Divalproex withdrawal symptoms
Depakote Withdrawal Help | Valproic Acid Side Effects, Treatment
Alternative to Meds News & Blog Articles
What is Depakote?
We have provided information below for anyone looking for information about Depakote withdrawal symptoms, divalproex sodium side effects, and holistic treatment help for Depakote withdrawal. Depakote comes in 5 different oral forms, given here in descending order of absorption rates:
VPA syrup: (valproic acid) sold as “Depakene”
VPA capsule: (valproic acid)
Divalproex sodium sprinkles Depakote sprinkles come in a capsule that can be opened and added to soft food
Divalproex sodium enteric-coated – delayed-release tablet
Divalproex sodium ER – extended-release tablet
You will find more information below regarding drug classification, information about its mechanism of action, long-term effects, and other treatment information including holistic treatment for Depakote withdrawal. Depakote is an FDA-approved anti-seizure (antiepileptic) medication.2
Black box warnings: include fatal liver disease, major birth defects such as spina bifida and neural tube malformations, and rapidly emerging life-threatening pancreatitis in all age groups. Though not included in the black box, a nearly doubled risk compared to placebo for suicidal thinking and behavior has been demonstrated in clinical trials in ALL populations.2,16
What is Depakote Used For?
Depakote is used in the treatment of seizure disorders, such as epilepsy, often in combination with other medications.
The FDA approved Depakote for the treatment of bipolar disorder after an unspecified number of 3-week long trials.2 Bipolar disorder has a high propensity for misdiagnosis.3,4 Manic episodes might be considered a bipolar symptom and are described as distinct periods of abnormally sustained elevated mood and other characteristics including irritability and hostility. Other mania symptoms include machine gun-type speech, reduced need to sleep, grandiosity, absence of good judgment, motor hyperactivity, and what can appear to be an expansive flood of fanciful ideas. Depakote was not safety-tested for longer 3-weeks for mania and cautions closely monitoring and reevaluating the usefulness of Depakote for a patient in this situation.2
Other mania symptoms include machine gun-type speech, reduced need to sleep, grandiosity, absence of good judgment, motor hyperactivity, and what can appear to be an expansive flood of fanciful ideas. Depakote was not safety-tested for longer 3-weeks for mania and cautions closely monitoring and reevaluating the usefulness of Depakote for a patient in this situation.2
Depakote is also approved for the prevention of migraine headaches in adults and children. Please see notes in the holistic treatment section of this article for documented efficacious holistic headache treatments that do not include antipsychotic or antiseizure medications.
Please note: Depakote is not recommended for pregnant women or women of child-bearing age for any reason due to the risks to what is now termed “fetal valproate syndrome.” Children born to mothers taking valproate during pregnancy may suffer withdrawals at birth, and there is a high risk for the baby to be born with birth defects or other medical problems.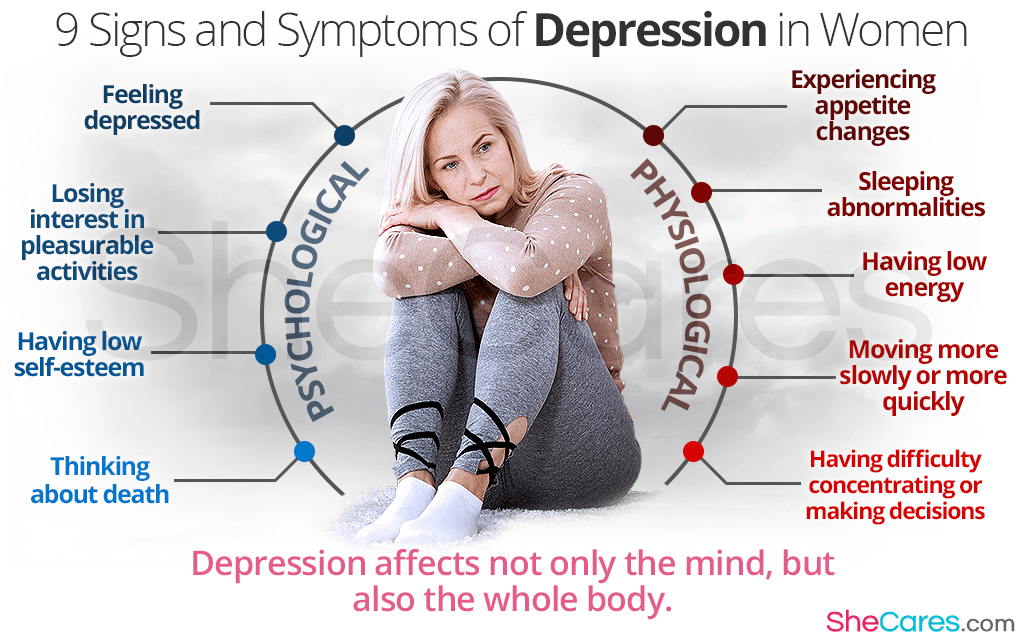 These adverse events were documented in clinical trials authored by Thisted and Ebbeson, and as reported by the National Organization of Rare Diseases.2,5,19,20
These adverse events were documented in clinical trials authored by Thisted and Ebbeson, and as reported by the National Organization of Rare Diseases.2,5,19,20
Depakote is sometimes used as an adjunctive or add-on medication in the management of schizophrenia, psychosis, or other psychiatric disorders. particular caution is advised when other medications are prescribed as they may slow or speed up the rate at which Depakote is metabolized.
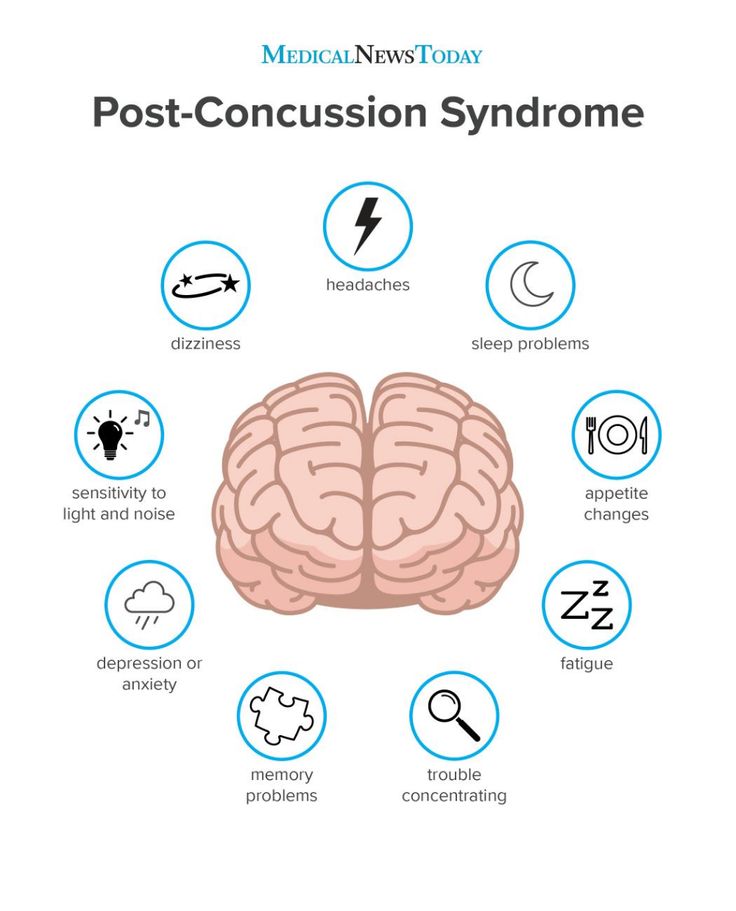
Off-label uses include the treatment of alcohol or other drug dependencies, diabetic neuropathy, and to quell impulsivity and aggressive behavior such as after traumatic brain injury, based on rat studies showing decreased permeability of the blood-brain barrier in rats who were given impacts to the brain with an electromagnetic cortical-impact device followed by valproate, and another study linking valproate with a decrease in neuronal damage after inducing continuous and repeated electrically-induced seizures in rats. 16,17,18 Where a drug does not have an accessible and robust body of documentation concerning human long-term clinical trials to rely on, one would be well-advised to do one’s own research on such medication as carefully and as thoroughly as possible to make informed decisions about starting or stopping such drugs. Additional important information on these topics follows.
16,17,18 Where a drug does not have an accessible and robust body of documentation concerning human long-term clinical trials to rely on, one would be well-advised to do one’s own research on such medication as carefully and as thoroughly as possible to make informed decisions about starting or stopping such drugs. Additional important information on these topics follows.
Notes on Depakote and Bipolar
It is vital to note that Depakote (valproate) was approved for treating bipolar disorder after only very short trials were done on hospitalized acute mania patients. No long-term trials were ever completed that demonstrated the long-term safety or effectiveness of Depakote. Nonetheless, Depakote has been prescribed to millions of people since its approval in 1983. There is a much larger body of evidence that has accumulated post-marketing of the drug that includes adverse side effects, symptoms of withdrawal, and other information below.
Always seek reliable medical advice before starting or stopping a prescription drug such as Depakote, and before adding other medications that may interact and cause unexpected reactions.
Discontinuing/Quitting Depakote
It may become necessary or desirable to stop Depakote. How to quit Depakote and Depakote alternatives are what we specialize in at Alternative to Meds Center. We have protocols for tapering Depakote and bridging over to natural alternatives to Depakote that can make the withdrawal from Depakote gentle and sustainable. Except in certain circumstances where immediate cessation is required to save the patient’s life, such as liver failure, life-threatening pancreatitis, or other conditions, Depakote should be gently tapered off with proper monitoring, support, and guidance.
The FDA label indicates that where hepatic dysfunction, pancreatitis, toxic levels of ammonia or other life-threatening conditions emerge, Depakote should be immediately stopped.2
If tapering is done correctly it can be a mild procedure. Done too fast, it can be extremely difficult and can introduce undesirable risks to health.
Depakote Alternative Names and Slang
Other trade names for the generic valproate, sodium valproate, or Divalproex delayed-release, include Depakene, Depakote ER (extended-release), Depakote Sprinkles, Stavzor, and Alti-Valproic.
The drug is available in a soft-gel capsule, tablet, or syrup form. Depakote Sprinkles are designed so that if a person cannot swallow a capsule or tablet, the drug can be sprinkled on applesauce or other types of soft food. One capsule of Sprinkles is meant to be used all at once.
Depakote Side Effects
Depakote is often administered as an adjunctive medication, for instance with antipsychotics, SSRIs, SNRIs, or other mood-stabilizing drugs. It may be difficult to ascertain in such circumstances exactly what drug is causing what side effect; therefore each patient should be monitored carefully in this regard for reactions needing medical attention.
The FDA2 has published some known adverse side effects that require careful monitoring while on Depakote, including:
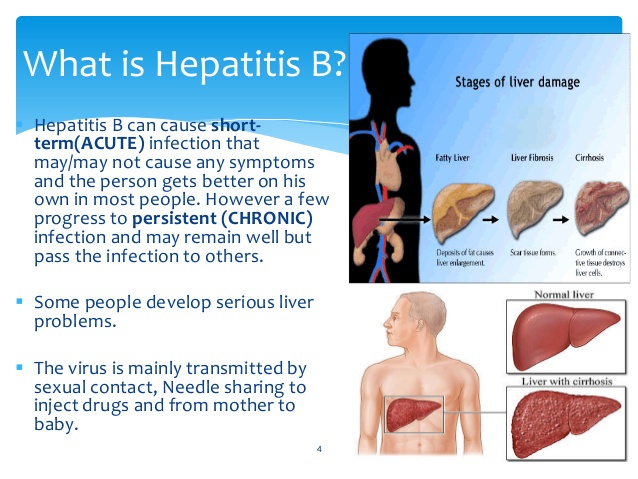
- Hepatotoxicity: liver failure, leading to fatality, which may follow symptoms such as weakness, lethargy, vomiting, anorexia, and facial edema.
 Especially if a person has a prior history of liver disease, regular physical examinations, as well as serum liver tests, should be done to monitor the person closely for signs of liver toxicity.
Especially if a person has a prior history of liver disease, regular physical examinations, as well as serum liver tests, should be done to monitor the person closely for signs of liver toxicity. - Birth defects are linked to taking Depakote during pregnancy, where the infant may develop deformities of the limbs, heart, craniofacial, and neural tube defects leading to spina bifida, and others. Birth defects occur 4 times higher where mothers took Depakote compared to other epileptic medications.
- Lowered cognitive scores after in utero exposure to Depakote: have been studied and shown as significantly lower in children born to epileptic mothers taking Depakote compared to children born to mothers taking some other AED or no AED. Since it has not been established if there is a specific period of risk during pregnancy for such birth defects including lowered IQ, the consensus is that women of child-bearing age should not be prescribed Depakote.
 However, should pregnancy occur while on a prescription of Depakote, the drug should not be withdrawn abruptly due to risk of seizure and other reactions, and possible fatality to the fetus.
However, should pregnancy occur while on a prescription of Depakote, the drug should not be withdrawn abruptly due to risk of seizure and other reactions, and possible fatality to the fetus. - Fatal pancreatitis: in both adult and children are linked to Depakote. Where this condition presents, it can progress rapidly and is considered life-threatening, requiring immediate hospitalization. Some warning signs of pancreatitis can include nausea, vomiting, pain in the abdomen, anorexia, and the patient should be immediately evaluated for hemorrhages and other symptoms of pancreatitis.
- Suicidality: a two-fold increase in suicidal ideation and behavior in both adults and children. Four suicides occurred within a twelve-week trial.
- Abnormal bleeding
- Hypothermia
- Other: side effects include rash, somnolence in the elderly, dizziness, indigestion.
Depakote Tapering Help | Valproic Acid Weaning, Titration Support
Alternative to Meds News & Blog Articles
Alternative to Meds Does Not Provide Rapid Detox
There are, rarely, instances when rapid or abrupt discontinuation of a drug like Depakote is medically necessary to save the life of the patient. For example, anticonvulsant-induced movement disorders, and other potentially life-threatening reactions such as Stevens-Johnson syndrome are rare but are known adverse events associated with Depakote. These must be treated in a hospital setting such as an emergency ward or ICU where abrupt discontinuation is most safely achieved.4,28 Alternative to Meds cannot provide the emergency medical treatment that is needed for rapid withdrawal in such cases, and we are not in a position to give guidance regarding rapid Depakote withdrawal.
For example, anticonvulsant-induced movement disorders, and other potentially life-threatening reactions such as Stevens-Johnson syndrome are rare but are known adverse events associated with Depakote. These must be treated in a hospital setting such as an emergency ward or ICU where abrupt discontinuation is most safely achieved.4,28 Alternative to Meds cannot provide the emergency medical treatment that is needed for rapid withdrawal in such cases, and we are not in a position to give guidance regarding rapid Depakote withdrawal.
Begin Depakote tapering only when you are in a stable condition.
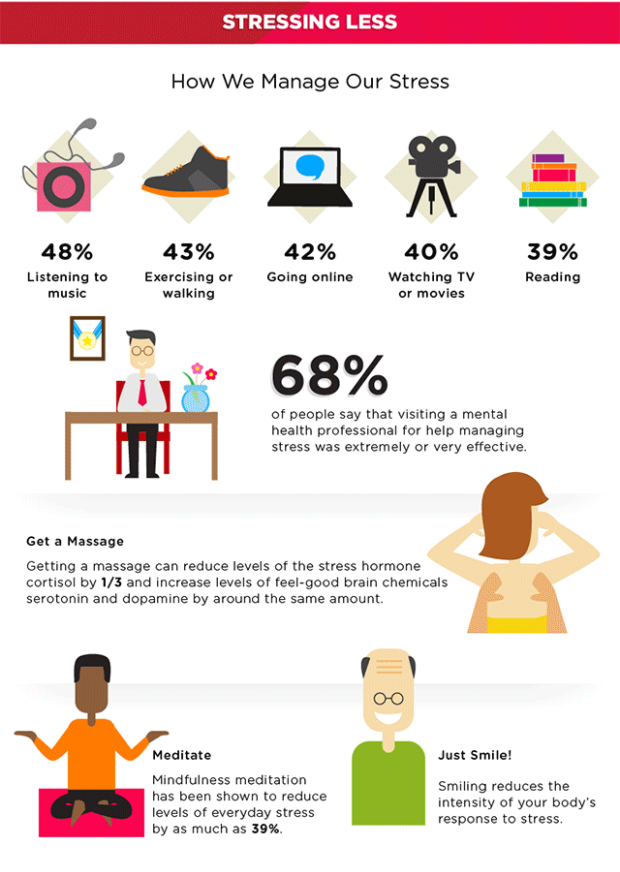
It is best to begin a Depakote taper when the person is reasonably tolerating the medication, sleeping well, eating regularly, doing regular exercise, is under competent medical oversight from a willing prescriber. The best candidate would have eliminated caffeine and other stimulants, alcohol use, marijuana, or other recreational drug use because these substances can interact with and interfere with the medication’s mechanisms of action.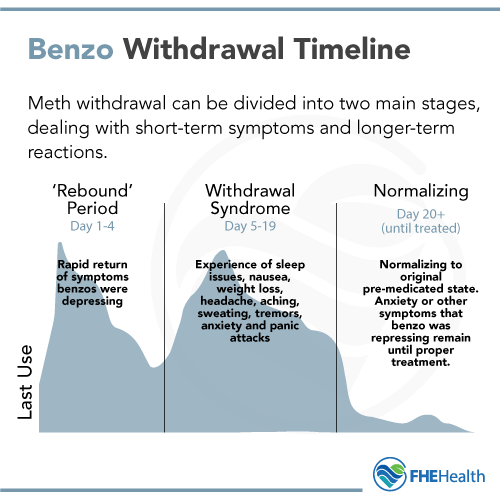 This can throw a wrench into any taper program. having a support circle is extremely beneficial for support from family, close friends, and sympathetic mentors. Also arranging one’s life in an organized fashion might include engaging in hobbies or light work to focus on. If you are not sleeping well, that should be taken care of with the help of your prescriber or using holistic means that work well for you beforehand.
This can throw a wrench into any taper program. having a support circle is extremely beneficial for support from family, close friends, and sympathetic mentors. Also arranging one’s life in an organized fashion might include engaging in hobbies or light work to focus on. If you are not sleeping well, that should be taken care of with the help of your prescriber or using holistic means that work well for you beforehand.
Contracting for safety — what it means.
A person in a manic state may become unwilling or unable to follow directions. However, following directions is vital for a successful taper. It is recommended to discuss and voluntarily draw up a written contract that can be presented when needed. Putting this solid commitment in writing to agree to follow the doctor’s tapering directions can get things back on track. For example, if the person has stopped their meds and has become manic or psychotic, they may become unwilling to continue the taper as agreed. This is a safety risk for the person that the contract for safety was put in place to remedy.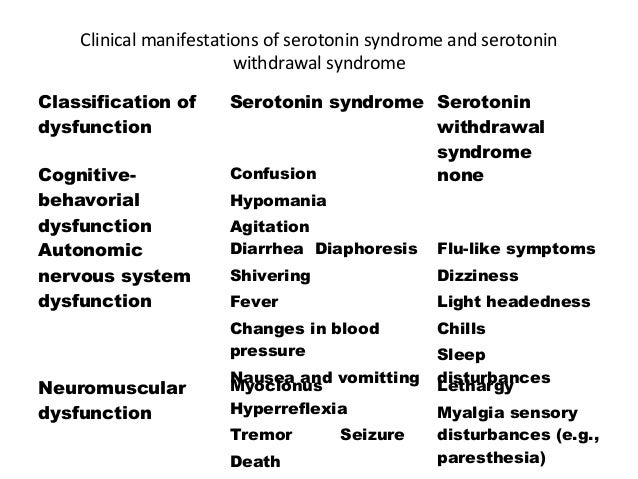 Part of the agreement would be to acknowledge that non-compliance will result in police involvement, or having to go to the hospital. For the person’s own safety and those around them, the contract for safety is a vital safety net for anyone tapering from ACDs and other unpredictable neuroleptic drugs.20
Part of the agreement would be to acknowledge that non-compliance will result in police involvement, or having to go to the hospital. For the person’s own safety and those around them, the contract for safety is a vital safety net for anyone tapering from ACDs and other unpredictable neuroleptic drugs.20
Set up medical support before your Depakote taper.
There are holistic psychiatrists and other prescribers who can assist you with an outpatient-style taper. Certainly, we recommend inpatient care when possible, but we know it may not always be possible or practical for everyone. When you find your outpatient doctor, you are welcome to share our information with them if you like, and we hope it helps open the discussion.
Eliminate all forms of caffeine or other stimulants, and recreational drugs.
This is so important it probably should be #1 on the list of guidelines. Use of stimulants, even too much coffee, tea, or soft drinks, alcohol or recreational drug use, can all potentially land you in the hospital. This is because of the mechanics of how stimulants and alcohol impact Depakote, resulting in a flood of excitatory neurochemicals. Restrict these items and stay safe.15,18,19
This is because of the mechanics of how stimulants and alcohol impact Depakote, resulting in a flood of excitatory neurochemicals. Restrict these items and stay safe.15,18,19
Food choices to control blood sugar spikes.
Blood sugar spikes and crashes can disrupt tapering with a vengeance. Choose low-glycemic, protein-based foods and snacks to prevent unnecessary problems. Don’t let hunger disrupt your progress. Breakfast should be protein-based giving a good start to the day. Follow up with smaller protein-based meals that also incorporate your favorite vegetables throughout the day. Experiment with some rutabaga or cauliflower for “mashed potatoes” — delicious with butter! Avoid refined flours and sugars or find low-carb replacements. Snacks like non-starchy veggies, peanut butter, avocado, raspberries, blueberries, dill pickles, cheeses, delicious cold cuts, and other sugar-free foods can deliciously fill in the gaps as needed.13
Many Benefits of Exercise.
Exercise has been documented well for the benefits to physical and mental health. For example, Sharma et al’s comprehensive summary24 of benefits lists improved mood, energy, and better sleep that should be emphasized and encouraged by mental health professionals. In addition to these benefits, Albrecht Messerschmidt’s 2010 book, Comprehensive Natural Products II, discusses the role of oxygen in certain chemical reactions, such as modulating dopamine molecules.25
This would be a very good reason to blend some aerobic, cardio exercise into the daily routine where a person with excess dopamine may benefit from this regulatory function. According to Science Daily, regulating the “happy hormone” dopamine is important. Too little dopamine is linked to Parkinson’s disease, and too much dopamine is linked to mania, hallucination, or other psychiatric symptoms. Exercise is an extremely good tool that can help regulate this important hormone.26
Use the smallest milligram dose of Depakote available to use for the taper.
The smallest milligram dose of Depakote is the dark pink oval 125mg tablet. This does not mean you want to drop to the lowest dose. Smaller pills will help configure the medication total accurately. For example, if you are on 1500mg Depakote, you will want to have the 125mg version available so that if you were to drop down to 1375mg, you could take two of the 500mg (for 1000mg), cut one of the 500mg in half (for 250mg), and then add one of the 125mg to equal a total of 1375mg. It also might be that you get the 250mg and the 125mg versions prescribed to make the math easier. You can cut the Depakote 125mg in half giving you 62.5mg. These small cuts are not necessary for everyone, but for some, slowing it way down is the only path to re-regulation after the use of the drug. You can cut any of the Depakote versions in half to configure the correct milligram dosing needed. However, if you are on Depakote ER when you cut the pill, it will lose the extended-release attribute.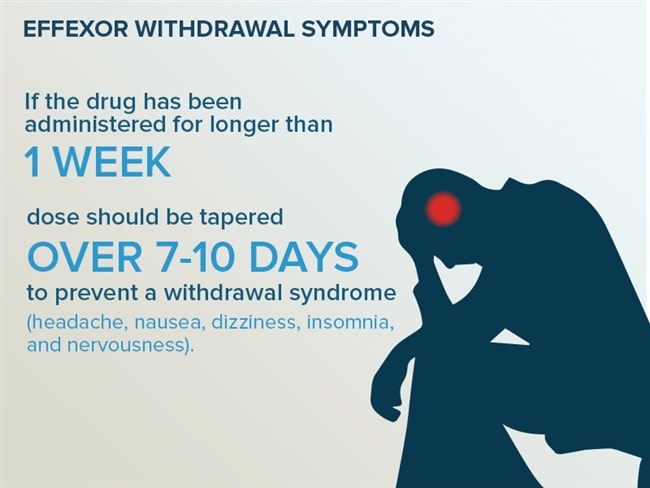 They do make a 250mg Depakote ER version. So if you are on the ER version, many people can configure the tapering dosing amount in 250mg increments. If you are planning to make smaller than 250mg cuts, the regular non-time-released version would be likely easier for that purpose. So let’s say a person is trying to get to 875mg. They might take three 250mg Depakote ER, and 125mg Depakote (non-time-release), for a total of 875mg. These configurations can be worked out with your prescribing physician for accuracy of dosage. Keep a written record — don’t rely on “mental math” in the middle of a Depakote taper.
They do make a 250mg Depakote ER version. So if you are on the ER version, many people can configure the tapering dosing amount in 250mg increments. If you are planning to make smaller than 250mg cuts, the regular non-time-released version would be likely easier for that purpose. So let’s say a person is trying to get to 875mg. They might take three 250mg Depakote ER, and 125mg Depakote (non-time-release), for a total of 875mg. These configurations can be worked out with your prescribing physician for accuracy of dosage. Keep a written record — don’t rely on “mental math” in the middle of a Depakote taper.
Other medications you are on.
The CDC reported that between 2015 and 2018 about 24% of the US population took 3 or more medications over a 30-day period, and over 12% took 5 or more medications in the same period. It is not at all unlikely that a person who has been taking Depakote for some time may have also been prescribed other medications for various reasons. Tapering within an inpatient setting would be particularly advised in this case.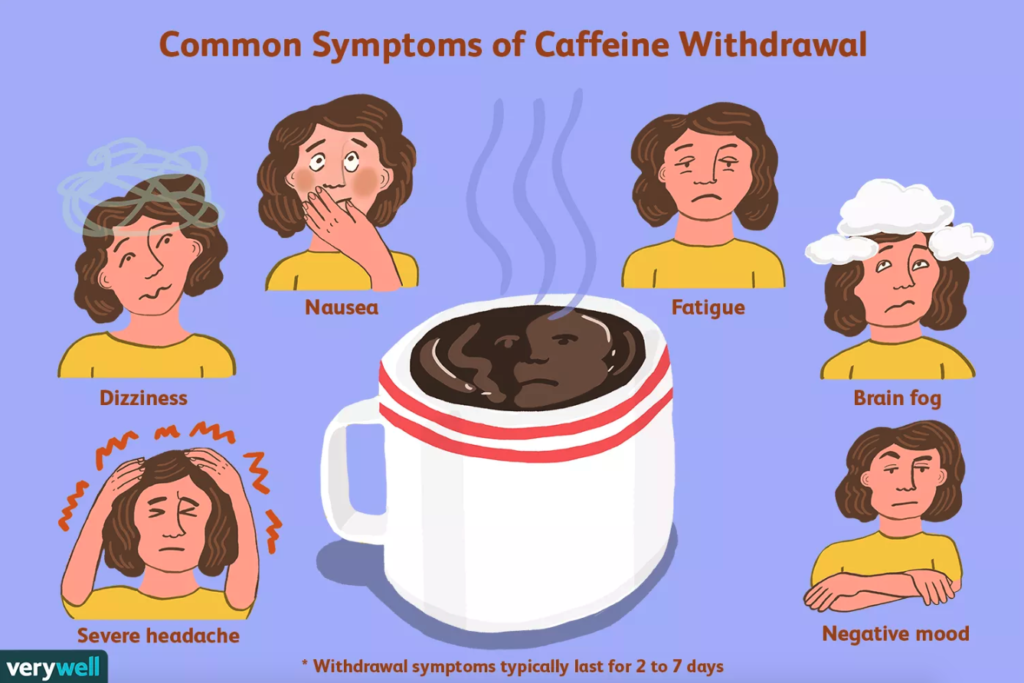 The order or sequence of which medications to taper is vital so as not to overwhelm the body by introducing too much change all at once. These matters can be assessed and managed more easily in an inpatient setting, as both the micro-changes and the broader modifications can be made when needed on an immediate basis.21 In any case it would be advised to speak with your prescribing doctor who is helping with your taper and discuss the best sequence, depending on what medications were prescribed and for what reasons they were originally prescribed.
The order or sequence of which medications to taper is vital so as not to overwhelm the body by introducing too much change all at once. These matters can be assessed and managed more easily in an inpatient setting, as both the micro-changes and the broader modifications can be made when needed on an immediate basis.21 In any case it would be advised to speak with your prescribing doctor who is helping with your taper and discuss the best sequence, depending on what medications were prescribed and for what reasons they were originally prescribed.
Factors that would have to be considered include how long a person was taking each drug, the symptoms the person was attempting to control, current symptoms, and other issues that are unique to each individual.
How long will Depakote tapering last?
Because each person has unique biomarkers, genetic profile, medical history, sensitivities, individualized sets of symptoms, and so on, there is no “one-size-fits-all” when it comes to Depakote tapering.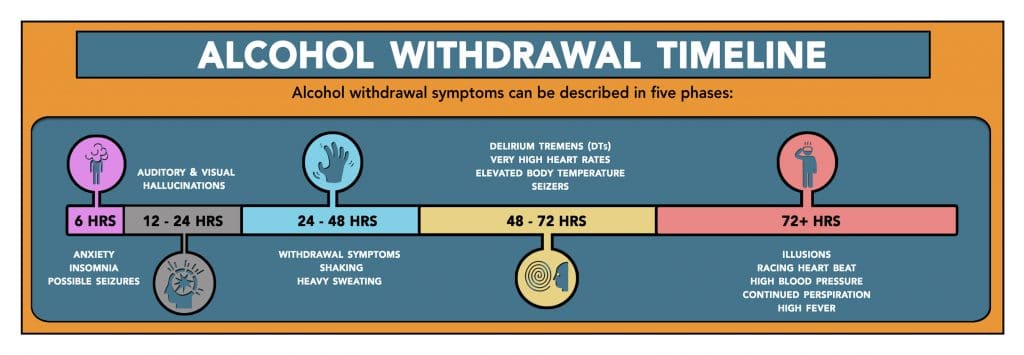 Like maneuvering down a mountain road, sometimes shifting to a lower gear is more effective than slamming on the brakes too aggressively. Slow and safe are the keywords to keep in mind.
Like maneuvering down a mountain road, sometimes shifting to a lower gear is more effective than slamming on the brakes too aggressively. Slow and safe are the keywords to keep in mind.
Some medications may take months, or even years to resolve as demonstrated in benzodiazepine clinical studies,22 as well as studies on discontinuation of mood stabilizers.23
However, we have observed that when effective tapering support is provided, these numbers typically decrease as the body is maximally assisted in the rehabilitation of its normal neurochemistry.
Red Flags of Depakote Tapering
Returning to our analogy of driving a logging truck down a mountain with switchbacks on an icy road, you have to go light on the accelerator — go slow — and be ready to use your brakes. If you are a patient, skillful driver, you will get safely down the mountain. Free-wheeling it will likely end in a crash — an avoidable disaster. Accelerating around the turns because it feels good can turn out like the wreck that you would anticipate in our driving scenario. We observe similar laws of gravity and inertia involved in Depakote tapering. Go slow so you can get down the mountain. That is the over-arching axiom.
We observe similar laws of gravity and inertia involved in Depakote tapering. Go slow so you can get down the mountain. That is the over-arching axiom.
Not eating, not sleeping, intense side effects, and perseverating (obsessing) over a certain topic that will not leave your mind are all red flags. These are signs you are heading into the danger zone. For instance, after the second day of not sleeping, that could be a signal to pay attention to. It may be that you need to go back up on your medications. Then you can work your way back to the earlier dose. Please talk to your prescriber about the likelihood of encountering these moments of crisis before you begin Depakote tapering so you have a better understanding of what to expect. Don’t try to figure it out mid-crisis. You don’t want to end up in the hospital back at square one. If you begin to feel you pose a danger to yourself or those around you, just play it safe and get checked in the hospital. Hospitalization is not a failure.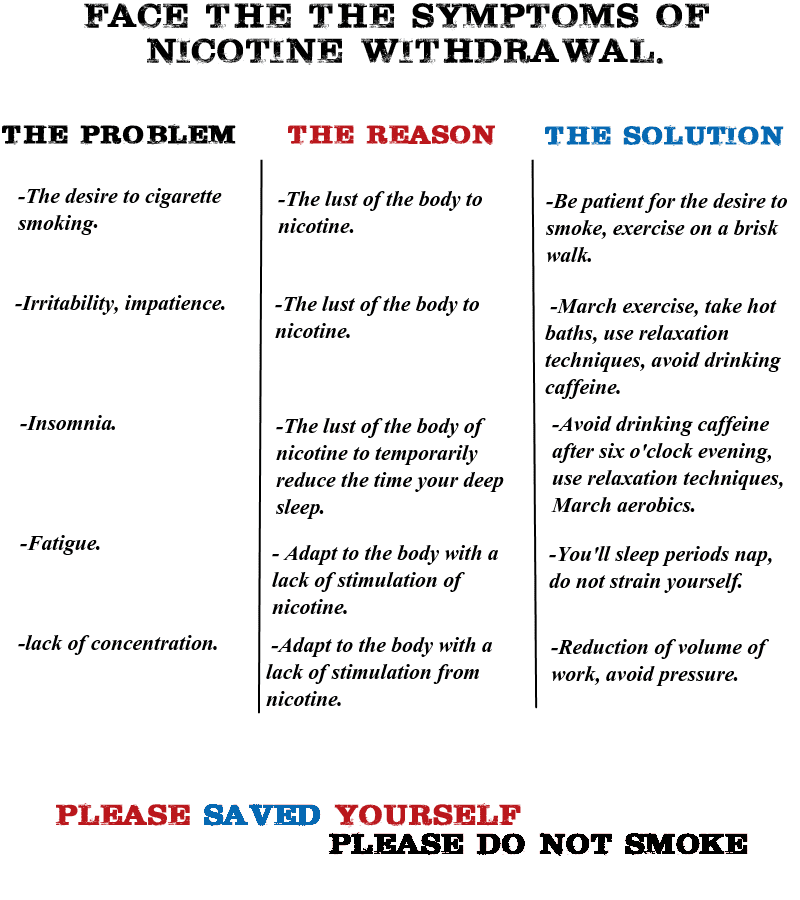 It could be that being medication-free is not the best outcome. Or it could signal that a much longer withdrawal period is needed. Watch for red flags and respond to them by collaborating with your prescriber without delay.
It could be that being medication-free is not the best outcome. Or it could signal that a much longer withdrawal period is needed. Watch for red flags and respond to them by collaborating with your prescriber without delay.
Bridge medications for Depakote tapering.
Some persons may do well using what are referred to as bridge medications to ease Depakote withdrawal. At Alternative to Meds Center, various methods of tapering can safely ease withdrawal issues and bridge medications can be designed on an individual basis.
Limiting stimulating media during Depakote Tapering.
Wrestling with life questions, religious matters, and watching over-stimulating movies or TV, can all be overwhelming for someone attempting Depakote tapering. Better activities might include outside walking, physical activity, hobbies you enjoy, light reading, light work, or things that can pleasantly extrovert the attention. These types of activities can act as grounding elements that support your tapering process very well.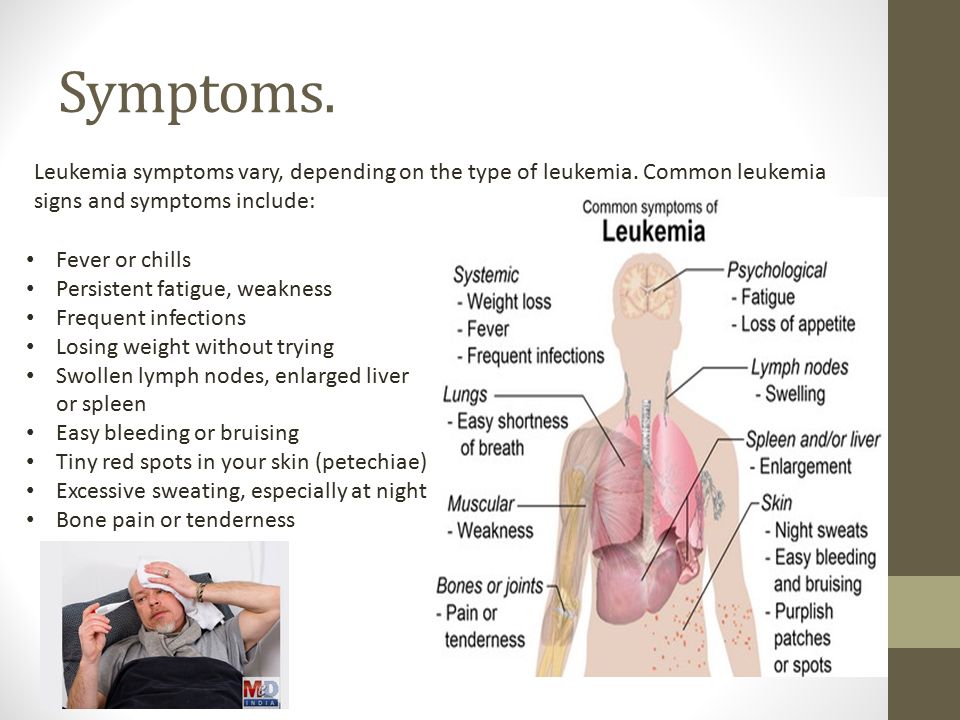
Depakote Alternatives and Depakote Withdrawal Links
We have pages on our site that address Depakote alternatives that can be used during the tapering process. We strongly recommend you review these pages. Quick links are Antipsychotic Alternatives for general information on nutrition, etc., and Depakote Alternatives. You may also want to consider reading the Depakote Withdrawal page.
Depakote Side Effects
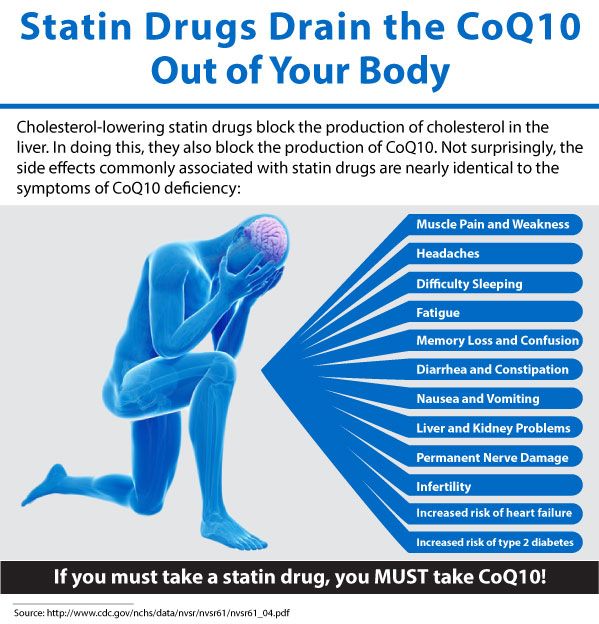
The FDA drug label3 lists the following:
- Life-threatening pancreatitis (all ages)
- Coma, severe or fatal encephalopathy (loss of brain function)3,8
- Dementia
- Liver failure (fatal hepatotoxicity)
- Seizures, tremors
- Suicidal thoughts and behavior as early as the 1st week of taking Depakote
- Decreased blood platelet levels
- Drowsiness, sedation, confusion, dizziness
- Stevens-Johnson syndrome, toxic skin necrolysis, temporary hair loss, rashes
- Nausea
- Constipation, diarrhea, abdominal cramps
- Headaches
- Sexual loss of interest
- Anxiety, nervousness
- Depression
- Mood swings, uncontrolled laughing or crying, often at inappropriate times
- Anorexia, weight gain, weight loss
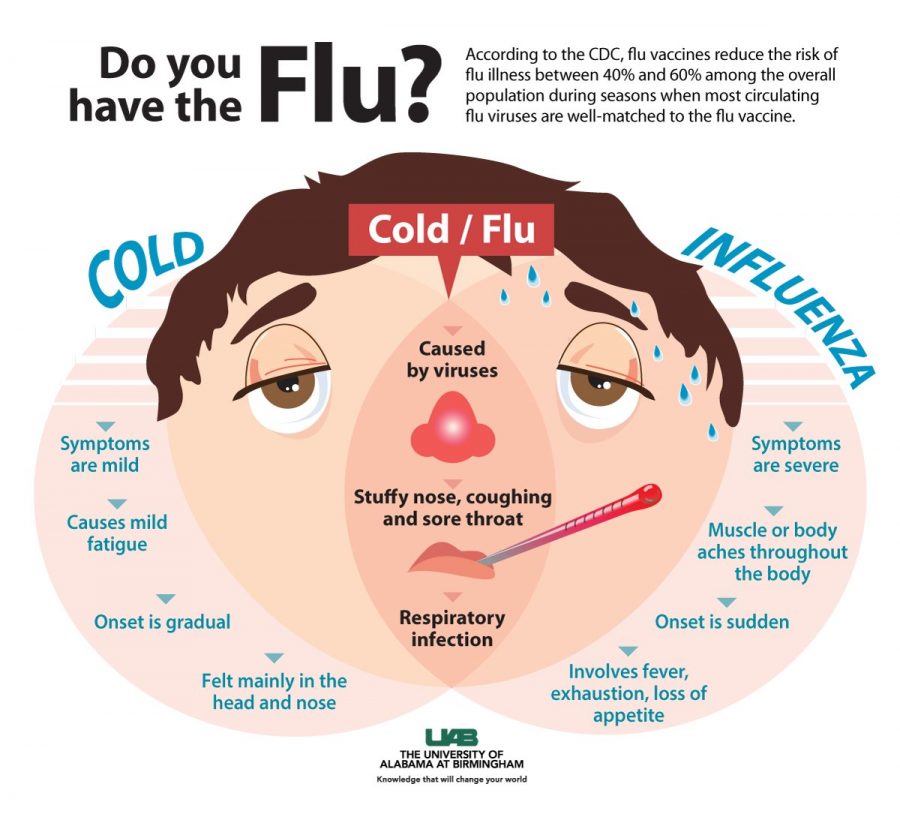
- Bronchitis, fever, flu syndrome
- Bleeding under the skin resulting in purple patches
- Amnesia
- Blurred vision, double vision
- Abnormal thinking
- Insomnia
- Abnormal muscle weakness
- Accidental injury
Notes on Rebound Symptoms after Stopping Depakote Too Quickly.
For a person with epilepsy to abruptly stop or even reduce Depakote, one of the most concerning reactions is episodes of seizures that do not stop, also called status epilepticus.6 For bipolar persons, a sudden cessation of Depakote can bring on a return of the person’s original symptoms such as mania, insomnia, etc. A person who was taking Depakote as a treatment for migraines may have a return of migraines, which may be considerably more severe than before taking valproate. A person taking Depakote as a mood stabilizer, for bipolar, for headaches, or for other conditions may find that reducing the drug too quickly can cause intense reactions. Sometimes these withdrawal adverse effects can linger on if they are not addressed in a healthy way as part of the tapering process.7
Depakote Withdrawal Symptoms
Depakote withdrawals can include both rebound (returning) symptoms and new symptoms, including the following:
- Rebound seizures
- Seizures in non-epileptic persons 9
- Anxiety, agitation, irritability
- Depression
- Insomnia
- Headache
- Muscle aches, weakness
- Loss of coordination, loss of concentration, feeling faint
- Twitching
- Nausea, vomiting
- Tremors, shaking
- Perspiring excessively
- Photophobia (hyper-sensitive to light)
- Impaired memory
- Tachycardia (racing heart rate at rest)
- Anorexia
Slowly reducing the medication with other support mechanisms in place are the means used to offset these reactions.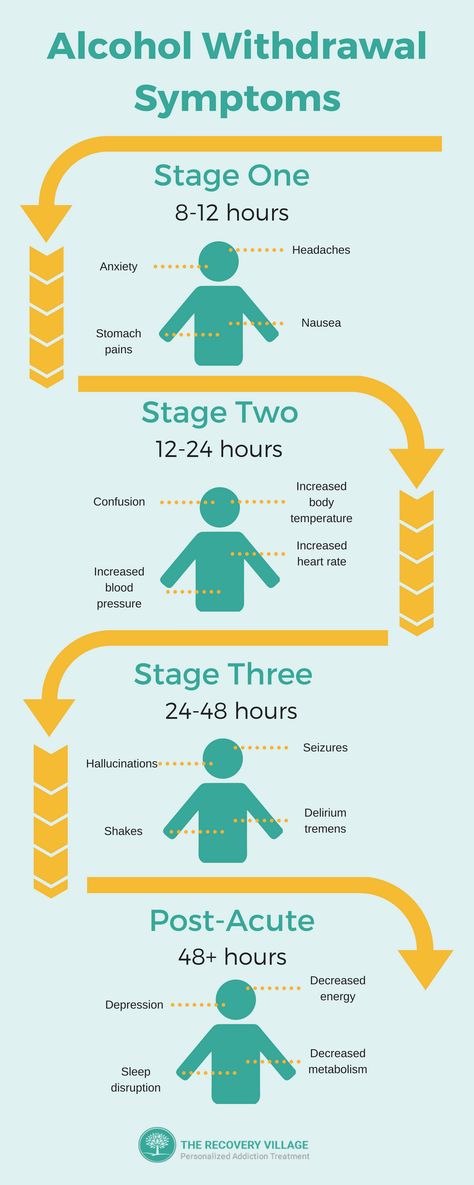
WARNING: Never abruptly or quickly stop taking Depakote. Find help to assist you with the challenges of Depakote tapering or coming off any psychoactive substance.
What is Depakote?
Depokate is an ACD or anticonvulsant drug, often used as a mood stabilizer in bipolar conditions, and used to control epileptic seizures and migraine headaches. The generic name is divalproex sodium or simply valproate or valproic acid. There is an extended-release version of the drug called Depakote ER (sustained-release), which is taken once a day and released slowly over a 24-hour period. There is also a “delayed-release” version called Depakote EC (enteric-coated) which is NOT time-release but has a protective enteric coating that dissolves only after it reaches the intestines, then releasing the medication all at once. The EC or delayed-release (non-sustained release) version must be taken several times a day. There is also a “sprinkles” version which is delayed-release (not 24-hr sustained-release) that was designed to be sprinkled on soft food for those who have trouble swallowing capsules.6
There is also a “sprinkles” version which is delayed-release (not 24-hr sustained-release) that was designed to be sprinkled on soft food for those who have trouble swallowing capsules.6
While this anticonvulsant drug is not a benzodiazepine, in their 2021 book entitled “Valproic Acid.” Rahman and Nguyen conclude that the mechanism of action is in some ways similar, and involves the control of GABA distribution (and other neurochemicals) along the CNS.10 GABA is a calming natural chemical, though the complex mechanism of action and its interactions with other transmitters and molecules and messaging systems are not entirely understood. Its calming properties make it useful in acute situations such as alcohol withdrawal, where controlling symptoms of alcohol withdrawal is desired without the use of benzodiazepines.11
Contact Alternative to Meds Center
You or your loved one may be struggling with side effects, tolerance, or other issues that may be blocking your ability to enjoy natural mental health and be truly well. You owe it to yourself to find out more about how the Alternative to Meds Depakote tapering program works, whether you feel you would be a good candidate, and how it could possibly assist you to overcome these challenges.
You owe it to yourself to find out more about how the Alternative to Meds Depakote tapering program works, whether you feel you would be a good candidate, and how it could possibly assist you to overcome these challenges.
Mental Disorders Treatment News #36
Prepared with the support of Doctor SAN Clinic of Psychiatry (St. Petersburg) disorders, but their role in pediatric practice has been little studied.
A case series presents positive therapeutic effects in non-compliant adolescents with severe mental illness. Three open studies have confirmed the clinical efficacy of extended-release risperidone injection in patients previously stabilized with oral risperidone. One study showed greater improvement in clinical symptoms and higher functioning at 12 months in young adults treated for an acute psychotic episode with paliperidone palmitate compared with oral risperidone. The types and frequency of APD side effects were comparable to those observed for oral antipsychotics. Two studies have shown better metabolic and neurological tolerability of APD compared to the oral form. However, the level of evidence (RoB2 instrument) was low for the efficacy of APD in pediatric practice and very low for tolerability and acceptability. nine0008
Two studies have shown better metabolic and neurological tolerability of APD compared to the oral form. However, the level of evidence (RoB2 instrument) was low for the efficacy of APD in pediatric practice and very low for tolerability and acceptability. nine0008
Source
Antipsychotic drugs are the mainstay of treatment for schizophrenia and are known to reduce the acute symptoms of the disorder. The original version of the review, published in 2012, examined the effectiveness of antipsychotics in preventing relapses versus no drugs in people with schizophrenia or schizophrenia-like psychosis based on data from randomized trials. The same review was updated and supplemented with additional parameters: remission and recovery rates, changes in social functioning and quality of life of patients. nine0008
Antipsychotics were more effective than placebo in preventing relapse at 1 year and in reducing hospital admissions. Quality of life appeared to be better in participants receiving pharmacotherapy; the same data for social functioning.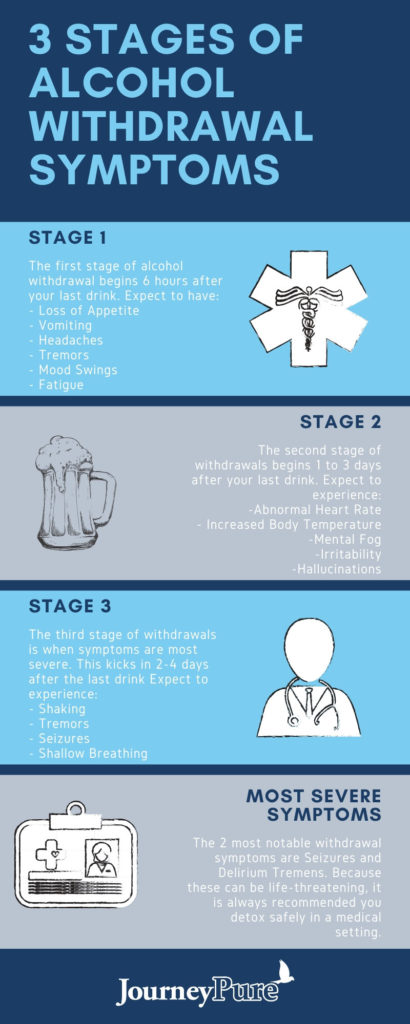 Based on evidence from fewer studies, maintenance therapy appeared to increase the likelihood of achieving symptom remission and maintaining it beyond 6 months. There was no recovery data. Antipsychotics as a group were associated with more participants experiencing side effects such as movement disorders (eg, at least one movement disorder) and weight gain. nine0008
Based on evidence from fewer studies, maintenance therapy appeared to increase the likelihood of achieving symptom remission and maintaining it beyond 6 months. There was no recovery data. Antipsychotics as a group were associated with more participants experiencing side effects such as movement disorders (eg, at least one movement disorder) and weight gain. nine0008
Source
Clozapine is the gold standard for the treatment of patients with treatment-resistant schizophrenia. However, approximately 60% of these patients do not respond to clozapine; moreover, clinical outcomes after discontinuation of clozapine are still unclear. In this regard, the authors conducted a systematic review to clarify the results after discontinuation of clozapine.
Three randomized controlled trials reported worsening of psychiatric symptoms. In 10 single-arm studies, the results of worsening and improving psychiatric symptoms were inconsistent.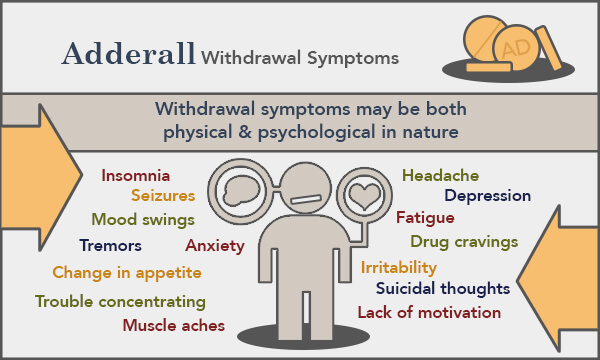 In one large retrospective cohort study, rechallenge of clozapine, olanzapine, and antipsychotic polypharmacy resulted in lower readmission rates compared with no treatment after clozapine was discontinued. In the other 14 retrospective studies, the vast majority of cases showed clinical deterioration after clozapine was discontinued. Among the five clinical outcome studies after returning to clozapine, four reported an improvement in clinical status in more than half of patients who restarted clozapine. Another study reported that the post-discontinuation clozapine group had a worse remission score than the continuous clozapine group. nine0008
In one large retrospective cohort study, rechallenge of clozapine, olanzapine, and antipsychotic polypharmacy resulted in lower readmission rates compared with no treatment after clozapine was discontinued. In the other 14 retrospective studies, the vast majority of cases showed clinical deterioration after clozapine was discontinued. Among the five clinical outcome studies after returning to clozapine, four reported an improvement in clinical status in more than half of patients who restarted clozapine. Another study reported that the post-discontinuation clozapine group had a worse remission score than the continuous clozapine group. nine0008
Source
Post-psychotic depression (PPD) after the first psychotic episode (PEP) differs from other depressive syndromes in chronic schizophrenia in its etiology, symptoms, and prognostic implications. The aim of the systematic review was to find out whether any pharmacological or non-pharmacological interventions for depressive symptoms after PES have proven effective.
PPD continues to be a diagnostic and therapeutic problem. Available data on the use of treatments, whether pharmacological or non-pharmacological, are limited. However, some approaches, such as online therapy and treatment with omega-3 polyunsaturated fatty acids (PUFAs), show promising results. For future research, it may be interesting to focus not only on the treatment of PPD, but also on diagnostic sample heterogeneity and tailoring the nature of the intervention to the individual. nine0008
Source
To date, there are limited data on the antidepressant effect of memantine in patients with serious mental illness. The authors conducted a systematic review and meta-analysis to evaluate the efficacy of memantine in such populations.
Memantine significantly reduced depressive symptom scores compared to controls with a small effect size. In terms of secondary outcomes, memantine had no significant effect on response or remission rates.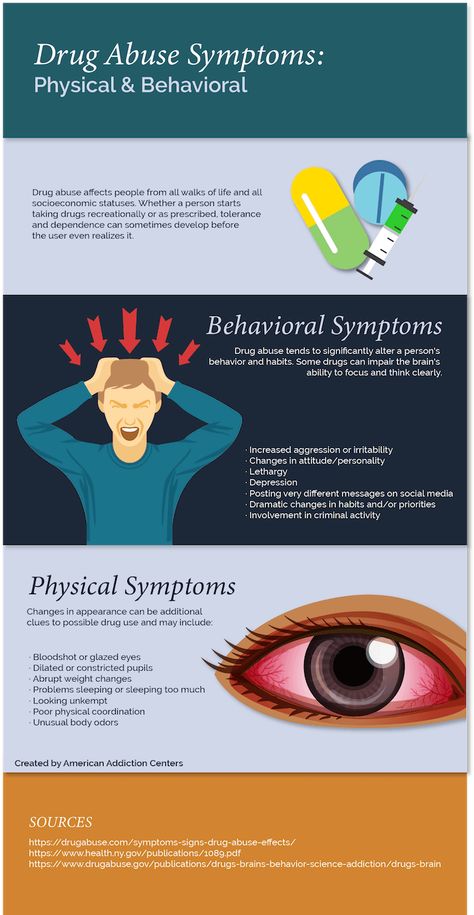 In a subgroup analysis, memantine significantly reduced depressive symptom scores in patients with mood disorders with a small effect size, but not in patients with schizophrenia. In addition, memantine was well tolerated and was acceptable to patients. nine0008
In a subgroup analysis, memantine significantly reduced depressive symptom scores in patients with mood disorders with a small effect size, but not in patients with schizophrenia. In addition, memantine was well tolerated and was acceptable to patients. nine0008
Source
Tiapride is an atypical antipsychotic used to treat alcohol withdrawal, aggressiveness and agitation, headache, dyskinesias, tics, and Tourette's syndrome. More recently, it has been proposed for the treatment of delirium and agitation in hospitalized patients with COVID-19. Although its safety profile makes it suitable for use in vulnerable populations, the use of tiapride in psychiatric disorders is limited. This systematic review focuses on the available data on the efficacy and tolerability of tiapride in individuals with psychiatric disorders. nine0008
Six studies (published between 1982 and 2010) were included in the review. These studies have shown that tiapride can be considered a relatively safe treatment option for selected patients with alcohol withdrawal or dementia agitation. However, there is no convincing evidence of its effectiveness in the scientific literature. High-quality trials are still needed to fully support its use in clinical practice.
However, there is no convincing evidence of its effectiveness in the scientific literature. High-quality trials are still needed to fully support its use in clinical practice.
Source
This study was designed to investigate the effectiveness of repetitive transcranial magnetic stimulation (rTMS) in the treatment of suicidal ideation in patients with mental illness.
Results of a systematic review showed that rTMS significantly reduced suicidal ideation and the severity of depressive symptoms in patients with major psychiatric disorders. In a subgroup analysis, rTMS reduced suicidal ideation in patients with non-resistant depression (non-TRD), but not in patients with TRD. rTMS as a combination therapy was more effective than monotherapy. Suicidal thoughts were significantly reduced in patients who completed more than ten treatment sessions. Importantly, the rTMS group demonstrated favorable tolerability without serious adverse events.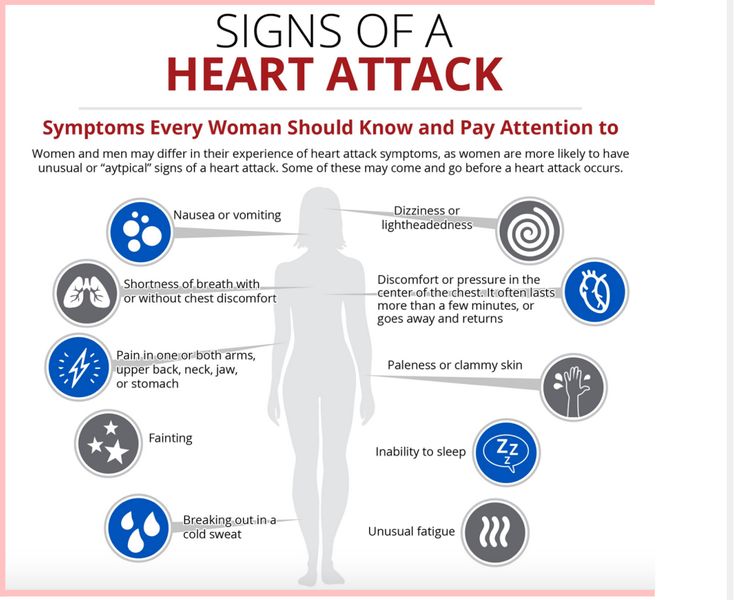 nine0008
nine0008
Source
Rapid cycling bipolar disorder is a severe and disabling condition that poses a significant challenge to the clinician. This systematic review reviewed existing strategies for the treatment of this disorder. Lithium, anticonvulsants, second-generation antipsychotics, antidepressants, and thyroid hormones were all evaluated as treatment options in the data presented.
There is still little evidence for the treatment of bipolar disorder with fast cycling. Evidence from a systematic review supports the use of aripiprazole, olanzapine, and valproate for acute manic or mixed episodes, quetiapine for acute depressive episodes, and aripiprazole and lamotrigine for relapse prevention.
Source
A new, once-daily, extended-release (ER) form of divalproex has been developed; this formulation prolongs therapeutic serum levels of the drug compared to the conventional twice-daily modified-release (DR) formulation of divalproex.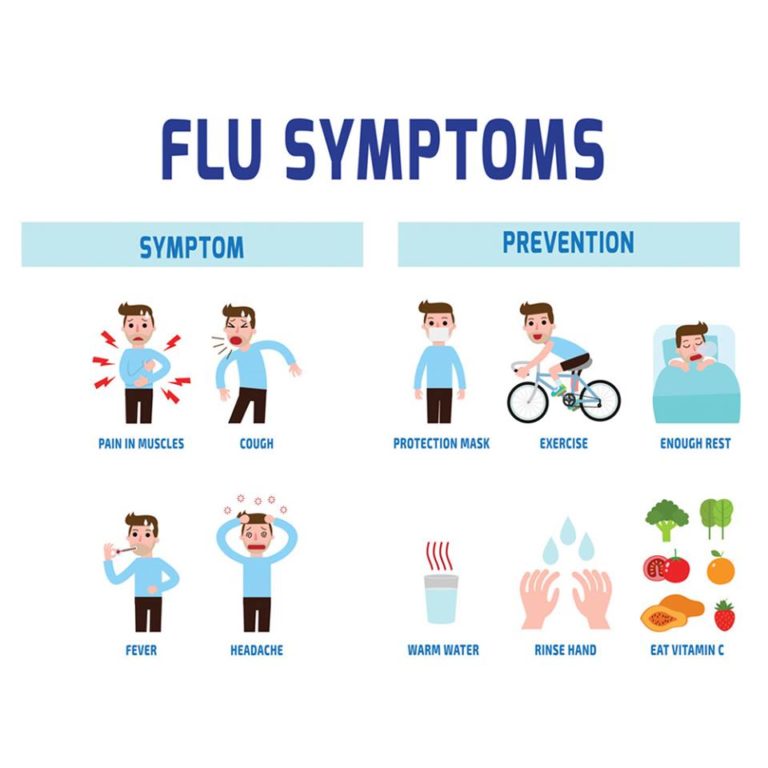 A meta-analysis of controlled clinical trials was aimed at studying and comparing the efficacy, safety and adherence rates of divalproex ER (VPA-ER) and conventional divalproex DR (VPA-DR). nine0008
A meta-analysis of controlled clinical trials was aimed at studying and comparing the efficacy, safety and adherence rates of divalproex ER (VPA-ER) and conventional divalproex DR (VPA-DR). nine0008
VPA-ER was significantly more effective than placebo in both bipolar and epileptic patients, providing similar efficacy to conventional VPA-DR. VPA-ER was well tolerated with a low incidence of adverse events compared with placebo. In addition, the acceptability and convenience of VPA-ER has contributed to adherence to long-term maintenance treatment of chronic diseases.
Source
Systematic review and meta-analysis data 17 studies (676 patients on lithium) do not support lithium as first-line therapy for acute bipolar depression. However, bipolar/monopolar sensitivity analysis and a slight advantage over placebo suggest that lithium may still be a viable treatment option. Larger, more carefully designed studies are needed to determine the full spectrum of efficacy of lithium versus placebo and other psychoactive drugs. nine0008
nine0008
Source
The material was prepared with the support of the Clinic of Psychiatry "Doctor SAN" (St. Petersburg)
Translated : Cherapkin E.S.
Compiled by : Kasyanov E.D.
Withdrawal from drugs and substances
Restriction of the use of drugs, antidepressants, alcohol, nicotine can lead to the development of a withdrawal syndrome. This condition is a natural reaction of the body to the cessation of the intake of various substances into the body, it is accompanied in most cases by intense symptoms that a person cannot get rid of on his own. nine0008
Yusupov hospital specialists with many years of experience treat withdrawal syndrome. Highly qualified psychiatrists and narcologists explain to patients what the drug withdrawal syndrome is characterized by and select the most effective methods for eliminating symptoms for patients.
Reasons for the development of the withdrawal syndrome
Drugs contain psychoactive substances, therefore, on the background of their long-term use, the patient may experience withdrawal symptoms when therapy is stopped.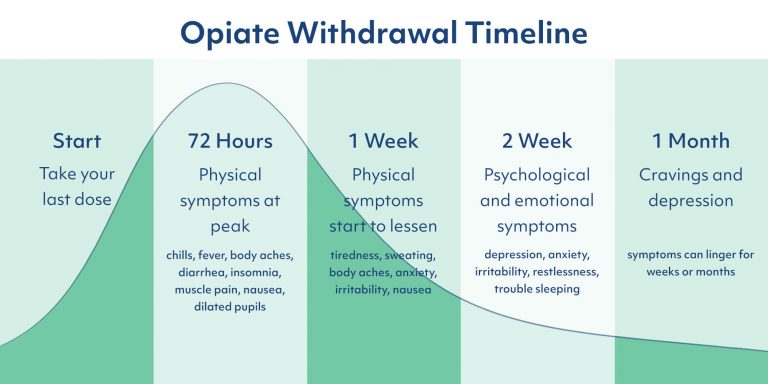 The action of these substances contributes to a change in the emotional background, psychological state, functioning of the nervous system. nine0008
The action of these substances contributes to a change in the emotional background, psychological state, functioning of the nervous system. nine0008
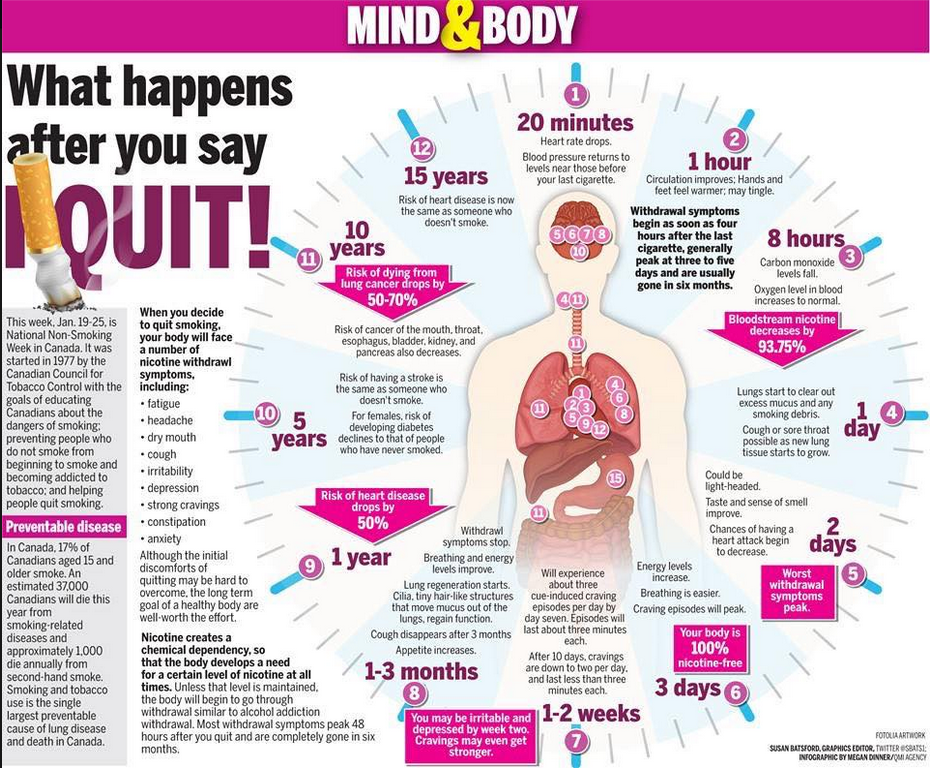
Different kinds of dependencies also cause this effect. For example, smokers may develop a nicotine withdrawal syndrome, but it takes a long period of time to form. Withdrawal symptoms can also be seen in alcoholism, opiomania, and cocainism.
Flenlepsin: withdrawal syndrome
Indications for the appointment of Flenlepsin are mental disorders, neurological disorders, alcohol withdrawal syndrome, epilepsy. However, stopping the use of the drug may cause a withdrawal syndrome. Phenibut also contains psychoactive substances, so withdrawal syndrome is a common problem with which patients come to the Yusupov hospital. nine0008
Psychiatrists at the Yusupov Hospital regularly study world experience in the field of addiction therapy, so they know how to treat withdrawal syndrome. A comfortable hospital is located on the basis of the Yusupov hospital, which allows you to limit patients from an undesirable environment and regularly monitor their condition and withdrawal symptoms.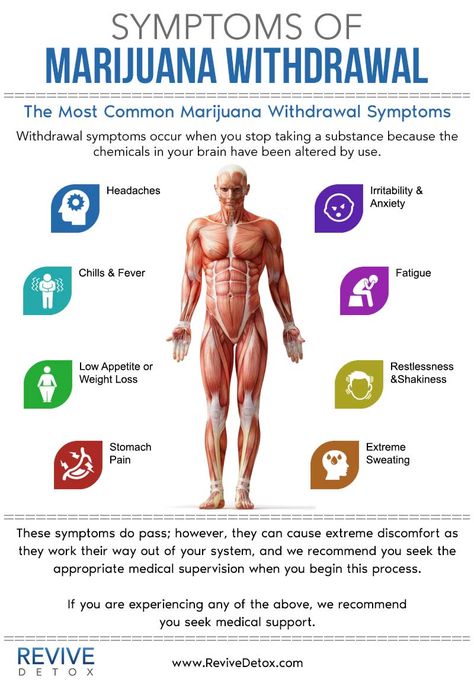
Clonazepam: Withdrawal Syndrome
Clonazepam is a sedative drug, so it is used in the treatment of panic attacks, headaches, phobias, anxiety. The duration of taking the drug should not exceed 2 weeks, most often clonazepam is used once to improve the mental state. nine0008
Patients who have taken the drug for more than 2 months need professional help, as they may show physical and psychological signs of dependence. Psychiatrists at the Yusupov Hospital cooperate with experienced narcologists and select methods for treating clonazepam withdrawal syndrome, taking into account the fact that its elimination from the body takes a long time.
Hashish withdrawal syndrome
Withdrawal syndrome after the use of hashish develops with its regular use and combination with alcohol. In the initial stages, a person experiences the following symptoms:
- depressed mood;
- aggression;
- lethargy and apathy;
- drowsiness and fatigue.

Morphine withdrawal has symptoms similar to hashish withdrawal. Patients who are in a state of depression, an excited state, cannot independently overcome the manifestations of the withdrawal syndrome. Psychiatrists at the Yusupov Hospital help patients with these addictions overcome their psychological addiction, professional narcologists carry out activities aimed at removing drugs from the body. nine0008
Lyrica: withdrawal syndrome
Lyrica tablets are a heavy psychotropic drug used in the treatment of depression, anxiety and other conditions. This drug, when administered to the body, causes mental and physical arousal. The development of drug dependence is one of the side effects of long-term use of Lyrica.
Psychiatrists of the Yusupov hospital study the world experience in the treatment of drug addictions, in particular, the subject of research is the withdrawal syndrome of beta blockers. Specialists with academic degrees use only world-class methods that have scientific justification and have passed clinical trials.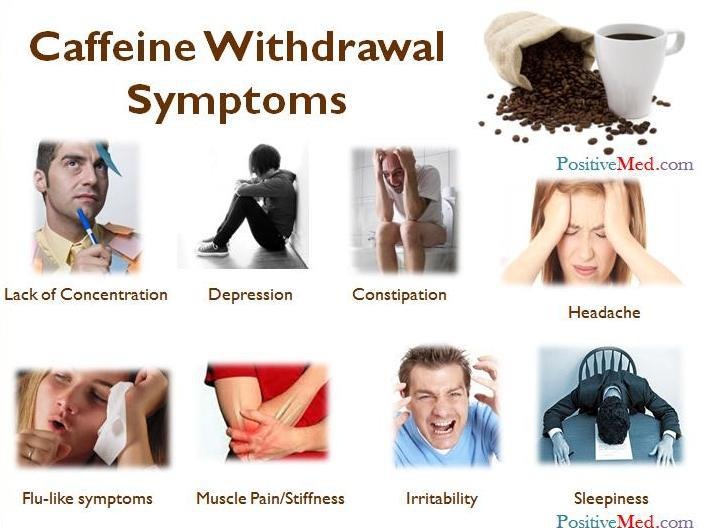 nine0008
nine0008
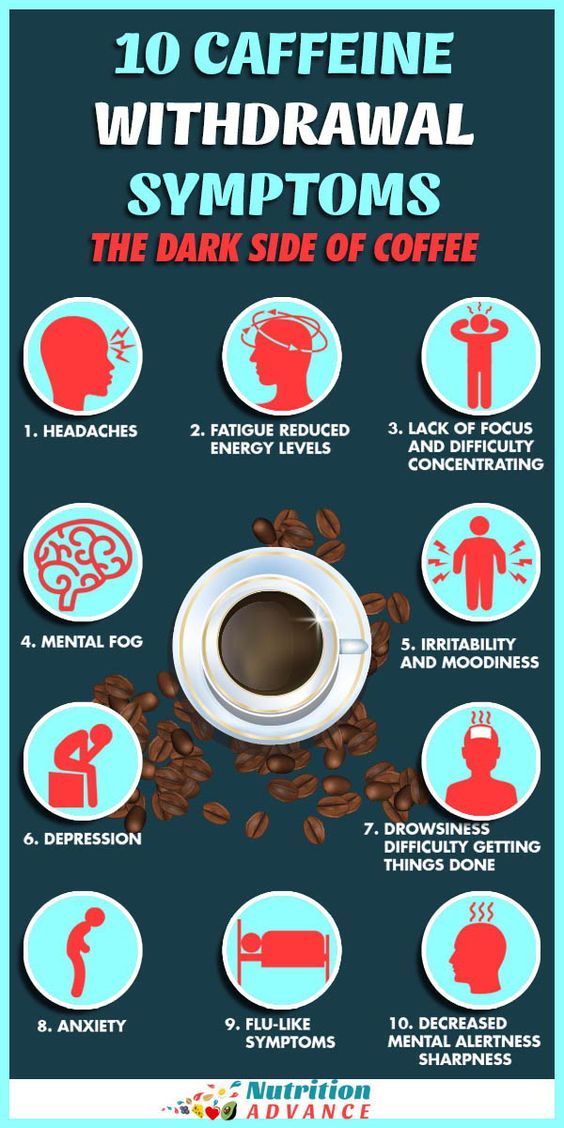
Caffeine withdrawal syndrome
Caffeine and energy drinks can cause addiction, to get rid of which psychiatrists of the Yusupov hospital carry out consistent work consisting of several stages:
- awareness of the problem and determination of the degree of dependence;
- assessment of the patient's physical condition;
- activities aimed at caffeine detoxification;
- developing a strategy for drinking caffeinated drinks. nine0191
Programs developed individually for each patient of the Yusupov Hospital are aimed at restoring psychological and physical health. The tactics of interaction with a patient who has been diagnosed with amphetamine withdrawal syndrome will differ significantly from getting rid of caffeine withdrawal. In addition, when treating patients with severe forms of addiction, work with the environment is carried out.
Smoking withdrawal syndrome
Prednisol withdrawal syndrome, the symptoms of which appear with prolonged use of the drug, differs from the signs of nicotine withdrawal. This syndrome has various manifestations: allergic reactions, insomnia, headaches, constipation, increased blood pressure, increased appetite. nine0008
This syndrome has various manifestations: allergic reactions, insomnia, headaches, constipation, increased blood pressure, increased appetite. nine0008
Some people cannot overcome their symptoms without help from a specialist and use cigarettes to relieve symptoms. Innovative methods, combined with traditional approaches to quitting smoking and relieving nicotine withdrawal syndrome, are used by psychiatrists at the Yusupov Hospital. The result of complex therapy is the patient's complete refusal to smoke cigarettes.
Withdrawal: how long does it take
The duration of withdrawal depends not only on the individual patient but also on the addictive substances. The prednisolone withdrawal syndrome is successfully treatable, its manifestations with complex treatment disappear within a few weeks. With the refusal to use hashish and other narcotic substances, the normalization of the condition occurs gradually over several months. nine0008
Treatment of withdrawal symptoms in Moscow
Multidisciplinary Yusupov Hospital is a modern medical facility that provides patients with medical services in accordance with international standards.