Different mental illnesses list
Types of mental health issues and illnesses
Mental illness is a general term for a group of illnesses that may include symptoms that can affect a person’s thinking, perceptions, mood or behaviour. Mental illness can make it difficult for someone to cope with work, relationships and other demands. The relationship between stress and mental illness is complex, but it is known that stress can worsen an episode of mental illness. Most people can manage their mental illness with medication, counselling or both.This page lists some of the more common mental health issues and mental illnesses.
Anxiety disorders
Anxiety disorders is a group of mental health disorders that includes generalised anxiety disorders, social phobias, specific phobias (for example, agoraphobia and claustrophobia), panic disorders, obsessive compulsive disorder (OCD) and post-traumatic stress disorder. Untreated, anxiety disorders can lead to significant impairment on people’s daily lives.
For more information see: Anxiety disorders.
Behavioural and emotional disorders in children
Common behaviour disorders in children include oppositional defiant disorder (ODD), conduct disorder (CD) and attention deficit hyperactivity disorder (ADHD). Treatment for these mental health disorders can include therapy, education and medication.
For more information see: Behavioural disorders in children.
Bipolar affective disorder
Bipolar affective disorder is a type of mood disorder, previously referred to as ‘manic depression’. A person with bipolar disorder experiences episodes of mania (elation) and depression. The person may or may not experience psychotic symptoms. The exact cause is unknown, but a genetic predisposition has been clearly established. Environmental stressors can also trigger episodes of this mental illness.
For more information see: Bipolar disorder.
Depression
Depression is a mood disorder characterised by lowering of mood, loss of interest and enjoyment, and reduced energy.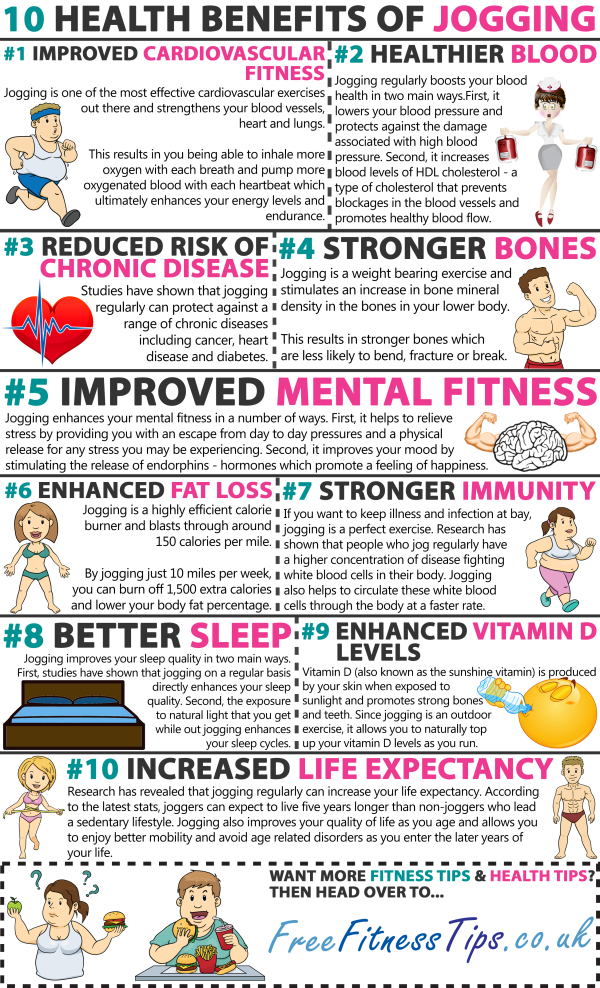 It is not just feeling sad. There are different types and symptoms of depression. There are varying levels of severity and symptoms related to depression. Symptoms of depression can lead to increased risk of suicidal thoughts or behaviours.
It is not just feeling sad. There are different types and symptoms of depression. There are varying levels of severity and symptoms related to depression. Symptoms of depression can lead to increased risk of suicidal thoughts or behaviours.
For more information see: Depression.
Dissociation and dissociative disorders
Dissociation is a mental process where a person disconnects from their thoughts, feelings, memories or sense of identity. Dissociative disorders include dissociative amnesia, dissociative fugue, depersonalisation disorder and dissociative identity disorder.
For more information see: Dissociation and dissociative disorders.
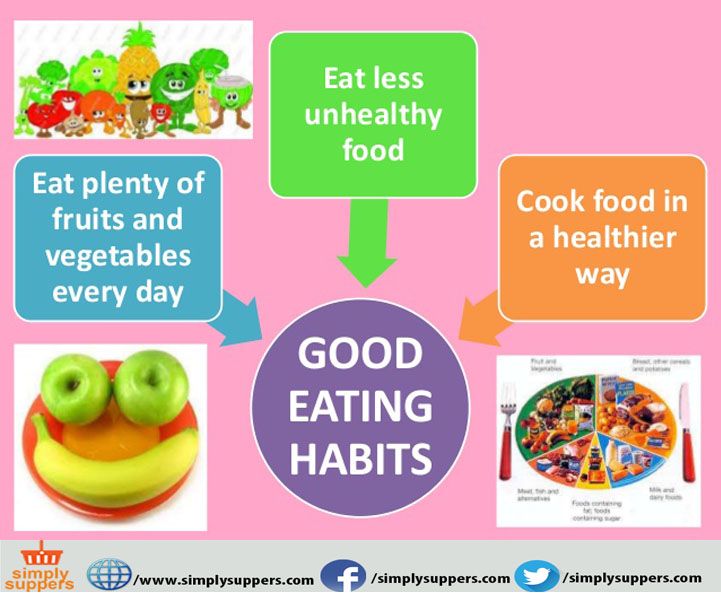
Eating disorders
Eating disorders include anorexia, bulimia nervosa and other binge eating disorders. Eating disorders affect females and males and can have serious psychological and physical consequences.
For more information see: Eating disorders.
Obsessive compulsive disorder
Obsessive compulsive disorder (OCD) is an anxiety disorder.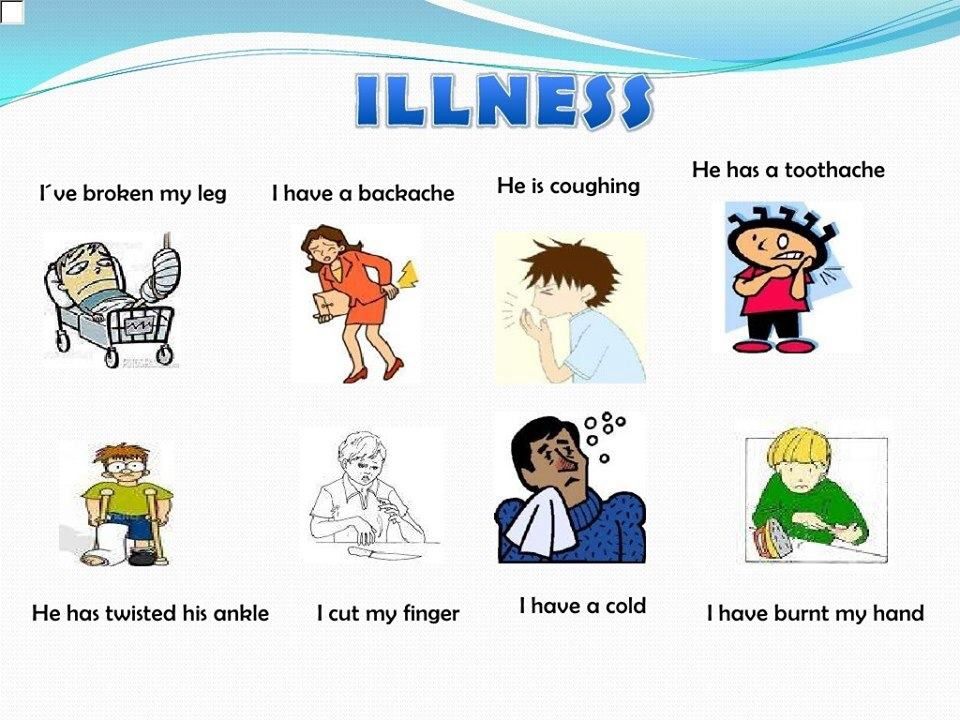 Obsessions are recurrent thoughts, images or impulses that are intrusive and unwanted. Compulsions are time-consuming and distressing repetitive rituals. Treatments include cognitive behaviour therapy (CBT), and medications.
Obsessions are recurrent thoughts, images or impulses that are intrusive and unwanted. Compulsions are time-consuming and distressing repetitive rituals. Treatments include cognitive behaviour therapy (CBT), and medications.
For more information see: Obsessive compulsive disorder.
Paranoia
Paranoia is the irrational and persistent feeling that people are ‘out to get you’. Paranoia may be a symptom of conditions including paranoid personality disorder, delusional (paranoid) disorder and schizophrenia. Treatment for paranoiainclude medications and psychological support.
For more information see: Paranoia.
Post-traumatic stress disorder
Post-traumatic stress disorder (PTSD) is a mental health condition that can develop as a response to people who have experienced any traumatic event. This can be a car or other serious accident, physical or sexual assault, war-related events or torture, or natural disasters such as bushfires or floods.
For more information see: Post-traumatic stress disorder.
Psychosis
People affected by psychosis can experience delusions, hallucinations and confused thinking.. Psychosis can occur in a number of mental illnesses, including drug-induced psychosis, schizophrenia and mood disorders. Medication and psychological support can relieve, or even eliminate, psychotic symptoms.
For more information see: Psychosis.
Schizophrenia
Schizophrenia is a complex psychotic disorder characterised by disruptions to thinking and emotions, and a distorted perception of reality. Symptoms of schizophrenia vary widely but may include hallucinations, delusions, thought disorder, social withdrawal, lack of motivation and impaired thinking and memory. People with schizophrenia have a high risk of suicide. Schizophrenia is not a split personality.
For more information see: Schizophrenia.
Where to get help
- Your GP (doctor)
- Mental health services
Who's who in mental health services
If you or someone you support is accessing treatment for a mental health condition, you will probably come across a range of mental healthcare and welfare professionals who will have a role in the treatment.
If you are unsure about the role of the person treating you, ask them to explain it to you. In some roles within mental health services, formal qualifications vary and educational backgrounds differ. It is your right to ask any private healthcare professional about their qualifications and experience. Counsellors, for example, might have skills in talking therapies for anxiety or depression but no formal medical qualifications. Psychiatrists can prescribe medications, and some might also be trained in talking therapy or counselling. A local doctor, while practising as a general practitioner, might have a specialist interest and experience in the mental health area making them more 'qualified' to help than another local doctor who does not.
The following 'who's who' list will help you understand who does what in the mental health sector.
General practitioners
Your local doctor (general practitioner or GP) can help determine if you have a mental health condition.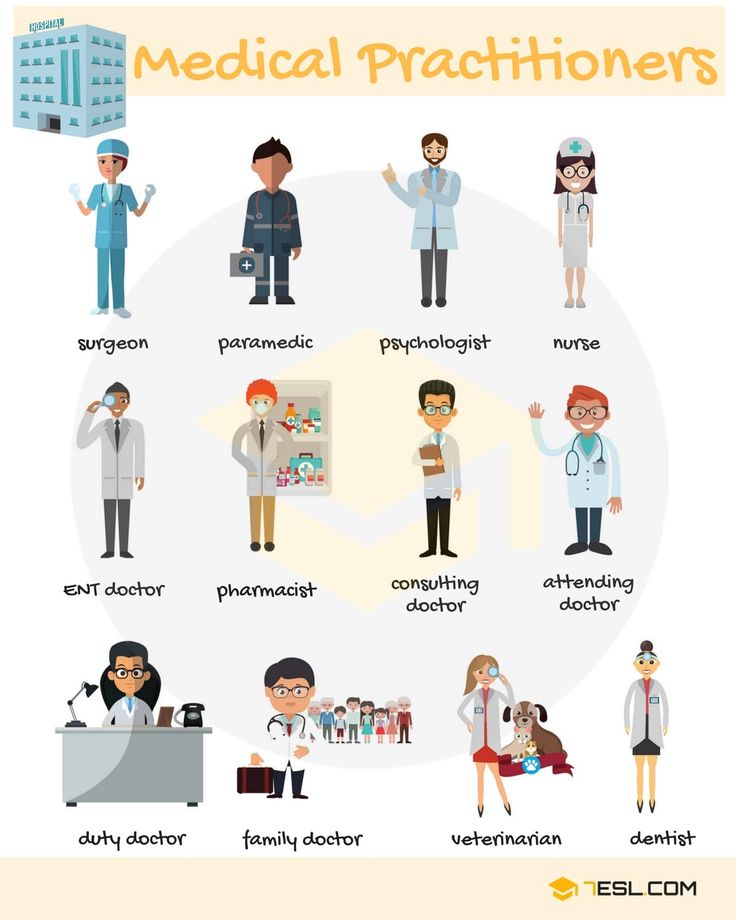 To do this, they will probably conduct a basic assessment of your mental health including a brief interview and physical examination, and they might order some laboratory tests. Your GP will ask about your mental health symptoms, your family history of mental illness and anything in your life that might be causing anxiety or stress.
To do this, they will probably conduct a basic assessment of your mental health including a brief interview and physical examination, and they might order some laboratory tests. Your GP will ask about your mental health symptoms, your family history of mental illness and anything in your life that might be causing anxiety or stress.
General practitioners hold a medical degree and, to practise in Victoria, must be registered through the Australian Health Practitioner Regulation Agency (AHPRA), with the Medical Board of Australia. To practise as a vocationally registered GP they must also be a fellow of the Royal Australian College of General Practitioners. They may also be a member of the Australian Medical Association. GP services are either partly or fully claimable through Medicare, depending on the individual GP.
If you have a mental health treatment plan written by a GP, it usually qualifies you for subsidised mental health treatment through Medicare or the government's Access to Allied Psychological Services (ATAPS) program.
GPs can write mental health treatment plans and, depending on your needs, might refer you to a counsellor, psychologist, psychiatrist or other mental health professional.
Psychologists
Psychologists study human behaviour, investigating the processes related to how people think and feel. They conduct research and provide therapy and counselling to reduce distress and to help people manage psychological problems. They help people to deal with relationship problems, trauma, eating disorders, learning difficulties, substance abuse, parenting issues, loss or grief and managing the effects of a chronic illness. Psychologists cannot prescribe medication.
Psychologists who are registered to work in Australia have completed a minimum four-year basic university program in psychology. Full registration as a professional psychologist requires a fifth and sixth year of graduate study in professional psychology.
Psychologists work in hospitals, community health services, schools, courts, prisons, the defence forces and private practice.
Psychologists practice different types of therapy, such as psychoanalysis, psychodynamic approaches, client centred approaches, cognitive behavioural therapy, and many more. You can ask your psychologist what types of therapy they are trained in, and discuss whether they are a good fit for your needs. For more information visit SANE.
You do not need a referral to see a psychologist. However, if you want to claim rebates through Medicare or to use the Access to Allied Psychological Services (ATAPS) program, you will need a mental health treatment plan, which your GP can develop. If you have private health insurance, you may be able to claim part of a psychologist’s fee, depending on your policy and level of cover.
Psychiatrists
Psychiatrists are medical doctors who have completed specialist training to help people with emotional and mental health problems. They diagnose and treat mental health issues. Psychiatrists can prescribe medication for mental health conditions, and some may also use talk-based therapies such as cognitive behavioural therapy.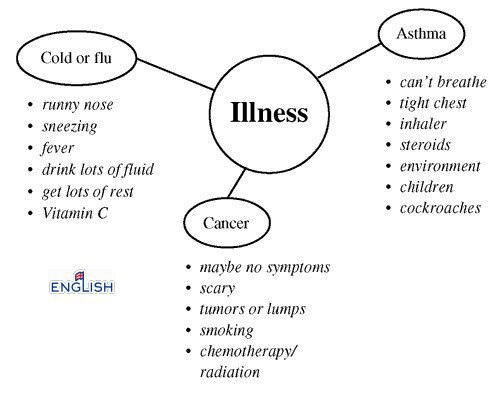
To practise in Victoria, psychiatrists must be registered with AHPRA.
You need a referral from a GP to see a psychiatrist and to claim rebates through Medicare.
Authorised psychiatrists
Authorised psychiatrists are psychiatrists who have specific powers under the Mental Health Act 2014 to decide whether a person with a mental illness should have compulsory mental health assessment or treatment.
Compulsory mental health treatment can only occur when a person is subject to a Temporary Treatment Order or Treatment Order following assessment by a medical or mental health practitioner (Assessment Order) that a person they have examined meets the criteria for an Assessment Order. This order enables an authorised psychiatrist to examine the person without their consent, to determine whether the person requires immediate treatment to stop serious deterioration or to stop serious harm to that person or another person.
Mental health nurses
Mental health nurses are specially trained (some in psychological therapies) to care for people with mental health conditions. They work with psychiatrists and other healthcare professionals to treat people with mental health issues, providing information, support and care.
They work with psychiatrists and other healthcare professionals to treat people with mental health issues, providing information, support and care.
The duties of a mental health nurse may include:
- assessment of people's mental health status
- giving medication
- assisting in behaviour modification programs and other activities
- visiting and treating people requiring mental health treatment in their homes.
Mental health nurses work in mental health units, hospitals, nursing homes or out in the community. They are registered nurses (division 1), and most have undertaken further study in mental health, earning a graduate diploma or master’s degree.
Aboriginal and Torres Strait Islander mental health workers
Aboriginal and Torres Strait Islander mental health workers are health workers who understand the mental health issues of Aboriginal people, using it to provide culturally safe and accessible mental health services.
They are generally not medically trained but might have undertaken training in mental health and psychological therapies.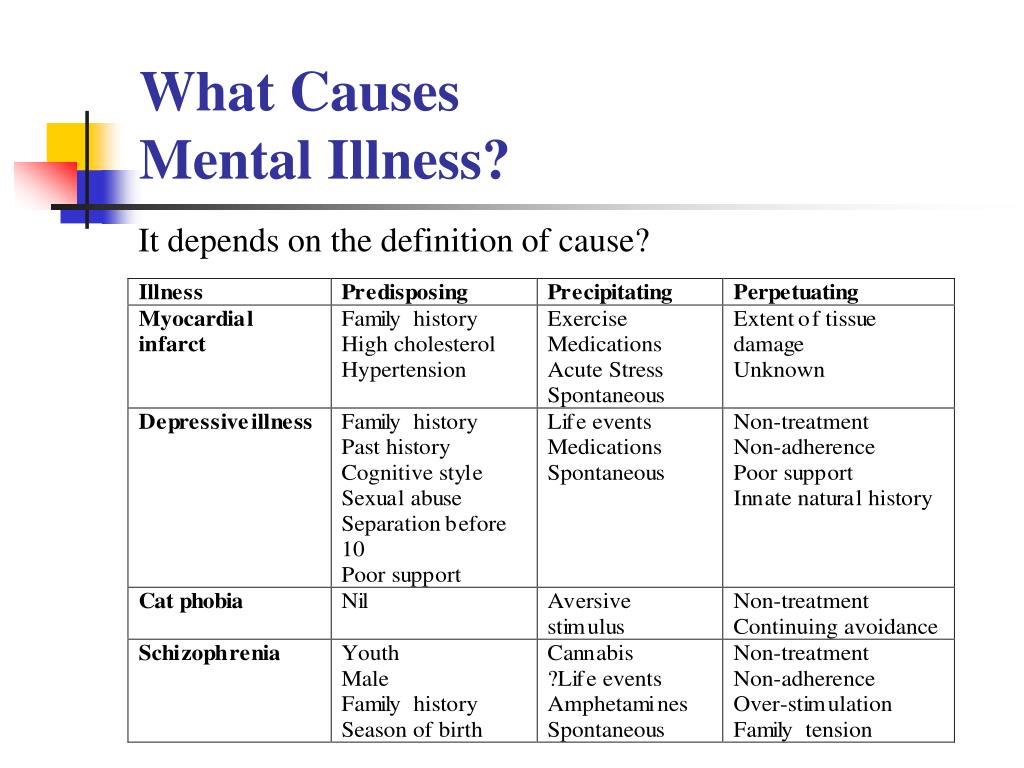 Their role often includes:
Their role often includes:
- counselling
- case management
- screening, assessment and referrals
- health promotion and education
- helping Aboriginal people to access mainstream mental health services
- supporting the families of Aboriginal people with mental health problems.
You can find Aboriginal and Torres Strait Islander mental health workers in some mental health clinics, hospitals and Aboriginal health services.
Mental health social workers work with people who are having a hard time because of a mental health issue. They support people with anxiety, for example, by helping them find ways to manage uncomfortable situations and understanding the causes of their anxiety, such as relationship issues, financial hardship and work stress.
Professional social workers hold a Bachelor of Social Work degree and you can find them in welfare agencies, hospitals, community health centres and other human services and justice organisations.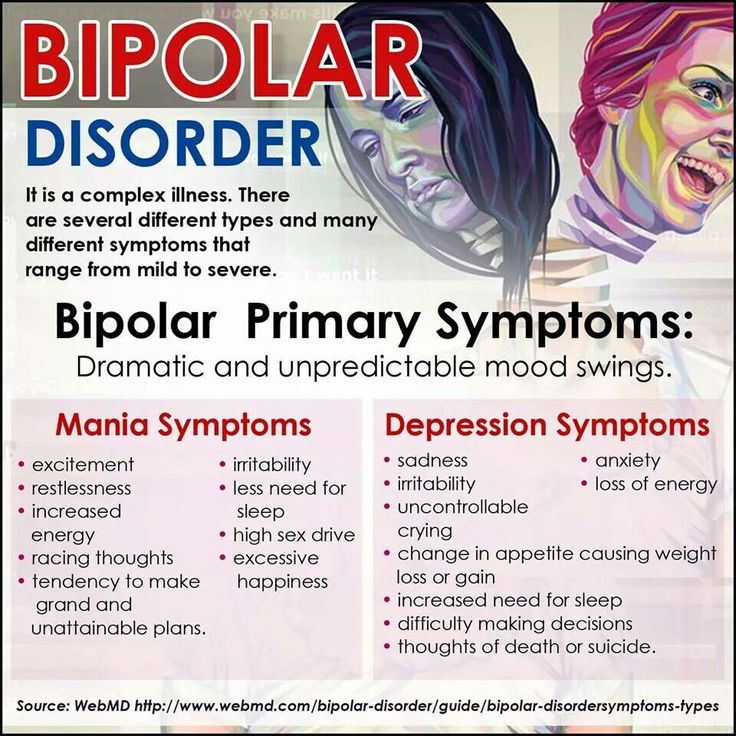 Some social workers are also qualified as counsellors.
Some social workers are also qualified as counsellors.
You can also see an eligible social worker through the Medicare-funded program Better Access, which requires you to start by getting a mental health treatment plan developed by your GP.
Counsellors
'Counsellor' is a general term for various professionals who offer some type of 'talking therapy'. A counsellor may primarily work as, for example, a nurse, social worker, occupational therapist or psychologist. Some have a specific counselling qualification such as a Bachelor or Master of Counselling degree.
Counsellors help people work through personal problems. They help people to recognise and define their emotional, health, mental and lifestyle problems and to understand themselves and their behaviour better. They help people by:
- explaining options
- setting goals
- providing therapy
- supporting them to take action.
Not all counsellors have specific training in treating mental health conditions and services offered by counsellors usually do not have a Medicare rebate available. Make sure you check that the counsellor has a qualification or has been recommended by your GP or other people experiencing the same issues as you. It is a good idea to check that the counsellor you choose to see is registered with an appropriate professional body.
Make sure you check that the counsellor has a qualification or has been recommended by your GP or other people experiencing the same issues as you. It is a good idea to check that the counsellor you choose to see is registered with an appropriate professional body.
Peer workers
Peer workers are trained mental health professionals who have their own personal experience of mental health problems and recovery. They have studied how to use personal experience in ways that are therapeutic. Peer workers do not base their work on diagnoses or standard treatments of mental illness, but instead on respect, shared responsibility and mutual agreement of what is helpful.
Peer workers can share their own experiences so that you know you are not alone, and you can explore different ways to make sense of your experiences. Research suggests that peer work can increase hope, independence and a sense of empowerment.
Peer workers are a relatively new type of mental health professional but are increasingly employed by many different types of mental health services.
Mental health occupational therapists
Occupational therapists work with people to help them to be better able to participate in everyday life, by helping people to enhance their own abilities, and by modifying the external environment. Occupational therapists who specialise in mental health have particular skills in understanding some of the ways that mental health problems might create barriers to participating in life, work and the home. They may be able to assist in developing coping strategies, building confidence and independence.
Professional occupational therapists hold a Bachelor of Occupational Therapy degree and they are required to be registered with AHPRA.
Occupational therapists work in welfare agencies, hospitals, community health centres and other human services and justice organisations. You can also see an eligible occupational therapist through the Medicare-funded program Better Access, which requires you to start by getting a mental health treatment plan developed by your GP.
Some occupational therapists have additional qualifications as counsellors.
Mental health recovery and rehabilitation workers
Mental health recovery and rehabilitation workers specialise in working with people who have developed a psychosocial disability as a result of a mental health condition. They may be qualified as social workers, psychologists, peer workers, occupational therapists, or have a Certificate IV in Mental Health (non-clinical).
Mental health recovery and rehabilitation workers offer support and rehabilitation services that aim to support people towards personal recovery. This means working with people to understand the impacts of mental health problems on their life, and developing goals that are meaningful to them.
Common areas of personal recovery include building social connectedness, finding hope, addressing the identity impacts of mental health problems, making sense of mental health experiences, finding meaning in life, and building a sense of empowerment.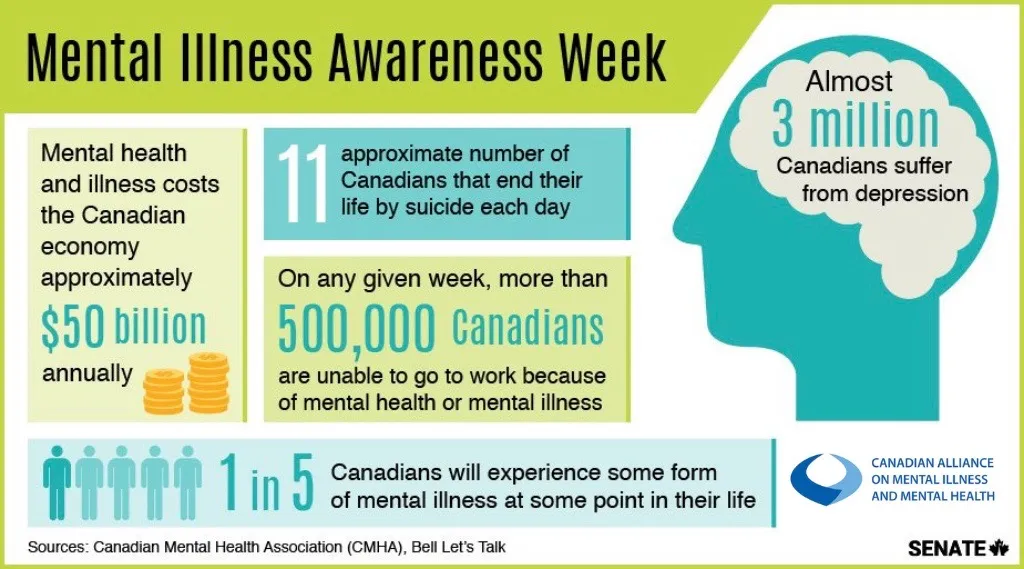 Mental health recovery and rehabilitation workers will often work with people to join or rejoin employment, and to find safe and secure housing.
Mental health recovery and rehabilitation workers will often work with people to join or rejoin employment, and to find safe and secure housing.
Mental health recovery and rehabilitation workers work in sub-acute mental health services, and in mental health community support services.
Where to get help
- Your GP (doctor)
- Mental healthcare professionals
What mental illnesses are inherited - Atlant, medical center
Are mental illnesses hereditary? This question worries many parents. After all, it is very scary to “reward” your child with a mental disorder.
How mental illness is transmitted
The fact that mental illness can be inherited has been noticed for a long time. Today, geneticists confirm: indeed, mental disorders are more likely to appear in a child in a family where a relative suffered from a similar illness. And the reason for this are violations in the structure of genes.
There is such a thing as the coefficient of hereditary risk. The higher this coefficient, the higher the likelihood that the child will inherit the disease of relatives.
The higher this coefficient, the higher the likelihood that the child will inherit the disease of relatives.
Only some mental illnesses are directly related to breakdowns in the genes, for example, Huntington's chorea, the hereditary risk coefficient of which is 5000. For comparison, for such a mental illness as schizophrenia, it is 9.
How does the degree of relationship affect hereditary diseases?
The risk of developing a mental illness depends on the degree of relationship with a sick family member and on the number of sick relatives.
The highest probability of transmission of the disease in identical twins, followed by 1st degree relationship (parents, children, brothers, sisters). In 2nd degree relatives, the risk is significantly reduced
So, with schizophrenia, which is present in the mother and father, the probability of its occurrence in children is 46%, if one parent is sick - about 13%, if the grandfather or grandmother is sick - 5%.
Which mental illnesses are most often inherited
1. Disorders of the mental development of children
- Attention deficit hyperactivity disorder (ADHD) is manifested by impulsivity, difficulty concentrating, increased motor activity. Often this disorder is combined with depression, behavioral disorders.
- Dyslexia - the inability to read, compare what is written with speech in some cases is hereditary.
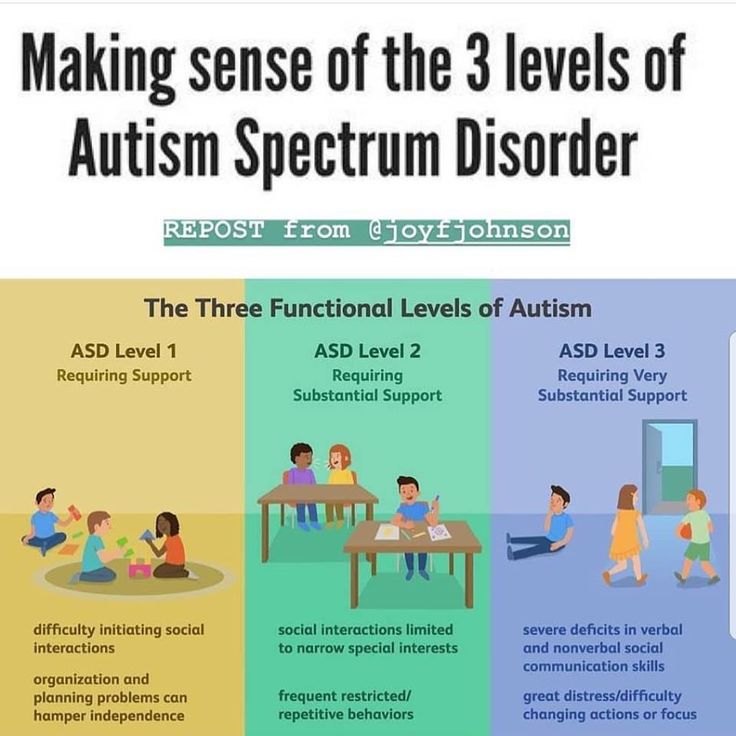
- Autism is a severe mental disorder, expressed in violation of social adaptation. An autistic child is closed, he does not want to communicate with the outside world, he exists in his personal space. He does not tolerate any change, he has his own rituals, which he strictly observes. He constantly repeats stereotypical movements (rocking, bouncing) or the same phrases.
Autism is usually diagnosed in the first three years of a child's life.
It is believed that the role of heredity in the occurrence of this disease is great.
2. Schizophrenia
This is a mental illness, which is characterized by disturbances in thinking, perception of the world, inappropriate behavior and an abnormal reaction to stimuli. The disease may be accompanied by agitation, delusions, hallucinations. Patients are prone to depression and suicidal.
As a rule, the onset of the disease falls on the age of 20-22 to 30 years.
Heredity plays a significant role in the occurrence of this disease, but other factors are no less important: complications during gestation, difficult childbirth in the mother, infections, difficult psycho-emotional situations, and even birth in winter.
3. Affective bipolar disorder
Otherwise, this mental illness is called manic-depressive psychosis. It proceeds with an alternation of phases: depression and excitement, sometimes with aggression. There may be gaps between these phases.
4. Alzheimer's disease
This disease develops after the age of 65 and is expressed first in forgetfulness, difficulty concentrating. Then there is confusion, loss of orientation in space. Irritability, unmotivated aggression appear, speech is disturbed. Dementia develops.
Then there is confusion, loss of orientation in space. Irritability, unmotivated aggression appear, speech is disturbed. Dementia develops.
Rarely enough, the disease begins earlier, and here the hereditary factor, the pathological gene, plays a significant role.
Other hereditary mental illnesses:
- epilepsy;
- psychopathy;
- alcohol dependence;
- dementia;
- Down syndrome;
- Huntington's chorea;
- "cat cry" syndrome;
- Klinefelter's syndrome.
All of these mental illnesses can be inherited. At the same time, they can appear in a family where no one has suffered from such disorders. True, the risk of disease in this case is less, but it exists. So, you can get schizophrenia in a completely “healthy” family with a probability of 1%.
If there is a risk
Many people are afraid of passing on hereditary diseases to their children (even if distant relatives suffered from them), especially mental disorders, and therefore prefer not to have a child. Is such an approach correct?
Is such an approach correct?
A hereditary disease does not mean at all that a child will definitely have it. Yes, there is such a risk, but it is also present in children from "hereditarily safe" families. Moreover, the chance of passing on a hereditary disease can be very low. It all depends on what kind of genetic disease exists in the family history, which of the relatives had a pathology, how severe the deviation was, and many other factors.
You can understand how big the risk is after passing a medical genetic examination. Therefore, in case of doubts and fears of “bad heredity”, the most correct approach would be to contact a geneticist.
Types of mental disorders
Call us
Make an appointment
Dear visitors and doctors of our Center! We congratulate you on the upcoming New Year! Health, longevity, happiness to you and your loved ones!
December 31 we are open from 10:00 to 18:00. 01, 02, 03 January - days off. From January 04, 2023, the Center operates as usual, from 10:00 to 21:00.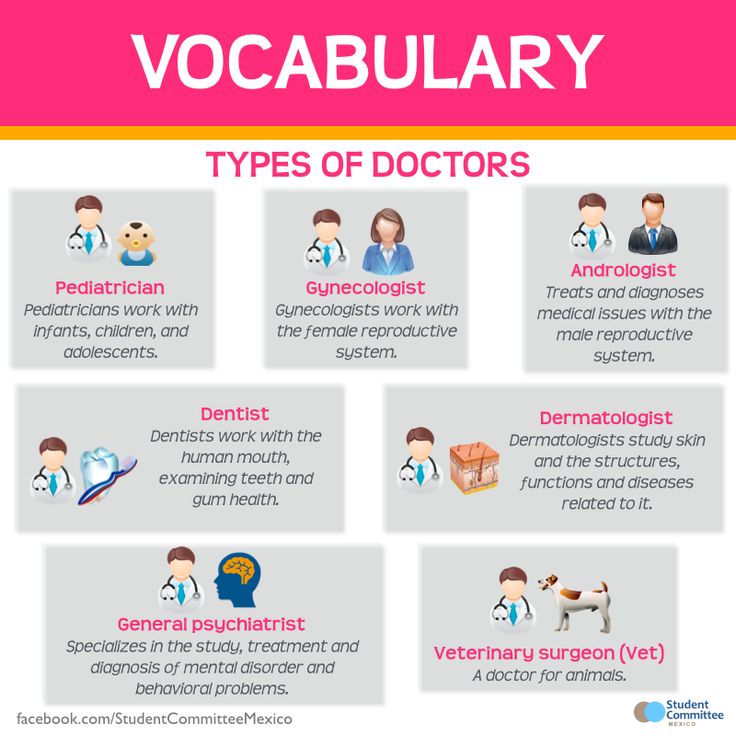
- Main page
- Psychiatry
- Types of mental disorders
- Types of mental disorders
Aggressive behavior
accompanies many mental illnesses. Manifested in hostility, threats and attacks. If these symptoms arose in a person for the first time and are generally not characteristic of him, most likely, he needs to immediately consult a psychiatrist. In other cases of aggressive behavior (especially - unreasonable) consultation with a psychiatrist is also desirable.
Apathy of the mentally ill
state of indifference, detachment, loss of interest and desire to do something. It is often a manifestation of depression, while it is painfully experienced. If apathy does not burden the patient, then this may be a manifestation of another mental or neurological disease.
Autism
Autism is a condition in which a person lives in an internal or unreal (virtual) world, and not in real events. Close such a person is seen as closed, uninterested in what is happening around, closed.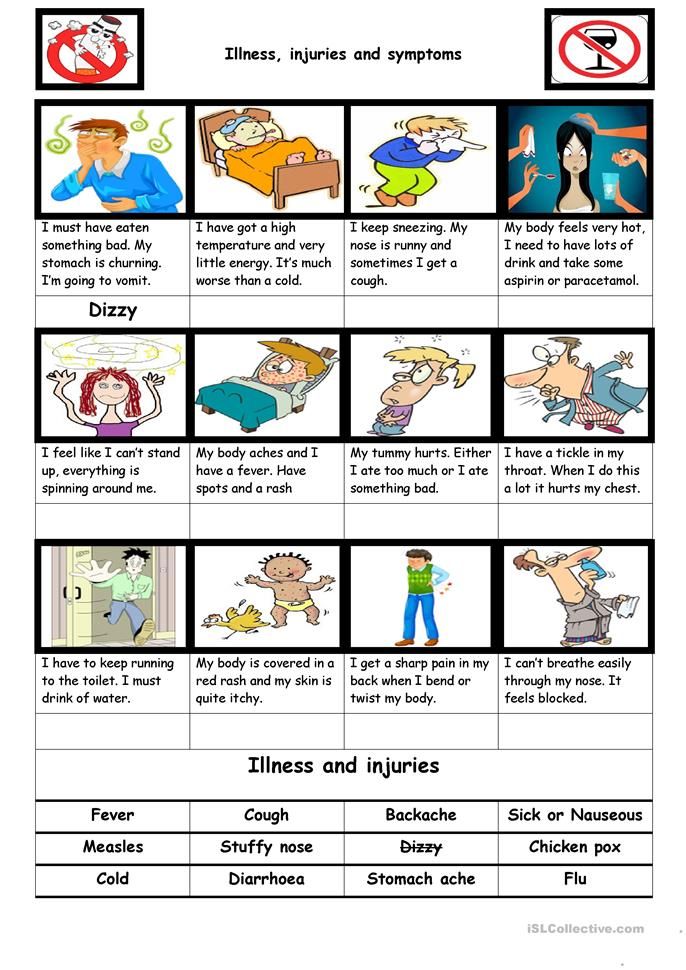 The world of fantasy overlaps reality, and therefore a person with autism is cold and indifferent to the people around him, including those close to him. An autistic person is often not burdened by the difficulties of social interaction and communication disorders. Autism occurs both in childhood and in adulthood, and in adults it can be not only a “continuation” of childhood autism, but also a consequence of a developed mental disorder.
The world of fantasy overlaps reality, and therefore a person with autism is cold and indifferent to the people around him, including those close to him. An autistic person is often not burdened by the difficulties of social interaction and communication disorders. Autism occurs both in childhood and in adulthood, and in adults it can be not only a “continuation” of childhood autism, but also a consequence of a developed mental disorder.
Delirium tremens (delirium)
occurs mainly in patients with alcoholism, at the second or third stage of the disease. It is important to note that delirium occurs more often not in intoxication, but on the 2nd-3rd day of abstinence from alcohol after drinking (at the peak of the withdrawal syndrome). It is characterized by confusion, increased body temperature, disorientation, agitation, vision of various hallucinatory images. For patients with delirium tremens, hallucinatory images of moving animals (running rats, cockroaches, gnomes, etc. ) are characteristic. Patients attract attention to themselves by their behavior: they are agitated, excited, try to catch hallucinatory images or brush them off, shake them off themselves, often talk to them.
) are characteristic. Patients attract attention to themselves by their behavior: they are agitated, excited, try to catch hallucinatory images or brush them off, shake them off themselves, often talk to them.
Delirium tremens is also possible in non-drinkers, especially in children and the elderly with diseases that occur with a high temperature. Thus, delirium tremens is a sign of intoxication of the body.
Insomnia
in chronically current mental disorders is an indicator of deterioration in mental well-being, since it often appears before all other symptoms.
Crazy ideas (strange judgments, delirium)
are most often perceived by close and surrounding people as strange judgments that do not correspond to reality. At the same time, a person with delusions cannot be persuaded, even if he does not know what to object to attempts to persuade him. Crazy ideas don't need proof. It is rather "knowledge", conviction. Because of this, the behavior of a person with delusional ideas is determined by the content of these ideas. According to the content, the main forms of delusions can be divided into delusions of persecution (what is popularly called “persecution mania”: the patient is pursued by special services or other organizations, they try to poison or rob relatives or neighbors; people on the street somehow in a special way, look unfriendly and whisper about him), delusions of grandeur (the patient is the heir to the royal family, the inventor of the time machine or the law of immortality, the ruler of the world, sometimes the messenger of God or God himself, or the devil, etc.) and delusions of self-abasement (accusing oneself of sins, numerous errors, delirium of a physical defect). A patient with delusional judgments needs to be treated by a psychiatrist.
According to the content, the main forms of delusions can be divided into delusions of persecution (what is popularly called “persecution mania”: the patient is pursued by special services or other organizations, they try to poison or rob relatives or neighbors; people on the street somehow in a special way, look unfriendly and whisper about him), delusions of grandeur (the patient is the heir to the royal family, the inventor of the time machine or the law of immortality, the ruler of the world, sometimes the messenger of God or God himself, or the devil, etc.) and delusions of self-abasement (accusing oneself of sins, numerous errors, delirium of a physical defect). A patient with delusional judgments needs to be treated by a psychiatrist.
Excitement or agitation
frequent and rather dangerous signs of mental disorders. Accompany anxiety, depression, psychotic states. With motor arousal in depressed patients, one should be on the alert: suicidal actions are possible.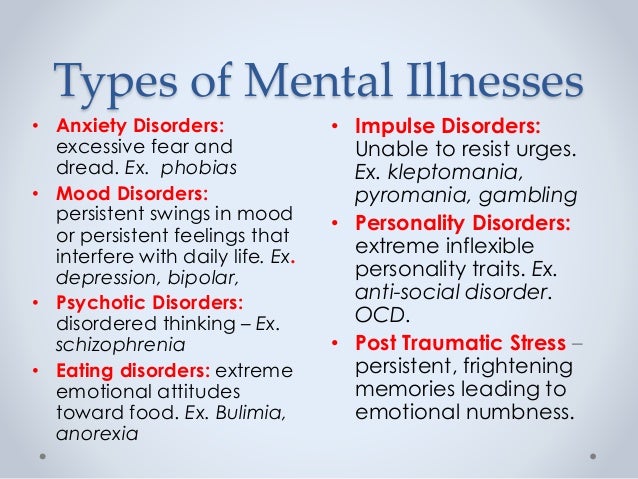 You should also be especially attentive to patients with psychotic arousal: impulsive (unpredictable), including aggressive actions are frequent, which can be dangerous both for the patient and for his environment.
You should also be especially attentive to patients with psychotic arousal: impulsive (unpredictable), including aggressive actions are frequent, which can be dangerous both for the patient and for his environment.
Hallucinations
perception of something that is not really there. Hallucinations are:
- visual (a person "sees" something that is not there: animals running around the house, people, paintings, sometimes whole panoramas: landscapes, battles),
- auditory (a person "hears" extraneous sounds - music, rustles , voices; at the same time, sounds can be localized both in external space: from the corner of the room, behind the wall, from the street, and inside the head, less often - another part of the body),
- olfactory (perception of foreign odors, more often - unpleasant)
- gustatory (strange, often unpleasant taste sensations)
- tactile (for example, sensation on the skin of "crawling" insects; accompanied by scratching, is a sign of serious intoxication)
Dementia (dementia)
, deterioration in the ability to judge and infer.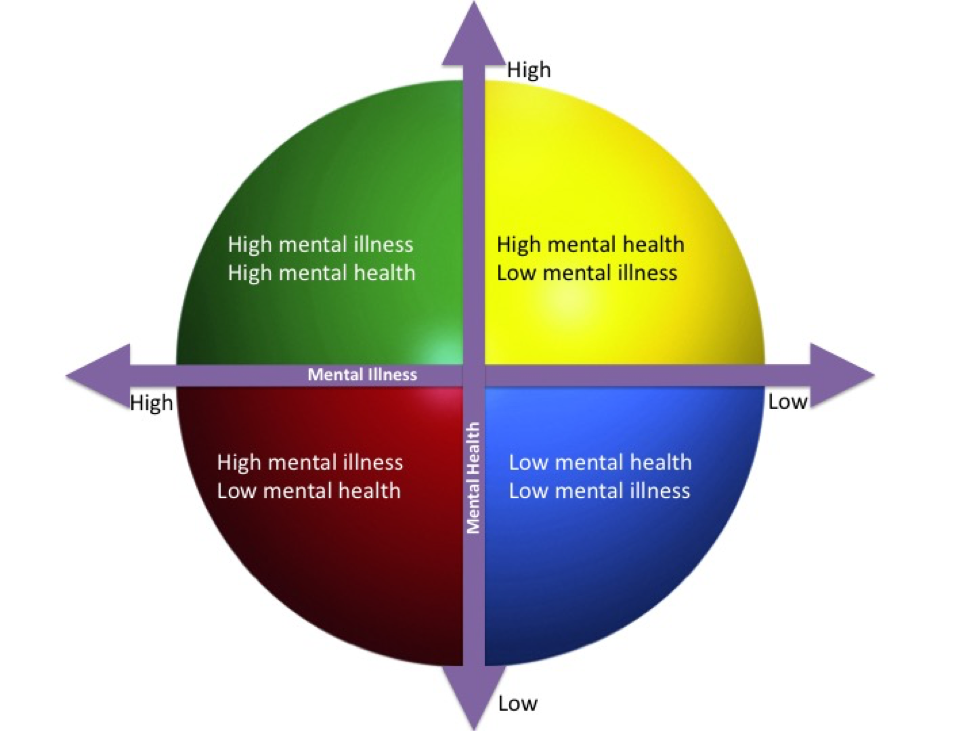 It usually occurs in old age. It can begin imperceptibly: with difficulty remembering words, narrowing the scope of attention, a slight change in mood (quick transitions from tearfulness to joy and back). The character gradually changes: the person becomes more stubborn, but at the same time more suggestible. The vocabulary is depleted, the stock of knowledge is depleted. The most common cause of dementia is damage to the cerebral vessels by an atherosclerotic process, as a result of which the vessels become narrower and blood flow to the brain tissues worsens. Having noticed in time, such changes can be stopped by properly selected therapy (which will also be the prevention of strokes). However, you should be careful if someone close to you has such changes in adulthood and unfolds very quickly: this may be a more complex disease (for example, Alzheimer's disease).
It usually occurs in old age. It can begin imperceptibly: with difficulty remembering words, narrowing the scope of attention, a slight change in mood (quick transitions from tearfulness to joy and back). The character gradually changes: the person becomes more stubborn, but at the same time more suggestible. The vocabulary is depleted, the stock of knowledge is depleted. The most common cause of dementia is damage to the cerebral vessels by an atherosclerotic process, as a result of which the vessels become narrower and blood flow to the brain tissues worsens. Having noticed in time, such changes can be stopped by properly selected therapy (which will also be the prevention of strokes). However, you should be careful if someone close to you has such changes in adulthood and unfolds very quickly: this may be a more complex disease (for example, Alzheimer's disease).
Dysmorphophobia / dysmorphomania
experiences, the content of which is the belief in one's own physical inferiority: a cosmetic defect, overweight, bad smell, in a word, a repulsive appearance.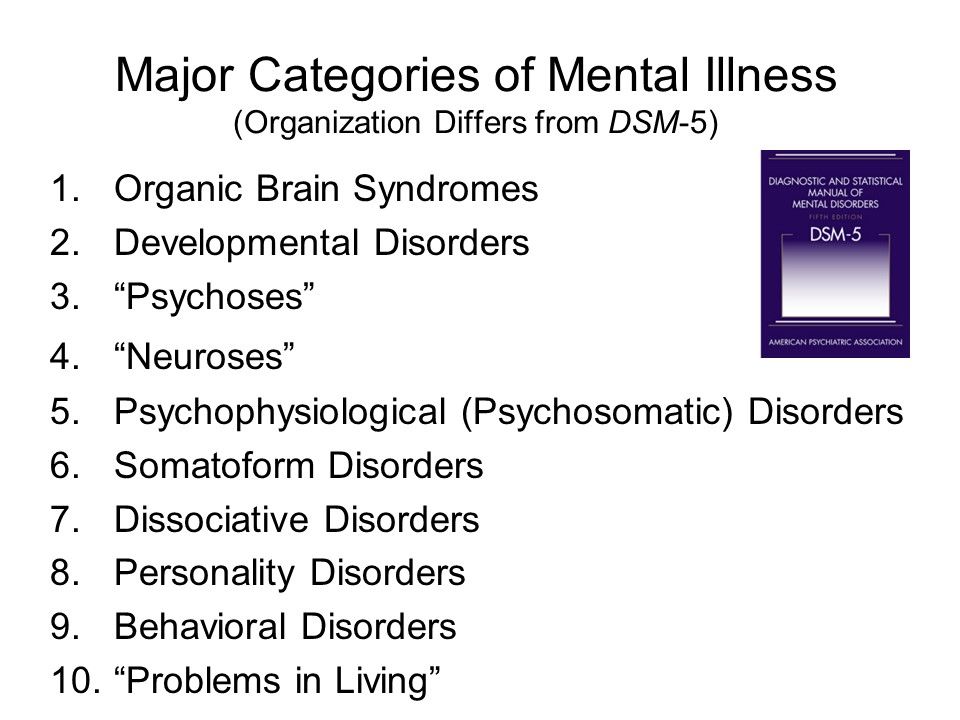 If a defect in appearance really does take place, and in a person’s life this circumstance is predominant, then we are talking about dysmorphophobia (a neurotic level of disorder). If there is actually no defect in appearance, or it is, but not so significant, and at the same time the person is downright convinced of his own ugliness, is seized by ideas of a physical defect, goes to doctors and even undergoes surgery with plastic surgeons, or falls into anorexia ( when convinced of excessive fullness), then here we are talking about dysmorphomania (delusional level of disorders).
If a defect in appearance really does take place, and in a person’s life this circumstance is predominant, then we are talking about dysmorphophobia (a neurotic level of disorder). If there is actually no defect in appearance, or it is, but not so significant, and at the same time the person is downright convinced of his own ugliness, is seized by ideas of a physical defect, goes to doctors and even undergoes surgery with plastic surgeons, or falls into anorexia ( when convinced of excessive fullness), then here we are talking about dysmorphomania (delusional level of disorders).
Hypochondria
state of increased concern about one's health. In this case, the disease of the body may or may not be present. A person suffering from hypochondria, as a rule, is afraid of a specific disease, but can also "generally" feel sick and "find" various diseases in himself (Moliere's "imaginary patient"). He constantly listens to his inner feelings and cannot experience pleasure simply from the process of life.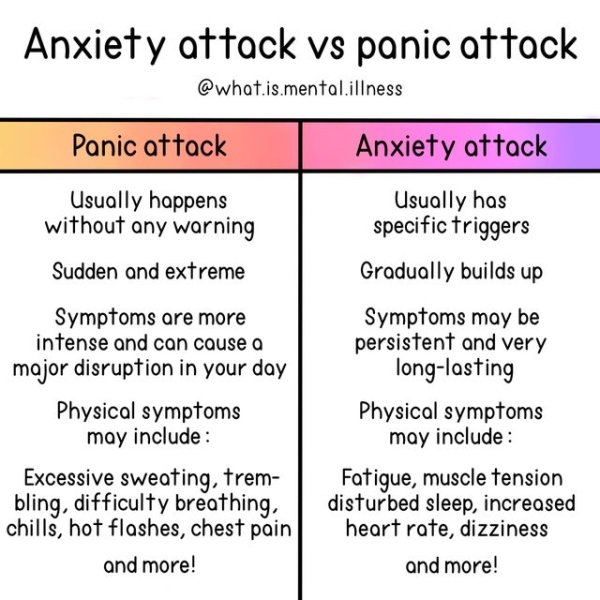 In general, hypochondria can be described as "the experience of Illness."
In general, hypochondria can be described as "the experience of Illness."
Treatment of anorexia
stubborn desire to limit oneself in food intake in order to lose weight. Often accompanied by the induction of artificial vomiting after eating, overly active physical exercises, taking large doses of laxatives. It occurs both with increased and with normal body weight. It is observed more often in girls. It is important to note that at first, anorexic behavior is carefully hidden from others, and is recognized by loved ones already at the stage of severe exhaustion.
Treatment of bulimia
How do you know if a person has bulimia? Often a person does not admit to the last that he overeats, tries to keep his addiction a secret. He is sure that he can solve the problem of nutrition on his own, by an effort of will. Signs of bulimia. Wolf hunger is a condition in which there is an uncontrolled intake of a huge amount of food. The lack of selectivity in food is characteristic, while saturation is not felt. As a rule, it occurs after a period of strict food abstinence, and, in fact, is the “back side” of anorexia.
As a rule, it occurs after a period of strict food abstinence, and, in fact, is the “back side” of anorexia.
Treatment of chronic depression
Not all depression can be cured by psychotherapy alone. Sometimes a temporary intake of specially selected drugs is required. Signs of the severity of depression are: suicidal tendencies, a feeling of despair, self-accusatory statements, anxious arousal, a feeling of general bodily change, physically experienced longing, as well as a painful loss of emotions (love, joy, compassion).
Persecution mania
without good reason are signs of a mental disorder. Such patients often hide their experiences, and then these disorders can be suspected by their behavior: a wary look, anxiety, fearfulness, absent-mindedness, window coverings, listening to something.
Unexplained somatic complaints
it happens (and more often lately) that a person feels physically ill, but no doctor finds any pathology in him.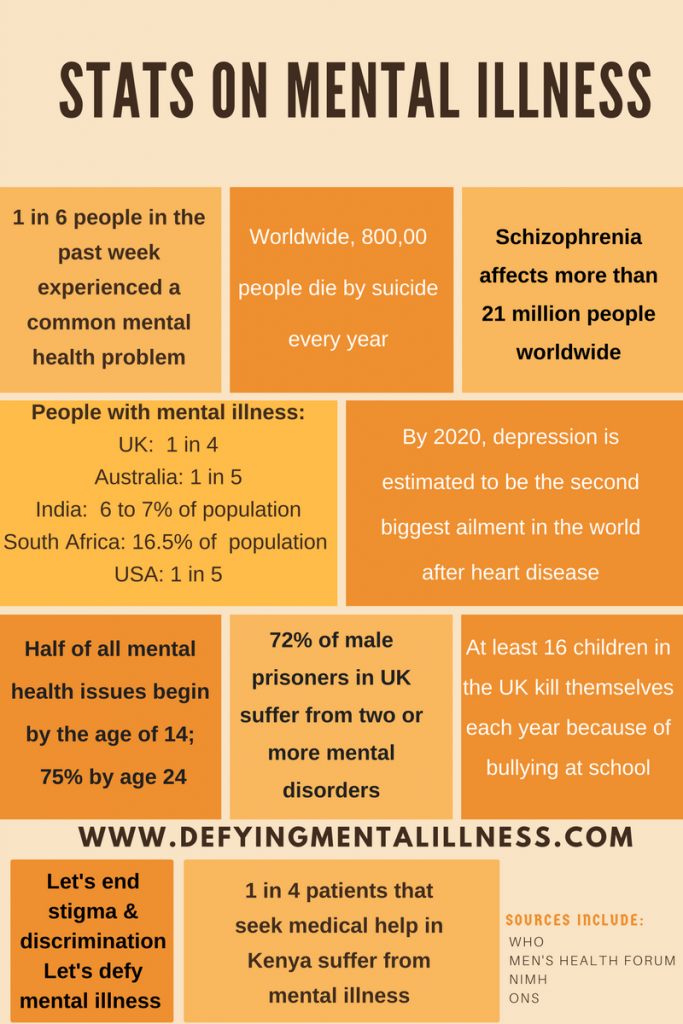 In this case, consultation with a psychiatrist is necessary: depression, neurosis, and an unresolved internal conflict may be hidden behind inexplicable somatic complaints.
In this case, consultation with a psychiatrist is necessary: depression, neurosis, and an unresolved internal conflict may be hidden behind inexplicable somatic complaints.
Sloppiness (neglect of hygiene)
occurs in patients with depression, psychoses, as well as in chronically current mental illnesses (schizophrenia, progressive dementia).
Fatigue
Fatigue can be a sign of both physical illness and mental illness. It is often noted in disorders of the depressive circle, while the patient may not feel a noticeable decrease in mood, but feels increasing lethargy, fatigue, inability to cope with the usual stress.
Loss of memory
is typical for the elderly, as well as those who have suffered severe traumatic brain injury, patients with alcoholism. It is a sign of a brain disease (vascular damage by atherosclerosis, atrophic processes in the cerebral cortex, past brain injuries, alcohol intoxication).
In vascular diseases in the elderly, forgetfulness of current and recent events and facts is characteristic, inability to learn new things.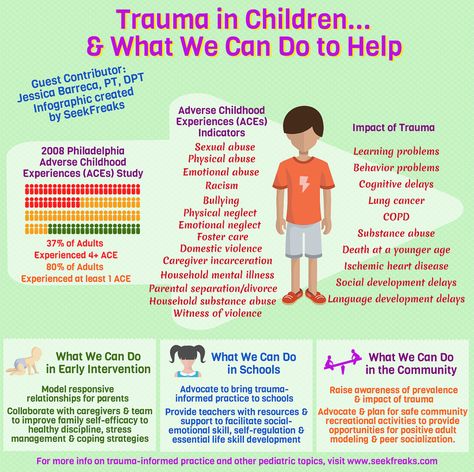 At the same time, the memory of long-standing events can remain intact for a very long time.
At the same time, the memory of long-standing events can remain intact for a very long time.
With atrophic processes in the brain, memory loss can be very rapid and abrupt. In this case, the onset of the disease in adulthood (45-55 years) is possible. In such cases, you should not delay contacting a specialist.
Psychosis
is a rather severe disorder of mental activity, the treatment of which is carried out mainly by medication. Family members of the affected person may seek help for unexplained behavioral changes, including bizarre or threatening behavior (withdrawal, suspicion, threats). Signs that should alert in terms of the development of a psychotic state: hallucinations (false or imagined sensations, for example, perceiving voices when no one is around), delusions (uncorrectable deliberately false beliefs, for example, the patient may be sure that he is being poisoned neighbors, that he receives messages from television or that he is being watched in a special way), agitation or unusual behavior, strange statements, sudden changes or instability of the emotional state. It should be noted that upon leaving the psychotic state, patients need psychotherapeutic assistance aimed at forming a critical attitude towards their disorders, improving socialization, and learning to recognize the first signs of a deterioration in mental well-being (prevention of recurrent psychosis).
It should be noted that upon leaving the psychotic state, patients need psychotherapeutic assistance aimed at forming a critical attitude towards their disorders, improving socialization, and learning to recognize the first signs of a deterioration in mental well-being (prevention of recurrent psychosis).
Latent depression
acts not as a distinct depression of mood and other mental functions, but as an internal bodily ill-being affecting various organs, functions, systems. Thus, depression can disguise itself as diseases of the cardiovascular, gastrointestinal, respiratory, and nervous systems. The well-known “pain of unclear etiology” (a diagnosis often encountered in the practice of therapists) often has the same nature.
Anguish
an oppressive painful feeling, which is often experienced as a "tightness", heaviness in the chest. Longing is much more intense than such worldly emotions as sadness or sadness. It often happens with depression and can occur without a significant reason.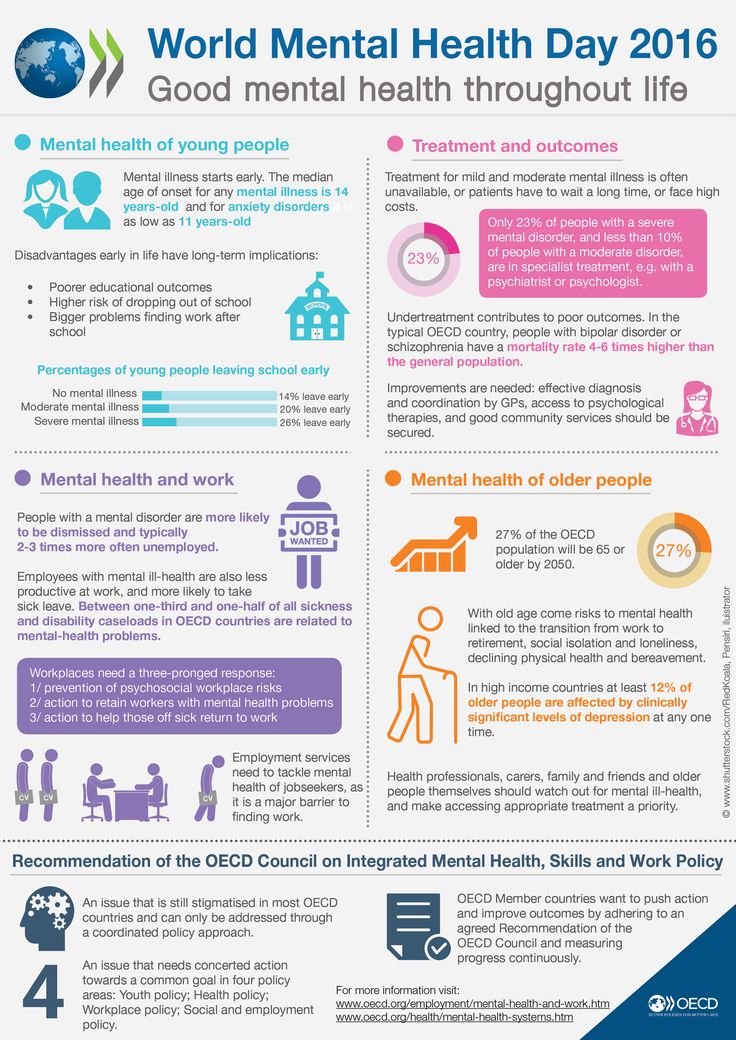
Anxiety in psychiatry
Uncertainty, suspense, feeling that something is about to happen. In other words, it is an emotional experience characterized by discomfort from the uncertainty of perspective. This is the most important human emotion, closely related to the need for security. Anxiety is sometimes felt bodily, like itching, excitement in the chest, internal trembling, and is often combined with motor excitement.
Epileptic seizure
in its most typical form is characterized by an abrupt onset: a person screams, loses consciousness, falls, then sharply strains, sometimes turns blue, followed by convulsions. After a seizure, a person is usually lethargic, lethargic and drowsy. This is the so-called convulsive seizure. However, often epileptic seizures are non-convulsive in nature, occur without a fall and may escape the attention of the patient's relatives. Signals indicating the need to see a doctor are:
- any sharp falls with loss of consciousness (even without convulsions),
- a tendency to suddenly “freeze” and “turn off” (sometimes for seconds, while stereotypical movements of the arms, head, facial muscles of the face are possible; this feature can be observed during a conversation , performing everyday activities),
- loss of memory of some events, facts, when a person was not drunk, could walk, perform some actions, which later he cannot remember anything.