Dissociative amnesia vs fugue
Dissociative Amnesia & Fugue - memory loss caused by trauma or stress
Dissociative Amnesia
Dissociative amnesia is the most common Dissociative Disorder. There are several different types of amnesia, and many different causes. Dissociative Amnesia is not caused by head injuries or physical damage to the brain, it is amnesia which has a psychological cause. It can occur as part of a number of other mental health conditions, including posttraumatic stress disorder and acute stress disorder, dissociative identity disorder, somatoform disorder, and anxiety disorders, [3]:298, [7] in any of those cases it would not be classed as a separate disorder. Dissociation Amnesia can last for between a few days to a few years, but is typically less than a week.[4] The period of time which cannot be remembered can range from minutes to decades.
Dissociative amnesia explained, the second part of the video involves a case caused by the suicide of a loved one.
The DSM-5 states that the key characteristic is "the inability to recall important autobiographical information that:
- should be successfully stored in memory and
- ordinarily would be readily remembered (Criteria A)."
Because there is no neurobiological damage or toxicity, and the difficulties are in retrieving a memory which was successfully stored, the amnesia is always "potentially reversible". [3]:298-299, [7] Neurocognitive disorders involving memory loss usually include cognitive (thinking) and intellectual impairments in memory, these are not present in people Dissociative Amnesia. [3]:300-301
Dissociative amnesia is more likely in people with a history of multiple adverse childhood experiences (especially if they include physical or sexual abuse), people who have experienced interpersonal violence (for example, domestic violence or physical assaults), and the risk increases with the "severity, frequency, and violence of the trauma".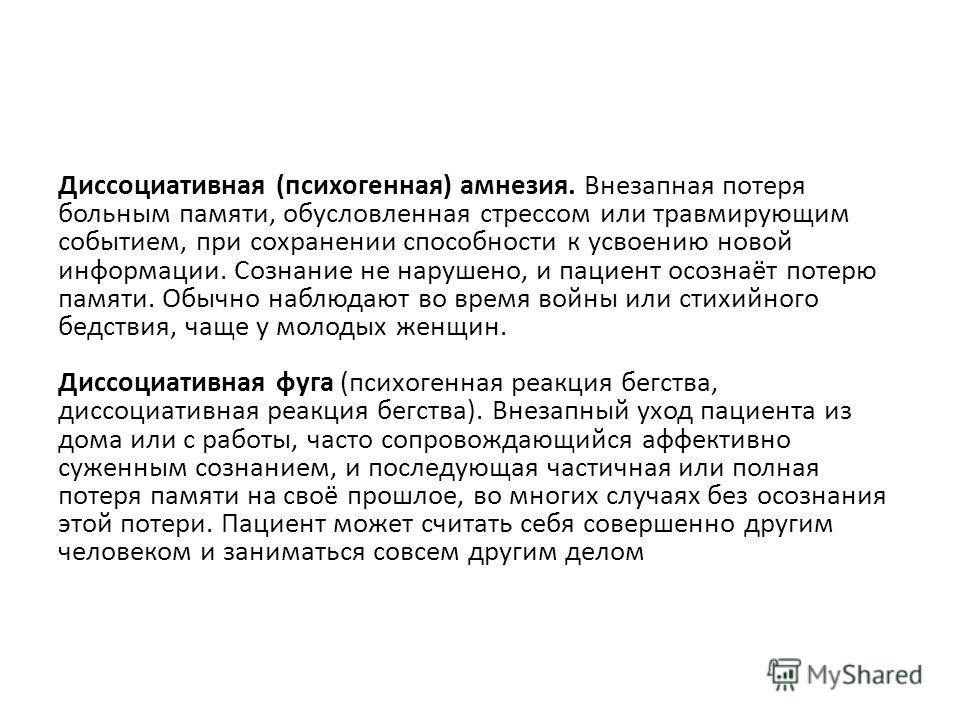 [3]:298-299 Clinical interviews to diagnose Dissociative Amnesia include the SCID-D (revised) by Dr Marlene Steinberg, and the Dissociative Disorders Interview Schedule (DDIS). Both of these are capable of diagnosing any dissociative disorder and a number of other disorders as well. [1]:124
[3]:298-299 Clinical interviews to diagnose Dissociative Amnesia include the SCID-D (revised) by Dr Marlene Steinberg, and the Dissociative Disorders Interview Schedule (DDIS). Both of these are capable of diagnosing any dissociative disorder and a number of other disorders as well. [1]:124
Types of Dissociative Amnesia
The three common types of dissociative amnesia are localized amnesia, selective amnesia (which may occur along with localized amnesia), and generalized amnesia. Generalized amnesia may involve the complete loss of a person's identity, in addition to all memories of their past.
Other forms of dissociative amnesia can also occur; people with generalized amnesia (the most severe type) may also lose semantic knowledge (previous knowledge about the world) and procedural knowledge (forgetting well-learned skills). [3]:298-299 Systematized amnesia is amnesia for a category of information (e.g., no memory of family, no memory of a specific person, or childhood sexual abuse).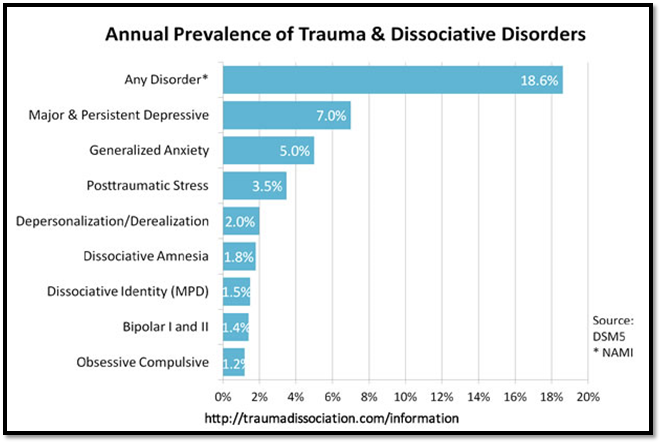 Continuous amnesia is unable to form new memories. [3]:298-299 Micro-amnesias are also typical in dissociative disorders, the amnesia is for very, very brief periods of time. The International Society for the Study of Trauma and Dissociation gives the example of forgetting the contents of a conversation from one moment to the next. The person may struggle to work out what was discussed while trying to avoid the other person realizing this. [7]
Continuous amnesia is unable to form new memories. [3]:298-299 Micro-amnesias are also typical in dissociative disorders, the amnesia is for very, very brief periods of time. The International Society for the Study of Trauma and Dissociation gives the example of forgetting the contents of a conversation from one moment to the next. The person may struggle to work out what was discussed while trying to avoid the other person realizing this. [7]
Dissociative Amnesia has been previously known as Psychogenic Amnesia, and Hysterical Amnesia.
DSM-5 Diagnostic Criteria for Dissociative Amnesia
The newly released guide to diagnosing mental disorders is the DSM-5, released in 2013.[3] gives the following diagnostic criteria:
Code 300.12
- "A. An inability to recall important autobiographic information, usually of a traumatic or stressful nature, that is inconsistent with ordinary forgetting.
Note: Dissociative Amnesia most often consists of localized or selective amnesia for a specific event or events; or generalized amnesia for identity and life history.
- B. The symptoms cause clinically significant distress or impairment in social, occupational, or other important areas of functioning.
- C. The disturbance is not attributable to the physiological effects of a substance (e.g., alcohol or other drug abuse, a medication) or a neurological or other medical condition (e.g., partial complex seizures, transient global amnesia, sequelae of a closed head injury/traumatic brain injury, other neurological condition).
- D. The disturbance is not better explained by dissociative identity disorder, posttraumatic stress disorder, acute stress disorder, somatic symptom disorder, or major or mild neurocognitive disorder." [1], [3]:298
Specify if:
Code 300.13
"With dissociative fugue: Apparently purposeful travel or bewildered wandering that is associated with amnesia for identity or other important autobiographical information."
Dissociative Fugue
org/MedicalCondition">During a Dissociative Amnesia with Fugue, a person normally acts in a way which is purposeful and has a specific goal; fugue states may last for days, weeks, or longer. A fugue occurs when there is sudden and unexpected travel away from home or work in combination with amnesia for a person's past, and either identity confusion or assumption of a new identity. [3]:301, [7] Dissociative Fugue is also known as Psychogenic Fugue,[7] and was previously a separate diagnosis, but is combined with Dissociative Amnesia in the DSM-5.
An experience of Dissociative Fugue
People experiencing a fugue appear normal to others, and are often unaware of their amnesia. [7] It can be distinguished from amnesia and the aimless wandering sometimes present during seizures using tests such as EEGs to establish if there is a relationship between seizure activity and the amnesia. [3]:301
[3]:301
ICD Diagnostic Criteria
The last edition of the International Classification of Diseases, the diagnostic guide published by the World Health Organization is the ICD-10, published in 1992 with minor updates since. [2] Dissociative Amnesia and Dissociative Fugue are separate diagnoses within the ICD manual. The draft ICD-11 criteria gives these descriptions:
ICD 11 draft - Dissociative Amnesia
Code 7B33
"Dissociative amnesia is characterized by an inability to recall important autobiographical memories, where recall would be expected and is inconsistent with ordinary forgetting. The extent of amnesia varies, but most commonly involves memories of recent traumatic or stressful events. There is no evidence that the symptoms are due to the direct effects of a substance or medication, including withdrawal, to exhaustion, to head trauma, or to a neurological condition (e.g., temporal lobe epilepsy). The symptoms are not better explained by another mental and behavioural disorder or by a sleep-wake disorder.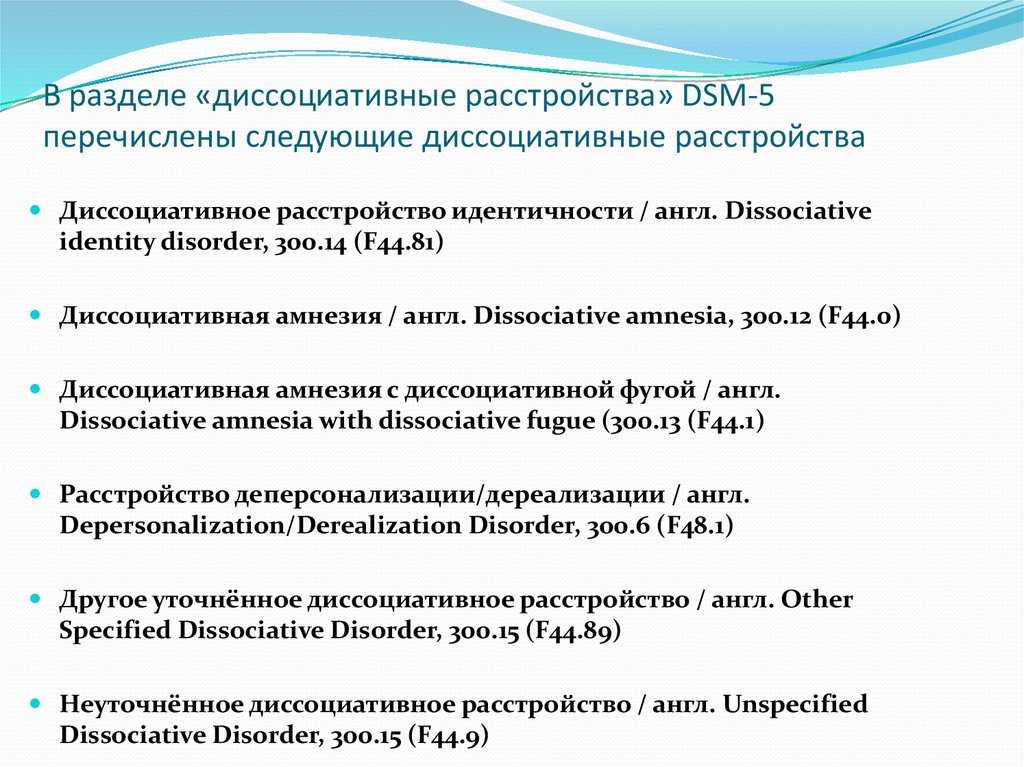 The symptoms are sufficiently severe to cause significant distress or impairment in personal, family, social, educational, occupational or other important areas of functioning."
The symptoms are sufficiently severe to cause significant distress or impairment in personal, family, social, educational, occupational or other important areas of functioning."
Also known as "amnesia neurosis" or "psychogenic amnesia".[6]
Exclude.:
Amnesia not otherwise specified, anterograde amnesia, amnestic disorder due to alcohol use, anterograde amnesia, retrograde amnesia, nonalcoholic organic amnesic syndrome, postictal amnesia in epilepsy [and amnestic disorder due to use of other specified psychoactive substance.[6] Last updated May 2016.
ICD 11 draft - Dissociative Fugue
Code 7B33.1
"Dissociative amnesia with dissociative fugue
Dissociative amnesia with dissociative fugue is characterized by all of the features of dissociative amnesia, together with sudden, apparently purposeful, travel away from home, work, or significant others for an extended period of time (days or weeks), or with bewildered wandering.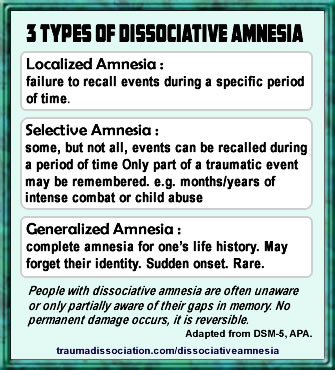 The amnesia is typically associated with confusion about one's identity, and presentation of a new identity may occur."
The amnesia is typically associated with confusion about one's identity, and presentation of a new identity may occur."
Alternate names: dissociative fugue and hysterical fugue. [6]
Exclude: postictal fugue in epilepsy. [6] Last updated May 2016.
Differences between the ICD-10 and Draft ICD-11
Dissociative amnesia now clearly excludes amnesia caused by head injury (commonly known as Traumatic Brain Injury), and refers to stressful events rather than only traumatic events as a likely cause. Dissociative Fugue now states that it must last at least a few days, and include either identity confusion or identity alteration. [5,6]
Also important is the fact that the group these disorders are part of has been renamed from Dissociative [Conversion] Disorders to just Dissociative Disorders. Descriptions may be changed when the final ICD-11 is published.
Dissociative Amnesia in the ICD-10
Code F44. 0
0
"The main feature is loss of memory, usually of important recent events, that is not due to organic mental disorder, and is too great to be explained by ordinary forgetfulness or fatigue. The amnesia is usually centered on traumatic events, such as accidents or unexpected bereavements, and is usually partial and selective. Complete and generalized amnesia is rare, and is usually part of a fugue (F44.1). If this is the case, the disorder should be classified as such. The diagnosis should not be made in the presence of organic brain disorders, intoxication, or excessive fatigue." [5] Exclude.: alcohol- or other psychoactive substance-induced amnesic disorder, amnesia not otherwise specified, anterograde amnesia, retrograde amnesia, nonalcoholic organic amnesic syndrome, postictal amnesia in epilepsy [5]
Dissociative Fugue in the ICD-10
Code F44.1
"Dissociative fugue has all the features of dissociative amnesia, plus purposeful travel beyond the usual everyday range.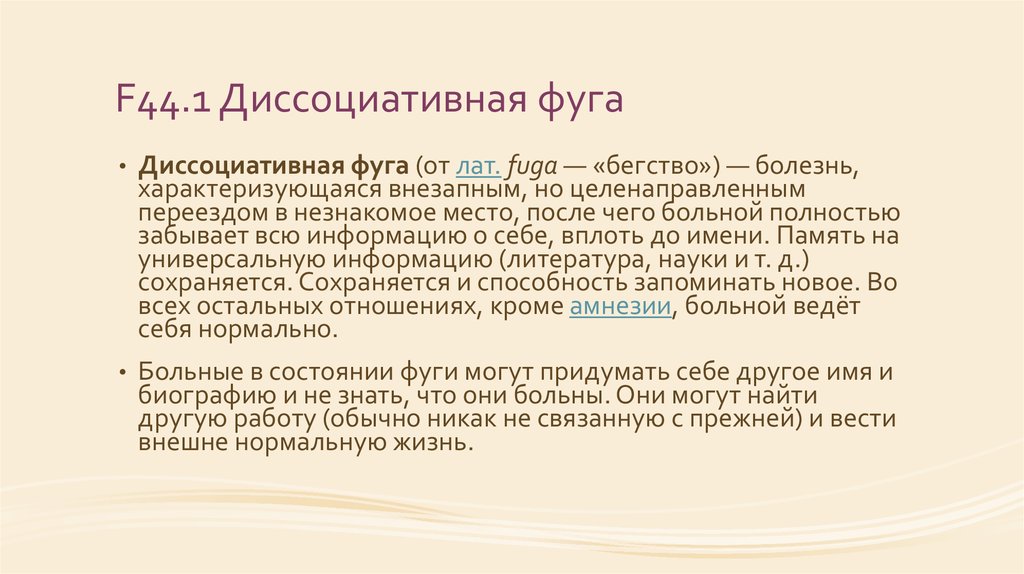 Although there is amnesia for the period of the fugue, the patient's behaviour during this time may appear completely normal to independent observers." [5]
Although there is amnesia for the period of the fugue, the patient's behaviour during this time may appear completely normal to independent observers." [5]
Excludes postictal fugue in epilepsy. [5]
Treatment
Note: this guidance only applies to dissociative amnesia which is without the presence of other disorders. If posttraumatic stress disorder or dissociative identity disorder are present, for example, the treatment guidelines for those conditions should be followed instead, for example the dissociative amnesia within Dissociative Identity Disorder is not a suggested method of diagnosis and medication is not the primary treatment method. [7]
Most cases of Dissociative Amnesia last less than a week.[4] Severe cases (acute amnesia) are treated by providing a safe environment, free of threatening stimuli, which may be enough for memories to return. Medication may also be used during interviewing. When memories return psychotherapy should be used to identify and discuss events that triggered the Dissociative Amnesia, and to explore effective coping mechanisms.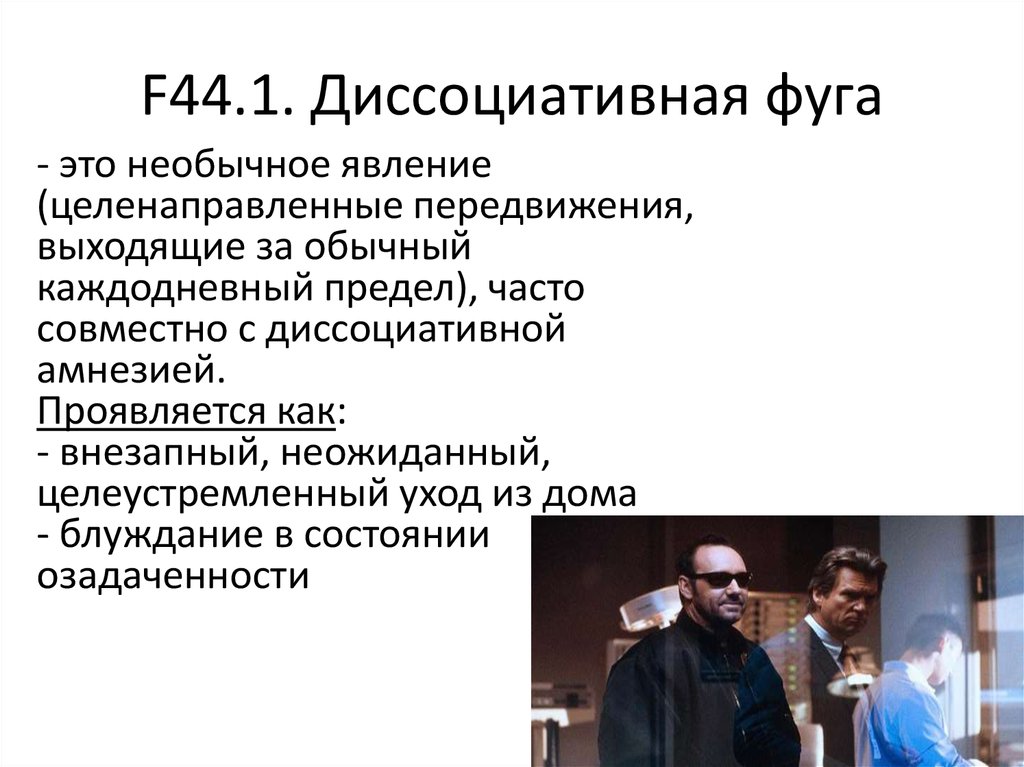 [7] Chronic amnesia refers to longer term amnesia; long-term psychotherapy is the recommended treatment, and medication to address the amnesia is not recommended. Psychotherapy should aim to help process and integrate the traumatic and dissociated material. Hypnosis may be ease the process of working through trauma. [7]
[7] Chronic amnesia refers to longer term amnesia; long-term psychotherapy is the recommended treatment, and medication to address the amnesia is not recommended. Psychotherapy should aim to help process and integrate the traumatic and dissociated material. Hypnosis may be ease the process of working through trauma. [7]
Dissociative amnesia occurring with fugue should be treated as soon as possible; psychotherapy is the recommended treatment. This should involve a safe environment for therapy and a strong therapeutic alliance. Treatment goals include the recovery of the person's identity, identifying the triggers linked to the start of the fugue, and working through the traumatic material. Medication given during interviews, and hypnosis may be also help.[7] Recovery is often rapid. [8] When memories begin to return a person often experiences emotions such as grief, rage, shame, guilt, depression and inner turmoil. Many people with Dissociative Amnesia develop Posttraumatic Stress Disorder at some point in their lives. [3]:302
[3]:302
References
Dissociative Amnesia & Fugue - memory loss caused by trauma or stress
Dissociative Amnesia
Dissociative amnesia is the most common Dissociative Disorder. There are several different types of amnesia, and many different causes. Dissociative Amnesia is not caused by head injuries or physical damage to the brain, it is amnesia which has a psychological cause. It can occur as part of a number of other mental health conditions, including posttraumatic stress disorder and acute stress disorder, dissociative identity disorder, somatoform disorder, and anxiety disorders, [3]:298, [7] in any of those cases it would not be classed as a separate disorder. Dissociation Amnesia can last for between a few days to a few years, but is typically less than a week.[4] The period of time which cannot be remembered can range from minutes to decades.
Dissociative amnesia explained, the second part of the video involves a case caused by the suicide of a loved one.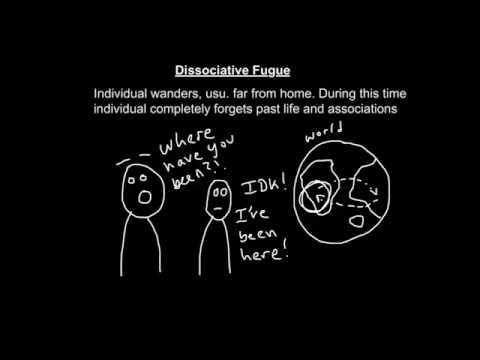
The DSM-5 states that the key characteristic is "the inability to recall important autobiographical information that:
- should be successfully stored in memory and
- ordinarily would be readily remembered (Criteria A)."
Because there is no neurobiological damage or toxicity, and the difficulties are in retrieving a memory which was successfully stored, the amnesia is always "potentially reversible". [3]:298-299, [7] Neurocognitive disorders involving memory loss usually include cognitive (thinking) and intellectual impairments in memory, these are not present in people Dissociative Amnesia. [3]:300-301
Dissociative amnesia is more likely in people with a history of multiple adverse childhood experiences (especially if they include physical or sexual abuse), people who have experienced interpersonal violence (for example, domestic violence or physical assaults), and the risk increases with the "severity, frequency, and violence of the trauma". [3]:298-299 Clinical interviews to diagnose Dissociative Amnesia include the SCID-D (revised) by Dr Marlene Steinberg, and the Dissociative Disorders Interview Schedule (DDIS). Both of these are capable of diagnosing any dissociative disorder and a number of other disorders as well. [1]:124
[3]:298-299 Clinical interviews to diagnose Dissociative Amnesia include the SCID-D (revised) by Dr Marlene Steinberg, and the Dissociative Disorders Interview Schedule (DDIS). Both of these are capable of diagnosing any dissociative disorder and a number of other disorders as well. [1]:124
Types of Dissociative Amnesia
The three common types of dissociative amnesia are localized amnesia, selective amnesia (which may occur along with localized amnesia), and generalized amnesia. Generalized amnesia may involve the complete loss of a person's identity, in addition to all memories of their past.
Other forms of dissociative amnesia can also occur; people with generalized amnesia (the most severe type) may also lose semantic knowledge (previous knowledge about the world) and procedural knowledge (forgetting well-learned skills). [3]:298-299 Systematized amnesia is amnesia for a category of information (e.g., no memory of family, no memory of a specific person, or childhood sexual abuse). Continuous amnesia is unable to form new memories. [3]:298-299 Micro-amnesias are also typical in dissociative disorders, the amnesia is for very, very brief periods of time. The International Society for the Study of Trauma and Dissociation gives the example of forgetting the contents of a conversation from one moment to the next. The person may struggle to work out what was discussed while trying to avoid the other person realizing this. [7]
Continuous amnesia is unable to form new memories. [3]:298-299 Micro-amnesias are also typical in dissociative disorders, the amnesia is for very, very brief periods of time. The International Society for the Study of Trauma and Dissociation gives the example of forgetting the contents of a conversation from one moment to the next. The person may struggle to work out what was discussed while trying to avoid the other person realizing this. [7]
Dissociative Amnesia has been previously known as Psychogenic Amnesia, and Hysterical Amnesia.
DSM-5 Diagnostic Criteria for Dissociative Amnesia
The newly released guide to diagnosing mental disorders is the DSM-5, released in 2013.[3] gives the following diagnostic criteria:
Code 300.12
- "A. An inability to recall important autobiographic information, usually of a traumatic or stressful nature, that is inconsistent with ordinary forgetting.
Note: Dissociative Amnesia most often consists of localized or selective amnesia for a specific event or events; or generalized amnesia for identity and life history.
- B. The symptoms cause clinically significant distress or impairment in social, occupational, or other important areas of functioning.
- C. The disturbance is not attributable to the physiological effects of a substance (e.g., alcohol or other drug abuse, a medication) or a neurological or other medical condition (e.g., partial complex seizures, transient global amnesia, sequelae of a closed head injury/traumatic brain injury, other neurological condition).
- D. The disturbance is not better explained by dissociative identity disorder, posttraumatic stress disorder, acute stress disorder, somatic symptom disorder, or major or mild neurocognitive disorder." [1], [3]:298
Specify if:
Code 300.13
"With dissociative fugue: Apparently purposeful travel or bewildered wandering that is associated with amnesia for identity or other important autobiographical information."
Dissociative Fugue
During a Dissociative Amnesia with Fugue, a person normally acts in a way which is purposeful and has a specific goal; fugue states may last for days, weeks, or longer. A fugue occurs when there is sudden and unexpected travel away from home or work in combination with amnesia for a person's past, and either identity confusion or assumption of a new identity. [3]:301, [7] Dissociative Fugue is also known as Psychogenic Fugue,[7] and was previously a separate diagnosis, but is combined with Dissociative Amnesia in the DSM-5.
An experience of Dissociative Fugue
People experiencing a fugue appear normal to others, and are often unaware of their amnesia. [7] It can be distinguished from amnesia and the aimless wandering sometimes present during seizures using tests such as EEGs to establish if there is a relationship between seizure activity and the amnesia. [3]:301
[3]:301
ICD Diagnostic Criteria
The last edition of the International Classification of Diseases, the diagnostic guide published by the World Health Organization is the ICD-10, published in 1992 with minor updates since. [2] Dissociative Amnesia and Dissociative Fugue are separate diagnoses within the ICD manual. The draft ICD-11 criteria gives these descriptions:
ICD 11 draft - Dissociative Amnesia
Code 7B33
"Dissociative amnesia is characterized by an inability to recall important autobiographical memories, where recall would be expected and is inconsistent with ordinary forgetting. The extent of amnesia varies, but most commonly involves memories of recent traumatic or stressful events. There is no evidence that the symptoms are due to the direct effects of a substance or medication, including withdrawal, to exhaustion, to head trauma, or to a neurological condition (e.g., temporal lobe epilepsy). The symptoms are not better explained by another mental and behavioural disorder or by a sleep-wake disorder. The symptoms are sufficiently severe to cause significant distress or impairment in personal, family, social, educational, occupational or other important areas of functioning."
The symptoms are sufficiently severe to cause significant distress or impairment in personal, family, social, educational, occupational or other important areas of functioning."
Also known as "amnesia neurosis" or "psychogenic amnesia".[6]
Exclude.:
Amnesia not otherwise specified, anterograde amnesia, amnestic disorder due to alcohol use, anterograde amnesia, retrograde amnesia, nonalcoholic organic amnesic syndrome, postictal amnesia in epilepsy [and amnestic disorder due to use of other specified psychoactive substance.[6] Last updated May 2016.
ICD 11 draft - Dissociative Fugue
Code 7B33.1
"Dissociative amnesia with dissociative fugue
Dissociative amnesia with dissociative fugue is characterized by all of the features of dissociative amnesia, together with sudden, apparently purposeful, travel away from home, work, or significant others for an extended period of time (days or weeks), or with bewildered wandering. The amnesia is typically associated with confusion about one's identity, and presentation of a new identity may occur."
The amnesia is typically associated with confusion about one's identity, and presentation of a new identity may occur."
Alternate names: dissociative fugue and hysterical fugue. [6]
Exclude: postictal fugue in epilepsy. [6] Last updated May 2016.
Differences between the ICD-10 and Draft ICD-11
Dissociative amnesia now clearly excludes amnesia caused by head injury (commonly known as Traumatic Brain Injury), and refers to stressful events rather than only traumatic events as a likely cause. Dissociative Fugue now states that it must last at least a few days, and include either identity confusion or identity alteration. [5,6]
Also important is the fact that the group these disorders are part of has been renamed from Dissociative [Conversion] Disorders to just Dissociative Disorders. Descriptions may be changed when the final ICD-11 is published.
Dissociative Amnesia in the ICD-10
Code F44. 0
0
"The main feature is loss of memory, usually of important recent events, that is not due to organic mental disorder, and is too great to be explained by ordinary forgetfulness or fatigue. The amnesia is usually centered on traumatic events, such as accidents or unexpected bereavements, and is usually partial and selective. Complete and generalized amnesia is rare, and is usually part of a fugue (F44.1). If this is the case, the disorder should be classified as such. The diagnosis should not be made in the presence of organic brain disorders, intoxication, or excessive fatigue." [5] Exclude.: alcohol- or other psychoactive substance-induced amnesic disorder, amnesia not otherwise specified, anterograde amnesia, retrograde amnesia, nonalcoholic organic amnesic syndrome, postictal amnesia in epilepsy [5]
Dissociative Fugue in the ICD-10
Code F44.1
"Dissociative fugue has all the features of dissociative amnesia, plus purposeful travel beyond the usual everyday range.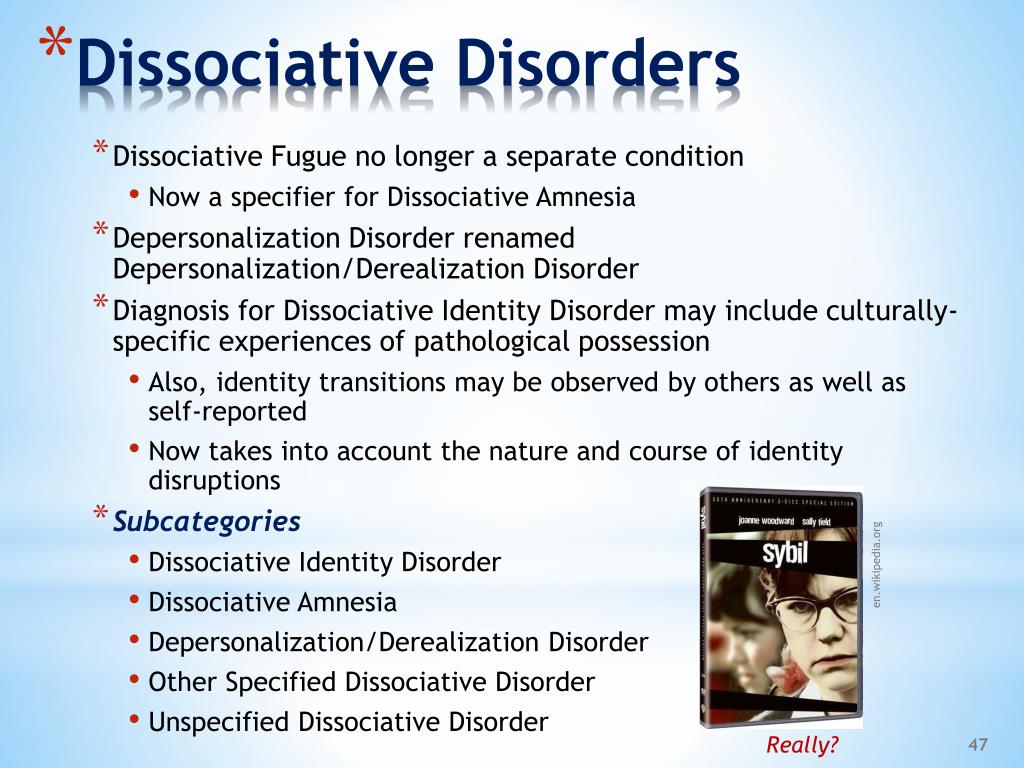 Although there is amnesia for the period of the fugue, the patient's behaviour during this time may appear completely normal to independent observers." [5]
Although there is amnesia for the period of the fugue, the patient's behaviour during this time may appear completely normal to independent observers." [5]
Excludes postictal fugue in epilepsy. [5]
Treatment
Note: this guidance only applies to dissociative amnesia which is without the presence of other disorders. If posttraumatic stress disorder or dissociative identity disorder are present, for example, the treatment guidelines for those conditions should be followed instead, for example the dissociative amnesia within Dissociative Identity Disorder is not a suggested method of diagnosis and medication is not the primary treatment method. [7]
Most cases of Dissociative Amnesia last less than a week.[4] Severe cases (acute amnesia) are treated by providing a safe environment, free of threatening stimuli, which may be enough for memories to return. Medication may also be used during interviewing. When memories return psychotherapy should be used to identify and discuss events that triggered the Dissociative Amnesia, and to explore effective coping mechanisms. [7] Chronic amnesia refers to longer term amnesia; long-term psychotherapy is the recommended treatment, and medication to address the amnesia is not recommended. Psychotherapy should aim to help process and integrate the traumatic and dissociated material. Hypnosis may be ease the process of working through trauma. [7]
[7] Chronic amnesia refers to longer term amnesia; long-term psychotherapy is the recommended treatment, and medication to address the amnesia is not recommended. Psychotherapy should aim to help process and integrate the traumatic and dissociated material. Hypnosis may be ease the process of working through trauma. [7]
Dissociative amnesia occurring with fugue should be treated as soon as possible; psychotherapy is the recommended treatment. This should involve a safe environment for therapy and a strong therapeutic alliance. Treatment goals include the recovery of the person's identity, identifying the triggers linked to the start of the fugue, and working through the traumatic material. Medication given during interviews, and hypnosis may be also help.[7] Recovery is often rapid. [8] When memories begin to return a person often experiences emotions such as grief, rage, shame, guilt, depression and inner turmoil. Many people with Dissociative Amnesia develop Posttraumatic Stress Disorder at some point in their lives. [3]:302
[3]:302
References
Dissociative Fugue
8.05.2012
Prevalence . Obtaining data on the epidemiology of dissociative fugue is difficult because the differentiation between dissociative amnesia, dissociative fugue and multiple personality disorder began to be carried out only relatively recently, previously all these disorders were considered in a single complex. It is assumed that psychogenic fugues are most often encountered in wartime, as a result of a natural disaster, or as a result of a crisis that accompanies intense internal personal conflict.
Causes . Predisposing factors are severe alcohol abuse, the presence of an emotionally unstable, hysterical or schizoid personality type, as well as concomitant affective pathology. It is based on a psychological factor associated with the desire to get away from painfully perceived circumstances. The etiopathogenetic mechanism is close to that described for dissociative amnesia. In addition to catastrophic circumstances, the fugue occurs in the context of everyday psychosocial stress (insult, emotionally significant loss, failure, family conflict, financial problems).
The etiopathogenetic mechanism is close to that described for dissociative amnesia. In addition to catastrophic circumstances, the fugue occurs in the context of everyday psychosocial stress (insult, emotionally significant loss, failure, family conflict, financial problems).
Clinic . A dissociative fugue is characterized by an unexpected trip or even travel in a state consistent with dissociative amnesia. Unlike psychogenic amnesia, the patient during a fugue episode is not aware of memory impairment and does not appear outwardly disoriented. The "new" personality in which he appears is usually different from his own, its features may be richly detailed or pale and fragmented. Behavior during the fugue does not outwardly indicate an intention to react to some specific psycho-traumatic experience. The patient may introduce himself by a new name, engage in a different profession, and engage in complex social interactions, but usually he does nothing that draws special attention to himself. In rare cases, outbursts of aggressiveness are possible, at the beginning of the episode - a short-term phase of obnubilation of consciousness.
In rare cases, outbursts of aggressiveness are possible, at the beginning of the episode - a short-term phase of obnubilation of consciousness.
The duration of the dissociative fugue is usually several hours/days. Rare cases can be delayed for several months, during which sometimes the patient manages to travel thousands of kilometers. The end of the episode, like the beginning, occurs suddenly, often at the exit from a night's sleep. The return to the memory of the circumstances preceding the episode is accompanied by a partial or complete forgetting of what happened during the fugue. Relapses are considered rare, but these patients have a high comorbidity with other dissociative disorders. An independent problem may be presented by the consequences of behavior during the episode.
Diagnosis . To diagnose the state of dissociative fugue, in addition to the signs common to dissociative disorders (F44), the following criteria must be met:
- an unexpected trip was taken away from the usual social environment, outwardly normally organized, with self-service generally preserved throughout the episode;
- partial or complete amnesia of the episode, corresponding to feature 2 of dissociative amnesia.
Differential diagnosis . In fugues against the background of organic brain disorders, behavior is usually not caused by a stress factor and is not as complex and socially adaptive as in psychogenic fugues. The same applies to fugues in temporal epilepsy, where, in addition, the orientation of the patient in his own personality is preserved and there are indications of paroxysmal disorders. Differentiation from simulative behavior is given under the heading of dissociative amnesia.
Treatment . Contact with a patient during a fugue episode is a clinical rarity. It usually comes to the attention of the psychiatrist at the end of the fugue. Therapy is similar to that for dissociative amnesia. It should also be established whether the patient's unconscious personality mechanisms that determine his behavior during the fugue are preserved and whether this "other" personality can be accessed by the methods used in the treatment of multiple personality disorder.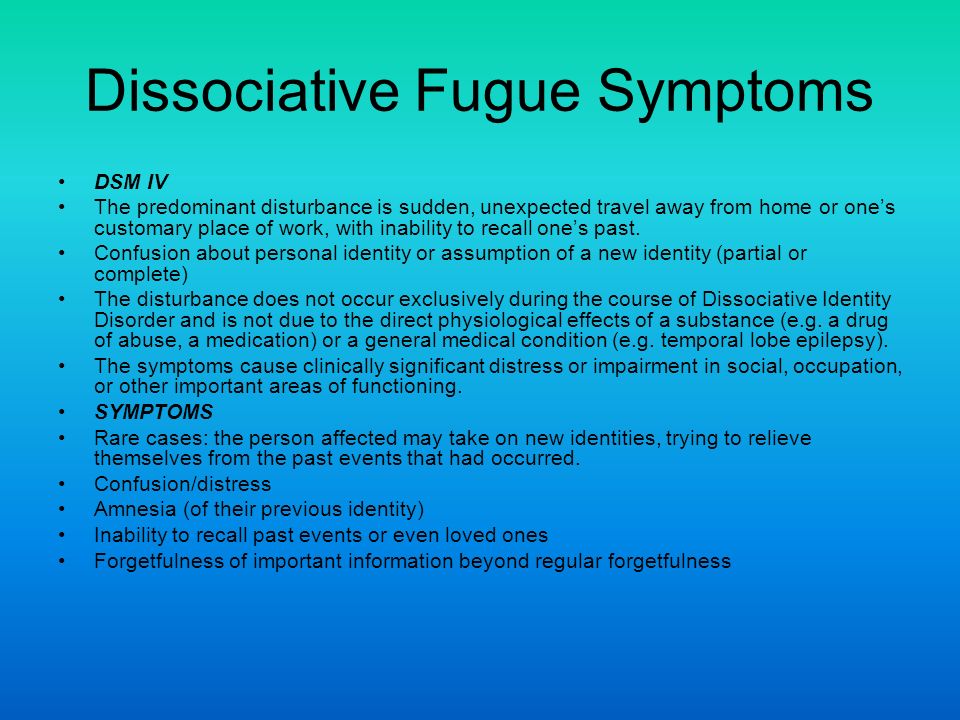 In general, one should not dwell in detail on the patient's awareness of the circumstances of an episode of dissociative fugue. It is important to equip him with effective skills to cope with stressful situations that cause frustration.
In general, one should not dwell in detail on the patient's awareness of the circumstances of an episode of dissociative fugue. It is important to equip him with effective skills to cope with stressful situations that cause frustration.
Key words: Dissociative
Source: Popov Yu.V., Vid V.D. Modern Clinical Psychiatry
| Related materials |
|---|
| Dissocial personality disorder Popov Yu.V., Vid V.D. Modern clinical psychiatry |
| Dissociative (conversion) disorders, case history Popov Yu.V., Vid V.D. Modern clinical psychiatry |
| Dissociative amnesia Popov Yu.V., Vid V.D. Modern clinical psychiatry |
Bereavement and Grief, Part 5 - Phoenix Center
Can a single visit to a psychiatrist be guaranteed to get rid of the devastating effects of grief?
No, because depressive symptoms tend to change in dynamics, and therefore a constant reassessment of the patient's mental state is required and adjustment of treatment and prescriptions is necessary.
For example, people (relatives) caring for dying patients develop hypochondriacal disorders over time: there is a conviction that they develop a serious illness (most often the same as that of the deceased - cancer, ulcerative colitis, kidney failure, disease Alzheimer's, etc.).
What mental disorders most often occur after loss?
Dissociative (conversion) disorders , which are expressed in the absence of conscious control over memory and sensations, on the one hand, and control of body movements, on the other. Psychogenic factors play a leading role in the origin, there is almost always a close connection in time with traumatic life circumstances, insoluble and unbearable events or broken relationships.
Dissociative amnesia - loss of memory (usually partial, rarely complete) for recent important events of a traumatic nature and is accompanied by confusion. The destruction of consciousness by a bereaved person is a way of dealing with emotional conflict or external stress.
Dissociative fugue (also a kind of deliverance from emotionally painful experiences) manifests itself in outwardly purposeful actions, travel, often for several days, combined with the phenomena of dissociative amnesia. Outwardly, the behavior appears to be perfectly normal. In some cases, the formation of a new personality is noted. The fugue period is amnesic.
Dissociative stupor proceeds with complete immobility, mutism and weakened reactions to irritation.
Dissociative motor disorders are manifested by complete or partial paralysis of the limbs (mono-, hemi- and para-paresis and plegia), ataxia, astasia-abasia, apraxia, akinesia, aphonia, dysarthria, blepharospasm. Assessment of the mental state of a patient with dissociative motor disorders suggests that the decline in productivity resulting from the loss of function helps him avoid unpleasant conflict or indirectly express his dependence or resentment. An important factor is the behavior aimed at attracting attention.
An important factor is the behavior aimed at attracting attention.
Dissociative convulsions. The duration of the convulsive syndrome is from several minutes to 2-3 hours. The demonstrative nature emphasizes what happens in the presence of outsiders and disappears when they lose interest in the patient. Abortive forms are more common - fainting, tears or laughter, tremor of the whole body with external signs of loss of consciousness without its actual loss. In childhood, seizures can occur as a protest reaction when adults refuse to comply with the child's demands.
Dissociative anesthesia or loss of sensory perception is a sensory disorder of psychogenic origin, which is characterized by a violation of one of the types of sensitivity, but is not based on objectively recorded lesions of the nervous system. Sensory dissociative disorders include hyperesthesia, paresthesia, anesthesia, blindness, deafness, and tunnel vision. Loss of vision in dissociative disorders is rarely total, and when it is disturbed, it is more often a loss of visual acuity, its general ambiguity, or a “narrowing of the field of visual perception”. Despite complaints of vision loss, the patient often has good general mobility and motor productivity. Much less common than loss of sensation or vision are dissociative deafness and anosmia.
Despite complaints of vision loss, the patient often has good general mobility and motor productivity. Much less common than loss of sensation or vision are dissociative deafness and anosmia.
In post-traumatic stress disorder (PTSD), the formative factor is the situation of an unexpected loss of an object of special affection or a significant other. The formation of PTSD occurs in the first 6 months after a traumatic event and lasts from 6 months to several years or more. These states differ in the following features: 1) they form in several stages, acquiring a prolonged course; 2) are determined by a polymorphic psychopathological structure; 3) in 6–20% of cases, they end with persistent residual conditions with phenomena of social maladaptation.
Thus, the development of psychopathological symptoms in complicated grief reaction requires dynamic monitoring, periodic retraining of the condition and changes in the treatment strategy, which can and should be carried out by a qualified psychiatrist.