Different types of mental health disorders
Autism
It is estimated that worldwide about one in 100 children has autism(1). This estimate represents an average figure, and reported prevalence varies substantially across studies. Some well-controlled studies have, however, reported figures that are substantially\r\n higher. The prevalence of autism in many low- and middle-income countries is unknown.
Causes
Available scientific evidence suggests that there are probably many factors that make a child more likely to have autism, including environmental and genetic factors.
Available epidemiological data conclude that there is no evidence of a causal association between measles, mumps and rubella vaccine, and autism. Previous studies suggesting a causal link were found to be filled with methodological flaws(2)(3).
There is also no evidence to suggest that any other childhood vaccine may increase the risk of autism. Evidence reviews of the potential association between the preservative thiomersal and aluminium adjuvants contained in inactivated vaccines and the\r\n risk of autism strongly concluded that vaccines do not increase the risk of autism.
Assessment and care
A broad range of interventions, from early childhood and across the life span, can optimize the development, health, well-being and quality of life of autistic people. Timely access to early evidence-based psychosocial interventions can improve the ability\r\n of autistic children to communicate effectively and interact socially. The monitoring of child development as part of routine maternal and child health care is recommended.
It is important that, once autism has been diagnosed, children, adolescents and adults with autism and their carers are offered relevant information, services, referrals, and practical support, in accordance with their individual and evolving needs and\r\n preferences.
The health-care needs of people with autism are complex and require a range of integrated services, that include health promotion, care and rehabilitation. Collaboration between the health sector and other sectors, particularly education, employment and\r\n social care, is important.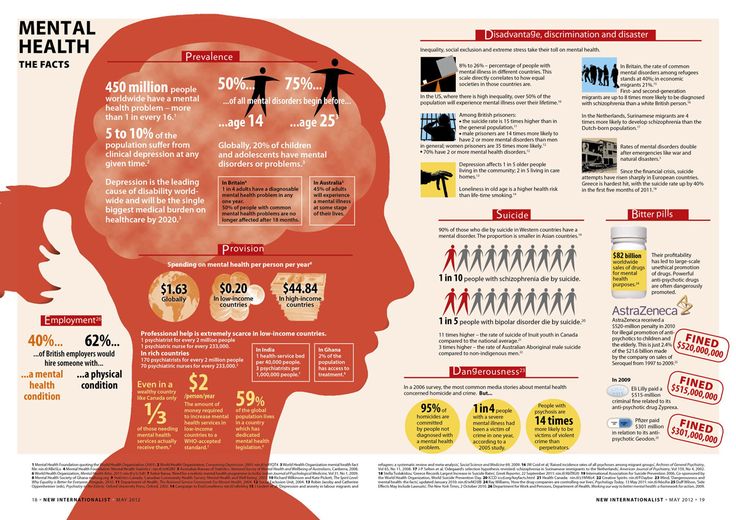
Interventions for people with autism and other developmental disabilities need to be designed and delivered with the participation of people living with these conditions. Care needs to be accompanied by actions at community and societal levels for greater accessibility, inclusivity and support.
Human rights
All people, including people with autism, have the right to the enjoyment of the highest attainable standard of physical and mental health.
And yet, autistic people are often subject to stigma and discrimination, including unjust deprivation of health care, education and opportunities to engage and participate in their communities.
People with autism have the same health problems as the general population. However, they may, in addition, have specific health-care needs related to autism or other co-occurring conditions. They may be more vulnerable to developing chronic noncommunicable\r\n conditions because of behavioural risk factors such as physical inactivity and poor dietary preferences, and are at greater risk of violence, injury and abuse.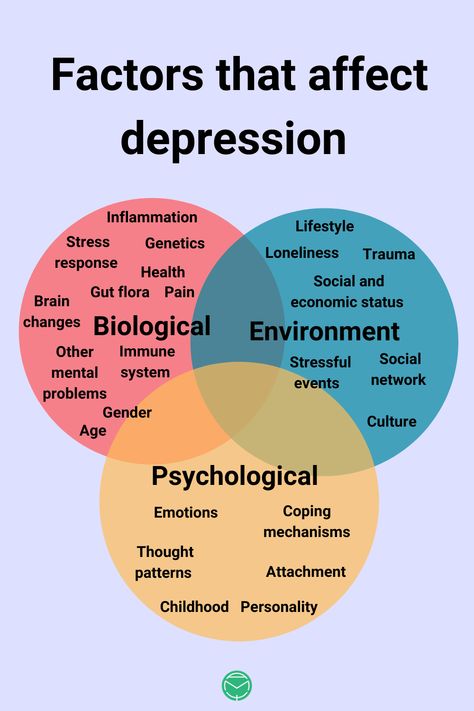
People with autism require accessible health services for general health-care needs like the rest of the population, including promotive and preventive services and treatment of acute and chronic illness. Nevertheless, autistic people have higher rates\r\n of unmet health-care needs compared with the general population. They are also more vulnerable during humanitarian emergencies. A common barrier is created by health-care providers’ inadequate knowledge and understanding of autism.
WHO resolution on autism spectrum disorders
In May 2014, the Sixty-seventh World Health Assembly adopted a resolution entitled Comprehensive and coordinated efforts for the management of autism spectrum disorders,\r\n which was supported by more than 60 countries.
The resolution urges WHO to collaborate with Member States and partner agencies to strengthen national capacities to address ASD and other developmental disabilities.
WHO response
WHO and partners recognize the need to strengthen countries' abilities to promote the optimal health and well-being of all people with autism.
WHO's efforts focus on:
- increasing the commitment of governments to taking action to improve the quality of life of people with autism;
- providing guidance on policies and action plans that address autism within the broader framework of health, mental and brain health and disabilities;
- contributing to strengthening the ability of the health workforce to provide appropriate and effective care and promote optimal standards of health and well-being for people with autism; and
- promoting inclusive and enabling environments for people with autism and other developmental disabilities and providing support to their caregivers.
WHO Comprehensive mental health action plan 2013–2030 and World Health Assembly Resolution WHA73.10 for “global actions on epilepsy and other neurological disorders” calls on countries to address the current significant\r\n gaps in early detection, care, treatment and rehabilitation for mental and neurodevelopmental conditions, which include autism.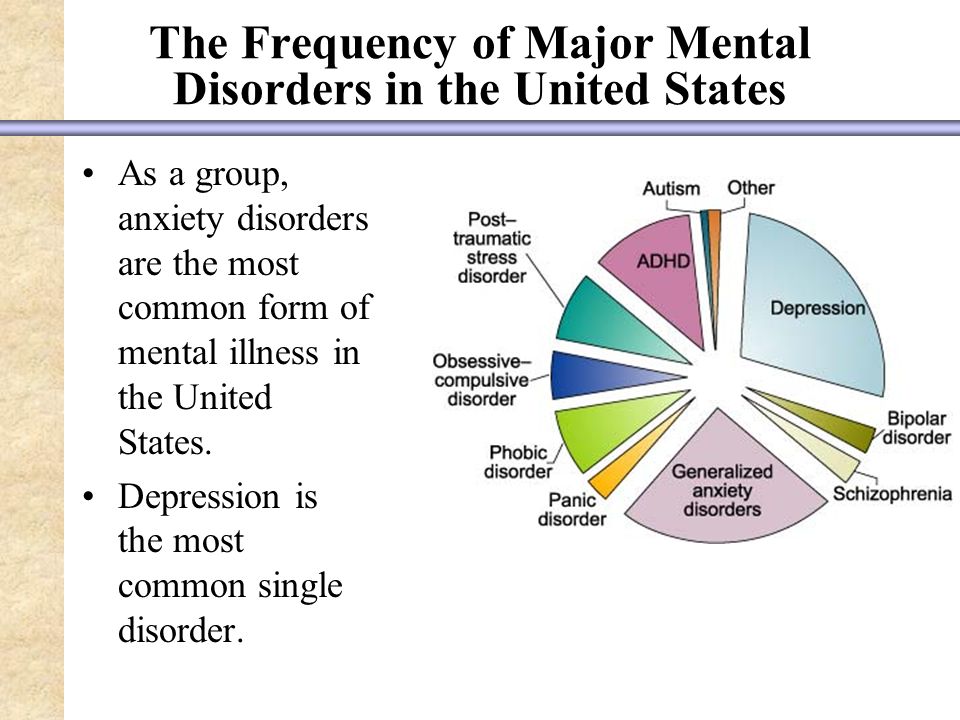 It also calls for counties to address the social, economic, educational and inclusion needs of people living with mental\r\n and neurological disorders, and their families, and to improve surveillance and relevant research.
It also calls for counties to address the social, economic, educational and inclusion needs of people living with mental\r\n and neurological disorders, and their families, and to improve surveillance and relevant research.
References
(1) Global prevalence of autism: A systematic review update. Zeidan J et al. Autism Research 2022 March.
(2) Wakefield's affair: 12 years of uncertainty whereas no link between autism and MMR vaccine has been proved. Maisonneuve H, Floret D. Presse Med. 2012 Sep; French (https://www.ncbi.nlm.nih.gov/pubmed/22748860).\r\n
(3) Lancet retracts Wakefield’s MMR paper. Dyer C. BMJ 2010;340:c696. 2 February 2010 (https://pubmed.ncbi.nlm.nih.gov/20124366/)\r\n
","datePublished":"2022-03-30T13:32:00.0000000+00:00","image":"https://cdn.who.int/media/images/default-source/health-topics/mental-health/autism.jpg?sfvrsn=d518329b_8","publisher":{"@type":"Organization","name":"World Health Organization: WHO","logo":{"@type":"ImageObject","url":"https://www. who.int/Images/SchemaOrg/schemaOrgLogo.jpg","width":250,"height":60}},"dateModified":"2022-03-30T13:32:00.0000000+00:00","mainEntityOfPage":"https://www.who.int/news-room/fact-sheets/detail/autism-spectrum-disorders","@context":"http://schema.org","@type":"Article"};
who.int/Images/SchemaOrg/schemaOrgLogo.jpg","width":250,"height":60}},"dateModified":"2022-03-30T13:32:00.0000000+00:00","mainEntityOfPage":"https://www.who.int/news-room/fact-sheets/detail/autism-spectrum-disorders","@context":"http://schema.org","@type":"Article"};
Schizophrenia
Schizophrenia- All topics »
- A
- B
- C
- D
- E
- F
- G
- H
- I
- J
- K
- L
- M
- N
- O
- P
- Q
- R
- S
- T
- U
- V
- W
- X
- Y
- Z
- Resources »
- Fact sheets
- Facts in pictures
- Multimedia
- Publications
- Questions & answers
- Tools and toolkits
- Popular »
- Air pollution
- Coronavirus disease (COVID-19)
- Hepatitis
- Monkeypox
- All countries »
- A
- B
- C
- D
- E
- F
- G
- H
- I
- J
- K
- L
- M
- N
- O
- P
- Q
- R
- S
- T
- U
- V
- W
- X
- Y
- Z
- Regions »
- Africa
- Americas
- South-East Asia
- Europe
- Eastern Mediterranean
- Western Pacific
- WHO in countries »
- Statistics
- Cooperation strategies
- Ukraine emergency
- All news »
- News releases
- Statements
- Campaigns
- Commentaries
- Events
- Feature stories
- Speeches
- Spotlights
- Newsletters
- Photo library
- Media distribution list
- Headlines »
- Focus on »
- Afghanistan crisis
- COVID-19 pandemic
- Northern Ethiopia crisis
- Syria crisis
- Ukraine emergency
- Monkeypox outbreak
- Greater Horn of Africa crisis
- Latest »
- Disease Outbreak News
- Travel advice
- Situation reports
- Weekly Epidemiological Record
- WHO in emergencies »
- Surveillance
- Research
- Funding
- Partners
- Operations
- Independent Oversight and Advisory Committee
- Data at WHO »
- Global Health Estimates
- Health SDGs
- Mortality Database
- Data collections
- Dashboards »
- COVID-19 Dashboard
- Triple Billion Dashboard
- Health Inequality Monitor
- Highlights »
- Global Health Observatory
- SCORE
- Insights and visualizations
- Data collection tools
- Reports »
- World Health Statistics 2022
- COVID excess deaths
- DDI IN FOCUS: 2022
- About WHO »
- People
- Teams
- Structure
- Partnerships and collaboration
- Collaborating centres
- Networks, committees and advisory groups
- Transformation
- Our Work »
- General Programme of Work
- WHO Academy
- Activities
- Initiatives
- Funding »
- Investment case
- WHO Foundation
- Accountability »
- Audit
- Budget
- Financial statements
- Programme Budget Portal
- Results Report
- Governance »
- World Health Assembly
- Executive Board
- Election of Director-General
- Governing Bodies website
- Home/
- Newsroom/
- Fact sheets/
- Detail/
- Schizophrenia
Key facts
- Schizophrenia causes psychosis and is associated with considerable disability and may affect all areas of life including personal, family, social, educational, and occupational functioning.

- Stigma, discrimination, and violation of human rights of people with schizophrenia are common.
- More than two out of three people with psychosis in the world do not receive specialist mental health care.
- A range of effective care options for people with schizophrenia exist and at least one in three people with schizophrenia will be able to fully recover.
Schizophrenia is characterised by significant impairments in the way reality is perceived and changes in behaviour related to:
- persistent delusions: the person has fixed beliefs that something is true, despite evidence to the contrary;
- persistent hallucinations: the person may hear, smell, see, touch, or feel things that are not there;
- experiences of influence, control or passivity: the experience that one’s feelings, impulses, actions, or thoughts are not generated by oneself, are being placed in one’s mind or withdrawn from one’s mind by others, or that one’s thoughts are being broadcast to others;
- disorganized thinking, which is often observed as jumbled or irrelevant speech;
- highly disorganised behaviour e.
 g. the person does things that appear bizarre or purposeless, or the person has unpredictable or inappropriate emotional responses that interfere with their ability to organise their behaviour;
g. the person does things that appear bizarre or purposeless, or the person has unpredictable or inappropriate emotional responses that interfere with their ability to organise their behaviour; - “negative symptoms” such as very limited speech, restricted experience and expression of emotions, inability to experience interest or pleasure, and social withdrawal; and/or
- extreme agitation or slowing of movements, maintenance of unusual postures.
People with schizophrenia often also experience persistent difficulties with their cognitive or thinking skills, such as memory, attention, and problem-solving.
At least one third of people with schizophrenia experiences complete remission of symptoms (1). Some people with schizophrenia experience worsening and remission of symptoms periodically throughout their lives, others a gradual worsening of symptoms over time.
Magnitude and impact
Schizophrenia affects approximately 24 million people or 1 in 300 people (0. 32%) worldwide. This rate is 1 in 222 people (0.45%) among adults (2). It is not as common as many other mental disorders. Onset is most often during late adolescence and the twenties, and onset tends to happen earlier among men than among women.
32%) worldwide. This rate is 1 in 222 people (0.45%) among adults (2). It is not as common as many other mental disorders. Onset is most often during late adolescence and the twenties, and onset tends to happen earlier among men than among women.
Schizophrenia is frequently associated with significant distress and impairment in personal, family, social, educational, occupational, and other important areas of life.
People with schizophrenia are 2 to 3 times more likely to die early than the general population (3). This is often due to physical illnesses, such as cardiovascular, metabolic, and infectious diseases.
People with schizophrenia often experience human rights violations both inside mental health institutions and in community settings. Stigma against people with this condition is intense and widespread, causing social exclusion, and impacting their relationships with others, including family and friends. This contributes to discrimination, which in turn can limit access to general health care, education, housing, and employment.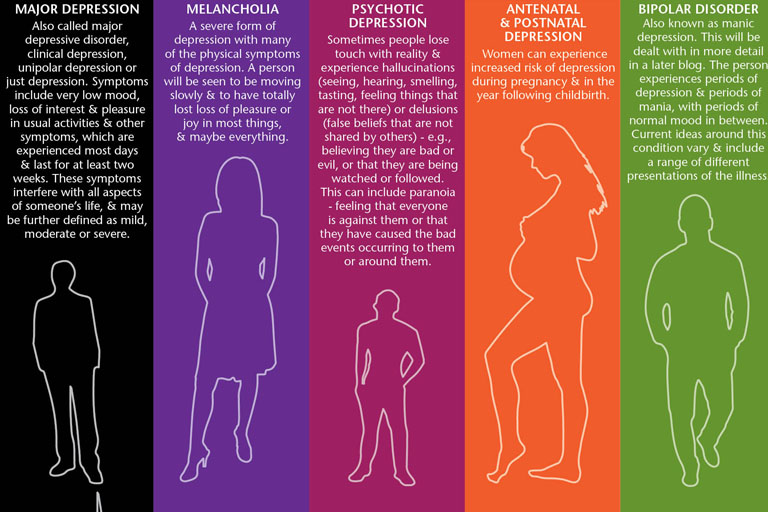
During humanitarian and public health emergencies, extreme stress and fear, breakdown of social supports, isolation and disruption of health-care services and supply of medication can occur. These changes can have an impact on the lives of people with schizophrenia, such as exacerbation of existing symptoms. During emergencies, people with schizophrenia are more vulnerable than others to various human rights violations, including neglect, abandonment, homelessness, abuse and exclusion.
Causes of schizophreniaResearch has not identified one single cause of schizophrenia. It is thought that an interaction between genes and a range of environmental factors may cause schizophrenia. Psychosocial factors may also affect the onset and course of schizophrenia. Heavy use of cannabis is associated with an elevated risk of the disorder.
ServicesCurrently, the vast majority of people with schizophrenia around the world are not receiving mental health care. Approximately 50% of people in mental hospitals have a schizophrenia diagnosis (4). Only 31.3% of people with psychosis receive specialist mental health care (5). Most resources for mental health services are inefficiently spent on care within mental hospitals.
Approximately 50% of people in mental hospitals have a schizophrenia diagnosis (4). Only 31.3% of people with psychosis receive specialist mental health care (5). Most resources for mental health services are inefficiently spent on care within mental hospitals.
There is clear evidence that mental hospitals are not effective in providing the care that people with mental health conditions need and, regularly, violate the basic human rights of persons with schizophrenia. Efforts to transfer care from mental health institutions to the community need to be expanded and accelerated. Such efforts start with the development of a range of quality community-based mental health services. Options for community-based mental health care include integration in primary health and general hospital care, community mental health centres, day centres, supported housing, and outreach services for home-based support. The engagement of the person with schizophrenia, family members and the wider community in providing support is important.
A range of effective care options for people with schizophrenia exist, and these include medication, psychoeducation, family interventions, cognitive-behavioural therapy and psychosocial rehabilitation (e.g., life skills training). Facilitated assisted living, supported housing and supported employment are essential care options that should be available for people with schizophrenia. A recovery-oriented approach – giving people agency in treatment decisions – is essential for people with schizophrenia and for their families and/or caregivers as well.
WHO responseWHO’s Comprehensive Mental Health Action Plan 2013-2030 highlights the steps required to provide appropriate services for people with mental disorders including schizophrenia. A key recommendation of the Action Plan is to shift services from institutions to the community. The WHO Special Initiative for Mental Health aims to further progress towards objectives of the Comprehensive Mental Health Action Plan 2013-2030 by ensuring 100 million more people have access to quality and affordable care for mental health conditions.
WHO's Mental Health Gap Action Programme (mhGAP) uses evidence-based technical guidance, tools and training packages to expand service in countries, especially in resource-poor settings. It focuses on a prioritized set of conditions, including psychosis, directing capacity building towards non-specialized health-care providers in an integrated approach that promotes mental health at all levels of care. Currently mhGAP is being implemented in more than 100 WHO Member States.
The WHO QualityRights Project involves improving the quality of care and human rights conditions in mental health and social care facilities and to empower organizations to advocate for the health of people with mental health conditions and psychosocial disabilities.
The WHO guidance on community mental health services and person-centred and rights-based approaches provides information and support to all stakeholders who wish to develop or transform their mental health system and services to align with international human rights standards including the UN Convention on the Rights of Persons with Disabilities.
(1) Harrison G, Hopper K, Craig T, Laska E, Siegel C, Wanderling J. Recovery from psychotic illness: a 15- and 25-year international follow-up study. Br J Psychiatry 2001;178:506-17.
(2) Institute of health Metrics and Evaluation (IHME). Global Health Data Exchange (GHDx). http://ghdx.healthdata.org/gbd-results-tool?params=gbd-api-2019-permalink/27a7644e8ad28e739382d31e77589dd7 (Accessed 25 September 2021)
(3) Laursen TM, Nordentoft M, Mortensen PB. Excess early mortality in schizophrenia. Annual Review of Clinical Psychology, 2014;10, 425-438.
(4) WHO. Mental health systems in selected low- and middle-income countries: a WHO-AIMS cross-national analysis. WHO: Geneva, 2009
(5) Jaeschke K et al. Global estimates of service coverage for severe mental disorders: findings from the WHO Mental Health Atlas 2017 Glob Ment Health 2021;8:e27.
WHO’s Comprehensive Mental Health Action Plan 2013-2030
WHO Special Initiative for Mental Health
WHO's Mental Health Gap Action Programme (mhGAP)
WHO QualityRights Project
WHO guidance on community mental health services and person-centred and rights-based approaches
More on mental health
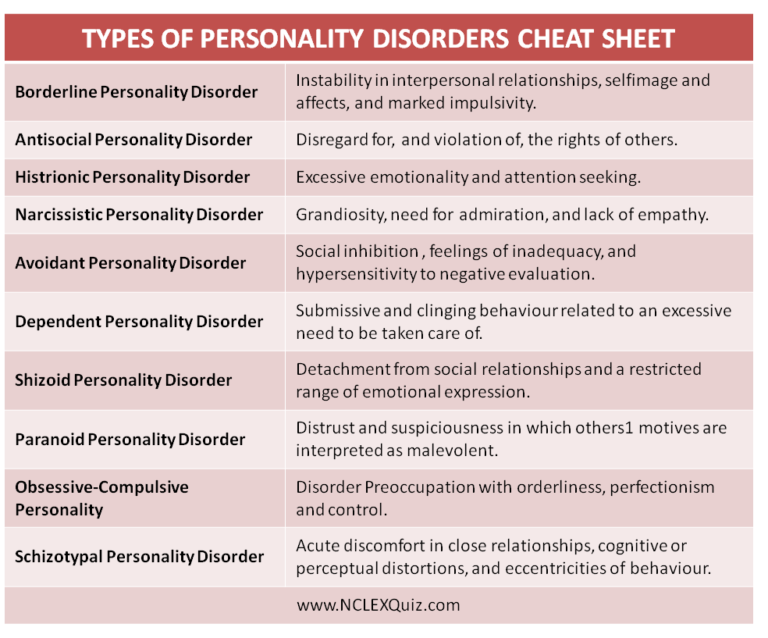
Types of mental disorders
Call us
Make an appointment
Dear visitors and doctors of our Center! We congratulate you on the upcoming New Year! Health, longevity, happiness to you and your loved ones!
December 31 we are open from 10:00 to 18:00. 01, 02, 03 January - days off. From January 04, 2023, the Center operates as usual, from 10:00 to 21:00.
01, 02, 03 January - days off. From January 04, 2023, the Center operates as usual, from 10:00 to 21:00.
- Main page
- Psychiatry
- Types of mental disorders
- Types of mental disorders
Aggressive behavior
accompanies many mental illnesses. Manifested in hostility, threats and attacks. If these symptoms arose in a person for the first time and are generally not characteristic of him, most likely, he needs to immediately consult a psychiatrist. In other cases of aggressive behavior (especially - unreasonable) consultation with a psychiatrist is also desirable.
Apathy of the mentally ill
a state of indifference, detachment, loss of interest and desire to do something. It is often a manifestation of depression, while it is painfully experienced. If apathy does not burden the patient, then this may be a manifestation of another mental or neurological disease.
Autism
Autism is a condition in which a person lives in an internal or unreal (virtual) world, and not in real events. Close such a person is seen as closed, uninterested in what is happening around, closed. The world of fantasy overlaps reality, and therefore a person with autism is cold and indifferent to the people around him, including those close to him. An autistic person is often not burdened by the difficulties of social interaction and communication disorders. Autism occurs both in childhood and in adulthood, and in adults it can be not only a “continuation” of childhood autism, but also a consequence of a developed mental disorder.
Close such a person is seen as closed, uninterested in what is happening around, closed. The world of fantasy overlaps reality, and therefore a person with autism is cold and indifferent to the people around him, including those close to him. An autistic person is often not burdened by the difficulties of social interaction and communication disorders. Autism occurs both in childhood and in adulthood, and in adults it can be not only a “continuation” of childhood autism, but also a consequence of a developed mental disorder.
Delirium tremens (delirium)
occurs mainly in patients with alcoholism, at the second or third stage of the disease. It is important to note that delirium occurs more often not in intoxication, but on the 2nd-3rd day of abstinence from alcohol after drinking (at the peak of the withdrawal syndrome). It is characterized by confusion, increased body temperature, disorientation, agitation, vision of various hallucinatory images. For patients with delirium tremens, hallucinatory images of moving animals (running rats, cockroaches, gnomes, etc. ) are characteristic. Patients attract attention to themselves by their behavior: they are agitated, excited, try to catch hallucinatory images or brush them off, shake them off themselves, often talk to them.
) are characteristic. Patients attract attention to themselves by their behavior: they are agitated, excited, try to catch hallucinatory images or brush them off, shake them off themselves, often talk to them.
Delirium tremens is also possible in non-drinkers, especially in children and the elderly with diseases that occur with a high temperature. Thus, delirium tremens is a sign of intoxication of the body.
Insomnia
in chronically current mental disorders is an indicator of deterioration in mental well-being, since it often appears before all other symptoms.
Crazy ideas (strange judgments, delirium)
are most often perceived by close and surrounding people as strange judgments that do not correspond to reality. At the same time, a person with delusions cannot be persuaded, even if he does not know what to object to attempts to persuade him. Crazy ideas don't need proof. It is rather "knowledge", conviction. Because of this, the behavior of a person with delusional ideas is determined by the content of these ideas.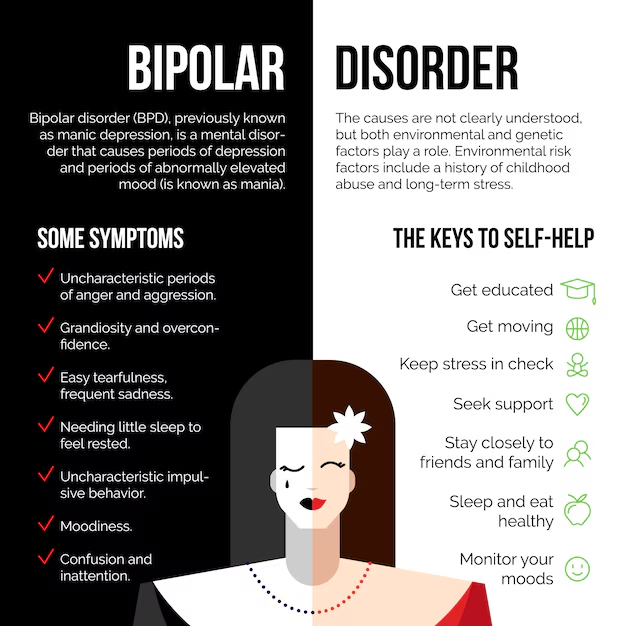 According to the content, the main forms of delusions can be divided into delusions of persecution (what is popularly called “persecution mania”: the patient is pursued by special services or other organizations, they try to poison or rob relatives or neighbors; people on the street somehow in a special way, look unfriendly and whisper about him), delusions of grandeur (the patient is the heir to the royal family, the inventor of the time machine or the law of immortality, the ruler of the world, sometimes the messenger of God or God himself, or the devil, etc.) and delusions of self-abasement (accusing oneself of sins, numerous errors, delirium of a physical defect). A patient with delusional judgments needs to be treated by a psychiatrist.
According to the content, the main forms of delusions can be divided into delusions of persecution (what is popularly called “persecution mania”: the patient is pursued by special services or other organizations, they try to poison or rob relatives or neighbors; people on the street somehow in a special way, look unfriendly and whisper about him), delusions of grandeur (the patient is the heir to the royal family, the inventor of the time machine or the law of immortality, the ruler of the world, sometimes the messenger of God or God himself, or the devil, etc.) and delusions of self-abasement (accusing oneself of sins, numerous errors, delirium of a physical defect). A patient with delusional judgments needs to be treated by a psychiatrist.
Excitement or agitation
frequent and rather dangerous signs of mental disorders. Accompany anxiety, depression, psychotic states. With motor arousal in depressed patients, one should be on the alert: suicidal actions are possible. You should also be especially attentive to patients with psychotic arousal: impulsive (unpredictable), including aggressive actions are frequent, which can be dangerous both for the patient and for his environment.
You should also be especially attentive to patients with psychotic arousal: impulsive (unpredictable), including aggressive actions are frequent, which can be dangerous both for the patient and for his environment.
Hallucinations
perception of something that is not really there. Hallucinations are:
- visual (a person "sees" something that is not there: animals running around the house, people, paintings, sometimes whole panoramas: landscapes, battles),
- auditory (a person "hears" extraneous sounds - music, rustles , voices; at the same time, sounds can be localized both in external space: from the corner of the room, behind the wall, from the street, and inside the head, less often - another part of the body),
- olfactory (perception of foreign odors, more often - unpleasant)
- gustatory (strange, often unpleasant taste sensations)
- tactile (for example, sensation on the skin of "crawling" insects; accompanied by scratching, is a sign of serious intoxication)
Dementia (dementia)
, deterioration in the ability to judge and infer. It usually occurs in old age. It can begin imperceptibly: with difficulty remembering words, narrowing the scope of attention, a slight change in mood (quick transitions from tearfulness to joy and back). The character gradually changes: the person becomes more stubborn, but at the same time more suggestible. The vocabulary is depleted, the stock of knowledge is depleted. The most common cause of dementia is damage to the cerebral vessels by an atherosclerotic process, as a result of which the vessels become narrower and blood flow to the brain tissues worsens. Having noticed in time, such changes can be stopped by properly selected therapy (which will also be the prevention of strokes). However, you should be careful if someone close to you has such changes in adulthood and unfolds very quickly: this may be a more complex disease (for example, Alzheimer's disease).
It usually occurs in old age. It can begin imperceptibly: with difficulty remembering words, narrowing the scope of attention, a slight change in mood (quick transitions from tearfulness to joy and back). The character gradually changes: the person becomes more stubborn, but at the same time more suggestible. The vocabulary is depleted, the stock of knowledge is depleted. The most common cause of dementia is damage to the cerebral vessels by an atherosclerotic process, as a result of which the vessels become narrower and blood flow to the brain tissues worsens. Having noticed in time, such changes can be stopped by properly selected therapy (which will also be the prevention of strokes). However, you should be careful if someone close to you has such changes in adulthood and unfolds very quickly: this may be a more complex disease (for example, Alzheimer's disease).
Dysmorphophobia / dysmorphomania
experiences, the content of which is the belief in one's own physical inferiority: a cosmetic defect, overweight, bad smell, in a word, a repulsive appearance.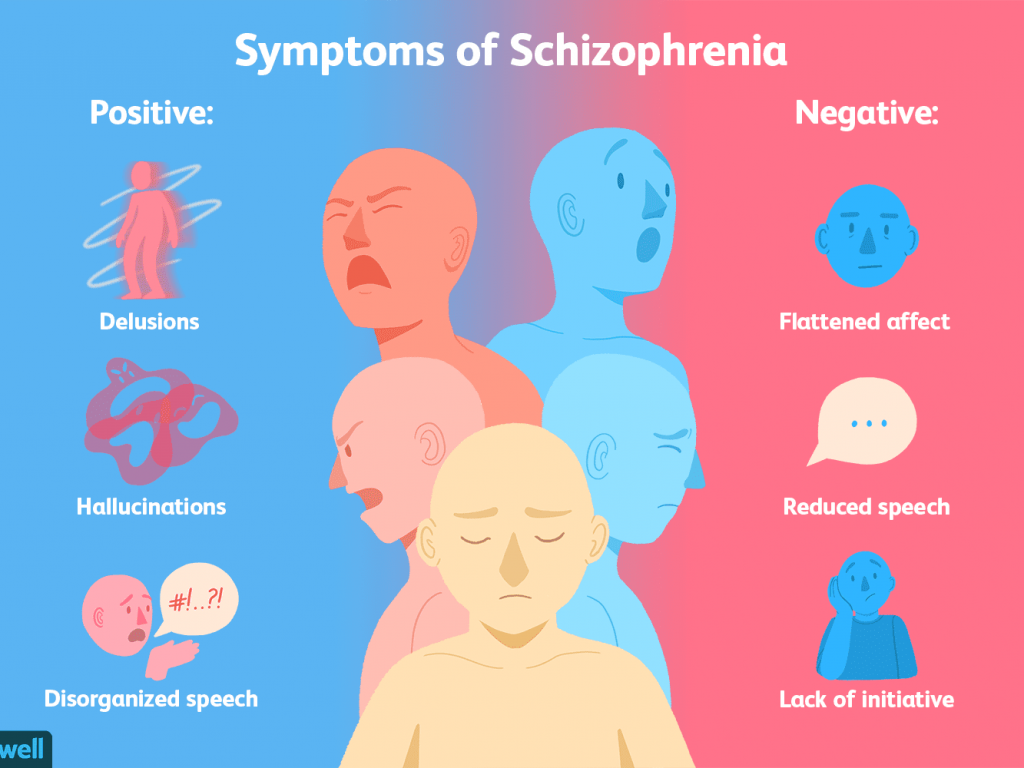 If a defect in appearance really does take place, and in a person’s life this circumstance is predominant, then we are talking about dysmorphophobia (a neurotic level of disorder). If there is actually no defect in appearance, or it is, but not so significant, and at the same time the person is downright convinced of his own ugliness, is seized by ideas of a physical defect, goes to doctors and even undergoes surgery with plastic surgeons, or falls into anorexia ( when convinced of excessive fullness), then here we are talking about dysmorphomania (delusional level of disorders).
If a defect in appearance really does take place, and in a person’s life this circumstance is predominant, then we are talking about dysmorphophobia (a neurotic level of disorder). If there is actually no defect in appearance, or it is, but not so significant, and at the same time the person is downright convinced of his own ugliness, is seized by ideas of a physical defect, goes to doctors and even undergoes surgery with plastic surgeons, or falls into anorexia ( when convinced of excessive fullness), then here we are talking about dysmorphomania (delusional level of disorders).
Hypochondria
state of increased concern about one's health. In this case, the disease of the body may or may not be present. A person suffering from hypochondria, as a rule, is afraid of a specific disease, but can also "generally" feel sick and "find" various diseases in himself (Moliere's "imaginary patient"). He constantly listens to his inner feelings and cannot experience pleasure simply from the process of life. In general, hypochondria can be described as "the experience of Illness."
In general, hypochondria can be described as "the experience of Illness."
Treatment of anorexia
stubborn desire to limit oneself in food intake in order to lose weight. Often accompanied by the induction of artificial vomiting after eating, overly active physical exercises, taking large doses of laxatives. It occurs both with increased and with normal body weight. It is observed more often in girls. It is important to note that at first, anorexic behavior is carefully hidden from others, and is recognized by loved ones already at the stage of severe exhaustion.
Treatment of bulimia
How do you know if a person has bulimia? Often a person does not admit to the last that he overeats, tries to keep his addiction a secret. He is sure that he can solve the problem of nutrition on his own, by an effort of will. Signs of bulimia. Wolf hunger is a condition in which there is an uncontrolled intake of a huge amount of food. The lack of selectivity in food is characteristic, while saturation is not felt. As a rule, it occurs after a period of strict food abstinence, and, in fact, is the “back side” of anorexia.
As a rule, it occurs after a period of strict food abstinence, and, in fact, is the “back side” of anorexia.
Treatment of chronic depression
Not all depression can be cured by psychotherapy alone. Sometimes a temporary intake of specially selected drugs is required. Signs of the severity of depression are: suicidal tendencies, a feeling of despair, self-accusatory statements, anxious arousal, a feeling of general bodily change, physically experienced longing, as well as a painful loss of emotions (love, joy, compassion).
Persecution mania
without good reason are signs of a mental disorder. Such patients often hide their experiences, and then these disorders can be suspected by their behavior: a wary look, anxiety, fearfulness, absent-mindedness, window coverings, listening to something.
Unexplained somatic complaints
it happens (and more often lately) that a person feels physically ill, but no doctor finds a pathology in him. In this case, consultation with a psychiatrist is necessary: depression, neurosis, and an unresolved internal conflict may be hidden behind inexplicable somatic complaints.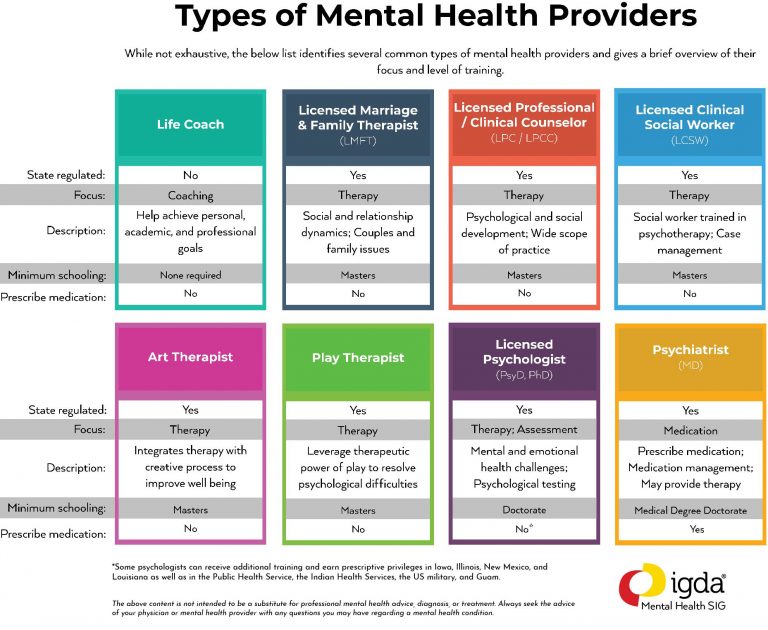
Sloppiness (neglect of hygiene)
occurs in patients with depression, psychoses, as well as in chronically current mental illnesses (schizophrenia, progressive dementia).
Fatigue
Fatigue can be a sign of both physical illness and mental illness. It is often noted in disorders of the depressive circle, while the patient may not feel a noticeable decrease in mood, but feels increasing lethargy, fatigue, inability to cope with the usual stress.
Memory loss
is typical for the elderly, as well as those who have suffered severe traumatic brain injury, patients with alcoholism. It is a sign of a brain disease (vascular damage by atherosclerosis, atrophic processes in the cerebral cortex, past brain injuries, alcohol intoxication).
In vascular diseases in the elderly, forgetfulness of current and recent events and facts is characteristic, inability to learn new things. At the same time, the memory of long-standing events can remain intact for a very long time.
With atrophic processes in the brain, memory loss can be very rapid and abrupt. In this case, the onset of the disease in adulthood (45-55 years) is possible. In such cases, you should not delay contacting a specialist.
Psychosis
is a fairly severe disorder of mental activity, the treatment of which is carried out mainly by medication. Family members of the affected person may seek help for unexplained behavioral changes, including bizarre or threatening behavior (withdrawal, suspicion, threats). Signs that should alert in terms of the development of a psychotic state: hallucinations (false or imagined sensations, for example, perceiving voices when no one is around), delusions (uncorrectable deliberately false beliefs, for example, the patient may be sure that he is being poisoned neighbors, that he receives messages from television or that he is being watched in a special way), agitation or unusual behavior, strange statements, sudden changes or instability of the emotional state. It should be noted that upon leaving the psychotic state, patients need psychotherapeutic assistance aimed at forming a critical attitude towards their disorders, improving socialization, and learning to recognize the first signs of a deterioration in mental well-being (prevention of recurrent psychoses).
It should be noted that upon leaving the psychotic state, patients need psychotherapeutic assistance aimed at forming a critical attitude towards their disorders, improving socialization, and learning to recognize the first signs of a deterioration in mental well-being (prevention of recurrent psychoses).
Latent depression
acts not as a clear depression of mood and other mental functions, but as an internal bodily ill-being affecting various organs, functions, systems. Thus, depression can disguise itself as diseases of the cardiovascular, gastrointestinal, respiratory, and nervous systems. The well-known “pain of unclear etiology” (a diagnosis often encountered in the practice of therapists) often has the same nature.
Anguish
an oppressive painful feeling, which is often experienced as a "tightness", heaviness in the chest. Longing is much more intense than such worldly emotions as sadness or sadness. It often happens with depression and can occur without a significant reason.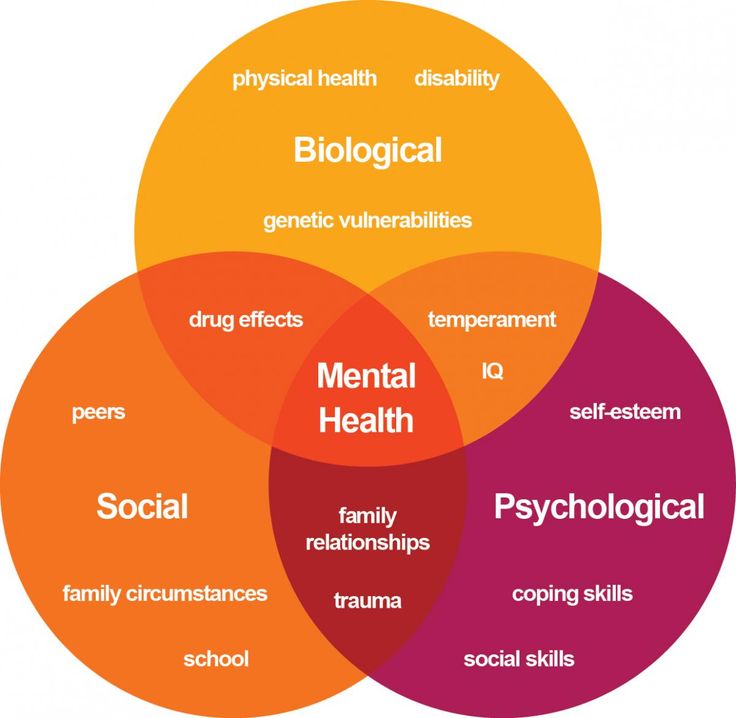
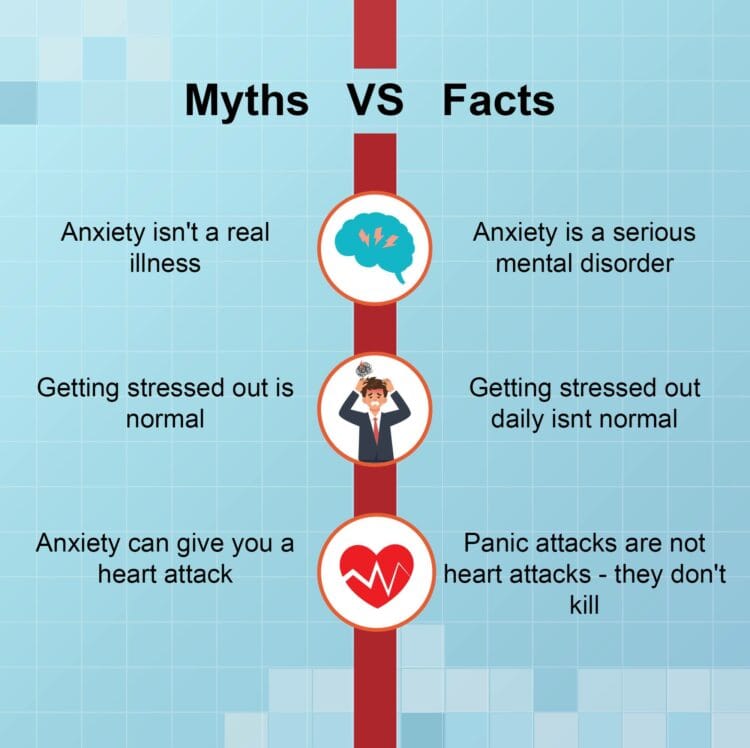
Anxiety in psychiatry
Uncertainty, suspense, feeling that something is about to happen. In other words, it is an emotional experience characterized by discomfort from the uncertainty of perspective. This is the most important human emotion, closely related to the need for security. Anxiety is sometimes felt bodily, like itching, excitement in the chest, internal trembling, and is often combined with motor excitement.
Epileptic seizure
in its most typical form is characterized by an abrupt onset: a person screams, loses consciousness, falls, then sharply strains, sometimes turns blue, followed by convulsions. After a seizure, a person is usually lethargic, lethargic and drowsy. This is the so-called convulsive seizure. However, often epileptic seizures are non-convulsive in nature, occur without a fall and may escape the attention of the patient's relatives. Signals indicating the need to see a doctor are:
- any sharp falls with loss of consciousness (even without convulsions),
- a tendency to suddenly "freeze" and "turn off" (sometimes for seconds, while stereotypical movements of the arms, head, facial muscles of the face are possible; this feature can be observed during a conversation , performing daily activities),
- loss of memory of some events, facts when a person was not drunk, could walk, perform some actions, which he later cannot remember anything about.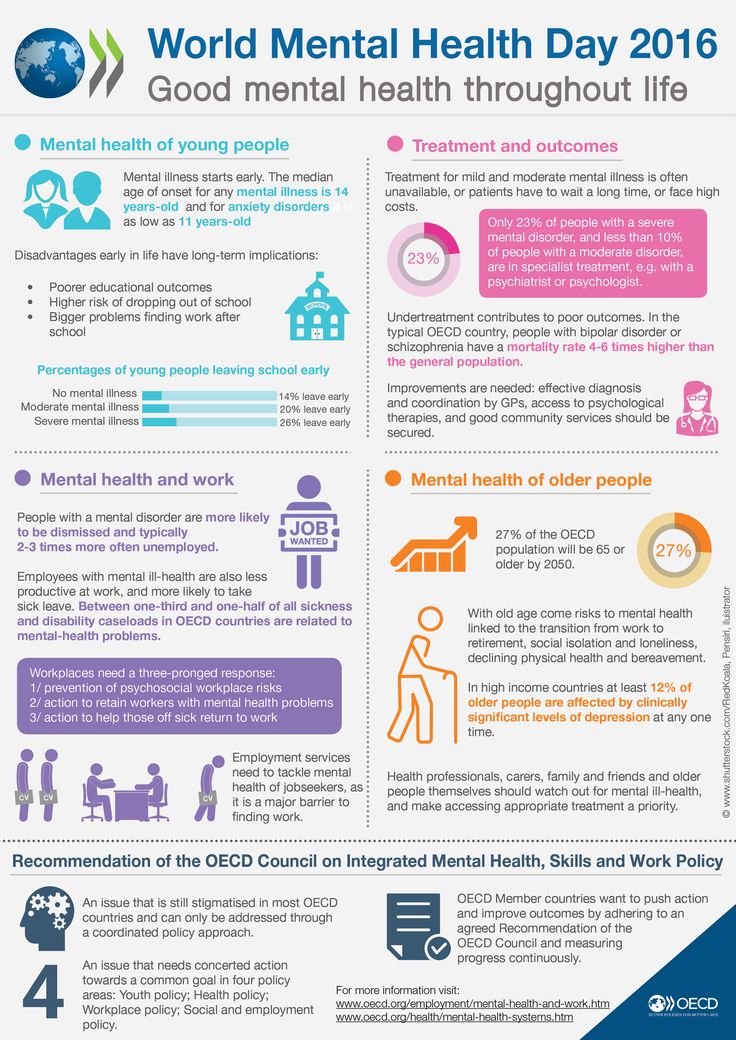
It should be noted that the presence of epileptic seizures does not always indicate epilepsy as a disease. Convulsive and non-convulsive seizures can be a consequence of brain damage (traumatic brain injury, consequences of alcohol intoxication, and in young children, convulsions are the only non-specific response of the body to many stimuli, in particular, an increase in body temperature).
- About psychiatry
- Types of psychiatric disorders
- Severe mental disorders
- Symptoms of disorders
- Psychiatric diseases
- Expert opinion
- Manic disorders
- Anorexia
- Child psychiatry
- Autism treatment
- Treatment for paranoia
11 most common mental disorders
Komsomolskaya Pravda
HEALTH medical news
Oleg KOLESOV
August 23, 2021 23:23
According to the World Health Organization. Check your cockroaches in your head
Photo: Ekaterina MARTINOVICH
Only mind you, let's not be like Jay from the cult story "Three men in a boat, not counting the dogs" at the first more or less similar symptoms.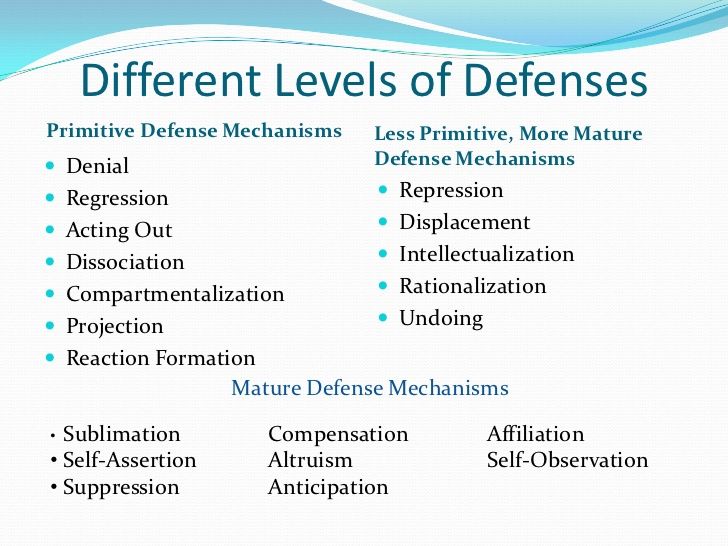 Let us recall that he undertook to somehow study the medical reference book and unexpectedly came to the conclusion that "the only disease I did not find in myself was puerperal fever ".
Let us recall that he undertook to somehow study the medical reference book and unexpectedly came to the conclusion that "the only disease I did not find in myself was puerperal fever ".
The diagnosis is made only by a doctor. And only after a series of analyzes and studies. So no self-diagnosis.
And now let's find out what it actually is, a mental disorder. In a nutshell, this is a violation of brain function, which can be caused by both external and internal causes. Often these reasons are interrelated. The causes of such disorders can be not only hereditary factors, but also head injuries, birth injuries, drug and drug poisoning, brain damage by infections, and even such unexpected moments as, for example, starvation, radiation, conflicts, and so on. Here are the 11 most common mental disorders in the world.
1. PHOBIA
Its main symptom is fear of specific situations or objects that usually do not cause excessive fear in themselves, for example, a spider or a height.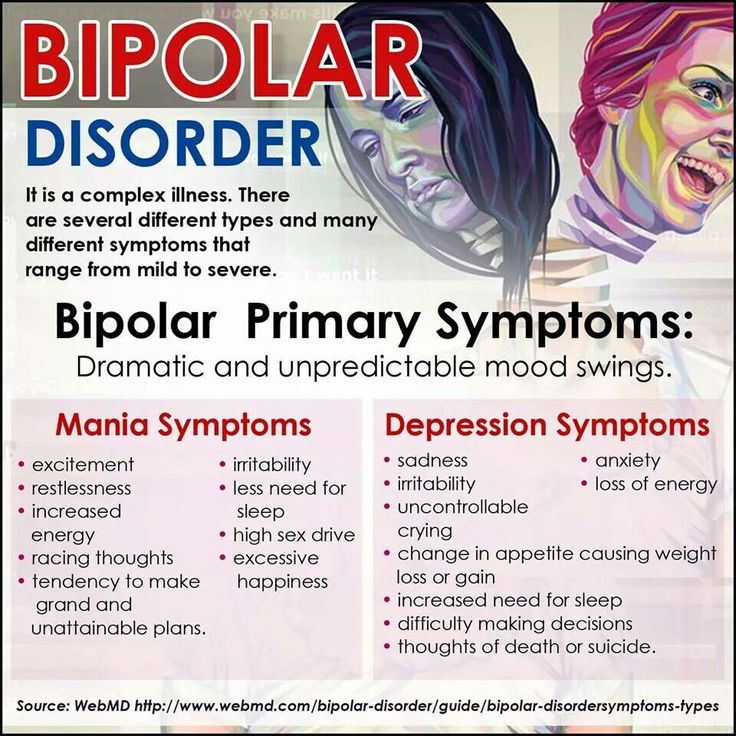
Phobia (in other words, fear) is often accompanied by sweating, tachycardia, depression, as well as panic attacks, darkening of the eyes, a state of horror. A test for anxiety and phobias, the so-called "Zang Self-Rating Anxiety Scale", is often used to identify a phobic disorder. Read: Our seven main fears.
We cope with the fear of heights in a wind tunnel - a transparent cylinder, inside which air is driven away with the help of a powerful fanPhoto: Ekaterina SEREDAVINA
Such people may take out their anger on others, have problems with work and in relationships, they often have mood swings and anxiety. At the same time, people are not critical enough to their behavior.
The development of these disorders begins in early youth and continues throughout life. Such patients often have a high level of intelligence. And the cause of a personality disorder can be not only genetics, but also improper upbringing or environment. This category includes paranoid personality disorder, affective disorders, schizoid personality disorder, emotionally unstable personality disorder, histrionic personality disorder, and so on.
Photo: GLOBAL LOOK PRESS
3. ALCOHOL AND DRUG DEPENDENCE
May be the result of both immediate exposure (often acute intoxication) and the result of prolonged exposure to alcohol. An alcoholic can drink himself into psychosis or dementia. The same goes for drug addiction.
It must be admitted that both such addictions are chronic diseases and can only go into remission. Therefore, treatment should be long and diverse. There are drugs that relieve cravings for alcohol, even cause disgust, but it seems to many alcoholics that if they got off the binge, then they were cured. This is not true.
4. OBESSIVE-COMPULSIVE DISORDER
In other words, unwanted thoughts and obsessive actions. Such people are often unsure whether they have locked the doors, turned off the lights, constantly checking something, knocking on wood, succumbing to superstitions, afraid to step on the manhole cover. Often there are exaggerated fears of contamination from contact with people or household items.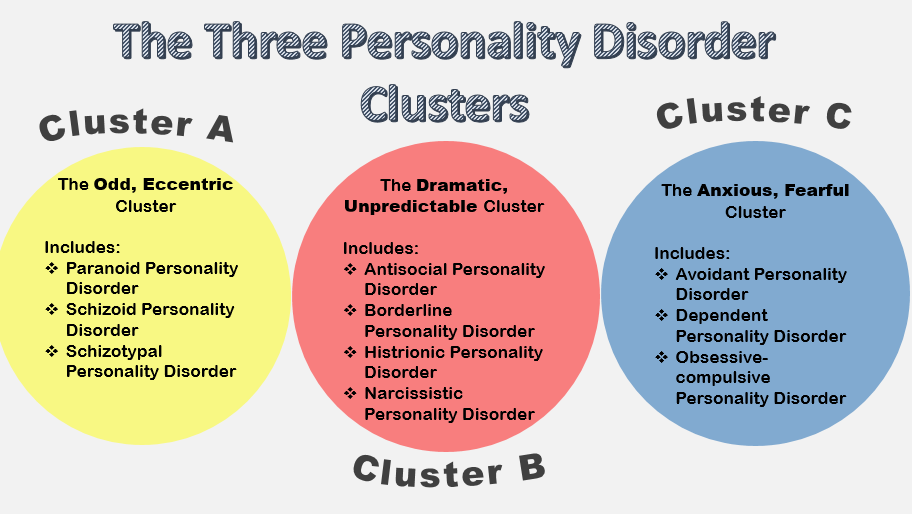 Such thoughts (physicians call them obsessional) cause anxiety, are repeated and begin to be perceived as reality.
Such thoughts (physicians call them obsessional) cause anxiety, are repeated and begin to be perceived as reality.
A person's life becomes a nightmare. An example can be given when a patient washed his hands 60 times before lunch so as not to become infected, and was still afraid. Another patient could not get to work, because he constantly returned home to check if the gas was turned on.
5. DEPENTITY
This term refers to a decrease in intelligence for various reasons. The course of the disease is usually gradual, and extremely rarely - sudden. It is characterized by fatigue, weakness, decreased performance, absent-mindedness, memory impairment. The most common diseases in this group are Alzheimer's, Pick's, Parkinson's, and Wilson's diseases.
The treatment of such brain diseases is currently faced with a number of complications. And first of all, not because it is difficult to treat, but because it is difficult to diagnose. Read: The likelihood of dementia and early aging depends on your blood type
The "Iron Lady" died at the age of 88 from Alzheimer's disease.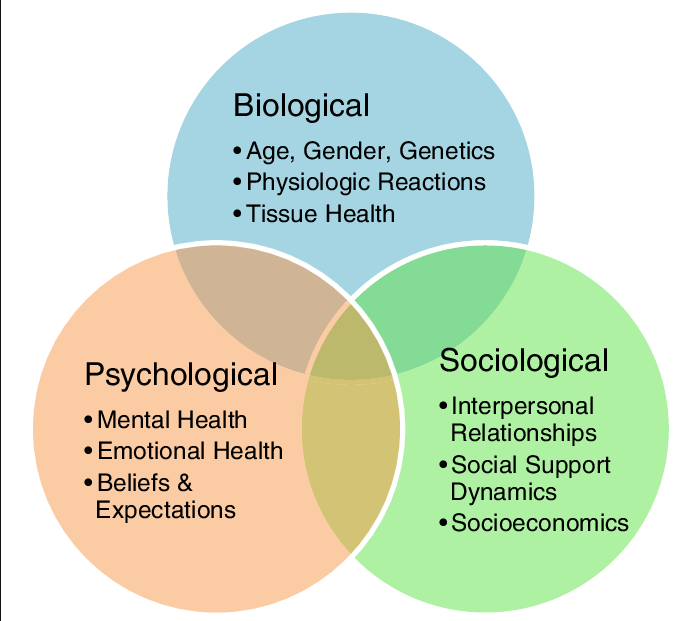 See photo gallery: Margaret Thatcher: Remembering the Iron Lady of World Politics
See photo gallery: Margaret Thatcher: Remembering the Iron Lady of World Politics
6. STRESS RESPONSE AND ADJUSTMENT DISORDER
This group of disorders is the result of tragic experiences and abrupt changes in life. There is a response to a mental trauma associated with a risk to life. It can occur after a natural disaster, the loss of a loved one, a serious crime, a social upheaval, such as a terrorist attack.
The patient again and again returns memories of the event experienced, he is haunted by anxiety, depression, sleep disturbance, sometimes aggressive tendencies or suicidal thoughts appear.
The same group includes phenomena that doctors have given the names "Vietnamese", "Afghan" or "Stockholm" syndromes. Read: 10 causes of stress in urban residents
Photo: GLOBAL LOOK PRESS
7. Neurasthenia
It is often confused with hysteria, which is a gross mistake. Neurasthenia is essentially an asthenic neurosis, it occurs as a result of exhaustion of the nervous system during prolonged mental or physical overload. And unlike hysteria, it occurs more often in men than in women. It develops with prolonged physical overstrain (when there is a lot of work, insufficient sleep, lack of rest), frequent stressful situations, personal tragedies, prolonged conflicts. Somatic diseases and chronic intoxication can contribute to the occurrence of neurasthenia.
And unlike hysteria, it occurs more often in men than in women. It develops with prolonged physical overstrain (when there is a lot of work, insufficient sleep, lack of rest), frequent stressful situations, personal tragedies, prolonged conflicts. Somatic diseases and chronic intoxication can contribute to the occurrence of neurasthenia.
Neurasthenia is accompanied by headache, feeling of weakness, fatigue, tension, insecurity, irritability, sleep disturbances, dizziness, indigestion.
Photo: GLOBAL LOOK PRESS
8. SCHIZOPHRENIA
Belongs to the category of psychoses. The disease affects several components of the psyche: mental, emotional, behavioral and the entire set of mental functions. There are different forms of schizophrenia (catatonic, simple, paranoid). Accordingly, the symptoms may vary, however, the most common are hallucinations, negativism, isolation, apathy. Read: Scientists have counted eight types of schizophrenia
At the same time, schizophrenia, although it has some hereditary relationship, cannot be called a purely genetic disease. Sometimes perfectly healthy parents without any mental family history give birth to children who, already in adolescence, fall ill with pubertal schizophrenia.
Sometimes perfectly healthy parents without any mental family history give birth to children who, already in adolescence, fall ill with pubertal schizophrenia.
Photo: Andrey GREBNEV
9. BIPOLAR DISORDER
The disease is also known as manic-depressive psychosis. A fairly common disease with alternating depressive and manic phases. Some well-known actors and singers suffered from this disease P read: Catherine Zeta-Jones again treats bipolar disorder
You can recognize the disease by first elevated mood, increased motor and speech activity of the patient, people of this type talk a lot, joke, laugh, take on a lot of things ... And then like this but sharply "fall off". They cannot concentrate. And as a result, many of their undertakings end in nothing.
10. SEXUAL DEVIATIONS
The most frequent sexual deviations are exhibitionism, voyeurism, frotterism, pathological sexual aggressiveness, transvestism, masochism, sadism, telephone hooliganism for sexual gratification.
11. EATING DISORDERS
The disease is common among girls, and today even in boys at a young age. Varieties of this disease are anorexia and bulimia. H Itite: 5 stars suffering from anorexia
Model Isabelle Karo in social advertising "No anorexia"
Read also
Scientists have found a way to cure dementia
that there were special sites in the DNA. - there are four of them, they are associated with the very skills of thinking. Accordingly, over time, these zones begin to work incorrectly, which provokes the process of dementia. This discovery will now lead to the development of new drugs for age-related dementia or methods to prevent its development (more)
A diet was created that prevented the development of Alzheimer's by 53 percent
Those who adhered strictly to the rules had a 53 percent decrease in the risk of Alzheimer's disease. For those who shirk from time to time, the risk decreased to 35 percent, which, however, is also quite a lot (further)
Age category of the site 18+
March 15, 2021
CHIEF EDITOR — OLESIA VYACHESLAVOVNA NOSOVA.
Acting EDITOR-IN-CHIEF OF THE SITE - KANSKY VICTOR FYODOROVICH.
THE AUTHOR OF THE MODERN VERSION OF THE EDITION IS SUNGORKIN VLADIMIR NIKOLAEVICH.
Messages and comments from site readers are posted without preliminary editing. The editors reserve the right to remove them from the site or edit them if the specified messages and comments are an abuse of freedom mass media or violation of other requirements of the law.
JSC "Publishing House "Komsomolskaya Pravda". TIN: 7714037217 PSRN: 1027739295781 127015, Moscow, Novodmitrovskaya d. 2B, Tel. +7 (495) 777-02-82.
Exclusive rights to materials posted on the website www.kp.ru, in accordance with the legislation of the Russian Federation for the Protection of the Results of Intellectual Activity belong to JSC Publishing House Komsomolskaya Pravda, and do not be used by others in any way form without the written permission of the copyright holder.
Acquisition of copyright and communication with the editors: kp@kp.