Treating adhd naturally in kids
Natural Remedies for ADHD Without Medication: Nutrition, Supplements, Sleep
No treatment plan for attention deficit hyperactivity disorder (ADHD) is complete if it doesn’t harness the power of nutrition, exercise, and sleep to improve wellbeing. What we eat, our physical activity levels, our sleep habits, and lifestyle factors ranging from stress management to screen time have a tremendous effect on health – a fact that’s amplified for ADHD brains and bodies.
Regardless of whether your child’s treatment includes medication, maximizing exercise, sleep, and nutrition can effectively transform them into natural remedies for ADHD, and arguably establish the foundation upon which to build other interventions.
Mounting research suggests that eating well contributes positively to the performance and abilities of any child with ADHD. 1
When working to improve your child’s wellbeing, begin by considering the glycemic index (GI), or how fast the body converts carbohydrates into sugar.
All carbohydrates turn into sugar, but some are converted faster (high glycemic index) and some slower (low GI). These rates of conversion affect a child’s energy levels over the day; anything that causes blood sugar levels to quickly spike (like sugary, processed foods) means that the body will work hard to quickly drop that sugar, actually bringing it below normal levels. The result is often an irritable, fidgety, or nervous child who can’t focus as well.
To maintain steady, normal blood sugar levels, ensure that your child’s meals, especially at the start of the day, are balanced:
A significant percentage of children with ADHD are sensitive (not allergic) to some kind of food. In one study that placed children with ADHD on a restricted elimination meal plan, more than half of subjects saw a 40% improvement on ADHD rating scale performance.4 The same results appeared in an older study, where hyperactive children saw improvement in behavior after being placed on a “few foods” plan. 5
5
In my practice, I estimate that about 30% to 50% of children I see do have some food sensitivity.
Not sure what food sensitives your child may have? Try this technique I use with my patients: eliminate a whole set of foods – dairy, wheat, corn, soy, eggs (common culprits) – for three weeks.
[Eggs, Dairy, Nuts, and Soy: Testing for Sensitivities with an ADHD Elimination Foods Plan]
Eliminating foods, in my experience, tend to work on children who primarily present symptoms of hyperactivity rather than inattentiveness. This method also works on children who already have a history of allergies, eczema, gastrointestinal issues, and other allergic-type manifestations.
Several studies show that artificial colors, flavors, and preservatives tend to increase hyperactivity in a sizable portion of children, ADHD or not.6 In addition, studies suggest that a subset of children with ADHD are sensitive to food dyes, and may see symptoms worsen. 7
7
Opt for whole foods to avoid synthetic dyes, and, as with food sensitivities, try to detect through a process of elimination if your child is sensitive to a particular dye.
This is the most common supplement used by patients with ADHD. Why? Studies show that omega-3 fatty acids (with high doses of EPA) are modestly effective in treating ADHD in children.8 Fish oil, which is associated with few/mild side effects, helps to increase levels of omega-3s that are often naturally lacking in children with ADHD, which in turn helps with brain functioning. Although dosing amounts are not established, I recommend 1000mg a day of combined EPA+DHA for children ages 5 to 8, 1500 mg a day for children ages 8 to 12, and 2000 mg a day for older children.
Can’t get your sensory-sensitive child to take fish oil supplements? Click here for tips.
Many children with ADHD are relatively iron (serum ferretin) deficient9, which may explain irregular dopamine regulation in the brain10. One small study showed that children with ADHD who took iron supplements saw an improvement in ADHD symptoms compared to children who took a placebo.11 Have your child’s doctor measure their serum ferritin levels to see if an iron supplement is necessary. For non-anemic patients, I recommend up to 40 mg of chelated iron a day. (The chelated form is associated with fewer gastrointestinal side effects.)
One small study showed that children with ADHD who took iron supplements saw an improvement in ADHD symptoms compared to children who took a placebo.11 Have your child’s doctor measure their serum ferritin levels to see if an iron supplement is necessary. For non-anemic patients, I recommend up to 40 mg of chelated iron a day. (The chelated form is associated with fewer gastrointestinal side effects.)
Multiple research studies shows that many children with ADHD clearly benefit from exercise.15 Even a single, 20-minute bout of aerobic exercise improves attention and academic performance in this group, according to one study.16 Another small study of children with ADHD found that acute exercise normalizes arousal and alertness levels, based on findings from EEG readings.17
Exercise can be so therapeutic for ADHD symptoms that I recommend against sacrificing exercise time for tutoring or because of poor grades. In fact, research seems to indicate that exercise improves academic scores perhaps better than spending the equivalent amount in class or study time. 18
18
The American Academy of Pediatrics (AAP) recommends at least one hour of moderate to vigorous exercise a day for children and adolescents.19 I recommend five days a week of exercise for my patients. (Physical education in school can count, so long as it increases heart rate and works up a sweat.) Interestingly, how much exercise helps any particular person may depend on genetics, with brain-derived neurotrophic factor (BDNF) playing a major role in the relationship.20
Some children with ADHD may prefer individual sports, like swimming, tennis, or cycling, as opposed to team sports. Some studies show that martial arts, especially taekwondo, benefit children with ADHD.21
If your child resists exercise, consider tying it to something virtually all children want: screen time. They can have an hour of tablet time, for example, only if they’re on a stationary bike or treadmill during that time. Some adolescents may benefit from working with a personal trainer to keep them accountable and motivated.
Don’t forget about time in nature. According to one study, green outdoor activities reduce ADHD symptoms in children more than activities conducted in other settings.22
Unstructured play is not the same as exercise, but it is just as important for all children. Unstructured, creative play is crucial for normal development, as it is where young children learn to work things out independently and forge social relationships23 — important skills for children with ADHD especially. So, let your child ride their bike, run around, or play outside with other children if it is safe to do so. Leave them be if they are on a play date. Find programs that emphasize and maximize independent play.
Adequate sleep is crucial for children with ADHD, who are already at a higher risk for a variety of sleep disturbances, like difficulty falling asleep, compared to children without ADHD.24 Inadequate sleep affects ADHD symptoms and overall functioning.
The American Academy of Sleep Medicine (AASM) establishes the following guidelines for daily sleep amounts in children, which are supported by the AAP:27
If sleep problems persist, consult with your child’s medical providers. They may be able to run a sleep study to test for disorders. Behavioral professional psychologists and counselors can also help with implementing healthy sleep routines. Ask the pediatrician to check your child’s serum ferritin levels, as low levels are associated with restless sleep.31
They may be able to run a sleep study to test for disorders. Behavioral professional psychologists and counselors can also help with implementing healthy sleep routines. Ask the pediatrician to check your child’s serum ferritin levels, as low levels are associated with restless sleep.31
By far, screen time/digital media use is the most difficult and argument-producing problem among the many families I help. Many studies link excessive screen time to issues like poor sleep quality, poor mental health, emotional dysregulation, lower academic achievement, lower levels of physical activity, and even developmental delays in children and teens.3233
Studies correlate increased screen time with symptoms of ADHD. According to a study of preschool-age children, those who had more than two hours of screen time a day were more likely to exhibit clinically significant symptoms of inattention compared to children with less than 30 minutes of screen time per day. 34 Another study found that higher frequency of digital media use was associated with subsequent symptoms of ADHD in adolescents after a two-year follow-up.35 Note, however, that research does not establish a causal link between screen time and ADHD.
34 Another study found that higher frequency of digital media use was associated with subsequent symptoms of ADHD in adolescents after a two-year follow-up.35 Note, however, that research does not establish a causal link between screen time and ADHD.
There also appears to be a subset of children with ADHD whose symptoms are worsened by even small amounts of screen time.36
For children 2 to 5 years of age, the AAP recommends one hour a day at most of co-viewed high-quality programming.37 For older children, it recommends a personalized media use plan that considers the individual child’s age, health, temperament, and developmental stage.38 Additional recommendations include the following:
In addition to the above guidance, I also encourage families to think of the following for managing screen time:
Stress is a natural part of life. But some children with ADHD, in my experience, are very sensitive to stress. Part of it is that these children – more than neurotypical children – can be exposed to a great deal of negative feedback on a regular basis which affects self-esteem and wellbeing.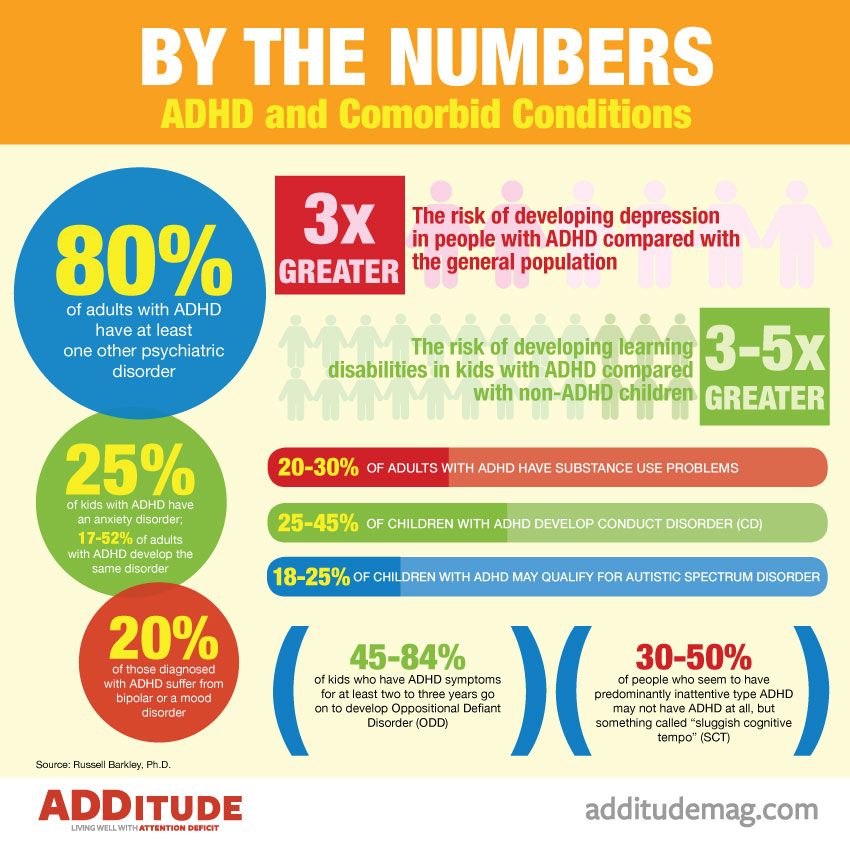 40 Use the following strategies to mitigate your child’s stress:
40 Use the following strategies to mitigate your child’s stress:
The content for this article was derived from the ADDitude Expert Webinars “How Nutrition, Sleep, Exercise & Behavioral Interventions Can Reduce ADHD Symptoms” and “Lifestyle Changes with the Biggest Impact on Kids with ADHD,” with Sanford Newmark, M.D., which were broadcast live on April 24, 2018 and August 4, 2022, respectively.
SUPPORT ADDITUDE
Thank you for reading ADDitude. To support our mission of providing ADHD education and support, please consider subscribing. Your readership and support help make our content and outreach possible. Thank you.
1 Del-Ponte, B., Quinte, G. C., Cruz, S., Grellert, M., & Santos, I. S. (2019). Dietary patterns and attention deficit/hyperactivity disorder (ADHD): A systematic review and meta-analysis. Journal of Affective Disorders, 252, 160–173. https://doi.org/10.1016/j.jad.2019.04.061
2 Cooper, S. , Bandelow, S., Nute, M., Morris, J., & Nevill, M. (2012). Breakfast glycaemic index and cognitive function in adolescent school children. British Journal of Nutrition, 107(12), 1823-1832. doi:10.1017/S0007114511005022
, Bandelow, S., Nute, M., Morris, J., & Nevill, M. (2012). Breakfast glycaemic index and cognitive function in adolescent school children. British Journal of Nutrition, 107(12), 1823-1832. doi:10.1017/S0007114511005022
3 Roberts, J. R., Dawley, E. H., & Reigart, J. R. (2019). Children’s low-level pesticide exposure and associations with autism and ADHD: a review. Pediatric Research, 85(2), 234–241. https://doi.org/10.1038/s41390-018-0200-z
4 Pelsser, Lidy M et al. (2011). Effects of a restricted elimination food plan on the behaviour of children with attention-deficit hyperactivity disorder (INCA study): a randomised controlled trial. The Lancet, Volume 377, Issue 9764, 494 – 503. https://doi.org/10.1016/S0140-6736(10)62227-1
5 Carter CM, Urbanowicz M, Hemsley R, et al.(1993). Effects of a few food plan in attention deficit disorder. Archives of Disease in Childhood, 69:564-568.
6 Nigg, J. T., & Holton, K. (2014). Restriction and elimination food plans in ADHD treatment. Child and adolescent psychiatric clinics of North America, 23(4), 937–953. doi:10.1016/j.chc.2014.05.010
T., & Holton, K. (2014). Restriction and elimination food plans in ADHD treatment. Child and adolescent psychiatric clinics of North America, 23(4), 937–953. doi:10.1016/j.chc.2014.05.010
7 Nigg, J. T., Lewis, K., Edinger, T., & Falk, M. (2012). Meta-analysis of attention-deficit/hyperactivity disorder or attention-deficit/hyperactivity disorder symptoms, restriction diet, and synthetic food color additives. Journal of the American Academy of Child and Adolescent Psychiatry, 51(1), 86–97.e8. https://doi.org/10.1016/j.jaac.2011.10.015
8 Bloch, M., Qawasmi, A. (2011). Omega-3 Fatty Acid Supplementation for the Treatment of Children With Attention-Deficit/Hyperactivity Disorder Symptomatology: Systematic Review and Meta-Analysis. Journal of the American Academy of Child and Adolescent Psychiatry, 50(10), 991-1000. https://doi.org/10.1016/j.jaac.2011.06.008
9 Konofal, E., Lecendreux, M.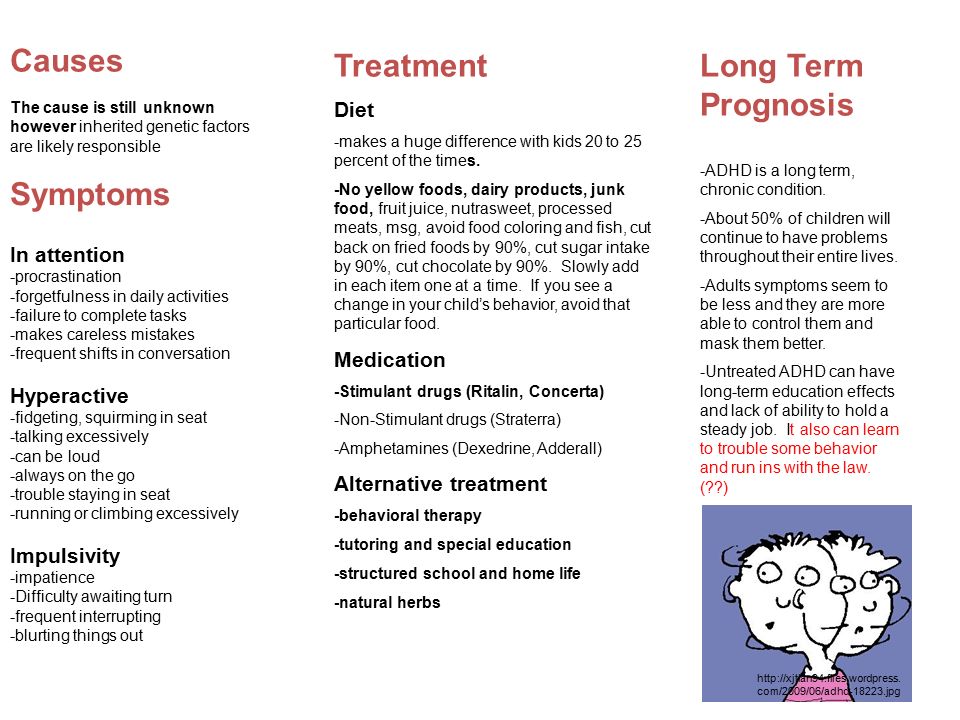 , Arnulf, I., & Mouren, M. C. (2004). Iron deficiency in children with attention-deficit/hyperactivity disorder. Archives of pediatrics & adolescent medicine, 158(12), 1113–1115. https://doi.org/10.1001/archpedi.158.12.1113
, Arnulf, I., & Mouren, M. C. (2004). Iron deficiency in children with attention-deficit/hyperactivity disorder. Archives of pediatrics & adolescent medicine, 158(12), 1113–1115. https://doi.org/10.1001/archpedi.158.12.1113
10 Wang, Y., Huang, L., Zhang, L., Qu, Y., & Mu, D. (2017). Iron Status in Attention-Deficit/Hyperactivity Disorder: A Systematic Review and Meta-Analysis. PloS one, 12(1), e0169145. https://doi.org/10.1371/journal.pone.0169145
11 Konofal, E., Lecendreux, M., et.al. (2008). Effects of iron supplementation on attention deficit hyperactivity disorder in children. Pediatric Neurology, 38(1), 20-26. https://doi.org/10.1016/j.pediatrneurol.2007.08.014
12Gan, J., Galer, P., Ma, D., Chen, C., & Xiong, T. (2019). The effect of vitamin d supplementation on attention-deficit/hyperactivity disorder: A systematic review and meta-analysis of randomized controlled trials. Journal of Child and Adolescent Psychopharmacology, 29(9), 670–687. https://doi.org/10.1089/cap.2019.0059
Journal of Child and Adolescent Psychopharmacology, 29(9), 670–687. https://doi.org/10.1089/cap.2019.0059
13Li, H. H., Yue, X. J., Wang, C. X., Feng, J. Y., Wang, B., & Jia, F. Y. (2020). Serum levels of vitamin a and vitamin d and their association with symptoms in children with attention deficit hyperactivity disorder. Frontiers in Psychiatry, 11, 599958. https://doi.org/10.3389/fpsyt.2020.599958
14Granero, R., Pardo-Garrido, A., Carpio-Toro, I. L., Ramírez-Coronel, A. A., Martínez-Suárez, P. C., & Reivan-Ortiz, G. G. (2021). The role of iron and zinc in the treatment of ADHD among children and adolescents: A systematic review of randomized clinical trials. Nutrients, 13(11), 4059. https://doi.org/10.3390/nu13114059
15Christiansen, L., Beck, M. M., Bilenberg, N., Wienecke, J., Astrup, A., & Lundbye-Jensen, J. (2019). Effects of exercise on cognitive performance in children and adolescents with ADHD: potential mechanisms and evidence-based recommendations. Journal of Clinical Medicine, 8(6), 841. https://doi.org/10.3390/jcm8060841
Journal of Clinical Medicine, 8(6), 841. https://doi.org/10.3390/jcm8060841
16Pontifex, M. B., Saliba, B. J., Raine, L. B., Picchietti, D. L., & Hillman, C. H. (2013). Exercise improves behavioral, neurocognitive, and scholastic performance in children with attention-deficit/hyperactivity disorder. The Journal of Pediatrics, 162(3), 543–551. https://doi.org/10.1016/j.jpeds.2012.08.036
17Huang, C. J., Huang, C. W., Hung, C. L., Tsai, Y. J., Chang, Y. K., Wu, C. T., & Hung, T. M. (2018). Effects of acute exercise on resting EEG in children with attention-deficit/hyperactivity disorder. Child Psychiatry and Human Development, 49(6), 993–1002. https://doi.org/10.1007/s10578-018-0813-9
18McPherson, A., Mackay, L., Kunkel, J., & Duncan, S. (2018). Physical activity, cognition and academic performance: An analysis of mediating and confounding relationships in primary school children. BMC Public Health, 18(1), 936. https://doi.org/10.1186/s12889-018-5863-1
https://doi.org/10.1186/s12889-018-5863-1
19Lobelo, F., Muth, N. D., Hanson, S., Nemeth, B. A., COUNCIL ON SPORTS MEDICINE AND FITNESS, & SECTION ON…(2020). Physical activity assessment and counseling in pediatric clinical settings. Pediatrics, 145(3), e20193992. https://doi.org/10.1542/peds.2019-3992
20Hopkins, M. E., Davis, F. C., Vantieghem, M. R., Whalen, P. J., & Bucci, D. J. (2012). Differential effects of acute and regular physical exercise on cognition and affect. Neuroscience, 215, 59–68. https://doi.org/10.1016/j.neuroscience.2012.04.056
21Kadri, A., Slimani, M., Bragazzi, N. L., Tod, D., & Azaiez, F. (2019). Effect of taekwondo practice on cognitive function in adolescents with attention deficit hyperactivity disorder. International Journal of Environmental Research and Public Health, 16(2), 204. https://doi.org/10.3390/ijerph26020204
22 Kuo, F. E., & Taylor, A. F. (2004). A potential natural treatment for attention-deficit/hyperactivity disorder: Evidence from a national study. American Journal of Public Health, 94(9), 1580–1586. https://doi.org/10.2105/ajph.94.9.1580
E., & Taylor, A. F. (2004). A potential natural treatment for attention-deficit/hyperactivity disorder: Evidence from a national study. American Journal of Public Health, 94(9), 1580–1586. https://doi.org/10.2105/ajph.94.9.1580
23 Lee, R., Lane, S., Brown, G., Leung, C., Kwok, S., & Chan, S. (2020). Systematic review of the impact of unstructured play interventions to improve young children’s physical, social, and emotional wellbeing. Nursing & Health Sciences, 22(2), 184–196. https://doi.org/10.1111/nhs.12732
24 Bondopadhyay, U., Diaz-Orueta, U., & Coogan, A. N. (2022). A systematic review of sleep and circadian rhythms in children with attention deficit hyperactivity disorder. Journal of Attention Disorders, 26(2), 149–224. https://doi.org/10.1177/1087054720978556
25 Hvolby A. (2015). Associations of sleep disturbance with ADHD: Implications for treatment. Attention Deficit and Hyperactivity Disorders, 7(1), 1–18. https://doi.org/10.1007/s12402-014-0151-0
https://doi.org/10.1007/s12402-014-0151-0
26 Wolraich, M. L., Hagan, J. F., Jr, Allan, C., Chan, E., Davison, D., Earls, M., Evans, S. W., Flinn, S. K., Froehlich, T., Frost, J., Holbrook, J. R., Lehmann, C. U., Lessin, H. R., Okechukwu, K., Pierce, K. L., Winner, J. D., Zurhellen, W., & SUBCOMMITTEE ON CHILDREN AND ADOLESCENTS WITH ATTENTION-DEFICIT/HYPERACTIVE DISORDER (2019). Clinical practice guideline for the diagnosis, evaluation, and treatment of attention-deficit/hyperactivity disorder in children and adolescents. Pediatrics, 144(4), e20192528. https://doi.org/10.1542/peds.2019-2528
27 Paruthi, S., Brooks, L. J., D’Ambrosio, C., Hall, W. A., Kotagal, S., Lloyd, R. M., Malow, B. A., Maski, K., Nichols, C., Quan, S. F., Rosen, C. L., Troester, M. M., & Wise, M. S. (2016). Recommended amount of sleep for pediatric populations: A consensus statement of the american academy of sleep medicine. Journal of Clinical Sleep Medicine : JCSM : Official Publication of the American Academy of Sleep Medicine, 12(6), 785–786. https://doi.org/10.5664/jcsm.5866
https://doi.org/10.5664/jcsm.5866
28 Shechter, A., Kim, E. W., St-Onge, M. P., & Westwood, A. J. (2018). Blocking nocturnal blue light for insomnia: A randomized controlled trial. Journal of Psychiatric Research, 96, 196–202. https://doi.org/10.1016/j.jpsychires.2017.10.015
29 Guadagna, S., Barattini, D. F., Rosu, S., & Ferini-Strambi, L. (2020). Plant Extracts for Sleep Disturbances: A Systematic Review. Evidence-Based Complementary and Alternative Medicine: eCAM, 2020, 3792390. https://doi.org/10.1155/2020/3792390
30 Haghayegh, S., Khoshnevis, S., Smolensky, M. H., Diller, K. R., & Castriotta, R. J. (2019). Before-bedtime passive body heating by warm shower or bath to improve sleep: A systematic review and meta-analysis. Sleep Medicine Reviews, 46, 124–135. https://doi.org/10.1016/j.smrv.2019.04.008
31 Cortese, S., Konofal, E., Bernardina, B. D., Mouren, M. C., & Lecendreux, M. (2009). Sleep disturbances and serum ferritin levels in children with attention-deficit/hyperactivity disorder. European Child & Adolescent Psychiatry, 18(7), 393–399. https://doi.org/10.1007/s00787-009-0746-8
C., & Lecendreux, M. (2009). Sleep disturbances and serum ferritin levels in children with attention-deficit/hyperactivity disorder. European Child & Adolescent Psychiatry, 18(7), 393–399. https://doi.org/10.1007/s00787-009-0746-8
32Madigan, S., Browne, D., Racine, N., Mori, C., & Tough, S. (2019). Association Between Screen Time and Children’s Performance on a Developmental Screening Test. JAMA Pediatrics, 173(3), 244–250. https://doi.org/10.1001/jamapediatrics.2018.5056
33 Stiglic, N., & Viner, R. M. (2019). Effects of screentime on the health and well-being of children and adolescents: a systematic review of reviews. BMJ Open, 9(1), e023191. https://doi.org/10.1136/bmjopen-2018-023191
34 Tamana, S. K., Ezeugwu, V., Chikuma, J., Lefebvre, D. L., Azad, M. B., Moraes, T. J., Subbarao, P., Becker, A. B., Turvey, S. E., Sears, M. R., Dick, B. D., Carson, V., Rasmussen, C., CHILD study Investigators, Pei, J.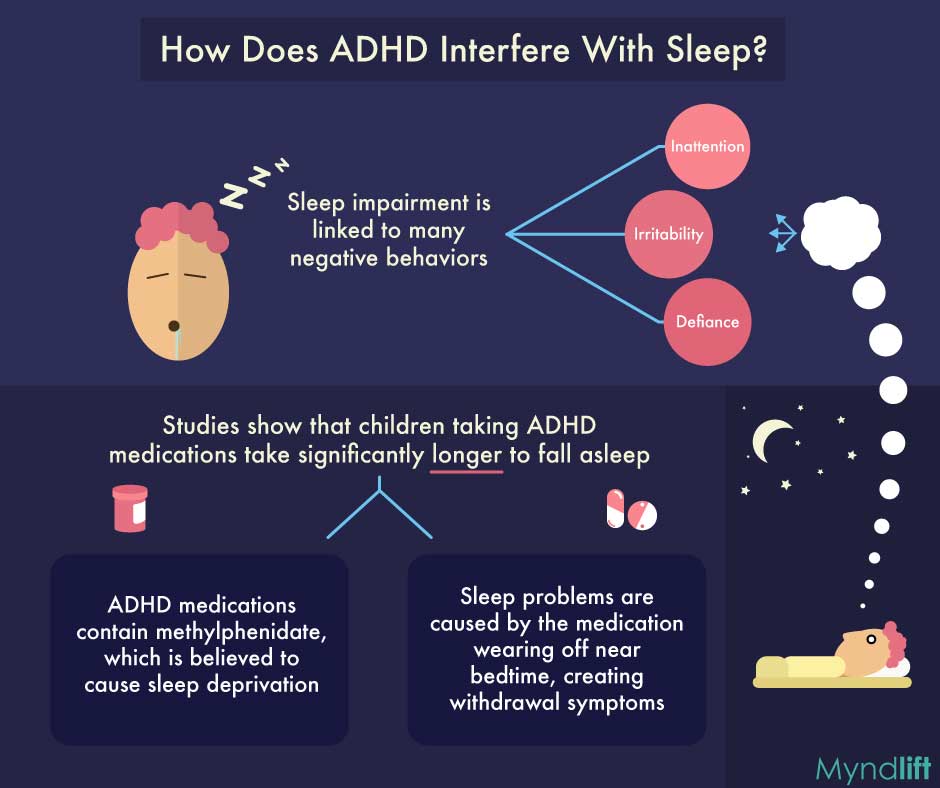 , & Mandhane, P. J. (2019). Screen-time is associated with inattention problems in preschoolers: Results from the CHILD birth cohort study. PloS one, 14(4), e0213995. https://doi.org/10.1371/journal.pone.0213995
, & Mandhane, P. J. (2019). Screen-time is associated with inattention problems in preschoolers: Results from the CHILD birth cohort study. PloS one, 14(4), e0213995. https://doi.org/10.1371/journal.pone.0213995
35 Ra, C. K., Cho, J., Stone, M. D., De La Cerda, J., Goldenson, N. I., Moroney, E., Tung, I., Lee, S. S., & Leventhal, A. M. (2018). Association of digital media use with subsequent symptoms of attention-deficit/hyperactivity disorder among adolescents. JAMA, 320(3), 255–263. https://doi.org/10.1001/jama.2018.8931
36 Vaidyanathan, S., Manohar, H., Chandrasekaran, V., & Kandasamy, P. (2021). Screen Time Exposure in Preschool Children with ADHD: A Cross-Sectional Exploratory Study from South India. Indian Journal of Psychological Medicine, 43(2), 125–129. https://doi.org/10.1177/0253717620939782
37 COUNCIL ON COMMUNICATIONS AND MEDIA (2016). Media and Young Minds. Pediatrics, 138(5), e20162591. https://doi.org/10.1542/peds.2016-2591
https://doi.org/10.1542/peds.2016-2591
38 COUNCIL ON COMMUNICATIONS AND MEDIA (2016). Media Use in School-Aged Children and Adolescents. Pediatrics, 138(5), e20162592. https://doi.org/10.1542/peds.2016-2592
39 Antshel, K. M., Faraone, S. V., & Gordon, M. (2014). Cognitive behavioral treatment outcomes in adolescent ADHD. Journal of Attention Disorders, 18(6), 483–495. https://doi.org/10.1177/1087054712443155
40 Harpin, V., Mazzone, L., Raynaud, J. P., Kahle, J., & Hodgkins, P. (2016). Long-Term Outcomes of ADHD: A systematic review of self-esteem and social function. Journal of Attention Disorders, 20(4), 295–305. https://doi.org/10.1177/1087054713486516
41 Zendarski, N., Haebich, K., Bhide, S. (2020). Student-teacher relationship quality in children with and without ADHD: A cross-sectional community based study. Early Childhood Research Quarterly, 51, 275-284. https://doi.org/10.1016/j.ecresq.2019.12.006
https://doi.org/10.1016/j.ecresq.2019.12.006
Augment ADD Treatment with Medication
A healthy diet is one way to treat adhd without medication.1 of 12
Do Natural Remedies for ADHD Work?
Medication is a valuable tool for managing the core symptoms of attention deficit hyperactivity disorder (ADHD). For those people who do not want to take the medication route behavioral therapy, nutrition and lifestyle changes, and/or brain training, among other natural therapies designed to improve focus and impulsivity may help alleviate some ADHD symptoms.
The fact remains: Between 80%-85% of patients with ADHD experience a positive response to methylphenidate and/or amphetamine — the two main classes of stimulant medication. Still, the widely-cited Multi-Modal MTA Cooperative Group Study1 concluded that medication combined with behavior therapy is the optimal treatment of ADHD in school-age children. Here, we discuss the natural treatments used by many individuals with ADHD to augment medication.
1 The MTA Cooperative Group. A 14-Month Randomized Clinical Trial of Treatment Strategies for Attention-Deficit/Hyperactivity Disorder. Arch Gen Psychiatry. 1999;56(12):1073–1086. doi:10.1001/archpsyc.56.12.1073
If you want to treat adhd without medication you must be open to other options such as excerise and a healthy diet.2 of 12
Treatment for ADHD: Overview
"There's no way to predict in advance if a child or an adult will be helped by any individual ADHD treatment, even medication," says Duke University's David Rabiner, Ph.D. His advice? It is critical to monitor your ADHD symptoms (and those of your child) to know what's working — and to be open to a variety of changes in nutrition, exercise, sleep habits, and more.
Many experts recommend keeping a symptom log to track improvements, setbacks, and side effects on a daily basis. This can help to pinpoint the areas of greatest need and, when shared with a medical professional, may suggest new strategies or treatment approaches.
3 of 12
Behavioral Therapy for ADHD
Behavioral therapy for ADHD is a structured discipline strategy that aims to teach children new ways of behaving by rewarding desired behavior, such as following directions, and eliminating undesired actions, such as losing homework. The American Psychological Association says that behavior therapy should be the first line of treatment for children with ADHD under five. It can be effective for older children as well.
[Free Download: What to Eat (and Avoid) for Improved ADHD Symptoms]
New research, additionally, shows that behavioral parent training (BPT)—which teaches parents skills for effective, productive interactions with their ADHD children— reduces parental stress and instances of non-compliance. Popular BPT programs like Incredible Years and Triple-P typically span 12 to 20 sessions, each of which focuses on teaching parents new, specific techniques for addressing problem behaviors. The ultimate goal of these programs is to strengthen the parent-child relationship while teaching strategies for long-term behavior improvement.
The ultimate goal of these programs is to strengthen the parent-child relationship while teaching strategies for long-term behavior improvement.
4 of 12
Omega-3 Fatty Acids for ADHD
The omega-3 fatty acids found in fish oil are important in brain and nerve cell function. The body cannot make omega-3 fatty acids by itself, so people have to get them through food, supplements, and vitamins. There are two types of omega-3 fatty acids in fish oil, EPA and DHA. The best supplements have two or three times more EPA than DHA.
[Free Download: Fish Oil Treatments for ADHD Symptoms]
While the benefits of omega-3 fatty acids are clear, evidence of their role in treating ADHD symptoms is currently inconclusive, according to the National Center for Complementary and Integrative Health. A 2018 review1 of several studies involving children with ADHD undergoing omega-3 treatment, for example, found some evidence to support the role of the nutrient in ADHD treatment, while a similar review in 20172 found otherwise.
1 Chang, JP., Su, KP., Mondelli, V., Pariante, CM. Omega-3 Polyunsaturated Fatty Acids in Youths with Attention Deficit Hyperactivity Disorder: a Systematic Review and Meta-Analysis of Clinical Trials and Biological Studies. Neuropsychopharmacology. July 25, 2019. Doi: 10.1038/npp.2017.160
2 Catala-Lopez, F., Hutton, B., Nunez-Beltran, A., Page, MJ., et. al. The pharmacological and non-pharmacological treatment of attention deficit hyperactivity disorder in children and adolescents: A systematic review with network meta-analyses of randomised trials. PLoS ONE 12(7): e0180355. https://doi.org/10.1371/journal.pone.0180355
One approach to treating adhd without medication is cognitive behavioral therapy.
5 of 12
Cognitive Behavioral Therapy (CBT) for ADHD
CBT aims to change irrational or negative thought patterns that interfere with staying on task or getting things done — two obstacles for individuals with ADHD. For a person with ADHD who thinks, "This has to be perfect or it's no good" or "I never do anything right," CBT challenges the truth of those thoughts by getting the patient to examine the evidence.
For a person with ADHD who thinks, "This has to be perfect or it's no good" or "I never do anything right," CBT challenges the truth of those thoughts by getting the patient to examine the evidence.
Some research supports the assertion that CBT can help adults better address their ADHD-related challenges. However, some in the scientific community would like to see more rigorous research conducted with carefully constructed controls. In its 2010 report1 titled, “Current Status of Cognitive Behavioral Therapy for Adults Attention-Deficit Hyperactivity Disorder,” researchers from Massachusetts General Hospital and Harvard Medical School wrote: “The conceptual and empirical basis for CBT approaches in adult ADHD is growing and suggests that targeted, skills-based interventions have a role in effectively treating this disorder, however… randomized controlled trials with active control groups are needed and intervention packages must be tested across multiple trials by more than one research group. ”
”
1 Knouse, LE., Safren, SA., Current status of cognitive behavioral therapy for adult attention-deficit hyperactivity disorder. Psychiatric Clinics of North America. September 2010. https://doi.org/10.1016/j.psc.2010.04.001
Milk, eggs, and nuts are all high in protein — a key ingredient in a healthy ADHD diet for kids.
6 of 12
Protein for ADD and ADHD
An ADHD diet rich in proper nutrition is a powerful tool for managing ADHD symptoms. Studies by Massachusetts Institute of Technology neuroscientist Richard Wurtman,Ph.D.1, and others have shown that protein triggers neurotransmitters responsible for inducing alertness while carbohydrates trigger drowsiness. Protein also prevents surges in blood sugar that may increase hyperactivity. High-fiber foods such as fruits and vegetables, whole grains, and legumes can help stabilize energy levels. If you or your child is taking a stimulant medication, a low-fat breakfast will maximize its effectiveness. Fats can cause the body to absorb the medication more slowly, delaying the drug’s effectiveness.
Fats can cause the body to absorb the medication more slowly, delaying the drug’s effectiveness.
Depending on their age, children need between 24 to 30 grams of protein a day. Adults need 45 to 70 grams. Many nutritionists recommend starting the day with a breakfast comprising a balance of complex carbohydrates and protein such as eggs with whole wheat toast or whole grain pancakes with yogurt.
1 Wurtman, Richard J. “Nutrients That Modify Brain Function.” Scientific American, vol. 246, no. 4, 1982, pp. 50–59., doi:10.1038/scientificamerican0482-50.
Several key vitamins and minerals are key to producing and regulating neurotransmitter levels in the brain, especially when a child or adult is deficient in one of them. Vitamin C is a building block of neurotransmitters, while iron and vitamin B6 increase dopamine levels. Zinc regulates dopamine, and may help the stimulant medication methylphenidate work more effectively.7 of 12
Iron, Zinc, and Vitamins C and B6 for ADHD
Several ADHD vitamins and minerals are key to producing and regulating neurotransmitter levels in the brain, especially when a child or adult is deficient in one of them. Vitamin C is a building block of neurotransmitters, while iron and vitamin B6 increase dopamine levels. Zinc regulates dopamine, and may help treat ADHD symptoms in some children when used with conventional medication and treatments.1
Vitamin C is a building block of neurotransmitters, while iron and vitamin B6 increase dopamine levels. Zinc regulates dopamine, and may help treat ADHD symptoms in some children when used with conventional medication and treatments.1
[Free Guide: The Best Food for ADHD Symptoms]
One small study2 showed ferritin levels (a measure of iron stores) to be low in 84% of children with ADHD, compared to 18% of a control group. Low iron levels — and low zinc levels, as well — correlate with severe ADHD, however, patients should not begin using supplements without the supervision and direction of their doctor.
1 Akhondzadeh, Shahin. “Zinc Sulfate as an Adjunct to Methylphenidate for the Treatment of Attention Deficit Hyperactivity Disorder in Children: A Double Blind and Randomized Trial.” BMC Psychiatry, vol. 4, no. 9, 2004, doi:10.1186/isrctn64132371.
2 Konofal, Eric, Michel Lecendreux, Isabelle Arnulf, and Marie-Christine Mouren. “Iron Deficiency in Children With Attention-Deficit/Hyperactivity Disorder.”Archives of Pediatrics & Adolescent Medicine, vol. 158, no. 12, 2004, pp. 1113.
“Iron Deficiency in Children With Attention-Deficit/Hyperactivity Disorder.”Archives of Pediatrics & Adolescent Medicine, vol. 158, no. 12, 2004, pp. 1113.
8 of 12
Exercise for ADHD
Exercise helps the ADHD brain function more effectively and efficiently. One well-known benefit of exercise is an increase in endorphins, which can improve mood. Exercise also elevates the brain’s levels of dopamine, norepinephrine, and serotonin, which increases focus and attention.
Studies have shown1 that short-term aerobic exercise, including yoga, has positive effects on attention, hyperactivity, impulsivity, executive function, and other ADHD symptoms. Walking for 30 minutes four times a week will also do the trick, and skill-based exercises like martial arts or ballet are especially effective for those with ADHD.
1 Cerrillo-Urbina, A., García-Hermoso, A., & Sánchez-López, M. , et.al. The effects of physical exercise in children with attention deficit hyperactivity disorder: a systematic review and meta-analysis of randomized control trials: Exercise and attention deficit hyperactivity disorder. Child Care Health and Development. 2015. doi: 10.1111/cch.12255
, et.al. The effects of physical exercise in children with attention deficit hyperactivity disorder: a systematic review and meta-analysis of randomized control trials: Exercise and attention deficit hyperactivity disorder. Child Care Health and Development. 2015. doi: 10.1111/cch.12255
9 of 12
Brain-Training Programs for ADHD
Brain training for ADHD is growing in popularity and availability. Programs can be found for smartphones, computers, tablets, and beyond. Various brain training systems claim to improve common executive functioning challenges among people with ADHD, such as attention, impulsivity, and working memory. Many of the programs have layouts that look and feel like video games but are designed to exercise these specific brain functions.
Programs generally fall under neurofeedback training — which aims to change physiological activity by monitoring brain waves — and cognitive training, which focuses on improving specific brain skills like problem-solving and reading comprehension mainly through games and other exercises.
Whether brain training definitively works to improve ADHD symptoms, however, is still being researched. Some studies have demonstrated improved brain functioning in users. Critics, however, question how much users are actually benefitting. “Existing research does suggest that neurofeedback can result in improved attention, diminished hyperactivity, and enhanced executive functions, including working memory, for some patients,” said David Rabiner, Ph.D., and Ed Hamlin, Ph.D., in a 2017 ADDitude webinar. “However, some of the most important researchers in the ADHD field would argue that the efficacy of neurofeedback for ADHD has not been conclusively established. The bottom line is that research support for both stimulant medication therapy and behavior therapy is stronger than it is for neurofeedback at the moment.”
One brain training program, Play Attention, bills itself as a learning system that uses both neurofeedback and cognitive training to help users boost focus, refine memory skills, ignore distractions, and finish tasks. A series1 of2 randomized, controlled studies by Tufts University School of Medicine found that its users showed greater improvements in attention, hyperactivity, and executive functioning than students who used other programs.
A series1 of2 randomized, controlled studies by Tufts University School of Medicine found that its users showed greater improvements in attention, hyperactivity, and executive functioning than students who used other programs.
[Free Webinar: The Right Way to Train Your Brain With Games and Apps]
1Steiner, Naomi J., et al. “Computer-Based Attention Training in the Schools for Children With Attention Deficit/Hyperactivity Disorder: A Preliminary Trial.” Clinical Pediatrics, vol. 50, no. 7, 10 May 2011, pp. 615–622., doi:10.1177/0009922810397887.
2 Steiner, Naomi J., et al. “Neurofeedback and Cognitive Attention Training for Children with Attention-Deficit Hyperactivity Disorder in Schools.” Journal of Developmental & Behavioral Pediatrics, vol. 35, no. 1, Jan. 2014, pp. 18–27., doi:10.1097/dbp.0000000000000009.
Spending time every day in the sunlight may also improve your plan to treat adhd without medication.
10 of 12
Green Time for ADHD
Green time is especially effective in helping kids recover from attention fatigue, which occurs after a long school day. Gardening, biking to school, and walking the dog in the park are all good ways to incorporate green time into the day.
Neurofeedback is a high tech approach to treating adhd without medication.11 of 12
Neurofeedback for ADHD
Neurofeedback is a high-tech way, which claims to ease ADHD symptoms. During a session, the patient dons an electrode-lined cap and is asked to perform a complex cognitive task. The aim is to teach patients to produce brain-wave patterns associated with focus. Sessions are brief (30 minutes) and painless, but expensive. A course of treatment can range from $2,000 to $5,000.
Neurofeedback’s efficacy in treating ADHD symptoms is not conclusive, with multiple studies and reviews revealing opposing or weak evidence for the treatment.
12 of 12
Mindfulness Meditation for ADHD
Mindful meditation for ADHD is attention/awareness training that helps manage stress, develop positive emotions, and strengthen self-regulation skills. It involves silent meditation and becoming more aware during daily activities. In other words, you stay "in the moment" as much as possible. Researchers wrote in a 2015 review1 of multiple, similar studies that mindfulness provides “promising preliminary support for its efficacy” in treating ADHD symptoms. More research, however, is needed to definitively prove its effectiveness.
1 Mitchell, J. T., Zylowska, L., & Kollins, S. H. (2015). Mindfulness Meditation Training for Attention-Deficit/Hyperactivity Disorder in Adulthood: Current Empirical Support, Treatment Overview, and Future Directions. Cognitive and behavioral practice, 22(2), 172–191. doi:10.1016/j.cbpra.2014.10.002
doi:10.1016/j.cbpra.2014.10.002
Treatment of Attention Deficit Hyperactivity Disorder ADHD, Lakhta Junior in St. Petersburg
Attention Deficit Hyperactivity Disorder ( ADHD ) is a complex of psychological and behavioral disorders, which in recent years has been increasingly discussed by both parents and specialists.
This disorder of higher nervous activity, which usually manifests itself in childhood, has long ceased to be a rarity: according to various estimates, attention deficit hyperactivity disorder in developed countries today affects from 2% to 15% children and adolescents (in Russia, the frequency of occurrence is about 10%).
Note that any relatively new diagnosis, new medical concept, or even just a new term very quickly acquires a lot of myths and misinterpretations, which fully affected ADHD. But let's not waste time quoting all the nonsense that you can hear or read on the Internet about this syndrome lately, but let's try to briefly figure out what it is about.
ADHD is a real-life disorder, not a "medical invention". It is included in the International Classification of Diseases and is associated with dysfunction of certain structures of the central nervous system responsible for the regulation of its work. In other words, the basis for the development of this syndrome is objective organic disorders that do not depend on the nature of the child or on the style of parenting. Here, however, there is a temptation for parents to attribute their own pedagogical helplessness to a fashionable diagnosis, relieving themselves of all responsibility and requiring specialists to treat hyperactivity syndrome where it does not exist.
How ADHD manifests itself
Real ADHD, as the full name implies, is manifested by the instability of voluntary concentration of attention: the child cannot concentrate and do one thing for a time sufficient, for example, to learn a new skill or achieve some result . We emphasize: it is that “can’t”, which is fundamentally different from “does not want” (“Borings, give me your smartphone, I don’t need it, I will be a blogger / model”, etc. , etc.) - that is a completely different story, where you have to deal with the problems of motivation and values, with negativism, emancipatory reactions, ordinary laziness, oppositional behavior or something like that.
, etc.) - that is a completely different story, where you have to deal with the problems of motivation and values, with negativism, emancipatory reactions, ordinary laziness, oppositional behavior or something like that.
Most likely, this has nothing to do with true ADHD. In a child with ADHD, under the influence of the slightest interference, stimulus, stimulus (or spontaneously), attention switches from object to object, without dwelling on any of them. Punishing for this is as pointless as panicking.
Another key point in the name is the capacious word “ hyperactivity ”, which is manifested by restlessness, impulsiveness, fussiness, an uncontrollable need to do something, and the real productivity of this activity is very low or equal to zero. Actually, the same thing as with attention happens with kinetics (from the Greek. "movement"), and it is no coincidence that ADHD is classified under the heading of hyperkinesis.
To this should be added the instability of memorization, the tendency to lose or leave the necessary things somewhere, to answer inappropriately, to interrupt, to react too hastily and abruptly.
It is quite natural that such violations of self-regulation can not only irritate the environment, but also have a very negative impact on studies, in communication with peers, on relationships with parents, and ultimately on general adaptability and self-esteem.
It is very important to understand that attention deficit hyperactivity disorder is not at all equivalent to intellectual disability. In the most powerful, beautiful, fast computer, the operating system can act up, but the processor does not get worse from this. Need fine tuning.
Symptoms of ADHD — what to pay attention to
If there is something in a child’s behavior that worries you in this context, try to look closely:
— how the child moves,
— how many and what movements he makes per unit of time,
— how appropriate and effective these movements,
- are they controlled or involuntary,
- what and how is it pronounced,
- how is the information coming from outside processed and how effectively used,
- whether all this is connected with the mood of the child, his well-being or the external situation (for example, general overexcitement at a noisy birthday party).
Perhaps the only thing that bothers you is that you personally act differently, in a different pace and style, because you have a different temperament, different experience and, as they say in medicine, psychomotor. But if the so-called intuitive diagnosis (and this phenomenon really works among close people) tells you unambiguously that the child’s behavior is abnormal and it does not depend on him, or on you, or on the situation, then it’s time to think about showing child to a specialist (psychiatrist, psychologist, psychotherapist, psychoneurologist, just a neurologist - for the first visit it is not so important), so that this visit looks as natural as possible and is minimally traumatic.
Of course, at that moment you should already know well who exactly you are addressing and why to this specialist, and not to that one. But it is a must to apply.
Treatment of ADHD in children
Given that the etiopathogenesis of ADHD (i.e., the causes and mechanisms of development of this syndrome) is still not well understood, it would be irresponsible of us to recommend any specific ways to correct this condition. But anyway the approach would be:
But anyway the approach would be:
First , complex - please do not expect a miracle pill that will immediately solve all problems with heredity, the balance of neurotransmitters, the functioning of the reticular formation of the brain, education, psychological microclimate, nutrition, daily routine, etc .; A lot will have to change, and not just the child.
Secondly , the strategy will be strictly individual, since ADHD, with all its prevalence and recognition, is never repeated exactly.
Thirdly, , do not count on the rapid and complete disappearance of all problems: in many cases, hyperactivity syndrome, softening to the degree of almost complete adaptation and normal quality of life, in such a reduced form still accompanies a person for many more decades.
Fourthly and most importantly, do not waste time on brilliant ideas like “she will outgrow”, “you need to be collected and attentive”, “would he join the army” or “we’ll give her in marriage, she will be like everyone else”; and do not poison with dietary supplements, tinctures, decoctions, advice, requirements, ultimatums and notations. It is clear that all this is with the best of intentions, but it does not work. ADHD is indeed a problem, but a medical problem. Therefore, contact a specialist at the Lakhta Junior Children's Clinic in St. Petersburg.
It is clear that all this is with the best of intentions, but it does not work. ADHD is indeed a problem, but a medical problem. Therefore, contact a specialist at the Lakhta Junior Children's Clinic in St. Petersburg.
| Attention Deficit Hyperactivity Disorder: Treatment for ADHD in Children
Attention deficit hyperactivity disorder in a child (ADHD) is a behavioral and emotional-volitional disorder, as a result of which the child experiences difficulties in concentrating attention, perseverance, keeping one or more instructions, often "misses everything by the ears", is unsuccessful in mastering the school curriculum . Such children cannot sit in one place for a long time, they are impatient, impulsive, sometimes capricious, their actions are often chaotic and aimless.
Often, parents and caregivers confuse these symptoms of a neurological disease with the characterological features of the child's personality. Therefore, children for a long time remain without due attention of specialists, which is fraught with the development of various adverse manifestations.
Children with Attention Deficit Hyperactivity Disorder (ADHD) often do not study well and are prone to antisocial changes in the future (prone to alcohol and drug addiction). In such children, the risk of headaches, neuroses, tics increases. Often develop diseases of the cardiovascular and digestive systems, sleep disorders and other adverse factors.
The main danger of this disorder lies in the fact that the external manifestations and symptoms are that the child gives the impression of being very active and energetic, overflowing with energy. Parents decide that the baby does not have enough places where he can throw out all his energy, and I begin to take the child to all possible sports clubs and sections. Thus, the child psychologically and emotionally begins to deplete. Remember, only swimming is shown to a hyperactive child from sports sections !!! External activity is deceptive, so the child is only self-stimulating, trying to concentrate and keep the instruction.
Highly qualified specialists of the neurological and speech therapy center "Above the Rainbow" successfully treat ADHD in Moscow.
Causes of ADHD in children
The exact cause of ADHD has not been determined by medical science. Scientists believe that this condition appears when exposed to a complex of factors. These include:
1. Negative influences during fetal development (pollution of the environment, food, intoxication of the body, infections, Rhesus conflict, the threat of miscarriage, pathological childbirth, etc.).
2. Factors that negatively affect the baby's brain at a very early age (hypoxia, anesthesia, antibiotics).
3. Burdened heredity.
The above causes can cause organic damage to the child's brain, which is expressed by characteristic behavior.
Types
There are 3 types of attention deficit hyperactivity disorder:
- With a predominance of hyperactivity. More common in boys. They cannot stay in one place, have a "field" behavior, are impatient and restless.

- With a predominance of attention deficit. More commonly seen in girls. It is difficult for them to concentrate on one type of activity, attention is sprayed on external stimuli.
- Mixed appearance, when hyperactivity and attention deficit are equally expressed.
ADHD treatment in Moscow at the "Above the Rainbow" center corrects any kind of behavioral disorders.
Early signs of ADHD
How can the disease be detected and treated in a timely manner for attention deficit hyperactivity disorder in a child? In children of the first years of life, certain symptoms of pathology are noted, the appearance of which should alert parents:
- Rapid physical development (before term they begin to hold their heads, do not crawl, but immediately tend to get up and walk, etc.).
- They fall asleep hard and for a long time, sleep less than the prescribed norm per day.
- When tired, they do not calm down, but fall into hysterics and whims.

- "Field" behavior - the inability to concentrate on one thing for more than 1-2 minutes; throw toys before they can be seen.
Before the age of 3 years, it is still difficult to determine whether the above manifestations are signs of pathology. By the age of 5-12, the symptoms become clearly visible. Therefore, the treatment of attention deficit hyperactivity disorder in a child must be carried out without fail.
The main symptoms of ADHD
The main signs of pathology include:
- Attention disorder. The child fails to concentrate on any type of activity, he avoids performing routine activities.
- Hyperactivity. The child performs many aimless movements, talks non-stop, has very expressive facial expressions.
- Impulsivity. He does not know how to follow the sequence of actions, plan, wait, is guided only by his own desires. These children have emotional lability, that is, a rapid transition from laughter to crying and vice versa.
 They do not feel danger, which is why they often perform actions that lead to traumatic injuries.
They do not feel danger, which is why they often perform actions that lead to traumatic injuries.
The IQ of a child with ADHD is usually age-appropriate or even superior. However, he has difficulty interacting with peers, being too intrusive or aggressive. Emotional development suffers. The child is characterized by such qualities as imbalance, capriciousness, excessive emotionality. Adults often compare him with other, more obedient children. In this regard, low self-esteem develops, the child withdraws from society or protests, becomes aggressive.
The nervous system of a child with ADHD is not able to adequately perceive external stimuli, and this behavior is an attempt to protect itself from external environmental factors. The baby's nervous system is often depleted, neurodynamics are very low. The kid gets tired quickly, especially from intellectual activities that require planning and long-term concentration. The child subconsciously seeks to run away from such activities, from the outside it seems that the baby takes on everything and quickly quits without completing it to the end.
Treatment of ADHD at the neurospeech and speech therapy center "Above the Rainbow"
Neuropsychologists of our center have extensive experience in non-drug treatment of ADHD in children from 3 to 18 years old. With a properly built correctional program, your child will be able to develop according to age, discover new talents, grow up as a self-sufficient and harmonious personality.
Specialists create an individual program of neuropsychological correction and behavioral therapy for each child individually. The psychologist also works with parents, helping to develop the right line of education.
Revolutionary methods of developing special abilities of the brain, along with innovative equipment, guarantee a positive result in the treatment of ADHD in children. Our center employs the best specialists who have passed a rigorous selection and training in the USA, Germany and France. The program of neuropsychological correction integrates sensory integration, kinesiological exercises, classes in the speleotherapy cave, sensory room, neurodynamic park, neuromaze, neurodrome, neuronetwork.