Dbt for dissociation
Three Distress Tolerance Skills to Help Cope with Dissociation
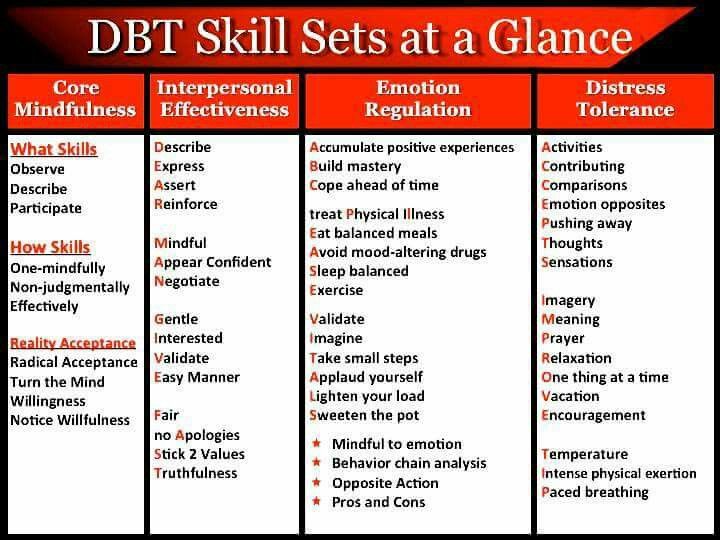
While dialectical behavior therapy (DBT) isn't the primary treatment option for dissociative identity disorder (DID), there are DBT skills, like distress tolerance skills, that can help people manage their dissociation symptoms. These skills come in handy in a crisis or when we feel ourselves heading towards dissociation. So how do you use the distress tolerance skills of DBT for the dissociation of DID?
Although DBT wasn't specifically created for people with dissociative disorders, we can certainly use some DBT skills to cope with DID. Here are three distress tolerance skills to try when dissociation feels imminent.
1. The TIPP Distress Tolerance Skill
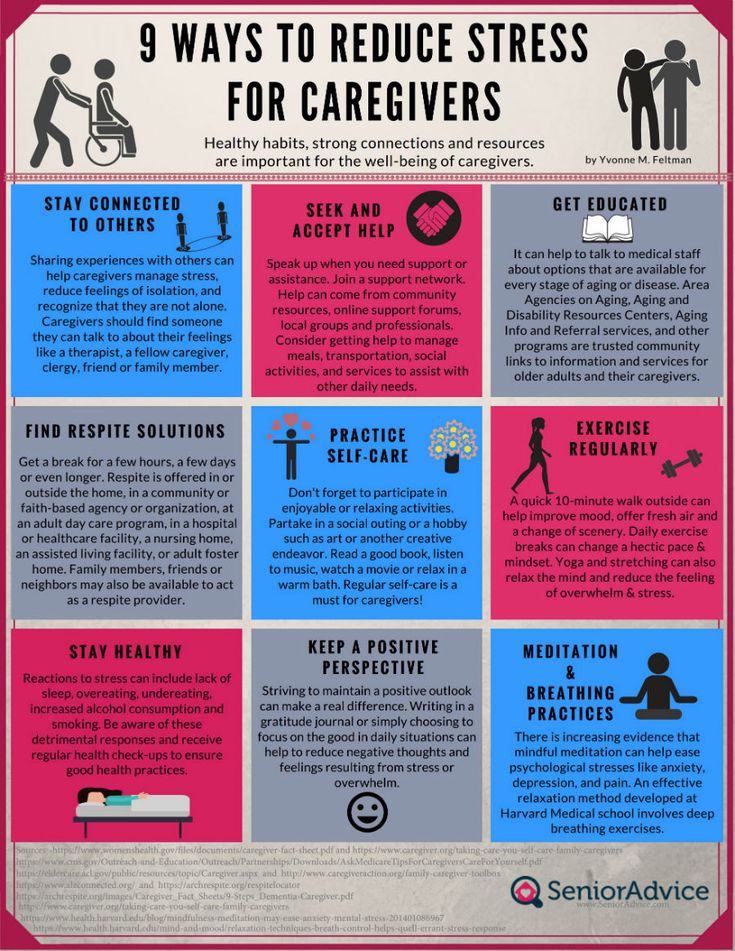
In DBT, the TIPP skill is used as part of crisis survival. If you feel your emotions getting out of control or feel yourself dissociating, you can use the TIPP skill to help ground you. The TIPP skill involves temperature change, intense exercise, and paced breathing/progressive muscle relaxation.
For temperature change, you can hold ice cubes, take a cold shower, or dunk your face in cold water. This helps to lower the intensity of your emotions and bring you back to the present. Intense exercise is helpful when you feel yourself numbing out (which can lead to dissociation) or to distract yourself from a trigger. Lastly, paced breathing and progressive muscle relaxation help change your focus to what is going on inside your body and can bring you outside of the emotions that may lead to dissociation.
2. The ACCEPTS Distress Tolerance Skill
DBT includes another distress tolerance skill called ACCEPTS which stands for
- Activities,
- Contributing,
- Comparisons,
- Emotions,
- Pushing away,
- Thoughts, and
- Sensations.
While not all of the parts of the ACCEPTS skill can be useful for those with DID, some of these methods of distraction as a distress tolerance skill can keep us from dissociating.
When practicing the ACCEPTS skill, we can distract ourselves from what may be triggering the dissociation by watching TV, reading a book, going outside to the beach or the park, listening to music, reaching out to someone, or doing something that jolts a physical sensation, like eating something cold or drinking a hot coffee.
3. Learn to Self-Soothe
Another DBT distress tolerance skill is self-soothing. With self-soothing, we try to use as many of the five senses -- taste, touch, smell, hearing, and sight in order to engage ourselves in the present moment. For those of us with DID or another dissociative disorder, staying in the present is important in order to decrease dissociation.
The best way to practice self-soothing is to create a self-soothe kit. The self-soothe kit can include anything and should be things that help to soothe you. Your favorite lotion, a small candle, mints or candy, a noisemaker, affirmation cards, grounding stones, clay -- the choices are up to you.
You can get a small pouch or box so you can have these items wherever you go. When you feel yourself becoming ungrounded or dissociated, you can pull out your self-soothe kit to comfort yourself and remind yourself that you are in the present moment.
Any of these DBT distress tolerance skills can help those with DID distract from triggers, keep us in the present moment, and decrease dissociation. So while DBT may not have been created for people with dissociative disorders, we can certainly learn a lot from the skills within.
So while DBT may not have been created for people with dissociative disorders, we can certainly learn a lot from the skills within.
APA Reference
Matulewicz, C. (2017, April 27). Three Distress Tolerance Skills to Help Cope with Dissociation, HealthyPlace. Retrieved on 2023, January 18 from https://www.healthyplace.com/blogs/dissociativeliving/2017/04/did-and-dbt-use-distress-tolerance-skills-for-dissociation
DBT Skills Heal Chronic Dissociation & Depersonalization
Chronic Dissociative Experiences
Depersonalization is a common type of dissociative experience that DBT therapy can do wonders with to decrease unwanted symptomatology. Chronic depersonalization, likely being the most common form of dissociation, is often found in most anxiety and trauma-related disorders. Many people are NOT aware that they are experiencing depersonalization, and DBT Skills can help people become more mindful and knowledgeable of what is happening, and why.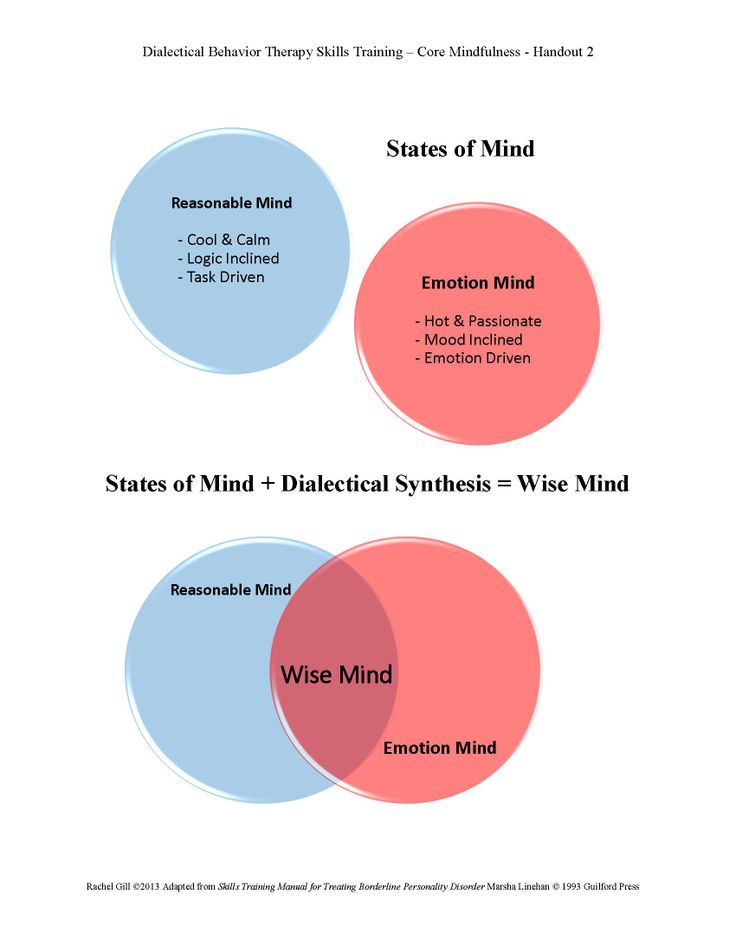 This starts the foundation toward effective healing.
This starts the foundation toward effective healing.
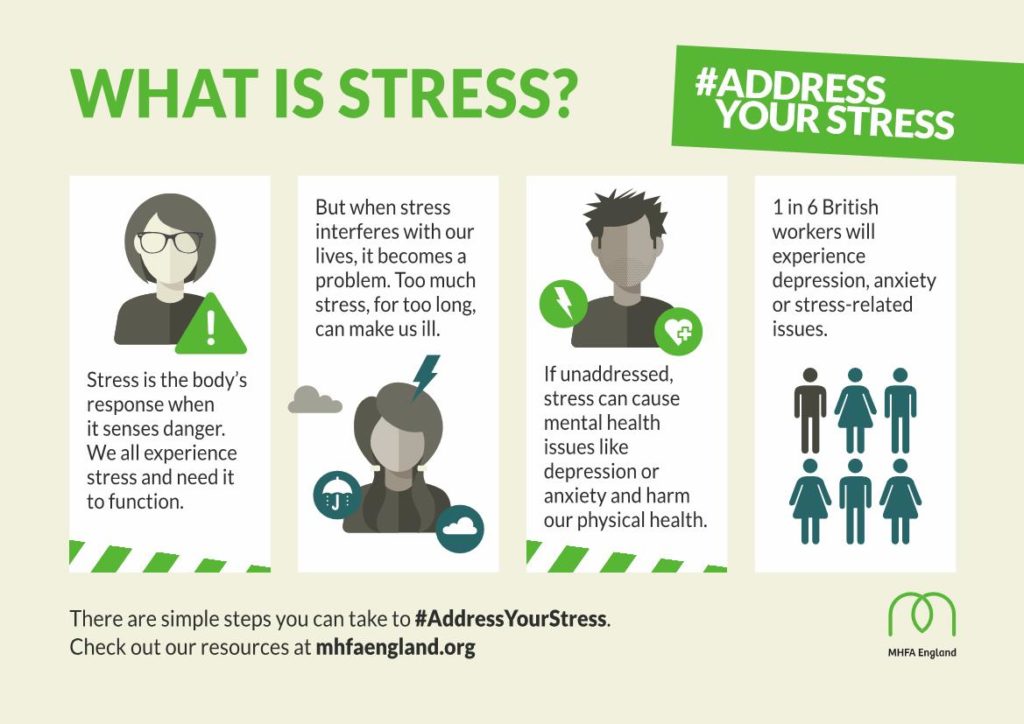
It is important to also appreciate that dissociation is not bad in itself, in fact, during times of distress, and trauma, it is an amazing and very adaptive capacity of our brain that protects us, and at times even saves our lives. It is the chronicity, and occurrence of continued dissociation, and depersonalization, when it is no longer necessary, that can be problematic. It can end up taking us out of being present in our lives and fosters the re-experiencing, consciously or unconsciously, the distressing symptoms, rather than resolving them.
To learn more, watch our videos: What is dissociation? And What is depersonalization?
What Does Depersonalization Look & Feel Like?
Dissociation and Depersonalization
Depersonalization is sensations and experiences of being alienated from your body. All of us have normal experiences of depersonalization from time to time. For example, you arrive home from work or the store and realize you do not remember the last 10-20 minutes of your drive.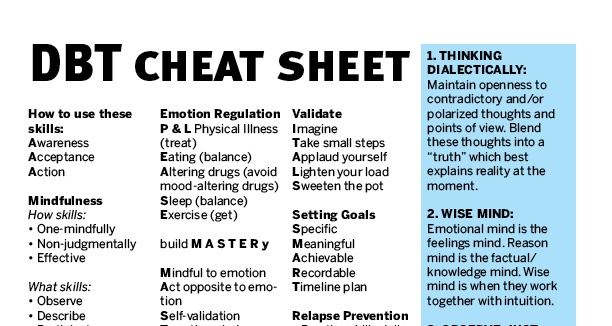 That is a natural and common experience we all have when something is familiar to us, and part of our mind goes into auto-drive and another part is somewhere else.
That is a natural and common experience we all have when something is familiar to us, and part of our mind goes into auto-drive and another part is somewhere else.
Depersonalization becomes a problem when it is taking us away from our ability to function in important areas of our life, or when it interferes with our significant relationships. For some people, it becomes a debilitating chronic experience. For moderate to severe, or chronic depersonalization, it is best to seek compassionate and effective help.
Check out our website and learn more about our counseling services.
What are the Symptoms of Depersonalization?
The symptoms of Depersonalization include, but are not limited to, the following types of experiences. Please note that it is important to rule out other medical, neurological, or organic causes for these experiences. Most moderate to severe Depersonalization stems from past overwhelming or traumatizing experiences that the mind dissociates to make it less distressing.
- Part(s) of the body feeling numb, blank, or as if they are partially or completely missing
- Experiences of watching yourself from outside of your body
- Seeing another part of you doing something
- Recalling your past without feelings of experiencing it
- Experiences and memories feel dreamlike, or movie-like
- Knowing something happened, but it doesn’t feel like it happened to me
- Feeling dead, unreal, and/or like a robot
- Feeling as you have no control over your actions
- Lack of feeling pain or other body sensations, such as heat, cold, hunger, or tired
- Can be temporary, acute, or chronic
What are the Causes of Dissociation & Depersonalization?
Causes of chronic dissociation and depersonalization, after ruling out medical or organic causes, may include invasive medical procedures, early emotional or physical neglect, all types of abuse, and/or early attachment disruptions. Other common causes are past experiences that were overwhelming around shame, humiliation, terror, panic, rejection, abandonment, hopelessness, or helplessness.
The good news is there is help if you, or a loved one, experiences chronic moderate to severe depersonalization and dissociation.
How Can DBT Skills Help with Dissociation?
DBT Skills Heal Dissociation
Using Dialectical Behavioral Therapy (DBT), or DBT Skills Groups, to heal from dissociation and depersonalization, helps because DBT encompasses Mindfulness, Distress Tolerance, and Emotional Regulation skills. Dissociation is about non-realization, so the opposite dialect is to realize, and to be present with. Being able to bring forth, and be with, emotional information in order to reflect and bring awareness is empowering and healing. When the information is too distressing though, we need tools and skills to make that possible. Mindfulness is about awareness of the present moment which essentially is a form of realization. Importantly realization is the opposite of dissociation, therefore being a remedy.
DBT helps you build a tolerance to what feels intolerable; to the distressing feelings, sensations, and memories that the mind avoids through Depersonalization (out of the body) dissociative experiences. Therefore, the antidote is to begin to tolerate and bring awareness, gently and safely.
Therefore, the antidote is to begin to tolerate and bring awareness, gently and safely.
Once you can tolerate more distress in your body and more of the inner experiences, you can use the emotion regulation skills to adaptively re-process the emotions and feelings that were NOT adaptatively processed, due to being dissociated. Dissociation inhibits regulation and processing of the experience, to protect us from overwhelm.
Therefore, by learning supportive, easy-to-understand, and doable DBT skills with a qualified and compassionate therapist, you can step back into your body and your life. This is what embodiment means. So empowering right?
Want to learn more about our DBT Skills Groups.
Additionally, DBT therapy can successfully set you up to do deeper trauma therapy, like EMDR Therapy and/or IFS therapy. Also, learn more about EMDR therapy and IFS below.
What Are Next Steps in Healing from Chronic Dissociation & Depersonalization?
DBT therapy sets the foundation to be more mindful, to be in our bodies and experience life more fully, and to tolerate and regulate distressing emotions. Inevitably, DBT skills empower us and change unwanted behaviors in our life, making it so we don’t need to suppress, avoid, escape, amplify, or push away our emotional experiences.
Inevitably, DBT skills empower us and change unwanted behaviors in our life, making it so we don’t need to suppress, avoid, escape, amplify, or push away our emotional experiences.
Once we can be more present with our own emotional experiences, which is essentially the opposite of what dissociation is, we can deepen our healing through reflection, thus, gaining insight and adaptive information. At Stacy Ruse Counseling Group, we utilize EMDR therapy and Internal Family Systems (IFS) therapy as our go-to trauma therapies, and for good reason. Both of these therapies are proven and evidence-based trauma therapies. They are also gentle, and empowering, allowing the person to play a collaborative role in therapy. And they WORK once we can tolerate our experiences, which is what DBT therapy does best, so we can do the trauma work.
EMDR Therapy Heals Dissociation
More on EMDR Therapy
EMDR stands for eye movement and desensitization reprocessing therapy. It is powerful, and from my extensive experience and based on the research, offers some of the most amazing therapeutic tools the world has to offer for healing trauma.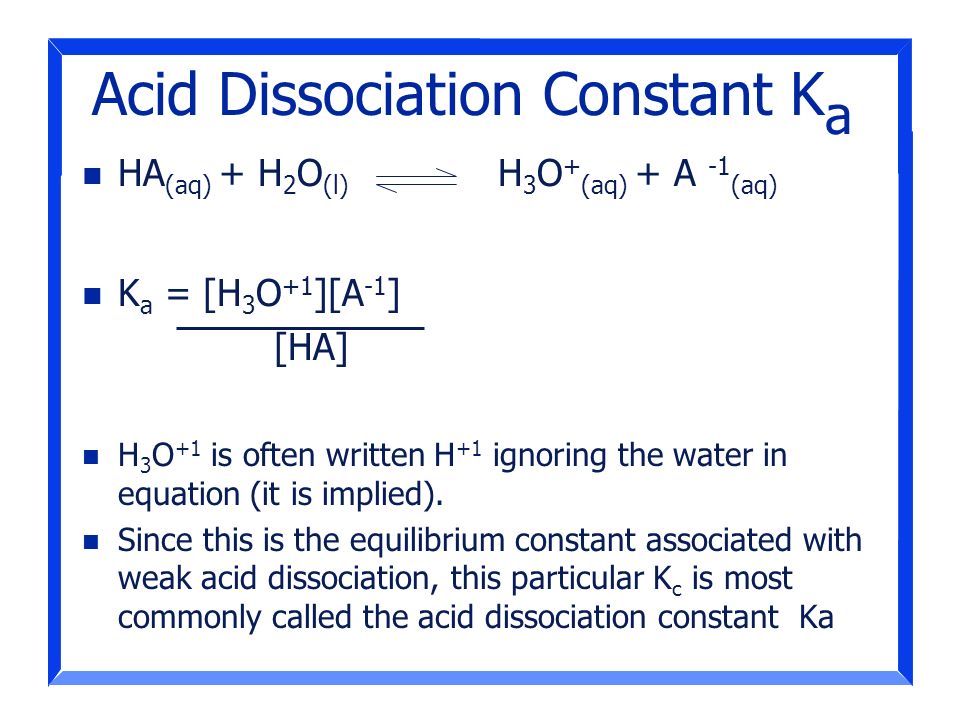
When it comes to trauma healing, slow and gentle is the fast track toward healing. Remember, trauma essentially is – too much – too fast, coming at us, thus we aren’t able to adaptively process the distress. So healing is about slowing it down and being with it, step by step, in order to reprocess the information, one piece at a time. When done in this way, with a trained EMDR therapist, we can resolve and move out the unwanted distress. EMDR effectively helps us do that.
The prerequisite is having the ability to have dual awareness in the process, which means you metaphorically have one foot in the past (the distress) and one foot in the present (the safety). It is not helpful, or therapeutic, for anyone to be completely overwhelmed and re-experiencing trauma. That is why DBT therapy offers a wonderful approach to building the foundation to do deep inner work. Once we have this foundation, we can safely reprocess and desensitization the overwhelming sensations, emotions, and experiences that were left fragmented and unresolved.
EMDR uses a combination of protocols and techniques, with the desensitization phase of the therapy, including bilateral stimulation (BLS), which EMDR is best known for. BLS engages both hemispheres of the brain and wakes up the areas of the brain that help us stay more present and grounded during the therapy, allowing the emotional information to organically process adaptively, even bringing the client deep insights and cathartic release.
Learn more about our counseling services.
Read our blog article EMDR is a Powerful Way to Heal Trauma
IFS Therapy Heals Dissociation
More about IFS Therapy
Internal Family Systems (IFS) therapy is one of the most upcoming and sought-after therapies in the world, and for good reason. Like DBT and EMDR, IFS therapy is highly endorsed and evidence-based. This wholistic therapy is gentle and transformational in its approach, working from the premise that we ALL have ‘Self-energy’ or a core Self, whether we realize or it or not.
When we tap into our self-energy, and that of others, we experience healing qualities of Compassion, Curiosity, Calmness, Clarity, Courage, Connectedness, Confidence, and Creativity. Importantly, in IFS therapy, the therapist also holds their own self-energy, and together, it is a collaborative, deep, beautiful, and powerful healing experience. This capacity is inherent, and IFS therapy helps us find these qualities within us, and through tapping into these energies, we are able to mindfully be with our experiences, even the most distressing, in an incredibly healing way.
Along with self-energy, there are what IFS calls inner parts, also referred to as ego in other contexts, and the premise is ALL parts are welcome. It makes so much sense, how many of us say all the time “a part of me feels this way, or a part does not want to do…”. Parts may be protective and others can be wounded, and need healing. Even the most destructive parts of us, have protective intentions for us and are often frozen in trauma-time when extreme behaviors and actions were needed. When we unburden the parts of us, they are able to unfreeze and move back into roles that are more balanced and purposeful for us.
When we unburden the parts of us, they are able to unfreeze and move back into roles that are more balanced and purposeful for us.
In these terms, dissociation is a combination of the non-realization, the frozen actions, the unwanted symptoms, the difficulty in accessing our self-energy, and the noncollaboration of our parts. By being mindful of our own inner systems, we can begin to harmonize our minds, untangle inner conflicts, and heal wounds.
“We often find that the harder we try to get rid of emotions and thoughts, the stronger they become. This is because parts, like people, fight back against being shamed or exhiled.” Richard Schwartz, founder of IFS
So the ‘internal family’ is all the parts of our internal system and at the core is our Self-energy. Like an external family that can be dysfunctional or functional, so can our internal family, in fact, our internal family is often similar to our family of origin, picking up the struggles, legacy burdens, hardships, and ineffective patterns.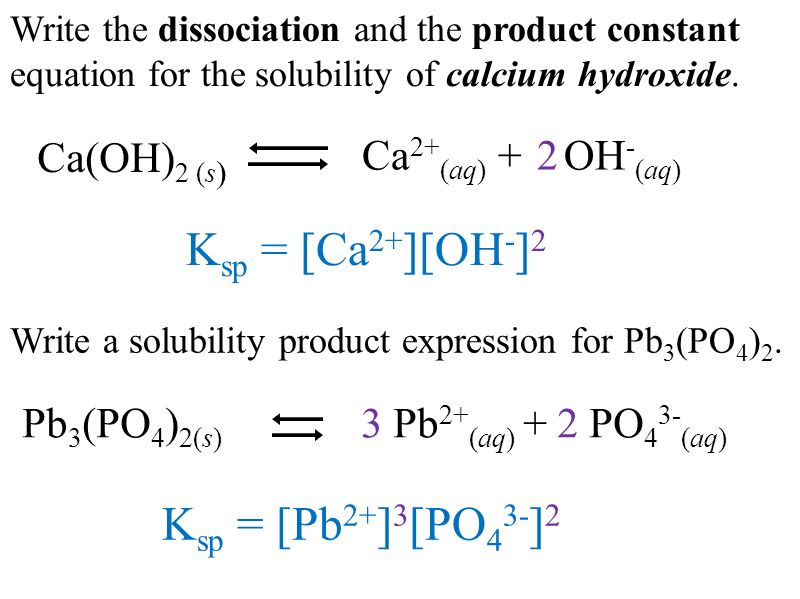 Additionally, we can also pick up the resiliency, effective patterns, and other positive qualities from our family and ancestors, and can tap into this for healing as well.
Additionally, we can also pick up the resiliency, effective patterns, and other positive qualities from our family and ancestors, and can tap into this for healing as well.
Therefore, we learn that over time, and through traumatizing and distressing experiences, our ‘parts’ or subpersonalities become more extreme and disintegrated. The purpose of IFS therapy is to reintegrate these parts into a healthy and better functioning system with the direction and leadership of the core self. The goals are to know yourself at a deeper level, to uncover and resolve inner conflicts, and to heal the hurt and wounds.
Learn more about IFS therapy or our other counseling services.
Read our blog article Are You a Trauma Survivor? Or watch our video series: Trauma Talks: The World Needs Healing
We would love to hear from you? What has been your experience with dissociation and/or depersonalization? Please make comments below.
Stacy Ruse Counseling Group envisions a new age of counseling for tweens, teens, adults, & groups that makes a REAL difference with core values of WELLBEING | COMPASSION | EQUALITY | INVESTMENT.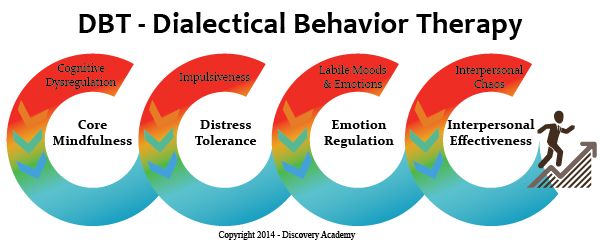
Author, Stacy Ruse LPC, EMDRIA Approved Consultant, DBT Certified Therapist, IFS Intensively Trained. Stacy is a modern-day Light-Worker, Trauma-Crusader, Shame-Untangler & Star-Seeker.
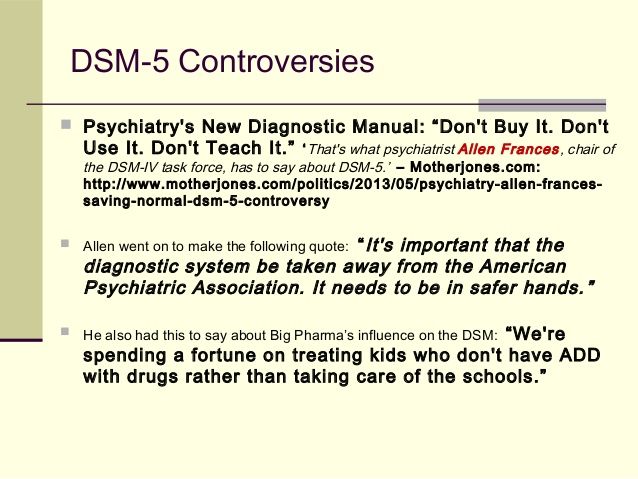
Effectiveness of DBT
DBT is the only treatment for borderline personality disorder (BPD) that has been sufficiently studied to allow for meta-analytical calculations (confirming its effectiveness) [Cohen, 1992; Kliem et al, 2010]. A meta-analysis by Binks et al (2006) showed that DBT in BPD leads to a reduction in self-injurious and suicidal behavior and thinking.
The first randomized clinical trial of DBT compared the effectiveness of this type of therapy with standard psychiatric treatment [Linehan et al., 1991; Linehan et al., 1993; Linehan et al., 1994]. Patients on DBT were significantly less likely to engage in parasuicidal behavior during the year from study entry, report fewer parasuicidal episodes at each follow-up assessment, and have less medically serious parasuicidal acts and incomplete suicide attempts.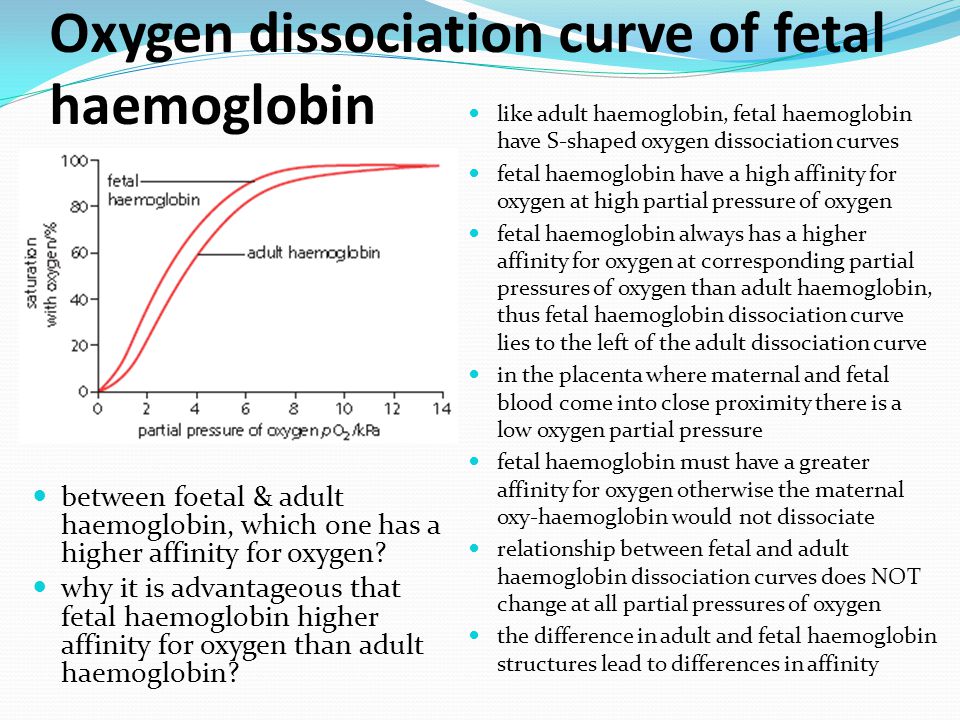 DBT was more effective than standard treatment in preventing premature discontinuation of therapy, the most severe treatment-impeding behavior. Patients treated with DBT were less likely to be hospitalized, spent fewer days in the hospital, and also showed greater improvement in global and social adjustment scales. Patients treated with DBT showed a significantly greater reduction in anger than patients in the control group. The superiority of DBT was maintained for one year after completion of therapy (i.e., for all two years of the study). Subsequently, 2 controlled randomized trials were performed that evaluated the effectiveness of DBT compared with standard treatment, as well as one case-control study comparing DBT with other types of psychotherapy. The results for most parameters confirmed the superiority of DBT noted in the first study. Koons et al. found that women with BPD who received the DBT program had greater reductions in self-injurious behavior, suicide attempts, and levels of depression compared to patients who received standard treatment.
DBT was more effective than standard treatment in preventing premature discontinuation of therapy, the most severe treatment-impeding behavior. Patients treated with DBT were less likely to be hospitalized, spent fewer days in the hospital, and also showed greater improvement in global and social adjustment scales. Patients treated with DBT showed a significantly greater reduction in anger than patients in the control group. The superiority of DBT was maintained for one year after completion of therapy (i.e., for all two years of the study). Subsequently, 2 controlled randomized trials were performed that evaluated the effectiveness of DBT compared with standard treatment, as well as one case-control study comparing DBT with other types of psychotherapy. The results for most parameters confirmed the superiority of DBT noted in the first study. Koons et al. found that women with BPD who received the DBT program had greater reductions in self-injurious behavior, suicide attempts, and levels of depression compared to patients who received standard treatment.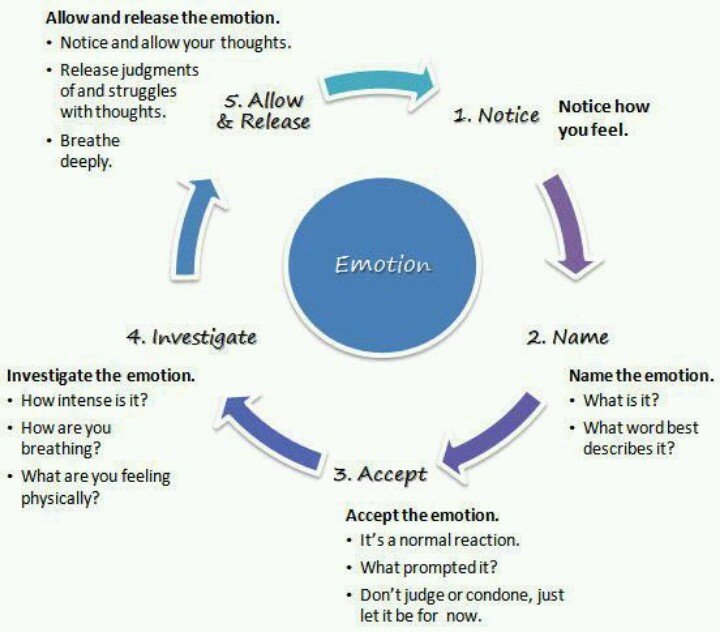 Finally, DBT (but not standard treatment) has been shown to lead to significant reductions in suicidal thoughts, feelings of hopelessness, anger, hostility, and dissociation [Koons et al., 2001]. In a sample of patients with addictive behaviors and BPD, DBT showed a greater improvement in substance abuse (based on structured interviews and urinalysis) both during treatment and at follow-up. DBT is accompanied by a large improvement in overall functioning and social adjustment during follow-up [Linehan et al., 1999].
Finally, DBT (but not standard treatment) has been shown to lead to significant reductions in suicidal thoughts, feelings of hopelessness, anger, hostility, and dissociation [Koons et al., 2001]. In a sample of patients with addictive behaviors and BPD, DBT showed a greater improvement in substance abuse (based on structured interviews and urinalysis) both during treatment and at follow-up. DBT is accompanied by a large improvement in overall functioning and social adjustment during follow-up [Linehan et al., 1999].
DBT is recognized by various authoritative medical organizations in developed countries (American Psychiatric Association guidelines for the diagnosis and treatment of borderline personality disorder [Oldham J.M. et al., 2001; 2005]; suicidal behavior [Jacobs D.M. et al., 2003]; British National Institute guidelines for Health and Care Excellence [NICE, 2009]; Australian Government National Health and Medical Research Council [Commonwealth of Australia, 2013] Australian Guidelines for BPD Treatment [Commonwealth of Australia, 2013]) as the most evidence-based treatment modality of any modality for the treatment of BPD, self-injurious and suicidal behavior. nine0003
nine0003
Long-term effect of DBT: reduction in hospital days
DBT targets (where possible) outpatient care and results in a significant reduction in the number and duration of hospitalizations, as confirmed by 12 comparative studies. Since DBT has a long-term effect, the amount of savings from using DBT increases every year after the intervention.
Thus, in the context of the current global and all-Russian trend towards a reduction in inpatient bed capacity, the use of DBT allows addressing the need for patients in medical care and reducing the need for repeated and prolonged hospitalizations. nine0003
Effective BPD treatment not only reduces health care costs, but also reduces the overall financial burden on society, including law enforcement, emergency services, social services, and the lost productivity of people with BPD, who often work below their capacity.
Reduction in the number of days in the hospital (data from randomized controlled trials DBT):
- Linehan et al (1991): patients treated with DBT for 12 months spent an average of 30.
 4 fewer days in the hospital than with conventional treatment; the decrease in hospital days persisted and became even more significant at follow-up a year later (Linehan et al, 1993).
4 fewer days in the hospital than with conventional treatment; the decrease in hospital days persisted and became even more significant at follow-up a year later (Linehan et al, 1993). - Linehan et al (1999): In the treatment of patients with BPD and substance dependence, DBT was superior to standard treatment in clinical outcomes. There were no statistically significant differences in the number of days of hospitalization during 12 months of therapy and 4 months of follow-up between DBT and standard care. nine0024
- Linehan et al (2002): DBT was superior to another treatment modality (12 steps + structured validation) in a sample of patients with BPD and opiate dependence, including fewer hospitalizations and days spent in the hospital during 12 months of therapy. The average number of nights spent in police stations was 7.7 for DBT patients and 18.8 for the comparison group.
- Batcheler (2005) in a 3-year prospective study reported a reduction in average days of hospital stay from 25.
 04 (12 months pre-DBT) to 4 (12 months DBT) and 1.09(12 months from completion of DBT).
04 (12 months pre-DBT) to 4 (12 months DBT) and 1.09(12 months from completion of DBT). - Bassington & Krawitz (2006) reported on a DBT study in a psychiatric hospital. The authors noted a decrease in the number of days of stay in the hospital from 3.42 during the 6 months before the start of the DBT course to 1.2 during the 6 months of therapy.
- Linehan et al (2006): DBT was superior to expert-led eclectic therapy in most measures. During the year of therapy, a significantly lower number of patients in the DBT program, compared with conventional therapy, were hospitalized in a psychiatric hospital (DBT -19.6%, conventional psychotherapy - 48.9%), including those hospitalized due to suicidal thoughts (9.8% and 35.6%, respectively).
- Prendergast & McCausland (Australia, 2007) reported a reduction in the average number of days of hospital stay during the 6 months before and during a DBT course from 6.09 to 1.73.
- McMain et al (2009): DBT and general mental health care showed similar efficacy across most parameters.
 However, in the DBT group, there was a decrease in the number of days spent in the hospital during the last 4 months of 12 months of therapy compared with 4 months before treatment (10.52 days to 3.73 days). nine0024
However, in the DBT group, there was a decrease in the number of days spent in the hospital during the last 4 months of 12 months of therapy compared with 4 months before treatment (10.52 days to 3.73 days). nine0024 - Carter et al (2010) showed a 33% reduction in psychiatric hospital admissions in the DBT group compared with standard care. The number of days in the hospital is not given, the duration of hospitalizations did not differ significantly.
- Carter et al. (2010) in a 6-month randomized controlled trial showed that outpatient DBT resulted in a non-significant but larger reduction in hospital admissions compared to standard therapy (0.61 psychiatric hospital admissions per patient per 6 months of therapy compared with 0.91 for conventional therapy; for a non-psychiatric (somatic) hospital, the corresponding values were 0.5 and 1.4).
- Williams et al. (2010) reported that participation in the 20-week DBT skills training group resulted in a significant reduction in the number of days spent in hospital during treatment (from 2.
 79 to 0.57), with the patients with the most active inpatient care having the most decrease in indicators (from 16.18 to 1.36 days). The achieved improvement was maintained for 6 months after the end of the course (decrease from 17.56 to 3.33 days, p=0.06). nine0024
79 to 0.57), with the patients with the most active inpatient care having the most decrease in indicators (from 16.18 to 1.36 days). The achieved improvement was maintained for 6 months after the end of the course (decrease from 17.56 to 3.33 days, p=0.06). nine0024 - Pasieczny & Connor (2011) showed that patients treated with a 6-month course of DBT in the Australian public health system had a significant reduction in the number of days spent in hospital compared to waiting list and standard care (2.23 versus 13.6 days) with a comparable initial number of hospital days in both groups.
Economic efficiency of DPT
- American Psychiatric Association (1998) reported a reduction in treatment costs of $26,000 per patient per year with DBT compared to the previous year ($20-46,000), a 77% reduction in hospital days, a 76% reduction in day care days, days in the intensive care unit by 56%.
- Linehan and Heard (1991, 1999) reported that DBT resulted in an average reduction of $9,000 per patient per year.
- A Swedish study [Perseius, 2004] showed a reduction in therapy costs of $17,000 per patient per year of DBT compared to the previous year. Comparison of treatment costs per month before DBT and 18 months from DBT initiation shows a cost reduction of $6,000/patient ($8,000 and $2,000, respectively). nine0024
- Prendergast and McCausland (2007) showed in an Australian public health study that the reduction in hospital admissions with DBT resulted in a reduction in pre/post 6-month DBT treatment costs of A$4,501 per 6 months per patient.
- Paisieczny and Connor (2011) in an Australian sample showed a reduction in treatment costs of A$5,927 per patient over a 6-month follow-up period when comparing DBT and standard care (Total cost of care was A$12.196 and A$18,123 respectively).
- Amner (2012), in a Welsh public mental health service study: a prospective study in Wales showed a reduction in total health care costs of £1,741 in the year following completion of a DBT course, compared with 12 months prior to treatment, in primarily due to a 20% reduction in the cost of hospital treatment.
http://behavioraltech.org/downloads/Research-on-DBT_Summary-of-Data-to-Date.pdf
http://www.nrepp.samhsa.gov/ViewIntervention.aspx?id=36
http://www.psychosocial.com/IJPR_15/DBT_Evaluation_DeVylder.html
http://behavioraltech.org/downloads/Financial-Cost -Effectiveness-DBT.pdf
Borderline personality disorder: signs, test, therapy
Some name
learned a lot
Author profile
My name is Sasha, I am 23 years old. I have borderline personality disorder and a couple of other psychiatric diagnoses.
I spend about 16,000 R per month on mental health. In this article, I will tell you what this money goes for, how this spending helps me feel better, and what services I manage to save on. nine0003
Beware!
The text describes scenes of violence and self-harm. If you are not in a stable psychological state right now, do not read this article.
My signs of a personality disorder
When I called the psychological support center to find a therapist, I was asked to indicate what kind of destructive behavior I have. Center staff listed six items as examples: binge eating, suicidal behavior, impulsive behavior, alcohol or drug use, and promiscuity. I answered: "All of the above." nine0003
Center staff listed six items as examples: binge eating, suicidal behavior, impulsive behavior, alcohol or drug use, and promiscuity. I answered: "All of the above." nine0003
I already knew then that I had borderline personality disorder, but I had not yet found a way to live with it. Doctors offered ineffective treatment regimens, and relatives blamed my character for all the problems. They can be understood: from the outside, I am a sweet and shy girl with a thin voice, who almost never argues with anyone. It is difficult for others to imagine and understand what storms are happening inside me.
Go see a doctor
Our articles are written with love for evidence-based medicine. We refer to authoritative sources and go to doctors with a good reputation for comments. But remember: the responsibility for your health lies with you and your doctor. We don't write prescriptions, we make recommendations. Relying on our point of view or not is up to you. nine0003
Anxiety and social phobia. I have been hypersensitive since childhood and have always had difficult relationships with others. It started in kindergarten, and at school it only intensified. It was difficult for me to respond in class and take initiative. I was often given bad grades, and I got used to looking at myself through the eyes of disgruntled teachers. Then I did not realize that I had increased anxiety and social phobia, and these qualities greatly influenced my behavior. The worse my grades were, the scarier it was to answer and go to class. The way out seemed to be behavior for which schoolgirls are usually condemned. While my classmates were playing catch-up during breaks, I drank beer with high school students in the hallways. nine0003
I have been hypersensitive since childhood and have always had difficult relationships with others. It started in kindergarten, and at school it only intensified. It was difficult for me to respond in class and take initiative. I was often given bad grades, and I got used to looking at myself through the eyes of disgruntled teachers. Then I did not realize that I had increased anxiety and social phobia, and these qualities greatly influenced my behavior. The worse my grades were, the scarier it was to answer and go to class. The way out seemed to be behavior for which schoolgirls are usually condemned. While my classmates were playing catch-up during breaks, I drank beer with high school students in the hallways. nine0003
I made several attempts to take up my studies, but never found enough support. When I did a good job, the teachers gave me bad grades out of inertia - they were sure that I had cheated. And sometimes my grades were lowered due to very minor shortcomings. These events caused me a storm of emotions and devastated me. I hated myself and other people. I constantly felt aggression, anger, fear.
These events caused me a storm of emotions and devastated me. I hated myself and other people. I constantly felt aggression, anger, fear.
Self-damaging behavior. At some point, I started damaging my body. It was a universal way to punish yourself, reduce the intensity of emotional experiences about your own worthlessness and feel alive. nine0003
Self-injurious behavior does not always indicate a desire to die, it is often a distraction.
When a person is physically injured, endorphin is released - a hormone that reduces pain and improves emotional state. I pierced my lips with a sewing needle several times when I became unbearably lonely and hurt. I cut my hands in a bath under hot water - this distracted me from suffering and negative thoughts. I did not pay attention to all the new scars and blood streams. This method of distraction quickly became a habit. nine0003
In parallel with this, bulimia developed - periods of uncontrolled overeating alternated with long hunger strikes. The fact that I endured long periods without food gave me a feeling of confidence in my appearance and even superiority. But even this did not help when I had to communicate with someone or some important event. I was so anxious that bouts of diarrhea happened 4-5 times in a row an hour before leaving the house. The thought of going to the school toilet made me even more anxious. nine0003
The fact that I endured long periods without food gave me a feeling of confidence in my appearance and even superiority. But even this did not help when I had to communicate with someone or some important event. I was so anxious that bouts of diarrhea happened 4-5 times in a row an hour before leaving the house. The thought of going to the school toilet made me even more anxious. nine0003
/eating-disorders/
How to cure eating disorders
Dissociation. In the eleventh grade, I started a relationship with a 21-year-old boy. One of the symptoms of borderline disorder is dissociation from one's body or personality. It is difficult for me to express my attitude to something and it often seems that events do not happen to me.
Only years later did I realize that this relationship was destructive to my psyche. Once that guy raped me for seven days in a row, and I thought it was my own fault. Later I realized that insecure people repel many people, but they are convenient for abusers. nine0003
nine0003
Over time, my condition stabilized. Sooner or later I left people who negatively affected my psyche. My parents supported me, and besides, I had friends who did not turn away from me. I managed to enter the university in philology and successfully complete my studies. It was very difficult: I was almost always depressed and suffered from bulimia. Fortunately, in the last year she went into remission.
Although my condition has improved over time, the typical features of borderline personality disorder are still with me. I often experience strong unreasonable anger, immerse myself in difficult memories, conflict with people, do not fully understand who I am and what I feel. My condition is changing rapidly and unpredictably. The path from endless love to hatred for a person can take one hour. nine0003
Problems with professional identity. But, of course, borderline disorder is not only about communication problems. I also have issues with my professional identity. Until recently, I have never worked in my profession, I have not stayed at any job for more than six months. I have never had stability in anything: neither in salary, nor in the amount of food and alcohol, nor in relationships. It is very difficult for me to find a balance in life, and not every psychologist can help me with this. nine0003
Until recently, I have never worked in my profession, I have not stayed at any job for more than six months. I have never had stability in anything: neither in salary, nor in the amount of food and alcohol, nor in relationships. It is very difficult for me to find a balance in life, and not every psychologist can help me with this. nine0003
Time once wrote that psychologists fear borderline disorders the most and many have no idea how to treat them. As psychologist Marsha Linehan noted, people with this disorder are analogous to patients with third-degree burns. They simply do not have an emotional skin, and even the slightest touch or movement causes them unimaginable suffering. However, there are already ways to alleviate their condition with proven effectiveness.
This is how my adaptation journey began. nine0003
Borderline Tests
Advanced Borderline Personality Test. Includes 50 questions.
More capacious test from bipolar.su, 20 questions.
Pinfo self-assessment test, 20 questions.
Remember that test results cannot be used to make a diagnosis. Contact a psychiatrist.
How I tried to solve the problem
I put off going to a psychotherapist for a long time. On the one hand, I doubted that my problems were significant, on the other hand, I was afraid that the doctors would see my hands and take me to a mental hospital. I always asked not to call an ambulance when my friends were bandaging my fresh cuts. nine0003
But while studying at the university, in the winter of 2019, I became very ill, I stopped leaving the house, talking to people and could not prepare for the session. I tried to cheer myself up with at least food: I had an attack of compulsive overeating. In four months, I gained 14 kilograms.
The first psychotherapist. Together with my mother, I went to a psychotherapist, who was advised to her. He talked first with me, and then with my mother. The conversation was pleasant, I was not examined or weighed. Mom was told that, in general, everything was not so bad and the specialist did not see a suicidal mood. Although, as I learned later, the risk of suicide cannot be predicted in the case of an individual patient. The antidepressant that I was prescribed, I stopped taking after a month. I did not tell the doctor everything and did not trust his recommendations. nine0003
Mom was told that, in general, everything was not so bad and the specialist did not see a suicidal mood. Although, as I learned later, the risk of suicide cannot be predicted in the case of an individual patient. The antidepressant that I was prescribed, I stopped taking after a month. I did not tell the doctor everything and did not trust his recommendations. nine0003
/psychotherapy-search/
How to choose a psychotherapist
The second psychotherapist is in the district PND. It wasn't until a year later that I decided to start regular psychotherapy. Then I lived in Minsk and applied to the district psycho-neurological dispensary. It was possible to visit a doctor for free, but the nurse warned me: then there could be problems with employment and obtaining a driver's license. I knew that theoretically, in my case, such problems should not arise, but in practice, unpleasant stories still happen. All risks can be avoided if you go to consultations anonymously, that is, for a fee. One consultation in translation into Russian currency cost me 500 R.
At that time, I had a very poor idea of what psychotherapist consultations should be like, so I did not immediately understand that something was wrong. Our sessions were held in an office in which a nurse sat all the time. One day, when I was talking to a therapist, she suddenly laughed. Another time, a nurse came into the office, unable to set up her phone, and everyone rushed to help her. I was too stiff to talk about my dissatisfaction and continued to walk and renew my prescription for antidepressants. nine0003
At some point, I told the psychotherapist that I got a job as a cleaner, and he corrected me: “That is, a cleaner.” After that, I did not appear in his office. In total, these consultations lasted four months, I spent about 8000 R.
/worst-therapy-session/
“After the session I was crushed and killed”: 5 signs of bad psychologists
The third psychotherapist. On the recommendation of a friend, I found another specialist - a Gestalt psychotherapist. He also received in a state institution, but even there it was possible to remain anonymous if consulted for a fee. In addition, the sessions were also inexpensive - about 1000 R. I continued to drink the antidepressant prescribed by the previous therapist. The new specialist did not correct this drug treatment in any way, although he did not notice significant changes in my behavior. nine0003
Symptoms of bipolar disorder
At some point, I realized that I had become unusually active: I got a lot of work, spent all my time in the office and in the gym, experienced brutal hunger, and also began to behave risky - I began to erratic sexual relations with strangers. Later, I learned that this state of high spirits, constant risk and excessive activity is called hypomania, and I have another diagnosis - bipolar disorder of the second type. nine0003
This is a disorder in which a person's life is subject to cycles of depressions and hypomanias - states when there is euphoria, an abnormally high level of energy and mood. Hypomania is often accompanied by risky behavior, difficulty concentrating, and increased irritability. In type 2 bipolar disorder, during hypomania, a person does not lose touch with reality, but episodes of depression are long and severe.
Hypomania is often accompanied by risky behavior, difficulty concentrating, and increased irritability. In type 2 bipolar disorder, during hypomania, a person does not lose touch with reality, but episodes of depression are long and severe.
/bipolarnoe-rasstroystvo/
How much does it cost to treat bipolar affective disorder
In a state of hypomania, people often do not understand that something is wrong and do not turn to a specialist. It seems that everything is in order, and if you do something spontaneous or stupid, you accept your actions simply and without suspicion.
When the hypomania passed and the high spirits, the enjoyment of life and energy began to change into opposite states, I decided that I needed to find a new psychiatrist and stop antidepressants under his supervision. It seemed to me: if I feel so bad, it means they don’t work. nine0003
What the psychiatrist prescribed for me
Then I had already moved to Moscow and turned to a psychiatrist from the Mental Health Center.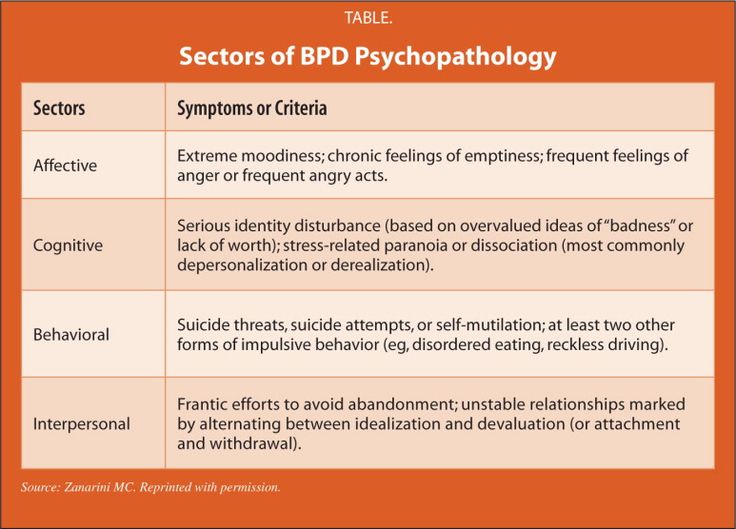 One consultation cost 6000 R.
One consultation cost 6000 R.
The psychiatrist listened to my story and made three diagnoses: eating disorder, borderline personality disorder and bipolar disorder. She completely changed my treatment by adding mood stabilizers, drugs that stabilize mood. She also reduced the dosage of the antidepressant, which she soon had to stop taking altogether. The last one was a big mistake. nine0003
/list/psychiatric-drugs-russia/
What will happen to medicines in Russia: we analyze 5 groups of psychiatric drugs
A certificate issued by a psychiatristTwo weeks after I stopped taking them, I felt as bad as ever. Sessions with a Gestalt therapist didn't help at all. It was very difficult to talk, with great difficulty I got to the clinic for an appointment with a psychiatrist - I had no strength, desire, faith at all.
Then the psychiatrist changed my treatment regimen again and said, “I strongly recommend changing therapists and trying DBT. Otherwise, you can look for another psychiatrist.” nine0003
Otherwise, you can look for another psychiatrist.” nine0003
What is DBT
Dialectical Behavioral Therapy, or DBT, is a form of Cognitive Behavioral Therapy that is similarly focused on working with destructive beliefs and replacing them with more beneficial ones. It was created in the 1980s by psychologist Marsha Linehan, who herself suffers from borderline personality disorder. DBT is now used for a wide variety of problems, but it is still considered effective for people at high risk of suicide.
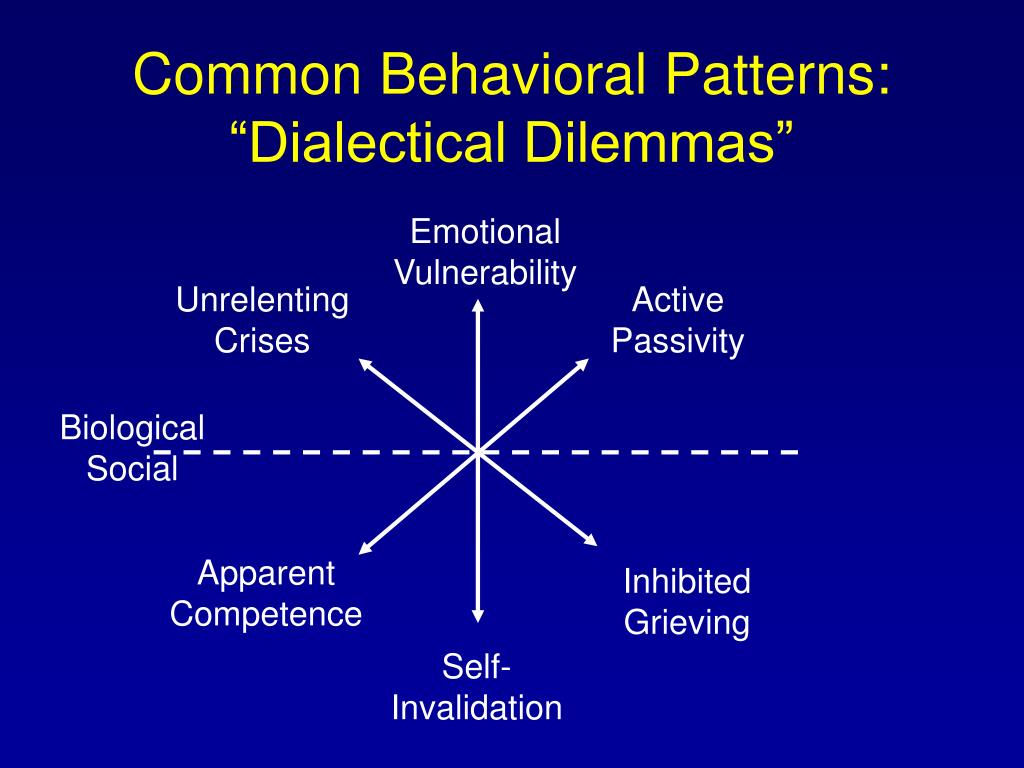
DBT assumes that people with borderline personality disorder lack important interpersonal skills, self-regulation, inadequate response to stress, distorted perception of the world, and black-and-white thinking. The purpose of such therapy is to teach a person to find emotional balance and independently regulate their condition in difficult moments. nine0003
/live-prl/
How I live with borderline personality disorder
The word "dialectical" means that DBT is simultaneously working on two seemingly opposite goals: acceptance of one's problems and behavior change.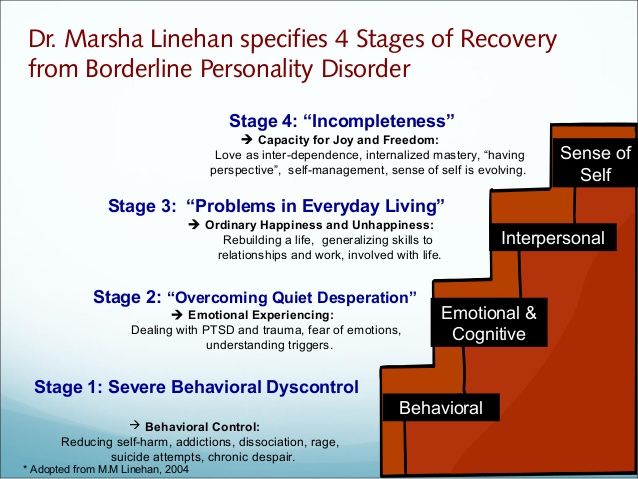 This can be expressed as follows: the therapist helps a person understand and accept his characteristics, but at the same time indicates that his skills can be improved. Another distinctive feature of this therapy is the practice of mindfulness. They are used as a key component in it. nine0003
This can be expressed as follows: the therapist helps a person understand and accept his characteristics, but at the same time indicates that his skills can be improved. Another distinctive feature of this therapy is the practice of mindfulness. They are used as a key component in it. nine0003
There are already many studies confirming the effectiveness of DBT in borderline personality disorder. It reduces the risk of suicide and the number of episodes of self-harm.
DBT cannot be called a treatment for borderline disorder because there is no cure, but this approach helps to learn to live with such features. According to a German study, 77% of patients with this disorder no longer fit the description of the diagnosis after a year of DBT therapy.
Basic assumptions DBT
An assumption is an idea that is difficult to test, but is taught to be accepted in therapy as true. Here are the assumptions in DBT:
- People do the best they can. If you were offended, this does not mean that the person wanted to hurt.
 Through his words, he tried to show his concern and help, but he could not do it right.
Through his words, he tried to show his concern and help, but he could not do it right. - People strive for the best. And this is our common quality.
- Each of us needs to try harder and increase our motivation to change. If you don't make an effort, life won't get better. nine0024
- Even if a person is not to blame for his problems, he will still have to solve them. This means that you need to change your behavior and adapt.
- New behaviors need to be taught in the right contexts. Skills should be applied where they are needed, not just in training.
- Any behavior, thoughts, emotions have a reason. Even if we don't know them.
- Identifying and changing the causes of unwanted behavior works better than judging and blaming.
How I was looking for a DBT group
I was looking for both an individual DBT therapist and group sessions. With the therapist it turned out relatively quickly. I turned to a specialist who was recommended to me by a psychiatrist. One consultation costs 4000 R — at first it seemed to me that it was expensive. But with this therapist, I feel changes and progress.
One consultation costs 4000 R — at first it seemed to me that it was expensive. But with this therapist, I feel changes and progress.
4000 R
I pay for one consultation with a DBT therapist
The group did not work out at first. After moving to Moscow, I was lonely. I am a misanthrope and a sociophobe, but I still need close and trusting relationships with the right people for me. The group helps not only to get along with yourself, but also to find a circle of like-minded people who will not need to explain how you live. nine0003
The psychiatrist recommended that I look at the website of the Russian DBT community. There you can find a list of teams with practicing therapists from different cities, the names of specialists and their contacts. I sent a newsletter to all teams from Moscow. I was told that in one of them a place would become vacant in a few months and it would be possible to join the group.
List of teams on the website of the Russian DBT community.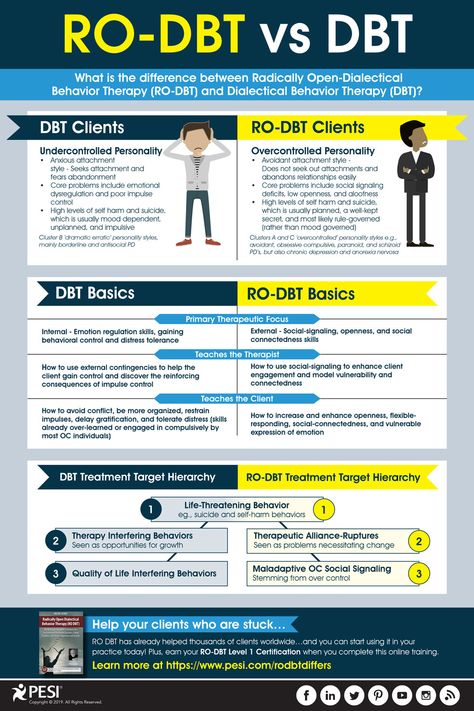 You can try to join them
You can try to join them In parallel, I tried to look for a group through the center where I see a psychiatrist. The clinic was already familiar and not as scary as a new place and new people. I applied several times, but, unfortunately, there were no free places. It was possible to sign up for the waiting list, but it is not known how long you will have to wait. nine0003
The next option is the well-known platform b17.ru, but there I did not find any options suitable for me. Perhaps because I am too biased towards others.
You can have group DBT therapy at Psychiatric Clinical Hospital No. 4. I tried to get into the group, but at that time the waiting list was under 100 people.
I kept googling the right place, but to no avail. It's much easier to find groups for other issues: eating disorders, addictions, social interactions, and more. And this can be understood - far from all specialists can work with "border guards". nine0003
In order not to start my condition, I decided to contact the Sunday BAD support group for people with bipolar disorder. The meeting costs 300 R, it is very budgetary and convenient - you can attend both online and offline in different cities. But unfortunately, I didn’t get along with the group. When I told my story, another participant wrote in the chat: “She talks for so long, I’ll fall asleep right now))”, and then added in a voice that she didn’t like my monologue. For someone it would be a trifle, but not for me. nine0003
The meeting costs 300 R, it is very budgetary and convenient - you can attend both online and offline in different cities. But unfortunately, I didn’t get along with the group. When I told my story, another participant wrote in the chat: “She talks for so long, I’ll fall asleep right now))”, and then added in a voice that she didn’t like my monologue. For someone it would be a trifle, but not for me. nine0003
People with borderline disorder have very poor self-esteem. It depends a lot on other people's opinions. Such a harsh statement shocked me and devalued my experience and feelings. The shame of criticism and the paralyzing powerlessness of it has always made me consider my life a misunderstanding. The organizers of the group supported me, but I could no longer engage in it.
/prl/
How much does the treatment of borderline personality disorder cost? Subscribers there organize support trainings themselves, without a specialist. At first I did not dare to try, although after a few months I realized that this was the best format for me.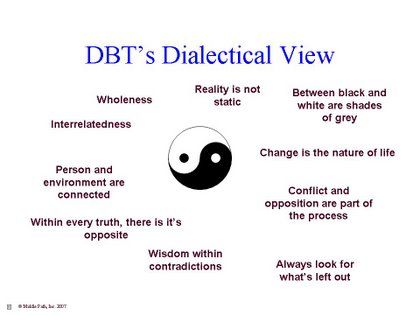 nine0003
nine0003
Cost of DBT therapy in Moscow
| Class type | Cost |
|---|---|
| DBT groups in private clinics | 10,000—12,000 R per month |
| Individual DBT Therapist | 1000-10 000 R per session |
| DBT groups in Psychiatric Hospital No. 4 | 1000-3000 R per meeting |
| DBT group with chat participants without therapist | 1000-1200 R per month for renting an office |
type of classes
Cost
DBT groups in private clinics
10 000-12 000 r for a month
Individual DBT-therapist
1000-10 000 R per session
DBETT-Dbtte groups in Psychiatric Hospital No. 4
1000-3000 R per meeting
DBT group with participants from the chat without a therapist
1000-1200 R per month for office rent
What else you need to know about borderline personality disorder
Kirill Sychev
psychiatrist and psychotherapist
Diagnosing borderline personality disorder is often difficult.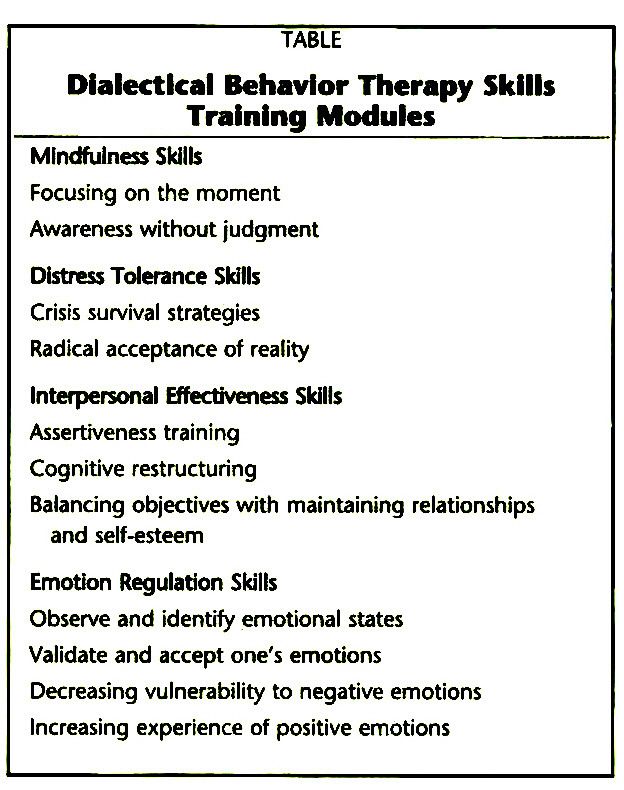 Usually we observe a person for several months before making such a diagnosis. Most of the symptoms don't show up on the outside, they're on the inside: unstable self-esteem, unstable intense relationships, great fear of avoiding abandonment. You can recognize suicidal behavior or thoughts, constant and frequent mood changes, but this happens in many other conditions. nine0003
Usually we observe a person for several months before making such a diagnosis. Most of the symptoms don't show up on the outside, they're on the inside: unstable self-esteem, unstable intense relationships, great fear of avoiding abandonment. You can recognize suicidal behavior or thoughts, constant and frequent mood changes, but this happens in many other conditions. nine0003
One of the biggest challenges in working with a person with borderline personality disorder is that it does not respond well to medication. Most often, they are used sparingly to relieve specific symptoms. For example, for anxiety - antidepressants. Mood stabilizers and antipsychotics are also prescribed. Otherwise, significant effects must be achieved with the help of psychotherapy.
For psychotherapy in this case, quite a lot of different steps and formats of work are used. DBT therapy has the highest efficiency: in the course of it, a person develops the skills of awareness, stress tolerance, building interpersonal relationships, and emotional regulation.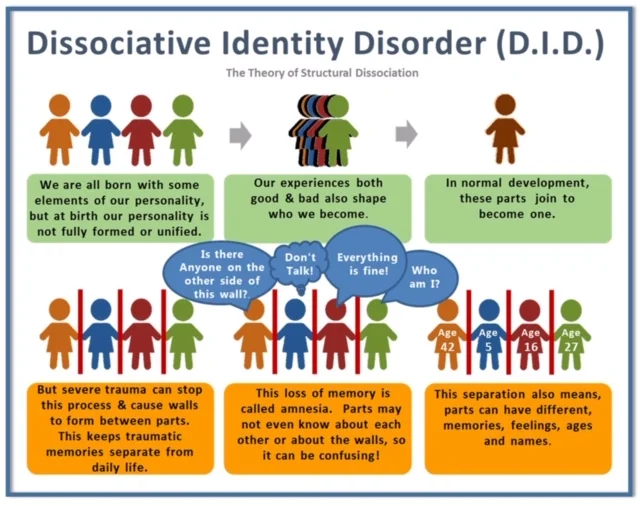 At the same time, all therapy for people with borderline disorder should take place in different formats: calls in crisis situations to get a brief consultation, individual therapy and group therapy. All these formats must be combined, which greatly complicates the process. As a rule, several specialists are required to correct borderline disorder. nine0003
At the same time, all therapy for people with borderline disorder should take place in different formats: calls in crisis situations to get a brief consultation, individual therapy and group therapy. All these formats must be combined, which greatly complicates the process. As a rule, several specialists are required to correct borderline disorder. nine0003
If a person receives multilateral assistance and his relatives support him, then very significant results can be achieved even in six months. But of course, in most cases, no one is treated this way, and therapy can last several years until a person learns to somehow regulate his conditions. It is difficult to name the average duration of therapy - everything is very individual.
If a person with a disorder does not receive help at all, then by the age of 40-50 he can gradually adapt to his condition and learn to build relationships, but this does not always happen. This requires a lot of human effort. nine0003
For a loved one with borderline personality disorder, it is important, on the one hand, not to be too intrusive, not to force — because this can cause a backlash.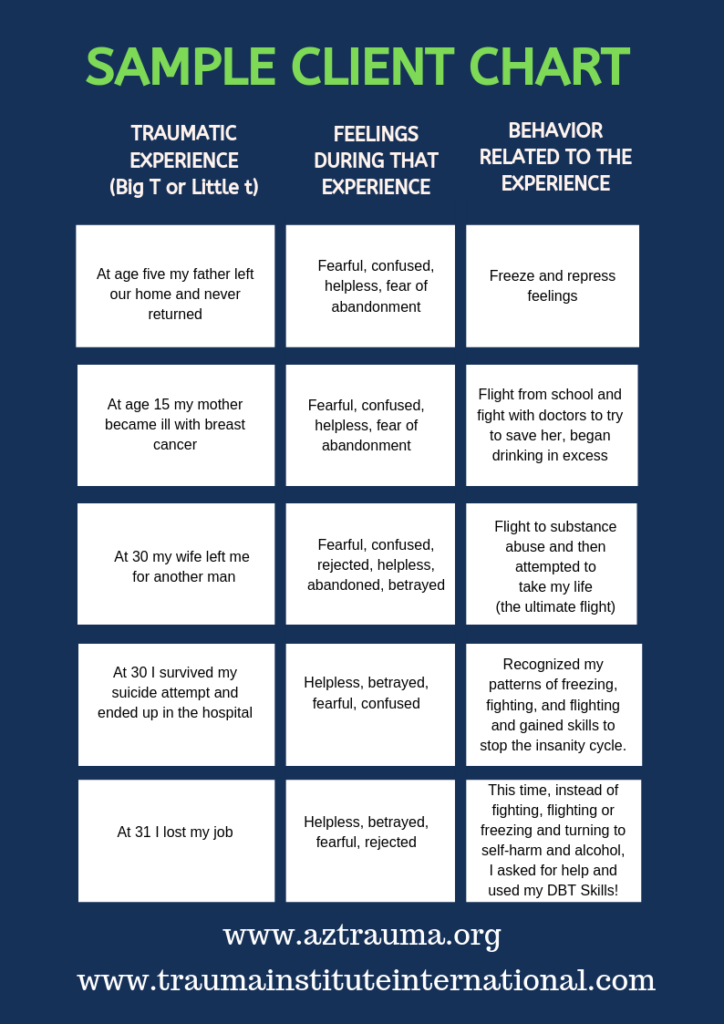 On the other hand, it is important for them to be ready to help in the psychotherapeutic process: to be together, to do exercises together. Also, everyone should discuss everything in detail: it often happens that people with borderline disorder have difficulty building any kind of relationship, and when they try to explain how to live, this leads to additional conflict. This should be avoided. nine0003
On the other hand, it is important for them to be ready to help in the psychotherapeutic process: to be together, to do exercises together. Also, everyone should discuss everything in detail: it often happens that people with borderline disorder have difficulty building any kind of relationship, and when they try to explain how to live, this leads to additional conflict. This should be avoided. nine0003
If you suspect that you have borderline personality disorder, the first thing to do is to see a psychiatrist. And then, if a psychiatrist makes or suggests such a diagnosis, undergo DBT therapy.
How I got started in the DBT group
First, I chose a group from the Russian DBT community, in which they promised a free place in a few months.
The traditional DBT group course lasts 24 weeks. In groups of six to ten participants. Before joining, you need to meet with the therapist several times. The first meeting is introductory and free, where you talk about yourself, your request and diagnosis.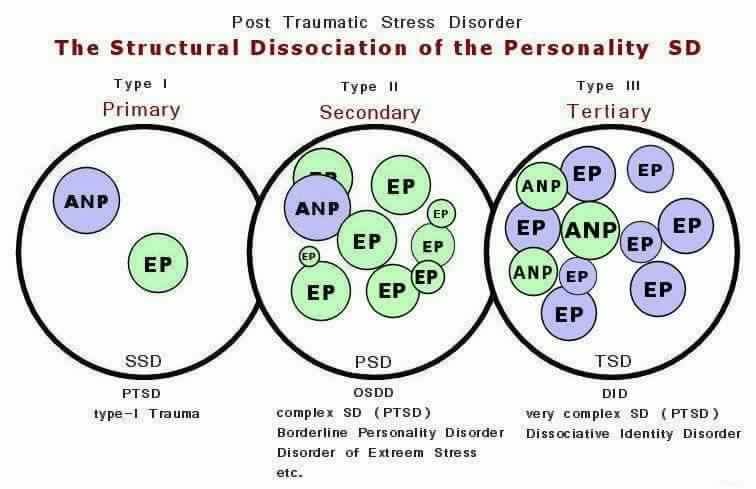 It also tells about the structure of the training sessions, the cost and frequency of meetings, and answers the questions that have arisen. Skills training takes place every week, costs 10,000 R per month and is paid up front to encourage participants to attend. nine0003
It also tells about the structure of the training sessions, the cost and frequency of meetings, and answers the questions that have arisen. Skills training takes place every week, costs 10,000 R per month and is paid up front to encourage participants to attend. nine0003
The second and third meetings are preparatory pre-trainings for participants. The first pre-training is carried out individually: they tell the rules, observe the reaction to real life examples, clarify the request and goals again. He walked for two hours and cost me 3500 R. To be honest, I didn’t like him: the lead therapist needed him more to protect himself and my potential accomplices. I was very sorry to spend this money.
The second pre-training took place with other participants and cost 2500 R. It was dedicated to mindfulness skills. We were taught how to nonjudgmentally observe our reactions, focus on the present moment, and how to balance the emotional and the rational: not be too judgmental or mood dependent.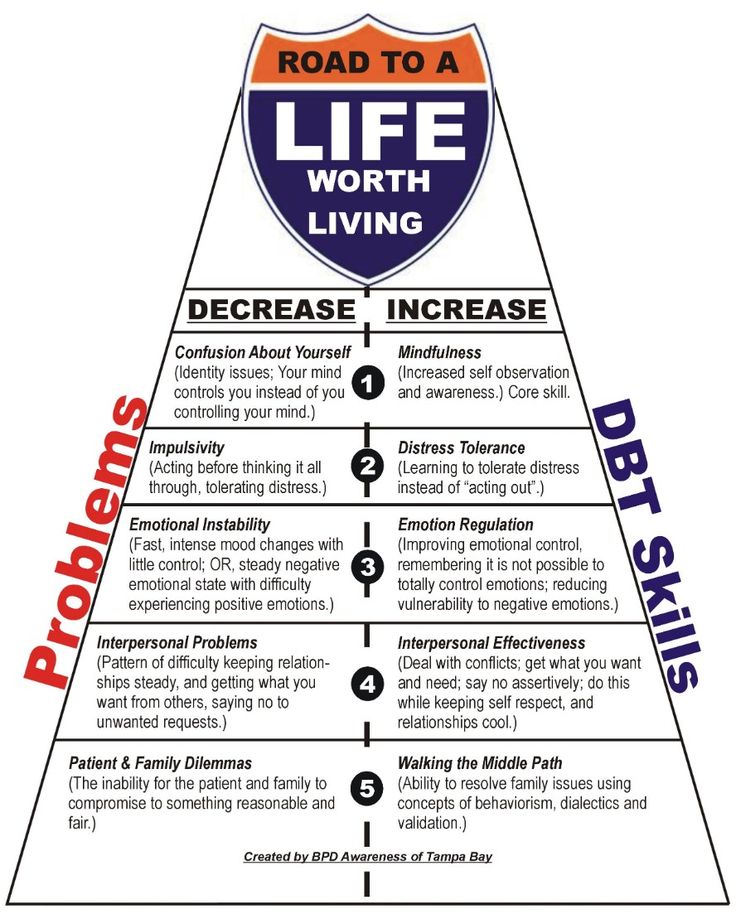 Here, too, I was dissatisfied. The proposed practices did not suit me specifically. Plus, it looked like half of the participants were forced to come to the training. They were uninitiated and did not start talking until their name was called. nine0003
Here, too, I was dissatisfied. The proposed practices did not suit me specifically. Plus, it looked like half of the participants were forced to come to the training. They were uninitiated and did not start talking until their name was called. nine0003
I also didn't feel connected to the therapists. They spoke excessively politely and were emphatically careful in their expressions. This made me feel like I was being suspected of something, and they were also checking my level in a game called Frontier Life.
I decided to leave this group and try the trainings that people with borderline disorder organize themselves. There is no trainer-psychotherapist in such a group, the group member acts as the leader. Each lesson this role passes to another participant. I impulsively joined the first group that came across - I wanted to start practicing my skills as soon as possible. nine0003
The first experience was not very successful. The meetings were held online, almost no one had experience in training.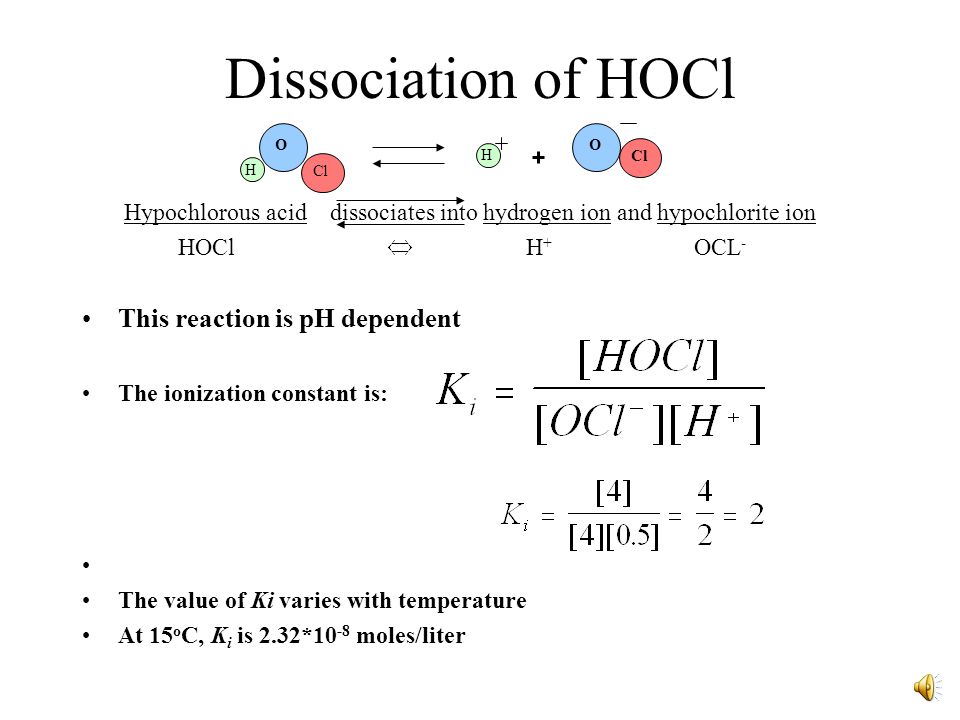 The structure was blurry and stretched. Each meeting, different participants joined us, so we had to spend part of the time on repeated acquaintances. It was impossible to gather everyone on the same day, determine the host and co-host and be sure that they would prepare and come to the meeting.
The structure was blurry and stretched. Each meeting, different participants joined us, so we had to spend part of the time on repeated acquaintances. It was impossible to gather everyone on the same day, determine the host and co-host and be sure that they would prepare and come to the meeting.
Fortunately, this experience did not dissuade me from the benefits of group therapy. One day, a message came to the chat of people with borderline disorder that new people were being recruited to the offline group to fill the vacant seats. I wrote and soon arrived for the meeting. A clear structure has already been established in this group. The participants passed the first round in six months and now they were going through the second one. Communication in the group was easy and caring: if one participant did not understand something, others shared their example and expressed sympathy, which is always so lacking. nine0003
At that time, I really lacked live communication and new acquaintances, and the group helped to close this need.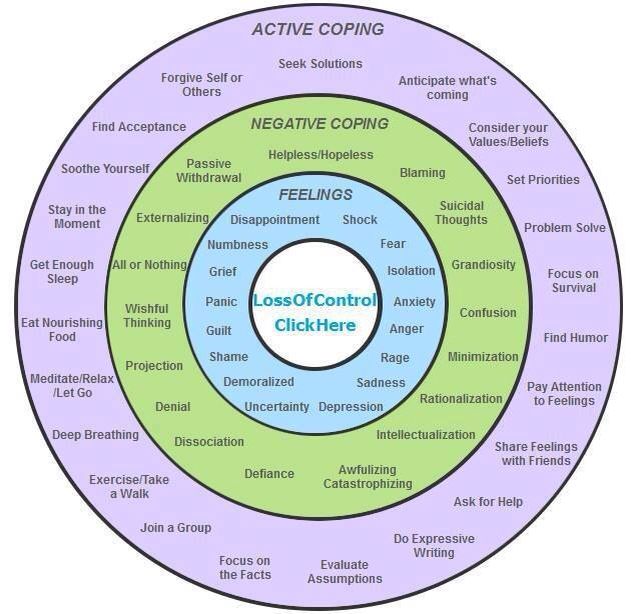 I communicate and move on with those who have similar problems and experiences. No one has ever understood me the way my classmates in skill training did. Instead of the words “why did you do this”, they sympathize with me, offer help and share their insights in such situations. I am in a safe environment and understand that I am not to blame for any of my injuries and have the right to experience any feeling. But this innocence does not relieve me of responsibility, nor does it make me feel like a victim. nine0003
I communicate and move on with those who have similar problems and experiences. No one has ever understood me the way my classmates in skill training did. Instead of the words “why did you do this”, they sympathize with me, offer help and share their insights in such situations. I am in a safe environment and understand that I am not to blame for any of my injuries and have the right to experience any feeling. But this innocence does not relieve me of responsibility, nor does it make me feel like a victim. nine0003
I feel immeasurably relieved when I hear that there is someone who also vomited all day in a row, experienced fear when near a stranger, impulsively left for another city or country, ended up in intensive care and was on the verge of life and death. We share experiences and often joke and laugh, while when a participant needs support and help, we validate his feelings and show tact in expressions.
Working in this group also somewhat reduced my financial anxiety.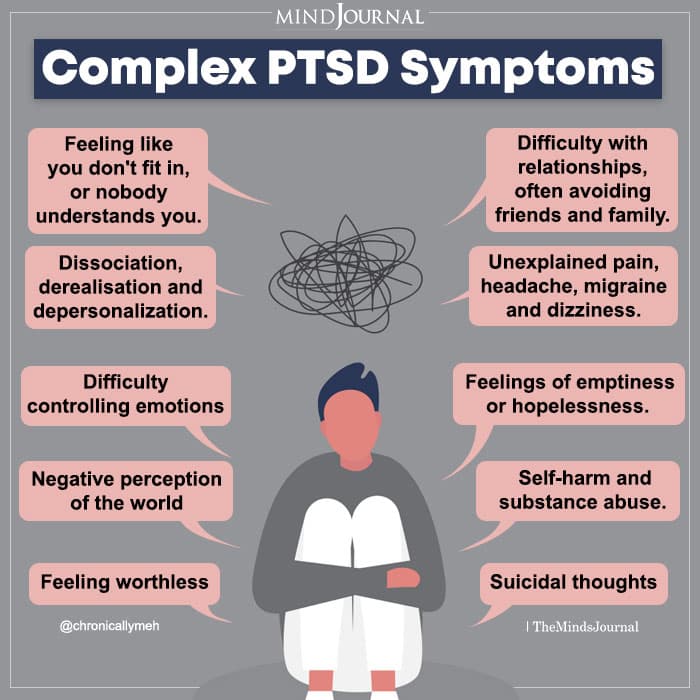 On the recommendation of a psychotherapist, I need to complete two rounds of skills training - this is about a year of classes. If I went to training with a therapist, I would have to spend 126,000 R during this time. Training without a psychotherapist over the same period will cost me approximately 14,400 R. I have to throw off 1,200 R a month - the money goes to rent the premises. nine0003
On the recommendation of a psychotherapist, I need to complete two rounds of skills training - this is about a year of classes. If I went to training with a therapist, I would have to spend 126,000 R during this time. Training without a psychotherapist over the same period will cost me approximately 14,400 R. I have to throw off 1,200 R a month - the money goes to rent the premises. nine0003
The savings of ten times is very significant, especially considering that my expenses for maintaining a psychological state are still high. Now I spend a little over 16,000 R per month on mental health. This amount increases by 6000 R in the months when I need to see a psychiatrist. Plus, spending on drugs can vary a little, now I spend 2000 R per month less on them than before.
I spend annually on mental health 230,400 R
| DBT psychotherapist | 144 000 R |
| Preparations | 48 000 R |
| Psychiatrist | 24 000 R |
| Skills training without a therapist | 14400 Р |
DBT psychotherapist
144 000 R
Preparations
48 000 R
Psychiatrist
24 000 R
Skills training without a therapist
9000 14 400 pWhere am I now and what do I plan to do next
I have been doing DBT therapy for about half a year.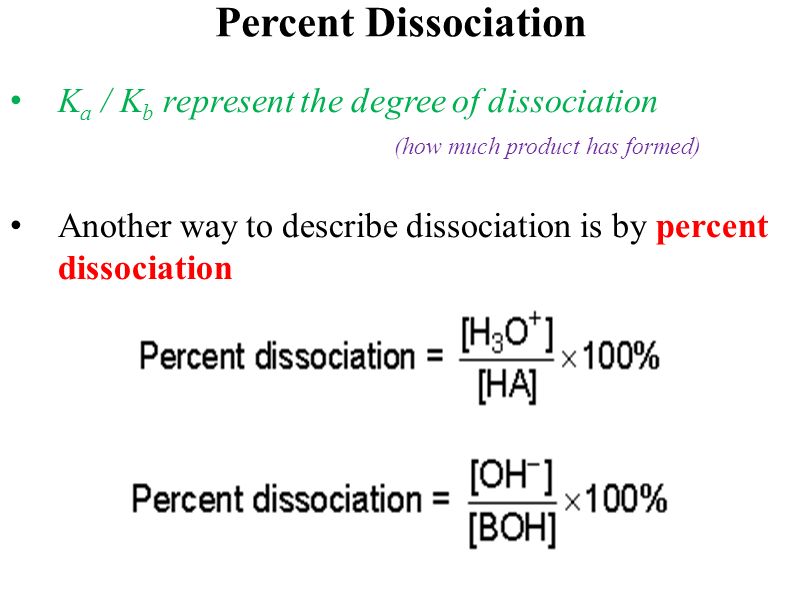 During this time, I became calmer, easier and more interesting with myself. I believe that life can be better than it is now, even though expectations are not always met. I am very pleased that I began to laugh more often - as if I had just learned this reaction.
During this time, I became calmer, easier and more interesting with myself. I believe that life can be better than it is now, even though expectations are not always met. I am very pleased that I began to laugh more often - as if I had just learned this reaction.
But some little things can still piss me off for no real reasons - most often my brain thinks out bad things on its own, because it is so familiar to it. I still perceive reality distortedly and bring my loved ones to tears. But now I more often anticipate possible conflict situations, I have learned to ask for forgiveness and choose adaptive behavior in time. nine0003
Thanks to DBT, I know a relatively quick way to make a choice. This is an exercise in pros and cons. These are the arguments I use when suddenly there is a desire to drink.
For and against example
| Do not take substances - alcohol, drugs, etc. | Take substances | |
|---|---|---|
| For | It's easier - you don't have to do anything Training discipline This will help you become healthier and can be replaced with good habits - for example, sports Long, healthy life Saving money Reason to be proud of yourself | A quick way to reduce stress Maintains a social circle No need to avoid friends and look for new ones You can always shoot and not spend money |
| Vs | Negative thoughts Need to make an effort Ashamed to refuse in front of friends Stress | A pleasure will quickly end Retail expensive disappointment will inevitably worsen health will have to spend time, resources on recovery negatively affects Relations Cunning can kill personality degradation Extra risk of any troubles |
Do not take substances - alcohol, drugs, etc. 0071 Exercise discipline
0071 Exercise discipline
This will help you become healthier and can be replaced with good habits, such as sports
Long, healthy life
Saving money
Reason to be proud of yourself
Against
Negative thoughts
Need to make an effort
Stressful in front of friends
Take substances
For
Quick way to reduce stress
Maintain social circle
No need to avoid friends and seek new ones
You can always “shoot” and not spend money
versus
The pleasure will quickly end
venue
expensive
Disappointment
will inevitably deteriorate health
will have to spend time, resources on recovery
negatively affects the relationship of
Bad habitation
can kill
Degradation of the personality
Shameful
Increased risk of any troubles
What is surprising with psychotherapy, while dealing with one problem, you can immediately solve others.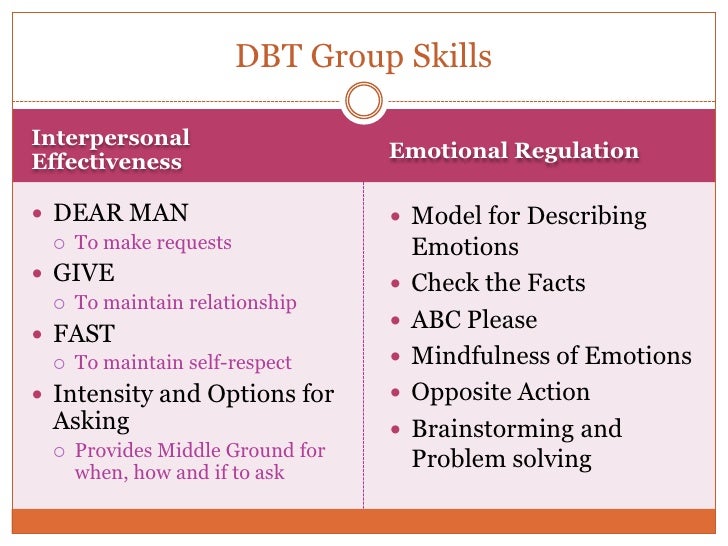 This is what happened with my eating disorder. First, I stopped overeating: I was finally able to eat so much that my brain stopped giving hunger signals. Then I managed to accept the increase in weight: the period of preoccupation with a sculpted flawless body, the division of food into right and wrong, passed. Now I allow myself to eat whatever I want and not weigh myself every day. I strive to do sports only for pleasure, although I still pay attention to unnecessary skin folds, cellulite, visible in light leggings, and the lack of the desired muscle volume on the buttocks. nine0003
This is what happened with my eating disorder. First, I stopped overeating: I was finally able to eat so much that my brain stopped giving hunger signals. Then I managed to accept the increase in weight: the period of preoccupation with a sculpted flawless body, the division of food into right and wrong, passed. Now I allow myself to eat whatever I want and not weigh myself every day. I strive to do sports only for pleasure, although I still pay attention to unnecessary skin folds, cellulite, visible in light leggings, and the lack of the desired muscle volume on the buttocks. nine0003
If a year ago I was most worried about pumping muscles, now it's about building harmonious and trusting relationships, getting rid of obsessive thoughts and starting to earn money with my skills. Of course, I have situations when I lose my temper and experience several emotions at the same time.
To get a sense of how I feel, I open the Handout book for the Dialectical Behavior Therapy training. It contains a detailed description of emotions: what are the variations of a particular emotion, what are its motivating events, how I interpret them, what I feel, how the feeling is expressed and what it can lead to. For example, when I feel jealous, disgust, fear, and shame often go along with it. nine0003 Schema for working with emotions from Dialectical Behavior Therapy by Marsha Linehan, the founder of this approach. The electronic version is sent free to the group members, but I bought myself a paper version
It contains a detailed description of emotions: what are the variations of a particular emotion, what are its motivating events, how I interpret them, what I feel, how the feeling is expressed and what it can lead to. For example, when I feel jealous, disgust, fear, and shame often go along with it. nine0003 Schema for working with emotions from Dialectical Behavior Therapy by Marsha Linehan, the founder of this approach. The electronic version is sent free to the group members, but I bought myself a paper version
After the emotion is identified and realized, it needs to be expressed. If this is not done, it will intensify or transform into another. For example, unexpressed anger can turn into longing and cause depression.
Expression of emotion will alleviate the situation, but will not solve the complex problem. To do this, you need to use the skill of the opposite action or the skill of solving the problem. The first is needed if the emotion is not justified: that is, I am not worried about the fact, but only because of my own interpretation.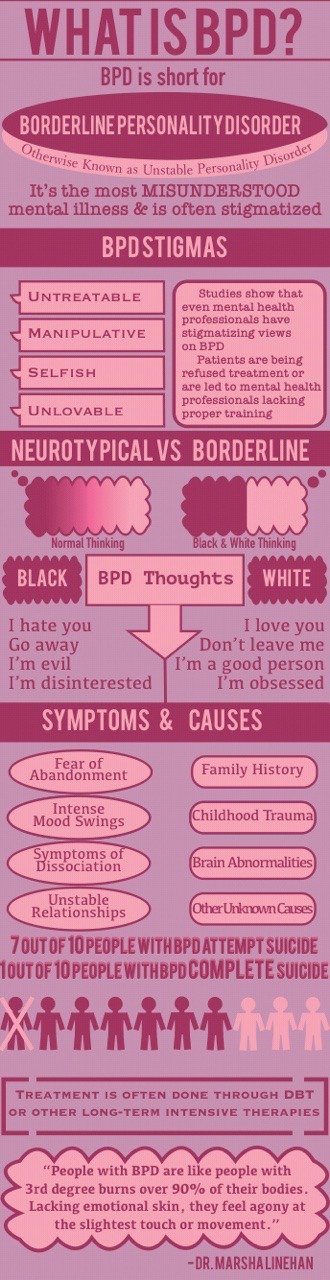 The second is when the problem is objective. nine0003 Schema from the book Dialectical Behavioral Therapy for cases when emotions are overwhelming
The second is when the problem is objective. nine0003 Schema from the book Dialectical Behavioral Therapy for cases when emotions are overwhelming
For example, I broke out at a New Year's party when a girl I didn't know put her hand on my boyfriend's shoulder. My emotion of anger is not substantiated by facts: I was around all the time and exclude the possibility of flirting, I trust my partner, and this girl was not familiar to both of us. Maybe other girls will react calmly if an unfamiliar girl puts her hand on the shoulder of their partner - I don’t know. But for me this is unacceptable. However, in any case, the emotion does not correspond to the facts: no one cheated on me, and I can apply the "Opposite Action" tactic. nine0003
According to the sentences in the table, I need to take a break, understand this girl, come up with a positive rationale for her actions, and do something nice for myself. I did so. When I went to catch my breath, my boyfriend reassured me, and we left in English. It was the best option at that moment.
It was the best option at that moment.
It is much easier for me to live when I feel the support of others. And DBT helps not to push away loved ones, but to strengthen relationships with them.
Of course, new specific problems also appear. For example, at the end of January, I had an appointment with a psychiatrist. My mental picture has changed. Those useful habits that were not there before have been added, but some traits that psychologists call maladaptive have become aggravated: for example, obsessive-compulsive and hypochondriacal. nine0003
Due to the coronavirus, I have become 5-10 times more likely to wash my hands and wipe the door handle where the trash can is with alcohol. I stopped wearing lenses because it constantly seems to have lint in my eyes. And also because of the large number of sexual partners that I had during hypomania, I still worry. I constantly retake tests for sexual infections, but still I continue to regularly suspect something in myself.