Postpartum depression symptoms in males
SAMHSA’s National Helpline | SAMHSA
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.
Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders.
This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative. Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs. In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems. Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.
Addresses concerns of children of parents with substance use/abuse problems.It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt. Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse. Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.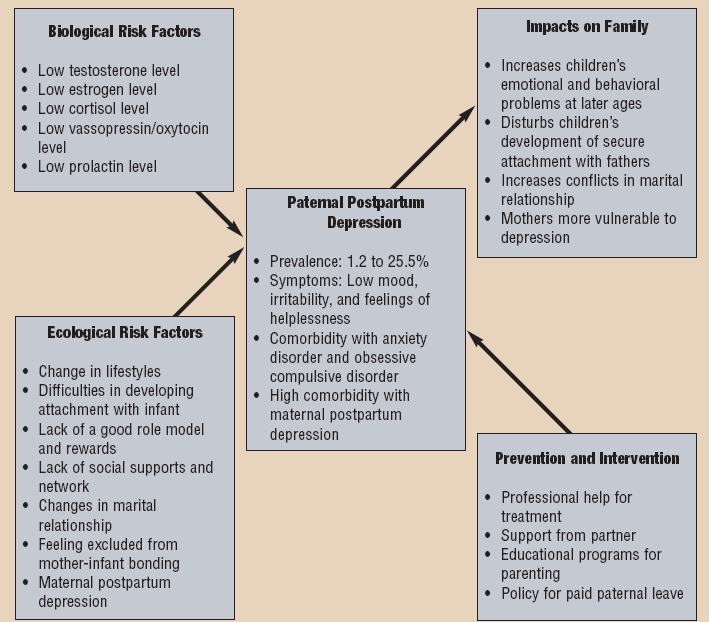
For additional resources, please visit the SAMHSA Store.
Last Updated: 08/30/2022
SAMHSA Behavioral Health Treatment Services Locator
HomeWelcome to the Behavioral Health Treatment Services Locator, a confidential and anonymous source of information for persons seeking treatment facilities in the United States or U.S. Territories for substance use/addiction and/or mental health problems.
PLEASE NOTE: Your personal information and the search criteria you enter into the Locator is secure and anonymous. SAMHSA does not collect or maintain any information you provide.
Please enter a valid location.
please type your address
-
FindTreatment.
 gov
gov Millions of Americans have a substance use disorder. Find a treatment facility near you.
-
988 Suicide & Crisis Lifeline
Call or text 988
Free and confidential support for people in distress, 24/7.
-
National Helpline
1-800-662-HELP (4357)
Treatment referral and information, 24/7.
-
Disaster Distress Helpline
1-800-985-5990
Immediate crisis counseling related to disasters, 24/7.
- Overview
- Locator OverviewLocator Overview
- Locator OverviewLocator Overview
- Finding Treatment
- Find Facilities for VeteransFind Facilities for Veterans
- Find Facilities for VeteransFind Facilities for Veterans
- Facility Directors
- Register a New FacilityRegister a New Facility
- Register a New FacilityRegister a New Facility
- Other Locator Functionalities
- Download Search ResultsDownload Search Results
- Use Google MapsUse Google Maps
- Print Search ResultsPrint Search Results
- Use Google MapsUse Google Maps
- Icon from Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers).
 Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers).
Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers). - Icon from Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers). Find programs providing methadone for the treatment of opioid addiction (heroin or pain relievers).
The Locator is authorized by the 21st Century Cures Act (Public Law 114-255, Section 9006; 42 U.S.C. 290bb-36d). SAMHSA endeavors to keep the Locator current. All information in the Locator is updated annually from facility responses to SAMHSA’s National Substance Use and Mental Health Services Survey (N-SUMHSS). New facilities that have completed an abbreviated survey and met all the qualifications are added monthly. Updates to facility names, addresses, telephone numbers, and services are made weekly for facilities informing SAMHSA of changes. Facilities may request additions or changes to their information by sending an e-mail to [email protected], by calling the BHSIS Project Office at 1-833-888-1553 (Mon-Fri 8-6 ET), or by electronic form submission using the Locator online application form (intended for additions of new facilities).
Updates to facility names, addresses, telephone numbers, and services are made weekly for facilities informing SAMHSA of changes. Facilities may request additions or changes to their information by sending an e-mail to [email protected], by calling the BHSIS Project Office at 1-833-888-1553 (Mon-Fri 8-6 ET), or by electronic form submission using the Locator online application form (intended for additions of new facilities).
Postpartum depression in fathers: does it happen?
In the first year of a child's life, a man may feel unhappy, tired, inept, and even superfluous
Maternal depression after the birth of a child began to be discussed only a few years ago. But experts believe that this problem also has a male face. How does the transformation of a man into a father affect the psyche?
What they mean when they talk about postpartum depression in men
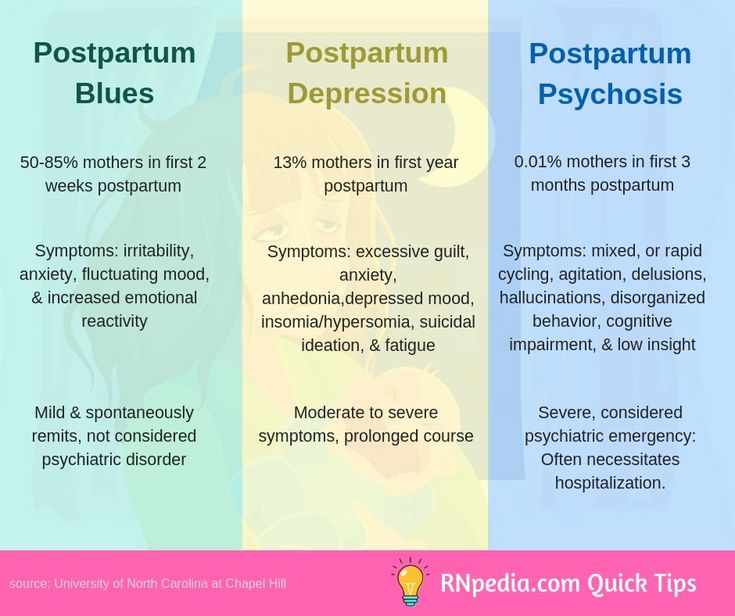
Postpartum depression in women is associated with changes that occur in the mother's body during pregnancy.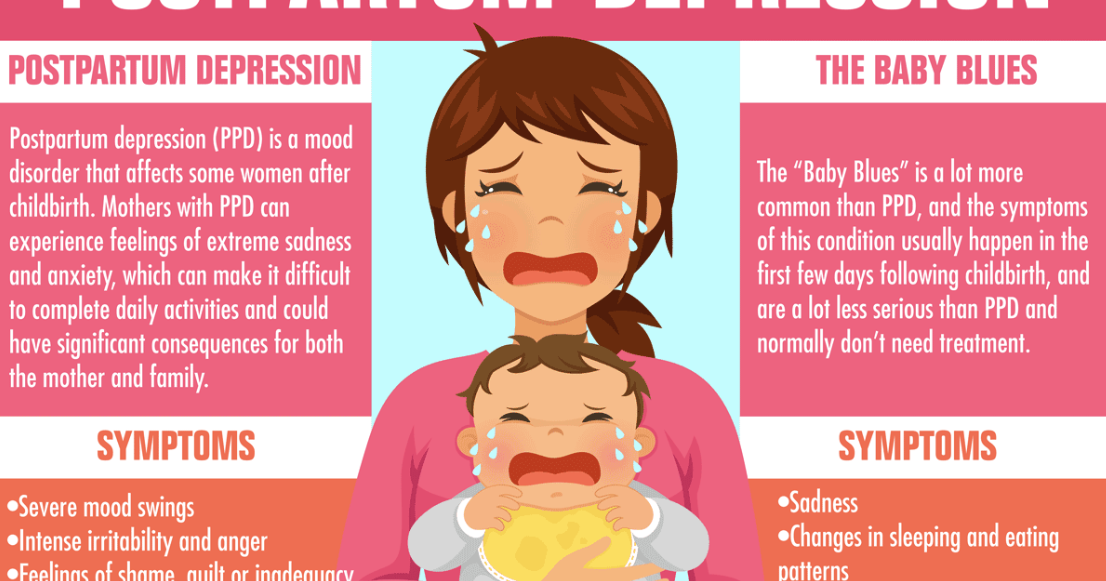 Some of them have a physiological and hormonal nature, so psychologists are cautious about depression with the same name in fathers.
Some of them have a physiological and hormonal nature, so psychologists are cautious about depression with the same name in fathers.
“Do men get postpartum depression? No, it doesn't. Do men have depression as a reaction to the appearance of a child in the family? It happens,” says clinical psychologist Irina Ushkova.
Researchers most often talk about emotional problems that complicate the life of men after the birth of a child in the family. For example, the Danish psychologist Sven Aage Madsen studied paternal depression for more than 25 years and concluded that fathers sometimes experience the same mental disorders as mothers.
Their symptoms are “depression, lack of feeling of closeness with the infant, anger and irritation towards him, desire to avoid responsibility. A person does not feel happy when he looks at his child, does not feel love for him, even if the child was very desirable, and because of this, a feeling of shame arises. Such thoughts and emotions are characteristic of almost all fathers and mothers, it’s just that someone copes with it better, someone worse. ”
”
Why is it difficult to be parents
According to some studies, depression in fathers after the birth of a child often depends on depression in mothers and develops in most cases by the third or sixth month of a baby's life. The depressed state of a woman, caused, among other things, by parental burnout, one way or another affects the state of a man.
“A widely discussed side of modern motherhood is burnout, which is accompanied by physical and emotional fatigue. It is important not to confuse it with depression as a disease that needs serious treatment with the help of psychotherapy or drugs,” explains systemic family psychotherapist Inna Khamitova. “But the extreme degree of burnout — loss of interest in a child, in a husband, in life in general — can turn into depression.”
How does the father of a newborn feel at this time, especially if he is responsible and conscious of his role, if together with his wife he painted a picture of happy days after the birth of the baby?
He holds the long-awaited child in his arms and rejoices at him.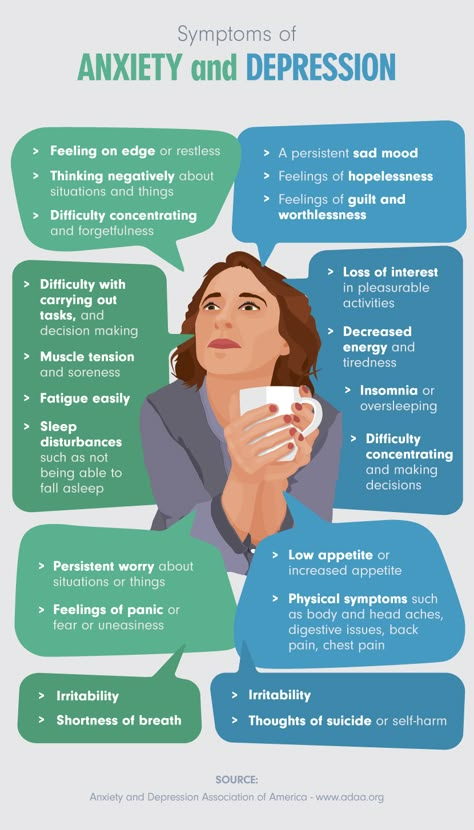 But at the same time, he, like his wife, does not sleep at night, shares responsibility with her to the best of his ability, earns a living for his family, gets tired and feels burned out. Previously, before the birth of a child, he could count on the emotional support of his wife, but now she is completely focused on the child and cannot be in close contact with her husband.
But at the same time, he, like his wife, does not sleep at night, shares responsibility with her to the best of his ability, earns a living for his family, gets tired and feels burned out. Previously, before the birth of a child, he could count on the emotional support of his wife, but now she is completely focused on the child and cannot be in close contact with her husband.
Despite the fact that the everyday side of life with a baby has become much easier, the burden on a young family remains large, especially considering that now most families live separately from older relatives, who in the past made life easier for young parents in one way or another.
“The mother of a newborn often experiences tactile overload: she is constantly with the child, her body does not belong to her,” says Inna Khamitova. - Even ordinary hugs can be a burden for her. Then the father not only experiences his own loneliness and fatigue, but also feels that he is losing the contact that he had with his wife before the baby was born.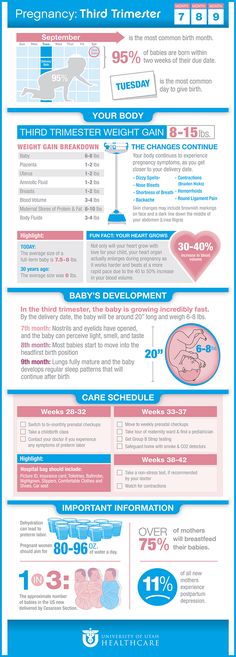
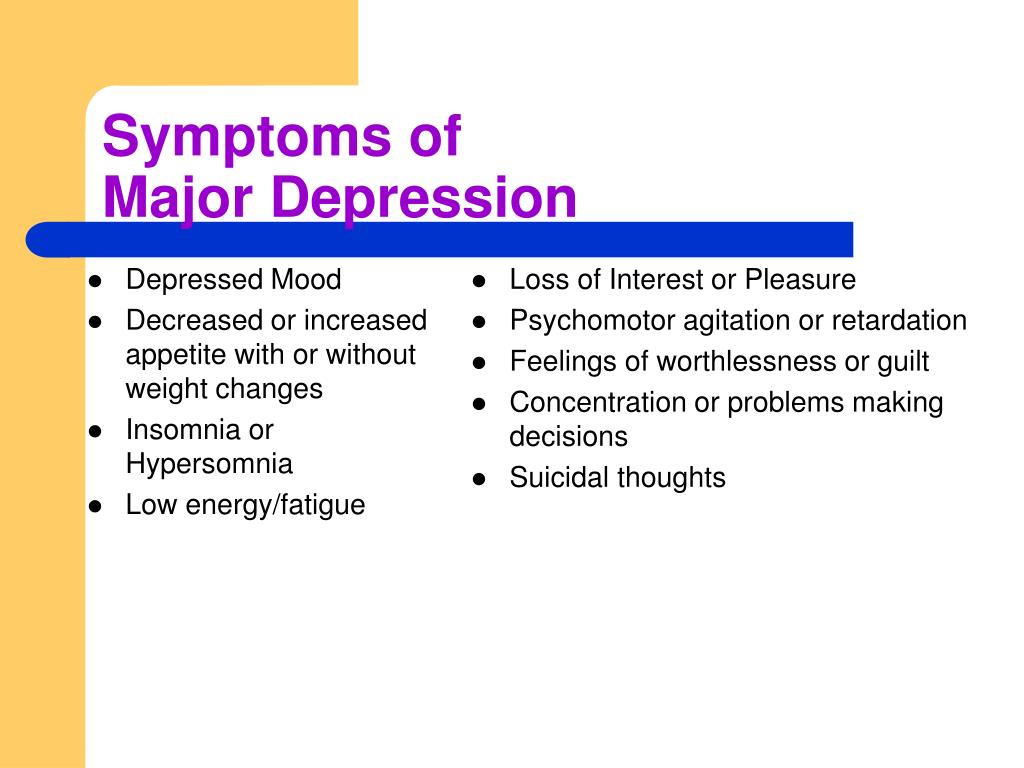
How paternal depression manifests itself
The father sleeps little, he is overworked, he does not receive support. It becomes anxious and suspicious: what if he somehow harms the child, drops it, doesn’t follow it, can’t calm it down, does something wrong?
Maybe you should stay away from the baby, do not touch it again? This is the road to self-isolation from the family, which can be a symptom of burnout or incipient depression.
Most often, men hide their condition, sometimes even from themselves. Practicing psychologists testify that fathers try to fight the manifestations of depression on their own to the last, which can only aggravate the situation. “Men, as a rule, do not show that they are having a hard time, but this burden is difficult to bear alone,” explains psychologist Irina Ushkova. “Therefore, to escape from negative thoughts, alcohol, drugs, risky behavior are used: extreme sports, fast driving without rules.”
A few more symptoms of postpartum depression in fathers:
- increased irritability and conflict, especially in situations that were previously perceived calmly;
- constant voltage;
- aggressive behavior, which in extreme cases is expressed in physical violence;
- avoidance of family and friends, social isolation;
- depression, melancholy, feeling of loneliness;
- pains of various origins, problems with the gastrointestinal tract;
- decreased concentration, distraction, forgetfulness;
- decrease in motivation, unwillingness to do what used to bring pleasure, loss of interest in hobbies;
- a man prefers to spend most of the day at work, thereby being less at home;
- fatigue, rapid exhaustion;
- discrepancy between expectations related to fatherhood and reality.

The story of one father
Russian men still rarely turn to psychologists and psychiatrists about manifestations of depression after the birth of a child. It is generally difficult for fathers to admit their weaknesses. Even those of them who consciously approach their parenthood rarely think about the fact that they have the right to psychological help.
“It’s hard to admit it: on the day my son was born, I didn’t feel the delight, the overwhelming joy that I expected,” the social psychologist, an Englishman of Indian origin, Viren Swami began the story of his depression with these words. — I was missing something: a sense of connection with my newborn son, maybe, but maybe something more. I did not immediately love him the way my wife did, the way I expected to love my son myself.
Viren shares his feelings: he felt anxious at the thought of touching his son, of being with him: “Every time he cried in my arms, I felt like he was rejecting me.”
As a result, the man moved away from his wife and son, moved away from them. “I hated myself when I did this, I felt worthless, I felt like a bad father and husband.”
“I hated myself when I did this, I felt worthless, I felt like a bad father and husband.”
Viren Swami cried a lot, suffered from his impotence, but tried to work hard so as not to feel anything - and yet he felt: longing. At the same time, it never occurred to him to ask for help - even though he himself described the symptoms of depression in men, studying this topic from a scientific point of view. “It was hard for me to admit that I could get depressed, especially at the moment when they expected me to be happy,” the psychologist explains. “There was also a lot of shame: for my weakness, my uselessness as a father, my inability to “cheer up” and take care of my son.”
Change your attitude towards your child and take care of yourself
“Most often, perinatal depression in fathers does not require any long-term treatment,” says Sven Aage Madsen. - It appears because of a child, and the task of a specialist is, first of all, to help change the attitude towards this child.
In most cases, not medicines are needed, but consultations. As a rule, a person feels much better after 4-6 consultations. The main thing is not to be afraid to go to the doctor.
If nothing is done, depression will continue, and this will inevitably affect the development of the child.”
Experts recommend not to bring parental burnout to a depressive state and advise young parents not to hesitate to seek help from a nanny if the financial situation allows, to involve grandparents, if possible.
“Free time is best used for sleep and recuperation. And also remember what used to bring pleasure, and spend part of the time getting this pleasure, ”says Irina Ushkova.
Psychologists also advise not to forget that father and mother remain husband and wife, despite the fact that their life after the birth of a child has changed a lot. “Hoping that everything will gradually get better by itself is an unconstructive position. Difficulties that are obvious to one of the partners do not always seem the same to another.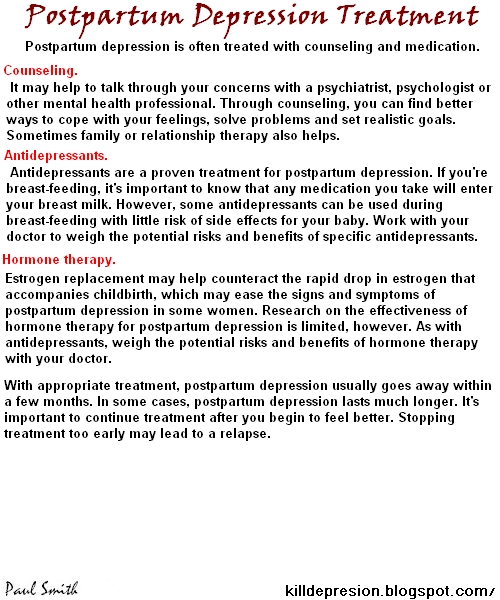 Instead of hushing up problems, it is better to share your experiences, fears, sorrows and joys,” says Inna Khamitova. Don't be silent - speak. And seek help from specialists if you can’t fix the situation on your own.
Instead of hushing up problems, it is better to share your experiences, fears, sorrows and joys,” says Inna Khamitova. Don't be silent - speak. And seek help from specialists if you can’t fix the situation on your own.
Viren Swami's story of depression is not over yet, but he is getting better. The wife helped: she insisted that her husband should see a doctor. “Now I am receiving treatment for depression and I feel better than when my son was born,” the man admits. "I'm still battling the disease and I still have a lot to learn about how to be a good parent."
“I'm worried that one day my son will know that his father couldn't handle his birth,” writes Viren Swami. — But we must be honest with our children... Despite anxiety and fear, despite self-hatred, my love for my son is most important. It grows every day - and it is she who gives me the strength to live. When my son grows up, I hope he will understand: I am bigger than my depression. And I will always love him. "
"
Photo: Collection/iStock
Postpartum depression in men: why it occurs and how to deal with it
Despite the fact that only women are diagnosed with postpartum depression, men also tend to feel sadness, apathy, and anxiety after having children. We talked about this with a young father, and also discussed the topic with clinical and social psychologists - we found out how depression can manifest itself in fathers and why this problem is so rarely talked about.
“When I found out that my wife was pregnant, I wept with joy. I wanted nothing more than to be a father. But sometimes our dreams do not match our expectations. When my wife first handed over our daughter Isabelle to me, I looked at this weak, swollen child and did not know what to do - I did not even want to hold her. I didn't feel anything. I expected a rush of emotions that parents and the media talk about so much, but there was none. Only emptiness. It seemed to me that it was caused by lack of sleep and the chaos associated with the birth of a child, but when a few days later I still did not feel anything, I realized that something was wrong. The numbness turned into indignation and hostility. Isabelle was constantly crying with me and wanted to be with her mother. I felt jealous: my daughter took all the time and attention of my wife, which, no matter how selfish it may sound, she used to give me.
The numbness turned into indignation and hostility. Isabelle was constantly crying with me and wanted to be with her mother. I felt jealous: my daughter took all the time and attention of my wife, which, no matter how selfish it may sound, she used to give me.
I even began to regret the birth of my daughter, which led to feelings of guilt. It was hard, but I told my wife about my experiences. Because I felt like I hated my own daughter.
At first I wanted to leave my family — it sincerely seemed that they would be better off without me. On my anniversary, I even wrote a letter to my wife about it. It was painful for her to watch how I did not want to be the father of the daughter I dreamed of, and it was painful for me to feel this.
This is how a British postman named Ross Hunt remembers the first months of fatherhood - for several years now he has been talking on his blog about the postpartum depression he faced.
Despite the fact that there is no official diagnosis of "postpartum depression in men", manifestations of this phenomenon are common.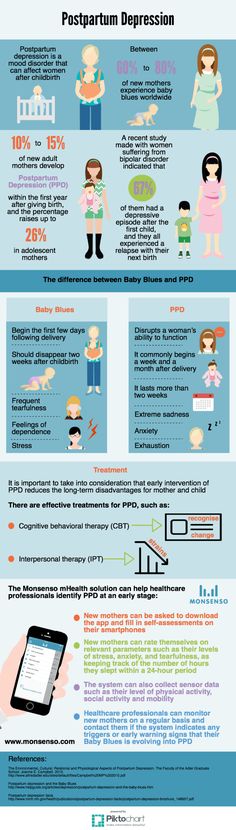 According to statistics, approximately 10% of fathers suffer from this disorder. However, it is much more difficult to establish the exact number of depressive episodes in men after the birth of a child than in women.
According to statistics, approximately 10% of fathers suffer from this disorder. However, it is much more difficult to establish the exact number of depressive episodes in men after the birth of a child than in women.
Men are less likely to talk about their emotions, even if they think something is going wrong everything that is stereotypically perceived as "feminine". Talking about feelings falls under this category. Traditional masculinity "allows" men to show only certain emotions (for example, aggression) and "forbids" others (empathy, kindness): "According to traditional masculinity, a man should cope with problems on his own. If you can’t deal with depression (which, by the way, is often perceived as “just a bad mood”), then what kind of man are you?
A man may not uphold the norms of traditional masculinity, but if he thinks that those around him approve of him, then he will adhere to these requirements. Moreover, sociological studies show that men, in principle, are less likely than women to turn to specialists if they have health problems - physical or mental. And they do not always speak honestly about their condition because of embarrassment or fear of changing their lifestyle on the advice of a doctor.
And they do not always speak honestly about their condition because of embarrassment or fear of changing their lifestyle on the advice of a doctor.
Vlad Krivoshchekov notes that the field of health in Russia is, in principle, very feminized: in heterosexual families, women are more often responsible for the health of all family members, and most of the advertising about medicines and doctors is addressed to mothers. As a result, many men have a poorly developed skill of contacting doctors for help. Often men go to the clinic only when their wives, mothers or sisters send them there.
How does postpartum depression manifest itself in men
Postpartum depression can manifest itself in completely different ways and affect both a person’s emotions and his physical condition. The father may experience depression, apathy, guilt, jealousy. He is characterized by manifestations of aggression. He can move away from the family and behave irrationally, get annoyed for any reason. A man with postpartum depression, says clinical psychologist Anastasia Tretyakova, does everything mechanically. He loses the initiative to do something. He wants to isolate himself from society, withdraws into himself, does not joke, does not go anywhere, does not think logically, does not show empathy. It is difficult for him to accept the point of view of another person. A person with a psychological disorder loses appetite, sleep problems appear, and libido decreases.
A man with postpartum depression, says clinical psychologist Anastasia Tretyakova, does everything mechanically. He loses the initiative to do something. He wants to isolate himself from society, withdraws into himself, does not joke, does not go anywhere, does not think logically, does not show empathy. It is difficult for him to accept the point of view of another person. A person with a psychological disorder loses appetite, sleep problems appear, and libido decreases.
Causes of postpartum depression in men
Causes of postpartum depression in men are very similar to factors of depression in women. Firstly, after the birth of a child, men can also change their hormonal levels. Modern research claims that new fathers, for example, have reduced testosterone levels.
Robin Edelstein, psychologist and director of the Personality, Relationships, and Hormones Laboratory at the University of Michigan, says these changes have a positive effect on the development of empathy and attachment to children: men with lower testosterone levels devote more time to children and family.
The second possible reason is additional responsibility and stress. “It can be difficult for men to cope with the burden of responsibility that they have placed on themselves. From now on, they have to work much more and earn more - this causes lack of sleep and chronic fatigue, ”says Anastasia Tretyakova.
Piotr, aged 37 :
“When our daughter was born, I was incredibly happy. I remember that I just jokingly thought: "Goodbye, that's it!" In fact, after that day, I almost completely said goodbye to music, writing and everything except work and home. There was almost never more time for this, no matter how I tried to find it. After the birth of the child, my wife and I began to sleep little. Our daughter was restless, often waking up and screaming. We rocked her for hours. Sometimes she would not stop yelling from morning to evening. Life was chaos, we literally survived. I worked in fits and starts when I could: during daytime sleep or walks with a stroller, at night in between awakenings from colic. Credit obligations began to put more pressure on my brain: my thoughts were only occupied by the question of how to provide for my family. Due to lack of sleep, I did everything automatically, not really thinking about how I felt. Apparently, this was my way of dealing with emotions - not connecting them. No one helped me deal with stress. It was I who had to help my wife and fight with my mother-in-law, who constantly prevented me from taking care of my daughter. There were no other options. I realized that I did not have the option to say that I could not carry a screaming child at night - who then could? There was no option not to make money. The concept of “tired” basically ceased to exist for me.”
Credit obligations began to put more pressure on my brain: my thoughts were only occupied by the question of how to provide for my family. Due to lack of sleep, I did everything automatically, not really thinking about how I felt. Apparently, this was my way of dealing with emotions - not connecting them. No one helped me deal with stress. It was I who had to help my wife and fight with my mother-in-law, who constantly prevented me from taking care of my daughter. There were no other options. I realized that I did not have the option to say that I could not carry a screaming child at night - who then could? There was no option not to make money. The concept of “tired” basically ceased to exist for me.”
How to distinguish depression from a depressive episode?
Full-blown depression differs from a depressive episode in duration and intensity. If the episode is repeated several times, it is worth thinking about the external causes of the disorder and ways to eliminate them.