Birth control help with anxiety
What You Need To Know
Content
- Overview
- How hormonal birth control works
- Why can stopping hormonal contraceptives cause anxiety?
- How long does it take for anxiety to go away after stopping birth control?
- How to manage anxiety after stopping hormonal contraceptives
- When to see a doctor about anxiety after stopping hormonal birth control
- The lowdown
Anxiety is a mood disorder with physical and psychological effects. It impacts everyone differently but is usually characterized by intense feelings of worry and concern. Anxiety symptoms are wide-ranging and include “butterflies” in the stomach, difficulty concentrating, nausea, rapid heartbeat, shortness of breath, and light-headedness.
Evidence¹ shows that anxiety in women tends to fluctuate according to hormonal changes. Significant hormonal changes typically occur during puberty, the time period after giving birth, and during menopause. It is also very common for anxiety to increase before menstruation —as many as 5–8%¹ of women experience premenstrual dysphoric disorder (PMDD), a mood disorder that causes severe anxiety.
There is a strong link¹ between hormonal fluctuation and anxiety. Since hormonal contraceptives like the birth control pill, intrauterine device (IUD), injection, and implant work by changing your hormone levels, withdrawing them can trigger or worsen anxiety.
It can be worrying if you have anxiety symptoms after stopping hormonal birth control, but this is quite normal. Although anxiety is temporary for many women, it is helpful to know how long it might last and when to see a doctor
Have you considered clinical trials for Anxiety?
We make it easy for you to participate in a clinical trial for Anxiety, and get access to the latest treatments not yet widely available - and be a part of finding a cure.
Check your eligibility
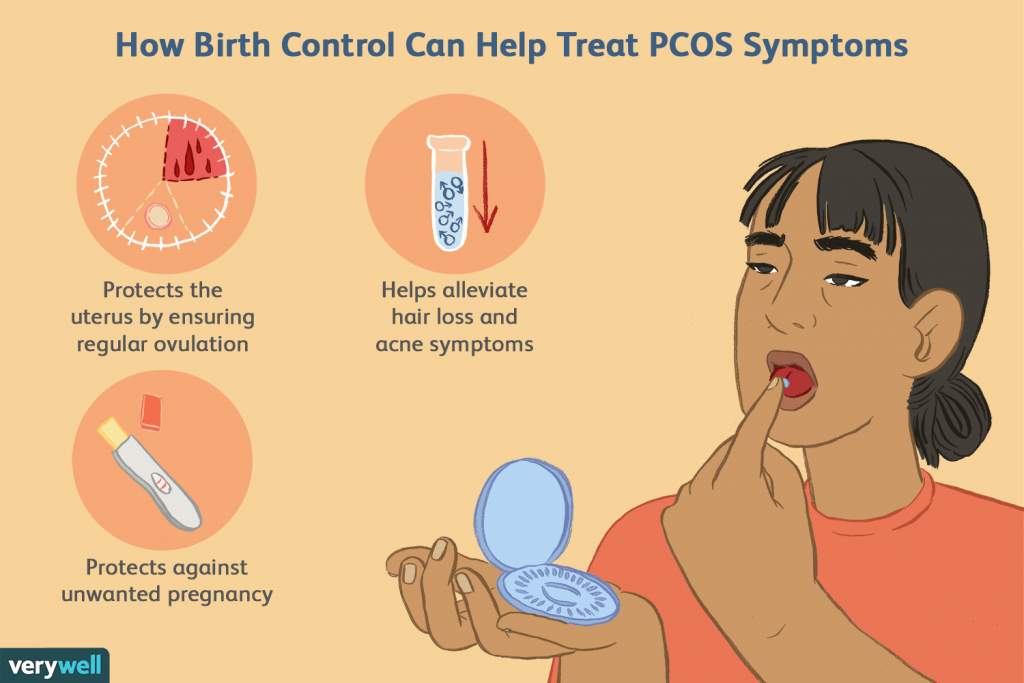
Hormonal contraceptives act on your hormones to prevent pregnancy. They contain synthetic versions of the sex hormones estrogen and progesterone and suppress the hormones your body produces naturally. These synthetic hormones work by tricking your body into thinking that you’re pregnant which stops ovulation. You can’t become pregnant without ovulating.
You can’t become pregnant without ovulating.
Depending on the method you use, contraceptives can contain just progestin (the synthetic version of progesterone) or a combination of progestin and estrogen. The most common hormonal birth control method² in the US is the combined oral contraceptive pill (COC) which contains both estrogen and progestin.
When you stop taking hormonal contraceptives, your hormone levels change. This happens within days of stopping the birth control pill or removing the implant, but it may take a few months if you stop having contraceptive injections.
You might develop anxiety after stopping hormonal birth control for the following two reasons:
1. Hormonal fluctuations
Rising or falling hormone levels can trigger or worsen anxiety, which is why many women experience anxiety during puberty, before menstruation, after having a baby, and during menopause.
Stopping hormonal contraceptives affects your hormone levels as you are withdrawing synthetic hormones and allowing your natural hormones to rise.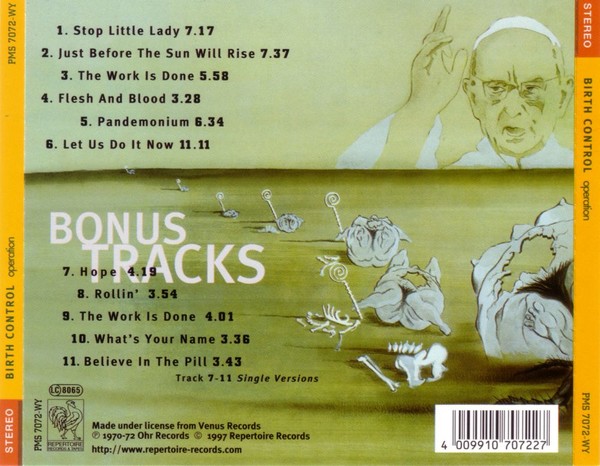 It can take up to six months for your hormone levels to settle down again.
It can take up to six months for your hormone levels to settle down again.
2. Existing anxiety
Studies have shown that oral contraceptives may alleviate some symptoms of anxiety,³ so taking them for an extended period might suppress your symptoms if you had anxiety before. If this is the case, your anxiety symptoms may be uncovered and become noticeable when you stop taking the birth control pill.
If your anxiety continues for longer than a few months, this is a sign that you may have had anxiety before taking oral contraceptives. In this case, you should speak to a doctor or mental health professional about treatment. If your anxiety was temporary and caused by fluctuating hormones, it would probably have subsided sooner.
More research is needed about the link between hormonal contraception and anxiety. While some women find their existing anxiety improves on hormonal contraception, many others find it gets worse. Without more research, it’s difficult to know who will be at risk of worsened anxiety when taking hormonal contraceptives.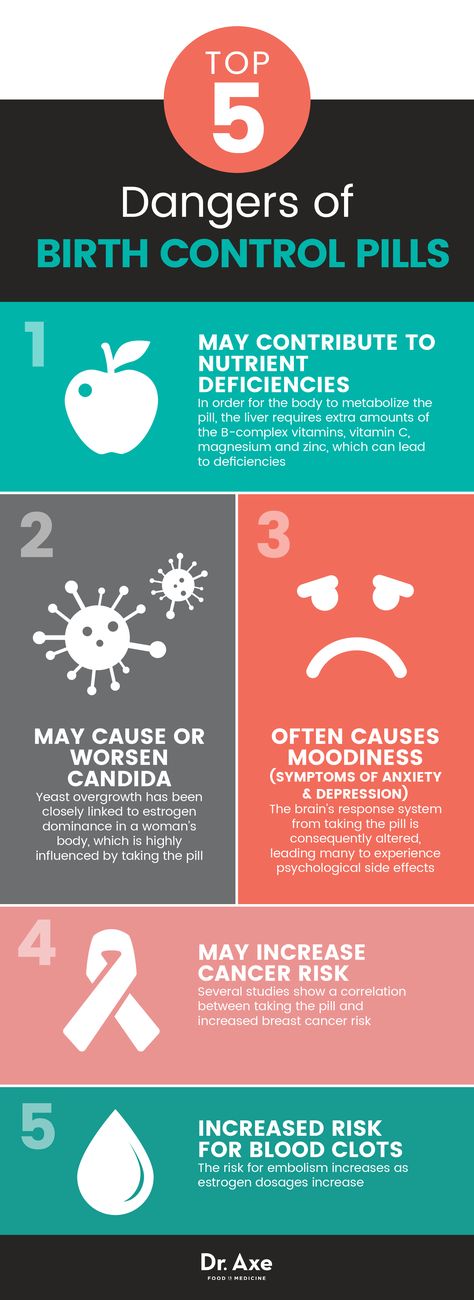
How long your anxiety lasts after stopping hormonal birth control depends on the cause.
If your anxiety was triggered by fluctuating hormones when you stopped birth control, your symptoms should ease as your hormones stabilize. This can take anywhere from four to six months, and longer if you were using long-lasting birth control, such as the injection.
If hormonal contraceptives were masking an existing anxiety disorder, your symptoms may persist even after your hormones have returned to normal levels.
If your anxiety is temporary and caused by fluctuating hormones, you might find the following methods help ease your symptoms while your hormones settle down. Keep in mind that these methods may not be as effective if you had pre-existing anxiety.
Take a vitamin B and folic acid supplement
Some evidence⁴ suggests that long-term use of oral contraceptives can lead to folate and vitamin B deficiencies which can worsen anxiety. Taking vitamin B and folic acid supplements for a few months after stopping your oral contraceptive might be helpful, as is a healthy and balanced diet.
Get moving
Keeping active has been shown⁵ to effectively alleviate anxiety symptoms, so try to exercise for the recommended 150 minutes each week.⁶ High-intensity exercise is proven to have the greatest effect on anxiety, so try to incorporate cardio exercises like running or high-intensity interval training into your routine.
Try mindfulness exercises
A 2013 trial⁷ found that meditating or following a mindfulness program can help reduce anxiety symptoms.
A Guide To Meditating For Anxiety
You should see a doctor if your anxiety lasts for longer than a few months after stopping hormonal contraceptives, if lifestyle measures do not ease your symptoms, or if your anxiety is severe enough to interfere with normal daily activities.
Your doctor will assess your health and symptoms and suggest treatment options like self-help strategies, medication, or talking therapies like cognitive behavioral therapy (CBT). They might also refer you to a psychiatrist.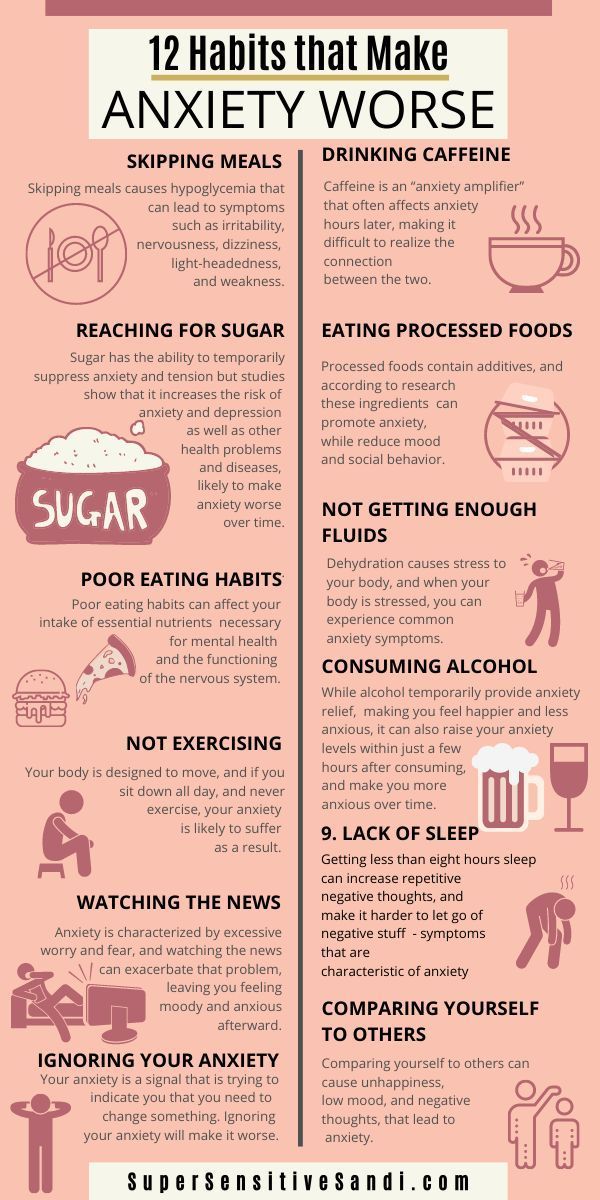
When hormonal contraceptives are removed from your body (for example, when you stop taking the pill or your implant is removed), your hormone levels will fluctuate and take time to settle down. These hormonal fluctuations can trigger or worsen anxiety.
You might experience anxiety symptoms after stopping hormonal contraception because the medication was suppressing pre-existing anxiety. In this case, your symptoms might continue even after your hormone levels have settled and you will need to speak to your doctor or a psychiatrist.
Lifestyle strategies like exercising, eating a balanced diet, taking vitamin B and folic acid supplements, and practicing mindfulness can alleviate your symptoms while your hormones stabilize.
What Happens, What to Do
Hormonal birth control involves everything from the pill and patch to the implant, IUD, and shot.
There are two main types: One contains a type of synthetic progesterone called progestin, and the other is a combined form that includes both progestin and estrogen.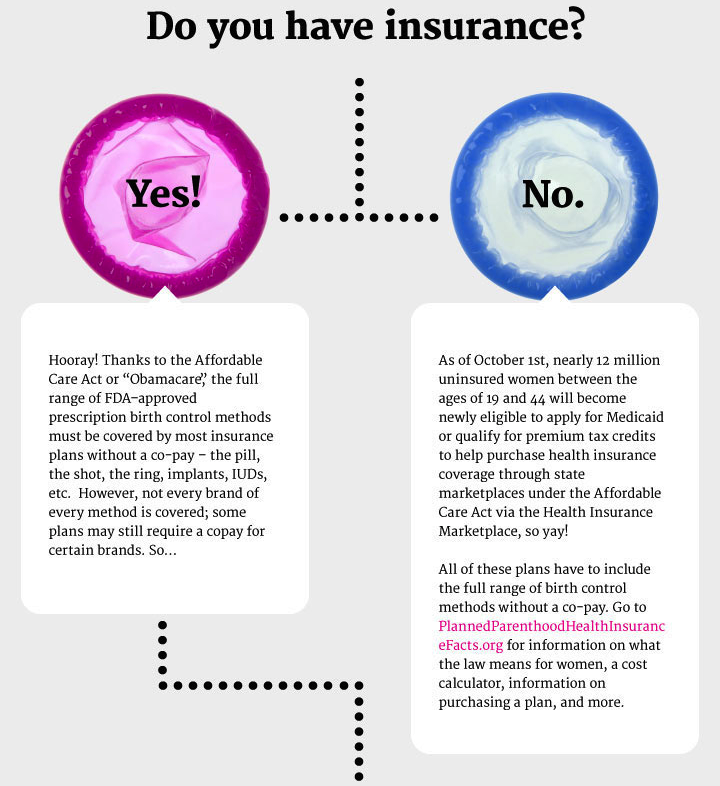
“These two hormones naturally flood the body during ovulation and create a lot of PMS symptoms,” explains Dr. Shirin Lakhani, an intimate health specialist and cosmetic doctor at Elite Aesthetics.
The synthetic hormones in birth control have also been linked to a range of side effects. If you’re wondering whether anxiety is one of them, read on.
Hormonal contraception can cause feelings of anxiety in some people. But other users may find their birth control relieves anxiety symptoms.
It all depends on the individual person.
When it comes to adverse effects, the pill is often the first contraceptive method that springs to mind.
But there’s a link between anxiety and all forms of hormonal contraception, says Dr. Enam Abood from London’s Harley Street Health Centre.
A 2004 review found hormonal contraceptive users had higher rates of anxiety than nonusers.
And a 2018 study noted that users of IUDs containing the hormone levonorgestrel also had higher anxiety rates.
But the pill seems to have been the focus of more research than other methods.
“Combination oral contraceptives and progesterone-only minipills are usually associated with depression and anxiety more than other options of birth control,” Lakhani says.
Between 4 and 10 percent of users report mood problems while on the combined pill. Most people, however, say they’re satisfied with it.
In fact, a review of studies published in the past 30 years found most combined hormonal contraceptive users — those using the combined pill, hormonal patch, or combined vaginal ring — had either no effect or a positive effect on their mood.
However, the review did conclude that non-oral combined hormonal contraceptive methods may result in fewer mood changes.
There are a few simple reasons.
First, there isn’t enough research into the mental and emotional effects of hormonal birth control.
Second, the research that does exist has produced conflicting results. (Again, this is likely because hormonal contraception’s effects differ from person to person.)
(Again, this is likely because hormonal contraception’s effects differ from person to person.)
And third: All of the above, plus varying research methods, has meant it’s impossible to prove cause and effect.
In other words, researchers are currently uncertain. It’s likely to remain that way until more studies are carried out.
If you have a personal history of anxiety or mood disorders, you may be more prone to the emotional effects of birth control.
This hasn’t been fully proven, but it is a theory put forward in several studies.
Unfortunately, it’s pretty difficult to determine what effect your contraceptive will have.
If your anxiety is related to the physical taking of a pill, for example, it’s safe to say an oral contraceptive is likely to worsen those feelings.
If you have a history of anxiety, hormonal birth control may mean you’re more likely to experience anxiety. Preexisting feelings may also intensify.
But if your anxiety is a result of PMS, some combined hormonal contraceptives — especially ones containing drospirenone — may help relieve symptoms.
It’s an altogether different story if you’re concerned about your birth control causing general anxiety.
Often, that spells a case of trial and error. Choose a method and stick with it for a few months before seeing how you feel.
Certain forms of birth control can cause anxiety simply because people worry they won’t use it properly.
A big example of this is, of course, the pill. Users may stress that they’ve forgotten to take it, or that they won’t take it at the same time each day.
The other cause of anxiety is thought to be the effect synthetic hormones can have on the body.
Most of the research into this has focused on the pill, which can contain forms of estrogen and progesterone, or the latter on its own.
“Both progesterone and estrogen are hormones that impact mood,” Lakhani explains.
And the hormone fluctuations that result from the pill — especially the estrogen — have been linked to anxiety, she says.
“Hormone contraceptive pills are believed to affect different regions of the brain,” Lakhani continues.
Indeed, a 2015 study found a link between oral contraceptive use and significant thinning in two brain areas.
As Abood explains, they were “the posterior cingulate cortex, [which is] linked to emotional stimuli based on our internal state of mind, or what is referred to as the view of self.”
The second was the side orbitofrontal cortex. This is “linked to emotion and behavior in relation to external stimuli,” Abood says.
Further research is needed to confirm whether the pill is causing brain thickness changes.
But, Abood says, these changes “suggest that hormonal contraceptives not only affect how [users] view external circumstances, but may also affect their view of themselves.”
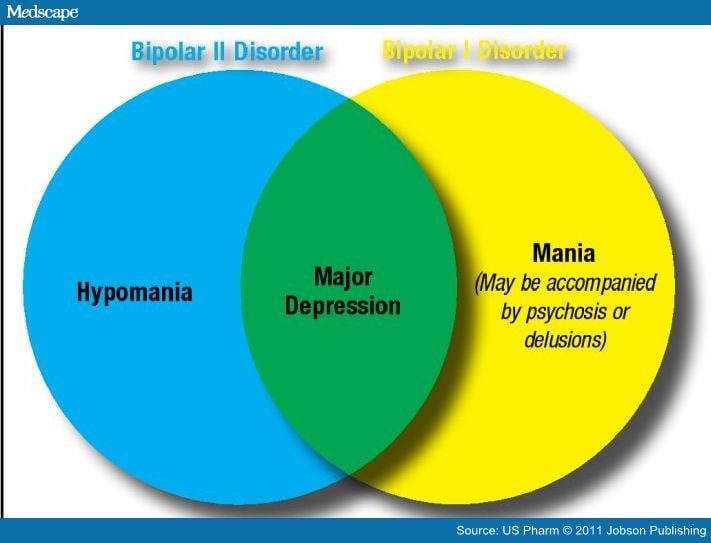
Hormonal birth control has also been linked to an increased risk of depression.
A 2016 study of more than 1 million Danish women found hormonal contraception was associated with first antidepressant use and first diagnosis of depression. The risk was especially present in adolescents.
But a 2013 study of women in the U.S. found the opposite: Hormonal contraception may reduce depression levels in young women.
Neither study proves that hormonal birth control causes or prevents depression — just that there may be a relationship between the two.
However, it’s worth noting some contraceptive methods — like the pill and ring — list mood changes as a potential side effect.
Some users have also reported experiencing panic attacks, though there’s very little research into this.
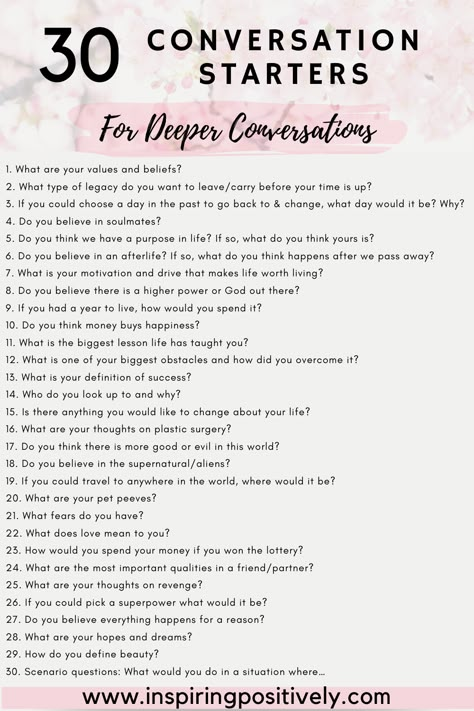
“There are a number of ways to manage anxiety,” Lakhani says, “from cognitive behavioral therapy (CBT) sessions and counseling to simple things that can be done at home, such as yoga and meditation.”
Lifestyle changes, like eating nutritious food and exercising regularly, can also help, Abood says.
Of course, you can consider changing your birth control method too.
If you already have an anxiety disorder or are worried about a specific type of contraception, speak to your doctor.
Be as open and honest as you can. Remember, their job is to help you decide which birth control method is right for you.
If you’re concerned that your current contraceptive is affecting your mood, track your symptoms in a diary and show it to your doctor.
“The earlier they can address those symptoms, the better,” Abood says.
Your doctor can then recommend self-help strategies, refer you to a mental health specialist for therapy, or prescribe medication, like an antidepressant.
Changing birth control may alleviate feelings of anxiety. But there’s a chance it could make little difference.
If you begin to experience anxiety or other mood changes, you can consider switching to a nonhormonal form of contraception. The list includes:
- copper IUD
- diaphragm
- condoms
Long-acting reversible contraception (known as LARC) is also a possibility for people who are worried they’ll forget to take a pill or apply a patch.
Your doctor can guide you down the best path.
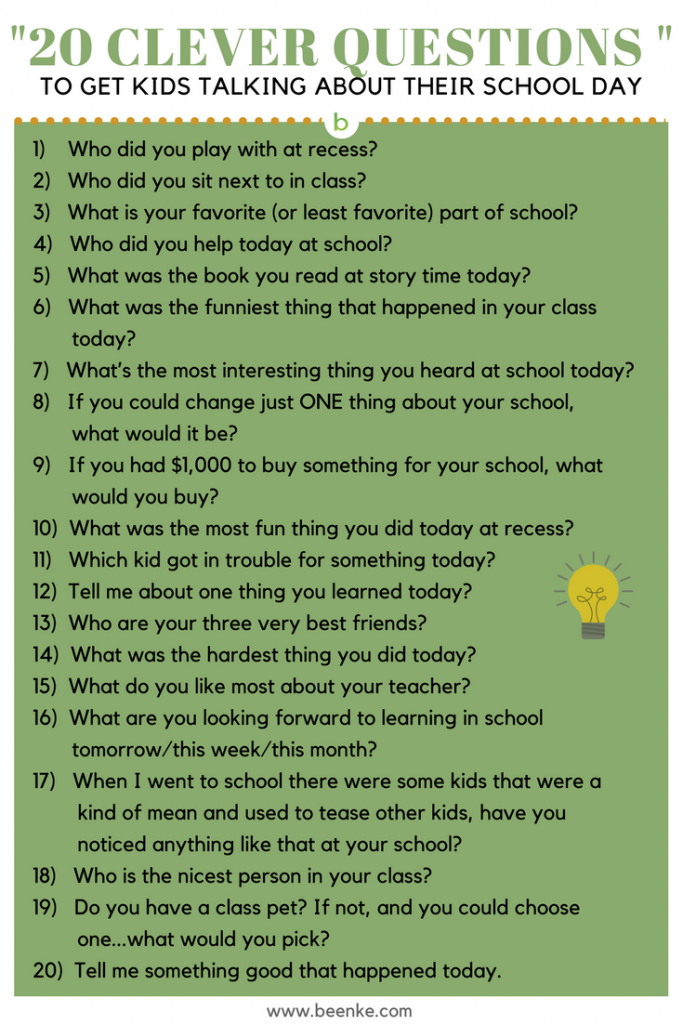
If you want to stop taking hormonal contraception, it’s entirely your choice.
But Lakhani advises never coming off your birth control without consulting with your doctor first.
Ask them the following:
- Can I get pregnant straight away?
- What side effects might I experience?
- What should I use for contraception now?
Some methods, like the pill and patch, can be stopped immediately. Others, like the implant, will need to be removed by a healthcare provider.
Something to consider: It’s good practice to not stop the pill or patch in the middle of your pack. Doing so can cause irregular bleeding.
The hormones from birth control should exit your body within a few days. (The shot, however, is designed to last for 3 months, so you may have to wait a little longer.)
Stopping any kind of hormonal birth control can have an impact on both your body and mind.
You may find that your menstrual cycle becomes irregular, or that your mood changes.
You may also experience symptoms your contraception was helping to manage, like painful periods and acne.
None of the side effects should be too severe. Many will right themselves as your body gets back to its usual hormone production.
But if your menstrual cycle is still irregular 3 months after stopping your birth control, or the effects are becoming difficult to manage, visit your doctor again.
It’s also important to know that you may get pregnant rather quickly. Use an alternative form of contraception if you don’t want to conceive.
Whether hormonal birth control will help or hinder anxiety is difficult to say.
Just because someone else has a bad experience doesn’t mean you will.
But before deciding on a contraceptive, weigh the potential effects.
And if you’re worried, speak to a doctor. They’ll work with you to find a method that suits your needs.
Lauren Sharkey is a journalist and author specializing in women’s issues. When she isn’t trying to discover a way to banish migraines, she can be found uncovering the answers to your lurking health questions. She has also written a book profiling young female activists across the globe and is currently building a community of such resisters. Catch her on Twitter.
When she isn’t trying to discover a way to banish migraines, she can be found uncovering the answers to your lurking health questions. She has also written a book profiling young female activists across the globe and is currently building a community of such resisters. Catch her on Twitter.
Birth control pills have not been proven to be linked to depression
Sign up for our 'Context' newsletter to help you sort things out.
Image copyright, BSIP
Image caption,Some of the side effects of birth control pills have been well known since they were on the market in the 1960s
One scientific study recently postulated an association between birth control pills and risk of depression .
This is not the first study purporting to find unwanted side effects of birth control pills.
But, as Elisabeth Kassin writes, an illiterate interpretation of statistics poses a much greater danger to women's health.
According to the World Health Organization, over 100 million women around the world use combined oral contraceptives, also known as birth control pills.
Some of the side effects of these tablets have been well known since they were introduced to the market in the 1960s. But a recent study allegedly established a link between birth control pills and depression.
Danish scientists studied the medical records of more than a million women aged 15 to 34 who had never suffered from depression in the past.
They found that those who took birth control pills were more likely to be prescribed antidepressants or diagnosed with depression later on by doctors.
The results of the study were reported in the press around the world. "Do you take birth control pills? You are more likely to be depressed: women who take contraceptives are 70% more likely to suffer from depression," one newspaper loudly declared. "Contraceptive pills are associated with depression.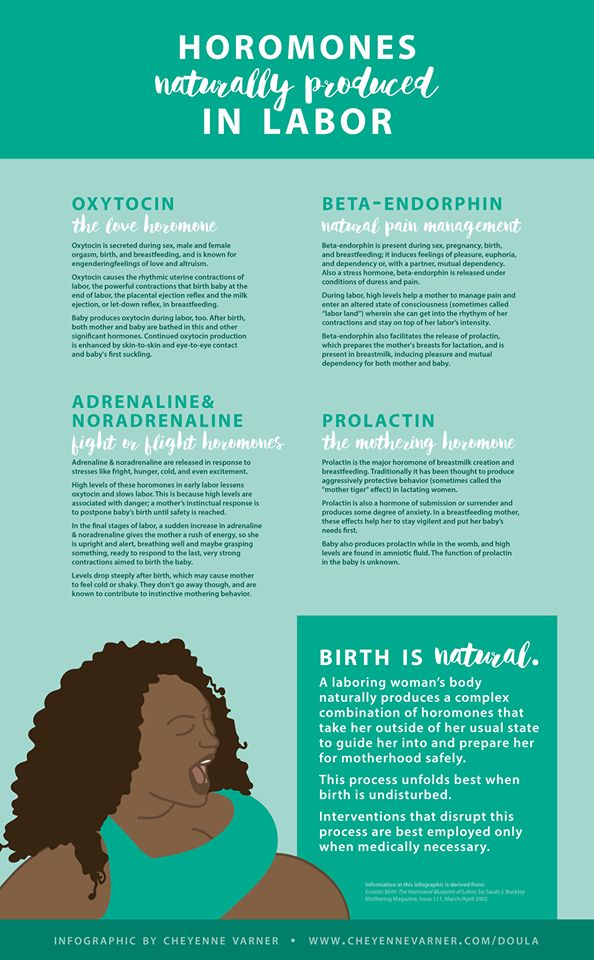 Why didn't a scandal erupt?" asked another.
Why didn't a scandal erupt?" asked another.
Image copyright, Getty Images
Image caption,Birth control pill randomized trial impossible
Skip the Podcast and continue reading.
Podcast
What was that?
We quickly, simply and clearly explain what happened, why it's important and what's next.
episodes
The End of the Story Podcast
However, as Phil Hannaford of the University of Aberdeen points out, the Danish study showed only "a small effect, if any."
Of every 100 women not taking birth control pills, 1.7 were using antidepressants. Among every 100 women taking oral contraceptives, this number is slightly higher - 2.2.
According to Hannaford, this is a very small difference. "The difference is 0.5, which is one woman in every 200," he says.
Although these data indicate a statistical relationship, they do not indicate a causal relationship, as some other factors may be at work in this case.
"For example, some of the women who take birth control pills may have separated from their partners. This, in turn, can lead to depression," he notes.
Such studies are sufficient to suggest a hypothesis, but we should not forget that they do not provide evidence for a causal relationship, adds Phil Hannaford.
This requires a large randomized controlled trial in which one group of women is given the test substance and another is given a placebo.
In this case, this is not possible (and unethical) because women who receive a placebo would think they are taking contraceptives and would not take other steps to prevent conception.
Image copyright, Getty Images
Image caption,Birth control pills from the 70s
This is not the first time scientists have been talking about the possible side effects of birth control pills.
Rare cases of blood clots, which can be life-threatening, attract the most attention.
But a poor understanding of the degree of risk can lead to undesirable consequences.
Professor Gerd Gigerenzer of the Harding Center for Risk Literacy in Berlin says that “There are many traditions in the UK, including scaring people about the risks associated with birth control pills. lead to thrombosis.
In 1995, the British Medicines Safety Board issued an official warning, citing a study showing third-generation birth control pills "doubled the risk of thrombosis".
"Alarms have been sounded all over the country," says Prof. Gigerenzer.
As a result of this panic, some women stopped taking contraceptives. According to some estimates, this led to an increase in the birth rate by 12,400 babies in 1996 and 13,600 additional abortions.
"This is an example of a lack of risk literacy - not understanding the difference between relative and absolute risk leads to an emotional reaction, which in turn leads to negative consequences for the women themselves," he says.
Image copyright, SCIENCE PHOTO LIBRARY
Photo caption,Pregnancy and childbirth lead to thrombosis more often than the birth control pill
What is the absolute risk? And how should women understand it?
The Guardian recently published a film about young women who died of blood clots after using hormonal contraceptives - birth control pills, vaginal rings and patches.
The authors of the film argue that if women knew about the mortality rate, they would stop using hormonal contraceptives. They also state that out of 10,000 women who use vaginal rings, at least a few die.
"It's not certain that a few out of 10,000 women will die," says Dr Sarah Hardman of the Department of Sexual and Reproductive Health at the Royal College of Obstetricians and Gynecologists.
"It would be more accurate to say that a few out of 10,000 women - between five and 12 - will develop thrombosis. But not all of them will die from this. In fact, only about 1% of women who develop thrombosis die" she says.
But not all of them will die from this. In fact, only about 1% of women who develop thrombosis die" she says.
"We are talking about the fact that three to 10 out of every million women die due to blood clots resulting from the use of hormonal contraception," - emphasizes Hardman.
For women of reproductive age who do not use hormonal contraceptives, only two out of 10,000 women per year face a fatal outcome.
But, of course, not using birth control pills to avoid thrombosis increases the risk of pregnancy. And pregnancy, in turn, in itself dramatically increases the risk of thrombosis.
"Among pregnant women, it's about 29 per 10,000," says Dr. Hardman.
"In the first few weeks after giving birth, 300 to 400 out of 10,000 women are at risk of developing blood clots," she continues.
In other words, pregnancy and childbirth are much more likely to cause thrombosis than the birth control pill.
In addition, the birth control pill is very effective in preventing pregnancy. Only the intrauterine device, implants or sterilization are more effective.
how to take, their action, types and classification
Hormonal contraceptives include the use of estrogen and progestin analogs to prevent unwanted pregnancy. The contraceptive effect is mediated by negative feedback in the hypothalamus, which ultimately leads to a decrease in pituitary secretion of follicle-stimulating (FSH) and luteinizing (LH) hormones.
Ovulation cannot occur without sufficient LH in the body. Low progestin levels reduce the chance of egg implantation by changing the structure of the cervical mucus, reducing the mobility of the fallopian tubes and proliferation of the endometrium. To date, taking hormonal contraceptives is the most common form of contraception.
Types of hormonal contraceptives
Oral drugs are best known in the form of tablets, but there are other types of drugs designed to change the hormonal background in the body.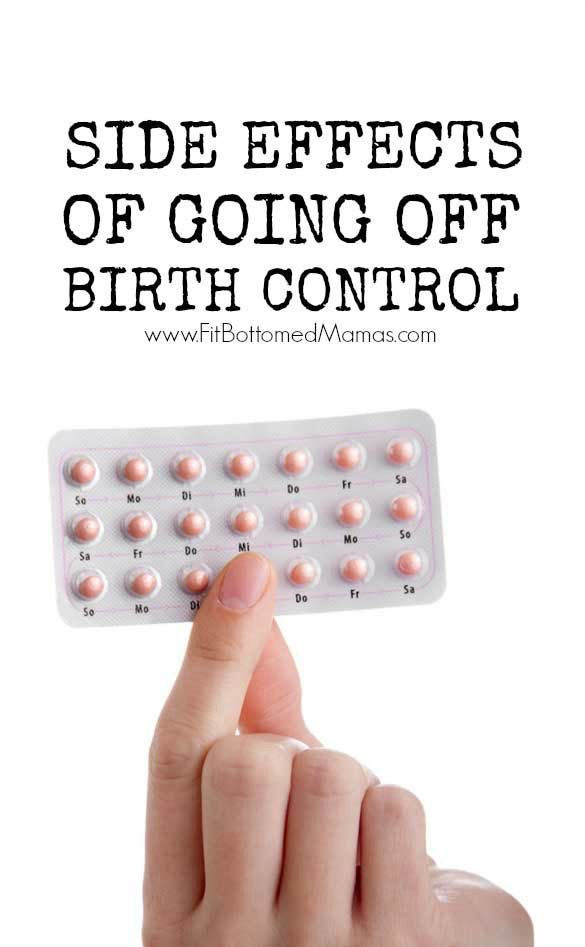 Among them:
Among them:
- plasters - patches with specialized impregnation;
- injections - injections to prevent fertilization of the egg;
- vaginal rings and intrauterine devices ;
- implants are hormonal contraceptives that are installed by a doctor in a gynecological office.
In combined monophasic oral contraceptives, the dose of estrogen and progestin remains constant, while in multiphasic preparations it changes during one cycle.
Reduced doses of multiphasic OCs alleviate some side effects. These include unpleasant symptoms such as breast tenderness, nausea, bloating, bleeding, and conditions such as venous thromboembolism. Due to the complications associated with taking OCs, their use is contraindicated in patients with severe symptoms of hypertension, coronary heart disease, or a history of stroke.
At the Harmony clinic, experienced specialists receive patients who want to individually choose an effective contraceptive.
After the examination and examination, the doctor writes out recommendations for preventing unwanted pregnancy. Since the funds are selected taking into account the personal characteristics of patients, the effectiveness is very high, and adverse reactions are minimal.
Review of drugs: the effect of hormonal contraceptives (COCs)
Oral contraceptive pills are the most popular group of drugs used by modern women to control conception. These drugs are a combination of estrogen and progesterone. They can be prescribed for polycystic ovary syndrome, endometriosis and amenorrhea.
Side effects include the risk of venous thromboembolism, hypertension and hepatic adenoma. For women over 35 who smoke or have estrogen-sensitive tumors, combined oral contraceptives are contraindicated. Allocate the following COC types :
- Monophasic - Each tablet contains the same dose of estrogen and progestin.
- Multiphasic - biphasic pills contain a fixed dose of, for example, ethinyl amtradiol and incremental doses of norethindrone, while triphasic tablets have different doses of each component over a standard 21-day cycle.
Indications for the use of this method are not only contraception, but also hyperandrogenism (pimples, hirsutism), menstrual disorders, control of symptoms in endometriosis and leiomyomas. Among modern pharmaceuticals in this group, the most popular brands can be distinguished.
Jess
Optimal formula for young women. Since the content of the hormonal component is extremely low, these tablets practically do not create a risk of developing vascular pathologies. Practice has shown that taking hormonal contraceptives of this spectrum is easily tolerated. Rarely there are adverse reactions from the digestive system. Regularly taken pills guarantee getting rid of pronounced premenstrual syndrome. They help to cope with such a complex condition as hormonal acne, improve the condition of hair and nails. Taking a contraceptive, you normalize the cycle, reduce the copious discharge of blood, and regulate weight.
Novinet
Contains 20 mcg of ethinyl estradiol per tablet and 150 mcg of desogestrel.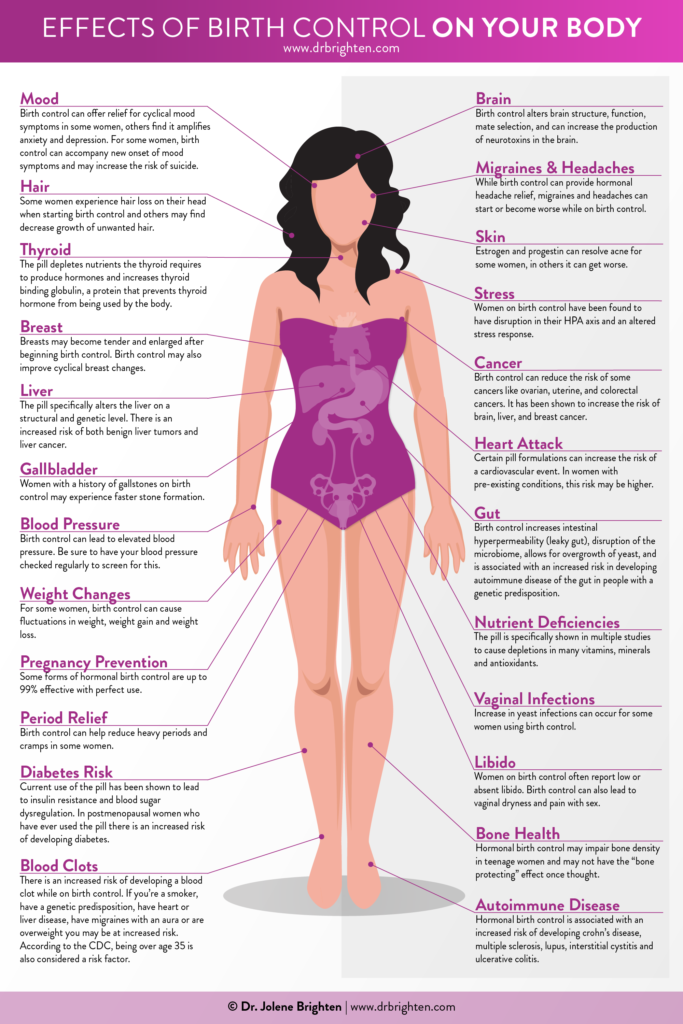 The medicine favorably affects the regulation of the menstrual cycle. Differs in the minimum number of adverse reactions. Like Jess, it is allowed to be taken on the 21st day after childbirth, if the woman is not breastfeeding.
The medicine favorably affects the regulation of the menstrual cycle. Differs in the minimum number of adverse reactions. Like Jess, it is allowed to be taken on the 21st day after childbirth, if the woman is not breastfeeding.
Janine
Monophasic oral contraceptive with a low dosage of active substances. It has a good antiandrogenic effect, easily eliminates acne, acne, blackheads and seborrhea from the surface of the body. Normalizes the fat balance of the skin, regulates hair growth.
Lindet 20
The content of hormones in these pills is low, which in no way detracts from their effectiveness in preventing unwanted conception. There are virtually no adverse reactions, in rare cases, a slight headache and nausea are possible.
Yarina
This is a new level of pharmaceuticals. In addition to eliminating skin problems, Yarina helps to normalize weight, reduce the level of elevated BMI. Reduces the symptoms of PMS.
Mini-drinks: powerful small agent
The next group of drugs is progestin-only hormonal pills (mini-pills or mini-pill contraceptives).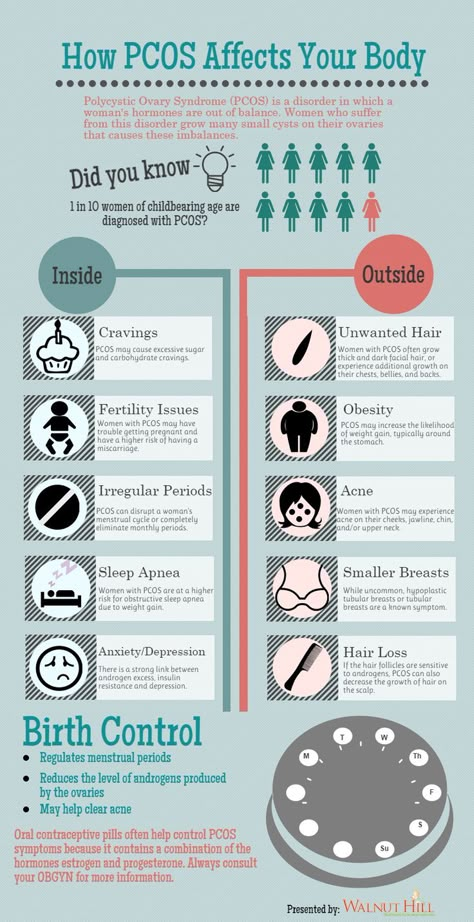 It is a short-acting reversible oral contraceptive containing low doses of norethindrone. It is an ideal contraceptive for women who are contraindicated in estrogen supplements.
It is a short-acting reversible oral contraceptive containing low doses of norethindrone. It is an ideal contraceptive for women who are contraindicated in estrogen supplements.
Among them:
- nursing mothers;
- overweight women;
- individuals with individual estrogen intolerance and premenopausal women.
Charozetta
The basis of this type of pharmacology is desogestrel (75 mcg). An ideally mild agent that is instantly absorbed, forming a biologically active metabolite of etonogestrel. The half-life is up to 30 hours. The order of taking the tablets is indicated on the package.
Lactinet
Desogestrel is contained in the same dose as the previous drug. It does not have a negative effect on weight, with the right selection, it even contributes to weight loss. A good option for women who are in the lactation period. One of the most common side effects is blood smearing, which resolves within 3 months of starting treatment.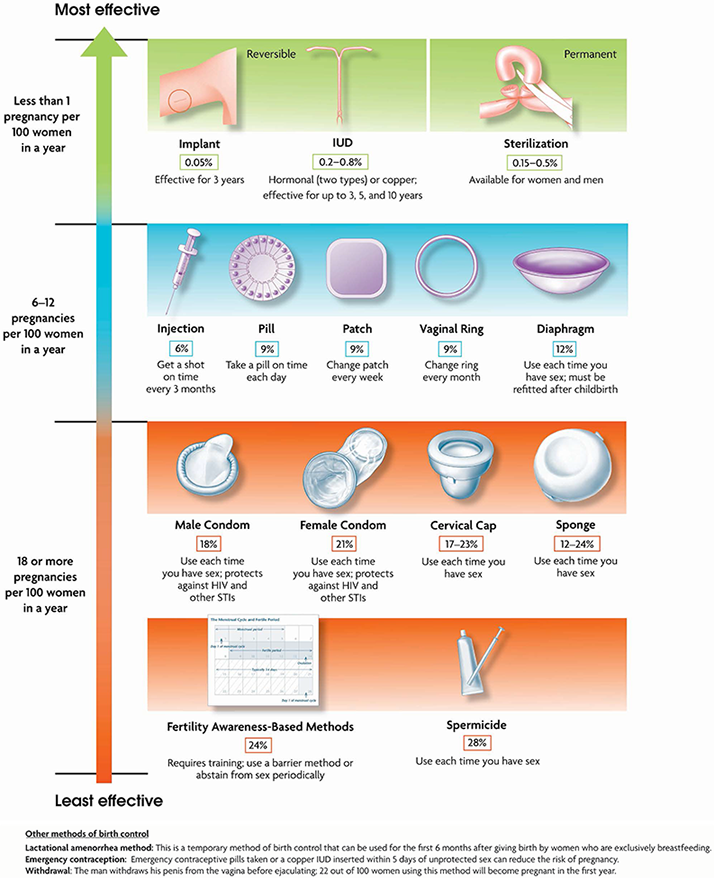
Exluton
Contains linestrenol 500 mcg. Normalizes hormonal balance, favorably affects a woman's sensuality, her libido. Suitable for use by nursing mothers.
Hormone patch: stick on and go
The action of hormonal contraceptives of this kind is really as simple as possible. Outwardly, this patch looks like a classic adhesive plaster, it is easily applied to the skin, fixed with a sticky layer and keeps flawlessly, despite clothing and simple hygiene procedures. Benefits of using this patch next :
- no need to interrupt sex to attach a sticker to the body;
- does not need to be examined before use. However, bearing in mind that this remedy is hormonal, it should be used with caution for the first time;
- reduces the flow of menstrual blood in those who suffer from heavy bleeding;
- reduces pain during menstruation;
- the sticker is changed according to the instructions given by the manufacturer.
 One patch is attached once a week, this procedure is repeated for 3 weeks. Then 1 week - a break;
One patch is attached once a week, this procedure is repeated for 3 weeks. Then 1 week - a break; - after the final removal, the woman quickly returns to normal and can plan a pregnancy on the recommendation of a doctor.
Studies have shown that patches are as good as combined oral contraceptives and minipills. It is enough to print the product, stick it on the cleansed skin of the shoulder, abdomen or buttocks.
How this product works :
- preventing the production of an egg by the ovaries;
- thickening of the mucous layer in the cervical region, which complicates the penetration of spermatozoa into the organ and makes fertilization impossible;
- thinning of the uterine mucosa, which prevents the introduction of the egg into the endometrial layer.
The use of hormonal contraceptives in the form of patches showed effectiveness in 91% cases.
Despite the good result, do not forget that the sticker does not provide protection against sexually transmitted infections, and therefore is recommended for use with other protective equipment. The disadvantage of this method of contraception is that it is noticeable, can be saturated with dust and look untidy on the skin. Not suitable for people with sensitive dermis, as it can provoke irritation.
Vaginal ring and injectable progestin
Indications for use are similar to those for oral contraceptives. The vaginal ring is flexible, acting through a combination of ethyl estradiol and etonogestrel. It is inserted into the vagina, held in place for 3 weeks, and then disposed of. After the menstrual bleeding caused by the withdrawal syndrome, a new ring is inserted and everything is repeated anew.
Injectable progestin is a synthetic form of progesterone. Used for contraception, as well as in the treatment of abnormal uterine bleeding and signs of endometriosis. Available as an intramuscular or subcutaneous injection. Entered once every three months. Its effectiveness is often higher than that of other contraceptives, it is 94% .
Available as an intramuscular or subcutaneous injection. Entered once every three months. Its effectiveness is often higher than that of other contraceptives, it is 94% .
Intrauterine device and subcutaneous implant
Considering all types of hormonal contraceptives, the intrauterine device (IUD) cannot be overlooked. A small contraceptive device is often made in a T-shape. The doctor inserts it into the woman's uterus to prevent pregnancy. Issued non-hormonal IUD and hormonal modifications.
The material from which these contraceptives are made is varied. It can be plastic, copper, silver and even gold. The price of intrauterine devices varies widely. These are long-term control devices that can remain in place for 3-5 years or more. It all depends on the type and brand. The efficiency is very high and is 99% . As for the implant, it is inserted subcutaneously into the forearm, acting for 3 years. The principle of exposure is the same, due to the content of progestin.
Emergency methods of contraception
General classification of hormonal contraceptives contains one more name. This is an emergency contraceptive technique that involves a slight malfunction in the body to prevent conception. As a rule, the drug is produced in the form of one, less often two tablets. Effective in case of unprotected intercourse if taken within 48-72 hours from the moment of sexual intercourse. The earlier the pill is drunk, the higher its effectiveness. Due to a large dose of hormones, the cycle changes. Not recommended for frequent use.
Indications for immediate cessation of hormonal contraceptive use
- sensory disorders, visual disturbances;
- migraines, frequent headaches;
- epileptic seizures;
- detection of tumors of unknown etiology;
- growth of uterine fibroids;
- jaundice, pregnancy, suspected thrombophlebitis.