned about this problem, see a neurologist. Sometimes a therapist can deal with a problem if the cause is not in the pathology of the nervous system.
The root cause of the changes
It can be glaucoma and other eye diseases, increased or decreased blood pressure, atherosclerosis of the vessels that feed the retina and neck vessels, cerebrovascular accident (stroke), poisoning with certain drugs, lack of trace elements (for example, iron, vitamin B12 and folic acid in the development of anemia). As well as a sharp rise from a lying or sitting position.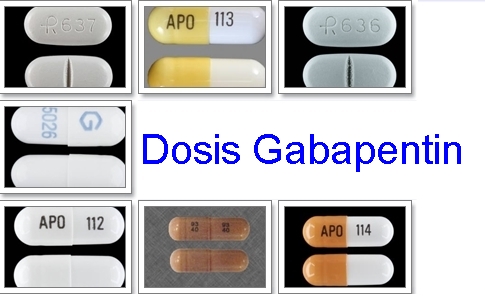
The degree of manifestation is within the normal range
If this condition occurs with a sudden change in position and there are no other symptoms that disturb the person, it does not require treatment. In other cases, it is necessary to find and eliminate the cause.
Tendency to the problem
This condition is possible due to eye fatigue due to a long stay at the computer.
Solution
The most important thing is to properly organize the workplace, relax your eyes - look out the window during breaks, and not at the phone. If it does not help, we run to the doctor.
Where to go?
Optometrist, neurologist.
The root cause of changes
This happens with orthostatic hypotension - redistribution of blood from the head to the lower extremities.
Degree of manifestation within the normal range
This can be normal or abnormal. Norm - if a person was sitting and jumped up abruptly, tall and thin people are especially prone to this state. In diseases of the endocrine system, as well as in the elderly, this is an additional factor in falls and requires treatment. This condition can be caused by drugs.
Norm - if a person was sitting and jumped up abruptly, tall and thin people are especially prone to this state. In diseases of the endocrine system, as well as in the elderly, this is an additional factor in falls and requires treatment. This condition can be caused by drugs.
Tendency to the problem
This problem often occurs in the elderly, as well as tall and thin people (due to the fact that the blood does not quickly have time to redistribute through the vessels).
Decision
The doctor recommends that you control your actions and try not to get up abruptly. If you still feel dizzy, then take a comfortable position - sit back or lie down and raise your legs at an angle of 45 degrees.
Where to go?
If the problem occurs frequently, then your specialist is a cardiologist, if necessary and the exclusion of cardiac pathology, he will redirect you to a neurologist.
The root cause of the changes
There are two types of headaches - primary and secondary. Primary ones occur in the absence of diseases that can cause headaches - hypertension, tumors in the brain, infectious diseases, heart disease, diabetes mellitus, lung diseases, pathology of the temporomandibular joint and others. Primary headaches include migraine (throbbing unilateral headache), tension headache (muscle spasm, when the head is squeezed by a hoop), cluster headache (shooting pain in the eye area, lacrimation) and some others.
Primary ones occur in the absence of diseases that can cause headaches - hypertension, tumors in the brain, infectious diseases, heart disease, diabetes mellitus, lung diseases, pathology of the temporomandibular joint and others. Primary headaches include migraine (throbbing unilateral headache), tension headache (muscle spasm, when the head is squeezed by a hoop), cluster headache (shooting pain in the eye area, lacrimation) and some others.
Tendency to the problem
Migraines are more common in women, cluster headaches are mostly in men, tension headaches occur with physical and mental overstrain, problems in the cervical spine, after traumatic brain injuries. Some foods, alcohol, lack of sleep or, conversely, an excess of sleep, stress, weather changes can provoke headaches.
Solution
Determine in what situations a headache occurs, if possible, avoid provoking factors, observe the daily routine. If headaches occur, try to relax, take an anesthetic. It should be prescribed by a doctor: it must be remembered that the abuse of painkillers in itself provokes a headache.
It should be prescribed by a doctor: it must be remembered that the abuse of painkillers in itself provokes a headache.
Where to go?
With this problem, you need to go to a neurologist.
Neuropathic pain: diagnosis - Pro Palliative
Contents
Instrumental diagnostic methods
Questionnaires
Neuropathic pain can be compared to an out-of-tune piano: the keys work, the legs and pedals are in place, but it is clear from the sound that the instrument is out of order. Outwardly, the nerve may look normal, but if you apply special diagnostic methods to a person with neuropathic pain, it turns out that the structure of the nerve is disturbed, and, accordingly, its function. The diagnosis of neuropathic pain consists of three parts: the patient's description of the pain, the location of the pain, and the nature of the pain. The first thing a doctor does when neuropathic pain is suspected is to examine the patient and take an anamnesis.
Neuropathic pain is characterized by very bright markers and verbal descriptors - a sensation of an electric current, a burn from an iron or spilled boiling water. Patients do not always call it pain, more often they complain of uncomfortable sensations of burning, numbness, shooting.
The patient's words about how he feels this pain and experiences it should always be decisive in the diagnosis of pain. Of course, patients can be confused in definitions and call pain mental discomfort, anxiety, painful experiences. The doctor's task is to determine whether a person has pain and understand what kind of pain it is.
Referring to the International Association for the Study of Pain (IASP) definition of pain, pain is physical and emotional suffering, an agonizing and unpleasant sensation. The vague definition of pain reflects our perceptions of how difficult pain can sometimes be to diagnose. Due to the difference in perceptions, the difficulties in describing one's feelings, it would be wrong to rely only on the patient's words about the sensations of pain, and we use two more criteria.
Essential criterion for the diagnosis of pain - assessment of localization , places where pain arises and spreads.
If the injury described by the patient as an agonizing sensation coincides with the area of innervation of a particular nerve, we consider that this structure is highly likely to be damaged. To establish a diagnosis, it is very important that these two blocks converge as contour maps.
Patients may change their sensitivity to neuropathic pain over time, as the process of its distribution is very dynamic and involves more and more parts of the nervous system. So, in the zone of primary damage, the patient may, on the contrary, have a feeling of anesthesia or numbness. If a person feels pain in the right leg, and upon examination, the doctor sees symptoms in the left, it is possible that the process in the right leg has already gone too far, and in the left it is just beginning.
The third diagnostic criterion is the nature of the pain . Neuropathic pain is more common in patients at rest. When a person moves, is distracted by something, incoming impulses from nearby zones can, as it were, “interrupt” neuropathic pain. And it starts to hurt at night, when the patient is resting and doing nothing. The person tries to sleep, but the pain becomes like a beacon in the night. Excruciating sensations, suffering at rest is a very characteristic sign of neuropathic pain, especially at the beginning of its development. In the future, the pain becomes more and more difficult to characterize.
Neuropathic pain is more common in patients at rest. When a person moves, is distracted by something, incoming impulses from nearby zones can, as it were, “interrupt” neuropathic pain. And it starts to hurt at night, when the patient is resting and doing nothing. The person tries to sleep, but the pain becomes like a beacon in the night. Excruciating sensations, suffering at rest is a very characteristic sign of neuropathic pain, especially at the beginning of its development. In the future, the pain becomes more and more difficult to characterize.
MRI, CT and ultrasound as diagnostic methods
Instrumental diagnostic methods are prescribed by a doctor if the description of pain and the area of nerve innervation do not match or the pain is unstable and migrates. With the help of computed tomography (CT) or ultrasound of the nervous system, a violation of the structure of the nerve can be seen. Magnetic resonance imaging (MRI) is prescribed if the doctor suggests compression of the vascular bundle or joint deformity. Also, these methods are used to exclude serious pathologies: tumors, aneurysms, neurodegenerative, autoimmune diseases with damage to the nervous system.
Also, these methods are used to exclude serious pathologies: tumors, aneurysms, neurodegenerative, autoimmune diseases with damage to the nervous system.
“Pain is determined not by the degree of damage, but by how the nervous system perceives damage” Neurologist Maxim Churyukanov on the biopsychosocial model of pain
However, doctors do not fully rely on the results of instrumental diagnostics. In the case of neuropathic pain, they are of little diagnostic value. The fact is that during instrumental examination, non-specific changes can be detected that can lead away from identifying the real cause of pain. People are different and arranged a little differently. If such changes do not bring discomfort to a person, they are normal, in addition, with age they usually become more and more. The most striking example is that detected in almost all people according to the results of any radiation method for studying osteochondrosis. Such changes occur in a person with age, they are natural and cannot be the cause of pain and other symptoms. Since it is usually not possible to find an unambiguous cause of pain using instrumental diagnostics, the value of such an examination is not high.
Such changes occur in a person with age, they are natural and cannot be the cause of pain and other symptoms. Since it is usually not possible to find an unambiguous cause of pain using instrumental diagnostics, the value of such an examination is not high.
Moreover, there is no point in sending pictures to the doctor with captions: “Look, I have pain somewhere here.” There can be a bunch of different changes in the picture that do not hurt, and the cause remains invisible. Therefore, MRI, CT and ultrasound should be performed only on the recommendation of a doctor, if he considers it necessary. And the results should be looked at only through the prism of examination and conversation with the doctor.
If we talk about peripheral nerves, then damage can be found in them with an accuracy of up to a centimeter. But before looking, you need to understand the cause of the pain and decide on the localization of the search.
Questionnaires
Questionnaires are necessary for the doctor at the stage of the first meeting with the patient.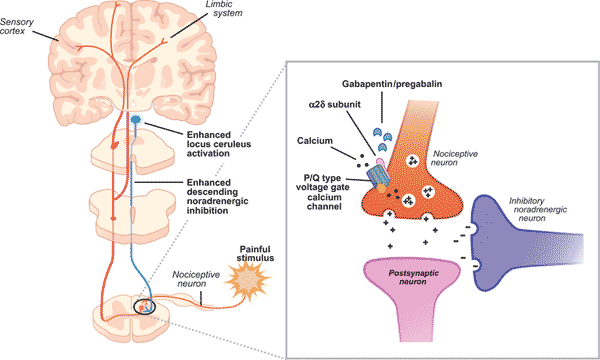 They take into account the subjective experience of the patient, his complaints and feelings. Questionnaires help the specialist summarize the information received and conclude whether the probability of neuropathic pain in a particular patient is high.
They take into account the subjective experience of the patient, his complaints and feelings. Questionnaires help the specialist summarize the information received and conclude whether the probability of neuropathic pain in a particular patient is high.
The most popular questionnaire is Pain Detect, which takes into account only the patient's feelings. Other questionnaires usually have a part that is filled out by the doctor based on the results of the examination. Typically, clinics use simple questionnaires with no more than ten questions that address the most common problems. The fewer questions and tests, the easier and faster it is to fill out the questionnaire, the more convenient it is for both the doctor and the patient. Of course, by minimizing information, we risk missing something important.
But there is another extreme, when the questionnaires include dozens of questions in several blocks, covering all aspects of the patient's life, including social and sexual activity. For example, the Canadian McGill Pain Questionnaire (MPQ) is incredibly difficult to perform.
For example, the Canadian McGill Pain Questionnaire (MPQ) is incredibly difficult to perform.
As a college educated person who has been dealing with pain for more than ten years, I was unable to complete this questionnaire. Now imagine a 70-year-old grandmother to whom I will give out these 20 questionnaire sheets: it will most likely be more interesting than a crossword puzzle, but it will take more than one week.
As an inquisitive person, as a scientist, I try to test the methods of diagnostics and treatment on myself before offering them to patients. When choosing a questionnaire, you need to find a balance between simplicity, speed and routine questionnaires with complex diagnostic systems, as well as take into account the patient's cognitive abilities.
Pain relief by ambulance What to do if an ambulance refuses to go to a person with breakthrough pain
We try not to overestimate this possibility and not treat questionnaires as a serious diagnostic tool. A low score on the questionnaire does not mean that the patient does not have neuropathic pain. And, unfortunately, the scattering of patient comments and mosaic of examination data cannot always be summarized with one figure in the questionnaire.
A low score on the questionnaire does not mean that the patient does not have neuropathic pain. And, unfortunately, the scattering of patient comments and mosaic of examination data cannot always be summarized with one figure in the questionnaire.
Reference information from questionnaires may be a reason for additional or closer diagnostics. Let's say a patient comes in with a typical nociceptive pain clinic, but the questionnaire suddenly reveals a high probability of neuropathic pain. As a doctor, I understand what conversation tactics should be chosen, I ask more questions, modify the examination and look at his complaints through this prism. Sometimes the data in the questionnaire may be the reason for a neurophysiological examination.
Rarely, however, the data in the questionnaire can be the basis for choosing a treatment method. Suppose a person experiences mixed pain, but complains about the neuropathic component, which means that it gives him more suffering and feelings.