Disease where you pull your hair out
Trichotillomania (hair pulling disorder) - NHS
Trichotillomania, also known as trich, is when someone cannot resist the urge to pull out their hair.
They may pull out the hair on their head or in other places, such as their eyebrows or eyelashes.
Trich is more common in teenagers and young adults.
Symptoms of trichotillomania
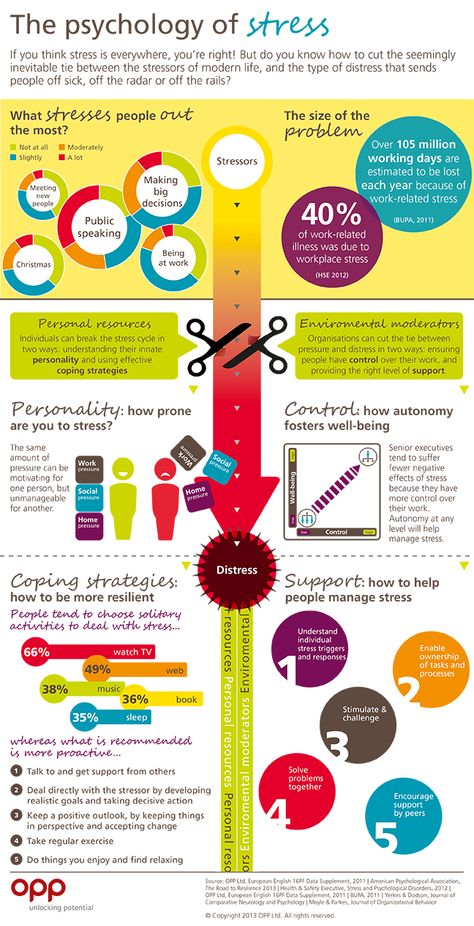
People with trich feel an intense urge to pull their hair out and they experience growing tension until they do. After pulling their hair out, they feel a sense of relief.
A person may sometimes pull their hair out in response to a stressful situation, or it may be done without really thinking about it.
Most people with trich pull out hair from their scalp, but some pull out hair from other areas, such as their:
- eyebrows
- eyelashes
- genital area
- beard or moustache
Bald patches on the head may have an unusual shape and affect 1 side of the head more than the other.
Trich may cause feelings of shame and low self-esteem. Those affected may try to keep their condition to themselves.
Causes of trichotillomania
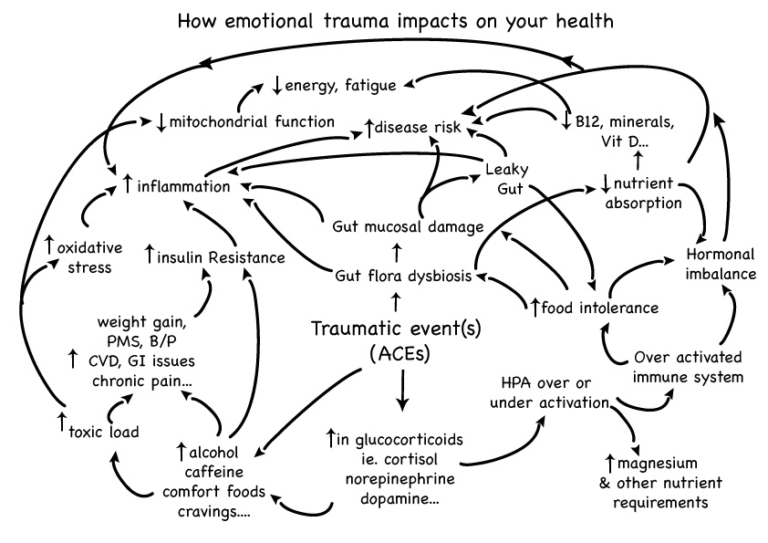
It's not entirely clear what causes trich. It could be:
- your way of dealing with stress or anxiety
- a chemical imbalance in the brain, similar to obsessive compulsive disorder (OCD)
- changes in hormone levels during puberty
For some people, hair pulling can be a type of addiction. The more they pull their hair out, the more they want to keep doing it.
When to see a GP
See your GP if you're pulling your hair out or if you notice that your child is.
You should also see your GP if you or your child has a habit of eating hair. This can cause hairballs to form in the stomach, leading to serious illness.
This can cause hairballs to form in the stomach, leading to serious illness.
Your GP may examine areas where the hair is missing to check that nothing else is causing the hair to come out, such as a skin infection.
If your GP thinks you have trich, you may be referred for a type of treatment called cognitive behavioural therapy (CBT).
Treating trichotillomania
Trich is commonly treated using a type of CBT called habit reversal training.
This aims to help you replace a bad habit with something that's not harmful. Treatment usually involves:
- keeping a diary of your hair pulling
- working out the triggers for your hair pulling and learning how to avoid them
- replacing hair pulling with another action, like squeezing a stress ball
- loved ones providing emotional support and encouragement
Antidepressants are not are not usually prescribed to treat trich.
Things you can try yourself
Here are some tips from people with trich that may help when you feel the urge to pull your hair:
- squeeze a stress ball or something similar
- form a ball with your fist and tighten the muscles in that arm
- use a fidget toy
- wear a bandana or a tight fitting hat, such as a beanie
- come up with a saying that you repeat out loud until the urge to pull passes
- take a soothing bath to ease any stress or anxiety
- practise deep breathing until the urge to pull goes away
- exercise
- put plasters on your fingertips
- cut your hair short
Getting support
It may also help to open up about your trich to people you trust, as hiding it can sometimes make your anxiety worse.
Many people who have learned to manage their trich say that speaking to others about the condition led to a reduction in hair pulling.
The charity Trichotillomania Support has information on treatments and self-help advice.
Page last reviewed: 29 January 2021
Next review due: 29 January 2024
What It Is, Causes & Treatment
Overview
Missing patches of hair are a possible sign of trichotillomania.What is trichotillomania?
Trichotillomania (often abbreviated as TTM) is a mental health disorder where a person compulsively pulls out or breaks their own hair. This condition falls under the classification of obsessive-compulsive disorder (OCD). When it’s severe, it often has extremely negative effects on a person’s happiness, well-being and overall quality of life.
Trichotillomania (pronounced trick-oh-till-oh-main-ee-uh) comes from three Greek words:
- Tricho: hair.

- Tillo: pull.
- Mania: excessive behavior or activity.
What is the difference between trichotillomania and obsessive-compulsive disorder?
TTM falls under the overall category of obsessive-compulsive disorder, but it has some key differences from OCD itself.
- Obsessions. OCD involves obsessions, which are thoughts or urges that a person can’t control and doesn’t want. TTM doesn’t involve obsessions.
- Feeling of reward. When people with TTM pull out their hair, they often feel relief or other positive emotions. OCD doesn’t involve positive feelings in that way.
Who does it affect?
TTM is especially common in children and adolescents. In young children and infants, it’s usually a short-lived concern and goes away on its own. The more serious form most commonly starts between ages 10 and 13.
In children, it happens equally between men and women. In adults, women outnumber men with this condition by as much as 9 to 1.
How common is this condition?
TTM is relatively uncommon. Research studies estimate it affects 0.5% to 3.4% of adults at some point in their lifetime.
How does this condition affect my body?
People with TTM compulsively pull out their hair, usually one strand at a time. Many people will pull hair from the same spot. The most common places people pull hair from are their scalp, eyelashes and eyebrows, and pubic hair.
The effects of trichotillomania also depend on the age at which it happens. Children commonly pull their hair in this way, but that behavior is often a self-soothing act. Children often grow out of this behavior and don’t have any long-term negative effects. Adolescents, teenagers and adults with this condition tend to have much more severe problems.
Mental health effects
People with TTM commonly feel anxiety, embarrassment or shame about this condition. This can affect their work and social lives. Many people with this condition don’t seek treatment because they feel embarrassed or ashamed.
Trichophagia
About 20% of people with this condition eat their hair after pulling it, a condition known as trichophagia (from Greek words “tricho” for hair and “phagia” for eating). This can lead to hairball-like blockages in their digestive tract. Those blockages are sometimes dangerous and often cause damage that needs surgery to repair.
People with TTM commonly hold back from telling their healthcare provider about this even after revealing details about TTM. This is often because they’re waiting until they feel they can trust their provider more before sharing that amount of detail.
Hair, skin and tissue damage
People who pull out their hair often cause damage to their skin and tissue just underneath the skin’s surface, especially if they use any kind of personal care tool like tweezers. Skin and tissue damage sometimes need repair or skin grafting to fix. Damage to skin caused by hair pulling can also cause permanent hair loss in affected areas.
Symptoms and Causes
What are the symptoms of trichotillomania?
According to the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders Fifth Edition (better known as the DSM-5), the diagnosis of TTM requires a person to meet five criteria:
- Repeated pulling out of hair that causes hair loss.

- Trying multiple times to stop this behavior or do it less often.
- Feeling that hair pulling negatively affects your life, especially your work and social life.
- The hair pulling or hair loss isn’t happening because of another condition (such as a skin-related disorder or problem).
- The hair pulling isn’t happening because of another mental health condition. An example of this is body dysmorphia, where hair pulling happens because a person believes there’s a problem with their appearance and is trying to fix it).
Some people with TTM pull their hair deliberately, such as when they feel a hair is out of place or looks different from others around it. Other people pull their hair automatically without thinking about it.
What causes trichotillomania?
While experts suspect several possible factors could lead to TTM, there aren’t any confirmed causes of this condition. Some of the suspected factors include:
- Genetics.
 TTM may happen because of certain DNA mutations. More research is needed to confirm this.
TTM may happen because of certain DNA mutations. More research is needed to confirm this. - Changes in brain structure or chemistry. People with TTM often have changes to certain areas in their brains or differences in their brain chemistry.
- Coping mechanism. Many people with TTM describe it as starting after a stressful time in their life. Others describe it starting because of boredom and that pulling their hair became a habit over time.
Other conditions that happen with TTM
There are several mental health conditions that a person is much more likely to have along with TTM. These can happen either as separate conditions or because of TTM (especially anxiety and depression). These include:
- OCD (this condition is a common misdiagnosis for people who, in reality, have TTM).
- Major depressive disorder.
- Anxiety disorders.
- Substance use disorders (alcohol and drugs).
Is it contagious?
No, TTM isn’t contagious, and it can’t spread to others. While some experts suspect it might be something you can inherit from your parents, more research is necessary to confirm that.
While some experts suspect it might be something you can inherit from your parents, more research is necessary to confirm that.
Diagnosis and Tests
How is trichotillomania diagnosed?
Diagnosing TTM involves a combination of a physical exam, where your healthcare provider looks for visible signs of the condition. They'll also ask questions about your health history, current circumstances and anything else that might have a connection to a medical problem.
TTM is a relatively straightforward condition to diagnose, but people with this condition often hide it out of shame or embarrassment. That can make it harder for your healthcare provider to diagnose this condition based solely on asking questions. That’s why a specific type of skin test may also help.
What tests will be done to diagnose it?
In some cases, a “punch biopsy” (where your healthcare provider takes a skin sample for lab analysis) is necessary to confirm a diagnosis of TTM. This test can also rule out other skin conditions that might be the true cause of hair loss or hair pulling.
In cases where your healthcare provider suspects a blockage from swallowed hair, you might also undergo other diagnostic tests. These include imaging tests like a computerized tomography (CT) scan, blood testing for anemia and more.
Management and Treatment
How is it treated, and is there a cure?
Treating TTM often involves therapy, medication or a combination of both. Ongoing research shows some medications for other mental health conditions might help TTM, but more research is necessary before any specific medication becomes a part of the standard care.
What medications and treatments are used?
Medication alone often isn’t enough to treat TTM. Healthcare providers may use combinations of medications, therapy techniques or both.
Medications
Medications that may treat, either on their own or in combinations, TTM include:
- Antidepressants. Selective serotonin reuptake inhibitors (commonly referred to as SSRIs) and tricyclic antidepressants can sometimes help with reducing the impulse to pull hair.
- Antipsychotics. These medications help balance your brain chemistry. While the name sounds like they have only one use, they actually treat many conditions, including dementia, bipolar disorder and schizophrenia.
- Anticonvulsants. These medications typically help treat seizures and other disorders that affect muscle movements, but they also can help with TTM.
- Nutraceuticals. These are nutrition products, such as amino acid supplements, that can help treat medical conditions.
Therapies
Therapy methods that may help treat TTM include:
- Habit reversal therapy. This method involves helping you become more aware of your behaviors and activity patterns. By helping you become more aware, this therapy teaches you to break habits like hair pulling. This method has the best odds of success out of any treatment option for TTM.
- Group therapy and peer support.
 People with TTM may benefit from specific types of group therapy or support.
People with TTM may benefit from specific types of group therapy or support.
People with TTM with hair loss or scarring may need to see other healthcare providers and specialists. In some cases, a dermatologist can help treat related skin problems or damage. Plastic and reconstructive surgeons may also help with skin grafting for affected areas of your body. Other healthcare providers can also offer solutions related to hair regrowth; though, regrowth isn’t always an option.
Complications/side effects of the treatment
The possible side effects that can happen with medications depend on the medications themselves, as well as your medical history and circumstances. Your healthcare provider can tell you more about possible side effects, including potential trouble signs and how you should react if you see those signs. They’re the best source of information about this because they can tailor the information they give you to your specific health needs, situation and circumstances.
How to take care of myself/manage symptoms?
TTM isn’t a condition you should diagnose on your own. That’s because a trained and experienced mental healthcare provider is better prepared to determine if you have TTM or another health condition. It’s also not something you should treat on your own, partly because both medication and therapy methods often need a prescription or other input from a healthcare provider.
How soon after treatment will I feel better?
The time it takes for you to feel better from medication, therapy or a combination of the two can be very different from person to person. Your healthcare provider can tell you more about what you can expect as you undergo treatment and what you can do to help yourself through the process.
Prevention
How can I reduce my risk or prevent this condition?
TTM is a mental health condition, which means it isn’t preventable. There’s also no known way of reducing your risk of developing it.
Outlook / Prognosis
What can I expect if I have this condition?
TTM isn’t usually a danger to your physical health (except in rare cases, especially when a person develops a digestive tract blockage from hair they’ve swallowed). However, it can be very disruptive and damaging to your mental health and quality of life.
Because people with TTM often feel ashamed or embarrassed of this condition, most avoid treatment. Those who avoid or delay treatment are much more likely to have issues like permanent hair loss, scarring and more severe mental health problems.
How long does TTM last?
The available research, while limited, shows that people with TTM have this condition for an average of about 22 years. In some cases, the condition is a lifelong problem. People also often describe that the condition has phases, becoming more or less severe for periods of time. Overall, early diagnosis and treatment are the best chance for limiting how long this condition lasts and how severely it impacts your life.
What’s the outlook for this condition?
The overall outlook for this condition depends partly on the age of the person who has it. Infants and children with TTM often have the best outlook, with the condition commonly going away on its own.
However, the older a person gets — especially from adolescence onward — the greater the odds that treating the condition becomes difficult. TTM on its own is rarely a life-threatening problem. But its impacts on a person’s life, especially their mental health, are often severe. Because of this, early diagnosis and treatment are very important.
Living With
How do I take care of myself?
If you have TTM, it’s important to see a healthcare provider (or multiple providers) with specialized training and experience in treating this condition. They can best guide you on what you can do to minimize the impact of this condition on your life.
In general, healthcare providers recommend the following:
- Be honest about what you’re experiencing.
 TTM is a medical condition that affects your mind and behaviors. Much like you would see a healthcare provider for a broken bone or an ear infection, you should also see a healthcare provider for mental health conditions like TTM. They can help treat your condition and help you deal with any negative emotions you’re facing in connection with it.
TTM is a medical condition that affects your mind and behaviors. Much like you would see a healthcare provider for a broken bone or an ear infection, you should also see a healthcare provider for mental health conditions like TTM. They can help treat your condition and help you deal with any negative emotions you’re facing in connection with it. - See your healthcare provider(s) as recommended. This is especially important for therapy sessions and other mental health visits.
- Take medications as prescribed, if prescribed. Medications can often help decrease how strongly or often you feel the urge to pull your hair.
When should I go to ER?
People with TTM who swallow their hair have a higher risk of blockages in their digestive tract. These blockages often cause severe or even life-threatening complications. The following symptoms are likely with a blockage and mean you should call your healthcare provider or go to the hospital:
- Changes in the color of your stool (poop) to dark green or black.

- Nausea and vomiting.
- Unexplained or unexpected weight loss.
- Diarrhea or constipation.
- Belly pain or discomfort.
A note from Cleveland Clinic
Trichotillomania, or hair pulling, can have a severe effect on your mental health. People with this condition often feel ashamed, embarrassed or guilty because of it. If you have TTM or know someone who does, it’s important to remember this is a medical condition and that hair pulling is very difficult to control or stop on your own. But with treatment, it’s possible to limit how often you pull your hair or stop pulling it. That can help you live a life where your hair and appearance don’t make you feel anxious or ashamed, so you can focus on things that matter most to you.
Diseases in which hair falls out, advice from a trichologist
There are a great many diseases and factors that cause hair loss, disruption of the hair structure. Let's take a look at the main, most common in our lives.
Classic alopecia. Androgenetic (male) and diffuse (female) alopecia
These are the two most common situations in medical practice. The cause of androgenetic alopecia (AGA) is most often genetics, followed by provoking factors: stress, lack of trace elements, vitamins, trichotoxic drugs, etc. Therefore, more often we call AGA not a disease, but a pathological condition.
The female type of hair loss is characterized by the fact that, in addition to genetics, hormonal problems (more often sex hormones) are in second place, and in this case, alopecia can often occur after various diseases.
Now let's consider the action of provoking factors in more detail.
Hormonal factors
A problem with any endocrine gland can lead to pathological hair loss. Most often it is the thyroid gland (hypo- or hyperfunction, which is very typical for our country, since we are in an endemic zone where there is a lack of iodine), ovaries (most often the cause is polycystic ovary syndrome, disturbances in the production of estradiol, dihydrotestosterone), as well as the adrenal glands (produce cortisol) and the pituitary gland (prolactin).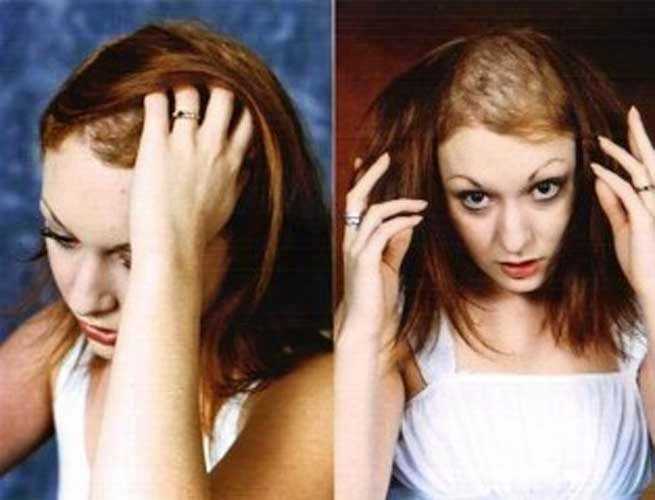 Often hair loss occurs in diabetes mellitus, mainly type 1.
Often hair loss occurs in diabetes mellitus, mainly type 1.
In any of these situations, the normal balance of hormones is disturbed, which leads to an increase in hair loss, a violation of restoration, or a deterioration in the structure of the hair shaft. In such cases, it is necessary to carry out complex therapy, treatment at the same time by a trichologist and an endocrinologist, since only normalization of the hormonal background can stop hair loss, but not improve hair growth and improve the structure. This is one of the main mistakes of patients who think that the normalization of hormone levels is enough.
Toxic factors
These include the effect of anesthesia during surgical interventions, taking a number of trichotoxic drugs (retinoid group, antibiotics, etc.). A separate risk group is cancer patients who are treated in the form of radiation or chemotherapy. It should be noted that in these situations, in most cases, the hair is restored on its own after the cessation of exposure. The criteria for this are the duration of the loss of no more than 2-3 weeks, a slight loss of volume, rapid recovery, hair growth. If this does not happen, then it is better to contact a trichologist.
The criteria for this are the duration of the loss of no more than 2-3 weeks, a slight loss of volume, rapid recovery, hair growth. If this does not happen, then it is better to contact a trichologist.
Diseases of the scalp
Such lesions are associated with fungal and bacterial flora. Microsporia, trichophytosis, lichen often affect not the bulb, but the shaft, that is, the hair itself and its root zone. It is almost always possible to achieve a full recovery. Only a dermatologist should treat such diseases!
Another group of diseases - folliculitis, pyoderma - involves damage to the hair root. Often, when the disease is cured, there are areas of scar tissue without bulbs. In this case, treatment is useless, only a transplant will help.
In all cases, specialized diagnostics (seeding for fungal and bacterial flora) is required to select adequate therapy.
Atypical types of hair loss
The so-called idiopathic alopecias (that is, with an unknown cause) are focal forms. They are characterized by the formation of areas devoid of hair. There are single, multiple, subtotal, total and universal forms of alopecia. With a single, first occurrence, the hairline often recovers on its own without treatment within a year (the exception is the universal form).
They are characterized by the formation of areas devoid of hair. There are single, multiple, subtotal, total and universal forms of alopecia. With a single, first occurrence, the hairline often recovers on its own without treatment within a year (the exception is the universal form).
The cicatricial form (Broca's pseudo-pelade) is also known. In this case, a transplant is indicated, the treatment is ineffective, since the root is replaced by connective tissue, that is, in fact, there is nothing to treat.
Post-hair loss
Recently, the number of patients complaining of very severe hair loss has increased. Very characteristic signs are heavy, abrupt hair loss, which occurs simultaneously, in one day, rapid (in 2-4 weeks) loss of volume 2-3 months after the COVID disease. Initially, doctors believed that this was a reaction to aggressive therapy, but then patients began to come who had the disease in a mild form or even on their feet. The conclusion is that the virus itself has a trichotoxic effect. Treatment with a trichologist is mandatory if the prolapse lasts more than 1-2 weeks. The prognosis is usually positive.
Treatment with a trichologist is mandatory if the prolapse lasts more than 1-2 weeks. The prognosis is usually positive.
Alopecia areata - Cosmedica Clinic
The Cosmedica Team
We are an international team committed to providing the best hair transplant services on the market and to informing and educating people around the world about hair loss and its treatments.
Contents of the article
Millions of people suffer from a disease in which hair falls out in round patches . This condition is called Alopecia areata (alopecia areata) .
Usually the disease occurs suddenly - one day everything is fine, then almost overnight the hair falls out, and round small bald patches appear on the head .
Alopecia areata is an autoimmune disease , that is, the body's immune system mistakenly identifies a part of the body as a foreign threat, such as a virus.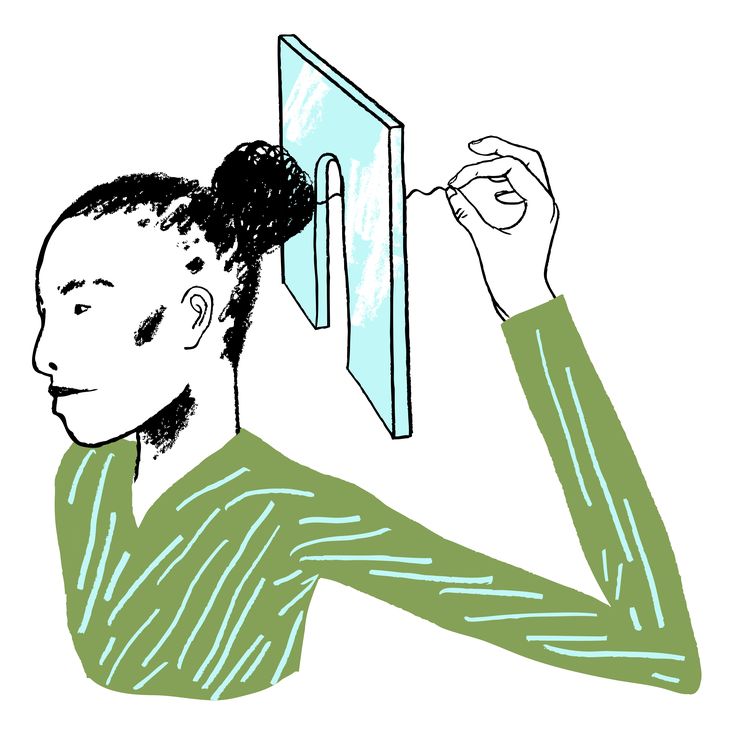 It is one of the most common types of hair loss, surpassing only genetic hair loss in frequency of occurrence.
It is one of the most common types of hair loss, surpassing only genetic hair loss in frequency of occurrence.
The most characteristic symptom of alopecia is round bald patches as the immune system attacks the hair follicles in this area, resulting in hair loss.
The factors that cause the development of alopecia are still not exactly clarified by doctors . In fact, to this day, this disease is a great mystery to doctors.
The facts are that it is an autoimmune disease and the second most common cause of hair loss, after the genetic hair loss known as androgenetic alopecia.
Many people consider baldness to be a traumatic or shocking event because it occurs suddenly. Because hair falls out in very distinct circles, hair loss can be very noticeable.
Alopecia areata causes.
Alopecia areata (alopecia areata) is an autoimmune disease. Suddenly and for no apparent reason, the body recognizes the hair follicles where the hair roots are formed as foreign bodies and starts attacking them accordingly.
This in turn leads to an inflammatory reaction in the affected area, causing the hair to fall out within a very short time .
Round or oval hairless areas remain, characteristic of this disease. Along their edges, broken hairs can be found.
In some cases, mostly pigmented hair falls out , while gray hairs remain . If a person has a lot of gray hair, then only they remain, which gives the impression that that the person turned gray prematurely.
The cause of alopecia areata has not yet been fully elucidated. As with hereditary hair loss (genetic predisposition), it is assumed that some people with alopecia areata are more prone to it than others. There is often a family history of the disease. In about 25% of cases, it also occurs in a family member or close relative.
In addition, people from trisomy 21 or with white spot disease (vitiligo) often suffer from patchy hair loss. Symptoms also occur in association with thyroid disorders such as Graves disease or Hashimoto . It is assumed that constant stress also sometimes provokes the development of alopecia areata.
Symptoms also occur in association with thyroid disorders such as Graves disease or Hashimoto . It is assumed that constant stress also sometimes provokes the development of alopecia areata.
Possible alopecia areata of the head, as well as the whole body.
Types and symptoms of alopecia areata
There are 5 different types of alopecia of the area:
- Alopecia Multilobular - bald spots appear in several places on the head
- Alotage - Hair falls only in one place on the head 9005 all hair on the head falls out
- Universal alopecia - instead of individual areas of hair loss, all hair on the body falls out
- Alopecia ophiasis - hair falls out in the form of a crown on the neck and ears (this is a special and unusual form of the disease).
The good news is that in all forms of alopecia areata, patient is able to grow hair after the episode ends.
However, the complexity of alopecia lies in the fact that the disease usually occurs in episodes.
This means, for example, that patchy hair loss can reappear as soon as the hair begins to grow. Quite often as a side symptom appear Spotted or furrowed nails.
Alopecia areata in women
Alopecia areata in women treatment.
Women are more likely to suffer from baldness than men. And especially often women suffer greatly when their hair falls out all at once.
Lush hair and thick hair are still considered a sign of femininity, although there are more and more women who have made a bald head their calling card.
Otherwise, the wig can at least visually hide it. If the hair does not grow back properly after overcoming the disease, the solution may be hair transplant . You can find out about the service by clicking on the link hair transplant for women .
You can find out about the service by clicking on the link hair transplant for women .
Alopecia areata in men
In men, circular hair loss can also occur in the beard area ( beard alopecia areata ). The disease can also affect the eyebrows and (very rarely) can be observed in body hair .
If the beard is affected, the beard can be shaved during an attack of alopecia areata. Since the area around the affected area is also free of hair, this makes it almost invisible.
Especially in the case of Alopecia Areata multilobularis and Alopecia Areata unilocularis , it is recommended to wear headgear , at least as a temporary solution. If a person's hair does not grow back properly after an episode, Hair Transplant in Turkey may be the solution. You can learn about the service by clicking on the link above.
Alopecia areata in children
Circular hair loss in children ( alopecia areata ) is surprisingly common. Typical symptoms of this disease appear almost overnight. These are round or slightly oval bald patches on the scalp.
Typical symptoms of this disease appear almost overnight. These are round or slightly oval bald patches on the scalp.
Alopecia areata in children treatment.
Many children grow their hair back within a year without medication . Sometimes steroid injections are used to suppress the local immune response. Alopecia areata can also be hereditary. Most young children suffering from circular hair loss are relatively calm about this condition. However, during adolescence, the situation can quickly change.
Alopecia areata treatment
How to treat alopecia areata?
Since the cause of the disease is not fully understood, there is no effective treatment for alopecia that would guarantee hair regrowth.
In mild cases of alopecia areata, hair grows back within three to six months . However, this self-healing can last for years.
A doctor, in this case a dermatologist, treats only the symptoms of the disease, e.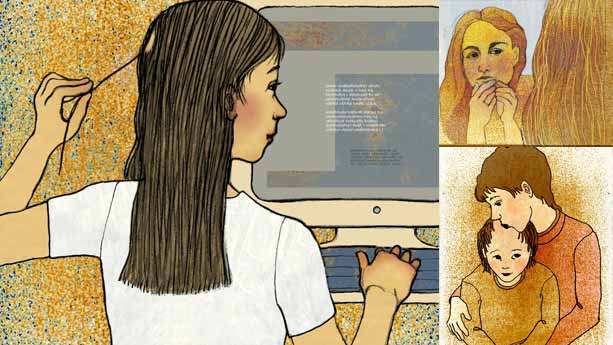 g.0051 using zinc tablets . Therapy with cortisone and with prednisolone may also be effective. However, they are associated with huge side effects as the drugs suppress the immune system. It also makes the patient vulnerable to other diseases and medical conditions.
g.0051 using zinc tablets . Therapy with cortisone and with prednisolone may also be effective. However, they are associated with huge side effects as the drugs suppress the immune system. It also makes the patient vulnerable to other diseases and medical conditions.
Meanwhile, great success has been achieved in the treatment of alopecia areata with topical immunotherapy . With this treatment, the scalp is sensitized by special allergens . The reaction thus elicited should stimulate hair growth.
In some cases, the immune response leading to baldness may be associated with prolonged and severe stress . It may happen that if the stress subsides, then the immune response also subsides, and normal hair growth can resume after a while.
However, the possibility of using such therapy always depends on the individual case. In addition, such treatment is carried out only in specialized medical practices or clinics.
In any case, if you suffer from alopecia areata, it is recommended that you consult your doctor.
Hair transplant for alopecia areata?
In principle, hair transplant is possible in alopecia areata. This is especially true when the hair no longer grows with the same density and bald patches remain.
However, it is very important that alopecia areata be completely cured . Otherwise, there is a risk that the immune system will attack the newly transplanted follicles and they will immediately fall out again.
A reputable trichologist will carefully examine the bald area to ensure that there is no risk of the immune system attacking the transplanted hair follicles again.
A good and reputable hair transplant clinic will never pressure you into having a hair transplant. In cases of alopecia areata, hair transplantation can give good results, but is only suitable under certain circumstances. In the wrong circumstances, it can do more harm than good.