Diagnosis code for psychotherapy
Top ICD-10 Codes for Mental & Behavioral Health Therapists
Top ICD-10 Codes for Mental and Behavioral Health
- Posted: May 29, 2018
- |
- TheraNest Team
Insurance billing is no easy task. It is made even more confusing by the vast amount of terminology (and acronyms) used for even the most simple of tasks. There are thousands of codes you have to juggle — CPT, ICD-10, and DSM 5, just for starters. It is easy to choose the wrong code but it can be a costly mistake. In this post, we’re breaking down and defining what ICD, DSM, and CPT mean and how you, as a therapist, use them every day.
ICD and DSM and CPT, Oh My!
You’ve probably seen or at least, heard of each of these terms before. But what do they actually mean?
CPT stands for Current Procedural Terminology. This is a standardized set of codes published and maintained by the American Medical Association (AMA). The CPT codes for psychiatry, psychology, and behavioral health underwent a revision in 2013 and aren’t scheduled for another revision anytime soon. To put things into perspective, the last time the codes were changed before 2013 was in 1998 (meaning you really only will need to learn the CPT codes you use once). CPT codes describe the action taken or the treatment provided to clients. These five-digit codes are used to quantify any treatment a client relieves whether that be a trip to the ER or a therapy session.
CPT codes are essential for billing. Whether you bill directly to insurance companies or you provide your clients with superbills, having the correct CPT codes is necessary if you want to get paid in full and avoid an insurance audit. CPT codes and add on codes are used to convey the exact service you provided to your client and from there they eventually determine how much you are paid.
Using the wrong CPT code can be detrimental for your pay cycle in specific and for the health of your practice in general.
 Two of the most common mistakes when it comes to CPT codes and medical billing is undercoding and upcoding:
Two of the most common mistakes when it comes to CPT codes and medical billing is undercoding and upcoding:
- Undercoding: This is when you use a CPT code that represents a lower-priced treatment or a less severe diagnosis. While this can be done by mistake, undercoding is often intentional. A provider intentionally leaves out a service rendered as a way to save money for the patient. Providers may also undercode to avoid auditing from an insurance company. Regardless of the reason it is done, undercoding is illegal.
- Upcoding: This is when you use a CPT code that represents a higher-priced treatment or a more severe diagnosis. Sometimes this can be done to receive higher reimbursement. Though, upcoding is illegal (and unethical), it is not always done with malicious intent. Upcoding often results from having an untrained staff member (remember even if this was an employee error if you get audited by an insurance company this blame falls on you so make sure to hire properly trained staff!).

There are over 8,000 CPT codes out there, however, the good news is only 24 of these codes are designated for psychotherapy. The even better news is that you, as a therapist, will likely only use about 8 of these regularly. The most common CPT codes used by therapists are:
- 90791 – Psychiatric Diagnostic Evaluation
- 90792 – Psychiatric Diagnostic Evaluation with medical services
- 90832 – Psychotherapy, 30 minutes (16-37 minutes)
- 90834 – Psychotherapy, 45 minutes (38-52 minutes)
- 90837 – Psychotherapy, 60 minutes (53 minutes and over)
- 90846 – Family or couples psychotherapy, without the patient present
- 90847 – Family or couples psychotherapy, with the patient present
- 90853 – Group Psychotherapy (not family)
- 90839 – Psychotherapy for crisis, 60 minutes (30-74 minutes).
- Used in conjunction with 90839: +90840 – Add-on code for an additional 30 minutes (75 minutes and over)
If you have more questions about CPT codes and billing, check out our Billing 101 eBook. Now you may be asking yourself, this is great, but what do CPT codes have to do with ICD-10 and DSM 5? The answer is everything.
Now you may be asking yourself, this is great, but what do CPT codes have to do with ICD-10 and DSM 5? The answer is everything.
Connecting ICD 10 and DSM 5 to CPT Code
Let’s take a step back. Before we explore the relationship between ICD-10/ DSM 5 and CPT codes– let’s talk about the relationship between ICD 10 and DSM 5 codes. Both ICD-10 and DSM 5 codes are used for diagnosis. How are they different? They’re not.
ICD codes are the World Health Organization (WHO)’s International Classification of Diseases and Related Health Problems and they are used together with CPT codes to bill insurances.
DSM 5 codes are the codes outlined in The Diagnostic and Statistical Manual of Mental Disorders(Fifth Edition). This manual is a taxonomic and diagnostic tool used published by the American Psychiatric Association.
ICD-10 and DSM 5 codes are the same. The DSM is a guide to picking the correct ICD code. The DSM 5 was published in May of 2013 and went into effect on January 1, 2014–right ahead of when the entire medical community switched from using ICD-9 to ICD-10 codes on October 1, 2015. The main difference between ICD-9 and ICD-10 is there are many more diagnosis pathways for clients in ICD-10 than there were in ICD-9 (check out our handy ICD-10 converter).
DSM is relevant to the mental health community because it endorses and lists most (but not all) mental and behavioral health ICD codes. The confusion whether DSM and ICD codes are the same or not stems from the fact that the DSM is the only accepted guide to ICD codes in the mental health industry. This leads many therapists to believe there is a separate list of DSM codes that are not connected with ICD codes when there is not. DSM is ICD–DSM directs therapists to the correct ICD diagnosis codes they need to bill.
This brings us back to our critical question, how are CPT and ICD related? The relationship between an ICD code and a CPT code is that the diagnosis supports the medical necessity of the treatment.
The DSM 5 was published in May of 2013 and went into effect on January 1, 2014–right ahead of when the entire medical community switched from using ICD-9 to ICD-10 codes on October 1, 2015. The main difference between ICD-9 and ICD-10 is there are many more diagnosis pathways for clients in ICD-10 than there were in ICD-9 (check out our handy ICD-10 converter).
DSM is relevant to the mental health community because it endorses and lists most (but not all) mental and behavioral health ICD codes. The confusion whether DSM and ICD codes are the same or not stems from the fact that the DSM is the only accepted guide to ICD codes in the mental health industry. This leads many therapists to believe there is a separate list of DSM codes that are not connected with ICD codes when there is not. DSM is ICD–DSM directs therapists to the correct ICD diagnosis codes they need to bill.
This brings us back to our critical question, how are CPT and ICD related? The relationship between an ICD code and a CPT code is that the diagnosis supports the medical necessity of the treatment. HIPAA, starting in 2003, made it mandatory to have an ICD code for any electronic transaction used for billing, reimbursement, or reporting purposes. So to bill insurance, you need to have a CPT code which explains the treatment/service you provided a client and an ICD 10 code that outlines the diagnosis for a patient which explains why the treatment/service you provided was necessary.
The most common ICD 10 codes for mental and behavioral health therapists and practitioners are:
HIPAA, starting in 2003, made it mandatory to have an ICD code for any electronic transaction used for billing, reimbursement, or reporting purposes. So to bill insurance, you need to have a CPT code which explains the treatment/service you provided a client and an ICD 10 code that outlines the diagnosis for a patient which explains why the treatment/service you provided was necessary.
The most common ICD 10 codes for mental and behavioral health therapists and practitioners are:
- F32.9 Major depressive disorder, single episode, unspecified
- F32.0 Major depressive disorder, single episode, mild
- F32.1 Major depressive disorder, single episode, mild
- F32.1 Major depressive disorder, single episode, moderate
- F32.2 Major depressive disorder, single episode, severe without psychotic features
- F32.3 Major depressive disorder, single episode, severe with psychotic features
- F32.
 4 Major depressive disorder, single episode, in partial remission
4 Major depressive disorder, single episode, in partial remission - F32.5 Major depressive disorder, single episode, in full remission
- F32.8 Other depressive episodes
- F33.1 Major depressive disorder, recurrent, moderate
- F33.2 Major depressive disorder, recurrent severe without psychotic features
- F33.3 Major depressive disorder, recurrent, severe with psychotic symptoms
- F39 Unspecified mood [affective] disorder
- F25.9 Schizoaffective disorder, unspecified; See also:
- F25.0 Schizoaffective disorder, bipolar type,
- F25.1 Schizoaffective disorder, depressive type,
- F25.8 Other schizoaffective disorders
- F29 Unspecified psychosis not due to a substance or known physiological condition
- F41.9 Anxiety disorder, unspecified
- F41.1 Generalized anxiety disorder
- F41.
 8 Other specified anxiety disorders
8 Other specified anxiety disorders - F41.0 Panic disorder [episodic paroxysmal anxiety] without agoraphobia
- F41.1 Generalized anxiety disorder
- F42 Obsessive-compulsive disorder
- F32.1 Agoraphobia with panic disorder
- F90.0 Attention-deficit hyperactivity disorder, predominantly inattentive type
- F90.1 Attention-deficit hyperactivity disorder, predominantly hyperactive type
- F90.2 Attention-deficit hyperactivity disorder, combined type
- F90.8 Attention-deficit hyperactivity disorder, other type
- F90.9 Attention-deficit hyperactivity disorder, unspecified type
- G30.0 Alzheimer’s disease with early-onset
- G30.1 Alzheimer’s disease with late-onset
- G30.8 Other Alzheimer’s disease
- G30.9 Alzheimer’s disease, unspecified
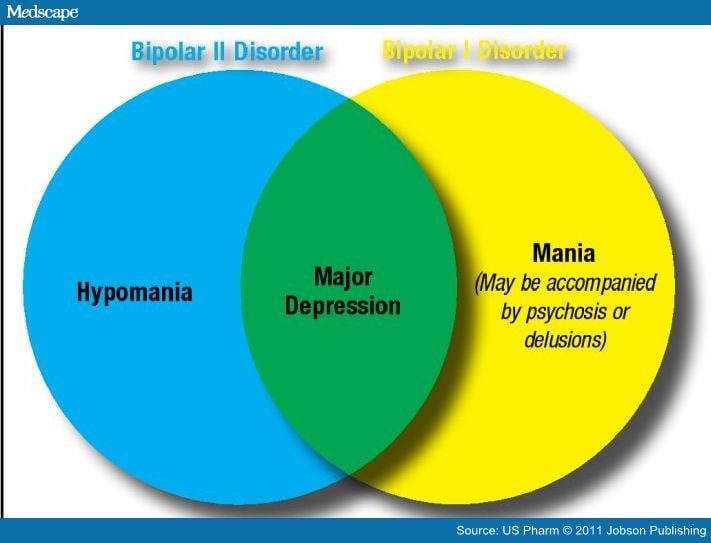
- F31.9 Bipolar disorder, unspecified
- F31.
 0 Bipolar disorder, current episode hypomanic
0 Bipolar disorder, current episode hypomanic - F31.10 Bipolar disorder, current episode manic without psychotic features, unspecified
- F31.11 Bipolar disorder, current episode manic without psychotic features, mild
- F31.12 Bipolar disorder, current episode manic without psychotic features, moderate
- F31.13 Bipolar disorder, current episode manic without psychotic features, severe
- F31.30 Bipolar disorder, current episode depressed, mild or moderate severity, unspecified
- F31.31 Bipolar disorder, current episode depressed, mild
- F11.20 Opioid dependence, uncomplicated
- F11.21 Opioid type dependence in remission
- F11.220 Opioid dependence with intoxication, uncomplicated
- F11.221 Opioid dependence with intoxication delirium
- F11.22 Opioid dependence with intoxication with perceptual disturbance
- F43.10 Posttraumatic stress disorder, unspecified
- F43.
 11 Posttraumatic stress disorder, acute
11 Posttraumatic stress disorder, acute - F43.12 Posttraumatic stress disorder, chronic
- F43.23 Adjustment disorder with mixed anxiety and depressed mood
- Z79.891 Long term (current) use of opiate analgesic
- Z79.899 Other long term (current) drug therapy
- Z03.89 Encounter for observation for other suspected diseases and conditions ruled out
Remember, this is not an exhaustive list. There may be clients you see who have conditions that we did not include above. This list serves only as an overview to show you some of the most common ICD-10 codes that other mental and behavioral health therapists use on a regular basis.
Though it can be easy to become overwhelmed with the number of different codes out there when it comes to medical billing as a therapist, we hope this post has helped breakdown some of the confusion you may have been experiencing.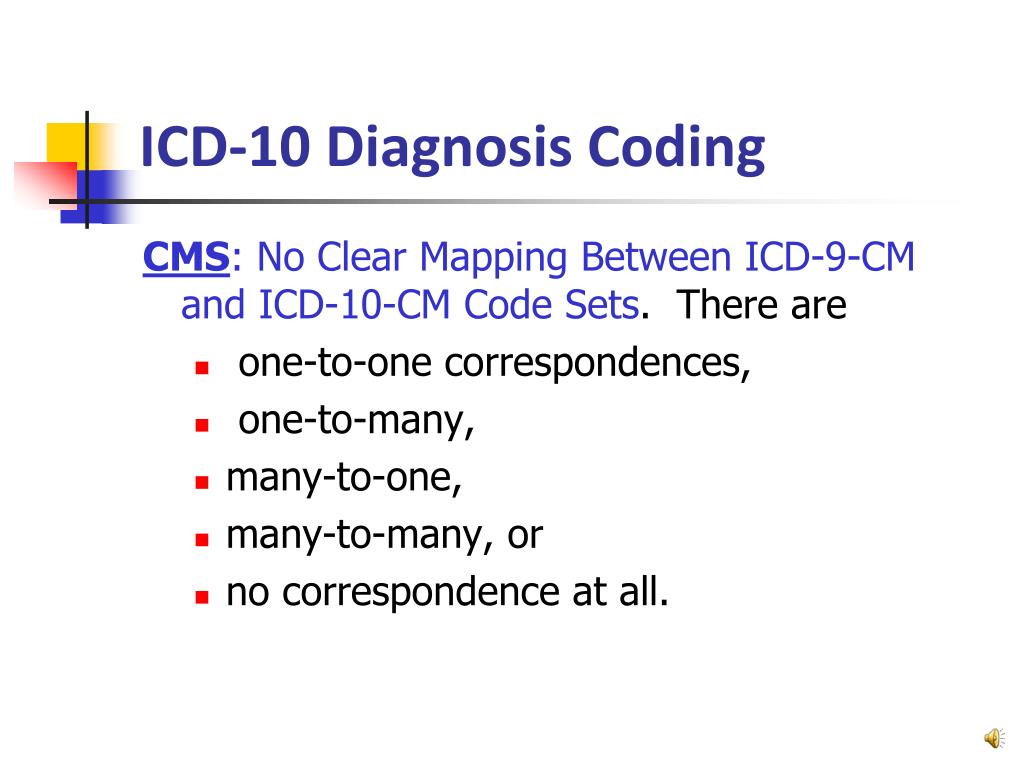 There’s no doubt that billing can be an exhausting task, we’re here to help make it as easy as we can.
Learn More About TheraNest Billing Solutions
There’s no doubt that billing can be an exhausting task, we’re here to help make it as easy as we can.
Learn More About TheraNest Billing Solutions
The 20 Most Commonly Used ICD-10 Codes in Mental Health in 2022
To get more insight into the usage and trends of the behavioral health community in 2021, we identified the most common ICD-10 codes in 2022 used by SimplePractice clinicians.
This data on the most frequently used ICD-10 codes is pulled from SimplePractice clinicians who have billed health insurance providers over the past calendar year, so this report represents common diagnostic codes used by solo or small group providers in the behavioral health space across the United States.
What Are ICD Codes Used For?
ICD codes are International Classification of Disease codes. They’re used to describe a diagnosis when billing insurance.
ICD codes were developed by the World Health Organization (WHO), and are used across the medical field to describe a huge variety of conditions.
In addition to being used to bill for healthcare services, they’re also a way to identify health and disease trends across countries using a standard diagnostic language.
Top Billed ICD-10 Diagnosis Codes List
This ICD codes list shows the most frequently billed ICD-10 codes used for mental health conditions diagnosed in 2022.
Perhaps it’s not surprising that the most used ICD-10 code for anxiety in America was for F41.1—generalized anxiety disorder.
This continues trends seen in the top billed codes in 2019 and even back in 2017 as well.
| Rank | Code | Diagnosis |
| 1 | F41.1 | Generalized anxiety disorder |
| 2 | F43.23 | Adjustment disorder with mixed anxiety and depressive mood |
| 3 | F33.1 | Major depressive disorder, recurrent, moderate |
| 4 | F43. 22 22 |
Adjustment disorder with anxiety |
| 5 | F43.20 | Adjustment disorder, unspecified |
| 6 | F41.9 | Anxiety disorder, unspecified |
| 7 | F43.10 | Post traumatic stress disorder, unspecified |
| 8 | F43.21 | Adjustment disorder with depressed mood |
| 9 | F43.12 | Post traumatic stress disorder, chronic |
| 10 | Z63.0 | Problem in relationship with spouse or partner |
| 11 | F33.0 | Major depressive disorder, recurrent, mild |
| 12 | F90.2 | Attention-deficit hyperactivity disorder, combined type |
| 13 | F32.1 | Major depressive disorder, single episode, moderate |
| 14 | F34. 1 1 |
Dysthymic disorder |
| 15 | F90.0 | Attention-deficit disorder, predominantly inattentive type |
| 16 | F33.2 | Major depressive disorder, recurrent, without psychotic features |
| 17 | F32.0 | Major depressive disorder, single episode, mild |
| 18 | F43.25 | Adjustment disorder with mixed disturbance of emotions and conduct |
| 19 | F41.0 | Panic disorder (episodic paroxysmal anxiety) |
| 20 | F84.0 | Autistic disorder |
Top Diagnoses Categories
To get a better understanding of the top mental health diagnoses made in 2022, we took the 20 ICD codes in 2022 listed above and rolled them up into 4 corresponding categories, as shown below.
| Rank | Category | % of total diagnoses |
| 1 | Adjustment disorders | 20% |
| 2 | Major depressive disorders | 20% |
| 3 | PTSD | 8% |
| 4 | Attention-deficit hyperactivity disorders | 8% |
Changes to ICD Codes in 2022
On January 1, 2022, the ICD-10 updated to the ICD-11, as mandated by the WHO.
The ICD-11 reflects advances in science and medicine, and aligns classifications with the latest knowledge of disease prevention and treatment. Some notable changes in the ICD-11 include:
- New core chapters for “diseases of the immune system,” “sleep-wake disorders,” and “conditions related to sexual health.”
- Overall coding improvements to allow more precise data collection, including new codes for antimicrobial resistance, specific coding for clinical stages of HIV, codes for common skin cancers, and more.
- Improved ease of coding requires less user-training, and new availability for online and offline functioning
To learn more about the updates to ICD-11, you can visit the WHO’s website dedicated to the update, where you’ll find more resources on the changes and how to implement them in your practice.
When Do You Have to Actually Start Using ICD-11?
There’s often a delay between when ICD updates are published and when they actually start being used, and the ICD-11 is no exception.
Although the updates officially became available to member states of the WHO as of January 1, 2022, the US doesn’t have an official implementation plan for rollout, and they may not be implemented until 2025.
It’s up to each country to make the shift, and it’ll take some time for the US to update from the ICD-10.
How the ICD Updates Impact Your Practice
Since ICD codes are used across multiple healthcare fields, there’ll probably be a lot of codes in each update that don’t apply to your billing.
That said, you do want to review the annual updates carefully—if you use a deleted code that’s no longer recognized, or try to use an old version of a code, the reimbursement for that service may be denied.
If you have a list of the previous codes that you use frequently in your practice, you can use the “Search” Function in documents from CMS to only look directly for what you need. That way you can quickly determine what changes, if any, have been made to your most regularly used codes and make the necessary adjustments to your billing documents.
The world of insurance billing can get complicated pretty quickly. To avoid getting stuck in endless billing conversations, set aside a block of time to go through all the new information thoroughly, and get all the relevant information. This will help you to become confident your billing is set up correctly, so you can spend more time with your clients, and less on billing.
SimplePractice
makes billing with
ICD-10 easyStart for freeList Checkmark
Free for 30 days
List CheckmarkNo credit card required
ICD-10 - codes of diseases - Psychotherapist Sergei Melnikov
To read the contents of the section, click on the title. Clicking again will collapse the section.
F00-F09 Organic, including symptomatic, psychiatric disorders
F00 Alzheimer's dementia
F00.0 Early-onset Alzheimer's dementia
F00. 1 Late-onset Alzheimer's dementia
1 Late-onset Alzheimer's dementia
F00.2 Alzheimer's dementia, atypical or mixed type
F00.9 Dementia of Alzheimer's disease, unspecified
F01 Vascular dementia
F01.0 Vascular dementia with an acute beginning of
F01.1 Multinfarct Dementia
F01.2 Subcortical vascular dementia 9000 F01.3 Mixed cortical dementia 9000 F01 .8 Other vascular dementia
F01.9 Vascular dementia, unspecified
F02 Dementia in diseases classified elsewhere
F02.0 Dementia in Pick's disease
F02.1 Dementia in Creutzfeldt-Jakob disease
F02.2 Dementia in Huntington's disease
F02.3 Dementia in Parkinson's disease
F02.4 Dementia in diseases associated with human immunodeficiency virus (HIV)
F02.8 Dementia in other specified diseases classified elsewhere
F03 Dementia, unspecified
A fifth character may be used to specify dementia in F00-F03:
. x0 without additional symptoms
. x1 with other symptoms, mostly delusional
. x1 with other symptoms, mostly hallucinatory
x1 with other symptoms, mostly hallucinatory
. x3 with other symptoms, predominantly depressive
. x4 with other mixed symptoms. A sixth character may be used to indicate the severity of dementia:
. xx0 Light
. xx1 Moderate
. хх2 Severe
F04 Organic amnesic syndrome, not caused by alcohol or other psychoactive substances
F05 Delirium, not caused by alcohol or other psychoactive substances
F05.0 Delirium, not associated with dementia
F05.1 Delirium associated with dementia
F05.8 Other delirium
F05.9 Delirium, unspecified
F06 Other mental disorders due to damage or dysfunction of the brain, or due to physical illness
F06.0 Organic hallucinosis
F06.1 Organic catatonic disorder
F06.2 Organic delusional (schizophrenia-like) disorder
F06.3 Organic (affective) disorders
F06.4 Organic anxiety disorder
F06.5 Organic dissociative disorders
F06.6 Organic emotionally labile (asthenic) disorders
F06. 7 Mild cognitive impairment
7 Mild cognitive impairment
F06.8 Other specified mental disorders due to damage and dysfunction of the brain and physical disease
F06.9 Unspecified mental disorders due to brain damage and dysfunction and physical disease
F07 Personality and behavioral disorders due to brain damage and dysfunction disease
F07.0 Organic personality disorder
F07.1 Post-encephalic syndrome
F07.2 Post-concussion syndrome
F07.8 Other organic personality and behavioral disorders due to disease of brain injury and dysfunction
F07.9 Unspecified mental disorders due to disease of brain injury and dysfunction brain
F09 Unspecified organic or symptomatic mental
F10-F19 Mental and behavioral disorders due to the use of psychoactive substances
F10 Mental and behavioral disorders due to the use of alcohol
F11 Mental and behavioral disorders due to the use of opioids
F12 Mental and behavioral disorders due to the use of cannabinoids
F13 Mental and behavioral disorders due to the use of sedatives or sedatives
F14 Mental and behavioral disorders due to cocaine use
F15 Mental and behavioral disorders due to use of other stimulants, including caffeine
F16 Mental and behavioral disorders due to hallucinogen use
F17 Mental and behavioral disorders due to tobacco use
F183 Mental and behavioral disorders due to use of tobacco use of volatile solvents
F19 Mental and behavioral disorders resulting from combined drug use and the use of other psychoactive substances The 4th and 5th characters can be used to clarify the clinical condition, and in appropriate cases of acute intoxication and withdrawal states, diagnostic criteria are given, specific for each psychoactive substance
F1x. 0 Acute intoxication
0 Acute intoxication
. 00 uncomplicated
. 01 with injury or other bodily injury
. 02 with other medical complications
. 03 with delirium
. 04 with perceptual disorders
. 05 with coma
. 06 with convulsions
. 07 morbid intoxication
F1x.1 Harmful use
F1x.2 Dependency syndrome
. 20 currently abstinence
. 200 Early remission
. 201 Partial remission
. 202 Complete remission
. 21 currently abstinence, but under conditions precluding the use of
. 22 currently under clinical supervision on maintenance or replacement therapy (controlled addiction)
. 23 currently abstinent but on treatment with aversive or blocking drugs
. 24 currently using a psychoactive substance (active addiction)
. 240 without physical symptoms
. 241 with physical symptoms
. 25 episodic use
F1x.3 Cancellation status
. 30 uncomplicated
. 31 with convulsions
F1x.4 State of withdrawal with delirium
. 40 without convulsions
40 without convulsions
. 41 with convulsions
F1x.5 Psychotic disorder
. 50 schizophreniform
. 51 predominantly delusional
. 52 predominantly hallucinatory
. 53 predominantly polymorphic
. 54 predominantly with depressive psychotic symptoms
. 55 predominantly with manic psychotic symptoms
. 56 mixed
F1x.6 Amnestic syndrome
F1x.7 Residual psychotic disorder and late onset psychotic disorder
. 70 reminiscences
. 71 personality or behavioral disorders
. 72 residual affective disorder
. 73 dementia
. 74 other persistent cognitive impairment
. 75 Late onset psychotic disorder
F1x.8 Other mental and behavioral disorders
F1x.9 Unspecified mental and behavioral disorder
F20-F29 schizophrenia, schizotypic and delusional disorders
F20 F20 of schizophrenia
F20. 0 Paranoid schizophrenia
0 Paranoid schizophrenia
F20.1 Hybephrenic schizophrenia 9000.2 Catatonic schizophrenia
F20.3 undifferentiated schizophrenia
F20.4 postshizophrenic depression 9000.5 f20s of reservo
F20.6 Simple schizophrenia
F20.8 Other forms of schizophrenia
F20.9 Schizophrenia, unspecified
The course of schizophrenic disorders may be classified using the following fifth characters:
. x0 continuous
. x1 episodic with growing defect
. x2 episodic with stable defect
. x3 episodic remitting
. x4 incomplete remission
. x5 complete remission
. x8 other
. x9 course unclear, follow-up period too short
F21 Schizotypal disorder
F22 Chronic delusional disorders
F22.0 Delusional disorder
F22.8 Other chronic delusional disorders
F22.9Chronic delusional disorder, unspecified
F23 Acute and transient psychotic disorders
F23.0 Acute polymorphic psychotic disorder without symptoms of schizophrenia
F23. 1 Acute polymorphic psychotic disorder with symptoms of schizophrenia
1 Acute polymorphic psychotic disorder with symptoms of schizophrenia
F23.2 Acute schizophrenia-like psychotic disorder predominantly 9304 delusional psychotic disorders
F23.8 Other acute and transient psychotic disorders
F23.9Acute and transient psychotic disorders, unspecified
A fifth character may be used to indicate the presence or absence of acute associated stress:
. x0 without associated acute stress
. x1 with associated acute stress
F24 Induced delusional disorder
F25 Schizoaffective disorders
F25.0 Schizoaffective disorder, manic type
F25.1 Schizoaffective psychosis
F25.2 Schizoaffective disorder, mixed type
F25.8 Other schizoaffective disorders
F25.9 Schizoaffective disorder, unspecified
The following fifth character subtypes may be distinguished:
. x0 simultaneously only affective and schizophrenic symptoms
. x1 both affective and schizophrenic symptoms, plus persistence of schizophrenic symptoms after the disappearance of affective symptoms
F28 Other non-organic psychotic disorders
F29 Unspecified non-organic psychosis
F30-F39 Affective mood disorders
F30 Manic episode
F30. 0 Hypomania
0 Hypomania
F30.1 Mania without psychotic symptoms
F30.2 Mania with psychotic symptoms
. 20 with mood-related psychotic symptoms
. 21 with mood-inappropriate psychotic symptoms
F30.8 Other manic episodes
F30.9 Manic episodes, unspecified
F31 Bipolar affective disorder
F31.0 Bipolar affective disorder, current hypomanic episode
F31.1 Bipolar affective disorder, current manic episode without psychotic symptoms
F31.2 Bipolar affective disorder, current manic episode with psychotic symptoms
. 20 with mood-related psychotic symptoms
. 21 with mood-inappropriate psychotic symptoms
F31.3 Bipolar affective disorder, current episode of moderate or mild depression
. 30 without somatic symptoms
. 31 with somatic symptoms
F31.4 Bipolar affective disorder, current episode of severe depression without psychotic symptoms
F31.5 Bipolar affective disorder, current episode of severe depression with psychotic symptoms
. 50 with mood-related psychotic symptoms
50 with mood-related psychotic symptoms
. 51 with mood inappropriate psychotic symptoms
F31.6 Bipolar affective disorder, current episode mixed
F31.7 Bipolar affective disorder, remission
F31.8 Other bipolar affective disorders
F31.9 Bipolar affective disorder, unspecified
F32 Depressive episode
F32.0 Mild depressive episode
. 00 without somatic symptoms
. 01 with somatic symptoms
F32.1 Moderate depressive episode
. 10 without somatic symptoms
. 11 with somatic symptoms
F32.2 Major depressive episode without psychotic symptoms
F32.3 Major depressive episode with psychotic symptoms
. 30 with mood-related psychotic symptoms
. 31 with mood inappropriate psychotic symptoms
F32.8 Other depressive episodes
F32.9 Depressive episodes, unspecified
F33 Recurrent depressive disorder
F33.0 Recurrent depressive disorder, current mild episode
. 00 without somatic symptoms
. 01 with somatic symptoms
01 with somatic symptoms
F33.1 Recurrent depressive disorder, moderate current episode
. 10 without somatic symptoms
. 11 with somatic symptoms
F33.2 Recurrent depressive disorder, current episode severe without psychotic symptoms
F33.3 Recurrent depressive episode, current episode severe with psychotic symptoms
. 30 with mood-related psychotic symptoms
. 31 with mood-inappropriate psychotic symptoms
F33.4 Recurrent depressive disorder, remission
F33.8 Other recurrent depressive disorders
F33.9 Recurrent depressive disorder, unspecified
F34 Chronic (affective) mood disorders
F34.0 Cyclothymia 9000 8 Other chronic affective disorders
F34.9 Chronic (affective) mood disorder, unspecified
F38 Other (affective) mood disorders
F38.0 Other single (affective) mood disorders
. 00 mixed affective episode
F38.1 Other recurrent (affective) mood disorders
. 10 recurrent brief depressive disorder
F38. 8 Other specified (affective) mood disorders 21
8 Other specified (affective) mood disorders 21
F39 Unspecified (affective) mood disorders
F40-F48 Neurotic, stress-related and somatoform disorders
F40 Anxiety-phobic disorders
F40.0 Agoraphobia
. 00 without panic disorder
. 01 with panic disorder
F40.1 Social phobias
F40.2 Specific (isolated) phobias
F40.8 Other phobic anxiety disorders
F40.9 Phobic anxiety disorder, unspecified
F41 Other anxiety disorders
F41.002 Panic disorder (episodic paroxysmal anxiety)
. 00 Moderate
. 01 Severe
F41.1 Generalized anxiety disorder
F41.2 Mixed anxiety and depressive disorder
F41.3 Other mixed anxiety disorders
F41.8 Other specified anxiety disorders
F41.9 Anxiety disorder, unspecified
-compulsive disorder F42
F42.0 Predominantly obsessive thoughts or ruminations (mental chewing)
F42. 1 Predominantly compulsive acts (obsessional rituals)
1 Predominantly compulsive acts (obsessional rituals)
F42.2 Mixed obsessive thoughts and actions
F42.8 Other obsessive-compulsive disorders
F42.9 Obsessive-compulsive disorder, unspecified
F43 Reaction to severe stress and adjustment disorders
F43.0 Acute reaction to stress
. 00 Lightweight
. 01 Moderate
. 02 Severe
F43.1 Post-traumatic stress disorder
F43.2 Adjustment disorder
. 20 short-term depressive reaction
. 21 prolonged depressive reactions
. 22 mixed anxiety and depressive reactions
. 23 with a predominance of disturbances of other emotions
. 24 with a predominance of behavioral disorders
. 25 mixed disorder of emotions and behavior
. 28 other specific predominant symptoms
F43.8 Other reactions to severe stress
F43.9 Reaction to severe stress, unspecified
F44 Dissociative (conversion) disorders
F44.0 Dissociative amnesia
F44.1 Dissociative fugue
F44. 2 Dissociative stupor
2 Dissociative stupor
F44.3 Trances and mastery states
F44.4 Dissociative motor disorders
F44.5 Dissociative convulsions
F44.6 Dissociative anesthesia and sensory loss
F44.7 Mixed dissociative (conversion) disorders
F4. 8 Other dissociative (conversion) disorders
. 80 Ranser syndrome
. 81 multiple personality disorders
. 82 transient dissociative (conversion) disorders occurring in childhood and adolescence
. 88 Other specified dissociative (conversion) disorders
F44.9 Dissocial (conversion) disorder, unexpected
F45 Somatoform Disorders
F45.0 Somatic disorder
F45.1 undifferentiated somato disorder
F45.2 Ipochondrial Ipochondrial Ipochondrial Ipochondrial Ipochondrial Ipochondrial Ipochondrial Ipochondrial Ipochondrial Ipochondrial Ipochondrial Ipochondrial Ipochondrial Ipochondrial Ipochondrial Ipochondrial Ipochondrial Ipochondrial Ipochondrial Ipochondrial Ipochondrial Ipochondrial Ipochondrial Ipochondrial Ipochondrial Ipochondrial Ipochondrial Ipochondrial Ipochondrial Ipochondrial Ipocha dysfunction
. 30 heart and circulatory system
30 heart and circulatory system
. 31 upper GI
. 32 lower GI
. 33 respiratory system
. 34 urogenital system
. 38 other organ or system
F45.4 Chronic somatoform pain disorder
F45.8 Other somatoform disorders
F45.9 Somatoform disorder, unspecified
F48 Other neurotic disorders
F48.0 Neurasthenia depersonalization
F48.1 .8 Other specific neurotic disorders
F48.9 Neurotic disorder, unspecified
F50-F59 Behavioral syndromes associated with physiological disorders and physical factors
F50 Eating disorders
F50.0 Anorexia nervosa
F50.1 Atypical anorexia nervosa
F50.2 Bulimia nervosa
F50.3 Atypical bulimia nervosa
F50.3 Atypical bulimia nervosa 90.44 Overeating associated with other disorders
F50.5 Vomiting associated with other psychological disorders
F50. 8 Other eating disorders
8 Other eating disorders
F50.9Eating disorder, unspecified
F51 Non-organic sleep disorders
F51.0 Non-organic insomnia
F51.1 Non-organic hypersomnia
F51.2 Non-organic sleep-wake disorder
F51.3 Sleepwalking (somnambulism)
F51.404 Sleep terrors (night terrors)
F51.5 Nightmares
F51.8 Other non-organic sleep disorders
F51.9 Non-organic sleep disorder, unspecified
F52 Sexual dysfunction not due to an organic disorder or disease
F52.0 Lack or loss of sexual desire
F52.1 Sexual aversion and lack of sexual satisfaction
. 10 sexual disgust
. 11 lack of sexual satisfaction
F52.2 Absence of genital response
F52.3 Orgasmic dysfunction
F52.4 Premature ejaculation
F52.5 Nonorganic vaginismus
F52.6 Nonorganic dyspareunia
F52.7 Increased sex drive
F52.9 Unspecified sexual dysfunction not due to an organic disorder or disease
F53 Mental and behavioral disorders associated with the puerperium, not elsewhere classified
F53. 0 Mild mental and behavioral disorders associated with the puerperium, not elsewhere classified
0 Mild mental and behavioral disorders associated with the puerperium, not elsewhere classified
F53.1 Severe mental and behavioral disorders associated with the puerperium, not elsewhere classified
F53.8 Other mental and behavioral disorders associated with the puerperium, not elsewhere classified
F53.9 Postpartum mental disorder, unspecified
F54 Psychological and behavioral factors associated with disorders or diseases classified elsewhere
F55 Abuse of non-addictive substances
F55.0 Antidepressants
F55.1 Laxatives
F55.2 Analgesics
F55.3 Acid reducers
F55.4 Vitamins
F55.5 Steroids or hormones
F55.6 Specific herbs and folk remedies
F55.8 Other non-addictive substances
F55.9 Unspecified
F59 Unspecified behavioral syndromes associated with physiological disorders and physical factors
F60-F69 Adult personality and behavior disorders
F60 Specific personality disorders
F60. 0 Paranoid personality disorder
0 Paranoid personality disorder
F60.1 Schizoid personality disorder
F60.2 Antisocial personality disorder
F60.3 Emotionally unstable personality disorder
. 30 impulsive type
. 31 borderline type
F60.4 Hysterical personality disorder
F60.5 Anancaste (obsessive-compulsive) personality disorder
F60.6 Anxious (avoidant) personality disorder
F60.7 Dependent personality disorder
F60.8 Other specific personality disorders
F60. 9 Personality disorder, unspecified
F61 Mixed and other personality disorders
F61.0 Mixed personality disorders
F61.1 Disturbing personality changes
F62 Chronic personality changes not associated with brain damage or disease
F62.0 Chronic personality changes after a disaster
F62.1 Chronic personality change after mental illness
F62.8 Other chronic personality changes
F62.9 Chronic personality change, unspecified
F63 Disorders of habits and drives
F63.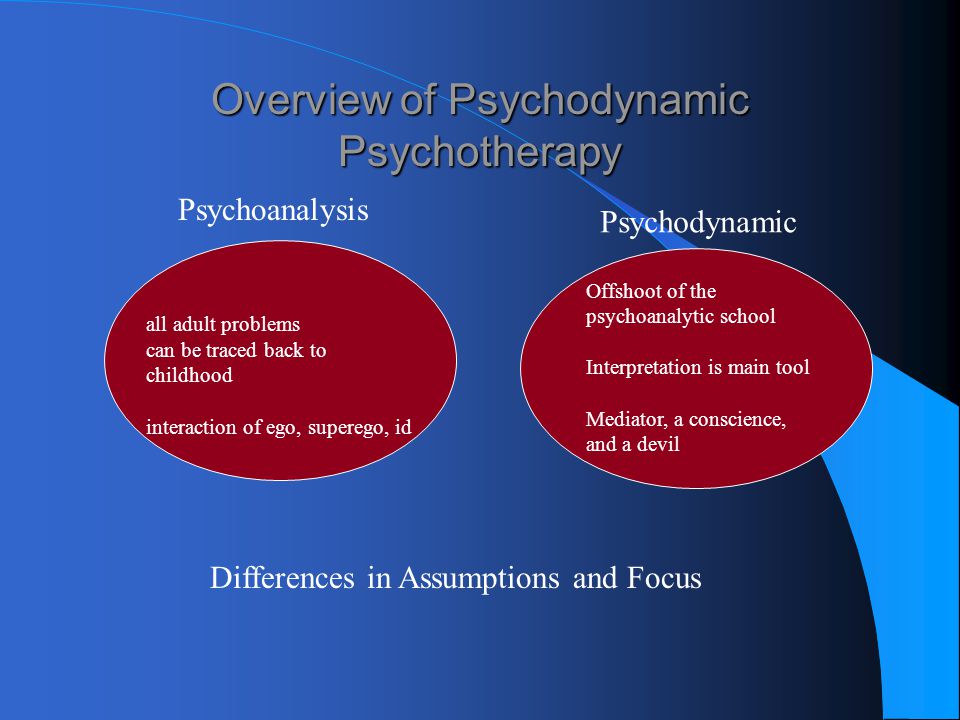 0 Pathological gambling
0 Pathological gambling
F63.1 Pathological arson (pyromania)
F63.2 Pathological theft (kleptomania)
F63.3 Trichotilomania
F63.8 Other disorders of habits and drives 900 F63.9 Habit and drive disorder, unspecified
F64 Gender identity disorder
F64.0 Transsexualism
F64.1 Dual role transvestism
F64.2 Gender identity disorder in children
F64.8 Other disorders of gender identity
F64.9 Gender identity disorder, unspecified
F65 Disorders of sexual preference
F65.0 Fetishism
F65.1 Fetishistic transvestism
F65.2 Exhibitionism F604 Peedism
F65.2
F65.5 Sadomasochism
F65.6 Multiple disorders of sexual preference
F65.8 Other disorders of sexual preference
F65.9 Sexual preference disorder, unspecified
F66 Psychological and behavioral disorders associated with sexual development and orientation
F66.0 Puberty disorder
F66.1 Ego-dystonic sexual orientation
F66. 2 Sexual relationship disorder
2 Sexual relationship disorder
F66.8 Other psychosocial developmental disorders
F66.9 Psychosocial developmental disorder, unspecified
F68 Other disorders of adult personality and behavior
F68.0 Exaggeration of physical symptoms for psychological reasons
F68.1 Intentionally causing or feigning symptoms or disability, physical or psychological (faking disorder)
F68.8 Other specific disorders of adult personality and behavior
F70-F79 Mental retardation
F70 Mild mental retardation
F71 Moderate mental retardation
F72 Severe mental retardation
F73 Profound mental retardation
F78 Other mental retardation
F79 Unspecified mental retardation
A fourth character may be used to specify the degree of behavioral impairment:
F7x.0 minimal or no behavioral impairment
F7x. 1 significant behavioral impairment requiring attention or treatment
1 significant behavioral impairment requiring attention or treatment
F7x.8 other behavioral impairment
F7x .9 behavioral disorders not identified
F80-F89 Disorders of psychological development
F80 Specific developmental disorders of speech
F80.0 Specific speech articulation disorders
F80.1 Expressive speech disorder
F80.2 Receptive speech disorder
F80.3 Acquired aphasia with epilepsy (Landau-Kleffner syndrome)
F80.8 Other developmental speech disorders
F80.9 Disorder Speech development, unspecified
F81 Specific developmental disorders of school skills
F81.0 Specific reading disorder
F81.1 Specific spelling disorder
F81.2 Specific numeracy disorder
F81.3 Mixed disorder of scholastic skills
F81.8 Other disorders of scholastic skills
F81.9 Developmental scholastic disorder, unspecified
F82 Specific developmental disorder of motor functions
F83 Mixed specific disorders
Other disorders of speech development 9000 , unspecified
F84 General developmental disorders
F84. 0 Childhood autism
0 Childhood autism
F84.1 Atypical autism
. 10 Atypical at onset
. 11 Atypicality in symptoms
. 12 Atypical in both age of onset and symptomatology
F84.2 Rett syndrome
F84.3 Other childhood disintegrative disorder
F84.4 Hyperactive disorder associated with mental retardation and stereotyped movements
F84.5 Asperger's syndrome
F84.8 Others general developmental disorders
F84.9 General developmental disorder, unspecified
F88 Other disorders of psychological development
F89 Unspecified developmental disorder
F90-F98 Behavioral and emotional disorders with onset usually in childhood and adolescence
F90 Hyperkinetic disorders
F90.0 Attention disturbance
F90.1 Hyperkinetic conduct disorder
F90.8 Other hyperkinetic disorders
F90.9 Hyperkinetic disorder, unspecified
F91 Conduct disorders
F91. 0 Conduct disorder limited to family
0 Conduct disorder limited to family
F91.1 Unsocialized conduct disorder
F91.2 Socialized conduct disorder
F91.3 Oppositional defiant disorder
F91.8 Other conduct disorders
F91.9 Conduct disorder, unspecified
F
2 Mixed conduct and emotion disorders F92.0 Depressive conduct disorder
F92.8 Other mixed conduct and emotion disorders
F92.9 Mixed conduct and emotion disorder, unspecified
F93 Childhood-specific emotional disorders
F93.0 Childhood separation anxiety disorder
F93.1 Childhood phobic anxiety disorder
F93.2 Childhood social anxiety disorder
F93.3 Sibling rivalry disorder 9004 F93.8 Other emotional disorders of childhood
80 Childhood generalized anxiety disorder
F93.9 Childhood emotional disorder, unspecified
F94 Disorders of social functioning with onset specific to childhood
F94.0 Selective mutism
F94.1 Reactive attachment disorder of childhood
F94. 2 Disinhibited attachment disorder of childhood
2 Disinhibited attachment disorder of childhood
F94.8 Other childhood social functioning disorders
F94. 9 Childhood social functioning disorder, unspecified
F95 Tic disorders
F95.0 Transient tic disorder
F95.1 Chronic motor or vocal tic disorder
F95.2 Combined vocal and multiple motor tic disorder (de la Tourette syndrome)
F95.8 Other tic disorders
F95.9 Tic disorder, unspecified
F98 Other behavioral and emotional disorders , usually onset in childhood and adolescence
F98.0 Non-organic enuresis
. 00 Nocturnal enuresis only
. 01 Only diurnal enuresis
. 02 Nocturnal and diurnal enuresis
F98.1 Non-organic encopresis
. 10 Failure to acquire physiological bowel control
. 11 Adequate bowel control and defecation at inappropriate sites with normal stool consistency
. 12 Contamination due to liquid stool
F98.2 Eating disorders in infancy
F98.3 Inedible eating (peak) in infancy and childhood
F98. 4 Stereotyped movement disorders
4 Stereotyped movement disorders
. 40 No self harm
. 41 Self-damaging
. 42 Mixed
F98.5 Stuttering
F98.6 Fluid speech
F98.8 Other specific behavioral and emotional disorders with onset usually in childhood and adolescence
F98.9 Unspecified behavioral and emotional disorders with onset usually in childhood and adolescence
Code of Ethics - Existential Therapy
Code of Ethics
Download code of ethics
I Definitions
1.1. In the content of the Code, the following concepts and abbreviations should be understood in the following manner:
1.1.1. The Code is the code of professional ethics of the Eastern European Association for Existential Therapy, which also regulates the professional behavior of students, teachers, supervisors and therapists of educational institutions for the training of psychotherapists;
1.1.2. VEAET or the Association is the Eastern European Association for Existential Therapy;
1. 1.3. The definitions apply equally to both the female and male genders;
1.3. The definitions apply equally to both the female and male genders;
1.1.4. The Ethics Committee or EC is the ethics committee of the Eastern European Association for Existential Therapy;
1.1.5. A psychotherapist or therapist is a person who practices psychotherapy/psychological counseling;
1.1.6. A client is a person or a group of persons who, within the framework of a professional relationship, receives psychotherapeutic assistance from a psychotherapist;
1.1.7. Psychotherapy is the professional assistance of a psychotherapist to a client in order to improve the client's quality of life;
1.1.8. Student - a person who is studying at an educational institution for the training of psychotherapists.
II General principles
2.1. The principles of professional ethics set forth in the Code are in line with the general principles of the "European Convention on Human Rights" and define what constitutes ethical behavior for a psychotherapist.
2.2. In professional activities, the psychotherapist strives for the highest standards of his profession, responsibly assessing his capabilities and limitations in the provision of professional services.
2.3. The psychotherapist in the practice of psychotherapy embodies respect for the personality of clients and colleagues.
III Liability
3.1. All members of the EEAET are subject to the requirements of this Code from the day they join the Association. They define both the relationship of psychotherapists with clients and the relationship of teachers/supervisors/therapists and students in the psychotherapy/counseling training process.
3.2. The psychotherapist must be clearly aware of his responsibility for professional actions, statements and recommendations arising from his professional role. Any decision of the psychotherapist in relation to the client must correspond to his professional competence, as well as take into account the scientific and methodological state of psychotherapy.
3.3. The psychotherapist, when making decisions, takes into account the personal, social and organizational context of his work. The therapist must be able to assess how these contexts may affect the quality of his work, including the client's use of the information provided by the therapist and the use of the therapist's professional influence (authority).
3.4. The psychotherapist must respond in time to obstacles of any kind that may interfere with joint work with the client. The therapist avoids relationships that may create conflicts of interest or distort the therapeutic process.
3.5. In all decisions in relation to the client, the psychotherapist must take into account his personal limitations (including emotional limitations, ethical ideas). If necessary, the psychotherapist should consult with other specialists or refer the client to them.
3.6. The therapist must be able to explain his decisions and actions in a way that the client can understand.
3.7. The psychotherapist must refrain from abusing his authority based on professional role and competence, and use it solely at the request and desire of the client with mutual consent.
3.8. The psychotherapist who is engaged in research work is responsible for the methodology chosen by him and the reliability of the results obtained. It is unacceptable to distort or one-sidedly present data obtained in scientific or research work in any way (except for the purpose of maintaining confidentiality).
3.9. The psychotherapist takes care that his actions, statements or interpretation of data do not degrade the dignity of age, ethnic, economic, social, gender and any other groups of the population.
IV Competence
4.1. Maintaining high standards of competence and responsibility by psychotherapists is the common goal of the EEAET for the benefit of society and psychotherapy in general.
4.2. The psychotherapist is obliged to constantly maintain and develop his professional competence, getting acquainted with the latest achievements in the theory and practice of psychotherapy, as well as in other areas of science related to psychotherapy. He must take care of the constant improvement of his professional and personal qualities. The psychotherapist must constantly supervise his work with colleagues.
He must take care of the constant improvement of his professional and personal qualities. The psychotherapist must constantly supervise his work with colleagues.
4.3. The psychotherapist, presenting himself in any context, accurately and truthfully reflects his education, professional training, limits of competence and experience. Confirmation of professional competence are diplomas and certificates of educational institutions offering professional psychotherapeutic education. As an additional training of a psychotherapist, education is indicated that allows the use of certain methods or techniques of psychotherapeutic work. It is unacceptable to mislead about the professional competence of current or potential clients, as well as colleagues.
4.4. The psychotherapist is aware of the impact of his personal problems and conflicts on the quality of his professional activity and refrains from entering into professional relationships in which the therapist's personal limitations may lead to inappropriate reactions, actions and decisions, and thus harm the client, student, colleague or research participant . If the therapist discovers the difficulties described above after entering into a professional relationship, he or she seeks professional help to determine the next steps. The psychotherapist must be prepared for the fact that in some cases it may be necessary to limit or stop professional activities.
If the therapist discovers the difficulties described above after entering into a professional relationship, he or she seeks professional help to determine the next steps. The psychotherapist must be prepared for the fact that in some cases it may be necessary to limit or stop professional activities.
4.5. Entering a new field of psychotherapeutic work (for example, supervision), the psychotherapist must have completed all the necessary professional training and meet the requirements of this field of activity. It is also important to make sure that there are no contradictions between different areas of his professional activity.
V Legal standards
5.1. If in the practice of a psychotherapist there are conflicts between the laws of the country in which he works, which define specific requirements for the professional behavior of psychotherapists (for example, the obligation to inform a client or a third party about a threat, access to the psychotherapist's records), and the EEAET code of ethics, the psychotherapist should adhere to the laws of their country. At the same time, it is necessary to strive for the possible reduction of these contradictions.
At the same time, it is necessary to strive for the possible reduction of these contradictions.
5.2. The psychotherapist avoids committing illegal actions, and also does not support the actions of third parties and institutions that lead to the violation of human rights.
5.3. If an investigation is initiated against a psychotherapist in connection with his professional activities, he informs the EEAET Ethics Committee in writing about this within two weeks.
VI Confidentiality
6.1. Maintaining the confidentiality of information obtained during psychotherapeutic work is the primary responsibility of the psychotherapist. This requirement remains valid even after the end or end of the therapeutic relationship. It is possible to transfer information about the client to third parties only with the permission of the client (or his legal representative), except for the following special cases. A psychotherapist may consider himself not bound by confidentiality obligations only if at least one of the following three conditions is met:
- there is no other way to help the client than in violation of the principle of confidentiality;
- it is obvious that if the psychotherapist observes the principle of confidentiality, there will be a danger to the health or life of the client, therapist and / or third parties;
- the psychotherapist must be sure that in case of violation of the principle of confidentiality, the danger to the client, therapist and / or third parties will be limited or completely removed.

The principle of confidentiality also applies to information about colleagues' clients.
6.2. The therapist informs the client about the boundaries of confidentiality. He must obtain the written permission of the client to provide (in writing or verbally) information about him to third parties and / or carefully change all identifying data. The only exceptions are cases where the psychotherapist is required to provide information in the manner prescribed by law. The client has the right to revoke his authorization at any time.
6.3. Information and data obtained in the course of psychotherapy, clinical interviews, testing, assessment and diagnosis of clients, students, employees, etc., can be discussed with colleagues without the written permission of the client only for professional purposes, when the provision of information is part of the training and assessment of professional qualifications psychotherapist or as part of supervision.
6.4. The psychotherapist takes steps to ensure confidentiality in the storage and use of his records.
6.5. The psychotherapist working with clients who are unable to take care of themselves is especially conscious of the interests of these clients and, if necessary, advises interested parties on this matter.
VII Principles of the psychotherapeutic process
7.1. The psychotherapist must be aware of his possible influence on clients, students and other persons who, to a certain extent, depend on his professional activity. He refrains from abusing his authority, based on his professional role and competence, by promoting dependence on the client or engaging in emotional, material or other kind of exploitation. The therapist must act responsibly, understanding the special nature of the psychotherapeutic relationship based on trust and partial dependence. The use and abuse of trust for the purpose of pursuing one's personal interests - emotional, sexual, social or material - is a gross violation of professionalism.
7.2. The psychotherapist refrains from dual relationships with the client (psychotherapy with employees, students, close friends or relatives, etc. ), which may influence the professional judgments and actions of the psychotherapist. Sexual intimacy with persons with whom the psychotherapist has professional relationships (therapy, research, training, supervision) is a gross violation of professional ethics.
), which may influence the professional judgments and actions of the psychotherapist. Sexual intimacy with persons with whom the psychotherapist has professional relationships (therapy, research, training, supervision) is a gross violation of professional ethics.
7.3. Two years after the termination of the professional relationship, the psychotherapist may not enter into another relationship with the client from which the therapist receives material or other benefits.
7.4. It is unacceptable to force someone to participate in psychotherapy or research without their voluntary consent.
7.5. The psychotherapist must explain to the client the principles, conditions and methods of the forthcoming psychotherapeutic work, and also, if necessary, return to the discussion of these principles while working with the client. These explanations should cover all aspects of psychotherapy that may affect the client's consent to participate in psychotherapy.
7.6. The psychotherapist, agreeing to work with a client at the request of a third party, clearly explains to each of the parties involved the specifics of the therapeutic relationship and the division of responsibility.
7.7. If any organization requires from the psychotherapist actions that violate ethical principles, the psychotherapist informs its representatives about the emerging ethical conflict and about the responsibility of each of the parties. If necessary, the psychotherapist applies (in writing) for help to the EEAET Ethics Committee.
7.8. The psychotherapist promptly, clearly and understandably for the client agrees with him on payment for his services. It is considered contrary to ethical principles to reward a client in any form for good reviews of the work of a psychotherapist. The psychotherapist finds an opportunity to spend part of his time working with clients who are unable to pay the usual fee or cannot pay at all for the services of a psychotherapist.
7.9. The therapist ends the therapeutic relationship if the client wants it to or if it is ineffective for the client. If necessary, the therapist offers the client alternative ways of getting help.
7. 10. The therapist refrains from making unrealistic promises to clients, that is, he does not promise results that are not guaranteed to be achieved in psychotherapy.
10. The therapist refrains from making unrealistic promises to clients, that is, he does not promise results that are not guaranteed to be achieved in psychotherapy.
7.11. At the beginning of psychotherapy, the psychotherapeutic contract concluded with the client should define the boundaries of psychotherapy, the client's goals in psychotherapy, the frequency and duration of meetings, the approximate total duration of psychotherapy, the degree of responsibility of the psychotherapist and the client in joint work, the procedure for completing psychotherapy, the form and amount of remuneration of the psychotherapist, the possibility of obtaining advice from other professionals.
7.12. The psychotherapist does not have the right to stop psychotherapy if there are no reasons beyond his control. If, nevertheless, psychotherapy has to be stopped at the initiative of the psychotherapist, he must explain his decision to the client in a form that is accessible to him, advise him on what can best be done under the circumstances and / or refer the client to another specialist.
7.13. The financial conditions of the psychotherapist's work - personal or institutional (insurance) payment for work, payment for missed and additional meetings, etc. - should be discussed with the client before starting psychotherapy. If psychotherapy is paid for by an institution, it is unacceptable to charge additional fees to clients.
7.14. In the process of psychotherapy, the psychotherapist should not allow the participation of other persons, unless the client agrees that part or all of his psychotherapy be under the supervision of other persons. “Others” does not include persons whose cooperation is necessary for psychotherapy.
7.15. The psychotherapist informs the client about the Code of Professional Ethics, the requirements of which the psychotherapist adheres to, and about the client's ability to appeal the psychotherapist's actions to the EEAET Ethics Committee.
VIII Professional relations
8.1. The psychotherapist respects the traditions, principles and practices of related professions, as well as other areas of psychotherapy, and cooperates with other specialists if necessary.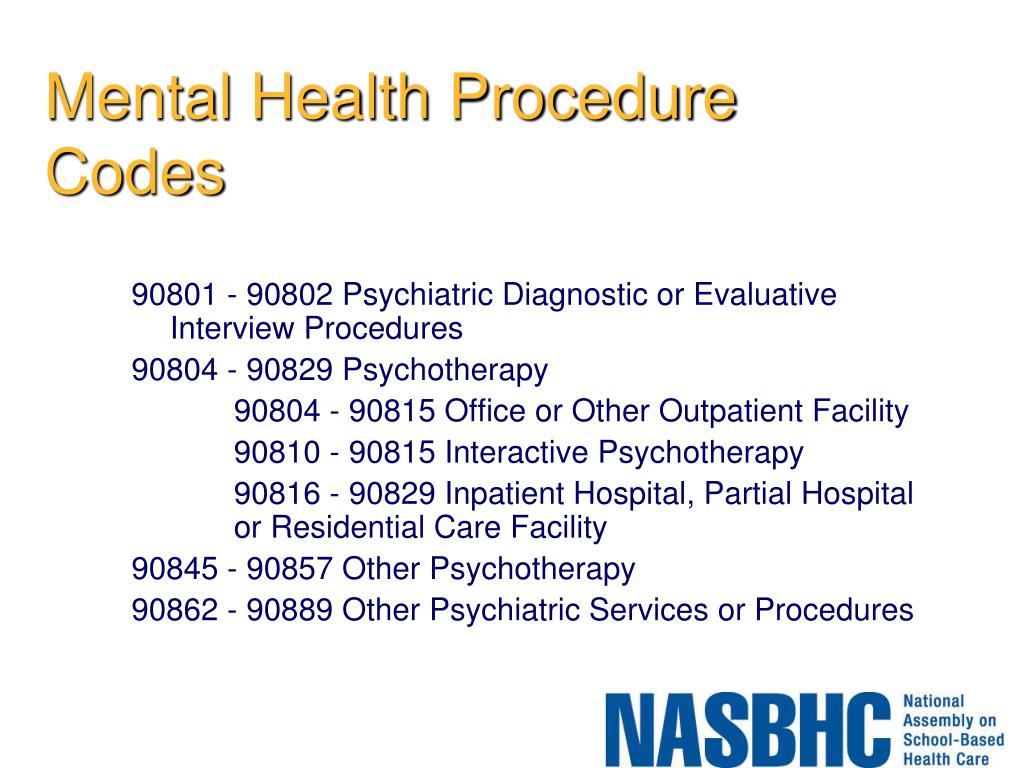
8.2. The psychotherapist is attentive to cases when the client simultaneously receives help from other specialists, and tries, together with the client, to minimize possible contradictions due to which the client's interests may suffer. When possible and with the consent of the client, the psychotherapist cooperates with other specialists.
8.3. The therapist does not use professional relationships with supervisees, students, staff, or research participants for personal gain.
8.4. If the psychotherapist notices the unethical actions of another psychotherapist, he tries, if possible, to inform the colleague about his vision of the act. If the act is associated with insufficient sensitivity, lack of experience or knowledge, such an informal attitude to the situation is appropriate; it is important to maintain confidentiality. If a colleague's unethical act is too serious to resolve the situation informally, a psychotherapist who knows about the unethical behavior of a colleague is obliged to notify the EEAET Ethics Committee or the professional organization of his country about this in writing.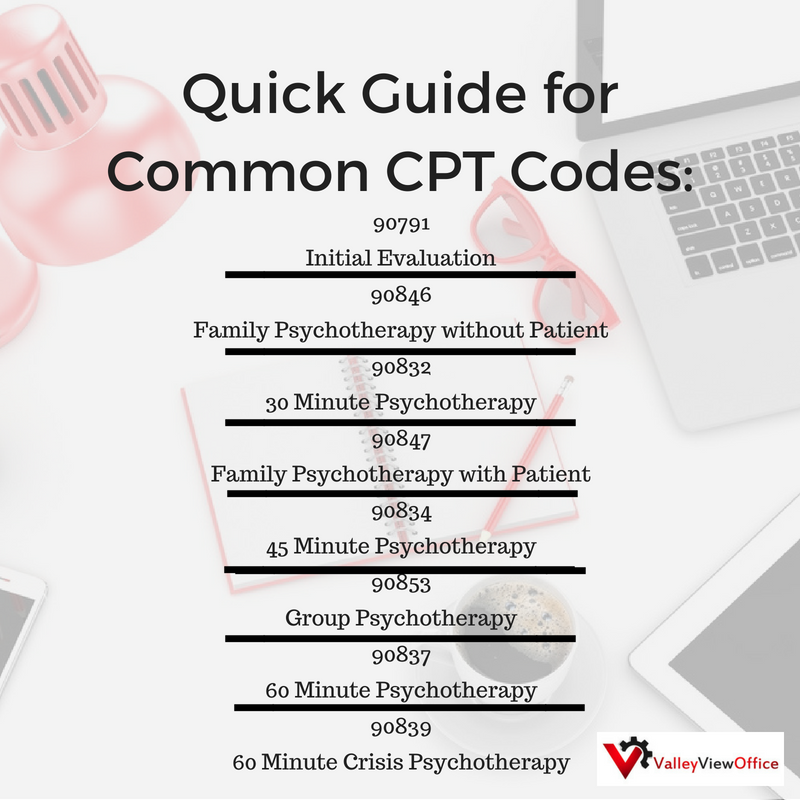
IX Publicity
9.1. In public information about their services, the psychotherapist is limited to the following information: name, surname, currently the highest degree of academic education, certificate of professional psychotherapeutic training, psychotherapist certificate and its validity, membership in professional organizations, address, telephone, a summary of the psychotherapeutic services offered , payment, working languages, contracts with insurance companies, as well as other relevant information that does not contradict the EEAET Code of Professional Ethics.
9.2. The psychotherapist, when publicly informing about his professional services, does not use information that may create a false impression about his education, qualifications and methods of work. Information of this kind should not give potential clients grounds for unrealistic expectations about the results of psychotherapy, and should not appeal to the fears, anxieties or other strong feelings of potential clients.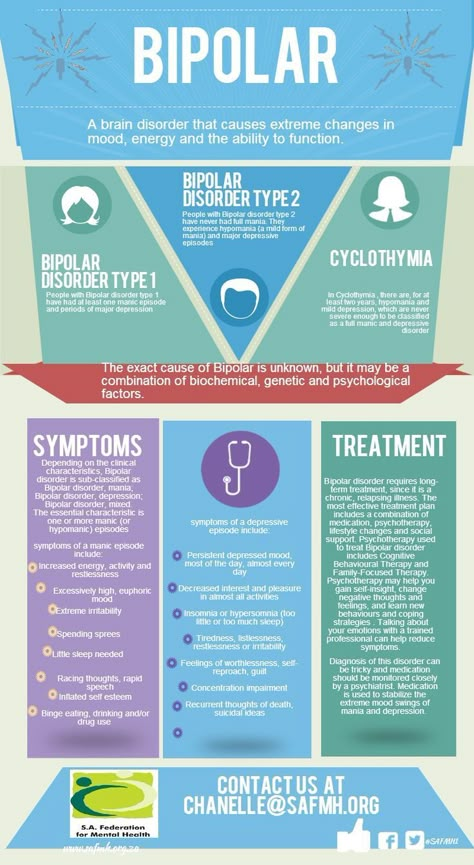 The therapist should also not emphasize the uniqueness of his abilities or methods of work.
The therapist should also not emphasize the uniqueness of his abilities or methods of work.
9.3. It is unacceptable for a psychotherapist to reward, including with his professional services, representatives of the press, radio, television and other media for advertising or other public information about his services. Paid advertising should be clearly understood as such.
9.4. Any public information, including advertising, about seminars, psychotherapy groups or training programs must contain clear information about their goals, qualifications of the facilitators, conditions and methods for conducting them, time frames and payment terms.
9.5. Psychotherapists who advertise or otherwise publicize psychotherapeutic techniques, books, or other information products must ensure that information about them is professional and ethical, without sensationalism or exaggeration.
9.6. A psychotherapist should not participate in advertising of non-psychological (non-psychotherapeutic) products, presenting himself in advertising as a psychotherapist.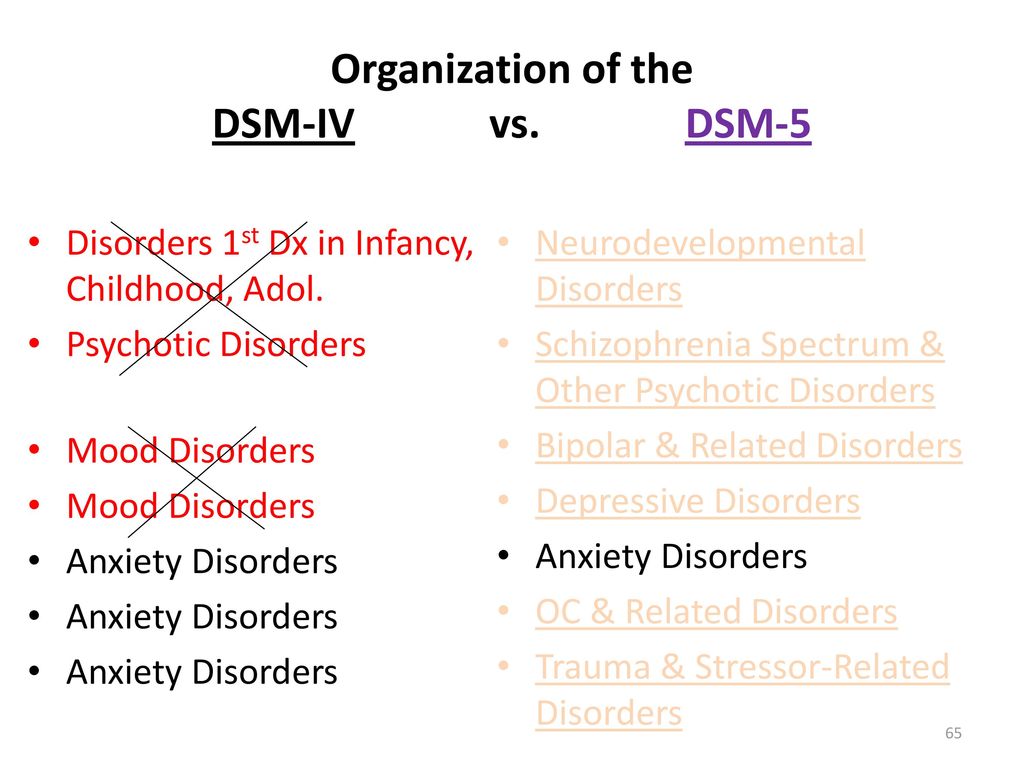
9.7. Psychotherapists as teachers or educators are responsible for the accuracy and ethics of the material offered, as well as for its relevance to the audience for which it is presented. This also applies to programs, catalogs and advertisements for psychotherapist talks.
9.8. The psychotherapist is obliged to respond to cases when colleagues disseminate information that is inconsistent with ethical principles about psychotherapists or psychotherapy.
9.9. Psychological diagnostics and other psychotherapeutic services are only relevant within a professional relationship. At lectures, demonstrations, and appearances in the media, the psychotherapist offers professional advice or assessment only if he is confident in the professionalism of his judgments.
X Psychological assessment, testing and research work
10.1. The psychotherapist, in working with a client or research participant, uses only those diagnostic techniques and research methods that serve the well-being and interests of the client. The psychotherapist respects the client's right to know and understand all the results of diagnostics, evaluation and research. If the psychotherapist works with persons who are unable to understand the essence of the work performed, the psychotherapist pays special attention to serving the interests of the client, and also gives the necessary recommendations to responsible persons involved in the care of the client.
The psychotherapist respects the client's right to know and understand all the results of diagnostics, evaluation and research. If the psychotherapist works with persons who are unable to understand the essence of the work performed, the psychotherapist pays special attention to serving the interests of the client, and also gives the necessary recommendations to responsible persons involved in the care of the client.
10.2. The psychotherapist is attentive to the confidentiality of data at any stage of their processing; he cares about the understanding of ethical principles by his employees.
10.3. The psychotherapist is convinced of the adequacy of the understanding and use of the results of assessment and research by others.
XI Ethical principles in the process of teaching psychotherapy
11.1. The ethical principles defined in this Code also govern professional relationships in the process of teaching psychotherapy within educational institutions. Teachers, supervisors, psychotherapists and students should cooperate with each other in accordance with the rules of professional ethical conduct.
11.2. The management of educational institutions is responsible for timely familiarization of all persons mentioned in clause 11.1 about the Code of Professional Ethics and the need to comply with its principles throughout the entire learning process. They are also informed about the possibility of appealing unethical acts.
11.3. Training in psychotherapy is incompatible with any kind of exploitation. The highest values in the process of teaching psychotherapy are freedom, responsibility, truthfulness, honesty and mutual respect for the participants in the educational process.
11.4. Teachers, supervisors and therapists at the beginning of their work as part of the learning process clearly explain to students the boundaries of confidentiality and return to this issue as necessary.
11.5. Teachers, supervisors, and therapists are responsible for setting boundaries with students that are consistent with the theoretical and practical guidelines of the existential paradigm.
11.6. The terms and conditions of training, supervision and therapy are negotiated with students before the start of training/supervision/therapy.
11.7. Teachers, supervisors and therapists should make sure in a timely manner that professional, personal, work or other relationships with students not related to the learning process will not harm the quality and effectiveness of teaching/supervision/personal therapy. If necessary, the teacher/supervisor/therapist should seek professional help to get out of this difficult situation.
11.8. Teachers/supervisors/therapists are responsible for discussing thoroughly with students the possible consequences of entering into a dual professional relationship when the roles of administrator, teacher, supervisor, and therapist intersect in the learning process.
11.9. The management of the educational institution, based on the recommendations of teachers, supervisors and therapists, has the right to decide whether (with an indication of the conditions) or prohibiting a student from practicing as a psychotherapist for some time. The student is responsible for its observance and following the received recommendations in relation to their work.
The student is responsible for its observance and following the received recommendations in relation to their work.
11.10. Teachers, supervisors, therapists and students are required to maintain the confidentiality principle in relation to all personal information obtained during training - in groups, in supervised consultations, in group supervisions and in any other classes. This also applies to information about the work of colleagues and students and information about clients whose work was discussed during supervision.
11.11. Information about clients at lectures and supervisions (in written or oral form) is provided only after it has been processed in such a way that the client cannot be identified. If such processing of information is not possible, a non-public presentation method should be chosen for this case.
11.12. Confidentiality may be violated during the evaluation of student work, but only if this is clearly stated before starting this process.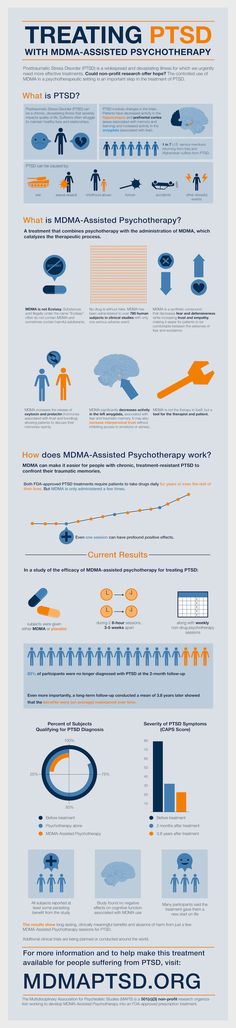 In these cases, teachers/supervisors can purposefully share the information they have received, which is necessary for assessing students.
In these cases, teachers/supervisors can purposefully share the information they have received, which is necessary for assessing students.
XII Complaints and their consideration
12.1. Clients and their authorized persons, students can appeal against any actions of psychotherapists - members of the EEAET (students - actions of teachers / supervisors / psychotherapists involved in the learning process), except for complaints about harm to health, which are considered in accordance with the laws of the countries in which the complaining persons live and the persons against whom the complaint is directed. Members of the Association may also appeal against the actions of fellow members of the Association if they believe that the actions of a colleague have harmed the results of their work or professional reputation.
12.2. Complaints are considered by the Complaint Review Commission (GRC), established by the Ethics Committee (EC) of the Association. The GRC is created to consider each specific complaint.
12.3. The EEAET EC considers only those complaints received in written (including electronic) form. The complaint shall indicate the name, surname of the complainant (plaintiff), the person against whom the complaint is directed, a short description of the complaint.
12.4. Only complaints related to cases of unethical behavior no more than three years old are considered.
12.5. After receiving a complaint, the EC creates a GRC from 3 EC members within 2 weeks. One of them is appointed chairman of the commission. Members of the GRC should not be associated with the plaintiff, the person against whom the complaint is directed, and among themselves by family, service, professional ties and material interests. If there are not enough such people in the Ethics Committee, the GRC can be supplemented by other members of the Association.
12.6. The EC informs the complainant in writing about the receipt of the complaint within a month, reports on the decision to accept or not to accept the complaint for consideration. The decision on accepting or not accepting the complaint for consideration is made by the EC by a majority of votes. If accepted, the complainant should also receive information about the procedure for considering a complaint and the composition of the established GRC. In addition, all specified information is sent to the person against whom the complaint is directed. If the complaint is not accepted, the complainant is informed in writing about this with the rationale for the decision.
The decision on accepting or not accepting the complaint for consideration is made by the EC by a majority of votes. If accepted, the complainant should also receive information about the procedure for considering a complaint and the composition of the established GRC. In addition, all specified information is sent to the person against whom the complaint is directed. If the complaint is not accepted, the complainant is informed in writing about this with the rationale for the decision.
12.7. If the complaint is accepted, the chairman of the GRC, having met with both parties and after listening to them, first of all, tries to reconcile them. If the complainant does not agree to take the complaint back, it is further considered in the GRC.
12.8. The complaint to the GRC must be considered within three months after the decision to start the review procedure. In the process of considering the complaint, both the plaintiff and the defendant should have the opportunity to explain or comment on the complaint in more detail in person or in writing.