Depression alcoholism treatment
What are the treatment options for comorbid alcohol abuse and depressive disorders?
Alcohol, probably one of the oldest mood-enhancing drugs discovered by humans, can induce depression. Levels of serotonin (5-HT) and its metabolites are low in some brain regions of alcohol-preferring rats and in the cerebrospinal fluid of people with alcohol dependence. Enhancing 5-HT neurotransmission reduces alcohol consumption in rats; in humans this intervention sometimes lessens depression and may contribute to the treatment of alcohol abuse.
A careful history is the first step, to establish chronology, category of depression and subtype of alcohol abuse.
Determining the relative chronology of alcoholism and depression is important. Most people with alcohol dependence who enter treatment, for instance in randomized trials, have high scores on depression rating scales. These ratings typically decline after a few weeks of either abstinence or normalized consumption. Therefore, the diagnosis of comorbid depression, and any associated treatment plan, must be withheld during this period, to determine if depressive symptoms are secondary to the alcohol abuse.
In cases where the depressive symptoms are primary, alcoholism has often developed in the course of attempts at self-medication. In this situation, the category of depression (e.g., dysthymia, major depression, bipolar disorder, subsyndromal mood disturbance) must be determined.
Finally, the subtype of alcohol dependence or abuse must be identified, as this information is important for treatment planning. Type I alcohol dependence is typically of late onset, occurring in both men and women with no family history of alcohol or other drug abuse, and no familial or personal antisocial traits. However, more psychosocial factors are involved, and the prognosis is better than for type II dependence. Type II alcohol dependence is typically of early onset and occurs mostly in men with a family history of alcoholism, more severe progression of the disorder, and personal and familial antisocial traits; response to treatment is generally poorer than for type I.
Once comorbidity of alcoholism and depression has been clearly established, 2 symptoms of the depressive spectrum require special attention. The risk of suicide among people with both conditions is higher than among people who do not abuse alcohol. Suicide is often impulsive and facilitated by intoxication. Insomnia occurring in these patients may last for months after they initiate abstinence and is a predictor of relapse.
The risk of suicide among people with both conditions is higher than among people who do not abuse alcohol. Suicide is often impulsive and facilitated by intoxication. Insomnia occurring in these patients may last for months after they initiate abstinence and is a predictor of relapse.
Alcohol dependence has as its essential characteristic impaired control over the use of alcohol and occurs because of changes in synaptic plasticity within the pathway underlying craving. The neurobiologic concomitants of depression contribute to this impairment and increase the risk of relapse.
Several modes of pharmacologic treatment are available:
Naltrexone, a mu receptor antagonist, reduces craving by attenuating the rewarding effects of alcohol. Its results are somewhat inconsistent.
Acamprosate (recently approved by the US Food and Drug Administration) blocks negative craving due to abstinence. Beneficial effects in preventing relapse have been consistent in many large studies.

Selective serotonin reuptake inhibitors are more effective for the depressive component than for alcohol consumption. They seem to improve outcome by treating the underlying depression rather than by changing drinking behaviour per se.
In addition, special mention must be made of ondansetron (16 μg/kg twice daily), a 5-HT3 antagonist, for the more “biologic” subtype of alcoholism (type II above). It has influenced favourably both depressive symptoms and alcohol consumption in several studies, in particular when combined with naltrexone. The duration of treatment must be left to the clinician's judgement, as it has not been specified in the published clinical trials. Interestingly, ondansetron has no significant effect in type I alcoholism, which is usually more accessible to psychosocial treatments.
Psychosocial and psychotherapeutic approaches — always provided in conjunction with pharmacologic therapy — include cognitive–behavioural therapy, which has proven effective for both depression and alcohol dependence, and the general strategies of motivational interviewing, which maximize the chances of lasting results.
Maurice Dongier, MD
Department of Psychiatry McGill University Douglas Hospital Research Centre Montréal, Que.
To submit questions for this regular feature, please send them to the Journal of Psychiatry & Neuroscience, CMA Media Inc., 1867 Alta Vista Dr., Ottawa ON K1G 3Y6, Canada; fax 613 729-9545; [email protected]. Please include details of any relevant case and your name, address, telephone and fax numbers as well as your email address.
The information in this column is not intended as a definitive treatment strategy but as a suggested approach for clinicians treating patients with similar histories. Individual cases may vary and should be evaluated carefully before treatment is provided.
Competing interests: None declared.
The Connection & Dual Treatment Near Me
Can drinking alcohol cause depression and, conversely, can depression lead to misusing alcohol? If you or someone you care about are struggling with depression and alcohol abuse, you may be interested in learning more about how alcohol can play a role in depression and vice versa, as well as the different factors that can affect alcohol, depression, and addiction.
Simultaneous treatment for alcohol use disorder and a depressive disorder can help you or your loved one take back control of your mental health, physical wellbeing, and overall happiness. Know that you’re not alone and help is available.
Ways to Get in Contact With Us
If you believe you or someone you love may be struggling with addiction, let us hear your story and help you determine a path to treatment.
There are a variety of confidential, free, and no obligation ways to get in contact with us to learn more about treatment.
- Call us at
- Verify Your Insurance Coverage for Treatment
Understanding Depression
Everyone feels blue or down from time to time, and people often say that they feel “depressed” during these temporary bouts of sadness. But clinical depression isn’t just a matter of feeling the occasional ups and downs or periodic sadness caused by issues of daily life.
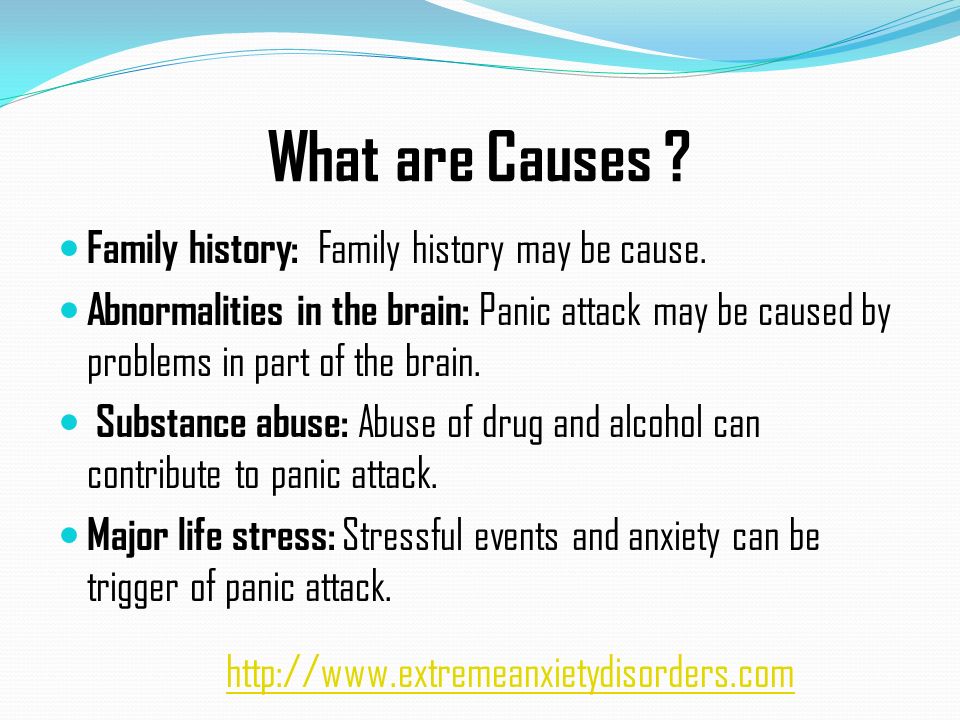
Major depressive disorder, persistent depressive disorder, and other depressive disorders are treatable mental health disorders that are characterized by symptoms of sadness, emptiness, or irritable mood that affects a person’s body and mind, specifically the ability to function. Although researchers have identified several risk factors for depressive disorders, they can occur in anyone. Not everyone who experiences risk factors will develop a depressive disorder, but risk factors can play a role in its development. These risk factors include:1,2,3,4,5
Although researchers have identified several risk factors for depressive disorders, they can occur in anyone. Not everyone who experiences risk factors will develop a depressive disorder, but risk factors can play a role in its development. These risk factors include:1,2,3,4,5
- Genetics and heritability. Genes are not destiny, but a family history of depression is considered a risk factor. First-degree family members of individuals with major depressive disorder have a risk two- to four-times higher than the general population.
- Biological factors and illness. This includes your physical health, such as having a serious illness like cancer, diabetes, or heart disease, as well as your levels of neurotransmitters (brain chemicals), which can become imbalanced and influence depression.
- Stress, major life changes, and exposure to trauma. Any of these can be a risk factor, but particularly if you experienced them in childhood.

- Taking certain medications. Some of the side effects of medications can cause or contribute to depressive symptoms.
- Low socioeconomic status. While socioeconomic status can play a role at any point in your lifespan, it can be a particular risk factor early in life.
- Using illicit substances or alcohol. Different substances can increase your risk of developing depression.
Signs and Symptoms of Depression
To be diagnosed with major depressive disorder or another depressive disorder, people typically need to display symptoms almost every day for at least 2 weeks. The symptoms are severe enough that they cause significant stress and impairment in social, occupational, or other important areas of functioning.5 While the specific types of depressive disorders can look a bit different, they tend to share common symptoms that include:1,5,6
- A persistent low mood, feelings of sadness, and/or feeling anxious or empty.

- Feeling hopeless or pessimistic.
- Irritability, frustration, or restlessness.
- Feeling excessively or inappropriately guilty, worthless, or helpless.
- Losing interest or pleasure in activities or hobbies you once enjoyed.
- A lack of energy or fatigue.
- Moving or talking more slowly than usual.
- Difficulty thinking, remembering, or making decisions.
- Changes in sleep, such as trouble falling or staying asleep (insomnia) or sleeping more than usual (hypersomnia).
- Changes in appetite with significant weight loss or weight gain (e.g., a change of more than 5% of body weight).
- Having thoughts of self-harm, death, or suicide, or making suicidal attempts.
- Aches, pains, headaches, cramps, or digestive problems that aren’t easily explainable and do not improve with treatment.
How Alcohol Abuse Can Factor into Depression
Can alcohol cause depression or vice versa? Research has shown that there seems to be a bidirectional relationship between alcohol use disorder (AUD) and depressive disorders; both disorders can exist together, each disorder increases the risk for the other disorder, and each disorder can worsen the other. 7 Regardless of the order of which came first, AUD or a depressive disorder, both issues are among the most prevalent psychiatric disorders and co-occur often.7,8,9,10
7 Regardless of the order of which came first, AUD or a depressive disorder, both issues are among the most prevalent psychiatric disorders and co-occur often.7,8,9,10
Are you in need of substance abuse and co-occurring mental health treatment? Plenty of American Addiction Centers locations across the nation offer specialized co-occurring disorder treatment. Call our admissions navigators today to discover your treatment options.
The pathways leading to the development of co-occurring AUD and a depressive disorder are complex and intertwined. Some individuals may be genetically susceptible to both. For others, symptoms of a depressive disorder can influence the development of an AUD. One possible contributor to cooccurrence is that people may alleviate symptoms of a depressive disorder with substances like alcohol. People who experience major depressive symptoms may start to rely on alcohol to ease their symptoms and feel better, but over time, this can develop into a full-blown alcohol use disorder. 10 Even in instances where a person doesn’t develop an AUD, self-medication may not be helpful long-term, as it is associated with increased psychiatric comorbidity, higher stress levels, and lower health-related quality of life.3,10 Research also has associated AUD with a risk not only for the onset of depressive symptoms but also depressive disorders.
10 Even in instances where a person doesn’t develop an AUD, self-medication may not be helpful long-term, as it is associated with increased psychiatric comorbidity, higher stress levels, and lower health-related quality of life.3,10 Research also has associated AUD with a risk not only for the onset of depressive symptoms but also depressive disorders.
It’s important to note that the co-occurrence of AUD and depressive disorders, specifically major depressive disorder and persistent depressive disorder, is associated with greater severity and worse prognosis than either disorder alone. This includes a heightened risk for suicidal behavior.7
It’s a vicious pairing that can be difficult to overcome, however, treatment can be effective.
Can Alcohol Make Depression Worse?
Yes, alcohol can exacerbate depression and depressive symptoms. In addition, a clinical review in the journal, Professional Psychology: Research and Practice explains that drinking can interfere with recovery from depression. Depressed study participants who were heavy drinkers displayed worse outcomes from depression treatment; furthermore, even mild to moderate amounts of alcohol appeared to worsen depression, with depressed patients who drank low levels of alcohol (less than 1 oz per day) experiencing worse outcomes from pharmacological treatments.13
Depressed study participants who were heavy drinkers displayed worse outcomes from depression treatment; furthermore, even mild to moderate amounts of alcohol appeared to worsen depression, with depressed patients who drank low levels of alcohol (less than 1 oz per day) experiencing worse outcomes from pharmacological treatments.13
Alcohol use disorders may be more prevalent in people who also have depression than they are in the general population. The occurrence of alcohol use disorder and a depressive disorder are associated with greater severity and a worse prognosis for both disorders.
How Long Does Alcohol-Induced Depression Last?
The duration of alcohol-induced depression can vary widely. Generally speaking, depressive symptoms associated with alcohol-induced depression have been shown to improve significantly after you’ve abstained from alcohol for a certain amount of time, typically 3-4 weeks in many cases.11 However, research also suggests that substance-induced depression can turn into independent depression should symptoms of depression persist following cessation of alcohol or other substances of abuse.
Take Our “Am I an Alcoholic?” Self-Assessment
Take our free, 5-minute “Am I an Alcoholic?” self-assessment below if you think you or someone you love might be struggling with an alcohol use disorder (AUD). The evaluation consists of 11 yes or no questions that are intended to be used as an informational tool to assess the severity and probability of an AUD. The test is free, confidential, and no personal information is needed to receive the result.
Treatment for Co-Occurring Depression and Alcohol Use Disorder
Treatment often includes an integrated approach to simultaneously address both alcohol use disorder and depression..
Many treatments can help co-occurring depression and AUD. Some of these can include:14,15,16
- Detox. This is usually the first step in the recovery process followed by entry into a formal drug rehabilitation program. Detox helps you safely and comfortably withdraw from alcohol.
- Antidepressants/Medications.
 You may receive antidepressants, which can help treat both the depression and some symptoms of AUD. In addition, you may receive naltrexone, a medication that helps people stop drinking and reduces depressive symptoms, disulfiram, which is used as an alcohol deterrent (it causes unpleasant symptoms if you drink alcohol), or acamprosate, which is used to help maintain abstinence from alcohol.
You may receive antidepressants, which can help treat both the depression and some symptoms of AUD. In addition, you may receive naltrexone, a medication that helps people stop drinking and reduces depressive symptoms, disulfiram, which is used as an alcohol deterrent (it causes unpleasant symptoms if you drink alcohol), or acamprosate, which is used to help maintain abstinence from alcohol. - Behavioral therapies. These can include:
- Cognitive-Behavioral Therapy (CBT). This helps you learn positive coping mechanisms to replace the thought and behavioral patterns that can contribute to or worsen AUD and depression.
- Dialectical Behavior Therapy (CBT). This is mainly used to help reduce self-harm and suicidal behavior.
- Behavioral Activation. This is a type of behavioral therapy that is effective for both AUD and depression. It involves developing an understanding of how negative life experiences and behaviors influence your mood and emotions and encourages you to take an active approach to increase your positive life experiences.

- Mutual support groups, which include 12-step groups like Alcoholics Anonymous (AA) and non-12-step groups like SMART Recovery. These groups are effective both as treatment and as aftercare for both AUD and depression. You’ll benefit from the support of others who know what it’s like to be in your shoes, which can lessen feelings of isolation and help you feel connected.
Find Drug and Alcohol Treatment Centers Near You
Other Frequently Asked Questions Regarding Alcohol & Depression
References
- National Institute of Mental Health. (2018). Depression.
- Çakıcı, M., Gökçe, Ö., Babayiğit, A., Çakıcı, E., & Eş, A. (2017).
- Kaltenboeck, A. & Harmer, C. (2018). The neuroscience of depressive disorders: A brief review of the past and some considerations about the future. Brain and Neuroscience Advances, 2.
- Kwong, A., López-López, J. A., Hammerton, G., Manley, D…& Pearson, R.
 M. (2019). Genetic and Environmental Risk Factors Associated With Trajectories of Depression Symptoms From Adolescence to Young Adulthood. JAMANetwork Open, 2(6), e196587.
M. (2019). Genetic and Environmental Risk Factors Associated With Trajectories of Depression Symptoms From Adolescence to Young Adulthood. JAMANetwork Open, 2(6), e196587. - American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing.
- Obeid, S., Akel, M., Haddad, C., Fares, K…& Hallit, S. (2020).
- McHugh, R. K., & Weiss, R. D. (2019). Alcohol Use Disorder and Depressive Disorders. Alcohol research : current reviews, 40(1), arcr.v40.1.01. https://doi.org/10.35946/arcr.v40.1.01.
- National Institute of Mental Health. (2021). Depression.
- Fergusson, D. M., Boden, J. M., & Horwood, L. J. (2009). Tests of causal links between alcohol abuse or dependence and major depression. Archives of general psychiatry, 66(3), 260–266.
- Turner, S., Mota, N., Bolton, J., & Sareen, J. (2018).
 Self-medication with alcohol or drugs for mood and anxiety disorders: A narrative review of the epidemiological literature. Depression and anxiety, 35(9), 851–860.
Self-medication with alcohol or drugs for mood and anxiety disorders: A narrative review of the epidemiological literature. Depression and anxiety, 35(9), 851–860. - American Society for Addiction Medicine (ASAM) Principles of Addiction Medicine, Sixth Edition (2 hard copies in our department library. Online access available—ask Scot for login credentials)
- Nunes EV, Liu X, Samet S, Matseoane K, Hasin D. Independent versus substance-induced major depressive disorder in substance-dependent patients: observational study of course during follow-up. J Clin Psychiatry. 2006 Oct;67(10):1561-7. doi: 10.4088/jcp.v67n1010. PMID: 17107247.
- Ramsey, S. E., Engler, P. A., & Stein, M. D. (2005). Alcohol Use Among Depressed Patients: The Need for Assessment and Intervention. Professional Psychology: Research and Practice, 36(2), 203–207.
- McHugh, R. K., & Weiss, R. D. (2019). Alcohol Use Disorder and Depressive Disorders.
 Alcohol Research: Current Reviews, 40(1), arcr.v40.1.01.
Alcohol Research: Current Reviews, 40(1), arcr.v40.1.01. - National Institute on Drug Abuse. (2020). Common Comorbidities with Substance Use Disorders Research Report: What are the treatments for comorbid substance use disorder and mental health conditions?
- National Alliance on Mental Illness. (2020). Substance Use Disorders.
- National Institute on Alcohol Abuse and Alcoholism. (2008). Genetics of Alcohol Use Disorder.
- National Alliance on Mental Illness. (2021). Medication Frequently Asked Questions.
Last Updated on Sep 15, 2022
Alcoholic depression - symptoms, causes, diagnosis and treatment of alcoholic depression
Article reviewed by an expert:
MAKE AN APPOINTMENT
Alcoholic depression is an affective disorder that occurs in people suffering from alcoholism. Usually lasts from 2 weeks to 1 month. The maximum severity of symptoms is usually observed during the development of withdrawal symptoms. This condition often occurs after an exit from alcoholic psychosis, it can also develop during periods of binges and remissions. It is accompanied by a decrease in mood, longing, a feeling of guilt, uselessness and uselessness. Suicidal thoughts and actions are possible. The diagnosis is exposed on the basis of the anamnesis and clinical manifestations. Treatment is drug therapy combined with psychotherapy.
The maximum severity of symptoms is usually observed during the development of withdrawal symptoms. This condition often occurs after an exit from alcoholic psychosis, it can also develop during periods of binges and remissions. It is accompanied by a decrease in mood, longing, a feeling of guilt, uselessness and uselessness. Suicidal thoughts and actions are possible. The diagnosis is exposed on the basis of the anamnesis and clinical manifestations. Treatment is drug therapy combined with psychotherapy.
Alcoholic depression - what is it?
Depression in alcoholism was described by Bleuler in 1920 under the name "alcoholic melancholia". Subsequent studies have confirmed both the presence of specific depressive and subdepressive conditions in alcoholics, and the complex, diverse links between alcoholism and depressive disorders. The frequency of development of the disease and the severity of symptoms directly correlates with the duration and severity of alcoholism. Middle-aged and elderly patients suffer from a depressive disorder more often than younger ones. Most of the patients are people over 40 years of age.
Middle-aged and elderly patients suffer from a depressive disorder more often than younger ones. Most of the patients are people over 40 years of age.
The average duration of post-alcoholic depression in alcoholism ranges from 2 weeks to 1 month. In severe cases, symptoms may persist for a year or more. The duration of the disease depends on the psycho-emotional characteristics, character traits, features of the constitution and the state of the body of patients. Women suffer more often than men, but in men, depression is more severe and is more often complicated by suicide attempts. The aggravation of male depression is facilitated by the fact that the representatives of the stronger sex rarely seek medical help during the development of the disease. Treatment of depression in alcoholism is carried out by specialists in the field of narcology, psychotherapy and psychiatry.
Causes of alcohol depression
Depression in alcoholism is a multifactorial disease. A whole range of circumstances leads to its development, including changes in general metabolism, disruption of brain receptors, personality changes, characteristic mental and somatic disorders, uncontrolled craving for alcohol, withdrawal phenomena when drinking alcohol is stopped, social and domestic problems. Narcologists constantly have to deal with alcoholic depression that develops in various clinical situations.
A whole range of circumstances leads to its development, including changes in general metabolism, disruption of brain receptors, personality changes, characteristic mental and somatic disorders, uncontrolled craving for alcohol, withdrawal phenomena when drinking alcohol is stopped, social and domestic problems. Narcologists constantly have to deal with alcoholic depression that develops in various clinical situations.
Alcoholic depression is part of the symptom complex of deprivation syndrome, acute alcohol intoxication, binge drinking and uncontrolled craving for alcohol. The most common cause of depressive mental disorder in alcoholics is withdrawal symptoms. Mental suffering of patients is provoked by severe physical and psychological discomfort and social problems, combined with a pathological need for alcohol.
Several bouts of depression occur in patients undergoing treatment for alcoholism in specialized clinics. In the initial stages of therapy, such patients develop a "sobriety phobia" - a pronounced fear of the possibility of life without alcohol. This stage is accompanied by a kind of mourning, due to the loss of alcohol. The second wave of depression is usually observed before the discharge of patients from the hospital, at the stage when the person no longer suffers from the consequences of intoxication. Longing for alcohol and psychological problems come to the fore.
This stage is accompanied by a kind of mourning, due to the loss of alcohol. The second wave of depression is usually observed before the discharge of patients from the hospital, at the stage when the person no longer suffers from the consequences of intoxication. Longing for alcohol and psychological problems come to the fore.
Sometimes depressive disorders develop against the background of remission, when a person feels lost, unable to fit in, “fallen out” of the normal rhythm of life and social environment, suffering from changes in habitual patterns of behavior, forced to solve numerous problems that arose during the period of alcoholism, without having enough external support and internal reserves. Such depressions can cause a breakdown and further alcoholization of the patient.
It should be borne in mind that the premorbid background is of some importance in the development of alcoholism. Even before the start of alcohol consumption, many patients have an increased tendency to mood swings, the development of asthenic conditions, depressive neurosis, subdepression and all kinds of borderline disorders. As alcoholism develops, this tendency is aggravated and aggravated due to secondary psycho-emotional and personality changes. There are also complications and neurosis after a complete rejection of alcohol.
As alcoholism develops, this tendency is aggravated and aggravated due to secondary psycho-emotional and personality changes. There are also complications and neurosis after a complete rejection of alcohol.
Symptoms and differential diagnosis of alcohol depression
Symptoms of depression in alcoholism are usually mild. Severe affective disorders are relatively rare. The mood is constantly depressed, the patient suffers from a feeling of emptiness and meaninglessness of existence. There is a feeling of loss of colors, the emotional colorlessness of the world, characteristic of depressive disorders. This perception causes depression and anxiety. Anhedonia develops - a person loses the ability to rejoice, cannot enjoy.
Psychological changes are combined with motor and intellectual retardation. Gait and movements slow down, the voice becomes quiet, monotonous. Mimic diversity disappears, the patient's face almost constantly retains a sad expression. The patient is in a state of inactivity for a significant part of the time, responds to questions with a delay, has difficulty trying to understand someone else's thought or instruction. It is difficult for him to think and formulate statements.
The patient is in a state of inactivity for a significant part of the time, responds to questions with a delay, has difficulty trying to understand someone else's thought or instruction. It is difficult for him to think and formulate statements.
Hallucinations and delusions are usually absent. Often there are overvalued ideas of one's own guilt, uselessness, uselessness, fatal inadequacy and inadequacy. There is a tendency to self-abasement and self-accusation. The future looks bleak, hopeless, unpromising. Some patients consider some of their own previous actions as a serious crime. Many patients have thoughts of suicide, suicide attempts are possible. Sometimes (mainly in older patients) alcoholic depression is combined with increased anxiety.
Alcoholic depression is differentiated from other depressive disorders and conditions that include individual symptoms of depression. Unlike a depressive disorder, "drunken grief" is not accompanied by a sense of the colorlessness of the world and the loss of the ability to feel a variety of emotions. This state arises on an "emotional wave" and passes within a few hours, occasionally - several days.
This state arises on an "emotional wave" and passes within a few hours, occasionally - several days.
Separate elements of depression are often observed in withdrawal syndrome, but, unlike real alcoholic depression, they disappear after abstinence from drinking alcohol for 1-3 days. Reactive depression on the background of alcoholism in patients develops against the background of severe traumatic events (death of a relative, divorce, etc.); with alcoholic depression, there are no such events in the recent past of patients. Alcohol intake can provoke an exacerbation of other mental illnesses (psychogenic depression, depressive phase of bipolar affective disorder), therefore, when affective symptoms appear in patients with alcoholism, a thorough history taking is necessary.
Treatment and prognosis for alcoholic depression
Treatment of depression in alcoholism is carried out in a narcological hospital. In the process of treatment, drugs, psychotherapy and non-drug methods are used. Patients are prescribed antidepressants for alcoholism (usually SSRIs, tricyclic antidepressants, or MAO inhibitors). With increased anxiety and sleep disorders, short-term courses of drug therapy and treatment with the use of hypnotics and tranquilizers (diazepam, phenazepam, tazepam, etc.) are carried out. In parallel, they carry out detoxification therapy and provide psychological assistance.
Patients are prescribed antidepressants for alcoholism (usually SSRIs, tricyclic antidepressants, or MAO inhibitors). With increased anxiety and sleep disorders, short-term courses of drug therapy and treatment with the use of hypnotics and tranquilizers (diazepam, phenazepam, tazepam, etc.) are carried out. In parallel, they carry out detoxification therapy and provide psychological assistance.
With early detection and timely hospitalization, the prognosis for alcoholic depression in most cases is relatively favorable. Single depressive episodes, as a rule, quickly stop, suicidal intentions disappear, working capacity is restored (if it was not impaired due to other diseases). However, if the patient continues to drink alcohol, these conditions may recur and worsen as alcoholism develops.
Antidepressants in the treatment of alcoholism
Alcoholism is classified as a socially significant disease with numerous adverse medical and social consequences.![]() The most dramatic consequence of alcohol abuse is alcohol-associated mortality, which annually causes millions of deaths around the world, hundreds of thousands of which are the deaths of young, relatively healthy people [9].
The most dramatic consequence of alcohol abuse is alcohol-associated mortality, which annually causes millions of deaths around the world, hundreds of thousands of which are the deaths of young, relatively healthy people [9].
Among the features of alcohol dependence that have an adverse effect on the course of alcoholism is frequent comorbidity with affective disorders. The frequency of comorbid depression reaches 30% in men who abuse alcohol, and 60-70% in women suffering from alcohol dependence [3, 5].
It is believed that in the "alcoholism-depression" pair, the development of each disease doubles the risk of the other, and the ability of the first of them to contribute to the onset of the second is more proven than vice versa [2]. Repeated heavy drinking increases the likelihood of developing depressive episodes (estimated at 40%), associated suicidal thoughts and attempts, as well as severe anxiety and insomnia [20].
Alcohol abuse increases the risk of suicide associated with major depressive disorder (MDD), especially in women, and marks an increased risk of suicide during pregnancy [3, 8].
Signs of alcohol abuse in the study of autopsy material of those who died due to depression are detected more often than in cases of death without an indication of affective disorders [23].
The complexity of the problem of depressive states in alcoholism lies in the fact that they often remain unrecognized, especially in older patients.
The high frequency of comorbidity of alcohol dependence and depression is usually explained, among other reasons, by the insufficient activity of serotonin (as well as dopamine, norepinephrine and other neurotransmitters), which is characteristic of both diseases [5]. It is believed that serotonergic dysfunction in alcoholism is associated with two factors: congenital disorders of serotonin activity and metabolism and changes in serotonergic processes due to alcohol abuse [18].
Serotonergic dysfunction (congenital or acquired), as well as associated comorbid mental disorders - depression and other psychopathological conditions - justifies the use of antidepressants in the treatment of alcoholism.
Citalopram and other selective serotonin reuptake inhibitors (SSRIs) indicated a decrease in alcohol consumption in alcohol dependent individuals (especially in combination with depressive disorders) in 90s of the last century [12, 13].
In a study of alcohol abusers and healthy volunteers [5], the former showed severe serotonergic dysfunction, manifested by a prolonged decrease in prolactin levels in response to the action of escitalopram and citalopram.
Successful treatment of alcohol dependence means reducing the mortality of the population, increasing the length and quality of life of alcoholics, and alleviating the overall burden of the disease for the individual, his family and society.
Currently, most authorities agree that the goals of alcohol dependence treatment include not only the complete cessation of alcohol consumption (which is most attractive, but unfortunately unattainable for most patients), but also the reduction of the severity of the disease with less alcohol consumption. , a decrease in the number of days of heavy drinking, a decrease in the amount of alcohol consumed and the prevention of binges or a reduction in their duration [6, 10, 17, 19].
, a decrease in the number of days of heavy drinking, a decrease in the amount of alcohol consumed and the prevention of binges or a reduction in their duration [6, 10, 17, 19].
Due to the impossibility of completely stopping the use of alcohol by many people suffering from alcohol dependence, treatment for alcoholism is often supportive rather than anti-relapse.
Diversification of treatment goals with the possibility of partial cessation of alcohol consumption (“controlled consumption”) allows the inclusion in treatment programs of patients who are not ready for complete sobriety and refuse treatment focused on the cessation of alcohol consumption in any quantities. Flexibility in setting the goals of anti-alcohol therapy means the possibility of a significant increase in its overall effectiveness [20].
Treatments for alcohol dependence with proven clinical efficacy include disulfiram, naltrexone and acamprosate. These drugs are included in the WHO treatment standards and are widely used in clinical practice in European and other countries.
In addition to the triad of anti-alcohol therapy, in the treatment of alcohol dependence, as already mentioned above, antidepressants can be used, and primarily SSRIs, of which escitalopram is a promising representative. Escitalopram exhibits the highest serotonin reuptake selectivity of the entire SSRI group, which is determined by a strong bond with the serotonin transporter and the virtual absence of interaction with other neurotransmission systems and receptors [7].
A notable feature of escitalopram, which determines its high efficiency in combination with the selectivity of action and a favorable tolerability profile, is also the dual nature of the effect on serotonergic transmission [7, 11].
The clinical efficacy and tolerability of escitalopram determine the priority of its choice in the treatment of depression, panic attacks and a number of other borderline mental disorders.
Based on data from several double-blind, randomized, placebo-controlled trials with clinical follow-up of 8 weeks, escitalopram 10 or 20 mg has a marked superiority over placebo in reducing the symptoms of major depressive disorder (MDD), as assessed using a scale Montgomery-Asberg - MADRS (Montgomery-Asberg Depression Rating Scale), Hamilton scales - HAM-D (Hamilton Rating Scale for Depression) and scales of general clinical impression - CGI [22].
A comparative evaluation of the efficacy and safety of 12 modern antidepressants (citalopram, escitalopram, fluoxetine, paroxetine, duloxetine, reboxetine, fluvoxamine, sertraline, milnacipran, mirtazapine, venlafaxine and bupropion) in the treatment of MDD was presented by A. Cipriani et al. [4] in a systematic review based on a meta-analysis of 117 randomized clinical trials conducted in 1991-2007. involving 25,928 patients. The authors found that mirtazapine, escitalopram, venlafaxine, and sertraline were significantly superior in efficacy to duloxetine, fluoxetine, fluvoxamine, paroxetine, and reboxetine, with sertraline showing the least significant benefit compared to the other three drugs. It is noted that escitalopram and sertraline are better tolerated than paroxetine and duloxetine; citalopram, escitalopram and sertraline are better tolerated than fluvoxamine; escitalopram is better tolerated than fluoxetine; Reboxetine is less well tolerated than other antidepressants. Based on the data obtained, the authors concluded that escitalopram is superior to other antidepressants both in terms of efficacy (second only to mirtazapine) and tolerability, is a first-line drug in the treatment of moderate and severe depression, and in this capacity can be compared with it. few other medicines.
Based on the data obtained, the authors concluded that escitalopram is superior to other antidepressants both in terms of efficacy (second only to mirtazapine) and tolerability, is a first-line drug in the treatment of moderate and severe depression, and in this capacity can be compared with it. few other medicines.
Escitalopram is characterized by a rapid onset of clinical effects (individual components of its action appear within 1-2 weeks) with an early and distinct difference from placebo [22].
Long-term (up to 52 weeks) follow-up demonstrates the superiority of escitalopram over placebo in reducing the frequency of relapses of depression and the frequency of remission [22].
Escitalopram has been proven effective in severe depression. In a 24-week MADRS study, escitalopram 20 mg was more effective than paroxetine 40 mg in the treatment of major depressive disorders, with the difference in favor of escitalopram increasing in parallel with the increase in the severity of the initial manifestations of depression. Similarly, an 8-week study demonstrated a greater reduction in symptoms of major depression with escitalopram 20 mg compared with venlafaxine 225 mg, with the difference being greater the more severe the initial affective disturbances were [21].
Similarly, an 8-week study demonstrated a greater reduction in symptoms of major depression with escitalopram 20 mg compared with venlafaxine 225 mg, with the difference being greater the more severe the initial affective disturbances were [21].
According to other data [11], compared to venlafaxine, escitalopram is characterized by an accelerated onset of action, a more pronounced ability to achieve early stable remission and better tolerability.
The clinical effects of escitalopram are largely determined by the polymorphism of the serotonin transporter gene. Significantly more significant reduction in symptoms of depression according to MADRS in LL genotype compared with SS/SL genotype was shown when escitalopram was prescribed to persons suffering from MDD in combination with alcohol dependence [15].
Like other serotonergic antidepressants, escitalopram is used in the treatment of anxiety disorders. A significant reduction in the symptoms of generalized anxiety disorder, social anxiety disorder and panic disorder under the influence of escitalopram was noted in double-blind, randomized, placebo-controlled trials with the drug for 8-12 weeks [22].
SSRIs (particularly fluoxetine, fluvoxamine, and citalopram) reduce alcohol consumption by alcoholics by 10-70% [16], and this effect may not necessarily be associated or not at all associated with the antidepressant effect of drugs [14] .
E.M. Krupitsky et al. [1] conducted a double-blind, randomized, placebo-controlled study of the effectiveness of a 12-week course of treatment with escitalopram in 60 people suffering from alcohol dependence in combination with depression during the period of remission of alcoholism. Symptoms of depression and anxiety were assessed on the basis of MADRS, HAM-D, the Tsung scale and the Spielberger-Khanin scale, alcohol craving was assessed using a number of diagnostic tools, including the Pennsylvania scale. The authors noted a decrease in symptoms of depression according to MADRS compared with baseline values during 4-13 weeks of treatment in patients of the main group who received escitalopram, while when patients in the control group received placebo, an improvement was observed only by 7. 9, 12 and 13 weeks. In accordance with the HAM-D in the main group, the symptoms of depression decreased by the 4th week and remained at a consistently low level throughout the entire observation period; in the control group, they decreased by the 5th week and were below the initial values only during the 8th and 10-13th weeks. There was also a difference in the rate of reduction of depression on the Zung scale: the severity of affective disorders was lower than the initial values during weeks 4–13 in the main group and during weeks 6 and 11–13 in the control group.
9, 12 and 13 weeks. In accordance with the HAM-D in the main group, the symptoms of depression decreased by the 4th week and remained at a consistently low level throughout the entire observation period; in the control group, they decreased by the 5th week and were below the initial values only during the 8th and 10-13th weeks. There was also a difference in the rate of reduction of depression on the Zung scale: the severity of affective disorders was lower than the initial values during weeks 4–13 in the main group and during weeks 6 and 11–13 in the control group.
Significant differences were also observed in the reduction of anxiety: in the main group, anxiety significantly differed from the initial values at the 4-13th week, in the control group - only at the 12-13th week; the level of anxiety in the main group was significantly lower than in the control group from 5 to 11 weeks of observation.
A difference was also shown in the dynamics of craving for alcohol, assessed according to the Pennsylvania scale: in the main group, the desire to drink alcohol significantly decreased at 5-13 weeks of the study, while in the control group it also gradually decreased, but without statistically significant differences from the baseline. values.
values.
In terms of treatment outcomes, in the study group, 10 patients completed treatment in remission, 10 relapsed, 9 discontinued for other reasons; in the control group, remission was noted in 5 patients, 20 relapsed, 6 people stopped treatment for other reasons [1].
E.M. Krupitsky et al. [1], suggests that escitalopram demonstrates a marked superiority over placebo in reducing the symptoms of depression and anxiety, as well as a pronounced ability to reduce craving for alcohol, increase the degree of completion of treatment programs and the frequency of remission of alcoholism.
Thus, the altered profiles of serotonergic processes in alcohol abusers and the high incidence of comorbid mental disorders and alcoholism determine the importance of antidepressants (including SSRIs) in the treatment of alcohol dependence complicated by depressive and anxiety disorders.
Pharmacological properties and research data allow us to consider escitalopram one of the most promising drugs for the treatment of alcohol dependence, combined with depression and anxiety.