How to support someone with a mental illness
SAMHSA’s National Helpline | SAMHSA
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.
Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders.
This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative. Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs. In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid.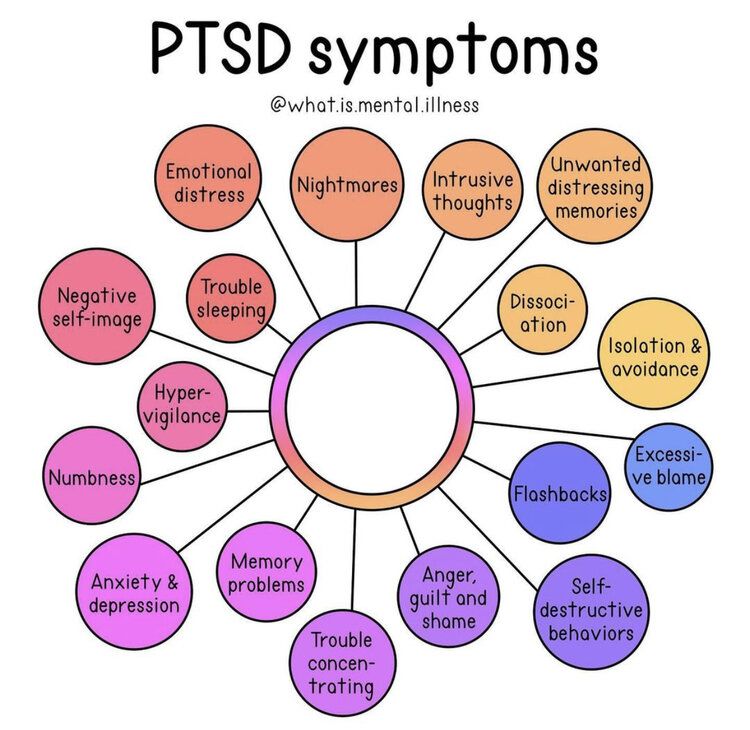 If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems. Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.
Addresses concerns of children of parents with substance use/abuse problems.It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt. Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse. Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.
For additional resources, please visit the SAMHSA Store.
Last Updated: 08/30/2022
Recovery and Recovery Support | SAMHSA
Recovery and Resilience
Resilience refers to an individual’s ability to cope with change and adversity. Resilience develops over time and gives an individual the capacity not only to cope with life’s challenges but also to be better prepared for the next stressful situation. Psychological resilience, the ability to cope with adversity and to adapt to stressful life events, varies widely from person to person and depends on environmental as well as personal factors. It refers to positive adaptation, or the ability to maintain mental and physical health despite participating in stressful situations. Resilience is playing up those protective factors so they can outweigh the risk factors. Optimism and the ability to remain hopeful are essential to resilience and the process of recovery.
Because recovery is a highly individualized process, recovery services and supports must be age appropriate and offered over the life course and flexible enough to ensure cultural relevancy. What may work for adults in recovery may be very different for youth or older adults in recovery. For example, the promotion of resiliency in young people, and the nature of social supports, peer mentors, and recovery coaching for adolescents and transitional age youth are different than recovery support services for adults and older adults.
What may work for adults in recovery may be very different for youth or older adults in recovery. For example, the promotion of resiliency in young people, and the nature of social supports, peer mentors, and recovery coaching for adolescents and transitional age youth are different than recovery support services for adults and older adults.
Recovery and Relationships
The process of recovery is supported through relationships and social networks. This often involves family members who become the champions of their loved one’s recovery. They provide essential support to their family member’s journey of recovery and similarly experience the moments of positive healing as well as the difficult challenges. Families of people in recovery may experience adversities in their social, occupational, and financial lives, as well as in their overall quality of family life.
These experiences can lead to increased family stress, guilt, shame, anger, fear, anxiety, loss, grief, and isolation. The concept of resilience in recovery is also vital for family members who need access to intentional supports that promote their health and well-being. The support of peers and friends is also crucial in engaging and supporting individuals in recovery.
The concept of resilience in recovery is also vital for family members who need access to intentional supports that promote their health and well-being. The support of peers and friends is also crucial in engaging and supporting individuals in recovery.
Peer support assists individuals to engage or stay connected to the recovery process through a shared understanding, respect, and mutual empowerment. Peer support extends beyond the reach of clinical treatment into the everyday environment providing non-clinical, strengths-based support. This relationship can help lay the foundation for SAMHSA’s four dimensions of recovery.
Recovery Support
SAMHSA advanced recovery support systems to promote partnering with people in recovery from mental and substance use disorders and their family members to guide the behavioral health system and promote individual, program, and system-level approaches that foster health and resilience; increase housing to support recovery; reduce barriers to employment, education, and other life goals; and secure necessary social supports in their chosen community.
Recovery support is provided in various settings. Recovery support services help people enter into and navigate systems of care, remove barriers to recovery, stay engaged in the recovery process, and live full lives in communities of their choice.
Recovery support services include culturally and linguistically appropriate services that assist individuals and families working toward recovery from mental and/or substance use problems. They incorporate a full range of social, legal, and other services (PDF | 409 KB). that facilitate recovery, wellness, and linkage to and coordination among service providers, and other supports shown to improve quality of life for people (and their families) in and seeking recovery.
Recovery support services may be provided before, during, or after clinical treatment, or may be provided to individuals who are not in treatment but seek support services.
These services, provided by professionals and peers, are delivered through a variety of community and faith-based groups, treatment providers, schools, and other specialized services. The broad range of service delivery options ensures the life experiences of all people are valued and represented.
The broad range of service delivery options ensures the life experiences of all people are valued and represented.
For example, in the United States there are 34 recovery high schools that help reduce the risk in high school environments for youth with substance use disorders. These schools typically have high retention rates and low rates of students returning to substance use.
Additionally, SAMHSA's Bringing Recovery Supports to Scale Technical Assistance Center Strategy (BRSS TACS) advances effective recovery supports and services for people with mental or substance use disorders and their families.
Find more Publications and Resources on Recovery and Recovery Support.
Help for a loved one with a mental disorder
Basic concepts
There is a lot of talk these days about the rise in the number of mental disorders in society, but many people have very vague ideas about this very vague concept. Despite the fact that now psychiatrists are doing everything possible to inform the population as best as possible about stress, depression, anxiety, neuroses, more severe mental disorders, there is very little literature written by experts for the average layman, and on the Internet there is an abundance of information written either difficult language, or simply illiterate. All this ultimately leads to the fact that such information is not only contrary to reality, but also harmful. nine0005
All this ultimately leads to the fact that such information is not only contrary to reality, but also harmful. nine0005
It is impossible to sort everything out in one article and give clear instructions on the relationship between the patient and his relatives, but it is possible to bring to a holistic picture the idea of this complex group of diseases (the terms "disease" and "disorder" from a medical point of view are largely close, but not identical*). Therefore, my task is to acquaint the reader with this complex problem, primarily related to relationships and assistance to those suffering from severe mental illnesses. nine0005
* It is desirable to know the most basic terms, then it will be easier for the doctor to help both the patient himself and his relatives. In addition, you should not use terms that are not well known to you, it is better to describe the situation or condition as you understand it.
So, mental (or mental, because psyche - translated from Greek means the soul ) disorders - are painful conditions of a person with psychopathological (i. e., with mental disorders) and behavioral (i.e., they do not always appear, for example, in case of neurosis, when a person by willpower keeps himself within the limits of cultural society up to a certain point) manifestations due to the influence of biological, psychological, social and other factors.
e., with mental disorders) and behavioral (i.e., they do not always appear, for example, in case of neurosis, when a person by willpower keeps himself within the limits of cultural society up to a certain point) manifestations due to the influence of biological, psychological, social and other factors.
Let's not confuse with psychosis (or psychotic) disorders, which are characterized by gross and contradictory environmental disorders of thinking, perception and behavior (delusions, in a medical, not philistine view; hallucinations; psychomotor agitation; suicidal behavior, etc.). nine0005
It is important to note that the problem of mental disorders is interdisciplinary and even interdepartmental, social. Rehabilitation is needed, not just treatment.
As for the diagnosis. Diagnosis - definition and recognition, an indication of the disease. In medicine, and especially in psychiatry, diagnosis does not always mean treatment in strict accordance with the diagnosis.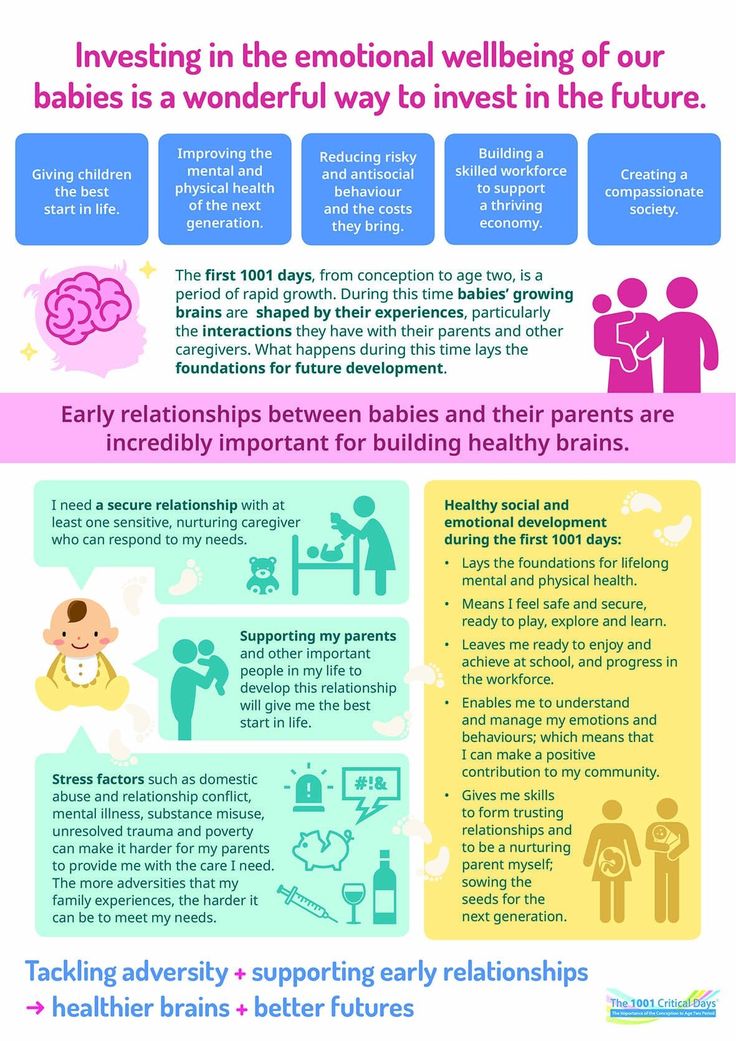 Diagnosis is often a statistical category needed to understand, roughly speaking, how the condition of one patient is similar to another. nine0005
Diagnosis is often a statistical category needed to understand, roughly speaking, how the condition of one patient is similar to another. nine0005
I am sometimes puzzled by the desire of a person to look at the records of a doctor. After all, a special interpretation, justification of the diagnosis, terminology can not only frighten and offend an unprepared person, but cause unreasonable distrust of a specialist and, even worse, aggravate disturbed mental balance, upset not only the patient, but also relatives.
It is much more important to trust each other (the doctor, the patient, his relatives), to ask questions of interest. It is on trust that the desired result is achieved - a cure or a stable remission, if the disorder is chronic. nine0005
I will not decipher concepts and terms much in this article. Let's talk about the topic corresponding to the title. We will talk about such diseases as schizophrenia, dementia, severe depression, drug addiction (alcoholism, drug addiction), etc.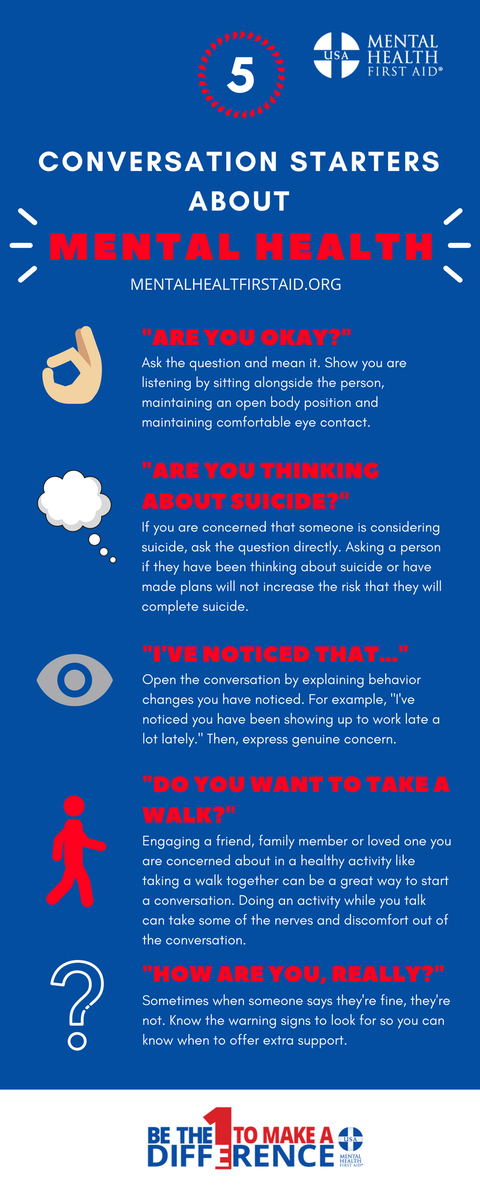 I will try to give basic, a kind of "universal" recommendations.
I will try to give basic, a kind of "universal" recommendations.
Recommendations
1 situation: a relative (both a 16-year-old child and an old grandfather, a researcher in the past or present) became “somehow not like that”, began to withdraw, get annoyed for no apparent reason, although “he had never been aggressive before ', to talk, to talk to oneself. nine0005
Usually, such behavior is first perceived as a joke, then surprise, then a discussion with a sick person begins, which can lead to serious conflicts and distrust. If you suspect that a person close to you has a mental disorder (we do not take emergency situations, for example, in case of severe aggression, the police and medical workers are already intervening here), you cannot argue.
It is also desirable not to support the painful delusions of a person, to try to be patient and caring, to persuade a loved one to seek medical help. Unfortunately, in our society, when it comes to psychiatry, in most cases it causes a smile, fear, surprise, but not sympathy and a desire to help a sick person, especially if it refers to a relative. Only later, when a sick person can feel and even understand that the help of a psychiatrist is for his benefit, will he himself reach out to her. nine0005
Only later, when a sick person can feel and even understand that the help of a psychiatrist is for his benefit, will he himself reach out to her. nine0005
At the initial stage, it is worth trying to persuade a person to calm down, assess his degree of adequacy (if he used to trust you, but now he doesn’t groundlessly, whether he understands you or is completely in his experiences, etc.), to understand whether there are threats to him and surrounding.
It is impossible to forcibly help a person (involuntary hospitalization in a psychiatric hospital is carried out only by a court decision), but everything possible must be done: to involve relatives who will correctly understand and support people who are authoritative for the patient, consult a doctor. nine0005
Situation 2: patients were brought to a psychiatrist. There can be 2 ways here. The doctor will help to understand the situation, make a diagnosis, prescribe treatment, give recommendations. Everything here is very individual.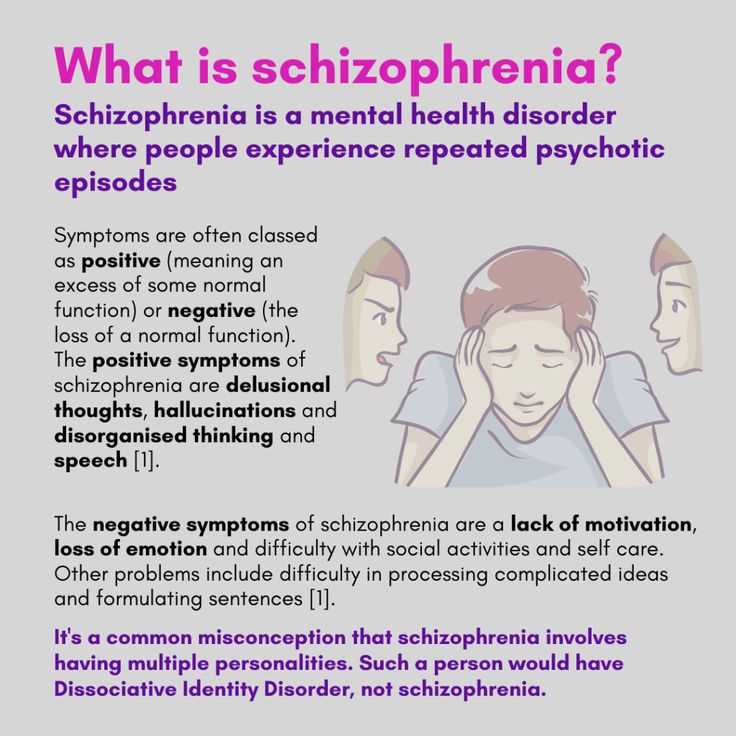 But it may also be that the doctor gives a recommendation, but not only the patient (due to inadequacy), but also a relative does not want to follow it.
But it may also be that the doctor gives a recommendation, but not only the patient (due to inadequacy), but also a relative does not want to follow it.
I can give an example. A mother brings her 20-year-old daughter to a psychotherapist. The daughter has painful sensations in her body: the bones, according to her, “go back and forth, fall through and hurt.” All specialists were examined, all studies were carried out, including MRI, no diseases were found, the symptoms do not correspond to the alleged physical pathology. nine0005
A mental illness was diagnosed, drugs were prescribed, and after a couple of months there was a significant improvement. The patient stops taking the medicine, after a while she comes to the doctor with her mother, complains about the deterioration, assures that the medicines do not help, refuses help, runs out of the office, rushes about, says that she does not want to live. Hospitalization is proposed, since adequate dosages of drugs can only be prescribed in a hospital, in response - a categorical refusal.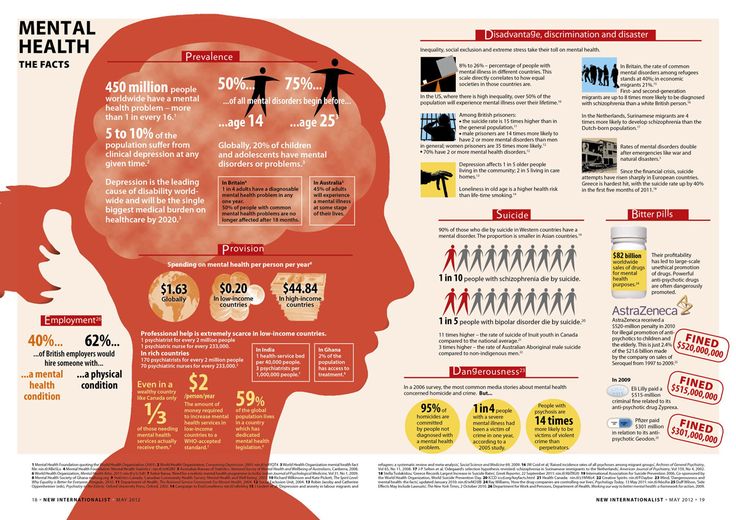 nine0005
nine0005
With difficulty he manages to calm down, persuade him to give an injection, agrees to resume taking medications. The doctor suggests that the mother call a psychiatric team to resolve the issue of hospitalization, in connection with the suicidal risk, to which he receives the answer: “Well, she will kill herself, then this is her fate, I will not put her in a psychiatric hospital.” On receipt released home. The mother calls the next day, the daughter gets a little better, then disappears for six months. Another call to the doctor's personal phone: the daughter lies in bed, does not want to get up, complains about "movements in the body of some creatures" that cause severe pain. nine0005
Recommendations were given, the patient was finally hospitalized in a psychiatric hospital with schizophrenia. She was discharged with improvement, criticism of her condition appeared, adequate therapy was selected.
Bottom line: fortunately, this story ended happily, but the patient suffered for several months, while the mother believed in the need for hospitalization; I had to prescribe heavier drugs, the treatment was delayed.
There is nothing wrong if the patient refuses this doctor (for example, the patient has included the doctor in his delusional system) or the doctor himself understands that he will not be able to provide adequate assistance. Then it is necessary to attract colleagues, send them to a hospital, together with relatives, think over options for assistance and choose the best one. It happens that the patient returns after treatment, apologizes for his behavior, because he did not understand the pain and inadequacy at that time. nine0005
You should not change specialists (sometimes people come to me with dozens of recommendations from different doctors of the same specialty, which is puzzling). Well, 2-3 opinions is understandable, but more than 10!? The most common reason is that medications do not immediately help, side effects.
Some patients soon stop taking their medications, and many diseases are chronic and require many months or even years of maintenance therapy. A natural deterioration sets in, the new doctor does not yet know the specifics of the course of the disorder in this patient, experiments with treatment begin, a new selection of medicines begins, resistance to treatment is formed, and previously effective drugs cease to work. nine0005
A natural deterioration sets in, the new doctor does not yet know the specifics of the course of the disorder in this patient, experiments with treatment begin, a new selection of medicines begins, resistance to treatment is formed, and previously effective drugs cease to work. nine0005
And one more thing: it is desirable, at the initial visit to the doctor, to bring, if not all, then the main examinations, extracts, and tests. A psychiatrist is a doctor like everyone else, and the more information about the patient, the easier it is to understand the diagnosis. For example, if a person has a pathology of the thyroid gland, it is advisable to bring the last tests for hormones, since when the hormonal background changes, the state of mind also changes (irritability, sleep disturbances, mood swings, etc.). nine0005
In some cases, antidepressants are not only not needed, but can be harmful, it may be worth limiting yourself to the appointments of an endocrinologist and psychotherapy.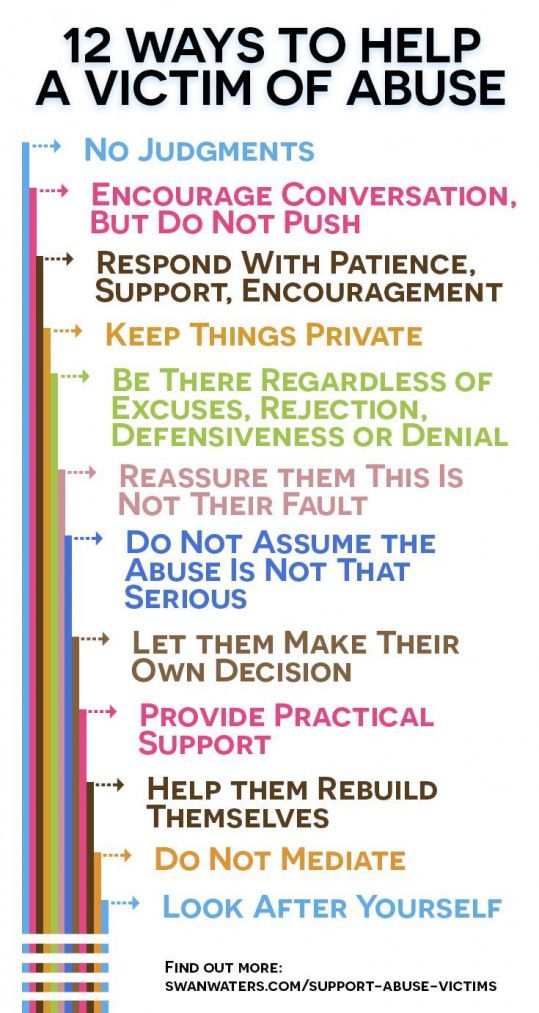 Elderly people with diabetes can confuse events and even behave inappropriately with an increase in blood glucose, here prescribed antipsychotics are also not always necessary.
Elderly people with diabetes can confuse events and even behave inappropriately with an increase in blood glucose, here prescribed antipsychotics are also not always necessary.
3 situation: the patient has been examined for a long time, the diagnosis is known, but the disease is progressing. Relatives begin to "look for a miracle": consult the patient with leading specialists, go to the main scientific centers, someone is looking for help abroad. nine0005
I have had a number of cases where patients have returned from the US, Europe, Israel, etc. with complaints that the prescription of drugs selected in Russia was refused, or that the treatment was simply ineffective, worsened. Here I would advise you to find a specialist you trust and coordinate your actions with him. Only together can we help sick people provide adequate assistance and, if not cured, then improve the quality of life as much as possible.
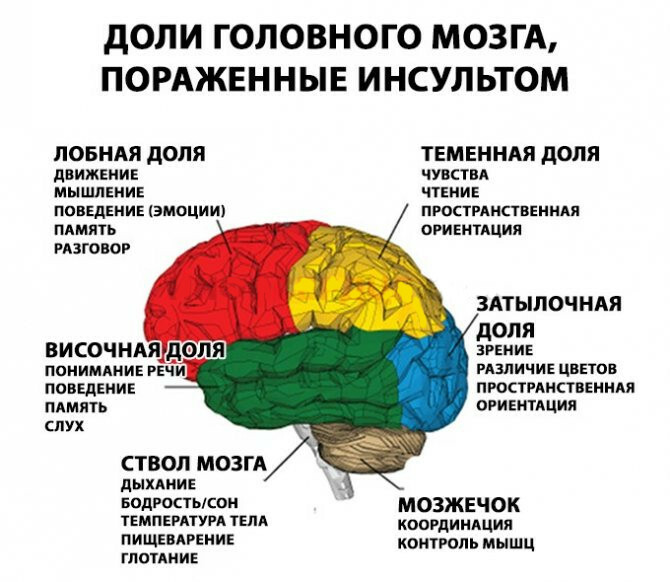
nine0003 4 situation: terminally ill patient in the final stage. There is an opinion, or rather another myth, that one does not die from mental illness, however, mental illness is the same as somatic (i.e. body diseases), only the brain is sick, regardless there is a visible focus there (for example, as a result of a craniocerebral injury to the damaged part of the brain) or not. For example, severe progressive dementia, the final stage of alcoholism with multiple organ disorders, the terminal stage in malignant forms of schizophrenia, and others. Here it is necessary to decide individually, depending on the specific case. nine0005
There is an opinion, or rather another myth, that one does not die from mental illness, however, mental illness is the same as somatic (i.e. body diseases), only the brain is sick, regardless there is a visible focus there (for example, as a result of a craniocerebral injury to the damaged part of the brain) or not. For example, severe progressive dementia, the final stage of alcoholism with multiple organ disorders, the terminal stage in malignant forms of schizophrenia, and others. Here it is necessary to decide individually, depending on the specific case. nine0005
“If a person cannot be cured, this does not mean that he cannot be helped.”
If you are destined to die, it is easier to do this among loving relatives on your bed, even if a person does not understand anything and does not recognize anyone. But he FEELS the attitude towards him. How a small child feels the caress of his mother, smiles or cries when his mother is gone. You will say - there is no comparison, children are our future, and here is a dying person who does not understand anything. Yes, this is true, but we must understand that any of us can, God forbid, be in the place of this person ... nine0005
Yes, this is true, but we must understand that any of us can, God forbid, be in the place of this person ... nine0005
Nursing staff
Well, a few words about help for those who care for the sick. It is difficult to give specific recommendations here, only one thing is clear: you cannot take the position of either a rescuer or a victim, you just need to fulfill your human duty to the best of your ability and ability. Don't forget yourself.
Any person who lives with a sick person, and even more so caring for him, experiences enormous personal and emotional stress. Therefore, you should think about how you will cope with the disease in the future. By understanding your own emotions properly, you will be able to deal more effectively with both the patient's problems and your own problems. You may have to experience emotions such as grief, shame, anger, embarrassment, loneliness and others. nine0005
For some people who care for the sick, the family is the best helper, for others it brings only grief.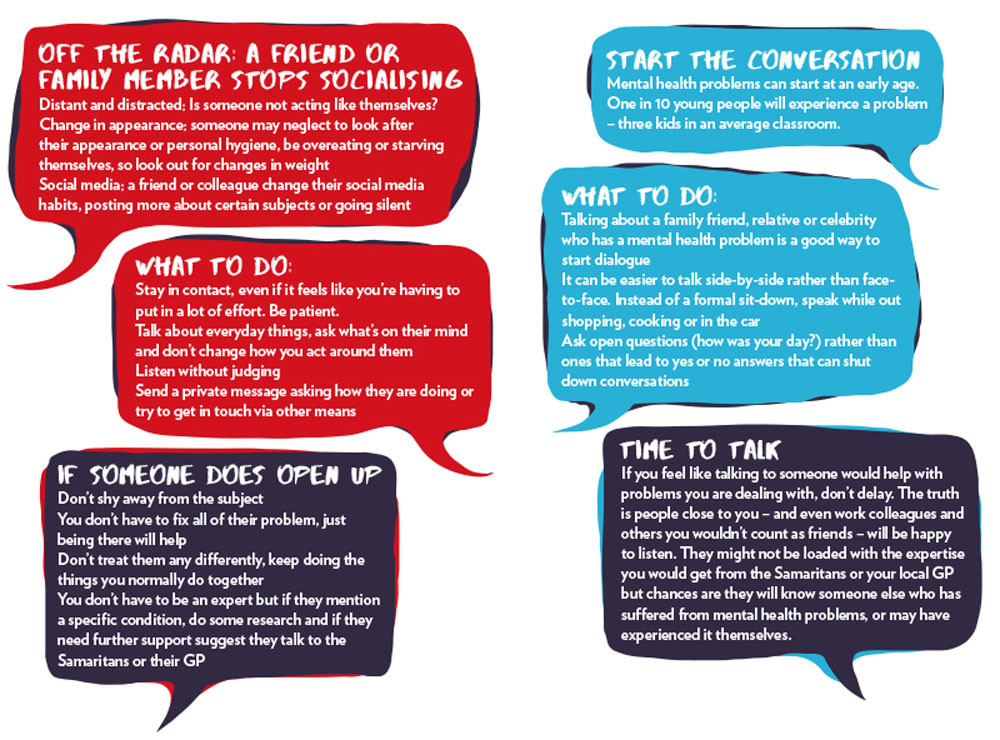 It is important not to reject the help of other family members if they have enough time, and not to try to bear the sometimes difficult burden of caring for the sick alone.
It is important not to reject the help of other family members if they have enough time, and not to try to bear the sometimes difficult burden of caring for the sick alone.
If family members upset you with their unwillingness to help, or criticize your work because of the lack of information about this disorder, you can form a family council to discuss care problems. In particular, make a decision to involve an employee, at least for the period of time necessary for your rest and recuperation, and, if necessary, treatment. nine0005
And the last. Don't keep problems to yourself. Feeling that your emotions are a natural reaction in your position, it will be easier for you to cope with your problems. Don't reject the help and support of others, even if you feel like you're making it difficult. Even psychotherapists themselves (seemingly knowing how to minimize stress as much as possible) often have their own psychotherapist, and it is bad for the doctor who neglects the help of his colleagues.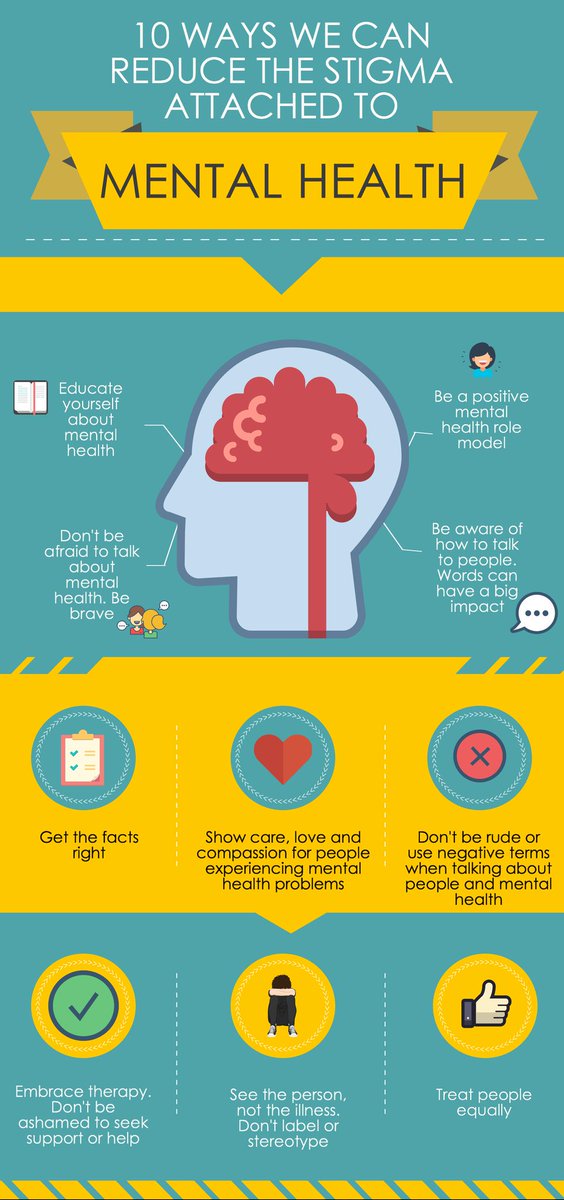
Prepared information for you: nine0005
Aronov Pavel Vladimirovich - psychiatrist, psychotherapist, narcologist, doctor of the highest category, candidate of medical sciences, associate professor. The doctor conducts an appointment in the building of the clinic on Baumanskaya.
How to communicate with a loved one who has a mental disorder: 9 simple rules about mom: she was diagnosed with a mental disorder when Paul was only seven. He was there when my mother refused to be treated, forgot to feed the children, offended loved ones. Paul shared with Afisha Daily the rules that have helped him and his mother all this time. nine0005
You can react to a diagnosis in completely different ways - and this is normal
When it all started, I was seven years old. Around the same time, I found out about my mother's depression - and felt relieved because she had been acting strange for a long time.
My sister and I were sometimes very scared: we lived in some kind of chaos, and after the doctors diagnosed my mother, we realized that this chaos has a name - a mental disorder. It helped us understand what was going on. nine0005
It helped us understand what was going on. nine0005
At some point, I began to realize that it was no longer safe to be around my mother. And it was kind of a test. I wanted to trust her and have a strong family relationship with her, but at the same time, I had to take care of myself and defend myself when needed.
If a person refuses to be treated, try to understand him
At the beginning of the illness, my mother was categorically against treatment. Already in my teens, I wanted to do everything to stop her manic episodes. And I wondered why she refused to be treated, but when I got older, I understood her skepticism in relation to medicines and everything else. nine0005
Medicines have a strong effect on your brain, changing your feelings, attitudes towards family, life and children. It is difficult to accept this, because you actually become a different person. I think the most important thing here is to listen to the person and try to understand what exactly he is afraid of. And support in every possible way.
For example, my mother went to sessions with a psychotherapist for a long time, and at one point I realized that I didn’t even know him and didn’t understand if I could trust him with my mother. It is not right. People often hope that if their loved ones go to the hospital, then sooner or later everything will be fine again. I think if you really care about the person, you need to talk to those who are trying to cure him .
Still need to communicate with each other. You can’t think that therapy with doctors is enough - it’s not. My sister and I were constantly talking to my mother, letting her know that we were there. It helps to figure out what is at the root of her problems.
When my mother started taking medication, she became very depressed: for example, she didn't like the city we live in because it had too many concrete buildings; she didn't like driving; she didn't like the food. I could tell her that she's crazy, that's why she perceives everything like that. But of course I didn't. I realized that anything can make her angry, so sometimes I just listened carefully to her and tried to calm her down, and sometimes I sincerely agreed with her. Then she understood that I was on her side. nine0005
Be angry not at your loved one, but at his illness
I got angry with my mother many times. When I was a teenager, and she still refused to take medicine, we often fought. Mom could just throw me out of the car in the city center, because we had a big fight and just couldn't be around.
When I realized her diagnosis, acceptance came to me. I learned to forgive not because I have to, but because I really wanted to . I realized that when she hurts me, it's not my mom, but her illness. But I'm sure that you can't just forgive and keep silent about it. When she hurt me, I always talked about how I feel. This helps to understand that the person hurts you not intentionally. nine0005
Learn to admit guilt and be responsible
It seems to me that psychologists who try to convince both parties that no one is to blame are wrong. A person who offended his relatives and children cannot be completely innocent. If he really believes that this is not his fault, he will not be able to realize that something is wrong with him.
I am against resentment, but I am for the realization of guilt . This applies to everyone, including those who struggle with mental illness. There is an episode in the film where my mother is talking to a psychologist and he is trying to help her think of herself as a small innocent child. But this is not so, she is not a child, she is an adult woman who has made mistakes. And the only way to overcome, to get over these mistakes is to admit them and take responsibility. nine0005
This also works the other way around: if I know I did something wrong with her, I will explain myself and apologize.
Sometimes you have to let a person vent their anger - and try not to take it to heart
It is important to understand that a person with a mental illness sometimes behaves asocially. It is very difficult to truly love someone who is experiencing such a state. Therefore, it seems to me that the best thing you can do is to ignore outbursts of anger. In the past, my mother has said so many horrible things to me that it's hard to imagine. If I took all this at face value, I would have already stopped communicating with her and left home forever. nine0005
Be more patient: it is difficult, but if you lose control of yourself at such moments, the situation can turn out to be deplorable . Give your loved one the opportunity to express their emotions without taking them to heart. And do not forget even at such moments to tell him how much you love him.
Sometimes it happens that you are the one who causes these outbreaks, because you spend a lot of time around a person, taking care of him. That was the case in my situation. Therefore, it is important to sometimes let your loved one be alone with you, to understand that he also needs personal space. nine0005
Share household chores and be understanding that your loved one might forget something
For a long time, none of us wanted to take responsibility for household chores: our house was filled with dirty dishes, laundry and garbage. It was terrible, but over time, my sister and I came to the conclusion that we should help my mother in many things. I learned how to take care of myself and others, cook, clean the house and keep everything clean and tidy. As is my sister.
Mom was never particularly good at household chores: she could forget that there was no food in the fridge, and we ate chocolate chip cookies all day long . And sometimes mom had so much energy that she could clean the whole house to perfect cleanliness. But, of course, most often these duties passed to me and my sister.
Find your favorite thing to do for the two of you - and appreciate the pleasant moments that you spent together0128 .
My mother is a very adventurous woman. One of my happiest childhood memories: my mother picked me up with my sister from school in the middle of the day and said that we were going skiing. It was a crazy adventure and we really appreciated the time spent together.
Try to find activities that your loved ones really enjoy and do them together as often as possible.
You will have many difficult moments in life, but you will experience them much easier if you remember the moments of joy. In addition, it helps to realize how much you love them. nine0005
Don't go through problems alone and discuss difficulties with other relatives
Talking to my sister and grandparents helped me a lot. We were all very close during the period when my mother started to get sick. I understand that not everyone has relatives to whom you can turn, but you need to find a person who can listen to you.
I would advise children to turn to adults - for example, to teachers at school. Because it's especially important for children to have someone they can trust completely so they can feel secure when their parents can't provide that protection. It is important that there is a person who will explain that their experiences are important, that all this is not easy. This is where support comes in. Of course, there are children who have to take all the burden of responsibility on themselves, because they have no one to turn to, and this is sad. nine0005
And most importantly. Do not forget about yourself - live
It is necessary to separate care for loved ones and care for yourself. These are two equally important things in your life . Always remember this.
I knew I had to do both. Therefore, when I became an adult, I sometimes went on business trips or trips, during which I tried to reflect on my life. Of course, I still worried, but when I didn’t have to take care of my mother, I had a lot of free time to focus on myself. nine0005
Now I got married, I have a child, and the responsibilities that came along with the appearance of a family are no less important than taking care of my mother.