Dealing with a manic person
Helping Someone with Bipolar Disorder
bipolar disorder
Dealing with a loved one’s bipolar disorder isn't easy. This guide will help you navigate the challenges and support your friend or family member.
How can you help someone with bipolar disorder?
Dealing with the ups and downs of bipolar disorder can be difficult—and not just for the person with the illness. The moods and behaviors of a person with bipolar disorder affect everyone around—especially family members and close friends. It can put a strain on your relationship and disrupt all aspects of family life.
During a manic episode, you may have to cope with reckless antics, outrageous demands, explosive outbursts, and irresponsible decisions. And once the whirlwind of mania has passed, it often falls on you to deal with the consequences. During episodes of depression, you may have to pick up the slack for a loved one who doesn’t have the energy to meet responsibilities at home or work.
The good news is that most people with bipolar disorder can stabilize their moods with proper treatment, medication, and support. Your patience, love, and understanding can play a significant part in your loved one’s treatment and recovery. Often, just having someone to talk to can make all the difference to their outlook and motivation.
But caring for a person with bipolar disorder can also take a toll if you neglect your own needs, so it’s important to find a balance between supporting your loved one and taking care of yourself.
Other ways to help someone with bipolar disorder
You can also support your loved one by:
Learning about bipolar disorder. Learn everything you can about the symptoms and treatment options. The more you know about bipolar disorder, the better equipped you'll be to help your loved one and keep things in perspective.
Encouraging the person to get help. The sooner bipolar disorder is treated, the better the prognosis, so urge your loved one to seek professional help right away. Don't wait to see if they will get better without treatment.
Being understanding. Let your friend or family member know that you're there if they need a sympathetic ear, encouragement, or assistance with treatment. People with bipolar disorder are often reluctant to seek help because they don't want to feel like a burden to others, so remind the person that you care and that you'll do whatever you can to help.
Showing patience. Getting better takes time, even when a person is committed to treatment. Don't expect a quick recovery or a permanent cure. Be patient with the pace of recovery and prepare for setbacks and challenges. Managing bipolar disorder is a lifelong process.
The importance of support in bipolar disorder recovery
People with bipolar disorder do better when they have support from family members and friends. They tend to recover more quickly, experience fewer manic and depressive episodes, and have milder symptoms.
Bipolar disorder and the family
Living with a person who has bipolar disorder can cause stress and tension in the home. On top of the challenge of dealing with your loved one's symptoms and their consequences, family members often struggle with feelings of guilt, fear, anger, and helplessness. Ultimately, the strain can cause serious relationship problems. But there are better ways to cope.
On top of the challenge of dealing with your loved one's symptoms and their consequences, family members often struggle with feelings of guilt, fear, anger, and helplessness. Ultimately, the strain can cause serious relationship problems. But there are better ways to cope.
The first step to successfully dealing with bipolar disorder is for families to learn to accept the illness and its difficulties. When you're feeling frustrated or guilty, remember that bipolar disorder isn't anyone's fault. Accepting bipolar disorder involves acknowledging that things may never again be “normal.”
Treatment can make a huge difference for your loved one, but it may not take care of all symptoms or impairments. To avoid disappointment and resentments, it's important to have realistic expectations. Expecting too much of your family member can be a recipe for failure. On the other hand, expecting too little can also hinder their recovery, so try to find a balance between encouraging independence and providing support.
With over 25,000 licensed counselors, BetterHelp has a therapist that fits your needs. Sign up today and get matched.
GET 20% OFF
Tips for coping with bipolar disorder in the family
Accept your loved one's limits. Your loved one with bipolar disorder can't control their moods. They can't just snap out of a depression or get a hold of themselves during a manic episode. Neither depression nor mania can be overcome through self-control, willpower, or reasoning. So telling your loved one to “Stop acting crazy” or to “Look on the bright side” won't help.
Accept your own limits. You can't rescue your loved one with bipolar disorder, nor can you force them to take responsibility for getting better. You can offer support, but ultimately, recovery is in the hands of the person with the illness.
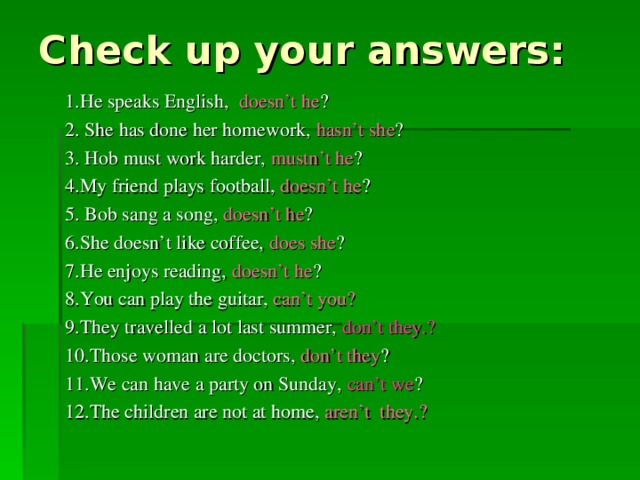
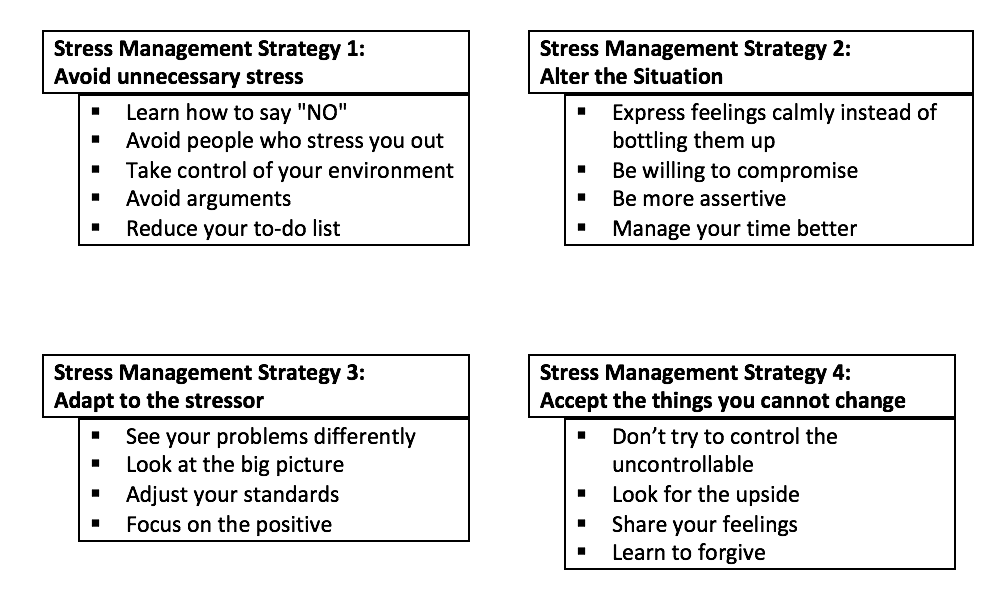
Reduce stress. Stress makes bipolar disorder worse, so try to find ways to reduce stress in your loved one's life. Ask how you can help and volunteer to take over some of the person's responsibilities if needed. Establishing and enforcing a daily routine—with regular times for getting up, having meals, and going to bed—can also reduce family stress.
Ask how you can help and volunteer to take over some of the person's responsibilities if needed. Establishing and enforcing a daily routine—with regular times for getting up, having meals, and going to bed—can also reduce family stress.
Communicate openly. Open and honest communication is essential to coping with bipolar disorder in the family. Share your concerns in a loving way, ask your loved one how they're feeling, and make an effort to truly listen—even if you disagree with your loved one or don't relate to what's being said.
Supporting a person with bipolar disorder
What you can say that helps:
- “You're not alone in this. I'm here for you.”
- “I understand that it's your illness that causes these thoughts and feelings.”
- “You may not believe it now, but the way you're feeling can and will change.”
- “I may not be able to understand exactly how you feel, but I care about you and want to help and support you.”
- “You are important to me.
 Your life is important to me.”
Your life is important to me.”
Convincing a person with bipolar disorder to see a doctor
Aside from offering emotional support, the best way to help your loved one with bipolar disorder is by encouraging and supporting treatment. Often, that can be more of a challenge than it sounds. Since people with bipolar disorder tend to lack insight into their condition, it's not always easy to get them to a doctor. When your loved one is manic, they feel great and don't realize there's a problem. When your loved one is depressed, they may recognize something's wrong, but often lack the energy to seek help.
If your loved one won't acknowledge the possibility of bipolar disorder, don't argue about it. The idea may be frightening to them, so be sensitive. Suggest a routine medical checkup instead, or a doctor's visit for a specific symptom, such as insomnia, irritability, or fatigue—then privately call ahead to tell the doctor of your concerns about bipolar disorder.
[Read: How to Help Someone with Mental Illness Accept Treatment]
Things you can say that might help:
- “Bipolar disorder is a real illness, like diabetes.
 It requires medical treatment.”
It requires medical treatment.” - “You're not to blame for bipolar disorder. You didn't cause it. It's not your fault.”
- “You can feel better. There are many treatments that can help.”
- “When bipolar disorder isn't treated, it usually gets worse.”
Supporting a loved one during bipolar disorder treatment
Once your friend or family member agrees to see a doctor, you can help by being a partner in treatment. Your support can make a big difference in their treatment success, so offer to be involved in any way your loved one wants or needs.
Things you can do to support a loved one's bipolar disorder treatment:
- Find qualified doctors and therapists.
- Set up appointments and go along.
- Offer your insights to the doctor.
- Monitor your loved one's moods.
- Learn about their medications.
- Track treatment progress.
- Watch for signs of relapse.
- Alert the doctor to problems.
Encourage your loved one to take bipolar disorder medication
Medication is the cornerstone of treatment for bipolar disorder, and most people need it to regulate their moods and avoid relapse. Despite the need for medication, many people with bipolar disorder stop taking it. Some quit because they're feeling better, others because of side effects, and yet others because they enjoy the symptoms of mania. People who don't think they have a problem are particularly likely to stop taking medication.
Despite the need for medication, many people with bipolar disorder stop taking it. Some quit because they're feeling better, others because of side effects, and yet others because they enjoy the symptoms of mania. People who don't think they have a problem are particularly likely to stop taking medication.
You can help your loved one stay on track by emphasizing the importance of medication and making sure they take all prescriptions as directed. Also encourage your loved one to speak to their doctor about any bothersome side effects.
Side effects can be very unpleasant if the dose of the medication is too low or too high, but a change in medication or dosage may solve the problem. Remind your loved one that abruptly stopping medication is dangerous.
Even if your loved one with bipolar disorder is committed to treatment, there may be times when their symptoms get worse. Take action right away if you notice any troubling symptoms or mood changes. Point out the emerging bipolar symptoms to your loved one and alert the doctor. With swift intervention, you may be able to prevent an episode of mania or depression from developing fully.
With swift intervention, you may be able to prevent an episode of mania or depression from developing fully.
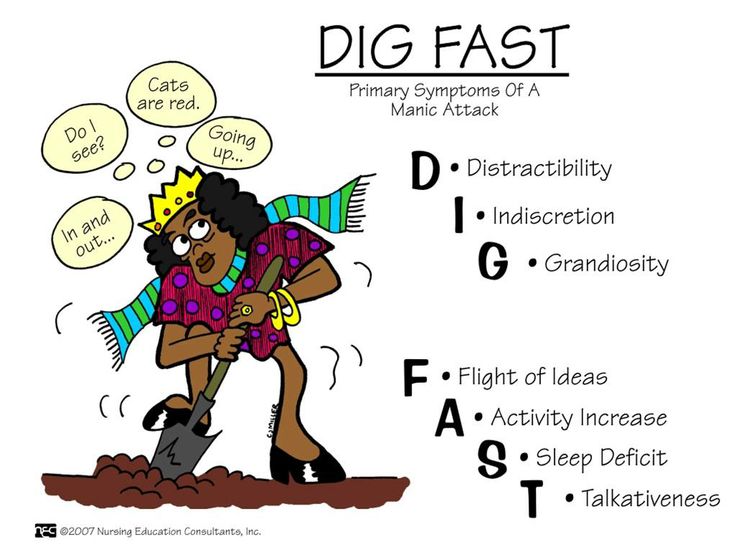
Mania warning signs and symptoms:
- Sleeping less
- Elevated mood
- Restlessness
- Speaking rapidly
- Increase in activity level
- Irritability or aggression
Depression warning signs and symptoms:
- Fatigue and lethargy
- Sleeping more
- Trouble concentrating
- Loss of interest in activities
- Withdrawing from others
- Change in appetite
Coping with mania and depression: Tips for family and friends
If it's not possible to prevent your loved one relapsing, there are things you can do to cope during a manic or depressive episode.
Don't take bipolar symptoms personally. When in the midst of a bipolar episode, people often say or do things that are hurtful or embarrassing. When manic, your loved one may be reckless, cruel, critical, and aggressive. When depressed, they may be rejecting, irritable, hostile, and moody. It's hard not to take such behaviors personally, but try to remember that they're symptoms of your loved one's mental illness, not the result of selfishness or immaturity.
When depressed, they may be rejecting, irritable, hostile, and moody. It's hard not to take such behaviors personally, but try to remember that they're symptoms of your loved one's mental illness, not the result of selfishness or immaturity.
Be prepared for destructive behaviors. When manic or depressed, people with bipolar disorder may behave in destructive or irresponsible ways. Planning ahead for how to handle such behavior can help. When your loved one is well, negotiate a treatment contract that gives you advance approval for protecting them when symptoms flare up. Agree on specific steps you'll take, such as removing credit cards or car keys, going together to the doctor, or taking charge of household finances.
Know what to do in a crisis. It's important to plan ahead for times of crisis so you can act quickly and effectively when it occurs. Having a crisis plan can help. Make sure to include a list of emergency contact information for doctors, therapists, and other friends or family members who will help. Also include the address and phone number of the hospital where you'll take your loved one if necessary.
Also include the address and phone number of the hospital where you'll take your loved one if necessary.
Call 911 (or your country's emergency services number) in an emergency. If your loved one with bipolar disorder is suicidal or violent, don't try to handle the situation alone. If you're worried that your loved one may hurt you, get to safety and then call the police. If your loved one is suicidal, don't leave them alone. Call for an ambulance and stay with your loved one until it arrives.
Supporting someone who is manic
- Spend time with your loved one. People who are manic often feel isolated from other people. Spending even short periods of time with them helps. If your loved one has a lot of energy, walk together. This allows your loved one to keep on the move but still share your company.
- Answer questions honestly. However, do not argue or debate with someone during a manic episode. Try to avoid intense conversation.

- Don't take any comments personally. During manic episodes, your loved one may say or do things that are out of character, including focusing on negative aspects of others. Try to avoid arguments.
- Prepare easy-to-eat meals and drinks. It's often difficult for someone who is manic to sit down to a meal, so try offering them sandwiches, apples, cheese crackers, and juices, for example.
- Avoid subjecting your loved one to a lot of activity and stimulation. It's better to keep surroundings as quiet as possible.
- Allow your loved one to sleep whenever possible. During periods of high energy, sleeping is difficult but short naps taken throughout the day can help. Sometimes a person who is manic may feel rested after only a few hours of sleep.
Taking care of yourself when a loved one has bipolar disorder
It's easy to neglect your own needs when you're supporting someone with a mental illness. But if you don't take care of yourself, you run the risk of burnout—and that won't help you or your loved one. When you take care of yourself both emotionally and physically, you'll be able to better cope with the stress of caring for someone with bipolar disorder and have the energy you need to support your loved one's recovery.
But if you don't take care of yourself, you run the risk of burnout—and that won't help you or your loved one. When you take care of yourself both emotionally and physically, you'll be able to better cope with the stress of caring for someone with bipolar disorder and have the energy you need to support your loved one's recovery.
Focus on your own life. Supporting your loved one may involve some life adjustments, but make sure you don't lose sight of your own goals and priorities. Don't give up friendships, plans, or activities that bring you joy.
Seek support. Dealing with a loved one's mental illness can be painful and isolating. Make sure you're getting the emotional support you need to cope. Talk to someone you trust about what you're going through. It can also help to get your own therapy or join a support group.
Set boundaries. Be realistic about the amount of care you're able to provide without feeling overwhelmed and resentful. Set limits on what you're willing and able to do, and stick to them. Letting bipolar disorder take over your life isn't healthy for you or your loved one.
Set limits on what you're willing and able to do, and stick to them. Letting bipolar disorder take over your life isn't healthy for you or your loved one.
Manage stress. Stress takes a toll on the body and mind, so find ways to keep it in check. Make sure you're eating right and getting enough sleep and exercise. You can also keep stress under control by practicing relaxation techniques such as meditation.
Ask for help. If your friend or family member needs more assistance than you can give, ask for help from others. Turn to other relatives or close friends, or contact a bipolar disorder support organization.
Authors: Jeanne Segal, Ph.D., Lawrence Robinson, and Melinda Smith, M.A.
- References
Bipolar and Related Disorders.
 (2013). In Diagnostic and Statistical Manual of Mental Disorders. American Psychiatric Association. https://doi.org/10.1176/appi.books.9780890425787.x03_Bipolar_and_Related_Disorders
(2013). In Diagnostic and Statistical Manual of Mental Disorders. American Psychiatric Association. https://doi.org/10.1176/appi.books.9780890425787.x03_Bipolar_and_Related_DisordersBobo, William V. “The Diagnosis and Management of Bipolar I and II Disorders: Clinical Practice Update.” Mayo Clinic Proceedings 92, no. 10 (October 2017): 1532–51. https://doi.org/10.1016/j.mayocp.2017.06.022
Bonnín, Caterina Del Mar, María Reinares, Anabel Martínez-Arán, Esther Jiménez, Jose Sánchez-Moreno, Brisa Solé, Laura Montejo, and Eduard Vieta. “Improving Functioning, Quality of Life, and Well-Being in Patients With Bipolar Disorder.” The International Journal of Neuropsychopharmacology 22, no. 8 (August 1, 2019): 467–77. https://doi.org/10.1093/ijnp/pyz018
Shrivastava, Amresh, Megan Johnston, and Yves Bureau. “Stigma of Mental Illness-1: Clinical Reflections.” Mens Sana Monographs 10, no. 1 (January 2012): 70–84. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3353607/
Altman, Susan, Sophia Haeri, Lisa J.
 Cohen, Aleksey Ten, Elysa Barron, Igor I. Galynker, and Katherine N. Duhamel. “Predictors of Relapse in Bipolar Disorder: A Review.” Journal of Psychiatric Practice 12, no. 5 (September 2006): 269–82. https://journals.lww.com/practicalpsychiatry/toc/2006/09000
Cohen, Aleksey Ten, Elysa Barron, Igor I. Galynker, and Katherine N. Duhamel. “Predictors of Relapse in Bipolar Disorder: A Review.” Journal of Psychiatric Practice 12, no. 5 (September 2006): 269–82. https://journals.lww.com/practicalpsychiatry/toc/2006/09000Johnson, Lars, Ola Lundström, Anna Åberg-Wistedt, and Aleksander A Mathé. “Social Support in Bipolar Disorder: Its Relevance to Remission and Relapse.” Bipolar Disorders 5, no. 2 (2003): 129–37. https://doi.org/10.1034/j.1399-5618.2003.00021.x
Lam, Dominic H., Peter Hayward, Edward R. Watkins, Kim Wright, and Pak Sham. “Relapse Prevention in Patients With Bipolar Disorder: Cognitive Therapy Outcome After 2 Years.” American Journal of Psychiatry 162, no. 2 (February 1, 2005): 324–29. https://doi.org/10.1176/appi.ajp.162.2.324
Helping a Friend or Family Member with Depression or Bipolar Disorder – Advice for friends and family. (Depression and Bipolar Support Alliance)
Family Self-Care and Recovery from Mental Illness – Looking after your own wellbeing while caring for a mentally ill family member. (HeretoHelp)
(HeretoHelp)
How to help Someone in Crisis – Handling a bipolar disorder crisis. (Depression and Bipolar Support Alliance)
Last updated: December 5, 2022
How can I help my loved one during a manic episode?
Note: NAMI volunteers are not medical or mental health professionals, and we cannot offer medical or mental health advice. The material outlined below is informational and we hope that it helps provide guidance toward getting support.
Seeing someone you care about experiencing a manic episode can be difficult. Mania is a symptom of several serious mental health conditions, including bipolar disorder, cyclothymic disorder and schizoaffective disorder, that cause dramatic shifts in a person’s mood, energy and ability to think clearly. People living with these conditions can experience high moods known as mania, which differ from the typical ups-and-downs most people experience. Hypomania is a milder form of mania that doesn’t include psychotic episodes. Some people will have episodes of mania or hypomania many times throughout their life; others may experience them only rarely.
Some people will have episodes of mania or hypomania many times throughout their life; others may experience them only rarely.
Although some individuals may find the elevated mood of mania appealing—especially if it occurs after depression—the “high” does not stop at a comfortable or controllable level. Moods can rapidly become more irritable, behavior more unpredictable and judgment more impaired. During periods of mania, people frequently behave impulsively, make reckless decisions and take unusual risks.Most of the time, people in manic states are unaware of the negative consequences of their actions. Learning from prior episodes what kinds of behavior signals “red flags” of manic behavior can help manage the symptoms of the illness.
Sometimes manic episodes also feature psychosis, a symptom that involves loss of contact with reality. People living with psychosis experience disruptions to their thoughts and perceptions that make it difficult to recognize what is real and what isn’t.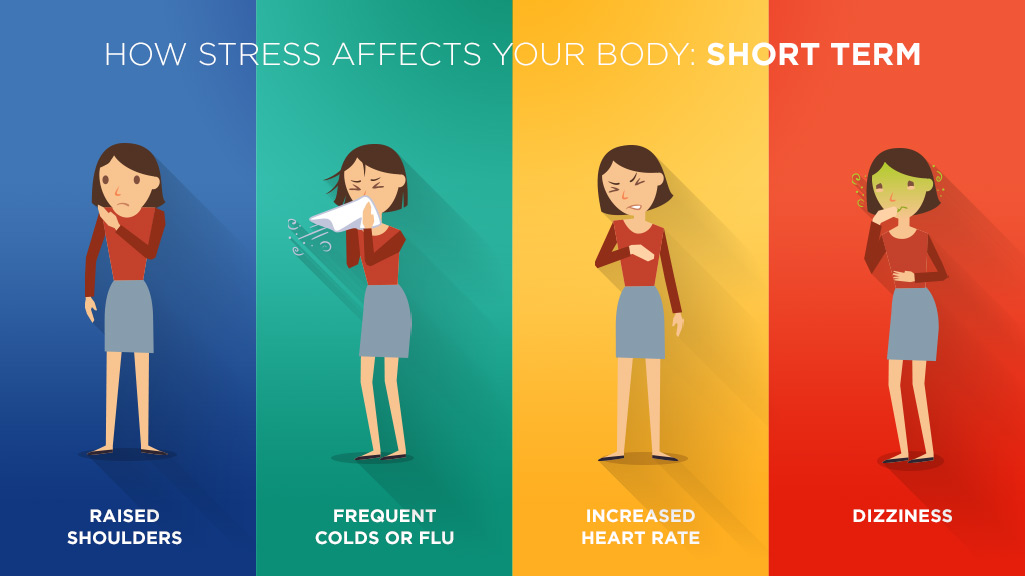 They may see, hear, feel, taste or smell things that aren’t there or have strange, persistent thoughts, behaviors, and emotions
They may see, hear, feel, taste or smell things that aren’t there or have strange, persistent thoughts, behaviors, and emotions
If you are concerned about a loved one who is experiencing a manic episode, NAMI can help. NAMI and NAMI Affiliates provide support and information about programs and community resources for you and your family. You can prepare yourself by learning more about serious mental illness. You may wish to consult the Bipolar Disorder page of NAMI’s website where you will find information on mania, current treatments, ways to support recovery, and links to NAMI Discussion Groups that focus on topics related to Bipolar Disorder.
You may want to reach out to your local NAMI affiliate to look into participation in a NAMI Family-To-Family class where you can find information and strategies for taking care of the person you love, or a NAMI Family Support Group where you can gain insight from the challenges and successes of others facing similar experiences.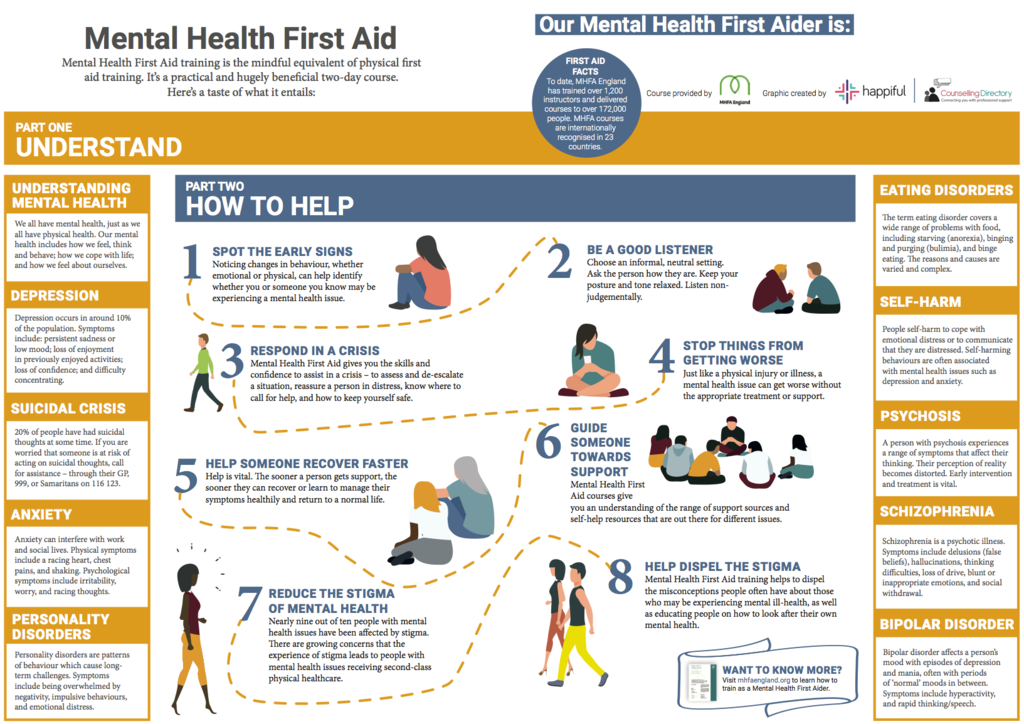 Also, NAMI Peer-to Peer is a free educational program where your loved one can get help better understanding themselves and their recovery, while NAMI Connection is a support group for individuals who experience mental illness. NAMI Peer-to-Peer Classes are free, eight-session educational program for adults with mental health conditions who are looking to better understand themselves and their recovery. Taught by trained leaders with lived experience, this program includes activities, discussions and informative videos. However, as with all NAMI programs, it does not include recommendations for treatment approaches.
Also, NAMI Peer-to Peer is a free educational program where your loved one can get help better understanding themselves and their recovery, while NAMI Connection is a support group for individuals who experience mental illness. NAMI Peer-to-Peer Classes are free, eight-session educational program for adults with mental health conditions who are looking to better understand themselves and their recovery. Taught by trained leaders with lived experience, this program includes activities, discussions and informative videos. However, as with all NAMI programs, it does not include recommendations for treatment approaches.
Additionally, you may find the following resources helpful:
- Depression & Bipolar Support Alliance (DBSA), (800) 826-3632, is a comprehensive resource for more than 23 million people in the U.S. who live with mood disorders, including information on treatment, resources, and support groups. Through the DBSA Support Group Locator you can search for in-person and online support groups that focus on support for individuals and families of those living with mood disorders.
- Information on additional Bipolar Disorder-specific organizations are included on the website of Bipolar Caregivers, which provides easily accessible information on its website for caregivers of people with bipolar disorder, including information and suggestions for caregivers about treatment and management of the disorder, ways to support recovery, and ways for caregivers to support themselves when caring for a loved one with bipolar disorder.
- Juvenile Bipolar Research Foundation provides extensive information for families on juvenile-onset of bipolar disorder and fear of harm through research, education, and outreach. Offers video conference support groups for parents and patients living with Fear of Harm.
- The website of bphope.com offers an online community that strives to increase the awareness of bipolar disorder and to provide hope and empowerment to those in the bipolar community — people with bipolar disorder, along with their families, caregivers, and health-care professionals.
 Provides numerous online support groups.
Provides numerous online support groups.
Helping During a Manic Episode
It can be distressing to see a loved one experiencing a manic episode, but there are some ways you can try to help.
- Stay calm. Respond calmly and gently; avoid arguing with or confronting your loved one about their beliefs or behaviors.
- Learn about anosognosia. People who experience mania may also experience anosognosia, a symptom of serious mental illnesses such as schizoaffective disorder or bipolar disorder, which damages the brain’s frontal lobe and affects a person’s ability to recognize that they are ill. Anosognosia is also experienced by many people living with Alzheimer’s, traumatic brain injury or strokes.
- Listen. Use active listening to build trust with your loved one: “I hear you saying that you have special powers. Do I have that right?”
- Be an ally. Offering empathy can build the kind of positive, trusting relationship with your loved one that may eventually help them agree to partner in their recovery.

- Offer assistance. Ask if you can help. “I know you’ve been feeling restless lately.Would you like to take a walk with me?”
- Quiet environment. Avoid highly stimulating environments (for example, big crowds, bright lights, lots of noise).
- Let it go. Mania sometimes causes individuals to become unusually irritable or disagreeable. Try not to take things personally.
- Give them space. Allow your loved one their personal space. Try not to stand too close or block their exit from the room.
- Redirect. Try to delay or redirect impulses, if possible. Suggest that your loved one hold off on big life changes, sudden travel, or major purchases.
- Focus on the person, not the mania. Being helpful to your loved one doesn’t mean confirming that their thoughts and experiences are real. Instead, try simple, supportive statements like, “I don’t know what to make of what you’re saying. It’s distressing to hear this, but I’m glad you’re telling me.
 How are you handling it?”
How are you handling it?” - Reach out for help. If your loved one’s symptoms reach a point where they are a risk to themselves or others, or they’re not meeting their basic needs (e.g., not eating, not drinking, putting themselves in danger), seek urgent help.
How Can I Get My Loved One to Realize They Need Help?
Often an individual living with a mental health diagnosis – particularly one that involves a serious mental health condition (or one complicated by substance use disorder) – may not actively participate in their own recovery. This is known as Anosognosia [Ah-no-zog-nosha], a symptom that can accompany a serious mental health condition and render the individual unable to recognize that they have a mental health condition and/or that they need to seek help. Anosognosia can be especially troubling for families and friends who are often responsible for providing care for their loved one.
To learn techniques for communicating with your loved one, and to help them agree to partner in their recovery, we would recommend reading I’m Not Sick, I Don’t Need Help!, a book by Dr. Xavier Amador - a psychologist whose experiences with his own family demonstrated how challenging this phenomenon could be. In his book, Dr. Amador discusses the condition of anosognosia and outlines strategies for communicating with a loved one to help them work toward recovery. Portions of the book are accessible to the public on our website here; the book is available in English and Spanish for purchase at online booksellers.
Xavier Amador - a psychologist whose experiences with his own family demonstrated how challenging this phenomenon could be. In his book, Dr. Amador discusses the condition of anosognosia and outlines strategies for communicating with a loved one to help them work toward recovery. Portions of the book are accessible to the public on our website here; the book is available in English and Spanish for purchase at online booksellers.
A broader discussion of the strategies of Dr. Amador’s LEAP method, including videos on how to apply the LEAP method, are available for public access here.
Being Prepared for a Crisis
Being prepared for a crisis by learning about resources and support services allows you to act fast and make good decisions. You may find the information contained in the section of NAMI’s website on Getting Treatment During a Crisis to be particularly helpful. You may also find our NAMI Guide, Navigating a Mental Health Crisis to be extremely informative. Practical tips for what to do and how to react when a loved one is experiencing psychosis and in or near a crisis may be found here (insert link from comment).Additionally, the My Mental Health Crisis Plan App lets individuals clearly state treatment preferences, decide who can make decisions on their behalf, and share a crisis plan with doctors and other members of their care team.
Practical tips for what to do and how to react when a loved one is experiencing psychosis and in or near a crisis may be found here (insert link from comment).Additionally, the My Mental Health Crisis Plan App lets individuals clearly state treatment preferences, decide who can make decisions on their behalf, and share a crisis plan with doctors and other members of their care team.
Bipolar affective disorder and everything you need to know about it
More than 60 million people in the world suffer from bipolar affective disorder (BAD). The essence of the disease is that a person has alternating periods of altered mood throughout his life: from a state with a minus sign to a state with a plus sign. How and why is this happening?
Marina KINKULKINA, psychiatrist of the highest category, head of the department of psychiatry and narcology, director of the Institute of Electronic Medical Education, First Moscow State Medical University. I. M. Sechenova, Corresponding Member of the Russian Academy of Sciences, Professor, Doctor of Medical Sciences
Moreover, it is often not just about sadness or fun, as is often the case with emotional people, but about extreme degrees of either despair or euphoria. The change in these moods can take place both gradually and suddenly, and often for no apparent reason. This disease is attributed to Byron and Hemingway, Virginia Woolf and Edgar Poe, Van Gogh, Schumann, Vivien Leigh and many others. There is an assumption that even “our everything” suffered from a mild degree of BAD (contemporaries often mentioned mood swings) A. S. Pushkin. Modern stars - Catherine Zeta-Jones and Mel Gibson - openly admit to having this mental disorder. And rapper Kanye West even put the inscription on the cover of his album: "I hate being bipolar, it's amazing." A very accurate description of the essence of this disease.
The change in these moods can take place both gradually and suddenly, and often for no apparent reason. This disease is attributed to Byron and Hemingway, Virginia Woolf and Edgar Poe, Van Gogh, Schumann, Vivien Leigh and many others. There is an assumption that even “our everything” suffered from a mild degree of BAD (contemporaries often mentioned mood swings) A. S. Pushkin. Modern stars - Catherine Zeta-Jones and Mel Gibson - openly admit to having this mental disorder. And rapper Kanye West even put the inscription on the cover of his album: "I hate being bipolar, it's amazing." A very accurate description of the essence of this disease.
Genetics does not solve everything
BAD affects both men and women, but the weaker sex - more often. As for the age of onset of the disease, this disorder can also appear in a teenager (especially if there is an appropriate heredity), and in an adult, and even in an elderly person. Everything is individual. The main risk factor is genetics, but a specific gene that would be responsible for the development of bipolar disorder has not been identified.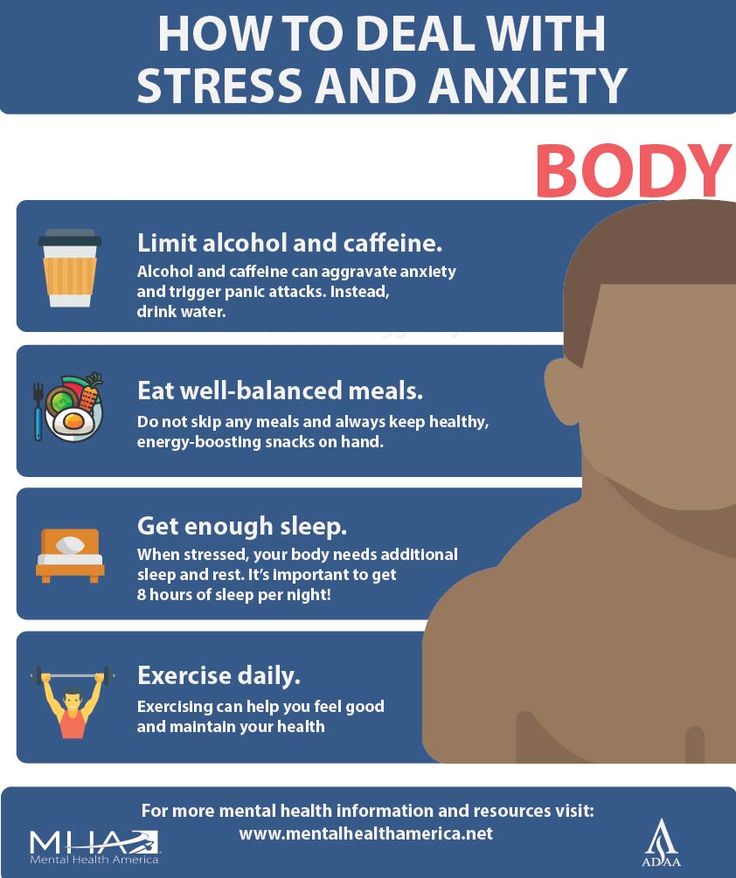 This is a polygenic disorder, and it makes no sense to take genetic tests to find out how great the risk of getting sick is, because scientists still do not have a consensus on what specific combination of genes can lead to a violation. But even if there is a genetic predisposition, it is not certain that the disease will develop. This was proven by studies on identical twins, one of which developed bipolar disorder over the years, while the other did not. Accordingly, there must be some other predisposing moments. Science knows about some of them: life at the limit of possibilities with constant hands-on work, stress and chronic lack of sleep, as well as night shift work, frequent flights with a significant change in hourly flights and, of course, the use of psychoactive substances contribute to the development of the disease. Therefore, they should be avoided. Scientists have yet to learn about other factors.
This is a polygenic disorder, and it makes no sense to take genetic tests to find out how great the risk of getting sick is, because scientists still do not have a consensus on what specific combination of genes can lead to a violation. But even if there is a genetic predisposition, it is not certain that the disease will develop. This was proven by studies on identical twins, one of which developed bipolar disorder over the years, while the other did not. Accordingly, there must be some other predisposing moments. Science knows about some of them: life at the limit of possibilities with constant hands-on work, stress and chronic lack of sleep, as well as night shift work, frequent flights with a significant change in hourly flights and, of course, the use of psychoactive substances contribute to the development of the disease. Therefore, they should be avoided. Scientists have yet to learn about other factors.
But not boring?
The number of people suffering from bipolar disorder among the population, according to various estimates, varies from fractions of one percent to several percent. Recently, psychiatrists note, the proportion of affective disorders has increased significantly, which can be explained by improved diagnostics. At first glance, the BAR does not look like something scary and dangerous. To ignorant people, this disorder even seems attractive - sometimes sad, sometimes fun, in general, you won’t get bored. In addition, being different from everyone else is now fashionable. And then, there is an opinion that people with BAD have higher intelligence and creative abilities than the “gray masses”. But even if this is so, then none of those who suffer from it will definitely call BAD a pleasant thing. It is especially difficult for those patients who do not seek medical help on time. Without treatment, both phases of bipolar disorder can last for months (although sometimes the disorder occurs with frequently alternating phases). Moreover, it is impossible to say which of the periods of the disease is more difficult, manic or depressive.
Recently, psychiatrists note, the proportion of affective disorders has increased significantly, which can be explained by improved diagnostics. At first glance, the BAR does not look like something scary and dangerous. To ignorant people, this disorder even seems attractive - sometimes sad, sometimes fun, in general, you won’t get bored. In addition, being different from everyone else is now fashionable. And then, there is an opinion that people with BAD have higher intelligence and creative abilities than the “gray masses”. But even if this is so, then none of those who suffer from it will definitely call BAD a pleasant thing. It is especially difficult for those patients who do not seek medical help on time. Without treatment, both phases of bipolar disorder can last for months (although sometimes the disorder occurs with frequently alternating phases). Moreover, it is impossible to say which of the periods of the disease is more difficult, manic or depressive.
Bad when very bad
Those who have experienced real depression say that this is the worst thing that can happen in life. In this state, the whole world is seen in black, the mood is depressed, self-esteem drops, life loses its meaning. A person suffering from BAD in the depressive phase perceives his very existence as a chain of tragic mistakes, constantly blaming himself for all the troubles and sins, even those that do not even exist. In addition to mental suffering, physical ones also arise: a person even moves with difficulty, as if swimming against the current, it is difficult for him to perform the most familiar actions. In addition, he can feel tension throughout the body, experience various pain sensations. With an average degree of depression, people often complain of debilitating pain in the abdomen and other parts of the body. On this occasion, they turn to doctors, but the diagnosis cannot be made. And the daily pain continues to harass. Psychiatrists call this somatoform symptomatology. With severe depression, many have the so-called atrial depression. Patients complain of pain and heaviness in the chest, they say that "a stone lies on the heart.
In this state, the whole world is seen in black, the mood is depressed, self-esteem drops, life loses its meaning. A person suffering from BAD in the depressive phase perceives his very existence as a chain of tragic mistakes, constantly blaming himself for all the troubles and sins, even those that do not even exist. In addition to mental suffering, physical ones also arise: a person even moves with difficulty, as if swimming against the current, it is difficult for him to perform the most familiar actions. In addition, he can feel tension throughout the body, experience various pain sensations. With an average degree of depression, people often complain of debilitating pain in the abdomen and other parts of the body. On this occasion, they turn to doctors, but the diagnosis cannot be made. And the daily pain continues to harass. Psychiatrists call this somatoform symptomatology. With severe depression, many have the so-called atrial depression. Patients complain of pain and heaviness in the chest, they say that "a stone lies on the heart.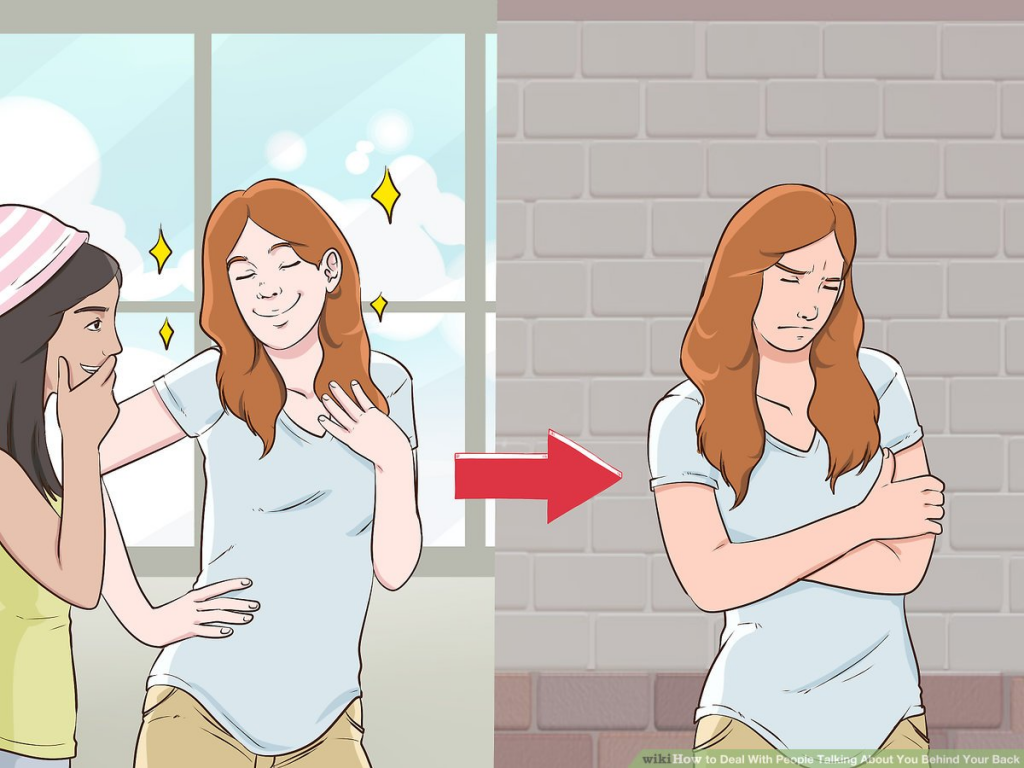 " But even an in-depth examination does not reveal cardiac causes.
" But even an in-depth examination does not reveal cardiac causes.
Often, with depression, patients (especially the elderly) complain of difficulty in thinking, memory impairment, they say that they have become stupid, they believe that they are developing dementia, they are afraid of “losing their mind”. In fact, affective disorders do not destroy the intellect. When treated with antidepressants, when the mood stabilizes, abilities are restored.
But the worst consequence of depression is suicide. Most suicide attempts are made in this state. Sometimes people in a very pronounced depression, believing that they have done something irreparable, and believing that the consequences of their actions can harm loved ones, decide on extended suicides, in which they settle scores not only with their lives, but also take their loved ones with them ( more often children).
Bad when too good
The manic stage of BAD is subjectively more pleasant. Patients are not just in a very good, but in a great mood: they love the whole world and themselves in it. The reflection in the mirror pleases, there is not the slightest doubt about one’s own talents and mind, there is more than enough strength and energy, a bonus is accelerated mental activity. Many in this stage sleep for an hour a day, but do not experience fatigue. Sometimes they don’t sleep for whole days - and at least they are cheerful, like an “energizer”. It seems to be great. But no. With mania, desires and new ideas arise too quickly, so a person grabs at each new business, but, as a rule, does not bring any to the end. So productivity at this stage is no more than during depression. But it would be nice if that was the only thing.
The reflection in the mirror pleases, there is not the slightest doubt about one’s own talents and mind, there is more than enough strength and energy, a bonus is accelerated mental activity. Many in this stage sleep for an hour a day, but do not experience fatigue. Sometimes they don’t sleep for whole days - and at least they are cheerful, like an “energizer”. It seems to be great. But no. With mania, desires and new ideas arise too quickly, so a person grabs at each new business, but, as a rule, does not bring any to the end. So productivity at this stage is no more than during depression. But it would be nice if that was the only thing.
The main danger of mania is that a person has no criticism at this moment, and he can do things that he will later regret very much. For example, he can give away all his property to others (sometimes to unfamiliar people or scammers who specifically use this state of his). Or, say, take out loans to go on a trip to the other side of the world, and take a bunch of friends with him. Maybe even steal something - for example, to make an expensive gift. Many patients at these moments enter into hasty intimate relationships, mistaking a chance meeting for the love of their life (and completely “forgetting” that family and children are waiting at home). Finally, often with mania, people, experiencing euphoria, ignore their severe somatic symptoms, as a result, they do not go to the doctor for a long time, and thus trigger a serious illness (pneumonia, for example). In addition, not all patients in the manic phase are "darlings." Often they show unreasonable aggression if, for example, others do not agree with their "brilliant" advice. As a result of such “angry mania”, conflicts and even situations arise that require the intervention of law enforcement agencies and the hospitalization of the patient without his consent in a psychiatric hospital.
Maybe even steal something - for example, to make an expensive gift. Many patients at these moments enter into hasty intimate relationships, mistaking a chance meeting for the love of their life (and completely “forgetting” that family and children are waiting at home). Finally, often with mania, people, experiencing euphoria, ignore their severe somatic symptoms, as a result, they do not go to the doctor for a long time, and thus trigger a serious illness (pneumonia, for example). In addition, not all patients in the manic phase are "darlings." Often they show unreasonable aggression if, for example, others do not agree with their "brilliant" advice. As a result of such “angry mania”, conflicts and even situations arise that require the intervention of law enforcement agencies and the hospitalization of the patient without his consent in a psychiatric hospital.
Good intentions…
The worst thing that relatives and friends of a person with bipolar disorder can do is ignore his problem, devalue suffering, while blaming the patient himself and appealing to his conscience. For example, they can call on a depressed person to “pull himself together, not become limp”, say that he is “mad with fat”, etc. A patient at the stage of mania is most often accused of immorality, irresponsibility, frivolity, promiscuity in relationships, etc. However, doing so is like blaming a person with diabetes for not being able to eat sweet cake, or a patient with heart failure for not running a marathon. BAD is a disease like many others. And she needs to be treated. The sooner you start the right therapy, the sooner you can stabilize the patient's condition and the better the further prognosis will be.
For example, they can call on a depressed person to “pull himself together, not become limp”, say that he is “mad with fat”, etc. A patient at the stage of mania is most often accused of immorality, irresponsibility, frivolity, promiscuity in relationships, etc. However, doing so is like blaming a person with diabetes for not being able to eat sweet cake, or a patient with heart failure for not running a marathon. BAD is a disease like many others. And she needs to be treated. The sooner you start the right therapy, the sooner you can stabilize the patient's condition and the better the further prognosis will be.
Psychiatrists don't bite
Despite the fact that recently people (especially young people) have ceased to be afraid to turn to psychiatrists, not everyone still decides to go to the doctor. Indeed, on the Internet in the public domain, you can find hundreds of questionnaires to test yourself for any mental disorder. And then, after reading various tips, you can also “cure”. Doctors strongly advise against doing this. The smallest harm of self-treatment is that it will not help or lead to incomplete improvement, but it can also worsen the condition. For example, inadequate intake of antidepressants in bipolar disorder can lead from a depressive phase into a severe manic state, from which it will then be difficult to get out. Only a psychiatrist (and not a psychologist, neurologist or doctor of any other somatic profile) can identify bipolar disorder and choose the right treatment. Treatment should be strictly individual, that is, the doctor selects it based on the characteristics of a particular patient and taking into account a specific moment in the course of the disease. The goal of therapy is not only to equalize the patient's mood, but also to prevent recurrence. In the treatment of bipolar disorder, the main role is played by drugs for stabilizing mood - mood stabilizers (lithium salts, some anticonvulsants (anticonvulsants) and antipsychotics of new generations).
Doctors strongly advise against doing this. The smallest harm of self-treatment is that it will not help or lead to incomplete improvement, but it can also worsen the condition. For example, inadequate intake of antidepressants in bipolar disorder can lead from a depressive phase into a severe manic state, from which it will then be difficult to get out. Only a psychiatrist (and not a psychologist, neurologist or doctor of any other somatic profile) can identify bipolar disorder and choose the right treatment. Treatment should be strictly individual, that is, the doctor selects it based on the characteristics of a particular patient and taking into account a specific moment in the course of the disease. The goal of therapy is not only to equalize the patient's mood, but also to prevent recurrence. In the treatment of bipolar disorder, the main role is played by drugs for stabilizing mood - mood stabilizers (lithium salts, some anticonvulsants (anticonvulsants) and antipsychotics of new generations). Modern drugs are much better tolerated than their predecessors, have fewer side effects, as they are designed for long-term use over many years. Against the background of their intake, women can even become pregnant and give birth. In depression, antidepressants are prescribed in exceptional cases, given the danger of changing the depressive stage to manic.
Modern drugs are much better tolerated than their predecessors, have fewer side effects, as they are designed for long-term use over many years. Against the background of their intake, women can even become pregnant and give birth. In depression, antidepressants are prescribed in exceptional cases, given the danger of changing the depressive stage to manic.
You won't be able to forget
The insidiousness of BAD is that this disease cannot be cured once and for all. But, alas, often, when the patient's mood can be balanced by medication and he begins to feel good (such a state - intermission - is completely indistinguishable from a state of complete health), he can stop taking the drugs. This is a big mistake that does not allow to achieve a stable result of treatment. Sometimes it is required to use medicines (necessarily under the supervision of a doctor) for several months, but more often for years (with periodic visits to the doctor). It is the long-term use of maintenance therapy individually selected by the doctor that allows patients to achieve a stable good condition and feel the joy of life for many years.
Link to publication: www.kiz.ru
Site embed code
More than 60 million people in the world suffer from bipolar affective disorder (BAD). The essence of the disease is that a person has alternating periods of altered mood throughout his life: from a state with a minus sign to a state with a plus sign. How and why is this happening?
Marina KINKULKINA, psychiatrist of the highest category, head of the department of psychiatry and narcology, director of the Institute of Electronic Medical Education, First Moscow State Medical University. I. M. Sechenova, Corresponding Member of the Russian Academy of Sciences, Professor, Doctor of Medical Sciences
Moreover, it is often not just about sadness or fun, as is often the case with emotional people, but about extreme degrees of either despair or euphoria. The change in these moods can take place both gradually and suddenly, and often for no apparent reason. This disease is attributed to Byron and Hemingway, Virginia Woolf and Edgar Poe, Van Gogh, Schumann, Vivien Leigh and many others. There is an assumption that even “our everything” suffered from a mild degree of BAD (contemporaries often mentioned mood swings) A. S. Pushkin. Modern stars - Catherine Zeta-Jones and Mel Gibson - openly admit to having this mental disorder. And rapper Kanye West even put the inscription on the cover of his album: "I hate being bipolar, it's amazing." A very accurate description of the essence of this disease.
This disease is attributed to Byron and Hemingway, Virginia Woolf and Edgar Poe, Van Gogh, Schumann, Vivien Leigh and many others. There is an assumption that even “our everything” suffered from a mild degree of BAD (contemporaries often mentioned mood swings) A. S. Pushkin. Modern stars - Catherine Zeta-Jones and Mel Gibson - openly admit to having this mental disorder. And rapper Kanye West even put the inscription on the cover of his album: "I hate being bipolar, it's amazing." A very accurate description of the essence of this disease.
Genetics does not solve everything
BAD affects both men and women, but the weaker sex - more often. As for the age of onset of the disease, this disorder can also appear in a teenager (especially if there is an appropriate heredity), and in an adult, and even in an elderly person. Everything is individual. The main risk factor is genetics, but a specific gene that would be responsible for the development of bipolar disorder has not been identified.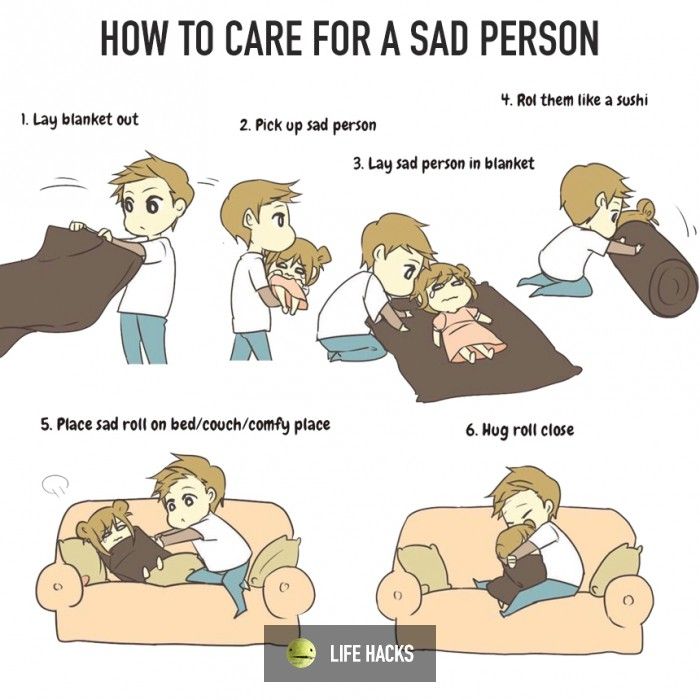 This is a polygenic disorder, and it makes no sense to take genetic tests to find out how great the risk of getting sick is, because scientists still do not have a consensus on what specific combination of genes can lead to a violation. But even if there is a genetic predisposition, it is not certain that the disease will develop. This was proven by studies on identical twins, one of which developed bipolar disorder over the years, while the other did not. Accordingly, there must be some other predisposing moments. Science knows about some of them: life at the limit of possibilities with constant hands-on work, stress and chronic lack of sleep, as well as night shift work, frequent flights with a significant change in hourly flights and, of course, the use of psychoactive substances contribute to the development of the disease. Therefore, they should be avoided. Scientists have yet to learn about other factors.
This is a polygenic disorder, and it makes no sense to take genetic tests to find out how great the risk of getting sick is, because scientists still do not have a consensus on what specific combination of genes can lead to a violation. But even if there is a genetic predisposition, it is not certain that the disease will develop. This was proven by studies on identical twins, one of which developed bipolar disorder over the years, while the other did not. Accordingly, there must be some other predisposing moments. Science knows about some of them: life at the limit of possibilities with constant hands-on work, stress and chronic lack of sleep, as well as night shift work, frequent flights with a significant change in hourly flights and, of course, the use of psychoactive substances contribute to the development of the disease. Therefore, they should be avoided. Scientists have yet to learn about other factors.
But not boring?
The number of people suffering from bipolar disorder among the population, according to various estimates, varies from fractions of one percent to several percent. Recently, psychiatrists note, the proportion of affective disorders has increased significantly, which can be explained by improved diagnostics. At first glance, the BAR does not look like something scary and dangerous. To ignorant people, this disorder even seems attractive - sometimes sad, sometimes fun, in general, you won’t get bored. In addition, being different from everyone else is now fashionable. And then, there is an opinion that people with BAD have higher intelligence and creative abilities than the “gray masses”. But even if this is so, then none of those who suffer from it will definitely call BAD a pleasant thing. It is especially difficult for those patients who do not seek medical help on time. Without treatment, both phases of bipolar disorder can last for months (although sometimes the disorder occurs with frequently alternating phases). Moreover, it is impossible to say which of the periods of the disease is more difficult, manic or depressive.
Recently, psychiatrists note, the proportion of affective disorders has increased significantly, which can be explained by improved diagnostics. At first glance, the BAR does not look like something scary and dangerous. To ignorant people, this disorder even seems attractive - sometimes sad, sometimes fun, in general, you won’t get bored. In addition, being different from everyone else is now fashionable. And then, there is an opinion that people with BAD have higher intelligence and creative abilities than the “gray masses”. But even if this is so, then none of those who suffer from it will definitely call BAD a pleasant thing. It is especially difficult for those patients who do not seek medical help on time. Without treatment, both phases of bipolar disorder can last for months (although sometimes the disorder occurs with frequently alternating phases). Moreover, it is impossible to say which of the periods of the disease is more difficult, manic or depressive.
Bad when very bad
Those who have experienced real depression say that this is the worst thing that can happen in life. In this state, the whole world is seen in black, the mood is depressed, self-esteem drops, life loses its meaning. A person suffering from BAD in the depressive phase perceives his very existence as a chain of tragic mistakes, constantly blaming himself for all the troubles and sins, even those that do not even exist. In addition to mental suffering, physical ones also arise: a person even moves with difficulty, as if swimming against the current, it is difficult for him to perform the most familiar actions. In addition, he can feel tension throughout the body, experience various pain sensations. With an average degree of depression, people often complain of debilitating pain in the abdomen and other parts of the body. On this occasion, they turn to doctors, but the diagnosis cannot be made. And the daily pain continues to harass. Psychiatrists call this somatoform symptomatology. With severe depression, many have the so-called atrial depression. Patients complain of pain and heaviness in the chest, they say that "a stone lies on the heart.
In this state, the whole world is seen in black, the mood is depressed, self-esteem drops, life loses its meaning. A person suffering from BAD in the depressive phase perceives his very existence as a chain of tragic mistakes, constantly blaming himself for all the troubles and sins, even those that do not even exist. In addition to mental suffering, physical ones also arise: a person even moves with difficulty, as if swimming against the current, it is difficult for him to perform the most familiar actions. In addition, he can feel tension throughout the body, experience various pain sensations. With an average degree of depression, people often complain of debilitating pain in the abdomen and other parts of the body. On this occasion, they turn to doctors, but the diagnosis cannot be made. And the daily pain continues to harass. Psychiatrists call this somatoform symptomatology. With severe depression, many have the so-called atrial depression. Patients complain of pain and heaviness in the chest, they say that "a stone lies on the heart. " But even an in-depth examination does not reveal cardiac causes.
" But even an in-depth examination does not reveal cardiac causes.
Often, with depression, patients (especially the elderly) complain of difficulty in thinking, memory impairment, they say that they have become stupid, they believe that they are developing dementia, they are afraid of “losing their mind”. In fact, affective disorders do not destroy the intellect. When treated with antidepressants, when the mood stabilizes, abilities are restored.
But the worst consequence of depression is suicide. Most suicide attempts are made in this state. Sometimes people in a very pronounced depression, believing that they have done something irreparable, and believing that the consequences of their actions can harm loved ones, decide on extended suicides, in which they settle scores not only with their lives, but also take their loved ones with them ( more often children).
Bad when too good
The manic stage of BAD is subjectively more pleasant. Patients are not just in a very good, but in a great mood: they love the whole world and themselves in it. The reflection in the mirror pleases, there is not the slightest doubt about one’s own talents and mind, there is more than enough strength and energy, a bonus is accelerated mental activity. Many in this stage sleep for an hour a day, but do not experience fatigue. Sometimes they don’t sleep for whole days - and at least they are cheerful, like an “energizer”. It seems to be great. But no. With mania, desires and new ideas arise too quickly, so a person grabs at each new business, but, as a rule, does not bring any to the end. So productivity at this stage is no more than during depression. But it would be nice if that was the only thing.
The reflection in the mirror pleases, there is not the slightest doubt about one’s own talents and mind, there is more than enough strength and energy, a bonus is accelerated mental activity. Many in this stage sleep for an hour a day, but do not experience fatigue. Sometimes they don’t sleep for whole days - and at least they are cheerful, like an “energizer”. It seems to be great. But no. With mania, desires and new ideas arise too quickly, so a person grabs at each new business, but, as a rule, does not bring any to the end. So productivity at this stage is no more than during depression. But it would be nice if that was the only thing.
The main danger of mania is that a person has no criticism at this moment, and he can do things that he will later regret very much. For example, he can give away all his property to others (sometimes to unfamiliar people or scammers who specifically use this state of his). Or, say, take out loans to go on a trip to the other side of the world, and take a bunch of friends with him. Maybe even steal something - for example, to make an expensive gift. Many patients at these moments enter into hasty intimate relationships, mistaking a chance meeting for the love of their life (and completely “forgetting” that family and children are waiting at home). Finally, often with mania, people, experiencing euphoria, ignore their severe somatic symptoms, as a result, they do not go to the doctor for a long time, and thus trigger a serious illness (pneumonia, for example). In addition, not all patients in the manic phase are "darlings." Often they show unreasonable aggression if, for example, others do not agree with their "brilliant" advice. As a result of such “angry mania”, conflicts and even situations arise that require the intervention of law enforcement agencies and the hospitalization of the patient without his consent in a psychiatric hospital.
Maybe even steal something - for example, to make an expensive gift. Many patients at these moments enter into hasty intimate relationships, mistaking a chance meeting for the love of their life (and completely “forgetting” that family and children are waiting at home). Finally, often with mania, people, experiencing euphoria, ignore their severe somatic symptoms, as a result, they do not go to the doctor for a long time, and thus trigger a serious illness (pneumonia, for example). In addition, not all patients in the manic phase are "darlings." Often they show unreasonable aggression if, for example, others do not agree with their "brilliant" advice. As a result of such “angry mania”, conflicts and even situations arise that require the intervention of law enforcement agencies and the hospitalization of the patient without his consent in a psychiatric hospital.
Good intentions…
The worst thing that relatives and friends of a person with bipolar disorder can do is ignore his problem, devalue suffering, while blaming the patient himself and appealing to his conscience. For example, they can call on a depressed person to “pull himself together, not become limp”, say that he is “mad with fat”, etc. A patient at the stage of mania is most often accused of immorality, irresponsibility, frivolity, promiscuity in relationships, etc. However, doing so is like blaming a person with diabetes for not being able to eat sweet cake, or a patient with heart failure for not running a marathon. BAD is a disease like many others. And she needs to be treated. The sooner you start the right therapy, the sooner you can stabilize the patient's condition and the better the further prognosis will be.
For example, they can call on a depressed person to “pull himself together, not become limp”, say that he is “mad with fat”, etc. A patient at the stage of mania is most often accused of immorality, irresponsibility, frivolity, promiscuity in relationships, etc. However, doing so is like blaming a person with diabetes for not being able to eat sweet cake, or a patient with heart failure for not running a marathon. BAD is a disease like many others. And she needs to be treated. The sooner you start the right therapy, the sooner you can stabilize the patient's condition and the better the further prognosis will be.
Psychiatrists don't bite
Despite the fact that recently people (especially young people) have ceased to be afraid to turn to psychiatrists, not everyone still decides to go to the doctor. Indeed, on the Internet in the public domain, you can find hundreds of questionnaires to test yourself for any mental disorder. And then, after reading various tips, you can also “cure”. Doctors strongly advise against doing this. The smallest harm of self-treatment is that it will not help or lead to incomplete improvement, but it can also worsen the condition. For example, inadequate intake of antidepressants in bipolar disorder can lead from a depressive phase into a severe manic state, from which it will then be difficult to get out. Only a psychiatrist (and not a psychologist, neurologist or doctor of any other somatic profile) can identify bipolar disorder and choose the right treatment. Treatment should be strictly individual, that is, the doctor selects it based on the characteristics of a particular patient and taking into account a specific moment in the course of the disease. The goal of therapy is not only to equalize the patient's mood, but also to prevent recurrence. In the treatment of bipolar disorder, the main role is played by drugs for stabilizing mood - mood stabilizers (lithium salts, some anticonvulsants (anticonvulsants) and antipsychotics of new generations).
Doctors strongly advise against doing this. The smallest harm of self-treatment is that it will not help or lead to incomplete improvement, but it can also worsen the condition. For example, inadequate intake of antidepressants in bipolar disorder can lead from a depressive phase into a severe manic state, from which it will then be difficult to get out. Only a psychiatrist (and not a psychologist, neurologist or doctor of any other somatic profile) can identify bipolar disorder and choose the right treatment. Treatment should be strictly individual, that is, the doctor selects it based on the characteristics of a particular patient and taking into account a specific moment in the course of the disease. The goal of therapy is not only to equalize the patient's mood, but also to prevent recurrence. In the treatment of bipolar disorder, the main role is played by drugs for stabilizing mood - mood stabilizers (lithium salts, some anticonvulsants (anticonvulsants) and antipsychotics of new generations). Modern drugs are much better tolerated than their predecessors, have fewer side effects, as they are designed for long-term use over many years. Against the background of their intake, women can even become pregnant and give birth. In depression, antidepressants are prescribed in exceptional cases, given the danger of changing the depressive stage to manic.
Modern drugs are much better tolerated than their predecessors, have fewer side effects, as they are designed for long-term use over many years. Against the background of their intake, women can even become pregnant and give birth. In depression, antidepressants are prescribed in exceptional cases, given the danger of changing the depressive stage to manic.
You won't be able to forget
The insidiousness of BAD is that this disease cannot be cured once and for all. But, alas, often, when the patient's mood can be balanced by medication and he begins to feel good (such a state - intermission - is completely indistinguishable from a state of complete health), he can stop taking the drugs. This is a big mistake that does not allow to achieve a stable result of treatment. Sometimes it is required to use medicines (necessarily under the supervision of a doctor) for several months, but more often for years (with periodic visits to the doctor). It is the long-term use of maintenance therapy individually selected by the doctor that allows patients to achieve a stable good condition and feel the joy of life for many years.
People with bipolar disorder tell how to properly support them
March 30 is celebrated as Bipolar Day around the world. With this disease, it is important to monitor mood changes, which can be difficult to do alone. The founder of the Bipolar Association, Masha Pushkina, has collected stories of people who are helped by treatment partners.
At the initiative of public organizations bringing together scientists, doctors and activists, every year on March 30, World Bipolar Day is celebrated. The date chosen was the birthday of Vincent van Gogh, an artist who, according to researchers, was the embodiment of a "bipolar genius."
With bipolar disorder, a person lives either in a state of high emotional uplift and excitement (mania), or in depression. According to world statistics, about 2% of people suffer from bipolar disorder in various forms. This means that in Russia there are at least three million bipolar people - this is about half of St. Petersburg.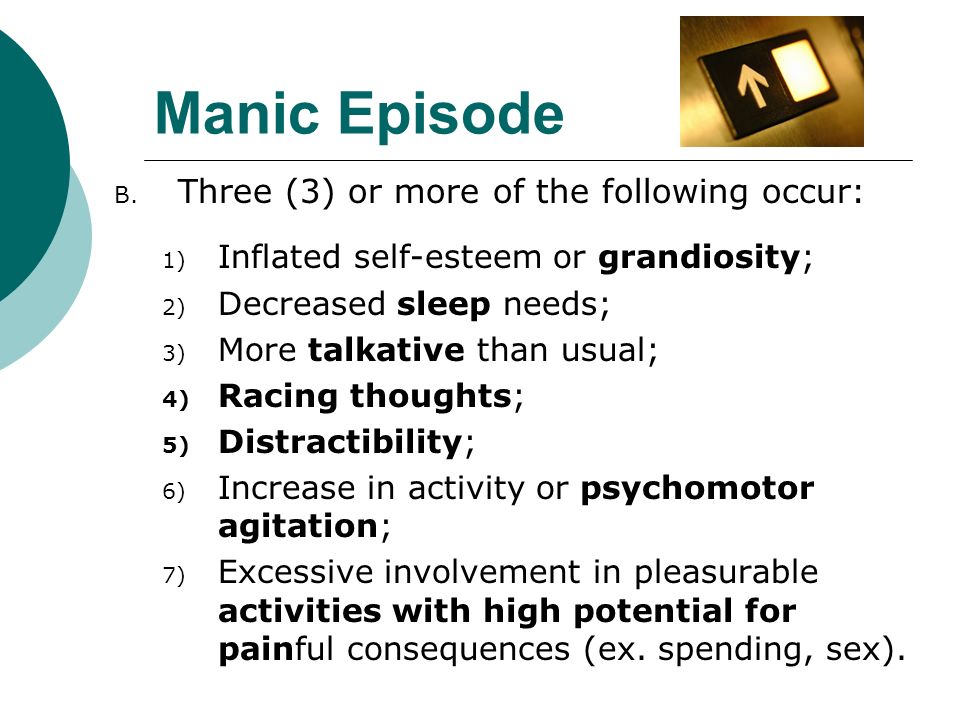
In most cases, this condition responds well to medication. But, unfortunately, many do not seek help or do not know how to find it. Without treatment, the disease progresses and ultimately leads to sad consequences: loss of family, job, disability in general, and in almost every seventh case, suicide.
These consequences can be avoided. The peculiarity of bipolar disorder is that the onset of remission depends not only on the doctor and medications, but also on the behavior of the patient himself. Very often, bipolar people provoke seizures "with their own hands." The mood of people with BAD (bipolar affective disorder. - Note ed. ) is very unstable, the balance is fragile, and you can “start” mania or depression in dozens of ways: the psyche is easily shaken by psychoactive substances, alcohol, lack of sleep, too intense work, travel and even love. So, a short time after the next course of treatment with powerful drugs, the person again ends up in the hospital. And each new attack reduces the chances of a long remission, affects social status, and even more painfully - self-esteem.
And each new attack reduces the chances of a long remission, affects social status, and even more painfully - self-esteem.
The experience of people with mental disorders around the world has proven that you are much more likely to cope with difficulties when you are supported by people who understand your problems and condition, but do not look at you as a patient. As practice shows, such a person can be not only a partner or close relative. An old friend, and even a person with whom you have never met in person, can help you get through the darkest times. Masha Pushkina, especially for Afisha Daily, spoke with several bipolar people about those in whom they found their support. The result is a story not about illness, but about friendship and trust, which can defeat even madness.
Yana, 31 years old
Housewife, collects books and is fond of confectionery
Purposefully, I didn't find out anywhere about ways to support, everything turned out quite naturally. I have been sick for 15 years. The first person who looked after me was my best friend, and now it's my husband.
I have been sick for 15 years. The first person who looked after me was my best friend, and now it's my husband.
When my hypomania (a mild degree of mania, which is characterized by a constantly high mood. - Note ed. ) accelerated into a full-fledged mania (this state is also characterized by a one-sided attraction to some topic, sometimes accompanied by delirium. - Note ed. ), it became clear that I needed to be looked after. A friend began to pay attention to repetitive patterns of behavior in one phase or another, and we decided together to find out what helps in such cases. I think my friend was afraid to take responsibility for my condition, but she turned out to be generous and selfless. When I got married, a friend passed this knowledge on to her husband, and he already supplemented it, based on his own experience. The husband initially knew with whom he connects his life. He says it didn't scare him.
I have obsessions during my manic episodes. My husband does not argue with me at this time, but he also does not feed them, trying to redirect my stormy energy in a different direction. You can’t argue, because the result will be the opposite: I will finally get stuck on the idea, I will consider that I must prove it at all costs, even if the whole world is against me, and there are enemies and conspiracies around. If this does not help, the husband agrees to discuss all these things, but at the same time tries to slow down their implementation by offering to draw up a specific and detailed plan. Sometimes it takes me a long time.
My husband does not argue with me at this time, but he also does not feed them, trying to redirect my stormy energy in a different direction. You can’t argue, because the result will be the opposite: I will finally get stuck on the idea, I will consider that I must prove it at all costs, even if the whole world is against me, and there are enemies and conspiracies around. If this does not help, the husband agrees to discuss all these things, but at the same time tries to slow down their implementation by offering to draw up a specific and detailed plan. Sometimes it takes me a long time.
For example, I always want to move somewhere. Right now, and why aren't we packing our things yet? My husband tries to make me write down what are the pros and cons of different cities, what attracts us to them. As a result, I sit for hours on different forums, make lists, think about how we will arrange our life, calculate the budget for different countries of the world. There is also a manic passion for travel, but after preparation, we usually implement these plans. And many years ago, in a fit of mania, I bought an apartment - with a mortgage, with hellish payments. Then it took a long time to resolve this situation, but, fortunately, everything worked out well.
And many years ago, in a fit of mania, I bought an apartment - with a mortgage, with hellish payments. Then it took a long time to resolve this situation, but, fortunately, everything worked out well.
My husband began to chart my mood. I also manage it, and we check the results so that they are objective. Quarrels due to the fact that the husband takes on the role of the elder often arise in the manic phase (never in depression). Then I become very suspicious, any attempts at control cause rage. But now the husband has learned from experience, so he does not react to attempts to unleash a conflict. With obvious attacks of rage and auto-aggression, he uses holding therapy (long strong hugs. - Note ed. ). We have seen this in autistic children, this is how their parents influence them.
When I'm depressed, he doesn't comfort me because it's pointless, but he tries to give reasonable arguments that this period has always ended and this time will also pass soon. We look at mood charts for the past months, discuss the duration of the attacks: two weeks have already passed and, judging by past experience, it should get better in a couple of weeks.
We look at mood charts for the past months, discuss the duration of the attacks: two weeks have already passed and, judging by past experience, it should get better in a couple of weeks.
Such support from the husband helps in many ways. When I was being treated by two doctors, taking all the medicines, I didn’t have such support, everything was very bad. Over time, I stopped disappearing from home in a manic state and inflicting serious injuries on myself. All my super-ideas remain on paper in the form of graphs and tables, I don’t even have time to start putting them into practice, so that later I don’t have to deal with the consequences with the whole family.
Alice, 27 years old
Biologist
To be honest, I do not always find understanding from my healthy environment, I often faced condemnation, devaluation of problems. But from a person who has a similar experience, you won’t hear “don’t invent”, “you can’t feel so bad”, “take a walk and it will pass”.
It just so happens that my best friend also suffers from bipolar disorder. I did not look for support in specialized communities where patients communicate, we met by chance. My friend is much older, he has much more life experience, and he was able to become a real mentor for me. Not once did his actions worsen my condition - I hope that he can say the same about me.
When I'm on the rise, I feel uncomfortable when he tries to slow me down and reduce my passions. But as soon as this state passes and I again take a sober look at the situation, each time I thank him for trying to stop the revelry and disgrace. My friend himself is currently not being treated, but he never imposed his position on me, and when I turn to doctors, he supports me in this.
I told the doctor about this source of support - he is all for it. Before meeting a friend, I had suicidal attempts, but during the entire time of our communication I never tried to say goodbye to life. When you know that there is a person who will understand everything and share warmth (while even my own family repels me), that there is a place where you can come in any condition and where they will accept me without unnecessary questions and teachings, this is a source of great strength. and hope.
and hope.
When I was expecting my second child, I was depressed. My husband did not yet fully understand the features of the disease and did not want to admit obvious things - this added problems, and my emotional state became extremely difficult. It seems that only thanks to the participation of my friend, I did not do anything to myself and successfully endured the pregnancy. The child was named after him.
Sergey, 49 years old
Freelancer
At the height of the depression, I was looking for any available support and ended up in an online group of anonymous debtors (people who have taken on large loans). One of the participants drew attention to my condition and said that I urgently need medical help. Despite the fact that she lives in the USA, we began to communicate regularly via Skype. Olga literally brought me to the hospital and helped me prepare for the treatment.
Americans are a pragmatic people, many young and healthy people have folders with wills and instructions in case of their death.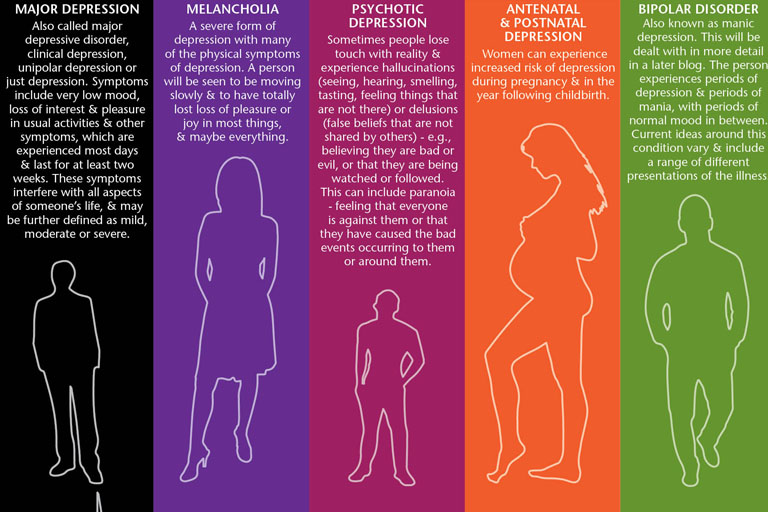 They also approach mental difficulties calmly and thoroughly. It is common practice for the patient to draw up detailed instructions in advance. In the United States, there is a practice of issuing Treatment Agreements for people with mental illness (Treatment Contract). This document is needed so that family, friends and doctors recognize the symptoms of deterioration in time and take into account your experience and wishes in the treatment. Typically, such a document contains: a list of trusted people; signs of a normal state; signs of an approaching episode; symptoms of mania and depression; actions that trusted people should take to help a person get better and keep him from destructive acts; plan of action in case of an emergency (for example, a suicide attempt). who and what will be done in case of his hospitalization, so that he can be treated without anxiety for household chores.
They also approach mental difficulties calmly and thoroughly. It is common practice for the patient to draw up detailed instructions in advance. In the United States, there is a practice of issuing Treatment Agreements for people with mental illness (Treatment Contract). This document is needed so that family, friends and doctors recognize the symptoms of deterioration in time and take into account your experience and wishes in the treatment. Typically, such a document contains: a list of trusted people; signs of a normal state; signs of an approaching episode; symptoms of mania and depression; actions that trusted people should take to help a person get better and keep him from destructive acts; plan of action in case of an emergency (for example, a suicide attempt). who and what will be done in case of his hospitalization, so that he can be treated without anxiety for household chores.
In a period of severe depression, there is a struggle inside a person between the craving for death and the desire to live - and many external things can outweigh in one direction or another. Every clue is important to help you get out. It is very difficult for one to cope with all this.
Every clue is important to help you get out. It is very difficult for one to cope with all this.
I madly didn’t want to go to the hospital and wouldn’t have made up my mind myself, until the last I hoped that somehow everything would go away on its own. But under the supervision of a friend, I drew up a preparation plan: warn the customer at work, arrange to look after my cats. Reported to her about every step. But then he could no longer simply “escape” [from hospitalization], because he felt obliged to both her and the doctor. During depression, one's own life has no value, but the people dear to me, the promises made to them, do.
At the most difficult moment, Olga became my “outer brain”, which told me what to do when I didn’t understand anything myself. After I was discharged from the hospital, I turned to four friends for support. Usually we call each other once a week, I tell what my condition is. It is important not only to chat online, but also to hear the voice, you can understand a lot from it. Friends immediately pay attention, if I suddenly disappear and stop calling, then something is wrong.
Friends immediately pay attention, if I suddenly disappear and stop calling, then something is wrong.
I think it is possible to find such a person if you set yourself such a goal. Take a closer look at people in support groups, religious or other communities - those who understand what compassion and mutual assistance are. This must be an internally mature person, ready to take responsibility for you in a difficult situation. If this person has similar problems, then he will better understand your experiences. For this reason, relatives are far from always suitable: they themselves can panic, seeing how bad you feel, choke you with their anxiety, overprotection.
It is necessary to establish the frequency of communication and observe it. And of course, in no case should you parasitize on someone else's kindness. The support system works when you yourself take responsibility for your life, and do not outweigh it completely on another.
Anna and Valeria, 21
Students
Anna: After a major depressive episode four years ago that almost ended in a suicide attempt, I started looking for information on [support].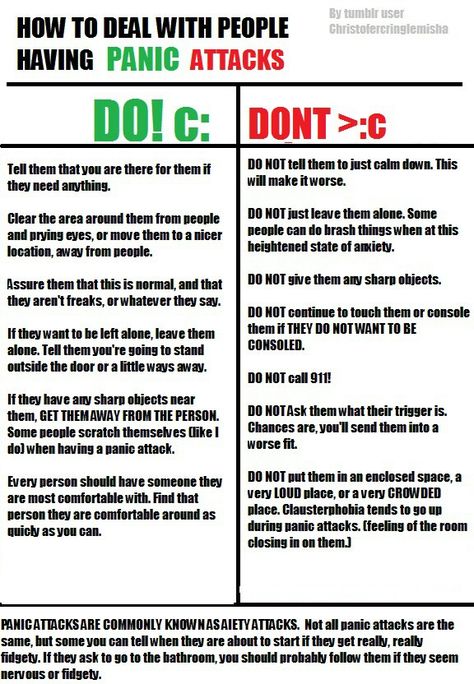 I managed to find a guide in English for relatives and friends on how to behave with such a person. I have sent this list to all my friends so that they have an idea of what is happening to me. For the past few years, Lera has been monitoring my emotional state on a daily basis, and if, in her opinion, it goes beyond the norm, she tells me about it. Lera just asks every day how I'm doing, and if she sees that I'm reacting strangely, she wonders if something happened. At first, it was very difficult, because, in principle, I did not like to regularly share personal experiences. But by regularly receiving feedback, I can imagine the dynamics: do the pills help, how long do the side effects last, does the depressive phase go into a moderate and severe degree, do I lose my critical thinking during hypomania.
I managed to find a guide in English for relatives and friends on how to behave with such a person. I have sent this list to all my friends so that they have an idea of what is happening to me. For the past few years, Lera has been monitoring my emotional state on a daily basis, and if, in her opinion, it goes beyond the norm, she tells me about it. Lera just asks every day how I'm doing, and if she sees that I'm reacting strangely, she wonders if something happened. At first, it was very difficult, because, in principle, I did not like to regularly share personal experiences. But by regularly receiving feedback, I can imagine the dynamics: do the pills help, how long do the side effects last, does the depressive phase go into a moderate and severe degree, do I lose my critical thinking during hypomania.
Valeria: We gradually established a very trusting relationship. Anya studied the topic of bipolar disorder up and down, and I read the articles that she sent me. The diagnosis did not change anything for me, because it remained the same. After that, we already discussed some formalities (for example, who to call in case of an emergency).
The diagnosis did not change anything for me, because it remained the same. After that, we already discussed some formalities (for example, who to call in case of an emergency).
Anna: I asked Lera to watch for hypomanic manifestations in which I lose an adequate assessment of my actions: impulsive night walks, alcohol begin.
Valeria: My friend is a very responsible and conscious girl who takes care of herself, her health and her wallet. Before buying something expensive, she asks for my advice - and then we are already sorting out the situation. We can entrust accounts to each other and not worry. I also know where and to whom to run in cases of exacerbation.
Anna: I react badly to prohibitions and reminders of illness. Yes, I periodically have to turn to relatives for help, change treatment or take long breaks, but I expect mutual respect so that they don’t look at me through the prism of the disease.
When the mood is unstable, harsh phrases like “the disease speaks in you”, “these are not your real emotions” cause persistent rejection, even when they are true. The line between accepting a loved one's illness and identifying him with a diagnosis for healthy people is extremely thin. Therefore, those who were able to grope it deserve great respect.
The line between accepting a loved one's illness and identifying him with a diagnosis for healthy people is extremely thin. Therefore, those who were able to grope it deserve great respect.
Anna: In the last year, I go to see the doctor with my parents. When the doctor notices that I may not be able to do it alone, she duplicates the instructions and advice for them. I, in turn, am a friend. The doctor has repeatedly emphasized that the change of episodes is more noticeable from the outside.
Valeriya: We don't have any kind of hierarchy in relationships, so there is no pressure when one makes decisions for another. This is not eating each other's emotional resources, but complementing and supporting.
Anna: The main danger in a relationship with a person with a serious illness is to fall into codependency. This format is equally bad for both the "controller" and the "subordinate". Unfortunately, I have been in such relationships before. It is worth maintaining mutual respect and treating each other as equals. Illness should not dominate a relationship. In difficult episodes, it temporarily comes to the fore, but you should always remember that you are not a disease.
It is worth maintaining mutual respect and treating each other as equals. Illness should not dominate a relationship. In difficult episodes, it temporarily comes to the fore, but you should always remember that you are not a disease.
Anna: I have memory problems: I don't remember some episodes. In such cases, I can ask Lera for help. If you remember the last weeks, then these are regular reminders to call the doctor. In mixed episodes, this becomes an acute problem, because I can suddenly change my mind or forget. Against the backdrop of a severe episode, I may develop psychosis, and this is the most dangerous thing in the disease. Thanks to our format, I manage to avoid such exacerbations almost always.
The advantages of observation from a loved one are an early response and the fact that he knows the patient's usual behavior very well and can notice even small changes. The main disadvantage is that normal friendly communication risks turning into constant monitoring of symptoms. Not every mentally healthy person is able to remain within the boundaries of reason.
Not every mentally healthy person is able to remain within the boundaries of reason.
It is important to agree in advance, before an attack, what is an undoubted sign of a worsening condition (for example, persistent insomnia), and what you do not need to pay special attention to (for example, loud indignation at something that you do not like). In a difficult situation, often a loved one begins to behave not as an equal, but as a “healthy” and “knowledgeable”. Not all relationships stand this test.
There is also a variant of "buddy" (when two people with mental disorders look after each other. - Note ed. ) - it is good precisely because it is the true request of the patient and more equal relations without mixing roles. But I don't know the buddy support system.
To choose a person you can rely on in a critical situation, take a closer look at your surroundings. Above all, a high level of trust is needed. Your assistant should be open to nonjudgmental and open dialogue and at the same time emotionally stable and resistant to stress.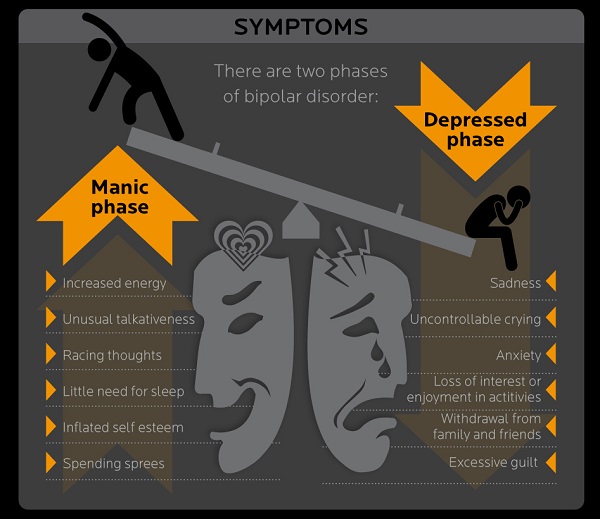
Support is essential for every person - very often we as mental health professionals need it. And with bipolar disorder, this problem is especially acute. At the initial stages, those closest to you often ignore the presence of the disease, and friends advise you to either "pull yourself together" or, conversely, "relax", sometimes with the help of alcohol. When it becomes obvious to everyone that the “condition” will not go away on its own, urgent hospitalization is already required. The saved patient receives the "stigma".
Psychiatrists then make it the responsibility of the uninitiated next of kin (parent or spouse) to monitor any changes in the patient, and they really try to do so. At the level of "laughing out loud - hypomania has begun, upset - depression." As a result, psychiatrists begin to treat quite normal human emotions based on complaints from relatives... and the circle closes.
For this to change, mental health literacy must play a major role. Relatives, in order to be able to help, need to understand well what is happening with a loved one.