Depression of the central nervous system
CNS depression: Symptoms, risks, and treatment
Central nervous system — or CNS — depression happens when the body’s normal neurological functions slow down. It can result from substance overdoses, poisoning, or other medical conditions.
Depression of the central nervous system or CNS often occurs when a person misuses a substance that slows brain activity. These substances are called CNS depressants.
Examples of CNS depressants include tranquilizers, hypnotics, and sedatives. In recent years, doctors have prescribed opioid painkillers for many conditions, but overuse of these drugs can lead to problems.
People also use them as recreational drugs. Recreational use can be illegal and dangerous, as people may not understand the risks of misuse.
Combining different CNS depressants, such as painkillers and alcohol, can be life-threatening.
Find out here more about the uses and risks of CNS depressants.
Share on PinterestPeople should use sleeping pills, pain-relief medication, and other CNS depressants with caution.A person may benefit from taking the correct dose of a CNS depressant, such as an opioid pain relief medication.
But, high doses of these drugs can reduce the activity of the CNS to dangerously low levels.
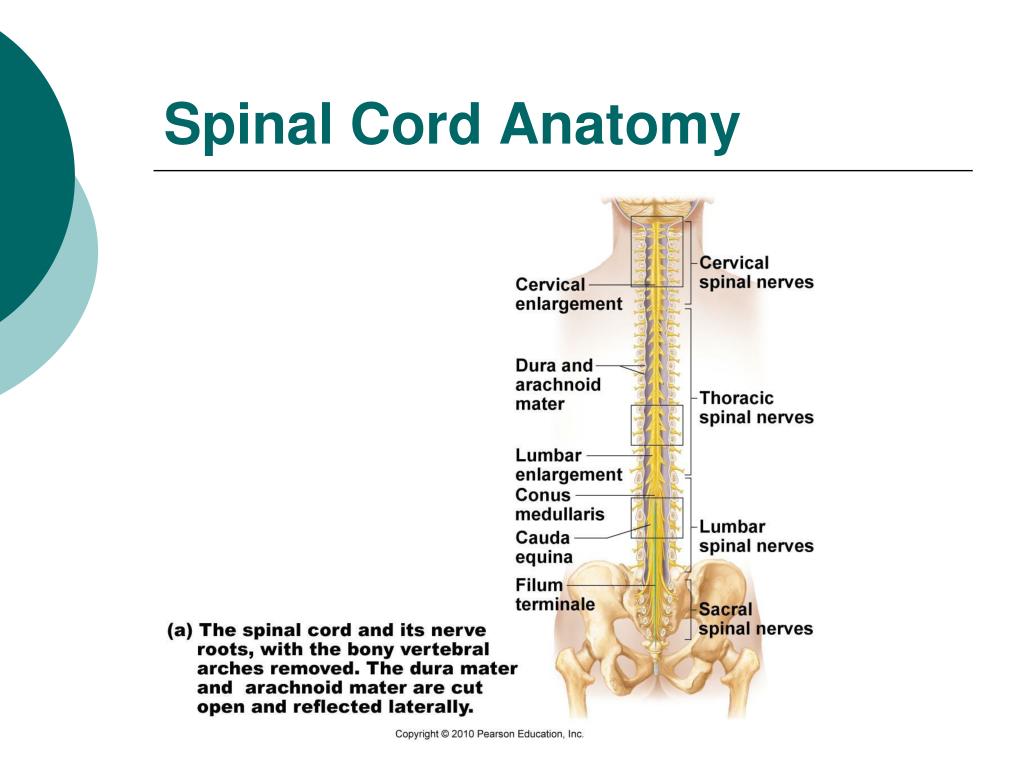
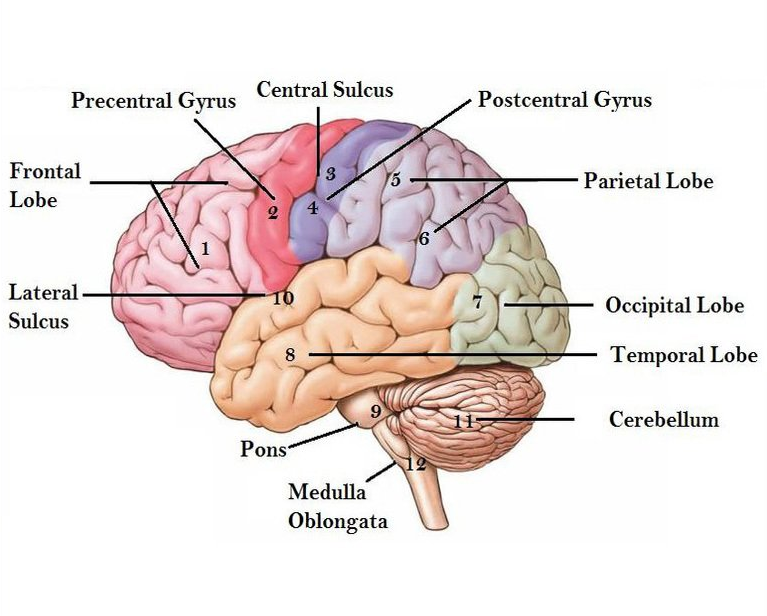
The CNS consists of the brain and spinal cord. It controls most bodily functions — including breathing and the heart — by sending messages between the brain and other nerves via the spinal cord.
It plays a role in essential bodily processes:
Involuntary processes: These do not need conscious thought. They regulate vital organs such as the heart, lungs, and stomach. They are responsible for functions, including digestion and blood circulation.
Voluntary processes: These involve conscious thought. They enable people to move their arms and legs, for example, or to blink their eyes.
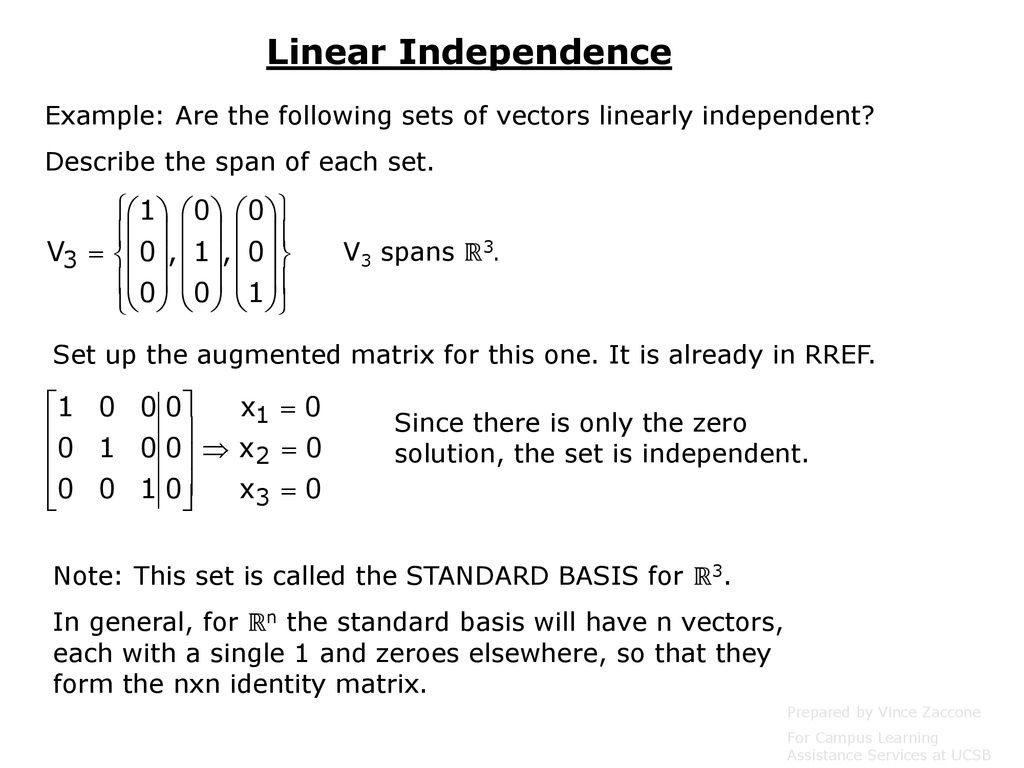
CNS depressants are medications and other substances that slow down the CNS.
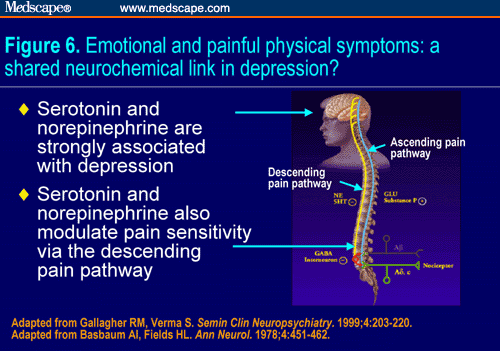
Many CNS depressants work by increasing the activity of the neurotransmitter gamma-aminobutyric acid (GABA), a chemical that prevents or slows the delivery of messages between cells.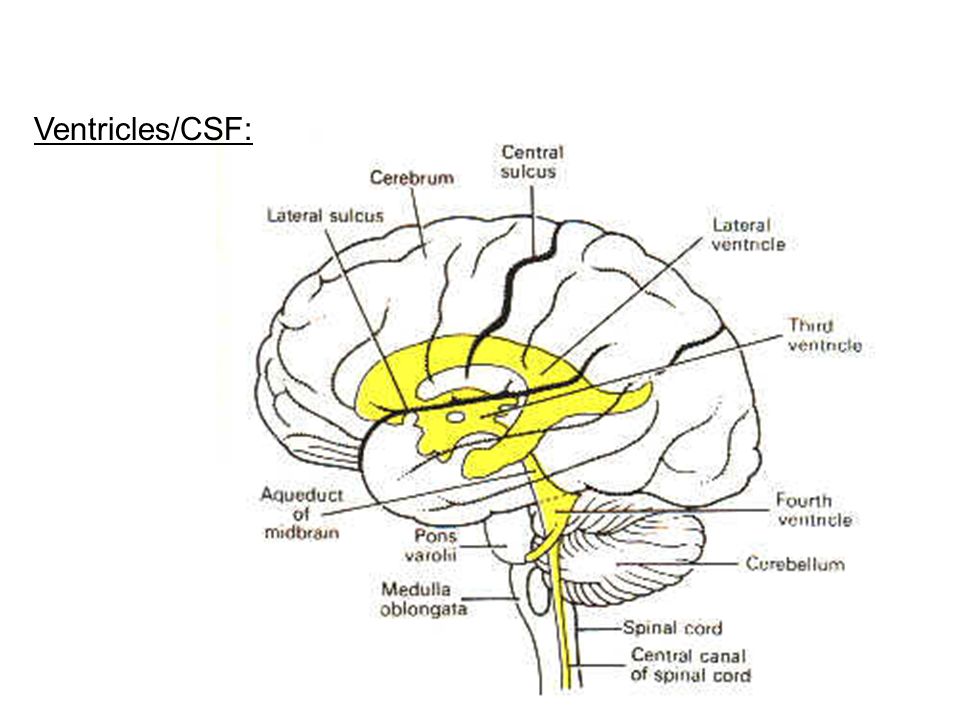
People can have varying symptoms of CNS depression or depressant overdose. Factors that affect the impact of CNS depression include:
- the cause
- the type and dose of a substance
- the severity of the illness or injury
- the size of the individual
- the person’s medical history
Mild symptoms
Mild symptoms of CNS depression include:
lack of coordination and impaired sense of space
- muscle weakness
- lethargy
- dizziness
- disorientation
- slurred speech or stuttering
- slight shortness of breath or shallow breathing
- slightly reduced heart rate
- constipation
- dry mouth
- restlessness and agitation
- euphoria
- blurred, altered, or double vision
Severe symptoms
Symptoms of severe CNS depression include:
- reduced heart rate
- low breathing rate of fewer than 10 breaths per minute
- extreme confusion or memory loss
- nausea and vomiting
- poor judgment
- blue lips or fingertips
- irritability and aggression
- clammy or cold skin
- sudden and intense mood swings
- slow reflexes
If a person has any of these symptoms, they should seek immediate medical care.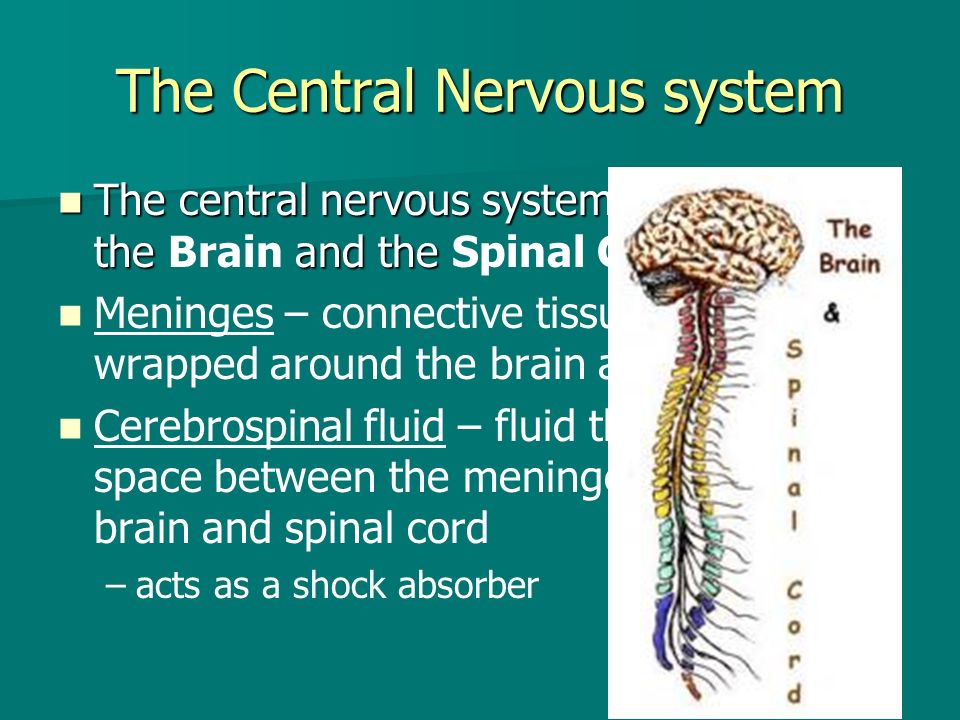 Ultimately, severe symptoms can lead to unresponsiveness, coma, and death.
Ultimately, severe symptoms can lead to unresponsiveness, coma, and death.
Long-term effects
Continued use of some CNS depressants can be harmful long-term, as the body becomes unable to flush out these substances.
Effects may include:
- problems with thought, memory, and judgment
- disorientation and confusion
- muscle weakness
- loss of coordination
- slurred speech
Also, the individual may need more and more of the drug to experience the same benefits. This greater need can lead to dependence. Some people may need rehabilitation therapy to stop using the drugs.
Several substances can depress the CNS, ranging from anti-anxiety and sleep medications to so-called recreational drugs, such as heroin.
Medications, drugs, and other substances
Share on PinterestOpioids can be useful in relieving pain, but they can be very dangerous, too.
The main substances that cause CNS depression are:
- alcohol
- barbiturates
- benzodiazepines
- opioids
Most of these drugs cause some combination of drowsiness, muscle relaxation, and anxiety reduction.
These substances carry a risk of addiction. Combining them can lead to severe and potentially life-threatening adverse effects.
Many medically prescribed and high-dose depressants are also common street drugs, and some people use them recreationally.
Non-drug causes
CNS depression does not only result from the use of medications and other substances.
Non-drug causes include:
- brain trauma or severe injury
- stroke
- infection
- tumor
- aneurysm
Other medical conditions that increase the risk of CNS depression include:
- kidney, lung, heart and liver disease
- diabetes
- thyroid disorders
People with any of these conditions should check with a doctor before using a CNS depressant.
Doctors commonly prescribe some types of CNS depressant for various reasons.
Opiates and opioids
These are strong pain-relieving drugs that come from opium, a substance made from the seeds of the poppy.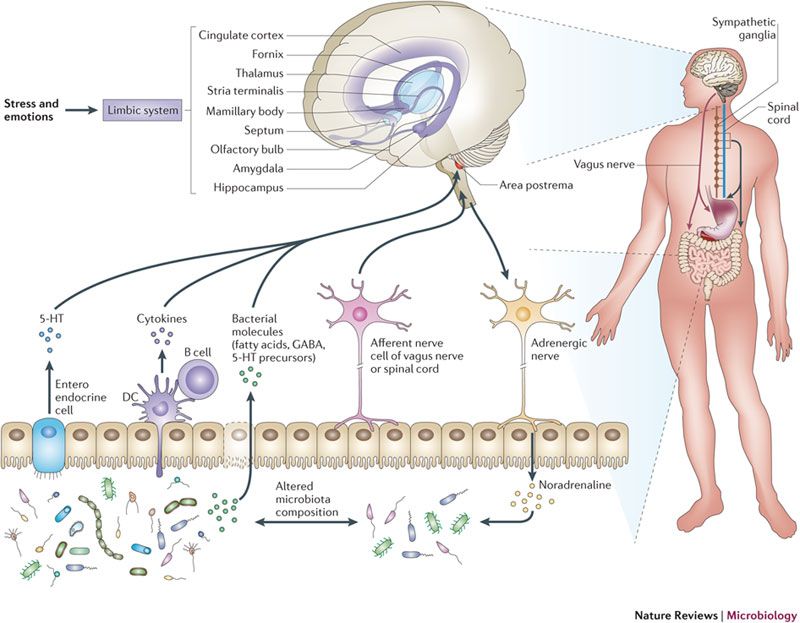
Opiates are the active ingredients in opium, heroin, morphine, and codeine. Opioids are derived from opiates, such as oxycodone, hydrocodone, and heroin.
Both opiates and opioids work by interfering with the CNS and blocking pain signals to the brain.
Commonly prescribed opiates and opioids are:
- oxycodone (OxyContin)
- hydrocodone (Vicodin)
- morphine (Kadian, Avinza)
- codeine
- fentanyl (Duragesic)
- methadone
- hydromorphone (Dilaudid)
Doctors may prescribe these drugs for pain relief. Given their strength and addictive qualities, only people who have a severe condition should use them.
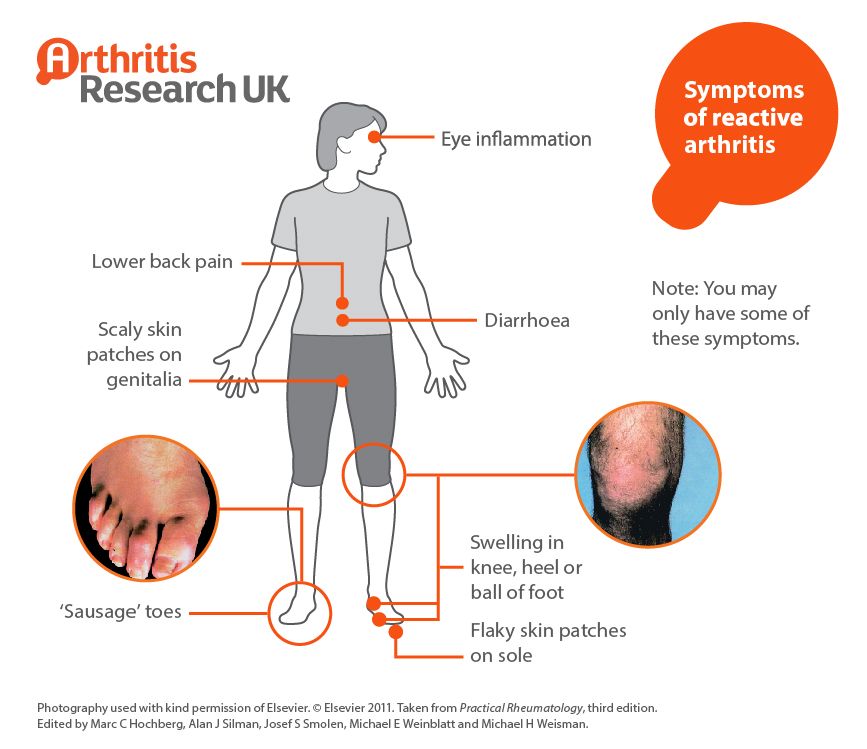
Some of these substances, for example, codeine, are present in medications for coughs or diarrhea. Doctors will prescribe these for short-term use only.
Some people also use opioids and opiates, such as heroin, as recreational drugs. Common street names include H, smack, oxy, and China white.
Sleep medications
These are chemically different from other CNS depressants, but they work by stimulating the same inhibitory neurotransmitter, GABA.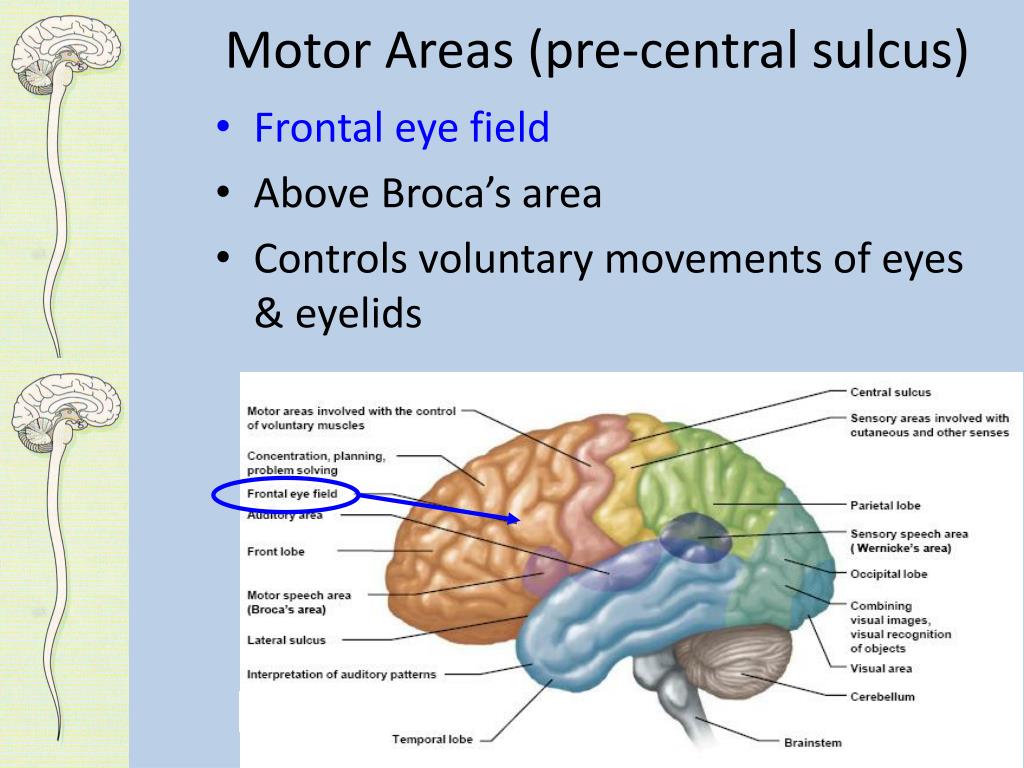
Common sleep medications that doctors may prescribe are:
- zolpidem (Ambien)
- zaleplon, (Sonata)
- eszopiclone (Lunesta)
Street names for sleep medications include zombie pills, sleepeasy, and tictacs.
Benzodiazepines
These are a treatment option for conditions that can include stress reactions, panic attacks, sleep disorders, and convulsions.
Examples of benzodiazepines include:
- alprazolam (Xanax)
- clonazepam (Klonopin)
- diazepam (Valium)
- lorazepam (Ativan)
- estazolam (ProSom)
Benzodiazepines can also be a drug of abuse. Street names include benzos, downers, and chill pills.
In 2020, the Food and Drug Administration (FDA) strengthened their warning that benzodiazepine use can lead to addiction. Combined with alcohol, opiods, and other CNS depressants, they can be life-threatening.
Barbiturates
These can treat seizure disorders and anxiety, but doctors rarely prescribe them nowadays.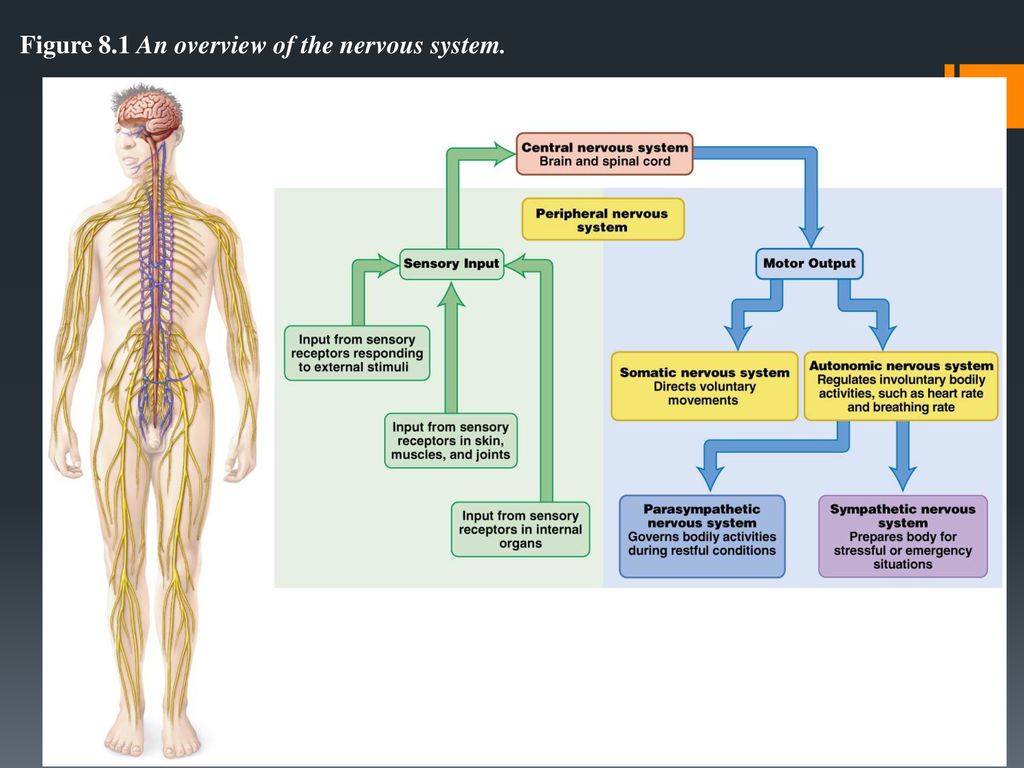 Before surgery, they may promote sleep and relaxation.
Before surgery, they may promote sleep and relaxation.
Examples include:
- mephobarbital (Mebaral)
- sodium phenobarbital (Nembutal)
As a recreational drug, people sometimes call them barbs, downers, or phennies, among other names.
Crime-related drug use
Sexual and violent crime are other areas where people are known to misuse CNS depressants. The sedative Xyrem, known as the “date rape drug,” commonly features in cases of sexual assault.
Xyrem is easily hidden in drinks, as it is odorless, colorless, and tasteless when mixed with liquid.
When people use CNS depressants, it can be hazardous for many reasons, including:
- dependency
- withdrawal symptoms when ending their use
- overdose
- long-term adverse effects
Misuse can also happen if a person uses someone else’s medication, if they take more than the recommended dose, or if they use drugs that a doctor has not prescribed.
Combining substances
Share on PinterestCombining CNS depressants, for example, alcohol with sleeping pills, can be dangerous.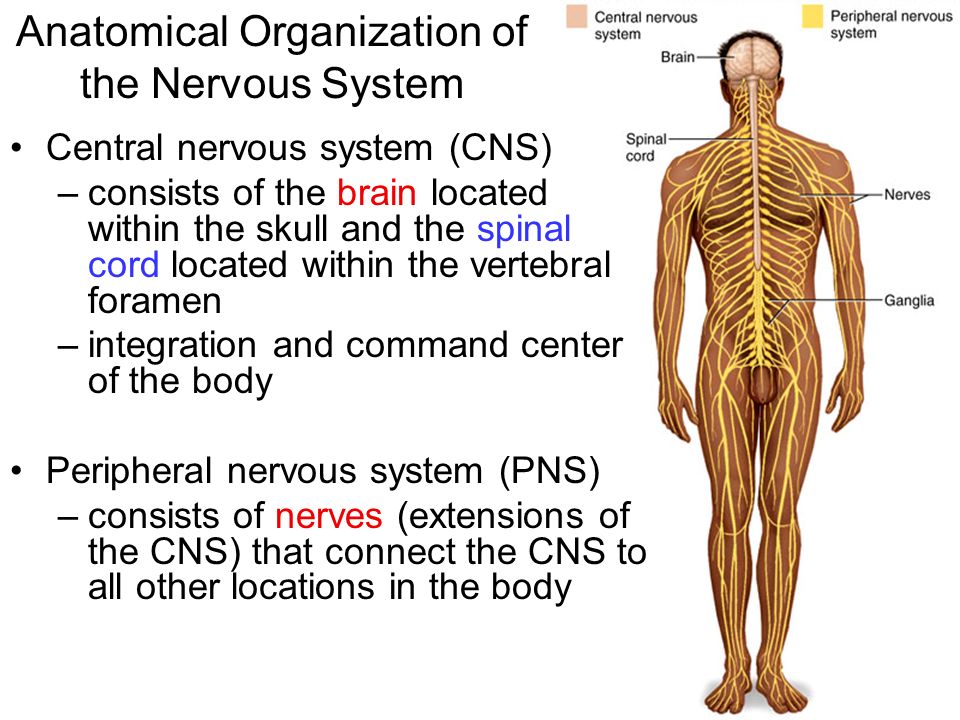
Mixing CNS depressants, opioids, and alcohol increases their effect. There may be severe adverse reactions and possibly life-threatening consequences.
Sometimes, a person may not realize they are at risk of an overdose, such as when they use opioid pain relief medication and then drink alcohol.
Prescription benzodiazepines and opioids carry the highest level of warning from the U.S. Food and Drug Administration (FDA), because of their risks.
People should check first with their doctor to find out if it is safe to take CNS depressant medication and any of the following:
- alcohol
- over-the-counter medicines with similar properties, such as painkillers
- allergy medications
- sleeping aids
Tricyclic and tetracyclic (TCA) antidepressants can also intensify the effects of CNS depressants, especially drowsiness.
Dependence and withdrawal
Some CNS depressants become less effective over time, so that a person may feel the need to take a larger dose. If they stop using the drug, the original symptoms can return more severely than before.
If they stop using the drug, the original symptoms can return more severely than before.
A person who wishes to stop using a CNS depressant may need to stop gradually to prevent adverse effects. A doctor can help them to do this.
Overdose
An overdose of a CNS depressant can happen by accident, but people sometimes choose to take more of the drug than a doctor recommends to get a more “intense” effect. This can lead to overdose and death. People have also been known to overdose on these medications deliberately to end their lives.
A person may recover from an overdose, but research in the Journal of Clinical Psychopharmacology shows that some may continue to have problems with everyday functioning after leaving the hospital.
Long-term effects
Some types of CNS depressant can also have long-term effects, causing someone to have difficulty thinking, confusion, speech problems, loss of coordination, and muscle weakness.
Addiction to CNS depressants may see a person experience social and family problems, difficulty working, and an inability to function in daily.
The opioid crisis: Some figures
Since 2000, more than 300,000 Americans have died of an opioid overdose. Data for 2016 estimates at least 64,000 drug overdose deaths, the highest number ever recorded in the United States.
Overdoses of prescription painkillers in the U.S. is a growing problem, especially among women, according to the Centers for Disease Control and Prevention (CDC).
Share on PinterestSevere symptoms of CNS depression include loss of consciousness, coma, and death. Anyone with these symptoms needs immediate medical help.
Treatment for CNS depression or CNS depressant overdose depends on the substances involved.
Some CNS drugs have antidotes that can reverse their effects. These include Naloxone for opioid overdoses and Flumazenil for overdoses of benzodiazepine.
A person may need emergency care if they are unaware that they are experiencing a CNS depressant overdose, especially after accidentally misusing their medication or due to a medical problem.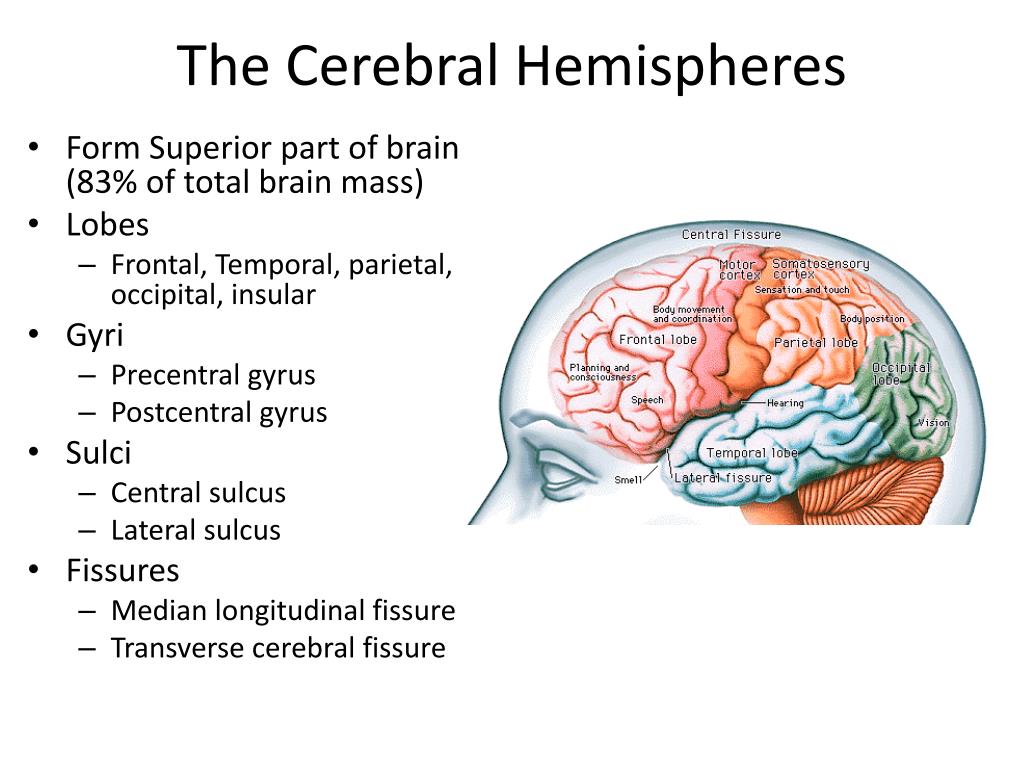
Anyone witnessing signs of CNS depression or an overdose in another person should call the emergency services or local poison control center for guidance.
In these cases, treatment may include:
- monitoring the person’s breathing and heart rate.
- giving oxygen via an oxygen mask or respirator
- administering stimulant drugs to increase a person’s heart rate
In the U.S., anyone who is concerned that they or someone they know is misusing CNS depressants can:
- call 1-800-662-HELP (4357) or 1-800-487-4889 to find their nearest Substance Abuse Treatment Facility for help and advice
- access the Substance Abuse and Mental Health Services Administration (SAMHSA) website for help and advice
These services offer free and confidential advice, 24/7, in English or Spanish.
The National Suicide Prevention Lifeline can help with a wide range of problems. People can contact them for a confidential chat on 1-800-273-8255 or 1-800-273-TALK.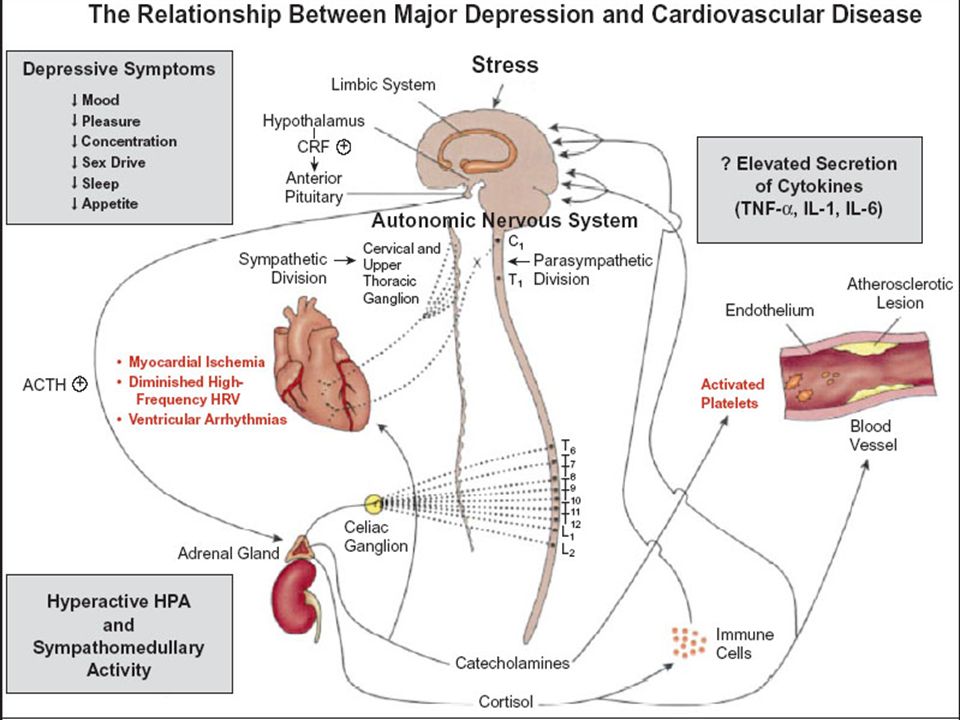
CNS depression or overdose is a common cause of poisoning in many developed countries, including the U.S. and Canada.
People who take CNS depressants must be aware of the risks and should never share drugs or take a substance without knowing what is in it.
Only a doctor should prescribe a CNS depressant, and people should only use these drugs for the specified purpose, according to the doctor’s instructions.
Q:
My doctor has prescribed Oxycodone for my chronic back pain. Is it dangerous for me to use this medication? Nothing else seems to work.
A:
There is no way to know who may become addicted to an opiate medication.
The most important thing is to be honest with your prescriber regarding your symptoms, and to communicate honestly. Discuss treatment goals and alternatives to the use of opiates so that opiate use is limited.
For some people, limiting the duration of use of opiate medications may not be possible, and in these cases, ongoing communication and honesty with your prescriber is essential for adequate monitoring of both pain and side effects.
Timothy J. Legg, PhD, CRNPAnswers represent the opinions of our medical experts. All content is strictly informational and should not be considered medical advice.
Central Nervous System (CNS) Depression: Know the Facts
What is CNS depression?
The central nervous system (CNS) consists of the brain and the spinal cord.
The brain is command central. It orders your lungs to breathe and your heart to beat. It rules virtually every other part of your body and mind, including how you feel about and interact with the world around you.
The spinal cord handles nerve impulses, allowing your brain to communicate with the rest of your body.
When CNS functions slow down, it’s called CNS depression. Slowing down a little isn’t necessarily dangerous. In fact, sometimes it’s even helpful. But if it slows down too much, it can quickly become a life-threatening event.
Continue reading to learn more about CNS depression and the warning signs of trouble.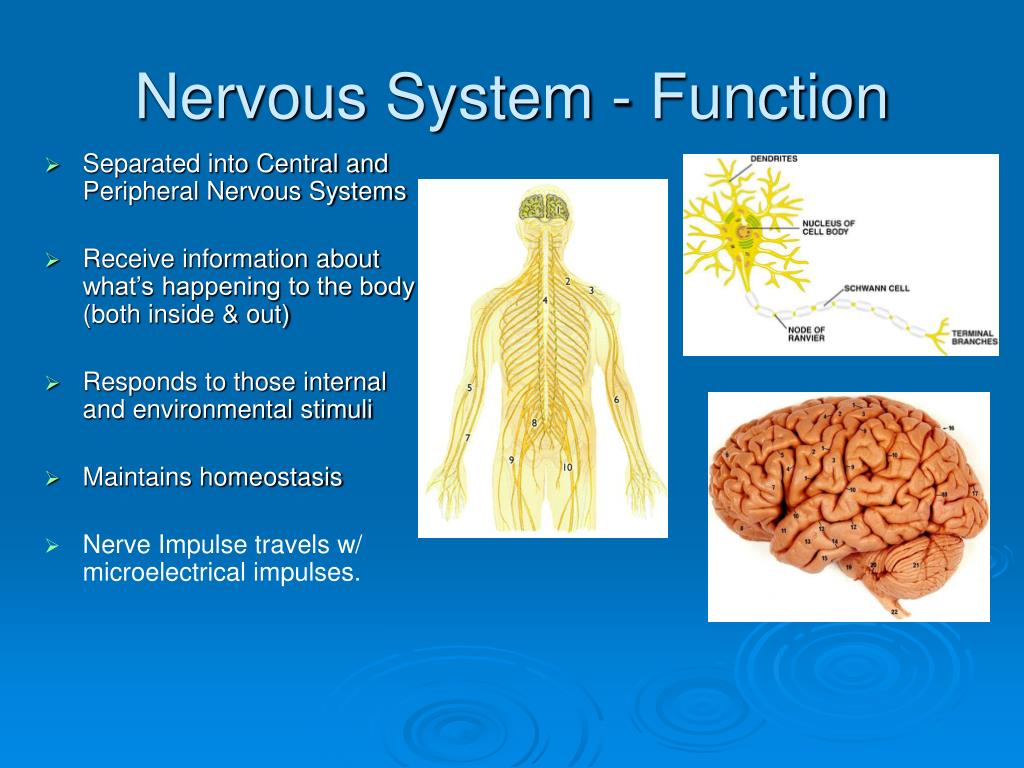
A mild slowing of the CNS may make you feel less anxious and more relaxed. That’s why CNS depressants (sedatives) are used to treat anxiety and insomnia.
In some cases, you may also exhibit:
- lack of coordination
- slowed or slurred speech
- drowsiness
If the CNS slowing worsens, symptoms may include:
- poor judgment
- slowed breathing
- slowed heart rate
- confusion
- lethargy
A severely depressed CNS can lead to delirium or coma. Without prompt treatment, this is potentially fatal.
Certain drugs affect the neurotransmitters in your brain, causing brain activity to slow. That, in turn, makes your breathing slower and shallower. It also makes your heart beat slower.
Common causes of CNS depression include the use of medications, drugs, or alcohol. Initially, they may cause a mild stimulant effect or even a feeling of euphoria. But make no mistake about it, these substances are CNS depressants.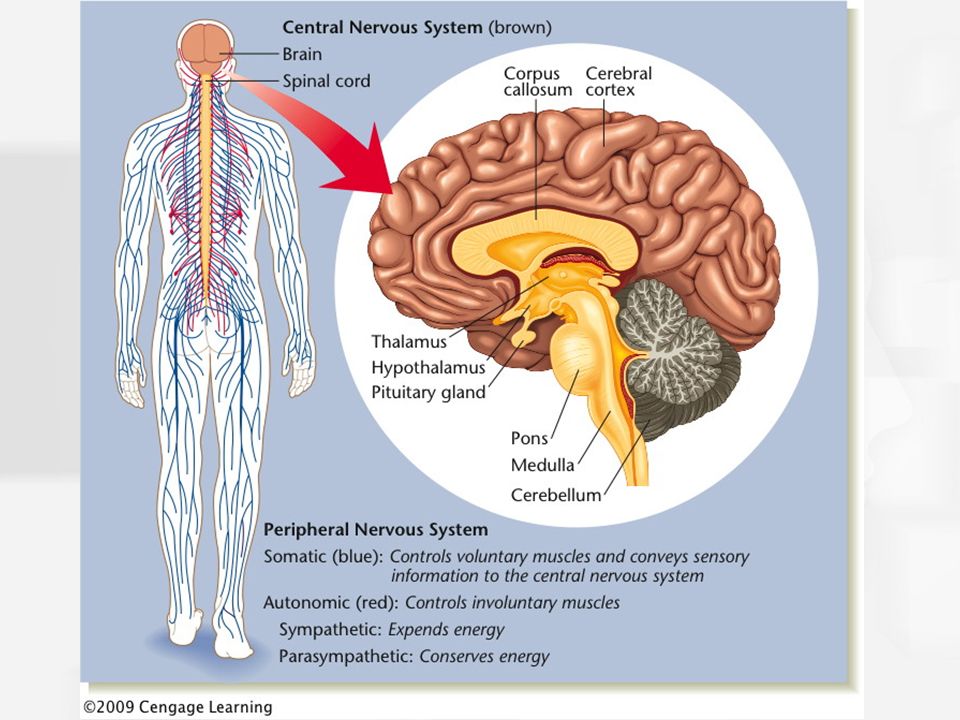 Some specific depressant drugs include:
Some specific depressant drugs include:
Barbiturates
These are sometimes prescribed prior to surgery to you help relax during the procedure. They can also be used as anticonvulsants. Because they’re so powerful, they currently aren’t prescribed for things like anxiety and insomnia as much as they used to be.
Drugs from this group include:
- mephobarbital (Mebaral)
- pentobarbital sodium (Nembutal)
- phenobarbital (Luminal Sodium)
Benzodiazepines
Considered safer than barbiturates, these drugs are prescribed to treat anxiety and insomnia. There are many benzodiazepines, including some you’ve probably heard of:
- alprazolam (Xanax)
- diazepam (Valium)
- triazolam (Halcion)
Opiates
These are usually prescribed for pain. Common opiates include:
- codeine
- hydrocodone (Vicodin)
- morphine (Kadian)
- oxycodone (Percocet)
Heroin is also an opiate.
Sleep medications
Certain sleeping aids also fall into this category. These include:
These include:
- eszopiclone (Lunesta)
- zaleplon (Sonata)
- zolpidem (Ambien)
In small doses, these drugs slow brain function, producing a calm or sleepy feeling. A higher dose can slow your heart and breathing rates. The danger is when the CNS is slowed too much, which can lead to unconsciousness, coma, and death.
Mixing alcohol with other CNS depressants magnifies their impact and in many instances can be fatal.
Medical causes
CNS depression can also result from severe health events.
Chronic medical conditions can put you at risk for CNS depression. This includes:
- diabetes
- thyroid problems
- liver disease
- kidney disease
Direct injury to the brain can also cause CNS depression. This includes:
- brain aneurysm
- tumor
- stroke
- infection
- trauma due to a fall or accident.
Any event that causes decreased blood flow and oxygen to the brain, such as a severe heart attack can also lead to CNS depression.
Other causes
A variety of other things in your environment can lead to CNS depression when ingested or inhaled. One such product is ethylene glycol, a chemical found in a variety of consumer goods, including antifreeze and de-icing products. When ingested, this chemical is toxic to the CNS, kidneys, and heart. It can cause serious health complications, including death.
Learn more: Tramadol vs. Vicodin: How they compare »
Having a history of addiction may put you at higher risk of CNS depression. That’s because you may be prone to taking more medication than prescribed or combining medication with other drugs or alcohol.
You may also be at higher risk if you have existing respiratory problems such as emphysema and sleep apnea.
Mild CNS depression due to prescription medication is to be expected and isn’t necessarily a problem if sedation is desired. However, if you feel too sluggish or overly sleepy while taking medications that depress the CNS, talk to your doctor. There may be an alternative treatment, or perhaps your dose can be adjusted.
There may be an alternative treatment, or perhaps your dose can be adjusted.
Severe CNS depression is a medical emergency, regardless of the cause. Call your local emergency services if you notice someone in distress with any of these signs or symptoms:
- skin is pale and clammy
- slowed or labored breathing
- confusion, inability to speak
- extreme lethargy
- fingernails or lips are purple or blue
- slow heartbeat
- unresponsive, unable to awaken
If someone’s heart stops beating, immediate CPR will be necessary to save their life. It is important to call your local emergency services right away. First responders will administer oxygen and begin monitoring the heart.
If a drug overdose is the cause of CNS depression, there are medications that can reverse these effects.
In a life-threatening situation, a drug called naloxone can reverse the toxic effects of an opioid overdose. It can be given intravenously, by injection, or nasal spray.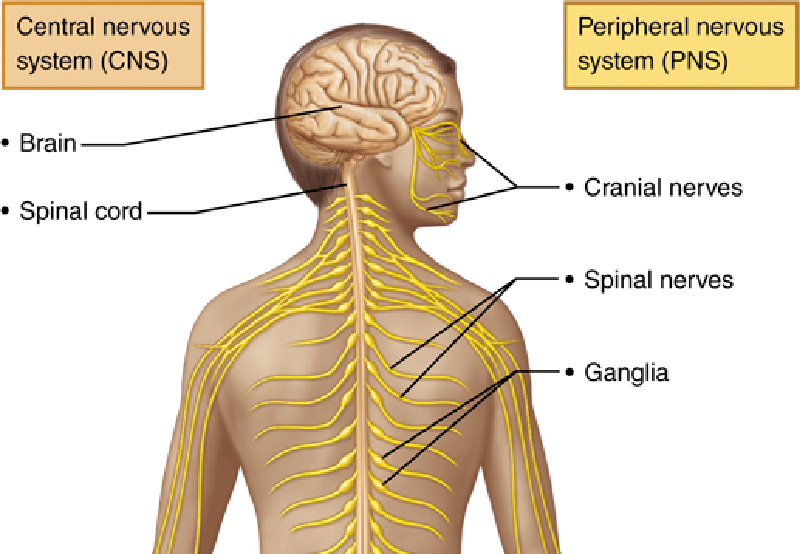
A drug called flumazenil can reverse the serious effects of benzodiazepines. It is administered intravenously.
To determine the cause of your CNS depression, your doctor will probably order a series of blood and urine tests. In many cases, they may also order a CT scan or MRI of the brain.
Once your CNS is back on track, you’ll need to address the source of the problem. If you have a condition that requires medication, you’ll need to follow your doctor’s instructions for care. If you’ve become addicted to alcohol or drugs, you’ll need to safely withdrawal from the chemicals and commit to long-term treatment for addiction.
The Healthline FindCare tool can provide options in your area if you need help finding a doctor.
If you are taking CNS depressant medications, some can be highly addictive. However, it can be dangerous to suddenly stop taking your prescription medications. If you’re concerned about your usage, talk to your doctor about how to taper off safely.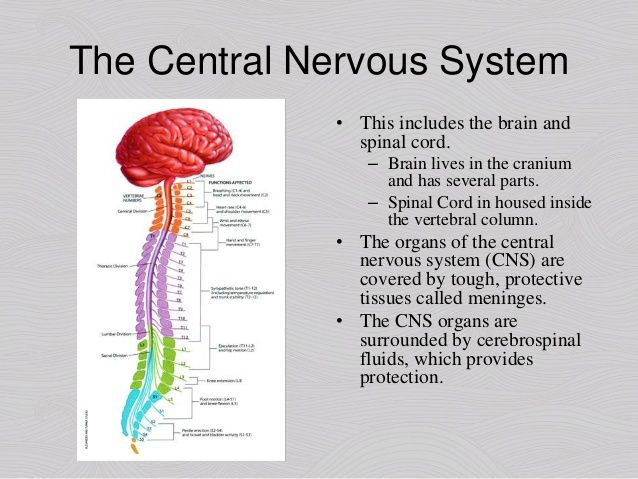
If you’ve ever had a substance abuse problem, you should continue to avoid alcohol and mediations that depress the CNS.
Prompt treatment of CNS depression offers the best chance of a full recovery. Delayed treatment can result in irreversible damage or death.
If you have a medical condition that puts you at risk for CNS depression, talk to your doctor. Discuss the best way to manage your health and how to recognize possible complications of your disease early on.
When your doctor prescribes a medication, make sure you understand its purpose and how long you’re expected to take it. Ask your doctor or pharmacist to explain the potential risks.
To lower the chances of CNS depression due to substances, follow these tips:
- Tell your doctor about other medications you take and any other medical conditions you have, including problems with addiction.
- Follow directions for taking your medications. Never increase the dose without consulting your doctor.
 Consult with your doctor when you want to stop taking the medication.
Consult with your doctor when you want to stop taking the medication. - When taking CNS depressants, don’t drink alcohol or take other medications that are also CNS depressants.
- Inform your doctor if you’re having troubling side effects.
Never share prescription medications with others. Store medicines, alcohol, and other potentially hazardous materials safely away from children and pets.
Keep reading: Lorazepam vs. Xanax: What’s the difference? »
Perinatal lesions of the central nervous system in Moscow - Central Clinical Hospital of the Russian Academy of Sciences
Section menu
Promotions
Contacts
Make an appointment
Leave your contact details to make an appointment
nine0016 I agree to the processing of personal dataApplication sent
Our specialists will contact you shortly
Latest news
Working hours of NCC No.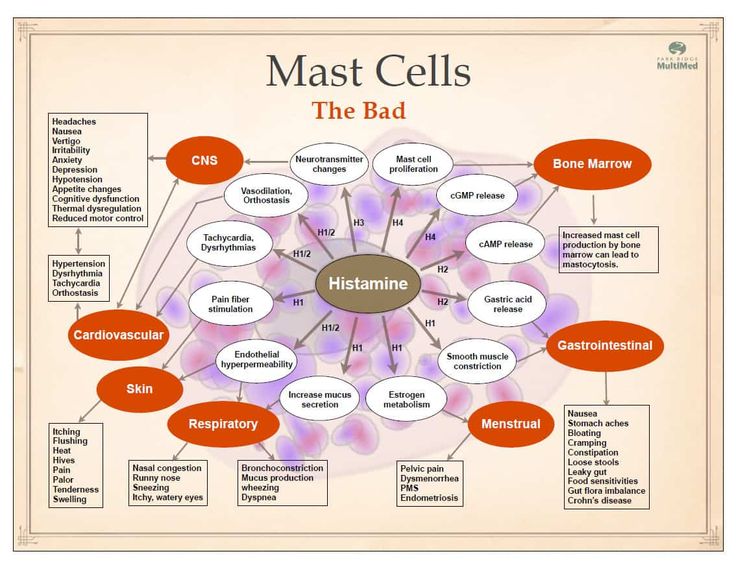 2 on holidays
2 on holidays
Publication date: 12/25/2022
Doctors of NCC No. 2 at the XII All-Russian Congress of Traumatologists and Orthopedists
Publication date: 12/22/2022
VIII Conference "Medical imaging in a multidisciplinary hospital" on the basis of NCC No. 2
Publication date: 12/20/2022
+7 (985) 134-83-11 (WhatsApp is open for applications)
Perinatal lesions of the central nervous system (PP CNS) or hypoxic-ischemic encephalopathy is a group of pathological conditions associated with brain damage in the perinatal period.
The main causes of PP CNS:
- Fetal hypoxia (chronic intrauterine; acute in childbirth) nine0011 Birth injury
- Intoxication (bilirubin encephalopathy)
- Hypoglycemia
- Infectious factor
Clinical manifestations of CNS PP
- Nervous system excitability syndrome: excessive and multiple movements, tremor of the chin, tongue, limbs, regurgitation, sleep disturbance (excessive wakefulness), spontaneous Moro reflex (spreading of the arms in the supine position)
- Syndrome of depression of the nervous system: decrease in spontaneous motor activity, short-term wakefulness, excessive sleep, weakness of the sucking reflex, insufficient emotional response when interacting with the child.
 nine0012
nine0012 - Syndrome of vegetative-visceral dysfunctions: thermoregulation disorders, transient cyanosis, disturbances in heart rate and respiratory rhythm, marbling of the skin, hypothermia of the extremities, vegetative-vascular spots on the skin, regurgitation, vomiting, unstable stool.
- Intracranial hypertension syndrome, hydrocephalic syndrome: excessive increase in head circumference, fontanelle bulging, head tilting back, loud monotonous crying (brain scream), head tilting back up to trunk arching (opisthotonus), persistent vomiting and regurgitation not associated with eating, increased sensitivity to sound stimuli (hyperesthesia), spontaneous bulging of the eyes (Gref's syndrome), difficulty falling asleep (wants to sleep, but cannot), short-term and superficial sleep, excitability. nine0012
- Convulsive syndrome: various sudden and repetitive contractions of the eyelids, facial muscles, abduction of the eyes, paroxysmal chewing, swallowing, sucking, sticking out of the tongue, swimming movements of the arms, pedaling, tonic tension of the trunk or limbs, single or group twitching of the muscles of the limbs, accompanied by convulsive movements eyes or "stopping" gaze, apnea.
- Dysregulation of muscle tone (muscle dystonia) increased, decreased, mixed muscle tone in the limbs, range of motion in the joints, spontaneous posture in sleep and wakefulness, position of the hands and feet, support during verticalization, head position during traction (pulling up) by the handles . nine0012
Outcomes and consequences of CNS PP
The consequences of PP CNS can be determined by the age of 1 year. Below are their main manifestations:
- Impaired motor development: delayed acquisition of head holding skills, coups, sitting, crawling, standing up, independent walking relative to the physical age of the child.
- Formation of paresis and paralysis of both one and several limbs (monoplegia, diplegia, hemiparesis, tetraparesis), which are related to various forms of cerebral palsy. nine0012
- Violation of psycho-speech development: delay in acquiring the skill of cooing, babble, the first words and phrases, the quality of the sounds uttered, the timing of the formation of pincer grip and pointing gesture, understanding of addressed speech, interest in surrounding objects and their intended use, the nature of the game, memorizing a new information, concentration of attention with the formation of attention deficit hyperactivity disorder.

- Violation of behavior and emotions: the timing of the formation of the animation complex, differentiation of relatives and strangers, emotional resonance, the degree of expression of emotions, communication with peers and adults, the possibility of playing together, the formation of skills of neatness, possibly leading to autism spectrum disorders. nine0012
- Hydrocephalus: excessive increase in head circumference, head deformity, pronounced saphenous veins in the temporal regions, signs of hypertension and hydrocephalus syndromes.
- Paroxysmal conditions of non-epileptic origin: affective-respiratory seizures, benign myoclonus of infancy (Fijerman's syndrome), benign neonatal sleep myoclonus, Sandiffer's syndrome, infantile torticolis, restless sleep, night terrors, rhythmic movements in sleep (rocking, shaking head, sucking thumb, gnashing of teeth). nine0012
- Age-related epileptic syndromes: early infantile epileptic encephalopathy (Otahara syndrome), early myoclonic encephalopathy, Dravet syndrome, West syndrome, benign neonatal epileptic syndromes, benign myoclonic epilepsy of infancy, benign partial epilepsy of infancy.

Instrumentation
In the CDC Research Institute of Pediatrics and Rehabilitation Treatment, instrumental diagnostics are carried out in order to clarify the diagnosis: nine0003
- Ultrasound of the brain (neurosonography)
- EEG of daytime sleep and wakefulness
- CT scan of the brain
- MRI of the brain and spine
Our help
Specialists from the Department of Developmental Neurobiology of the Research Institute of Pediatrics and Health Protection of the Central Clinical Hospital of the Russian Academy of Sciences work on the basis of the CDC:
- Diagnosis, monitoring and treatment are carried out by experienced neurologists, PhDs with 20 years of experience in this problem. Our specialists are the authors of the book "Modern neurobiological aspects of perinatal lesions of the CNS", published by the Russian Academy of Sciences. nine0012
- Defectologists and clinical psychologists are involved in the diagnosis to help clarify the presence of developmental disorders.
 Development assessment is carried out according to unified development tables.
Development assessment is carried out according to unified development tables. - If necessary, children can receive specialized treatment and correctional, developing classes with specialists in early development, aimed at stimulating sensory, visual, auditory, tactile, coordinating functions.
- It is possible to comprehensively monitor children with perinatal CNS damage with the involvement of qualified specialists, candidates of medical sciences. nine0012
- Accompanying an experienced pediatrician who will answer all questions about care, nutrition, prevention of rickets and SARS, hardening.
- Vaccination department: consultation of a vaccinologist-immunologist in order to draw up an individual vaccination schedule and direct vaccination under his supervision.
- Involvement of any other pediatric specialists, including orthopedists and ophthalmologists.
Perinatal lesions of the central nervous system / Articles of specialists / Family clinic "Tanar"
What are perinatal lesions of the central nervous system?
Perinatal lesions of the central nervous system (CNS) is a general term for neurological distress in newborns from a variety of causes.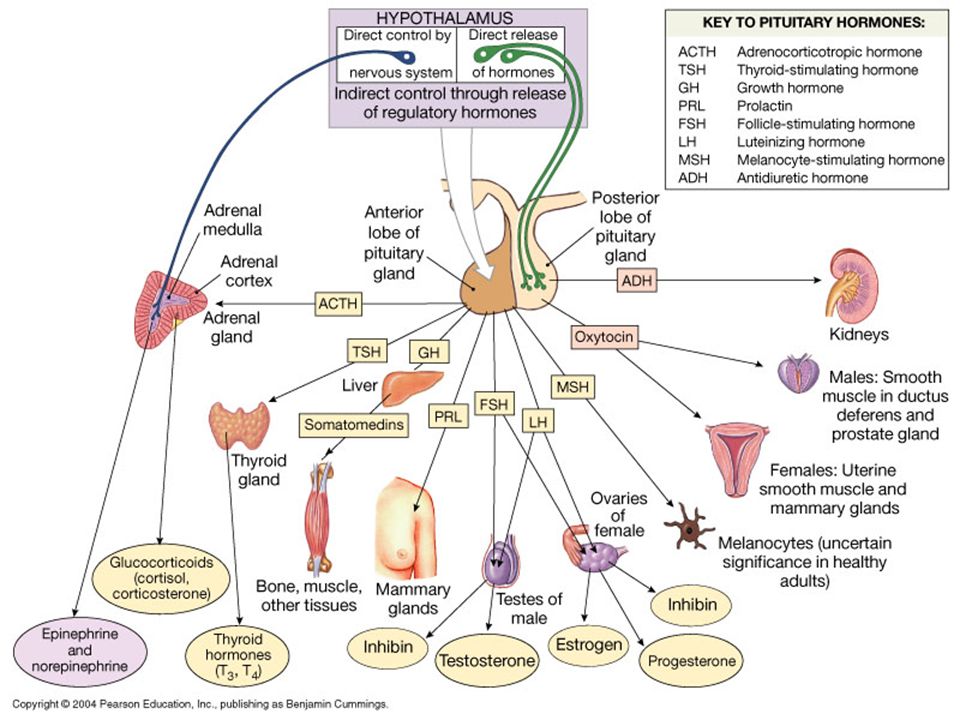
How common are perinatal lesions of the central nervous system?
Between 5 and 55% of children in their first year of life receive this diagnosis, since this number sometimes includes children with mild transient disorders of the nervous system. Severe forms of perinatal CNS lesions are observed in 1.5-10% of full-term and 60-70% of premature babies. nine0003
Why do perinatal lesions of the central nervous system occur?
The main cause of perinatal damage to the CNS in the fetus and newborn is hypoxia (oxygen deficiency), which occurs under the influence of various factors. Unfavorable conditions for the development of the fetus in the womb can be laid long before the onset of pregnancy due to various diseases in a teenage girl, a future mother. Infectious and non-infectious diseases, hormonal disorders, bad habits, occupational hazards during pregnancy cause increased hypoxia of the unborn child. Previous abortions lead to impaired blood flow between the mother and fetus and, consequently, to intrauterine hypoxia. An important role in the development of perinatal lesions of the central nervous system is played by sexually transmitted infections (chlamydia, herpes, syphilis). The cause of acute asphyxia in childbirth can be various violations of the normal course of labor, rapid or protracted labor, incorrect position of the umbilical cord loops. Mechanical trauma to a child rarely leads to perinatal damage to the central nervous system (especially the brain). The risk of trauma to the child and acute asphyxia increases if the birth takes place outside a medical facility, including during childbirth in the water. In premature babies, due to their immaturity, perinatal damage to the central nervous system is observed more often. nine0003
An important role in the development of perinatal lesions of the central nervous system is played by sexually transmitted infections (chlamydia, herpes, syphilis). The cause of acute asphyxia in childbirth can be various violations of the normal course of labor, rapid or protracted labor, incorrect position of the umbilical cord loops. Mechanical trauma to a child rarely leads to perinatal damage to the central nervous system (especially the brain). The risk of trauma to the child and acute asphyxia increases if the birth takes place outside a medical facility, including during childbirth in the water. In premature babies, due to their immaturity, perinatal damage to the central nervous system is observed more often. nine0003
Are perinatal lesions of the central nervous system dangerous?
Severe perinatal brain lesions (including intracranial hemorrhage, severe cerebral ischemia) pose a real threat to the life and health of the child, even with timely provision of highly qualified medical care in a perinatal center. Moderate and mild forms of brain damage do not pose an immediate threat to life, but they can cause mental disorders and the development of motor activity in a child. nine0003
Moderate and mild forms of brain damage do not pose an immediate threat to life, but they can cause mental disorders and the development of motor activity in a child. nine0003
How do perinatal lesions of the central nervous system manifest themselves?
Features of disorders in perinatal lesions of the central nervous system depend on the nature of brain damage (hemorrhage in various brain structures, ischemia, infectious lesions), their severity, the degree of maturity of the child, the stage of the disease.
For example, in premature babies with severe brain damage, general deep depression prevails with respiratory failure, sometimes with short-term convulsions. In full-term newborns, both depression and increased excitability (motor restlessness, irritated cry), prolonged convulsions are possible. By the end of the first month of a child's life, lethargy, apathy can be replaced by increased excitability, muscle tone increases (muscles are too tense), an incorrect position of the limbs (clubfoot, etc.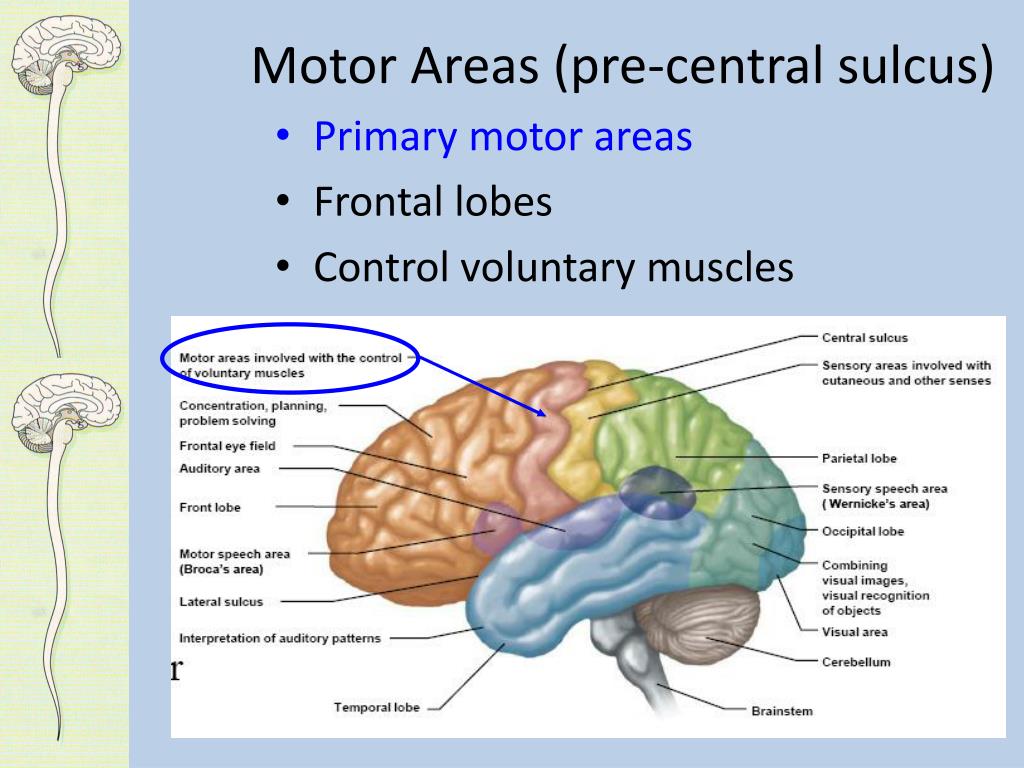 ) is formed. In addition, the development of internal or external dropsy of the brain (hydrocephalus) is possible. The manifestations of a spinal cord injury depend on the location and extent of the lesion. For example, if the cervical spinal cord or nerve plexuses are affected, “obstetric paralysis” occurs - sagging or inactivity of the arm on the affected side. nine0003
) is formed. In addition, the development of internal or external dropsy of the brain (hydrocephalus) is possible. The manifestations of a spinal cord injury depend on the location and extent of the lesion. For example, if the cervical spinal cord or nerve plexuses are affected, “obstetric paralysis” occurs - sagging or inactivity of the arm on the affected side. nine0003
With moderate brain damage, vegetative-visceral manifestations may predominate: persistent regurgitation, delayed or increased stools, bloating, thermoregulation disorders (the body's response to heat and cold), pallor and marbling of the skin, lability of the cardiovascular and respiratory systems, and etc.
In children with severe perinatal lesions of the central nervous system, already from the end of the first month of life, a delay in the development of the psyche and movements is noted: the reaction to communication is a sluggish, monotonous cry (emotionally uncolored). Perhaps early (at 3-4 months) the formation of persistent motor disorders of the type of cerebral palsy. nine0003
nine0003
It should be noted that moderate (and sometimes severe) lesions of the central nervous system may be asymptomatic and manifest at 2-3 months of life. Parents should be alerted by insufficient physical activity or its excess, bouts of unreasonable anxiety, lack of a clear reaction to sounds and visual stimuli in a full-term baby older than 2 weeks, as well as a stable (habitual) position of the body with a turn to one side, crossing the legs in an upright position, support “on tiptoe”, persistent tilting of the head, bulging or pulsating fontanel, divergence of cranial sutures, habitual strabismus or rolling of the eyes (symptom of the “setting sun”). nine0003
How is perinatal damage to the central nervous system diagnosed?
The diagnosis is based on the data of a medical examination, anamnestic data and is confirmed by instrumental studies. Of great importance is an ultrasound examination (ultrasound) of the brain with an assessment of the state of its vessels (Dopplerography). If necessary, X-ray examination of the skull, spine, computed tomography (CT), magnetic resonance imaging (MRI) is used. nine0003
If necessary, X-ray examination of the skull, spine, computed tomography (CT), magnetic resonance imaging (MRI) is used. nine0003
What methods of treatment and prevention of perinatal lesions of the central nervous system exist?
In the acute period, severe perinatal brain lesions are treated in the neonatal intensive care unit. First of all, they eliminate disturbances in the work of the respiratory, cardiovascular systems and metabolic disorders, eliminate convulsions (if necessary, carry out artificial ventilation of the lungs, intravenous infusions, parenteral nutrition). Next, the newborns are transferred to a special department, where they continue individual treatment depending on the nature and severity of brain damage: anticonvulsants are used, dehydration drugs are used in developing hydrocephalus, as well as drugs that stimulate capillary growth and improve nutrition of damaged brain tissues. The same drugs, as prescribed by a neurologist, can be used during the first year of life in repeated courses.