Depression disability benefit
SAMHSA’s National Helpline | SAMHSA
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.
Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders.
This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative. Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs. In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems. Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.
Addresses concerns of children of parents with substance use/abuse problems.It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt. Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse. Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.
For additional resources, please visit the SAMHSA Store.
Last Updated: 08/30/2022
SAMHSA Behavioral Health Treatment Services Locator
HomeWelcome to the Behavioral Health Treatment Services Locator, a confidential and anonymous source of information for persons seeking treatment facilities in the United States or U.S. Territories for substance use/addiction and/or mental health problems.
PLEASE NOTE: Your personal information and the search criteria you enter into the Locator is secure and anonymous. SAMHSA does not collect or maintain any information you provide.
Please enter a valid location.
please type your address
-
FindTreatment.
 gov
gov Millions of Americans have a substance use disorder. Find a treatment facility near you.
-
988 Suicide & Crisis Lifeline
Call or text 988
Free and confidential support for people in distress, 24/7.
-
National Helpline
1-800-662-HELP (4357)
Treatment referral and information, 24/7.
-
Disaster Distress Helpline
1-800-985-5990
Immediate crisis counseling related to disasters, 24/7.
- Overview
- Locator OverviewLocator Overview
- Locator OverviewLocator Overview
- Finding Treatment
- Find Facilities for VeteransFind Facilities for Veterans
- Find Facilities for VeteransFind Facilities for Veterans
- Facility Directors
- Register a New FacilityRegister a New Facility
- Register a New FacilityRegister a New Facility
- Other Locator Functionalities
- Download Search ResultsDownload Search Results
- Use Google MapsUse Google Maps
- Print Search ResultsPrint Search Results
- Use Google MapsUse Google Maps
- Icon from Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers).
 Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers).
Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers). - Icon from Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers). Find programs providing methadone for the treatment of opioid addiction (heroin or pain relievers).
The Locator is authorized by the 21st Century Cures Act (Public Law 114-255, Section 9006; 42 U.S.C. 290bb-36d). SAMHSA endeavors to keep the Locator current. All information in the Locator is updated annually from facility responses to SAMHSA’s National Substance Use and Mental Health Services Survey (N-SUMHSS). New facilities that have completed an abbreviated survey and met all the qualifications are added monthly. Updates to facility names, addresses, telephone numbers, and services are made weekly for facilities informing SAMHSA of changes. Facilities may request additions or changes to their information by sending an e-mail to [email protected], by calling the BHSIS Project Office at 1-833-888-1553 (Mon-Fri 8-6 ET), or by electronic form submission using the Locator online application form (intended for additions of new facilities).
Updates to facility names, addresses, telephone numbers, and services are made weekly for facilities informing SAMHSA of changes. Facilities may request additions or changes to their information by sending an e-mail to [email protected], by calling the BHSIS Project Office at 1-833-888-1553 (Mon-Fri 8-6 ET), or by electronic form submission using the Locator online application form (intended for additions of new facilities).
FGBNU NTsPZ. ‹‹Depression in General Medicine: A Guide for Physicians››
Depressive states are the most common form of mental pathology in patients seeking help in general medical institutions, both outpatient and hospital networks.
According to modern estimates, the proportion of depression in patients of this contingent ranges from 10 [Katon W., Sulliven M. D., 1990] to 22-33% [Shmaonova L. M., Bakalova E. A., 1998; Ustun T. V., Sartorius N., 1995; Lyketsos C. G. et al, 1999].
Among elderly and senile patients who visit the territorial polyclinic, patients with depression make up 17. 4% [Zozulya T.V., 1998].
4% [Zozulya T.V., 1998].
Among the outpatients of the neurological clinic, as evidenced by the data of S. Kirk and M. Saunders (1997), when examining 2716 patients, affective disorders are found in 17% of cases.
When studying an approximately equal sample size (1927 patients of a psychiatric office of one of the territorial polyclinics of Moscow), the proportion of depressive disorders was 38.2% of the identified mental pathology. Reactive depressions predominate - 28.1% (of which 18.9% mild and 9.2% moderately severe), the remaining 10.1% are shallow endogenous depressions within the framework of cyclothymia [Shmaonova L.M., Bakalova E.A., 1998].
As a result of our [Smulevich A. B. et al., 1999] on the basis of a territorial polyclinic of a continuous clinical and epidemiological examination of 495 patients who applied to a local therapist, it was found that depressive disorders in the aggregate occur in 21.5% of cases.
In economically developed countries (Sweden, Spain, USA, Australia, Japan, etc. ), the frequency of depressive states in patients in a somatic hospital who applied for psychiatric counseling is comparable to the above indicator and reaches 20-29% [Ruskin P. E., 1985; Pauser H. et al., 1987; Al-Ansari E. A. et al., 1990; Hattori T. et al., 1990; Bertolo L D. et al., 1996].
), the frequency of depressive states in patients in a somatic hospital who applied for psychiatric counseling is comparable to the above indicator and reaches 20-29% [Ruskin P. E., 1985; Pauser H. et al., 1987; Al-Ansari E. A. et al., 1990; Hattori T. et al., 1990; Bertolo L D. et al., 1996].
Endogenous depressions (38.5%) and dysthymia (33.8%) predominate, accounting for 2/3 of depressive disorders (72.3%).
The third place in frequency is occupied by vascular depressions - 16.9%, which coincides with the data of T. M. Siryachenko and N. M. Mikhailova (1998), according to which the frequency of vascular depressions in geriatric outpatient practice (specialized psychiatric office of the Moscow polyclinic) is 14 %.
Psychogenic depressions account for 10.8% (of which 6.2% are nosogenic and 4.6% are reactive).
According to the data of a continuous clinical and epidemiological survey of 921 patients of a large multidisciplinary hospital in Moscow [Smulevich A. B. et al., 1999], the frequency of depressive disorders approximately corresponds to the indicators obtained in the territorial polyclinic: every fifth (20.5%) patient suffers from depression.
B. et al., 1999], the frequency of depressive disorders approximately corresponds to the indicators obtained in the territorial polyclinic: every fifth (20.5%) patient suffers from depression.
In contrast to the outpatient contingent, psychogenic depressions are most common here. Their share is more than half (59.3%) of all depressive conditions. This part of depressive disorders is represented mainly by nosogenic depressions (45%), while reactive depressions associated with other psycho-traumatic effects were detected in 14.3% of patients.
Dysthymia accounts for about 1/5 of cases of depressive states (21.2%).
Endogenous depressions (cyclothymia) are much less common - 13.8%, and vascular depressions are at least - only 5.7%.
Analysis of the ratio of depressive disorders of various origins with somatic diseases reveals the following dependencies (Table 4).
Table 4
Correlation between the form (nosological affiliation) of depression and the diagnosis of a somatic disease
| Nosological affiliation of depression |
Diagnosis of a somatic disease | Patients with depression (% of the total number of patients diagnosed with this disease) |
| Psychogenic nosogenic* | myocardial infarction | 39 |
| eye injury | 38. | |
| Mallory-Weiss syndrome | 38 | |
| Acute peritonitis | 37 | |
| Systemic scleroderma | 34 | |
| Lung cancer | 33 | |
| Pancreas cancer | 33 | |
| primary tuberculosis | 33 | |
| Severe concomitant injury | 27 | |
| ENT Cancer | 33 | |
| Rectal cancer | 25 | |
| prostate cancer | 25 | |
| Chronic circulatory failure | 17 | |
| Chronic ischemic heart disease | 7 | |
| chronic colitis | 43 | |
| Osteochondrosis of the thoracic spine | 27 | |
| Osteochondrosis of the cervical spine | eighteen | |
| Type II diabetes | fourteen | |
| Chronic gastritis | 12 | |
| Cholelithiasis | 7 | |
| Residual effects after cerebrovascular accident | eight | |
| Congestive chronic circulatory failure | 7 | |
| chronic pneumonia | 7 | |
| Emphysema | 7 | |
| Encephalopathy | b |
* Reactive depressions due to other (non-nosogenic) psychotraumatic effects are evenly distributed across all categories of somatic diseases .
Among psychogenic depressions, nosogenic depressions (45% of all depressive disorders) are significantly more common in patients with severe, life-threatening or disabling somatic diseases. Such depressions are detected in more than 30 patients who have had a myocardial infarction, patients with oncological pathology (lung cancer, pancreatic cancer) and systemic connective tissue diseases, as well as in people with primary tuberculosis. The frequency of nosogenic depressions is quite high (37.5%) in patients with acute surgical pathology requiring urgent surgical intervention (acute peritonitis, Mallory-Weiss syndrome), as well as in patients with severe concomitant trauma (27%) and traumatic lesions of the organs of vision ( 38.5%).
At the same time, reactive depressions, which make up 14.3% of all depressions in the studied sample, do not show preference in relation to any individual forms of pathology of the internal organs. This, apparently, is explained by the fact that, unlike nosogenic depressions, reactive depressions are not directly related to somatic suffering and are caused by events related to family life or work.
Dysthymic disorder, which occurs in 22.1% of patients suffering from depression in a somatic hospital, is associated with protracted somatic diseases and occurs with a frequency of up to 25-30% in cancer patients (cancer of the rectum, ENT organs, prostate), less often (17 %) in chronic circulatory failure and even less frequently (7%) in chronic ischemic heart disease.
Endogenous depressions (13.8% of all depressions in the study sample) show a significant relationship with gastroenterological and neurological pathology. This type of depressive disorder is more common in patients with the main diagnoses of chronic colitis (43%), chronic gastritis (12%), cholelithiasis (7%). The frequency of endogenous depressions in patients diagnosed with osteochondrosis of the thoracic and cervical spine is 27 and 18%, respectively. Similar indicators for this pathology are also given by other researchers. Some authors believe that these calculations reflect an inadequately broad diagnosis of somatic pathology (osteochondrosis, colitis), but in reality we are talking about symptoms of depression that occurs with somatic algic and functional disorders. In our opinion, it is more adequate to consider the discussed ratios in connection with the negative impact of an affective disorder on the somatic state of the patient - with the manifestation of depression, the symptoms of diseases such as chronic gastritis, chronic colitis worsen, pain in patients with spinal osteochondrosis aggravates, which necessitates more intensive care and, accordingly, seeking inpatient care.
In our opinion, it is more adequate to consider the discussed ratios in connection with the negative impact of an affective disorder on the somatic state of the patient - with the manifestation of depression, the symptoms of diseases such as chronic gastritis, chronic colitis worsen, pain in patients with spinal osteochondrosis aggravates, which necessitates more intensive care and, accordingly, seeking inpatient care.
Vascular depressions (5.7% of all depressions in the studied sample) are significantly more often associated with diseases associated with impaired blood supply to the brain (residual effects after acute disorders of cerebral circulation - 8%, dyscirculatory encephalopathy - 6%, congestive chronic circulatory failure - 7% ). Vascular depression has a similar frequency (7%) also in patients with chronic lung diseases (chronic pneumonia, emphysema) accompanied by cerebral hypoxia. It should also be emphasized that vascular depressions are more common in neurological and cardiological clinics.
The data obtained generally confirm the results of other studies. The calculations given by the authors depend on the nature of the clinical manifestations and the characteristics of the course of the disease. It has been shown that with a high frequency of depression, reaching 20-25%, in patients with oncological diseases, in general [Plumb B., Holland J., 1977; Kathol R. et al, 1990] this indicator depends on the localization of the malignant neoplasm: with the greatest frequency, depressive disorders are detected in patients with pancreatic cancer and lung cancer [Holland J. C., 1986; Green A., Austin S., 1993; Passik S. D., Breitbart W., 1996; Zabora J. R. et al., 1996]. According to the results of our own study [Smulevich A. B. et al., 1999], in these forms of cancer, nosogenic depression prevails, the frequency of which reaches 33%, while dysthymic depressions are more typical for patients with prostate and colon cancer (25% ). The risk of developing depression increases in proportion to the duration of the oncological disease, the degree of maladjustment, the severity of the pain syndrome and other symptoms of cancer [Derogatis L. R. et al., 1983; Bukberg J. et al., 1984]. If the prevalence of depression in women is revealed in the population (in a ratio of 2: 1), then in oncological practice these disorders are approximately equally distributed among both sexes [DeFlorio M. L, Massie M. J., 1995].
R. et al., 1983; Bukberg J. et al., 1984]. If the prevalence of depression in women is revealed in the population (in a ratio of 2: 1), then in oncological practice these disorders are approximately equally distributed among both sexes [DeFlorio M. L, Massie M. J., 1995].
A number of diseases of the digestive system are also associated with an increased frequency of depressive disorders. These include, in particular, Crohn's disease and ulcerative colitis [Addolorato G. et al, 1997]. The highest frequency of comorbid depressive states in the so-called functional gastrointestinal disorders. Thus, in irritable bowel syndrome, the lifetime prevalence of depression reaches 60-70% [Walker E. et al., 1990; Tollefson G. et al., 1991]. A high frequency of depressive disorders has also been established for other variants of functional disorders of the gastrointestinal tract (GIT) - functional dyspepsia, gallbladder dysfunction, etc. [Drossman A. D. et al., 1994]. In such cases, endogenous (cyclothymic) and chronic (dysthymia) depressions predominate, the frequency of which reaches 60% (a joint study of the Department for the Study of Borderline Mental Pathology and Psychosomatic Disorders of the RAMS Scientific Center for Health and Psychology and the Laboratory of Chronobiology and Clinical Gastroenterology of the Russian Academy of Medical Sciences) [Komarov F. I. et al. ., 1999].
I. et al. ., 1999].
The frequency of depressive disorders in patients with acquired immunodeficiency syndrome (AIDS), as already mentioned, is at least 20% of the number of corporatized [May M., 1996]. The value of this indicator may depend on several factors (the psycho-traumatic content of information about the incurability of the infection, its progressive, disabling course), the importance of which increases due to the young age of patients and the negative attitude towards the AIDS patient of family members, colleagues and society as a whole.
We have received statistically significant confirmation of the adverse effect of depression of various origins on the adaptation of somatically ill patients, as already partly discussed in the introduction. The proportion of disabled people of groups I and II in terms of somatic disease with comorbid depression significantly exceeds the corresponding indicator for the studied sample as a whole.
Given in table. 5 differentiated data make it possible to verify that relatively more severe and prolonged vascular and endogenous depressions are especially unfavorable for the patient's adaptation to the manifestations of a somatic disease: when they are added to a somatic disease, the probability of disability in group 2 almost doubles (45.5 and 46.2% respectively, against 20.4% of patients of group 2 in the studied sample as a whole). The least favorable prognosis for working capacity in vascular depression, when almost 9times more often disability of the 1st group is registered (9.1% versus 0.9% in the general sample).
5 differentiated data make it possible to verify that relatively more severe and prolonged vascular and endogenous depressions are especially unfavorable for the patient's adaptation to the manifestations of a somatic disease: when they are added to a somatic disease, the probability of disability in group 2 almost doubles (45.5 and 46.2% respectively, against 20.4% of patients of group 2 in the studied sample as a whole). The least favorable prognosis for working capacity in vascular depression, when almost 9times more often disability of the 1st group is registered (9.1% versus 0.9% in the general sample).
Table 5. Correlation of depression with disability due to somatic disease in patients of a large multidisciplinary hospital, % ( n = 921)
| Physical disability | The proportion of disabled people with depression of various origins | For the entire sample | ||||
| Psychogenic | Vascular | Endogenous | Dysthymia | |||
| nosogenic | reactive | |||||
| I group | 1. | 3.7* | 9.1* | 0 | 2.5* | 0.9 |
| II group | 31.8* | 37.0* | 45.5* | 46.2* | 17.5 | 20.4 |
* Significantly higher than in the studied sample as a whole (p < 0.05) .
It can also be seen that reactive depressions also have a negative impact on the performance and adaptation of somatic patients. Disability is more severe when physical illness and reactive depression occur in connection with the same event (eg, myocardial infarction and depression due to a family tragedy). Such psychosomatic diseases are especially difficult - the frequency of registration of disability in group II increases from 20 to 37%, and in group I - from 0.9up to 3.7%.
Disability is more severe when physical illness and reactive depression occur in connection with the same event (eg, myocardial infarction and depression due to a family tragedy). Such psychosomatic diseases are especially difficult - the frequency of registration of disability in group II increases from 20 to 37%, and in group I - from 0.9up to 3.7%.
We also note the significant role of nosogenic depressions, in which group II disability due to a somatic disease is registered more often than in patients without depression (31.8 versus 20%). However, in comparison with reactive nosogenic depressions, they have a less severe and protracted course, and therefore the proportion of patients with group I disability among patients with nosogenic depressions does not differ from that in the studied sample as a whole.
How to get disability for depression in Israel
How to get disability for depression in Israel
- Post author: Lawyer in Israel
- The entry was published by: November 23, 2021
- Post category: Disability / Claims for insurance
“I have severe depression, can I get a disability?”. This question is no longer a rarity. With the advent of the corona period, there is a trend towards an increase in the number of people suffering from depression. So, let's look at what depression is, what are its signs and symptoms. How to get disability for depression and how to apply for disability benefits in Israel.
This question is no longer a rarity. With the advent of the corona period, there is a trend towards an increase in the number of people suffering from depression. So, let's look at what depression is, what are its signs and symptoms. How to get disability for depression and how to apply for disability benefits in Israel.
Depression, its signs and symptoms
Depression is a mental disorder characterized by low mood and loss of the ability to enjoy anything. Most often this is manifested by a depressed and dreary mood. Anxiety and panic disorders. Another sign of depression can be indifference to the outside world and a decrease in interest in everything that happens.
Depressive conditions are not only related to a person's mood.
There are several types of depression depending on the severity:
- postpartum depression
- seasonal depression
- mild depression
- clinical depression (MDD).
Depression can be the result of somatic diseases, taking any drugs, psychological trauma, an accident or microtrauma at work. Pregnancy and childbirth are also considered risk factors for depression.
Pregnancy and childbirth are also considered risk factors for depression.
Moreover, depression can be manifested both by psychological symptoms and expressed at the physical level.
A person with severe depression may experience motor and mental retardation.
People suffering from severe depression are unable to perform many types of work. For example, they cannot perform physically demanding work, work that requires a high degree of concentration and responsibility. With such a diagnosis, work is contraindicated, for example, with vulnerable segments of the population, for example, with the disabled, the elderly and young children.
Depression Disability Filing
Often, those who are dealing with severe depression are reluctant to file for disability. Even in the case when they are entitled to a disability due to depression. Someone is embarrassed by disability or thinks that disability is a stamp about disability for life.
Do not be afraid of disability. After all, if you cannot work to the fullest, then you cannot provide for yourself. And disability will allow you to receive the payments due to you in this difficult situation.
After all, if you cannot work to the fullest, then you cannot provide for yourself. And disability will allow you to receive the payments due to you in this difficult situation.
Disability due to depression is initially given as temporary. If your condition improves, it will be canceled.
You get a lot of benefits with your disability. In the case of more than 40% mental disability, a person is entitled to receive a rehabilitation basket (sal shikum).
Depression disability refers to a mental disability. But compared to those who suffer from psychotic illnesses, such as schizophrenia or other syndromes, it is much more difficult for a person with depression to prove that he is entitled to a disability.
Receipt of mental disability benefits
Documents for registration of disability for depression are the same as for general disability. This is the standard procedure for filing a disability claim with certain modifications.
To start the procedure, you need:
- Obtain medical certificates.

 5
5 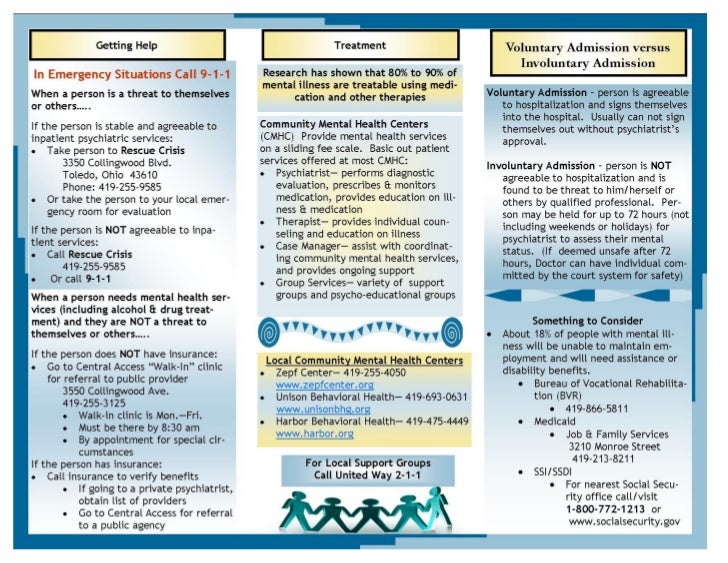 2
2