Dna testing for bipolar disorder
Largest Genetic Study of Bipolar Disorder Identifies 64 Regions of the Genome That Increase Risk for the Condition | Mount Sinai
- Press Release
International consortium of leading psychiatric genetics scientists studied thousands of DNA sequences, more than doubling the number of regions previously identified
Niamh Mullins, PhD
Mount Sinai Health System
Newsroom
- New York, NY
- (May 13, 2021)
In the largest genetic study of bipolar disorder to date, researchers have identified 64 regions of the genome containing DNA variations that increase risk of bipolar disorder - more than double the number previously identified.
The research team also found overlap in the genetic bases of bipolar disorder and other psychiatric disorders.
Furthermore, the study supports a role of sleep habits, alcohol, and substance usage in the development of bipolar disorder, although further research is needed to confirm these findings. The study results are published May 17 in Nature Genetics.
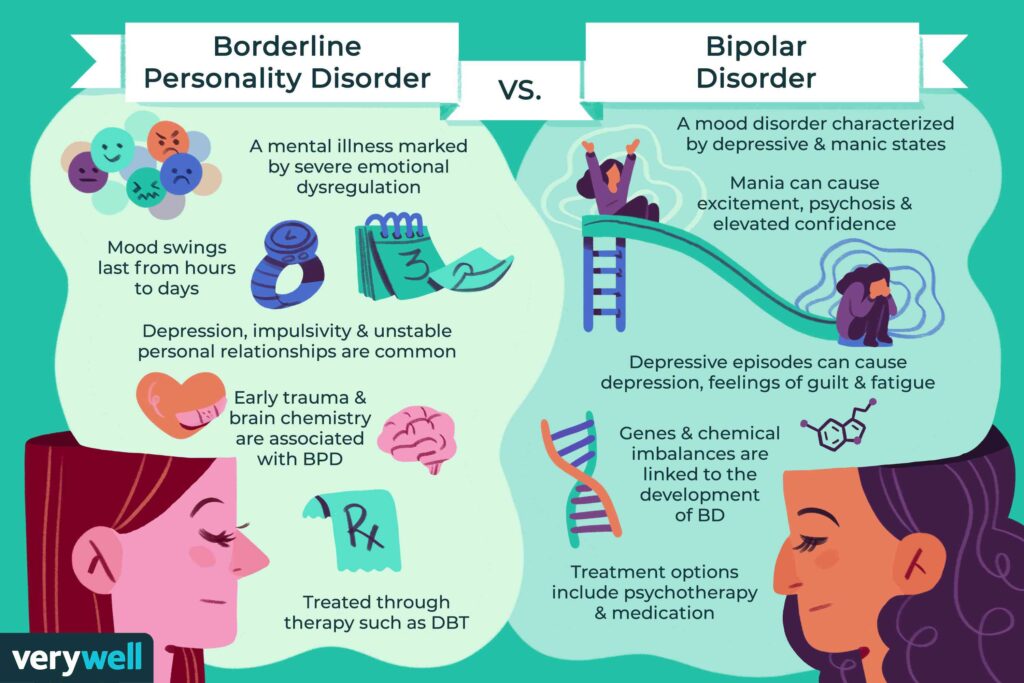
Bipolar disorder, a complex psychiatric disorder characterized by recurrent episodes of severely high and low mood, affects an estimated 40 to 50 million people worldwide. It typically begins in young adulthood, often takes a chronic course, and carries an increased risk of suicide, making it a major public health concern and cause of global disability.
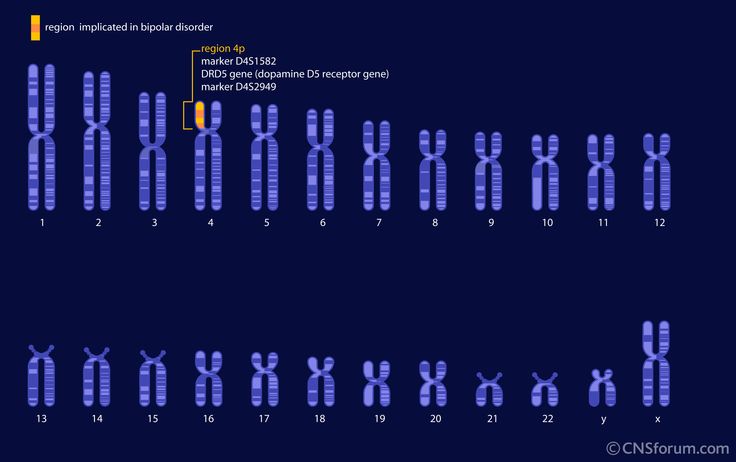
To help elucidate the underlying biology of bipolar disorder, an international team of scientists from within the Psychiatric Genomics Consortium conducted a genome-wide association study. This means they scanned the DNA of lots of people, looking for genetic markers that were more common in those who had bipolar disorder. This involved scanning more than 7.5 million common variations in the DNA sequence of nearly 415,000 people, more than 40,000 of whom had bipolar disorder.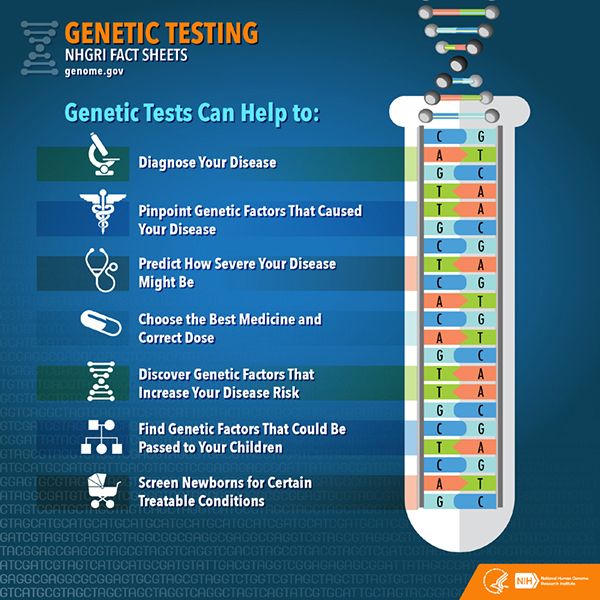 The study identified 64 regions of the genome that contain DNA variations that increase risk of bipolar disorder.
The study identified 64 regions of the genome that contain DNA variations that increase risk of bipolar disorder.
“It is well-established that bipolar disorder has a substantial genetic basis and identifying DNA variations that increase risk can yield insights into the condition’s underlying biology,” says Niamh Mullins, PhD, Assistant Professor of Psychiatric Genomics at the Icahn School of Medicine at Mount Sinai and lead author of the paper. “Our study found DNA variations involved in brain cell communication and calcium signaling that increase risk of bipolar disorder.
The findings suggest that drugs, such as calcium channel blockers that are already used for the treatment of high blood pressure and other conditions of the circulatory system, could be investigated as potential treatments for bipolar disorder, yet it's important to note that future research to directly assess whether these medications are effective is essential.”
The study also found overlap in the genetic basis of bipolar disorder and that of other psychiatric disorders and confirmed the existence of partially genetically distinct subtypes of the disorder. Specifically, they found that bipolar I disorder shows a strong genetic similarity with schizophrenia and bipolar II disorder is more genetically similar to major depression.
Specifically, they found that bipolar I disorder shows a strong genetic similarity with schizophrenia and bipolar II disorder is more genetically similar to major depression.
“This research would not have been possible without the collaborative efforts of scientists worldwide that enabled the study of hundreds of thousands of DNA sequences,” said Ole Andreassen, MD, PhD, Professor of Psychiatry, Institute of Clinical Medicine and Oslo University Hospital and senior author of the paper. “Through this work, we prioritized some specific genes and DNA variations which can now be followed up in laboratory experiments to better understand the biological mechanisms through which they act to increase risk of bipolar disorder.”
The biological insights gained from this research could ultimately lead to the development of new and improved treatments or precision medicine approaches to stratify patients at high genetic risk who may benefit from targeted treatment or intervention strategies.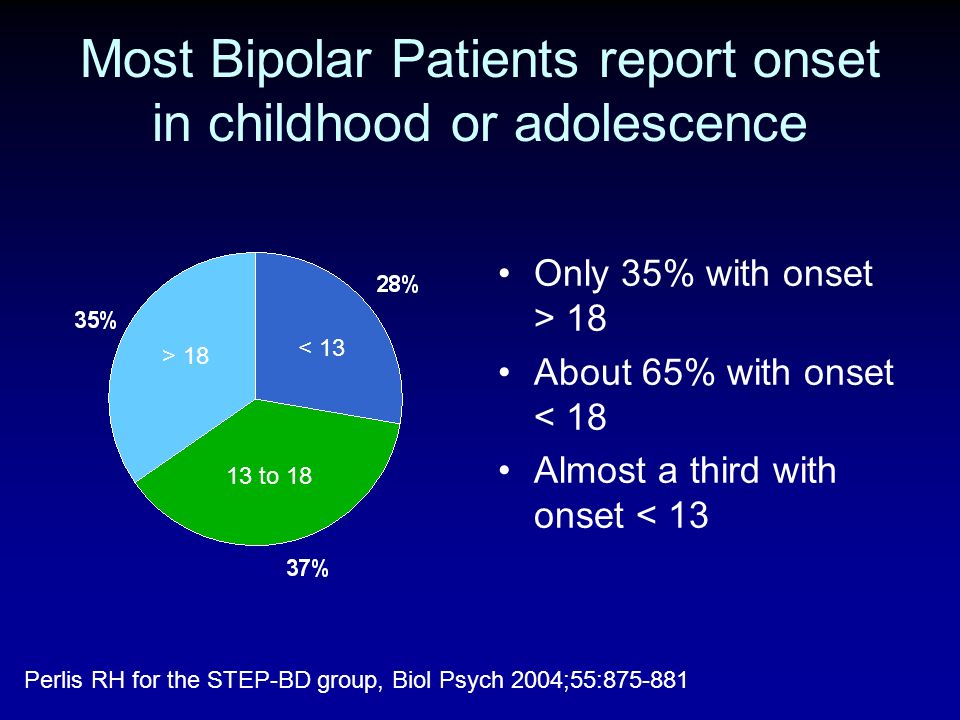 Understanding causal risk could aid clinical decision-making in the prevention or management of the illness. Future genetic studies in larger and more diverse populations are now needed to pinpoint the genes relevant to risk of bipolar disorder in other areas of the genome.
Understanding causal risk could aid clinical decision-making in the prevention or management of the illness. Future genetic studies in larger and more diverse populations are now needed to pinpoint the genes relevant to risk of bipolar disorder in other areas of the genome.
The Psychiatric Genomics Consortium (PGC) is an international consortium of scientists dedicated to studying the genetic basis of psychiatric disorders and includes over 800 researchers, from more than 150 institutions from over 40 countries.
Tags: Icahn School of Medicine at Mount Sinai, Niamh Mullins, PhD
About the Mount Sinai Health System
Mount Sinai Health System is one of the largest academic medical systems in the New York metro area, with more than 43,000 employees working across eight hospitals, over 400 outpatient practices, nearly 300 labs, a school of nursing, and a leading school of medicine and graduate education.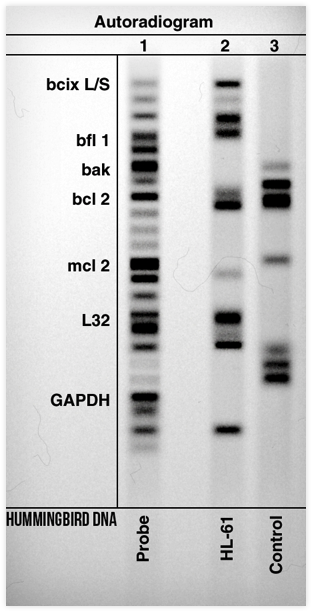 Mount Sinai advances health for all people, everywhere, by taking on the most complex health care challenges of our time — discovering and applying new scientific learning and knowledge; developing safer, more effective treatments; educating the next generation of medical leaders and innovators; and supporting local communities by delivering high-quality care to all who need it.
Mount Sinai advances health for all people, everywhere, by taking on the most complex health care challenges of our time — discovering and applying new scientific learning and knowledge; developing safer, more effective treatments; educating the next generation of medical leaders and innovators; and supporting local communities by delivering high-quality care to all who need it.
Through the integration of its hospitals, labs, and schools, Mount Sinai offers comprehensive health care solutions from birth through geriatrics, leveraging innovative approaches such as artificial intelligence and informatics while keeping patients’ medical and emotional needs at the center of all treatment. The Health System includes approximately 7,300 primary and specialty care physicians; 13 joint-venture outpatient surgery centers throughout the five boroughs of New York City, Westchester, Long Island, and Florida; and more than 30 affiliated community health centers. We are consistently ranked by U.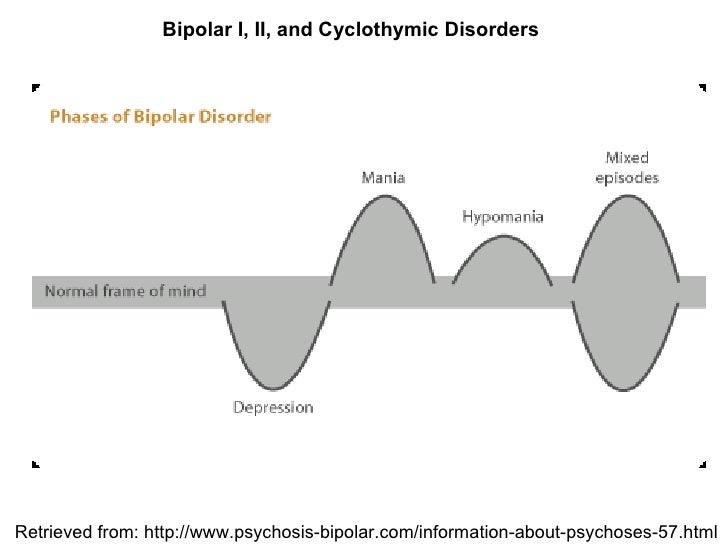 S. News & World Report's Best Hospitals, receiving high "Honor Roll" status, and are highly ranked: No. 1 in Geriatrics and top 20 in Cardiology/Heart Surgery, Diabetes/Endocrinology, Gastroenterology/GI Surgery, Neurology/Neurosurgery, Orthopedics, Pulmonology/Lung Surgery, Rehabilitation, and Urology. New York Eye and Ear Infirmary of Mount Sinai is ranked No. 12 in Ophthalmology. U.S. News & World Report’s “Best Children’s Hospitals” ranks Mount Sinai Kravis Children's Hospital among the country’s best in several pediatric specialties. The Icahn School of Medicine at Mount Sinai is one of three medical schools that have earned distinction by multiple indicators: It is consistently ranked in the top 20 by U.S. News & World Report's "Best Medical Schools," aligned with a U.S. News & World Report "Honor Roll" Hospital, and top 20 in the nation for National Institutes of Health funding and top 5 in the nation for numerous basic and clinical research areas.
S. News & World Report's Best Hospitals, receiving high "Honor Roll" status, and are highly ranked: No. 1 in Geriatrics and top 20 in Cardiology/Heart Surgery, Diabetes/Endocrinology, Gastroenterology/GI Surgery, Neurology/Neurosurgery, Orthopedics, Pulmonology/Lung Surgery, Rehabilitation, and Urology. New York Eye and Ear Infirmary of Mount Sinai is ranked No. 12 in Ophthalmology. U.S. News & World Report’s “Best Children’s Hospitals” ranks Mount Sinai Kravis Children's Hospital among the country’s best in several pediatric specialties. The Icahn School of Medicine at Mount Sinai is one of three medical schools that have earned distinction by multiple indicators: It is consistently ranked in the top 20 by U.S. News & World Report's "Best Medical Schools," aligned with a U.S. News & World Report "Honor Roll" Hospital, and top 20 in the nation for National Institutes of Health funding and top 5 in the nation for numerous basic and clinical research areas.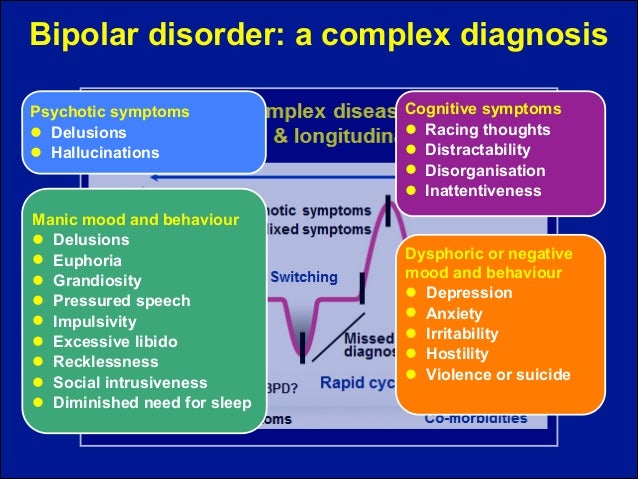 Newsweek’s “The World’s Best Smart Hospitals” ranks The Mount Sinai Hospital as No. 1 in New York and in the top five globally, and Mount Sinai Morningside in the top 20 globally.
Newsweek’s “The World’s Best Smart Hospitals” ranks The Mount Sinai Hospital as No. 1 in New York and in the top five globally, and Mount Sinai Morningside in the top 20 globally.
For more information, visit https://www.mountsinai.org or find Mount Sinai on Facebook, Twitter and YouTube.
Newsroom
In This Story
Show More
For Media Inquiries
View All Media Contacts
For Media Inquiries
View All Media Contacts
Bipolar Disorder Treatment and Pharmacogenetic Testing
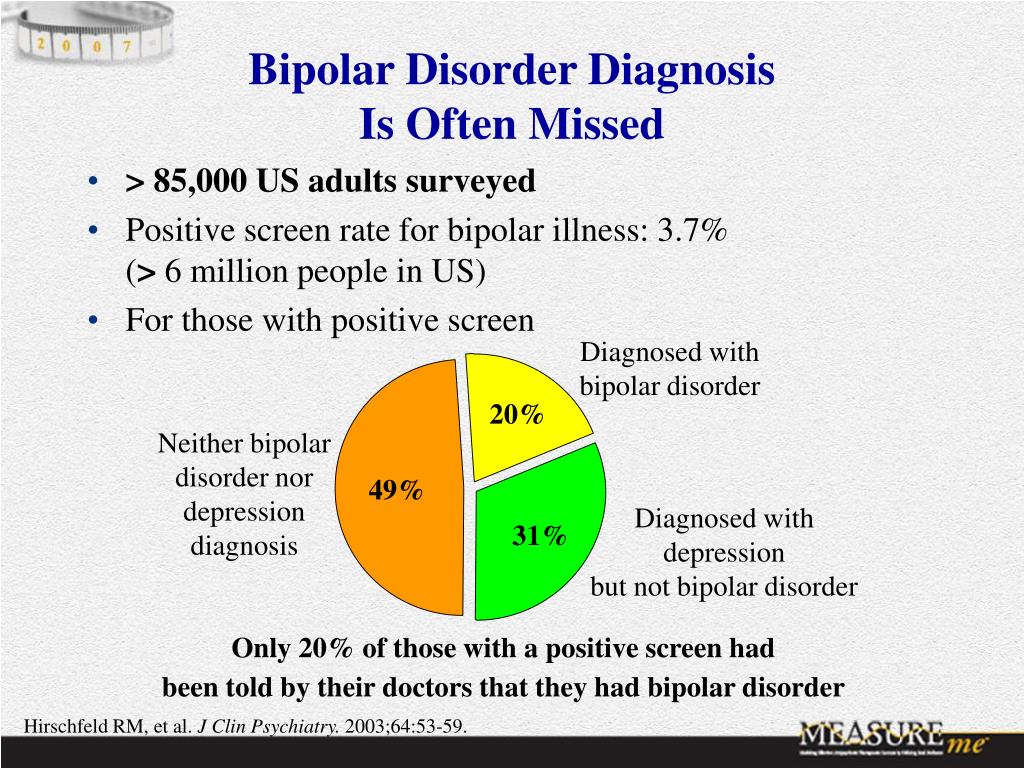
Everyone experiences mood swings from time to time, but bipolar disorder takes those highs and lows to a more severe level. Approximately 4% of all U.S. adults will experience bipolar disorder, with women and men equally likely to be affected.
Whether a close friend is dealing with bipolar disorder or you’re struggling with it yourself, getting effective treatment can be crucial. Here’s what you need to know about bipolar disorder, including how pharmacogenetic testing (PGx) can be a helpful tool in your treatment.
Here’s what you need to know about bipolar disorder, including how pharmacogenetic testing (PGx) can be a helpful tool in your treatment.
What is Bipolar Disorder?
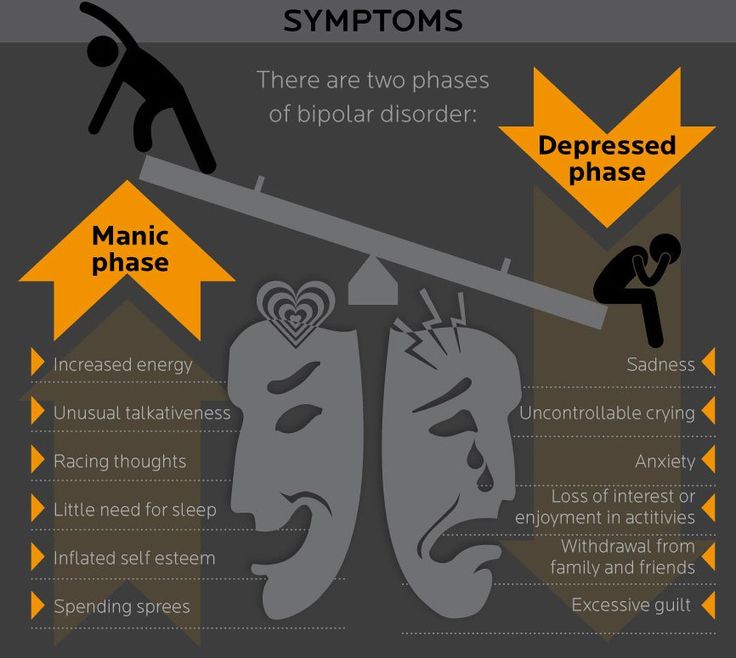
Bipolar disorder is a mental health disorder that causes someone to experience significant shifts in mood. This affects everything from their demeanor to their energy levels as well as their basic ability to function and make it through the day. An individual with bipolar disorder may experience manic, hypomanic, and/or depressive stages.
Dealing with changes in moods and emotions can seem confusing, and it may be difficult to recognize the signs of bipolar disorder.
What does a manic episode feel like?
Some common manic symptoms of bipolar disorder may include:
- Feeling jumpy, wired, or irritable.
- Needing less sleep than usual.
- Having racing thoughts.
- Talking louder, faster, or having pressured speech.
- Having an inflated ego, for example thinking you can do things that normally you could not do.
What does a depressive episode feel like?
Some common depressive symptoms of bipolar disorder may include:
- Feeling sluggish or restless.
- Increased or decreased appetite.
- Sleeping too much or having trouble falling asleep.
- Difficulty focusing or making decisions.
- Losing interest in things you ordinarily enjoy.
- Having suicidal thoughts.
These mood swings don’t always happen consecutively. An individual may go through a manic episode, feeling heightened energy and self-confidence, only to fall into a depressive state a few days or weeks later. Alternatively, they may return to normal functioning for weeks or months before the next depressive or manic episode occurs.
Types of Bipolar Disorder
It is the intensity of manic episodes that helps us further categorize bipolar disorder. There are three main types:
There are three main types:
- Bipolar I is defined by manic episodes that last at least seven days, and typically lead to hospitalization. Bipolar I can also include depression lasting up to two weeks, or frequent switches between manic and depressive episodes.
- Bipolar II is characterized by hypomania, or a milder manic episode. This is an elevated mood or state of mind that may cause high energy levels and make it more difficult to focus. Symptoms must be present for at least four days in order to be defined as hypomania. Bipolar II always involves depressive episodes as well, which mirror clinical depression. Usually depressive periods occur more often than hypomanic episodes.
- Cyclothymic Disorder is characterized by mild hypomanic and depressive symptoms that occur over the course of two years but are not serious enough to be defined as episodes.
If you think you may have bipolar disorder, it’s important to speak to your healthcare clinician about your symptoms.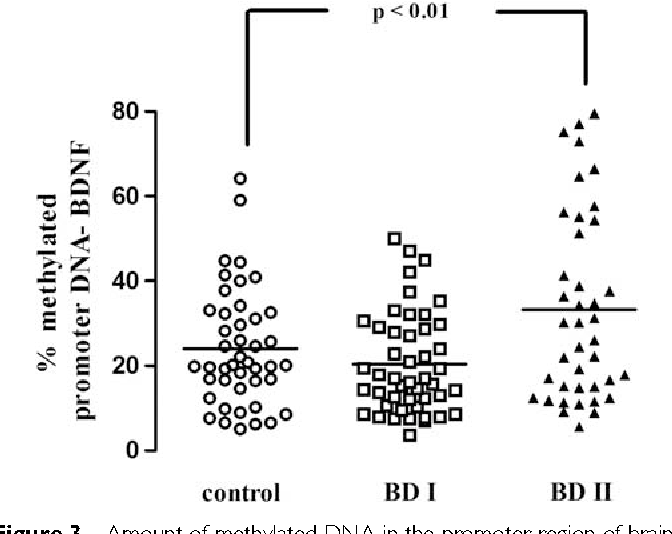
Bipolar Disorder Treatments
The first step to treating bipolar disorder is to make an appointment with your primary healthcare provider. They will likely start with a physical exam to rule out other causes of symptoms, then refer you to a specialist, such as a psychiatrist. From there, your treatment plan may include a combination of cognitive behavior therapy, lifestyle modifications, and medication.
There are several prescription medications used to treat bipolar disorder, such as mood stabilizers (like lithium) , antipsychotics, and antidepressants, which may help stabilize your mood and may prevent the swing between manic and depressive episodes.
Possible Side Effects of Bipolar Medication
While medication may be an important and essential part of treating bipolar disorder, certain drugs may cause side effects. Potential side effects with medications used to treat bipolar disorder include:
- Weight gain.
- Increased blood pressure or blood sugars and altered cholesterol levels.

- Feeling lethargic (sluggish) or sedated.
- Akathisia, or feeling restless and unable to physically sit still.
Research published in the Journal of Affective Disorders states that these side effects may lead to non-adherence, or individuals not taking their medication as directed.
Can Bipolar Be Genetic?
There is no single bipolar gene that determines if an individual will be diagnosed with bipolar during their lifetime, but there is a hereditary component to the disorder. One review published in Neuroscience found that bipolar is one of the most heritable medical disorders.
Twin studies have corroborated this, estimating bipolar disorder to be 60-80% heritable. For example, having a parent who has bipolar can make you more genetically susceptible to having bipolar as well. Your risk increases if more than one immediate family member, say your other parent, has the condition too.
However, as with most mental health disorders, genetics is only part of the equation.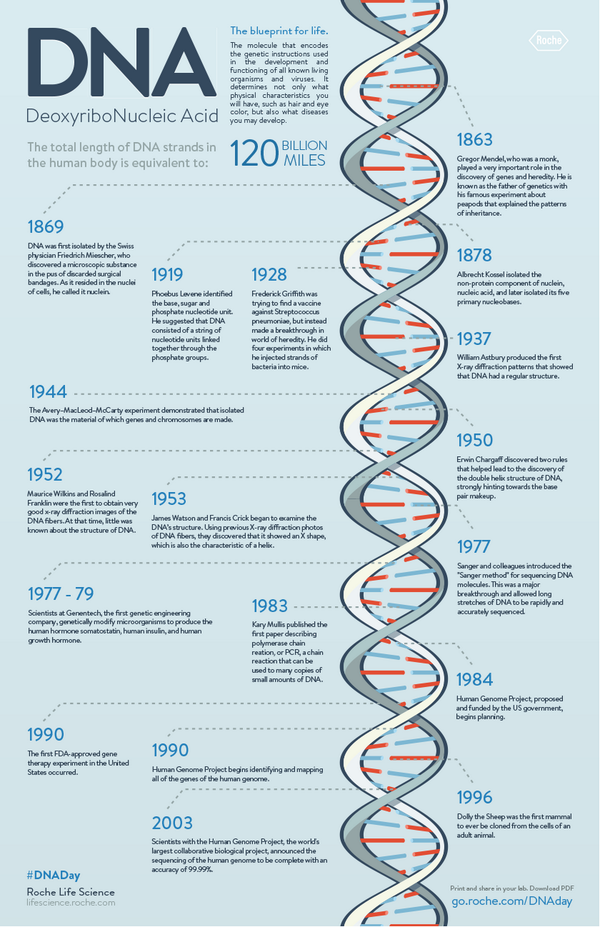 Mental health is a combination of genetics, experiences, lifestyle choices, and your surrounding environment, both past and present.
Mental health is a combination of genetics, experiences, lifestyle choices, and your surrounding environment, both past and present.
Genetic Testing for Bipolar Medication
Your personal genetic profile can provide information on the likelihood of effectiveness and side effects with various medicines, as well as information on how your body processes medications. This does not have to be something you find out by trial and error. By being proactive and getting this information before starting a medication, your clinician can make more informed decisions when prescribing medication(s).
The Genomind Pharmacogenetic (PGx) test looks at 24 genes related to mental health treatment and can be used to help determine medication options to manage bipolar disorder. It provides guidance across 130 medications used to treat a multitude of neuropsychiatric disorders to help clinicians determine:
- Which medications may be more or less likely to be effective.
- Which medications may be more or less likely to show side effects.
- How you metabolize medications for personalized dosing guidance.
The Genomind PGx test can be done at a clinician’s office—or from the comfort of your home. It requires a prescription, and Genomind can help connect you with a verified Genomind provider near you. Get started by filling out this form.
Is Your Bipolar Medication Working for You?
Bipolar disorder can be a difficult condition to manage, and difficulty in finding medication(s) that relieve symptoms and/or a stable treatment plan can be discouraging to both patients and providers.
Genetic assay testing provides insight into how your genes may play a part in your response or tolerability to different prescriptions. This pharmacogenomic testing gives your clinician information they can leverage to help you avoid trial and error and find appropriate treatment.
How DNA Tests Help Treat Mental Disorders - T&P
People with mental disorders are forced to take medications that sometimes cause unpleasant side effects or no effect at all on the disease.
 To avoid trial and error, you can do a pharmacogenetic test that will accurately indicate the right medicine for this particular person. Natalya Zakharova, a candidate of medical sciences and a psychiatrist, told more about how this happens. T&P recorded the main.
To avoid trial and error, you can do a pharmacogenetic test that will accurately indicate the right medicine for this particular person. Natalya Zakharova, a candidate of medical sciences and a psychiatrist, told more about how this happens. T&P recorded the main. Candidate of Medical Sciences, psychiatrist, senior researcher, PKB No. 1 named after. ON THE. Alekseeva
Is it possible to cure schizophrenia with drugs?
According to statistics, the number of registered drugs and generics is growing in Russia, in 2010 this figure reached 20,000 different drugs. Pharmacotherapy remains the mainstay of treatment for mental illness.
In practice, the doctor is guided by the official standards of care, which are based on the results of fundamental sciences and clinical trials of drugs. In psychiatry, the guide of Professor Steven Stahl is popular, which provides information about modern psychotropic drugs, indicates their receptor activity and participation in the functioning of neurotransmitters, that is, at the biological level, the spectrum of the clinical effect of active substances is presented. Knowing the receptor profile of the drug, one can confidently assume whether the drug will calm or excite, cause drowsiness or activate, reduce anxiety or stop hallucinations.
Knowing the receptor profile of the drug, one can confidently assume whether the drug will calm or excite, cause drowsiness or activate, reduce anxiety or stop hallucinations.
Despite the variety of existing drugs, about 38-40% of forms of depression are resistant to pharmacological treatment; for other mental disorders, the prognosis is also not always favorable. For the treatment of schizophrenia and schizophrenia spectrum disorders, 3,720 drug names and 32 main active (original) substances are registered in the Russian Medicines Register (RLS). In addition, in case of ineffectiveness of monotherapy (treatment with one drug), methods of augmentation have been developed - enhancing the action of the main substance by adding additional drugs to the therapy regimen: antidepressants, tranquilizers, mood stabilizers or nootropic drugs. In case of ineffectiveness of drugs, non-drug methods are used: electroconvulsive therapy, transcranial magnetic stimulation (TMS), various methods of psychotherapy, psychocorrection and psychoeducation.
However, when analyzing all these actions, it still turns out that from 30% to 70% of patients with schizophrenia and schizophrenia spectrum disorders are resistant to therapy. This does not mean that people are incurable - it all depends on what is considered complete remission. By analogy with a broken limb, after which a scar on the body or a callus may remain,
a person may have residual symptoms after suffering a mental disorder. But in this case, they will still be considered a disease, and it is they who can be resistant to any impact.
Genes and side effects
Pharmacogenetics is by far the most promising field in the study of mental disorders. It studies the interaction of human genes and drugs. There are no single genes for mental disorders, it is always a combination of a huge number of interactions, including genetic ones. There is no gene for schizophrenia or a gene for depression: there is a predisposition, and it is impossible to predict it today.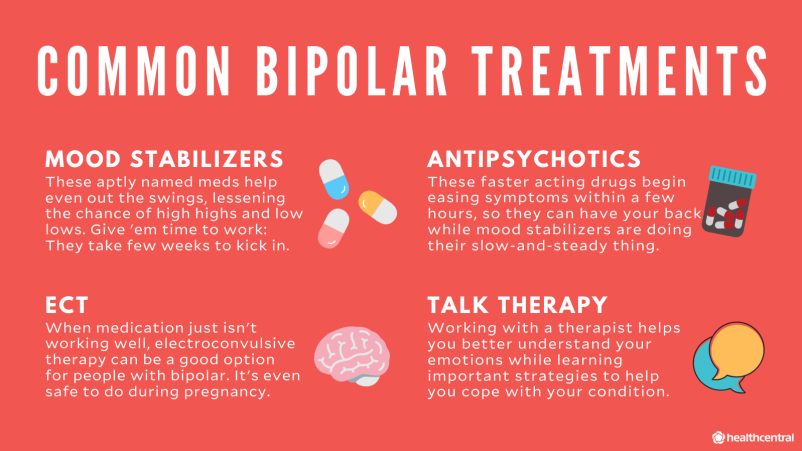 Perhaps in the future, with the development of technology, we will understand more, but the only thing that we can really do today is to conduct a pharmacogenetic test to determine the effectiveness and tolerability of psychotropic drugs.
Perhaps in the future, with the development of technology, we will understand more, but the only thing that we can really do today is to conduct a pharmacogenetic test to determine the effectiveness and tolerability of psychotropic drugs.
At the very beginning of treatment, we wait for some kind of response to therapy and check its tolerability. If there are no adverse events in the first days, then we continue therapy.
Let's see what happens to the drug in the body. After absorption, the process of metabolism occurs, this process is designated as pharmacokinetics , liver cytochromes come into play - biotransformation enzymes. There is a whole family of them, and complex combinations of inhibition and activation of each other are possible between them and drugs. Next step - pharmacodynamic , delivery of a substance molecule to the target of exposure. At this stage, carrier proteins, ion channel activators, receptors, lipoproteins and, finally, brain receptors are connected.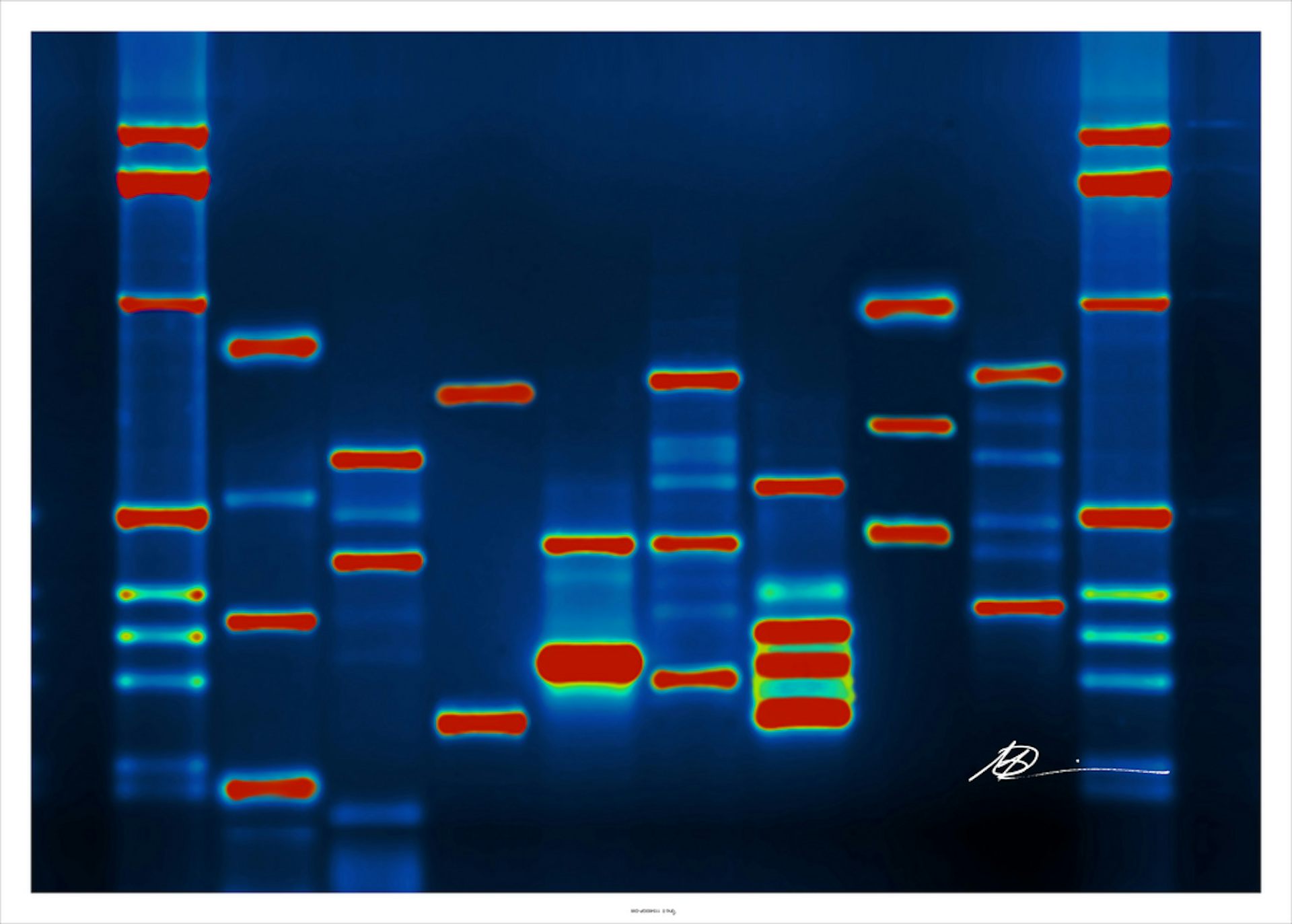 All these factors have a peptide structure, which means they are encrypted in DNA. In the instructions for many drugs, there is already a clause about the type of metabolizer in a person (features of the patient's metabolism in relation to this drug. - Note T & P) . There are fast, slow and ultra-fast metabolizers. In accordance with this, the calculation of the dosage and the possible toxic effect are indicated.
All these factors have a peptide structure, which means they are encrypted in DNA. In the instructions for many drugs, there is already a clause about the type of metabolizer in a person (features of the patient's metabolism in relation to this drug. - Note T & P) . There are fast, slow and ultra-fast metabolizers. In accordance with this, the calculation of the dosage and the possible toxic effect are indicated.
Tens of thousands of studies are being conducted around the world on genetic factors for the effectiveness and safety of drugs. To systematize the accumulated knowledge, open access knowledge bases are created. Scientists upload the results of their work to one platform. One of these bases is PharmGKB, this is pharmacogenetic knowledge from all over the world: efficacy, metabolic features, toxicity and side effects, dosage for a patient with a certain genotype. Taking information from this database and knowing the patient's genotype, one can safely prescribe a drug to him without risking his health due to possible complications. If a person has a genotype that is not in the database, the doctor will correlate the risks and benefits of prescribing the drug, realizing that side effects are possible.
If a person has a genotype that is not in the database, the doctor will correlate the risks and benefits of prescribing the drug, realizing that side effects are possible.
One of the important problems of treatment with psychotropic drugs is that, in addition to side effects here and now , there are often delayed side effects associated with changes in hormonal levels and metabolic processes in the body.
For example, hyperprolactinemia is common, a side effect of the hypothalamic-pituitary system in the form of an increase in prolactin. This undesirable phenomenon does not appear in everyone after three to six months from the start of treatment, and although it is reversible, it is much better to avoid it. There is evidence in which genotype the risk of developing triglyceridemia, hyperprolactinemia and other disorders is high, that is, in which genotype this phenomenon will develop for sure, and in which it will not manifest itself at all.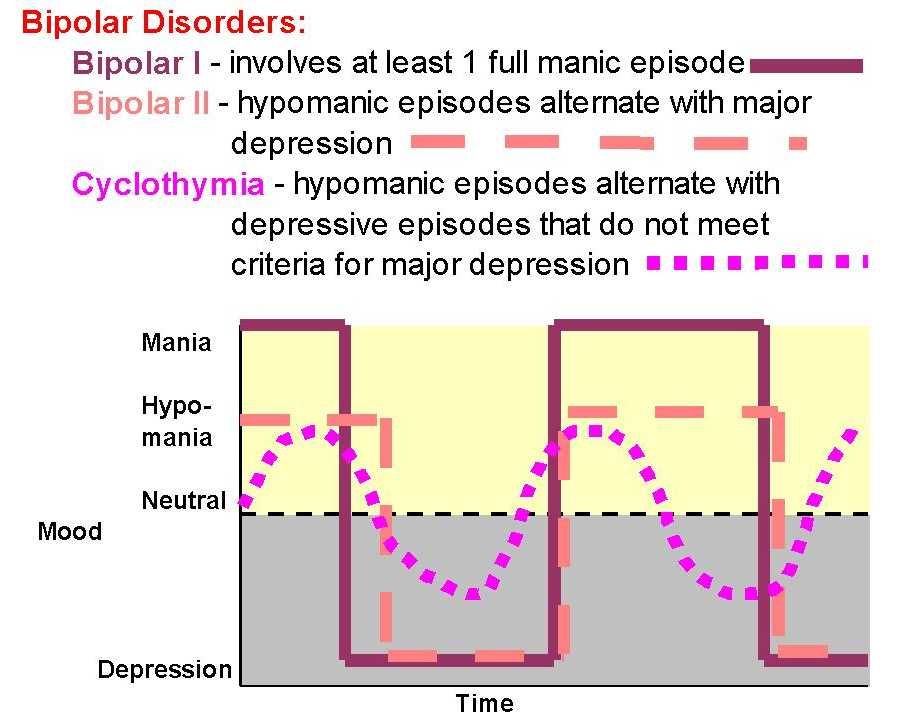 In such cases, it is advisable to conduct genetic testing at the beginning of treatment, as this will avoid the development of delayed adverse events and save resources for their subsequent correction.
In such cases, it is advisable to conduct genetic testing at the beginning of treatment, as this will avoid the development of delayed adverse events and save resources for their subsequent correction.
What tests can do
How accurate are genetic tests? Depends on the panel developer. Obviously, the more genetic "points" a test contains, the more informative it is; if the test takes into account drug interactions (the same inhibition and activation, for example, of cytochromes), it is simply invaluable.
Ref. It is possible to program a test for hundreds of thousands of indicators, regardless of the quality of the results of previous pharmacogenetic studies. Let me explain. The result of a study of a sample of several people for one polymorphism is not very informative.
Pharmacogenetic tests require results only from those studies that meet a high level of evidence -
A or B. That is, results obtained by analogy with clinical trials in double-blind, placebo-controlled multicenter programs or data collected at the level of high-quality meta-analysis .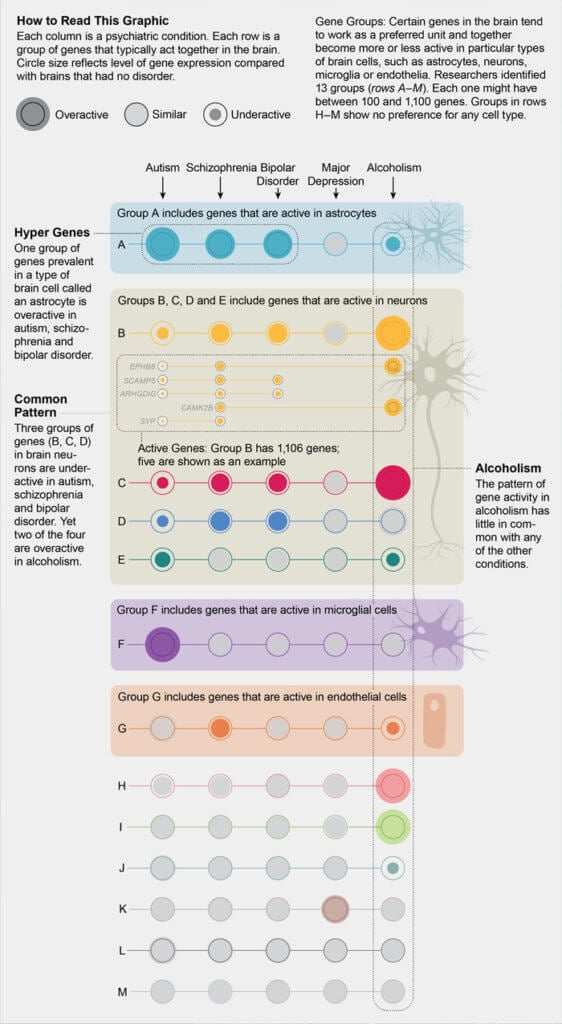
Levels of evidence
I/A: large, double-blind, placebo-controlled trials, as well as data from a meta-analysis of several randomized controlled trials.
II/B: small randomized controlled trials in which statistical calculations are performed on a limited number of patients.
III/C: Non-randomized clinical trials in a limited number of patients.
IV/D: A group of experts reach consensus on a specific issue.
As a clinical example, I always talk about the very first patient, we carried out the result of genetic testing using high-density chips (more than 600,000 polymorphisms) in Russia. A 35-year-old man suffering from bipolar affective disorder who was admitted to psychiatric clinics three times in his life. Previously prescribed therapy either was ineffective or led to weight gain, which is why he stopped taking it. Recently, he was limited to an empirically selected drug and generally felt good. He passed the 23andMe genetic test out of curiosity and gave us information about the decoded genome. After working with the databases of pharmacogenetic companies, we found out which drugs are effective for him, which are not, which can cause side effects. It turned out that what was prescribed in hospitals (according to the guidelines and clinical recommendations for his illness) did not suit him genetically. Only two antidepressants were consistent with his genotype (that is, according to PharmGKB, they did not have a toxic effect and showed normal or increased efficacy). Now this young man feels great, is in a relatively stable remission: he got married and works successfully.
After working with the databases of pharmacogenetic companies, we found out which drugs are effective for him, which are not, which can cause side effects. It turned out that what was prescribed in hospitals (according to the guidelines and clinical recommendations for his illness) did not suit him genetically. Only two antidepressants were consistent with his genotype (that is, according to PharmGKB, they did not have a toxic effect and showed normal or increased efficacy). Now this young man feels great, is in a relatively stable remission: he got married and works successfully.
What will happen tomorrow
Today, our arsenal is mainly monoaminergic (dopaminergic and serotonergic) drugs that indirectly involve other receptor mechanisms (noradrenergic or histamine). Drugs whose action is aimed at correcting other etiopathogenetic pathways are just approaching extensive clinical trials. We have high hopes for pharmaceutical design specialists, but for now, all we can be guided by to optimize the treatment process is knowledge about the genetics of metabolism, pharmacodynamics and pharmacokinetics of existing drugs. This knowledge is still enough to prescribe drugs with a high degree of confidence, achieve remission in a short time, avoid the development of resistance or the development of delayed adverse events.
This knowledge is still enough to prescribe drugs with a high degree of confidence, achieve remission in a short time, avoid the development of resistance or the development of delayed adverse events.
The development of technology and the expansion of our understanding of psychopharmacogenetics show completely unexpected results.
Literature
- Nasyrova R. F., Ivanov M. V., Neznanov N. G. Introduction to psychopharmacogenetics. - St. Petersburg: Publishing Center of St. Petersburg NIPNI im. V.M. Bekhtereva, 2015.
We publish abridged recordings of lectures, webinars, podcasts - that is, oral presentations. The opinion of the speaker may not coincide with the opinion of the editors. We request links to primary sources, but their provision is at the discretion of the speaker.
Test for Bipolar II Disorder (HCL-32) • Psychologist Yaroslav Isaikin
Russian version for detecting hypomanic states. Typically used to detect type II bipolar disorder among patients with a current diagnosis of RDD (recurrent depressive disorder).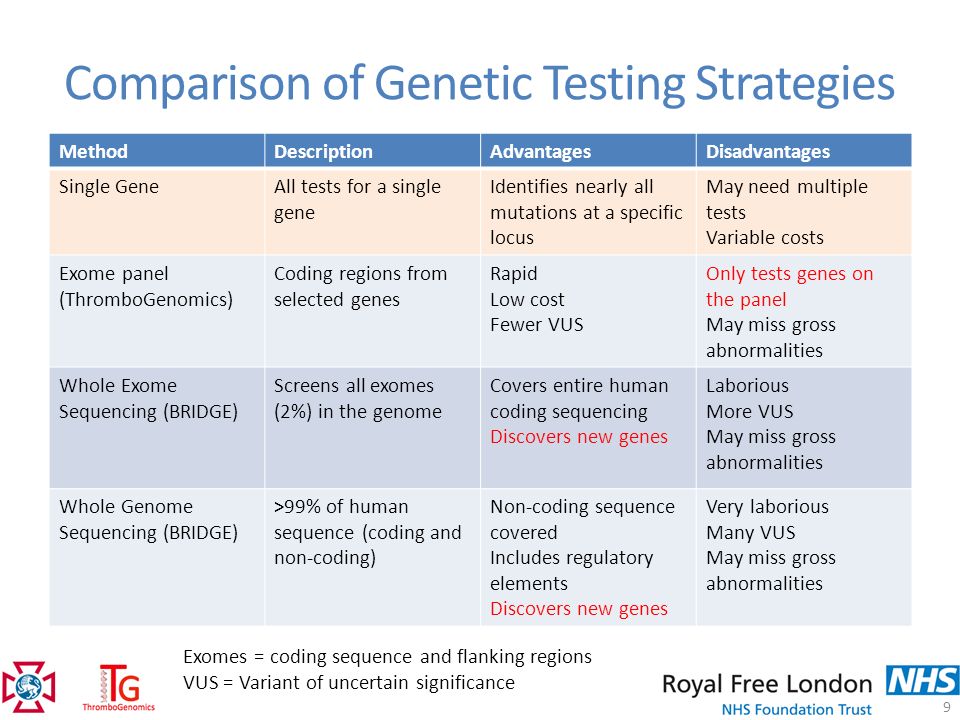
In case of exceeding 14 points, "a suspicion of bipolar affective disorder type II" is set, and a psychiatric consultation on this issue is recommended.
Bipolar affective disorder (old. MDP - manic-depressive psychosis) is an endogenous mental disorder. A feature of BAD is the sequential alternation of “phases”, some of which are manic, and some are depressive. Phases can have different severity, duration, alternation and frequency of occurrence, which determines the specific clinical picture. Since manic episodes are a much more specific manifestation of bipolar disorder than depressive episodes, the diagnosis of bipolar disorder in the framework of the questionnaire is based on diagnosing a manic phase of a certain severity (the main part) and the presence of a sign of alternating "phases" of mood.
Other Bipolar Spectrum Tests:
Bipolar Spectrum Diagnostic Scale for Bipolar Spectrum Disorders
Mood Disorder Questionare for Bipolar I Type
Instructions:
Try to remember a period of "high" condition that was not caused by drugs or alcohol and LASTED MORE THAN A COUPLE OF DAYS (4-6 consecutive days)
How did you feel then?
Please answer questions no matter how you feel right now.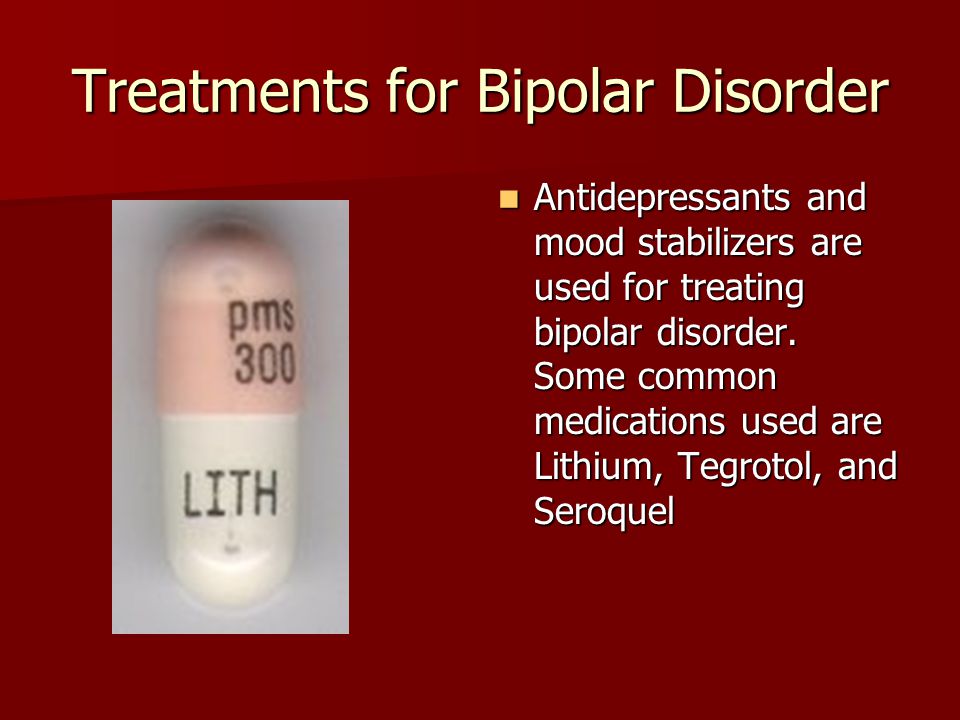
1. I needed less sleep
Yes
No
2. I had more energy and was (was) more active
Yes
No
3. I was (was) more confident
Yes
No
4. Work gave me more pleasure
Yes
No
5. I became more sociable (phoned more often, corresponded with people more often, left the house more)
Yes
No
6. I wanted to travel and actually traveled much more
Yes
No
7. I took risks more often, for example, I began to drive a car at a higher speed
Yes
No
8. I spent more (too much) money
Yes
No
9. In everyday life, I often found myself in risky situations (both at work and in other circumstances)
Yes
No
10. I began to move more (go in for sports, walk, etc.)
Yes
No
11. I had many plans, projects
Yes
No
12. I became more inventive, I had many ideas
I became more inventive, I had many ideas
Yes
No
13. I became less shy and "notorious"
Yes
No
14. I dressed (dressed) more brightly and extravagantly (I used brighter make-up)
Yes
No
15. I wanted to meet people more often, and I really communicated with many
Yes
No
16. I became more interested in sex than usual, sexual desire increased
Yes
No
17. I flirted more often and/or was more sexually active
Yes
No
18. I talked a lot
Yes
No
19. I was thinking faster than usual
Yes
No
20. I joked and punned a lot
Yes
No
21. I am easily distracted
Yes
No
22. I have a lot of new things to do
Yes
No
23. My thoughts jumped from one to another
Yes
No
24. I did everything much faster and easier than usual
Yes
No
25.