Does depression affect sleep
SAMHSA’s National Helpline | SAMHSA
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.
Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders.
This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative. Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs. In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems.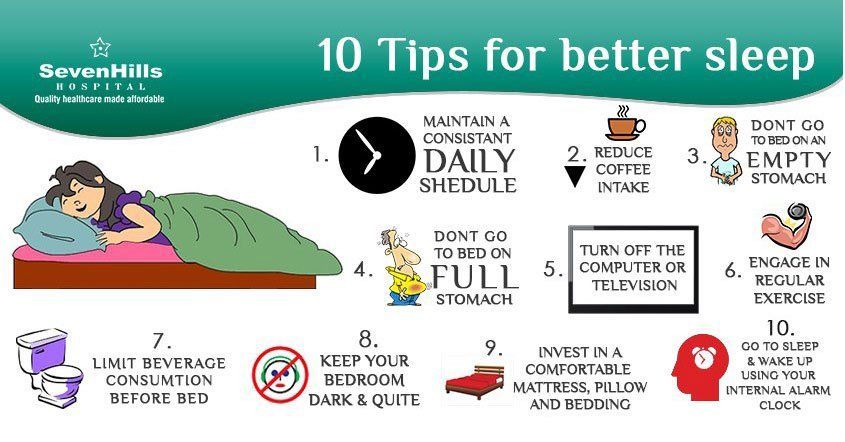 Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.
Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt. Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse. Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.
Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.For additional resources, please visit the SAMHSA Store.
Last Updated: 08/30/2022
Alcohol, Tobacco, and Other Drugs
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Misusing alcohol, tobacco, and other drugs can have both immediate and long-term health effects.The misuse and abuse of alcohol, tobacco, illicit drugs, and prescription medications affect the health and well-being of millions of Americans. NSDUH estimates allow researchers, clinicians, policymakers, and the general public to better understand and improve the nation’s behavioral health. These reports and detailed tables present estimates from the 2021 National Survey on Drug Use and Health (NSDUH).
Alcohol
Data:
- Among the 133.1 million current alcohol users aged 12 or older in 2021, 60.0 million people (or 45.1%) were past month binge drinkers. The percentage of people who were past month binge drinkers was highest among young adults aged 18 to 25 (29.2% or 9.8 million people), followed by adults aged 26 or older (22.4% or 49.3 million people), then by adolescents aged 12 to 17 (3.8% or 995,000 people). (2021 NSDUH)
- Among people aged 12 to 20 in 2021, 15.1% (or 5.9 million people) were past month alcohol users. Estimates of binge alcohol use and heavy alcohol use in the past month among underage people were 8.3% (or 3.2 million people) and 1.6% (or 613,000 people), respectively. (2021 NSDUH)
- In 2020, 50.0% of people aged 12 or older (or 138.5 million people) used alcohol in the past month (i.e., current alcohol users) (2020 NSDUH)
- Among the 138.5 million people who were current alcohol users, 61.6 million people (or 44.
 4%) were classified as binge drinkers and 17.7 million people (28.8% of current binge drinkers and 12.8% of current alcohol users) were classified as heavy drinkers (2020 NSDUH)
4%) were classified as binge drinkers and 17.7 million people (28.8% of current binge drinkers and 12.8% of current alcohol users) were classified as heavy drinkers (2020 NSDUH) - The percentage of people who were past month binge alcohol users was highest among young adults aged 18 to 25 (31.4%) compared with 22.9% of adults aged 26 or older and 4.1% of adolescents aged 12 to 17 (2020 NSDUH)
- Excessive alcohol use can increase a person’s risk of stroke, liver cirrhosis, alcoholic hepatitis, cancer, and other serious health conditions
- Excessive alcohol use can also lead to risk-taking behavior, including driving while impaired. The Centers for Disease Control and Prevention reports that 29 people in the United States die in motor vehicle crashes that involve an alcohol-impaired driver daily
Programs/Initiatives:
- STOP Underage Drinking interagency portal - Interagency Coordinating Committee on the Prevention of Underage Drinking
- Interagency Coordinating Committee on the Prevention of Underage Drinking
- Talk.
 They Hear You.
They Hear You. - Underage Drinking: Myths vs. Facts
- Talking with your College-Bound Young Adult About Alcohol
Relevant links:
- National Association of State Alcohol and Drug Abuse Directors
- Department of Transportation Office of Drug & Alcohol Policy & Compliance
- Alcohol Policy Information Systems Database (APIS)
- National Institute on Alcohol Abuse and Alcoholism
Tobacco
Data:
- In 2020, 20.7% of people aged 12 or older (or 57.3 million people) used nicotine products (i.e., used tobacco products or vaped nicotine) in the past month (2020 NSDUH)
- Among past month users of nicotine products, nearly two thirds of adolescents aged 12 to 17 (63.1%) vaped nicotine but did not use tobacco products. In contrast, 88.9% of past month nicotine product users aged 26 or older used only tobacco products (2020 NSDUH)
- Tobacco use is the leading cause of preventable death, often leading to lung cancer, respiratory disorders, heart disease, stroke, and other serious illnesses.
 The CDC reports that cigarette smoking causes more than 480,000 deaths each year in the United States
The CDC reports that cigarette smoking causes more than 480,000 deaths each year in the United States - The CDC’s Office on Smoking and Health reports that more than 16 million Americans are living with a disease caused by smoking cigarettes
Electronic cigarette (e-cigarette) use data:
- In 2021, 13.2 million people aged 12 or older (or 4.7%) used an e-cigarette or other vaping device to vape nicotine in the past month. The percentage of people who vaped nicotine was highest among young adults aged 18 to 25 (14.1% or 4.7 million people), followed by adolescents aged 12 to 17 (5.2% or 1.4 million people), then by adults aged 26 or older (3.2% or 7.1 million people).
- Among people aged 12 to 20 in 2021, 11.0% (or 4.3 million people) used tobacco products or used an e-cigarette or other vaping device to vape nicotine in the past month. Among people in this age group, 8.1% (or 3.1 million people) vaped nicotine, 5.4% (or 2.1 million people) used tobacco products, and 3.
 4% (or 1.3 million people) smoked cigarettes in the past month. (2021 NSDUH)
4% (or 1.3 million people) smoked cigarettes in the past month. (2021 NSDUH) - Data from the Centers for Disease Control and Prevention’s 2020 National Youth Tobacco Survey. Among both middle and high school students, current use of e-cigarettes declined from 2019 to 2020, reversing previous trends and returning current e-cigarette use to levels similar to those observed in 2018
- E-cigarettes are not safe for youth, young adults, or pregnant women, especially because they contain nicotine and other chemicals
Resources:
- Tips for Teens: Tobacco
- Tips for Teens: E-cigarettes
- Implementing Tobacco Cessation Programs in Substance Use Disorder Treatment Settings
- Synar Amendment Program
Links:
- Truth Initiative
- FDA Center for Tobacco Products
- CDC Office on Smoking and Health
- National Institute on Drug Abuse: Tobacco, Nicotine, and E-Cigarettes
- National Institute on Drug Abuse: E-Cigarettes
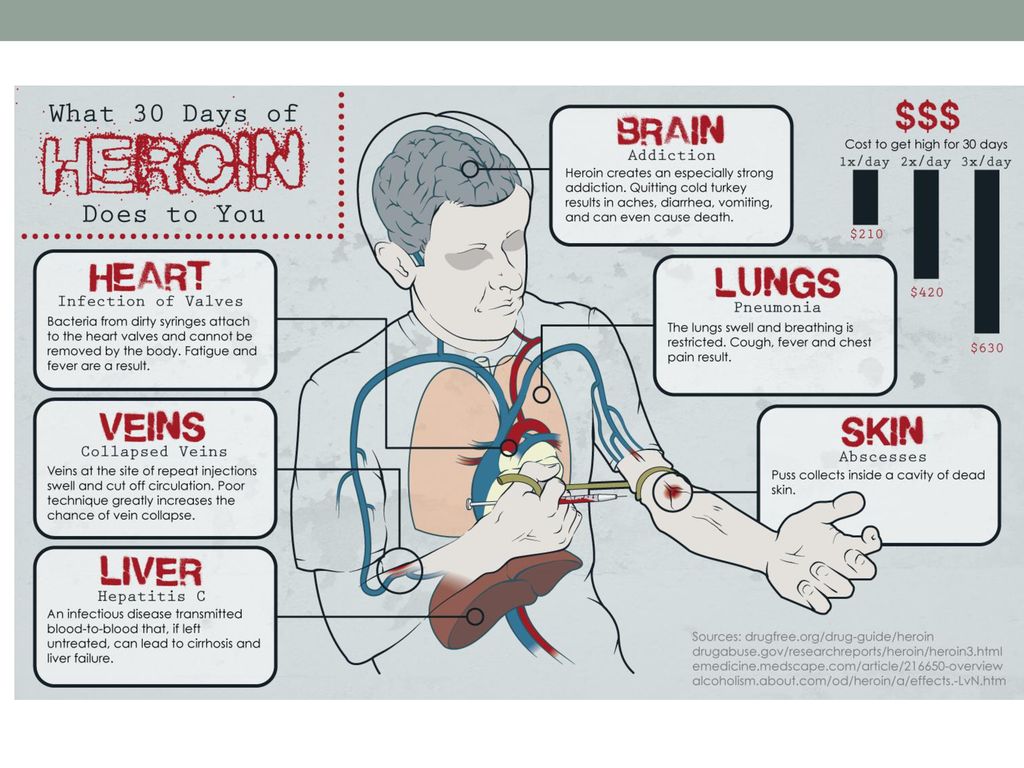
Opioids
Data:
- Among people aged 12 or older in 2021, 3.
 3% (or 9.2 million people) misused opioids (heroin or prescription pain relievers) in the past year. Among the 9.2 million people who misused opioids in the past year, 8.7 million people misused prescription pain relievers compared with 1.1 million people who used heroin. These numbers include 574,000 people who both misused prescription pain relievers and used heroin in the past year. (2021 NSDUH)
3% (or 9.2 million people) misused opioids (heroin or prescription pain relievers) in the past year. Among the 9.2 million people who misused opioids in the past year, 8.7 million people misused prescription pain relievers compared with 1.1 million people who used heroin. These numbers include 574,000 people who both misused prescription pain relievers and used heroin in the past year. (2021 NSDUH) - Among people aged 12 or older in 2020, 3.4% (or 9.5 million people) misused opioids in the past year. Among the 9.5 million people who misused opioids in the past year, 9.3 million people misused prescription pain relievers and 902,000 people used heroin (2020 NSDUH)
- According to the Centers for Disease Control and Prevention’s Understanding the Epidemic, an average of 128 Americans die every day from an opioid overdose
Resources:
- Medications for Substance Use Disorders
- Opioid Overdose Prevention Toolkit
- TIP 63: Medications for Opioid Use Disorder
- Use of Medication-Assisted Treatment for Opioid Use Disorder in Criminal Justice Settings
- Opioid Use Disorder and Pregnancy
- Clinical Guidance for Treating Pregnant and Parenting Women With Opioid Use Disorder and Their Infants
- The Facts about Buprenorphine for Treatment of Opioid Addiction
- Pregnancy Planning for Women Being Treated for Opioid Use Disorder
- Tips for Teens: Opioids
- Rural Opioid Technical Assistance Grants
- Tribal Opioid Response Grants
- Provider’s Clinical Support System - Medication Assisted Treatment Grant Program
Links:
- National Institute on Drug Abuse: Opioids
- National Institute on Drug Abuse: Heroin
- HHS Prevent Opioid Abuse
- Community Anti-Drug Coalitions of America
- Addiction Technology Transfer Center (ATTC) Network
- Prevention Technology Transfer Center (PTTC) Network
Marijuana
Data:
- In 2021, marijuana was the most commonly used illicit drug, with 18.
 7% of people aged 12 or older (or 52.5 million people) using it in the past year. The percentage was highest among young adults aged 18 to 25 (35.4% or 11.8 million people), followed by adults aged 26 or older (17.2% or 37.9 million people), then by adolescents aged 12 to 17 (10.5% or 2.7 million people).
7% of people aged 12 or older (or 52.5 million people) using it in the past year. The percentage was highest among young adults aged 18 to 25 (35.4% or 11.8 million people), followed by adults aged 26 or older (17.2% or 37.9 million people), then by adolescents aged 12 to 17 (10.5% or 2.7 million people). - The percentage of people who used marijuana in the past year was highest among young adults aged 18 to 25 (34.5%) compared with 16.3% of adults aged 26 or older and 10.1% of adolescents aged 12 to 17 (2020 NSDUH)
- Marijuana can impair judgment and distort perception in the short term and can lead to memory impairment in the long term
- Marijuana can have significant health effects on youth and pregnant women.
Resources:
- Know the Risks of Marijuana
- Marijuana and Pregnancy
- Tips for Teens: Marijuana
Relevant links:
- National Institute on Drug Abuse: Marijuana
- Addiction Technology Transfer Centers on Marijuana
- CDC Marijuana and Public Health
Emerging Trends in Substance Misuse:
- Methamphetamine—In 2019, NSDUH data show that approximately 2 million people used methamphetamine in the past year.
 Approximately 1 million people had a methamphetamine use disorder, which was higher than the percentage in 2016, but similar to the percentages in 2015 and 2018. The National Institute on Drug Abuse Data shows that overdose death rates involving methamphetamine have quadrupled from 2011 to 2017. Frequent meth use is associated with mood disturbances, hallucinations, and paranoia.
Approximately 1 million people had a methamphetamine use disorder, which was higher than the percentage in 2016, but similar to the percentages in 2015 and 2018. The National Institute on Drug Abuse Data shows that overdose death rates involving methamphetamine have quadrupled from 2011 to 2017. Frequent meth use is associated with mood disturbances, hallucinations, and paranoia. - Cocaine—In 2019, NSDUH data show an estimated 5.5 million people aged 12 or older were past users of cocaine, including about 778,000 users of crack. The CDC reports that overdose deaths involving have increased by one-third from 2016 to 2017. In the short term, cocaine use can result in increased blood pressure, restlessness, and irritability. In the long term, severe medical complications of cocaine use include heart attacks, seizures, and abdominal pain.
- Kratom—In 2019, NSDUH data show that about 825,000 people had used Kratom in the past month. Kratom is a tropical plant that grows naturally in Southeast Asia with leaves that can have psychotropic effects by affecting opioid brain receptors.
 It is currently unregulated and has risk of abuse and dependence. The National Institute on Drug Abuse reports that health effects of Kratom can include nausea, itching, seizures, and hallucinations.
It is currently unregulated and has risk of abuse and dependence. The National Institute on Drug Abuse reports that health effects of Kratom can include nausea, itching, seizures, and hallucinations.
Resources:
- Tips for Teens: Methamphetamine
- Tips for Teens: Cocaine
- National Institute on Drug Abuse
More SAMHSA publications on substance use prevention and treatment.
Last Updated: 03/22/2023
Sleep disorders in anxiety and anxiety-depressive disorders | Kovrov G.V., Lebedev M.A., Palatov S.Yu., Merkulova T.B., Posokhov S.I.
In clinical practice, sleep disorders are usually associated with anxiety and depression. Existing studies show a close relationship between sleep disorders and anxiety and depressive disorders [1, 2]. A clear dependence of the severity of the course of both groups of diseases on concomitant sleep disorders was shown [1]. In general somatic practice, the prevalence of insomnia reaches 73% [3], in borderline psychiatry, clinically defined insomnia occurs in 65%, and changes in nocturnal sleep according to polysomnography are noted in 100% of cases [4].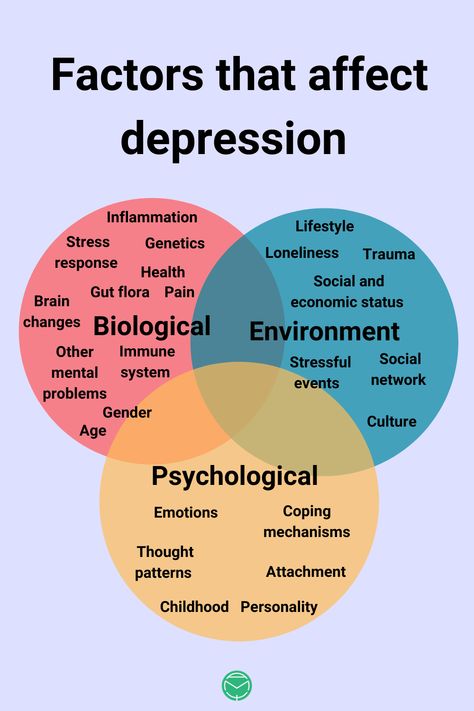
Combination of sleep disorders and anxiety disorders
It is known that the relationship between sleep disorders and anxiety disorders is noted, on the one hand, when sleep disorders can provoke the development of anxiety disorders [5], and on the other hand, when the onset of an anxiety disorder precedes the onset of sleep disorders. Complaints about problems associated with sleep are typical for patients with all diseases included in the group of anxiety disorders. In the case of major generalized disorder and post-traumatic stress disorder (PTSD), sleep disturbances are one of the criteria required for a diagnosis. There are objective reasons for the development of sleep disorders within anxiety disorders, namely: anxiety is manifested by increased cortical activation, which entails the difficulty of falling asleep and maintaining sleep.
In the clinic, anxiety is manifested by anxiety, irritability, motor excitation, decreased concentration of attention, increased fatigue [6].
The most striking manifestation of anxiety disorders is generalized anxiety disorder (GAD), which is diagnosed on the basis of the presence of at least 3 of the following symptoms: restlessness, fatigue, difficulty concentrating, irritability, muscle tension, sleep disturbances. The duration of the disease should be at least 6 months, the symptoms should cause psychosomatic discomfort and / or social disadaptation.
Sleep disorders in this situation are one of the 6 diagnostic criteria for GAD. The main symptom of GAD, excessive, persistent anxiety, is a major predisposing factor in the development of insomnia. Insomnia and GAD are closely related, usually comorbid disorders. The difference between insomnia in anxiety disorder and primary insomnia, not associated with other diseases, is the nature of the experiences in the process of falling asleep. In the case of GAD, the patient is concerned about current problems [7] (work, study, relationships), which hinders the process of falling asleep.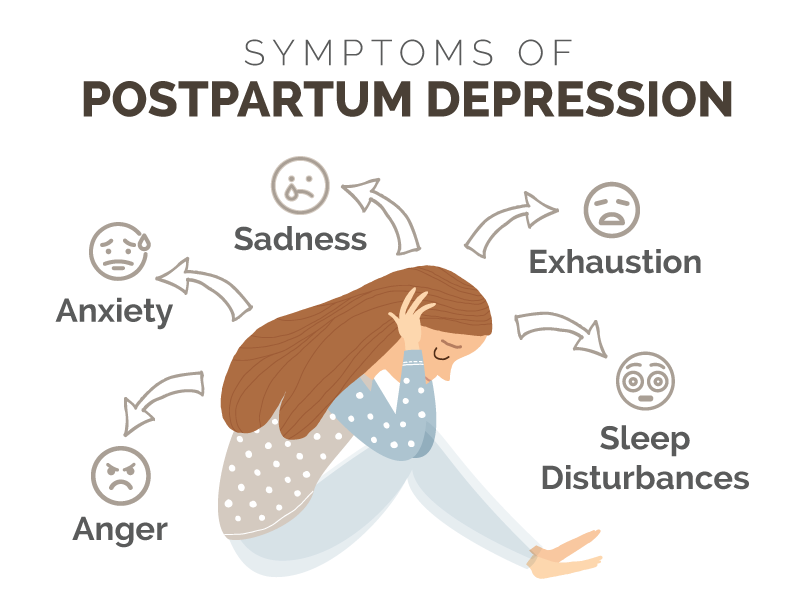 In the case of primary insomnia, the anxiety itself is caused by the disease itself.
In the case of primary insomnia, the anxiety itself is caused by the disease itself.
A polysomnographic study can reveal changes characteristic of insomnia: increased time to fall asleep, frequent awakenings, reduced sleep efficiency, and a decrease in its total duration.
Another striking example of anxiety disorders is panic disorder, which is manifested by recurrent states of severe anxiety (panic). Attacks are accompanied by phenomena of depersonalization and derealization, as well as severe autonomic disorders. In the behavior of the patient, avoidance of situations in which the attack occurred for the first time is noted. There may be a fear of loneliness, a repetition of the attack. A panic attack occurs spontaneously, outside of formal situations of danger or threat.
Panic disorder is more common in women and typically begins around the age of 20. A hallmark of panic disorder are spontaneous episodes of panic attacks, characterized by bouts of fear, anxiety, and other autonomic manifestations.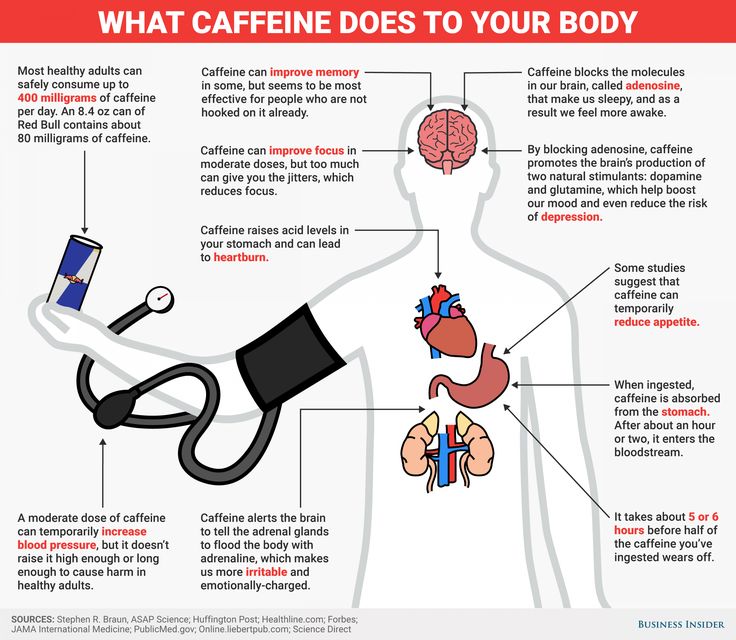 About 2/3 of patients with this disorder experience some form of sleep disturbance. Patients complain of difficulty falling asleep, non-restorative sleep, and characteristic nocturnal panic attacks. It should be noted that the presence of certain problems associated with sleep can lead to aggravation of anxiety disorders, including panic disorder.
About 2/3 of patients with this disorder experience some form of sleep disturbance. Patients complain of difficulty falling asleep, non-restorative sleep, and characteristic nocturnal panic attacks. It should be noted that the presence of certain problems associated with sleep can lead to aggravation of anxiety disorders, including panic disorder.
Polysomnographic examination can detect frequent awakenings, reduced sleep efficiency and a reduction in its total duration [8]. It is not uncommon to see depression coexisting with anxiety disorders, and it is possible that the presence of other changes in sleep patterns in patients with panic disorder is associated with comorbid depression, and therefore the diagnosis of depression should be ruled out in patients with similar sleep disorders.
The sleep paralysis characteristic of narcolepsy can also occur with panic disorder. It is a movement paralysis that occurs during falling asleep or waking up, during which patients experience fear, a feeling of pressure in the chest, and other somatic manifestations of anxiety.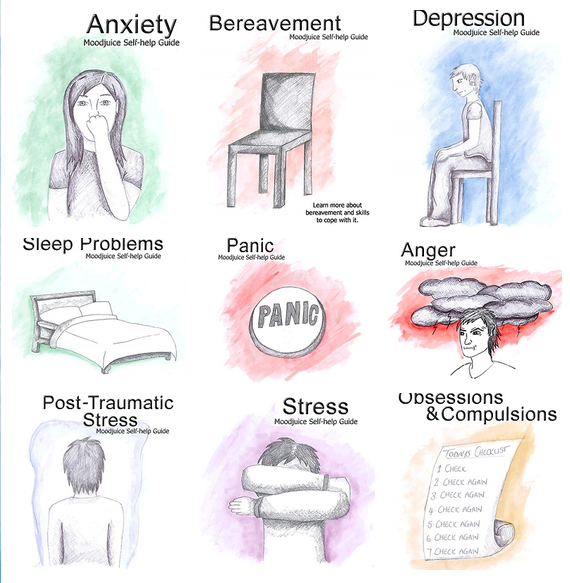 This symptom also occurs in patients with post-traumatic stress disorder.
This symptom also occurs in patients with post-traumatic stress disorder.
Nighttime panic attacks are a common occurrence in this disease [9]. They are manifested by a sudden awakening and all the symptoms characteristic of panic attacks. Awakening occurs during the phase of non-REM sleep, which most likely excludes their connection with dreams. It was also found that nocturnal attacks are an indicator of a more severe course of the disease. It must be remembered that patients, fearing the recurrence of such episodes, deprive themselves of sleep, which leads to more serious disorders and, in general, reduces the quality of life of these patients.
PTSD is a disease from the group of anxiety disorders, in which sleep disturbances are a diagnostic criterion. Sleep disorders in this disease include 2 main symptoms: nightmares and insomnia. Other phenomena inherent in PTSD and associated with sleep are: somnambulism, sleep-talking, hypnagogic and hypnopompic hallucinations.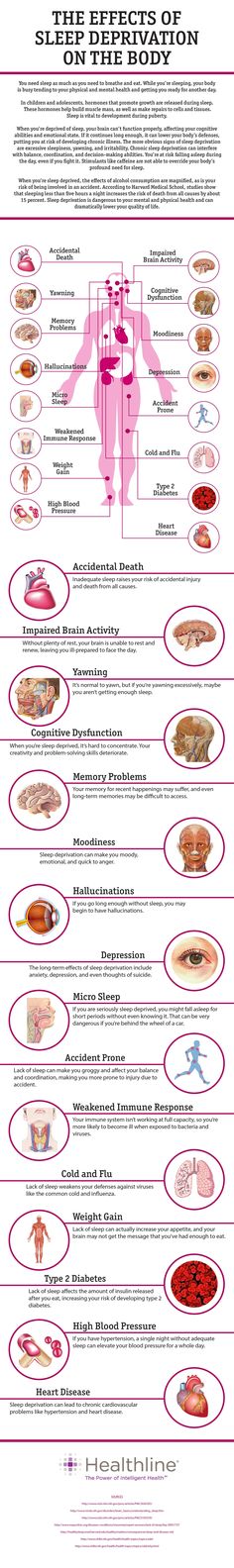 The changes detected by polysomnography are not specific and in some cases may be absent. Possible changes include: an increase in the representation of the 1st stage of sleep, a decrease in the representation of the 4th stage of sleep. Also, with PTSD, breathing disorders during sleep are often found.
The changes detected by polysomnography are not specific and in some cases may be absent. Possible changes include: an increase in the representation of the 1st stage of sleep, a decrease in the representation of the 4th stage of sleep. Also, with PTSD, breathing disorders during sleep are often found.
Agoraphobia can also be a manifestation of anxiety disorders, which is defined as anxiety that occurs in response to situations, the way out of which, according to the patient, is difficult. In the clinical picture, as a rule, there is a persistent fear of the patient to be in a crowded place, public places (shops, open squares and streets, theaters, cinemas, concert halls, workplaces), fear of independent long trips (by various modes of transport). The situational component of the agoraphobia syndrome is expressed in the confinement of phobic experiences to certain situations and in the fear of getting into situations in which, according to patients, a repetition of painful sensations is likely. Often, agoraphobic symptoms cover many fears of various situations, forming panagoraphobia - the fear of leaving the house with the development of deep social maladaptation. There are attempts by the patient to overcome their own experiences, in adverse cases, there is a restriction of social activity.
Often, agoraphobic symptoms cover many fears of various situations, forming panagoraphobia - the fear of leaving the house with the development of deep social maladaptation. There are attempts by the patient to overcome their own experiences, in adverse cases, there is a restriction of social activity.
Specific phobias are characterized by an association of anxiety with certain situations (air travel, contact with animals, the sight of blood, etc.), also accompanied by an avoidance reaction. Patients are critical of their experiences, however, phobias have a significant impact on various areas of activity of patients. There are the following forms: cardiophobia, cancerophobia, claustrophobia, etc. Sleep disturbances in these patients are non-specific, and from the point of view of the patient, they are a minor manifestation of the disease.
In general, the most common manifestations of sleep disturbances in anxiety states are presomnic disorders. The initial phase of sleep consists of 2 components: drowsiness, a kind of craving for sleep, and actually falling asleep.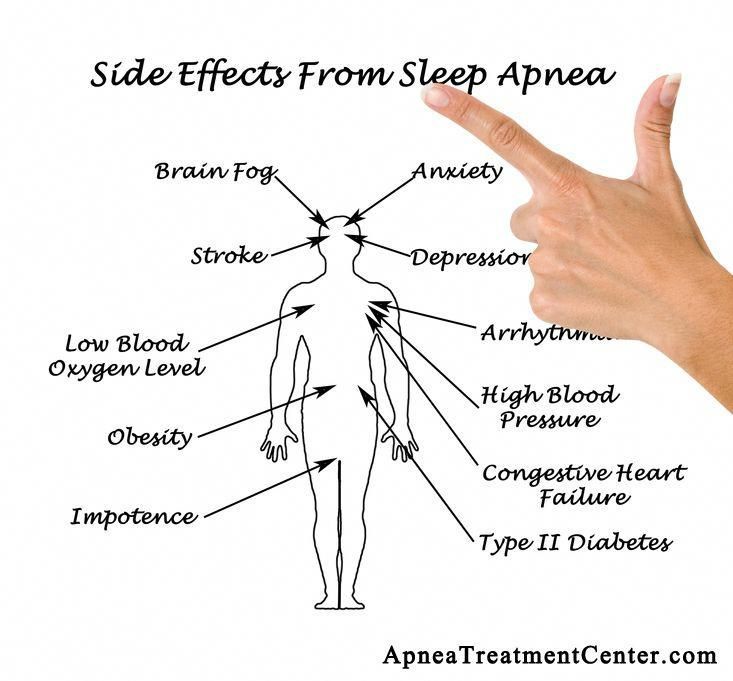 Often, patients have no desire to sleep, no desire to sleep, muscle relaxation does not occur, they have to perform various actions aimed at falling asleep. In other cases, there is an inclination to sleep, but its intensity is reduced, drowsiness becomes intermittent, undulating. Drowsiness occurs, the muscles relax, the perception of the environment decreases, the patient takes a comfortable position for falling asleep, and a slight drowsiness appears, but soon it is interrupted, disturbing thoughts and ideas arise in the mind. In the future, the state of wakefulness is again replaced by mild drowsiness and superficial drowsiness. Such changes in states can be repeated several times, leading to emotional discomfort that prevents the onset of sleep.
Often, patients have no desire to sleep, no desire to sleep, muscle relaxation does not occur, they have to perform various actions aimed at falling asleep. In other cases, there is an inclination to sleep, but its intensity is reduced, drowsiness becomes intermittent, undulating. Drowsiness occurs, the muscles relax, the perception of the environment decreases, the patient takes a comfortable position for falling asleep, and a slight drowsiness appears, but soon it is interrupted, disturbing thoughts and ideas arise in the mind. In the future, the state of wakefulness is again replaced by mild drowsiness and superficial drowsiness. Such changes in states can be repeated several times, leading to emotional discomfort that prevents the onset of sleep.
In a number of patients, experiences about disturbed sleep can acquire an overvalued hypochondriacal coloration and come to the fore according to the mechanisms of actualization, often there is an obsessive fear of insomnia - agripnophobia. It is usually combined with an anxious and painful expectation of sleep, certain requirements for others and the creation of the above-mentioned special conditions for sleep.
It is usually combined with an anxious and painful expectation of sleep, certain requirements for others and the creation of the above-mentioned special conditions for sleep.
Anxiety depression is characterized by the patient's constant experience of anxiety, a sense of impending danger and insecurity. Anxious experiences change: anxiety about their loved ones, fears about their condition, their actions. The structure of anxious depression, as a rule, includes anxiety, feelings of guilt, motor restlessness, fussiness, fluctuations in affect with worsening in the evening, and somatovegetative symptoms. Anxious and melancholy affects often occur simultaneously, in many cases it is impossible to determine which of them is leading in the patient. Anxiety depression is most often found in people of involutionary age and proceeds according to the type of protracted phases. In addition, it is actually the leading type of neurotic depression [10].
The patient exhibits a variety of symptoms of anxiety and depression.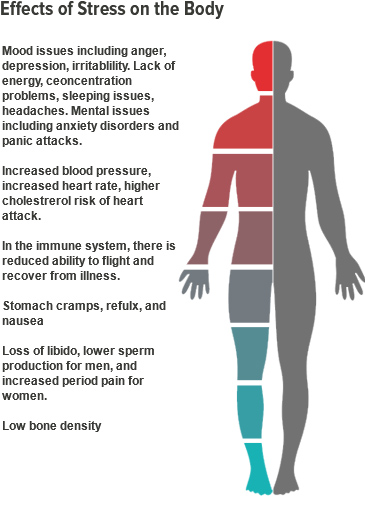 Initially, one or more physical symptoms (eg, fatigue, pain, sleep disturbances) may be present. Further questioning allows us to state a depressive mood and/or anxiety.
Initially, one or more physical symptoms (eg, fatigue, pain, sleep disturbances) may be present. Further questioning allows us to state a depressive mood and/or anxiety.
Signs of anxiety depression:
- depressed mood;
- loss of interest;
- severe anxiety.
The following symptoms are also often seen:
- sleep disorders;
- physical weakness and loss of energy;
- fatigue or reduced activity;
- difficulty concentrating, fidgeting;
- impaired concentration;
- excitation or retardation of movements or speech;
- appetite disorders;
- dry mouth;
- tension and anxiety;
- irritability;
- tremor;
- heartbeat;
- dizziness;
- suicidal thoughts.
Often with anxiety depression, variants of presomnic disorders are observed, in which the desire to sleep is pronounced, drowsiness increases rapidly, and the patient falls asleep relatively easily, but wakes up suddenly after 5-10 minutes, drowsiness completely disappears, and then within 1-2 hours he does not can fall asleep. This period without sleep is characterized by unpleasant ideas, thoughts, fears, reflecting to a greater or lesser extent the experienced conflict situation and the reaction to the inability to sleep. There is also hyperesthesia to sensory stimuli. Those suffering from this form of sleep disorder react extremely painfully to the slightest sensory stimuli, up to flashes of affect.
This period without sleep is characterized by unpleasant ideas, thoughts, fears, reflecting to a greater or lesser extent the experienced conflict situation and the reaction to the inability to sleep. There is also hyperesthesia to sensory stimuli. Those suffering from this form of sleep disorder react extremely painfully to the slightest sensory stimuli, up to flashes of affect.
For disturbed falling asleep, lengthening of the drowsy period is characteristic. This drowsy state is often accompanied by motor, sensory and visceral automatisms, sharp shudders, vivid perceptions of sounds and visual images, palpitations, sensations of muscle spasms. Often these phenomena, awakening the patient, cause various painful ideas and fears, sometimes acquiring an obsessive character.
Sleep disorders and their polysomnographic manifestations among mental illnesses are the most studied for depressive disorder. Among the sleep disorders in depressive disorder, insomnia is the most common. The severity and duration of insomnia are manifestations of a more severe depressive disorder, and the appearance of insomnia during remission indicates the imminent occurrence of a recurrent depressive episode [1]. In addition, sleep disorders in this disease are the most persistent symptom. The close relationship of this disorder with sleep disorders is explained by the biochemical processes characteristic of depression. In particular, in depressive disorder, there is a decrease in the level of serotonin, which plays a role in the initiation of REM sleep and the organization of delta sleep [11]. Depressive disorder is characterized by the following manifestations of sleep disturbances: difficulty falling asleep [10], non-restorative sleep, as a rule, reduced total sleep time. The most specific symptoms for depression are frequent nocturnal awakenings and early terminal awakenings. Complaints about difficulty falling asleep are more often observed in young patients, and frequent awakenings are more characteristic of the elderly [12].
The severity and duration of insomnia are manifestations of a more severe depressive disorder, and the appearance of insomnia during remission indicates the imminent occurrence of a recurrent depressive episode [1]. In addition, sleep disorders in this disease are the most persistent symptom. The close relationship of this disorder with sleep disorders is explained by the biochemical processes characteristic of depression. In particular, in depressive disorder, there is a decrease in the level of serotonin, which plays a role in the initiation of REM sleep and the organization of delta sleep [11]. Depressive disorder is characterized by the following manifestations of sleep disturbances: difficulty falling asleep [10], non-restorative sleep, as a rule, reduced total sleep time. The most specific symptoms for depression are frequent nocturnal awakenings and early terminal awakenings. Complaints about difficulty falling asleep are more often observed in young patients, and frequent awakenings are more characteristic of the elderly [12].
With masked depression, complaints of sleep disturbances may be the only manifestation of the disease. In depression, in contrast to primary insomnia, there are complaints of sleep disturbances typical of this disease: frequent awakenings, early morning awakening, etc. [12].
In polysomnographic study, the following changes are observed: an increase in the time to fall asleep, a decrease in sleep efficiency. The most common and depressive disorder-specific symptoms are shortened REM sleep latency and reduced delta sleep. It has been found that patients with a higher proportion of delta sleep stay in remission longer than those with a decrease in the proportion of delta sleep [13].
Attempts have been made to explore the possibility of using depression-specific sleep disturbances as markers of depressive disorder. Due to the heterogeneity of the manifestations of sleep disorders, this issue remains not fully resolved.
The features of sleep disorders in various types of depression were also highlighted. For patients with a predominance of the anxious component, difficulty falling asleep and early awakenings are more characteristic. With this type of depression, dream plots are associated with persecution, threats, etc. In addition, in these patients, in general, there was a high level of wakefulness before falling asleep. For depressions with the leading affect of melancholy, early morning awakenings and dreams of static types of gloomy content are most characteristic. Depression with the affect of apathy is characterized by early awakenings and rare, unsaturated dreams. Also typical of depression with apathetic affect is the loss of a sense of boundaries between sleep and wakefulness. Patients with bipolar disorder have a similar polysomnographic pattern [14].
For patients with a predominance of the anxious component, difficulty falling asleep and early awakenings are more characteristic. With this type of depression, dream plots are associated with persecution, threats, etc. In addition, in these patients, in general, there was a high level of wakefulness before falling asleep. For depressions with the leading affect of melancholy, early morning awakenings and dreams of static types of gloomy content are most characteristic. Depression with the affect of apathy is characterized by early awakenings and rare, unsaturated dreams. Also typical of depression with apathetic affect is the loss of a sense of boundaries between sleep and wakefulness. Patients with bipolar disorder have a similar polysomnographic pattern [14].
Features of sleep disturbance in bipolar disorder are a significant decrease in the duration of sleep during a manic episode and a greater tendency of patients to hypersomnia during depressive episodes compared with the unipolar course of the disorder.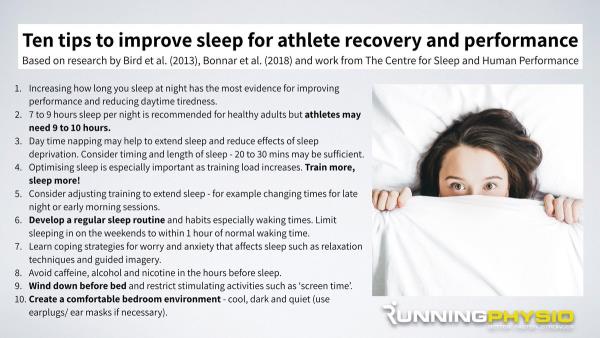 Complaints of sleep disturbances during manic episodes are usually absent.
Complaints of sleep disturbances during manic episodes are usually absent.
Treatment
For the treatment of anxiety and depressive disorders, drugs of various pharmacological groups are used: tranquilizers (mainly long-acting or short-acting benzodiazepine drugs), selective serotonin reuptake inhibitors, selective serotonin reuptake stimulants, tricyclic antidepressants. All these drugs, to one degree or another, affect a person’s sleep, making it easier to fall asleep, reducing the number and duration of nocturnal awakenings, thereby affecting the recovery processes that occur during a night’s sleep. When constructing tactics for the treatment of sleep disorders associated with anxiety and depressive manifestations, it is important to remember that insomnia itself can increase anxiety, worsen well-being, mood, as a rule, in the morning hours after poor sleep [15]. In this regard, the use of hypnotics in the treatment may be promising in the presence of a predominance of insomnia symptoms in the clinical picture in order to prevent exacerbation of anxiety and depressive disorders.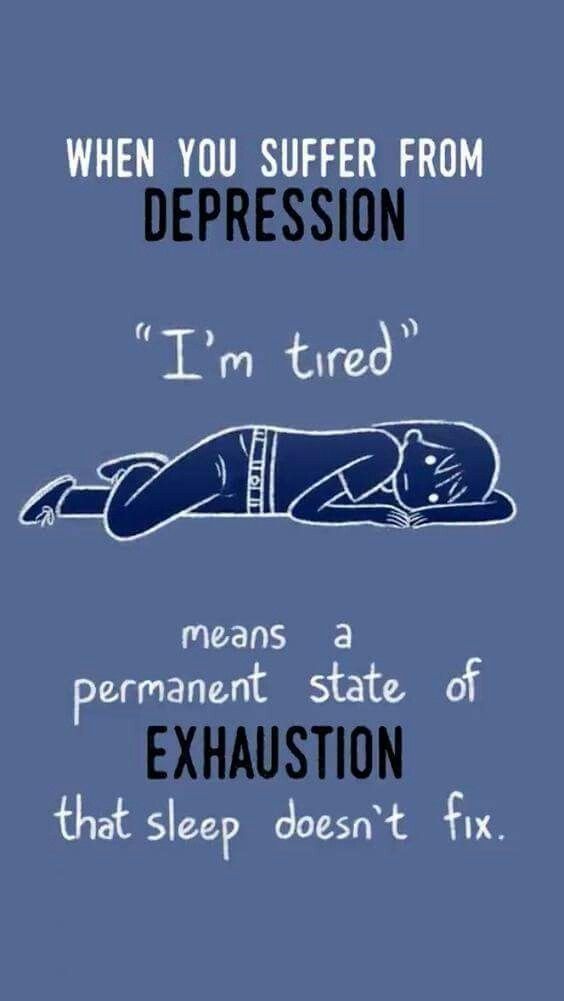 In this regard, the most effective helpers can be sleeping pills that affect the GABAergic (GABA - γ-aminobutyric acid) system - histamine receptor blockers (Valocordin®-Doxylamine) and melatonin preparation. The most convenient to use in the treatment of insomnia is Valocordin®-Doxylamine, which is available in drops, which allows you to select an individual dose of the drug.
In this regard, the most effective helpers can be sleeping pills that affect the GABAergic (GABA - γ-aminobutyric acid) system - histamine receptor blockers (Valocordin®-Doxylamine) and melatonin preparation. The most convenient to use in the treatment of insomnia is Valocordin®-Doxylamine, which is available in drops, which allows you to select an individual dose of the drug.
Valocordin®-Doxylamine is a unique drug used as a hypnotic. Most known hypnotic drugs (benzodiazepines, cyclopyrrolones, imidazopyridines, etc.) act on the GABAergic complex, activating the activity of somnogenic systems, while histamine receptor blockers act on wakefulness systems, not sleep ones, reducing their activation. A fundamentally different mechanism of hypnotic action makes it possible to use Valocordin®-Doxylamine more widely: when changing one drug to another, reducing the dosages of "habitual hypnotics", and also, if necessary, canceling hypnotics.
A drug study conducted on healthy subjects showed that doxylamine succinate leads to a decrease in the duration of nocturnal awakenings and stage 1 sleep and an increase in stage 2 without a significant effect on the duration of stages 3 and 4 sleep and REM sleep.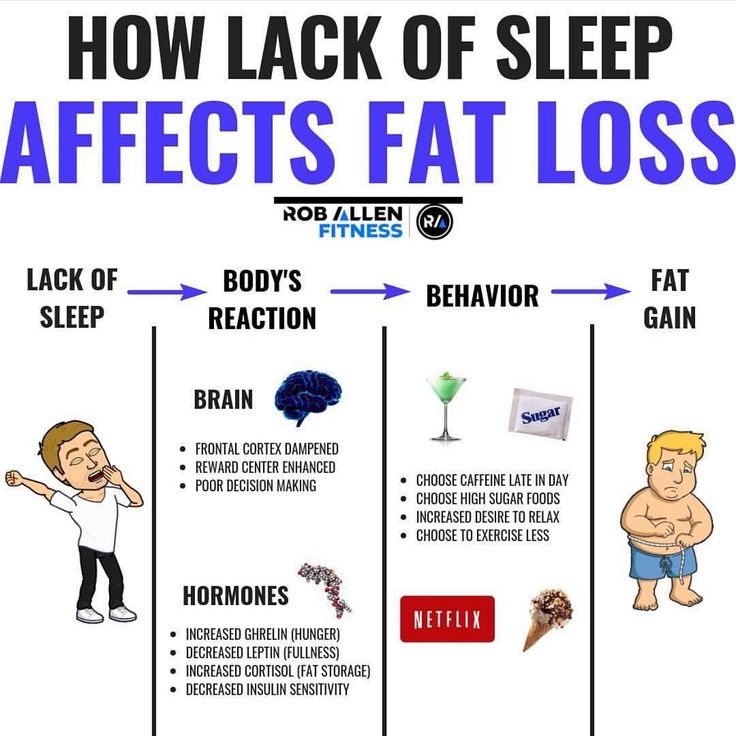 There was no significant subjective effect on the reports of healthy volunteers, however, compared with placebo, doxylamine increased the depth of sleep and improved its quality [16].
There was no significant subjective effect on the reports of healthy volunteers, however, compared with placebo, doxylamine increased the depth of sleep and improved its quality [16].
In Russia, one of the first studies was carried out under the supervision of A.M. Wayne [17]. It has been shown that under the influence of doxylamine such subjective characteristics of sleep as the duration of falling asleep, the duration and quality of sleep, the number of night awakenings and the quality of morning awakenings improve. An analysis of the objective characteristics of sleep showed that while taking doxylamine, there was a reduction in the time of wakefulness during sleep, a decrease in the duration of falling asleep, an increase in the duration of sleep, the time of the REM sleep phase, and the sleep quality index. It was also shown that doxylamine did not reduce the effectiveness of other drugs in patients, such as antihypertensive, vasoactive, etc. The results of a study of the effect of doxylamine on patients with insomnia indicate the effectiveness of this drug in these patients.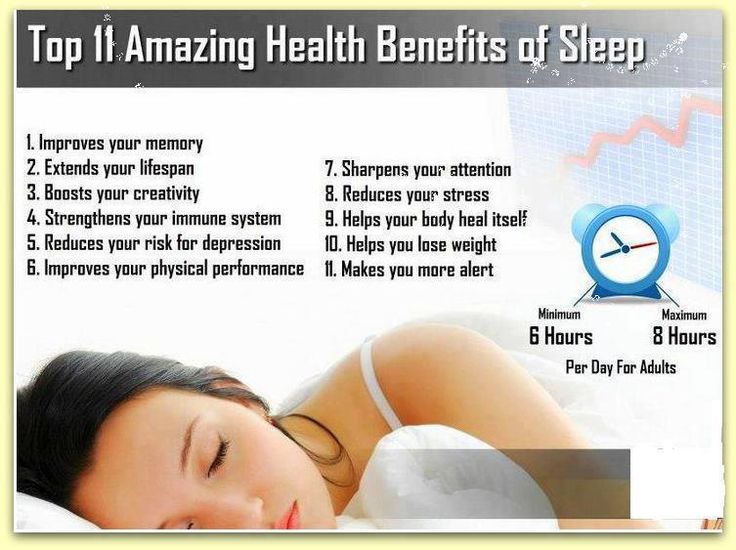 Subjective feelings of a positive effect are confirmed by objective studies of the structure of sleep, which undergoes positive shifts, which affect such indicators as sleep duration, falling asleep duration, REM sleep phase. Of great importance is also the absence of any changes in the results of personal data regarding drowsiness and sleep apnea syndrome, which indicates the absence of an aftereffect of the drug in relation to the worsening of the course of obstructive sleep apnea syndrome. However, if obstructive sleep apnea is suspected, doxylamine should be used with caution.
Subjective feelings of a positive effect are confirmed by objective studies of the structure of sleep, which undergoes positive shifts, which affect such indicators as sleep duration, falling asleep duration, REM sleep phase. Of great importance is also the absence of any changes in the results of personal data regarding drowsiness and sleep apnea syndrome, which indicates the absence of an aftereffect of the drug in relation to the worsening of the course of obstructive sleep apnea syndrome. However, if obstructive sleep apnea is suspected, doxylamine should be used with caution.
Modern clinical studies do not reveal serious side effects in the treatment of therapeutic doses of the drug, but it is always necessary to remember the possible appearance of symptoms that arise due to the individual characteristics of the body, and contraindications (glaucoma; difficulty urinating due to benign prostatic hyperplasia; age up to 15 years; increased drug sensitivity).
Simultaneous administration of the drug Valocordin®-Doxylamine and sedative drugs that affect the central nervous system (CNS): neuroleptics, tranquilizers, antidepressants, hypnotics, analgesics, anesthetics, antiepileptic drugs, may enhance their effect. Procarbazines and antihistamines should be combined with caution to minimize CNS depression and possible drug potentiation. During treatment with Valocordin®-Doxylamine, alcohol should be avoided as it may unpredictably affect the effects of doxylamine succinate.
Procarbazines and antihistamines should be combined with caution to minimize CNS depression and possible drug potentiation. During treatment with Valocordin®-Doxylamine, alcohol should be avoided as it may unpredictably affect the effects of doxylamine succinate.
During the use of this drug, it is recommended to exclude driving a car and working with mechanisms, as well as other activities accompanied by an increased risk, at least at the first stage of treatment. The attending physician is advised to evaluate the individual reaction rate when choosing a dose. It is important to consider these features of the effect of the drug in the treatment of patients with insomnia in order to increase the effectiveness of Valocordin®-Doxylamine and exclude possible undesirable effects.
Conclusion
When diagnosing a disease, it is important to remember that, as a rule, problems falling asleep indicate the presence of severe anxiety, early awakenings are a manifestation of depression. When choosing treatment tactics at all stages of the development of anxiety-depressive syndrome (ADS), the appointment of modern hypnotic drugs at the stage of unexpressed TDS is a promising tactic aimed at reducing the risk of a further increase in symptoms of anxiety and depression.
When choosing treatment tactics at all stages of the development of anxiety-depressive syndrome (ADS), the appointment of modern hypnotic drugs at the stage of unexpressed TDS is a promising tactic aimed at reducing the risk of a further increase in symptoms of anxiety and depression.
No sleep, no rest for the tormented soul
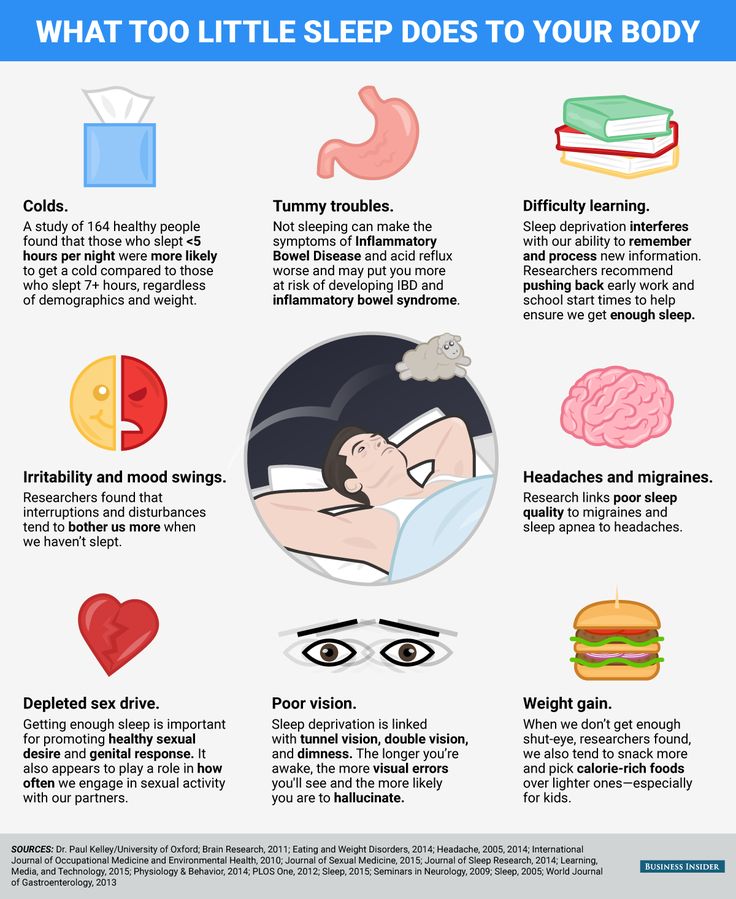
Sleep is one of the basic needs of the human body, and its lack leads to severe psychological and physical stress: not only mood and cognitive abilities suffer, but also the cardiovascular system and metabolism. Nevertheless, for almost 50 years, sleep deprivation has been trying to treat one of the most difficult and terrible conditions for the human psyche - depression. We set out to explore what forced sleep therapy for psychiatric disorders is, why it can be effective, and why it should be used with caution.
Anyone who has not slept for a long time at least once knows perfectly well what this is fraught with: lethargy appears, attention decreases, mood deteriorates and severe physical fatigue occurs.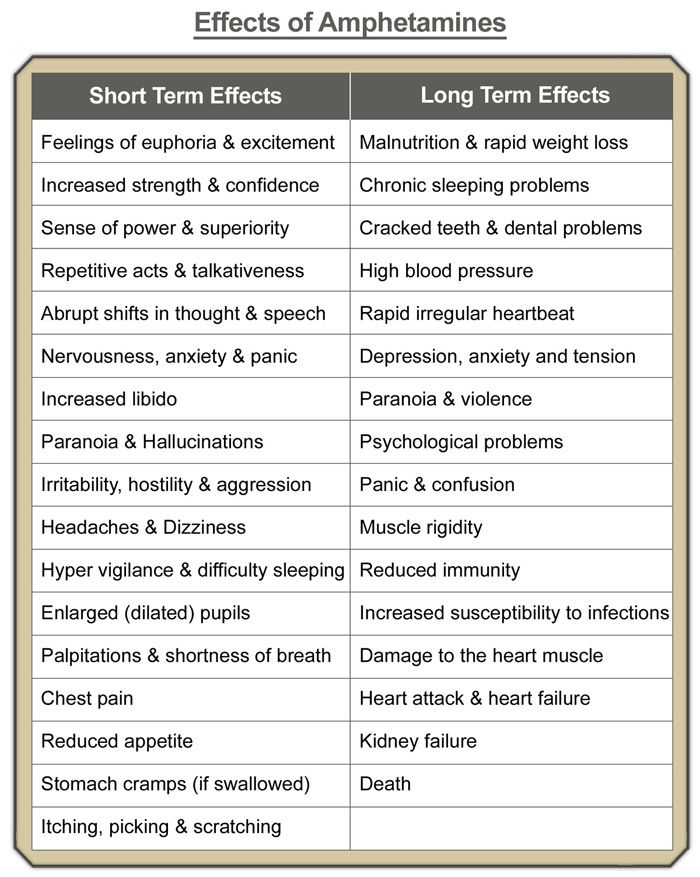 Available stimulants like caffeine stop working (their mechanism of action is rather limited), and the only way out is to take a break and still rest.
Available stimulants like caffeine stop working (their mechanism of action is rather limited), and the only way out is to take a break and still rest.
In chronic sleep deprivation and insomnia (we talked about it in detail in the material “Your words rock well”, prepared for World Sleep Day last year), deeper and more serious conditions and diseases are added to superficial symptoms.
For example, the consequences of lack of sleep include cardiovascular disease, nutritional and metabolic problems (from overeating to type 2 diabetes), and various mental disorders. Last but not least, lack of sleep is closely associated with depression, which is surprising in its own way, because sleep deprivation is often used to treat it, and at times quite successfully.
At least that's what the meta-analyses suggest. One, conducted in 2017, focuses on 66 studies published since 1974 to 2016: it states that sleep deprivation is effective in 50 percent of patients in randomized control trials and 45 percent in other studies.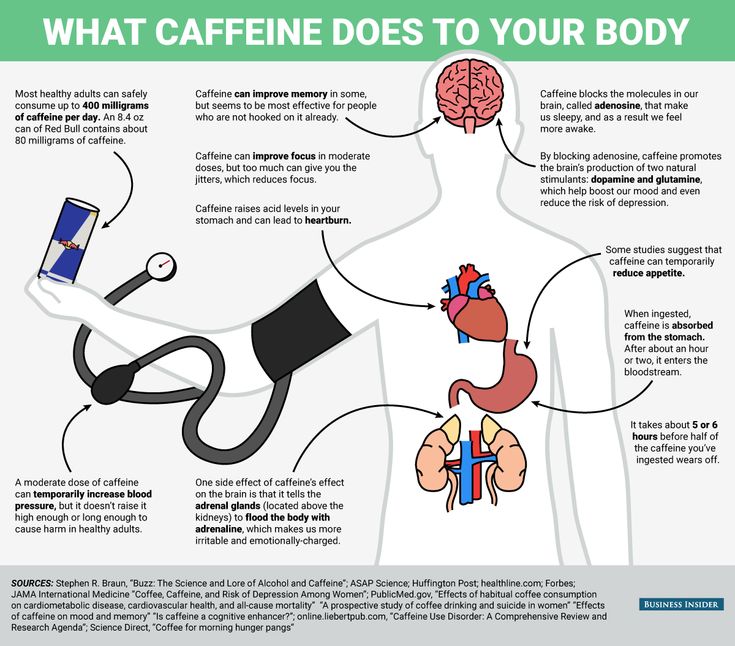 The effect did not depend on what experimental technique was used, on what preparations the patient was sitting, and also on his gender and age.
The effect did not depend on what experimental technique was used, on what preparations the patient was sitting, and also on his gender and age.
The authors of the study call the effect significant, but given the fact that the side variables that would provide the desired effect could not be found, the result can be called random - of course, if we consider the use of sleep deprivation as a binary variable. In other words, when psychiatrists give patients with depression forced sleep therapy, it can either help or not - as luck would have it.
At the same time, sleep deprivation is still considered a fairly effective way to treat depression, and why this is so (even if it is intuitively clear that lack of sleep is more likely to be harmful) should still be understood.
Intervene experimentally
The relationship between sleep quality and mental disorders is complex. First of all, the relationship between them is two-way: insomnia, as well as hypersomnia - excessive sleep duration and daytime sleepiness, are considered both symptoms of depression and factors that largely affect its development.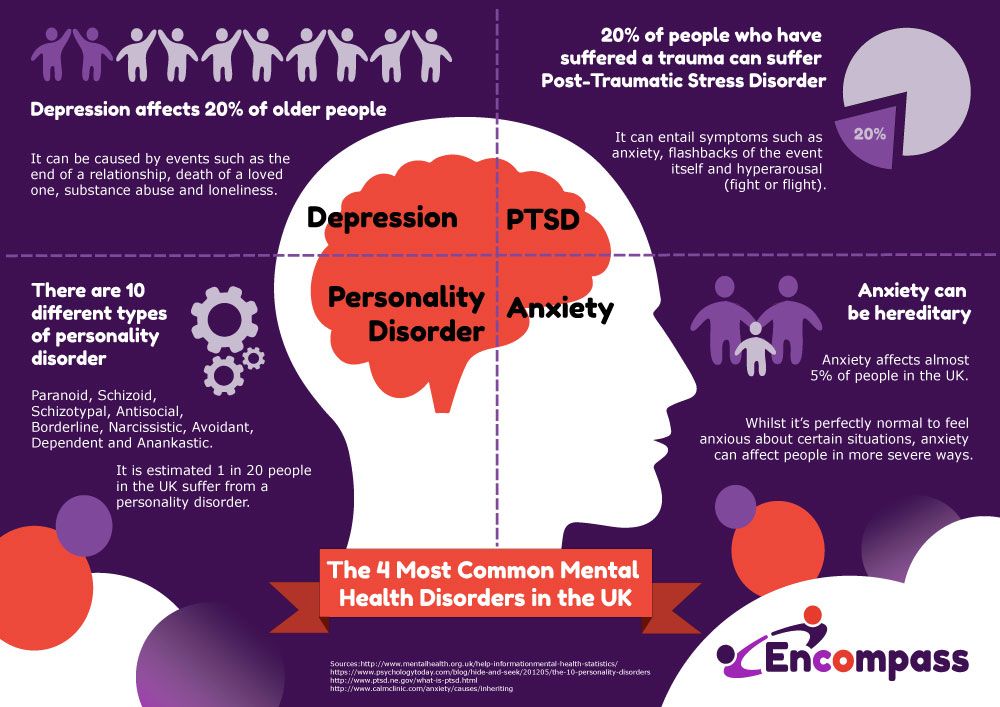
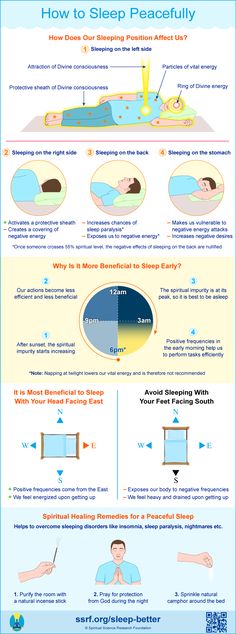
First of all, therefore, in case of depression, it is necessary to restore normal sleep hygiene: do not eat a few hours before going to bed, go to bed at the same time, sleep the number of hours recommended for age (for an adult - about seven to eight hours a day). day) and do not put off rest for the weekend in anticipation of a cumulative effect.
Obviously this can be quite difficult; in this case, patients with depression are prescribed drugs from the group of neuroleptics or other substances with anti-anxiety (trouble, as you know, does not come alone: with depression, the risk of developing anxiety is higher) or sedative effect.
In the early 1970s, the German psychiatrist Walter Schulte discovered and studied that sleep deprivation could have a therapeutic effect on depression. He observed three patients diagnosed with depressive disorder: two teachers and one doctor. Each of them reported to Schulte that after a sleepless night at work or playing sports, they feel an improvement in their mental state.
Of course, it is impossible to base an entire psychiatric practice on three cases, so after the first statements about the benefits of sleep deprivation (after Schulte, two more of his colleagues managed to achieve a significant effect in 23 out of 34 patients), scientists began to actively conduct research.
First, it was necessary to determine exactly how many hours of sleep deprivation it takes to achieve at least some effect - and at what time to start the experiment. Usually, sleep deprivation therapy involves a whole day (or even more: sometimes up to 36-40 hours) of forced wakefulness: the patient is woken up at about one in the morning, after which he does not sleep the whole next day and sometimes even the whole next night.
With this therapy, the intake of any CNS stimulants (even coffee) is excluded, and it is also recommended to combine forced insomnia with light therapy (however, both are considered branches of chromotherapy - artificial "tuning" of sleep and wake cycles).
The effect is quite fast: with sleep deprivation in a depressed patient, visible improvements are immediately observed. However, this is a rather deceptive success: studies indicate that in 50-80 percent of patients the state returns to the usual depressive state after they do get some sleep. At the same time, in 10-15 percent of patients, improvements, on the contrary, appear only after sleep following deprivation. In 2-7 percent of patients, the condition may worsen, and symptoms of mania may be added to depression (sleep deprivation, therefore, is not recommended for people with bipolar disorder - even in the depressive phase).
Some vagueness of the effect can be explained by the fact that a day or more without sleep is still quite painful for the body. Therefore, scientists tried to reduce the time of forced wakefulness to a few hours at night. To do this, for example, you can wake up the patient in the middle of the night and keep him awake for a couple of hours. Such a study was conducted in the early 1990s, but forced wakefulness until five in the morning after waking up at three did not give any special effect.
Such a study was conducted in the early 1990s, but forced wakefulness until five in the morning after waking up at three did not give any special effect.
Although meta-analyses indicate that there are no precise confounding variables that would provide the desired effect of sleep deprivation, anecdotal studies still state that several conditions must be met for such a method to be effective.
For example, sleep deprivation works best on patients with endogenous depression, rather than depression caused by external factors. In addition, the variation in the patient's mood during the day must also be taken into account: sleep deprivation works most effectively in those who feel better in the evening, rather than during the day.
The mechanism of the therapeutic effect of sleep deprivation has not been fully established. For example, recent research suggests the role of the neurotransmitter adenosine, which accumulates in the brain during the day and is ultimately responsible for making us feel tired and fall asleep.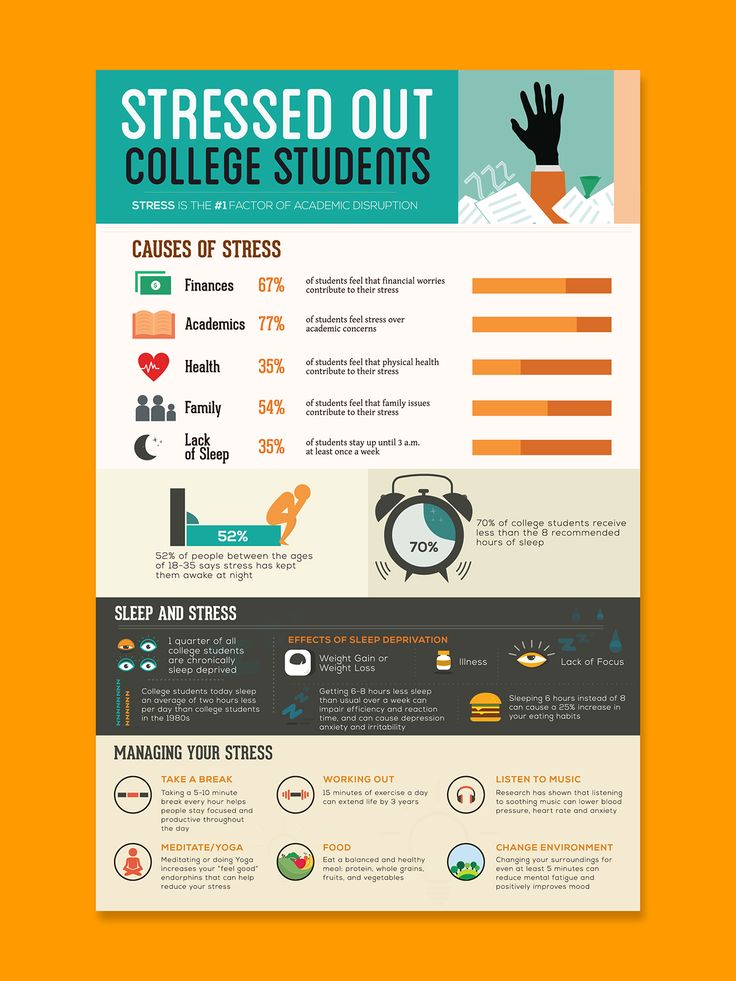
Other studies point to the involvement of the serotonergic system, which is central to the pathology of depression, in such therapy. When taking the drug pindolol, which blocks serotonin autoreceptors and improves the effect of antidepressants from the group of selective serotonin reuptake inhibitors, sleep deprivation more effectively improves well-being in depression.
A logical reason for the effectiveness of lack of sleep seems to be its comparison with the use of psychostimulants (eg, amphetamine). Indeed, in the absence of sleep, effects similar to taking psychoactive substances are sometimes observed (you may be familiar with this: sometimes, with a long wakefulness, it seems that there is more strength and energy).
In both cases, the concentration of monoamines in the brain increases (primarily, however, not serotonin, but dopamine), due to which the work of the limbic system stabilizes, and mental well-being improves. Such a theory is consistent with the fact that the effect of sleep deprivation is often unstable and short-lived - like psychostimulants.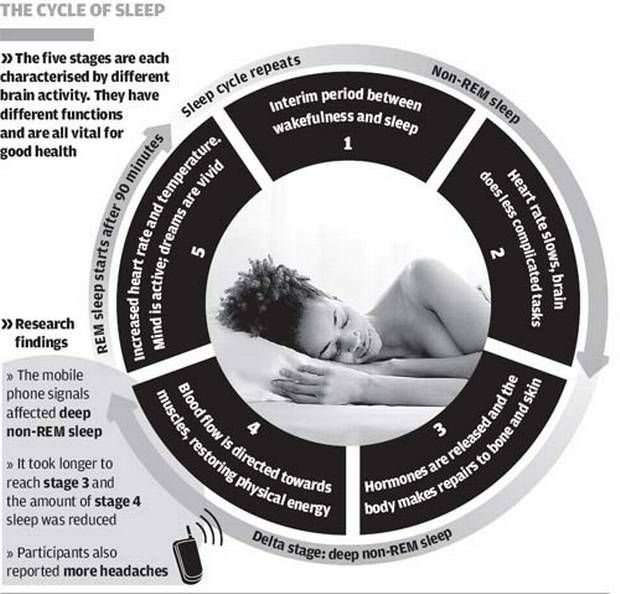 However, this is still just a theory.
However, this is still just a theory.
Use with caution
Despite a fairly long history of study and use in psychiatric practice, sleep deprivation still remains an experimental treatment for depression and is not included in the standard treatment recommendations along with antidepressant drugs and psychotherapy. This is evidenced both by the fact that depression is often treated with sleep deprivation only under controlled conditions (under the supervision of doctors), and by the fact that sleepless nights have many negative consequences.
One of the most serious is the possible increased risk of developing Alzheimer's disease even from one night of sleeplessness. Two proteins play a key role in the development of the disease: beta-amyloid, which forms plaques in the brain, and tau, which contributes to the formation of intracellular neurofibrillary cords.
Studies show that just one sleepless night significantly increases the concentration of beta-amyloid in the brain and tau in the blood. The mechanism of such an action is not fully known in either case, and it is also not clear whether there are actually any negative consequences.
It is also interesting that lack of sleep leads to increased feelings of loneliness and social isolation. Here the effect, however, is more psychological: the lack of sleep makes people look for a variety of ways to escape from the accumulated fatigue, which increases the need for communication. Other people, on the contrary, find a sleepy person more repulsive and do not want to make contact with him.
A rather understandable conflict arises, which makes it difficult to establish communication with others - hence the feeling of loneliness appears. And with depression (unless, of course, it was not there before, since loneliness is one of the common psychological symptoms of a disorder), it is definitely not necessary.
In addition, a recent study showed that a sleepless night reduces the activity of the prefrontal cortex, which is responsible, among other things, for cognitive control. With a decrease in cognitive control, in turn, anxiety increases significantly - and it can significantly worsen the condition of depression.
However, it should be borne in mind that the use of sleep deprivation for the treatment of insomnia and the same technique for behavioral research are two different things. Healthy people without mental disorders take part in the latter; in them, control studies of sleep deprivation therapy show that not getting a night's rest only increases irritability—and doesn't work the way it does for people with depression, even in the short term.
Therefore, it is logical to assume that lack of sleep may not bring negative behavioral and mental aspects to people with depression: review studies also speak about the severity of the presence of mental disorders for the effectiveness of sleep deprivation. But do not forget about the average effectiveness of 50 percent (as well as the fact that the drug treatment of depression has about the same indicators).