Bipolar and vitamin deficiency
How Vitamin D Helps With Bipolar Depression
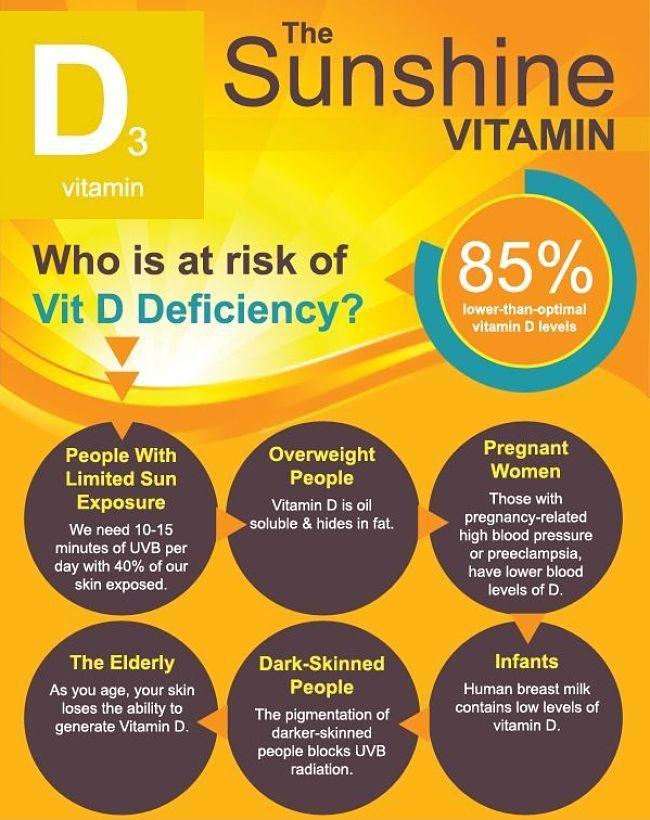
Many people are vitamin D deficient due to poor diet or a lack of daily sun exposure. Recent research has found a correlation between low vitamin D levels and neuropsychiatric illness. Specifically, it has been noted that vitamin D deficiency has been found to be associated with bipolar depression. With this new information comes the assertion that an increase in vitamin D levels can decrease symptoms associated with bipolar depression.
Vitamin D is a fat-soluble vitamin responsible for regulating cells and the immune system. It also works with calcium to promote strong bones. Foods like milk, salmon, eggs, and fortified cereal are good sources of vitamin D, and getting enough sunlight ensures that vitamin D will be absorbed into the body.
Vitamin D deficiency is quite common in many people, but has a higher occurrence in those with dark skin, and occurs when intake levels are too low. This is most commonly caused by a lack of sunlight, however it can also be caused by poor diet as well. Vitamin D deficiency can cause weak bones, muscle weakness, and bone pain.
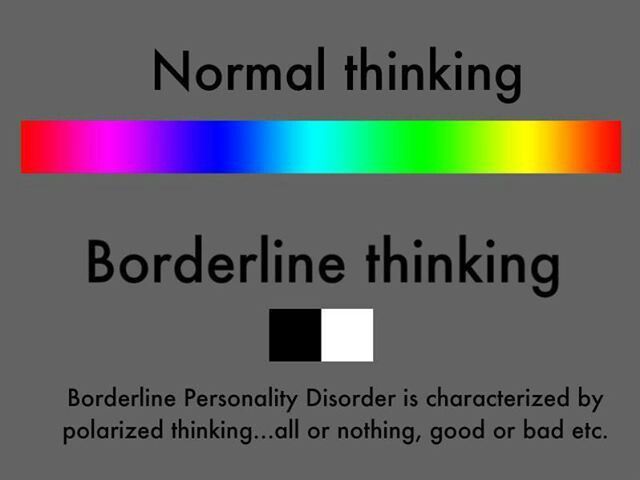
Bipolar disorder is defined by periods of mania and depression, and bipolar depression is the name given to the depressive state that occurs. Bipolar depression is similar to unipolar depression, however it does have one main difference and that is those suffering from bipolar depression have intermittent highs caused by their manic episodes. Simply stated, bipolar disorder is the occurrence of major depression combined with manic episodes lasting at least one week.
Vitamin D has been found to be involved in neurological processes such as nerve growth factor enhancement and neurotransmitter synthesis regulation. Regulating neurotransmitters like dopamine, adrenaline, and noradrenaline are important in the process of mood regulation and mood disorder treatment. It has also been found that those individuals with depression, including bipolar depression, have been found to also be vitamin D deficient. It is also interesting to note that populations at risk for vitamin D deficiency, including the elderly, adolescents, obese individuals, and those with chronic illnesses, are all the same populations that have a higher risk of depression.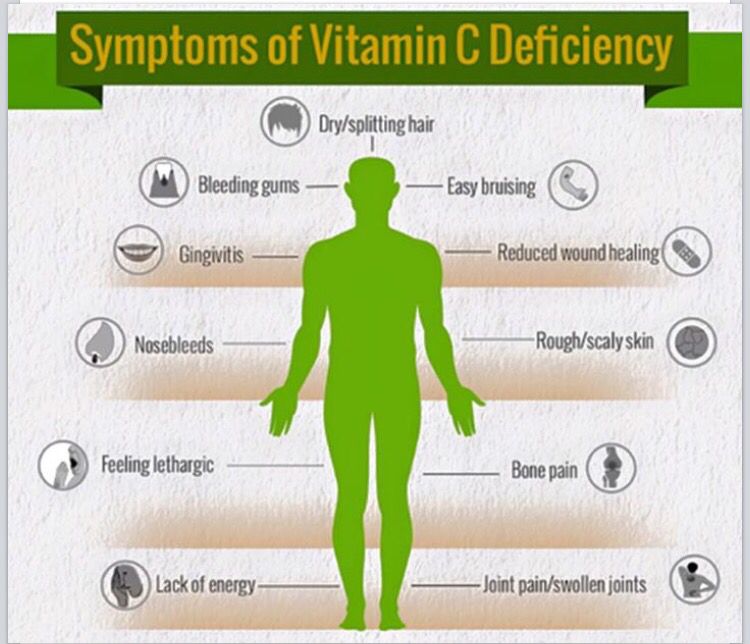
Although there is no current research exclusively stating that vitamin D can improve symptoms of depression, there have been several trends noticed that reaffirm the notion that vitamin D does, in fact, affect neuro pathways and can affect mood in a positive way. Even though the specific link between vitamin D and mood improvement is not clear, it is nevertheless recommended to increase levels of vitamin D in patients with bipolar depression.
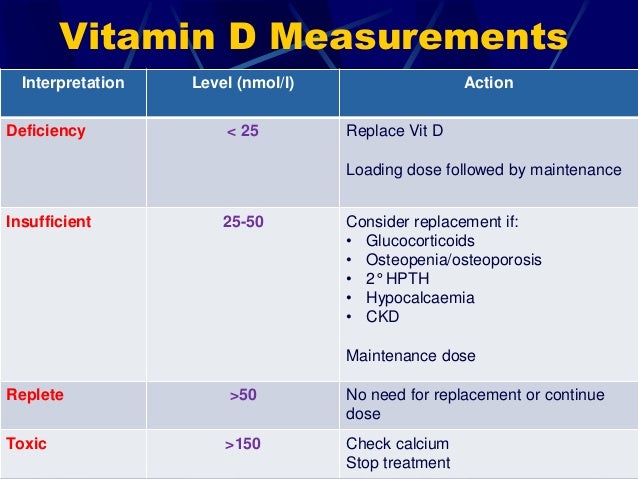
To accomplish this, it is recommended to improve your diet, get at least ten minutes of sunlight a day, and take a vitamin D supplement ranging from 2,000 IU to 10,000 IU. The amount needed will be dependant on the deficiency levels. It was once believed that a normal level of vitamin D was 20 ng/ml, however recent studies have found that this may be too low and individuals should instead shoot for 30 ng/ml. If you are concerned you may be vitamin D deficient, or if you have bipolar depression and would like to see if vitamin D can improve your mood, schedule an appointment with Dr. Thompson today!
Thompson today!
Copyright © 2022 Optimized360 LLC | All Rights Reserved | Privacy Policy | Terms of Use | Disclaimer | Web Accessibility Statement
The role of vitamin D in bipolar disorder: Epidemiology and influence on disease activity
Save citation to file
Format: Summary (text)PubMedPMIDAbstract (text)CSV
Add to Collections
- Create a new collection
- Add to an existing collection
Name your collection:
Name must be less than 100 characters
Choose a collection:
Unable to load your collection due to an error
Please try again
Add to My Bibliography
- My Bibliography
Unable to load your delegates due to an error
Please try again
Your saved search
Name of saved search:
Search terms:
Test search terms
Email: (change)
Which day? The first SundayThe first MondayThe first TuesdayThe first WednesdayThe first ThursdayThe first FridayThe first SaturdayThe first dayThe first weekday
Which day? SundayMondayTuesdayWednesdayThursdayFridaySaturday
Report format: SummarySummary (text)AbstractAbstract (text)PubMed
Send at most: 1 item5 items10 items20 items50 items100 items200 items
Send even when there aren't any new results
Optional text in email:
Create a file for external citation management software
Full text links
Elsevier Science
Full text links
Review
. 2021 Jan 1;278:209-217.
2021 Jan 1;278:209-217.
doi: 10.1016/j.jad.2020.09.039. Epub 2020 Sep 12.
Guido Cereda 1 , Paolo Enrico 1 , Valentina Ciappolino 2 , Giuseppe Delvecchio 3 , Paolo Brambilla 4
Affiliations
Affiliations
- 1 Department of Pathophysiology and Transplantation, University of Milan, Milan, Italy.
- 2 Department of Neurosciences and Mental Health, Fondazione IRCCS Ca' Granda, Ospedale Maggiore Policlinico, Milan, Italy.
- 3 Department of Pathophysiology and Transplantation, University of Milan, Milan, Italy.
 Electronic address: [email protected].
Electronic address: [email protected]. - 4 Department of Pathophysiology and Transplantation, University of Milan, Milan, Italy; Department of Neurosciences and Mental Health, Fondazione IRCCS Ca' Granda, Ospedale Maggiore Policlinico, Milan, Italy.
- PMID: 32971313
- DOI: 10.1016/j.jad.2020.09.039
Review
Guido Cereda et al. J Affect Disord. .
. 2021 Jan 1;278:209-217.
doi: 10.1016/j.jad.2020.09.039. Epub 2020 Sep 12.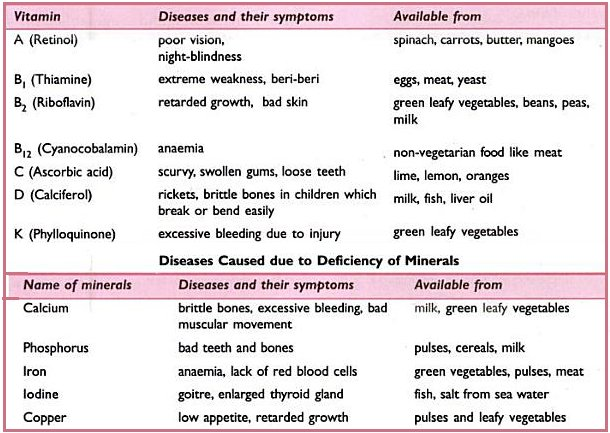
Authors
Guido Cereda 1 , Paolo Enrico 1 , Valentina Ciappolino 2 , Giuseppe Delvecchio 3 , Paolo Brambilla 4
Affiliations
- 1 Department of Pathophysiology and Transplantation, University of Milan, Milan, Italy.
- 2 Department of Neurosciences and Mental Health, Fondazione IRCCS Ca' Granda, Ospedale Maggiore Policlinico, Milan, Italy.
- 3 Department of Pathophysiology and Transplantation, University of Milan, Milan, Italy. Electronic address: giuseppe.delvecchio@unimi.
 it.
it. - 4 Department of Pathophysiology and Transplantation, University of Milan, Milan, Italy; Department of Neurosciences and Mental Health, Fondazione IRCCS Ca' Granda, Ospedale Maggiore Policlinico, Milan, Italy.
- PMID: 32971313
- DOI: 10.1016/j.jad.2020.09.039
Abstract
Background: Although many studies found an association between psychiatric disorders, especially major depressive disorder, and vitamin D deficiency, little is still known about the association between vitamin D and bipolar disorder (BD). Therefore, the present review aims at providing an overview of the available literature exploring the role of vitamin D in BD patients in different phases of the disease.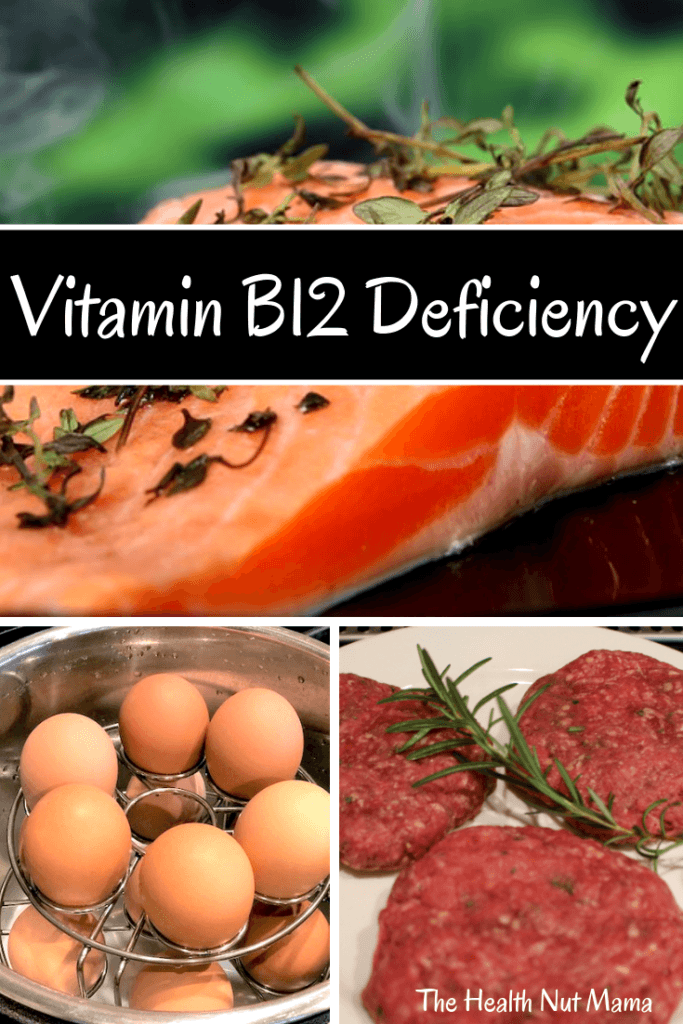
Methods: From a bibliographic research in PubMed until April 2020, we collected ten original studies that fulfilled our inclusion criteria.
Results: No significant differences in vitamin D levels between BD patients and other psychiatric disorders were found by most of the studies. In the majority of the studies, the average values of vitamin D in BD population were sub-threshold for vitamin D deficiency. Moreover, although an association between vitamin D levels and clinical symptomatology was observed in BD patients, it cannot be considered a specific marker of this disorder but a common characteristic shared with other psychiatric disorders, including schizophrenia and major depressive disorder. Finally, vitamin D supplementation was associated with a reduction in both depressive and manic symptoms.
Limitations: Few studies with small and heterogeneous populations.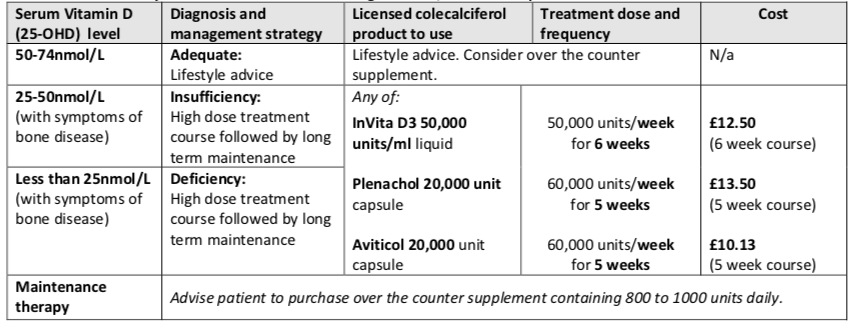 Methodological heterogeneity in terms of vitamin D measurement and threshold.
Methodological heterogeneity in terms of vitamin D measurement and threshold.
Conclusions: The results showed that vitamin D status does not differ between BD and other psychiatric conditions. However, given the correlation between vitamin D levels and depressive or manic symptoms, we could hypothesize that an adequate vitamin D status could positively affect the mood balance thanks to its immunomodulatory activity.
Keywords: Bipolar disorder; Depression; Mania; Micronutrient; Vitamin D.
Copyright © 2020. Published by Elsevier B.V.
Similar articles
-
Exploring the relationship between vitamin D and mania: correlations between serum vitamin D levels and disease activity.
Altunsoy N, Yüksel RN, Cingi Yirun M, Kılıçarslan A, Aydemir Ç.
 Altunsoy N, et al. Nord J Psychiatry. 2018 Apr;72(3):221-225. doi: 10.1080/08039488.2018.1424238. Epub 2018 Jan 7. Nord J Psychiatry. 2018. PMID: 29308715
Altunsoy N, et al. Nord J Psychiatry. 2018 Apr;72(3):221-225. doi: 10.1080/08039488.2018.1424238. Epub 2018 Jan 7. Nord J Psychiatry. 2018. PMID: 29308715 -
The prevalence and illness characteristics of DSM-5-defined "mixed feature specifier" in adults with major depressive disorder and bipolar disorder: Results from the International Mood Disorders Collaborative Project.
McIntyre RS, Soczynska JK, Cha DS, Woldeyohannes HO, Dale RS, Alsuwaidan MT, Gallaugher LA, Mansur RB, Muzina DJ, Carvalho A, Kennedy SH. McIntyre RS, et al. J Affect Disord. 2015 Feb 1;172:259-64. doi: 10.1016/j.jad.2014.09.026. Epub 2014 Oct 12. J Affect Disord. 2015. PMID: 25451425
-
Cognitive deficits in bipolar disorders: Implications for emotion.
Lima IMM, Peckham AD, Johnson SL.
 Lima IMM, et al. Clin Psychol Rev. 2018 Feb;59:126-136. doi: 10.1016/j.cpr.2017.11.006. Epub 2017 Nov 21. Clin Psychol Rev. 2018. PMID: 29195773 Free PMC article. Review.
Lima IMM, et al. Clin Psychol Rev. 2018 Feb;59:126-136. doi: 10.1016/j.cpr.2017.11.006. Epub 2017 Nov 21. Clin Psychol Rev. 2018. PMID: 29195773 Free PMC article. Review. -
Prevalence of Vitamin D Deficiency in Adult Outpatients With Bipolar Disorder or Schizophrenia.
Boerman R, Cohen D, Schulte PF, Nugter A. Boerman R, et al. J Clin Psychopharmacol. 2016 Dec;36(6):588-592. doi: 10.1097/JCP.0000000000000580. J Clin Psychopharmacol. 2016. PMID: 27662458
-
[Antipsychotics in bipolar disorders].
Vacheron-Trystram MN, Braitman A, Cheref S, Auffray L. Vacheron-Trystram MN, et al. Encephale. 2004 Sep-Oct;30(5):417-24. doi: 10.1016/s0013-7006(04)95456-5. Encephale. 2004. PMID: 15627046 Review.
 French.
French.
See all similar articles
Cited by
-
25(OH)D levels are decreased in patients with difficult-to-treat depression.
Grudet C, Lindqvist D, Malm J, Westrin Å, Ventorp F. Grudet C, et al. Compr Psychoneuroendocrinol. 2022 Feb 9;10:100126. doi: 10.1016/j.cpnec.2022.100126. eCollection 2022 May. Compr Psychoneuroendocrinol. 2022. PMID: 35755210 Free PMC article.
-
Therapeutic Interventions to Mitigate Mitochondrial Dysfunction and Oxidative Stress-Induced Damage in Patients with Bipolar Disorder.
Madireddy S, Madireddy S. Madireddy S, et al. Int J Mol Sci. 2022 Feb 6;23(3):1844. doi: 10.3390/ijms23031844. Int J Mol Sci. 2022. PMID: 35163764 Free PMC article.
 Review.
Review. -
Environmental Risk Factors for Schizophrenia and Bipolar Disorder and Their Relationship to Genetic Risk: Current Knowledge and Future Directions.
Robinson N, Bergen SE. Robinson N, et al. Front Genet. 2021 Jun 28;12:686666. doi: 10.3389/fgene.2021.686666. eCollection 2021. Front Genet. 2021. PMID: 34262598 Free PMC article. Review.
Publication types
MeSH terms
Substances
Full text links
Elsevier Science
Cite
Format: AMA APA MLA NLM
Add to Collections
- Create a new collection
- Add to an existing collection
Name your collection:
Name must be less than 100 characters
Choose a collection:
Unable to load your collection due to an error
Please try again
Send To
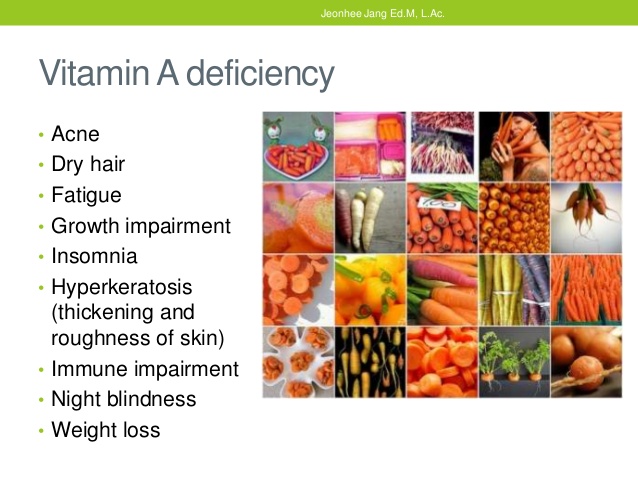
How vitamin deficiency affects the psyche?
Baku, March 4, AZERTAC
We know that nutrients are necessary for the normal functioning of the body. So how much do they affect our minds? AZERTAC with reference to "Home Hearth" talks about how beriberi affects the psyche.
So how much do they affect our minds? AZERTAC with reference to "Home Hearth" talks about how beriberi affects the psyche.
How much do trace elements affect our minds?
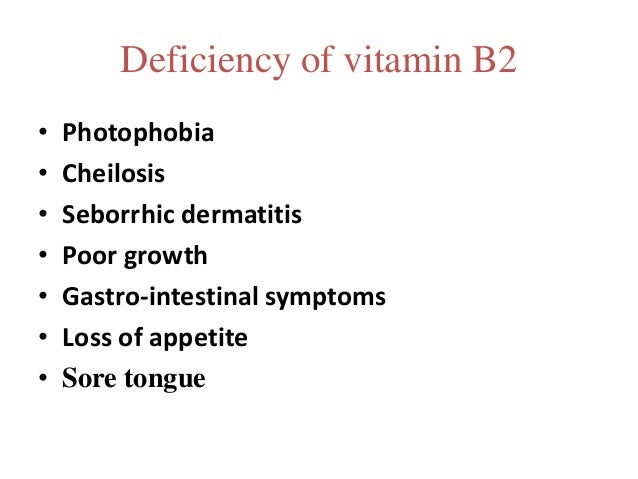
Optimal mental health requires adequate vitamins, minerals, amino acids, and fatty acids—the building blocks for brain cells and neurotransmitters. Simply put, if the diet is not varied enough, and nutrients are poorly absorbed, mental health suffers.
With good nutrition, there should be no cause for concern. In other cases, the doctor may prescribe you a course of vitamins if the body does not absorb nutrients properly, or if you are unable to eat certain foods for health reasons. And, most likely, in the pharmacy you will find simple and relatively inexpensive drugs instead of the ruinous super-jars from the ads of Instagram bloggers.
Mind and Body Care
Because we are all unique, one person may be more deficient in a particular micronutrient (such as vitamin D) than another.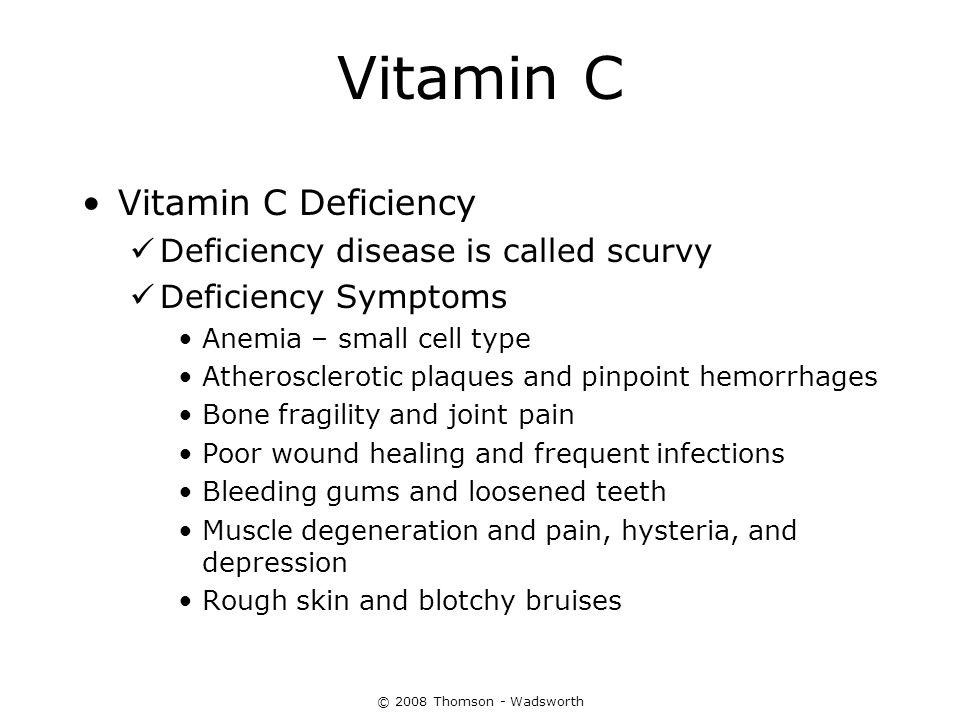 This applies to most vitamins and minerals.
This applies to most vitamins and minerals.
Nutritional deficiencies can affect your mental health in many ways, ranging from minor inconveniences to frightening symptoms. Studies have shown that a lack of important elements in the diet can contribute to anxiety and depression, as well as exacerbate symptoms in people with certain mental illnesses, such as obsessive-compulsive disorder or bipolar disorder. And even if you are healthy, malnutrition can worsen your mood and emotional background.
Scientists still have a lot to figure out, the space for research is huge. But here's what scientists have already learned about the relationship between nutrition and mood:
Vitamin D
This fat-soluble vitamin affects the expression of more than 1000 genes that regulate mood and sleep, and also affects the protection and synthesis of neurons (our brain cells and nervous system). Throughout our body, including the brain, there are vitamin D receptors, the state of which affects perception, motivation, memory, and even pleasure.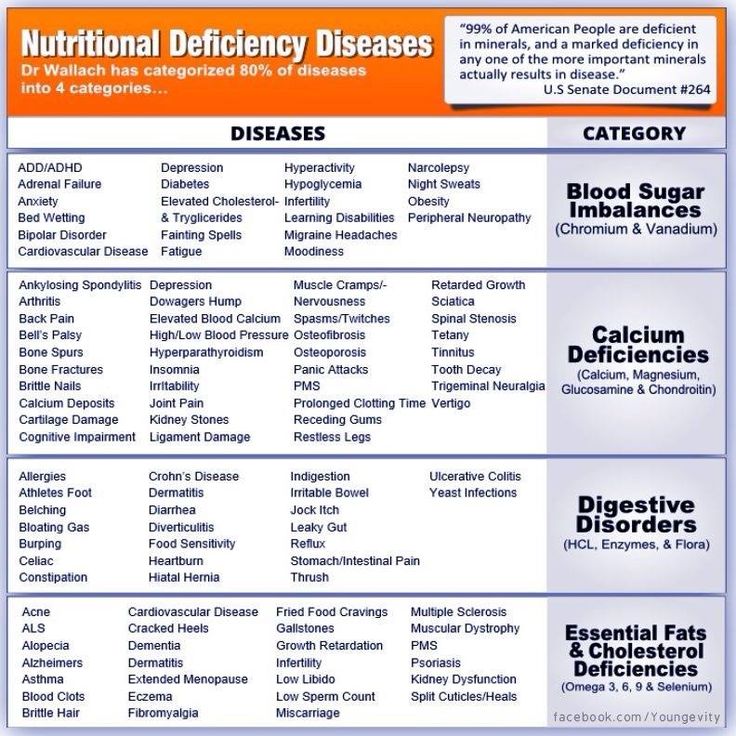
Vitamin D deficiency symptoms: depression; anxiety; irritability; fatigue.
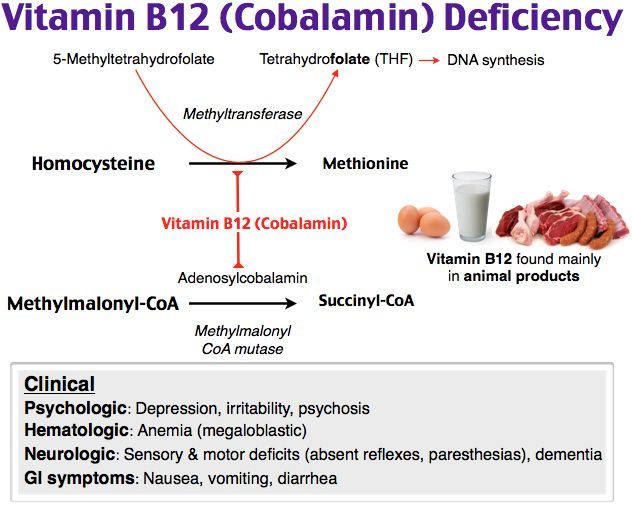
Vitamin B12
This vitamin, like the previous one, helps in the formation of valuable neurons (nerve cells are restored!). It plays an important role in the regulation of mood-enhancing chemicals (such as serotonin and dopamine) or stress-management chemicals (such as norepinephrine).
Vitamin B12 deficiency symptoms: fatigue; decrease in concentration; numbness and tingling; shortness of breath, etc.
Vitamin B6
The concentration of vitamin B6 is about 100 times higher in the brain than in the rest of the body, and it is difficult to overestimate its importance for the functioning of your gray cells. This vitamin directly affects the production of brain-beneficial chemicals, including serotonin, dopamine, and gamma-aminobutyric acid.
B6 (like B12) helps the body control levels of the amino acid homocysteine, which helps regulate mood.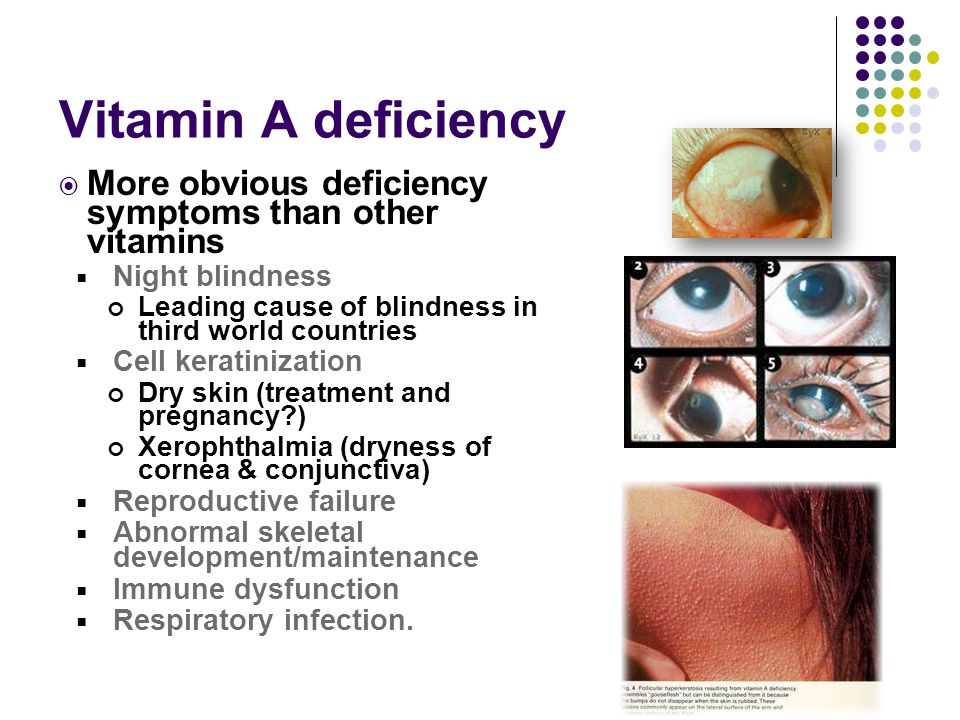 People with kidney disease or malabsorption suffer from B6 deficiency much more often than others.
People with kidney disease or malabsorption suffer from B6 deficiency much more often than others.
Magnesium
In mental health, magnesium helps moderate the stress response and is considered one of nature's mood stabilizers. Magnesium deficiency is rare, but there are exceptions.
Low magnesium symptoms: fatigue; nausea; loss of appetite; abrupt mood swings.
Zinc
Zinc is the main assistant of vitamin B6, and most people get enough just from food. Deficiency can occur in pregnant or breastfeeding women, vegetarians, and people with gastrointestinal conditions.
Zinc deficiency symptoms: loss of appetite or taste; irritability; depression; learning difficulties.
Iron
In addition to regulating oxygen transport throughout the body and to the brain, iron helps create and balance mood-regulating substances such as serotonin and dopamine. At risk are women (due to menstruation), the elderly and vegans.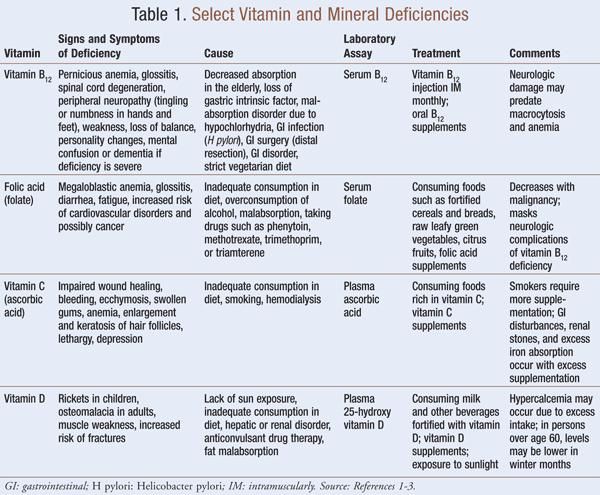
Symptoms of iron deficiency: fatigue; difficulty concentrating; dizziness.
Omega-3 fatty acids
Omega-3 fatty acids contain DHA and EPA, which play an important role in brain function. They prevent inflammation, keep nerve cells healthy, and improve communication between neurons.
Omega-3 deficiency symptoms: depressed mood; dry skin; fatigue; manifestations of allergic reactions; chronic thirst.
How do you know if you have a deficit and what to do about it?
Self-treatment is risky, pointless and often very expensive. You should not multiply entities: it is wiser to discuss with your doctor what is bothering you and talk about your diet. On the recommendation of a therapist, you can take tests for a deficiency of certain trace elements and, based on the results of the study, agree on further actions with a specialist.
If you find a mistake in the text, highlight it by pressing ctrl + enter and send it to us.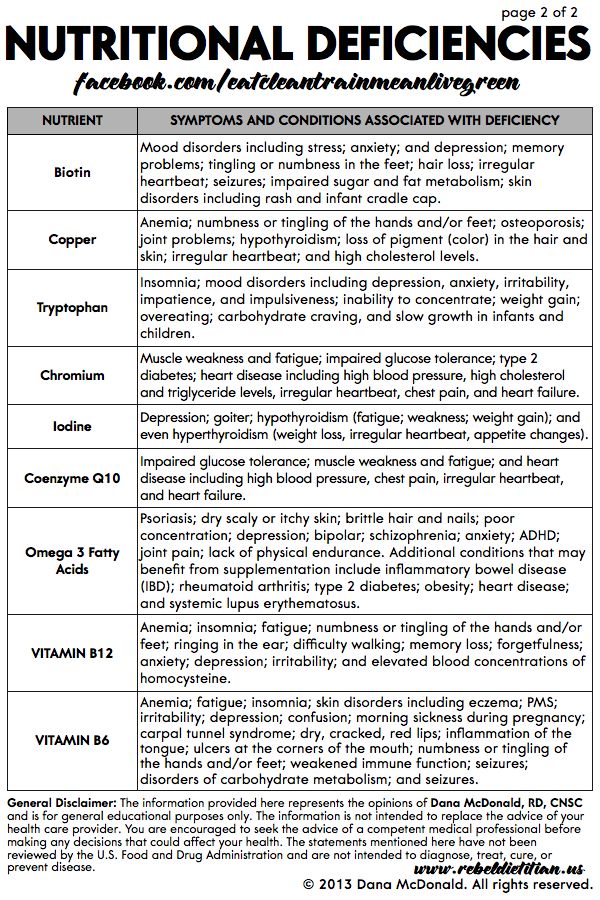 So how much do they affect our minds?
So how much do they affect our minds?
Anastasia Nikiforova
It's hard to miss vitamin commercials these days. Fashion brands and purveyors of luxurious-looking supplement jars promise that their products will help make up for the lack of essential elements. But don’t make up for it - then blame yourself, get ready for health and mental problems!...
Is this true? How much do trace elements affect our mind?
Very strong. Optimal mental health requires adequate amounts of vitamins, minerals, amino acids, and fatty acids—the building blocks for brain cells and neurotransmitters. Simply put, if the diet is not varied enough, and nutrients are poorly absorbed, mental health suffers.
With good nutrition, there should be no cause for concern. In other cases, the doctor may prescribe you a course of vitamins if the body does not absorb nutrients properly, or if you cannot eat certain foods for health reasons. And, most likely, in a pharmacy you will find simple and relatively inexpensive drugs instead of ruinous super-cans from Instagram bloggers.
And, most likely, in a pharmacy you will find simple and relatively inexpensive drugs instead of ruinous super-cans from Instagram bloggers.
Mind and body care
Because we are all unique, one person may be more deficient in a particular micronutrient (such as vitamin D) than another. This applies to most vitamins and minerals.
Nutritional deficiencies can affect your mental health in many ways, ranging from minor inconvenience to frightening symptoms. Studies have shown that the lack of important elements in the diet can contribute to anxiety and depression, as well as exacerbate symptoms in people with certain mental illnesses, such as obsessive-compulsive disorder or bipolar disorder. And even if you are healthy, malnutrition can worsen your mood and emotional background.
Scientists still have a lot to figure out, the space for research is huge. But here is what scientists have already learned about the relationship between nutrition and mood:
Vitamin D
This fat-soluble vitamin affects the expression of more than 1000 genes that regulate mood and sleep, and also affects the protection and synthesis of neurons (our brain cells and nervous system).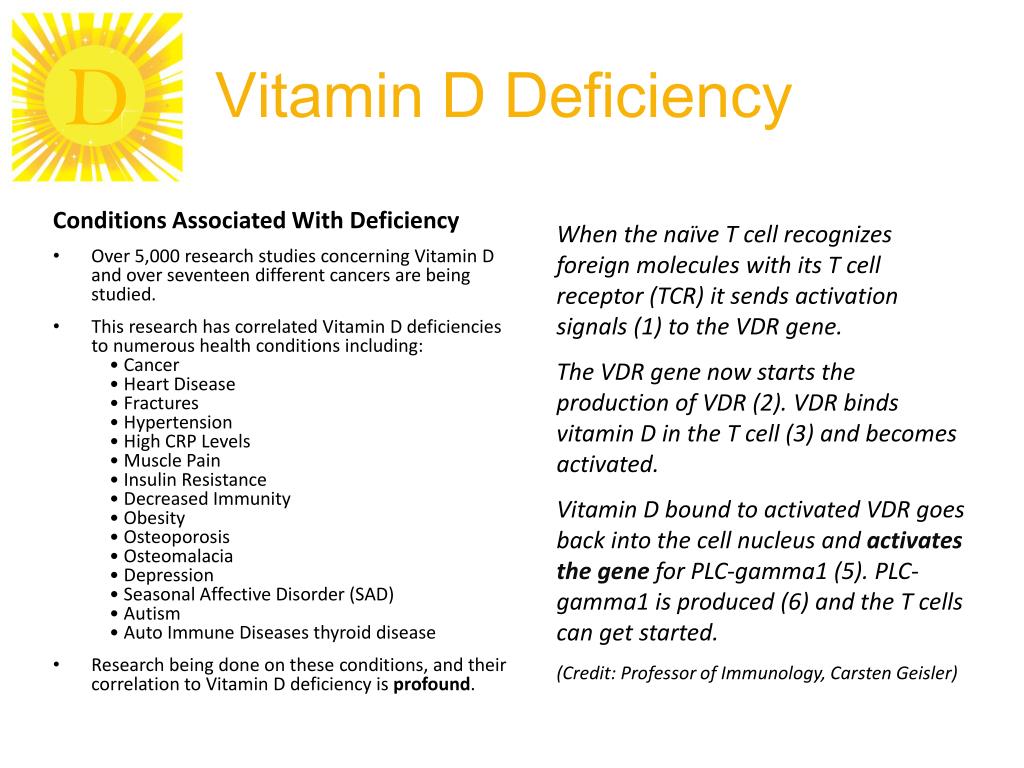 Throughout our body, including the brain, there are vitamin D receptors, the state of which affects perception, motivation, memory, and even pleasure.
Throughout our body, including the brain, there are vitamin D receptors, the state of which affects perception, motivation, memory, and even pleasure.
Vitamin D deficiency symptoms:
- depression
- anxiety
- irritability
- fatigue.
Vitamin B12
This vitamin, like the previous one, helps in the formation of valuable neurons (nerve cells are restored!). It plays an important role in the regulation of mood-enhancing chemicals (such as serotonin and dopamine) or stress-management chemicals (such as norepinephrine).
Vitamin B12 deficiency symptoms:
- fatigue
- decreased concentration
- numbness and tingling
- shortness of breath, etc.
Vitamin B6
The concentration of vitamin B6 is approximately 100 times higher in the brain than in the rest of the body, and it is difficult to overestimate its importance for the work of your gray cells. This vitamin directly affects the production of brain-beneficial chemicals, including serotonin, dopamine, and gamma-aminobutyric acid.
This vitamin directly affects the production of brain-beneficial chemicals, including serotonin, dopamine, and gamma-aminobutyric acid.
B6 (like B12) helps the body control levels of the amino acid homocysteine, which helps regulate mood. People with kidney disease or malabsorption suffer from B6 deficiency much more often than others.
Magnesium
In mental health, magnesium helps moderate the stress response and is considered one of nature's mood stabilizers. Magnesium deficiency is rare, but there are exceptions.
Low magnesium symptoms:
- fatigue
- nausea
- loss of appetite
- mood swings.
Zinc
Zinc is the main assistant of vitamin B6, and most people get enough just from food. Deficiency can occur in pregnant or breastfeeding women, vegetarians, and people with gastrointestinal conditions.
Zinc deficiency symptoms:
- loss of appetite or taste
- irritability
- depression
- learning difficulties.
Iron
In addition to regulating oxygen transport throughout the body and to the brain, iron helps create and balance mood-regulating substances such as serotonin and dopamine. At risk are women (due to menstruation), the elderly and vegans.
Symptoms of iron deficiency:
- fatigue
- difficulty concentrating
- dizziness.
Omega-3 fatty acids
Omega-3 fatty acids contain DHA and EPA fatty acids, which play an important role in brain function. They prevent inflammation, keep nerve cells healthy, and improve communication between neurons.
Omega-3 deficiency symptoms:
- depressed mood
- dry skin
- fatigue
- manifestations of allergic reactions
- chronic thirst.