Difference between type 1 and 2 bipolar
Bipolar 1 vs. Bipolar 2: Know the Difference
People with bipolar I disorder experience mania in a different way than people with bipolar II disorder. In addition, people with bipolar I disorder may not have major depressive episodes, while all people with bipolar II disorder do.
Most people have emotional ups and downs from time to time. But if you have a condition called bipolar disorder, your moods can reach very high or low levels.
Sometimes you may feel immensely excited or energetic. Other times, you may find yourself sinking into depression. Some of these emotional peaks and valleys can last for weeks or months.
There are four basic types of bipolar disorder:
- bipolar I disorder
- bipolar II disorder
- cyclothymic disorder (cyclothymia)
- other specified and unspecified bipolar and related disorders
Bipolar I and II disorders are more common than the other types of bipolar disorder. Read on to learn how these two types are alike and different.
All types of bipolar disorder are characterized by mood episodes. The highs are known as manic episodes. The lows are known as depressive episodes. Not all bipolar disorder types have episodes of depression.
The main difference between bipolar I and bipolar II disorders lies in the severity of the manic episodes caused by each type.
A person with bipolar I will experience an episode of mania, while a person with bipolar II will experience a hypomanic episode (a period less severe than a full manic episode).
A person with bipolar I may or may not experience a depressive episode, while someone with bipolar II will experience a major depressive episode.
What is bipolar I disorder?
You must have had at least one manic episode lasting 7 or more days to receive a bipolar I disorder diagnosis. A person with bipolar I disorder may or may not have a major depressive episode. The symptoms of a manic episode may require hospital care.
Manic episodes are usually characterized by the following:
- high energy
- restlessness
- trouble concentrating
- feelings of euphoria (extreme happiness)
- behaviors that can lead to harmful consequences
- poor sleep
What is bipolar II disorder?
Bipolar II disorder involves a major depressive episode lasting at least 2 weeks and at least one hypomanic episode. People with bipolar 2 typically don’t experience manic episodes intense enough to require hospitalization.
People with bipolar 2 typically don’t experience manic episodes intense enough to require hospitalization.
Bipolar II is sometimes misdiagnosed as depression, as depressive symptoms may be the major symptom when the person seeks medical attention. When there are no manic episodes to suggest bipolar disorder, the depressive symptoms become the focus.
As mentioned above, bipolar I disorder involves episodes of mania and may involve depression, while bipolar II disorder includes hypomania and depression. Let’s learn more about what these symptoms mean.
Mania
A manic episode is more than just a feeling of elation, high energy, or distraction. During a manic episode, the mania can interfere with daily activities.
People having an episode of mania may make some irrational decisions, such as spending large amounts of money that they can’t afford to spend. They may also engage in behaviors that may have harmful consequences.
An episode is not considered manic if caused by outside influences such as alcohol, drugs, or another health condition.
Hypomania
A hypomanic episode is a period of mania less severe than a manic episode. However, in a hypomanic episode, behavior still differs from your usual state. The differences will be extreme enough that people around you may notice.
Officially, a hypomanic episode isn’t considered hypomania if it’s influenced by drugs or alcohol.
Depression
Depressive symptoms in someone with bipolar disorder are like those of someone with major depressive disorder. They may include extended periods of sadness and hopelessness. You may also experience a loss of interest in people you once enjoyed spending time with and activities you used to like. Other symptoms include:
- tiredness
- irritability
- trouble concentrating
- changes in sleeping habits
- changes in eating habits
- thoughts of suicide
Scientists don’t know what causes bipolar disorder. Physical characteristics of the brain or an imbalance in certain brain chemicals may be among the main causes.
As with many medical conditions, bipolar disorder tends to run in families. If you have a parent or sibling with bipolar disorder, your risk of developing it is higher. The search continues for the genes responsible for bipolar disorder.
Researchers also believe severe stress, drug or alcohol misuse, or upsetting experiences may trigger bipolar disorder. These experiences can include childhood abuse or the death of a loved one.
A psychiatrist or other mental health professional typically diagnoses bipolar disorder. The diagnosis will include a review of both your medical history and any symptoms you have that are related to mania and depression. A trained professional will know what questions to ask.
It can be very helpful to bring a partner or close friend with you during the doctor’s visit. They may be able to answer questions about your behavior that you may not answer easily or accurately.
If you have symptoms of bipolar I or bipolar II, you can always start by telling your doctor. Your doctor may refer you to a mental health specialist if your symptoms appear serious.
Your doctor may refer you to a mental health specialist if your symptoms appear serious.
A blood test may also be part of the diagnostic process. There are no markers for bipolar disorder in the blood, but a blood test and a comprehensive physical exam may help rule out other possible causes for your behavior.
Doctors usually treat bipolar disorder with a combination of medications and psychotherapy.
Mood stabilizers are often the first drugs used in treatment. These may be used long term.
Lithium has been a widely used mood stabilizer for many years. It does have several potential side effects. These include low thyroid function, joint pain, and indigestion. It also requires blood tests to monitor the therapeutic levels of the medication, as well as kidney function. Antipsychotics can be used to treat manic episodes.
Your doctor may start you on a low dose of whichever medication you both decide to use to see how you respond. You may need a stronger dose than what they initially prescribe. You may also need a combination of medications or different medications to manage symptoms.
You may also need a combination of medications or different medications to manage symptoms.
All medications have potential side effects and interactions with other drugs. If you’re pregnant or you take other medications, be sure to tell your doctor before taking any new medications.
Writing in a diary can be an especially helpful part of your treatment. Keeping track of your moods, sleeping and eating patterns, and significant life events can help you and your doctor understand if therapy and medications are working.
If your symptoms don’t improve or worsen, your doctor may order a change in your medications or a different type of psychotherapy.
Online therapy options
Read our review of the best online therapy options to find the right fit.
With proper treatment and support from family and friends, you can manage bipolar disorder symptoms and maintain your quality of life.
It’s important that you follow your doctor’s instructions regarding medications and other lifestyle choices. This includes:
This includes:
- alcohol use
- drug use
- exercise
- diet
- sleep
- stress reduction
Including your friends and family members in your care can be especially helpful.
It’s also helpful to learn as much as you can about bipolar disorder. The more you know about the condition, the more in control you may feel as you adjust to life after diagnosis.
You may be able to repair strained relationships. Educating others about bipolar disorder may make them more understanding of hurtful events from the past.
Support groups, both online and in person, can be helpful for people with bipolar disorder. They can also be beneficial for your friends and relatives. Learning about others’ struggles and triumphs may help you get through any challenges you may have.
The Depression and Bipolar Support Alliance maintains a website that provides:
- personal stories from people with bipolar disorder
- contact information for support groups across the United States
- information about the condition and treatments
- material for caregivers and loved ones of those with bipolar disorder
The National Alliance on Mental Illness can also help you find support groups in your area. Good information about bipolar disorder and other conditions can also be found on its website.
Good information about bipolar disorder and other conditions can also be found on its website.
If you have a diagnosis of bipolar I or bipolar II, remember that this is a condition you can manage. You aren’t alone. Talk with your doctor or call a local healthcare center to find out about support groups or other local resources.
Bipolar 1 vs. Bipolar 2: Know the Difference
People with bipolar I disorder experience mania in a different way than people with bipolar II disorder. In addition, people with bipolar I disorder may not have major depressive episodes, while all people with bipolar II disorder do.
Most people have emotional ups and downs from time to time. But if you have a condition called bipolar disorder, your moods can reach very high or low levels.
Sometimes you may feel immensely excited or energetic. Other times, you may find yourself sinking into depression. Some of these emotional peaks and valleys can last for weeks or months.
There are four basic types of bipolar disorder:
- bipolar I disorder
- bipolar II disorder
- cyclothymic disorder (cyclothymia)
- other specified and unspecified bipolar and related disorders
Bipolar I and II disorders are more common than the other types of bipolar disorder. Read on to learn how these two types are alike and different.
Read on to learn how these two types are alike and different.
All types of bipolar disorder are characterized by mood episodes. The highs are known as manic episodes. The lows are known as depressive episodes. Not all bipolar disorder types have episodes of depression.
The main difference between bipolar I and bipolar II disorders lies in the severity of the manic episodes caused by each type.
A person with bipolar I will experience an episode of mania, while a person with bipolar II will experience a hypomanic episode (a period less severe than a full manic episode).
A person with bipolar I may or may not experience a depressive episode, while someone with bipolar II will experience a major depressive episode.
What is bipolar I disorder?
You must have had at least one manic episode lasting 7 or more days to receive a bipolar I disorder diagnosis. A person with bipolar I disorder may or may not have a major depressive episode. The symptoms of a manic episode may require hospital care.
Manic episodes are usually characterized by the following:
- high energy
- restlessness
- trouble concentrating
- feelings of euphoria (extreme happiness)
- behaviors that can lead to harmful consequences
- poor sleep
What is bipolar II disorder?
Bipolar II disorder involves a major depressive episode lasting at least 2 weeks and at least one hypomanic episode. People with bipolar 2 typically don’t experience manic episodes intense enough to require hospitalization.
Bipolar II is sometimes misdiagnosed as depression, as depressive symptoms may be the major symptom when the person seeks medical attention. When there are no manic episodes to suggest bipolar disorder, the depressive symptoms become the focus.
As mentioned above, bipolar I disorder involves episodes of mania and may involve depression, while bipolar II disorder includes hypomania and depression. Let’s learn more about what these symptoms mean.
Mania
A manic episode is more than just a feeling of elation, high energy, or distraction. During a manic episode, the mania can interfere with daily activities.
During a manic episode, the mania can interfere with daily activities.
People having an episode of mania may make some irrational decisions, such as spending large amounts of money that they can’t afford to spend. They may also engage in behaviors that may have harmful consequences.
An episode is not considered manic if caused by outside influences such as alcohol, drugs, or another health condition.
Hypomania
A hypomanic episode is a period of mania less severe than a manic episode. However, in a hypomanic episode, behavior still differs from your usual state. The differences will be extreme enough that people around you may notice.
Officially, a hypomanic episode isn’t considered hypomania if it’s influenced by drugs or alcohol.
Depression
Depressive symptoms in someone with bipolar disorder are like those of someone with major depressive disorder. They may include extended periods of sadness and hopelessness. You may also experience a loss of interest in people you once enjoyed spending time with and activities you used to like. Other symptoms include:
Other symptoms include:
- tiredness
- irritability
- trouble concentrating
- changes in sleeping habits
- changes in eating habits
- thoughts of suicide
Scientists don’t know what causes bipolar disorder. Physical characteristics of the brain or an imbalance in certain brain chemicals may be among the main causes.
As with many medical conditions, bipolar disorder tends to run in families. If you have a parent or sibling with bipolar disorder, your risk of developing it is higher. The search continues for the genes responsible for bipolar disorder.
Researchers also believe severe stress, drug or alcohol misuse, or upsetting experiences may trigger bipolar disorder. These experiences can include childhood abuse or the death of a loved one.
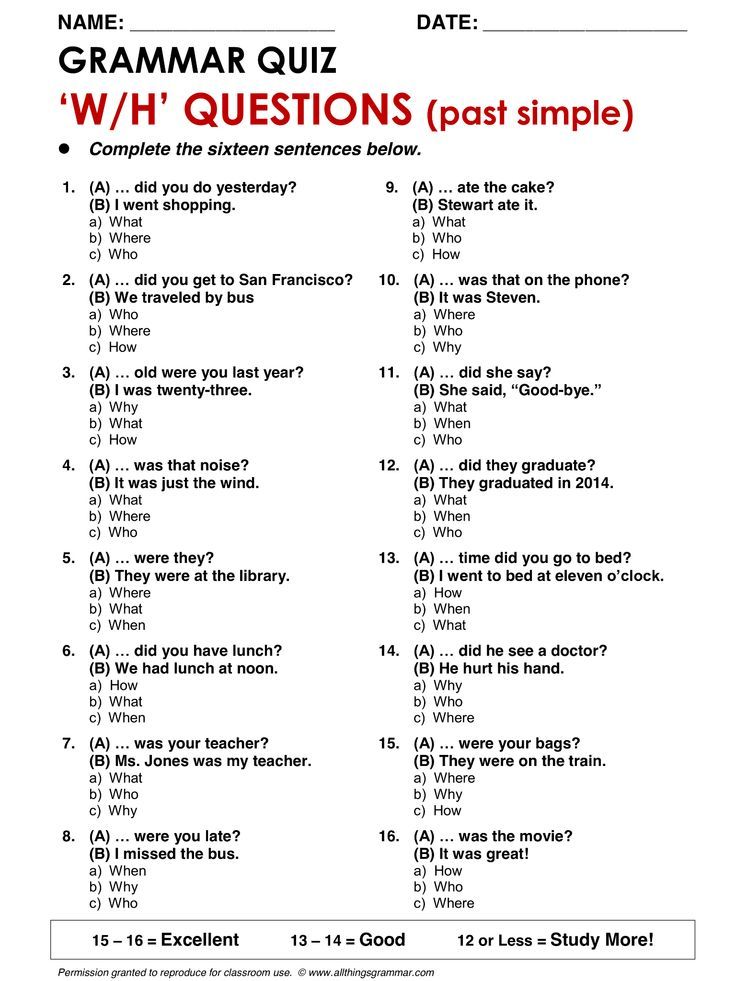
A psychiatrist or other mental health professional typically diagnoses bipolar disorder. The diagnosis will include a review of both your medical history and any symptoms you have that are related to mania and depression. A trained professional will know what questions to ask.
A trained professional will know what questions to ask.
It can be very helpful to bring a partner or close friend with you during the doctor’s visit. They may be able to answer questions about your behavior that you may not answer easily or accurately.
If you have symptoms of bipolar I or bipolar II, you can always start by telling your doctor. Your doctor may refer you to a mental health specialist if your symptoms appear serious.
A blood test may also be part of the diagnostic process. There are no markers for bipolar disorder in the blood, but a blood test and a comprehensive physical exam may help rule out other possible causes for your behavior.
Doctors usually treat bipolar disorder with a combination of medications and psychotherapy.
Mood stabilizers are often the first drugs used in treatment. These may be used long term.
Lithium has been a widely used mood stabilizer for many years. It does have several potential side effects. These include low thyroid function, joint pain, and indigestion. It also requires blood tests to monitor the therapeutic levels of the medication, as well as kidney function. Antipsychotics can be used to treat manic episodes.
It also requires blood tests to monitor the therapeutic levels of the medication, as well as kidney function. Antipsychotics can be used to treat manic episodes.
Your doctor may start you on a low dose of whichever medication you both decide to use to see how you respond. You may need a stronger dose than what they initially prescribe. You may also need a combination of medications or different medications to manage symptoms.
All medications have potential side effects and interactions with other drugs. If you’re pregnant or you take other medications, be sure to tell your doctor before taking any new medications.
Writing in a diary can be an especially helpful part of your treatment. Keeping track of your moods, sleeping and eating patterns, and significant life events can help you and your doctor understand if therapy and medications are working.
If your symptoms don’t improve or worsen, your doctor may order a change in your medications or a different type of psychotherapy.
Online therapy options
Read our review of the best online therapy options to find the right fit.
With proper treatment and support from family and friends, you can manage bipolar disorder symptoms and maintain your quality of life.
It’s important that you follow your doctor’s instructions regarding medications and other lifestyle choices. This includes:
- alcohol use
- drug use
- exercise
- diet
- sleep
- stress reduction
Including your friends and family members in your care can be especially helpful.
It’s also helpful to learn as much as you can about bipolar disorder. The more you know about the condition, the more in control you may feel as you adjust to life after diagnosis.
You may be able to repair strained relationships. Educating others about bipolar disorder may make them more understanding of hurtful events from the past.
Support groups, both online and in person, can be helpful for people with bipolar disorder. They can also be beneficial for your friends and relatives. Learning about others’ struggles and triumphs may help you get through any challenges you may have.
They can also be beneficial for your friends and relatives. Learning about others’ struggles and triumphs may help you get through any challenges you may have.
The Depression and Bipolar Support Alliance maintains a website that provides:
- personal stories from people with bipolar disorder
- contact information for support groups across the United States
- information about the condition and treatments
- material for caregivers and loved ones of those with bipolar disorder
The National Alliance on Mental Illness can also help you find support groups in your area. Good information about bipolar disorder and other conditions can also be found on its website.
If you have a diagnosis of bipolar I or bipolar II, remember that this is a condition you can manage. You aren’t alone. Talk with your doctor or call a local healthcare center to find out about support groups or other local resources.
Bipolar disorder type 1 and 2. What is the difference?
12/29/2022 Asya Melkonyan, psychologist Most important, Encyclopedia 0
In 2021, a new ICD-11 classification of diseases was introduced, in which bipolar disorder types 1 and 2 appeared.
- 6A80 Bipolar I disorder
- 6A81 Bipolar II disorder
- 6A82 Cyclothymic disorder
- 6A8Y Other specified bipolar or related disorders
- 6A8Z Bipolar or related disorders, unspecified
Bipolar disorder type 1
Bipolar disorder type 1 is characterized by: pronounced extended manic (or mixed) episodes. Which are usually replaced by depression. Psychotic symptoms in the form of delusions and hallucinations may be observed. These symptoms are seen in both mania and depression.
Mania is always present in bipolar 1 disorder. Mania is often accompanied by strong agitation and inappropriate behavior of the patient. For a diagnosis to be made, the condition must be experienced at least once in a lifetime. At other times, he may suffer from hypomania or be depressed. Treatment for bipolar 1 disorder is usually aimed at relieving the symptoms of manic psychosis or preventing them from occurring in the future.
This is a classic variant of the course of bipolar disorder, which was described by Kraepelin. Its manifestations are quite bright, easily diagnosed and successfully treated.
The prevalence of bipolar disorder of the first type is 1% of the general population. Men are more often affected, more often than women.
Diagnostic criteria for a diagnosis of bipolar 1 disorder:
At least one manic or mixed episode is required.
Consider this type of bipolar disorder using the example of Mikhail's story, which was published in the book How Bipolar People Live and Dream.
“I was working on a complex project as an IT architect, combined with project management, and I also had the functions of a team leader. I put myself into this work completely, which, as a result, led to a serious decline in strength. I got depressed. There was a feeling of shaking, unrest inside. For a year I tried to fight it, I went to a psychologist, to a neurologist, but it did not help.
I only got worse. Over time, the state became such that I could no longer do anything. I had to leave the project. My family was concerned about my health. As a result, a relative, a doctor, took me to the City Center for Borderline Conditions. I agreed not to go to the hospital, but to visit doctors regularly. Thus, he was constantly under observation. But the treatment, apparently, was incorrect, and my mania was rapidly unfolding. I myself was partly to blame for this, since I began to take antidepressants "by mood", at my own discretion.
The state of mania itself seems interesting and very fun, it's just wonderful to be in it. From the inside, it does not look like something bad, abnormal. You experience constant euphoria, high spirits, there are many interesting, fresh, incredible ideas and projects that you begin to thoughtlessly grasp. It's actually very dangerous and not fun at all. Now I understand that during the period of mania I did a huge amount of stupid things.
Being in a kind of “flight”, I started a large number of “businesses”, using the services of different people. As it turned out later, most of these "colleagues" were swindlers and sucked out of me a huge amount of money.
As a result, I owed about four million. The mania, meanwhile, was replaced by a protracted depression.
Bipolar Type 2
Bipolar Type 2 is a disorder in which the patient may be hypomanic but never enters a manic psychosis. In a hypomanic or premanic state, the patient is aware of what is happening and can perceive what is said to him. Doctors often mistake bipolar 2 disorder for other illnesses, such as ADHD, panic attacks, or an anxiety disorder. An incorrect diagnosis leads to the prescription of drugs and a course of psychotherapy that does not correspond to the real disease. Ultimately, the patient loses a lot of time and effort on treatment, which turns out to be ineffective.
In type 2 bipolar disorder, an episode of depression is long and often severe. A manic episode, on the contrary, is often short and implicit. This type of mild mania is called hypomania.
A manic episode, on the contrary, is often short and implicit. This type of mild mania is called hypomania.
Hypomania is sometimes difficult to notice and can be perceived as an active period in life, full of efficiency and good mood.
She seems so attractive that most patients dream of having her back. And some may even assess their normal state as slightly depressive.
Therefore, patients often do not take into account periods of hypomania and do not report it to the doctor. As a result, they can be treated exclusively for depression for a long time.
In this case, they receive only antidepressants as treatment. And taking them without mood stabilizers or antipsychotics (which are mandatory for bipolar disorder) can aggravate the course of the disease, for example, provoke a rapid cyclicity.
Diagnostic criteria for diagnosis:
Must have one major depressive episode and at least one hypomanic episode.
Bipolar 1 and 2 Videos
- Type 1 Bar
- Type 2 Bar
Website creator, psychologist, works with clients with bipolar disorder. She has been studying bipolar affective disorder for over 6 years. She has experience in personal and group therapy, regularly undergoes supervision. More about education and counseling
Bipolar affective disorder (BAD) - causes, symptoms, treatment
Bipolar affective disorder (BAD) is a severe mental illness characterized by mood and energy swings with recurring episodes of depression followed by episodes of mania or hypomania. BD is highly heritable. Early onset, chronic course and lack of optimal treatment make it one of the most disabling diseases. The lifetime prevalence of bipolar disorder across the spectrum is estimated at 2–4% of the general population and is the sixth leading cause of disability worldwide.
BD is highly heritable. Early onset, chronic course and lack of optimal treatment make it one of the most disabling diseases. The lifetime prevalence of bipolar disorder across the spectrum is estimated at 2–4% of the general population and is the sixth leading cause of disability worldwide.
The average age at onset of bipolar affective disorder varies. According to epidemiological studies, the peak period is 20 years. It is also reported that approximately 20% of all patients show some signs of the disease in adolescence, about 50% by 30 years and 99% by 60 years.
Overall, the data indicate that bipolar disorder is more common in women, but the disease is also widespread among men. Currently, no relationship has been found between incidence and belonging to any social class. By comparison, there is a clear downward social drift among schizophrenic patients.
BAR types
The current diagnostic classification describes two main subtypes: bipolar I disorder and bipolar II disorder, which are distinguished by the absence of full-blown manic episodes in type II bipolar disorder. Type I bipolar disorder can be diagnosed on the basis of a single manic episode, but depressive episodes occur in most cases. Type II bipolar disorder is diagnosed if at least one hypomanic and one depressive episode has occurred. Hypomanic episodes are, by definition, clinically less severe than manic episodes, potentially of shorter duration, not markedly impaired in social or occupational functioning, and do not require hospitalization; the appearance of any psychotic symptoms qualifies the episode as manic.
Type I bipolar disorder can be diagnosed on the basis of a single manic episode, but depressive episodes occur in most cases. Type II bipolar disorder is diagnosed if at least one hypomanic and one depressive episode has occurred. Hypomanic episodes are, by definition, clinically less severe than manic episodes, potentially of shorter duration, not markedly impaired in social or occupational functioning, and do not require hospitalization; the appearance of any psychotic symptoms qualifies the episode as manic.
Causes of bipolar disorder
The mechanisms of the development of the disease are complex, multifaceted and not fully established. Among them, there are genetic predisposition, disturbances in the metabolism of neurotransmitters at the level of the brain, endocrine causes, environmental factors, and others.
Psychiatric genetic research has led to the understanding that bipolar affective disorder and its associated diagnoses undoubtedly have a genetic basis, however, they are not caused by a single abnormal gene, but rather have a highly polygenic structure that is not specific to a particular diagnosis. Large pedigree studies show that BAD accumulates in families. The relative risk for immediate family members of patients with bipolar affective disorder is ~7–10%. It is also known that bipolar I disorder tends to aggregate more in families than bipolar type Ⅱ disorder. BAD runs in families with related diagnoses such as major depressive disorder and schizophrenia. At the same time, schizophrenia is more often associated with BAD type Ⅰ compared to BAD type Ⅱ, and major depressive disorder is clearly not combined with a specific BAD subtype.
Large pedigree studies show that BAD accumulates in families. The relative risk for immediate family members of patients with bipolar affective disorder is ~7–10%. It is also known that bipolar I disorder tends to aggregate more in families than bipolar type Ⅱ disorder. BAD runs in families with related diagnoses such as major depressive disorder and schizophrenia. At the same time, schizophrenia is more often associated with BAD type Ⅰ compared to BAD type Ⅱ, and major depressive disorder is clearly not combined with a specific BAD subtype.
In the 1960s, the instrumental possibilities for conducting experiments with brain samples expanded. It became realistic to evaluate their response to the introduction of certain drugs. The results of such experiments, combined with clinical observations, have generated many hypotheses about a single neurotransmitter responsible for the development of a particular mental illness. The catecholamine theory of the occurrence of bipolar affective disorder is popular. Its central principle is that the two clinical poles of bipolar disorder - mania and depression - arise as a result of functional changes in the activity of catecholamines, while low activity causes a depressive state, and high activity causes a manic state. There is currently strong evidence that the clinical symptoms of BAD can be mimicked and alleviated by pharmacological modulation of the catecholamine system, but there is no direct evidence that the catecholamine system is involved in the pathogenesis of BAD. The same conclusion has been drawn from contemporary evaluations of other influential hypotheses, such as the dopamine hypothesis of schizophrenia.
Its central principle is that the two clinical poles of bipolar disorder - mania and depression - arise as a result of functional changes in the activity of catecholamines, while low activity causes a depressive state, and high activity causes a manic state. There is currently strong evidence that the clinical symptoms of BAD can be mimicked and alleviated by pharmacological modulation of the catecholamine system, but there is no direct evidence that the catecholamine system is involved in the pathogenesis of BAD. The same conclusion has been drawn from contemporary evaluations of other influential hypotheses, such as the dopamine hypothesis of schizophrenia.
The influence of environmental factors is not studied as widely as the influence of genes. However, some reviews show the role of childhood adversity in the development of bipolar disorder, as well as the role of perinatal complications, maternal influenza infection during pregnancy, exposure to maternal smoking in utero, older paternal age at conception, and others.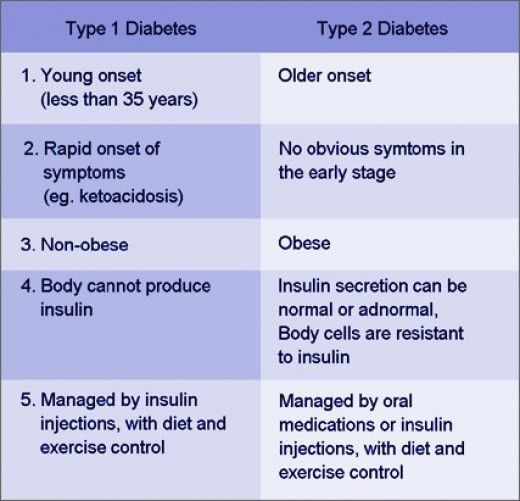
Although stressful life events in and of themselves are not considered a cause of bipolar disorder, they can be a trigger for relapse.
Clinical picture
Bipolar affective disorder refers to mood disorders. It manifests itself in different types of episodes - manic, depressive, mixed, which can be expressed in mild, moderate and severe degrees.
In the case of a depressive syndrome, this can range from subclinical depression to a severe condition that patients perceive as the worst thing that happened in their life. The addition of psychotic symptoms to a severe depressive episode is also likely. These may be delusional ideas of sinfulness, imminent poverty and other misfortunes, for which, according to the patient, he himself is responsible. Auditory hallucinations insult and humiliate, accuse a person, and olfactory hallucinations are most often represented by the smell of sewage. The patient perceives his life as a series of tragic mistakes. Psychomotor retardation can develop up to stupor. Severe depression at least deprives a person of the opportunity to work and maintain social relationships, and in the worst case can lead to suicide.
Psychomotor retardation can develop up to stupor. Severe depression at least deprives a person of the opportunity to work and maintain social relationships, and in the worst case can lead to suicide.
Patients with a mild or even moderate depressive episode certainly experience a reluctance to engage in daily activities, but they usually do not stop functioning fully. They have a significant decrease in mood, loss of interest in the surrounding reality, anhedonia - an inability to enjoy, they feel weak, fatigued. Other symptoms include a decrease in the ability to concentrate, low self-esteem, ideas of one's own insignificance, gloomy ideas about the future, sleep disturbances, and a decrease in appetite.
For a definite diagnosis of depression in bipolar affective disorder, the duration of an episode must be at least two weeks.
Manic syndrome can also be expressed in varying degrees: from hypomania to severe mania with psychotic symptoms.
During the period of hypomania, patients are more socially adapted than in mania.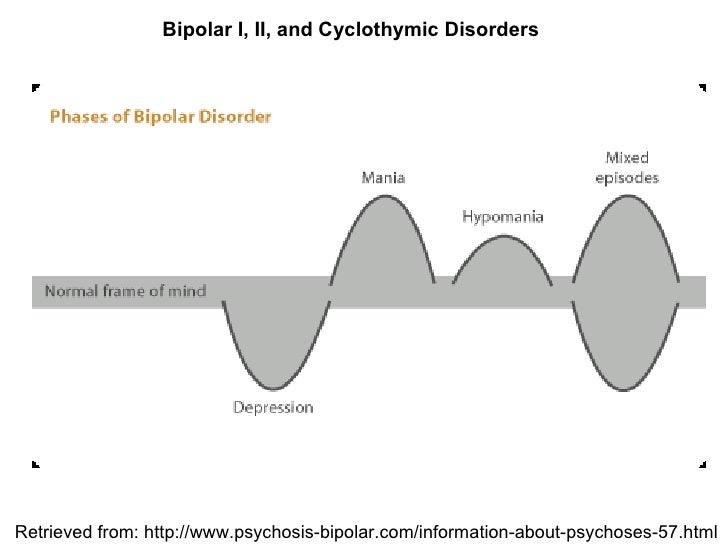 However, in both cases, an important detail is missing - criticism of one's own condition, awareness of oneself as sick.
However, in both cases, an important detail is missing - criticism of one's own condition, awareness of oneself as sick.
The manic stage of bipolar disorder is subjectively more pleasant than the depressive stage. Classical mania, the so-called "jolly mania", is characterized by a typical triad of symptoms: increased mood, ideational-psychic excitement, desire for activity. Patients are in a great mood, they love the whole world, they love themselves. They do not have the slightest doubt in their own abilities, in their own genius, and in addition they have a large supply of energy: many sacrifice sleep for the sake of activity, sleep an hour a day, while not feeling overwhelmed. A person in mania has a false sense of being productive, but new ideas come to him so quickly that old ones remain unfulfilled.
The danger lies in the many rash actions performed by a person on the rise. To give away property, to collect loans, to have questionable sexual contacts, leaving the family and children - a patient with bipolar affective disorder is capable of all this, and he will later have to regret all this.
In addition to classical mania, angry, dysphoric mania also takes place in the structure of the disease. The patient becomes irritable and aggressive beyond measure, especially towards those who do not support his ideas.
The mixed episode combines seemingly incompatible manifestations: melancholy with significant motor arousal, excellent mood simultaneously with stupor, many ideas in parallel with suicidal thoughts. A person is extremely emotionally unstable, which may be a harbinger of an unfavorable outcome of the course of BAD.
The German psychiatrist Emil Kraepelin noted as early as the 19th century that states of manic arousal can vary greatly in duration from weeks to months, and that more severe forms of mania with marked arousal and psychotic features tend to have relatively long episodes. He also believed that melancholic (depressive) states are usually longer than manic episodes, can sometimes persist for years, and tend to become more pronounced than mania at older ages. Modern research confirms these ancient ideas.
Modern research confirms these ancient ideas.
Diagnostics
Bipolar disorder of both types (BAD type Ⅰ and BAD type Ⅱ) is difficult to accurately diagnose in clinical practice, especially in the early stages. Only 20% of patients with bipolar disorder who have had a depressive episode are diagnosed within the first year after seeking treatment, and the average delay between onset and diagnosis is 5–10 years. The main reason for the difficulty in diagnosis is to differentiate bipolar type I or II disorder from unipolar depression, a disease characterized by recurrent depressive episodes, especially in patients who present directly during a depressive episode and in those who do not have a clear history. mania or hypomania. Unipolar depression has been reported to be a common misdiagnosis in patients with bipolar disorder, especially in bipolar II disorder, since patients with this disorder, by definition, never experience major manic episodes.
In recent years, the diagnostic criteria for bipolar disorder have been revised to address this problem to include both mood changes and activity or energy changes. New rating scales for self-administration and clinical use have been developed to help improve the early detection of clinical signs suggestive of a diagnosis of bipolar disorder in people with a history of depressive episodes.
As with most mental illnesses, physicians are forced to focus only on a carefully collected history and observation of the clinical picture, due to the lack of laboratory or instrumental studies that could help establish the diagnosis of bipolar disorder. It requires an analysis of subjective - collected from the words of the patient, as well as objective - collected from the words of the immediate environment, anamnestic data, isolating information about affective episodes, the nature, duration and severity of their course.
Features of the course of BAD in women
There is not much difference between the sexes in lifetime prevalence of bipolar affective disorder. However, there are several clinical characteristics that distinguish men and women with bipolar disorder.
Women have a later age of onset than men. They are more likely to debut during the fifth decade. Women with bipolar disorder are more likely to experience an episode of depression followed by mania, while men with bipolar disorder are either as likely or more likely to experience episodes of mania followed by depression.
A bimodal peak in psychiatric hospitalizations in spring and autumn is observed in women with bipolar disorder compared to a unimodal peak in men in the spring.
Some studies have shown gender differences in the long-term outcome of bipolar disorder. Women face significantly greater disruption to social/recreational and family life. This, apparently, is due to their irritability, increased self-confidence, talkativeness, windiness and excessive financial extravagance, since such behavior on the part of a woman is more condemned in society than on the part of a man.
Women are hospitalized much more often than men because they feel worse and tend to seek medical attention more often.
Complications
The most formidable complication of the disease, of course, is the possible suicide of the patient. The determination of suicidal risk is carried out at the very first diagnostic stage of the survey. It includes clarification of anamnestic data related to previous suicide attempts (if any), as well as an assessment of risk factors. There are special questionnaires that can help with this, for example, the Columbia Suicidal Intention Severity Scale.
Loss of connection with reality during the period of mania, in turn, can also lead to a person causing harm of varying degrees of severity to both himself and others.
BAD treatment
Medical therapy
Due to advances in research on pharmacological and psychosocial treatments for bipolar disorder, recommendations for the treatment of the disorder are frequently revised.
According to recent data, there are several types of treatment for acute mania: mood stabilizers (such as lithium and valproic acid) are widely used in combination with atypical antipsychotics (quetiapine, olanzapine, aripiprazole, risperidone, asenapine, paliperidone, and cariprazine). Typical neuroleptics are also effective in mania, although there is a risk of it switching to depression.
On the other hand, treatment options for acute bipolar depression are relatively limited. There is evidence supporting the efficacy of quetiapine and olanzapine, as well as the combination of olanzapine and fluoxetine, an antidepressant from the group of selective serotonin reuptake inhibitors. In the depressive phase, it is also possible to prescribe lithium.
Widely available and common tricyclic antidepressants can cause rapid episode cycling and manic reversal, so they should not be used in bipolar disorder, even when combined with mood stabilizers.
Ketamine, which has a rapid antidepressant effect on treatment-resistant depression, can also be used to treat bipolar depression.
Neuromodulation
Electroconvulsive therapy finds its use in therapeutically resistant depression in bipolar disorder.
Transcranial magnetic stimulation is effective in unipolar depression and mania, but its effectiveness in bipolar depression has not yet been proven.
Other drugs and supplements
Some research suggests a possible beneficial effect of N-acetylcysteine, an antioxidant, on bipolar depression and ramelteon, a melatonin agonist, on mood stability. A meta-analysis found that omega-3 fatty acids are effective for bipolar depression but not for mania. Clinical trials of nutritional supplements that improve mitochondrial function are currently ongoing.
Psychosocial treatments
In the treatment of bipolar disorder, pharmacological and psychosocial approaches must work closely together.
With regard to psychosocial treatment, psychoeducation is paramount and should be carried out for all patients, as this significantly reduces the number of relapses.
Various types of psychotherapy are used in the treatment of bipolar disorder: interpersonal and social rhythm therapy (IPSRT) - a modified version of interpersonal therapy specifically designed for the treatment of bipolar disorder, family therapy, cognitive behavioral therapy (CBT).